Investing in the next generation of medical and research pioneers
Masks strongly recommended but not required in maryland, starting immediately.
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Understanding Clinical Trials
Clinical research: what is it.

Your doctor may have said that you are eligible for a clinical trial, or you may have seen an ad for a clinical research study. What is clinical research, and is it right for you?
Clinical research is the comprehensive study of the safety and effectiveness of the most promising advances in patient care. Clinical research is different than laboratory research. It involves people who volunteer to help us better understand medicine and health. Lab research generally does not involve people — although it helps us learn which new ideas may help people.
Every drug, device, tool, diagnostic test, technique and technology used in medicine today was once tested in volunteers who took part in clinical research studies.
At Johns Hopkins Medicine, we believe that clinical research is key to improve care for people in our community and around the world. Once you understand more about clinical research, you may appreciate why it’s important to participate — for yourself and the community.
What Are the Types of Clinical Research?
There are two main kinds of clinical research:
Observational Studies
Observational studies are studies that aim to identify and analyze patterns in medical data or in biological samples, such as tissue or blood provided by study participants.
Clinical Trials
Clinical trials, which are also called interventional studies, test the safety and effectiveness of medical interventions — such as medications, procedures and tools — in living people.
Clinical research studies need people of every age, health status, race, gender, ethnicity and cultural background to participate. This will increase the chances that scientists and clinicians will develop treatments and procedures that are likely to be safe and work well in all people. Potential volunteers are carefully screened to ensure that they meet all of the requirements for any study before they begin. Most of the reasons people are not included in studies is because of concerns about safety.
Both healthy people and those with diagnosed medical conditions can take part in clinical research. Participation is always completely voluntary, and participants can leave a study at any time for any reason.
“The only way medical advancements can be made is if people volunteer to participate in clinical research. The research participant is just as necessary as the researcher in this partnership to advance health care.” Liz Martinez, Johns Hopkins Medicine Research Participant Advocate
Types of Research Studies
Within the two main kinds of clinical research, there are many types of studies. They vary based on the study goals, participants and other factors.
Biospecimen studies
Healthy volunteer studies.
Clinical trials study the safety and effectiveness of interventions and procedures on people’s health. Interventions may include medications, radiation, foods or behaviors, such as exercise. Usually, the treatments in clinical trials are studied in a laboratory and sometimes in animals before they are studied in humans. The goal of clinical trials is to find new and better ways of preventing, diagnosing and treating disease. They are used to test:
Drugs or medicines

New types of surgery

Medical devices

New ways of using current treatments

New ways of changing health behaviors

New ways to improve quality of life for sick patients

Goals of Clinical Trials
Because every clinical trial is designed to answer one or more medical questions, different trials have different goals. Those goals include:
Treatment trials
Prevention trials, screening trials, phases of a clinical trial.
In general, a new drug needs to go through a series of four types of clinical trials. This helps researchers show that the medication is safe and effective. As a study moves through each phase, researchers learn more about a medication, including its risks and benefits.
Is the medication safe and what is the right dose? Phase one trials involve small numbers of participants, often normal volunteers.
Does the new medication work and what are the side effects? Phase two trials test the treatment or procedure on a larger number of participants. These participants usually have the condition or disease that the treatment is intended to remedy.
Is the new medication more effective than existing treatments? Phase three trials have even more people enrolled. Some may get a placebo (a substance that has no medical effect) or an already approved treatment, so that the new medication can be compared to that treatment.
Is the new medication effective and safe over the long term? Phase four happens after the treatment or procedure has been approved. Information about patients who are receiving the treatment is gathered and studied to see if any new information is seen when given to a large number of patients.
“Johns Hopkins has a comprehensive system overseeing research that is audited by the FDA and the Association for Accreditation of Human Research Protection Programs to make certain all research participants voluntarily agreed to join a study and their safety was maximized.” Gail Daumit, M.D., M.H.S., Vice Dean for Clinical Investigation, Johns Hopkins University School of Medicine
Is It Safe to Participate in Clinical Research?
There are several steps in place to protect volunteers who take part in clinical research studies. Clinical Research is regulated by the federal government. In addition, the institutional review board (IRB) and Human Subjects Research Protection Program at each study location have many safeguards built in to each study to protect the safety and privacy of participants.
Clinical researchers are required by law to follow the safety rules outlined by each study's protocol. A protocol is a detailed plan of what researchers will do in during the study.
In the U.S., every study site's IRB — which is made up of both medical experts and members of the general public — must approve all clinical research. IRB members also review plans for all clinical studies. And, they make sure that research participants are protected from as much risk as possible.
Earning Your Trust
This was not always the case. Many people of color are wary of joining clinical research because of previous poor treatment of underrepresented minorities throughout the U.S. This includes medical research performed on enslaved people without their consent, or not giving treatment to Black men who participated in the Tuskegee Study of Untreated Syphilis in the Negro Male. Since the 1970s, numerous regulations have been in place to protect the rights of study participants.
Many clinical research studies are also supervised by a data and safety monitoring committee. This is a group made up of experts in the area being studied. These biomedical professionals regularly monitor clinical studies as they progress. If they discover or suspect any problems with a study, they immediately stop the trial. In addition, Johns Hopkins Medicine’s Research Participant Advocacy Group focuses on improving the experience of people who participate in clinical research.
Clinical research participants with concerns about anything related to the study they are taking part in should contact Johns Hopkins Medicine’s IRB or our Research Participant Advocacy Group .
Learn More About Clinical Research at Johns Hopkins Medicine
For information about clinical trial opportunities at Johns Hopkins Medicine, visit our trials site.
Video Clinical Research for a Healthier Tomorrow: A Family Shares Their Story
Clinical Research for a Healthier Tomorrow: A Family Shares Their Story

Clinical Trials Versus Clinical Studies: What’s The Difference?

There are varying opinions on what constitutes a clinical study or a clinical trial. According to Good Clinical Practice (GCP) – specifically the ICH E6 guidelines – the terms clinical trial and clinical study can be used synonymously. GCP defines a clinical trial or study as:
“Any investigation in human subjects intended to discover or verify the clinical, pharmacological, and/or other pharmacodynamic effects of an investigational product(s), and/or to identify any adverse reactions to an investigational product(s), and/or to study absorption, distribution, metabolism, and excretion of an investigational product(s) with the object of ascertaining its safety and/or efficacy.”
Others distinguish between clinical studies and clinical trials. The National Institutes of Health (NIH), for example, describes two kinds of clinical study: “A clinical study involves research using human volunteers (also called participants) that is intended to add to medical knowledge. There are two main types of clinical studies: clinical trials (also called interventional studies) and observational studies.”
Observational Versus Interventional
These two main types of clinical study – observational and interventional – describe the approaches taken in each:
- In observational studies, researchers observe study participants and record the effects of their current treatment without making any changes. Observational studies tend to be less involved for participants, who might need to complete questionnaires, for example. Participants will typically be people undergoing treatment for a medical condition, and the researchers will collect information about the results of that treatment without changing it or comparing the results to a control group.
- In interventional studies – clinical trials – an intervention is tested in a group of participants, usually compared to a control group that does not receive the intervention but a placebo in its place. A clinical trial could be testing a potential drug, procedure or device. Clinical trials have evolved over hundreds of years and have a structured framework.
Medicine authorities like the Food and Drug Administration (FDA) in the US or the European Medicines Agency (EMA) in the EU require clinical trials proving the safety and efficacy of a drug before they will allow it on the market. They often then require the company or research institute that developed an approved drug to monitor its safety and efficacy over time through observational studies.
The Clinical Trial: An Important Clinical Research Study

The clinical trial is an intervention study – a specific type of clinical research study that aims to answer a defined question about a treatment. The treatment under investigation could be a new drug, medical device or behavior, for example. The question being posed is usually around the safety or efficacy of the intervention.
A clinical trial is preceded by a long process of preclinical research. First, the intervention is studied in the lab. These tests begin in vitro and often involve toxicity screening. Then they will progress to animals, such as mice or ferrets, for further toxicity and safety testing and to gather initial efficacy results. Animals are needed at this stage, as bodies are much more complex than pure tissues grown in the lab. It’s important to understand the impact of an intervention on various biological systems, such as the nervous and circulatory systems, before the drug is tested in patients.
If an intervention still appears promising after preclinical research, it will enter the five phases of a clinical trial:
- Phase 0 – pharmacodynamics and pharmacokinetics trial on a small number of people
- Phase I – safety trial on a small number of people
- Phase II – efficacy trial with a control versus test group to determine dosage and efficacy
- Phase III – safety and efficacy trial with a large number of people (usually over 1,000)
- Phase IV – continuous monitoring through observation
Understanding Clinical Research
The distinction between types of clinical research study differs depending on who is defining them, and this is an important consideration for those undertaking clinical studies to take a treatment to market. For example, the NIH refers to interventional studies, while the FDA calls them clinical trials. This is the kind of information you can expect a CRO to know.
If you have specific questions about the research you want to undertake, or you’re looking for support with your trial, you can contact Siron Clinical .
STARTING A CLINICAL TRIAL IN THE EU?
Download our RFI to learn more. You'll learn how you can leverage our experience to help you with your clinical trials.
Check your email for the ebook!
Submit a comment cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Submit Comment

Clinical Trials VS Clinical Studies – What’s The Difference?
Clinical trials and studies are sometimes used interchangeably but they are actually different subgroups of clinical research. A clinical trial is a part of a clinical study. Participants in studies and trials agree to participate under the scientists’ or doctors’ guidelines.
If you’re considering clinical research or participating in a clinical trial, it’s a good idea to know what you’re getting into. Let’s take a look at the different between clinical studies and clinical trials.
What is a Clinical Study?
Clinical studies assist researchers and clinicians in understanding medical conditions and treatments. Clinical trials and observational studies are the most popular forms of clinical studies. Both teach doctors and nurses about new pharmaceuticals, devices, surgical procedures, and therapies to treat or prevent patients’ ailments. They also develop diagnostic tools to detect and prevent diseases.
Who Conducts Clinical Studies?
Sponsors finance medical studies. Sponsors include university medical centers, pharmaceutical businesses, volunteers, and federal entities like the National Institutes of Health (NIH and the Department of Defense (DoD). Investors in clinical trials frequently seek new medical insights or possible remedies.
Who Leads a Clinical Study?
Doctors are the principal investigators or leaders of all research investigations. The lead investigator is the head of a research team and the team typically include professionals of varied skill levels like doctors, nurses, social workers, etc. The research is mainly done in hospitals, health facilities, or universities.
Can Anyone Participate in a Study?
The research team follows tight guidelines when setting study conditions. This assures success and that can determine who is allowed to participate in a study. Membership eligibility is based on predetermined criteria. Common factors include age, gender, ethnicity, presence of a certain disease, disease stage, and previous medical treatment.
Researchers occasionally randomly select people and ask them to participate if they meet particular requirements.
What’s a Clinical Trial?
Clinical trials are part of clinical studies. Participants must follow certain protocols and interventions of the clinical trial. Medicines, technologies, and behavioral changes are some of the interventions involved. Occasionally, a combination of intervention or protocols are used.
What Are Scientists Looking for in Clinical Trials?
Trials help doctors discover insights on new illness treatments and prevention methods. The study team meticulously records participant replies to study protocols. Clinical trials can:
- Compare current and old medical procedures
- Evaluate two well-established medical therapies and compare their results
- Compare the effects of a new drug to those obtained using a placebo to determine its effectiveness
How Do Trials Work?
The FDA has a four-step clinical trial approach to help researchers find effective dosages, identify potential side effects, and, ideally, secure FDA approval for widespread clinical use. Each phase must focus on safety and effectiveness. The phases are:
- Phase I clinical trials are small-scale experiments on healthy adults of diverse ages. This phase assesses the efficacy and side effects to determine the dose.
- Phase II clinical trials involve 100–300 patients and is used to assess if a pharmaceutical or medical device is safe and effective for treating an illness or symptom.
- Phase III clinical trials typically involve thousands of participants. Researchers analyze doses, populations, and other features. In Phase III, the FDA may approve an experimental drug or technology for widespread use.
- Phase IV clinical trials are the final step in drug or device development. During Phase IV, the efficacy and safety in larger representative groups is evaluated. Due to the delayed onset of side effects and other adverse responses, Phase IV patients receiving the new medication or treatment in a real-world settings are carefully watched.
How to Participate in Clinical Trials
Before you enroll in a clinical trial, consult your doctor. They may need to provide permission for you to participate. Your doctor’s office may enroll patients in a clinical study or refer you to another center if your doctor gives permission. You can also search for a trial or join a free service that alerts you to new clinical trials.
If you’re interested in participating in a clinical trial, regularly check back on our website for all our volunteer opportunities. If you have any questions, please fill out our online contact form .
Interested in Volunteering?
- First Name *
- Last Name *
- Area of Interest * Area of Interest Women's Studies Urology Vaccines Dermatology Vaccines Internal Medicine Neurology Ophthalmology Gastrointestinal Rheumatology Infectious Disease Aesthetic Medicine Pediatrics COVID-19
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- For Patients
- Clinical Trials: What Patients Need to Know
Clinical Research Versus Medical Treatment
What is clinical research.
Clinical research refers to studies in which people participate as patients or healthy volunteers. Different terms are used to describe clinical research, including:
What is Clinical Research
Read the What is Clinical Research? text alternative
clinical studies
clinical trials
Clinical research may have a number of goals, such as:
developing new treatments or medications
identifying causes of illness
studying trends
evaluating ways in which genetics may be related to an illness.
The idea for a clinical research study—also known as a clinical trial—often starts in the laboratory. After researchers test new therapies or procedures in the laboratory and in animal studies, the most promising experimental treatments are moved into clinical trials, which are conducted in phases. During a trial, more information is gained about an experimental treatment, its risks, and its effectiveness.
Strict rules for clinical studies have been put in place by National Institutes of Health and the FDA. Some studies involve promising new treatments that may directly benefit participants. Others do not directly benefit participants, but may help scientists learn better ways to help people.
Confidentiality is an important part of clinical research and ensures that personal information is seen only by those authorized to have access. It also means that the personal identity and all medical information of clinical trial participants is known only to the individual patient and researchers. Results from a study will usually be presented only in terms of trends or overall findings and will not mention specific participants.
Clinical research is much different from the medical treatment you receive in a Healthcare Provider's office.
| Clinical Research Versus Medical Treatment | ||
|---|---|---|
| Answers specific questions through research involving numerous research volunteers. | Address the needs of individual patients. | |
| Generally designed and intended to benefit future patients. | Intended to benefit the individual patient. | |
| Paid for by drug developers and government agencies. | Funded by individual patients and their health plans. | |
| Depends on the research protocol. | Requires real-time decisions. | |
| Requires written informed consent. | May or may not require informed consent. | |
| Involves periodic and systematic assessment of patient data. | Based on as-needed patient assessment. | |
| Protected by government agencies, institutional review boards, professional standards, informed consent, and legal standards. | Guided by state boards of medical practice, professional standards, peer review, informed consent, and legal standards. | |
| Tests products and procedures of unproven benefit to the patient. | Uses products and procedures accepted by the medical community as safe and effective. | |
| Considered confidential intellectual property. | Available to the general public through product labeling. | |
| Published in medical journals, after clinical research ends. | Individual medical records are not released to the general public. | |
Who should consider clinical trials and why?
Some people participate in clinical trials because none of the standard (approved) treatment options have worked, or they are unable to tolerate certain side effects. Clinical trials provide another option when standard therapy has failed. Others participate in trials because they want to contribute to the advancement of medical knowledge.
All clinical trials have guidelines, called eligibility criteria, about who can participate. The criteria are based on such factors as age, sex, type and stage of disease, previous treatment history, and other medical conditions. This helps to reduce the variation within the study and to ensure that the researchers will be able to answer the questions they plan to study. Therefore, not everyone who applies for a clinical trial will be accepted.
It is important to test drugs and medical products in the people they are meant to help. It is also important to conduct research in a variety of people, because different people may respond differently to treatments. FDA seeks to ensure that people of different ages, races, ethnic groups, and genders are included in clinical trials. Learn more about FDA’s efforts to increase diversity in clinical trials .
Where are clinical trials conducted?
Clinical trials can be sponsored by organizations (such as a pharmaceutical company), Federal offices and agencies (such as the National Institutes of Health or the U.S. Department of Veterans Affairs), or individuals (such as doctors or health care providers). The sponsor determines the location(s) of the trials, which are usually conducted at universities, medical centers, clinics, hospitals, and other Federally or industry-funded research sites.
Are clinical trials safe?
FDA works to protect participants in clinical trials and to ensure that people have reliable information before deciding whether to join a clinical trial. The Federal government has regulations and guidelines for clinical research to protect participants from unreasonable risks. Although efforts are made to control the risks to participants, some may be unavoidable because we are still learning more about the medical treatments in the study.
The government requires researchers to give prospective participants complete and accurate information about what will happen during the trial. Before joining a particular study, you will be given an informed consent document that describes your rights as a participant, as well as details about the study, including potential risks. Signing it indicates that you understand that the trial is research and that you may leave at any time. The informed consent is part of the process that makes sure you understand the known risks associated with the study.
What should I think about before joining a clinical trial?
Before joining a clinical trial, it is important to learn as much as possible. Discuss your questions and concerns with members of the health care team conducting the trial. Also, discuss the trial with your health care provider to determine whether or not the trial is a good option based on your current treatment. Be sure you understand:
what happens during the trial
the type of health care you will receive
any related costs once you are enrolled in the trial
the benefits and risks associated with participating.
What is FDA’s role in approving new drugs and medical treatments?
FDA makes sure medical treatments are safe and effective for people to use. We do not develop new therapies or conduct clinical trials. Rather, we oversee the people who do. FDA staff meet with researchers and perform inspections of clinical trial study sites to protect the rights of patients and to verify the quality and integrity of the data.
Learn more about the Drug Development Process .
Where can I find clinical trials?
One good way to find out if there are any clinical trials that might help you is to ask your doctor. Other sources of information include:
FDA Clinical Trials Search . Search a database of Federally and privately supported studies available through clinicaltrials.gov. Learn about each trial’s purpose, who can participate, locations, and who to contact for more information.
Clinicaltrials.gov. Conduct more advanced searches
National Cancer Institute or call 1–800–4–CANCER (1–800–422–6237). Learn about clinical trials for people with cancer.
What is a placebo and how is it related to clinical trials?
A placebo is a pill, liquid, or powder that has no treatment value. It is often called a sugar pill. In clinical trials, experimental drugs are often compared with placebos to evaluate the treatment’s effectiveness.
Is there a chance I might get a placebo?
In clinical trials that include placebos, quite often neither patients nor their doctors know who is receiving the placebo and how is being treated with the experimental drug. Many cancer clinical trials, as well as trials for other serious and life-threatening conditions, do not include placebo control groups. In these cases, all participants receive the experimental drug. Ask the trial coordinator whether there is a chance you may get a placebo rather than the experimental drug. Then, talk with your doctor about what is best for you.
How do I find out what Phase a drug is in as part of the clinical trial?
Talk to the clinical trial coordinator to find out which phase the clinical trial is in. Learn more about the different clinical trial phases and whether they are right for you.
What happens to drugs that don't make it out of clinical trials?
Most drugs that undergo preclinical (animal) research never even make it to human testing and review by the FDA. The drug developers go back to begin the development process using what they learned during with their preclinical research. Learn more about drug development .
Learn more about the basics of clinical trial participation, read first hand experiences from actual clinical trial volunteers, and see explanations from researchers at the NIH Clinical Research Trials and You Web site.

Clinical Research
NIH defines human clinical research as research with human subjects that is:
(1) Patient-Oriented Research. Research Conducted with human subjects (or on material of human origin such as tissues, specimens, and cognitive phenomena) for which an investigator (or colleague) directly interacts with human subjects. Excluded from this definition are in vitro studies that utilize human tissues that cannot be linked to a living individual. Patient-oriented research includes:
(a) mechanisms of human disease,
(b) therapeutic interventions,
(c) clinical studies, or
(d) development of new technologies.
(2) Epidemiologic and Behavioral Studies.
(3) Outcomes Research and Health Services Research.
Note: Studies falling under Exemption 4 for human subjects research are not considered clinical research by this definition.
Clinical Trial*
The NIH defines a clinical trial as a research study in which one or more human subjects are prospectively assigned to one or more interventions (which may include placebo or other control) to evaluate the effects of those interventions on health-related biomedical or behavioral outcomes.
- The term "prospectively assigned" refers to a pre-defined process (e.g., randomization) specified in an approved protocol that stipulates the assignment of research subjects (individually or in clusters) to one or more arms (e.g., intervention, placebo or other control) of the clinical trial.
- An intervention is defined as a manipulation of the subject or subject's environment for the purpose of modifying one or more health-related processes and/or endpoints. Examples include, but are not limited, to: drugs/small molecules/compounds, biologics, devices; procedures (e.g., surgical techniques); delivery systems (e.g., telemedicine, face-to-face); strategies to change health-related behavior (e.g., diet, cognitive therapy, exercise, development of new habits); and, treatment, prevention, and diagnostic strategies.
- A health-related biomedical or behavioral outcome is defined as the pre-specified effect of an intervention on the study subjects. Examples include positive or negative changes to physiological or biological parameters (e.g., improvement of lung capacity, gene expression); psychological or neurodevelopmental parameters (e.g., mood management intervention for smokers; reading comprehension and/or information retention); disease processes; health-related behavior; and, well-being or quality of life.
- Biomedical clinical trials of an experimental drug, treatment, device, or behavioral intervention may proceed through four phases: Phase I. Tests a new biomedical intervention in a small group of people (e.g. 20-80) for the first time to determine efficacy and evaluate safety (e.g., determine a safe dosage range and identify side effects). Phase II. Study the biomedical or behavioral intervention in a larger group of people (several hundred) to determine efficacy and further evaluate safety. Phase III . Study to determine efficacy of the biomedical or behavioral intervention in large groups of people (from several hundred to several thousand) by comparing the intervention to other standard or experimental interventions as well as to monitor adverse effects, and to collect information that will allow the interventions to be used safely. NIH-Defined Phase III Clinical Trial. For the purpose of the Guidelines an NIH-defined Phase III clinical trial is a broadly based prospective Phase III clinical investigation, usually involving several hundred or more human subjects, for the purpose of evaluating an experimental intervention in comparison with a standard or controlled intervention or comparing two or more existing treatments. Often the aim of such investigation is to provide evidence leading to a scientific basis for consideration of a change in health policy or standard of care. The definition includes pharmacologic, non-pharmacologic, and behavioral interventions given for disease prevention, prophylaxis, diagnosis, or therapy. Community trials and other population-based intervention trials are also included. Phase IV. Studies conducted after the intervention has been marketed. These studies are designed to monitor the effectiveness of the approved intervention in the general population and to collect information about any adverse effects associated with widespread use.
* Reminder: Ensure compliance with clinicaltrials.gov registration requirements for applicable clinical trials
Is your study a Clinical Trial?
See the Clinical Trials page to determine if your study is a clinical trial and what you need to know when conducting a clinical trial. [ HTML ]
Investigational Drug Service [ HTML ] Phone: 859-2178-0630
Office of Sponsored Projects Administration (OSPA) [ HTML ] Email: [email protected]
Proposal Development Office (PDO) [ HTML ] Email: [email protected]
Center for Clinical and Translational Science (CCTS) [ HTML ] Email: [email protected]
Clinical Research Support Office (CRSO) [ HTML ] Email: [email protected]
- Education Home
- Medical Education Technology Support
- Graduate Medical Education
- Medical Scientist Training Program
- Public Health Sciences Program
- Continuing Medical Education
- Clinical Performance Education Center
- Center for Excellence in Education
- Research Home
- Biochemistry & Molecular Genetics
- Biomedical Engineering
- Cell Biology
- Microbiology, Immunology, & Cancer Biology (MIC)
- Molecular Physiology & Biological Physics
- Neuroscience
- Pharmacology
- Public Health Sciences
- Office for Research
- Clinical Research
- Clinical Trials Office
- Funding Opportunities
- Grants & Contracts
- Research Faculty Directory
- Cancer Center
- Cardiovascular Research Center
- Carter Immunology Center
- Center for Behavioral Health & Technology
- Center for Brain Immunology & Glia
- Center for Diabetes Technology
- Center for Immunity, Inflammation & Regenerative Medicine
- Center for Public Health Genomics
- Center for Membrane & Cell Physiology
- Center for Research in Reproduction
- Myles H. Thaler Center for AIDS & Human Retrovirus Research
- Child Health Research Center (Pediatrics)
- Division of Perceptual Studies
- Research News: The Making of Medicine
- Core Facilities
- Virginia Research Resources Consortium
- Center for Advanced Vision Science
- Charles O. Strickler Transplant Center
- Keck Center for Cellular Imaging
- Institute of Law, Psychiatry & Public Policy
- Translational Health Research Institute of Virginia
- Clinical Home
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Neurosurgery
- Obstetrics & Gynecology
- Ophthalmology
- Orthopaedic Surgery
- Otolaryngology
- Physical Medicine & Rehabilitation
- Plastic Surgery, Maxillofacial, & Oral Health
- Psychiatry & Neurobehavioral Sciences
- Radiation Oncology
- Radiology & Medical Imaging
- UVA Health: Patient Care
- Diversity Home
- Diversity Overview
- Student Resources
- GME Trainee Resources
- Faculty Resources
- Community Resources
What is Clinical Research?
Clinical research is the study of health and illness in people. It is the way we learn how to prevent, diagnose and treat illness. Clinical research describes many different elements of scientific investigation. Simply put, it involves human participants and helps translate basic research (done in labs) into new treatments and information to benefit patients. Clinical trials as well as research in epidemiology, physiology and pathophysiology, health services, education, outcomes and mental health can all fall under the clinical research umbrella.
Clinical Trials
A clinical trial is a type of clinical research study. A clinical trial is an experiment designed to answer specific questions about possible new treatments or new ways of using existing (known) treatments. Clinical trials are done to determine whether new drugs or treatments are safe and effective. Clinical trials are part of a long, careful process which may take many years to complete. First, doctors study a new treatment in the lab. Then they often study the treatment in animals. If a new treatment shows promise, doctors then test the treatment in people via a clinical trial.
Clinical Research vs. Medical Care
People often confuse a clinical research or clinical trials with medical care. This topic can be especially confusing if your doctor is also the researcher. When you receive medical care from your own doctor, he or she develops a plan of care just for you. When you take part in a clinical research study, you and the researcher must follow a set plan called the “study protocol.” The researcher usually can’t adjust the plan for you – but the plan includes steps to follow if you aren’t doing well. It’s important to understand that a clinical trial is an experiment. By its nature, that means the answer to the research question is still unknown. You might or might not benefit directly by participating in a clinical research study. It is important to talk about this topic with your doctor/the researcher.
- Clinical Trials Unit
- Diversity in Clinical Research
- Research Resources
- Study Management
- Participate in a Trial
- +91-7672005050
- [email protected]
Difference between Clinical Trial and Clinical Study
Frequently asked questions.
Yes. The status of enrolment of the trial subjects shall be intimated to the CLA on quarterly basis or as appropriate as per the duration of treatment in accordance with the approved clinical trial protocol, whichever is earlier. Further, six monthly status report of each clinical trial, as to whether it is ongoing, completed or terminated, shall be submitted in SUGAM portal. In case of termination of any clinical trial the detailed reasons for such termination shall be communicated to CLA.
Related Articles
Medical devices |, current regulatory scenario for conducting medical device clinical trials in india · cliniexperts.
Current Regulatory Scenario for Conducting Medical Device Clinical Trials in India Medical devices complement the physician’s or surgeon’s expertise in examination, diagnosis, treatment, or follow-up. Access to medical devices helps a physician come up with the right diagnosis of the patient’s medical condition, or a surgeon to carry out a procedure accurately. These devices enjoy

