Interventions to improve nurses' job satisfaction: A systematic review and meta-analysis
Affiliations.
- 1 Research Unit of Nursing Science and Health Management, University of Oulu, Oulu, Finland.
- 2 Azienda per l'Assistenza Sanitaria n. 5 "Friuli Occidentale", Pordenone, Italy.
- 3 Center for Life Course Health Research, University of Oulu, Oulu, Finland.
- 4 Medical Research Center Oulu, Oulu University Hospital and University of Oulu, Oulu, Finland.
- 5 Nursing Research Foundation, Helsinki, Finland.
- 6 The Finnish Centre for Evidence-Based Health Care, Helsinki, Finland.
- 7 WHO Collaborating Centre for Nursing, Helsinki, Finland.
- 8 Oulu University of Applied Sciences, Oulu, Finland.
- 9 Northern Ostrobothnia Hospital District, Finland.
- PMID: 32128864
- DOI: 10.1111/jan.14342

Abstract in English, Chinese
Aims: To identify current best evidence on the types of interventions that have been developed to improve job satisfaction among nurses and on the effectiveness of these interventions.
Design: The systematic review is a quantitative systematic review and meta-analysis following a profile-likelihood random-effects model.
Data sources: CINAHL, Medic, and Pubmed (Medline).
Review methods: PICOS eligibility criteria were used to select original studies published between 2003-2019. The articles were screened by title (N = 489), abstract (N = 61), and full-text (N = 47). A total of 20 articles remained after the full-text screening process and further assess on risk of bias. The screening process was conducted by two authors independently and finally agreed together. A meta-analysis was performed to determine how the identified interventions influence nurses' job satisfaction.
Results: The interventions were primarily educational and consisted of workshops, educational sessions, lessons, and training sessions. The postintervention differences between intervention and control groups in meta-analysis revealed that two interventions significantly improved nurses' job satisfaction. Notably, the spiritual intelligence training protocol and Professional Identity Development Program were found to be effective in improving job satisfaction.
Conclusion: Healthcare organizations and managers should consider implementing effective interventions to improve nurses' job satisfaction and reduce turnover. The results reported in this study highlight that nurse managers should focus on organizational strategies that will foster the intrinsic motivation of employees.
Impact: The current nursing shortage and increased turnover intentions are proving to be a global problem. For this reason, it is imperative that nurse managers plan strategies to improve nurses´ job satisfaction. The effective interventions detected in this study are a first step for developing human resource strategies for healthcare organizations. These findings propose that extrinsic factors (e.g., salary and rewards) will never be as effective in maintaining job satisfaction as intrinsic factors (e.g., spiritual intelligence, professional identity, and awareness).
目的: 识别提高护士工作满意度的介入治疗类型及其有效性的现有最佳证据。 设计: 系统综述指的是遵循子集似然随机效应模型的定量系统综述与荟萃分析。 数据来源: CINAHL护理学数据库、Medic国际医疗器械展览会和Pubmed文献服务检索系统(Medline联机医学文献分析和检索系统)。 审查方法: 采用PICOS合格标准用于甄选2003年至2019年期间发表的原创研究。按照标题(N=489)、摘要(N=61)和全文(N=47)对文章进行筛选。在完成全文筛选后,留下20篇文章,进一步评估偏倚风险。由两位作者独立进行筛选过程,并最终达成一致。并且还要进行荟萃分析,以探讨所确定的介入治疗对护士工作满意度的影响。 结果: 介入治疗以教育为主,包括讲习班、教育班、上课和培训班。通过荟萃分析,从干预后介入治疗组与对照组的差异可以看出,两种介入治疗显著提高了护士的工作满意度。值得注意的是,灵性智力训练方案和职业认同发展计划能够行之有效地提高工作满意度。 结论: 医疗机构和管理者应考虑实施有效的介入治疗,以提高护士的工作满意度,减少离职率。本研究报告的结果强调,护士部门的管理人员应当侧重能够培养护士内在动机的组织策略。 影响: 当下医护人员的短缺和离职意愿的攀升被证明是一个全球普遍化的问题。为此,护士部门的管理人员制定提高护士工作满意度的策略势在必行。本研究中发现的有效介入治疗是制定医疗机构人力资源战略的第一步。这些发现表明,在维持护士的工作满意度方面,外在因素(如工资和报酬)永远不及内在因素(如灵性智力、职业认同和认识)来得有效。.
Keywords: interventional study; job satisfaction; meta-analysis; nurses; systematic review.
© 2020 John Wiley & Sons Ltd.
Publication types
- Meta-Analysis
- Systematic Review
- Job Satisfaction
- Nursing Staff, Hospital*
- Personnel Turnover
- Research article
- Open access
- Published: 07 August 2018
Job satisfaction and career intentions of registered nurses in primary health care: an integrative review
- Elizabeth Halcomb ORCID: orcid.org/0000-0001-8099-986X 1 ,
- Elizabeth Smyth 1 &
- Susan McInnes 1
BMC Family Practice volume 19 , Article number: 136 ( 2018 ) Cite this article
18k Accesses
67 Citations
23 Altmetric
Metrics details
There has been a significant growth of the international primary health care (PHC) nursing workforce in recent decades in response to health system reform. However, there has been limited attention paid to strategic workforce growth and evaluation of workforce issues in this setting. Understanding issues like job satisfaction and career intentions are essential to building capacity and skill mix within the workforce. This review sought to explore the literature around job satisfaction and career intentions of registered nurses working in PHC.
An integrative review was conducted. Electronic databases including: CINAHL, MEDLINE, Scopus and Web of Science, and reference lists of journal publications were searched for peer-reviewed literature published between 2000 and 2016 related to registered nurse job satisfaction and career intentions. Study quality was appraised, before thematic analysis was undertaken to synthesise the findings.
Twenty papers were included in this review. Levels of job satisfaction reported were variable between studies. A range of factors impacted on job satisfaction. Whilst there was agreement on the impact of some factors, there was a lack of consistency between studies on other factors. Four of the six studies which reported career intentions identified that nearly half of their participants intended to leave their current position.
This review identifies gaps in our understanding of job satisfaction and career intentions in PHC nurses. With the growth of the PHC nursing workforce internationally, there is a need for robust, longitudinal workforce research to ensure that employment in this setting is satisfying and that skilled nurses are retained.
Peer Review reports
The recruitment and retention of nurses is problematic worldwide. There is a maldistribution of human resources for health, a shortage in the overall number of qualified nurses and an aging nursing workforce [ 1 ]. Job satisfaction has been cited as an important factor contributing to the turnover of nurses and as an antecedent to nursing retention [ 2 , 3 , 4 ]. Therefore, understanding factors that impact on job satisfaction is important to inform recruitment and retention strategies.
The concept of job satisfaction is multifaceted and complex. Job satisfaction has been the focus of much research around organisational behaviour. Lu, et al. [ 5 ] define job satisfaction as not only how an individual feels about their job but also the nature of the job and the individuals’ expectation of what their job should provide. To this end, job satisfaction is comprised of various components, including; job conditions, communication, the nature of the work, organisational policies and procedures, remuneration and conditions, promotion / advancement opportunities, recognition / appreciation, security and supervision / relationships [ 5 ]. Whilst levels of job satisfaction vary, several common factors emerge across studies [ 6 , 7 ]. These include working conditions and the organisational environment, levels of stress, role conflict and ambiguity, role perceptions and content and organisational and professional commitment [ 5 , 6 , 7 , 8 ]. Given these factors it becomes clear that research about job satisfaction cannot be undertaken across the nursing profession as a whole, but rather needs to consider various settings and organisational environments to understand the issues facing different nursing groups.
Career intentions can be described as the intention to leave ones’ job voluntarily [ 9 ]. This process may start with a psychological response to negative situations in the workplace or undesirable aspects of the job. Subsequently, a cognitive decision is made to leave the position and withdrawal behaviours occur as the person moves out of the workplace [ 10 ]. Like job satisfaction, a number of common determinants for career intention have been identified. These include organisational factors, management style, workload and stress, role perceptions, empowerment, remuneration and employment conditions and opportunities for advancement [ 10 ]. In several studies, job satisfaction has been shown to impact on career intentions [ 11 , 12 ].
Despite the common themes in this workforce literature, much of the research around job satisfaction and career intentions reported to date has focussed on acute care nurses [ 2 , 5 , 6 , 10 , 11 , 13 , 14 ]. Given the impact of organisational factors, roles and employment conditions it is important to consider different groups of nurses, such as those employed in PHC, who are employed in settings unlike those of their acute care colleagues. PHC nurses practice in a range of settings, including general practices, schools, refugee health services, correctional settings, non-government organisations and community health centres [ 15 ]. As such, their employment conditions and work environments are unlike those of acute care nurses who are employed by large health providers or government funded health services (17). The small business nature of primary care in many countries and the predominance of charities and non-government health providers makes employment in the PHC setting unique [ 16 , 17 , 18 ]. Lorenz and De Brito Guirardello [ 19 ] describe the PHC work environment as “not always favourable to the professional practice of nurses”(p. 927), citing lack of equipment, inappropriate physical environment and occupational risks as key contributors to dissatisfaction. Additionally, there are significant difference between the roles, responsibilities and work environments of acute and PHC nurses [ 20 ]. These differences and the impact of such factors on job satisfaction and career intentions mean that acute care nursing workforce research cannot be simply generalised to the PHC setting. With the growth in the PHC nursing workforce and the need for a strong nursing workforce in this setting it is timely to explore the job satisfaction and career intentions of PHC nurses. Therefore, this review sought to critically synthesise the literature around the job satisfaction and career intentions of registered nurses working in PHC.
The underlying research questions are:
What was known about the main outcomes of studies regarding PHC registered nurses job satisfaction?
What was known about the career intentions of PHC registered nurses?
Registered nurses are the focus of the review as they are the largest nursing workforce in PHC [ 21 ].
This integrative literature review is informed by Whittemore and Knafls [ 22 ] framework. It provides a thorough examination of the existing literature following the five stages of review: problem identification, literature search, data evaluation, data analysis and presentation [ 22 ].
Search strategy
A systematic search strategy was designed to guide the search of electronic databases: CINAHL, MEDLINE, Scopus and Web of Science. Key search terms included; nurs*, primary health care, community care and job satisfaction or career intention. The search was confined to English language peer reviewed papers of original research. Given the significant changes in PHC systems internationally, only papers published between January 2000 and 2016 were considered. The reference lists of publications were also reviewed to identify further literature.
Inclusion criteria
Table 1 details the inclusion and exclusion criteria. Papers were excluded if they focussed on a particular nursing specialty (e.g. community mental health nurses) or were based in residential care settings (e.g. nursing homes), as the issues with this workforce are somewhat different to other PHC settings. Studies that focussed on nurse practitioners and/or advanced practice nurses (e.g. [ 23 ]), or specifically on nurse managers were excluded as these nurses may have different perceptions and experiences to registered nurses. Remoteness itself was not considered to constitute PHC nursing, therefore, papers focussed on rural or remote nurses without being specifically PHC focussed were excluded. Research articles were also excluded if the findings did not isolate PHC nurses from acute care nurses or other health professionals.
Study selection
After removal of duplicates, 477 citations were yielded from the search. These citations were exported to Endnote X8™ for review of their titles, followed by closer evaluation of the abstract. This process identified that 346 papers did not meet the inclusion criteria, leaving 131 papers where the full-text was retrieved. Of these papers, 111 did not meet the inclusion criteria, and so were excluded. This left 20 papers for inclusion in the review. (Fig. 1 ).
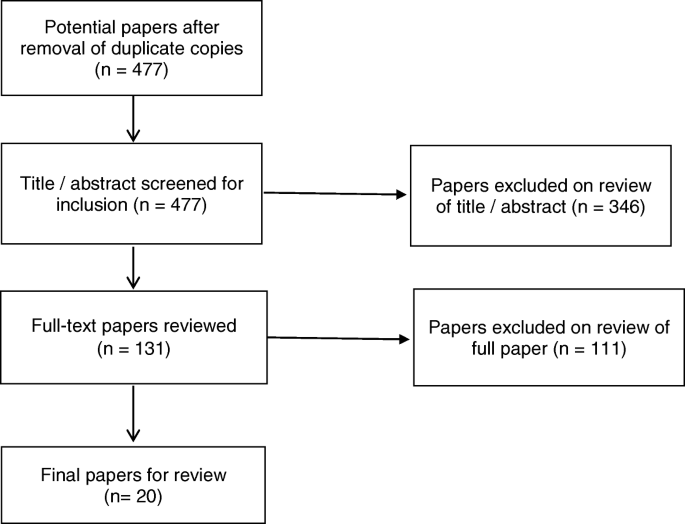
Process of paper selection – Prisma Flow diagram [ 24 ]
Appraisal of methodological quality
Determining the methodological quality of the included studies was difficult due to the broad sampling frame and various research designs [ 22 ]. As identified by Whittemore and Knafl [ 22 ], there is no gold standard for evaluating quality in research reviews. In this review we conducted quality appraisal using the tool provided by the Center for Evidence Based Management [ 25 ]. The major areas of concern were around the quality of reporting of the instrument development and validity / reliability measures in some papers [ 26 , 27 , 28 , 29 , 30 , 31 ]. Given the relatively small number of included papers and the minor nature of the limitations identified none of the studies were excluded based on their methodological quality.
Data abstraction and synthesis
Once the included papers were identified all data was abstracted into a summary table. The main characteristics that were extracted included;
Study design
Main outcomes related to job satisfaction or career intention
The nature of the included papers, in terms of the heterogeneity of the measures used, meant that thematic analysis was the most appropriate technique for aggregating the findings. Therefore, data is presented in a narrative form around the key themes that emerged from the literature.
Of the 20 included papers (Table 2 ), 15 (75%) described quantitative studies, 4 (20%) papers described qualitative projects, and the remaining paper (5%) employed a mixed-method approach. Most of the included papers reported research undertaken in Canada ( n = 8, 40%), with other studies coming out of the United Kingdom ( n = 4, 20%), the United States of America ( n = 5, 25%), one paper each from Saudi Arabia, South Africa, and Brazil.
The sample sizes of included studies varied from 31 [ 30 ] to 1044 participants [ 26 ]. Participants spanned the scope of PHC and included community nurses, primary health nurses, general practice nurses, school nurses, and district nurses. In some studies the data from various primary care nursing groups was reported in an aggregated form [ 32 ], whilst in other papers there was an attempt to tease out the differences between groups [ 26 , 29 ].
Eleven (55%) papers focussed on job satisfaction only [ 27 , 28 , 30 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 ], and three (15%) papers reported only data on career intention or turnover [ 31 , 32 , 41 ]. A further six (30%) papers combined measures of job satisfaction and career intention within the same study [ 2 , 19 , 26 , 29 , 42 , 43 ].
The key features and predominant findings of papers are summarised in Table 2 . Five overarching themes emerged, namely; levels of job satisfaction, factors that enhanced job satisfaction, factors that reduced levels of job satisfaction, career intentions, and, factors that impacted on career intentions.
Levels of job satisfaction
The variation in measurement of job satisfaction across studies and the differences in respondent characteristics makes comparison difficult. Most tools measured job satisfaction quantitatively using a Likert scale (agree to disagree) [ 2 , 19 , 26 , 37 , 38 , 39 ], whilst one study used qualitative data collected from focus groups and interviews [ 28 ]. Studies measured different aspects of job satisfaction including; overall satisfaction (enjoyment, pride), specific aspects of the job (pay, rewards, resources, task requirements, work conditions, training, quality of care, time) and supervision (authority, autonomy, feedback, appreciation, organisational policies, interaction).
In some studies just over half of the respondents were reported to be satisfied with their job [ 19 , 39 ], whilst in other studies a greater majority indicated that they were satisfied [ 28 ]. A small number of studies reported moderate [ 2 , 38 ] to low levels of satisfaction [ 37 , 42 ]. Those studies which reported lower levels of satisfaction used more items to measure satisfaction (42 items and 80 items respectively) [ 37 , 42 ], compared to studies reporting high levels of satisfaction which used only 4 items [ 19 , 39 ].
Factors influencing job satisfaction
The ten studies which explored the relationship between job satisfaction and demographics / professional variables demonstrated significant variation [ 2 , 19 , 29 , 34 , 36 , 37 , 38 , 39 , 40 , 43 ]. Whilst two studies found that age had no significant impact on job satisfaction [ 2 , 43 ], three others demonstrated that older nurses were more satisfied than their younger colleagues [ 29 , 37 , 38 ]. Similarly, there were variable findings related to the impact of education, with three papers finding no relationship with job satisfaction or inconclusive findings [ 2 , 36 , 37 ], and two papers demonstrating that nurses with higher educational qualifications had reported higher work satisfaction [ 34 , 40 ]. In contrast, Delobelle et al. [ 2 ] found that Nursing Assistants and Enrolled Nurses were more satisfied than Registered Nurses.
