Why Are Nurses Important To Society – (20 TOP REASONS)
Are you a new nurse or considering becoming one? Do you wonder if being a nurse is significant? Perhaps you have asked the question, “Why are nurses important to society?” I understand; after all, you want to know you have chosen a career where you can make a difference and positively impact the world around you. In the field of nursing, you will have countless opportunities to do just that! Nurses play a HUGE role in healthcare and are vital to the medical field. In this article, I will share 20 reasons why nurses are so important to society and tell you how your actions can directly impact patients, families, and communities.

Why are Nurses Important to Society?
Reason #1: nurses are patient advocates, reason #2: nurses provide most of the direct patient care, reason #3: nurses provide compassionate care, reason #4: nurses perform vital patient assessments, reason #5: nurses play a huge role in emergency response, reason #6: nurses assist patients with medication management, reason #7: nurses are a source of emotional support, reason #8: nurses are critical thinkers, reason #9: nurses ensure patient safety, reason #10: nurses are a source of health education for patients, reason #11: nurses are care coordinators, reason #12: nurses aid in health promotion and disease prevention, reason #13: nurses empower patients, reason #14: nurses contribute to healthcare innovation, reason #15: nurses play a significant role in infection control, reason #16: nurses help patients manage their pain, reason #17: nurses engage in lifelong learning to promote positive patient outcomes, reason #18: nurses serve in leadership roles throughout healthcare, reason #19: nurses contribute to industry research and evidence-based practices, reason #20: nurses provide telehealth and telemedicine services, my final thoughts, list of sources used for this article.


The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity (2021)
Chapter: 5 the role of nurses in improving health equity, 5 the role of nurses in improving health equity.
Being a nurse … in 2020 must mean being aware of social injustices and the systemic racism that exist in much of nursing … and having a personal and professional responsibility to challenge and help end them.
—Calvin Moorley, RN, and colleagues, “Dismantling Structural Racism: Nursing Must Not Be Caught on the Wrong Side of History”
When this study was envisioned in 2019, it was clear that the future of nursing would look different by 2030; however, no one could predict how rapidly and dramatically circumstances would shift before the end of 2020. Over the coming decade, the nursing profession will continue to be shaped by the pressing health, social, and ethical challenges facing the nation today. Having illuminated many
of the health and social inequities affecting communities across the nation, the COVID-19 pandemic, along with other health crises, such as the opioid epidemic ( Abellanoza et al., 2018 ), presents an opportunity to take a critical look at the nursing profession, and society at large, and work collaboratively to enable all individuals to have a fair and just opportunity for health and well-being, reflecting the concept of “social mission” described by Mullan (2017, p. 122) as “making health not only better but fairer.” This chapter examines health equity and the role of nursing in its advancement in the United States.
As stated previously, health equity is defined as “the state in which everyone has the opportunity to attain full health potential and no one is disadvantaged from achieving this potential because of social position or any other socially defined circumstance” ( NASEM, 2017a , p. 32). While access to equitable health care, discussed in Chapter 4 , is an important part of achieving health equity, it is not sufficient. Health is affected by a wide range of other factors, including housing, transportation, nutrition, physical activity, education, income, laws and policies, and discrimination. Chapter 2 presents the Social Determinants of Health and Social Needs Model of Castrucci and Auerbach (2019) , in which upstream factors represent the social determinants of health (SDOH) that affect individuals and communities in a broad and, today, inequitable way. Low educational status and opportunity, income disparities, discrimination, and social marginalization are examples of upstream factors that impede good health outcomes. Midstream factors comprise social needs, or the individual factors that may affect a person’s health, such as homelessness, food insecurity, and trauma. Finally, downstream factors include disease treatment and chronic disease management.
Much of the focus on the education and training of nurses and the public perception of their role is on the treatment and management of disease. This chapter shifts that focus to nurses’ role in addressing SDOH and social needs, including their potential future roles and responsibilities in this regard, and describes existing exemplars. First, the chapter provides a brief overview of nurses’ role in addressing health equity. Next, it describes opportunities for nurses to improve health equity through four approaches: addressing social needs in clinical settings, addressing social needs and SDOH in the community, working across disciplines and sectors to meet multiple needs, and advocating for policy change. The chapter then details the opportunities and barriers associated with each of these approaches.
NURSES’ ROLE IN ADDRESSING HEALTH EQUITY
As described in Chapter 1 , the history of nursing is grounded in social justice and community health advocacy ( Donley and Flaherty, 2002 ; Pittman, 2019 ; Rafferty, 2015 ; Tyson et al., 2018 ), and as noted in Chapter 2 , the Code of Ethics for Nurses with Interpretive Statements, reiterated by American Nurses Association (ANA) President Ernest J. Grant in a public statement, “obligates nurses to be allies and to advocate and speak up against racism, discrimination, and injustice” ( ANA, 2020 ).
Addressing social needs across the health system can improve health equity from the individual to the system level. The report Integrating Social Care into the Delivery of Health Care identifies activities in five complementary areas that can facilitate the integration of social care into health care: adjustment, assistance, alignment, advocacy, and awareness ( NASEM, 2019 ) (see Figure 5-1 and Table 5-1 ). In

TABLE 5-1 Definitions of Areas of Activities That Strengthen Integration of Social Care into Health Care
| Activity | Definition | Transportation-Related Example |
|---|---|---|
| Awareness | Activities that identify the social risks and assets of defined patients and populations. | Ask people about their access to transportation. |
| Adjustment | Activities that focus on altering clinical care to accommodate identified social barriers. | Reduce the need for in-person health care appointments by using other options such as telehealth appointments. |
| Assistance | Activities that reduce social risk by providing assistance in connecting patients with relevant social care resources. | Provide transportation vouchers so that patients can travel to health care appointments. Vouchers can be used for ride-sharing services or public transit. |
| Alignment | Activities undertaken by health care systems to understand existing social care assets in the community, organize them to facilitate synergies, and invest in and deploy them to positively affect health outcomes. | Invest in community ride-sharing or time-bank programs. |
| Advocacy | Activities in which health care organizations work with partner social care organizations to promote policies that facilitate the creation and redeployment of assets or resources to address health and social needs. | Work to promote policies that fundamentally change the transportation infrastructure within the community. |
SOURCE: NASEM, 2019 .
the area of awareness, for example, clinical nurses in a hospital setting can identify the fall risks their patients might face upon discharge and the assets they can incorporate into their lives to improve their health. In the area of adjustment, telehealth and/or home health and home visiting nurses can alter clinical care to reduce the risk of falls by, for example, helping patients to adjust risks in their homes and learn to navigate their environment. And these activities can continue to the high level of system change through advocacy for health policies aimed at altering community infrastructure to help prevent falls.
In short, improving population health entails challenging and changing the factors and institutions that give rise to health inequity through interventions and reforms that influence the institutions, social systems, and public policies that drive health ( Lantz, 2019 ). It is important to note, however, that there are shortcomings in how evaluations of health equity interventions are carried out (see Box 5-1 ).
ADDRESSING SOCIAL NEEDS IN CLINICAL SETTINGS
Although the provision of clinical care is a downstream determinant of health, the clinical setting presents an opportunity for nurses to address midstream determinants, or social needs, as well. Screening for social needs and making referrals to social services is becoming more commonplace in clinical settings as part of efforts to provide holistic care ( Gottlieb et al., 2016 ; Makelarski et al., 2017 ; Thomas-Henkel and Schulman, 2017 ). Nurses may conduct screenings; review their results; create care plans based on social needs as indicated by those results; refer patients to appropriate professionals and social services; and coordinate care by interfacing with social workers, community health workers, and social services providers. Although the importance of screening people for social needs has led more providers to take on this role, it has yet to become a universal practice ( CMS, 2020 ; NASEM, 2016 ), as most physician practices and hospitals do not perform screenings for the five key domains of social need 1 : food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence ( CMS, 2020 ; Fraze et al., 2019 ). As trusted professionals that spend significant time with patients and families, nurses are well equipped to conduct these screenings ( AHA, 2019 ). Federally qualified health centers (FQHCs)—community-based health centers that receive funds from the Health Resources and Services Administration’s (HRSA’s) Health Center Program—often screen for social needs.
In many clinical settings, however, challenges arise with screening for social needs. Individuals may be hesitant to provide information about such issues as housing or food insecurity, and technology is required to collect social needs data and once obtained, to share these data across settings and incorporate them into
___________________
1 These five domains of social needs are part of the Centers for Medicare & Medicaid Services’ Accountable Health Communities Model ( Fraze et al., 2019 ).
nursing practice in a meaningful way. While nurses have an educational foundation for building the skills needed to expand their role from assessing health issues to conducting assessments and incorporating findings related to social needs into care plans, this focus needs to be supported by policies where nurses are employed. As the incorporation of social needs into clinical consideration expands, nurses’ education and training will need to ensure knowledge of the impact of social needs and SDOH on individual and population health (see Chapter 7 ). Communicating appropriately with people about social needs can be difficult, and training is required to ensure that people feel comfortable responding to personal questions related to such issues as housing instability, domestic violence, and financial insecurity ( Thomas-Henkel and Schulman, 2017 ). Finally, the utility of social needs screening depends on networks of agencies that offer services and resources in the community. Without the ability to connect with relevant services, screenings and care plans can have little impact. Consequently, it is important for health care organizations to dedicate resources to ensuring that people are connected to appropriate resources, and to follow up by tracking those connections and offering other options as needed ( Thomas-Henkel and Schulman, 2017 ).
ADDRESSING SOCIAL NEEDS AND SOCIAL DETERMINANTS OF HEALTH IN THE COMMUNITY
While interest in and action to address social needs in the clinical setting is rapidly expanding, nurse engagement in these issues in community settings has been long-standing. Nurses serving in the community often work directly to address social needs at the individual and family levels, and often work as well to address SDOH at the community and population levels. Public health nurses in particular have broad knowledge of health issues and the associated SDOH, as well as needs and resources, at the community level. Embedded within the community, they also are well positioned to build trust and are respected among community leaders. Also playing important roles in addressing social needs within the community are home visiting nurses. At the individual and family levels, home visiting nurses often represent the first line of health care providers with sustained engagement in addressing social needs for many individuals. They recognize and act on the limitations associated with social needs, such as the inability to afford transportation, or may work with an interdisciplinary team at the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) clinic to address food issues and other social needs. By connecting with individuals in their neighborhoods and homes, public health and other community-based nurses promote health and well-being for families within communities and engage in this work with partners from across social, health, and other services.
At the population health level, public health nurses work to achieve health equity within communities through both health promotion and disease prevention and control. They often work in municipal and state health departments and apply
nursing, social, epidemiology, and other public health sciences in their contributions to population health ( Bigbee and Issel, 2012 ; IOM, 2011 [see AARP, 2010 ]; Larsen et al., 2018 ). They offer a wide range of services to individuals and community members and are engaged in activities ranging from policy development and coalition building to health teaching and case management ( Minnesota Department of Health, n.d. ). Public health nurses serve populations that include those with complex health and social needs, frail elderly, homeless individuals, teenage mothers, and those at risk for a specific disease ( Kulbok et al., 2012 ). Their interventions may target specific health risks, such as substance use disorder, HIV, and tobacco use, or populations at risk for health problems, such as individuals with complex health and social needs. Specific knowledge and skills they bring to communities include the ability to perform assessments of individual, family, and community health needs; use data and knowledge of environmental factors to plan for and respond to public health issues in their community; provide community and health department input in the development of policies and programs designed to improve the health of the community; implement evidence-based public health programs; and develop and manage program budgets ( Minnesota Department of Health, n.d. ).
Public health nursing roles are characterized by collaboration and partnerships with communities to address SDOH ( Kulbok et al., 2012 ). Core to public health nursing is working across disciplines and sectors to advance the health of populations through community organizing, coalition building, policy analysis, involvement in local city and county meetings, collaboration with state health departments, and social marketing ( Canales et al., 2018 ; Keller et al., 2004 ). Yet, while the work of public health nurses is foundational to the health of communities, their work is rarely visible. Additionally, regarding measurable reductions in health disparities, little research is available that connects directly and explicitly to public health nursing roles ( Davies and Donovan, 2016 ; Schaffer et al., 2015 ; Swider et al., 2017 ).
Recent experiences with H1N1, Ebola, Zika, and COVID-19 underscore the importance of having strong, well-connected, well-resourced social services, public health, and health care systems, matched by an adequate supply of well-educated nurses. A 2017 report from the National Academies of Sciences, Engineering, and Medicine focused on global health notes that when infectious disease outbreaks occur, significant costs are often associated with fear and the worried-well seeking care ( NASEM, 2017b ). In their role as trusted professionals, and given their widespread presence in communities, incorporating public health nurses into community, state, and federal government strategies for health education and dissemination of information can help extend the reach and impact of messaging during infectious disease outbreaks and other public health emergencies. Nurses can serve as expert sources of information (e.g., on preventing infectious disease transmission within their communities) ( Audain and Maher, 2017 ). In the United States, for example, as Zika infections were
identified and spreading, one of the strategies used by the U.S. Department of Health and Human Services (HHS) was to work through nursing associations to reach nurses and through them, help reach the public with factual information and minimize unnecessary resource use ( Minnesota Department of Health, 2019 ). Given their expertise in community engagement and knowledge of local and state government health and social services assets, public health nurses are well positioned to link to and share health-related information with community partners to help reach underresourced populations, including homeless individuals, non-English-speaking families, and others.
WORKING ACROSS DISCIPLINES AND SECTORS TO MEET MULTIPLE NEEDS
As nurses work in concert with other sectors and disciplines, interventions that address multiple and complex needs of individuals and communities can have far-reaching impacts on health outcomes and health care utilization. Through partnerships, community-based nurses work to address an array of health-related needs ranging from population-level diabetes management to community-based transportation to enable low-income families to access health care services.
Because multiple factors influence individual and population health, a multidisciplinary, multisectoral approach is necessary to improve health and reduce health inequity. While an approach focusing on only one SDOH may improve one dimension of health, such as food insecurity, intersectional approaches that simultaneously address complex, holistic needs of individuals, families, and communities are often required. Commonly found across underresourced communities are layers of intersecting challenges impacting health, ranging from adverse environmental exposures to food deserts. Health care systems, community-based organizations, government entitities, nurses, and others are increasingly working together to design interventions that reflect this complexity ( NASEM, 2017a , 2019 ). Creative alliances are being built with for-profit and not-for-profit organizations, community groups, federal programs, hospitals, lending institutions, technology companies, and others ( NASEM, 2019 ).
Work to prioritize and address health disparities and achieve health equity is predicated on meaningful, often multidimensional, assessments of community characteristics. One key opportunity to inform multisectoral efforts lies in community health needs assessments. The Patient Protection and Affordable Care Act requires nonprofit hospitals to conduct these assessments every 3 years, with input from local public health agencies. These assessments are then used to identify and prioritize significant health needs of the community served by the hospital while also identifying resources and plans for addressing these needs. Conducting a community health needs assessment is itself a multisectoral collaboration as it requires engaging community-based stakeholders ( Heath, 2018 ). The results of the assessment present opportunities for multiple sectors to work
together. For example, a hospital may partner with public health and area food banks to address food insecurity. Or it may partner with a health technology company and a local school board to address digital literacy for underserved youth and their families, and also extend the reach of broadband to support health care access through telehealth technology and strengthen digital literacy. In assessing the community’s health needs, these hospitals are required to obtain and consider community-based input, including input from individuals or organizations with knowledge of or expertise in public health. The reports produced as part of this process are required to be publicly available ( IRS, 2020 ).
These and other community engagement efforts can involve nurses from a variety of clinical and community-based settings in any and all steps of the process, from design to implementation and evaluation of the assessments themselves or the processes and programs established to address identified priorities. For example, the Magnet recognition program of the American Nurses Credentialing Center requires participating hospitals to involve nurses in their community health needs assessments ( ANCC, 2017 ).
A variety of models feature nurses directly addressing health and social needs through multidisciplinary, multisectoral collaboration. Two illustrative programs are described below: the Camden Core Model and Edge Runner.
Camden Core Model
The Camden Coalition, based in Camden, New Jersey, is a multidisciplinary, nonprofit organization that works across sectors to address health and social needs. The Coalition’s formation was based on the recognition that the U.S. health care system far too often fails people with complex health and social needs. These individuals cycle repeatedly through multiple health care, social services, and other systems without realizing lasting improvements in their health or well-being. The Coalition employs multiple approaches that include using faith-based partnerships to deliver health services and encourage healthy choices; sharing data among the criminal justice, health care, and housing sectors to identify points of intervention; and building local and national coalitions to support and educate others interested in implementing this model ( Camden Coalition, n.d. ). One of the Coalition’s best-known programs is the Camden Core Model. This nationally recognized care management intervention is an example of a nurse-led care management program for people with complex medical and social needs. It applies the principles of trauma-informed care and harm reduction with the aim of empowering people with the skills and support they need to avoid preventable hospital use and improve their well-being ( Finkelstein et al., 2020 ; Gawande, 2011 ). The model uses real-time data on hospital admissions to identify “superutilizers,” people with complex health issues who frequently use emergency care. An interprofessional team of registered nurses (RNs) and licensed practical nurses (LPNs), social workers, and community health workers engage in person
with these individuals to help them navigate their care by connecting them with medical care, government benefits, and social services ( Camden Coalition, n.d. ; Finkelstein et al., 2020 ). With federal funding, similar versions of the model have been extended to cities outside of Camden ( AF4Q, 2012 ; Crippen and Isasi, 2013 ; Mann, 2013 ).
Camden Coalition partnerships optimize the use of nurses in the community in several ways. An interprofessional team of nurses, social workers, and community health workers visits program participants, helps reconcile their medications, accompanies them to medical visits, and links them to social and legal services. Critical to the model’s success is recruiting nurses who are from the local community, capitalizing on their cultural and systems-level knowledge to facilitate and improve access to and utilization of local health and social services. The culture of the Camden Coalition model has been key to its success. The uniform commitment of nurses, staff, and leadership to addressing people’s complex needs has created a supportive work environment in which each team member’s role is optimized. Care Team members have accompanied people to their meetings and appointments for primary care, helped with applications for such public benefits as food stamps, provided referrals to social services and housing agencies, arranged for medication delivery in partnership with local pharmacies, and coordinated care among providers.
The Camden Coalition focuses on “authentic healing relationships,” defined as secure, genuine, and continuous partnerships between Care Team members and patients. This emphasis has evolved into a framework for patient engagement known as COACH, which stands for C onnect tasks with vision and priorities, O bserve the normal routine, A ssume a coaching style, C reate a backward plan, and H ighlight progress with data. An interprofessional team of nurses, social workers, and community health workers visits participants in the community. Team members are trained to problem solve with patients to achieve the program goals of helping them manage their chronic health conditions and reducing preventable hospital admissions.
Early evidence of the program’s effect in a small sample showed a 56 percent reduction in monthly hospital charges, a roughly 40 percent reduction in monthly visits to hospitals and emergency departments, and an approximately 52 percent increase in rates of reimbursement to care providers ( Green et al., 2010 ), although later evidence from a randomized controlled trial (RCT) indicated that the Camden Core Model did not reduce hospital readmissions ( Finkelstein et al., 2020 ). Other RCTs, conducted in Philadelphia and Chicago, showed that similar social care programs using case management and community health workers can reduce hospital admissions and save money in addition to improving health and quality of health care. Kangovi and colleagues (2018) conducted an RCT in Philadelphia to assess Individualized Management for Patient-Centered Targets (IMPaCT), a standardized community health worker intervention addressing unmet social needs across three health systems ( Kangovi et al., 2018 ). After 6 months, patients
in the intervention group compared with controls were more likely to report the highest quality of care and spent fewer total days in the hospital (reduced by about two-thirds), saving $2.47 for each dollar invested by Medicaid annually ( Kangovi et al., 2020 ). The RCT in Chicago assessed the effectiveness of a case management and housing program in reducing use of urgent medical services among homeless adults with chronic medical conditions and found a 29 percent reduction in hospitalizations and a 24 percent reduction in emergency department visits ( Sadowski et al., 2009 ).
Edge Runner
The American Academy of Nurses’ Edge Runner initiative identifies and promotes nurse-designed models of care and interventions that can improve health, increase health care access and quality, and/or reduce costs ( AAN, n.d.a ). As of February 2020, 59 such programs had been evaluated against a set of criteria and designated as part of this initiative. Many Edge Runner programs are built around the needs of underserved communities and seek to improve health through holistic care that addresses social needs and SDOH, including a range of upstream, midstream, and downstream determinants. Mason and colleagues (2015) assessed 30 Edge Runner models identified as of 2012, finding four main commonalities that illustrate these programs’ broad and encompassing approach to health.
A holistic definition of health. Across the programs, health was defined broadly to include physical, psychological, social, spiritual, functional, quality-of-life, personal happiness, and well-being aspects. Additionally, the definition of health was based on the values of clients and shaped around their preferences. Typically, programs were grounded in SDOH to inform their design of individual- and community-level interventions.
Individual-, family-, and community-centric design. Most programs prioritized individual, family, and community goals over provider-defined goals through a “participant-led care environment” and “meeting people where they are.” Thus, interventions were tailored to the values and culture present at each of these three levels.
Relationship-based care. The programs reflected the importance of building trusting relationships with individuals, families, and communities to help them engage in ways to create and sustain their own health.
Ongoing group and public health approaches to improving the health of underserved populations. The nurses who designed the programs viewed serving underserved populations as a moral imperative. Through peer-to-peer education, support groups, and public health approaches, they sought to empower clients, give them a sense of control, build self-care agency, and increase resilience.
An in-depth study of three Edge Runner programs (the Centering Pregnancy model, INSIGHTS, and the Family Practice and Counseling Network) revealed particular lessons: the essential role of collaboration and leaders who can col-
laborate with a wide range of stakeholders, the need for plans for scalability and financial sustainability, and the importance of social support and empowerment to help people ( Martsolf et al., 2017 ). In these and other models, the capacity and knowledge associated with building meaningful, sustained partnerships across sectors is a key dimension of nursing practice that impacts health equity. The Edge Runner programs emphasize how, in the pursuit of improving care, lowering costs, and increasing satisfaction for people and families, nurses are actively working to achieve person-centered care that addresses social needs and SDOH and focusing on the needs of underserved populations to promote health equity ( Martsolf et al., 2016 , 2017 ; Mason et al., 2015 ). However, evidence directly linking the programs to decreases in disparities is generally not available. Two examples of Edge Runner programs are described in Box 5-2 .
As models continue to evolve and be disseminated, it is critical to establish an evidence base that can help understand their impact on health and well-being and their contribution to achieving the broader aim of health equity. For care management programs incorporating social care, it is important to consider a broad array of both quantitative and qualitative measures beyond health care utilization ( Noonan, 2020 ). Although RCTs generate the most reliable evidence, this evidence can be limited in scope. For example, the RCTs cited above assessed neither the multidimensional nature of care management/social care models that might be reflected in such outcomes as client self-efficacy, satisfaction, or long-term health outcomes nor their potential social impacts. Also important to note is that care management models incorporating social care are limited by the availability of resources in the community, such as behavioral health services, addiction treatment, housing, and transportation. Programs that connect clients to health and social
services are unlikely to work if relevant services are unavailable ( Noonan, 2020 ). Important to underscore in the context of this report is that multisector engagement, as well as health care teams that may involve social workers, community health workers, physicians, and others engaging alongside nurses, all are oriented to a shared agenda focused on improving health and advancing health equity.
ADVOCATING FOR POLICY CHANGE
Public policies have a major influence on health care providers, systems, and the populations they serve. Accordingly, nurses can help promote health equity by bringing a health lens to bear on public policies and decision making at the community, state, and federal levels. Informing health-related public policy can involve communicating about health disparities and SDOH with the public, policy makers, and organizational leaders, focusing on both challenges and solutions for addressing health through actions targeted to achieving health equity.
When nurses engage with policy change as an upstream determinant of health, they can have a powerful and far-reaching impact on the health of populations. In the National Academy of Medicine’s Vital Directions series, Nancy Adler and colleagues (2016) note that “powerful drivers of health lie outside the conventional medical care delivery system…. Health policies need to expand to address factors outside the medical system that promote or damage health.” Because health inequities and SDOH are based in social structures and policies, efforts to address them upstream as the root of poor health among certain populations and communities need to focus on policy change ( NASEM, 2017a ). Nurses alone cannot solve the problems associated with upstream SDOH that exist outside of health care systems. However, by engaging in efforts aimed at changing local, state, or federal policy with a Health in All Policies approach, 2 they can address SDOH that underlie poor health ( IOM, 2011 ; NASEM, 2017a ; Williams et al., 2018 ). Whether nurses engage in policy making full time or work to inform policy part time as a professional responsibility, their attention to policies that either create or eliminate health inequities can improve the underlying conditions that frame people’s health. Nurses can bring a health and social justice lens to public policies and decision making at the community, state, and federal levels most effectively by serving in public- and private-sector leadership positions. Much of this work is discussed in Chapter 9 on nursing leadership, but it is noted in this chapter given the substantial
2 Health in All Policies (HiAP) is a collaborative approach that integrates health considerations into policy making across sectors. It recognizes that health is created by a multitude of factors beyond health care and in many cases, beyond the scope of traditional public health activities. In accordance with HiAP, for example, decision makers in the health care sector should consider transportation, education, housing, commerce, and other sectors impacting communities. HiAP stresses the need to work across government agencies and with private partners from these different sectors to achieve healthy and safe communities. It also encourages partnerships between the health care sector and community developers, for example ( CDC, 2016 ).
influence that policy decisions have on health equity. Nurses can and should use their expertise to promote policies that support health equity.
For example, a nurse in Delaware was influential in getting the state’s legislature to pass legislation to implement a colorectal cancer screening program that has increased access to care and reduced disparities in morbidity and mortality from colorectal cancer (see Box 5-3 ). While individual nurses, often through their workplace and professional associations, engage in upstream efforts to impact health equity, there have been repeated calls from within the nursing community for more nurses to engage in informing public policy to improve health outcomes for individuals and populations.
CONCLUSIONS
In the coming decade, the United States will make substantial progress in achieving health equity only if it devotes resources and attention to addressing the adverse effects of SDOH on the health of underresourced populations. As 2030 approaches, numerous initiatives to address health equity are likely to be launched at the local, state, and national levels. Many of these initiatives will focus on health care equity. Yet, while expanding access to quality care is critical to reducing disparities and improving health outcomes, such efforts need to be accompanied by additional efforts to identify and change the social institutions, dynamics, and systems underlying health inequities from the local to the national level. Nurses can contribute to reshaping the landscape of health equity over the coming decade by serving in expanded roles, working in new settings and new ways, and partnering with communities and other sectors beyond health care. Some nurses are already working in roles and settings that support health equity and are engaged in educating about and advocating for health equity through their professional associations. Nonetheless, broader engagement as a core activity of every nurse will help advance health equity nationwide. To achieve this aim will require
- support for and the willingness of the nursing workforce to take on new roles in new settings in the community;
- consistency in nurses’ preparation for engaging in downstream, midstream, and upstream strategies aimed at improving health equity by addressing issues that compromise health, such as geographic disparities, poverty, racism, homelessness, trauma, drug abuse, and behavioral health conditions;
- more experiential learning and opportunities to work in community settings throughout nursing education to ensure that nurses have skills and competencies to address individuals’ complex needs and promote efforts to improve the well-being of communities;
- nursing education that goes beyond teaching the principles of diversity, equity, and inclusion to provide sustained student engagement in hands-on community and clinical experiences with these issues;
- funding to support new models of care and functions that address SDOH, health equity, and population health; and
- evaluation of models to build the evidence needed to scale programs and the policies and resources necessary to sustain them.
These issues are discussed in the chapters that follow. Programs described in this chapter, such as the Camden Coalition and the Edge Runner initiatives, are exemplars of the kind of multidisciplinary, multisector efforts that will be necessary to address the complex needs of individuals and communities and make a lasting impact by eliminating health disparities, with the goal of achieving health equity. Central to these future efforts, however, are parallel efforts that evaluate
and provide the evidence base on which to determine the effectiveness of models. One of the greatest challenges this committee faced was finding evidence directly linking the efforts of nurses to address social needs and SDOH to reductions in health disparities that would signal improved population health outcomes and health equity. Such evidence is essential to informing payment policy decisions that can ensure the sustainability of and nurse engagement in these models (discussed further in Chapter 6 ). Through evidence, the nursing profession can leverage its own potential, and the public, other professionals, and other sectors can understand the impact and value of such nursing engagement.
Conclusion 5-1: Nurses are in a position to improve outcomes for the underserved and can work to address the structural and institutional factors that produce health disparities in the first place.
Conclusion 5-2: Nurses can use their unique expertise and perspective to help develop and advocate for policies and programs that promote health equity.
AAN (American Academy of Nursing). n.d.a. Transforming America’s health system through nursing solutions . https://www.aannet.org/initiatives/edge-runners (accessed November 3, 2020).
AAN. n.d.b. ¡Cuídate!: A culturally-based program to reduce sexual risk behavior among Latino youth . https://www.aannet.org/initiatives/edge-runners/profiles/edge-runners--cuidate (accessed November 3, 2020).
AAN. n.d.c. Insights into children’s temperament: Supporting the development of low-income children . https://www.aannet.org/initiatives/edge-runners/profiles/edge-runners--insights-into-childrens-temperament (accessed November 3, 2020).
AARP. 2010. Preparation and roles of nursing care providers in America. http://championnursing.org/resources/preparation-and-roles-nursing-care-providers-america (accessed June 3, 2021).
Abellanoza, A., N. Provenzano-Hass, and R. J. Gatchel. 2018. Burnout in ER nurses: Review of the literature and interview themes. Journal of Applied Biobehavioral Research 23(1):e12117.
Adler, N. E., M. M. Glymour, and J. Fielding. 2016. Addressing social determinants of health and health inequalities. Journal of the American Medical Association 316(16):1641–1642.
AF4Q (Aligning Forces for Quality). 2012. Expanding “hot spotting” to new communities . http://forces4quality.org/node/5182.html (accessed November 3, 2020).
Agurs-Collins, T., S. Persky, E. D. Paskett, S. L. Barkin, H. I. Meissner, T. R. Nansel, S. S. Arteaga, X. Zhang, R. Das, and T. Farhat. 2019. Designing and assessing multilevel interventions to improve minority health and reduce health disparities. American Journal of Public Health 109(S1):S86–S93.
AHA (American Hospital Association). 2019. Screening for social needs: Guiding care teams to engage patients. Chicago, IL: American Hospital Association.
ANA (American Nurses Association). 2020. ANA president condemns racism, brutality and senseless violence against black communities . https://www.nursingworld.org/news/news-releases/2020/ana-president-condemns-racism-brutality-and-senseless-violence-against-black-communities (accessed September 17, 2020).
ANCC (American Nurses Credentialing Center). 2017. 2019 Magnet ® application manual. Silver Spring, MD: American Nurses Credentialing Center.
Audain, G., and C. Maher. 2017. Prevention and control of worldwide mosquito-borne illnesses: Nurses as teachers. Online Journal of Issues in Nursing 22(1):5.
Bigbee, J. L., and L. M. Issel. 2012. Conceptual models for population-focused public health nursing interventions and outcomes: The state of the art. Public Health Nursing 29(4):370–379.
Braveman, P., E. Arkin, T. Orleans, D. Proctor, and A. Plough. 2017. What is health equity? And what difference does a definition make? Princeton, NJ: Robert Wood Johnson Foundation.
Bridge, J. A., L. Asti, L. M. Horowitz, J. B. Greenhouse, C. A. Fontanella, A. H. Sheftall, K. J. Kelleher, and J. V. Campo. 2015. Suicide trends among elementary school–aged children in the United States from 1993 to 2012. JAMA Pediatrics 169(7):673–677.
Brown, A. F., G. X. Ma, J. Miranda, E. Eng, D. Castille, T. Brockie, P. Jones, C. O. Airhihenbuwa, T. Farhat, L. Zhu, and C. Trinh-Shevrin. 2019. Structural interventions to reduce and eliminate health disparities. American Journal of Public Health 109(S1):S72–S78.
Camden Coalition. n.d. Camden core model . https://camdenhealth.org/care-interventions/camden-core-model (accessed November 4, 2020).
Canales, M. K., D. J. Drevdahl, and S. M. Kneipp. 2018. Letter to the editor: Public health nursing. Nursing Outlook 66(2):110–111.
Castrucci, B., and J. Auerbach. 2019. Meeting individual social needs falls short of addressing social determinants of health. Health Affairs Blog . doi: 10.1377/hblog20190115.234942.
CDC (Centers for Disease Control and Prevention). 2016. Health in all policies . https://www.cdc.gov/policy/hiap/index.html (accessed June 2, 2021).
CMS (Centers for Medicare & Medicaid Services). 2020. Z codes utilization among Medicare fee-for-service (FFS) beneficiaries in 2017. Baltimore, MD: Centers for Medicare & Medicaid Services Office of Minority Health.
Crippen, D., and F. Isasi. 2013. The untold story of 2013: Governors lead in health care transformation. Health Affairs Blog . https://www.healthaffairs.org/do/10.1377/hblog20131217.035878/full (accessed June 2, 2021).
Davies, N., and H. Donovan. 2016. National survey of commissioners’ and service planners’ views of public health nursing in the UK. Public Health 141:218–221.
Donley, R., and M. J. Flaherty. 2002. Revisiting the American Nurses Association’s first position on education for nurses. Online Journal of Issues in Nursing 7(2):2.
Duran, D., Y. Asada, J. Millum, and M. Gezmu. 2019. Harmonizing health disparities measurement. American Journal of Public Health 109(S1):S25–S27.
Dye, B. A., D. G. Duran, D. M. Murray, J. W. Creswell, P. Richard, T. Farhat, N. Breen, and M. M. Engelgau. 2019. The importance of evaluating health disparities research. American Journal of Public Health 109(S1):S34–S40.
Finkelstein, A., A. Zhou, S. Taubman, and J. Doyle. 2020. Health care hotspotting—A randomized, controlled trial. New England Journal of Medicine 382(2):152–162.
Fraze, T. K., A. L. Brewster, V. A. Lewis, L. B. Beidler, G. F. Murray, and C. H. Colla. 2019. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by us physician practices and hospitals. JAMA Network Open 2(9):e1911514.
Gawande, A. 2011 (January 24). The hot spotters . https://www.newyorker.com/magazine/2011/01/24/the-hot-spotters (accessed October 14, 2020).
Gottlieb, L. M., D. Hessler, D. Long, E. Laves, A. R. Burns, A. Amaya, P. Sweeney, C. Schudel, and N. E. Adler. 2016. Effects of social needs screening and in-person service navigation on child health: A randomized clinical trial. JAMA Pediatrics 170(11):e162521.
Green, S. R., V. Singh, and W. O’Byrne. 2010. Hope for New Jersey’s city hospitals: The Camden initiative. Perspectives in Health Information Management 7(Spring):1d.
Grubbs, S. S., B. N. Polite, J. Carney, Jr., W. Bowser, J. Rogers, N. Katurakes, P. Hess, and E. D. Paskett. 2013. Eliminating racial disparities in colorectal cancer in the real world: It took a village. Journal of Clinical Oncology 31(16):1928–1930.
Healthy Delaware. 2020. Welcome Consortium Members and Partners . https://www.healthydelaware.org/Consortium (accessed November 3, 2020).
Heath, S. 2018. 3 things to know to conduct a community health needs assessment . https://patientengagementhit.com/news/3-things-to-know-to-conduct-a-community-health-needs-assessment (accessed October 6, 2020).
IOM (Institute of Medicine). 2011. The future of nursing: Leading change, advancing health . Washington, DC: The National Academies Press.
IRS (Internal Revenue Service). 2020. Community health needs assessment for charitable hospital organizations-Section 501(r)(3) . https://www.irs.gov/charities-non-profits/community-health-needs-assessment-for-charitable-hospital-organizations-section-501r3 (accessed June 2, 2021).
Jones, N. L., N. Breen, R. Das, T. Farhat, and R. Palmer. 2019. Cross-cutting themes to advance the science of minority health and health disparities. American Journal of Public Health 109(S1):S21–S24.
Kangovi, S., N. Mitra, L. Norton, R. Harte, X. Zhao, T. Carter, D. Grande, and J. A. Long. 2018. Effect of community health worker support on clinical outcomes of low-income patients across primary care facilities: A randomized clinical trial. JAMA Internal Medicine 178(12):1635–1643.
Kangovi, S., N. Mitra, D. Grande, J. Long, and D. Asch. 2020. Evidence-based community health worker program addresses unmet social needs and generates positive return on investment. Health Affairs 39(2). doi: 10.1377/hlthaff.2019.00981.
Keller, L. O., S. Strohschein, M. A. Schaffer, and B. Lia-Hoagberg. 2004. Population-based public health interventions: Innovations in practice, teaching, and management. Part II. Public Health Nursing 21(5):469–487.
Krist, A. H., T. A. Wolff, D. E. Jonas, R. P. Harris, M. L. LeFevre, A. R. Kemper, C. M. Mangione, C.-W. Tseng, and D. C. Grossman. 2018. Update on the methods of the U.S. Preventive Services task force: Methods for understanding certainty and net benefit when making recommendations. American Journal of Preventive Medicine 54(1 Suppl 1):S11–S18.
Kulbok, P. A., E. Thatcher, E. Park, and P. S. Meszaros. 2012. Evolving public health nursing roles: Focus on community participatory health promotion and prevention. Online Journal of Issues in Nursing 17(2):1.
Lantz, P. M. 2019. The medicalization of population health: Who will stay upstream? Milbank Quarterly 97(1):36–39.
Larsen, R., J. Ashley, T. Ellens, R. Frauendienst, K. Jorgensen-Royce, and M. Zelenak. 2018. Development of a new graduate public health nurse residency program using the core competencies of public health nursing. Public Health Nursing 35(6):606–612.
Makelarski, J. A., E. Abramsohn, J. H. Benjamin, S. Du, and S. T. Lindau. 2017. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. American Journal of Public Health 107(11):1812–1817.
Mann, C. 2013. CMCS informational bulletin: Targeting Medicaid super-utilizers to decrease costs and improve quality. Baltimore, MD: Centers for Medicare & Medicaid Services.
Martsolf, G. R., T. Gordon, L. Warren May, D. Mason, C. Sullivan, and A. Villarruel. 2016. Innovative nursing care models and culture of health: Early evidence. Nursing Outlook 64(4):367–376.
Martsolf, G. R., D. J. Mason, J. Sloan, C. G. Sullivan, and A. M. Villarruel. 2017. Nurse-designed care models: What can they tell us about advancing a culture of health? Santa Monica, CA: RAND Corporation.
Mason, D. J., D. A. Jones, C. Roy, C. G. Sullivan, and L. J. Wood. 2015. Commonalities of nurse-designed models of health care. Nursing Outlook 63(5):540–553.
Minnesota Department of Health. 2019. Public health interventions: Applications for public health nursing practice , 2nd ed. St. Paul, MN: Minnesota Department of Health.
Minnesota Department of Health. n.d. Public health nurse orientation and resource guide . https://www.health.state.mn.us/communities/practice/ta/phnconsultants/guide-phn.html (accessed October 5, 2020).
Mullan, F. 2017. Social mission in health professions education: Beyond flexner. Journal of the American Medical Association 318(2):122–123.
NASEM (National Academies of Sciences, Engineering, and Medicine). 2016. Accounting for social risk factors in Medicare payment: Identifying social risk factors . Washington, DC: The National Academies Press.
NASEM. 2017a. Communities in action: Pathways to health equity . Washington, DC: The National Academies Press.
NASEM. 2017b. Global health and the future role of the United States . Washington, DC: The National Academies Press.
NASEM. 2019. Integrating social care into the delivery of health care: Moving upstream to improve the nation’s health . Washington, DC: The National Academies Press.
Noonan, K. 2020. Disappointing randomized controlled trial results show a way forward on complex care in Camden and beyond. Health Affairs Blog . doi: 10.1377/hblog20200102.864819.
Pittman, P. 2019. Rising to the challenge: Re-embracing the Wald model of nursing. American Journal of Nursing 119(7):46–52.
Rafferty, A. M. 2015 (January 27). Reinventing nursing’s social mission . Video. https://www.youtube.com/watch?v=8PjoiO8v-dE (accessed September 6, 2020).
Sadowski, L. S., R. A. Kee, T. J. VanderWeele, and D. Buchanan. 2009. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: A randomized trial. Journal of the American Medical Association 301(17):1771–1778.
Schaffer, M. A., L. O. Keller, and D. Reckinger. 2015. Public health nursing activities: Visible or invisible? Public Health Nursing 32(6):711–720.
Swider, S. M., P. F. Levin, and V. Reising. 2017. Evidence of public health nursing effectiveness: A realist review. Public Health Nursing 34(4):324–334.
Thomas-Henkel, C., and M. Schulman. 2017. Screening for social determinants of health in populations with complex needs: Implementation considerations. Trenton, NJ: Center for Health Care Strategies.
Tyson, T., C. J. Kenon, Jr., and K. Nance. 2018. Nursing at historically black colleges and universities. Journal of Professional Nursing 34(3):167–170.
Williams, D. R., and V. Purdie-Vaughns. 2016. Needed interventions to reduce racial/ethnic disparities in health. Journal of Health Politics, Policy and Law 41(4):627–651.
Williams, S. D., J. M. Phillips, and K. Koyama. 2018. Nurse advocacy: Adopting a health in all policies approach. Online Journal of Issues in Nursing 23(3).
Woolf, S. H., J. Q. Purnell, S. M. Simon, E. B. Zimmerman, G. J. Camberos, A. Haley, and R. P. Fields. 2015. Translating evidence into population health improvement: Strategies and barriers. Annual Review of Public Health 36(1):463–482.
This page intentionally left blank.
The decade ahead will test the nation's nearly 4 million nurses in new and complex ways. Nurses live and work at the intersection of health, education, and communities. Nurses work in a wide array of settings and practice at a range of professional levels. They are often the first and most frequent line of contact with people of all backgrounds and experiences seeking care and they represent the largest of the health care professions.
A nation cannot fully thrive until everyone - no matter who they are, where they live, or how much money they make - can live their healthiest possible life, and helping people live their healthiest life is and has always been the essential role of nurses. Nurses have a critical role to play in achieving the goal of health equity, but they need robust education, supportive work environments, and autonomy. Accordingly, at the request of the Robert Wood Johnson Foundation, on behalf of the National Academy of Medicine, an ad hoc committee under the auspices of the National Academies of Sciences, Engineering, and Medicine conducted a study aimed at envisioning and charting a path forward for the nursing profession to help reduce inequities in people's ability to achieve their full health potential. The ultimate goal is the achievement of health equity in the United States built on strengthened nursing capacity and expertise. By leveraging these attributes, nursing will help to create and contribute comprehensively to equitable public health and health care systems that are designed to work for everyone.
The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity explores how nurses can work to reduce health disparities and promote equity, while keeping costs at bay, utilizing technology, and maintaining patient and family-focused care into 2030. This work builds on the foundation set out by The Future of Nursing: Leading Change, Advancing Health (2011) report.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Jump to Cookie Consent
Help us improve your website experience! Take a brief survey >>
Visit the COVID Information Center >>