- Patient Login
- Partner Login
- Become A Member
- Search Clinical Trials
- About Clinical Trials
- Virtual Clinical Trials
Latest Blog Posts
Services for research sites.
- Study Listings
- Clinical Ad Network™
- Patient Direct Mail Alerts
- Create Partner Account
National Recruitment Services
- Multicenter Study Listings
- Digital Marketing Strategies
- Site Identification Services
- Direct to Patient Advertising
News And Information
- Case Studies
- Patient Recruitment Insider Blog
- For Research Sites
- Study Screening Websites
What is the Difference Between A Clinical Trial and A Clinical Study

People often use the terms "clinical trial" and "clinical study" interchangeably. Both fall under the umbrella term "clinical research," which is the study of health and illness in humans. This research involves people voluntarily participating under conditions set by the clinical researchers. If considering participating in clinical research , it's important to understand the differences between these terms.
What is a Clinical Study?
A clinical study is research using human participants to help experts learn about different medical conditions and treatments. There are two primary types of clinical studies: clinical trials and observational studies. Both are designed to help health care professionals expand their knowledge of viable treatment—or preventative—options for patients, including medications, medical devices, surgery techniques, and therapies (e.g. radiation). Clinical studies may also focus on the development of diagnostic tools to help detect or prevent diseases and other medical conditions.
Who Creates a Clinical Study?
Clinical studies are often sponsored by entities that pay for the research. Typical sponsors are academic medical centers, pharmaceutical companies, voluntary groups, and federal agencies, such as the National Institutes of Health (NIH), Department of Veterans Affairs (VA), and Department of Defense (DoD). Sponsors initiating clinical research want to learn more about medical conditions or identify viable treatments.
Who is in Charge of the Clinical Study?
Every study is led by a principal investigator, usually a medical doctor. It's common for studies to have research teams that include experts of varying degrees of expertise and experience. A clinical study team is often composed of doctors, nurses, social workers, and other types of healthcare professionals. Studies often take place in different facilities, including hospitals, community clinics, universities, or doctors' offices.
Can Anyone Join a Study?
When study parameters are built, the research team sets stringent protocols to help the study succeed. This determines eligibility criteria. Who can join will depend on if they meet established inclusion and exclusion criteria. Common criteria include:
- Having specific illnesses or health conditions
- Stage of a disease
- Previous treatment history for a medical condition
Sometimes research teams choose individuals and ask them to participate if they meet predetermined eligibility factors.
What is a Clinical Trial?
A clinical trial is a component of a clinical study. People who participate in clinical trials are directed to follow the specific interventions set by the initial research protocols for the purpose of the study. Interventions may include drugs, devices, or modifications to a participants' behavior (e.g. diet and exercise). Sometimes it'll be a combination of one or more protocols.
What are Research Teams Looking for in Trials?
Trials are designed to help professionals gain insight and knowledge that will help identify effective new treatments or preventative strategies for medical conditions. The research team carefully tracks participants and how they react to the protocols within the study's parameters. To meet these goals, a clinical trial may:
- Compare new with traditional, already-established medical treatments or interventions.
- Compare two established medical treatments or interventions.
- Compare a new drug treatment's effectiveness to a placebo (inert compound).
These are only a handful of techniques used. What the research teams establish depends upon the type of study and the outcome they're seeking (e.g. treatment for specific cancer types or medications to combat diseases) to determine safety and effectiveness.
How are Trials Conducted?
Trials are broken into four phases which are defined by the U.S. Food and Drug Administration (FDA) and established to help researchers find the right dosages, identify potential side effects, and, if all goes as hoped, gain FDA approval for clinical use. Each phase emphasizes a focus on safety and effectiveness.
- Phase I clinical trials are experimental treatments, usually performed on a small group of (often) healthy people of a wide age range. This phase focuses on safety and side effects to determine correct uses or dosages.
- Phase II clinical trials increase the number of participants (100 to 300), putting an emphasis on effectiveness and obtaining preliminary data to see if a drug (or device) works in people with certain diseases or conditions. Phase II can last years.
- Phase III clinical trials increase participants further, frequently to thousands of participants. Researchers look at different populations and dosage amounts, along with using the treatment with other parameters (e.g. drug combinations). If Phase III succeeds, the FDA may approve the experimental drug or device for widespread use.
- Phase IV clinical trials are the final stage where researchers monitor the drug or device's effectiveness and safety in large, diverse populations. Sometimes, side effects or other adverse reactions don't occur immediately, so safety is carefully monitored throughout Phase IV trials in patients that are receiving the new treatments in real-world settings.
People participate in clinical trials for many reasons. Some suffer from diseases where current treatment options don't work for them or there are no treatments at all. Healthy people participate to aid the development of new treatments or preventative measures.
How Can People Join Clinical Trials?
People who want to participate in clinical trials should first speak with their doctor. If their doctor agrees, they may be enrolled in a clinical trial through their medical office or be referred to another center. Other ways to join are to search for clinical trials or join clinicalconnection.com to receive notifications when new trials are available.
ClinicalConnection, founded by pharmaceutical research professionals, has been helping connect people with clinical trials since 2000.
Recent Posts

- Artificial Intelligence in Medicine: Transformative Medical Breakthroughs
- Exploring the Microbiome: Gut Health, Probiotics and Clinical Trials

- Nutrition and Clinical Trials: Latest Clinical Research on Diet's Role in Disease

- Personalized Medicine: The Power of Genetics in Clinical Trials
Top Searches
- Lupus (SLE)
- Ulcerative Colitis
- Alzheimer's Disease
- Chronic Inflammatory Demyelinating Polyneuropathy (CIDP)
- Hypertension
- Bronchiectasis

© 1998-2024 | All trademarks are property of their legal owners. | All Rights Reserved
ClinicalConnection.com is a resource that provides information on clinical trials and other research opportunities worldwide.
ClinicalConnection.com does not conduct or endorse this research. Please consult your physician before participating.
Useful Links
1998-2024 © All Rights Reserved. Privacy Policy | Terms of Service
Study record managers: refer to the Data Element Definitions if submitting registration or results information.
Search for terms
Clinical Trials vs. Clinical Research: What’s to Know?
“Wherever the art of medicine is loved, there is also a love of humanity” – Hippocrates
When new drugs, vaccines, and medical devices are developed and marketed, one of the most important things to address is safety—the tracking of adverse events related to the usage of medicinal products. But what goes on behind the scenes before a game-changing drug makes its market entry? The answer is clinical trials and clinical research. Let’s consider each of these activities
Clinical Trials
A clinical trial is a type of clinical research study. A clinical trial is an experiment designed to answer specific questions about possible new treatments or new ways of using existing (known) treatments. Clinical trials are done to determine whether new drugs or treatments are safe and effective. They are usually part of a long, careful process that may take many years to complete. Clinical trials are conducted in four phases:
- Phase 1 – Tests carried out using an experimental drug or treatment on a small group, typically between 20 to 100 people, to evaluate the treatment for factors including identification of a safe dosage range, patient safety, and detection of side-effects.
- Phase 2 – Experimental drug or treatment is given to a larger group of 100 to 300 people to evaluate its safety and to determine the drug’s efficacy.
- Phase 3 – Testing of drug on a larger group of 300 to 3000 people to assess efficacy, effectiveness and safety.
- Phase 4 – Post-marketing studies commence after treatment approvals by the approved regulatory body for drugs, e.g., the National Agency for Food and Drug Administration and Control (NAFDAC) in Nigeria and the Food and Drug Administration (FDA) in the US.
Clinical Research
Clinical research is the study of health and illness in people. It is a more encompassing discipline investigating how to prevent, diagnose and treat illness. Clinical research describes many different elements of scientific investigations. Simply put, it involves human participants and helps translate basic research carried out in laboratories into new information and treatments to benefit patients. There are different types of clinical research including treatment research, epidemiological studies, diagnostic research, and others.
Critical Contribution to Healthcare
Clinical research, therefore, includes the processes of clinical trials, epidemiological research, and health services. It also covers education, outcome management, and mental health services for participating individuals. These elements are all vital for medical innovation.
Clinical trials will not be a success without volunteers and participants. However, volunteers and participants must be informed of the risks and benefits of a successful clinical trial.
Volunteers who participate in these studies may benefit from accessing highly-effective treatments that could be deployed for debilitating illnesses. A volunteer can also gain full access to new medical treatments before they are widely available.
Without a doubt, the year 2020 presented many challenges to the healthcare industry–the COVID-19 pandemic ranking as the global antagonist. Those challenges are yet to be completely eliminated even in 2021, but they have brought endless opportunities to improve clinical trial processes across the world.
At Xcene Research, we continue to work at supporting clinical sites and sponsors in creating more efficient, decentralized processes with the patient always top of mind. Bringing care directly to patients is what we do best and we are excited to be part of this new frontier.
Related Posts
Children in covid-19 trials, the evolution of clinical trials, sickle cell disease management: past and future, 4 thoughts on “clinical trials vs. clinical research: what’s to know”.
Pingback: Rare Diseases - Xcene Innovate
Pingback: Clinical Trials Participation Made Easy - Xcene Innovate
Pingback: Career Paths In Clinical Research - Xcene Innovate
Pingback: clinical trials vs research studies - infoslist
Leave a Comment Cancel Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Human Subjects Office
Medical terms in lay language.
Please use these descriptions in place of medical jargon in consent documents, recruitment materials and other study documents. Note: These terms are not the only acceptable plain language alternatives for these vocabulary words.
This glossary of terms is derived from a list copyrighted by the University of Kentucky, Office of Research Integrity (1990).
For clinical research-specific definitions, see also the Clinical Research Glossary developed by the Multi-Regional Clinical Trials (MRCT) Center of Brigham and Women’s Hospital and Harvard and the Clinical Data Interchange Standards Consortium (CDISC) .
Alternative Lay Language for Medical Terms for use in Informed Consent Documents
A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
ABDOMEN/ABDOMINAL body cavity below diaphragm that contains stomach, intestines, liver and other organs ABSORB take up fluids, take in ACIDOSIS condition when blood contains more acid than normal ACUITY clearness, keenness, esp. of vision and airways ACUTE new, recent, sudden, urgent ADENOPATHY swollen lymph nodes (glands) ADJUVANT helpful, assisting, aiding, supportive ADJUVANT TREATMENT added treatment (usually to a standard treatment) ANTIBIOTIC drug that kills bacteria and other germs ANTIMICROBIAL drug that kills bacteria and other germs ANTIRETROVIRAL drug that works against the growth of certain viruses ADVERSE EFFECT side effect, bad reaction, unwanted response ALLERGIC REACTION rash, hives, swelling, trouble breathing AMBULATE/AMBULATION/AMBULATORY walk, able to walk ANAPHYLAXIS serious, potentially life-threatening allergic reaction ANEMIA decreased red blood cells; low red cell blood count ANESTHETIC a drug or agent used to decrease the feeling of pain, or eliminate the feeling of pain by putting you to sleep ANGINA pain resulting from not enough blood flowing to the heart ANGINA PECTORIS pain resulting from not enough blood flowing to the heart ANOREXIA disorder in which person will not eat; lack of appetite ANTECUBITAL related to the inner side of the forearm ANTIBODY protein made in the body in response to foreign substance ANTICONVULSANT drug used to prevent seizures ANTILIPEMIC a drug that lowers fat levels in the blood ANTITUSSIVE a drug used to relieve coughing ARRHYTHMIA abnormal heartbeat; any change from the normal heartbeat ASPIRATION fluid entering the lungs, such as after vomiting ASSAY lab test ASSESS to learn about, measure, evaluate, look at ASTHMA lung disease associated with tightening of air passages, making breathing difficult ASYMPTOMATIC without symptoms AXILLA armpit
BENIGN not malignant, without serious consequences BID twice a day BINDING/BOUND carried by, to make stick together, transported BIOAVAILABILITY the extent to which a drug or other substance becomes available to the body BLOOD PROFILE series of blood tests BOLUS a large amount given all at once BONE MASS the amount of calcium and other minerals in a given amount of bone BRADYARRHYTHMIAS slow, irregular heartbeats BRADYCARDIA slow heartbeat BRONCHOSPASM breathing distress caused by narrowing of the airways
CARCINOGENIC cancer-causing CARCINOMA type of cancer CARDIAC related to the heart CARDIOVERSION return to normal heartbeat by electric shock CATHETER a tube for withdrawing or giving fluids CATHETER a tube placed near the spinal cord and used for anesthesia (indwelling epidural) during surgery CENTRAL NERVOUS SYSTEM (CNS) brain and spinal cord CEREBRAL TRAUMA damage to the brain CESSATION stopping CHD coronary heart disease CHEMOTHERAPY treatment of disease, usually cancer, by chemical agents CHRONIC continuing for a long time, ongoing CLINICAL pertaining to medical care CLINICAL TRIAL an experiment involving human subjects COMA unconscious state COMPLETE RESPONSE total disappearance of disease CONGENITAL present before birth CONJUNCTIVITIS redness and irritation of the thin membrane that covers the eye CONSOLIDATION PHASE treatment phase intended to make a remission permanent (follows induction phase) CONTROLLED TRIAL research study in which the experimental treatment or procedure is compared to a standard (control) treatment or procedure COOPERATIVE GROUP association of multiple institutions to perform clinical trials CORONARY related to the blood vessels that supply the heart, or to the heart itself CT SCAN (CAT) computerized series of x-rays (computerized tomography) CULTURE test for infection, or for organisms that could cause infection CUMULATIVE added together from the beginning CUTANEOUS relating to the skin CVA stroke (cerebrovascular accident)
DERMATOLOGIC pertaining to the skin DIASTOLIC lower number in a blood pressure reading DISTAL toward the end, away from the center of the body DIURETIC "water pill" or drug that causes increase in urination DOPPLER device using sound waves to diagnose or test DOUBLE BLIND study in which neither investigators nor subjects know what drug or treatment the subject is receiving DYSFUNCTION state of improper function DYSPLASIA abnormal cells
ECHOCARDIOGRAM sound wave test of the heart EDEMA excess fluid collecting in tissue EEG electric brain wave tracing (electroencephalogram) EFFICACY effectiveness ELECTROCARDIOGRAM electrical tracing of the heartbeat (ECG or EKG) ELECTROLYTE IMBALANCE an imbalance of minerals in the blood EMESIS vomiting EMPIRIC based on experience ENDOSCOPIC EXAMINATION viewing an internal part of the body with a lighted tube ENTERAL by way of the intestines EPIDURAL outside the spinal cord ERADICATE get rid of (such as disease) Page 2 of 7 EVALUATED, ASSESSED examined for a medical condition EXPEDITED REVIEW rapid review of a protocol by the IRB Chair without full committee approval, permitted with certain low-risk research studies EXTERNAL outside the body EXTRAVASATE to leak outside of a planned area, such as out of a blood vessel
FDA U.S. Food and Drug Administration, the branch of federal government that approves new drugs FIBROUS having many fibers, such as scar tissue FIBRILLATION irregular beat of the heart or other muscle
GENERAL ANESTHESIA pain prevention by giving drugs to cause loss of consciousness, as during surgery GESTATIONAL pertaining to pregnancy
HEMATOCRIT amount of red blood cells in the blood HEMATOMA a bruise, a black and blue mark HEMODYNAMIC MEASURING blood flow HEMOLYSIS breakdown in red blood cells HEPARIN LOCK needle placed in the arm with blood thinner to keep the blood from clotting HEPATOMA cancer or tumor of the liver HERITABLE DISEASE can be transmitted to one’s offspring, resulting in damage to future children HISTOPATHOLOGIC pertaining to the disease status of body tissues or cells HOLTER MONITOR a portable machine for recording heart beats HYPERCALCEMIA high blood calcium level HYPERKALEMIA high blood potassium level HYPERNATREMIA high blood sodium level HYPERTENSION high blood pressure HYPOCALCEMIA low blood calcium level HYPOKALEMIA low blood potassium level HYPONATREMIA low blood sodium level HYPOTENSION low blood pressure HYPOXEMIA a decrease of oxygen in the blood HYPOXIA a decrease of oxygen reaching body tissues HYSTERECTOMY surgical removal of the uterus, ovaries (female sex glands), or both uterus and ovaries
IATROGENIC caused by a physician or by treatment IDE investigational device exemption, the license to test an unapproved new medical device IDIOPATHIC of unknown cause IMMUNITY defense against, protection from IMMUNOGLOBIN a protein that makes antibodies IMMUNOSUPPRESSIVE drug which works against the body's immune (protective) response, often used in transplantation and diseases caused by immune system malfunction IMMUNOTHERAPY giving of drugs to help the body's immune (protective) system; usually used to destroy cancer cells IMPAIRED FUNCTION abnormal function IMPLANTED placed in the body IND investigational new drug, the license to test an unapproved new drug INDUCTION PHASE beginning phase or stage of a treatment INDURATION hardening INDWELLING remaining in a given location, such as a catheter INFARCT death of tissue due to lack of blood supply INFECTIOUS DISEASE transmitted from one person to the next INFLAMMATION swelling that is generally painful, red, and warm INFUSION slow injection of a substance into the body, usually into the blood by means of a catheter INGESTION eating; taking by mouth INTERFERON drug which acts against viruses; antiviral agent INTERMITTENT occurring (regularly or irregularly) between two time points; repeatedly stopping, then starting again INTERNAL within the body INTERIOR inside of the body INTRAMUSCULAR into the muscle; within the muscle INTRAPERITONEAL into the abdominal cavity INTRATHECAL into the spinal fluid INTRAVENOUS (IV) through the vein INTRAVESICAL in the bladder INTUBATE the placement of a tube into the airway INVASIVE PROCEDURE puncturing, opening, or cutting the skin INVESTIGATIONAL NEW DRUG (IND) a new drug that has not been approved by the FDA INVESTIGATIONAL METHOD a treatment method which has not been proven to be beneficial or has not been accepted as standard care ISCHEMIA decreased oxygen in a tissue (usually because of decreased blood flow)
LAPAROTOMY surgical procedure in which an incision is made in the abdominal wall to enable a doctor to look at the organs inside LESION wound or injury; a diseased patch of skin LETHARGY sleepiness, tiredness LEUKOPENIA low white blood cell count LIPID fat LIPID CONTENT fat content in the blood LIPID PROFILE (PANEL) fat and cholesterol levels in the blood LOCAL ANESTHESIA creation of insensitivity to pain in a small, local area of the body, usually by injection of numbing drugs LOCALIZED restricted to one area, limited to one area LUMEN the cavity of an organ or tube (e.g., blood vessel) LYMPHANGIOGRAPHY an x-ray of the lymph nodes or tissues after injecting dye into lymph vessels (e.g., in feet) LYMPHOCYTE a type of white blood cell important in immunity (protection) against infection LYMPHOMA a cancer of the lymph nodes (or tissues)
MALAISE a vague feeling of bodily discomfort, feeling badly MALFUNCTION condition in which something is not functioning properly MALIGNANCY cancer or other progressively enlarging and spreading tumor, usually fatal if not successfully treated MEDULLABLASTOMA a type of brain tumor MEGALOBLASTOSIS change in red blood cells METABOLIZE process of breaking down substances in the cells to obtain energy METASTASIS spread of cancer cells from one part of the body to another METRONIDAZOLE drug used to treat infections caused by parasites (invading organisms that take up living in the body) or other causes of anaerobic infection (not requiring oxygen to survive) MI myocardial infarction, heart attack MINIMAL slight MINIMIZE reduce as much as possible Page 4 of 7 MONITOR check on; keep track of; watch carefully MOBILITY ease of movement MORBIDITY undesired result or complication MORTALITY death MOTILITY the ability to move MRI magnetic resonance imaging, diagnostic pictures of the inside of the body, created using magnetic rather than x-ray energy MUCOSA, MUCOUS MEMBRANE moist lining of digestive, respiratory, reproductive, and urinary tracts MYALGIA muscle aches MYOCARDIAL pertaining to the heart muscle MYOCARDIAL INFARCTION heart attack
NASOGASTRIC TUBE placed in the nose, reaching to the stomach NCI the National Cancer Institute NECROSIS death of tissue NEOPLASIA/NEOPLASM tumor, may be benign or malignant NEUROBLASTOMA a cancer of nerve tissue NEUROLOGICAL pertaining to the nervous system NEUTROPENIA decrease in the main part of the white blood cells NIH the National Institutes of Health NONINVASIVE not breaking, cutting, or entering the skin NOSOCOMIAL acquired in the hospital
OCCLUSION closing; blockage; obstruction ONCOLOGY the study of tumors or cancer OPHTHALMIC pertaining to the eye OPTIMAL best, most favorable or desirable ORAL ADMINISTRATION by mouth ORTHOPEDIC pertaining to the bones OSTEOPETROSIS rare bone disorder characterized by dense bone OSTEOPOROSIS softening of the bones OVARIES female sex glands
PARENTERAL given by injection PATENCY condition of being open PATHOGENESIS development of a disease or unhealthy condition PERCUTANEOUS through the skin PERIPHERAL not central PER OS (PO) by mouth PHARMACOKINETICS the study of the way the body absorbs, distributes, and gets rid of a drug PHASE I first phase of study of a new drug in humans to determine action, safety, and proper dosing PHASE II second phase of study of a new drug in humans, intended to gather information about safety and effectiveness of the drug for certain uses PHASE III large-scale studies to confirm and expand information on safety and effectiveness of new drug for certain uses, and to study common side effects PHASE IV studies done after the drug is approved by the FDA, especially to compare it to standard care or to try it for new uses PHLEBITIS irritation or inflammation of the vein PLACEBO an inactive substance; a pill/liquid that contains no medicine PLACEBO EFFECT improvement seen with giving subjects a placebo, though it contains no active drug/treatment PLATELETS small particles in the blood that help with clotting POTENTIAL possible POTENTIATE increase or multiply the effect of a drug or toxin (poison) by giving another drug or toxin at the same time (sometimes an unintentional result) POTENTIATOR an agent that helps another agent work better PRENATAL before birth PROPHYLAXIS a drug given to prevent disease or infection PER OS (PO) by mouth PRN as needed PROGNOSIS outlook, probable outcomes PRONE lying on the stomach PROSPECTIVE STUDY following patients forward in time PROSTHESIS artificial part, most often limbs, such as arms or legs PROTOCOL plan of study PROXIMAL closer to the center of the body, away from the end PULMONARY pertaining to the lungs
QD every day; daily QID four times a day
RADIATION THERAPY x-ray or cobalt treatment RANDOM by chance (like the flip of a coin) RANDOMIZATION chance selection RBC red blood cell RECOMBINANT formation of new combinations of genes RECONSTITUTION putting back together the original parts or elements RECUR happen again REFRACTORY not responding to treatment REGENERATION re-growth of a structure or of lost tissue REGIMEN pattern of giving treatment RELAPSE the return of a disease REMISSION disappearance of evidence of cancer or other disease RENAL pertaining to the kidneys REPLICABLE possible to duplicate RESECT remove or cut out surgically RETROSPECTIVE STUDY looking back over past experience
SARCOMA a type of cancer SEDATIVE a drug to calm or make less anxious SEMINOMA a type of testicular cancer (found in the male sex glands) SEQUENTIALLY in a row, in order SOMNOLENCE sleepiness SPIROMETER an instrument to measure the amount of air taken into and exhaled from the lungs STAGING an evaluation of the extent of the disease STANDARD OF CARE a treatment plan that the majority of the medical community would accept as appropriate STENOSIS narrowing of a duct, tube, or one of the blood vessels in the heart STOMATITIS mouth sores, inflammation of the mouth STRATIFY arrange in groups for analysis of results (e.g., stratify by age, sex, etc.) STUPOR stunned state in which it is difficult to get a response or the attention of the subject SUBCLAVIAN under the collarbone SUBCUTANEOUS under the skin SUPINE lying on the back SUPPORTIVE CARE general medical care aimed at symptoms, not intended to improve or cure underlying disease SYMPTOMATIC having symptoms SYNDROME a condition characterized by a set of symptoms SYSTOLIC top number in blood pressure; pressure during active contraction of the heart
TERATOGENIC capable of causing malformations in a fetus (developing baby still inside the mother’s body) TESTES/TESTICLES male sex glands THROMBOSIS clotting THROMBUS blood clot TID three times a day TITRATION a method for deciding on the strength of a drug or solution; gradually increasing the dose T-LYMPHOCYTES type of white blood cells TOPICAL on the surface TOPICAL ANESTHETIC applied to a certain area of the skin and reducing pain only in the area to which applied TOXICITY side effects or undesirable effects of a drug or treatment TRANSDERMAL through the skin TRANSIENTLY temporarily TRAUMA injury; wound TREADMILL walking machine used to test heart function
UPTAKE absorbing and taking in of a substance by living tissue
VALVULOPLASTY plastic repair of a valve, especially a heart valve VARICES enlarged veins VASOSPASM narrowing of the blood vessels VECTOR a carrier that can transmit disease-causing microorganisms (germs and viruses) VENIPUNCTURE needle stick, blood draw, entering the skin with a needle VERTICAL TRANSMISSION spread of disease
WBC white blood cell
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- Wunderkinds Nomination
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
Expand community-based research to make clinical trials more diverse
By Robert Metcalf and Jeffrey Francer July 10, 2024

