Cookies on this website
We use cookies to ensure that we give you the best experience on our website. If you click 'Accept all cookies' we'll assume that you are happy to receive all cookies and you won't see this message again. If you click 'Reject all non-essential cookies' only necessary cookies providing core functionality such as security, network management, and accessibility will be enabled. Click 'Find out more' for information on how to change your cookie settings.

- Institutes and units

Oxford Institute of Digital Health
Connected health for better health
This dynamic, interdisciplinary hub for digital health research and teaching address es critical challenges and identif ies solutions harnessing innovations to improve health and health care.
The rapid development of digital technologies is a catalyst for a fundamental shift in both how we live, and how we manage our health. The digital transformation of health systems has the potential to deliver leaner, greener, and more person-centered services. The Oxford Institute of Digital Health is a forward thinking, interdisciplinary, and collaborative hub across academia, industry, health systems, and government agencies to ensure maximum social impact through the shaping of the future of health and health care.
It will harness digital technologies to provide solutions to some of the biggest health challenges for individuals and populations. To create an enduring legacy, the Institute will:
• unite disciplines and sectors to harness digital technology to tackle the health challenges of the twenty-first century;
• provide international leadership in this vital area for the future of health systems;
• develop much needed global capacity through a training pipeline of Master’s and Doctoral students; and
• undertake world-leading research using innovative methods with national and international collaborators.
In the first five years the Institute will focus on transforming primary care and public health in areas where health disparities are most pressing. Based in the Nuffield Department of Primary Care Health Sciences, it will leverage considerable expertise in data science and artificial intelligence, an outstanding track record in the development and evaluation of digital health technology, and leading work investigating the social and ethical aspects of health care to improve patient care and experience across areas such as cardiovascular diseases, mental health, and work with marginalised populations.
Our vision is for digital health to enable those at most risk of illness to be identified and treated earlier and given the tools to manage their health and care better. Richard Hobbs, Head of Department
Supporting the Oxford Institute of Digital Health
HOW YOU CAN HELP – GIVING TO THE OXFORD INSTITUTE OF DIGITAL HEALTH
We are seeking partners who share our vision in shaping the future of global health care and who will support the work of this ground-breaking Institute.
We offer a range of philanthropic opportunities.
Teaching, Capacity Building & Future Leaders

Evidence-Based Health Care

Applied Digital Health

Translational Health Sciences

Global Healthcare Leadership
Our key research themes.
- The Digital Transformation of Care
- Data Science and Artificial Intelligence
- Innovative Methods in Digital Health
- Building a Knowledge Powerhouse

DEVELOPING POPULATION BASED SYSTEMS TO DELIVER BETTER VALUE HEALTH CARE
One of our teams is leading work on value-based health care, which aims to get improved outcomes for patients at no greater cost, with the new G20 Hub for value based health care, in Rome and in Sao Paulo for Latin America.

During the pandemic, we rapidly engineered a secure new Oxford Clinical Informatics Digital Hub (ORCHID) to support clinical research. ORCHID immediately supported two national COVID-19 community treatment trials – PRINCIPLE for repurposed drugs and PANORAMIC for novel antivirals; national flu and COVID-19 surveillance; COVID-19 community diagnostics (RAPTOR); and COVID-19 risk and service recovery. New clinical trials will utilise ORCHID to accelerate recruitment and reduce costs.

RESEARCH SAVING LIVES THROUGH EARLIER CANCER DETECTION
An innovative new computer algorithm which screens an individual’s medical record to identify their risk of bowel cancer has been trialled successfully in 2.5 million patients.

During the peak of the first wave of COVID-19, Professor Ben Goldacre and colleagues developed the fully open-source, privacy-preserving software platform, OpenSAFELY to allow the open and reproducible analysis of 17 million electronic health records. Following this, the team published the preprint of their first study, examining risk factors for COVID-19 death which has been cited and used globally. This demonstrates the power of novel approaches to data science unlocking evidence from data.

ADOLESCENT MENTAL HEALTH
Using creative arts and digital methods to collect experience data, the ATTUNE collaborative led by will build a digital public health resource and a serious game including elements of narrative exposure therapy.

DIGITAL INTERVENTION TO REDUCE SUICIDAL IDEATION FOR SYRIAN REFUGEES
This PhD project explores Syrian refugees’ cultural conceptualisations of mental health and wellbeing, coping strategies and help-seeking behaviour and will co-design the digital intervention to reduce suicidal ideation.
Events and Resources
Events: click here for more information Resources: click here for more information
Digital health news
OpenSAFELY provides vital real-time data to support NHS ambition for safer opioid use
27 June 2024
World hypertension day: How we’re tackling high blood pressure from pregnancy to later life
17 May 2024
Student perspectives on leveraging digital health for better patient care and a greener healthcare system
23 April 2024
Bennett Institute for Applied Data Science part of project to help evaluate the new NHS Pharmacy First service
13 February 2024
PhD (Digital Health)
- RMIT Europe
- RMIT Global
- RMIT Vietnam
- Study online
- Courses by study area
- Undergraduate courses
- Postgraduate courses
- Vocational studies
- Pre-university studies
- Online courses and degrees
- Entry pathways
- Single courses
- Short courses and microcredentials
- Courses for international students
- How to apply
- Scholarships
- School leaver information
- Student services
- Student experience
- Frequently asked questions
- Career advisers
- Study experience
- Student life
- Support for students
- Global opportunities
- Industry connections
- Our strategy
- Governance & management
- Schools & colleges
- Respect for Australian Indigenous cultures
- Our locations and facilities
- Our heritage
- Our research
- Partnerships
- Centres and collaborations
- Research degrees
- Find researchers
- Recruit students and graduates
- Workforce development
- Collaborate with RMIT
- Research partnerships
- Facilities, equipment and services
- Contact Industry Engagement
- Giving to RMIT
- Study in Australia
- Apply to RMIT as an international student
- International student enquiries
- Fees and scholarships for international students
- International student services
- Key dates for international students
Apply your advanced research skills to shape the future of digital healthcare.