- MyChart Login
- Find a Location
Healthy Driven Blogs
Why nurses are the heart of healthcare.
If you’ve never been cared for by a nurse, you likely will be eventually.
Nurses are the foundation of healthcare. They play a vital role in providing care, comfort and compassion for their patients and patients’ families.
Despite their caring demeanor, nurses would rather not see you in the hospital. Preventive healthcare is their priority for patients — getting regular checkups and keeping health concerns from developing into a serious condition is key to avoiding the hospital, not to mention the intensive care unit.
"One of the biggest things is preventative healthcare," says Marguerite Manseau, RN , at Edward Hospital. “If your baseline overall health that has accumulated over 40 plus years is not good, a lot of the conditions people develop that land them in the hospital are not as easy to cure."
Many chronic conditions can be prevented by living a healthier lifestyle.
Also, stay on top of warning signs. "Listen to your body. If something doesn't feel right, get it checked out," says Marijana Vidovic, RN , at Elmhurst Hospital.
What it means to be a nurse
Being a nurse isn’t always easy. Nurses work hard. During the pandemic, and even before, nurses have experienced burnout. They emotionally invest in their patients and patients’ families, which can be exhausting during tough times. It’s even contributed to a national nurse shortage.
There are also times nurses need a thick skin. They can face heartbreaking situations, and it can be a stressful job. But nurses are realistic. Knowing what to expect and having the support of a team helps them get through stressful times.
"Having a level head is sometimes difficult. We're human and have emotions," Manseau says. "There are days you leave work and you're just so physically tired from not just how much physical work you've done but how much mental work. That accumulates over time.
"Being bombarded by anything and everything for 12 hours means nurses need to find healthy channels to get support and blow off steam so we avoid compassion fatigue."
Staying in the moment and maintaining perspective helps, the nurses say. Connection with the nursing team is also crucial for mental well-being, as nursing coworkers understand what each other is facing and can offer vital support.
The rewards
Becoming a nurse starts with nursing school. A good foundation in nursing school helps nurses understand and think critically about their duties.
Technology is involved in every aspect of a nurse’s day. From electronic records to the pharmacy and bedside technology, nurses need to know how it all works.
Nurses don’t just provide clinical care and medication, they provide emotional support for their patients and the patient’s family members, which is particularly important in the hospital where it helps to have a human connection during what is often a scary time.
Nurses work together and help coordinate care from physicians, physical therapists and others to do what's best for each patient. Working with the team is a rewarding part of the job, says Vidovic. Watching a patient walk out of the hospital after a lengthy hospitalization or being on a ventilator is also an amazing reward, they say.
Nurses are needed now more than ever
Nurses are in high demand, as the American healthcare industry faces a shortage of nurses. And it’s not just bedside nurses — there is so much you can do as a nurse beyond working in a hospital. You can become a teacher; you can become an APN. You can always expand your skills — specialize, do clinicals or teach. That's the beauty of a nursing degree.
"Really, if you think about your daily life, there's probably a nurse involved in some capacity at every step,” Manseau says. “Elementary school, there’s a nurse. You can work in an operating room. You can work at the bedside. You can teach. If you have a specific interest in something, you can find a program to get certified in it.”
Nurses are an unstoppable force. Providing care, comfort and compassion is all in a day’s work. In this Health 360 with Dr. G podcast episode, “Shout out to nurses: Heroes in healthcare,” host Mark Gomez, MD, and his guests discuss nurse life and the future of nursing. Listen to the podcast.
Edward-Elmhurst Health is hiring nurses! Learn more about nursing and search for nursing opportunities.
You may be interested in

Preparing for the “Big Game”

5 signs of a healthy relationship

Winter blues? How to boost your mood
If you have reached this screen, your current device or browser is unable to access the full Edward-Elmhurst Health Web site.
To see the full site, please upgrade your browser to the most recent version of Safari, Chrome, Firefox or Internet Explorer. If you cannot upgrade your browser, you can remain on this site.
This website uses cookies that measure website usage and help us give you the best experience. By continuing to use this website, you consent to this website’s use of these cookies and you accept and agree to our Privacy Statement and Terms of Use .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

The Exemplary Practice Life of the Nurse
Joan m. riley.
a Emmanuel College, Boston, MA 02115, United States of America
Judy A. Beal
b Simmons University, Boston, MA 02115, 27 Upton St. Unit 2, Boston, MA 02118, United States of America
Patricia Reid Ponte
c Boston College, Chestnut Hill, MA 02467, United States of America
Nurses consistently stand out in extraordinary ways especially during a global crisis, recently confirmed in the current Covid-19 pandemic. What is opportune this time is the call for clarity around what nurses do and what society can expect from them. Nurses, as members of a global profession, need a platform to build a contemporary practice life. This paper proposes the model: The Exemplary Practice Life of the Nurse . It provides a framework to explicate the essence of the role of the nurse. The model posits four inter-related essential components or pillars that ground a nurse's behavior and commitment: professionalism, leadership, scholarly practice, and stewardship. This uncomplicated, straightforward model is universally applicable for nurses to apply in whatever roles they hold and at any point in their careers. The use of a holistic model, as a guide across a full career trajectory, supports the nurse's ability to prioritize individual pillars while understanding the inter-relationship and influence among the four pillars. The authors pose assumptions that form the basis of the registered nurse role and provide the foundation for the exemplary practice life of the nurse. They make recommendations to nurses, the profession, the workplace, the academy, and the community.
Nurses have always been central to managing and abating health crises such as the recent COVID-19 pandemic health crisis. They will continue to be pivotal as the nation heals, all while the urgent need to reduce health disparities continues to soar. Nurses carried out their awe-inspiring and innovative work in hundreds of diverse roles and settings. They demonstrated true leadership in the most professional way ( Rushton & Thompson, 2020 ). This extraordinary contribution centers nurses in the midst of a “landmark” multi-year performance in every part of the globe. This truly was exemplary nursing practice at its best. This recognition amplifies the fact that nurses, as members of a global profession, require a common platform to build a contemporary exemplary practice life.
At the same time, the profession, while earning the designation as a major global workforce in the health care industry, continues to grapple with two key variables. The first is the slow transition within the United States for the BSN as the preferred degree for entry into the profession. The second is that practice roles are undergoing transformative changes in every part of the health care delivery system. As a result, nurses face extraordinary challenges to meet the emerging health care needs in a society that has experienced a long response to a global pandemic and faces significant health disparities. Nurses are positioned extraordinarily well to design innovative, and new models of care to respond to these challenges with a selfless commitment to remain true to the core work of the profession.
For eighteen years, the American public has acknowledged nursing as the most trusted profession in the United States ( Gallup, 2021 ; Reinhart, 2020 ). As the current COVID-19 pandemic has demonstrated, nursing is an essential profession whose members are highly valued, trusted, and respected. But the practice of nursing remains uneven – a reflection of wide variations in educational preparation, clinical expertise, and professional growth among its millions of individual clinicians. Nurses themselves often have difficulty articulating the essence of their practice. It is therefore not surprising that the public it serves has yet to fully grasp a consistent understanding of nursing's unique contributions to society much beyond nurses' uniform person-centered caring, comforting presence, reliable judgment, and technical expertise.
The protracted Covid-19 pandemic highlights the need to fully define what nurses do through the lens of what we, the authors, call the exemplary practice life for all nurses. Recently there have been calls that recognize the need to clearly describe the roles and expectations of nurses ( Godsey et al., 2020 ; Ulrich et al., 2020 ). We are proposing a universally applicable, compelling, straightforward conceptual model to explicate what nurses do. This model can guide nurses in their work, in whatever setting and in whatever the current stage of their careers. We believe that a universal holistic model is needed given the complexities of a global economy, the disparities embedded in the health care needs of society, the demand for expanded knowledge development, technological innovation, the pace of change in health care systems, and the public need to understand the work of nurses.
The aim of this paper is to describe a new holistic conceptual model that visually depicts what constitutes exemplary practice for a registered nurse formatively educated at the baccalaureate or master's entry level. To better understand exemplary professional nursing practice, we developed a model that describes such a person's essential attitude, behavior, and capability within the context of four independent, yet inter-related, pillars of: professionalism, scholarly practice, leadership, and stewardship. This model is named The Exemplary Practice Life of the Nurse . We define exemplary nursing practice as the best of the best of the art and science of nursing, and it represents the highest level of knowledge, expertise, and competence. While baccalaureate or master's entry graduates are prepared for an exemplary practice life, this evolves over a full career trajectory and is applicable across all professional nursing roles and practice settings.
Assumptions for an Exemplary Practice Life of the Nurse
The following are a set of assumptions that we believe underpin a framework for all nurse work, and as a result form the foundation of an exemplary practice life. These assumptions have been shaped by the history of the profession of nursing and are relevant to nurses in the present and for the future.
Assumption one
Society can expect that each nurse who has completed formative education at the baccalaureate or master ' s entry level will possess knowledge , attitude , behavior , and capability to care for all who need it regardless of setting .
The complexity of current practice environments requires critical thinking skills and a strong foundation in the art and science of nursing that are more completely developed during baccalaureate and master's entry level education. Society can expect that the knowledge, attitude, behavior, and the capability of a nurse will deepen over the course of a full career. Career advancement is tied to aspiration, experience, intent, formal education, and professional development. Optimal work settings support nurses throughout their careers to meet their developmental goals.
Assumption two
Society can expect each nurse to accept and value all persons as equal , worthy of respect and with intrinsic worth , regardless of all other considerations .
Nurses are formatively educated with a holistic and generalist framework that sets the background for a career that embraces diverse roles in diverse settings with and for diverse people, anywhere and in whatever roles to assure the public that healthcare is available for all. Furthermore, nurses are socialized to fulfill the expectation that a humanistic, individualized, person-centered approach to care uses social justice tenets as the foundation of interactions with others.
Assumption three
Society can uniformly expect each nurse to possess a set of role attributes and role functions that guide the scholarly work of all nurses .
Nurses use knowledge that prioritizes the ability to form therapeutic relationships; they appreciate the necessity to partner with people in their practice; they develop the capacity to teach; they are competent in the use of scientific knowledge and creativity to critically analyze phenomena and deliver evidence-based care. Nurses exert their capability to effectively collaborate with all stakeholders involved with the health and wellness of the public; they have been educated and socialized to be leaders in communities and within their practice settings. Nurses possess the ability to provide expert humanistic and holistic care to self and others that reflects kindness, compassion, respect, and mindfulness in their practice.
Assumption four
Society can expect that each nurse is adaptive to change and committed to the core tenets of professional practice regardless of the practice setting or role .
Working in complex environments that are constantly changing calls upon the nurse to understand the essence of the professional role. Leading change in formal and informal processes that result in improvements is a key role of the nurse and results in continuous learning by self and others. To best serve the health and wellness needs of society, the core of nursing's work centers on a strong collaboration with interdisciplinary partners and the people they serve. These collaborations often serve as natural laboratories for the design and implementation of dynamic innovations. Most importantly, nurses are committed to live and conduct practice with integrity, dignity and respect that includes a social, personal, and professional responsibility and accountability for one's actions as a member of the profession.
The model: The Exemplary Practice Life of the Nurse
In this model, the exemplary practice life of a nurse is illustrated as four essential pillars that provide a foundation for nurses as they evolve professionally. We envision this model as a holistic guide that affords the nurse the ability to prioritize individual pillars while always understanding the relationship and influence of pillars to each other and to the whole. There are four pillars in this model: professionalism, leadership, scholarly practice, and stewardship.
As shown in Fig. 1 , the four pillars in the model support the exemplary practice life of a nurse that, in turn, serves to advance the health and wellness of society. The placement of health and wellness of society represents the pinnacle to be achieved of in terms of exemplary practice. Its position as the highest point in the model serves to recognize the direct impact of an exemplary practice life of a nurse on society. The pillars link to a cross-directional arrow that represents the inter-related, yet independent, relationship among pillars. The model also illustrates the essential characteristics of each pillar. For example, the nurse exercises core responsibilities in professionalism when he or she invests in lifelong learning and self-care, accepts responsibility and accountability for the health and wellness of society, and comports with a strong professional identity. Each pillar of the model is subsequently explained in detail.