I nnovations in clinical trial designs and tools have the potential to unlock a new era of research that is more convenient for patients, more reflective of real-world treatment conditions, and more likely to enable participation of a diverse set of individuals. But a recent study reveals how far the U.S. is from realizing this potential: regions of the country with the worst social drivers of health are the least likely to host clinical trials.
The disconnect between need and where clinical trials are conducted is a longstanding one. But it was recently highlighted by University of Michigan researchers through an examination of demographic data for people enrolled in clinical trials for new cancer medicines. The most socially vulnerable counties were far less likely to have any nearby trial, a disparity that has worsened over time.
advertisement
Research sponsors and the Food and Drug Administration can respond to this challenge by continuing to support community-based clinical trials. But the regulatory framework that governs these and other modern approaches has not kept pace with innovations in clinical trials and must be updated to enable expansion of trials into more communities.
Clinical trials are essential for establishing the safety and effectiveness of new medicines. Trial results have a greater impact when participants reflect the demographic diversity of those who could potentially benefit from the treatments being evaluated. The University of Michigan research is one more confirmation that the U.S.’s existing clinical trial infrastructure often fails to meet these goals.
Designing and implementing clinical trials is hard work. Reports over time suggest that up to 85% of clinical trials don’t meet their recruitment goals and up to 80% are delayed due to recruitment challenges.
Large-scale clinical trials are typically hosted by large research hospitals and academic institutions, most of which are in big cities. This can exclude people in rural communities from participating in clinical trials, and can present logistical challenges even for individuals who live relatively close to these centers because they may not have the economic means or schedule flexibility to attend multiple appointments.
Today’s clinical trial regulations were created for a different era, when the technology of the time necessitated that studies be conducted at a single location under the direct supervision of an investigator and staff who carried out all aspects of the trial. Participants were required to come to that location. Clinical research still largely relies on this outmoded approach, which frequently requires participants to organize their lives around the trial, and often includes traveling, finding a place to stay, and taking time off from work.
New tools and approaches developed by clinical trial sponsors, working with the FDA, should help make trials more representative. The FDA has signaled an openness to supporting trial designs that make them more accessible for participants, more reflective of real-world conditions, and enable more diverse participation. This modernization of the regulatory framework is critically needed and will contribute to healthier communities by speeding the development of new and better treatments that address unmet medical needs.
Community-based trials, also known as decentralized trials, have the potential to significantly increase participation and diversity in clinical research. By forcing a shift to this model, the Covid-19 pandemic showed just how successful these types of studies can be. To help ensure studies could continue during the pandemic, investigators, trial sponsors, and regulators worked collaboratively during the nationwide shutdown to reverse the process, bringing trials to participants rather than participants to trials.
Lilly, the company we work for, partnered with a leading decentralized research organization to bring our Covid-19 research to at-risk patients in long-term care facilities. An innovative cloud-based system helped recruit participants across multiple sites and make adjustments as needed in real time.
This model allowed Lilly to move quickly, reach more people who were traditionally underrepresented in clinical trials, and protect the health of participants and trial staff during the pandemic, all while maintaining the highest standards of scientific research, patient safety, and data integrity. To be sure, Lilly wasn’t alone in doing this: companies across the biopharmaceutical industry can share similar stories of leveraging innovative, community-based approaches to keep clinical trials running during the Covid-19 crisis.
These updated approaches shouldn’t fade away with the pandemic. Drug developers, investigators, and regulators must build on what was learned. Several key updates to the U.S. clinical trial regulatory framework will be crucial to supporting this progress:
Ease the burden on clinical trial investigators. Enabling better support from sponsor staff can create efficiencies and fill resource needs for community-based providers. Local health care professionals are essential to the success of community-based trials, but most of them do not have the resources or infrastructure to manage many of the demands of clinical studies, such as recruiting participants, providing them with logistical support, and shipping investigational products to them. Trial sponsor staff have the capability to perform tasks like these that involve limited or no contact with participants to avoid conflict of interest. Current regulatory rules, however, provide little guidance on what types of sponsor roles are appropriate, which creates uncertainty for sponsors that can discourage such support.
Update the role of investigators. The shift in clinical trial services to multiple care settings, such as community clinics, mobile medical units, and participants’ homes, must be accompanied by updating how clinical trial investigators provide oversight of these settings. Current regulations state that an investigator must personally conduct or supervise a trial. This requirement can create confusion for a community-based study that includes multiple care settings in numerous communities.
To better accommodate community-based trials without compromising patient safety or data integrity, FDA regulations should be updated to clarify that trial investigators may provide oversight by ensuring that study staff such as local health care providers are appropriately qualified and trained for the trial-related activities they will perform. Such assurance could include confirming proper education and qualifications and meeting state licensing requirements.
Current regulations also state that investigators may administer an investigational product only to study participants they personally supervise. Such regulations do not lend themselves to the flexibility needed to enable community-based research, where patients can receive clinical trial services in many types of settings.
Consistently support the use of digital health technologies. Wearable devices and other advances can help make trials more convenient for participants by enabling remote collection of data from them in real time as they go about their daily lives. This convenience can promote diversity by reducing the number of clinic visits needed, making it possible for people to participate in trials whose income, work, or travel issues would prevent multiple in-person visits. Yet current FDA guidance lacks clarity on what evidence is needed to validate the use of digital health technologies. A modernized approach for qualifying digital health technologies is needed. Sponsors of new drug trials are currently encouraged to use the drug development tools pathway , which was not designed for digital health technologies and can be cumbersome and complicated for this use.
It also is not clear how digital health technologies will be reviewed when multiple FDA divisions or offices are involved. Providing greater clarity on the evidence required for validation and on cross-agency standards will support acceleration of the application of digital health technologies, further enabling community-based clinical trials.
By the end of this decade, we believe that community-based clinical trials will become the norm, not the outlier. To achieve this, all clinical trial stakeholders — including the FDA, drug developers, and investigators — must work together to foster a patient-centric clinical trial culture that embraces innovation and brings trials closer to potential participants. The result will be a win for everyone.
Robert Metcalf, Ph.D., is group vice president for clinical design, delivery and analytics, China and Japan medical, for Lilly. Jeffrey Francer, J.D., is Lilly’s vice president, head of global regulatory policy and strategy.
LETTER TO THE EDITOR
Have an opinion on this essay submit a letter to the editor here ., about the authors reprints, robert metcalf, jeffrey francer.
Clinical trials
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

Preparing schools for the H5N1 bird flu they’re likely to face

Doctors ‘overprescribing’ opioids isn’t the cause of the overdose epidemic — and it never was

STAT Plus: Troubled for-profit chains are stealthily operating dozens of psychiatric hospitals under nonprofits’ names

STAT Plus: Biopharma layoffs are leaving the industry’s scientists reeling — and in search of scarce opportunities

STAT Plus: Pulling back the curtain on psychiatric hospital joint ventures
This paper is in the following e-collection/theme issue:
Published on 11.7.2024 in Vol 26 (2024)
Comparison of the Response to an Electronic Versus a Traditional Informed Consent Procedure in Terms of Clinical Patient Characteristics: Observational Study
Authors of this article:

Original Paper
- Anna G M Zondag 1 , MSc ;
- Marieke J Hollestelle 2 , PhD ;
- Rieke van der Graaf 2 , PhD ;
- Hendrik M Nathoe 3 , MD, PhD ;
- Wouter W van Solinge 1 , PhD ;
- Michiel L Bots 2 , MD, PhD ;
- Robin W M Vernooij 2, 4 , PhD ;
- Saskia Haitjema 1 , MD, PhD ;
- UCC-CVRM study group 5
1 Central Diagnostic Laboratory, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
2 Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
3 Department of Cardiology, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
4 Department of Nephrology and Hypertension, University Medical Center Utrecht, Utrecht, Netherlands
5 See Acknowledgements
Corresponding Author:
Anna G M Zondag, MSc
Central Diagnostic Laboratory
University Medical Center Utrecht
Utrecht University
Heidelberglaan 100
Utrecht, 3584 CX
Netherlands
Phone: 31 631117922
Email: [email protected]
Background: Electronic informed consent (eIC) is increasingly used in clinical research due to several benefits including increased enrollment and improved efficiency. Within a learning health care system, a pilot was conducted with an eIC for linking data from electronic health records with national registries, general practitioners, and other hospitals.
Objective: We evaluated the eIC pilot by comparing the response to the eIC with the former traditional paper-based informed consent (IC). We assessed whether the use of eIC resulted in a different study population by comparing the clinical patient characteristics between the response categories of the eIC and former face-to-face IC procedure.
Methods: All patients with increased cardiovascular risk visiting the University Medical Center Utrecht, the Netherlands, were eligible for the learning health care system. From November 2021 to August 2022, an eIC was piloted at the cardiology outpatient clinic. Prior to the pilot, a traditional face-to-face paper-based IC approach was used. Responses (ie, consent, no consent, or nonresponse) were assessed and compared between the eIC and face-to-face IC cohorts. Clinical characteristics of consenting and nonresponding patients were compared between and within the eIC and the face-to-face cohorts using multivariable regression analyses.
Results: A total of 2254 patients were included in the face-to-face IC cohort and 885 patients in the eIC cohort. Full consent was more often obtained in the eIC than in the face-to-face cohort (415/885, 46.9% vs 876/2254, 38.9%, respectively). Apart from lower mean hemoglobin in the full consent group of the eIC cohort (8.5 vs 8.8; P =.0021), the characteristics of the full consenting patients did not differ between the eIC and face-to-face IC cohorts. In the eIC cohort, only age differed between the full consent and the nonresponse group (median 60 vs 56; P =.0002, respectively), whereas in the face-to-face IC cohort, the full consent group seemed healthier (ie, higher hemoglobin, lower glycated hemoglobin [HbA 1c ], lower C-reactive protein levels) than the nonresponse group.
Conclusions: More patients provided full consent using an eIC. In addition, the study population remained broadly similar. The face-to-face IC approach seemed to result in a healthier study population (ie, full consenting patients) than the patients without IC, while in the eIC cohort, the characteristics between consent groups were comparable. Thus, an eIC may lead to a better representation of the target population, increasing the generalizability of results.
Introduction
The use of electronic informed consent (eIC) procedures in clinical research is increasing due to several benefits, including increased enrollment and improved efficiency, by reducing the need for on-site research staff and the associated paperwork [ 1 - 3 ]. eICs have the potential to improve the patient experience (eg, patient understanding and confidence) of the informed consent (IC) process, in part because of the ability to include digital multimedia [ 4 , 5 ]. Alternatively, concerns were raised about whether eIC forms are easily accessible to an elderly population and those with limited digital literacy [ 6 ], making it more difficult to assess whether the patient has fully understood the IC form, one of the requirements for a valid IC [ 7 ]. Standardized best practices for eIC procedures are still lacking [ 5 , 8 ].
In 2014, the University Medical Center (UMC) Utrecht in the Netherlands initiated the Utrecht Cardiovascular Cohort-CardioVascular Risk Management (UCC-CVRM) as a learning health care system (LHS). The UCC-CVRM LHS aims to improve uniform assessment and registration of cardiovascular risk indicators, based on Dutch national guidelines, in electronic health records (EHRs) for all patients referred to the UMC Utrecht for cardiovascular evaluation [ 9 ]. In an LHS, care and research are integrated in such a way that health care activities are continuously analyzed and the knowledge gained from these analyses is used to improve care by changing health care practices [ 10 ]. In the case of UCC-CVRM LHS, a traditional face-to-face IC procedure was used for blood sample storage in a biobank and the reuse of routine care data for scientific research purposes including linkage of data from EHRs to national registries [ 9 ]. In 2020, during the COVID-19 pandemic, the UCC-CVRM steering committee evaluated the study including the IC procedure [ 11 , 12 ]. In short, less than half of the patients who were invited to participate, 41.5% (2378/5730), provided written IC [ 12 ]. Next, patients who did consent differed in clinical characteristics from those nonconsenting or nonresponding, clearly leading to a selection of patients not representable for all eligible patients. For example, consenting patients had a lower cardiovascular disease burden than nonconsenting patients [ 11 , 12 ]. In addition, structured registration of cardiovascular risk management (CVRM) indicators in the EHR was worse compared with consenting patients. This selection is detrimental to an LHS, as the population included in the LHS may be less representative of the target population as a whole [ 11 , 12 ]. Finally, eligible patients were not invited, mainly because of the time-consuming and unsustainable IC procedure due to changes in personnel and changes in priorities during peak periods (eg, the COVID-19 pandemic) [ 13 ].
Therefore, the UCC-CVRM steering committee decided to alter the approach. Identification of eligible patients for the LHS was to be automated and CVRM data, to be assessed regularly in patients at higher cardiovascular risk, were extracted from structured fields in the EHR. To still enable the linkage of this patient information to data from national registries, general practitioners (GPs), and other hospitals, an eIC procedure was piloted. This study aims to evaluate the eIC procedure by studying the response to the IC form. In addition, we aim to assess whether the change in the IC procedure leads to a different study population by investigating potential differences in clinical characteristics between the response categories of the eIC compared with the former face-to-face IC procedure.
We used the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement as a reporting guideline for this study.
Study Setting
Patients visiting the UMC Utrecht for the first time for the evaluation of cardiovascular disease or risk factors were eligible for inclusion in the UCC-CVRM LHS. The full rationale of UCC-CVRM has been described elsewhere [ 9 ]. The eIC pilot was conducted between November 2021 and August 2022. During this period, all patients (18 years and older) visiting the cardiology outpatient clinic for first-time evaluation automatically received an email. This email notified these patients about UCC-CVRM and the associated eIC form that was available for completion in the UMC Utrecht patient portal. The IC procedures of the face-to-face IC and eIC are illustrated in Figure 1 . The full details eIC form presented to the patients in the patient portal are included in Multimedia Appendix 1 .
In both the face-to-face IC and the eIC forms, IC was asked for linkage with national registries, GPs, and other hospitals through the following two statements: (1) I consent to future requests to link with various international or national registries, such as the Central Bureau of Statistics (also known as Statistics Netherlands) where all causes of death are registered, the Dutch Cancer Registration (NKR), where all people with cancer are registered, the National Basic Registration of Hospital Care (LBZ), where all hospital admissions are registered, the Foundation for Pharmaceutical Statistics (SFK), where all people who use medicines are registered, and other regional and national registries. (2) I consent to the retrieval of my medical information from my GP, my pharmacy, and any other hospitals where I have been treated in the past.