Curtis and Glacken [ 37 ] reported that those employed for over 10 years had a significantly higher level of job satisfaction than other nurses. However, other studies reported an inverse relationship between years worked in PHC and satisfaction [ 40 ] and no significant differences between satisfaction and years of nursing [ 2 ].
Other factors that positively contributed to satisfaction included control over clinical practice and decision-making [ 19 , 34 , 39 , 40 ], community satisfaction [ 43 ], organisational support [ 19 ], remuneration [ 38 ], and workload [ 39 ].
There was significant agreement between studies in terms of the factors that contributed positively to job satisfaction. These included the professional role, respect and recognition from clients and managers, workplace relationships, autonomy, access to resources and the flexibility of the role [ 2 , 27 , 28 , 29 , 30 , 31 , 33 , 34 , 37 , 43 ].
Factors negatively impacting job satisfaction
There was a high level of agreement amongst included studies about factors that negatively impacted respondents’ levels of satisfaction. Seven studies identified concerns about adequate remuneration [ 2 , 28 , 29 , 34 , 35 , 37 , 43 ]. When comparing hospital and community nurses, Campbell, et al. [ 34 ] identified that hospital nurses were significantly more likely than community nurses to be satisfied with their pay.
Another key factor identified in several studies related to the time pressures and high administrative workloads that impact on patient care [ 2 , 26 , 30 , 33 , 37 ]. Other factors identified to negatively impact job satisfaction included; a lack of recognition [ 2 , 28 , 33 , 34 ], poor role clarity [ 30 , 34 , 37 ] and poor organisational communication [ 29 , 34 ].
Career intentions
The included studies present an important picture around career intentions. However, caution needs to be applied in the interpretation of these data, as most studies comprise of an ageing workforce who will naturally retire in the near future. Six studies sought to explore the factors impacting on retention [ 2 , 32 , 34 , 41 , 42 , 43 ] The highest reported career intentions was reported by Delobelle, et al. [ 2 ] with half of all nurse participants ( n = 69; 51.1%) considering leaving PHC in the next 2 years. Both Betkus and MacLeod [ 43 ] and Almalki, et al. [ 42 ] also reported that nearly half (48 and 40%) intended to leave their current PHC job in the next year. Royer [ 32 ] similarly identified that some 46% of participants aged 35–45 years were considering leaving, and almost 40% of those aged 56–65 were thinking about leaving. The remaining two studies reported that few participants intended to leave their current position [ 34 , 41 ].
The findings of the three studies which explored job satisfaction and quality of worklife [ 2 , 42 , 43 ], lacked consistency. Almalki, et al. [ 42 ] demonstrated that quality of worklife was significantly related to turnover intent ( p < 0.001), however, this only explained 26% of the variance and was not included in the final model. Whilst Betkus and MacLeod [ 43 ] reported no correlation between job satisfaction and retention, Delobelle, et al. [ 2 ] found that turnover intent was significantly explained by job satisfaction, age and education ( p < 0.001). Other factors that were identified as having an impact on career intentions included gender [ 42 ], work environment [ 42 ], remuneration [ 42 ], education [ 2 , 41 , 42 ], satisfaction with supervision [ 2 ], feelings of isolation [ 41 ], length of time in position / years of experience [ 32 , 42 ].
This review provides the first synthesis of the literature around job satisfaction and career intentions of registered nurses working in PHC. Given the differences in organisational context, employment conditions and practice environment that likely impact job satisfaction and career intention [ 17 , 18 , 19 ] it is important that this group are explored beyond the context of the broader nursing workforce. Considering the imperatives to grow the workforce in PHC settings, to meet community demand, understanding this literature is important to inform both practice and policy. Dissatisfaction with nursing employment is reported in the broader nursing workforce literature. In their survey of 33,659 medical–surgical nurses across 12 European countries, Aiken, et al. [ 44 ] concluded that more than one in five nurses were dissatisfied with their employment. The variation in job satisfaction identified in this review highlights the need for further large well-designed longitudinal investigations of the PHC nurse workforce to monitor workforce issues, such as satisfaction and career intentions, over time. Given the links between nurse satisfaction and both retention and patient outcomes [ 44 ], this issue should be prioritised.
Our review demonstrated agreement between studies in terms of the positive impact of a professional role, respect, recognition, workplace relationships and autonomy upon job satisfaction. This is consistent with the acute care nursing literature where modifiable factors within the workplace have been demonstrated to influence both job and career satisfaction [ 45 ]. In their study, Nantsupawat, et al. [ 46 ] demonstrated that job dissatisfaction and intention to leave were significantly lower in nurses who worked in a better work environment. Similarly, in their systematic review, Cicolini, et al. [ 14 ] found a significant link between nurses empowerment and satisfaction. The significant role of such modifiable factors highlights an opportunity for managers, employers and policy makers to implement strategies which can improve the workplace and, subsequently, enhance satisfaction.
A key finding of this review was the negative impact of poor remuneration on job satisfaction. Whilst concerns about pay have been previously identified in the acute sector [ 44 , 47 ], the challenge of lower rates of pay in PHC compared to the acute sector has long been reported [ 17 , 48 ]. This review adds to the evidence-base around the impact of this disparity on the PHC nursing workforce and highlights the significant implications of not addressing this issue.
Our review also revealed that in many studies large numbers of nurses were intending to leave PHC employment in the near future [ 2 , 42 , 43 ]. This clearly has significant implications for the workforce and service delivery. However, measures of the factors affecting career intentions were variable across included studies as were findings. The difficulties in synthesising such disparate data have been previously identified in the acute care literature [ 13 ]. Despite this, there were clear similarities between our review and the broader literature around nurse turnover and intention to leave. In their systematic review of nurses intention to leave their employment, Chan, et al. [ 13 ] identified that intention to leave was impacted by a complex combination of organisational and individual factors. Organisational factors included the work environment, culture, commitment, work demands and social support. In contrast, individual factors related to job satisfaction, burnout and demographic factors. The complex interplay of multiple factors that underlie retention is probably the reason that retention is the highest when interventions such as mentoring and in-depth orientations are used to support staff [ 49 ].
In their study of acute care nurses Galletta, et al. [ 50 ] conclude that the quality of relationships among staff is an important factor in nurses’ decisions to leave. Interprofessional relationships in PHC have long been identified as presenting unique challenges [ 48 , 51 ]. The complex environment of PHC, whereby services are funded by small businesses or non-government agencies [ 52 ], combines with the relatively rapid shift towards interdisciplinary care to create challenges for staff in developing positive relationships [ 53 ]. The importance of positive relationships, respect of roles and recognition of value between co-workers demonstrated in our review highlights the value of further work to enhance interprofessional collaboration.
Limitations
Whilst this review synthesised the available literature, the variation in measurement instruments and sample sizes made comparison difficult. Since not all papers reported the reliability or validity of the instruments they used it is possible that these instruments had issues in their validity. The data presented, however, represents the best available evidence to address the research question.
A further limitation is the variation between PHC settings and international PHC systems that makes comparison difficult. Whilst this review has included all papers written about PHC nurses internationally, local variations mean that care needs to be taken when generalising findings to other contexts, even within PHC.
This review has identified some key factors that impact on both job satisfaction and career intentions amongst PHC nurses. The importance of the work environment and workplace relationships highlights the need to implement strategies that enhance modifiable workplace factors. The numbers of nurses across studies indicating an intention to leave is a significant concern at a time when we need to build the PHC workforce internationally. Findings from this review highlight the need for action by managers, educators, employers and policy makers to enhance support for nurses in PHC.
Implications for practice and research
There is urgent need to build capacity within the PHC nursing workforce internationally to meet service demands. This review has highlighted a number of issues around job satisfaction and career intention that impact on the retention of nurses in PHC. Exploring strategies to address the modifiable antecedents to nurse job dissatisfaction has the potential to improve retention. Maintaining happy and skilled nurses in the workforce has the potential to build workforce capacity and enhance patient outcomes.
This review has demonstrated that gaps remain in our knowledge around job satisfaction and career intention among PHC registered nurses. Further well-designed longitudinal research is required to explore the trajectory of careers in PHC. Additionally, mixed methods approaches are likely required to explore not only quantitative job satisfaction, but also to reveal how the aspects of satisfaction impact on PHC nurses.
Abbreviations
Primary Health Care
Buchan J, Twigg D, Dussault G, Duffield C, Stone PW. Policies to sustain the nursing workforce: an international perspective. Int Nurs Rev. 2015;62(2):162–70.
Article PubMed CAS Google Scholar
Delobelle P, Rawlinson JL, Ntuli S, Malatsi I, Decock R, Depoorter AM. Job satisfaction and turnover intent of primary healthcare nurses in rural South Africa: a questionnaire survey. J Adv Nurs. 2011;67(2):371–83.
Article PubMed Google Scholar
AbuAlRub R, El-Jardali F, Jamal D, Al-Rub NA. Exploring the relationship between work environment, job satisfaction, and intent to stay of Jordanian nurses in underserved areas. ANR. 2016;31:19–23.
PubMed Google Scholar
Spence Laschinger HK, Zhu J, Read E. New nurses’ perceptions of professional practice behaviours, quality of care, job satisfaction and career retention. J Nurs Manag. 2016;24(5):656–65.
Lu H, Barriball KL, Zhang X, While AE. Job satisfaction among hospital nurses revisited: a systematic review. Int J Nurs Stud. 2012;49(8):1017–38.
Hayes B, Bonner A, Pryor J. Factors contributing to nurse job satisfaction in the acute hospital setting: a review of recent literature. J Nurs Manag. 2010;18(7):804–14.
Atefi N, Abdullah K, Wong L, Mazlom R. Factors influencing registered nurses perception of their overall job satisfaction: a qualitative study. Int Nurs Rev. 2014;61(3):352–60.
Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. 2015;12(1):652–66.
Article PubMed PubMed Central Google Scholar
Takase M, Yamashita N, Oba K. Nurses' leaving intentions: antecedents and mediating factors. J Adv Nurs. 2008;62(3):295–306.
Hayes LJ, O’Brien-Pallas L, Duffield C, Shamian J, Buchan J, Hughes F, Laschinger HKS, North N. Nurse turnover: a literature review – an update. Int J Nurs Stud. 2012;49(7):887–905.
Kim J-K, Kim M-J. A review of research on hospital nurses' turnover intention. J Korean Acad Nurs. 2011;17(4):538–50.
Article Google Scholar
Liu Y. Job satisfaction in nursing: a concept analysis study job satisfaction in nursing. Int Nurs Rev. 2016;63(1):84–91.
Chan ZC, Tam WS, Lung MK, Wong WY, Chau CW. A systematic literature review of nurse shortage and the intention to leave. J Nurs Manag. 2013;21(4):605–13.
Cicolini G, Comparcini D, Simonetti V. Workplace empowerment and nurses' job satisfaction: a systematic literature review. J Nurs Manag. 2014;22(7):855–71.
Australian Institute of Health and Welfare: Australian Nursing and Midwifery Workforce Data and additional information. Canberra, Australia; 2014.
Google Scholar
Freund T, Everett C, Griffiths P, Hudon C, Naccarella L, Laurant M. Skill mix, roles and remuneration in the primary care workforce: who are the healthcare professionals in the primary care teams across the world? Int J Nurs Stud. 2015;52(3):727–43.
Halcomb E, Ashley C, James S, Smythe E. Employment conditions of Australian PHC nurses. Collegian. 2018;25(1):65–71.
Halcomb EJ, Ashley C. Australian primary health care nurses most and least satisfying aspects of work. J Clin Nurs. 2017;36(3–4):535–45.
Lorenz VR, De Brito Guirardello E. The environment of professional practice and burnout in nurses in primary healthcare. Rev Lat Am Enfermagem. 2014;22(6):926–33.
Poghosyan L, Liu J, Shang J, D’Aunno T. Practice environments and job satisfaction and turnover intentions of nurse practitioners: implications for primary care workforce capacity. Health Care Manag Rev. 2015;
Health Workforce Australia: Health Workforce 2025 - Doctors, Nurses and Midwives. Adelaide; 2012.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Desborough J, Parker R, Forrest L. Nurse satisfaction with working in a nurse led primary care walk-in Centre: an Australian experience. Aust J Adv Nurs. 2013;31(1):11–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Center for Evidence Based Management. Critical Appraisal Checklist for Cross-Sectional Study. 2014. https://www.cebma.org/wp-content/uploads/Critical-Appraisal-Questions-for-a-Cross-Sectional-Study-july-2014.pdf . Accessed May 22 2017.
Armstrong-Stassen M, Cameron SJ. Concerns, satisfaction, and retention of Canadian community health nurses. J Community Health Nurs. 2005;22(4):181–94.
Flynn L, Deatrick JA. Home care Nurses' descriptions of important agency attributes. J Nurs Scholarsh. 2003;35(4):385–90.
Junious DL, Johnson RJ, Peters RJ Jr, Markham CM, Kelder SH, Yacoubian GS Jr. A study of school nurse job satisfaction. Journal of School Nursing (Allen Press Publishing Services Inc). 2004;20(2):88–93.
Storey C, Cheater F, Ford J, Leese B. Retaining older nurses in primary care and the community. J Adv Nurs. 2009;65(7):1400–11.
Stuart EH, Jarvis A, Daniel K. A ward without walls? District nurses' perceptions of their workload management priorities and job satisfaction. J Clin Nurs. 2008;17(22):3012–20.
Tourangeau A, Patterson E, Rowe A, Saari M, Thomson H, MacDonald G, Cranley L, Squires M. Factors influencing home care nurse intention to remain employed. J Nurs Manag. 2014;22(8):1015–26.
Royer L. Empowerment and commitment perceptions of community/public health nurses and their tenure intention. Public Health Nurs. 2011;28(6):523–32.
Best MF, Thurston NE. Canadian public health nurses' job satisfaction. Public Health Nurs. 2006;23(3):250–5.
Campbell SL, Fowles ER, Weber BJ. Organizational structure and job satisfaction in public health nursing. Public Health Nurs. 2004;21(6):564–71.
Cameron S, Armstrong-Stassen M, Bergeron S, Out J. Recruitment and retention of nurses: challenges facing hospital and community employers. Can J Nurs Leadersh. 2004;17(3):79–92.
Cole S, Ouzts K, Stepans MB. Job satisfaction in rural public health nurses. J Public Health Manag Pract. 2010;16(4):E1–6.
Curtis EA, Glacken M. Job satisfaction among public health nurses: a national survey. J Nurs Manag. 2014;22(5):653–63.
Doran D, Pickard J, Harris J, Coyte PC, MacRae AR, Laschinger HS, Darlington G, Carryer J. The relationship between managed competition in home care nursing services and nurse outcomes. Can J Nurs Res. 2007;39(3):151–65.
Graham KR, Davies BL, Woodend AK, Simpson J, Mantha SL. Impacting Canadian public health nurses' job satisfaction. Can J Public Health. 2011;102(6):427–31.
Tullai-McGuinness S. Home healthcare practice environment: predictors of RN satisfaction. Res Nurs Health. 2008;31(3):252–60.
O'Donnell C, Jabareen H, Watt G. Practice nurses' workload, career intentions and the impact of professional isolation: a cross-sectional survey. BMC Nurs. 2010;9(1):2.
Almalki MJ, Fitzgerald G, Clark M. The relationship between quality of work life and turnover intention of primary health care nurses in Saudi Arabia. BMC Health Serv Res. 2012;12:314.
Betkus MH, MacLeod MLP. Retaining public health nurses in rural British Columbia: the influence of job and community satisfaction. Can J Public Health. 2004;95(1):54–8.
Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W. Nurses' reports of working conditions and hospital quality of care in 12 countries in Europe. Int J Nurs Stud. 2013;50(2):143–53.
Laschinger HKS. Job and career satisfaction and turnover intentions of newly graduated nurses. J Nurs Manag. 2012;20(4):472–84.
Nantsupawat A, Kunaviktikul W, Nantsupawat R, Wichaikhum OA, Thienthong H, Poghosyan L. Effects of nurse work environment on job dissatisfaction, burnout, intention to leave. Int Nurs Rev. 2017;64(1):91–8.
Al-Dossary R, Vail J, Macfarlane F. Job satisfaction of nurses in a Saudi Arabian university teaching hospital: a cross-sectional study. Int Nurs Rev. 2012;59(3):424–30.
Halcomb EJ, Davidson PM, Griffiths R, Daly J. Cardiovascular disease management: time to advance the practice nurse role? Aust Health Rev. 2008;32(1):44–55.
Lartey S, Cummings G, Profetto-McGrath J. Interventions that promote retention of experienced registered nurses in health care settings: a systematic review. J Nurs Manag. 2014;22(8):1027–41.
Galletta M, Portoghese I, Battistelli A, Leiter MP. The roles of unit leadership and nurse–physician collaboration on nursing turnover intention. J Adv Nurs. 2013;69(8):1771–84.