You're viewing program information for local students.
RMIT considers you a local student if you are:
- a citizen or permanent resident of Australia, or
- a New Zealand citizen, or
- a person seeking asylum who holds either a: Temporary Protection Visa (TPV), or Safe Haven Enterprise Visa (SHEV) or Bridging Visa E or Humanitarian Stay (Temporary) visa or Temporary Humanitarian Concern Visa.
Asylum seekers who reside in Australia and study onshore are required to pay international onshore tuition fees for higher education courses.
If you are unsure or hold a different visa type, please contact Study@RMIT for more information.
Not a local student?
You're viewing program information for international students..
RMIT considers you an international student if you are:
- intending to study on a student visa, or
- not a citizen or permanent resident of Australia, or
- not a New Zealand citizen, or
- not a a person seeking asylum who holds either a: Temporary Protection Visa (TPV), or Safe Haven Enterprise Visa (SHEV) or Bridging Visa E or Humanitarian Stay (Temporary) visa or Temporary Humanitarian Concern Visa.
If you are unsure or hold a different visa type, please contact Study@RMIT for more information.
Not an international student?
Not applicable
Research Training Scheme
See admissions
AU$36,480 (2024 annual)
Apply your advanced research skills to shape the future of digital healthcare.
Digital health research plays an important role in enhancing our knowledge of the application and impact of digital technologies in healthcare and medicine. The School of Health and Biomedical Sciences conducts discovery, translational and clinical research focused on healthy ageing and chronic diseases.
This is an interdisciplinary course, focused on building the capacity for digitally enabled healthcare. Our digital health research interests encompass electronic health records, mobile health applications, wearable devices, virtual care, health informatics, artificial intelligence (AI) in healthcare and data analytics.
Why study digital health at RMIT?
Interdisciplinary networks.
Take advantage of interdisciplinary focused research with clinical and industry connections.
Practical applications
Gain the opportunity to help build the digital health capacity of the healthcare workforce.
Holistic approach
Enjoy a bench-to-bedside-to-community approach involving clinical, non-clinical, experimental and educational research.
How you will learn
Research at rmit, time spent on research.
Full-time candidates are expected to commit at least four days per week (or at least two days per week for part-time candidates) to their research. The academic year is 48 weeks.
Regular contact with your supervisor
A schedule of meetings with your supervisor/s must be established to assess progress against milestones and timely completion.
Resources, facilities and support
You will have access to the Learning Hub and other online and digital resources through the myRMIT student portal.
You will be part of an active research community and have access to resources and workshops to help you succeed.
School of Graduate Research
The School of Graduate Research works with Schools to further support candidates during their postgraduate research degree.
This course maintains strong local, national and international connections and collaborations with industry, including various health and medical sectors, the biotechnology and pharmaceutical industry, government and public health, hospitals and research institutes.
Many of the projects are conducted in collaboration with industry and industry partners. This broadens your knowledge and skill of the field, and can also unlock valuable interdisciplinary opportunities for the future.
Learning outcomes
The knowledge and skills you will acquire throughout this degree and how they can be applied in your career are described in the learning outcomes .
Electives and course plan
You will complete this program under academic supervision.
The PhD program is structured to enable you to:
- complete a compulsory research methods course
- receive training in research integrity and ethics
- select studies in qualitative and quantitative research techniques
- complete a thesis/project which demonstrates your original contribution to the field and your ability to communicate complex or original research for peers and the community to an international standard
Research integrity modules
You are required to complete the online modules:
- Research integrity
- Copyright and intellectual property
Research methods for sciences
Research methods courses step you through the literature review and preparing your research proposal for confirmation of candidature. They are taught in large discipline groups.
You may need to complete an ethics module to ensure your research is ethical and responsible.
Research techniques
You may elect to take (where relevant) electives in qualitative or quantitative research techniques once data collection has begun. You can use your own data to explore different research analysis techniques. Your supervisor will help you decide when you should take these electives.
Co-curricular activities
You are encouraged to participate in activities offered with the university, college and school according to your needs and interests.
This PhD may be undertaken in a project, thesis by publication or thesis mode. Prospective candidates should discuss these modes of submission with their potential supervisor/s.
Course structure
Choose a plan below to find out more about the subjects you will study and the course structure.
*The maximum duration of the PhD program is 4 years full-time and 8 years part-time. However, candidates are expected to complete their program within 3-4 years full-time equivalent and 6-8 years part-time equivalent.
*The maximum duration of the PhD program is 4 years full-time. However, candidates are expected to complete their program within 3-4 years full-time equivalent.
Note: International student visa holders can only study full-time.
As a graduate, you will be highly sought after for a research or research-related career (including senior leadership and management positions) in various health and medical sectors, such as the biotechnology and pharmaceutical industry, government and public health, hospitals, universities and research institutes.
Expected career pathways for graduates of this degree include:
- research and academic positions in universities, hospitals and research institutes
- pharmaceutical or biotechnology industry roles in research and development, data analysis, quality control, regulatory affairs, medical affairs or leadership and management
- government and public health careers, investigating public health issues, epidemiology, health policy and contributing to evidence-based decision-making.
Minimum requirements for admission
Prerequisites, selection tasks.
The minimum requirements for admission to a PhD program are:
- a bachelor degree requiring at least four years of full-time study in a relevant discipline awarded with honours. The degree should include a research component comprised of a thesis, other research projects or research methodology courses that constitute at least 25% of a full-time academic year (or part-time equivalent). The applicant must have achieved at least a distinction average in the final year; or
- a master degree that includes a research component comprised of at least 25% of a full-time academic year (or part-time equivalent) with an overall distinction average or a master degree without a research component with at least a high distinction average; or
- evidence of appropriate academic qualifications and/or experience that satisfies the Associate Deputy Vice-Chancellor, Research Training and Development or nominee that the applicant has developed knowledge of the field of study or cognate field and the potential for research sufficient to undertake the proposed program.
At RMIT a grade of distinction represents academic achievement of 70% or higher and a high distinction is 80% or higher.
If you are a current master by research candidate, you are able to apply for a transfer to a doctor of philosophy program through the process prescribed in the RMIT Higher Degree by Research policy .
There are no prerequisite subjects required for entry into this qualification.
These entrance requirements are the minimum academic standard you must meet in order to be eligible to apply for the program. You will need to complete a selection task as part of your application.
A selection process will be conducted in conjunction with the School and supervisors you nominate.
For further information on the steps you need to take to apply for a research program see How to apply – Research programs .
English language requirements
Research proposal and supervisor.
You must attach a substantive research proposal that is 2 to 5 pages in length which articulates the intent, significance and originality of the proposed topic using the following headings:
a) title / topic b) research questions to be investigated in the context of existing research/literature in the area c) significance and impact of the research d) methodology / research tasks required to undertake the research e) particular needs (e.g. resources, facilities, fieldwork or equipment that are necessary for your proposed research program, if applicable).
Your application will not be considered if you have not discussed your research topic with a proposed senior and associate supervisor or joint senior supervisors. You must provide the names of the academic staff in the school you have applied to and with whom you have discussed your proposed research.
To study this course you will need to complete one of the following English proficiency tests:
- IELTS (Academic): minimum overall band of 6.5 (with no individual band below 6.0)
- TOEFL (Internet Based Test - IBT): minimum overall score of 79 (with minimum of 13 in Reading, 12 in Listening, 18 in Speaking and 21 in Writing)
- Pearson Test of English (Academic) (PTE (A)): minimum score of 58 (with no communication band less than 50)
- Cambridge English: Advanced (CAE): minimum of 176 with no less than 169 in any component.
For detailed information on English language requirements and other proficiency tests recognised by RMIT, visit English language requirements and equivalency information .
Don't meet the English language test scores? Complete an English for Academic Purposes (EAP) Advanced Plus Certificate at RMIT English Worldwide .
You can gain entry to this program from a range of RMIT four year Bachelor and Honours degrees or Postgraduate or Masters by Research programs.
Fee summary
Fee information for masters by research and doctorate (PhD) programs.
If you are an Australian citizen, Australian permanent resident or New Zealand citizen you may be eligible for a Research Training Scheme (RTS) place where your tuition costs are funded by the Commonwealth Government under the RTS and you have full exemption from tuition fees.
Acceptance in an RTS place is very competitive and places are granted on the condition that you meet annual progress requirements and complete within the allotted time for your program and your status as a part-time or full-time candidate.
This means a maximum of 2 years for a full-time Masters by Research or 4 years for a PhD (or the equivalent part-time).
Contact the School of Graduate Research for more information.
The student services and amenities fee (SSAF) is used to maintain and enhance services and amenities that improve your experience as an RMIT student.
In addition to the SSAF there may be other expenses associated with your program.
Income tax deductions
Candidates may be eligible to apply for income tax deductions for education expenses linked to their employment. See the Australian Taxation Office (ATO) website for more information.
RMIT awards more than 2000 scholarships every year to recognise academic achievement and assist students from a variety of backgrounds.
International applicants
- Fees information for international candidates looking to study at RMIT's Melbourne campuses.
- PhD and masters by research fees for international candidates studying offshore.
Other costs
Important fee information.
Find out more details about how fees are calculated and the expected annual increase.
Applying for refunds
Find information on how to apply for a refund as a continuing international student.
Frequently Asked Questions (FAQs)
Looking for answers or more general information.
Use our Frequently Asked Questions to learn about the application process and its equity access schemes, find out how to accept or defer your offer or request a leave of absence, discover information about your fees, refunds and scholarships, and explore the various student support and advocacy services, as well as how to find out more about your preferred program, and more.
- Find a project
Course saved!
You can compare up to courses.
You can compare more courses.
View comparison dashboard
Compare limit reached!
To save more courses you will need to unsave some courses in your dashboard.