Data Collection
We collected data from all patients aged 18 years or older referred to a cardiology outpatient clinic. We used the Utrecht Patient Oriented Database to collect data from the patients who participated in the eIC pilot, referred to as the “eIC cohort.” The Utrecht Patient Oriented Database comprises data on, among others, patient characteristics and laboratory tests for all patients treated at the UMC Utrecht since 2004 [ 14 ]. We collected routine care data related to the patient’s demographics and cardiovascular risk, namely blood pressure, BMI, and laboratory measurements (serum lipids, glycated hemoglobin [HbA 1c ], hemoglobin, and renal function). These data were also collected for the cardiology patients who were invited during the period in which a face-to-face IC procedure was in place, referred to as the “face-to-face IC cohort.” From the face-to-face IC cohort, only patients invited up until December 31, 2019, were included because the COVID-19 pandemic significantly hampered the face-to-face IC procedure.
All measurements were extracted from structured fields in the EHR. Blood pressure values were extracted from the EHR ±7 days from the date of the visit at the cardiology outpatient clinic. For other measurements, the closest value, within ±21 days of the visit date, was extracted. If no measurements were found within these cutoffs, the measurement was considered missing. An overview of missingness per variable is added as Multimedia Appendix 2 . Age was calculated by subtracting the date of the visit from the patient’s date of birth. The estimated glomerular filtration rate was calculated using the Chronic Kidney Disease Epidemiology Collaboration equation and used as a measure of renal function [ 15 ].
Data Analyses
We presented the yield for both the eIC and face-to-face IC cohort as counts and the percentages of patients who, (1) consented to the linkage of their data with their GP, pharmacy, and other hospitals, and linkage with national registries (ie, “full consent”); (2) did not consent for the linkage of their data with their GP, pharmacy, and other hospitals, nor to the linkage with national registries (ie, “nonconsent”); (3) consented to only 1 of the 2; and (4) the percentage of patients who did not respond at all or provided an answer for only 1 of the 2 statements (ie, “nonresponse”). Due to the limited number of observations in some IC response groups (n<25), especially in the eIC cohort, other than the full consent (n=1291) and nonresponse (n=1477) group, further analyses were restricted to the full consent and nonresponse group only.
To assess differences in patient groups, characteristics of the patients with full consent were stratified by cohort (ie, eIC cohort vs face-to-face IC cohort). As a supplement, we also explored the characteristics of the nonresponders by cohort. Finally, we assessed the differences in patient characteristics between the response categories within each cohort (ie, full consent versus nonresponse).
Clinical characteristics were presented as means with corresponding SDs, medians with corresponding interquartile ranges, or counts and percentages, as appropriate. To quantify differences in characteristics between cohorts, or response categories within cohorts, we performed multivariable linear regression analyses, adjusted for age, categorized into 4 categories with an approximately equal number of observations (18 to 47, 48 to 60, 61 to 70, and 71 to 95 years old), and sex. The assumptions of linear regression (eg, approximate normal distribution of the error terms, homoscedasticity of errors) were assessed. Where needed, we used the Box-Cox method to estimate the most appropriate transformation of the dependent variable to stabilize the variance and improve the accuracy of our estimations [ 16 ]. Similarly, multivariable linear regression was used to assess the difference in age (as a continuous variable) between groups, adjusted for sex. Multivariable logistic regression was used to assess the difference in sex between the groups (ie, between the 2 cohorts and between the response categories within each cohort), adjusted for age (categorized into 4 categories with an approximately equal number of observations). As a sensitivity analysis, we repeated the adjusted regression analyses with age as a continuous variable, to assess whether the categorization led to different results.
We used the Bonferroni correction to reduce the risk of a type I error resulting from the multiple tests [ 17 ]. Thus, the α that we considered as cutoff, .05, was divided by the number of analyses (N=13) performed per comparison. Therefore, a P value ≤.0038 was considered statistically significant.
All statistical analyses were performed using R software (version 4.0.5; The R Foundation) [ 18 ].
Ethical Considerations
We obtained an additional ethical waiver (number 19/641) from the Research Ethics Committee Utrecht to examine the characteristics of patients in all IC response categories. Patients who objected to the use of their clinical data for research purposes via the UMC Utrecht opt-out procedure were excluded from this study. Data were pseudonymized and the patients did not receive any compensation for their participation in this study.
Yield of the IC Procedure
In total, 3139 patients participated in this study, of whom 885 (28.2%) participated in the eIC pilot cohort and 2254 (71.8%) in the face-to-face IC cohort ( Multimedia Appendix 3 ). Of all patients from the eIC cohort, 49.9% (442/885) completed the eIC form, 50.1% (443/885) did not respond. Of all patients who completed the eIC form, we obtained full consent for linkage with GPs, hospitals, and national registries from 93.9% (415/442) of the patients. In the face-to-face IC cohort, 54.1% (1220/2254) of all patients completed the IC form, and 45.9% (1034/2254) patients did not respond. The percentage of responding patients with full consent was higher in the eIC cohort as compared with the face-to-face IC cohort (415/442, 93.9% vs 876/1220, 71.8%, respectively).
Differences in Characteristics Between the eIC and Face-to-Face Cohorts
Overall, fully consenting patients had similar patient characteristics ( Table 1 ). Adjusted for sex and age, the eIC cohort had lower hemoglobin levels and higher HbA 1c levels than the face-to-face IC cohort, reaching the multiple testing threshold for statistical significance for hemoglobin ( P =.0021).
Similarly, we compared the (clinical) characteristics of the nonresponding patients between cohorts, shown in Multimedia Appendix 4 . Adjusted for sex, the nonresponders of the eIC cohort were significantly younger and had, adjusted for age and sex, lower c-reactive protein values than the nonresponders of the face-to-face cohort. No other differences were observed.
| Variable | Full consent | value | |||||
| eIC (n=415) | F2F IC (n=876) | ||||||
| Age (years), median (IQR) | 60.0 (48.0-70.0) | 61.0 (50.0-69.0) | .2529 | ||||
| Male | 237 (57.1) | 476 (54.3) | — | ||||
| Female | 178 (42.9) | 400 (45.7) | .3239 | ||||
| BMI (kg/m ), mean (SD) | 26.6 (5.2) | 26.7 (5.7) | .8981 | ||||
| SAP (mm Hg), mean (SD) | 132.1 (19.4) | 137.6 (19.6) | .0586 | ||||
| Hemoglobin (mmol/L), mean (SD) | 8.5 (1.4) | 8.8 (0.9) | .0021 | ||||
| HbA (mmol/mol), median (IQR) | 37.5 (34.0-44.0) | 37.0 (34.0-40.0) | .0454 | ||||
| Cholesterol (mmol/L), mean (SD) | 4.8 (1.2) | 5.1 (1.3) | .1266 | ||||
| HDL -cholesterol (mmol/L), mean (SD) | 1.3 (0.4) | 1.4 (0.4) | .0676 | ||||
| LDL -cholesterol (mmol/L), mean (SD) | 2.7 (1.1) | 2.9 (1.1) | .1086 | ||||
| Triglycerides (mmol/L), median (IQR) | 1.7 (1.1-2.6) | 1.6 (1.0-2.1) | .3023 | ||||
| CRP (mg/L), median (IQR) | 2.0 (0.5-10.0) | 2.6 (1.1-8.5) | .6666 | ||||
| Creatinine (µmol/L), median (IQR) | 76.0 (64.2-94.0) | 74.0 (64.0-88.0) | .7760 | ||||
| eGFR CKD-EPI (mL/min/1.73 m ), mean (SD) | 83.3 (23.1) | 84.5 (22.3) | .7068 | ||||
a eIC: electronic informed consent.
b F2F IC: face-to-face informed consent.
c Reference group.
d SAP: systolic arterial blood pressure.
e HbA 1c : glycated hemoglobin.
f HDL: high-density lipoprotein.
g LDL: low-density lipoprotein.
h CRP: c-reactive protein.
i eGFR CKD-EPI: estimated glomerular filtration rate calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.
Differences in Characteristics Between Response Categories
Within each cohort, we assessed whether there were differences in characteristics between the response categories (ie, full consent vs nonresponse). In the eIC cohort, the nonresponse group was significantly younger than the full consent group ( Table 2 ). Other than that, the clinical characteristics of the full consent group were similar to those of the nonresponse group.
More differences were found between the response categories of the face-to-face IC cohort. Adjusted for age and sex, patients in the full consent group had higher hemoglobin, but lower HbA 1c and c-reactive protein values than the nonresponse group ( Table 3 ).
| Variable | Full consent (n=415) | Nonresponse (n=443) | value | |
| Age (years), median (IQR) | 60.0 (48.0-70.0) | 56.0 (28.0-72.0) | .0002 | |
| Male | 237 (57.1) | 222 (50.1) | — | |
| Female | 178 (42.9) | 221 (49.9) | .0420 | |
| BMI (kg/m ), mean (SD) | 26.6 (5.2) | 26.0 (4.9) | .3673 | |
| SAP (mm Hg), mean (SD) | 132.1 (19.4) | 130.4 (19.6) | .4168 | |
| Hemoglobin (mmol/L), mean (SD) | 8.5 (1.4) | 8.4 (1.3) | .2397 | |
| HbA (mmol/mol), median (IQR) | 37.5 (34.0-44.0) | 37.5 (34.0-40.2) | .1940 | |
| Cholesterol (mmol/L), mean (SD) | 4.8 (1.2) | 4.6 (1.5) | .2852 | |
| HDL -cholesterol (mmol/L), mean (SD) | 1.3 (0.4) | 1.2 (0.5) | .3371 | |
| LDL -cholesterol (mmol/L), mean (SD) | 2.7 (1.1) | 2.6 (0.9) | .9304 | |
| Triglycerides (mmol/L), median (IQR) | 1.7 (1.1-2.6) | 1.4 (1.1-2.0) | .4167 | |
| CRP (mg/L), median (IQR) | 2.0 (0.5-10.0) | 3.0 (0.5-12.0) | .5922 | |
| Creatinine (µmol/L), median (IQR) | 76.0 (64.2-94.0) | 79.0 (64.0-100.5) | .0897 | |
| eGFR CKD-EPI (mL/min/1.73 m ), mean (SD) | 83.3 (23.1) | 82.0 (30.7) | .1103 | |
a Reference group.
b SAP: systolic arterial blood pressure.
c HbA 1c : glycated hemoglobin.
d HDL: high-density lipoprotein.
e LDL: low-density lipoprotein.
f CRP: c-reactive protein.
g eGFR CKD-EPI: estimated glomerular filtration rate calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.
| Variable | Full consent (n=876) | Nonresponse (n=1034) | value | |
| Age, median (IQR) | 61.0 (50.0-69.0) | 61.0 (48.0-71.0) | .9461 | |
| Male | 476 (54.3) | 552 (53.4) | — | |
| Female | 400 (45.7) | 482 (46.6) | .7859 | |
| BMI (kg/m ), mean (SD) | 26.7 (5.7) | 26.2 (5.5) | .1063 | |
| SAP (mm Hg), mean (SD) | 137.6 (19.6) | 136.3 (22.0) | .1093 | |
| Hemoglobin (mmol/L), mean (SD) | 8.8 (0.9) | 8.3 (1.2) | <.0001 | |
| HbA (mmol/mol), median (IQR) | 37.0 (34.0-40.0) | 38.0 (34.0-42.0) | .0001 | |
| Cholesterol (mmol/L), mean (SD) | 5.1 (1.3) | 5.0 (1.4) | .4493 | |
| HDL -cholesterol (mmol/L), mean (SD) | 1.4 (0.4) | 1.3 (0.4) | .0898 | |
| LDL -cholesterol (mmol/L), mean (SD) | 2.9 (1.1) | 2.9 (1.1) | .2754 | |
| Triglycerides (mmol/L), median (IQR) | 1.6 (1.0-2.1) | 1.6 (1.0-2.4) | .0435 | |
| CRP (mg/L), median (IQR) | 2.6 (1.1-8.5) | 8.1 (2.0-38.2) | <.0001 | |
| Creatinine (µmol/L), median (IQR) | 74.0 (64.0-88.0) | 75.0 (63.0-92.0) | .4361 | |
| eGFR CKD-EPI (mL/min/1.73 m ), mean (SD) | 84.5 (22.3) | 81.3 (29.0) | .0946 | |

Sensitivity Analysis
We repeated the regression analyses adjusted for sex and age. In these regression analyses, age was maintained continuous instead of categorized, to assess whether the categorization of age led to different results. The results were similar ( Multimedia Appendix 5 ).
Principal Results
We showed that by using an eIC in an LHS, patients more often provided full consent to link their data to national registries, GPs, and other hospitals compared with a face-to-face IC procedure. The clinical characteristics of patients with full consent remained largely similar after changing the IC procedure to an eIC. Except for age, we did not find any differences between the response categories of the eIC cohort, whereas in the face-to-face cohort, several differences were found. These differences potentially suggest a higher (cardiovascular) disease burden in the nonresponse group compared with the full consent group, indicative of a potentially more pronounced selection in the face-to-face approach.
A possible explanation for the differences in characteristics between the response categories in the face-to-face cohort is that patients may have been too ill or frail to attend the physical appointment with the research nurse to discuss and sign the IC form, resulting in nonresponse. The inability to attend the appointment was probably less of an issue in the eIC cohort, as patients were able to access the eIC form remotely. The finding suggests that the use of eIC results in a study population (ie, those who give full consent) that is more representative of the full target population. Our findings agree with a previous study showing that providing computer-based clinical study information leads to more willingness to participate [ 19 ], as the increased willingness to participate is consistent with the higher full consent rates found in the eIC group compared with the face-to-face IC group in our study.
Frequently Mentioned Challenges of eICs in the Literature
Concerns have been raised about whether consent given via an eIC is truly an “informed” consent [ 8 ]. According to the principles of the Declaration of Helsinki [ 7 ], potential participants must be adequately informed about various aspects of the study, such as its purpose, sources of funding, the anticipated benefits and potential risks, and the right to refuse or withdraw consent to participate without giving a reason [ 7 ]. According to previous research, comprehension assessment is more challenging when an eIC procedure is used as there is no direct interaction between the potential participant and researcher [ 6 ]. As a result, patients might provide consent without fully understanding what they are consenting to, or, conversely, patients may be less likely to consent because of the lack of personal interaction with the researcher or clinician, especially those who were already doubtful about participating in the first place. However, our findings indicate that the latter might not have been the case in our pilot study, as we observed a higher percentage of patients with full consent in the eIC cohort compared with the face-to-face IC cohort.
Another frequently mentioned concern is that studies using an eIC procedure could become inaccessible to patients who lack the digital literacy needed to access and understand the eIC form [ 6 ]. In 2021, the Netherlands had the highest percentage (ie, 79%) of 17- to 74-year-olds with at least basic digital skills in Europe [ 20 ]. Therefore, incomprehension of the eIC due to limited digital literacy may appear less of an issue in our study. However, the percentage of persons with basic digital skills varied considerably by age, with older people being less literate [ 20 ]. A sensitivity analysis showed that the age distribution of responding patients was similar between the eIC and the face-to-face approach ( Multimedia Appendix 6 ), indicating that the eIC was not less accessible than the face-to-face IC for certain age groups. However, accessibility may be an issue for geriatric patients, who are generally older than cardiology patients and often have geriatric syndromes that sometimes affect comprehension and literacy [ 21 ]. These syndromes generally make it difficult to obtain IC from the elderly [ 21 ]. eIC could, therefore, also be seen as an opportunity. Unlike paper-based ICs, multiple formats can be used to inform the patient about the purpose of the eIC and to provide technical support, for example, by using instructional videos or audio. The use of multiple formats in IC forms for the elderly has been recommended by, among others, Barron et al [ 22 ]. Furthermore, UCC-CVRM’s eIC form is available in UMC Utrecht’s long-existing patient portal. In the portal, patients have the opportunity to, among others, ask questions to their clinician via an e-consult, which can be used if parts of the eIC are unclear [ 23 ]. Another possibility would be a hybrid format, allowing patients who prefer correspondence by regular mail to respond using a paper-based IC form. However, it is questionable whether this would be helpful and it would negate the positive aspects of the eIC highlighted in this study (eg, less pronounced selection).
Legislation and Regulation Regarding eIC
Since July 2022, eICs have been permitted in the Netherlands when certain conditions are met [ 24 ]. A total of 6 conditions are described in the guideline written by the Central Committee on Research Involving Human Subjects (Centrale Commissie Mensgebonden Onderzoek) and the Dutch Association of Medical Research Ethics Committees (Nederlandse Vereniging voor Medisch-Ethische toetsingscommissies) [ 25 ]. The most important conditions are (1) eIC must be appropriate for the study, meaning that the study is associated with low potential risk and burden for the patient, (2) the eIC process must be sufficiently reliable and confidential, guaranteed by an electronic system that is compliant to the Dutch General Data Protection Regulation (UAVG in Dutch) and ensures the validity of the electronic signatures, and (3) the eIC procedure must be described in the study protocol [ 24 , 25 ]. The implementation of an eIC seems appropriate in the case of the UCC-CVRM, as no potential risk or burden for the patient is involved. Furthermore, in the eIC of the UCC-CVRM, data security, identity verification, and the validity of the electronic signature are ensured by the Dutch digital ID, an identification method for accessing web-based services [ 26 ]. Regarding the third condition, an amendment to the UCC-CVRM approach, including the eIC, was submitted and approved by the Research Ethics Committee.
Clinical Implications
Based on the results of our study, the use of eIC to obtain IC might be a sustainable and adequate way to enable researchers to link with national registries, GPs, and other hospitals. The use of the eIC seemed to have resulted in a population with consent that is more similar to the target population compared with the face-to-face IC, which is of great importance in an LHS. Results from the LHS would be more generalizable to the target population, namely to all patients at higher cardiovascular risk. Yet, one may argue whether ≈50% response to both the electronic and face-to-face IC for an LHS approach is sufficient. In addition, it should be noted that the extractability of CVRM indicators from structured fields in the EHR was much lower in the eIC cohort compared with the face-to-face IC cohort. Groenhof et al [ 13 ] showed that the former, protocolized, face-to-face UCC-CVRM approach led to more systematic registration of the cardiovascular risk profile in the EHR, which had a positive effect on CVRM guideline adherence in consenting patients, compared with the situation before UCC-CVRM was introduced [ 13 ]. The substantial missingness in the eIC cohort of our study may suggest that these improvements are at risk when the approach is automated, as deviations from the initial protocol are made, potentially leading to suboptimal CVRM in clinical care.
Exploring the views and experiences of patients could help to further improve the eIC form. Therefore, we recommend further qualitative research into the accessibility and understandability of eICs used for similar purposes and in similar settings as the UCC-CVRM LHS from a patient’s perspective.
Strengths and Limitations
To the best of our knowledge, we are among the first to investigate the differences in clinical patient characteristics between response categories of an eIC compared with those of a traditional face-to-face IC, specifically in the context of a cardiovascular LHS in a large sample of patients. Our uniqueness, however, limits the ability to compare our findings to the literature, as most research on eIC has focused on user perspectives, experiences, and the ethical considerations of eICs. For example, Chen et al [ 5 ] showed that in most included studies, participants had a better understanding of the information when using an eIC compared with a traditional paper-based face-to-face IC, while others found no difference [ 5 ]. Nevertheless, they [ 5 ] and others [ 2 , 6 , 27 ] indicated that face-to-face interaction should remain part of the IC process, especially for more complex and higher-risk studies. However, as the UCC-CVRM LHS is not a complex or high-risk study, the face-to-face interaction may be less necessary. Furthermore, the nonresponders in the eIC cohort may not be fully comparable to the nonresponders in the face-to-face IC cohort because, in the eIC cohort, patients received the eIC after their appointment at the cardiology outpatient clinic, whereas in the face-to-face IC cohort, cardiology patients were identified as eligible and received information about the UCC-CVRM LHS prior to their appointment. This means that patients who, for example, canceled their appointment at the last minute would still be included in the face-to-face cohort as nonresponders. It may be that patients who did not attend their appointment at all had different characteristics to those who attended but did not respond to the eIC, potentially affecting the validity of the comparisons made. Finally, the eIC form was piloted in the patient population of the cardiology outpatient clinic only. Although our results indicated that there were only minor differences (ie, hemoglobin) between patients providing full consent using the eIC compared with the face-to-face IC, it remains to be seen whether this would still be the case after implementation of the eIC in other clinical departments.
Conclusions
To conclude, our findings suggest that using an eIC may lead to a better representation of the target population by consenting patients. This increases the generalizability of results from studies using the data collected within the LHS from consenting patients.
Acknowledgments
The Utrecht Cardiovascular Cohort-Cardiovascular Risk Management (UCC-CVRM) is primarily financed by the University Medical Center (UMC) Utrecht (contact information of UCC-CVRM is [email protected]). AGMZ was supported by a grant from the European Union’s Horizon 2020 research and innovation program (grant agreement number 101017331; ODIN). MJH and RvdG were supported by the ZonMw, ETHMIRE project (grant agreement number 91217027). The funding sources were not involved in the design of the study, the analysis and interpretation of the data, the writing of the manuscript, and the decision to submit the manuscript for publication. Members of the UCC-CVRM study group were the following: GJ de Borst, Department of Vascular Surgery; ML Bots (chair), Julius Center for Health Sciences and Primary Care; M Hollander, Julius Center for Health Sciences and Primary Care; MH Emmelot, Department of Geriatrics; PA de Jong, Department of Radiology; AT Lely, Department of Obstetrics/Gynecology; HM Nathoe, Department of Cardiology; IE Hoefer, Central Diagnostic Laboratory; NP van der Kaaij, Department of Cardiothoracic Surgery; YM Ruigrok, Department of Neurology; and MC Verhaar, Department of Nephrology and Hypertension, FLJ Visseren, Department of Vascular Medicine, University Medical Center Utrecht and Utrecht University.
Authors' Contributions
AGMZ, HMN, WWvS, MLB, SH, and RWMV contributed to the conceptualization of the project. AGMZ, RWMV, SH, WWvS, and MLB contributed to the methodology of the project. AGMZ analyzed the data and drafted the manuscript. AGMZ, MJH, RvdG, HMN, WWvS, MLB, SH, and RWMV contributed substantially to the interpretation of the data. The final manuscript was critically reviewed and edited by all authors. Approval of the final manuscript was obtained by all authors.
Conflicts of Interest
None declared.
The electronic informed consent form as presented in the patient portal of the UMC (University Medical Center) Utrecht (translated from Dutch to English).
Missingness per variable in count and percentage, by cohort and informed consent response strata.
Yield (ie, response to the informed consent invitation), by type of informed consent. eIC: electronic informed consent; GP: general practitioner.
Differences between patients who did not respond, by cohort, adjusted for age and sex.
Results of the sensitivity analysis in which age is treated as a continuous variable instead of categorical variable.
Age distribution of patients who completed the informed consent form, stratified by cohort.
- Simon CM, Klein DW, Schartz HA. Traditional and electronic informed consent for biobanking: a survey of U.S. biobanks. Biopreserv Biobank. 2014;12(6):423-429. [ CrossRef ] [ Medline ]
- Skelton E, Drey N, Rutherford M, Ayers S, Malamateniou C. Electronic consenting for conducting research remotely: a review of current practice and key recommendations for using e-consenting. Int J Med Inform. 2020;143:104271. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Phillippi JC, Doersam JK, Neal JL, Roumie CL. Electronic informed consent to facilitate recruitment of pregnant women into research. J Obstet Gynecol Neonatal Nurs. 2018;47(4):529-534. [ CrossRef ] [ Medline ]
- Boutin NT, Mathieu K, Hoffnagle AG, Allen NL, Castro VM, Morash M, et al. Implementation of electronic consent at a biobank: an opportunity for precision medicine research. J Pers Med. 2016;6(2):17. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Chen C, Lee P, Pain KJ, Delgado D, Cole CL, Campion TR. Replacing paper informed consent with electronic informed consent for research in academic medical centers: a scoping review. AMIA Jt Summits Transl Sci Proc. 2020;2020:80-88. [ FREE Full text ] [ Medline ]
- Yusof MYPM, Teo CH, Ng CJ. Electronic informed consent criteria for research ethics review: a scoping review. BMC Med Ethics. 2022;23(1):117. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Declaration of helsinki - ethical principles for medical research involving human subjects. World Medical Association. 2022. URL: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ [accessed 2023-05-05]
- Lunt H, Connor S, Skinner H, Brogden G. Electronic informed consent: the need to redesign the consent process for the digital age. Intern Med J. 2019;49(7):923-929. [ CrossRef ] [ Medline ]
- Asselbergs FW, Visseren FL, Bots ML, de Borst GJ, Buijsrogge MP, Dieleman JM, et al. Uniform data collection in routine clinical practice in cardiovascular patients for optimal care, quality control and research: the Utrecht cardiovascular cohort. Eur J Prev Cardiol. 2017;24(8):840-847. [ CrossRef ] [ Medline ]
- Wouters RHP, van der Graaf R, Voest EE, Bredenoord AL. Learning health care systems: highly needed but challenging. Learn Health Syst. 2020;4(3):e10211. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Groenhof TKJ, Mostert M, Lea NC, Haitjema S, de Vries MC, van Dijk WB, et al. How traditional informed consent impairs inclusivity in a learning healthcare system: lessons learned from the Utrecht cardiovascular cohort. J Clin Epidemiol. 2022;149:190-194. [ CrossRef ] [ Medline ]
- Zondag AGM, Groenhof TKJ, van der Graaf R, van Solinge WW, Bots ML, Haitjema S, et al. UCC-CVRM study group. Asking informed consent may lead to significant participation bias and suboptimal cardiovascular risk management in learning healthcare systems. BMC Med Res Methodol. 2023;23(1):98. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Groenhof TKJ, Haitjema S, Lely AT, Grobbee DE, Asselbergs FW, Bots ML, et al. UCC-CVRMUPOD Study groups. Optimizing cardiovascular risk assessment and registration in a developing cardiovascular learning health care system: women benefit most. PLOS Digit Health. 2023;2(2):e0000190. [ FREE Full text ] [ CrossRef ] [ Medline ]
- ten Berg MJ, Huisman A, van den Bemt PMLA, Schobben AFAM, Egberts ACG, van Solinge WW. Linking laboratory and medication data: new opportunities for pharmacoepidemiological research. Clin Chem Lab Med. 2007;45(1):13-19. [ CrossRef ] [ Medline ]
- Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604-612. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Glen S. Box cox transformation: definition, examples. Statistics How To. URL: https://www.statisticshowto.com/probability-and-statistics/normal-distributions/box-cox-transformation/ [accessed 2023-08-09]
- VanderWeele TJ, Mathur MB. Some desirable properties of the bonferroni correction: is the bonferroni correction really so bad? Am J Epidemiol. 2019;188(3):617-618. [ FREE Full text ] [ CrossRef ] [ Medline ]
- R: a language and environment for statistical computing. R foundation for statistical computing. 2021. URL: https://www.R-project.org/ [accessed 2022-08-31]
- Karunaratne AS, Korenman SG, Thomas SL, Myles PS, Komesaroff PA. Improving communication when seeking informed consent: a randomised controlled study of a computer-based method for providing information to prospective clinical trial participants. Med J Aust. Apr 2010;192(7):388-392. [ CrossRef ] [ Medline ]
- Dutch digital skills at the top in Europe. CBS. 2022. URL: https://www.cbs.nl/en-gb/news/2022/19/dutch-digital-skills-at-the-top-in-europe [accessed 2023-04-20]
- Cherubini A, Gasperini B. How to increase the participation of older subjects in research: good practices and more evidence are needed! Age Ageing. 2017;46(6):878-881. [ CrossRef ] [ Medline ]
- Barron JS, Duffey PL, Byrd LJ, Campbell R, Ferrucci L. Informed consent for research participation in frail older persons. Aging Clin Exp Res. 2004;16(1):79-85. [ CrossRef ] [ Medline ]
- My UMC Utrecht patient portal. UMC Utrecht. URL: https://www.umcutrecht.nl/nl/inloggen-patientenportaal?lang=en [accessed 2023-08-10]
- Consent: on paper or electronic (in Dutch only). CCMO. URL: https://tinyurl.com/bdzach6u [accessed 2023-04-11]
- Guide to granting electronic consent for participation in medical-scientific research (in Dutch only). CCMO, NVMETC. 2022. URL: https://www.ccmo.nl/metcs/publicaties/publicaties/2022/08/31/handreiking-elektronische-toestemmingsverlening [accessed 2023-04-11]
- What is DigiD? Netherlands Worldwide. 2024. URL: https://www.netherlandsworldwide.nl/digid-abroad/what-is-digid [accessed 2023-07-26]
- De Sutter E, Zaçe D, Boccia S, Di Pietro ML, Geerts D, Borry P, et al. Implementation of electronic informed consent in biomedical research and stakeholders' perspectives: systematic review. J Med Internet Res. 2020;22(10):e19129. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
| cardiovascular risk management |
| electronic health record |
| electronic informed consent |
| general practitioner |
| glycated hemoglobin |
| informed consent |
| learning health care system |
| Strengthening the Reporting of Observational Studies in Epidemiology |
| Utrecht Cardiovascular Cohort-Cardiovascular Risk Management |
| University Medical Center |
Edited by A Mavragani; submitted 29.11.23; peer-reviewed by CMJ Wong, H Kondylakis; comments to author 28.02.24; revised version received 15.04.24; accepted 10.05.24; published 11.07.24.
©Anna G M Zondag, Marieke J Hollestelle, Rieke van der Graaf, Hendrik M Nathoe, Wouter W van Solinge, Michiel L Bots, Robin W M Vernooij, Saskia Haitjema, UCC-CVRM study group. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 11.07.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research (ISSN 1438-8871), is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
- There are no suggestions because the search field is empty.
Careers Developers Support 日本語
Building Blocks of Efficient IMP Supply and Distribution Strategies
Get our content delivered to your inbox.