McInnes S, Peters K, Bonney A, Halcomb E. An integrative review of facilitators and barriers influencing collaboration and teamwork between general practitioners and nurses working in general practice. J Adv Nurs. 2015;71(9):1973–85.
McInnes S, Peters K, Bonney A, Halcomb E. The influence of funding models on collaboration in Australian general practice. Aust J Prim Health. 2017;23(1):31–6.
Williams A, Sibbald B. Changing roles and identities in primary health care: exploring a culture of uncertainty. J Adv Nurs. 1999;29(3):737–45.
Download references
No funding was received for this study.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and affiliations.
School of Nursing, University of Wollongong, Northfields Ave, Wollongong, NSW, 2522, Australia
Elizabeth Halcomb, Elizabeth Smyth & Susan McInnes
You can also search for this author in PubMed Google Scholar
Contributions
EH conceived the study, conducted the initial search and participated in the data analysis and drafting of the paper. ES confirmed the initial search and participated in the data analysis and drafting of the paper. SM participated in the data analysis and drafting of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Elizabeth Halcomb .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
Professor Elizabeth Halcomb is an Associate Editor of BMC Family Practice. Nil other competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Halcomb, E., Smyth, E. & McInnes, S. Job satisfaction and career intentions of registered nurses in primary health care: an integrative review. BMC Fam Pract 19 , 136 (2018). https://doi.org/10.1186/s12875-018-0819-1
Download citation
Received : 08 February 2018
Accepted : 12 July 2018
Published : 07 August 2018
DOI : https://doi.org/10.1186/s12875-018-0819-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary health care
- Job satisfaction
- Career intention
BMC Primary Care
ISSN: 2731-4553
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Fam Pract

Job satisfaction and career intentions of registered nurses in primary health care: an integrative review
Elizabeth halcomb.
School of Nursing, University of Wollongong, Northfields Ave, Wollongong, NSW 2522 Australia
Elizabeth Smyth
Susan mcinnes, associated data.
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
There has been a significant growth of the international primary health care (PHC) nursing workforce in recent decades in response to health system reform. However, there has been limited attention paid to strategic workforce growth and evaluation of workforce issues in this setting. Understanding issues like job satisfaction and career intentions are essential to building capacity and skill mix within the workforce. This review sought to explore the literature around job satisfaction and career intentions of registered nurses working in PHC.
An integrative review was conducted. Electronic databases including: CINAHL, MEDLINE, Scopus and Web of Science, and reference lists of journal publications were searched for peer-reviewed literature published between 2000 and 2016 related to registered nurse job satisfaction and career intentions. Study quality was appraised, before thematic analysis was undertaken to synthesise the findings.
Twenty papers were included in this review. Levels of job satisfaction reported were variable between studies. A range of factors impacted on job satisfaction. Whilst there was agreement on the impact of some factors, there was a lack of consistency between studies on other factors. Four of the six studies which reported career intentions identified that nearly half of their participants intended to leave their current position.
This review identifies gaps in our understanding of job satisfaction and career intentions in PHC nurses. With the growth of the PHC nursing workforce internationally, there is a need for robust, longitudinal workforce research to ensure that employment in this setting is satisfying and that skilled nurses are retained.
The recruitment and retention of nurses is problematic worldwide. There is a maldistribution of human resources for health, a shortage in the overall number of qualified nurses and an aging nursing workforce [ 1 ]. Job satisfaction has been cited as an important factor contributing to the turnover of nurses and as an antecedent to nursing retention [ 2 – 4 ]. Therefore, understanding factors that impact on job satisfaction is important to inform recruitment and retention strategies.
The concept of job satisfaction is multifaceted and complex. Job satisfaction has been the focus of much research around organisational behaviour. Lu, et al. [ 5 ] define job satisfaction as not only how an individual feels about their job but also the nature of the job and the individuals’ expectation of what their job should provide. To this end, job satisfaction is comprised of various components, including; job conditions, communication, the nature of the work, organisational policies and procedures, remuneration and conditions, promotion / advancement opportunities, recognition / appreciation, security and supervision / relationships [ 5 ]. Whilst levels of job satisfaction vary, several common factors emerge across studies [ 6 , 7 ]. These include working conditions and the organisational environment, levels of stress, role conflict and ambiguity, role perceptions and content and organisational and professional commitment [ 5 – 8 ]. Given these factors it becomes clear that research about job satisfaction cannot be undertaken across the nursing profession as a whole, but rather needs to consider various settings and organisational environments to understand the issues facing different nursing groups.
Career intentions can be described as the intention to leave ones’ job voluntarily [ 9 ]. This process may start with a psychological response to negative situations in the workplace or undesirable aspects of the job. Subsequently, a cognitive decision is made to leave the position and withdrawal behaviours occur as the person moves out of the workplace [ 10 ]. Like job satisfaction, a number of common determinants for career intention have been identified. These include organisational factors, management style, workload and stress, role perceptions, empowerment, remuneration and employment conditions and opportunities for advancement [ 10 ]. In several studies, job satisfaction has been shown to impact on career intentions [ 11 , 12 ].
Despite the common themes in this workforce literature, much of the research around job satisfaction and career intentions reported to date has focussed on acute care nurses [ 2 , 5 , 6 , 10 , 11 , 13 , 14 ]. Given the impact of organisational factors, roles and employment conditions it is important to consider different groups of nurses, such as those employed in PHC, who are employed in settings unlike those of their acute care colleagues. PHC nurses practice in a range of settings, including general practices, schools, refugee health services, correctional settings, non-government organisations and community health centres [ 15 ]. As such, their employment conditions and work environments are unlike those of acute care nurses who are employed by large health providers or government funded health services (17). The small business nature of primary care in many countries and the predominance of charities and non-government health providers makes employment in the PHC setting unique [ 16 – 18 ]. Lorenz and De Brito Guirardello [ 19 ] describe the PHC work environment as “not always favourable to the professional practice of nurses”(p. 927), citing lack of equipment, inappropriate physical environment and occupational risks as key contributors to dissatisfaction. Additionally, there are significant difference between the roles, responsibilities and work environments of acute and PHC nurses [ 20 ]. These differences and the impact of such factors on job satisfaction and career intentions mean that acute care nursing workforce research cannot be simply generalised to the PHC setting. With the growth in the PHC nursing workforce and the need for a strong nursing workforce in this setting it is timely to explore the job satisfaction and career intentions of PHC nurses. Therefore, this review sought to critically synthesise the literature around the job satisfaction and career intentions of registered nurses working in PHC.
The underlying research questions are:
- What was known about the main outcomes of studies regarding PHC registered nurses job satisfaction?
- What was known about the career intentions of PHC registered nurses?
Registered nurses are the focus of the review as they are the largest nursing workforce in PHC [ 21 ].
This integrative literature review is informed by Whittemore and Knafls [ 22 ] framework. It provides a thorough examination of the existing literature following the five stages of review: problem identification, literature search, data evaluation, data analysis and presentation [ 22 ].
Search strategy
A systematic search strategy was designed to guide the search of electronic databases: CINAHL, MEDLINE, Scopus and Web of Science. Key search terms included; nurs*, primary health care, community care and job satisfaction or career intention. The search was confined to English language peer reviewed papers of original research. Given the significant changes in PHC systems internationally, only papers published between January 2000 and 2016 were considered. The reference lists of publications were also reviewed to identify further literature.
Inclusion criteria
Table 1 details the inclusion and exclusion criteria. Papers were excluded if they focussed on a particular nursing specialty (e.g. community mental health nurses) or were based in residential care settings (e.g. nursing homes), as the issues with this workforce are somewhat different to other PHC settings. Studies that focussed on nurse practitioners and/or advanced practice nurses (e.g. [ 23 ]), or specifically on nurse managers were excluded as these nurses may have different perceptions and experiences to registered nurses. Remoteness itself was not considered to constitute PHC nursing, therefore, papers focussed on rural or remote nurses without being specifically PHC focussed were excluded. Research articles were also excluded if the findings did not isolate PHC nurses from acute care nurses or other health professionals.
Inclusion / Exclusion Criteria
Study selection
After removal of duplicates, 477 citations were yielded from the search. These citations were exported to Endnote X8™ for review of their titles, followed by closer evaluation of the abstract. This process identified that 346 papers did not meet the inclusion criteria, leaving 131 papers where the full-text was retrieved. Of these papers, 111 did not meet the inclusion criteria, and so were excluded. This left 20 papers for inclusion in the review. (Fig. 1 ).

Process of paper selection – Prisma Flow diagram [ 24 ]
Appraisal of methodological quality
Determining the methodological quality of the included studies was difficult due to the broad sampling frame and various research designs [ 22 ]. As identified by Whittemore and Knafl [ 22 ], there is no gold standard for evaluating quality in research reviews. In this review we conducted quality appraisal using the tool provided by the Center for Evidence Based Management [ 25 ]. The major areas of concern were around the quality of reporting of the instrument development and validity / reliability measures in some papers [ 26 – 31 ]. Given the relatively small number of included papers and the minor nature of the limitations identified none of the studies were excluded based on their methodological quality.
Data abstraction and synthesis
Once the included papers were identified all data was abstracted into a summary table. The main characteristics that were extracted included;
- Study design
- Main outcomes related to job satisfaction or career intention
The nature of the included papers, in terms of the heterogeneity of the measures used, meant that thematic analysis was the most appropriate technique for aggregating the findings. Therefore, data is presented in a narrative form around the key themes that emerged from the literature.
Of the 20 included papers (Table 2 ), 15 (75%) described quantitative studies, 4 (20%) papers described qualitative projects, and the remaining paper (5%) employed a mixed-method approach. Most of the included papers reported research undertaken in Canada ( n = 8, 40%), with other studies coming out of the United Kingdom ( n = 4, 20%), the United States of America ( n = 5, 25%), one paper each from Saudi Arabia, South Africa, and Brazil.
Summary table
The sample sizes of included studies varied from 31 [ 30 ] to 1044 participants [ 26 ]. Participants spanned the scope of PHC and included community nurses, primary health nurses, general practice nurses, school nurses, and district nurses. In some studies the data from various primary care nursing groups was reported in an aggregated form [ 32 ], whilst in other papers there was an attempt to tease out the differences between groups [ 26 , 29 ].
Eleven (55%) papers focussed on job satisfaction only [ 27 , 28 , 30 , 33 – 40 ], and three (15%) papers reported only data on career intention or turnover [ 31 , 32 , 41 ]. A further six (30%) papers combined measures of job satisfaction and career intention within the same study [ 2 , 19 , 26 , 29 , 42 , 43 ].
The key features and predominant findings of papers are summarised in Table Table2. 2 . Five overarching themes emerged, namely; levels of job satisfaction, factors that enhanced job satisfaction, factors that reduced levels of job satisfaction, career intentions, and, factors that impacted on career intentions.
Levels of job satisfaction
The variation in measurement of job satisfaction across studies and the differences in respondent characteristics makes comparison difficult. Most tools measured job satisfaction quantitatively using a Likert scale (agree to disagree) [ 2 , 19 , 26 , 37 – 39 ], whilst one study used qualitative data collected from focus groups and interviews [ 28 ]. Studies measured different aspects of job satisfaction including; overall satisfaction (enjoyment, pride), specific aspects of the job (pay, rewards, resources, task requirements, work conditions, training, quality of care, time) and supervision (authority, autonomy, feedback, appreciation, organisational policies, interaction).
In some studies just over half of the respondents were reported to be satisfied with their job [ 19 , 39 ], whilst in other studies a greater majority indicated that they were satisfied [ 28 ]. A small number of studies reported moderate [ 2 , 38 ] to low levels of satisfaction [ 37 , 42 ]. Those studies which reported lower levels of satisfaction used more items to measure satisfaction (42 items and 80 items respectively) [ 37 , 42 ], compared to studies reporting high levels of satisfaction which used only 4 items [ 19 , 39 ].
Factors influencing job satisfaction
The ten studies which explored the relationship between job satisfaction and demographics / professional variables demonstrated significant variation [ 2 , 19 , 29 , 34 , 36 – 40 , 43 ]. Whilst two studies found that age had no significant impact on job satisfaction [ 2 , 43 ], three others demonstrated that older nurses were more satisfied than their younger colleagues [ 29 , 37 , 38 ]. Similarly, there were variable findings related to the impact of education, with three papers finding no relationship with job satisfaction or inconclusive findings [ 2 , 36 , 37 ], and two papers demonstrating that nurses with higher educational qualifications had reported higher work satisfaction [ 34 , 40 ]. In contrast, Delobelle et al. [ 2 ] found that Nursing Assistants and Enrolled Nurses were more satisfied than Registered Nurses.
Curtis and Glacken [ 37 ] reported that those employed for over 10 years had a significantly higher level of job satisfaction than other nurses. However, other studies reported an inverse relationship between years worked in PHC and satisfaction [ 40 ] and no significant differences between satisfaction and years of nursing [ 2 ].
Other factors that positively contributed to satisfaction included control over clinical practice and decision-making [ 19 , 34 , 39 , 40 ], community satisfaction [ 43 ], organisational support [ 19 ], remuneration [ 38 ], and workload [ 39 ].
There was significant agreement between studies in terms of the factors that contributed positively to job satisfaction. These included the professional role, respect and recognition from clients and managers, workplace relationships, autonomy, access to resources and the flexibility of the role [ 2 , 27 – 31 , 33 , 34 , 37 , 43 ].
Factors negatively impacting job satisfaction
There was a high level of agreement amongst included studies about factors that negatively impacted respondents’ levels of satisfaction. Seven studies identified concerns about adequate remuneration [ 2 , 28 , 29 , 34 , 35 , 37 , 43 ]. When comparing hospital and community nurses, Campbell, et al. [ 34 ] identified that hospital nurses were significantly more likely than community nurses to be satisfied with their pay.
Another key factor identified in several studies related to the time pressures and high administrative workloads that impact on patient care [ 2 , 26 , 30 , 33 , 37 ]. Other factors identified to negatively impact job satisfaction included; a lack of recognition [ 2 , 28 , 33 , 34 ], poor role clarity [ 30 , 34 , 37 ] and poor organisational communication [ 29 , 34 ].
Career intentions
The included studies present an important picture around career intentions. However, caution needs to be applied in the interpretation of these data, as most studies comprise of an ageing workforce who will naturally retire in the near future. Six studies sought to explore the factors impacting on retention [ 2 , 32 , 34 , 41 – 43 ] The highest reported career intentions was reported by Delobelle, et al. [ 2 ] with half of all nurse participants ( n = 69; 51.1%) considering leaving PHC in the next 2 years. Both Betkus and MacLeod [ 43 ] and Almalki, et al. [ 42 ] also reported that nearly half (48 and 40%) intended to leave their current PHC job in the next year. Royer [ 32 ] similarly identified that some 46% of participants aged 35–45 years were considering leaving, and almost 40% of those aged 56–65 were thinking about leaving. The remaining two studies reported that few participants intended to leave their current position [ 34 , 41 ].
The findings of the three studies which explored job satisfaction and quality of worklife [ 2 , 42 , 43 ], lacked consistency. Almalki, et al. [ 42 ] demonstrated that quality of worklife was significantly related to turnover intent ( p < 0.001), however, this only explained 26% of the variance and was not included in the final model. Whilst Betkus and MacLeod [ 43 ] reported no correlation between job satisfaction and retention, Delobelle, et al. [ 2 ] found that turnover intent was significantly explained by job satisfaction, age and education ( p < 0.001). Other factors that were identified as having an impact on career intentions included gender [ 42 ], work environment [ 42 ], remuneration [ 42 ], education [ 2 , 41 , 42 ], satisfaction with supervision [ 2 ], feelings of isolation [ 41 ], length of time in position / years of experience [ 32 , 42 ].
This review provides the first synthesis of the literature around job satisfaction and career intentions of registered nurses working in PHC. Given the differences in organisational context, employment conditions and practice environment that likely impact job satisfaction and career intention [ 17 – 19 ] it is important that this group are explored beyond the context of the broader nursing workforce. Considering the imperatives to grow the workforce in PHC settings, to meet community demand, understanding this literature is important to inform both practice and policy. Dissatisfaction with nursing employment is reported in the broader nursing workforce literature. In their survey of 33,659 medical–surgical nurses across 12 European countries, Aiken, et al. [ 44 ] concluded that more than one in five nurses were dissatisfied with their employment. The variation in job satisfaction identified in this review highlights the need for further large well-designed longitudinal investigations of the PHC nurse workforce to monitor workforce issues, such as satisfaction and career intentions, over time. Given the links between nurse satisfaction and both retention and patient outcomes [ 44 ], this issue should be prioritised.