Acknowledgement of Country
RMIT University acknowledges the people of the Woi wurrung and Boon wurrung language groups of the eastern Kulin Nation on whose unceded lands we conduct the business of the University. RMIT University respectfully acknowledges their Ancestors and Elders, past and present. RMIT also acknowledges the Traditional Custodians and their Ancestors of the lands and waters across Australia where we conduct our business - Artwork 'Luwaytini' by Mark Cleaver, Palawa.
RMIT University acknowledges the people of the Woi wurrung and Boon wurrung language groups of the eastern Kulin Nation on whose unceded lands we conduct the business of the University. RMIT University respectfully acknowledges their Ancestors and Elders, past and present. RMIT also acknowledges the Traditional Custodians and their Ancestors of the lands and waters across Australia where we conduct our business.
- Levels of study
- Applying to RMIT
- International students
- Careers advisers
- Research contacts
- Staff development and training
- Facilities and equipment services
- Governance and management
- Sustainability
- Schools and colleges
- Copyright © 2024 RMIT University |
- Accessibility |
- Website feedback |
- Complaints |
- ABN 49 781 030 034 |
- CRICOS provider number: 00122A |
- TEQSA provider number: PRV12145 |
- RTO Code: 3046 |
- Open Universities Australia
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
- Global Digital Health Certificate Program
Sponsored By: Department of International Health
Onsite | Part-Time | 1-3 years
- MAS Application Fee Waiver Requirements
- Master of Arts (MA) in Geography and Environmental Engineering
- Master of Arts and Master of Science in Public Health (MA/MSPH)
- Master of Arts in Public Health Biology (MAPHB)
- Master of Bioethics (MBE)
- Mission, Vision, and Values
- Student Experience
- Program Outcomes
- For Hopkins Undergraduate Students
- Master of Health Science (MHS) - Department of Biochemistry and Molecular Biology
- Master of Health Science (MHS) - Department of Epidemiology
- Alumni Update
- MHS Combined with a Certificate Program
- Master of Health Science (MHS) - Department of Molecular Microbiology and Immunology
- Alumni Highlights
- Post-Baccalaureate Program in Environmental Health for Pre-Medicine Students
- Bachelor's/MHS in Health Economics and Outcomes Research
- MHS HEOR Careers
- Frequently Asked Questions
- Master of Health Science (MHS)
- Concurrent School-Wide Master of Health Science Program in Biostatistics
- Master of Health Science - Department of Population, Family and Reproductive Health
- Master of Health Science Online (MHS) - Department of Population, Family and Reproductive Health
- Careers in Health Economics
- Core Competencies
- Meet the Director
- What is Health Economics
- MPH Capstone Schedule
- Concentrations
- Online/Part-Time Format
- Requirements
- Tuition and Funding
- Executive Board Faculty
- Master of Science (MS) in Geography and Environmental Engineering
- Independent Professional Project and Final Essay
- Program Objectives and Outcomes
- Internships
- Master of Science (ScM) - Department of Biochemistry and Molecular Biology
- Master of Science (ScM) - Department of Biostatistics
- Master of Science (ScM) - Department of Epidemiology
- Master of Science (ScM) - Department of Molecular Microbiology and Immunology
- ScM Faculty Advisers
- Master of Science in Engineering (MSE) in Geography and Environmental Engineering
- Bachelor's/MSPH in Health Policy
- FAQ for MSPH in Health Policy
- Field Placement Experience
- MSPH Capstone
- MSPH Practicum
- Required and Elective Courses
- Student Timeline
- Career Opportunities
- 38-Week Dietetics Practicum
- Completion Requirements
- MSPH/RD Program FAQ
- Program Goals
- Master's Essay Titles
- Application Fee Waiver Requirements
- Doctor of Philosophy (PhD) - Department of Biostatistics
- Doctor of Philosophy (PhD) - Department of Epidemiology
- Program Goals and Expectations
- Doctor of Philosophy (PhD) - Department of Molecular Microbiology and Immunology
- Doctor of Philosophy (PhD) - Department of Population, Family and Reproductive Health
- Doctor of Philosophy (PhD) in Clinical Investigation
- Track in Environmental Sustainability, Resilience, and Health
- Track in Exposure Sciences and Environmental Epidemiology
- Track in Health Security
- Track in Toxicology, Physiology and Molecular Mechanisms
- PhD in Geography and Environmental Engineering Faculty Advisers
- Recent Graduates and Dissertation Titles
- PhD Funding
- PhD TA Requirement
- Recent Dissertation Titles
- JHU-Tsinghua Doctor of Public Health
- Core Course Requirements
- Concentration in Women’s and Reproductive Health
- Custom Track
- Concentration in Environmental Health
- Concentration in Global Health: Policy and Evaluation
- Concentration in Health Equity and Social Justice
- Concentration in Health Policy and Management
- Concentration in Implementation Science
- Meet Current Students
- Combined Bachelor's / Master's Programs
- Concurrent MHS Option for BSPH Doctoral Students
- Concurrent MSPH Option for JHSPH Doctoral students
- Doctor of Medicine and Doctor of Philosophy (MD/PhD)
- Adolescent Health Certificate Program
- Bioethics Certificate Program
- Climate and Health Certificate Program
- Clinical Trials Certificate Program
- Community- Based Public Health Certificate Program
- Demographic Methods Certificate Program
- Environmental and Occupational Health Certificate Program
- Epidemiology for Public Health Professionals Certificate Program
- Evaluation: International Health Programs Certificate Program
- Food Systems, the Environment and Public Health Certificate Program
- Frequently Asked Questions for Certificate Programs
- Gender and Health Certificate Program
- Gerontology Certificate Program
- Global Health Certificate Program
- Global Health Practice Certificate Program
- Health Communication Certificate Program
- Health Disparities and Health Inequality Certificate Program
- Health Education Certificate Program
- Health Finance and Management Certificate Program
- Health and Human Rights Certificate Program
- Healthcare Epidemiology and Infection Prevention and Control Certificate Program
- Humane Sciences and Toxicology Policy Certificate Program
- Humanitarian Health Certificate Program
- Implementation Science and Research Practice Certificate Program
- Injury and Violence Prevention Certificate Program
- International Healthcare Management and Leadership Certificate Program
- Leadership for Public Health and Healthcare Certificate Program
- Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) Public Health Certificate Program