In an era of constant growth in the scale and complexity of clinical trials, planning properly for efficient manufacturing and distribution of investigational medicinal products (IMPs) is more important than ever. With many constraints and dependencies inherent in clinical supply chain management, waste, overages, or shortages are costly propositions in terms of overall study schedules and budgets. Consider the driving trends in clinical research:
- Research takes place at more sites and in more countries than ever before
- Study designs are increasingly complex, with many different treatment arms and drug types
- Movement restrictions and regulatory complexities related to the global coronavirus pandemic add new logistical difficulties
- Newer models of study conduct emphasize the location of participants rather than sites
All of this can make studies involving products that are expensive, limited in supply, or short on shelf life such as those for oncology, much more difficult. Signant’s Clinical Supplies (CS) team spearheads the technology and logistical strategy for thousands of such research programs, and offers these first-hand insights to help sponsors build risk mitigation strategies.
1. Include the clinical supplies team early in study planning
While this may seem obvious, clinical supply chain considerations can easily get lost in the fold when study teams are focused on the many other aspects of clinical research design, planning, and execution. However, it is often the most critical link in the chain. If there is a delay upstream, it falls to the CS team to make up for lost time and flawlessly execute extremely complicated and interdependent operational processes. Allow the CS team to establish the strategy and perform risk assessments early.
2. Develop a granular picture of supply needs
When forecasting supply needs for a study, sponsors may opt to plan around “worst case” assumptions, but this model does not account for variables that ultimately dictate the actual needs of an active trial and can result in shortages or overages. Once underway, be sure to deploy an RTSM that can manage inventory in a way that accounts for each patient’s specific position in the trial based on visit schedules, visit-specific dispensing windows for each kit type, country-specific lead times based on sites’ locations, country-specific lookout windows, and varying do not ship values. You can use this data to ship earlier-dated study drugs for shorter visits and longer-dated materials for longer visits. In our experience, this approach reduces supply waste due to expiry events.
3. Take a campaigned approach to re-supply and distribution
Often, formulations and packaging designs can change after a study has launched, prompting the need to update kit types mid-trial. Initial manufacturing and labeling plans are created prior to launch based on anticipated enrollment rates. If your plan does not account for the factors outlined in number two above, there is high risk of interrupting the trial or wasting materials when not enough or too much material is produced and shipped. A campaigned re-supply plan allows clinical supplies teams to manufacture fewer kits initially. This prevents waste but it requires granular supply predictions to allow ample time for production and distribution.
4. Consider a pooling strategy
Drug pooling at the depot-level allows products to be shared across studies that utilize the same compound. This drastically reduces the amount of inventory needed, simplifies logistics and administration, and provides study teams with the flexibility needed to direct supply to sites or patients dynamically in response to factors such as staggered study timelines, unexpected delays, or changing priorities.
5. Know your RTSM system well, or partner with those who do
Everything is carried out in the RTSM system – from managing patient demand to building out the study’s logistics and resupply strategy – it keeps operations running smoothly. Therefore, it’s imperative to have both the technology as well as specialized expertise support complex clinical supply manufacturing and distribution operations.
As clinical trials become more complex and investigational medicinal products become more expensive, sponsors benefit from employing more advanced systems that can handle the inherent challenges of today’s clinical research and that are poised for innovation to accommodate new challenges in the future.
To learn about Signant’s innovative SmartSignalsTM RTSM , contact us to speak to our experts.
Similar posts
Webinar recap: how edc can support modern clinical trials , webinar recap: applied ai for enhanced clinical data operations, clinical research technology: telemedicine vs video conferencing, get notified on new marketing insights.
Here mention the benefits of subscribing
- Open access
- Published: 02 July 2024
Does an instructional video as a stand-alone tool promote the acquisition of practical clinical skills? A randomised simulation research trial of skills acquisition and short-term retention
- Thomas Ott ORCID: orcid.org/0000-0001-7510-7679 1 ,
- Tim Demare 1 ,
- Julia Möhrke 1 ,
- Saskia Silber 1 ,
- Johannes Schwab 1 ,
- Lukas Reuter 1 ,
- Ruben Westhphal 2 ,
- Irene Schmidtmann 2 ,
- Sven-Oliver Dietz 3 ,
- Nina Pirlich 1 ,
- Alexander Ziebart 1 &
- Kristin Engelhard 1
BMC Medical Education volume 24 , Article number: 714 ( 2024 ) Cite this article
141 Accesses
Metrics details
The effectiveness of instructional videos as a stand-alone tool for the acquisition of practical skills is yet unknown because instructional videos are usually didactically embedded. Therefore, we evaluated the acquisition of the skill of a humeral intraosseous access via video in comparison to that of a self-study with an additional retention test.
After ethical approval, we conducted two consecutive studies. Both were designed as randomised controlled two-armed trials with last-year medical students as independent samples at our institutional simulation centre of a tertiary university hospital centre. In Study 1, we randomly assigned 78 participants to two groups: Vid-Self participants watched an instructional video as an intervention, followed by a test, and after seven days did a self-study as a control, followed by a test. Self-Vid ran through the trial in reverse order.
In Study 2, we investigated the influence of the sequence of the two teaching methods on learning success in a new sample of 60 participants: Vid-Self watched an instructional video and directly afterward did the self-study followed by a test, whereas Self-Vid ran through that trial in reverse order.
In Studies 1 and 2, the primary outcome was the score (worst score = 0, best score = 20) of the test after intervention and control. The secondary outcome in Study 1 was the change in score after seven days.
Study 1: The Vid-Self (Participants n = 42) was superior to the Self-Vid ( n = 36) (mean score 14.8 vs. 7.7, p < 0.001). After seven days, Self-vid outperformed Vid-Self (mean score 15.9 vs. 12.5, p < 0.001).
Study 2: The Vid-Self ( n = 30) and Self-Vid ( n = 30) scores did not significantly differ (mean 16.5 vs. mean 16.5, p = 0.97).
An instructional video as a stand-alone tool effectively promotes the acquisition of practical skills. The best results are yielded by a combination of an instructional video and self-study right after each other, irrespective of sequence.
Trial registrations
ClinicalTrials.gov: NCT05066204 (13/04/2021) (Study 1) and NCT04842357 (04/10/2021) (Study 2).
Peer Review reports
Instructional videos
Instructional videos are increasingly applied in medical education.[ 1 , 2 , 3 , 4 ] The advantage of instructional videos, in contrast to lectures and face-to-face teaching, is greater flexibility in learning when provided independently of time.[ 1 , 2 , 5 ] The need for distance learning during the COVID-19 pandemic as well as the aspired individualisation and flexibility of learning within curricula foster the intensified expansion of online teaching and particularly instructional videos.[ 6 , 7 , 8 ] Instructional videos have a positive effect on knowledge.[ 9 ] However, their impact on the acquisition of practical skills is controversial due to inconsistent results.[ 10 , 11 , 12 , 13 , 14 ] Moreover, previous studies evaluated instructional videos in comparison to face-to-face teaching, or the videos were didactically embedded, which means that they were also implemented to tutor practical training and were applied repetitively.[ 10 , 11 , 12 ] To our knowledge, no study has focused on instructional videos as a stand-alone tool without didactic embedding. If instructional videos prove to be effective as stand-alone tools, crucial implications could be deduced for their deliberate application in medical school concerning distance learning, standardisation and flexibility.
- Intraosseous access
To evaluate the value of an instructional video as a stand-alone tool on technical skills acquisition, two factors must be considered. First, it is advantageous to use a procedure that is essential for patient care and that can be devided into well-defined steps. Second, it should be a procedure that has received little attention in curricula to reduce bias concerning previous experience of the participants. [ 15 , 16 , 17 ] Therefore, we chose to apply intraosseous access (IOA) to the humeral head. IOAs show high success rates in patients and can be effectively trained using skill trainers.[ 18 , 19 , 20 , 21 , 22 ] For emergencies, the application of an IOA is most common at the proximal tibial plateau and less common at the humeral head.[ 20 , 23 ] In the case of contraindications to accessing the tibia, a humeral IOA must be mastered as an alternative. Interestingly, humeral IOA training has received less attention in the literature than tibial IOA training.[ 19 , 24 ] Therefore, we produced a ten-minute instructional video on humeral IOA for adult emergency patients and evaluated its effect on students.[ 25 ].
In Study 1, we evaluated the effect of this video by comparing the intervention ‘ INSTRUCTIONAL video’ to the control ‘self-study’ on the acquisition of the skill in two study groups. The performance was quantified by a test that results in a score. Our null hypothesis with respect to the primary endpoint was as follows: The group that watched an instructional video did not differ in score from the group that did self-study at the same time. To evaluate skill retention as a secondary endpoint and to ensure the same overall training experience for both groups, we repeated that trial seven days later in reverse order of both groups. The results of the secondary endpoints of Study 1 yielded findings that are described below and are worthy of further evaluation. Therefore, six months later, we recruited a new sample with similar demographic characteristics and defined this new investigation as Study 2 . In this study, the instructional video and self-study were conducted directly after each other, and participants were tested directly afterwards. Only the order of the teaching methods differed between the two groups. The null hypothesis was formulated as follows: The group that watched an instructional video before self-study did not differ in score from the group that watched an instructional video after self-study.
Ethical aspects
The responsible ethics committee (Ethical Review Committee of the State Chamber of Physicians of Rhineland-Palatinate, Deutschhausplatz 3, 55,116 Mainz, Germany; Chairperson: Professor S. Letzel) approved Study 1 on 29. April 2021 under 2021–15807 and Study 2 on 21. October 2021 under the number 2021–16112. Participation was voluntary, and written informed consent was signed before participation.
Study design
We conducted two prospective randomised controlled two-armed simulation-based research studies as investigator-initiated trials with independent samples, aiming for a 1:1 ratio concerning the number of participants in each group. Study 1 included three points in time, and Study 2 included two points in time (Fig. 1 a, b).

a CONSORT flow chart of Study 1. In Study 1, the Self-Vid group first had to complete a self-assessment (T0), then had to perform the self-study and was tested afterwards, followed by a second self-assessment (T1). After seven days, the group watched the instructional video, was tested, and had to repeat the self-assessment for the third time (T2). The Vid-Self group first completed a self-assessment (T0) and then watched the instructional video, followed by the test and the second self-assessment (T1). After seven days, the group performed the self-study, was tested, and then, the self-assessment was repeated for the last time (T2). b CONSORT flow chart of Study 2. In Study 2, both groups had to complete a self-assessment, and then the instructional video and self-study were conducted in immediate succession according to group assignment. After that, a self-assessment was performed again
Participants, previous experience and setting
We recruited 78 last-year medical students for Study 1 and an additional 60 students for Study 2. The studies were conducted during the mandatory institutional final year training at our institutional simulation centre. One year before this training, all participants attended a curricular 20-min session of face-to-face practical training without video presentation or standardised didactic conception to a maximum of five students at a time concerning IOA located in the tibia; students applied the device several times, but without a defined number of attempts. The same device and skill trainer were used in the present study.
Study 1 was conducted in May and June, and Study 2 was conducted in November and December 2021.
Intraosseous equipment
We used the Arrow EZ-IO Intraosseous Vascular Access System (Teleflex Medical Europe Ltd., Athlone, Ireland) with cannulas of three sizes. As a skill trainer, we used the EZ-IO humeral training bone (Teleflex Medical Europe Ltd., Athlone, Ireland) for a maximum of 5 attempts. As all participants had undergone curricular IOA-training one year before the study no further familiarisation was deemed necessary and hence none was provided.
Measuring tools
The test was videotaped for evaluation. Participants were put in front of a video camera (Lumifix F2000, Panasonic, Kadoma, Japan) that pointed from the participant´s shoulder to a table containing the IOA equipment. First, participants demonstrated and explained the location of humeral IOA on their own extremity; they wore scrubs to do this. Then, the participants prepared the equipment and performed the IOA in the skill trainer. The performance of the students was assessed by a score that was designed and tested by our study group.
Currently, there are no validated checklists for assessing humeral IOA. Hence, authors who are experienced in IOA in patients performed five rounds of focus group sessions according to Schutz et al. and adapted an already validated score for tibial IOA to the needs of the present study.[ 26 , 27 ] The resulting checklist consisted of 15 weighted items quantifying the performance of humeral IOA and is cited in additional file 1. The sum of the particular items results in a score of 0 (worst performance) or 20 (best performance). The entire procedure is described in detail in additional file 2.
Evaluation of the test
Two authors (TD, JM) evaluated the videotapes as raters in a randomised sequence and were blinded to the participants’ group assignment and the time points that are described in the following section. The videotapes were observed by both rates simultaneously using Windows Media Player (Windows X, Microsoft, Redmond, USA). After watching each individual video they discussed discrepancies thoroughly and agreed on one score per videotape.
Self-assessment
Participants had to self-estimate their general capability of applying an IOA on a scale from 1 (very good) to 6 (very bad) as a global rating scale.[ 28 ].
Intervention and control
Intervention: instructional video.
A ten-minute instructional video about humeral intraosseous access was produced by the authors according to the current literature and the manufacturer’s instructions. An identical device and skill trainer were used for the instructional video and the test. Participants individually watched this video on an iPad (iPad Pro 2. Gen., Apple, Silicon Valley, USA) in a quiet room during the mandatory training.
Control: self-study
The self-study included ten minutes of unsupervised hands-on exercise with the device and the skill trainer in separate rooms. No further instructional materials were provided.
Data collection
Randomisation was performed and controlled by certain authors (TD, JM, SS, JS, and LR). Participants were randomly allocated into one of two groups by drawing a lot from an opaque box in Study 1. In Study 2, separate opaque boxes for male and female participants were provided, thus allowing us to stratify the randomisation by sex due to gender differences that were observed in Study 1 and are detailed in the Results section. Participants were instructed not to disclose information on their allocation before everybody had drawn their lots, thus ensuring allocation concealment. The two study groups were:
The ‘Vid-Self’ group (first, INSTRUCTIONAL video; second, self-study)
In Study 1, participants in the ‘Vid-Self’ group first watched the instructional video, subsequently took the test and performed the self-assessment. Seven days later, they performed a 10-min self-study and subsequently took the test and the self-assessment again.
In Study 2, participants in the ‘Vid-Self’ group watched the instructional video and then did the self-study immediately afterwards. Then they did the test and then performed the self-assessment.
The Self-Vid group (first self-study, second INSTRUCTIONAL video)
In Study 1, participants in the ‘Self-Vid’ group first performed a 10-min self-study and then took the test. Seven days later, they watched the instructional video and subsequently took the test and self-assessment.
In Study 2, participants in the ‘Self-Vid’ group performed self-study first, watched the instructional video, did the test and then performed the self-assessment.
The data were collected at three consecutive points in time (T) in Study 1. At T0, randomisation was performed, and the participants’ demographic information, previous experiences and self-assessment were collected. At T1, participants underwent the intervention or control and then took the test and self-assessment. At T2 (retention), seven days after T1, the groups were switched between intervention and control , after which the test and self-assessment were performed.
The data were collected at two consecutive points in time (T) in Study 2: T0 was identical to that in Study 1. At T1, participants had already performed the self-study and watched the instructional video in a randomised order, and then took the test and self-assessment.
Sample size considerations
For Study 1, initially we had planned pre-post-comparisons to evaluate the individual learning success in each sequence group. For this, based on the publication of Oriot et al., [ 26 ] we had assumed an improvement from the level of inexperienced participants (mean 11.06; standard deviation (SD) 4.08) halfway to the level of experienced physicians (mean 19,13; SD 1,48) and a correlation of 0.5 between both measurements. For a two-sided paired t-test to establish this improvement at the 5% significance level with 80% power, 11 participants in each group were required. However, we changed our study design due to concerns that setting a preliminary test before any study might influence students learning efforts too much. Therefore, we decided to omit the preliminary test and to focus on the comparison between instructional video and self-study as a first learning exposure as our primary endpoint. This lead to considering a difference of 3 points in the score as relevant and assumed a standard deviation of 4 based on the publication of Oriot et al., [ 26 ] which resulted in an effect size of 0.75. To obtain a power of 90% to detect such an effect at the 5% level with a two-sided two-sample t-test two groups of 39 students each were required.
For Study 2, we used our data from Study 1. The observed means and standard deviations resulted in an effect size of 1.14. Using a two-sided two-sample t-test, such an effect could be established at the 5% level with 80% power if 14 students per group were included. However, more students were interested in taking part and we did not want to exclude anybody. Therefore, actually 60 students were included in study 2. Thus, the actual sample size was sufficient to reproduce the effect of study 1 if the effect of the sequence of learning methods within a short period is indeed the same as the effect of the sequence of learning methods with a gap of one week and first test after the first learning sequence.
For both studies, we performed intention to treat analyses and included all participants with available test results. For quantitative data, the score of each group at each point in time was quoted as the mean and SD and displayed as a boxplot. For Study 1, the differences within groups are also reported as the mean and SD.
To test for differences between the Vid-Self group and Self-Vid group, a two-sided two sample t-test was performed for the primary endpoint: the difference in the sum of scores at T1 between the groups in both studies. All the other tests applied to the analysis of the secondary endpoints were exploratory; therefore, no correction for multiple testing was applied. In Study 1, we performed a two-sided two sample t-test for differences in scores between the two groups at T2. We performed paired t-tests for differences in scores within each group (dependent samples) between T1 and T2. To make test scores and self-assessments, which were measured on different scales, comparable, we standardised the variables in both studies by subtracting the mean for the complete sample from each score and dividing it by the standard deviation (SD) and computed the difference between the two standardised measurements. Small differences correspond to consistency of self-assessment and score, large differences correspond to inconsistency. We then tested for differences of these differences between genders with a two-sided two sample t-test.
In Study 1, 78 participants were tested at T1: 42 (54%) participants were assigned to Vid-Self, and 36 (46%) were assigned to Self-Vid. At T2, 59 participants were analysed, as 21 participants did not appear: 31 (53%) participants were evaluated in the Vid-Self group, and 28 (48%) in the Self-Vid group. In Study 2, 30 of 60 (50%) participants were assigned to each study group, and all were analysed. The demographic data are shown in Table 1 . (Table 1 see below).
Primary endpoint of study 1
In Study 1, the group that watched the instructional video at that point in time scored significantly greater than the group that did self-study (Self-Vid at T1) (at T1: Vid-Self: mean 14.8, SD 3.5 vs. Self-Vid: mean 7.7, SD 2.6, p < 0.001) (Fig. 2 a, additional file 3).

Boxplot of the scores of Study 1 and Study 2. These boxplots display the scores of the two groups on the abscissa: The Self-Vid group and the Vid-Self group. The ordinate shows the score with a minimum of 0 and a maximum of 20. The horizontal thick lines indicate the median, the thin lines indicate the first and third quartiles, and the vertical bars indicate the minimum and maximum scores. The dots indicate extreme values, and the rhombs indicate the means of the scores. a Boxplot of the scores in Study 1 at T1. Study 1 (primary endpoint): Boxplot of the score at Time 1: The ‘Vid-Self’ group obtained a significantly greater score after the INSTRUCTIONAL video than did the ‘Self-Vid’ group after the self-study. (primary endpoint of Study 1: p < 0.01). b Boxplot of the scores in Study 1 at T2. Study 1 (secondary endpoint): Boxplot of the score at Time 2 (seven days after T1): The ‘Vid-Self’ group had a significantly lower score after the self-study than did the ‘Self-Vid’ group after the instructional video (secondary endpoint of Study 1: p < 0.01). c Boxplot of the scores in Study 2. Study 2 (primary endpoint): Boxplot of the score: The ‘Vid-self’ and ‘Self-Vid’ groups did not differ in terms of the achieved scores ( p = 0.97)
Secondary endpoints of study 1
In Study 1, at T2 (after seven days), Vid-Self tended to yield lower scores than Self-Vid (mean 12.5, SD 3.6 vs. mean 15.9, SD 2.2, p < 0.001) (Fig. 2 b). From T1 to T2, the scores tended to decrease for Vid-Self (T1: mean 14.8, SD 3.5; T2: mean 12.5, SD 3.6, p < 0.001) and increase for Self-Vid (T1: mean 7.7, SD 2.6, p < 0.001; T2: mean: 15.9, SD 2.2, p < 0.001).
The absolute value of the score of Vid-Self tended to decrease less than the score increased in Self-Vid (mean change from T1 to T2:—2.8 vs. 7.9, p < 0.001).
The details of the individual weighted items of the scores of those participants attending T1 and T2 are shown in Fig. 3 .