The Exemplary Practice Life of the Nurse .
In this model, the four core pillars rest on stakeholders. Stakeholders include individuals and groups who have an interest or an investment in supporting the exemplary practice life of the nurse and in turn the health and wellness of society. These include: the nursing profession (the body of individual nurses and professional associations/organizations, regulatory and credentialing bodies); education or the academy (colleges and universities that prepare nurses at the formative level); the workplaces (where nurses and inter-professional health care colleagues are employed); and the community (an essential part of society that shares common characteristics, aspirations, and challenges). These stakeholder groups are represented by the labels: Profession , Education , Workplace , and Community .
In the following sections, we describe each of the pillars and provide evidence for the choice of each in the model.
Professionalism
To understand professionalism as one of the pillars of an exemplary practice life of a nurse, we recognize the varied and rich history of nursing. Early historians noted that nursing's initial primary work centered on a sense of obligation to community through service of others ( Donahue, 1996 ). Over time, nurses, individually and collectively, engaged in societal struggle to address the need for equity ( Dock & Stewart, 1938 ). The term professionalism was rarely used in the literature prior to the 20th century. But what is informally described in the historical narratives are behaviors and characteristics used in the practice work of nurses during such times. The narratives connect the past to the present and offer guidance for the future.
Although controversial in the historical record, Florence Nightingale, with strong views about health and wellness and the unwillingness to accept the dictates of the politics of the day, brought professionalism into the lexicon of nurse work ( Donahue, 1996 ). She advocated for nurses to move beyond benevolence as the model of care to one where education preceded practice; where practice was a duty to society; where the character, values, passion for the care of the sick and their communities were frequently stated ideals for nurses. Nightingale recognized the importance of full nurse engagement, a positive approach to health promotion and informed decision making, and the pursuit of social justice as the bedrock of a professional life ( Beck, 2010 ; MacQueen, 2007 ; Wagner & Whaite, 2010 ;).
Two centuries later, the concept of professionalism continues as both multifaceted and complex.
Studies identify a wide range of dimensions, attributes and influences linked to the development of professionalism ( Ali et al., 2020 ; Garcia-Moyano et al., 2019 ; Ohlen & Segesten, 1998 ). The International Society for Professional Identity in Nursing (ISPIN) has committed its core work to developing the science to order to understand identity formation in nurses ( Godfrey, 2020 ; Joseph et al., 2021 ). Their work is grounded in a concept of professionalism that incorporates two distinct professional paradigms, social and psychological, into the nurse's professional identity ( Crigger & Godfrey, 2014 ).
Nurses often express the view that professionalism is easier for them to describe as situationally related actions than to define as a complete set of behaviors. There is no universally accepted definition of professionalism. This fact is not surprising given the complexity of the concept. Johnson (2015) reported counting sixty words or concepts in an informal review of the term professionalism. Regardless, professionalism remains a personally important concept for nurses. To explain its meaning, one needs to begin with the fact that no one is born a professional. Rather, it is an intentional process of development that begins in formative education, transitions into the workplace, and continues through the major stages of a nurse's career. “Developing and nurturing professionalism in nursing takes time, authentic presence of leaders, engagement of colleagues and somehow creating a feel of value in the contribution of each nurse, from the bedside to the boardroom” (p. 266, Leclerc, 2017 ). Professionalism is a purposively evolving mode of thinking and acting ( Johnson, 2015 ).
There is recognition that professionalism requires the individual nurse to act as the fully accountable agent of professional responsibility, throughout their career. Stakeholders, who are invested in the practice life of the nurse, are also recognized as important influencers because they support the development and promotion of conditions that are conducive to sustaining professionalism ( American Nurses Association, 2014 ). Professionalism offers a covenant with society as to what attitude, behavior, and process govern the work of nurses no matter where they practice and whatever their practice role.
As such, we posit that professionalism is a multidimensional lived experience that includes a combination of characteristics, values, conduct and actions. Professionalism includes identity formation, comportment, acceptance and accountability for professional responsibilities and expectations. Reflection, the need to form a therapeutic relationship integral to the caring relationship, passion for the work of a scholarly practice, as well as civic and social responsibility further define the understanding of professionalism. Nurses prioritize being available for others: for people, patients and families, colleagues, peers, workplace, and communities.
Professionalism informs the blueprint for educational programs, statements of workplace expectations and signposts for the nurse to incorporate into the other pillars of an exemplary practice life of the nurse. The newly approved AACN Essentials details the domain of Professionalism with its related descriptors, contextual statements, and competencies to be achieved during formative education ( AACN, 2021 ). Professionalism, in all its dimensions, clearly is an essential pillar of an exemplary practice life of the nurse.
Scholarly practice
Scholarly practice has consistently been part of the discussion surrounding the essential components of nursing practice. Since 1922, Sigma Theta Tau, the International Nursing Honor Society has recognized and promoted nursing scholarship as one of its major tenets ( Sigma Theta Tau, 2020 ). Carper's (1978) seminal work formulated what she coined “nurses' patterns of knowing” which set the foundation for scholarly practice. Benner's model From Novice to Expert further advanced this discussion as an explanation of how knowledge and skills are acquired and applied to nursing practice ( Benner, 1982 , Benner, 1984 ). While the dialogue on how to define scholarly practice continues to evolve, the message of its importance to the profession and to quality patient care outcomes remains consistently strong. Riley et al. (2002) , described a universal holistic model of scholarly nursing practice consisting of the scholarship of knowing teaching, practice, and service. This model evolved later to include the role attributes of “who I am” and “what I do” ( Riley et al., 2008 ). Participants ( N = 36) in this qualitative study shared that they think of themselves as: 1) available for others, 2) active learners, 3) out of the box thinkers, 4) passionate about nursing, and 5) confident. They carry these values while leading, caring, sharing knowledge, and being self-reflective. We believe that scholarly practice includes the characteristics of developing new knowledge, improving practice, basing practice decisions on evidence, designing, and implementing innovative practices, using creative approaches to individualize the needs of the people we serve, and advancing system-wide priorities and initiatives.
There is professional consensus that formative nursing education programs have the responsibility to prepare their graduates for a scholarly practice. The competencies attained by baccalaureate and master's entry prepared nurses within their formative education are driven by the National League for Nursing (NLN) and the American Association of Colleges of Nursing (AACN). These competencies set the stage for a lifetime of scholarly practice. The National League for Nursing (2021) identifies four core competencies for all graduates of all formative educational programs, two of which support the expectation of scholarly practice. These include the spirit of inquiry and nursing judgment both of which prepare graduates for a “practice that is informed by a body of knowledge and ensures that all members of the public receive safe, quality care” ( NLN, 2021 ). The approved 2021 AACN Essentials ( AACN, 2021 ) labels this competency as ‘Scholarship for the Nursing Discipline’ and defines it as “the generation, synthesis, translation, application and dissemination of nursing knowledge to improve health and transform health care” p.11. The related sub-competencies include: advancing the scholarship of nursing; integrating best evidence and promoting the ethical conduct of scholarly activities.
After completing formative education at the baccalaureate or master's entry level, nurses, in partnership with the workplace and other stakeholders, assume responsibility for building on the foundation for scholarly practice competency attained in nursing education. As nurses transition into practice settings across a diverse and complex healthcare system, it is imperative that practice settings, in partnership with individual nurses and professional associations, fully support and help shape, evolve, and make a commitment to implementation of scholarly practice. Organizational credentialing bodies such as the American Nurses Credentialing Center (ANCC) and others promote the development of scholarly practice through a culture of individual and organizational scholarly practice. ANCC's include the ANCC Magnet Recognition Program, The ANCC Pathway to Excellence Program and The Practice Transition Accreditation Program (PTAP). While not all health care organizations are magnet designated, we believe that each individual nurse must commit to scholarly practice wherever they practice.
Scholarly practice is as much about attitude as it is about using a systematic approach to plan and deliver care and conduct other work of professional nurses. This attitude or mindset includes a commitment to systematic inquiry with the following questions in mind: How can we do this better? What does the evidence at all levels tell us? How can we do this in a way that meets the needs of this particular person or groups of people? How can what we learn be applied to broader groups of people within society served in a variety of contexts?
We believe that all nurses are capable of engaging in a scholarly practice. This capacity matures throughout a nurse's career. Nurses and the public have been socialized to think of scholars as educators and researchers employed by colleges and universities. According to Broome (2021) , “Despite our own internal conversations, the public does not think of us as scholars and scientists…” p. 250. Because of this prevailing belief, many nurses have been reluctant to embrace themselves as practice scholars and capable of scholarly practice. Nurses, however, do think of themselves as highly creative, resilient, and accountable for seeking information, and scientific and aesthetic evidence to help formulate their plans, decisions, and actions.
Nurses with a scholarly practice prioritize learning; they know the people they care for; they believe that knowledge is ever evolving. Nurses recognize that, for them to be at their best, they need to continually learn in formal and informal ways. They collaborate and partner with others including the people they serve to find solutions to healthcare and societal challenges. This is scholarly practice!
As such, nurses with a scholarly practice accept responsibility for implementing and disseminating new knowledge for the advancement of the health and wellness of society. This important process occurs in the clinical care setting, in the classroom, in the conduct of research, in whatever setting and role the nurse holds. Scholarly practice with its direct connection to the health and wellness of society is an essential pillar of an exemplary practice life of the nurse.
The early literature on leadership was primarily driven by leaders and scholars from the world of business ( Kouzes and Posner, 2003 ). More recently, other professional disciplines including nursing have joined in the development and analysis of the theories and practice of leadership. There remains considerable debate about what leadership really is and how it differs from management. As a result, there is a plethora of definitions of leadership from both within and outside nursing. Diers (2004) , in one of her classic editorials, wrote that leadership is viewed as multi-dimensional, encompassing the wise use of power, managerial functions, and human relations processes. We believe that leadership is a set of actions and behaviors used by individuals or groups of individuals within their environment that facilitates the establishment and acquisition/achievement of shared goals ( MA Department of Higher Education, 2016 ).
The following review of the literature centers on understanding leadership and its expected behaviors. From the world of business, Kouzes and Posner have been writing about exemplary leadership since 2003. In their seminal work, they define essential leadership practices that are important to promoting growth of an individual and an organization. This definition includes engaging and empowering all members in the organization to establish sustainable outcomes intentionally and collaboratively. They describe five leadership practices: 1) ‘modeling the way’, 2) ‘inspiring a shared vision’, 3) ‘challenging the process’, 4) ‘enabling others to act’, and 5) ‘encouraging the heart’. While ‘encouraging the heart’ has not typically been viewed as a leadership competency, executive coach Daskell (2017) wrote that love is a leadership competency. By leading with compassion, commitment, kindness, and competence one can motivate others toward achieving greatness.
The long running and highly effective Robert Wood Johnson Executive Nurse Fellows Program (1997–2017) identified core competencies for nurse leaders ( Bellack & Morjikian, 2005 ). These include:
- • Self - knowledge , or self - awareness is the ability to understand and develop oneself in the context of organizational challenges, interpersonal demands, and individual motivation.
- • Strategic Visioning is the ability to connect broad social, economic, and political changes to the strategic direction of organizations. Strategic nurse leaders are always thinking about the next step.
- • Risk - taking and Creativity is the ability to transform both oneself and the organization by moving outside the traditional and patterned ways of success. A leader who is a risk taker often feels uncomfortable and learns to accept this discomfort.
- • Interpersonal and Communication Effectiveness is the ability to translate a strategic vision into compelling and motivating messages. Great leaders care about people with whom they work. They stay on mission but are always listening to divergent voices.
- • Inspiring and Leading Change is the ability to inspire, structure, lead and effectively implement organizational change in an inclusive way. Great nurse leaders lead from their values. Their personal integrity and moral courage are the cornerstones of their legacies.
While the RWJ program was a formal program directed toward nurses aspiring to advance in their leadership roles, we believe that these five constructs are applicable to leadership development of all nurses, regardless of title or work setting.
Leadership identity has typically been associated with a hierarchical, authoritative, and formal position ( deZuleuta, 2015 ; Van de Mieroop et al., 2020 ). However, there is support in the nursing literature for the importance of informal leadership where the leader may not have a formal titular position or authority over a group of individuals. Informal leadership roles are exercised by those individuals who are situationally willing to step up and take actions; they are the “go-to nurses” ( Clifton, 2014 , p. 68). Within the culture of workplace organizations, an informal leader has been described as anyone who directs/guides a group toward accomplishing desired outcomes ( Ross, 2014 ). Nurses, who engage in scholarly practice throughout the healthcare enterprise, assume informal leadership roles in acknowledged and unacknowledged ways.
Riley et al. (2008) in their study that explored perspectives of thirty- six experienced nurses' descriptions of their scholarly nursing practice, found that participants' perspectives of leadership differed from more traditional views of formal leadership. Participants spoke to a non-hierarchical approach to leadership that they repeatedly called “stepping up the plate over and over again to guarantee the highest level of care…to develop others and to advance practice” (pg. 431). Informal leadership was their expectation for their exemplary practice life. We believe that informal leadership needs to not only be further developed and supported but included in the performance expectations for every nurse in every workplace.
Based on experience, research, and a synthesis of the literature, we believe that all nurses educated at the baccalaureate or master's entry level are prepared to be leaders. Whether in informal or formal leadership positions, nurses are held to the following expectations: developing oneself and others; embracing cultural humility, inclusivity, and diversity; modeling professional practice and behavior with a non-hierarchical approach; communicating with colleagues and others with clarity and purpose; managing resources effectively; and collaborating with others to advance the practice and profession of nursing and health care for the benefit of society. Nurses as leaders are reflective, visionary, and strategic thinkers who feel comfortable taking risks and innovating in even the most challenging situations ( Bellack & Morjikian, 2005 ).
We believe that both the formal and informal nurse leader is obligated to advance oneself, others, and the profession with humility, inclusivity, and generosity of spirit. Whatever the role, a nurse leader has the ability to influence others and build consensus toward a mutually shared goal or decision on both the micro and macro level. For example, the nurse leader has the responsibility to advocate for advancing health equity for all by removing practice barriers and supporting nurses in their efforts to understand the impact of the social determinants of health ( NASEM, 2021 ). For these many reasons, leadership is one of the four pillars that supports the exemplary practice life of the nurse.
Stewardship
Identifying stewardship as one of the four pillars supporting the exemplary practice life of the nurse is both timely and necessary. Nursing is charged with preparing for its future while living in the present. All nurses are called upon to assume a stewardship responsibility for the conservation of the ideals of nursing while leading consequential changes in health care environments that impact the health and wellness of society.
The concept of stewardship, outside the boundaries of a profession, has a long history. When the word stewardship first appeared in the English language during the Middle Ages, it functioned as a job description, denoting the office of a steward , or manager of a large household ( Merriam-Webster, 2020 ). Over the centuries, the understanding of stewardship expanded to include the oversight by the courts and many organizations. In recent years, the long-established “management” sense of stewardship has evolved into a positive meaning emphasizing “careful and responsible management” ( Merriam-Webster, 2020 ). The historical evolution of stewardship carries forward a set of ideals that include duties, shared responsibilities, oversight, resource preservation, prudence, and advocacy into a modern era.
Twenty first century stewardship ideals are addressed in business as integrated leader behaviors that place long term best interests of the business entity and stakeholders over self-interest ( Hernandez, 2008 ; Hernandez, 2012 ). Leaders, committed to their role as steward, see the benefit of this scope of social responsibility to their workforce and to society. Hernandez (2012) calls stewardship behaviors a “type of prosocial action” that carries with it a positive effect on people. Although primarily associated within a formal leadership role, there is current recognition that stewardship can and should live in all levels of organizations, adopted by all individuals, regardless of positional power ( Dalcher, 2019 ).
In a traditional view of stewardship, nurse leaders and scholars are entrusted to preserve and hold in trust the value priorities of stakeholders ( Milton, 2014 ). According to Haase-Herrick (2005) the simple essence of the diversity of stewardship actions for nurse leaders is grounded in the imperative to leave a profession, discipline, and scholarly practice in a better place than where it was found. This imperative does not apply only to nurses who are in formal leadership or scholar roles.
In broadening the responsibility of stewardship to include all nurses, the exercise of stewardship actions becomes a transformative experience that assures transparency and accountability for conserving what is essential in the profession and beneficial to society. With a more inclusive view of stewardship, all nurses, as stewards of the profession, exercise their responsibility to preserve what is intrinsically good and valuable in the profession, while promoting what knowledge and practice benefits the health of society ( Murphy, 2009 ; Murphy & Roberts, 2008 ).
Stewardship is not a one size fits all paradigm. Nurses are advocates at the point of practice or wherever they do their work. The consistent outcome of their advocacy is to preserve the core values of a practice profession while embracing practice changes that improve experience and outcomes of care. For educators, curricular learning opportunities that reinforce the expectations and responsibilities of being a steward of the profession begin to emerge at the point of formation of future nurses. For leaders of the profession, opportunities emerge at the nexus of transforming practice environments to meet society's current and future health needs. For researchers, stewardship implies a commitment to use their requisite abilities and curiosity to delve into the study of core nursing phenomena that address health issues that burden society. Being a steward of the profession stems from a nurse's passion and a sense of responsibility to advance the profession's work.
In a national study of chief academic nursing officers ( Beal & Riley, 2015 ), participants shared that they believed that every nurse, regardless of role or practice setting, is a steward of the nursing profession and of scholarly practice. Participants' collective vision for the future of baccalaureate education was that educational programs would place more focus on “helping students think about themselves as members and future stewards of the profession” ( Beal & Riley, 2015 , p. 382). In a recent national study, senior nurse leaders in magnet hospitals confirmed that “nursing culture is both significant and consequential to the nursing milieu as well as the overall organization” ( Beal & Riley, 2019 , p.192). Embedding expectations of stewardship for all nurses, not just leaders, into the nursing culture of health systems adds potential for significant influence within the organization.
The key question then becomes: Who is responsible for stewardship of the profession? We believe the expectation for stewardship must be expanded to include a responsibility for all nurses, operationalized in different ways, across the lifetime of a career. This expectation broadens meaningful actions to include sharing knowledge with others, mentoring, and teaching, using knowledge of the business of healthcare to specifically impact health policy, regulation, ethical and financial decisions. These are actions that support the essence of the profession. As a touchstone for both preservation and change, stewardship in today's health care enterprise, leads to a wide range of critical opportunities for all nurses. We therefore believe that this expanded stewardship paradigm earns its placement as a supporting pillar for the exemplary practice life of a nurse. The legacy of stewardship is a future workforce that is comfortable with their professional heritage yet sensitively responsive to the changing healthcare needs of society.
Summary of the model
The holistic model The Exemplary Practice Life of the Nurse calls for nurses to commit to developing an exemplary practice throughout one's career. Table 1 : Core Commitments with the Holistic Model: Exemplary Practice Life of the Nurse summarizes the essential attitudes, behaviors, and capabilities within the context of the four independent but inter-related pillars.
Core commitments with the holistic model: exemplary practice life of the nurse.
| Professionalism | |
| Scholarly practice | |
| Leadership | |
| Stewardship |
The proposed model emanates from nursing's historical roots, respectful of its past while positing perspectives to guide the profession to meet current and future societal needs. Understanding the relationship between and among pillars represents the essence of an exemplary practice life. A holistic model adds equipoise in the components of nurse work. The model allows for counterbalancing the essential components while offering guidance to nurses in the whatever the situation that they confront in meeting the universally stated goal of health and wellness of all members of society. Because of the nature of their work, nurses need a holistic model to serve as foundational to their practice life. Such a model transcends all roles and work-settings and offers stability within an ever-changing health care environment. An unexpected benefit could be that the society will more clearly understand the essential elements of a nurse's practice life.
Each of the four pillars of this model has been separately described in the literature. What was not discussed in the literature was the inter-relationship of these four essential pillars to each other and how, as independent but inter-related entities, they holistically support the exemplary practice life of the nurse. The importance and value of informal leadership has also been overlooked. Three pillars (Professionalism, Leadership, and Scholarly Practice) are incorporated into competencies that drive formative education, advanced education, and workplace norms. Their relationship to each other, within these systems, however, is not well articulated within the competencies. Historically, stewardship, the fourth pillar, has been assigned and well-described for executive levels of leadership but not addressed as a responsibility for all nurses. There has been a recent call to make stewardship an explicit component of PhD education programs ( Morris et al., 2021 ). While important, the call must be expanded to include educating all students to be stewards of the profession.
We fully acknowledge the significant contributions of the academy and professional organizations over decades of dedication to the advancement of nursing education ( AACN, 2021 ; NLN, 2021 ). We recognize that they have a long-standing commitment to the development of specific essential competencies and principles for educating nurses. Faculty have developed curricula guided by the professional educational standards of these organizations. The complexity of today's nursing curricula calls for a simple, concise, and holistic translation the nursing competencies for each student and nurse to internalize what it means to have an exemplary practice life. We believe that this is the ultimate goal of nursing education at the baccalaureate and master's entry levels. To accomplish this translation, and at the same time provide a seamless transition to practice, faculty should integrate and emphasize the four pillars of this proposed model into teaching/learning experiences throughout the curriculum. The model offers a pragmatic framework to guide and support a nurse's practice life. Currently we know of no model or framework that captures the essence of exemplary practice life in a simple, concise, and holistic manner.
We introduced this paper with the important recognition that society once again acknowledges nursing as the most trusted profession in the United States ( Gallup, 2021 ; Reinhart, 2020 ). Globally, the International Year of the Nurse and Midwife continues to link the exemplary life of the nurse with stories of contemporary exemplary practice. At the same time, there are reports in recent literature about three distinct but related calls for nurses and the profession that are discussed in the following paragraphs: 1. The need to claim an authoritative role as leaders in health care services; 2. The need to claim a complete and accurate professional image for nurses; 3. The need to reclaim values foundational to the profession.
While nurses are clearly viewed as trustworthy, we are not perceived by the public as leaders, scholars, or innovators who make major contributions to healthcare delivery ( American Nurses Association, American Organization of Nurse Leaders, Johnson and Johnson, 2020 ; Broome, 2021 ; Prybil et al., 2019 ). The study findings of Godsey et al. (2020) address the need for change in the brand image of the nurse. These findings report factors contributing to the inconsistent and often negative image of nursing. They posit that variability in educational preparation, lack of visionary leadership, lack of leadership development, and an inconsistent professional image are significant contributors to the inability of the profession to demonstrate full leadership throughout the healthcare system.
The 2020–21 Covid-19 pandemic exposed fractures and vulnerabilities in our health care delivery system ( Ulrich et al., 2020 ) that include oppressive and discriminatory structures that are embedded in the organizations in which nurses work ( NASEM, 2021 ). These papers call for the need for nurses to step forward to lead substantive institutional reform. This will require an increased emphasis on supporting nurses in these endeavors ( NASEM, 2021 ). This call is an urgent message to see, as one endpoint in the pandemic, an opportunity to reclaim “values foundational to our profession and to establish new norms of communication and teamwork, intentionally address [ing] disparities” (p. 843, Ulrich et al., 2020 ).
These calls offer some insights that are germane to the proposed model. The Exemplary Practice Life of the Nurse is a simple yet compelling description of the essential work of every nurse integrated into four inter-related pillars. The model answers the calls for a strong professional image and compelling leadership that embrace the foundational values of the profession. It is consequential for formative education at the baccalaureate and master's entry level education. Most importantly the model acknowledges a consistent universal recognition of what nurses do in all roles, in all work-settings and within our global society. This model can be part of the solution of clearly describing the important work of nurses.
Recommendations
Proposing the model.
The Exemplary Practice Life of the Nurse , in conjunction with the greatest public health crisis since the 1918 flu epidemic, provided an opportunity to reflect on the rich past, the present, and the emerging future or our profession. Guided by this perspective we provide recommendations for the use of this model for individual nurses, the workplace, the academy, the profession, and the community. Specifically;
- • We ask all nurses to consider re-framing their practice life to include the inter-related pillars of professionalism, scholarly practice, leadership, and stewardship. We recognize that the implementation of this model may look different at specific stages of a nurse's career.
- • We ask that workplace leaders commit to examining and integrating this model as a mechanism to support all nurses throughout early, mid, and late career phases. We ask them to consider the integration of the model in systematic performance evaluation matrices that foster an exemplary practice environment.
- • For the academy, we ask that leaders commit to conducting a systematic curricular appraisal to ensure that the model components are equally integrated throughout educational formation. Formative clinical learning needs to shift from a predominately skill acquisition model to a model that recognizes a more equitable distribution of the four essential pillars as the foundation for developing an exemplary nurse. Accomplishing the integration of this model into the curriculum is the first step in preparing the nurse of the future.
- • We ask the leaders of professional associations to use their collective voice to advocate for the privilege of all nurses to have an exemplary practice life. The right of all members of society to have their health and wellness needs met equally requires no less than all nurses having an exemplary practice life. Furthermore, we ask that professional associations work collaboratively with certification, accreditation, legislative and regulatory bodies to commit to advancing the BSN as the preferred professional nursing degree. While efforts have been made in the past, there is a greater sense of urgency as the complexity of care continues to increase.
- • For communities, we recognize their position as a guardian and supporter of society's health and wellness needs. We ask for continued support in new and emerging ways that reflect the conditions, commitments, changes, and requirements that must be confronted.
In conclusion, we ask service and academic leaders, and individual nurses, as partners, to review, implement and evaluate this model to seamlessly support career transition and the development of an exemplary practice life for all nurses.
- Ali A., Anakin M., Tweed M., Wilkinson T. Towards a definition of distinction in professionalism. Teaching and Learning in Medicine. 2020; 32 (2):126–138. doi: 10.1080/10401332.2019.1705826. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- American Association of Colleges of Nursing (2021). The Essentials: Core Competencies for Professional Nursing Education. Accessed 6.21.21 aacnnursing.org/Portals/42/AcademicNursing/pdf/Essentials-2021.pdf .
- American Nurses Association (2014). Professional Role Competency. Accessed 1.8.21 at https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-statements/id/professional-role-competence/ .
- American Nurses Association, American Organization of Nurse Leaders, Johnson and Johnson, (2020). The Impact of COVID-19 on the Nursing Profession in the U.S: 2020 Quantitative Survey Summary. https://kentucky-nurses.nursingnetwork.com/nursing-news/183228-ana-aonl-and-johnson-johnson-release-the-impact-of-covid-19-on-the-nursing-profession-in-the-u-s-2020-quantitative-survey-summary-white-paper .
- Beal J., Riley J. The development of a clinical nurse scholar in baccalaureate education. Journal of Professional Nursing. 2015; 31 (5):379–387. doi: 10.1016/j.profnurs.2015.03.005. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beal J., Riley J. Best organizational practices that foster scholarly nursing practice in magnet hospitals. Journal of Professional Nursing. 2019; 35 (3):187–194. doi: 10.1016/j.profnurs.2019.01.001. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Beck D. Remembering Florence Nightingale’s panorama. Journal of Holistic Nursing. 2010; 28 (4):291–301. doi: 10.1177/0898010109354519/. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bellack J.P., Morjikian R.L. The RWJ executive nurse fellows’ program, part 2. Journal of Nursing Administration. 2005; 35 (12):533–540. [ PubMed ] [ Google Scholar ]
- Benner P. From novice to expert. American Journal of Nursing. 1982; 82 (3):402–407. [ PubMed ] [ Google Scholar ]
- Benner P. Pearson; Menlo Park: 1984. From novice to expert: Excellence and power in clinical nursing practice. [ Google Scholar ]
- Broome M. Dialogue and debate: The soul of scholarship. Nursing Outlook. 2021; 69 :249–250. doi: 10.1016/j.outlook.2021.03.013. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carper B. Fundamental patterns of knowing in nursing. Advances in Nursing Science. 1978; 1 (1):13–23. doi: 10.1097/00012272-197810000-00004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clifton C.A. The benefits of informal leadership. Nurse Leader. 2014;(October 2014) [ Google Scholar ]
- Crigger N., Godfrey N. From the inside out: A new approach to teaching professional identity formation and professional ethics. Journal of Professional Nursing. 2014; 30 (5):376–382. doi: 10.10161/j.profnurs.2014.03.004. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dalcher, D. (2019). Taking responsibility for our actions: The return of stewardship. PM World Journal, VIII (VII), 1-11s.
- Daskell L. The leadership gap: What gets between you and your greatness. NY: Portfolio/Penguin. Accessed 2.1.21 at. 2017. https://www.lollydaskal.com/leadership/love-is-a-leadership-competency/
- deZuleuta P.C. Developing compassionate leadership in healthcare: An integrative review. Journal of Healthcare Leadership. 2015 doi: 10.2147/JHL.S93724. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Diers D. Jones and Bartlett, Inc; London: 2004. Speaking of nursing: Narratives of practice, research, policy and the and the profession. [ Google Scholar ]
- Dock, L.L., & Stewart, I.M. (1938). A short history of nursing, ed. 4. New York: GP Putnam's Sons.
- Donahue M.P. 2nd ed. Mosby-Year Book, Inc.; St. Louis: 1996. Nursing the finest art. [ Google Scholar ]
- Gallup (2021). America trusts the most trusted profession more than ever. Accessed 1.8.21 at https://dailynurse.com/gallup-2020-america-trusts-the-most-trusted-profession-more-than-ever/ https://dailynurse.com/gallup-2020-america-trusts-the-most-trusted-profession-more-than-ever/ .
- Garcia-Moyano, L., Altisent, R., Pellicer-Garcia, B., Guerrero-Portillo, S., Arrazola-Alberdi, O., Delgade-Marroquin, M (2019). A concept analysis of professional commitment in nursing. Nursing Ethics, 26(3), 778–797. doi: 10.1177/0969733017720847. [ PubMed ] [ CrossRef ]
- Godfrey N. How to think/act/feel like a nurse: Forming a professional identity in nursing. Deans Notes. 2020; 41 (4):1–3. [ Google Scholar ]
- Godsey J.A., Houghton D.M., Hayes T. Registered nurse perception of factors contributing to the inconsistent brand image of the nursing profession. Nursing Outlook. 2020; 68 (6):808–821. doi: 10.1016/j.outlook.2020.06.005. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Haase-Herrick K.S. The opportunities of stewardship. Nursing Administration Quarterly. 2005; 29 (2):115–118. [ PubMed ] [ Google Scholar ]
- Hernandez M. Promoting stewardship behavior in organizations: A leadership model. Journal of Business Ethics. 2008; 80 :121–128. doi: 10.1007/s10551-007-9440-2. [ CrossRef ] [ Google Scholar ]
- Hernandez M. Toward an understanding of the psychology of stewardship. Academy of Management Review. 2012; 37 (2):172–183. doi: 10.5465/amr.2010.0363. [ CrossRef ] [ Google Scholar ]
- Johnson J.A. Nursing professionalism: Innate, taught, or caught? Journal for Nurses in Professional Development. 2015; 31 (2):114–115. doi: 10.1097/NND.0000000000000149. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Joseph, M.L., Phillips, B.C., Edmonson, C., Godfrey, N., Liebit, D., & Weybrew, K. (2021). The nurse leader's role: A conduit for professional identity formation and sustainability. Nurse Leader, 19 (1), 27–31.
- Kouzes J.M., Posner B.Z. CA: Jossey-Bass Publishers; San Francisco: 2003. Exemplary leadership. [ Google Scholar ]
- Leclerc L. The journey of 10,000 miles begins with 1 step. Nurse Leader. 2017;(August):266–270. doi: 10.1016/j.mnl.2017.03.01524. [ CrossRef ] [ Google Scholar ]
- MA Department of Higher Education (2016). Massachusetts nurse of the future core competencies. Accessed 1/16/21 at mass.edu/nahi/documents/NOFRNCompetencies-upadated-March2016.pdf.
- MacQueen J.S. Florence nightingale’s nursing practice. Nursing History Review. 2007; 15 :29–47. [ PubMed ] [ Google Scholar ]
- Merriam-Webster.com Dictionary, (2020). Merriam-Webster, https://marriam-webster.com/dictionary/stewardship . Access 12/28/20.
- Milton, Constance. (2014). Stewardship and leadership in nursing. Nursing Science Quarterly, 27 (2), 108–110. http://doi.org/10.117/089431841452261. [ PubMed ]
- Morris N.S., Wassef M.E., Sullivan-Bolyai S., Bova C., Kane A. Making explicit the development of PhD-prepared nurses to steward the discipline. Nursing Outlook. 2021; 69 (1):50–56. doi: 10.1016/j.outlook.2020.08.002. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Murphy N., Roberts D. Nurse leaders as stewards at the point of service. Nursing Ethics. 2008; 15 (2):243–253. [ PubMed ] [ Google Scholar ]
- Murphy N.S. Nurse leaders as stewards: The beginning of change. The Open Journal of Nursing. 2009; 3 :39–44. doi: 10.2174/1874434600903010039. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Academies of Sciences, Engineering and Medicine, 2021. The future of nursing 2020-2030: Charting a path to achieve health equity. Washington, DC: The National Academies Press. 10.17226/25982 . [ PubMed ]
- National League for Nursing. (2021). NLN competencies for graduates of nursing programs. Accessed 3.3.21 at http://www.nln.org/professional-development-programs/competencies-for-nursing-education/nln-competencies-for-graduates-of-nursing-programs .
- Ohlen J., Segesten K. The professional identity formation of the nurse: Concept analysis and development. Journal of Professional Nursing. 1998; 28 (4):720–727. [ PubMed ] [ Google Scholar ]
- Prybil L.D., Popa G.J., Warshawsky N.E., Sundean L.J. Building the case for including nurse leaders on healthcare organization boards. Nursing Economics. 2019; 37 (4):169–177. (197) [ Google Scholar ]
- Reinhart R.J. Nurses continue to rate highest in honesty, ethics. Politics. 2020 https://news.gallup.com/poll/274673/nurses-continue-rate-highest-honesty-ethics.aspx Accessed at. [ Google Scholar ]
- Riley J., Beal J., Lancaster D. Scholarly nursing practice from the perspectives of experienced nurses. Journal of Advanced Nursing. 2008; 61 (4):425–435. [ PubMed ] [ Google Scholar ]
- Riley J., Beal J., Levi P., McCausland M. Revisioning nursing scholarship. Journal of Nursing Scholarship. 2002; 34 (2):383–390. [ PubMed ] [ Google Scholar ]
- Ross, C.A. (2014). The benefits of informal leadership. Nurse Leader, 12(5). https://doi.org/10.1016 jmnl.2014.01.015.
- Rushton C.H., Thompson L. Moral outrage: Promise or peril? Nursing Outlook. 2020; 68 (5):536–538. doi: 10.1016/j.outlook.2020.07.006. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sigma Theta Tau International (2020). Sigma organizational fact sheet. Accessed 1.8.21 at https://www.sigmanursing.org/why-sigma/about-sigma/sigma-organizational-fact-sheet .
- Ulrich C.M., Rushton C.H., Grady C. Nurses confronting the coronavirus: Challenges met and lessons learned thus far. Nursing Outlook. 2020; 68 (6):838–844. doi: 10.1016/j.outlook.2020.08.018. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Van de Mieroop D., Clifton J., Verhelst A. Investigating the interplay between formal and informal leaders in a shared leadership configuration: A multi-modal conversation analytical study. Human Relations. 2020; 73 (4):490–515. doi: 10.1177/0018726719895077. [ CrossRef ] [ Google Scholar ]
- Wagner D., Whaite B. An exploration of the nature of caring relationships in the Writings of Florence Nightingale. Journal of Holistic Nursing. 2010; 28 (4):225–234. doi: 10.1177/0898010110386609. [ PubMed ] [ CrossRef ] [ Google Scholar ]
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Aiken LH, Sloane DM, Bruyneel L Nurse staffing and education and hospital mortality in nine European countries: a retrospective observational study. Lancet. 2014; 383:(9931)1824-1830 https://doi.org/10.1016/S0140-6736(13)62631-8
Anthony AS. Gender bias and discrimination in nursing education: can we change it?. Nurse Educ. 2004; 29:(3)121-125 https://doi.org/10.1097/00006223-200405000-00011
Arber S, Ginn J. Gender differences in informal caring. Health and Social Care in the Community. 1995; 3:(1)19-31 https://doi.org/10.1111/j.1365-2524.1995.tb00003.x
Austgard KI. What characterises nursing care? A hermeneutical philosophical inquiry. Scand J Caring Sci. 2008; 22:(2)314-9 https://doi.org/10.1111/j.1471-6712.2007.00526.x
Beasley C. Focusing on careers: a new national framework will provide a route map for nursing careers. Nursing Standard. 2006; 20:(21)28-29
Brodie DA, Andrews GJ, Andrews JP, Thomas GB, Wong J, Rixon L. Perceptions of nursing: confirmation, change and the student experience. Int J Nurs Stud. 2004; 41:(7)721-33 https://doi.org/10.1016/j.ijnurstu.2004.02.009
Caring: the compassion and wisdom of nursing. In: Brykczyns K (ed). London: Arnold; 1997
Dahlberg L, Demack S, Bambra C. Age and gender of informal carers: a population-based study in the UK. Health Soc Care Community. 2007; 15:(5)439-445 https://doi.org/10.1111/j.1365-2524.2007.00702.x
Finfgeld-Connett D. Meta-synthesis of caring in nursing. J Clin Nurs. 2008; 17:(2)196-204
Report of the Mid Staffordshire NHS Foundation Trust public inquiry. 2013. https://tinyurl.com/ycydkya5 (accessed 7 February 2022)
Genua JA. The vision of male nurses: roles, barriers and stereotypes. Interaction. 2005; 23:(4)4-7
Grander SL, Hagedorn ME. Holding nurses accountable. AWHONN Lifelines. 1997; 1:(1)55-56 https://doi.org/10.1111/j.1552-6356.1997.tb01310.x
Hall C, Ritchie D. What is nursing?.London: SAGE/Learning Matters; 2009
Hallam J. Nursing the image: media, culture and professional identity.London: Routledge; 2000
Hamilton M, Essat Z. Minority ethnic users experiences and expectations of nursing care. Journal of Research in Nursing. 2008; 13:(2)102-110 https://doi.org/10.1177/1744987108088638
Health Education England. Nursing associate curriculum framework. 2017. https://tinyurl.com/55je45hm (accessed 7 February 2022)
Henderson V. The nature of nursing. Am J Nurs. 1964; 64:(8)62-68
Hoeve Y, Jansen G, Roodbol P. The nursing profession: public image, self-concept and professional identity. A discussion paper. J Adv Nurs. 2014; 70:(2)295-309 https://doi.org/10.1111/jan.12177
Hyde JS, Bigler RS, Joel D, Tate CC, van Anders SM. The future of sex and gender in psychology: five challenges to the gender binary. Am Psychol. 2019; 74:(2)171-193 https://doi.org/10.1037/amp0000307
International Council of Nursing. Nursing definitions. 2002. https://www.icn.ch/nursing-policy/nursing-definitions (accessed 7 February 2022)
Uniforms and workwear: an evidence base for developing local policy. 2007. https://tinyurl.com/ytvtjz73 (accessed 7 February 2022)
Jinks AM, Bradley E. Angel, handmaiden, battleaxe or whore? A study which examines changes in newly recruited student nurses’ attitudes to gender and nursing stereotypes. Nurse Educ Today. 2004; 24:(2)121-7 https://doi.org/10.1016/j.nedt.2003.10.011
What is a nurse? Baffling number of job roles leaves patients and bosses confused. 2017. https://tinyurl.com/3kyejupe (accessed 7 February 2022)
Leary A, Maclaine K, Trevatt P, Radford M, Punshon G. Variation in job titles within the nursing workforce. J Clin Nurs. 2017; 26:(23-24)4945-4950 https://doi.org/10.1111/jocn.13985
Petition calls for the protection of ‘nurse’ title for the sake of patient safety. 2021. https://tinyurl.com/3kyn67mc (accessed 7 February 2022)
NHS Digital. Narrowing of the NHS gender divide but men still the majority in senior roles. 2018. https://tinyurl.com/2p8ndwt3 (accessed 7 February 2022)
Nursing and Midwifery Council. Future nurse: standards of proficiency for registered nurses. 2018. https://tinyurl.com/23asmew5 (accessed 7 February 2022)
Nursing and Midwifery Council. Who we are and what we do. 2021. https://www.nmc.org.uk/about-us/our-role/ (accessed 7 February 2022)
Pennebaker JW, Chung CK, Frazee J, Lavergne GM, Beaver DI. When small words foretell academic success: the case of college admissions essays. PLoS One. 2014; 9:(12) https://doi.org/10.1371/journal.pone.0115844
Phillips J. Working carers: caring workers. In: Bernard M, Harding Davies V, Machin L, Phillips J (eds). London: Routledge; 2000
Romero-Martín M, Gómez-Salgado J, Robles-Romero JM, Jiménez-Picón N, Gómez-Urquiza JL, Ponce-Blandón JA. Systematic review of the nature of nursing care described by using the Caring Behaviours Inventory. J Clin Nurs. 2019; 28:(21-22)3734-3746 https://doi.org/10.1111/jocn.15015
Royal College of Nursing. Defining nursing. 2003. https://tinyurl.com/2p8rwmkb (accessed 7 February 2022)
Royal College of Nursing. Safe and effective staffing: nursing against the odds. 2017. https://www.rcn.org.uk/professional-development/publications/pub-006415 (accessed 8 February 2022)
Shaw K, Timmons S. Exploring how nursing uniforms influence self image and professional identity. Nurs Times. 2010; 106:(10)21-23
Skorupski VJ, Rea RE. Patients' perceptions of today's nursing attire: exploring dual images. JONA: Journal of Nursing Administration. 2006; 36:(9)393-401 https://doi.org/10.1097/00005110-200609000-00005
Sollami A, Caricati L, Mancini T. Ambivalent stereotypes of nurses and physicians: impact on students' attitude toward interprofessional education. Acta Biomed. 2015; 86:19-28
Nurses ranked the ‘most trusted profession’ in 2018. 2019. https://tinyurl.com/2p8ytrtv (accessed 7 February 2022)
Sweet SJ, Norman IJ. The nurse-doctor relationship: a selective literature review. J Adv Nurs. 1995; 22:(1)165-170 https://doi.org/10.1046/j.1365-2648.1995.22010165.x
Tausczik YR, Pennebaker JW. The psychological meaning of words: LIWC and computerized text analysis methods. J Lang Soc Psychol. 2010; 29:(1)24-54 https://doi.org/10.1177/0261927X09351676
Taylor EJ. Nurses caring for the spirit: patients with cancer and family caregiver expectations. Oncol Nurs Forum. 2003; 30:(4)585-590 https://doi.org/10.1188/03.ONF.585-590
Weaver R, Ferguson C, Wilbourn M, Salamonson Y. Men in nursing on television: exposing and reinforcing stereotypes. J Adv Nurs. 2014; 70:(4)833-842 https://doi.org/10.1111/jan.12244
Weng HC, Chen HC, Chen HJ, Lu K, Hung SY. Doctors' emotional intelligence and the patient–doctor relationship. Med Educ. 2008; 42:(7)703-711 https://doi.org/10.1111/j.1365-2923.2008.03039.x
White K. Nursing as vocation. Nurs Ethics. 2002; 9:(3)279-290 https://doi.org/10.1191/0969733002ne510oa
White R. The effects of the NHS on the nursing profession 1948-61.London: The King's Fund; 1985
Yam BMC. From vocation to profession: the quest for professionalization of nursing. Br J Nurs. 2004; 13:(16)978-982 https://doi.org/10.12968/bjon.2004.13.16.15974
Nursing in the 21st century: results of a pilot survey on attitudes towards nurses and nursing
Julia Woodland
Assistant Discipline Lead of Associate Healthcare Practice and Nursing Apprenticeships, School of Nursing and Professional Practice, College of Health and Social Care, University of Derby, Derby
View articles · Email Julia
Kendal Foster
Lecturer in Associate Healthcare Practice and Nursing Apprenticeships, School of Nursing and Professional Practice, College of Health and Social Care, University of Derby, Derby
View articles
David Robertshaw
Head of School, Nursing and Midwifery, School of Nursing and Professional Practice, College of Health and Social Care, University of Derby, Derby