- Maternal and Child Health Certificate Program
- Mental Health Policy, Economics and Services Certificate Program
- Non-Degree Students General Admissions Info
- Pharmacoepidemiology and Drug Safety Certificate Program
- Population Health Management Certificate Program
- Population and Health Certificate Program
- Product Stewardship for Sustainability Certificate Program
- Public Health Advocacy Certificate Program
- Public Health Economics Certificate Program
- Public Health Informatics Certificate Program
- Public Health Practice Certificate Program
- Declaration of Intent - Public Health Preparedness
- Public Health Training Certificate for American Indian Health Professionals
- Public Mental Health Research Certificate Program
- Quality, Patient Safety and Outcomes Research Certificate Program
- Quantitative Methods in Public Health Certificate Program
- Requirements for Successful Completion of a Certificate Program
- Rigor, Reproducibility, and Responsibility in Scientific Practice Certificate Program
- Risk Sciences and Public Policy Certificate Program
- Spatial Analysis for Public Health Certificate Program
- Training Certificate in Public Health
- Tropical Medicine Certificate Program
- Tuition for Certificate Programs
- Vaccine Science and Policy Certificate Program
- Online Student Experience
- Online Programs for Applied Learning
- Barcelona Information
- Registration, Tuition, and Fees
- Agency Scholarship Application
- General Scholarship Application
- UPF Scholarship Application
- Course Evaluations
- Online Courses
- Registration
- General Institute Tuition Information
- International Students
- Directions to the Bloomberg School
- All Courses
- Important Guidance for ONSITE Students
- D.C. Courses
- Registration and Fees
- Cancellation and Closure Policies
- Application Procedures
- Career Search
- Current Activities
- Current Trainees
- Related Links
- Process for Appointing Postdoctoral Fellows
- Message from the Director
- Program Details
- Admissions FAQ
- Current Residents
- Elective Opportunities for Visiting Trainees
- What is Occupational and Environmental Medicine?
- Admissions Info
- Graduates by Year
- Compensation and Benefits
- How to Apply
- Academic Committee
- Course Details and Registration
- Tuition and Fees
- ONLINE SOCI PROGRAM
- Principal Faculty
- Johns Hopkins RAPID Psychological First Aid
- General Application
- JHHS Application
- Areas of Study
- Important Dates
- Our Faculty
- Welcome Letter
- Descripción los Cursos
- Programa en Epidemiología para Gestores de Salud, Basado en Internet
- Consultants
- Britt Dahlberg, PhD
- Joke Bradt, PhD, MT-BC
- Mark R. Luborsky, PhD
- Marsha Wittink, PhD
- Rebekka Lee, ScD
- Su Yeon Lee-Tauler, PhD
- Theresa Hoeft, PhD
- Vicki L. Plano Clark, PhD
- Program Retreat
- Mixed Methods Applications: Illustrations
- Announcements
- 2023 Call for Applications
- Jennifer I Manuel, PhD, MSW
- Joke Bradt, PhD
- Josiemer Mattei, PhD, MPH
- Justin Sanders, MD, MSc
- Linda Charmaran, PhD
- Nao Hagiwara, PhD
- Nynikka R. A. Palmer, DrPH, MPH
- Olayinka O. Shiyanbola, BPharm, PhD
- Sarah Ronis, MD, MPH
- Susan D. Brown, PhD
- Tara Lagu, MD, MPH
- Theresa Hoft, PhD
- Wynne E. Norton, PhD
- Yvonne Mensa-Wilmot, PhD, MPH
- A. Susana Ramírez, PhD, MPH
- Animesh Sabnis, MD, MSHS
- Autumn Kieber-Emmons, MD, MPH
- Benjamin Han, MD, MPH
- Brooke A. Levandowski, PhD, MPA
- Camille R. Quinn, PhD, AM, LCSW
- Justine Wu, MD, MPH
- Kelly Aschbrenner, PhD
- Kim N. Danforth, ScD, MPH
- Loreto Leiva, PhD
- Marie Brault, PhD
- Mary E. Cooley, PhD, RN, FAAN
- Meganne K. Masko, PhD, MT-BC/L
- PhuongThao D. Le, PhD, MPH
- Rebecca Lobb, ScD, MPH
- Allegra R. Gordon, ScD MPH
- Anita Misra-Hebert, MD MPH FACP
- Arden M. Morris, MD, MPH
- Caroline Silva, PhD
- Danielle Davidov, PhD
- Hans Oh, PhD
- J. Nicholas Dionne-Odom, PhD RN ACHPN
- Jacqueline Mogle, PhD
- Jammie Hopkins, DrPH, MS
- Joe Glass, PhD MSW
- Karen Whiteman, PhD MSW
- Katie Schultz, PhD MSW
- Rose Molina, MD
- Uriyoán Colón-Ramos, ScD MPA
- Andrew Riley, PhD
- Byron J. Powell, PhD, LCSW
- Carrie Nieman MD, MPH
- Charles R. Rogers, PhD, MPH, MS, CHES®
- Emily E. Haroz, PhD
- Jennifer Tsui, Ph.D., M.P.H.
- Jessica Magidson, PhD
- Katherine Sanchez, PhD, LCSW
- Kelly Doran, MD, MHS
- Kiara Alvarez, PhD
- LaPrincess C. Brewer, MD, MPH
- Melissa Radey, PhD, MA, MSSW
- Sophia L. Johnson, PharmD, MPH, PhD
- Supriya Gupta Mohile, MD, MS
- Virginia McKay, PhD
- Andrew Cohen, MD, PhD
- Angela Chen, PhD, PMHNP-BC, RN
- Christopher Salas-Wright, PhD, MSW
- Eliza Park MD, MS
- Jaime M. Hughes, PhD, MPH, MSW
- Johanne Eliacin, PhD, HSPP
- Lingrui Liu ScD MS
- Meaghan Kennedy, MD
- Nicole Stadnick, PhD, MPH
- Paula Aristizabal, MD
- Radhika Sundararajan, MD
- Sara Mamo, AuD, PhD
- Tullika Garg, MD MPH FACS
- Allison Magnuson, DO
- Ariel Williamson PhD, DBSM
- Benita Bamgbade, PharmD, PhD
- Christopher Woodrell MD
- Hung-Jui (Ray) Tan, MD, MSHPM
- Jasmine Abrams, PhD
- Jose Alejandro Rauh-Hain, MD
- Karen Flórez, DrPH, MPH
- Lavanya Vasudevan, PhD, MPH, CPH
- Maria Garcia, MD, MPH
- Robert Brady, PhD
- Saria Hassan, MD
- Scherezade Mama, DrPH
- Yuan Lu, ScD
- 2021 Scholars
- Sign Up for Our Email List
- Workforce Training
- Cells-to-Society Courses
- Course/Section Numbers Explained
- Pathway Program with Goucher College
- The George G. Graham Lecture
About the Global Digital Health Certificate Program
Digital health refers to the development and use of digital technologies—which includes m/eHealth, health informatics, telemedicine, data analytics, big data, artificial intelligence—utilized in and throughout health systems to improve health.
The Global Digital Health Certificate program provides concrete training—grounded in real-world challenges and informed by leading-edge scholarship—in the contexts of digital health use in low- and middle-income country settings and focused on methodology, monitoring and evaluation of digital health interventions, and digital health leadership skills.
This certificate program is for students interested in digital health and pursuing a terminal master’s program who plan to join academic, government, or private-sector employment, and for students who plan to pursue additional advanced degrees (e.g., DrPH, PhD). This certificate is brought to you by the Center for Global Digital Health Innovation and is sponsored by the Department of International Health where the Center is based. Students pursuing the certificate are encouraged to consider joining the Digital Health Society, a student-led organization at Johns Hopkins.
Educational Objectives
- Students will better understand how digital health is implemented and evaluated in low- and middle-income contexts, which can be applied to domestic and international settings.