Details of the weighted scores of participants in Study 1. a The diagram contains the data of participants of the Vid-Self group in Study 1 who performed the tests at both points in time ( n = 31). For those participants, the diagram displays the sum of the single items of the score with respect to their weighting, as described in the “Methods” section. The values of the single items were weighted from 1 to 3 concerning the maximum number of achievable points according to their impact on clinical relevance (additional file 1). For example, the maximum score for the item “Anatomical access point” was 3 points, so for 31 participants it was were equivalent to 93 points. The points in time are displayed as follows. T 1: orange, T 2: blue. b The diagram contains data from participants of the Self-Vid group in Study 1 who performed the test at both points in time ( n = 24)
We investigated whether these changes in score within the seven days could be explained by the sequence (video then self-study or vice versa) or represented a decrease in skill in study 2.
In study 1 Vid-Self compassed 19 female and 17 male participants whereas Self-Vid compassed 25 female and 17 male participants.
Separated by gender, female and male participants did not exhibit substantial differences in score over both groups (T1: mean: 11.2, SD 4.8 vs. mean 12.0, SD 4.6, p = 0.459; T2: mean 13.3, SD 3.8 vs. mean 14.9, SD 2.9, p = 0.069, additional file 3).
Separated by gender and study groups at T1 female and male participants did not show a difference either (additional file 3). At T2 female participants of Vid-self tended to show a lower score than male (female mean: 10.9, SD 3.1, male mean: 14.4, SD 3.3, p = 0.007) whereas there was no difference at T2 between sexes in Self-Vid (additional file 3).
Concerning self-assessment female participants generally tended towards a worse self-assessment than male (T0: p < 0.001, T1: p = 0.027, T2, p = 0.001, additional file 3).
Separated by gender and study groups at T0 female participants of the Vid-Self group tended to show a worse self-assessment than male participants whereas in the Self-Vid group sexes did not exhibit differences in self-assessment (Vid-Self: p = 0.002, Self-Vid: p = 0.1, additional file 3).
When addressing gender differences in consistency of self-assessment and score, a significant difference of differences between females and males was observed only at T2 in the Self-Vid group ( p = 0.049); moreover, there was no difference in the other points over time (particular p > 0.05). Due to this sex difference at T2, we stratified for sex in Study 2.
Primary endpoint of study 2
In Study 2, neither group differed in score (Vid-Self: mean 16.5, SD 3.0 vs. Self-Vid: mean 16.5, SD 3.1, p = 0.97) (Fig. 2 c).
Secondary endpoints of study 2
In Study 2, self-assessments were recorded for the Vid-Self group (mean 4.5, SD 1.2; mean 2.9, SD 0.9), and the Self-Vid group (mean 4.1, SD 1.1; mean 2.5, SD 0.9). Again, female and male participants did not exhibit substantial differences in score (mean 16.8, SD 2.8 vs. mean 16.2, SD 3.2, p = 0.417). Again, male participants tended to have slightly better self-assessments than did their scores, while the opposite trend was observed for female participants, but the difference was not statistically significant ( p > 0.1). An overview of the entire results is provided in additional file 3.
Two studies showed that an instructional video, as a stand-alone tool without didactic embedding, promoted the acquisition of practical clinical skills. Furthermore, participants generally obtained the highest scores after watching the instructional video (Vid-Self group: 14.8 points on day one; Self-Vid group: 15.9 points on day seven). In comparison, the participants performed significantly worse directly after self-study (Self-Vid group: 7.7 points on day one; Vid-Self group: 12.5 points on day seven). The decline in score in Study 1 over seven days in the Vid-Self group suggested that there was a short-term decline in this skill, even though self-study was performed directly before the test. The follow-up study (Study 2) showed that, regardless of the sequence of the skill acquisition methods (self-study or video), the immediate combination of the two skill acquisition methods was most successful, as both groups scored 16.5 points (Fig. 2 b). We deduce that an instructional video as a stand-alone tool effectively promotes the acquisition of this practical skill, and self-study even fosters that acquisition.
Acquisition of practical skills
Traditionally, practical skills were taught face-to-face in group sessions. Due to the pandemic, groups had to be reduced in size, which required an increased number of instructors as well as sessions. Therefore, recently, alternative teaching methods such as instructional videos have been more frequently integrated into medical education.[ 1 , 2 , 3 , 6 , 7 ] Instructional videos teach identical content in a cross-sectional and longitudinal manner and therefore may ensure more standardisation of a specific content than face-to-face instruction.[ 1 , 3 ] A previous study evaluated the effect of a ten-minute video followed by ten minutes of untutored training in comparison to 20 min of face-to-face instruction concerning paediatric tibial IOA.[ 12 ] The video group scored significantly higher on the subsequent test than did the control group (7.56 vs. 6.00, maximum possible: 10). Although the latter study included a smaller but more highly qualified sample, the present study showed similar results for inexperienced participants. Another previous study evaluated three teaching methods concerning subcuticular suturing but in an elaborate didactic embedding procedure involving eight minutes of video, face-to-face instruction and independent practice.[ 10 ] The main difference from our study was that those participants watched the video first and subsequently were randomised into the cited groups. Furthermore, the video group repeatedly watched the video. However, as in our study, video promoted the acquisition of the skill, as did instructor-led training, whereas independent practice was less effective. However, the present study revealed that an instructional video as a stand-alone tool can teach practical skills well without additional didactic embedding or extensive previous experience. To optimise learning success, a combination of an instructional video with self-study is recommended, independent of the sequence of both teaching methods.
Skill decline
A decrease in clinical skills depends on affective, cognitive, and psychomotor aspects, time, frequency of practice, and prior experience. [ 29 , 30 , 31 , 32 ] Over a 12-month period, experienced providers show a decline in the skill of accessing IOA, as do undergraduates in basic life support.[ 30 , 31 ] Furthermore, experienced providers show better retention of internal pacemaker placement skills over a three-month period than inexperienced physicians.[ 32 ] In novices, the ability to perform paracentesis decreases within three months, and the ability to perform endoscopic intubation decreases within two months. The performance of focused transthoracic echocardiography and suturing decreases within one month.[ 11 , 33 , 34 , 35 ] Only the above cited study described a decrease in skill concerning subcuticular suturing within one week.[ 10 ] The group that was trained by a video declined less (12.74 to 12.41) than the instructor trained (14.17 to 13.00) and the independent practice group (13.54 to 11.2) [ 10 ]. As mentioned above, the videos in that study were used repetitively. Therefore, participants were exposed to more video experience than in the present study. Future trials should focus on how repetitive videos foster skill retention.
To explore this decrease in skill, we analysed the development of single items in our score (additional file 1) in both groups (Fig. 3 ). The score consists of 15 weighted items and a maximum score of 20 (additional file 2). Figure 3 shows the sum of the scores for each item and its weights. In the Vid-Self group in Study 1, the decrease in score from T1 to T2 was based mainly on the following items: anatomical access (weighted: 3), angle of insertion (weighted: 2), injection of local anaesthetic, fixation of the cannula, and marking of the patient (weighted: 1 each). The first two items are clinically relevant for successfully applying an IOA. These factors appear to contribute most to the decline. In the Self-Vid group, the increase in scores was caused mainly by the same items and also by the item arm position. Therefore, in our opinion, the score adequately reflects performance in terms of relevant clinical aspects. Furthermore, the cited items of the score seem to be efficiently taught via an instructional video.
Gender aspects
In Study 1, we noticed trends, however, without a statistically significant difference: Female participants tended to have a lower mean score in all groups. Due to the greater proportion of female participants in the Vid-Self group who had a lower score after seven days, this could be a confounder or a gender issue. The latter has been controversially discussed in many fields of medicine.[ 36 , 37 , 38 , 39 ] Furthermore, males in the Self-Vid group had better self-assessments than did their performance, while females had worse self-assessments than did their performance. Therefore, we stratified patients by sex in Study 2. However, there was no statistically significant difference concerning sex in Study 2.
Limitations
First, any simulation-based study has limitations due to the artificial environment. Therefore, the results should be interpreted with caution concerning possible transferability in patient care, and generalizability is limited to laboratory conditions.[ 11 , 12 ] Second, we found no validated score for the evaluation of humeral IOA; therefore, we thoroughly performed the adoption of this validated score for tibial access (additional file 2) according to an established procedure.[ 27 ] We partially used weighted items within this score that may influence the achieved score disproportionally high concerning the particular item and we did not perform a statistical validation. However, we developed our score out of a validated score and estimated this as appropriate for our needs. Further validation is worthwhile. Third, although all students attended a curricular training in intraosseous vascular access one year before the study 49 of 78 (62%) participants in study 1 and 21 of 60 (35%) in study 2 stated not to have had any training before. Apparently, this training had no substantial impact on the participants and further studies should include familiarisation with the equipment used. Fourth, a dropout in Study 1 of 27% (21/78) of the participants in the follow-up at Time 2 (seven days after Time 1) was quite high. This was probably caused by the organisational effort of those participants being engaged in remote hospitals to attend the follow-up. However, dropout may have caused an imbalance in the sex ratio at time 2, influencing us to reevaluate our findings in Study 2, as discussed above. Fifth, self-study as a control instrument seems to be trivial because teaching is certainly better than not teaching. Nevertheless, our aim was to evaluate a video as a stand-alone tool, so we needed the best possible inert control group. All participants had already completed curricular IOA training for the tibial access site one year before the study. Therefore, we decided not to perform a pretest concerning the video, as in previous studies, but rather defined self-study as the best possible control for contrasting the effect of the video.[ 10 , 11 ].
Conclusions
A practical skill can be efficiently acquired by an instructional video as a stand-alone tool without didactic embedding and is superior to self-study despite previous curricular experience. Therefore, instructional videos can be used to a satisfactory extent for skill acquisition when direct teaching is impossible, such as during a pandemic. A decline in performance can be observed within seven days after the instructional video, which cannot be prevented even by self-study immediately before testing. However, the best results could be achieved by the immediate combination of instructional video and self-study. Hereby, the sequence of the methods has no influence on the acquisition. Gender differences could not be detected in the present studies. The evaluated instructional video proved to be a stand-alone tool for the acquisition of the defined practical skill. Instructional videos could greatly increase the efficiency of teaching in medical schools and provide a useful supplement to students' education.
Availability of data and materials
The dataset supporting the conclusions of this article is available in the LabArchives repository, https://doi.org/10.25833/8cc7-eb07 at https://doi.org/10.25833/8cc7-eb07
The raw data were anonymised according to the protocols of the present study.
Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? a systematic review and meta-analysis. Med Educ Online. 2019;24(1):1666538.
Srinivasa K, Chen Y, Henning MA. The role of online videos in teaching procedural skills to post-graduate medical learners: a systematic narrative review. Med Teach. 2020;42(6):689–97.
Article Google Scholar
Forbes H, Oprescu FI, Downer T, Phillips NM, McTier L, Lord B, et al. Use of videos to support teaching and learning of clinical skills in nursing education: a review. Nurs Educ Today. 2016;42:53–6.
Dong CY, Goh PS. Twelve tips for the effective use of videos in medical education. Med Teach. 2015;37(2):140–5.
Coyne E, Rands H, Frommolt V, Kain V, Plugge M, Mitchell M. Investigation of blended learning video resources to teach health students clinical skills: an integrative review. Nurs Educ Today. 2018;63:101–7.
Hodgson JC, Hagan P. Medical education adaptations during a pandemic: transitioning to virtual student support. Med Educ. 2020;54(7):662–3.
Sandhu P, de Wolf M. The impact of COVID-19 on the undergraduate medical curriculum. Med Educ Online. 2020;25(1):1764740.
Theoret C, Ming X. Our education, our concerns: the impact on medical student education of COVID-19. Med Educ. 2020;54(7):591–2.
Brockfeld T, Muller B, de Laffolie J. Video versus live lecture courses: a comparative evaluation of lecture types and results. Med Educ Online. 2018;23(1):1555434.
Shippey SH, Chen TL, Chou B, Knoepp LR, Bowen CW, Handa VL. Teaching subcuticular suturing to medical students: video versus expert instructor feedback. J Surg Educ. 2011;68(5):397–402.
Xeroulis GJ, Park J, Moulton CA, Reznick RK, Leblanc V, Dubrowski A. Teaching suturing and knot-tying skills to medical students: a randomized controlled study comparing computer-based video instruction and (concurrent and summary) expert feedback. Surgery. 2007;141(4):442–9.
Lee JC, Boyd R, Stuart P. Randomized controlled trial of an instructional DVD for clinical skills teaching. Emerg Med Australas. 2007;19(3):241–5.
Hilal Z, Kumpernatz AK, Rezniczek GA, Cetin C, Tempfer-Bentz EK, Tempfer CB. A randomized comparison of video demonstration versus hands-on training of medical students for vacuum delivery using objective structured assessment of technical skills (OSATS). Medicine (Baltimore). 2017;96(11): e6355.
Woodworth GE, Chen EM, Horn JL, Aziz MF. Efficacy of computer-based video and simulation in ultrasound-guided regional anesthesia training. J Clin Anesth. 2014;26(3):212–21.
Petitpas F, Guenezan J, Vendeuvre T, Scepi M, Oriot D, Mimoz O. Use of intra-osseous access in adults: a systematic review. Crit Care. 2016;20(102):1–9.
Crickmer M, Lam T, Tavares W, Meshkat N. Do PGY-1 residents in Emergency medicine have enough experiences in resuscitations and other clinical procedures to meet the requirements of a competence by design curriculum? Can Med Educ J. 2021;12(3):100–4.
Google Scholar
Thim S, Nayahangan LJ, Paltved C, Jensen RD, Konge L, Hertel NT, et al. Identifying and prioritising technical procedures for simulation-based curriculum in paediatrics: a Delphi-based general needs assessment. BMJ Paediatr Open. 2020;4(1): e000697.
Levitan RM, Bortle CD, Snyder TA, Nitsch DA, Pisaturo JT, Butler KH. Use of a battery-operated needle driver for intraosseous access by novice users: skill acquisition with cadavers. Ann Emerg Med. 2009;54(5):692–4.
Gendron B, Cronin A, Monti J, Brigg A. Military medic performance with employment of a commercial intraosseous infusion device: a randomized. crossover study military medicine. 2018;183(5–6):E216–22.
Chreiman KM, Dumas RP, Seamon MJ, Kim PK, Reilly PM, Kaplan LJ, et al. The intraosseous have it: a prospective observational study of vascular access success rates in patients in extremis using video review. J Trauma Acute Care Surg. 2018;84(4):558–63.
Liu YY, Wang YP, Zu LY, Zheng K, Ma QB, Zheng YA, et al. Comparison of intraosseous access and central venous catheterization in Chinese adult emergency patients: a prospective, multicenter, and randomized study. World J Emerg Med. 2021;12(2):105–10.
Afzali M, Kvisselgaard AD, Lyngeraa TS, Viggers S. Intraosseous access can be taught to medical students using the four-step approach. BMC Med Educ. 2017;17(1):50.
Sorgjerd R, Sunde GA, Heltne JK. Comparison of two different intraosseous access methods in a physician-staffed helicopter emergency medical service - a quality assurance study. Scand J Trauma Resusc Emerg Med. 2019;27(1):15.
Rush S, D’Amore J, Boccio E. A review of the evolution of intraosseous access in tactical settings and a feasibility study of a human cadaver model for a humeral head approach. Mil Med. 2014;179(8 Suppl):24–8.
Bordes SJ, Walker D, Modica LJ, Buckland J, Sobering AK. Towards the optimal use of video recordings to support the flipped classroom in medical school basic sciences education. Med Educ Online. 2021;26(1):1841406.
Oriot D, Darrieux E, Boureau-Voultoury A, Ragot S, Scepi M. Validation of a performance assessment scale for simulated intraosseous access. Simul Healthc. 2012;7(3):171–5.
Schmutz J, Eppich WJ, Hoffmann F, Heimberg E, Manser T. Five steps to develop checklists for evaluating clinical performance: an integrative approach. Acad Med. 2014;89(7):996–1005.
Ilgen JS, Ma IW, Hatala R, Cook DA. A systematic review of validity evidence for checklists versus global rating scales in simulation-based assessment. Med Educ. 2015;49(2):161–73.
Offiah G, Ekpotu LP, Murphy S, Kane D, Gordon A, O’Sullivan M, et al. Evaluation of medical student retention of clinical skills following simulation training. BMC Med Educ. 2019;19(1):263.
Derikx HJ, Gerritse BM, Gans R, van der Meer NJ. A randomized trial comparing two intraosseous access devices in intrahospital healthcare providers with a focus on retention of knowledge, skill, and self-efficacy. Eur J Trauma Emerg Surg. 2014;40(5):581–6.
de Ruijter PA, Biersteker HA, Biert J, van Goor H, Tan EC. Retention of first aid and basic life support skills in undergraduate medical students. Med Educ Online. 2014;19:24841.
Langhan TS, Rigby IJ, Walker IW, Howes D, Donnon T, Lord JA. Simulation-based training in critical resuscitation procedures improves residents’ competence. CJEM. 2009;11(6):535–9.
Yamamoto R, Clanton D, Willis RE, Jonas RB, Cestero RF. Rapid decay of transthoracic echocardiography skills at 1 month: a prospective observational study. J Surg Educ. 2018;75(2):503–9.
Sall D, Warm EJ, Kinnear B, Kelleher M, Jandarov R, O’Toole J. See One, Do One, Forget One: early skill decay after paracentesis training. J Gen Intern Med. 2021;36(5):1346–51.
Latif RK, Bautista A, Duan X, Neamtu A, Wu D, Wadhwa A, et al. Teaching basic fiberoptic intubation skills in a simulator: initial learning and skills decay. J Anesth. 2016;30(1):12–9.
Thorson CM, Kelly JP, Forse RA, Turaga KK. Can we continue to ignore gender differences in performance on simulation trainers? J Laparoendosc Adv Surg Tech A. 2011;21(4):329–33.
Stanek K, Phillips N, Staffa SJ, Saldanha FYL, Rogers-Vizena CR. Gender differences in plastic surgery trainee confidence: a pilot analysis during cleft lip simulation. Plast Reconstr Surg Glob Open. 2023;11(12): e5428.
Tramer L, Becker C, Schumacher C, Beck K, Tschan F, Semmer NK, et al. Association of self-esteem, personality, stress and gender with performance of a resuscitation team: a simulation-based study. PLoS ONE. 2020;15(5): e0233155.
Addison P, Bitner D, Chung P, Kutana S, Dechario S, Husk G, et al. Blinded intraoperative skill evaluations avoid gender-based bias. Surg Endosc. 2022;36(11):8458–62.
Download references
Acknowledgements
We sincerely thank the Chair of our Department of Anaesthesiology and the staff coordination, as well as the Department of Research and Training, for their great support while conducting the study. This manuscript contains portions of the doctoral thesis of Tim Demare, University Medical Centre of the Johannes Gutenberg University, Mainz, Germany. Parts of the study were presented as a scientific online poster during the annual congress of the German Society of Anaesthesiology and Intensive Care Medicine (Deutsche Gesellschaft für Anästhesiologie und Intensivmedizin) 12.-14. May 2022, DAC Digital (Deutscher Anästhesie Congress), Nürnberg, Germany ( https://www.ai-online.info/images/ai-ausgabe/2022/05-2022/Supplement_8-2022_DAC_Abstracts.pdf —page 194).
Open Access funding enabled and organized by Projekt DEAL. There was no financial support or funding.
Author information
Authors and affiliations.
Department of Anaesthesiology, University Medical Centerof the, Johannes Gutenberg-University Mainz, Langenbeckstr. 1, Mainz, 55131, Germany
Thomas Ott, Tim Demare, Julia Möhrke, Saskia Silber, Johannes Schwab, Lukas Reuter, Nina Pirlich, Alexander Ziebart & Kristin Engelhard
Institute of Medical Biostatistics, Epidemiology, and Informatics, University Medical Centerof the, Johannes Gutenberg-University Mainz, Obere Zahlbacher Str. 69, Mainz, 55131, Germany
Ruben Westhphal & Irene Schmidtmann
Department of Orthopaedics and Traumatology, University Medical Centerof the, Johannes Gutenberg-University Mainz, Langenbeckstr. 1, Mainz, 55131, Germany
Sven-Oliver Dietz
You can also search for this author in PubMed Google Scholar
Contributions
All the authors have made substantial intellectual contributions to the conception, design, data acquisition, analysis and interpretation of the data collected in this study and further drafted the manuscript. The following contains only the specific main focuses of the contributions of the particular author. T.O., T.D., S.D., J.M., S.S., J.S., R.W., and L.R. contributed to the conception, design and development of the study. The focus group rounds, literature research and development of the score were realised by T.D., T.O., J.M., J.S., L.R. and S.S. The instructional video was planned, scripted and produced by T.O., J.S., J.M., L.S. and T.D. The data acquisition was mainly planned, coordinated and performed by T.D., L.R., J.M., S.S., J.S. T.D. and J.M. evaluated all the videotapes of all the tests. T.O., R.W., I. S., T.D., A.Z. and N.P. contributed to the analysis and interpretation of the data. The draft of the manuscript was created by T.O., I.S., T.D., S.D., N.P., A.Z. and K.E. All the authors critically revised the manuscript concerning the intellectual content. All the authors approved the final manuscript and agreed to be accountable for all the aspects of the work.
Corresponding author
Correspondence to Thomas Ott .
Ethics declarations
Ethics approval and consent to participate.
The trial was carried out in accordance with the Declaration of Helsinki and all relevant guidelines and regulations. This study was approved by the responsible ethical review board: ethics committee of the Medical Association of the State Rhineland-Palatinate (Ethical Review Committee of the State Chamber of Physicians of Rhineland-Palatinate, Deutschhausplatz 3, 55116 Mainz, Germany; Chairperson: Professor S. Letzel) concerning Study 1 on 29. April 2021 under the number 2021–15807 and Study 2 on 21. October 2021 under the number 2021–16112.
The study was conducted during the mandatory institutional final year training at our institutional simulation centre. All participants signed a written informed consent concerning anonymous data analysis and publication. Participation was voluntary, and denial of participation did not have any consequence on participation in the mandatory training.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ott, T., Demare, T., Möhrke, J. et al. Does an instructional video as a stand-alone tool promote the acquisition of practical clinical skills? A randomised simulation research trial of skills acquisition and short-term retention. BMC Med Educ 24 , 714 (2024). https://doi.org/10.1186/s12909-024-05714-6
Download citation
Received : 23 February 2023
Accepted : 25 June 2024
Published : 02 July 2024
DOI : https://doi.org/10.1186/s12909-024-05714-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Instructional video
- Clinical skill
- Undergraduate students
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dtsch Arztebl Int
- v.106(15); 2009 Apr
Types of Study in Medical Research
Bernd röhrig.
1 MDK Rheinland-Pfalz, Referat Rehabilitation/Biometrie, Alzey
Jean-Baptist du Prel
2 Zentrum für Präventive Pädiatrie, Zentrum für Kinder- und Jugendmedizin, Mainz
Daniel Wachtlin
3 Interdisziplinäres Zentrum Klinische Studien (IZKS), Fachbereich Medizin der Universität Mainz
Maria Blettner
4 Institut für Medizinische Biometrie, Epidemiologie und Informatik (IMBEI), Johannes Gutenberg Universität Mainz
The choice of study type is an important aspect of the design of medical studies. The study design and consequent study type are major determinants of a study’s scientific quality and clinical value.
This article describes the structured classification of studies into two types, primary and secondary, as well as a further subclassification of studies of primary type. This is done on the basis of a selective literature search concerning study types in medical research, in addition to the authors’ own experience.
Three main areas of medical research can be distinguished by study type: basic (experimental), clinical, and epidemiological research. Furthermore, clinical and epidemiological studies can be further subclassified as either interventional or noninterventional.
Conclusions
The study type that can best answer the particular research question at hand must be determined not only on a purely scientific basis, but also in view of the available financial resources, staffing, and practical feasibility (organization, medical prerequisites, number of patients, etc.).
The quality, reliability and possibility of publishing a study are decisively influenced by the selection of a proper study design. The study type is a component of the study design (see the article "Study Design in Medical Research") and must be specified before the study starts. The study type is determined by the question to be answered and decides how useful a scientific study is and how well it can be interpreted. If the wrong study type has been selected, this cannot be rectified once the study has started.
After an earlier publication dealing with aspects of study design, the present article deals with study types in primary and secondary research. The article focuses on study types in primary research. A special article will be devoted to study types in secondary research, such as meta-analyses and reviews. This article covers the classification of individual study types. The conception, implementation, advantages, disadvantages and possibilities of using the different study types are illustrated by examples. The article is based on a selective literature research on study types in medical research, as well as the authors’ own experience.
Classification of study types
In principle, medical research is classified into primary and secondary research. While secondary research summarizes available studies in the form of reviews and meta-analyses, the actual studies are performed in primary research. Three main areas are distinguished: basic medical research, clinical research, and epidemiological research. In individual cases, it may be difficult to classify individual studies to one of these three main categories or to the subcategories. In the interests of clarity and to avoid excessive length, the authors will dispense with discussing special areas of research, such as health services research, quality assurance, or clinical epidemiology. Figure 1 gives an overview of the different study types in medical research.