Nursing is one of the most trusted professions, yet it is poorly defined. There are many definitions and characterisations of nursing. This study sought to pilot a survey exploring the views of nursing in the 21st century. Methods: This study piloted an electronic survey with open and closed questions. Descriptive statistics were collated for closed questions using Excel. Open-ended questions were analysed using the text analysis program Linguistic Inquiry and Word Count (LIWC) for tone, emotion and criticality. Results: This pilot study recruited 72 participants from professional and non-professional backgrounds. Respondents displayed diversity in their perceptions of nursing, the role of nurses and the role that nurses perform. Conclusion: Nursing is a complex, multifaceted profession. The view of nursing was generally positive and authentic although not easy to define. Nursing was felt to be an inclusive profession; however, it is extremely diverse in nature. Further research is required to explore these concepts in greater depth.
Nursing continues to be one of the most trusted professions ( Stone, 2019 ). In 2020, the nursing profession celebrated the 200th anniversary of the birth of Florence Nightingale and the 100th anniversary of the Nurses Registration Act 1919, legislation bringing regulation and recognition for nurses. These milestones prompted the authors to explore perceptions of nursing in the 21st century. In 2021 there were almost 745 000 registered nurses, nursing associates and midwives in England and Wales ( Nursing and Midwifery Council (NMC), 2021 ). Nursing is complex and multifaceted; nurses work across all fields—at home, close to home and in hospital ( Health Education England, 2017 ).‘Registered nurse’ is a legally protected title in the UK, yet there is still no clear definition. In addition, the term ‘nurse’ is not a protected title but whether this should be regulated is a contemporary topic of discussion. There is an ongoing debate regarding whether the title ‘nurse’ should also be protected in law. For example, registered nurses who are removed from the NMC register are still legally entitled to call themselves a ‘nurse’, regardless of the reason for their removal ( Mitchell, 2021 ).
Register now to continue reading
Thank you for visiting British Journal of Nursing and reading some of our peer-reviewed resources for nurses. To read more, please register today. You’ll enjoy the following great benefits:
What's included
Limited access to clinical or professional articles
Unlimited access to the latest news, blogs and video content
Signing in with your registered email address
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

The role of the public health nurse in a changing society

2010, Journal of Advanced Nursing
Related Papers
Journal of Clinical Nursing
Trish Markham
Journal of Research in Nursing
Gill Coverdale
Public health nursing (Boston, Mass.)
Pamela Kulbok
The Australian journal of advanced nursing: a quarterly publication of the Royal Australian Nursing Federation
Marcella Kelly
Nurse Education in Practice
Maxine L Holt
Public Health Nursing
Marla Salmon
Practice Development in Health Care
Susan M Carr
kate Frazer
Nursing outlook
Andrew Rome
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Julie Fairman
Journal of Advanced Nursing
Nigel Boldero
Dean Whitehead
Patricia Leahy-warren
Sinead Keeney
Shawn Kneipp
Sarah A Cowley , Sinéad Hanafin
Megan Aston
Client – centered Nursing Care Journal
Tommy Pangandaheng
Peter Griffiths
Epidemiology Biostatistics and Public Health
Assunta Guillari
Helen Mulcahy
Catherine Heffernan
International Journal of Environmental Research and Public Health
Global Pediatric Health
Amanda Phelan
World Journal of Advanced Research and Reviews
Pushpendra Saini
Anne Clancy
Primary Health Care Research and Development
grace christie
Marc Banogon
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
How Nurses Shape the Wellness of Society
Nursing August 15, 2017

Nursing has deep social implications. No, we’re not talking about Facebook, Twitter or other social media, but rather nursing’s intrinsic social context. Nursing is responsible to society through its mission to serve the public interest: specifically, the overall health of our society. As healthcare remains a major focus in the United States, nurses are being thrust into societal leadership roles pertaining to our health and healthcare. In effect, nurses today are being asked not to act as individuals, caring for individual patients…but as a group, with America as their patient. More and more, nurses are being asked to assume leadership roles – especially for the prevention of disease and to enhance patient outcomes.
How Nurses Interact with Society
How do nurses advance change and enhanced healthcare? Our society validates nursing’s core values and ethics through licensure and public affirmation and, in return, nurses provide quality care to all in need, regardless of their social or cultural standing and economic wherewithal. We all have a need for qualified, professional care-givers, and nurses fill that need. By providing the best possible healthcare to the population as a whole, nurses have earned the distinction of being part of one of the country’s most-trusted professions. With some three million registered nurses in the field, nursing is the largest healthcare profession and the foundation of America’s healthcare workforce. The complexity, size and culture of the healthcare system virtually mandates direct human intervention between patient and care-giver. This is a role nurses not only fill, but are re-educating themselves to fill with a population-based approach. In today’s environment, nurses are developing a more broad-based knowledge in order to keep abreast of healthcare changes, including collaboration with inter-professional teams on a new model of care. As the backbone of healthcare, a growing number of providers believe nurses should be given positions of greater influence – especially in the areas of quality care, determining health policy planning and management, promoting wellness, and improving efficiency. Since they have the pulse of America’s health, nurses will always be a strong component of how our healthcare is…and should be…administered.
Joining the Nursing Industry
Fortis College and Institute campuses in several states can help you enter the nursing profession through an Associate Degree in Nursing (RN) degree or Practical Nursing and Vocational Nursing diploma programs. There’s also an RN to BSN online program available through affiliated Denver School of Nursing for those seeking an advanced degree in the field. Visit our site for more information, and get started on the path to an amazing career.
Share this content
Previous Article
4 Reasons Why the Healthcare Industry Is a Wise Career Choice
Next Article
Why Be a Nurse? Here are 3 Top Reasons
Related articles.