- Students will be able to apply their knowledge to develop and implement evaluations for digital health interventions
Student Learning Outcomes
- Identify and describe key types of digital interventions applied to improve a variety of health services and the essential components for implementing digital health intervention.
- Discuss and examine the practical issues related to the implementation of digital health interventions as well as the social, political, and economic factors that influence global digital health research and priorities. This includes discussions around ethics and privacy considerations, research and evaluation methods, novel interventions, partnership building, and stakeholder engagement.
- Critically appraise technical considerations for the selection, adaptation, and implementation considerations for various digital health platforms.
- Develop requirements, data flow diagrams, and a process to conceptualize implementation of digital health interventions.
- Develop an implementation and evaluation plan for a digital health intervention, which includes explaining key reporting requirements, describing different innovative methodologies that could be utilized to evaluate such interventions, differentiating strengths and weaknesses of evaluation methods, and selecting the appropriate quantitative and qualitative data collection methods.
Curriculum for the Global Digital Health Certificate Program
Please visit our Academic Catalogue to see the full certificate curriculum requirements. Please also review the certificate completion requirements .
Admissions Requirements
Degree students.
The certificate program is only open to master's and doctoral students currently enrolled in a degree program at the Bloomberg School of Public Health; it is not open to graduate students in other JHU divisions. MAS degree students are not eligible to apply.
Applicants must submit the declaration of intent form and select "Global Digital Health" prior to starting coursework.
Eligible Start Terms :
Summer, 1st, 2nd, 3rd, and 4th
Non-Degree Students
This certificate program is only open to individuals who are currently matriculated in a degree program in the Johns Hopkins Bloomberg School of Public Health.
Information regarding the cost of tuition and fees can be found on the Bloomberg School's Certificate Programs Tuition page.
Questions about the program? We're happy to help.
Sponsoring Department International Health
Certificate Program Contact Karen Unterberger
Faculty Co-Sponsors Shivani Pandya and Smisha Agarwal
We have 111 digital health PhD Projects, Programmes & Scholarships
All disciplines
All locations
Institution
All Institutions
All PhD Types
All Funding
digital health PhD Projects, Programmes & Scholarships
Digital health: innovating relationships between industry, health and care providers and universities (advert reference: rdf24/bl/eis/wilson2), phd research project.
PhD Research Projects are advertised opportunities to examine a pre-defined topic or answer a stated research question. Some projects may also provide scope for you to propose your own ideas and approaches.
Funded PhD Project (UK Students Only)
This research project has funding attached. It is only available to UK citizens or those who have been resident in the UK for a period of 3 years or more. Some projects, which are funded by charities or by the universities themselves may have more stringent restrictions.
Digital literacy for workers in ageing health workforces
Funded phd project (students worldwide).
This project has funding attached, subject to eligibility criteria. Applications for the project are welcome from all suitably qualified candidates, but its funding may be restricted to a limited set of nationalities. You should check the project and department details for more information.
PhD Digital health in bronchiectasis
Self-funded phd students only.
This project does not have funding attached. You will need to have your own means of paying fees and living costs and / or seek separate funding from student finance, charities or trusts.
Secure AI-enhanced Policy Framework for Digital Health Data
A decentralized, data driven health monitoring and diagnostics platform based on artificial intelligence (ai) and wearable/portable internet of medical things (iomt) sensors, intelligent proxies to support health and social care for older adults., a taste of home: exploring migrating food heritage and food information practices, keep on keep up for stroke survivors (koku4stroke): an investigation of the usability and acceptability of a digital rehabilitation program to train balance and strength and fitness in stroke survivors (ref: sf24/hls/ser/moore), investigating the relationship between digital media use and children’s mental health, novel applications of remote sensing for health, competition funded phd project (students worldwide).
This project is in competition for funding with other projects. Usually the project which receives the best applicant will be successful. Unsuccessful projects may still go ahead as self-funded opportunities. Applications for the project are welcome from all suitably qualified candidates, but potential funding may be restricted to a limited set of nationalities. You should check the project and department details for more information.
AI-based interventions for mental health conditions
Reviewing and optimising the use of electronic prescribing systems to improve medicine safety in integrated care systems, low-cost digital twin for building performance monitoring and control system operation, visual system vulnerability in dementia: from detection to determinants, the use digital tools and online information for the self-management of health.
FindAPhD. Copyright 2005-2024 All rights reserved.
Unknown ( change )
Have you got time to answer some quick questions about PhD study?
Select your nearest city
You haven’t completed your profile yet. To get the most out of FindAPhD, finish your profile and receive these benefits:
- Monthly chance to win one of ten £10 Amazon vouchers ; winners will be notified every month.*
- The latest PhD projects delivered straight to your inbox
- Access to our £6,000 scholarship competition
- Weekly newsletter with funding opportunities, research proposal tips and much more
- Early access to our physical and virtual postgraduate study fairs
Or begin browsing FindAPhD.com
or begin browsing FindAPhD.com
*Offer only available for the duration of your active subscription, and subject to change. You MUST claim your prize within 72 hours, if not we will redraw.