Our review demonstrated agreement between studies in terms of the positive impact of a professional role, respect, recognition, workplace relationships and autonomy upon job satisfaction. This is consistent with the acute care nursing literature where modifiable factors within the workplace have been demonstrated to influence both job and career satisfaction [ 45 ]. In their study, Nantsupawat, et al. [ 46 ] demonstrated that job dissatisfaction and intention to leave were significantly lower in nurses who worked in a better work environment. Similarly, in their systematic review, Cicolini, et al. [ 14 ] found a significant link between nurses empowerment and satisfaction. The significant role of such modifiable factors highlights an opportunity for managers, employers and policy makers to implement strategies which can improve the workplace and, subsequently, enhance satisfaction.
A key finding of this review was the negative impact of poor remuneration on job satisfaction. Whilst concerns about pay have been previously identified in the acute sector [ 44 , 47 ], the challenge of lower rates of pay in PHC compared to the acute sector has long been reported [ 17 , 48 ]. This review adds to the evidence-base around the impact of this disparity on the PHC nursing workforce and highlights the significant implications of not addressing this issue.
Our review also revealed that in many studies large numbers of nurses were intending to leave PHC employment in the near future [ 2 , 42 , 43 ]. This clearly has significant implications for the workforce and service delivery. However, measures of the factors affecting career intentions were variable across included studies as were findings. The difficulties in synthesising such disparate data have been previously identified in the acute care literature [ 13 ]. Despite this, there were clear similarities between our review and the broader literature around nurse turnover and intention to leave. In their systematic review of nurses intention to leave their employment, Chan, et al. [ 13 ] identified that intention to leave was impacted by a complex combination of organisational and individual factors. Organisational factors included the work environment, culture, commitment, work demands and social support. In contrast, individual factors related to job satisfaction, burnout and demographic factors. The complex interplay of multiple factors that underlie retention is probably the reason that retention is the highest when interventions such as mentoring and in-depth orientations are used to support staff [ 49 ].
In their study of acute care nurses Galletta, et al. [ 50 ] conclude that the quality of relationships among staff is an important factor in nurses’ decisions to leave. Interprofessional relationships in PHC have long been identified as presenting unique challenges [ 48 , 51 ]. The complex environment of PHC, whereby services are funded by small businesses or non-government agencies [ 52 ], combines with the relatively rapid shift towards interdisciplinary care to create challenges for staff in developing positive relationships [ 53 ]. The importance of positive relationships, respect of roles and recognition of value between co-workers demonstrated in our review highlights the value of further work to enhance interprofessional collaboration.
Limitations
Whilst this review synthesised the available literature, the variation in measurement instruments and sample sizes made comparison difficult. Since not all papers reported the reliability or validity of the instruments they used it is possible that these instruments had issues in their validity. The data presented, however, represents the best available evidence to address the research question.
A further limitation is the variation between PHC settings and international PHC systems that makes comparison difficult. Whilst this review has included all papers written about PHC nurses internationally, local variations mean that care needs to be taken when generalising findings to other contexts, even within PHC.
This review has identified some key factors that impact on both job satisfaction and career intentions amongst PHC nurses. The importance of the work environment and workplace relationships highlights the need to implement strategies that enhance modifiable workplace factors. The numbers of nurses across studies indicating an intention to leave is a significant concern at a time when we need to build the PHC workforce internationally. Findings from this review highlight the need for action by managers, educators, employers and policy makers to enhance support for nurses in PHC.
Implications for practice and research
There is urgent need to build capacity within the PHC nursing workforce internationally to meet service demands. This review has highlighted a number of issues around job satisfaction and career intention that impact on the retention of nurses in PHC. Exploring strategies to address the modifiable antecedents to nurse job dissatisfaction has the potential to improve retention. Maintaining happy and skilled nurses in the workforce has the potential to build workforce capacity and enhance patient outcomes.
This review has demonstrated that gaps remain in our knowledge around job satisfaction and career intention among PHC registered nurses. Further well-designed longitudinal research is required to explore the trajectory of careers in PHC. Additionally, mixed methods approaches are likely required to explore not only quantitative job satisfaction, but also to reveal how the aspects of satisfaction impact on PHC nurses.
No funding was received for this study.
Availability of data and materials
Abbreviation, authors’ contributions.
EH conceived the study, conducted the initial search and participated in the data analysis and drafting of the paper. ES confirmed the initial search and participated in the data analysis and drafting of the paper. SM participated in the data analysis and drafting of the paper. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Competing interests.
Professor Elizabeth Halcomb is an Associate Editor of BMC Family Practice. Nil other competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Elizabeth Halcomb, Phone: +61 2 4221 3784, Email: ua.ude.wou@bmoclahe .
Elizabeth Smyth, Email: [email protected] .
Susan McInnes, Email: ua.ude.wou@sennicms .
- Open access
- Published: 07 September 2023
Nursing workforce competencies and job satisfaction: the role of technology integration, self-efficacy, social support, and prior experience
- Mohammed Hamdan Alshammari 1 &
- Atallah Alenezi 2
BMC Nursing volume 22 , Article number: 308 ( 2023 ) Cite this article
5569 Accesses
3 Citations
1 Altmetric
Metrics details
The nursing profession has significant importance in delivering high-quality healthcare services. Nursing practitioners who have essential competencies and who are satisfied with their job are vital in achieving optimum patient outcomes. Understanding the effects of technology integration on nurse workforce competencies and job satisfaction is crucial due to the fast progress of technology in healthcare settings. Furthermore, many elements, including self-efficacy, social support, and prior experience have been recognized as possible mediators or moderators within this association. The primary objective of this quantitative research was to examine the influence of nursing education and the integration of technology on the competencies and job satisfaction of nursing professionals. Additionally, this study aimed to explore the potential mediating and moderating effects of self-efficacy and social support in this relationship.
This cross-sectional, quantitative study employed an online survey questionnaire with standardized scales to measure nursing workforce competencies, job satisfaction, self-efficacy, social support, and prior experience. It was completed by 210 registered nurses from various healthcare settings in the Kingdom of Saudi Arabia. Data were analyzed by descriptive statistics, Pearson correlation analysis, multiple regression analysis, and structural equation modeling performed with SPSS 23 and SmartPLS 3.0 software.
The study’s findings revealed that nursing workforce competencies and job satisfaction were significantly predicted by nursing training and technology integration. The relationship between nursing training and technology integration, as well as nursing workforce competencies and job satisfaction, was partially mediated by self-efficacy and social support. Furthermore, prior experience moderated the relationship between nursing education and technological integration, nursing workforce competencies, and job satisfaction.
Conclusions
The study’s findings suggest that nursing training and technology integration can improve nursing workforce competencies and job satisfaction and that self-efficacy and social support play an important role in mediating this relationship. Furthermore, prior experience can have an impact on the efficacy of nursing training and technology integration programs for developing nursing workforce competencies. The study has several practical implications for nursing education, training, and professional development programs, as well as strategies used by healthcare organizations to improve nursing workforce competencies and job satisfaction. To maximize their impact on nursing workforce competencies and job satisfaction, this study recommends that nursing training and technology integration programs focus on enhancing self-efficacy and social support. Furthermore, the study emphasizes the significance of prior experience when designing and implementing nursing training and technology integration programs.
Peer Review reports
Introduction
The nursing profession is an important part of the healthcare industry and plays an important part in ensuring the health and well-being of patients [ 1 ]. The process of incorporating technological tools, resources, and systems into existing operations, practices, and environments is known as technology integration [ 2 ]. It involves integrating technology with established methods and strategies to attain particular objectives and results. The purpose of technology integration is to maximize the potential of technology to enhance processes, collaboration, communication, and overall performance [ 3 ]. The incorporation of technology into nursing education and practice in recent years has had a significant impact on the nursing workforce’s overall competency levels as well as their level of job satisfaction. The combination of nursing training and technological advancements has been found to improve the level of job satisfaction among nurses, which in turn results in better healthcare outcomes for patients [ 4 ].
The nursing workforce’s competencies and their level of satisfaction in their jobs are both essential components of nursing practice necessary for delivering high-quality care to patients [ 5 ]. Job satisfaction refers to the level of contentment and fulfillment that is experienced by nurses in their jobs, while nursing workforce competencies refer to the knowledge, skills, and abilities required for nurses to effectively perform their duties [ 6 ]. Nursing workforce competencies are important because they ensure that nurses have the knowledge and abilities necessary to provide care that is safe, effective, and centered on the patient. It is absolutely necessary to provide competent nursing care in order to reduce healthcare costs, improve patient satisfaction, and prevent unfavorable patient outcomes. Additionally, competent nursing care makes a contribution to the overall quality of the delivery of healthcare as well as the safety of the patient [ 7 ].
The retention of nurses is essential to the upkeep of a steady nursing workforce and job satisfaction is one factor that contributes to their motivation to stay in their positions. Researchers have found a correlation between high levels of job satisfaction and low rates of employee turnover, improved patient outcomes, and increased productivity [ 8 ]. Nurses who report higher levels of job satisfaction are also more likely to participate in activities that contribute to their ongoing learning and professional development, which in turn increases their level of expertise and efficiency as providers of healthcare [ 4 ].
Despite the fact that a number of studies have investigated the effect that nursing training and the incorporation of technology has had on the nursing workforce’s competencies and job satisfaction [ 9 , 10 , 11 ], there is a deficiency in the body of research concerning the factors that influence the success of these relations. To be more specific, there is a dearth of research on the ways in which individual differences, such as personality traits, moderate the relationship between nursing training and technology integration and nursing workforce competencies and job satisfaction [ 12 ].
The moderating role of prior experience in the effectiveness of nursing training and technology integration interventions highlights the necessity to consider individual differences when designing and implementing these interventions [ 13 ]. However, additional research is required on other potential moderators, such as personality traits, that may have an impact on the efficacy of nursing education and training programs. It is essential to gain an understanding of the moderating factors that have an effect on the efficacy of nursing education and training programs in order to design nursing interventions that are both more effective and better tailored to meet the varied requirements of the nursing workforce [ 12 ] In addition, nursing educators and practitioners can gain a better understanding of the underlying mechanisms of the interventions’ effects on nursing workforce competencies and job satisfaction by locating potential mediators such as self-efficacy and social support. Self-efficacy and social support were chosen as mediating variables for “individual differences” because they play important roles in shaping individual behavior, attitudes, and results [ 14 , 15 ].
Self-efficacy is an individual’s belief in their own ability to complete activities and accomplish desired results. It determines how people approach problems, persevere in the face of adversity, and recover from disappointments. Higher degrees of self-efficacy promotes motivation, confidence, and goal-directed behavior, whereas lower levels might hamper performance and personal growth [ 16 ]. Social support, on the other hand, refers to the assistance, encouragement, and resources supplied by people inside an individual’s social network [ 17 ]. It could come from family, friends, coworkers, or managers. Social support is critical in relieving stress, increasing well-being, and facilitating adaptation to new situations or obstacles. Strong social support networks give emotional support, guidance, and practical aid, positively influencing an individual’s beliefs, behaviors, and overall functioning [ 18 ].
The objectives of this study were:
To investigate the impact of nursing training and technology integration on nursing workforce competencies.
To explore the relationship between nursing training and technology integration and job satisfaction among the nursing workforce.
To examine the mediating role of self-efficacy and social support in the relationship between nursing training and technology integration and nursing workforce competencies and job satisfaction.
To determine the moderating role of prior experience in the effectiveness of nursing training and technology integration interventions on nursing workforce competencies and job satisfaction.
These objectives aimed to fill a gap in the existing literature and provide a comprehensive understanding of the impact of nursing training and technology integration on nursing workforce competencies and job satisfaction, as well as the mediating and moderating factors that may influence the efficacy of these interventions. In addition, these objectives sought to identify the factors that may influence the effectiveness of these interventions. The conclusions from this study have the potential to inform nursing educators and practitioners on how to design and implement more effective training programs that cater to the diverse needs of the nursing workforce and better prepare them for the future of healthcare.
This research makes a significant contribution to the existing body of literature on nursing education and training by delivering an in-depth understanding of the influence that nursing training and the integration of technology have had on the competencies of nursing workforces and on job satisfaction. This study provides insight into how nursing educators and practitioners can design and implement more effective training programs that cater to the diverse needs of the nursing workforce. This was accomplished by exploring the mediating and moderating factors that influence the effectiveness of these interventions.
Literature review
Training and nursing workforce competence.
Evidence from an ever-expanding body of research suggests that training has a material and beneficial effect on the nursing workforce’s level of competence. Simulation-based training programs have been found to greatly enhance nursing competence [ 19 ]. According to the findings of the study, the simulation-based training program increased nursing competence in a number of areas, including clinical judgment, communication, and care that is focused on the patient. The authors arrived at the conclusion that training based on simulation has the potential to be an efficient way of improving the nursing workforce’s competency. Moreover, well-structured and supervised clinical training greatly improves nursing competency [ 20 ]. Effective preceptorship programs, mentorship, and constructive feedback all contribute to the successful development of nursing competence during clinical training. Targeted educational interventions have been found to improve nursing competence [ 13 ]. Active learning tactics such as case studies, role-playing, and interactive conversations aid in knowledge retention and practical application, ultimately leading to increased nursing competence. In a similar vein, a review found that training interventions have a beneficial influence on nursing competence [ 21 ]. According to the findings of the review, training interventions, such as simulation-based training, clinical training, and educational interventions, significantly enhanced nursing competence. The authors came to the conclusion that educational interventions are necessary in order to improve the nursing workforce’s overall competence and the results for patients. Thus, the first hypothesis for this study was:
H1: Training has a significant and positive impact on nursing workforce competence.

Training and job satisfaction
Training appears to have a large and beneficial effect on job satisfaction, according to a growing amount of research that has been conducted on the topic. Training has been found to have a beneficial impact on job satisfaction [ 14 ]. According to the findings of the study, job satisfaction was significantly higher among workers who had received training compared to workers who had not received training. The authors arrived at the conclusion that training was an important component that can have a considerable influence on occupational fulfillment. In a similar vein, training was found to have a favorable influence on job satisfaction [ 22 ]. According to the findings of the study, levels of job satisfaction were much greater for workers who had received training as opposed to workers who had not received training. The authors came to the conclusion that training was an essential component that can have a major effect on occupational fulfillment. Thus, the second hypothesis was:
H2: Training has a significant and positive impact on job satisfaction.
Technology integration and nursing workforce competence
Evidence from a growing corpus of research demonstrates that the incorporation of technology has an important and beneficial effect on the nursing workforce’s level of competence. Technology integration has been found to have a beneficial effect on nursing workforce competence [ 23 ]. According to the findings of the study, nurses who made use of technology to assist them in their work exhibited higher levels of competence than their counterparts who did not make use of technology. The authors came to the conclusion that the incorporation of technology is a necessary component that has the potential to greatly influence nursing workforce competence. In a similar vein, another study found a favorable impact of technology integration on nursing workforce competency [ 24 ]. They found that technology integration has a favorable impact on nursing workforce competence. According to the findings of the study, nurses who made use of technology to assist them in their work exhibited higher levels of competence than their counterparts who did not make use of technology. The authors arrived at the conclusion that the incorporation of technology was an essential component that has the potential to greatly influence nursing workforce competence. Therefore, our third hypothesis:
H3: Technology integration has a significant and positive impact on nursing workforce competence.
Technology integration and job satisfaction
The incorporation of technology into the working environment is now widely acknowledged as a critical component in the process of elevating employee happiness with their jobs. Many studies have been conducted to study the effect that the integration of technology has on job satisfaction, and all of them have revealed favorable findings. According to the findings of an investigation on the relationship between technology integration and job happiness, technology integration has a beneficial effect on job satisfaction [ 25 ]. According to the findings of the study, workers who had access to various forms of technology at their places of employment reported higher levels of job satisfaction than their counterparts who did not have such access. The authors arrived at the conclusion that the incorporation of technology was an essential component that can have a substantial effect on occupational fulfillment. In a similar vein, another study found that technology integration has a favorable influence on job satisfaction [ 26 ]. According to the findings of the study, levels of job satisfaction were much greater among workers who utilized technology to assist their work compared to workers who did not utilize technology. The authors arrived at the conclusion that the integration of technology was an important component that can have a major impact on occupational satisfaction. Therefore, our fourth hypothesis is:
H4: Technology integration has a significant and positive impact on job satisfaction.
Self-efficacy and nursing workforce competence
The concept of self-efficacy relates to an individual’s belief in their own capacity to successfully carry out a specific activity or task. Research has been conducted to study the relationship between self-efficacy and nursing workforce competency, and all has revealed favorable findings. Self-efficacy was shown to have a favorable impact on nursing workforce competence [ 27 ]. According to the findings of the study, nurses who rated themselves as having high levels of self-efficacy had greater levels of nursing workforce competence than their colleagues who rated themselves as having low levels of self-efficacy. The authors came to the conclusion that self-efficacy was a crucial component that can have a considerable impact on the competence of the nursing workforce. Similarly, another study found that self-efficacy had a favorable influence on nursing workforce competence [ 4 ]. Based on the results of the investigation, it was observed that nurses who self-assessed their levels of self-efficacy as high exhibited higher levels of nursing workforce competence in comparison to their peers who self-assessed their levels of self-efficacy as low. The researchers reached the determination that self-efficacy was a significant factor that can exert a substantial influence on the proficiency of the nursing labor force.