Modal Question
Academic Support for Nursing Students
No notifications.
Critically analyse the nurses' roles and responsibilities within care provision
One of our expert writers has created this bespoke sample nursing essay that shows the quality that is guaranteed with every nursing paper ordered. Secure your academic success and place an order today or view our services .
- Undergraduate 1st
- Undergraduate 2:1
- Undergraduate 2:2
- Masters Distinction
- Masters Merit
- Masters Pass
Nurses have a range of roles and responsibilities in order to provide society with the highest quality of care (Peate, 2016). The Royal College of Nursing (RCN, 2014:3) define nursing as the ability to ‘improve, maintain, or recover health, to cope with health problems, and to achieve the best quality of life’ for patients until their death. This essay will critically analyse the nurses’ role and responsibilities within care provision, discussing their role as a primary caregiver, a leader, advocate, educator, collaborator, practitioner, in addition to their responsibilities in line with professional codes of practice (Nursing and Midwifery Council, 2015).
The nurse has a role as a primary caregiver, adhering to succinct evidence-based practice in order to meet the holistic needs of every patient and their families through the use of clinical judgement and expertise (RCN, 2017). They show compassion and knowledge in order to provide direct care to patients within each setting or different environments (Masters, 2015). Illness prevention and the promotion of public health initiatives are also vital roles in nursing care (Joel, 2017). However, political and societal issues place strain on the nursing workforce, hindering their ability to adhere to their roles which can negatively impact on the provision of high quality care (Ryan, 2018). For instance, with the introduction of an English test by the Nursing and Midwifery Council following Brexit, the number of EU nurses has reduced by 89% (Tapper, 2017). Furthermore, the government has removed the nursing bursary, which in turn has led to a reduction in the number of nursing students, thus leading to nurse shortages (Adams, 2017). Many nurses have stressed that they find it difficult to carry out their roles and responsibilities as a healthcare professional (Tapper, 2017).
Nurses must act as leaders, coordinating care as members of multidisciplinary care teams, contributing to a collaboration of care (Crowell, 2015). This involves physical and psychosocial assessment, provision of education, support and diagnostic testing to navigate patients through appropriate care pathways (Crowell, 2015). The nurse coordinator is a key resource for patients and families who are an integral point of contact during their care (Weberg et al, 2018). Nurse leaders need to continually contribute to the development of other healthcare professionals, ensuring that they are educated and equipped with evidence-based knowledge in order to provide high quality care (Weberg et al, 2018). Different leadership styles can be utilised to carry out this role, primarily the use of a transformational style. A transformational style encourages and motivates other staff members to improve the provision of care, without dictating information (Marshall, 2016). However, a more transactional leadership style is necessary in time-sensitive, critical situations (Stanley, 2016). These aspects are considered within the role of nurse leaders.
Nurses also act as advocates and educators, ensuring appropriate information is relayed to patients, enabling informed decisions which are fundamental to maintain patients’ autonomy (Scott, 2017). This includes developing therapeutic relationships to support and empower patients (Stein-Parbury, 2017). The nurse must provide holistic care in order to meet unmet needs through professional intervention (Weberg et al, 2018). This is especially important if a patient lacks the capacity to make informed decisions and so the nurse is responsible for adhering to health legislation (McEwen and Wills, 2017). The Mental Capacity Act 2005 provides the framework in order to protect a patient who cannot make an informed decision. Nurses should carry out an assessment in order to evaluate levels of capacity, in an appropriate manner in which the patient can understand. If the patient is found to lack capacity, the least restrictive option should be chosen in order to provide care in their best interests (McEwen and Wills, 2017). Nurses must also be aware that capacity can change at any moment and so succinct clinical judgement is key in order to provide high quality and ethical care (Stanley, 2016).
If you need assistance with writing your essay, our professional Essay Writing Service is here to help!
Another important role of the nurse is as an educator, to patients, families, society, other healthcare professionals and students (Bastable, 2017). Within a hospital environment, they provide knowledge about illness and teach patients how to self-manage their conditions (Bastable, 2017). Emphasis and facilitation of self-care are vital components of nursing, especially as approximately 15 million individuals within England have one or more long-term condition (RCN, 2018). Furthermore, with the increasing concern of antimicrobial resistance, education and self-care are important, to ensure that antibiotics are taken correctly to uphold the health of society (RCN, 2018). Health education is a necessity and a key responsibility of nurses throughout the world (Bastable, 2017).
Nurses must ensure they collaborate with other professionals within multidisciplinary teams, remaining accountable with sound clinical judgement and excellent communication skills (Joel, 2017). They must appreciate the expertise of other professionals and learn from their experience in order to care holistically for patients (Bogaert and Clarke, 2018). This must include adherence to patient and family- centred care, with enthusiasm to work towards the best patient outcome (Finkelman, 2017). This role is grounded within professional and personal values, expertise, theories and practice that encompass innovative and evidence-based care, whilst complementing other healthcare providers (Joel, 2017). Patient-centred care is beneficial in that is ensures patients are treated with compassion and respect (Finkelman, 2017). Improvements are also witnessed in regards to staff performance and morale when patient-centred care is provided (Stein-Parbury, 2017).
Nurses have the responsibility to remain up-to-date with relevant evidence-based research in addition to adhering to professional standards of practice (Ellis, 2016). These standards are in place to create boundaries and a level of accountability (NMC, 2015). This will incorporate various aspects such as ethics, competence, knowledge, confidentiality, accountability and how evidence can be applied in a practical environment (Avery, 2016). Nurses are held accountable for every aspect of care, with continual documentation under the direction of management (Standing, 2017). Ethical principles are also adhered to, such as a patient’s right to autonomy, non-beneficence, maleficence and justice (Beauchamp and Childress, 2013). However, the individual self-perception of one’s role can differ, influenced by individual background, societal attitude, government policies and trends (Joel, 2017). Within contemporary nursing, role theory can be used to theoretically explain the role of the profession, with Brookes et al. (2007) noting three main perspectives that emerge from evidence-based research. They include; social structuralism, symbolic interactionism and a dramaturgical perspective. Social structuralism argues that a nurses’ role will differ in regards to different structures within society throughout time, whereas symbolic interactionism is in relation to a nurses’ environment. Dramaturgical theory notes a connection between time, place and audience (Brookes et al, 2007). However, quality assurance is expected of all nurses, within standards, legislation and society (Sherwood and Barnsteiner, 2017). These standards ensure that all professionals are providing care with utmost competence and the ability to apply evidence-based research within practice. The nurse has a responsibility to remain up-to-date and educated, as quality assurance standards across many different environments, countries and time are in a continual state of evolution (Brown, 2017).
Upholding confidentiality is an additional responsibility of a nurse, that is mandatory in order to provide high quality patient care (Tingle and Cribb, 2013). Privacy is a key aspect of legislation within the UK and throughout the world, as nurses are expected to maintain confidentiality, in terms of medical records and verbal conversations (Drury, 2017). It is discussed in detail within the Nursing and Midwifery Council Code of Conduct, to uphold dignity and to provide high quality care (NMC, 2015). However, from a critical perspective there are times in which this idealism may be breached, to uphold the health of the patient or society (Blightman and Griffiths, 2013). The legitimate exceptions to confidentiality rights are in relation to disclosures with consent, disclosures required by legislation and those made in society’s best interests (Blightman and Griffiths, 2013). The NHS has historically struggled to uphold patient confidentiality, which led to the Caldicott Report, outlining a succinct process in order to protect and maintain privacy (Peate, 2012). This includes the need to justify disclosure, utilise the minimum amount of information necessary, maintain anonymity when possible, access on a ‘need-to-know’ basis and strict adherence with the law (Herring, 2015). This extends to social media platforms in which patient information should never be disclosed (Blightman and Griffiths, 2013). Confidentiality and disclosure is also influenced by capacity and so nurses have a legal and professional duty of care to consider capacity when consent is expressed (Joel, 2017). This can be challenging if a patient is in severe pain which can impact upon conscious levels and so clinical judgement is a necessity (Griffith and Tengnah, 2017).
Free Undergraduate Lectures
Nurses should also appraise their abilities, in relation to strengths, weaknesses and their preferences during the provision of care (Stanley, 2016). This should involve the process of self-analysis, to recognise one’s abilities in line with the care standard necessary, with realistic expectations to maintain high quality, safe care (Stanley, 2016). Nurses need to be able to recognise early signs and symptoms of illness, to take quick and appropriate action in addition to noting potential problems that could arise (Gulanick and Myers, 2016). This involves a succinct understanding and initiation of assessment, analysis, diagnosis, planning, an intervention and evaluation of the provision of care (Gulanick and Myers, 2016). Furthermore, these stages should be documented in a clear and concise manner, without the use of jargon or abbreviated terms in order to enhance patient-centred care and understanding (Monsen, 2017). During the provision of patient care, nurses are also required to remain self-aware, in order to evaluate personal strengths and an awareness of when to ask for help in line with personal limitations (Monsen, 2017). This upholds patient safety and the provision of high quality care (Stein-Parbury, 2017). Lastly, a nurse must be organised, with the ability to prioritise workloads in order to uphold their role (Monsen, 2017).
To conclude, the roles and responsibilities of a nurse have advanced within different spheres of practice, which will continue to adapt as healthcare within the UK evolves. As discussed, a nurse’s role is influenced by social structuralism, symbolic interactionism and a dramaturgical perspective (Brookes et al, 2007). The role and responsibility of the profession will change in regards to self-perception, influence of society, environment, time place and audience. Legislation also affects the role of a nurse, with ever changing political and legislative focus. However, there are aspects of the role which continue to prevail. For instance, the need to uphold confidentiality, dignity, competency and adhere to professional standards. Ultimately, the main role of a nurse is to provide high quality, safe care to all patients within society, with compassion, humanity, effective leadership and collaboration within multi-disciplinary teams to uphold good standards. This is in line with the Nursing and Midwifery Code of Conduct, which outlines the professional practice necessary to provide high quality care. Self-awareness is also paramount, to note personal strengths and limitations in order to uphold a sense of accountability, safe practice and protection against litigation. If nurses do not uphold the perceived roles and responsibilities of a nurse, they may be subjected to the legal implications which may impact on their ability to practice as a nurse.
Bibliography
- Adams, R. (2017) ‘Nursing Degree Applications Slump after NHS Bursaries Abolished,’ The Guardian, 2nd Feb 2017. Available at: https://www.theguardian.com/education/2017/feb/02/nursing-degree-applications-slump-after-nhs-bursaries-abolished Accessed: 24.02.18
- Avery, G. (2016) Law and Ethics in Nursing and Healthcare: An Introduction, London: Sage.
- Bastable, S. (2017) Nurse as Educator: Principles of Teaching and Learning for Nursing Practice, London: Jones and Bartlett Learning.
- Beauchamp, T, Childress, J. (2013) Principles of Biomedical Ethics, Oxford: Oxford University Press.
- Blightman, K, Griffiths, S. (2013) ‘Patient Confidentiality: When can a Breach be Justified?’ BJA, 2 (1) pp.52-56.
- Bogaert, P. Clarke, S. (2018) The Organisational Context of Nursing Practice: Concepts, Evidence and Interventions for Improvement, London: Springer.
- Brookes, K, Davidson, P, Daly, J, Halcomb, E. (2007) ‘Role Theory: A Framework to Investigate the Community Nurse Role in Contemporary Health Care Systems,’ Contemp Nursing, 25 (1-2) pp.146-155.
- Brown, J. (2017) Evidence-Based Practice for Nurses, Burlington: Jones and Bartlett Learning.
- Crowell, D. (2015) Complexity Leadership: Nursing’s Role in Health-Care Delivery, Philadelphia: Davis Company.
- Drury, P. (2017) Core EU Legislation 2017-2018, London: Palgrave MacMillan.
- Ellis, P. (2016) Evidence-based Practice in Nursing, London: Sage.
- Finkelman, A. (2017) Professional Nursing Concepts: Competencies for Quality Leadership, London: Jones and Bartlett Learning.
- Griffith, R, Tengnah, C. (2017) Law and Professional Issues in Nursing, London: Sage.
- Gulanick, M, Myers, J. (2016) Nursing Care Plans: Diagnoses, Interventions and Outcomes, London: Elsevier.
- Herring, J. (2015) Medical Law, London: Routledge.
- Joel, L. (2017) Advanced Practice Nursing: Essentials for Role Development, Philadelphia: Davis Company.
- Marshall, E. (2016) Transformational Leadership in Nursing, London: Springer.
- Masters, K. (2015) Role Development in Professional Nursing Practice, Burlington: Jones and Bartlett Publishing.
- McEwen, M, Wills, E. (2017) Theoretical Basis for Nursing, London: Lippincott Williams and Wilkins.
- Monsen, K. (2017) Intervention Effectiveness Research: Quality Improvement and Program Evaluation, London: Springer.
- NMC. (2015) The Code, London: NMC.
- Peate, I. (2016) The Essential Guide to Becoming a Staff Nurse, London: Wiley Blackwell.
- Peate, I. (2012) The Student’s Guide to Becoming a Nurse, London: Wiley Blackwell.
- RCN. (2018) Self Care, London: RCN.
- RCN. (2017) Principles of Nursing Practice, London: RCN.
- Royal College of Nursing. (2014) Defining Nursing, London: RCN.
- Ryan, F. (2018) ‘Waiting for an Ambulance, Unable to Breathe, Brings Austerity Home,’ The Guardian, 8th February 2018. Available at: https://www.theguardian.com/commentisfree/2018/feb/08/ambulance-austerity-cuts Accessed: 24.02.18
- Scott, A. (2017) Key Concepts and Issues in Nursing Ethics, London: Springer.
- Sherwood, G, Barsteiner, J. (2017) Quality and Safety in Nursing: A Competency Approach to Improving Outcomes, London: Wiley Blackwell.
- Standing, M. (2017) Clinical Judgement and Decision Making in Nursing, London: Sage.
- Stanley, D. (2016) Clinical Leadership in Nursing and Healthcare: Values into Action, London: Wiley Blackwell.
- Stein-Parbury, J. (2017) Patient and Person: Interpersonal Skills in Nursing, London: Elsevier.
- Tapper, J. (2017) ‘Difficulty of NHS Language Test ‘Worsens Nurse Crisis’, Says Recruiters,’ The Guardian, 24th June 2017. Available at: https://www.theguardian.com/society/2017/jun/24/english-speaking-ovserseas-nurses-fail-nhs-too-tough-language-test Accessed: 24.02.18
- Tingle, J, Cribb, A. (2013) Nursing Law and Ethics, London: Wiley Blackwell.
- Weberg, D, Porter-O’Grady, T, Mangold, K. (2018) Leadership in Nursing Practice, London: Jones and Bartlett Publishing.
Cite This Work
To export a reference to this article please select a referencing stye below:
Delivered on-time or your money back
Rated 4.6 / 5
Give yourself the academic edge today
Each order includes
- On-time delivery or your money back
- A fully qualified writer in your subject
- In-depth proofreading by our Quality Control Team
- 100% confidentiality, the work is never re-sold or published
- Standard 7-day amendment period
- A paper written to the standard ordered
- A detailed plagiarism report
- A comprehensive quality report
Our Press Coverage

- Free Samples
- Premium Essays
- Editing Services Editing Proofreading Rewriting
- Extra Tools Essay Topic Generator Thesis Generator Citation Generator GPA Calculator Study Guides Donate Paper
- Essay Writing Help
- About Us About Us Testimonials FAQ
- Studentshare
- The Role of Nursing in Society
The Role of Nursing in Society - Essay Example
- Subject: Nursing
- Type: Essay
- Level: College
- Pages: 2 (500 words)
- Downloads: 2
Extract of sample "The Role of Nursing in Society"
Apparently, the general public is aware and expects that as experts in the field of caring, nurses show evidence in the application of learned, modern techniques within personalities that project an aura of healing. Normally, this should further be enhanced by the accurate execution of contemporary primary care to ensure comfort among medical care clients regardless of the medical care setting. As health care workers and civil service providers, nurse's priority concern is the public interest while living an ideal, reserve, and humble life.
Thus, nurses as professionals in the practice of their expertise embody an attitude that goes beyond personal limitations and discriminations. Nursing is a distinct vocation because, as experts in a particular field, it focuses on activities engage in extending assistance to individuals who are ill. It is in the performance of help oriented activities that nursing best contributes to the healing of the sick, which is likewise, a speedy recovery from pain and illness. Apparently, the meaning of the profession has progressed from its simple beginnings indicating a womanly task which is basic and does not have to be studied (Donahue, 1996).
It was from suckling an infant to one that has become a stylish and vastly educated line of work (Donahue, 1996). Practically, this shift is manifested in the developed and enhanced role of nursing. Beginning with the 19th-century developments, nursing as a profession and work has been expanded to not only tending the sick. It also means undergoing the education. This is the best way of nurturing the sick. It goes further to executing such responsibility under the direction of a medical doctor (Donahue, 1996).
This task was promoted to include child-nursing and sick-nursing (Donahue, 1996). Child-nursing which eventually was specialized nursemaid and governess is allied to teaching and training of children (Donahue, 1996). While sick-nursing is linked to healing ability, care for the sick, the aged, the vulnerable, and the people who are in poor health, the handicapped, and the sponsorship of wellbeing (Donahue, 1996). The latter further included such factors as affection, concern, solitude, and responsibility for personal wants and desires.
Conclusion Virtually, care and caring underpin nursing, despite the vagueness of the phrase as a sweeping statement of the realities of the profession (Daly, Speedy, Jackson, Lambert, & Lambert, 2005). This is because nursing turned out to be multi-dimensional. It is driven by sophisticated concepts assumed as attitude and at the same time discipline (Daly et al, 2005). Similarly, nurse caring is characterized as giving value to individual interactions, well-versed of the doctrine of sharing, candor, compassion, and self-discipline.
Additionally, nurse caring includes reverence, the guarantee of individual attendance, cheerful association, expert understanding and ability, and courtesy. Moreover, affection and effort are supplementary facets to nurse caring.
- Cited: 1 times
- Copy Citation Citation is copied Copy Citation Citation is copied Copy Citation Citation is copied
CHECK THESE SAMPLES OF The Role of Nursing in Society
Advocacy roles in professional nursing, the relationship between the doctor or physician and the nurses, roles of state boards of nursing in the expanded role of the nurse, the advantages of the nursing profession to any society, nursing role models, analyzing family phenomenon, evolving public health nursing role, clinical skills and nursing roles.

- TERMS & CONDITIONS
- PRIVACY POLICY
- COOKIES POLICY
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A personal essay on the role of the nurse
Affiliation.
- 1 Tropical Health Research Unit, James Cook University and Townsville Health District, Townsville, QLD, Australia.
- PMID: 23485224
- DOI: 10.5172/conu.2013.43.2.213
Nursing has suffered a lack of understanding by the general public, who often can see no further than stereotypes of heroine, harlot, harridan or handmaiden. These have colored nursing's development as a profession, in Australia as in the rest of the world. Australia, as the 'lucky country' has one of the best health systems in the world, and Australian nurses are amongst those at the forefront of the profession. However, it appears that Australian nurses, as with many sections of Australian society, do not recognize that they hold high professional standards. With the influence of the international nursing shortage and the ever-growing technological advances within health care, alternatives to nurses, and to the registered nurse, are emerging. It is vitally important that nursing controls and regulates these developments. Only by protecting the legitimate role of the nurse, ensuring that education standards are maintained at the highest appropriate level, and generating and using new nursing knowledge will outcomes for all those who come to us for care be of the highest order. This essay proposes that Australian nurses need to overcome the 'cultural cringe' and recognize that they are in charge of a profession which meets the highest international standards.
PubMed Disclaimer
Similar articles
- Making us what we are: noteworthy people and achievements in Queensland mental health nursing. McAllister M, Happell B, Bradshaw J. McAllister M, et al. Int J Ment Health Nurs. 2010 Aug;19(4):250-6. doi: 10.1111/j.1447-0349.2010.00666.x. Int J Ment Health Nurs. 2010. PMID: 20618525
- Promoting leadership and management in Australian general practice nursing: what will it take? Halcomb EJ, Davidson PM, Patterson E. Halcomb EJ, et al. J Nurs Manag. 2008 Oct;16(7):846-52. doi: 10.1111/j.1365-2834.2008.00938.x. J Nurs Manag. 2008. PMID: 19017247 Review.
- Beyond profession: nursing leadership in contemporary healthcare. Sorensen R, Iedema R, Severinsson E. Sorensen R, et al. J Nurs Manag. 2008 Jul;16(5):535-44. doi: 10.1111/j.1365-2834.2008.00896.x. J Nurs Manag. 2008. PMID: 18558924
- A phenomenographic study of registered nurses' understanding of their role in student learning--an Australian perspective. Brammer J. Brammer J. Int J Nurs Stud. 2006 Nov;43(8):963-73. doi: 10.1016/j.ijnurstu.2005.11.004. Epub 2005 Dec 19. Int J Nurs Stud. 2006. PMID: 16360656
- Shaping the future of practice through political activity: how nurses can influence health care policy. Ennen KA. Ennen KA. AAOHN J. 2001 Dec;49(12):557-69; quiz 570. AAOHN J. 2001. PMID: 11806495 Review.
- Angels and Heroes: The Unintended Consequence of the Hero Narrative. Stokes-Parish J, Elliott R, Rolls K, Massey D. Stokes-Parish J, et al. J Nurs Scholarsh. 2020 Sep;52(5):462-466. doi: 10.1111/jnu.12591. Epub 2020 Aug 27. J Nurs Scholarsh. 2020. PMID: 32856396 Free PMC article. No abstract available.
- Search in MeSH
LinkOut - more resources
Full text sources.
- Taylor & Francis
Other Literature Sources
- scite Smart Citations
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Open access
- Published: 03 July 2024
The impact of evidence-based nursing leadership in healthcare settings: a mixed methods systematic review
- Maritta Välimäki 1 , 2 ,
- Shuang Hu 3 ,
- Tella Lantta 1 ,
- Kirsi Hipp 1 , 4 ,
- Jaakko Varpula 1 ,
- Jiarui Chen 3 ,
- Gaoming Liu 5 ,
- Yao Tang 3 ,
- Wenjun Chen 3 &
- Xianhong Li 3
BMC Nursing volume 23 , Article number: 452 ( 2024 ) Cite this article
458 Accesses
Metrics details
The central component in impactful healthcare decisions is evidence. Understanding how nurse leaders use evidence in their own managerial decision making is still limited. This mixed methods systematic review aimed to examine how evidence is used to solve leadership problems and to describe the measured and perceived effects of evidence-based leadership on nurse leaders and their performance, organizational, and clinical outcomes.
We included articles using any type of research design. We referred nurses, nurse managers or other nursing staff working in a healthcare context when they attempt to influence the behavior of individuals or a group in an organization using an evidence-based approach. Seven databases were searched until 11 November 2021. JBI Critical Appraisal Checklist for Quasi-experimental studies, JBI Critical Appraisal Checklist for Case Series, Mixed Methods Appraisal Tool were used to evaluate the Risk of bias in quasi-experimental studies, case series, mixed methods studies, respectively. The JBI approach to mixed methods systematic reviews was followed, and a parallel-results convergent approach to synthesis and integration was adopted.
Thirty-one publications were eligible for the analysis: case series ( n = 27), mixed methods studies ( n = 3) and quasi-experimental studies ( n = 1). All studies were included regardless of methodological quality. Leadership problems were related to the implementation of knowledge into practice, the quality of nursing care and the resource availability. Organizational data was used in 27 studies to understand leadership problems, scientific evidence from literature was sought in 26 studies, and stakeholders’ views were explored in 24 studies. Perceived and measured effects of evidence-based leadership focused on nurses’ performance, organizational outcomes, and clinical outcomes. Economic data were not available.
Conclusions
This is the first systematic review to examine how evidence is used to solve leadership problems and to describe its measured and perceived effects from different sites. Although a variety of perceptions and effects were identified on nurses’ performance as well as on organizational and clinical outcomes, available knowledge concerning evidence-based leadership is currently insufficient. Therefore, more high-quality research and clinical trial designs are still needed.
Trail registration
The study was registered (PROSPERO CRD42021259624).
Peer Review reports
Global health demands have set new roles for nurse leaders [ 1 ].Nurse leaders are referred to as nurses, nurse managers, or other nursing staff working in a healthcare context who attempt to influence the behavior of individuals or a group based on goals that are congruent with organizational goals [ 2 ]. They are seen as professionals “armed with data and evidence, and a commitment to mentorship and education”, and as a group in which “leaders innovate, transform, and achieve quality outcomes for patients, health care professionals, organizations, and communities” [ 3 ]. Effective leadership occurs when team members critically follow leaders and are motivated by a leader’s decisions based on the organization’s requests and targets [ 4 ]. On the other hand, problems caused by poor leadership may also occur, regarding staff relations, stress, sickness, or retention [ 5 ]. Therefore, leadership requires an understanding of different problems to be solved using synthesizing evidence from research, clinical expertise, and stakeholders’ preferences [ 6 , 7 ]. If based on evidence, leadership decisions, also referred as leadership decision making [ 8 ], could ensure adequate staffing [ 7 , 9 ] and to produce sufficient and cost-effective care [ 10 ]. However, nurse leaders still rely on their decision making on their personal [ 11 ] and professional experience [ 10 ] over research evidence, which can lead to deficiencies in the quality and safety of care delivery [ 12 , 13 , 14 ]. As all nurses should demonstrate leadership in their profession, their leadership competencies should be strengthened [ 15 ].
Evidence-informed decision-making, referred to as evidence appraisal and application, and evaluation of decisions [ 16 ], has been recognized as one of the core competencies for leaders [ 17 , 18 ]. The role of evidence in nurse leaders’ managerial decision making has been promoted by public authorities [ 19 , 20 , 21 ]. Evidence-based management, another concept related to evidence-based leadership, has been used as the potential to improve healthcare services [ 22 ]. It can guide nursing leaders, in developing working conditions, staff retention, implementation practices, strategic planning, patient care, and success of leadership [ 13 ]. Collins and Holton [ 23 ] in their systematic review and meta-analysis examined 83 studies regarding leadership development interventions. They found that leadership training can result in significant improvement in participants’ skills, especially in knowledge level, although the training effects varied across studies. Cummings et al. [ 24 ] reviewed 100 papers (93 studies) and concluded that participation in leadership interventions had a positive impact on the development of a variety of leadership styles. Clavijo-Chamorro et al. [ 25 ] in their review of 11 studies focused on leadership-related factors that facilitate evidence implementation: teamwork, organizational structures, and transformational leadership. The role of nurse managers was to facilitate evidence-based practices by transforming contexts to motivate the staff and move toward a shared vision of change.
As far as we are aware, however, only a few systematic reviews have focused on evidence-based leadership or related concepts in the healthcare context aiming to analyse how nurse leaders themselves uses evidence in the decision-making process. Young [ 26 ] targeted definitions and acceptance of evidence-based management (EBMgt) in healthcare while Hasanpoor et al. [ 22 ] identified facilitators and barriers, sources of evidence used, and the role of evidence in the process of decision making. Both these reviews concluded that EBMgt was of great importance but used limitedly in healthcare settings due to a lack of time, a lack of research management activities, and policy constraints. A review by Williams [ 27 ] showed that the usage of evidence to support management in decision making is marginal due to a shortage of relevant evidence. Fraser [ 28 ] in their review further indicated that the potential evidence-based knowledge is not used in decision making by leaders as effectively as it could be. Non-use of evidence occurs and leaders base their decisions mainly on single studies, real-world evidence, and experts’ opinions [ 29 ]. Systematic reviews and meta-analyses rarely provide evidence of management-related interventions [ 30 ]. Tate et al. [ 31 ] concluded based on their systematic review and meta-analysis that the ability of nurse leaders to use and critically appraise research evidence may influence the way policy is enacted and how resources and staff are used to meet certain objectives set by policy. This can further influence staff and workforce outcomes. It is therefore important that nurse leaders have the capacity and motivation to use the strongest evidence available to effect change and guide their decision making [ 27 ].
Despite of a growing body of evidence, we found only one review focusing on the impact of evidence-based knowledge. Geert et al. [ 32 ] reviewed literature from 2007 to 2016 to understand the elements of design, delivery, and evaluation of leadership development interventions that are the most reliably linked to outcomes at the level of the individual and the organization, and that are of most benefit to patients. The authors concluded that it is possible to improve individual-level outcomes among leaders, such as knowledge, motivation, skills, and behavior change using evidence-based approaches. Some of the most effective interventions included, for example, interactive workshops, coaching, action learning, and mentoring. However, these authors found limited research evidence describing how nurse leaders themselves use evidence to support their managerial decisions in nursing and what the outcomes are.
To fill the knowledge gap and compliment to existing knowledgebase, in this mixed methods review we aimed to (1) examine what leadership problems nurse leaders solve using an evidence-based approach and (2) how they use evidence to solve these problems. We also explored (3) the measured and (4) perceived effects of the evidence-based leadership approach in healthcare settings. Both qualitative and quantitative components of the effects of evidence-based leadership were examined to provide greater insights into the available literature [ 33 ]. Together with the evidence-based leadership approach, and its impact on nursing [ 34 , 35 ], this knowledge gained in this review can be used to inform clinical policy or organizational decisions [ 33 ]. The study is registered (PROSPERO CRD42021259624). The methods used in this review were specified in advance and documented in a priori in a published protocol [ 36 ]. Key terms of the review and the search terms are defined in Table 1 (population, intervention, comparison, outcomes, context, other).
In this review, we used a mixed methods approach [ 37 ]. A mixed methods systematic review was selected as this approach has the potential to produce direct relevance to policy makers and practitioners [ 38 ]. Johnson and Onwuegbuzie [ 39 ] have defined mixed methods research as “the class of research in which the researcher mixes or combines quantitative and qualitative research techniques, methods, approaches, concepts or language into a single study.” Therefore, we combined quantitative and narrative analysis to appraise and synthesize empirical evidence, and we held them as equally important in informing clinical policy or organizational decisions [ 34 ]. In this review, a comprehensive synthesis of quantitative and qualitative data was performed first and then discussed in discussion part (parallel-results convergent design) [ 40 ]. We hoped that different type of analysis approaches could complement each other and deeper picture of the topic in line with our research questions could be gained [ 34 ].
Inclusion and exclusion criteria
Inclusion and exclusion criteria of the study are described in Table 1 .
Search strategy
A three-step search strategy was utilized. First, an initial limited search with #MEDLINE was undertaken, followed by analysis of the words used in the title, abstract, and the article’s key index terms. Second, the search strategy, including identified keywords and index terms, was adapted for each included data base and a second search was undertaken on 11 November 2021. The full search strategy for each database is described in Additional file 1 . Third, the reference list of all studies included in the review were screened for additional studies. No year limits or language restrictions were used.
Information sources
The database search included the following: CINAHL (EBSCO), Cochrane Library (academic database for medicine and health science and nursing), Embase (Elsevier), PsycINFO (EBSCO), PubMed (MEDLINE), Scopus (Elsevier) and Web of Science (academic database across all scientific and technical disciplines, ranging from medicine and social sciences to arts and humanities). These databases were selected as they represent typical databases in health care context. Subject headings from each of the databases were included in the search strategies. Boolean operators ‘AND’ and ‘OR’ were used to combine the search terms. An information specialist from the University of Turku Library was consulted in the formation of the search strategies.