Do you want hassle-free information and advice?
Create your FindAPhD account and sign up to our newsletter:
- Find out about funding opportunities and application tips
- Receive weekly advice, student stories and the latest PhD news
- Hear about our upcoming study fairs
- Save your favourite projects, track enquiries and get personalised subject updates

Create your account
Looking to list your PhD opportunities? Log in here .
Filtering Results
Digital Health
Explore the opportunities and difficulties facing widespread adoption of digital technologies in health care.

Associated Schools

Harvard Medical School
What you'll learn.
Understand how digital technologies can address critical pain points in health care
Learn how to think about applications of collecting and using data to inform health care, and the privacy risks and analytical pitfalls unique to health care data
Explore the opportunities and difficulties of enabling digital approaches, such as artificial intelligence, machine learning, apps, and sensors
Navigate the systemic barriers and often conflicting needs of health care stakeholders in bringing digital technologies to market
Become adept at analyzing gaps in health care that can be closed with technology and data
Course description
Millions of health-related data points are captured every day, from individual-level information collected by our personal devices and tests at the doctor's office to population-level data about disease prevalence and treatment outcomes. Digital technologies have transformed how we buy and listen to music and how we plan our travel. Can health care be next?
Throughout this online course, you’ll take part in a fictional hackathon, working alongside other learners to determine which digital tools to invest in. With the help of real-world case studies and protagonists, you will become the judge and evaluate how well the hackathon competitors fit the needs of patients, physicians, payers, and, ultimately, future health care ecosystems. In doing so, you’ll consider the impact digital tools have on patients, providers, and payers to understand how data tracking and digital technologies can improve patient care, enhance communications between doctors and patients, increase employee benefits and happiness, and share data to track health trends and develop solutions.
Can you transform health care with the touch of a mouse?
The Harvard Medical School is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
This activity has been approved for AMA PRA Category 1 Credits™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Upon successful completion of the course, participants will have access to claim their credits through the Harvard Medical School’s continuing education platform.
Instructors

Stanley Y. Shaw
You may also like.

Executive Leadership in Health Care | Certificate of Specialization
Advance your career in health care with the Executive Leadership in Health Care Certificate of Specialization from Harvard T.H. Chan School of Public Health Executive and Continuing Professional Education.

Global Health Delivery
Understand the interrelated biological and social factors found in complex global health challenges with our global health delivery online course.

The Opioid Crisis in America
Learn about the opioid epidemic in the United States, including information about treatment and recovery from opioid addiction.
Join our list to learn more