H5: Self-efficacy has a significant and positive impact on nursing workforce competence.
Self-efficacy and job satisfaction
Self-efficacy is a factor that can influence job satisfaction in the workplace. Employees who have high levels of self-efficacy are more confident in their skills to successfully carry out the responsibilities associated with their jobs. Much research has been conducted to study the relationship between self-efficacy and job satisfaction, and all of them have reported favorable findings. Researchers found that self-efficacy has a beneficial effect on job satisfaction [ 28 ]. According to the findings of the study, workers who rated themselves as having high levels of self-efficacy reported greater levels of job satisfaction than those workers who rated themselves as having low levels of self-efficacy. The authors concluded that self-efficacy was important and can have a considerable effect on occupational contentment.
H6: Self-efficacy has a significant and positive impact on job satisfaction.
Social support and nursing workforce competence
The help, assistance, and comfort that an individual receives from their social network are all examples of what is referred to as social support. Numerous studies have shown positive findings on the relationship between social support and nursing workforce competence. Social support was found to have a beneficial effect on nursing workforce competence [ 29 ]. Registered nurses who had high levels of social support reported better levels of nursing workforce competence compared to those who had low levels of social support [ 30 ]. The authors concluded that social support is an important aspect that can have a substantial impact on the competence of nursing personnel.
H7: Social support has a significant and positive impact on nursing workforce competence.
Social support and job satisfaction
Social support has been found to have a favorable influence on job satisfaction [ 31 ]. According to the findings of the study, workers who received high levels of social support reported higher levels of happiness in their jobs compared to workers who received low levels of social support. The authors concluded that social support was an essential component that can have a considerable effect on occupational fulfillment.
H8: Social support has a significant and positive impact on job satisfaction.
Self-efficacy as a mediator
Self-efficacy increases as a result of training, which in turn leads to an improvement in the overall competence of the nursing staff. A sense of self-efficacy acts as a partial mediator of the connection between schooling and nursing workforce competence [ 4 ]. The authors came to the conclusion that education raised levels of self-efficacy, which in turn improved the competence of the nursing staff. In addition, self-efficacy acts as a moderator in the connection that exists between training and performance [ 32 ]. According to Bandura’s theory, self-efficacy may be improved by training, which in turn boosts performance and raises job satisfaction. The author made the argument that one of the most important factors that determine motivation, conduct, and performance was one’s views regarding one’s level of self-efficacy. Many researchers have investigated the connection between the incorporation of technology, self-efficacy, and the level of nursing workforce competency. In one such study, the incorporation of technology positively improved the competency of nursing personnel [ 22 ]. The authors also discovered that a person’s sense of self-efficacy acted as a mediator between the relationship between technology integration and the competence of the nursing staff. The authors came to the conclusion that increased use of technology led to greater feelings of self-sufficiency, which in turn led to improvements in nursing workforce competency. Another study looked into the relationship between the adoption of new technologies, feelings of self-efficacy, and levels of job satisfaction [ 22 ]. According to the findings of the study, the incorporation of technology had a favorable influence on occupational satisfaction. The authors also discovered that a sense of self-efficacy acted as a mediator between the relationship between integrating technology and feeling satisfied with one’s work. The authors concluded that greater use of technology led to greater feelings of self-efficacy, which in turn led to increased job satisfaction.
H9a: Self-efficacy mediates the relationship between training and nursing workforce competence.
H9b: Self-efficacy mediates the relationship between training and job satisfaction.
H9c: Self-efficacy mediates the relationship between technology integration and nursing workforce competence.
H9d: Self-efficacy mediates the relationship between technology integration and job satisfaction.
Social support as a mediator
An individual who is struggling may receive social support in the form of emotional, informational, or physical assistance from the people around them. The provision of social support can come from a variety of different sources, such as managers and coworkers, relatives and friends, and friends of friends. The significance of social support in the nursing profession has recently come to light because it has the potential to influence both the level of care that nurses deliver and the overall enjoyment they derive from their work [ 33 ]. Additionally, feedback, mentoring, and resources can be provided via social support, which is another way it can boost the efficiency of training programs. The connection between social support and nursing workforce competency has been the subject of investigation. It was discovered that social support was a mediator of the association between nursing training and nursing competence [ 34 ]. To improve employees’ knowledge, abilities, and overall competence, it is necessary to implement training and development programs. On the other hand, training by itself might not be enough to guarantee that people are happy in their jobs. The connection between getting trained and being happy in one’s career might be mediated by having social support.
The relationship between the incorporation of technology and the competence of the nursing staff is mediated by social support. For instance, a study came to the conclusion that the social support that nurses received from their coworkers and superiors had a substantial influence in boosting their ability to make use of electronic health records [ 35 ]. Similarly, it was found that social support from mentors mediated the association between technology integration and nursing workforce competency [ 36 ]. Their findings were published in the journal Nursing Research. By providing employees with the resources and direction they require in order to properly use technology, social support was able to help reduce the negative consequences that technology use can have. For instance, coworkers can provide pointers and advice on how to use a particular piece of software or tool, while supervisors can provide training and support to ensure that employees have the skills necessary to carry out the responsibilities associated with their jobs. In addition, social support can help employees have a feeling of community and belonging in their workplace, both of which can contribute to increased levels of job satisfaction. When workers have the sense that they are a part of a community that cares about them, they are more likely to have a good outlook on their occupations and to be driven to do well in their work.
H10a: Social support mediates the relationship between training and nursing workforce competence.
H10b: Social support mediates the relationship between training and job satisfaction.
H10c: Social support mediates the relationship between technology integration and nursing workforce competence.
H10d: Social support mediates the relationship between technology integration and job satisfaction.
Prior experience as a moderator
Nurses who have worked for longer periods may have already gained some of the knowledge and abilities that were taught in training programs as a result of their previous employment. As a result, they may gain more from training programs than nurses with less experience. On the other hand, nurses with less experience may have more to gain from training programs than those with more experience because they may have had fewer opportunities to develop the requisite skills and knowledge from their previous work experiences. Training programs can have a beneficial effect on job satisfaction by giving employees the knowledge, skills, and confidence they need to properly fulfill their job obligations. This has been demonstrated by research to be the case. Yet, the effect that training has on employees’ levels of happiness with their jobs may differ based on the amount of prior experience that each worker possesses. According to the findings of several studies, the experience can help regulate the relationship between the incorporation of technology and the nursing workforce’s level of competence. For instance, it was discovered that the positive association between technology integration and nursing workforce competency was larger for nurses who had more prior experience in utilizing technology [ 37 ]. Similarly, another study discovered that the association between technology use and nursing workforce competency was stronger for nurses who had a greater amount of prior experience [ 38 ].
H11a: Prior Experience moderates the relationship between training and nursing workforce competence.
H11b: Prior Experience moderates the relationship between training and job satisfaction.
H11c: Prior Experience moderates the relationship between technology integration and nursing workforce competence.
H11d: Prior Experience moderates the relationship between technology integration and job satisfaction.
Conceptual model
The hypotheses from the literature review are connected in a conceptual model as shown in Fig. 1 .
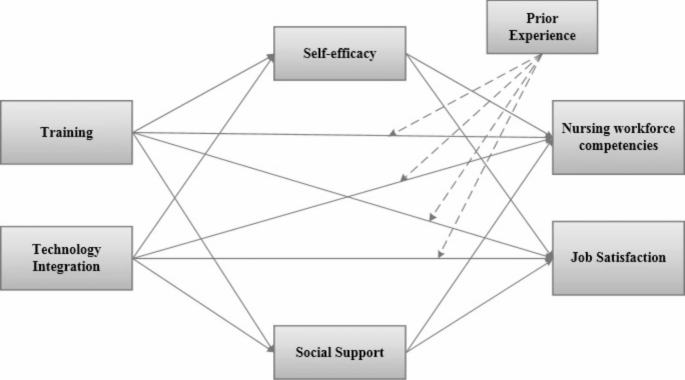
Conceptual Framework
Research design
In this cross-sectional, quantitative study, an online survey was used as the research method to investigate the impact of nursing training and technology integration on nursing workforce competencies and job satisfaction, as well as to investigate the moderating role of prior experience and the mediating roles of self-efficacy and social support.
The population of registered nurses employed in healthcare settings in the Kingdom of Saudi Arabia were the focus of this study.
Participants and sampling determination
The minimum desired sample size was determined using G-Power, applying the following parameters: a medium effect size of 0.30, a significance level of 0.05, and a power analysis of 0.95. By using these parameters, the minimum desired sample size for this study was 134. In order to aviod bias, a questionnaire was distributed to 300 targets using the convenience sampling method; 210 completed responses were received, exceeding the minimum desired sample size.
Measures of the study varaibles
A scale with three items that was taken from [ 39 ] and used to measure training. Items used to measure training were abbrivated T1, T2, and T3. Cronbach’s Aplha had a value of 0.776. Sample items included “My nursing training program adequately prepared me for the demands of the nursing profession”.
Technology integration
A scale with three items that was taken from [ 40 ] and used to measure technology integration. Items used to measure technology intergration were abbrivated TI1, TI2, and TI3. The value of Cronbach’s Aplha was 0.822. Sample items included “Technology has made my job as a nurse easier and more efficient”.
- Nursing workforce competencies
A scale with three items was taken from [ 30 ] and used to measure nursing workforce competencies. Items used to measure workforece competencies were abbrivated NWC1, NWC2, and NWC3. The value of Cronbach’s Aplha was 0.888. Sample items included “I possess the necessary clinical skills to provide quality patient care.”
- Job satisfaction
A scale with three items was taken from [ 41 ] and used to measure job satisfaction. Items used to measure job satisfaction were abbrivated JS1, JS2, and JS3. The value of Cronbach’s Aplha was 0.877. Sample items included “I find my work meaningful and fulfilling.”
- Self-efficacy
A scale with three items was taken from [ 42 ] and used to measure self-efficacy. Items used to measure self-efficacy were abbrivated SE1, SE2, and SE3. The value of Cronbach’s Aplha was 0.860. Sample items included “I am able to manage my time effectively to meet the demands of my job.”
Social support
A scale with three items was taken from [ 43 ] and used to measure social support. Items used to measure social support were abbrivated SS1, SS2, and SS3. The value of Cronbach’s Aplha was 0.823. Sample items included “I feel comfortable seeking help and support from my colleagues and supervisors.”
- Prior experience
A scale with three items was taken from [ 44 ] and used to measure prior experience. Items used to measure prior experience were abbrivated PE1, PE2, and PE3. The value of Cronbach’s Aplha was 0.748. Sample items included “My prior experience has helped me to become a more effective nurse.”
Data collection
A platform for conducting online surveys, specifically Google Forms, was used to collect the data. The survey questionnaire consisted of four sections. In the first section, the participants were asked to provide basic demographic information, including age, gender, years of experience, and level of education. A validated instrument, the Nursing Competency Scale, was utilized in the second section in order to measure the nursing workforce’s level of competency [ 30 ]. The third section used a validated instrument, the Index of Work Satisfaction [ 41 ], to measure job satisfaction. In the fourth section, self-efficacy and social support were measured with instruments that have been previously validated [ 43 , 44 ]. Data was collected from August 2, 2022 to November 20, 2022.
Ethical considerations
Everyone who took part in the research project provided their informed consent, and participation in the study was entirely voluntary. Eliminating all personally identifying information from the questionnaires served to protect respondents’ privacy and maintain their anonymity.
Data analysis
Data were analyzed by SPSS 21 and SmartPLS 3.0 software. Descriptive statistics were used to summarize the demographic characteristics of the sample. Pearson correlation coeffiecient was used to investigate the relationships between nursing training and technology integration, nursing workforce competencies, job satisfaction, self-efficacy, and social support. Analyses of mediation and moderation were carried out in order to investigate the roles that self-efficacy, social support, and prior experience play in mediating and moderating relationships through multiple resgression anlsysis using PLS-SEM software. Significance level was considered at p < 0.05.
Sample profile
Out of the 210 surveys, 84% of the participants completed the questionnaire in Arabic, while 16% of the respondents did so in English. Table 1 lists the respondents’ demographic information. 42.9% of the responders were men and 57.1% were women based on gender. The bulk of respondents (28.6% and 27.1%, respectively), were in the age ranges of 30–40 years and 41–50 years. They represented a variety of experience, including 1 year (31%), 1–3 years (28.6%), 3–5 years (38.6%), and more than 5 years (1.9%).
CFA loadings, reliability and validity test (convergent validity)
The concept indicators were compared to what was known about the variables’ nature using a confirmatory factor analysis (CFA). The CFA’s objective was to determine whether the data fit the suggested measurement model. The values of factor loading of all the items were greater than 0.4, which is shown in Table 2 .
Furthermore, it was necessary to perform both a reliability test and a validity test on the data to investigate the validity and reliability of the collected data. This is an essential step in ensuring that empirical research maintains the highest standards of scientific integrity. Cronbach’s coefficient and combined reliability (CR) are two methods that are utilized in academic research to evaluate the reliability of a model. In addition, the model’s convergent validity was evaluated with the help of factor loadings and the average extracted variance (AVE). The findings are presented in Table 2 , below. All of the variables’ indicators satisfied the requirements, which suggests that the variables chosen by the model have decisive reliability and internal consistency. The majority of academics use the criterion that the square root of AVE must be greater than the correlation coefficient between variables when evaluating the discriminant validity of a model. This is because this criterion ensures that the model accurately represents the world. As can be seen in Table 3 , all values that are not on the diagonal have a lower absolute value than those values that are on the diagonal. This demonstrates that each variable in this model possessed good discriminative validity.
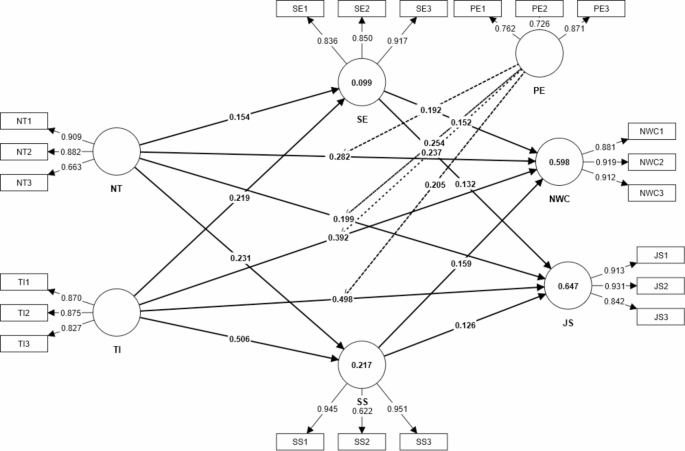
Measurement Model
PLS-SEM analysis
From the above reliability and validity analysis results, it is assumed that the model can carry out the next path impact analysis. Using SmartPLS software and the Bootstrapping method (n = 5000), the effect of each variable was estimated. All results were significant at the significance level of 0.5%, as shown in Table 4 . Training and technology integration had a positive impact on nursing workforce competencies, with the path coefficients of 0.282 and 0.392, respectively, supporting hypotheses H1 and H3. Similarly, training and technology integration had a positive effect on job satisfaction with path coefficients of 0.199 and 0.498, respectively, supporting hypotheses H2 and H4. Moreover, self-efficacy and social support had positive impacts on nursing workforce competencies and job satisfaction with the path coefficients being 0.152 (H5), 0.159 (H7), 0.132 (H6) and 0.126 (H8), as shown in Fig. 2 .
Mediation analysis
Within the context of the relationship between news framing and public opinion, the purpose of this study was to investigate the mediating impact of self-efficacy between training and nursing workforce competence, training and job satisfaction, technology integration and nursing workforce competence, and technology integration and job satisfaction. The H9a hypothesis posited that self-efficacy mediates the relationship between training and nursing workforce competence. This hypothesis was supported by the findings, which show that self-efficacy mediates the relationship between training and nursing workforce competence (p = 0.000). In a similar vein, the H9b hypothesis posited that self-efficacy mediates the relationship between training and job satisfaction. This hypothesis was supported by the findings, which show that self-efficacy mediates the relationship between training and job satisfaction (p = 0.002). The H9c hypothesis posited that self-efficacy mediates the relationship between technology integration and nursing workforce competence. This hypothesis was supported by the findings, which show that self-efficacy mediates the relationship between technology integration and nursing workforce competence (p = 0.042). Similarly, The H9d hypothesis posited that self-efficacy mediates the relationship between technology integration and job satisfaction. This hypothesis was supported by the findings, which show that self-efficacy mediates the relationship between technology integration and job satisfaction (p = 0.048).