Study selection
All identified citations were collated and uploaded into Covidence software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia www.covidence.org ), and duplicates were removed by the software. Titles and abstracts were screened and assessed against the inclusion criteria independently by two reviewers out of four, and any discrepancies were resolved by the third reviewer (MV, KH, TL, WC). Studies meeting the inclusion criteria were retrieved in full and archived in Covidence. Access to one full-text article was lacking: the authors for one study were contacted about the missing full text, but no full text was received. All remaining hits of the included studies were retrieved and assessed independently against the inclusion criteria by two independent reviewers of four (MV, KH, TL, WC). Studies that did not meet the inclusion criteria were excluded, and the reasons for exclusion were recorded in Covidence. Any disagreements that arose between the reviewers were resolved through discussions with XL.
Assessment of methodological quality
Eligible studies were critically appraised by two independent reviewers (YT, SH). Standardized critical appraisal instruments based on the study design were used. First, quasi-experimental studies were assessed using the JBI Critical Appraisal Checklist for Quasi-experimental studies [ 44 ]. Second, case series were assessed using the JBI Critical Appraisal Checklist for Case Series [ 45 ]. Third, mixed methods studies were appraised using the Mixed Methods Appraisal Tool [ 46 ].
To increase inter-reviewer reliability, the review agreement was calculated (SH) [ 47 ]. A kappa greater than 0.8 was considered to represent a high level of agreement (0–0.1). In our data, the agreement was 0.75. Discrepancies raised between two reviewers were resolved through discussion and modifications and confirmed by XL. As an outcome, studies that met the inclusion criteria were proceeded to critical appraisal and assessed as suitable for inclusion in the review. The scores for each item and overall critical appraisal scores were presented.
Data extraction
For data extraction, specific tables were created. First, study characteristics (author(s), year, country, design, number of participants, setting) were extracted by two authors independently (JC, MV) and reviewed by TL. Second, descriptions of the interventions were extracted by two reviewers (JV, JC) using the structure of the TIDIeR (Template for Intervention Description and Replication) checklist (brief name, the goal of the intervention, material and procedure, models of delivery and location, dose, modification, adherence and fidelity) [ 48 ]. The extractions were confirmed (MV).
Third, due to a lack of effectiveness data and a wide heterogeneity between study designs and presentation of outcomes, no attempt was made to pool the quantitative data statistically; the findings of the quantitative data were presented in narrative form only [ 44 ]. The separate data extraction tables for each research question were designed specifically for this study. For both qualitative (and a qualitative component of mixed-method studies) and quantitative studies, the data were extracted and tabulated into text format according to preplanned research questions [ 36 ]. To test the quality of the tables and the data extraction process, three authors independently extracted the data from the first five studies (in alphabetical order). After that, the authors came together to share and determine whether their approaches of the data extraction were consistent with each other’s output and whether the content of each table was in line with research question. No reason was found to modify the data extraction tables or planned process. After a consensus of the data extraction process was reached, the data were extracted in pairs by independent reviewers (WC, TY, SH, GL). Any disagreements that arose between the reviewers were resolved through discussion and with a third reviewer (MV).
Data analysis
We were not able to conduct a meta-analysis due to a lack of effectiveness data based on clinical trials. Instead, we used inductive thematic analysis with constant comparison to answer the research question [ 46 , 49 ] using tabulated primary data from qualitative and quantitative studies as reported by the original authors in narrative form only [ 47 ]. In addition, the qualitizing process was used to transform quantitative data to qualitative data; this helped us to convert the whole data into themes and categories. After that we used the thematic analysis for the narrative data as follows. First, the text was carefully read, line by line, to reveal topics answering each specific review question (MV). Second, the data coding was conducted, and the themes in the data were formed by data categorization. The process of deriving the themes was inductive based on constant comparison [ 49 ]. The results of thematic analysis and data categorization was first described in narrative format and then the total number of studies was calculated where the specific category was identified (%).
Stakeholder involvement
The method of reporting stakeholders’ involvement follows the key components by [ 50 ]: (1) people involved, (2) geographical location, (3) how people were recruited, (4) format of involvement, (5) amount of involvement, (6) ethical approval, (7) financial compensation, and (8) methods for reporting involvement.
In our review, stakeholder involvement targeted nurses and nurse leader in China. Nurse Directors of two hospitals recommended potential participants who received a personal invitation letter from researchers to participate in a discussion meeting. Stakeholders’ participation was based on their own free will. Due to COVID-19, one online meeting (1 h) was organized (25 May 2022). Eleven participants joined the meeting. Ethical approval was not applied and no financial compensation was offered. At the end of the meeting, experiences of stakeholders’ involvement were explored.
The meeting started with an introductory presentation with power points. The rationale, methods, and preliminary review results were shared with the participants [ 51 ].The meeting continued with general questions for the participants: (1) Are you aware of the concepts of evidence-based practice or evidence-based leadership?; (2) How important is it to use evidence to support decisions among nurse leaders?; (3) How is the evidence-based approach used in hospital settings?; and (4) What type of evidence is currently used to support nurse leaders’ decision making (e.g. scientific literature, organizational data, stakeholder views)?
Two people took notes on the course and content of the conversation. The notes were later transcripted in verbatim, and the key points of the discussions were summarised. Although answers offered by the stakeholders were very short, the information was useful to validate the preliminary content of the results, add the rigorousness of the review, and obtain additional perspectives. A recommendation of the stakeholders was combined in the Discussion part of this review increasing the applicability of the review in the real world [ 50 ]. At the end of the discussion, the value of stakeholders’ involvement was asked. Participants shared that the experience of participating was unique and the topic of discussion was challenging. Two authors of the review group further represented stakeholders by working together with the research team throughout the review study.
Search results
From seven different electronic databases, 6053 citations were identified as being potentially relevant to the review. Then, 3133 duplicates were removed by an automation tool (Covidence: www.covidence.org ), and one was removed manually. The titles and abstracts of 3040 of citations were reviewed, and a total of 110 full texts were included (one extra citation was found on the reference list but later excluded). Based on the eligibility criteria, 31 studies (32 hits) were critically appraised and deemed suitable for inclusion in the review. The search results and selection process are presented in the PRISMA [ 52 ] flow diagram Fig. 1 . The full list of references for included studies can be find in Additional file 2 . To avoid confusion between articles of the reference list and studies included in the analysis, the studies included in the review are referred inside the article using the reference number of each study (e.g. ref 1, ref 2).
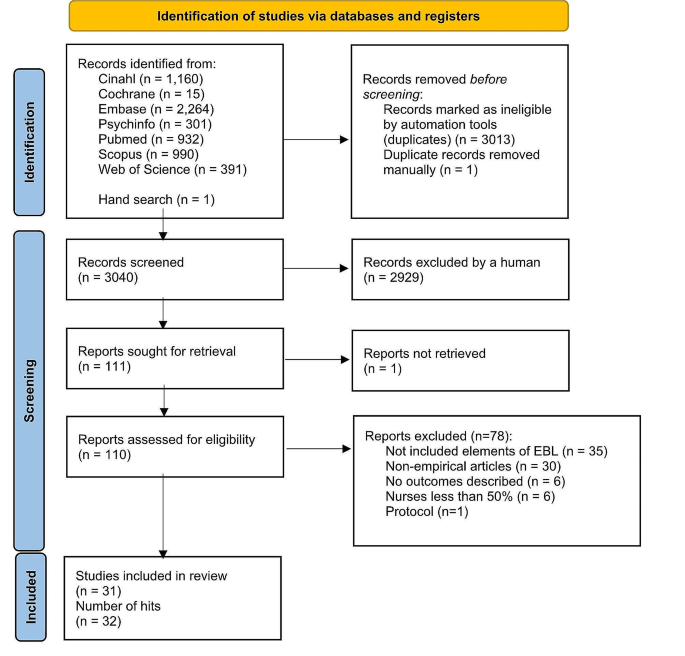
Search results and study selection and inclusion process [ 52 ]
Characteristics of included studies
The studies had multiple purposes, aiming to develop practice, implement a new approach, improve quality, or to develop a model. The 31 studies (across 32 hits) were case series studies ( n = 27), mixed methods studies ( n = 3) and a quasi-experimental study ( n = 1). All studies were published between the years 2004 and 2021. The highest number of papers was published in year 2020.
Table 2 describes the characteristics of included studies and Additional file 3 offers a narrative description of the studies.
Methodological quality assessment
Quasi-experimental studies.
We had one quasi-experimental study (ref 31). All questions in the critical appraisal tool were applicable. The total score of the study was 8 (out of a possible 9). Only one response of the tool was ‘no’ because no control group was used in the study (see Additional file 4 for the critical appraisal of included studies).
Case series studies . A case series study is typically defined as a collection of subjects with common characteristics. The studies do not include a comparison group and are often based on prevalent cases and on a sample of convenience [ 53 ]. Munn et al. [ 45 ] further claim that case series are best described as observational studies, lacking experimental and randomized characteristics, being descriptive studies, without a control or comparator group. Out of 27 case series studies included in our review, the critical appraisal scores varied from 1 to 9. Five references were conference abstracts with empirical study results, which were scored from 1 to 3. Full reports of these studies were searched in electronic databases but not found. Critical appraisal scores for the remaining 22 studies ranged from 1 to 9 out of a possible score of 10. One question (Q3) was not applicable to 13 studies: “Were valid methods used for identification of the condition for all participants included in the case series?” Only two studies had clearly reported the demographic of the participants in the study (Q6). Twenty studies met Criteria 8 (“Were the outcomes or follow-up results of cases clearly reported?”) and 18 studies met Criteria 7 (“Q7: Was there clear reporting of clinical information of the participants?”) (see Additional file 4 for the critical appraisal of included studies).
Mixed-methods studies
Mixed-methods studies involve a combination of qualitative and quantitative methods. This is a common design and includes convergent design, sequential explanatory design, and sequential exploratory design [ 46 ]. There were three mixed-methods studies. The critical appraisal scores for the three studies ranged from 60 to 100% out of a possible 100%. Two studies met all the criteria, while one study fulfilled 60% of the scored criteria due to a lack of information to understand the relevance of the sampling strategy well enough to address the research question (Q4.1) or to determine whether the risk of nonresponse bias was low (Q4.4) (see Additional file 4 for the critical appraisal of included studies).
Intervention or program components
The intervention of program components were categorized and described using the TiDier checklist: name and goal, theory or background, material, procedure, provider, models of delivery, location, dose, modification, and adherence and fidelity [ 48 ]. A description of intervention in each study is described in Additional file 5 and a narrative description in Additional file 6 .
Leadership problems
In line with the inclusion criteria, data for the leadership problems were categorized in all 31 included studies (see Additional file 7 for leadership problems). Three types of leadership problems were identified: implementation of knowledge into practice, the quality of clinical care, and resources in nursing care. A narrative summary of the results is reported below.
Implementing knowledge into practice
Eleven studies (35%) aimed to solve leadership problems related to implementation of knowledge into practice. Studies showed how to support nurses in evidence-based implementation (EBP) (ref 3, ref 5), how to engage nurses in using evidence in practice (ref 4), how to convey the importance of EBP (ref 22) or how to change practice (ref 4). Other problems were how to facilitate nurses to use guideline recommendations (ref 7) and how nurses can make evidence-informed decisions (ref 8). General concerns also included the linkage between theory and practice (ref 1) as well as how to implement the EBP model in practice (ref 6). In addition, studies were motivated by the need for revisions or updates of protocols to improve clinical practice (ref 10) as well as the need to standardize nursing activities (ref 11, ref 14).
The quality of the care
Thirteen (42%) focused on solving problems related to the quality of clinical care. In these studies, a high number of catheter infections led a lack of achievement of organizational goals (ref 2, ref 9). A need to reduce patient symptoms in stem cell transplant patients undergoing high-dose chemotherapy (ref 24) was also one of the problems to be solved. In addition, the projects focused on how to prevent pressure ulcers (ref 26, ref 29), how to enhance the quality of cancer treatment (ref 25) and how to reduce the need for invasive constipation treatment (ref 30). Concerns about patient safety (ref 15), high fall rates (ref 16, ref 19), dissatisfaction of patients (ref 16, ref 18) and nurses (ref 16, ref 30) were also problems that had initiated the projects. Studies addressed concerns about how to promote good contingency care in residential aged care homes (ref 20) and about how to increase recognition of human trafficking problems in healthcare (ref 21).
Resources in nursing care
Nurse leaders identified problems in their resources, especially in staffing problems. These problems were identified in seven studies (23%), which involved concerns about how to prevent nurses from leaving the job (ref 31), how to ensure appropriate recruitment, staffing and retaining of nurses (ref 13) and how to decrease nurses’ burden and time spent on nursing activities (ref 12). Leadership turnover was also reported as a source of dissatisfaction (ref 17); studies addressed a lack of structured transition and training programs, which led to turnover (ref 23), as well as how to improve intershift handoff among nurses (ref 28). Optimal design for new hospitals was also examined (ref 27).
Main features of evidence-based leadership
Out of 31 studies, 17 (55%) included all four domains of an evidence-based leadership approach, and four studies (13%) included evidence of critical appraisal of the results (see Additional file 8 for the main features of evidence-based Leadership) (ref 11, ref 14, ref 23, ref 27).
Organizational evidence
Twenty-seven studies (87%) reported how organizational evidence was collected and used to solve leadership problems (ref 2). Retrospective chart reviews (ref 5), a review of the extent of specific incidents (ref 19), and chart auditing (ref 7, ref 25) were conducted. A gap between guideline recommendations and actual care was identified using organizational data (ref 7) while the percentage of nurses’ working time spent on patient care was analyzed using an electronic charting system (ref 12). Internal data (ref 22), institutional data, and programming metrics were also analyzed to understand the development of the nurse workforce (ref 13).
Surveys (ref 3, ref 25), interviews (ref 3, ref 25) and group reviews (ref 18) were used to better understand the leadership problem to be solved. Employee opinion surveys on leadership (ref 17), a nurse satisfaction survey (ref 30) and a variety of reporting templates were used for the data collection (ref 28) reported. Sometimes, leadership problems were identified by evidence facilitators or a PI’s team who worked with staff members (ref 15, ref 17). Problems in clinical practice were also identified by the Nursing Professional Council (ref 14), managers (ref 26) or nurses themselves (ref 24). Current practices were reviewed (ref 29) and a gap analysis was conducted (ref 4, ref 16, ref 23) together with SWOT analysis (ref 16). In addition, hospital mission and vision statements, research culture established and the proportion of nursing alumni with formal EBP training were analyzed (ref 5). On the other hand, it was stated that no systematic hospital-specific sources of data regarding job satisfaction or organizational commitment were used (ref 31). In addition, statements of organizational analysis were used on a general level only (ref 1).
Scientific evidence identified
Twenty-six studies (84%) reported the use of scientific evidence in their evidence-based leadership processes. A literature search was conducted (ref 21) and questions, PICO, and keywords were identified (ref 4) in collaboration with a librarian. Electronic databases, including PubMed (ref 14, ref 31), Cochrane, and EMBASE (ref 31) were searched. Galiano (ref 6) used Wiley Online Library, Elsevier, CINAHL, Health Source: Nursing/Academic Edition, PubMed, and the Cochrane Library while Hoke (ref 11) conducted an electronic search using CINAHL and PubMed to retrieve articles.
Identified journals were reviewed manually (ref 31). The findings were summarized using ‘elevator speech’ (ref 4). In a study by Gifford et al. (ref 9) evidence facilitators worked with participants to access, appraise, and adapt the research evidence to the organizational context. Ostaszkiewicz (ref 20) conducted a scoping review of literature and identified and reviewed frameworks and policy documents about the topic and the quality standards. Further, a team of nursing administrators, directors, staff nurses, and a patient representative reviewed the literature and made recommendations for practice changes.
Clinical practice guidelines were also used to offer scientific evidence (ref 7, ref 19). Evidence was further retrieved from a combination of nursing policies, guidelines, journal articles, and textbooks (ref 12) as well as from published guidelines and literature (ref 13). Internal evidence, professional practice knowledge, relevant theories and models were synthesized (ref 24) while other study (ref 25) reviewed individual studies, synthesized with systematic reviews or clinical practice guidelines. The team reviewed the research evidence (ref 3, ref 15) or conducted a literature review (ref 22, ref 28, ref 29), a literature search (ref 27), a systematic review (ref 23), a review of the literature (ref 30) or ‘the scholarly literature was reviewed’ (ref 18). In addition, ‘an extensive literature review of evidence-based best practices was carried out’ (ref 10). However, detailed description how the review was conducted was lacking.
Views of stakeholders
A total of 24 studies (77%) reported methods for how the views of stakeholders, i.e., professionals or experts, were considered. Support to run this study was received from nursing leadership and multidisciplinary teams (ref 29). Experts and stakeholders joined the study team in some cases (ref 25, ref 30), and in other studies, their opinions were sought to facilitate project success (ref 3). Sometimes a steering committee was formed by a Chief Nursing Officer and Clinical Practice Specialists (ref 2). More specifically, stakeholders’ views were considered using interviews, workshops and follow-up teleconferences (ref 7). The literature review was discussed with colleagues (ref 11), and feedback and support from physicians as well as the consensus of staff were sought (ref 16).
A summary of the project findings and suggestions for the studies were discussed at 90-minute weekly meetings by 11 charge nurses. Nurse executive directors were consulted over a 10-week period (ref 31). An implementation team (nurse, dietician, physiotherapist, occupational therapist) was formed to support the implementation of evidence-based prevention measures (ref 26). Stakeholders volunteered to join in the pilot implementation (ref 28) or a stakeholder team met to determine the best strategy for change management, shortcomings in evidence-based criteria were discussed, and strategies to address those areas were planned (ref 5). Nursing leaders, staff members (ref 22), ‘process owners (ref 18) and program team members (ref 18, ref 19, ref 24) met regularly to discuss the problems. Critical input was sought from clinical educators, physicians, nutritionists, pharmacists, and nurse managers (ref 24). The unit director and senior nursing staff reviewed the contents of the product, and the final version of clinical pathways were reviewed and approved by the Quality Control Commission of the Nursing Department (ref 12). In addition, two co-design workshops with 18 residential aged care stakeholders were organized to explore their perspectives about factors to include in a model prototype (ref 20). Further, an agreement of stakeholders in implementing continuous quality services within an open relationship was conducted (ref 1).
Critical appraisal
In five studies (16%), a critical appraisal targeting the literature search was carried out. The appraisals were conducted by interns and teams who critiqued the evidence (ref 4). In Hoke’s study, four areas that had emerged in the literature were critically reviewed (ref 11). Other methods were to ‘critically appraise the search results’ (ref 14). Journal club team meetings (ref 23) were organized to grade the level and quality of evidence and the team ‘critically appraised relevant evidence’ (ref 27). On the other hand, the studies lacked details of how the appraisals were done in each study.
The perceived effects of evidence-based leadership
Perceived effects of evidence-based leadership on nurses’ performance.
Eleven studies (35%) described perceived effects of evidence-based leadership on nurses’ performance (see Additional file 9 for perceived effects of evidence-based leadership), which were categorized in four groups: awareness and knowledge, competence, ability to understand patients’ needs, and engagement. First, regarding ‘awareness and knowledge’, different projects provided nurses with new learning opportunities (ref 3). Staff’s knowledge (ref 20, ref 28), skills, and education levels improved (ref 20), as did nurses’ knowledge comprehension (ref 21). Second, interventions and approaches focusing on management and leadership positively influenced participants’ competence level to improve the quality of services. Their confidence level (ref 1) and motivation to change practice increased, self-esteem improved, and they were more positive and enthusiastic in their work (ref 22). Third, some nurses were relieved that they had learned to better handle patients’ needs (ref 25). For example, a systematic work approach increased nurses’ awareness of the patients who were at risk of developing health problems (ref 26). And last, nurse leaders were more engaged with staff, encouraging them to adopt the new practices and recognizing their efforts to change (ref 8).
Perceived effects on organizational outcomes
Nine studies (29%) described the perceived effects of evidence-based leadership on organizational outcomes (see Additional file 9 for perceived effects of evidence-based leadership). These were categorized into three groups: use of resources, staff commitment, and team effort. First, more appropriate use of resources was reported (ref 15, ref 20), and working time was more efficiently used (ref 16). In generally, a structured approach made implementing change more manageable (ref 1). On the other hand, in the beginning of the change process, the feedback from nurses was unfavorable, and they experienced discomfort in the new work style (ref 29). New approaches were also perceived as time consuming (ref 3). Second, nurse leaders believed that fewer nursing staff than expected left the organization over the course of the study (ref 31). Third, the project helped staff in their efforts to make changes, and it validated the importance of working as a team (ref 7). Collaboration and support between the nurses increased (ref 26). On the other hand, new work style caused challenges in teamwork (ref 3).
Perceived effects on clinical outcomes
Five studies (16%) reported the perceived effects of evidence-based leadership on clinical outcomes (see Additional file 9 for perceived effects of evidence-based leadership), which were categorized in two groups: general patient outcomes and specific clinical outcomes. First, in general, the project assisted in connecting the guideline recommendations and patient outcomes (ref 7). The project was good for the patients in general, and especially to improve patient safety (ref 16). On the other hand, some nurses thought that the new working style did not work at all for patients (ref 28). Second, the new approach used assisted in optimizing patients’ clinical problems and person-centered care (ref 20). Bowel management, for example, received very good feedback (ref 30).
The measured effects of evidence-based leadership
The measured effects on nurses’ performance.
Data were obtained from 20 studies (65%) (see Additional file 10 for measured effects of evidence-based leadership) and categorized nurse performance outcomes for three groups: awareness and knowledge, engagement, and satisfaction. First, six studies (19%) measured the awareness and knowledge levels of participants. Internship for staff nurses was beneficial to help participants to understand the process for using evidence-based practice and to grow professionally, to stimulate for innovative thinking, to give knowledge needed to use evidence-based practice to answer clinical questions, and to make possible to complete an evidence-based practice project (ref 3). Regarding implementation program of evidence-based practice, those with formal EBP training showed an improvement in knowledge, attitude, confidence, awareness and application after intervention (ref 3, ref 11, ref 20, ref 23, ref 25). On the contrary, in other study, attitude towards EBP remained stable ( p = 0.543). and those who applied EBP decreased although no significant differences over the years ( p = 0.879) (ref 6).
Second, 10 studies (35%) described nurses’ engagement to new practices (ref 5, ref 6, ref 7, ref 10, ref 16, ref 17, ref 18, ref 21, ref 25, ref 27). 9 studies (29%) studies reported that there was an improvement of compliance level of participants (ref 6, ref 7, ref 10, ref 16, ref 17, ref 18, ref 21, ref 25, ref 27). On the contrary, in DeLeskey’s (ref 5) study, although improvement was found in post-operative nausea and vomiting’s (PONV) risk factors documented’ (2.5–63%), and ’risk factors communicated among anaesthesia and surgical staff’ (0–62%), the improvement did not achieve the goal. The reason was a limited improvement was analysed. It was noted that only those patients who had been seen by the pre-admission testing nurse had risk assessments completed. Appropriate treatment/prophylaxis increased from 69 to 77%, and from 30 to 49%; routine assessment for PONV/rescue treatment 97% and 100% was both at 100% following the project. The results were discussed with staff but further reasons for a lack of engagement in nursing care was not reported.
And third, six studies (19%) reported nurses’ satisfaction with project outcomes. The study results showed that using evidence in managerial decisions improved nurses’ satisfaction and attitudes toward their organization ( P < 0.05) (ref 31). Nurses’ overall job satisfaction improved as well (ref 17). Nurses’ satisfaction with usability of the electronic charting system significantly improved after introduction of the intervention (ref 12). In handoff project in seven hospitals, improvement was reported in all satisfaction indicators used in the study although improvement level varied in different units (ref 28). In addition, positive changes were reported in nurses’ ability to autonomously perform their job (“How satisfied are you with the tools and resources available for you treat and prevent patient constipation?” (54%, n = 17 vs. 92%, n = 35, p < 0.001) (ref 30).
The measured effects on organizational outcomes
Thirteen studies (42%) described the effects of a project on organizational outcomes (see Additional file 10 for measured effects of evidence-based leadership), which were categorized in two groups: staff compliance, and changes in practices. First, studies reported improved organizational outcomes due to staff better compliance in care (ref 4, ref 13, ref 17, ref 23, ref 27, ref 31). Second, changes in organization practices were also described (ref 11) like changes in patient documentation (ref 12, ref 21). Van Orne (ref 30) found a statistically significant reduction in the average rate of invasive medication administration between pre-intervention and post-intervention ( p = 0.01). Salvador (ref 24) also reported an improvement in a proactive approach to mucositis prevention with an evidence-based oral care guide. On the contrary, concerns were also raised such as not enough time for new bedside report (ref 16) or a lack of improvement of assessment of diabetic ulcer (ref 8).
The measured effects on clinical outcomes
A variety of improvements in clinical outcomes were reported (see Additional file 10 for measured effects of evidence-based leadership): improvement in patient clinical status and satisfaction level. First, a variety of improvement in patient clinical status was reported. improvement in Incidence of CAUTI decreased 27.8% between 2015 and 2019 (ref 2) while a patient-centered quality improvement project reduced CAUTI rates to 0 (ref 10). A significant decrease in transmission rate of MRSA transmission was also reported (ref 27) and in other study incidences of CLABSIs dropped following of CHG bathing (ref 14). Further, it was possible to decrease patient nausea from 18 to 5% and vomiting to 0% (ref 5) while the percentage of patients who left the hospital without being seen was below 2% after the project (ref 17). In addition, a significant reduction in the prevalence of pressure ulcers was found (ref 26, ref 29) and a significant reduction of mucositis severity/distress was achieved (ref 24). Patient falls rate decreased (ref 15, ref 16, ref 19, ref 27).
Second, patient satisfaction level after project implementation improved (ref 28). The scale assessing healthcare providers by consumers showed improvement, but the changes were not statistically significant. Improvement in an emergency department leadership model and in methods of communication with patients improved patient satisfaction scores by 600% (ref 17). In addition, new evidence-based unit improved patient experiences about the unit although not all items improved significantly (ref 18).
Stakeholder involvement in the mixed-method review
To ensure stakeholders’ involvement in the review, the real-world relevance of our research [ 53 ], achieve a higher level of meaning in our review results, and gain new perspectives on our preliminary findings [ 50 ], a meeting with 11 stakeholders was organized. First, we asked if participants were aware of the concepts of evidence-based practice or evidence-based leadership. Responses revealed that participants were familiar with the concept of evidence-based practice, but the topic of evidence-based leadership was totally new. Examples of nurses and nurse leaders’ responses are as follows: “I have heard a concept of evidence-based practice but never a concept of evidence-based leadership.” Another participant described: “I have heard it [evidence-based leadership] but I do not understand what it means.”
Second, as stakeholder involvement is beneficial to the relevance and impact of health research [ 54 ], we asked how important evidence is to them in supporting decisions in health care services. One participant described as follows: “Using evidence in decisions is crucial to the wards and also to the entire hospital.” Third, we asked how the evidence-based approach is used in hospital settings. Participants expressed that literature is commonly used to solve clinical problems in patient care but not to solve leadership problems. “In [patient] medication and care, clinical guidelines are regularly used. However, I am aware only a few cases where evidence has been sought to solve leadership problems.”
And last, we asked what type of evidence is currently used to support nurse leaders’ decision making (e.g. scientific literature, organizational data, stakeholder views)? The participants were aware that different types of information were collected in their organization on a daily basis (e.g. patient satisfaction surveys). However, the information was seldom used to support decision making because nurse leaders did not know how to access this information. Even so, the participants agreed that the use of evidence from different sources was important in approaching any leadership or managerial problems in the organization. Participants also suggested that all nurse leaders should receive systematic training related to the topic; this could support the daily use of the evidence-based approach.
To our knowledge, this article represents the first mixed-methods systematic review to examine leadership problems, how evidence is used to solve these problems and what the perceived and measured effects of evidence-based leadership are on nurse leaders and their performance, organizational, and clinical outcomes. This review has two key findings. First, the available research data suggests that evidence-based leadership has potential in the healthcare context, not only to improve knowledge and skills among nurses, but also to improve organizational outcomes and the quality of patient care. Second, remarkably little published research was found to explore the effects of evidence-based leadership with an efficient trial design. We validated the preliminary results with nurse stakeholders, and confirmed that nursing staff, especially nurse leaders, were not familiar with the concept of evidence-based leadership, nor were they used to implementing evidence into their leadership decisions. Our data was based on many databases, and we screened a large number of studies. We also checked existing registers and databases and found no registered or ongoing similar reviews being conducted. Therefore, our results may not change in the near future.