- Open Campus
The Hasso Plattner Institute offers a practically-oriented computer science study program at an internationally recognized institute. This study includes the Germany-wide unique IT-Systems Engineering program and the five master programs Cybersecurity, Data Engineering, Digital Health, IT-Systems Engineering and Software Systems Engineering.
- Studying at the Hasso Plattner Institute in Potsdam
- Before your Studies
- During your Studies
- After your Studies
- Design Thinking
- Entrepreneurship
- Executive Education
- Degree Programs
- Application
- Advisory Service for Prospective Students
- Events for prospective students
- Why study at HPI?
- Beginning your Studies
- Professional Skills
- Campus Life
- Advisory Service for HPI students
- International Student and Scholar Services (ISSS)
- Career Management/HPI Connect
- PhD Program
- Executive Education/HPI Academy
- Statements on Design Thinking
- HPI School of Design Thinking
- Design Thinking Research Program
- HPI Academy
Our researchers at HPI benefit from an inspiring scientific environment as well as a collaborative and inclusive atmosphere. In this environment, they obtain insights and findings that achieve societal impact. Our scientific work is structured within research clusters. In addition, we work together with scientific institutions, companies, and public institutions in numerous research programs worldwide.
- Research Clusters
- Research Groups
- Infrastructure
- Publications
- Research Partnerships
- Data and AI
- Foundations
- Digital Health
- Algorithm Engineering
- Artificial Intelligence and Intelligent Systems
- Artificial Intelligence and Sustainability
- Operating Systems and Middleware
- Business Process Technology
- Computer Graphics Systems
- Cybersecurity – Enterprise Security
- Cybersecurity – Identity Management
- Cybersecurity - Mobile & Wireless
- Data Analytics and Computational Statistics
- Data Engineering Systems
- Data-Intensive Internet Computing
- Design Thinking and Innovation Research
- Digital Global Public Health
- Digital Health - Connected Healthcare
- Digital Health - Machine Learning
- Digital Health, Economics & Policy
- Digital Technology, Governance and Policy
- Human Computer Interaction
- Information Systems
- Internet Technologies and Softwarization
- Software Architecture
- System Analysis and Modeling
- School of Design Thinking
- Future SOC Lab (service-oriented-computing)
- HPI Data Engineering Lab
- Habilitations
- Dissertations
- Technical Reports
- Research Schools
- Research Program "Designing for Sustainability"
- Strategic Scientific Partners
- Economical Partners
- Projects Partners
- Scientific Partner Institutions
The Hasso Plattner Institute in Potsdam is unique on the German academic landscape. The institute's program continues to grow with the support of its founder Hasso Plattner and through international cooperation. Find out more about the founder, events and studies at HPI.
- Founder and Hasso Plattner Foundation
- Organization
- Mission Statement
- Senior Researchers
- Commissioners
- Internal contact and advice points at HPI
- HPI-Fellows
- Conferences
- Events Archive
The Hasso Plattner Institute has educational programs for both high school students and working professionals. It operates its own IT learning platform - openHPI - which provides free online courses. The Youth Academy organizes computer science camps and events for high school students. Professionals can take advantage of educational opportunities in the field of Design Thinking at the HPI Academy.
- HPI Connect / Job Portal
- Initiatives for Women
- HPI Initiatives
- Workshops for individuals
- Workshops for companies
- Innovation & Transformation
- IT & Digitalization
- empowerHER - inspiring Girls, creating Opportunities
- Women in Tech Empower Pack
- EmpowerHER+
- FQ Lounge @ HPI
- Travel Scholarships
- Digital educational platforms
- Sustainability
- IT security
The press area of the Hasso Plattner Institute provides you with the latest press material, news, information on our social media channels and contact details.
- Press Information
- Social Media
- Videos and Pictures
- Persons in charge
- Press Releases
- HPI Newsletter
- Scientific Publications
- IT Summit Blog
- Neuland Podcast 2024
- Neuland Podcast 2023
- Neuland Podcast 2022
- Neuland Podcast 2021
- Neuland Podcast 2020
- Neuland Podcast 2019
- Infographics
- HPI TV Videos
- Research Areas
- Current courses
- Topics for Master Thesis
- Prof. Dr. h.c. mult. Hasso Plattner
- Ph.D. Students
- Autonomous Data Management
- Enterprise Software Engineering
- Data-Driven Decision Support
- Data-Driven Causal Inference
- Dynamic Pricing under Competition
- Project Archive
- All Publications
- Hyrise Blog
- Prof. Dr. Holger Giese
- Kerstin Miers
- Dr. Maria Maximova
- Lucas Sakizloglou
- Dr. Sven Schneider
- Christian Medeiros Adriano
- Matthias Barkowsky
- Thomas Brand
- Sona Ghahremani
- Mustafa Ghani
- Joachim Hänsel
- Christian Schäffer
- Bachelor Projects
- Master Projects
- Bachelor's Theses
- Master's Theses
- Research Area
- Events and Community
- List of Publications
- Annual Reports
- Prof. Dr. Anja Lehmann
- Open Positions
- Knowledge Tech
- Security Eng
- Labs & Systems
- Prof. Dr. Christoph Meinel
- Web Portals & Blogs
- Patents & Publications
- Interviews & Media
- Previous Pages
- Tele-Lectures
- Master Theses
- PhD Students
- D-School teaching
- Research Seminars
- Learning Engineering