The H10a hypothesis posited that social support mediates the relationship between training and nursing workforce competence. This hypothesis was supported by the findings, which show that social support mediates the relationship between training and nursing workforce competence (p = 0.023). In a similar vein, the H10b hypothesis posited that social support mediates the relationship between training and job satisfaction. This hypothesis was supported by the findings, which show that social support mediates the relationship between training and job satisfaction (p = 0.005). The H10c hypothesis posited that social support mediates the relationship between technology integration and nursing workforce competence. This hypothesis was supported by the findings, which show that social support mediates the relationship between technology integration and nursing workforce competence (p = 0.005). Similarly, the H10d hypothesis posited that social support mediates the relationship between technology integration and job satisfaction. This hypothesis was supported by the findings, which show that social support mediates the relationship between technology integration and job satisfaction (p = 0.029). Table 5 shows the result of mediation analysis.
Hypotheses 11a,11b,11c, and 11d posited that prior experience moderates the relationship between training and nursing workforce competence, training and job satisfaction, technology integration and nursing workforce competence, and technology integration and job satisfaction. According to the findings of this study, prior experience acts as a moderating factor in the relationship between training and nursing workforce competence (p = 0.007), training and job satisfaction (p = 0.000), technology integration and nursing workforce competence (p = 0.000), and technology integration and job satisfaction(p = 0.000), confirming the hypotheses. The data collected during the study proves beyond a reasonable doubt the accuracy of these speculations. Table 6 ; Fig. 3 show the results of moderation analysis.
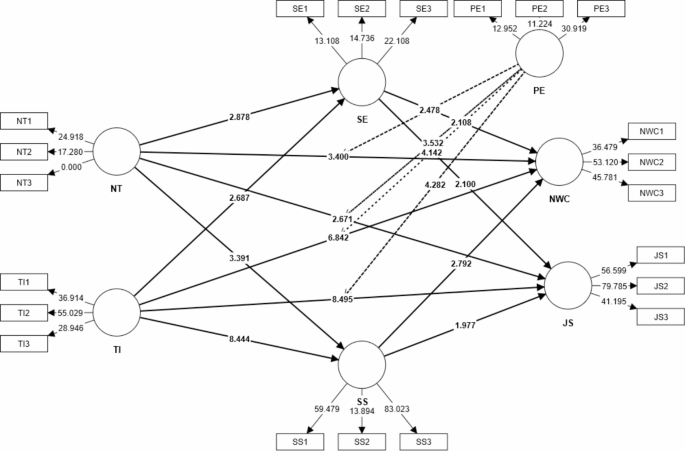
Structural Model
The first hypothesis (H1) was supported with training having a significant and positive impact on nursing workforce competence. Nurses who participate in ongoing education are in a better position to handle difficult patient cases and are more conversant with the most recent treatment procedures and technological advances [ 19 ]. Training can also assist nurses in recognizing and responding appropriately to urgent circumstances, which can lead to improved results for their patients. The ability of nurses to engage with patients and their families is significantly improved when they receive training in communication skills. Increased patient satisfaction and decreased patient anxiety can be achieved through enhanced communication, which in turn leads to better clinical outcomes and a more positive patient experience [ 45 ].
The second hypothesis (H2) was supported with training having a significant and positive impact on job satisfaction. Training has a strong and favorable impact on both overall job satisfaction and individual job satisfaction. It enhances employee morale and motivation, creates possibilities for career growth, gives employees the skills and information necessary to properly fulfill their job obligations, and develops a culture of learning and development inside a business [ 14 ]. As a result, businesses ought to make investments in employee training and development programs in order to boost levels of job satisfaction and encourage the retention of employees. Training gives employees the skills and information they need to effectively do their jobs, leading to improved levels of job satisfaction overall. When workers believe they possess the relevant expertise to successfully carry out the responsibilities of their jobs, they experience an increase in self-assurance in their capabilities. This, in turn, contributes to a sense of accomplishment and overall job satisfaction [ 46 ].
The third hypothesis (H3) was supported with technology integration having a significant and positive impact on nursing workforce competence. Integration of new technologies has a materially beneficial effect on the professional level of the nursing workforce. It has improved communication and collaboration between healthcare professionals, improved access to patient data, provided advanced tools for diagnosis and treatment, improved the ability of healthcare professionals to communicate with one another, and made continuing education and training more accessible [ 47 ]. Healthcare organizations must maintain their investments in the incorporation of technology into nursing practice in order to enhance the nursing workforce’s level of competency and the outcomes for patients. Because of advancements in technology, nurses are now able to take part in continuing education and training programs, which has led to an increase in the overall competency of the nursing workforce. It is now much simpler for registered nurses to acquire training materials and continue their education while working thanks to the proliferation of online training programs, webinars, and other virtual learning platforms [ 48 ]. This has resulted in increased levels of job satisfaction among nurses, as well as improved levels of nursing skills and better outcomes for patients.
The fourth hypothesis (H4) was supported with technology integration having a significant and positive impact on job satisfaction. The implementation of technology has made it possible for employees to operate more effectively, collaboratively, and flexibly, which has contributed to increased levels of job satisfaction. According to the findings of one study, the incorporation of technology had a beneficial effect on occupational fulfillment, particularly in the areas of task diversity, autonomy, and feedback [ 49 ]. According to the findings of the study, employees were able to complete a greater diversity of jobs thanks to the implementation of technology in the workplace. This led to an increase in task variety, which was found to be positively associated with job satisfaction. Also, employees were able to work more independently and received more frequent feedback on their job performance as a result of technological advancements, which contributed to improved levels of job satisfaction.
The fifth hypothesis (H5) was supported with self-efficacy having a significant and positive impact on nursing workforce competence. Self-efficacy was found to have a favorable correlation with the problem-solving abilities of nurses, which are an essential component of nursing practice [ 4 ]. According to the findings of the study, nurses who had higher levels of self-efficacy were more confident in their ability to solve problems and were more competent when it came to managing difficult patient scenarios.
The sixth hypothesis (H6) was supported with self-efficacy having a significant and positive impact on job satisfaction. It has been discovered that an individual’s belief in their ability to perform a specific task or achieve a specific goal has a significant and positive impact on job satisfaction. Self-efficacy is defined as an individual’s belief in their ability to perform a specific task or achieve a specific goal. According to the findings of another study [ 17 ], a positive relationship exists between self-efficacy and job satisfaction among healthcare professionals. According to the findings of the study, healthcare professionals who had higher levels of self-efficacy were more engaged in their work and reported higher levels of job satisfaction than their counterparts who had lower levels of self-efficacy.
The seventh hypothesis (H7) was supported with social support having a significant and positive impact on nursing workforce competence. The supply of emotional, informational, or instrumental aid to a person by other people who are a part of that person’s social network is what is meant by the term “social support.“ Freshly graduated nurses who had social support reported higher levels of nursing competence and job satisfaction [ 18 , 50 ]. According to the findings of the study, recently graduated nurses who received social support from their coworkers exhibited higher levels of nursing competence as well as greater levels of job satisfaction than those newly graduated nurses who did not receive social support.
The eighth hypothesis (H8) was supported with the impact of social support having a significant and positive impact on job satisfaction. It has been discovered that having a strong social support network has a large and favorable impact on the level of job satisfaction experienced by nurses. According to the findings of a study [ 51 ], a favorable association between social support and job satisfaction was identified among nurses. According to the findings of the study, nurses who reported receiving social support from their coworkers reported higher levels of job satisfaction than those nurses who did not report receiving social support.
Hypotheses H9a, H9b, H9c, and H9d investigated the mediating impact of self-efficacy between training and nursing workforce competence, training and job satisfaction, technology integration and nursing workforce competence, and technology integration and job satisfaction. All hypotheses were supported. Healthcare organizations place their primary emphasis on the development of training programs and the integration of technology in a manner that improves nurses’ sense of self-efficacy in order to boost both their level of professional achievement and their level of job satisfaction [ 14 ]. Students in the nursing profession who rated themselves highly in this area were more inclined to put into practice the skills and information they had acquired in school. Nurses’ job satisfaction can be boosted by training programs that boost their sense of competence. Mobile technology can help nurses feel more confident in their abilities, which increases the quality of care provided by the nursing profession as a whole. Self-efficacy in the use of electronic health records was associated with increased job satisfaction among nurses [ 52 ].
Hypotheses H10a, H10b, H10c, and H10d investigated the mediating impact of social support on the relationship between training and nursing workforce competence, training and job satisfaction, technology integration and nursing workforce competence, and technology integration and job satisfaction. All hypotheses were supported. In order to increase nurses’ level of expertise and overall level of job satisfaction, healthcare companies place a primary emphasis on cultivating a friendly working environment and fostering social support from coworkers and managers [ 21 ]. Nurses who had the backing of their superiors and peers throughout training were more likely to put what they had learned into practice, ultimately leading to a more capable nursing workforce. Nurses’ job happiness might be boosted by social support from coworkers and managers during training. Nurses’ ability to effectively implement clinical decision support systems was found to increase when they received social support from peers and superiors. This shows that a good outlook on work and increased job satisfaction might result from receiving social support from coworkers and superiors while using electronic health records.
Hypotheses H11a, H11b, H11c, and H11d investigated the impact of prior experience moderating the relationship between training and nursing workforce competence, training and job satisfaction, technology integration and nursing workforce competence, and technology integration and job satisfaction. All hypotheses were supported. To optimize the effects of training programs and the introduction of new technology on the competence and job satisfaction of the nursing workforce, healthcare organizations should take into account nurses’ varying degrees of experience [ 52 ]. Due to their presumably lower levels of expertise, nurses with less experience benefited more from training. Nurses with less experience may benefit more from training, and those who receive it may be more content with their careers. More seasoned nurses have a simpler time learning to use EHRs and other cutting-edge tools, which could boost the overall quality of the nursing staff [ 53 ]. In certain cases, nurses’ job satisfaction rises when they gain experience because they become more adept at using telehealth tools.
Implications
Self-efficacy and social support are two crucial factors that play a mediating role in the relationship between nursing education and the incorporation of new technologies, on the one hand, and the competencies of the nursing workforce, on the other. The effect of nursing training and the incorporation of technology on nursing workforce competencies and job satisfaction is moderated, in part, by prior experience, which plays an important role in the process. The use of technology in nursing education has the potential to boost the self-efficacy of nurses, which in turn can have a positive impact on the level of job satisfaction and competency they experience. The effectiveness of nursing training and the incorporation of technology can be significantly improved with the addition of social support from coworkers and superiors. This can ultimately lead to an increase in nursing workforce competencies and job satisfaction. From a purely pragmatic standpoint, nursing organizations ought to put money into technological advancements that will improve nursing education and work on formulating plans for incorporating these advancements into the nursing workforce. The self-efficacy of nurses should be a primary focus of nursing education programs, along with the development of social support networks among coworkers and superiors. When developing nursing education programs and integrating technology, it is important to take previous experience into account. The health and happiness of employees should be a top priority for nursing organizations, and this can be accomplished by providing sufficient resources, support, and opportunities for training. The best way for nursing managers to improve their employees’ skills and overall job satisfaction is to create a supportive working environment that promotes teamwork and open communication among nursing staff members. It is possible for nursing organizations to improve the efficacy of their training programs and encourage a nursing workforce that is both more satisfied and more competent by taking into consideration the theoretical and practical implications discussed here.
Limitations and future directions
Some limitations exist for the current study. In the first place, the research was only conducted in a single geographical area, which makes it difficult to extrapolate the findings to other countries or regions. The second limitation of the study was that it uses a cross-sectional methodology, which means that it is not possible to determine whether or not there is a cause-and-effect relationship between the different variables that were investigated. Self-reported measures of job satisfaction and competencies may also be subject to bias or social desirability effects, both of which have the potential to affect the accuracy of the results. Last, but not least, the research did not take into account any of the other potential moderating variables, such as age, gender, or educational background, all of which have the potential to affect the success of nursing training and technology integration.
To address these limitations, future research could use longitudinal designs to investigate the causal relationships between nursing training, technology integration, self-efficacy, social support, competencies, and job satisfaction. Furthermore, future research could look into the role of other potential mediators in the relationship between nursing training, technology integration, competencies, and job satisfaction, such as motivation, job demands, and work-life balance. Comparative research across regions or countries could also aid in identifying cultural, social, and organizational factors that influence the effectiveness of nursing education and technology integration. Furthermore, research could concentrate on developing and evaluating training interventions that promote self-efficacy and social support among nurses in order to improve their competencies and job satisfaction. Finally, research into the impact of technology integration on nursing training, workforce competencies, and job satisfaction is still in its early stages, and future studies could look into the long-term effects of technology integration on the nursing workforce. Researchers can improve our understanding of the impact of nursing training and technology integration on nursing workforce competencies and job satisfaction by addressing these limitations and pursuing these future directions.
The current study emphasizes the significance of nursing education and technological integration in improving nursing workforce competencies and job satisfaction. Self-efficacy and social support were discovered to be important mediators of this relationship, with prior experience serving as a critical moderator. The incorporation of technology into nursing education can increase nurses’ self-efficacy, leading to increased job satisfaction and competencies. Social support from colleagues and superiors can significantly improve the effectiveness of nursing training and technology integration, promoting nursing workforce competencies and job satisfaction. Practical implications include investing in technology and developing strategies for its integration into the nursing workforce, prioritizing the well-being and job satisfaction of nursing staff, and fostering a supportive work environment. The study’s limitations include its cross-sectional design, self-reported measures, and regional focus. Future research could use longitudinal designs, investigate additional potential mediators and moderators, and investigate the long-term effects of technology integration on the nursing workforce. Overall, the current study emphasizes the significance of nursing education and technology integration in fostering a competent and satisfied nursing workforce.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Liu H-Y, Chao C-Y, Kain VJ, Sung S-C. The relationship of personal competencies, social adaptation, and job adaptation on job satisfaction. Nurse Educ Today. 2019;83:104199.
PubMed Google Scholar
Ogunjimi A, Rahman M, Islam N, Hasan R. Smart mirror fashion technology for the retail chain transformation. Technol Forecast Soc Chang. 2021;173:121118.
Google Scholar
Zhang Y, Li W, Mao S, Zheng Z. A simple method for constructing orthogonal arrays by the Kronecker sum. J Syst Sci Complexity. 2006;19:266–73.
Choi H, Tak SH. Nurses’ behavioral intention in using virtual clinical simulation training: by structural equation modeling. Nurse Educ Pract. 2022;65:103492.
Tramontano C, Grant C, Clarke C. Development and validation of the e-Work Self-Efficacy Scale to assess digital competencies in remote working. Computers in Human Behavior Reports. 2021;4:100129.
PubMed PubMed Central Google Scholar
Yoon I, Kim M. Dynamic patterns of teachers’ professional development participation and their relations with socio-demographic characteristics, teacher self-efficacy, and job satisfaction. Teach Teacher Educ. 2022;109:103565.
Pueyo-Garrigues M, Pardavila-Belio MI, Canga-Armayor A, Esandi N, Alfaro-Díaz C, Canga-Armayor N. NURSES’knowledge, skills and personal attributes for providing competent health education practice, and its influencing factors: a cross-sectional study. Nurse Educ Pract. 2022;58:103277.
CAS PubMed Google Scholar
Kosters J, Janus SI, van den Bosch KA, Andringa TC, Oomen-de Hoop E, de Boer MR, et al. Soundscape awareness intervention reduced neuropsychiatric symptoms in nursing home residents with dementia: a cluster-randomized Trial with MoSART+. J Am Med Dir Assoc. 2023;24(2):192–8. e5.
Chien Y-A, Lee Y-H, Chang Y-P, Lee D-C, Chow C-C. Exploring the relationships among training needs, willingness to participate and job satisfaction in disaster nursing: the mediating effect of achievement motivation. Nurse Educ Pract. 2022;61:103327.
Hentschel E, Tran HT, Nguyen VH, Tran T, Yousafzai AK. The effects of a childcare training program on childcare quality and child development: evidence from a quasi-experimental study in Vietnam. Child Youth Serv Rev. 2023;147:106844.
Zarafshani K, Solaymani A, D’Itri M, Helms MM, Sanjabi S. Evaluating technology acceptance in agricultural education in Iran: a study of vocational agriculture teachers. Social Sci Humanit Open. 2020;2(1):100041.
Jang SJ, Cho S. Disaster nursing competencies of rural nurses during COVID-19: a cross-sectional study. Collegian. 2023;30(2):264–9.
Lavilla-Gracia M, Pueyo-Garrigues M, Fotopoulou M, Canga-Armayor A, Esandi N, Alfaro-Díaz C, et al. Training nursing students in motivational interviewing for alcohol misuse: a mixed method study. Nurse Educ Today. 2023;125:105775.
LaForett DR, De Marco A. A logic model for educator-level intervention research to reduce racial disparities in student suspension and expulsion. Cult Divers Ethnic Minor Psychol. 2020;26(3):295.