Classification of different study types
*1 , sometimes known as experimental research; *2 , analogous term: interventional; *3 , analogous term: noninterventional or nonexperimental
This scheme is intended to classify the study types as clearly as possible. In the interests of clarity, we have excluded clinical epidemiology — a subject which borders on both clinical and epidemiological research ( 3 ). The study types in this area can be found under clinical research and epidemiology.
Basic research
Basic medical research (otherwise known as experimental research) includes animal experiments, cell studies, biochemical, genetic and physiological investigations, and studies on the properties of drugs and materials. In almost all experiments, at least one independent variable is varied and the effects on the dependent variable are investigated. The procedure and the experimental design can be precisely specified and implemented ( 1 ). For example, the population, number of groups, case numbers, treatments and dosages can be exactly specified. It is also important that confounding factors should be specifically controlled or reduced. In experiments, specific hypotheses are investigated and causal statements are made. High internal validity (= unambiguity) is achieved by setting up standardized experimental conditions, with low variability in the units of observation (for example, cells, animals or materials). External validity is a more difficult issue. Laboratory conditions cannot always be directly transferred to normal clinical practice and processes in isolated cells or in animals are not equivalent to those in man (= generalizability) ( 2 ).
Basic research also includes the development and improvement of analytical procedures—such as analytical determination of enzymes, markers or genes—, imaging procedures—such as computed tomography or magnetic resonance imaging—, and gene sequencing—such as the link between eye color and specific gene sequences. The development of biometric procedures—such as statistical test procedures, modeling and statistical evaluation strategies—also belongs here.
Clinical studies
Clinical studies include both interventional (or experimental) studies and noninterventional (or observational) studies. A clinical drug study is an interventional clinical study, defined according to §4 Paragraph 23 of the Medicines Act [Arzneimittelgesetz; AMG] as "any study performed on man with the purpose of studying or demonstrating the clinical or pharmacological effects of drugs, to establish side effects, or to investigate absorption, distribution, metabolism or elimination, with the aim of providing clear evidence of the efficacy or safety of the drug."
Interventional studies also include studies on medical devices and studies in which surgical, physical or psychotherapeutic procedures are examined. In contrast to clinical studies, §4 Paragraph 23 of the AMG describes noninterventional studies as follows: "A noninterventional study is a study in the context of which knowledge from the treatment of persons with drugs in accordance with the instructions for use specified in their registration is analyzed using epidemiological methods. The diagnosis, treatment and monitoring are not performed according to a previously specified study protocol, but exclusively according to medical practice."
The aim of an interventional clinical study is to compare treatment procedures within a patient population, which should exhibit as few as possible internal differences, apart from the treatment ( 4 , e1 ). This is to be achieved by appropriate measures, particularly by random allocation of the patients to the groups, thus avoiding bias in the result. Possible therapies include a drug, an operation, the therapeutic use of a medical device such as a stent, or physiotherapy, acupuncture, psychosocial intervention, rehabilitation measures, training or diet. Vaccine studies also count as interventional studies in Germany and are performed as clinical studies according to the AMG.
Interventional clinical studies are subject to a variety of legal and ethical requirements, including the Medicines Act and the Law on Medical Devices. Studies with medical devices must be registered by the responsible authorities, who must also approve studies with drugs. Drug studies also require a favorable ruling from the responsible ethics committee. A study must be performed in accordance with the binding rules of Good Clinical Practice (GCP) ( 5 , e2 – e4 ). For clinical studies on persons capable of giving consent, it is absolutely essential that the patient should sign a declaration of consent (informed consent) ( e2 ). A control group is included in most clinical studies. This group receives another treatment regimen and/or placebo—a therapy without substantial efficacy. The selection of the control group must not only be ethically defensible, but also be suitable for answering the most important questions in the study ( e5 ).
Clinical studies should ideally include randomization, in which the patients are allocated by chance to the therapy arms. This procedure is performed with random numbers or computer algorithms ( 6 – 8 ). Randomization ensures that the patients will be allocated to the different groups in a balanced manner and that possible confounding factors—such as risk factors, comorbidities and genetic variabilities—will be distributed by chance between the groups (structural equivalence) ( 9 , 10 ). Randomization is intended to maximize homogeneity between the groups and prevent, for example, a specific therapy being reserved for patients with a particularly favorable prognosis (such as young patients in good physical condition) ( 11 ).
Blinding is another suitable method to avoid bias. A distinction is made between single and double blinding. With single blinding, the patient is unaware which treatment he is receiving, while, with double blinding, neither the patient nor the investigator knows which treatment is planned. Blinding the patient and investigator excludes possible subjective (even subconscious) influences on the evaluation of a specific therapy (e.g. drug administration versus placebo). Thus, double blinding ensures that the patient or therapy groups are both handled and observed in the same manner. The highest possible degree of blinding should always be selected. The study statistician should also remain blinded until the details of the evaluation have finally been specified.
A well designed clinical study must also include case number planning. This ensures that the assumed therapeutic effect can be recognized as such, with a previously specified statistical probability (statistical power) ( 4 , 6 , 12 ).
It is important for the performance of a clinical trial that it should be carefully planned and that the exact clinical details and methods should be specified in the study protocol ( 13 ). It is, however, also important that the implementation of the study according to the protocol, as well as data collection, must be monitored. For a first class study, data quality must be ensured by double data entry, programming plausibility tests, and evaluation by a biometrician. International recommendations for the reporting of randomized clinical studies can be found in the CONSORT statement (Consolidated Standards of Reporting Trials, www.consort-statement.org ) ( 14 ). Many journals make this an essential condition for publication.
For all the methodological reasons mentioned above and for ethical reasons, the randomized controlled and blinded clinical trial with case number planning is accepted as the gold standard for testing the efficacy and safety of therapies or drugs ( 4 , e1 , 15 ).
In contrast, noninterventional clinical studies (NIS) are patient-related observational studies, in which patients are given an individually specified therapy. The responsible physician specifies the therapy on the basis of the medical diagnosis and the patient’s wishes. NIS include noninterventional therapeutic studies, prognostic studies, observational drug studies, secondary data analyses, case series and single case analyses ( 13 , 16 ). Similarly to clinical studies, noninterventional therapy studies include comparison between therapies; however, the treatment is exclusively according to the physician’s discretion. The evaluation is often retrospective. Prognostic studies examine the influence of prognostic factors (such as tumor stage, functional state, or body mass index) on the further course of a disease. Diagnostic studies are another class of observational studies, in which either the quality of a diagnostic method is compared to an established method (ideally a gold standard), or an investigator is compared with one or several other investigators (inter-rater comparison) or with himself at different time points (intra-rater comparison) ( e1 ). If an event is very rare (such as a rare disease or an individual course of treatment), a single-case study, or a case series, are possibilities. A case series is a study on a larger patient group with a specific disease. For example, after the discovery of the AIDS virus, the Center for Disease Control (CDC) in the USA collected a case series of 1000 patients, in order to study frequent complications of this infection. The lack of a control group is a disadvantage of case series. For this reason, case series are primarily used for descriptive purposes ( 3 ).
Epidemiological studies
The main point of interest in epidemiological studies is to investigate the distribution and historical changes in the frequency of diseases and the causes for these. Analogously to clinical studies, a distinction is made between experimental and observational epidemiological studies ( 16 , 17 ).
Interventional studies are experimental in character and are further subdivided into field studies (sample from an area, such as a large region or a country) and group studies (sample from a specific group, such as a specific social or ethnic group). One example was the investigation of the iodine supplementation of cooking salt to prevent cretinism in a region with iodine deficiency. On the other hand, many interventions are unsuitable for randomized intervention studies, for ethical, social or political reasons, as the exposure may be harmful to the subjects ( 17 ).
Observational epidemiological studies can be further subdivided into cohort studies (follow-up studies), case control studies, cross-sectional studies (prevalence studies), and ecological studies (correlation studies or studies with aggregated data).
In contrast, studies with only descriptive evaluation are restricted to a simple depiction of the frequency (incidence and prevalence) and distribution of a disease within a population. The objective of the description may also be the regular recording of information (monitoring, surveillance). Registry data are also suited for the description of prevalence and incidence; for example, they are used for national health reports in Germany.
In the simplest case, cohort studies involve the observation of two healthy groups of subjects over time. One group is exposed to a specific substance (for example, workers in a chemical factory) and the other is not exposed. It is recorded prospectively (into the future) how often a specific disease (such as lung cancer) occurs in the two groups ( figure 2a ). The incidence for the occurrence of the disease can be determined for both groups. Moreover, the relative risk (quotient of the incidence rates) is a very important statistical parameter which can be calculated in cohort studies. For rare types of exposure, the general population can be used as controls ( e6 ). All evaluations naturally consider the age and gender distributions in the corresponding cohorts. The objective of cohort studies is to record detailed information on the exposure and on confounding factors, such as the duration of employment, the maximum and the cumulated exposure. One well known cohort study is the British Doctors Study, which prospectively examined the effect of smoking on mortality among British doctors over a period of decades ( e7 ). Cohort studies are well suited for detecting causal connections between exposure and the development of disease. On the other hand, cohort studies often demand a great deal of time, organization, and money. So-called historical cohort studies represent a special case. In this case, all data on exposure and effect (illness) are already available at the start of the study and are analyzed retrospectively. For example, studies of this sort are used to investigate occupational forms of cancer. They are usually cheaper ( 16 ).