We found that after identifying the leadership problems, 26 (84%) studies out of 31 used organizational data, 25 (81%) studies used scientific evidence from the literature, and 21 (68%) studies considered the views of stakeholders in attempting to understand specific leadership problems more deeply. However, only four studies critically appraised any of these findings. Considering previous critical statements of nurse leaders’ use of evidence in their decision making [ 14 , 30 , 31 , 34 , 55 ], our results are still quite promising.
Our results support a previous systematic review by Geert et al. [ 32 ], which concluded that it is possible to improve leaders’ individual-level outcomes, such as knowledge, motivation, skills, and behavior change using evidence-based approaches. Collins and Holton [ 23 ] particularly found that leadership training resulted in significant knowledge and skill improvements, although the effects varied widely across studies. In our study, evidence-based leadership was seen to enable changes in clinical practice, especially in patient care. On the other hand, we understand that not all efforts to changes were successful [ 56 , 57 , 58 ]. An evidence-based approach causes negative attitudes and feelings. Negative emotions in participants have also been reported due to changes, such as discomfort with a new working style [ 59 ]. Another study reported inconvenience in using a new intervention and its potential risks for patient confidentiality. Sometimes making changes is more time consuming than continuing with current practice [ 60 ]. These findings may partially explain why new interventions or program do not always fully achieve their goals. On the other hand, Dubose et al. [ 61 ] state that, if prepared with knowledge of resistance, nurse leaders could minimize the potential negative consequences and capitalize on a powerful impact of change adaptation.
We found that only six studies used a specific model or theory to understand the mechanism of change that could guide leadership practices. Participants’ reactions to new approaches may be an important factor in predicting how a new intervention will be implemented into clinical practice. Therefore, stronger effort should be put to better understanding the use of evidence, how participants’ reactions and emotions or practice changes could be predicted or supported using appropriate models or theories, and how using these models are linked with leadership outcomes. In this task, nurse leaders have an important role. At the same time, more responsibilities in developing health services have been put on the shoulders of nurse leaders who may already be suffering under pressure and increased burden at work. Working in a leadership position may also lead to role conflict. A study by Lalleman et al. [ 62 ] found that nurses were used to helping other people, often in ad hoc situations. The helping attitude of nurses combined with structured managerial role may cause dilemmas, which may lead to stress. Many nurse leaders opt to leave their positions less than 5 years [ 63 ].To better fulfill the requirements of health services in the future, the role of nurse leaders in evidence-based leadership needs to be developed further to avoid ethical and practical dilemmas in their leadership practices.
It is worth noting that the perceived and measured effects did not offer strong support to each other but rather opened a new venue to understand the evidence-based leadership. Specifically, the perceived effects did not support to measured effects (competence, ability to understand patients’ needs, use of resources, team effort, and specific clinical outcomes) while the measured effects could not support to perceived effects (nurse’s performance satisfaction, changes in practices, and clinical outcomes satisfaction). These findings may indicate that different outcomes appear if the effects of evidence-based leadership are looked at using different methodological approach. Future study is encouraged using well-designed study method including mixed-method study to examine the consistency between perceived and measured effects of evidence-based leadership in health care.
There is a potential in nursing to support change by demonstrating conceptual and operational commitment to research-based practices [ 64 ]. Nurse leaders are well positioned to influence and lead professional governance, quality improvement, service transformation, change and shared governance [ 65 ]. In this task, evidence-based leadership could be a key in solving deficiencies in the quality, safety of care [ 14 ] and inefficiencies in healthcare delivery [ 12 , 13 ]. As WHO has revealed, there are about 28 million nurses worldwide, and the demand of nurses will put nurse resources into the specific spotlight [ 1 ]. Indeed, evidence could be used to find solutions for how to solve economic deficits or other problems using leadership skills. This is important as, when nurses are able to show leadership and control in their own work, they are less likely to leave their jobs [ 66 ]. On the other hand, based on our discussions with stakeholders, nurse leaders are not used to using evidence in their own work. Further, evidence-based leadership is not possible if nurse leaders do not have access to a relevant, robust body of evidence, adequate funding, resources, and organizational support, and evidence-informed decision making may only offer short-term solutions [ 55 ]. We still believe that implementing evidence-based strategies into the work of nurse leaders may create opportunities to protect this critical workforce from burnout or leaving the field [ 67 ]. However, the role of the evidence-based approach for nurse leaders in solving these problems is still a key question.
Limitations
This study aimed to use a broad search strategy to ensure a comprehensive review but, nevertheless, limitations exist: we may have missed studies not included in the major international databases. To keep search results manageable, we did not use specific databases to systematically search grey literature although it is a rich source of evidence used in systematic reviews and meta-analysis [ 68 ]. We still included published conference abstract/proceedings, which appeared in our scientific databases. It has been stated that conference abstracts and proceedings with empirical study results make up a great part of studies cited in systematic reviews [ 69 ]. At the same time, a limited space reserved for published conference publications can lead to methodological issues reducing the validity of the review results [ 68 ]. We also found that the great number of studies were carried out in western countries, restricting the generalizability of the results outside of English language countries. The study interventions and outcomes were too different across studies to be meaningfully pooled using statistical methods. Thus, our narrative synthesis could hypothetically be biased. To increase transparency of the data and all decisions made, the data, its categorization and conclusions are based on original studies and presented in separate tables and can be found in Additional files. Regarding a methodological approach [ 34 ], we used a mixed methods systematic review, with the core intention of combining quantitative and qualitative data from primary studies. The aim was to create a breadth and depth of understanding that could confirm to or dispute evidence and ultimately answer the review question posed [ 34 , 70 ]. Although the method is gaining traction due to its usefulness and practicality, guidance in combining quantitative and qualitative data in mixed methods systematic reviews is still limited at the theoretical stage [ 40 ]. As an outcome, it could be argued that other methodologies, for example, an integrative review, could have been used in our review to combine diverse methodologies [ 71 ]. We still believe that the results of this mixed method review may have an added value when compared with previous systematic reviews concerning leadership and an evidence-based approach.
Our mixed methods review fills the gap regarding how nurse leaders themselves use evidence to guide their leadership role and what the measured and perceived impact of evidence-based leadership is in nursing. Although the scarcity of controlled studies on this topic is concerning, the available research data suggest that evidence-based leadership intervention can improve nurse performance, organizational outcomes, and patient outcomes. Leadership problems are also well recognized in healthcare settings. More knowledge and a deeper understanding of the role of nurse leaders, and how they can use evidence in their own managerial leadership decisions, is still needed. Despite the limited number of studies, we assume that this narrative synthesis can provide a good foundation for how to develop evidence-based leadership in the future.
Implications
Based on our review results, several implications can be recommended. First, the future of nursing success depends on knowledgeable, capable, and strong leaders. Therefore, nurse leaders worldwide need to be educated about the best ways to manage challenging situations in healthcare contexts using an evidence-based approach in their decisions. This recommendation was also proposed by nurses and nurse leaders during our discussion meeting with stakeholders.
Second, curriculums in educational organizations and on-the-job training for nurse leaders should be updated to support general understanding how to use evidence in leadership decisions. And third, patients and family members should be more involved in the evidence-based approach. It is therefore important that nurse leaders learn how patients’ and family members’ views as stakeholders are better considered as part of the evidence-based leadership approach.
Future studies should be prioritized as follows: establishment of clear parameters for what constitutes and measures evidence-based leadership; use of theories or models in research to inform mechanisms how to effectively change the practice; conducting robust effectiveness studies using trial designs to evaluate the impact of evidence-based leadership; studying the role of patient and family members in improving the quality of clinical care; and investigating the financial impact of the use of evidence-based leadership approach within respective healthcare systems.
Data availability
The authors obtained all data for this review from published manuscripts.
World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. 2020. https://www.who.int/publications/i/item/9789240003279 . Accessed 29 June 2024.
Hersey P, Campbell R. Leadership: a behavioral science approach. The Center for; 2004.
Cline D, Crenshaw JT, Woods S. Nurse leader: a definition for the 21st century. Nurse Lead. 2022;20(4):381–4. https://doi.org/10.1016/j.mnl.2021.12.017 .
Article Google Scholar
Chen SS. Leadership styles and organization structural configurations. J Hum Resource Adult Learn. 2006;2(2):39–46.
Google Scholar
McKibben L. Conflict management: importance and implications. Br J Nurs. 2017;26(2):100–3.
Article PubMed Google Scholar
Haghgoshayie E, Hasanpoor E. Evidence-based nursing management: basing Organizational practices on the best available evidence. Creat Nurs. 2021;27(2):94–7. https://doi.org/10.1891/CRNR-D-19-00080 .
Majers JS, Warshawsky N. Evidence-based decision-making for nurse leaders. Nurse Lead. 2020;18(5):471–5.
Tichy NM, Bennis WG. Making judgment calls. Harvard Business Rev. 2007;85(10):94.
Sousa MJ, Pesqueira AM, Lemos C, Sousa M, Rocha Á. Decision-making based on big data analytics for people management in healthcare organizations. J Med Syst. 2019;43(9):1–10.
Guo R, Berkshire SD, Fulton LV, Hermanson PM. %J L in HS. Use of evidence-based management in healthcare administration decision-making. 2017;30(3): 330–42.
Liang Z, Howard P, Rasa J. Evidence-informed managerial decision-making: what evidence counts?(part one). Asia Pac J Health Manage. 2011;6(1):23–9.
Hasanpoor E, Janati A, Arab-Zozani M, Haghgoshayie E. Using the evidence-based medicine and evidence-based management to minimise overuse and maximise quality in healthcare: a hybrid perspective. BMJ evidence-based Med. 2020;25(1):3–5.
Shingler NA, Gonzalez JZ. Ebm: a pathway to evidence-based nursing management. Nurs 2022. 2017;47(2):43–6.
Farokhzadian J, Nayeri ND, Borhani F, Zare MR. Nurse leaders’ attitudes, self-efficacy and training needs for implementing evidence-based practice: is it time for a change toward safe care? Br J Med Med Res. 2015;7(8):662.
Article PubMed PubMed Central Google Scholar
American Nurses Association. ANA leadership competency model. Silver Spring, MD; 2018.
Royal College of Nursing. Leadership skills. 2022. https://www.rcn.org.uk/professional-development/your-career/nurse/leadership-skills . Accessed 29 June 2024.
Kakemam E, Liang Z, Janati A, Arab-Zozani M, Mohaghegh B, Gholizadeh M. Leadership and management competencies for hospital managers: a systematic review and best-fit framework synthesis. J Healthc Leadersh. 2020;12:59.
Liang Z, Howard PF, Leggat S, Bartram T. Development and validation of health service management competencies. J Health Organ Manag. 2018;32(2):157–75.
World Health Organization. Global Strategic Directions for Nursing and Midwifery. 2021. https://apps.who.int/iris/bitstream/handle/10665/344562/9789240033863-eng.pdf . Accessed 29 June 2024.
NHS Leadership Academy. The nine leadership dimensions. 2022. https://www.leadershipacademy.nhs.uk/resources/healthcare-leadership-model/nine-leadership-dimensions/ . Accessed 29 June 2024.
Canadian Nurses Association. Evidence-informed decision-making and nursing practice: Position statement. 2018. https://hl-prod-ca-oc-download.s3-ca-central-1.amazonaws.com/CNA/2f975e7e-4a40-45ca-863c-5ebf0a138d5e/UploadedImages/documents/Evidence_informed_Decision_making_and_Nursing_Practice_position_statement_Dec_2018.pdf . Accessed 29 June 2024.
Hasanpoor E, Hajebrahimi S, Janati A, Abedini Z, Haghgoshayie E. Barriers, facilitators, process and sources of evidence for evidence-based management among health care managers: a qualitative systematic review. Ethiop J Health Sci. 2018;28(5):665–80.
PubMed PubMed Central Google Scholar
Collins DB, Holton EF III. The effectiveness of managerial leadership development programs: a meta-analysis of studies from 1982 to 2001. Hum Res Dev Q. 2004;15(2):217–48.
Cummings GG, Lee S, Tate K, Penconek T, Micaroni SP, Paananen T, et al. The essentials of nursing leadership: a systematic review of factors and educational interventions influencing nursing leadership. Int J Nurs Stud. 2021;115:103842.
Clavijo-Chamorro MZ, Romero-Zarallo G, Gómez-Luque A, López-Espuela F, Sanz-Martos S, López-Medina IM. Leadership as a facilitator of evidence implementation by nurse managers: a metasynthesis. West J Nurs Res. 2022;44(6):567–81.
Young SK. Evidence-based management: a literature review. J Nurs Adm Manag. 2002;10(3):145–51.
Williams LL. What goes around comes around: evidence-based management. Nurs Adm Q. 2006;30(3):243–51.
Fraser I. Organizational research with impact: working backwards. Worldviews Evidence-Based Nurs. 2004;1:S52–9.
Roshanghalb A, Lettieri E, Aloini D, Cannavacciuolo L, Gitto S, Visintin F. What evidence on evidence-based management in healthcare? Manag Decis. 2018;56(10):2069–84.
Jaana M, Vartak S, Ward MM. Evidence-based health care management: what is the research evidence available for health care managers? Eval Health Prof. 2014;37(3):314–34.
Tate K, Hewko S, McLane P, Baxter P, Perry K, Armijo-Olivo S, et al. Learning to lead: a review and synthesis of literature examining health care managers’ use of knowledge. J Health Serv Res Policy. 2019;24(1):57–70.
Geerts JM, Goodall AH, Agius S, %J SS. Medicine. Evidence-based leadership development for physicians: a systematic literature review. 2020;246: 112709.
Barends E, Rousseau DM, Briner RB. Evidence-based management: The basic principles. Amsterdam; 2014. https://research.vu.nl/ws/portalfiles/portal/42141986/complete+dissertation.pdf#page=203 . Accessed 29 June 2024.
Stern C, Lizarondo L, Carrier J, Godfrey C, Rieger K, Salmond S, et al. Methodological guidance for the conduct of mixed methods systematic reviews. JBI Evid Synthesis. 2020;18(10):2108–18. https://doi.org/10.11124/JBISRIR-D-19-00169 .
Lancet T. 2020: unleashing the full potential of nursing. Lancet (London, England). 2019. p. 1879.
Välimäki MA, Lantta T, Hipp K, Varpula J, Liu G, Tang Y, et al. Measured and perceived impacts of evidence-based leadership in nursing: a mixed-methods systematic review protocol. BMJ Open. 2021;11(10):e055356. https://doi.org/10.1136/bmjopen-2021-055356 .
The Joanna Briggs Institute. Joanna Briggs Institute reviewers’ manual: 2014 edition. Joanna Briggs Inst. 2014; 88–91.
Pearson A, White H, Bath-Hextall F, Salmond S, Apostolo J, Kirkpatrick P. A mixed-methods approach to systematic reviews. JBI Evid Implement. 2015;13(3):121–31.
Johnson RB, Onwuegbuzie AJ. Mixed methods research: a research paradigm whose time has come. Educational Researcher. 2004;33(7):14–26.
Hong, Pluye P, Bujold M, Wassef M. Convergent and sequential synthesis designs: implications for conducting and reporting systematic reviews of qualitative and quantitative evidence. Syst Reviews. 2017;6(1):61. https://doi.org/10.1186/s13643-017-0454-2 .
Ramis MA, Chang A, Conway A, Lim D, Munday J, Nissen L. Theory-based strategies for teaching evidence-based practice to undergraduate health students: a systematic review. BMC Med Educ. 2019;19(1):1–13.
Sackett DL, Rosenberg WM, Gray JM, Haynes RB, Richardson WS. Evidence based medicine: what it is and what it isn’t. Bmj. British Medical Journal Publishing Group; 1996. pp. 71–2.
Goodman JS, Gary MS, Wood RE. Bibliographic search training for evidence-based management education: a review of relevant literatures. Acad Manage Learn Educ. 2014;13(3):322–53.
Aromataris E, Munn Z. Chapter 3: Systematic reviews of effectiveness. JBI Manual for Evidence Synthesis. 2020; https://synthesismanual.jbi.global .
Munn Z, Barker TH, Moola S, Tufanaru C, Stern C, McArthur A et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. 2020;18(10): 2127–33.
Hong Q, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed methods Appraisal Tool (MMAT) Version 2018: user guide. Montreal: McGill University; 2018.
McKenna J, Jeske D. Ethical leadership and decision authority effects on nurses’ engagement, exhaustion, and turnover intention. J Adv Nurs. 2021;77(1):198–206.
Maxwell M, Hibberd C, Aitchison P, Calveley E, Pratt R, Dougall N, et al. The TIDieR (template for intervention description and replication) checklist. The patient Centred Assessment Method for improving nurse-led biopsychosocial assessment of patients with long-term conditions: a feasibility RCT. NIHR Journals Library; 2018.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Pollock A, Campbell P, Struthers C, Synnot A, Nunn J, Hill S, et al. Stakeholder involvement in systematic reviews: a scoping review. Syst Reviews. 2018;7:1–26.
Braye S, Preston-Shoot M. Emerging from out of the shadows? Service user and carer involvement in systematic reviews. Evid Policy. 2005;1(2):173–93.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Reviews. 2021;10(1):1–11.
Porta M. Pilot investigation, study. A dictionary of epidemiology. Oxford University Press Oxford; 2014. p. 215.
Kreis J, Puhan MA, Schünemann HJ, Dickersin K. Consumer involvement in systematic reviews of comparative effectiveness research. Health Expect. 2013;16(4):323–37.
Joseph ML, Nelson-Brantley HV, Caramanica L, Lyman B, Frank B, Hand MW, et al. Building the science to guide nursing administration and leadership decision making. JONA: J Nurs Adm. 2022;52(1):19–26.
Gifford W, Davies BL, Graham ID, Tourangeau A, Woodend AK, Lefebre N. Developing Leadership Capacity for Guideline Use: a pilot cluster Randomized Control Trial: Leadership Pilot Study. Worldviews Evidence-Based Nurs. 2013;10(1):51–65. https://doi.org/10.1111/j.1741-6787.2012.00254.x .
Hsieh HY, Henker R, Ren D, Chien WY, Chang JP, Chen L, et al. Improving effectiveness and satisfaction of an electronic charting system in Taiwan. Clin Nurse Specialist. 2016;30(6):E1–6. https://doi.org/10.1097/NUR.0000000000000250 .
McAllen E, Stephens K, Swanson-Biearman B, Kerr K, Whiteman K. Moving Shift Report to the Bedside: an evidence-based Quality Improvement Project. OJIN: Online J Issues Nurs. 2018;23(2). https://doi.org/10.3912/OJIN.Vol23No02PPT22 .
Thomas M, Autencio K, Cesario K. Positive outcomes of an evidence-based pressure injury prevention program. J Wound Ostomy Cont Nurs. 2020;47:S24.
Cullen L, Titler MG. Promoting evidence-based practice: an internship for Staff nurses. Worldviews Evidence-Based Nurs. 2004;1(4):215–23. https://doi.org/10.1111/j.1524-475X.2004.04027.x .
DuBose BM, Mayo AM. Resistance to change: a concept analysis. Nursing forum. Wiley Online Library; 2020. pp. 631–6.
Lalleman PCB, Smid GAC, Lagerwey MD, Shortridge-Baggett LM, Schuurmans MJ. Curbing the urge to care: a bourdieusian analysis of the effect of the caring disposition on nurse middle managers’ clinical leadership in patient safety practices. Int J Nurs Stud. 2016;63:179–88.
Article CAS PubMed Google Scholar
Martin E, Warshawsky N. Guiding principles for creating value and meaning for the next generation of nurse leaders. JONA: J Nurs Adm. 2017;47(9):418–20.
Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, et al. The association between nurse staffing and omissions in nursing care: a systematic review. J Adv Nurs. 2018;74(7):1474–87. https://doi.org/10.1111/jan.13564 .
Lúanaigh PÓ, Hughes F. The nurse executive role in quality and high performing health services. J Nurs Adm Manag. 2016;24(1):132–6.
de Kok E, Weggelaar-Jansen AM, Schoonhoven L, Lalleman P. A scoping review of rebel nurse leadership: descriptions, competences and stimulating/hindering factors. J Clin Nurs. 2021;30(17–18):2563–83.
Warshawsky NE. Building nurse manager well-being by reducing healthcare system demands. JONA: J Nurs Adm. 2022;52(4):189–91.
Paez A. Gray literature: an important resource in systematic reviews. J Evidence-Based Med. 2017;10(3):233–40.
McAuley L, Tugwell P, Moher D. Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet. 2000;356(9237):1228–31.
Sarah S. Introduction to mixed methods systematic reviews. https://jbi-global-wiki.refined.site/space/MANUAL/4689215/8.1+Introduction+to+mixed+methods+systematic+reviews . Accessed 29 June 2024.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Download references
Acknowledgements
We want to thank the funding bodies, the Finnish National Agency of Education, Asia Programme, the Department of Nursing Science at the University of Turku, and Xiangya School of Nursing at the Central South University. We also would like to thank the nurses and nurse leaders for their valuable opinions on the topic.
The work was supported by the Finnish National Agency of Education, Asia Programme (grant number 26/270/2020) and the University of Turku (internal fund 26003424). The funders had no role in the study design and will not have any role during its execution, analysis, interpretation of the data, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Nursing Science, University of Turku, Turku, FI-20014, Finland
Maritta Välimäki, Tella Lantta, Kirsi Hipp & Jaakko Varpula
School of Public Health, University of Helsinki, Helsinki, FI-00014, Finland
Maritta Välimäki
Xiangya Nursing, School of Central South University, Changsha, 410013, China
Shuang Hu, Jiarui Chen, Yao Tang, Wenjun Chen & Xianhong Li
School of Health and Social Services, Häme University of Applied Sciences, Hämeenlinna, Finland
Hunan Cancer Hospital, Changsha, 410008, China
Gaoming Liu
You can also search for this author in PubMed Google Scholar
Contributions
Study design: MV, XL. Literature search and study selection: MV, KH, TL, WC, XL. Quality assessment: YT, SH, XL. Data extraction: JC, MV, JV, WC, YT, SH, GL. Analysis and interpretation: MV, SH. Manuscript writing: MV. Critical revisions for important intellectual content: MV, XL. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Xianhong Li .
Ethics declarations
Ethics approval and consent to participate.
No ethical approval was required for this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Differences between the original protocol
We modified criteria for the included studies: we included published conference abstracts/proceedings, which form a relatively broad knowledge base in scientific knowledge. We originally planned to conduct a survey with open-ended questions followed by a face-to-face meeting to discuss the preliminary results of the review. However, to avoid extra burden in nurses due to COVID-19, we decided to limit the validation process to the online discussion only.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, supplementary material 4, supplementary material 5, supplementary material 6, supplementary material 7, supplementary material 8, supplementary material 9, supplementary material 10, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Välimäki, M., Hu, S., Lantta, T. et al. The impact of evidence-based nursing leadership in healthcare settings: a mixed methods systematic review. BMC Nurs 23 , 452 (2024). https://doi.org/10.1186/s12912-024-02096-4
Download citation
Received : 28 April 2023
Accepted : 13 June 2024
Published : 03 July 2024
DOI : https://doi.org/10.1186/s12912-024-02096-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based leadership
- Health services administration
- Organizational development
- Quality in healthcare
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Role of Public Health Nurse Expository Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Public health nursing as a career is concerned with the general well-being of populations. The general role of a public health nurse is the promotion of the well-being of persons as far as health is concerned by use of the knowledge of nursing, social sciences, as well as public health sciences.
Due to the broadness of this role, public health nurses are expected to promote health in various categories which defines the individual roles of a public health nurse. Although the overall objective of the public health nursing profession is the promotion of the public health, the approaches employed by a public health nurse who works in a school environment differs form the roles of a public health nurse who works in a parish or in a health facility. The paper will examine the roles of public health nursing in schools and in the community.
The first role of a public health nurse in a school is to promote the overall health of the school population (Lancaster, 2008, pp 1043). A public health nurse who works in a school environment helps in the overall promotion of health by helping in health policy formulation at the school level.
This way, public health nurses in school environments as well as in other working environments provide vital inputs to all interdisciplinary programs tasked with the roles of evaluation, monitoring and anticipation of various health problems in order to formulate formidable responses to health challenges. The nurses are also expected to evaluate the environmental health challenges that may affect the area of operation.
Public health nurses in schools are also expected to promote children’s health through the observance of children’s behavior and further advice on the best approaches that can improve their health. Some of the practices that the public health nurses that work in schools are expected to accomplish includes the coordination of immunization programs both at school level and to coordinate with local communities to ensure that the children who are of the school going age are immunized.
School based public health nurses are usually employed by school districts or by other relevant school management board. However, the use of school district as the principal employing unit is higher than it is done by other employers. School-based nurses can also be staffed through the family nurse practitioner program. The main mission of all organizations that hires school based community health nurses is to improve the overall health positions of the school going children (Lundy & Janes, 2009, pp 76).
Another category of community health nurse is the community oriented nurse and consultant. Community-oriented nurse and consultant have the role of a change agent. They are also expected to offer their advice to various stakeholders to ensure that the community is running in a way that is agreeable to the goals of community health nursing (Lancaster, 2008, pg 1017).
It is the role of a public health nurse in the community to promote the application of health sciences as well as the knowledge of social sciences through relevant interventions (Lancaster, 2008, pg 1012). They also integrate their community of practice into programs that would promote their understanding of health issues especially by the aid of family experiences. As change agents, they champion the desired change at their community of practice hence promoting the overall well-being of the society.
The organization that registers community health nurses is the American Public Health Association where aspiring members are expected to complete the relevant courses, pass the entry exams and pay the required subscription amount for membership. Once a person joins, he/she is expected to adhere to the codes of professional conduct of the organization and remain professional while offering services.
Currently, the organization has over 50,000 health professions. It also boasts as the oldest organization of health professionals. The vision of this organization is to have “A Healthy Global Society” while its mission is to “Improve the health of the public and achieve equity in health status” (American Public Health Association, 2011 para 3 and 4).
In conclusion, it is evident that public health nurses play a vital role in the promotion of overall health of the populations. Although the overall objective of public health nurses is to improve the overall health of the populations, each category of health nurses has its own area of interest which makes the approaches employed by each of the approaches different. The subdivision of public health nursing is vital in that it helps in the overall performance of the public health nurses.
American Public Health Association. (2011). American Public Health Association : Overview. Web.
Lancaster, S., M. (2008). Community and Public Health Nursing. 7 th Ed. St. Louis: Mosby.
Lundy, K., S. & Janes S. (2009). Community health nursing: caring for the public’s health. New York: Jones & Bartlett Learning.
- Management Consultant: Developing Strategic Plan
- Virtual School Consultant Project
- Duties of a Professional Consultant
- Areas of Potential Liability for the Advanced Practice Nurse
- Nursing and Philosophy
- The Overview of Nursing Association in the US
- Reduce Hospitalization of Nursing Home Residents
- Impact of Transcultural Nursing Society Website on Nursing Health Care
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, October 10). Role of Public Health Nurse. https://ivypanda.com/essays/role-of-public-health-nurse/
"Role of Public Health Nurse." IvyPanda , 10 Oct. 2018, ivypanda.com/essays/role-of-public-health-nurse/.
IvyPanda . (2018) 'Role of Public Health Nurse'. 10 October.
IvyPanda . 2018. "Role of Public Health Nurse." October 10, 2018. https://ivypanda.com/essays/role-of-public-health-nurse/.
1. IvyPanda . "Role of Public Health Nurse." October 10, 2018. https://ivypanda.com/essays/role-of-public-health-nurse/.
Bibliography
IvyPanda . "Role of Public Health Nurse." October 10, 2018. https://ivypanda.com/essays/role-of-public-health-nurse/.
School of Nursing
- Which Program is Right for Me Overview
- Comparing the PhD & DNP
- Technical Standards
- Bachelor of Science in Nursing
- Master of Nursing
- PhD in Nursing
- Doctor of Nursing Practice
- Certificate Overview
- Adult Gerontological Acute Care Nurse Practitioner Certificate
- Leadership in Health Information Technology for Health Professionals Certificate
- Population Health Informatics and Technology (PHIT) Certificate
- Post-Graduate Certificate Program Overview
- Meet Our Students
- Current Student Resources
- Office of Student & Career Advancement Services
- Research Overview
- Research Projects
- Research Day
- Faculty Grants
- Faculty Experts
- Laboratory of Clinical Exercise Physiology
- Publications Overview
- Books by Faculty
- Research Seminars
- Student Research Resources
- About the Office of Nursing Research and Scholarship
- News & Events Overview
- Minnesota Nursing Magazine Overview
- Current Issue
- Magazine Issue Archive
- Clinical Preceptors Overview
- BSN/MN (Prelicensure) Preceptor Information
- DNP Preceptor Information
- Clinical Preceptor e-Toolkit
- Nurse-midwifery specialty
- DNP Project Ideas
- Nurse Practitioners Clinic
- School of Nursing at a Glance
- School of Nursing Leadership
- Our Faculty
- Faculty Emeriti & Faculty Ad Honorem
- Cooperatives
- Faculty Honors and Awards
- Employment Opportunities
- Our Facilities Overview
- Bentson Health Communities Innovation Center
- Bakken Center for Spirituality and Healing
- Global Health Overview
- Visiting Scholars
- Global Collaborations
- Global Health Faculty Scholars
- Opportunities for Students
- Inclusivity, Diversity & Equity
- Professional Development
- Giving to Nursing Overview
- Areas of Need
- Scholarships
- Impact Stories
- Ways to Give
- Board of Trustees
- History Overview
- Heritage Committee
- History of Our School Leadership
- Program Histories
- Historical Videos and Photos
- Sigma Theta Tau International Overview
- Zeta Chapter Board
- Grants & Awards
- Volunteer Opportunities
- Alumni Overview
- Submit a Class Note
- Alumni Society Awards Overview
- Rising Star Award
- Distinguished Alumni Humanitarian Award
- Excellence in Practice Award
- Board of Directors
- Degree Verification
- Volunteering
- Centers Overview
- Center for Adolescent Nursing Overview
- Center Projects
- Learning Opportunities
- Publications
- Center for Aging Science & Care Innovation Overview
- Center for Child and Family Health Promotion Research Overview
- Get Connected
- Center projects
- Center for Nursing Informatics Overview
- 2024 Nursing Knowledge: Big Data Science Conference
- Previous Conferences
- Nursing Knowledge Big Data Science Initiative
- Center for Planetary Health and Environmental Justice Overview
- Katharine J. Densford International Center for Nursing Leadership Overview
- Leadership Model
- Directorate
- Initiatives
- Contact the Center
- 2024 Planting Seeds of Innovation Colloquium
Mueller receives Doris Schwartz Gerontological Nursing Research Award
July 9, 2024