Sigursteinsdottir H, Karlsdottir FB. Does social support matter in the workplace? Social support, job satisfaction, bullying and harassment in the workplace during COVID-19. Int J Environ Res Public Health. 2022;19(8):4724.
CAS PubMed PubMed Central Google Scholar
Javed A, Iqbal J, Iqbal SMJ, Imran M. Sustainable leadership and employee innovative behavior: discussing the mediating role of creative self-efficacy. J Public Affairs. 2021;21(3):e2547.
Almeida MH, Ramos AO, Santos CM. Linking social support with job satisfaction: the role of global empowerment in the workplace. Safety and health for workers-research and practical perspective. 2020.
Patterer AS, Yanagida T, Kühnel J, Korunka C. Daily receiving and providing of social support at work: identifying support exchange patterns in hierarchical data. Eur J Work Organizational Psychol. 2023:1–17.
Shore CB, Maben J, Mold F, Winkley K, Cook A, Stenner K. Delegation of medication administration from registered nurses to non-registered support workers in community care settings: a systematic review with critical interpretive synthesis. Int J Nurs Stud. 2022;126:104121.
Chen S, Wang R, Xu N, Zhang J, Liu Y, Cong S, et al. Identification of factors influencing core competence promotion among professional nurses and midwives: a qualitative study using the COM-B model. Nurse Educ Pract. 2023;69:103619.
Shahin M, Khanam M, Aktar S, Siddiqua A, Sharif N. Resiliency of livelihood and empowerment of women: results of a cash-based intervention in Bangladesh’s Lalmonirhat District. Int J Disaster Risk Reduct. 2022;79:103137.
Ali S, Kleib M, Paul P, Petrovskaya O, Kennedy M. Compassionate nursing care and the use of digital health technologies: a scoping review. Int J Nurs Stud. 2022;127:104161.
To VT, Swabey K, Bown A, Thai B. Multiple perspectives on the benefits of teaching of vietnamese to preschool children in an australian early childhood context. Int J Early Years Educ. 2022;30(2):339–54.
Reisenwitz TH, Fowler JG. Information sources and the tourism decision-making process: an examination of Generation X and Generation Y consumers. Global Bus Rev. 2019;20(6):1372–92.
Umair A, Conboy K, Whelan E, UNDERSTANDING THE INFLUENCE. OF TECHNOSTRESS ON WORKERS’JOB SATISFACTION IN GIG-ECONOMY: AN EXPLORATORY INVESTIGATION. 2019.
Christ-Brendemühl S, Schaarschmidt M. The impact of service employees’ technostress on customer satisfaction and delight: a dyadic analysis. J Bus Res. 2020;117:378–88.
Tseng T-J, Guo S-E, Hsieh H-W, Lo K-W. The effect of a multidimensional teaching strategy on the self-efficacy and critical thinking dispositions of nursing students: a quasi-experimental study. Nurse Educ Today. 2022;119:105531.
Zeng X, Zhang X, Chen M, Liu J, Wu C. The influence of perceived organizational support on police job burnout: a moderated mediation model. Front Psychol. 2020;11:948.
McKenzie H, Hayes L, Acret L, Boustany C, Kim B, Fethney J, et al. Patient perceptions of a community-based intervention designed to provide support post administration of anti-cancer systemic treatments: a qualitative evaluation. Eur J Oncol Nurs. 2022;58:102148.
Wong HM, Bridges SM, Ma KW, Yiu CKY, McGrath CP, Zayts OA. Advanced informatics understanding of clinician-patient communication: a mixed-method approach to oral health literacy talk in interpreter-mediated pediatric dentistry. PLoS ONE. 2020;15(3):e0230575.
Aliakbari M, Khany R, Adibpour M. EFL teachers’ reflective practice, job satisfaction, and school context variables: exploring possible relationships. TESOL J. 2020;11(1):e00461.
Nikolopoulou K, Gialamas V, Lavidas K. Habit, hedonic motivation, performance expectancy and technological pedagogical knowledge affect teachers’ intention to use mobile internet. Computers and Education Open. 2021;2:100041.
Kang Y, Ha J, Ham G, Lee E, Jo H. A structural equatin model of the relationships between social-emotional competence, social support, depression, and aggression in early adolescents in South Korea. Child Youth Serv Rev. 2022;138:106498.
Yang J, Lawrence JF, Grøver V. Parental expectations and home literacy environment: a Questionnaire Study of Chinese-Norwegian Dual Language Learners. J Res Child Educ. 2023;37(1):159–73.
Sipanoun P, Oulton K, Gibson F, Wray J. The experiences and perceptions of users of an electronic patient record system in a pediatric hospital setting: a systematic review. Int J Med Informatics. 2022;160:104691.
Teo T, Unwin S, Scherer R, Gardiner V. Initial teacher training for twenty-first century skills in the Fourth Industrial Revolution (IR 4.0): a scoping review. Comput Educ. 2021;170:104223.
Jiang Y, Ramachandran HJ, Teo JYC, Leong FL, Lim ST, Nguyen HD, et al. Effectiveness of a nurse-led smartphone‐based self‐management programme for people with poorly controlled type 2 diabetes: a randomized controlled trial. J Adv Nurs. 2022;78(4):1154–65.
Gardner-Neblett N, De Marco A, Ebright BD. Do Katie and Connor tell better stories than Aaliyah and Jamaal? Teachers’ perceptions of children’s oral narratives as a function of race and narrative quality. Early Child Res Q. 2023;62:115–28.
Pirani S, Freemyer B, Furuta S, Teruya K, Oba Y, Detor L, et al. Efficacy of interprofessional sport concussion simulation training for health care students and teacher candidates. J Interprofessional Educ Pract. 2022;28:100516.
Demissie EB, Labiso TO, Thuo MW. Teachers’ digital competencies and technology integration in education: insights from secondary schools in Wolaita Zone. Ethiopia Social Sciences & Humanities Open. 2022;6(1):100355.
Ozkan AH. The Effect of Burnout and work attitudes on turnover intention: a Meta-Analytical comparison between Asia, Oceania, and Africa. J Asia-Pac Bus. 2022;23(2):113–41.
Zahra TT, Waheed A. Influence of ethical leadership on innovative work behavior: examination of individual-level psychological mediators. Pakistan J Commer Social Sci (PJCSS). 2017;11(2):448–70.
Bray L, Appleton V, Sharpe A, ‘If. I knew what was going to happen, it wouldn’t worry me so much’: children’s, parents’ and health professionals’ perspectives on information for children undergoing a procedure. J Child Health Care. 2019;23(4):626–38.
Wang X, Guchait P, Paşamehmetoğlu A, Wen X. Hospitality employees’ affective experience of shame, self-efficacy beliefs and job behaviors: the alleviating role of error tolerance. Int J Hospitality Manage. 2022;102:103162.
Gandra EC, da Silva KL, Schreck RSC, Rocha LL, De Lima KCO, Paiva ACDO. Teaching strategies to develop skills to address social inequalities in nursing education: a scoping review. Nurse Educ Today. 2022:105697.
Aburumman O, Salleh A, Omar K, Abadi M. The impact of human resource management practices and career satisfaction on employee’s turnover intention. Manage Sci Lett. 2020;10(3):641–52.
Gomes J, Fleer M. Is science really everywhere? Teachers’ perspectives on science learning possibilities in the preschool environment. Res Sci Educ. 2020;50:1961–89.
Bauce K, Kaylor MB, Staysniak G, Etcher L. Use of theory to guide integration of virtual reality technology in nursing education: a scoping study. J Prof Nurs. 2023;44:1–7.
Califf CB, Sarker S, Sarker S. The bright and dark sides of technostress: a mixed-methods study involving healthcare IT. MIS Q. 2020;44(2).
Jolly PM, Kong DT, Kim KY. Social support at work: an integrative review. J Organizational Behav. 2021;42(2):229–51.
Zahoor N, Donbesuur F, Christofi M, Miri D. Technological innovation and employee psychological well-being: the moderating role of employee learning orientation and perceived organizational support. Technol Forecast Soc Chang. 2022;179:121610.
Aldhahi MI, Baattaiah BA, Alqahtani AS, editors. Predictors of electronic learning self-efficacy: A cross-sectional study in saudi arabian universities. Frontiers in Education; 2021: Frontiers Media SA.
Stephanie L, Sharma RS. Digital health eco-systems: an epochal review of practice-oriented research. Int J Inf Manag. 2020;53:102032.
Download references
Acknowledgements
The authors would like to thank the Deanship of Scientific Research at Shaqra University for supporting this work.
This research has received no specific funding.
Author information
Authors and affiliations.
Mental Health Nursing Department, College of Nursing, University of Ha’il, Ha’il City, KSA, Saudi Arabia
Mohammed Hamdan Alshammari
College of Applied Medical Science, Master of Nursing in Mental Health, BSN, Shaqra University, Aldwadmi-Shaqra Road, 15572, Shaqra City, Riyadh Province, Saudi Arabia
Atallah Alenezi
You can also search for this author in PubMed Google Scholar
Contributions
M.A conceptualized the study. M.A A.A, collected, organized, and analyzed the data, and participated in writing and reviewing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Atallah Alenezi .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki. The study design was approved by the Standing Committee for Research Ethics at University of Hail (H-2022-289) in Saudi Arabia. All of the respondents agreed to participate voluntarily before completing the questionnaire. All responses were kept strictly confidential for research purposes only, and the results did not personally identify respondents. An informed consent was obtained from all participants before answering the questions.
Consent for publication
Not Applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Alshammari, M.H., Alenezi, A. Nursing workforce competencies and job satisfaction: the role of technology integration, self-efficacy, social support, and prior experience. BMC Nurs 22 , 308 (2023). https://doi.org/10.1186/s12912-023-01474-8
Download citation
Received : 16 March 2023
Accepted : 31 August 2023
Published : 07 September 2023
DOI : https://doi.org/10.1186/s12912-023-01474-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Technology Integration
- Social Support
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Bureaus and Offices
- Contact HRSA
- Data & Research
- Health Workforce Research
Job Satisfaction Among Registered Nurses – Pre-COVID
This brief provides information on job satisfaction among the 3,272,872 registered nurses (RNs) employed in the United States, based on the 2018 National Sample Survey of Registered Nurses (NSSRN).
The survey was administered between April and October 2018, with most information reported as of December 31, 2017. It does not reflect the impact of the COVID-19 pandemic on workforce morale. This brief will be updated when data from the 2022 NSSRN becomes available.
Most Nurses Were Satisfied or Extremely Satisfied
Exhibit 1. Job Satisfaction Among Registered Nurses, 2017
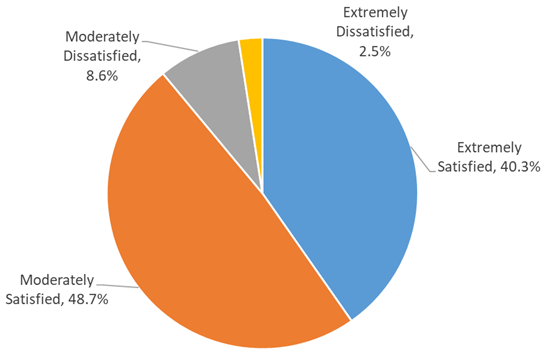
Detailed Description of Exhibit 1
The majority of registered nurses (RNs) were either moderately satisfied (48.7%) or extremely satisfied (40.3%) with their primary nursing position.
About 11% of nurses expressed some degree of dissatisfaction with their primary nursing position.
Job Satisfaction Varies by Area of Specialization
Exhibit 2. Share of Nurses Indicating Extremely Satisfied or Moderately Satisfied With Primary Nursing Position, Select Area of Specialty
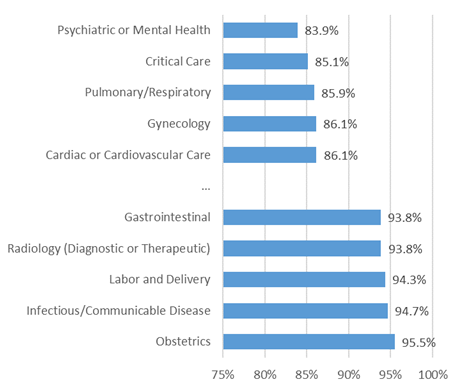
Detailed Description of Exhibit 2
There is little difference in job satisfaction between nurses with and without patient care responsibilities.
- Overall, 88.7% of RNs with patient care responsibilities indicated they were either extremely or moderately satisfied with their primary nursing position.
- 90.2% of RNs without patient care responsibilities expressed satisfaction with their primary nursing position.
Among nurses with patient care responsibilities, satisfaction varies across areas of specialization, ranging from a low of 83.9% for psychiatric or mental health nurses (including substance abuse and counseling), to a high of 95.5% for RNs specializing in obstetrics.
Despite Generally High Levels of Job Satisfaction, Stress and Burnout Remain a Problem
Exhibit 3a. Most Commonly Cited Reasons for Leaving Primary Nursing Position After December 31, 2017
RNs No Longer Working in Nursing
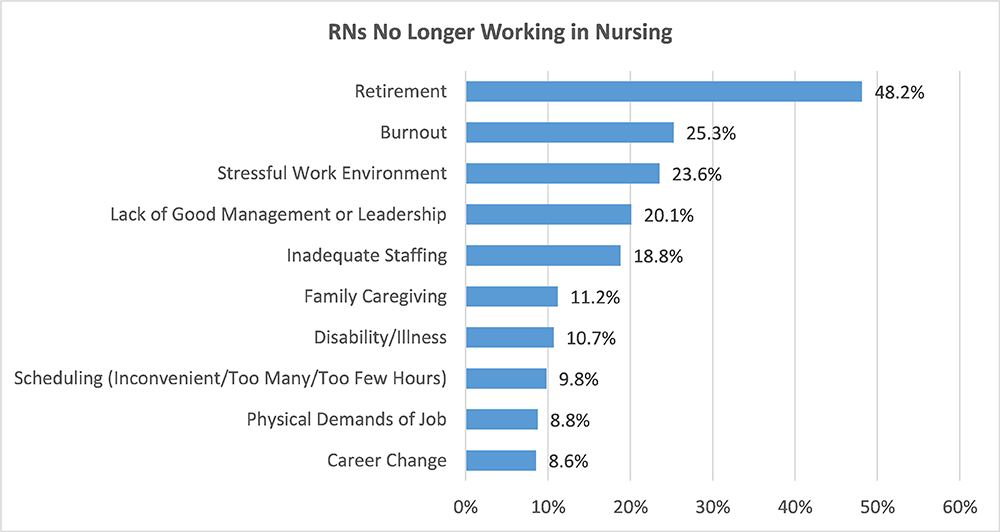
Detailed Description of Exhibit 3a
Exhibit 3b. RNs Still Employed in Nursing
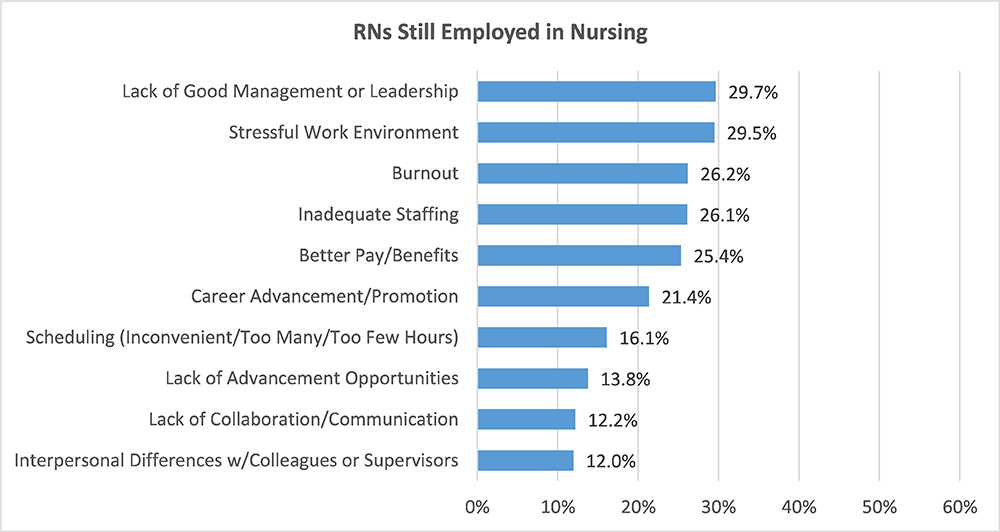
Detailed Description of Exhibit 3b
Despite generally high satisfaction among nurses, 12.8% of RNs left their primary nursing position between December 31, 2017, and the date they responded to the survey in 2018.
- Of the RNs that left their primary nursing position, the majority (79.2%) continued to work in nursing.
- Only 2.7% of RNs employed on December 31, 2017, left nursing altogether.