Graphical depiction of a prospective cohort study (simplest case [2a]) and a retrospective case control study (2b)
In case control studies, cases are compared with controls. Cases are persons who fall ill from the disease in question. Controls are persons who are not ill, but are otherwise comparable to the cases. A retrospective analysis is performed to establish to what extent persons in the case and control groups were exposed ( figure 2b ). Possible exposure factors include smoking, nutrition and pollutant load. Care should be taken that the intensity and duration of the exposure is analyzed as carefully and in as detailed a manner as possible. If it is observed that ill people are more often exposed than healthy people, it may be concluded that there is a link between the illness and the risk factor. In case control studies, the most important statistical parameter is the odds ratio. Case control studies usually require less time and fewer resources than cohort studies ( 16 ). The disadvantage of case control studies is that the incidence rate (rate of new cases) cannot be calculated. There is also a great risk of bias from the selection of the study population ("selection bias") and from faulty recall ("recall bias") (see too the article "Avoiding Bias in Observational Studies"). Table 1 presents an overview of possible types of epidemiological study ( e8 ). Table 2 summarizes the advantages and disadvantages of observational studies ( 16 ).
| Study of rare diseases such as cancers | Case control studies |
| Study of rare exposure, such as exposure to industrial chemicals | Cohort studies in a population group in which there has been exposure (e.g. industrial workers) |
| Study of multiple exposures, such as the combined effect of oral contraceptives and smoking on myocardial infarction | Case control studies |
| Study of multiple end points, such as mortality from different causes | Cohort studies |
| Estimate of the incidence rate in exposed populations | Exclusively cohort studies |
| Study of covariables which change over time | Preferably cohort studies |
| Study of the effect of interventions | Intervention studies |
| Selection bias | N/A | 2 | 3 | 1 |
| Recall bias | N/A | 3 | 3 | 1 |
| Loss to follow-up | N/A | N/A | 1 | 3 |
| Confounding | 3 | 2 | 2 | 1 |
| Time required | 1 | 2 | 2 | 3 |
| Costs | 1 | 2 | 2 | 3 |
1 = slight; 2 = moderate; 3 = high; N/A, not applicable.
*Individual cases may deviate from this pattern.
Selecting the correct study type is an important aspect of study design (see "Study Design in Medical Research" in volume 11/2009). However, the scientific questions can only be correctly answered if the study is planned and performed at a qualitatively high level ( e9 ). It is very important to consider or even eliminate possible interfering factors (or confounders), as otherwise the result cannot be adequately interpreted. Confounders are characteristics which influence the target parameters. Although this influence is not of primary interest, it can interfere with the connection between the target parameter and the factors that are of interest. The influence of confounders can be minimized or eliminated by standardizing the procedure, stratification ( 18 ), or adjustment ( 19 ).
The decision as to which study type is suitable to answer a specific primary research question must be based not only on scientific considerations, but also on issues related to resources (personnel and finances), hospital capacity, and practicability. Many epidemiological studies can only be implemented if there is access to registry data. The demands for planning, implementation, and statistical evaluation for observational studies should be just as high for observational studies as for experimental studies. There are particularly strict requirements, with legally based regulations (such as the Medicines Act and Good Clinical Practice), for the planning, implementation, and evaluation of clinical studies. A study protocol must be prepared for both interventional and noninterventional studies ( 6 , 13 ). The study protocol must contain information on the conditions, question to be answered (objective), the methods of measurement, the implementation, organization, study population, data management, case number planning, the biometric evaluation, and the clinical relevance of the question to be answered ( 13 ).
Important and justified ethical considerations may restrict studies with optimal scientific and statistical features. A randomized intervention study under strictly controlled conditions of the effect of exposure to harmful factors (such as smoking, radiation, or a fatty diet) is not possible and not permissible for ethical reasons. Observational studies are a possible alternative to interventional studies, even though observational studies are less reliable and less easy to control ( 17 ).
A medical study should always be published in a peer reviewed journal. Depending on the study type, there are recommendations and checklists for presenting the results. For example, these may include a description of the population, the procedure for missing values and confounders, and information on statistical parameters. Recommendations and guidelines are available for clinical studies ( 14 , 20 , e10 , e11 ), for diagnostic studies ( 21 , 22 , e12 ), and for epidemiological studies ( 23 , e13 ). Since 2004, the WHO has demanded that studies should be registered in a public registry, such as www.controlled-trials.com or www.clinicaltrials.gov . This demand is supported by the International Committee of Medical Journal Editors (ICMJE) ( 24 ), which specifies that the registration of the study before inclusion of the first subject is an essential condition for the publication of the study results ( e14 ).
When specifying the study type and study design for medical studies, it is essential to collaborate with an experienced biometrician. The quality and reliability of the study can be decisively improved if all important details are planned together ( 12 , 25 ).
Acknowledgments
Translated from the original German by Rodney A. Yeates, M.A., Ph.D.
Conflict of interest statement
The authors declare that there is no conflict of interest in the sense of the International Committee of Medical Journal Editors.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 11 July 2024
Turnover intention and its related factors of clinical research coordinator in Hunan, China: a cross-sectional study
- Juan Li 1 ,
- JinHua Li 1 ,
- ZhengDi She 1 ,
- LiWen Guo 1 ,
- ShanZhi Gu 1 &
Scientific Reports volume 14 , Article number: 16054 ( 2024 ) Cite this article
Metrics details
- Health occupations
To explore the related factors of turnover intention in clinical research coordinators (CRCs) and assess the mediating effects of professional identity on the association between job burnout and turnover intention. In China, CRC has become increasingly common among clinical trial teams in recent years. However, limited published research focused on the status of turnover intention in CRCs. We invited all the 220 CRCs currently working at Hunan Cancer Hospital located in Changsha city in the central south of China from March to June 2018. Participants were asked to complete structured questionnaires regarding basic demographic information, job burnout, professional identity and turnover intention. A total of 202 participants were included in this study, with a response rate of 91.82%. The main reason for turnover intention among CRCs was human resources, followed by communications, management and material resources (per item score in each dimension: 2.14 vs. 2.43 vs. 2.65 vs. 2.83). All the correlations among job burnout, professional identity and turnover intention were statistically significant, with coefficients ranging from −0.197 to 0.615. Multiple liner regression analysis showed that older age, longer workhours per week, and lower level of professional identity were associated with the prevalence of turnover intention among CRCs. Besides, the association between job burnout and turnover intention was fully mediated by professional identity. This study revealed the status and causes of turnover intention among Chinese CRCs. Effective measures on decreasing working time and improving professional identity should be taken in order to reduce CRCs’ turnover intention.
Introduction
In recent years, the number of clinical trials in China has rapidly increased to meet the needs of development of new drugs. Until September 2021, 14,615 applications of clinical trials were registered by the Center for Drug Evaluation of National Medical Products Administration (NMPA) in China 1 . We are facing a crucial problem—how to ensure the authenticity and reliability of such huge clinical trial data. In fact, NMPA issued The Announcement of Self-examination and Inspection of Drug Clinical Trial Data in July 2015, launching the most stringent drug registration self-examination and inspection in history 2 . Every drug registration application must go through an onsite inspection of clinical trial to prove that its data are authentic before it can be approved.In order to conduct high-quality clinical trials, clinical research coordinator (CRC) is necessary to assist investigators with simple but tedious tasks 3 . Generally speaking, an eligible CRC usually has an educational background in medicine, nursing or pharmacy, and is directly employed in medical institutions 4 . As the person who interacts most with the subjects 5 , CRC is able to coordinate a variety of activities and improve the compliance of subjects with protocols 6 .
The need for CRCs is still expanding worldwide. For example, the job market for CRCs in the U.S. is estimated to grow by 9.9% between 2016 and 2026 7 . While it brings opportunities, it also ushers in more challenges. The strengthened regulation of clinical trials has raised the expectations for CRCs, calling for a greater emphasis on skills, training, and medical knowledge 8 . To ensure that the hired CRCs carry out their job properly and responsibly, companies invest a great deal of time and training, making it costly once CRCs leave their current job 9 . However, the turnover of CRCs is increasingly frequent in few decades. The CRC role has now become a temporary position for coordinators seeking to gain clinical experience prior to medical school or other graduate positions 10 . A study conducted in Italy discovered that only 13.8% of the CRCs was hired with a permanent contract, which would directly affect their future career plans 11 . China also faces the problem of excessive turnover of clinical research coordinator 12 . Therefore, reducing the turnover rates of CRCs is urgently needed for clinical research. Turnover intention is considered to be the main and immediate precursor of actual turnover behavior 13 , 14 .
However, the emerged abundant researches on CRCs in recent years, mostly concentrated on the application and impact of CRCs in clinical trials 15 , 16 , 17 . Little study focused on CRCs’ personal psychological characteristics including turnover intention, job burnout, or professional identity.To our knowledge, only one study has deeply investigated the severe situation of turnover among CRCs 18 . Focusing on CRCs’ personal psychological characteristics can help organizations and researchers identify areas for intervention, develop targeted support systems, and improve recruitment and selection strategies, ultimately leading to higher job satisfaction, lower burnout, and reduced turnover among CRCs.
The Job Embeddedness theory suggests that employees’ turnover intention may depend on the sense of embeddedness towards their professional and social environment 19 . However, this sense of professional identity can be gradually eroded by job burnout, which may ultimately increase employees’ likelihood of leaving their job 20 . Therefore, we hypothesized that professional identity directly affects turnover intention, and mediates the association between job burnout and turnover intention.In this study, we aimed to explore: (1) the current situation and influencing factors of turnover intention in CRCs; and (2) the role of professional identity between the association of job burnout with turnover intention. The findings may provide government and medical institutions with strategies to manage turnover intention among CRCs.
Study population
A cross-sectional survey was conducted in Hunan Provincial Tumor Hospital in China from 1st March 2021 to 30th June 2021. All methods were performed in accordance with the ethical principles of the Declaration of Helsinki.Targeted participants included CRCs who were currently employed in the hospital for at least one year. Participation in the survey was voluntary and we invited 220 CRCs to take part in this study. The inclusion and exclusion criteria are as follows: (1) The inclusion criteria: all the CRCs who were currently employed in the hospital for at least one year, regardless of their intention to leave the hospital in the future. (2) The exclusion criteria: CRCs who rejected to participant in this study. Eventually, a total of 202 participants were recruited for this study, with a response rate of 91.82%. The local institutional review board approved this study. All the participating CRCs gave their informed consent at his or her enrollment.
Instrument and measurement
Demographic characteristics.
We collected participants’ information on demographic characteristics including age, gender, educational level (associate’s degree or below, and bachelor’s degree or above), marital status (married, unmarried, and other), per capita monthly income (< 6000, 6000–8000, 8000–10,000, and > 10,000 Chinese Yuan (CNY)), working years (1–2, 3–4, ≥ 5 years), working hours per week (≤ 40 h, 40–50 h, 50–60 h, > 60 h), number of patients to manage (1–10, 11–20, 21–30, > 30), number of children to raise (0, 1, ≥ 2), and level of CRC (CRC, Senior CRC, and CRC leader).
Turnover intention
Turnover intention was assessed by the adapted Chinese version of the MISSCARE survey scale. The original scale was invented by Kalisch & Williams in 2009 21 , and the Chinese version was developed by Si and Qian 22 . Both scales consisted of two parts that part one evaluated the degree of missed nursing care and part two addressed the reasons 21 , 22 . Different from the original version whose part two consisted of three dimensions with 17 items, the Chinese version included 19 items in part two, indicating four factors named as management, communications, human resources and material resources 22 . In this study, we utilized the part two of Chinese version and adapted some of the descriptions to make them more appropriate to CRCs. Higher scores of the scale indicate lower level of turnover intention among CRCs.The adapted survey scales for CRCs were validated by confirmatory factor analysis (data not shown).
Job burnout
Job burnout was measured using the 22-item Maslach Burnout Inventory-Human Services Survey (MBI-HSS), with each item ranging from ‘never’ (0 point) to ‘every day’ (6 points) 23 . This scale contains three dimensions, including emotional exhaustion (9 items), depersonalization (5 items), and personal accomplishment (8 items). Higher scores on emotional exhaustion and depersonalization indicate higher level of job burnout, while the score of personal accomplishment is inversely correlated with job burnout. The Chinese version of MBI-HSS has been validated and widely used in Chinese population 24 , 25 , 26 .
Professional identity
Professional identity was assessed by Professional Identity Scale for Nurses developed by Liu and colleagues 27 . This 30-item instrument is a 5-point Likert scale comprising 5 dimensions: professional identity evaluation (9 items), professional social support (6 items), professional social proficiency (6 items), dealing with professional frustration (6 items), and professional self-reflection (3 items). The total score ranges from 30 to 150 points, with higher score indicating a higher level of professional identity. The scale showed good reliability with a Cronbach's coefficient of 0.94 and a split-half reliability of 0.88 in Chinese nurses 27 . In order to adapt the scale to CRCs, we modified some elements of the scale as appropriate.
Statistical analysis
Descriptive statistics were presented as mean with standard deviation (SD). Student t test or one-way analysis of variance test was utilized to examine the difference of turnover intention scores among subgroups of individual demographic variables, as appropriate. Pearson correlation analyses were applied to determine the relationships among turnover intention, job burnout and professional identity. In addition, multiple linear analysis was used to explore the potential related factors of turnover intention.Before each linear analysis, the four assumptions including linear, independence, normality and homoscedasticity were checked.
Previous studies have revealed that job burnout and professional identity were potential predictors of turnover intention 28 , 29 . In this study, we hypothesized that job burnout may lead to turnover intention among CRCs through lack of professional identity. Thus, mediation analysis was performed to address whether professional identity mediated the association between job burnout and turnover intention in CRCs. We used the PROCESS for SPSS with 5000 bootstrap resamples 30 . Whether the mediating effect existed depended on the significance of indirect effect between job burnout and turnover intention. In brief, full mediation was defined when indirect effect was significant whereas direct effect was non-significant, and partial mediation was defined when both indirect and direct effect were significant.
All statistical analyses were performed using the SPSS 21.0 software package (SPSS Institute, Chicago) with two-tailed tests where P < 0.05 was considered statistically significant.
Ethics approval
This study was reviewed and approved by the Ethics Committee for Clinical Trials, Hunan cancer hospital, and written informed consent was obtained for all participants. All participants enrolled in the study provided written informed consent.
Characteristics of study population
Table 1 summarizes the demographics of the study participants and the distribution of turnover intention scores in categorical items. The sample comprised 202 CRCs, 98.0% of whom were females and whose ages ranged from 16 to 35 years (Mean ± SD: 25.37 ± 3.04). Age groups showed differences in the mean scores of management dimension ( P = 0.015). As for working hours, 6.9%, 53.5%, 28.7% and 10.9% of CRCs worked for less than 40 h, 40 to 50 h, 50 to 60 h and more than 60 h per week, respectively. Groups for working hours per week performed differences in the mean scores of management dimension ( P = 0.038), communication dimension ( P = 0.005), human resources dimension ( P < 0.001) and the total score ( P = 0.003). Of the participants, the majority (85.6%) had no child yet and 11.9% CRCs had only one child to raise. Groups based on number of children to raise showed differences in the mean scores of management dimension ( P = 0.043). In addition, the turnover intention score had no statistical difference in the other characteristics of study population (all P > 0.05).
Reasons for turnover intention
Table 2 presents total means of each dimension of reasons for turnover intention in CRCs. By examining the total mean score for each dimension, human resources had the lowest mean score (Mean ± SD: 2.14 ± 0.66), and thus were the most prevalent reason for turnover intention; while the following mean scores for communications, management and material resources dimensions were 2.43 (SD = 0.74), 2.65 (SD = 0.79) and 2.83 (SD = 0.86), respectively.
The correlation among job burnout, professional identity, and turnover intention
Pearson correlation analysis between professional identity and turnover intention revealed a positive correlation (r = 0.413, P < 0.001) (see Table 3 ), which indicated that higher level of professional identity was related to lower level of turnover intention among CRCs. As for each job burnout dimension, higher levels of motional exhaustion (r = −0.197, P < 0.01), depersonalization (r = −0.212, P < 0.01) and felling of low personal accomplishment (r = 0.198, P < 0.01) were related to higher level of turnover intension. In addition, each job burnout dimension also displayed statistical correlations with professional identity (motional exhaustion: r = −0.365; depersonalization: r = −0.291; felling of low personal accomplishment: r = 0.364). In sum, job burnout, professional identity and turnover intention were correlated with each other.
The influencing factors of turnover intention assessed by multiple linear regression analysis
The factors associated with CRCs’ turnover intention are presented in Table 4 . All the assumptions of linear regression including linear, independence, normality and homoscedasticity were met (data not show).From Tables 1 and 3 , we firstly extracted the factors that were statistically associated or correlated with turnover intention. Then, those factors were included in the multiple liner regression model. According to the regression analysis, CRCs who were relatively older, who worked longer per week were more likely to report a higher risk of turnover intention. While, higher level of professional identity was independently associated with lower risk of turnover intention among CRCs.
Mediation effect of professional identity on job burnout and turnover intention
Figure 1 illustrates the constructed mediation model of professional identity on job burnout and turnover intention. For motional exhaustion subscale, the standardized effect value of motional exhaustion on professional identity was −0.4664 (path a1, P < 0.001) and the standardized effect value of professional identity on turnover intention was 0.2787 (path b1, P < 0.001). Thus, the standardized indirect effect value of motional exhaustion on turnover intention through professional identity was -0.1300 (path a1*b1, P < 0.001), confirming a significant mediation effect. However, the direct effect of motional exhaustion on turnover intention was not statistically significant (path c’ = −0.0486, P = 0.4391). Therefore, professional identity fully mediated the association between motional exhaustion and turnover intention. In the same manner, professional identity also fully mediated the association between depersonalization and turnover intention, and the association between reduced personal accomplishment and turnover intention. More detailed information on the outputs of mediation analysis was shown in Table 5 .
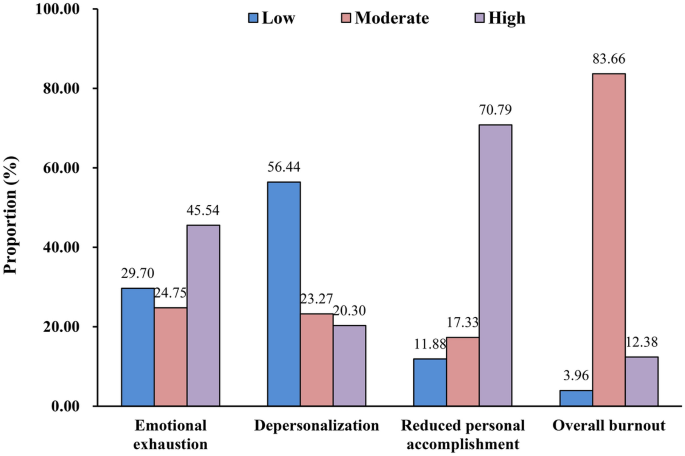
The constructed mediation models of professional identity on the association between job burnout [motional exhaustion ( a ), depersonalization ( b ), felling of low personal accomplishment ( c )] and turnover intention.
Key findings
To our knowledge, this may be the first study focusing on the turnover intention among CRCs in China. In this study, three major findings were obtained. Firstly, the main reason for turnover intention among CRCs was human resources, followed by communications, management and material resources. Secondly, older age, longer workhour per week, and lower level of professional identity were associated with the prevalence of turnover intention among CRCs. Thirdly, professional identity fully mediated the association between job burnout and turnover intention. Our research findings may not only expand the understandings of turnover intention in CRCs, but also provide evidence for policy-making to reduce turnover intention of CRCs in China.
Epidemiological evidence
Vanderbilt University Medical Center conducted a survey on CRCs over a 12-month period from October 2017 to September 2018 18 . The study discovered 9 significant predictors related to retention including salary, level of CRC and so on. Nevertheless, in our study, salary and level of CRC were not significantly associated with turnover in CRCs. Instead, we found older age, longer working hours per week, and lower level of professional identity were predictors of turnover intention. One possible reason was the different occupational environment between the USA and China. CRCs in China may care less about their own career development under China's immature CRC management system. On the other hand, the American study did not collect information related to age, level of education, or working hours, which were taken into account in our study. In fact, these basis characteristics have been suggested influencing factors with turnover of other medical staff, such as nurses and doctors 31 , 32 , 33 .
In this study, we applied adapted MISSCARE survey scale to evaluate the turnover intention of CRCs 22 . The scale consisted of four factors named as management, communications, human resources and material resources. According to our results, human resources were the most prevalent reason for turnover intention of CRCs. Such findings were consistent with most studies on nurses 34 , 35 . In fact, CRCs and nurses were similar to some extent, at least their most time was spent on dealing with patients. Besides, they both may be faced with staffing inadequacy or heavy workloads, which belong to the human resources dimension. Such reasons could be effectively resolved by hospitals or companies through promotions on supportive work environment, work schedule management, and enhancing CRCs’ teamwork. In addition, CRCs also needed to improve their time management skills and working competence in order to deal with the tedious work.
Mediation effect
In sociology, job burnout, professional identity and turnover intention have been researched extensively by sociologists. Many previous studies have revealed the complex relationships among the three variables in other occupational populations 28 , 29 . For example, Zhang et al. 28 found that professional identity had an indirect negative effect on turnover intention through the mediating effect of burnout among general practitioners. In this study, we discovered that professional identity fully mediated the associations between job burnout and turnover intention among CRCs. The results seemed to be inconsistent with previous studies, because the mediator has changed from job burnout to professional identity. The phenomenon could be interpretated appropriately. For nurses or doctors, they were cultivated their sense of professional identity as early as their school years. Once they had a high degree of identity with their career, they would reduce the incidence of job burnout 36 , which in turn caused a reduction of turnover intention 37 , 38 . As for CRCs, they usually lack education or training on identity with their career when they were in school or pre-employment due to the undeveloped CRC management system in China. Thus, their unstable professional identity may be easily altered by feelings of burnout.
In our study, we found that professional identity had direct effect on turnover intention, which was consistent with previous studies 39 , 40 .When CRCs had a high level of professional identity with their career, they would be willing to devote more time and efforts to their work, without considering leaving their present career. This finding suggests that improving CRCs' professional identity could serve as an effective way to reduce turnover intention. Actions such as providing pre-job training, reducing the work intensity, extending break time, increasing communications between CRCs and principal investigators are warranted to improve the degree of professional identity of CRCs.
Limitations
To our knowledge, to date, this is the first study to assess the situation of turnover intention among CRCs and to explore the role of professional identity in the association of job burnout with turnover intention in China. However, this study also has several limitations. First, our study could not confirm the temporality and causality of the observed relationships due to its cross-sectional design. Second, CRCs’ turnover intention and professional identity were evaluated by adapted MISSCARE survey scale and Professional Identity Scale 22 , 27 , respectively, whereas the two scales were initially developed for nurses. Worth mentioning, we were in the process of verifying the reliability and validity of the two adapted scales. Third, some potential influencing factors were not included into our questionnaire, such as work schedules, sleep quality, social support, health status, mental health and so on. Fourth, the study was conducted in a relatively narrow time frame from 1st March 2021 to 30th June 2021, which may result in seasonal bias. In addition, The R 2 in the regression models showed a little small which may suggest a poor fit of the model to the data. However, it could still provide evidence of the mediating effect to some extent, even if the overall explanatory power of the model is limited. Finally, CRCs in our study were recruited from Hunan Cancer Hospital, which may limit the externality of our results to general hospitals or other specialized hospitals. Further research on this topic is needed to include more potential influencing factors and expand the sample selection in the future.
Implications and recommendations for practice
CRCs play important roles in promoting project implementation and enhancing quality of clinical trials. Awareness and management of turnover intention in CRCs may stabilize the workforce in the field of clinical trials. Therefore, the government and medical institutions should establish a more developed management system to reduce the loss of CRCs. Measures such as enhancing CRCs’ professional identity and reducing working hours appropriately would be effective approaches.
Conclusions
Our study may be the first to assess the situation of turnover intention among CRCs in China. It revealed that the main reason for turnover intention of CRCs was human resources. Age, working hours per week, and professional identity were influencing factors of turnover intention. Besides, professional identity had fully mediating effect on the association of job burnout with turnover intention. Institutional and policy changes such as reducing burdensome working hours and increasing professional identity should be implemented to lower turnover intentions among CRCs. A reasonable management system on CRCs is appealed in the near future.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
National Medical Products Administration
Clinical research coordinator
Maslach Burnout Inventory-Human Services Survey
Standard deviation
NMPA. Drug clinical trial registration and information publicity platform. http://www.chinadrugtrials.org.cn/
NMPA. The Announcement of Self-examination and Inspection of Drug Clinical Trial Data. July 22, 2015 Announcement No. 117. https://www.nmpa.gov.cn/xxgk/ggtg/qtggtg/20150722173601172.html .
Cinefra, M. et al. The critical role of the clinical research coordinator for clinical trials: A survey in oncology. Med Access Point Care. 1 , e76-81 (2017).
Article Google Scholar
Karen, S. et al. The role and potential contribution of clinical research nurses to clinical trials. J Clin Nurs. 17 (4), 549–557 (2010).
Google Scholar
Davis, A. M., Hull, S. C., Grady, C., Wilfond, B. S. & Henderson, G. E. The invisible hand in clinical research: The study coordinator’s critical role in human subjects protection. J Law Med Ethics. 30 (3), 411–419 (2002).
Article PubMed PubMed Central Google Scholar
Cagnazzo, C. et al. Clinical research coordinators: a crucial resource. Recenti Prog Med. 110 (2), 65–67 (2019).
PubMed Google Scholar
The job market for clinical research coordinators in the United States, 2021. https://www.careerexplorer.com/careers/clinical-research-coordinator/job-market/
Fisher, E. et al. Finding the right candidate: Developing hiring guidelines for screening applicants for clinical research coordinator positions. J Clin Transl Sci. 6 (1), e20. https://doi.org/10.1017/cts.2021.853 (2021).
Gullatte, M. M. & Jirasakhiran, E. Q. Retention and recruitment: reversing the order. Clin J Oncol Nurs 9 , 597–604. https://doi.org/10.1188/05.CJON.597-604 (2005).
Article PubMed Google Scholar
Buchanan, D. A. et al. Empowering the clinical research coordinator in academic medical centers. Mayo Clin Proc Innov Qual Outcomes 5 , 265–273. https://doi.org/10.1016/j.mayocpiqo.2020.09.014 (2020).
Cagnazzo, C. et al. Clinical research: Enough players to get out there?. Recenti Prog Med 110 , 285–291. https://doi.org/10.1701/3182.31609 (2019).
Cao, L. Y., Chen, Y. C., Guo, W. & Xie, L. L. Status quo and countermeasures of job mobility among clinical research coordinator/clinical research associate in Chongqing. China Pharm. 33 (03), 275–279 (2022) ( (In Chinese) ).
Fukui, S., Rollins, A. L. & Salyers, M. P. Characteristics and job stressors associated with turnover and turnover intention among community mental health providers. Psychiatr Serv 71 , 289–292. https://doi.org/10.1176/appi.ps.201900246 (2020).
Feijen-de Jong, E. I., van der Voort-Pauw, N., Nieuwschepen-Ensing, E. G. & Kool, L. Intentions to leave and actual turnover of community midwives in the Netherlands: A mixed method study exploring the reasons why. Women Birth S1871–5192 (22), 00029–00034. https://doi.org/10.1016/j.wombi.2022.02.004 (2022).
Lv, Z. et al. Exploration of application of clinical research coordinator in acupuncture and moxibustion study. Zhongguo Zhen Jiu. 36 (7), 747–749 (2016).
Zhu, W. et al. The validation of a questionnaire to delineate clinical research coordinator roles in China. Perspect Psychiatr Care. 56 (3), 629–635 (2020).
Chen, L., Chen, Z. & Chen, H. The appearance and increase in the quantity and proportion of the clinical research coordinator’s service fee in drug clinical trial research fund and its impact on trial quality. Cost Eff Resour Alloc. 19 (1), 41 (2021).
Buchanan, D. A. et al. Empowering the clinical research coordinator in academic medical centers. Mayo Clin Proc Innov Qual Outcomes. 5 (2), 265–273 (2020).
Yildiz, B. & Elibol, E. Turnover intention linking compulsory citizenship behaviours to social loafing in nurses: A mediation analysis. J Nurs Manag 29 , 653–663. https://doi.org/10.1111/jonm.13200 (2021).
Kuilanoff, E. Burnout and our professional identity crisis as clinical educators. Acad Med 96 , 616–617. https://doi.org/10.1097/ACM.0000000000003994 (2021).
Kalisch, B. J. & Williams, R. A. Development and psychometric testing of a tool to measure missed nursing care. J Nurs Adm. 39 (5), 211–219 (2009).
Si, F. & Qian, Z. G. The Chinese version of MISSCARE survey scale and its reliability and validity. J. Qilu Nurs. 23 (24), 32–35 (2017) ( (In Chinese) ).
Maslach, C. & Jackson, S. E. The measurement of experienced burnout. J Organ Behav. 2 (2), 99–113 (1981).
Ye, Z. H., Luo, H. & Jiang, A. L. Diagnostic standard and norms of Maslach Burnout Inventory for nurses in Hangzhou. Chin. J. Nurs. 43 (3), 207–209 (2008) ( (In Chinese) ).
Deng, Y. T. et al. A multicenter study on the validation of the Burnout Battery: A new visual analog scale to screen job burnout in oncology professionals. Psychooncology. 26 (8), 1120–1125 (2017).
Gan, Y. et al. Prevalence of burnout and associated factors among general practitioners in Hubei, China: A cross-sectional study. BMC Public Health. 19 (1), 1607 (2019).
Liu, L., Hao, Y. & Liu, X. Development of professional identity scale for nurses. Nurs. J. Chin. People’s Liberation Army. 28 (2A), 18–20 (2011) ( (in Chinese) ).
Zhang, T. et al. Association of professional identity, job satisfaction and burnout with turnover intention among general practitioners in China: Evidence from a national survey. BMC Health Serv Res. 21 (1), 382 (2021).
Article CAS PubMed PubMed Central Google Scholar
Steffens, N. K., Yang, J., Jetten, J., Haslam, S. A. & Lipponen, J. The unfolding impact of leader identity entrepreneurship on burnout, work engagement, and turnover intentions. J Occup Health Psychol. 23 (3), 373–387 (2018).
Hayes, A. F. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach 1st edn. (The Guilford Press, 2013).
Oh, S. & Kim, H. Turnover intention and its related factors of employed doctors in Korea. Int J Environ Res Public Health. 16 (14), 2509 (2019).
Labrague, L. J., Gloe, D. S., McEnroe-Petitte, D. M., Tsaras, K. & Colet, P. C. Factors influencing turnover intention among registered nurses in Samar Philippines. Appl Nurs Res. 39 , 200–206 (2018).
Chegini, Z. et al. Missed nursing care and related factors in Iranian hospitals: A cross-sectional survey. J Nurs Manag. 28 (8), 2205–2215 (2020).
Du, H., Yang, Y., Wang, X. & Zang, Y. A cross-sectional observational study of missed nursing care in hospitals in China. J Nurs Manag. 28 (7), 1578–1588 (2020).
Saqer, T. J. & AbuAlRub, R. F. Missed nursing care and its relationship with confidence in delegation among hospital nurses. J Clin Nurs. 27 (13–14), 2887–2895 (2018).
Yu, J. et al. Professional self-concept and burnout among medical school faculty in South Korea: A cross-sectional study. BMC Med Educ. 19 (1), 248 (2019).
Jiang, H. et al. Satisfaction, burnout and intention to stay of emergency nurses in Shanghai. Emerg Med J. 34 (7), 448–453 (2017).
Na, S. Y. & Park, H. The effect of nurse’s emotional labor on turnover intention: Mediation effect of burnout and moderated mediation effect of authentic leadership. J Korean Acad Nurs. 49 (3), 286–297 (2019).
Sabanciogullari, S. & Dogan, S. Relationship between job satisfaction, professional identity and intention to leave the profession among nurses in Turkey. J Nurs Manag. 23 (8), 1076–1085 (2015).
Jourdain, G. & Chênevert, D. Job demands-resources, burnout and intention to leave the nursing profession: a questionnaire survey. Int J Nurs Stud. 47 (6), 709–722 (2010).
Download references
Acknowledgements
The authors thank all of the participants, coordinators, and administrators for their support and help during the research.
Author information
Authors and affiliations.
Hunan Cancer Hospital, Changsha, Hunan, China
Juan Li, JinHua Li, ZhengDi She, LiWen Guo, ShanZhi Gu & Wen Lu
You can also search for this author in PubMed Google Scholar
Contributions
ShanZhi Gu,and Wen Lu contributed to the conception or design of the work. Juan Li, ZhengDi She and, LiWen Guo contributed to the acquisition, analysis, or interpretation of data for the work. Juan Li , Wen Lu and ShanZhi Gu drafted the manuscript and critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding authors
Correspondence to ShanZhi Gu or Wen Lu .
Ethics declarations
Competing interests.
All authors have read and approved this version of the article, and declared that they had no competing or financial interests to disclosure.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Li, J., Li, J., She, Z. et al. Turnover intention and its related factors of clinical research coordinator in Hunan, China: a cross-sectional study. Sci Rep 14 , 16054 (2024). https://doi.org/10.1038/s41598-024-66960-8
Download citation
Received : 14 October 2023
Accepted : 05 July 2024
Published : 11 July 2024
DOI : https://doi.org/10.1038/s41598-024-66960-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

COMMENTS
What is clinical research, and is it right for you? Clinical research is the comprehensive study of the safety and effectiveness of the most promising advances in patient care. Clinical research is different than laboratory research. It involves people who volunteer to help us better understand medicine and health.
This is all described as clinical research - the study of human health and disease. Clinical research involves human participants in some way and aims at moving findings from bench to bedside - translating basic research into ways of helping patients. Clinical research can include direct studies involving humans, such as clinical trials ...
Clinical research is an alternative terminology used to describe medical research. Clinical research involves people, and it is generally carried out to evaluate the efficacy of a therapeutic drug, a medical/surgical procedure, or a device as a part of ...
Interested in clinical research? Learn about the phases of clinical trials, why older and diverse participants are needed, and what to ask before participating.
A type of study in which people are observed or certain outcomes are measured. No attempt is made by the researcher to affect the outcome — for example, no treatment is given by the researcher. Clinical trial (interventional study). During clinical trials, researchers learn if a new test or treatment works and is safe.
Clinical studies assist researchers and clinicians in understanding medical conditions and treatments. Clinical trials and observational studies are the most popular forms of clinical studies. Both teach doctors and nurses about new pharmaceuticals, devices, surgical procedures, and therapies to treat or prevent patients' ailments.
What are clinical trials? Clinical trials are research studies in which people volunteer to help find answers to specific health questions.
Abstract. The goal of this review was to present the essential steps in the entire process of clinical research. Research should begin with an educated idea arising from a clinical practice issue. A research topic rooted in a clinical problem provides the motivation for the completion of the research and relevancy for affecting medical practice ...
Different types of clinical research are used depending on what the researchers are studying. Below are descriptions of some different kinds of clinical research.
Clinical research occurs in many formats and can involve anyone. Learn how you can participate and contribute to medical advances.
The idea for a clinical research study—also known as a clinical trial—often starts in the laboratory. After researchers test new therapies or procedures in the laboratory and in animal studies ...
The term "clinical research" refers to the entire process of studying and writing about a drug, a medical device or a form of treatment, which includes conducting interventional studies ( clinical trials) or observational studies on human participants. [1] [3] Clinical research can cover any medical method or product from its inception in the ...
Understanding Clinical Studies. Part of the challenge of explaining clinical research to the public is describing the important points of a study without going into a detailed account of the study's design. There are many different kinds of clinical studies, each with their own strengths and weaknesses, and no real shorthand way to explain them.
The NIH defines a clinical trial as a research study in which one or more human subjects are prospectively assigned to one or more interventions (which may include placebo or other control) to evaluate the effects of those interventions on health-related biomedical or behavioral outcomes. The term "prospectively assigned" refers to a pre ...
What is Clinical Research? Clinical research is the study of health and illness in people. It is the way we learn how to prevent, diagnose and treat illness. Clinical research describes many different elements of scientific investigation. Simply put, it involves human participants and helps translate basic research (done in labs) into new treatments and […]
Clinical studies are a broader category of research conducted on human participants to study about different diseases and their treatments. Clinical trials, also known as interventional studies, are a type of clinical study carried out to answer a defined question on the research conducted. It is a specific category which falls under clinical ...
A clinical trial is a component of a clinical study. People who participate in clinical trials are directed to follow the specific interventions set by the initial research protocols for the purpose of the study. Interventions may include drugs, devices, or modifications to a participants' behavior (e.g. diet and exercise).
The study design used to answer a particular research question depends on the nature of the question and the availability of resources. In this article, which is the first part of a series on "study designs," we provide an overview of research study designs and their classification. The subsequent articles will focus on individual designs.
During clinical research. Clinical research happens in many ways, depending on the type of study. Studies can take place at hospitals, clinics, research centers, universities, over the phone, or on the internet. They may take a few days, weeks, or even years. Researchers may assign participants into different groups.
A clinical trial is a type of clinical research study. A clinical trial is an experiment designed to answer specific questions about possible new treatments or new ways of using existing (known) treatments. Clinical trials are done to determine whether new drugs or treatments are safe and effective. They are usually part of a long, careful ...
Clinical research is the study of health and illness in people. Scientists may have many reasons for doing a clinical study, such as: • To explore the cause of a disease or a set of symptoms • To test if a treatment will help with a symptom or condition • To learn how a certain behavior affects people's health.
This glossary of terms is derived from a list copyrighted by the University of Kentucky, Office of Research Integrity (1990). For clinical research-specific definitions, see also the Clinical Research Glossary developed by the Multi-Regional Clinical Trials (MRCT) Center of Brigham and Women's Hospital and Harvard and the Clinical Data ...
Increasing the use of community-based trials requires updating the regulatory framework that governs innovative clinical trial designs.
There are various types of scientific studies such as experiments and comparative analyses, observational studies, surveys, or interviews. The choice of study type will mainly depend on the research question being asked. When making decisions, patients and doctors need reliable answers to a number of questions. Depending on the medical condition and patient's personal situation, the following ...
Background: Electronic informed consent (eIC) is increasingly used in clinical research due to several benefits including increased enrollment and improved efficiency. Within a learning health care system, a pilot was conducted with an eIC for linking data from electronic health records with national registries, general practitioners, and other hospitals.
Consider the driving trends in clinical research: Research takes place at more sites and in more countries than ever before; Study designs are increasingly complex, with many different treatment arms and drug types; Movement restrictions and regulatory complexities related to the global coronavirus pandemic add new logistical difficulties
The effectiveness of instructional videos as a stand-alone tool for the acquisition of practical skills is yet unknown because instructional videos are usually didactically embedded. Therefore, we evaluated the acquisition of the skill of a humeral intraosseous access via video in comparison to that of a self-study with an additional retention test.
Three main areas of medical research can be distinguished by study type: basic (experimental), clinical, and epidemiological research. Furthermore, clinical and epidemiological studies can be further subclassified as either interventional or noninterventional.
To explore the related factors of turnover intention in clinical research coordinators (CRCs) and assess the mediating effects of professional identity on the association between job burnout and ...
This study's limitations include the absence of a sedentary control group and groups exclusively focused on aerobic or strength training exercises. Although the research presents new compelling data on combined exercise training and its impact on blood pressure, further studies are needed to investigate discrepancies within the groups of ...