Professor Christine Mueller, PhD, RN, FGSA, FAAN, was named the recipient of the prestigious Doris Schwartz Gerontological Nursing Research Award by the Gerontological Society of America (GSA).
The award is presented to a GSA member who has a record of outstanding and sustained contribution to geriatric nursing research.
Mueller is a nationally recognized nurse scientist with expertise in the quality of care for residents in nursing homes as influenced by nurses and organizational factors like staffing and leadership.
The GSA is the country’s largest interdisciplinary organization devoted to the field of aging.
The award presentation will take place at GSA’s 2024 Annual Scientific Meeting, which will be held from Nov. 13-16 in Seattle, Washington.
Categories: School News
Media Contacts
Related stories.

As nursing homes prep for the new staffing mandate, optimizing the role of the RN should also be considered
After decades of advocacy, the Centers for Medicare and Medicaid Services (CMS) released a highly anticipated final rule in April that creates requirements for 24-hour, 7-day a week registered nurse (RN) staffing at nursing homes as well as setting a minimum of .55 hours per resident day of RN staffing.

Nursing Knowledge: Big Data Science Conference focuses on AI, ethics and innovation
This year’s conference, held June 5-7 at McNamara Alumni Center, explored artificial intelligence (AI), nursing innovations, and the ethical implications of using technologies for nursing care.

Eccles elected secretary of National Forum of State Nursing Workforce Centers board
Jennifer Eccles, PhD, RN, FAADN, was elected to serve as secretary of the National Forum of State Nursing Workforce Centers board of directors.
- Admission Requirements
- Required Courses
- Admissions Requirements
- How to Apply
- Post-Graduate Certificate Program Plans by Specialty
- Message from the Dean
- Board of Visitors
- Adult & Gerontological Health
- Child & Family Health
- Population Health & Systems
- Tenured Faculty Opportunities
- Tenure-Track Faculty
- Clinical Track Faculty Opportunities
- Postdoctoral Fellowship Program
- Guidance for Applicants for faculty positions
- Marie Manthey Endowed Professorship
- Leaving a Nursing Legacy
- 100 Distinguished Nursing Alumni (A-E)
- 100 Distinguished Nursing Alumni (F-J)
- 100 Distinguished Nursing Alumni (K-O)
- 100 Distinguished Nursing Alumni (P-T)
- 100 Distinguished Nursing Alumni (U-Z)
- Distinguished Faculty Alumni
- Program Histories Overview
- Adult-Gero Nurse Practitioner Programs
- DNP Program
- Geriatric Nurse Practitioner/Geriatric Clinical Nurse Specialist
- Health Innovation and Leadership
- Integrative Health and Healing
- Master of Nursing Administration
- Nurse Anesthesia
- Nurse Midwifery
- Nursing Informatics
- Pediatric Primary Care Nurse Practitioner
- PhD Program
- Practical Nursing Program
- Pre-licensure programs
- Psychiatric-Mental Health
- Public Health Nursing
- Women's Health Nurse Practitioner
- Evidence-based Practice Grants
- Research Grants
- Travel Grants
- Summer Institute in Adolescent Health
- Past Summer Institutes in Adolescent Health
- Clinical Teaching in Nursing Homes
- Resources for Clinical Teaching in Nursing Homes
- Competencies for Public Health Nursing Practice Instrument
- Doctoral Education Pathway for American Indian/Alaska Native Nurses
- Accreditation
- Call for Abstracts
- Registration
- Online Teaching Resources
- 2022 Nursing Knowledge: Big Data Science Conference
- 2020 Nursing Knowledge: Big Data Science Conference
- 2019 Workgroups
- 2018 Workgroups
- 2017 Nursing Knowledge: Big Data Science Conference
- 2016 Workgroups
- 2015 Workgroups
- 2014 Nursing Knowlege: Big Data Science Conference
- 2013 Nursing Knowledge: Pre-conference Materials
- Vision and Mission
- Five-Year Strategic Plan
- Steering committee
- Resources for Workgroup Members
- Nursing Knowledge: Big Data Science Conference
- Nursing Big Data Repository
- Contact information and social media
- Foresight Leadership
The Role and Impact of Muckraking in Journalism
This essay is about muckraking a form of investigative journalism that emerged in the early 20th century to expose corruption scandal and injustices in society. It discusses how muckrakers like Upton Sinclair Ida Tarbell and Lincoln Steffens revealed unethical practices in industries and governments leading to significant social and political reforms. The essay highlights the role of publications that supported muckraking and its lasting influence on modern investigative journalism. Despite criticisms regarding ethical boundaries and sensationalism muckraking remains crucial for promoting accountability and transparency contributing to justice and integrity in society.
How it works
Muckraking a term cooked up back in the early 1900s is all about digging deep into society’s dirt to expose corruption scandals and unfairness. It was a big deal during the Progressive Era in the United States when it really shook things up in social political and economic circles. President Theodore Roosevelt even called these reporters “Man with the Muck-rake” likening them to a character from John Bunyan’s “Pilgrim’s Progress” who was more interested in society’s mess than its good bits.
Muckraking was all about finding the truth and making sure folks in power were held accountable. Journalists doing this work were driven by a sense of fairness wanting to let the public know what was really going on behind closed doors. It wasn’t just about grabbing attention—it was about making real changes by digging deep and telling it like it is.
One of the most famous muckrakers was Upton Sinclair. His book “The Jungle” painted a grim picture of how meatpacking plants in Chicago were treating workers and handling food. People were shocked by his vivid descriptions and it sparked a huge outcry. Thanks to Sinclair’s work laws like the Pure Food and Drug Act and the Meat Inspection Act were passed in 1906 to make sure our food was safe and clean.
Ida Tarbell was another big name in muckraking. She went after the Standard Oil Company and how it was taking over the oil industry. Her detailed investigation in “The History of the Standard Oil Company” exposed all the sneaky ways John D. Rockefeller was using to squash competition and control everything. Her work was a big reason why Standard Oil got busted up in 1911 showing just how much impact muckraking could have on business and government rules.
Then there’s Lincoln Steffens who aimed his pen at political corruption in American cities. His articles put together in “The Shame of the Cities” laid bare how crooked city governments were and how big businesses were in on the game. Steffens’ work got folks fired up about cleaning up politics and making things more fair and open.
Muckraking wasn’t just about individual reporters—it was a whole movement that found a home in magazines like “McClure’s” “Collier’s” and “Everybody’s Magazine.” These magazines gave muckrakers a platform to share their findings with a wide audience. They played a key role in getting people riled up and ready for change stirring the pot for social and political reforms.
Today muckraking lives on in the spirit of investigative journalism. Reporters still dig into stories about big companies doing wrong government officials bending the rules and unfairness in society. They stick to the same principles: digging deep telling the truth and looking out for the public good. Just look at Bob Woodward and Carl Bernstein who broke the Watergate scandal wide open leading to President Nixon stepping down. More recently the Panama Papers blew the lid off global tax dodging and corruption.
But muckraking isn’t without its critics. Some say muckrakers sometimes go too far crossing ethical lines to get their story. Others worry that flashy headlines might overshadow the real issues. Still these criticisms don’t take away from how important muckraking is for keeping folks honest and making sure everyone plays by the rules.
In the end muckraking has been a game-changer in journalism pushing for big changes in how our society works. Thanks to muckrakers we’ve seen corruption brought to light important issues raised and laws changed for the better. It’s a reminder that as long as there’s unfairness to uncover and truths to tell muckraking will keep on being a crucial part of keeping our society fair and free.
Cite this page
The Role and Impact of Muckraking in Journalism. (2024, Jul 06). Retrieved from https://papersowl.com/examples/the-role-and-impact-of-muckraking-in-journalism/
"The Role and Impact of Muckraking in Journalism." PapersOwl.com , 6 Jul 2024, https://papersowl.com/examples/the-role-and-impact-of-muckraking-in-journalism/
PapersOwl.com. (2024). The Role and Impact of Muckraking in Journalism . [Online]. Available at: https://papersowl.com/examples/the-role-and-impact-of-muckraking-in-journalism/ [Accessed: 11 Jul. 2024]
"The Role and Impact of Muckraking in Journalism." PapersOwl.com, Jul 06, 2024. Accessed July 11, 2024. https://papersowl.com/examples/the-role-and-impact-of-muckraking-in-journalism/
"The Role and Impact of Muckraking in Journalism," PapersOwl.com , 06-Jul-2024. [Online]. Available: https://papersowl.com/examples/the-role-and-impact-of-muckraking-in-journalism/. [Accessed: 11-Jul-2024]
PapersOwl.com. (2024). The Role and Impact of Muckraking in Journalism . [Online]. Available at: https://papersowl.com/examples/the-role-and-impact-of-muckraking-in-journalism/ [Accessed: 11-Jul-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
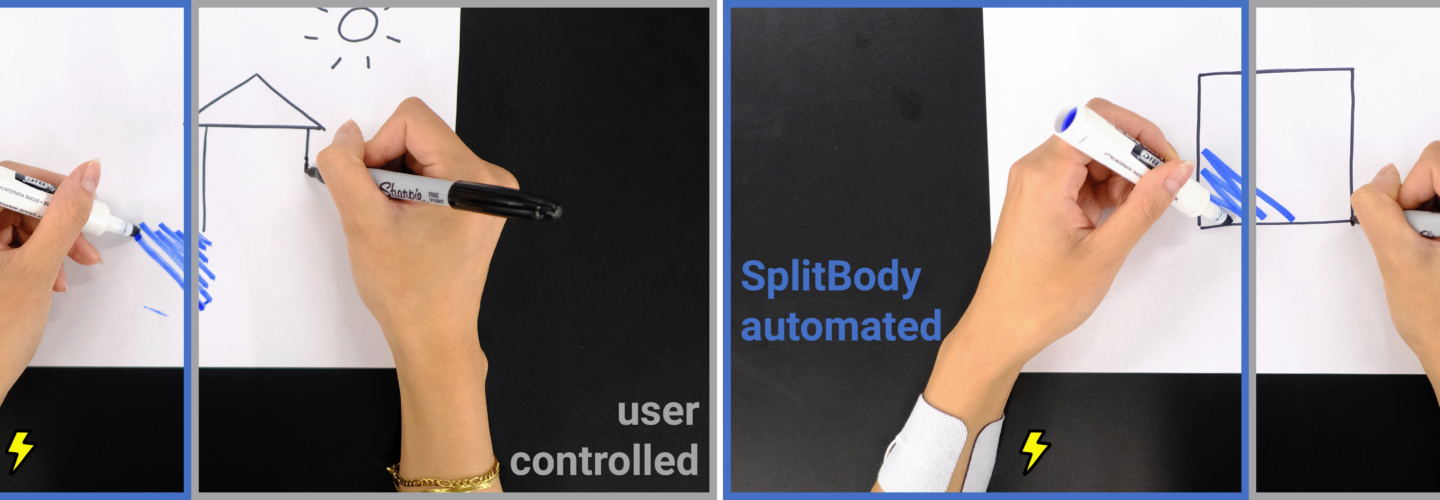
Enhancing Multitasking Efficiency: The Role of Muscle Stimulation in Reducing Mental Workload
As society becomes increasingly efficient and connected, people experience the mounting pressure to be as productive as they can be at all times. This has often led to multitasking, which is a key feature of almost all computer interfaces—they allow us to more easily and quickly perform many tasks at once. However, the same cannot be said for physical tasks. For example, imagine cooking and drafting an essay at the same time — here computing technologies do not provide much in the way of assistance to ease the burden of concentrating on the two physical tasks. In Associate Professor Pedro Lopes ’ Human Computer Integration lab at the University of Chicago’s Department of Computer Science , fifth-year PhD student Romain Nith and incoming PhD student Yun Ho wondered whether it was possible to partially automate the multitasking process by incorporating muscle stimulation technology.
Electrical muscle stimulation has been used for decades in the field of rehabilitation and physiotherapy. It consists of delivering a small electrical impulse via electrodes placed on the user’s skin, atop of a muscle. This causes the muscle to involuntary contract. In other words, it moves the body via electricity. Although Nith received his Bachelors in computer engineering at McGill University, he had the opportunity to work on a muscle stimulation project through Lopes’ lab as his senior capstone. This internship encouraged him to further pursue his interest in muscle stimulation by joining Lopes’ lab as a PhD student.
“The lab works a lot with muscle stimulation, but always in a way that it performs tasks for the user, e.g., you are trying to gesture in sign language and the muscle stimulation completes the gesture for you,” Nith said referring to his past work at ACM UIST 2021 (which is also featured in the Guinness Book of World Records ) . “However, for SplitBody , we took a different turn from the existing applications of muscle stimulation. One day we thought, what if we put this in the background and automate some repetitive task? We decided to conduct a user study to find out if people actually do multitask better with muscle stimulation.”
In their recent paper titled SplitBody: Reducing Mental Workload while Multitasking via Muscle Stimulation , Nith and Ho studied whether electrical muscle stimulation (EMS) would ultimately be more or less distracting for a user that is performing two demanding physical tasks at once (multitasking). They designed a user study that involved both a cognitive task (dominant hand) and a movement task (non-dominant hand). The cognitive task involved the use of a 2-back test, where participants were given a series of letters and asked to recall if the current letter matched a previous letter. The movement task involved doing a sequence of hand gestures (up, down, left, right) in a non-repetitive order. The twelve participants were asked to perform the multitask twice, once as a baseline, or control, experiment where the participant performed the multitask by themselves. In the second experiment, EMS was used to perform the second task.

Lopes envisions a new world of interfaces enabled by these findings. “Computers have transformed the way people learn cognitive skills, but haven’t done much for physical skills,” he stated. “The best interface these days for a new skill is watching a video. But with our body-integrated devices that directly move the user’s body, we can enable someone to learn a complex physical skill piece by piece. For example, in one of our demonstrations, you can learn how to play the drums by having the muscle stimulation take care of the tricky musical parts that you cannot multitask, like the syncopation between the cymbal and the kick drum, while you focus on a simpler movement such as playing the snare—this is a completely new way to have interfaces that act on the real world and assist us with physical tasks”.
In addition to refining the tests for the multitask, Nith and Ho also heavily considered the safety and ethics of conducting such an experiment. In their paper, they stated that “any interactive system with the capability of moving the body must be ethically designed by grounding it in the principles of user-agency & safety”. They intentionally designed the SplitBody EMS system to be easily activated and deactivated by the participant themselves, emphasizing the user’s own agency during the process. The authors only used external methods of application to connect the SplitBody hardware. Most importantly, the system ensures that the user’s limbs remain under their full control by only activating a subset of muscles for each task with measures to override and turn off the stimulation.
“There are robots that vacuum for you, like the Roomba,” Nith explained. “Some robots are cooking for you. Our phone automates a lot of things. And now we’re moving to automation in the cloud, like ChatGPT. All that is great, but the issue is that the user is losing agency — sometimes you don’t even know that these things are happening in the background. With this project, we tried to give back to the user some of that agency while still keeping the automation part of the conversation.”
Ultimately, EMS was found to increase the efficiency of multitasking, but there is a lot more to explore. To dive deeper into this topic, Nith and Ho are interested in exploring how muscle stimulation affects the user and how it could be made more transparent and trustworthy to the user. Nith is also keen on investigating whether EMS could be used to teach specific motor skills, such as playing the piano or drumming. To learn more about Nith and his work at the Human Computer Integration lab, please visit their website here .
Related News

Unveiling Attention Receipts: Tangible Reflections on Digital Consumption

University of Chicago Computer Science Researchers To Present Ten Papers at CHI 2024
FabRobotics: The Fusion of 3D Printing and Mobile Robots

High School Students In The Collegiate Scholars Program Get To Know Robots
UChicago Computer Scientists Design Small Backpack That Mimics Big Sensations
Computer Science Class Shows Students How To Successfully Create Circuit Boards Without Engineering Experience

UChicago CS Researchers Shine at CHI 2023 with 12 Papers and Multiple Awards

New Prototypes AeroRigUI and ThrowIO Take Spatial Interaction to New Heights – Literally

Computer Science Displays Catch Attention at MSI’s Annual Robot Block Party

UChicago, Stanford Researchers Explore How Robots and Computers Can Help Strangers Have Meaningful In-Person Conversations

High School Students Find Their Place in Computing Through Wearables Workshop

UChicago CS Researchers Create Living Smartwatch to Explore Human-Device Relations
Advertisement
Justices Limit Power of Federal Agencies, Imperiling an Array of Regulations
A foundational 1984 decision had required courts to defer to agencies’ reasonable interpretations of ambiguous statutes, underpinning regulations on health care, safety and the environment.
- Share full article

By Adam Liptak
Reporting from Washington
- June 28, 2024
The Supreme Court on Friday reduced the power of executive agencies by sweeping aside a longstanding legal precedent, endangering countless regulations and transferring power from the executive branch to Congress and the courts.
The precedent, Chevron v. Natural Resources Defense Council , one of the most cited in American law, requires courts to defer to agencies’ reasonable interpretations of ambiguous statutes. There have been 70 Supreme Court decisions relying on Chevron, along with 17,000 in the lower courts.
The decision is all but certain to prompt challenges to the actions of an array of federal agencies, including those regulating the environment, health care and consumer safety.
The vote was 6 to 3, dividing along ideological lines.
“Chevron is overruled,” Chief Justice John G. Roberts Jr. wrote for the majority. “Courts must exercise their independent judgment in deciding whether an agency has acted within its statutory authority.”
In dissent, Justice Elena Kagan said the ruling amounted to a judicial power grab. “A rule of judicial humility,” she wrote, “gives way to a rule of judicial hubris.”
Justice Kagan summarized her dissent from the bench, a rare move and a sign of profound disagreement. “Courts, in particular this court, will now play a commanding role” in setting national policy, she said.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

COMMENTS
REASON #13: Nurses Empower Patients. It is not only a nurse's job to care for patients when they are sick or weak, but it is also our job to empower patients to become as independent as possible and able to care for themselves. This process of empowering patients looks different from patient to patient.
The Role of Nurses in Improving Health Equity. Being a nurse … in 2020 must mean being aware of social injustices and the systemic racism that exist in much of nursing … and having a personal and professional responsibility to challenge and help end them. —Calvin Moorley, RN, and colleagues, "Dismantling Structural Racism: Nursing Must ...
Neuman (2012) notes that this profession is dynamic and is evolving along with social needs and trends. In this paper, I describe the expanding role of the nurse in society and potential areas of my efforts to advocate for patients and influence positive social change in health care. Get a custom essay on Nurses Are Changing the World and Society.
This essay will discuss the critical role nurses play in society. It will cover their impact on patient care, public health, and community well-being. The piece will highlight the diverse roles nurses fulfill and how they contribute significantly to the healthcare system and patient outcomes.
nursing because society and the public widely accepted their role but through the ever-evolv-ing profession, men have made their presence known and the value they bring to the care for patients. They ensure that male patients feel represented and their needs addressed by indi-viduals that look like them. Currently, nurses play a huge role in the
of the health and social inequities affecting communities across the nation, the COVID-19 pandemic, along with other health crises, such as the opioid epidemic (Abellanoza et al., 2018), presents an opportunity to take a critical look at the nursing profession, and society at large, and work collaboratively to enable all individuals to have a fair and just opportunity for health and well-being ...
Attempts to shape nursing work have lacked understanding of how nurses contribute to healthcare, with negative consequences. For example, the recent introduction of Nursing Associate roles (Department of Health and Social Care, 2017) in the UK, ostensibly to be a compassionate, patient-facing role and reduce costs, overlooks evidence that replacing registered nurses with other providers leads ...
Nurses are the foundation of healthcare. They play a vital role in providing care, comfort and compassion for their patients and patients' families. Despite their caring demeanor, nurses would rather not see you in the hospital. Preventive healthcare is their priority for patients — getting regular checkups and keeping health concerns from ...
NURSES' ROLES IN EXPANDING ACCESS TO QUALITY HEALTH CARE. The United States spends more than $3.5 trillion per year on health care, 25 percent more per capita than the next highest-spending country, and under-performs on nearly every metric (Emanuel et al., 2020).Life expectancy, infant mortality, and maternal mortality are all worse in the United States than in most developed countries.
Assumption two. Society can expect each nurse to accept and value all persons as equal, worthy of respect and with intrinsic worth, regardless of all other considerations.. Nurses are formatively educated with a holistic and generalist framework that sets the background for a career that embraces diverse roles in diverse settings with and for diverse people, anywhere and in whatever roles to ...
Nursing is complex and multifaceted; nurses work across all fields—at home, close to home and in hospital (Health Education England, 2017).'Registered nurse' is a legally protected title in the UK, yet there is still no clear definition. In addition, the term 'nurse' is not a protected title but whether this should be regulated is a ...
To understand the role of practitioners in society, one needs to understand the process of becoming a nurse and their responsibilities in the healthcare sector. This essay is based on information acquired from a practicing nurse who shared insightful knowledge of the profession. Get a custom essay on Nursing Profession: Nurse Profile Essay.
Health Promotion: The Role of Nurses Essay. Nurses play a significant role in the promotion of health in the public sector. Each community has its own different culture, values, and beliefs. In this scenario, a nurse's work is to understand the principles and views of the community in which they are practicing their clinical work (Murdaugh et ...
The American Nurses Association lists advocacy as a "pillar of nursing" and considers it one of the most significant reasons why nurses are important in healthcare. The advocacy role of a nurse can take many forms too. For example, when speaking with a patient's family member, a nurse might uncover a critical detail not reflected in the ...
Journal of Advanced Nursing 66(4), 743-752. doi: 10.1111/j.1365-2648.2009.05226.x BEGLEY C. (2010) Abstract Title. The role of the public health nurse in a changing society. Aim. This study is a report of a study to clarify the role of the public health nurse in one Irish community care area in the light of acknowledged problems in defining ...
A personal essay on the role of the nurse. L INDA SHIELDS. T ropical Health Research Unit, James Cook University and T ownsville Health District, Townsville, QLD, Australia; School of Medicine ...
Nurses promote healthy lifestyles, advocate for patients and provide health education. They also provide direct patient care. As key members of healthcare teams, they provide our communities with the knowledge needed for healthy living. The exact roles of nurses have changed somewhat over the years, but their importance in healthcare remains ...
Nursing is responsible to society through its mission to serve the public interest: specifically, the overall health of our society. As healthcare remains a major focus in the United States, nurses are being thrust into societal leadership roles pertaining to our health and healthcare. In effect, nurses today are being asked not to act as ...
Nurses have a range of roles and responsibilities in order to provide society with the highest quality of care (Peate, 2016). The Royal College of Nursing (RCN, 2014:3) define nursing as the ability to 'improve, maintain, or recover health, to cope with health problems, and to achieve the best quality of life' for patients until their death.
Summary. In the essay "The Role of Nursing in Society" the author analyzes nursing as exceptional expertise in the field of medical health care. Early civilizations view nursing as a vital service to humanity especially along with the preservation of life, as well as the continued existence of the human race….
A personal essay on the role of the nurse Contemp Nurse. 2013 Feb;43(2) :213-8. doi ... it appears that Australian nurses, as with many sections of Australian society, do not recognize that they hold high professional standards. With the influence of the international nursing shortage and the ever-growing technological advances within health ...
Global health demands have set new roles for nurse leaders [].Nurse leaders are referred to as nurses, nurse managers, or other nursing staff working in a healthcare context who attempt to influence the behavior of individuals or a group based on goals that are congruent with organizational goals [].They are seen as professionals "armed with data and evidence, and a commitment to mentorship ...
Nursing Role in the Society Nurses are the care professions who are a part of a health care team. They play a substantial role in quality of patient care. The core of nursing is patient care and patient advocay. Nurses are increasingly working to promote people's health and prevent illness from hospital setting to community health.
Essay Example: Nurse Ratched the infamous antagonist in Ken Kesey's "One Flew Over the Cuckoo's Nest" is a character whose presence is as chilling as it is pivotal. Often referred to as "Big Nurse" her role as the head nurse in a mental institution transcends the boundaries of a mere healthcare
The general role of a public health nurse is the promotion of the well-being of persons as far as health is concerned by use of the knowledge of nursing, social sciences, as well as public health sciences. Get a custom essay on Role of Public Health Nurse. Due to the broadness of this role, public health nurses are expected to promote health in ...
The award is presented to a GSA member who has a record of outstanding and sustained contribution to geriatric nursing research. Mueller is a nationally recognized nurse scientist with expertise in the quality of care for residents in nursing homes as influenced by nurses and organizational factors like staffing and leadership.
The essay highlights the role of publications that supported muckraking and its lasting influence on modern investigative journalism. Despite criticisms regarding ethical boundaries and sensationalism muckraking remains crucial for promoting accountability and transparency contributing to justice and integrity in society.
The paper envisions several applied scenarios where EMS may be helpful. Split-chef involves preparing caramel while writing an essay, Split-draw enables synchronous shadow drawing and coloring while sketching, Split-drum involves learning to drum one limb at a time, and Split-musician involves alternating foreground and background musical tasks. In all of these examples, one movement is the ...
A foundational 1984 decision had required courts to defer to agencies' reasonable interpretations of ambiguous statutes, underpinning regulations on health care, safety and the environment.