For those that left nursing, retirement was the most commonly given reason for leaving, followed by burnout, a stressful working environment, lack of good management or leadership, and inadequate staffing.
For those that left their primary position for another nursing position, lack of good management or leadership, a stressful working environment, and burnout were the most common reasons given.
More Than Half of RNs Have Considered Leaving Their Primary Position
Exhibit 4. Most Common Reasons Given for Considering Leaving Primary Nursing Position
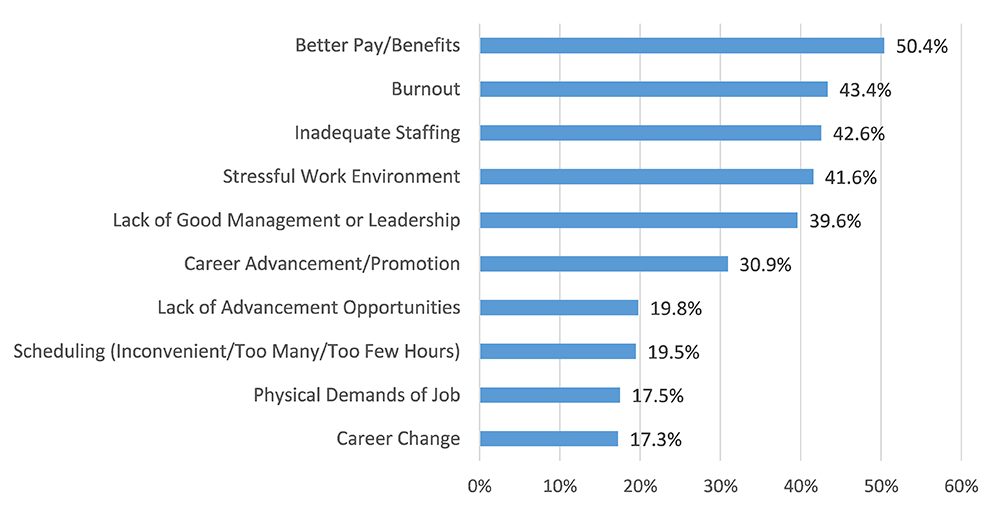
Detailed Description of Exhibit 4
Of the RNs that remained in their primary nursing position between December 31, 2017, and the date they responded to the survey, more than half (54.6%) indicated that they have considered leaving their position at some point in the past. Nearly half (49.6%) indicated that they considered leaving their primary nursing position in the past year.
Better pay and benefits, burnout, inadequate staffing, a stressful work environment, and a lack of good management or leadership were the most common reasons cited for considering leaving.
Nearly Half of RNs Plan to Leave Their Primary Position in the Next 3 Years
Exhibit 5. When Do You Plan on Leaving Primary Nursing Position?
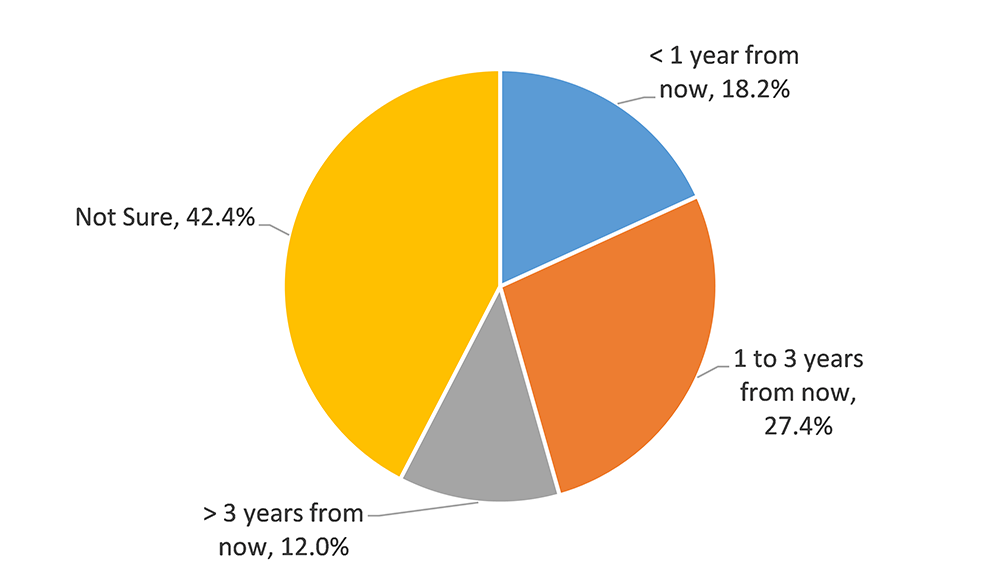
Detailed Description of Exhibit 5
For RNs that have considered leaving their primary nursing position, 18.2% plan to leave within the next year, while 27.4% indicated they plan to leave between one and three years from now.
Most RNs Plan to Continue in Nursing After Leaving Their Current Position
Exhibit 6. Majority of RNs Considering Leaving Primary Position Plan to Continue in Nursing
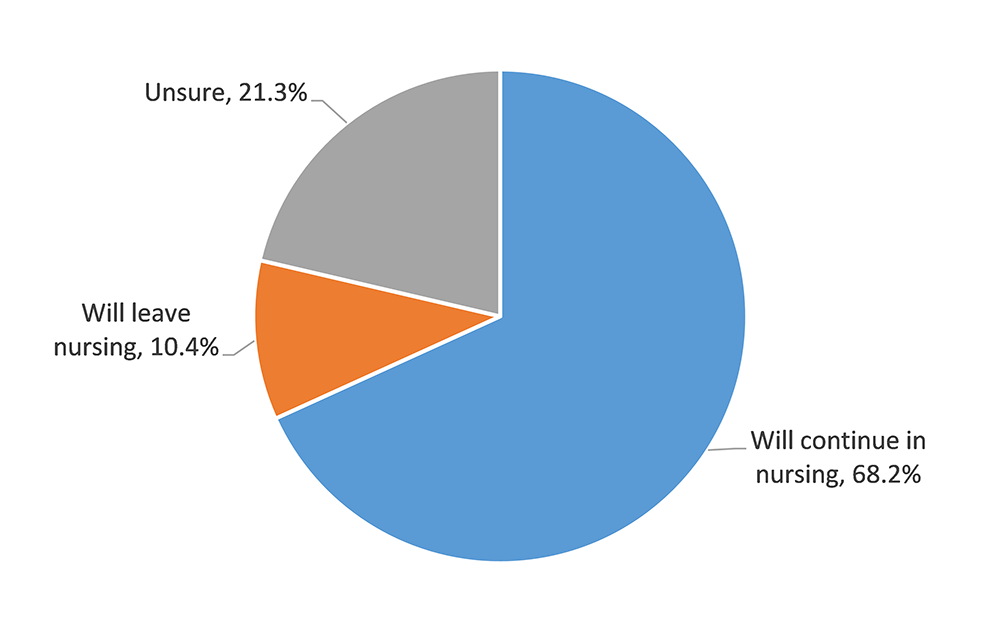
Detailed Description of Exhibit 6
Most RNs (68.2%) that have considered leaving their primary nursing position plan to continue in nursing after leaving their current position. Only 10.4% indicated that they planned to leave nursing altogether, while 21.3% were unsure if they would continue in nursing or not.
The Average Nurse Worked Nearly 3 Hours a Week Longer Than Scheduled in 2017
Exhibit 7. Average Number of Hours Scheduled and Worked in a Typical Week
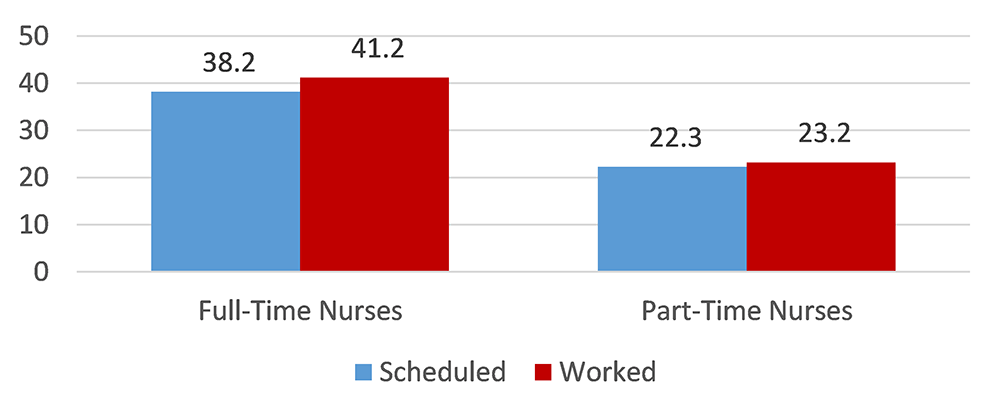
Detailed Description of Exhibit 7
Another factor that may impact job satisfaction among RNs is scheduling and hours worked.
In 2017, the average nurse worked nearly three hours more than scheduled in a typical week (37.5 hours worked, compared to 34.9 hours scheduled).
Full-time nurses experienced a greater discrepancy between hours scheduled and hours worked than part-time nurses.
Nurses Earned a Median Income of $68,774 in 2017
Exhibit 8. Distribution of Earnings from Primary Nursing Position (Full-Time and Part-Time RNs)
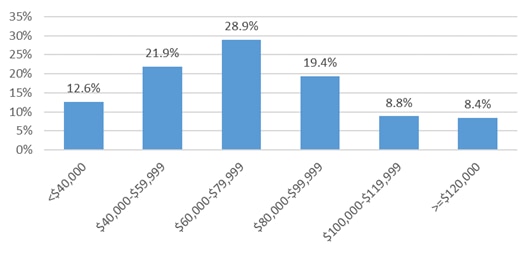
Detailed Description of Exhibit 8
Better pay or benefits was a common reason cited by RNs for leaving or considering leaving their primary nursing position.
Overall, RNs earned a median income of $68,774 from their primary nursing position in 2017. Median earnings for full-time RNs were $73,929, while part-time RNs earned a median income of $39,985 from their primary nursing position. Exhibit 8 shows the distribution of earnings for all RNs in 2017.
The median annual earnings for RNs across all nursing-related employment was $69,898 for the year ended December 31, 2017.
11% of RNs Held More Than One Nursing Job in 2017
Exhibit 9. Overall Median Earnings From Nursing Employment, Nurses With Secondary Nursing Employment in 2017
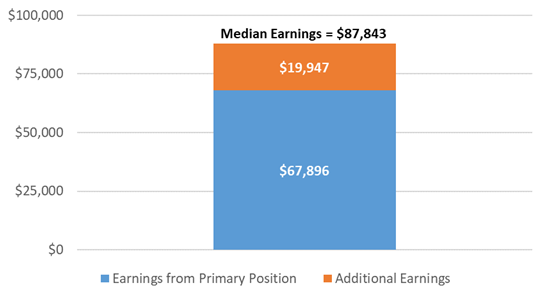
Detailed Description of Exhibit 9
Nurses whose primary nursing position was part-time were slightly more likely to hold a secondary nursing position than their full-time counterparts (12.4% compared to 10.7%).
RNs with secondary nursing employment earned a combined median annual income of $87,843 from all nursing positions, a difference of nearly $20,000 compared to their earnings from their primary position ($67,896).
About the Data
The National Sample Survey of Registered Nurses (NSSRN) is the longest running survey of registered nurses (RNs) in the United States. Since its inaugural assessment in 1977, the NSSRN has provided educators, health workforce leaders, and policymakers with key details and developments of the nursing workforce supply and includes information on the demographics, educational attainment, licenses and certifications, and employment characteristics of RNs in the United States.
In collaboration with the U.S Census Bureau, the National Center for Health Workforce Analysis administered the 10th NSSRN data collection in 2018. From April 2018 to October 2018, a total of 50,273 registered nurses completed the survey via a web form or a paper questionnaire with an unweighted response rate of 50.1% (49.1% weighted). This survey gathered data from participants with active RN licenses from all U.S. states revealing a comprehensive look into the RN and Advanced Practice Register Nurse (APRN) workforce.
Planning is currently underway for the 2022 NSSRN, which will collect data on RNs with active licenses as of December 31, 2021. This survey will provide an important point of reference for understanding how the nursing profession is impacted by the COVID-19 pandemic. We will update this brief when data from the 2022 NSSRN is available.
To learn more about the NSSRN or to download data and reports, visit National Sample Survey of Registered Nurses (NSSRN) .

IMAGES
VIDEO
COMMENTS
1. Introduction. Health professions especially nurses spend almost half of their waking hours in the workplace. Therefore, job satisfaction and work environment are of great importance [].As one of the most challenging organizational concepts, job satisfaction forms the fundamentals of most management policies to increase the productivity and efficiency of the organization [].
In fact, job satisfaction for nurse s in outpatient, ambulatory, and other clinical settings declined by just over 2 percentage points between 2017 and 2021, from 90.8% to 88.6%. In contrast, job satisfaction among hospital-based RNs declined by 11.8 percentage points, from 89.0% to 77.2%, between 2017 and 2021.
Job dissatisfaction is the. commonest cause for the nurses to give up their. job, which leads to high turnover and shortage of. the nurses. 2 A major target of the health care. delivery system is ...
Job performance. Hou et al. (2013) investigated the influence of nurses' job satisfaction on the job performance of staff nurses. They found that, after controlling for demographic variables, nurses' job satisfaction independently explained 11.8% of the total variance of job performance. 3.1.6. Effort and reward.
The findings of this study indicate that, in this particular context, clinical supervision has the potential to enhance the job satisfaction of qualified primary health care nurses. This conclusion is drawn from the observation that job satisfaction improved after a six-month follow-up period. [ 25] Finland.
Aims: To identify current best evidence on the types of interventions that have been developed to improve job satisfaction among nurses and on the effectiveness of these interventions. Design: The systematic review is a quantitative systematic review and meta-analysis following a profile-likelihood random-effects model. Data sources: CINAHL, Medic, and Pubmed (Medline).
88% showed a significant correlation between leadership style and nurses' job satisfaction. Trans-. formational style had the highest number of positive correlations followed by authentic ...
The recruitment and retention of nurses is problematic worldwide. There is a maldistribution of human resources for health, a shortage in the overall number of qualified nurses and an aging nursing workforce [].Job satisfaction has been cited as an important factor contributing to the turnover of nurses and as an antecedent to nursing retention [2,3,4].
Background Poor job conditions and limited resources are reducing job satisfaction and motivation among nurses in low-income countries, which may affect the quality of services and attrition rates. The objective of this study was to examine job satisfaction, motivation and associated factors among nurses working in the public health facilities of Ethiopia, with the aim of improving performance ...
2013). Other factors that contribute to the nursing shortage are low job satisfaction and burnout (Khamisa, Peltzer, Ilic & Oldenburg, 2016). Many conditions in nursing may contribute to low job satisfaction, burnout and intent to leave. Macken and Hyrkas (2014) reported that registered nurses who worked 12-hour shifts acknowledged moderate to
Given these factors it becomes clear that research about job satisfaction cannot be undertaken across the nursing profession as a whole, but rather needs to consider various settings and organisational environments to understand the issues facing different nursing groups. ... Nursing Job Satisfaction Scale • 98% female, mean age 45 years ...
Methods Research design. In this cross-sectional, quantitative study, an online survey was used as the research method to investigate the impact of nursing training and technology integration on nursing workforce competencies and job satisfaction, as well as to investigate the moderating role of prior experience and the mediating roles of self-efficacy and social support.
satisfaction can contribute to nurse retention, and lower levels of job satisfaction can lead. to increased attrition (Boudreau, 2012). The dataset was collected over a period of 30 to. 33 months from March 2008 to May 2011, taking 3 years to gather the survey data from.
Research Proposal Gender and Job Satisfaction Among Nurses in the US Dana Kaileh, Jingming Cen, La Dayo Mithell, Maryam Mujaddide and Myriam Rubio ... Nurses' job satisfaction significantly impacts the quality of patient care, nurses' dedication to healthcare organizations, their well-being, and turnover. Job satisfaction is defined
The workload imposed on educators, from the time of research proposal approval to the publication of the article, has negative effects on their job satisfaction (Sussman, 2012). ... To improve job satisfaction in nurse educators, managers and authorities are recommended to use preventive behaviors such as continuous surveys with nurse educators ...
This brief provides information on job satisfaction among the 3,272,872 registered nurses (RNs) employed in the United States, based on the 2018 National Sample Survey of Registered Nurses (NSSRN). The survey was administered between April and October 2018, with most information reported as of December 31, 2017. It does not reflect the impact of the COVID-19 pandemic on workforce morale.
Nursing Research: March 1990 - Volume 39 - Issue 2 - p 113-116. Buy; Abstract. Thirty-three items originally developed to measure three dimensions of nurses' job satisfaction were subjected to a series of checks designed to determine the number of dimensions being measured and the reliability and validity of the measures of these dimensions ...