- Machine Learning & Artifical Intelligence
- Innovation Research
- Former Topics
- Security Awareness and Education
- Security Analytics
- Secure Identity Lab
- Former Projects and Research Areas
- Former Team Members
- Tele-Lab IT Security
- Book Chapters
- Conference Papers
- Reports & Studies
- Felix Naumann
- Diana Stephan
- Tobias Bleifuß
- Leon Bornemann
- Dr. Lisa Ehrlinger
- Mazhar Hameed
- Swinda Krause
- Daniel Lindner
- Francesco Pugnaloni
- Sebastian Schmidl
- Alejandro Sierra-Múnera
- Phillip Wenig
- Open positions
- Course archive
- Bachelorprojekte
- Research Projects - Overview
- Data Profiling and Analytics
- Data Quality and Cleansing
- Data Preparation
- Distributed Computing
- Web Science
- RDBMS Genealogy
- Repeatability
- Conferences and Workshops
- Selected Presentations
- Digital Health - Connected Health
- Digital Health & Machine Learning
- Summer Term 2024
- Winter Term 2023/24
- Master's Program
- Thesis and Project Work (Open Topics)
- Current Courses
- Course Archive
- Prof. Dr. Tilmann Rabl
- Thomas Bodner
- Martin Boissier
- Florian Schmeller
- Ilin Tolovski
- Interpretable deep learning for novel pathogen detection from DNA sequences
- Towards Generalizable Hierarchical Classification with HiClass
- ML and networks for drug response prediction
- > Organization
- > Doctoral Student (Ph.D.) in Digital Healt...
Doctoral Student (Ph.D.) in Digital Health: Machine Learning in Medical Care
May 2021 – april 2024.
We are looking for a highly motivated computer science Master’s graduate to fill the project-funded open position on the development and application of machine learning methods in medical care.
Please submit your application documents via email to Bert.Arnrich(at)hpi.de
CASSANDRA – Clinical ASSist AND aleRt Algorithms in visceral surgery
Among the 7.1 million surgical procedures performed annually in Germany, approximately 110,000 operations are related to the four major abdominal organ systems: liver, pancreas, upper gastrointestinal tract (esophagus and stomach) and intestine (small bowl and colon). These rather complex operations are associated with high rates of postoperative complications such as serious bleeding, acute kidney failure, intraabdominal infections and sepsis. In fact, at least one out of four surgical patients experiences at least one severe complication after major abdominal surgery with mortality rates being subsequently as high as 12% according to recent studies. Of particular note, these complications often occur multiple days after surgery - hence, when the patient has already been transferred from an intensive care unit (ICU) to a regular ward with reduced monitoring capacities only. However, early detection of patient deterioration is of key importance to prevent beginning complications from aggravating and finally becoming life-threatening. In septic patients, for instance, every hour of delayed antibiotic therapy induction increases patient mortality by 2%.
Given the crucial need to improve patient monitoring after surgery, the C linical A ssist AND A lert A lgorithm ( CASSANDRA )-Project aims at developing and evaluating the use of machine learning (ML) algorithms in detecting and predicting postoperative intra-abdominal infections and other complication entities. The computational challenge in this field emerges from combining static preoperative risk parameters (eg. patient age, medical history, etc.) and static intraoperative data (e.g. duration, blood loss, etc.) with dynamic real time parameters on the ICU as well as on regular wards – the latter using a telemetric continuous vital parameter monitoring device. Taken together, the results may pave the way for an autonomous real-time monitoring system on surgical wards in the long term. The CASSANDRA -project will be conducted in close collaboration with the Surgical Department of the Charité - Universitätsmedizin Berlin and is funded by the Innovation Fonds of the Federal Joint Committee (Gemeinsamer Bundesausschuss G-BA) from May 2021 until April 2024.
Responsibilities
- Support with the setup of a wireless network on a normal ward in order to collect patient vital signs from wearables in real-time.
- Create a pipeline for automatic signal processing.
- Build automatic signal quality checks.
- Clean and filter the signals.
- Extract condensed information from continuous signals.
- Investigate different clinical endpoints like ‘occurrence of a post-surgical complication’ or ‘patient death’.
- Investigate model performance for different subsets of data representing different times during the inpatient stay.
Qualifications
- Master’s degree in computer/data science
- Experience in data mining, computational statistics and machine learning
- Excellent skills in high-level programming languages
- Self-reliance, goal-oriented creativity, dedication, team spirit
- Excellent English language skills
About the Hasso Plattner Institute
The Hasso Plattner Institute (HPI) for Digital Engineering gGmbH is an institute for teaching and research founded by Hasso Plattner in 1998 as a unique public-private partnership, partially funded by the Hasso Plattner Foundation. The HPI focusses on the design, construction, maintenance and analysis of large-scale IT systems. In recent years, the HPI has been expanding towards new areas in information technology, among others digital heath.
Since 2018, the new research group Digital Health – Connected Healthcare addresses the collection and analysis of health-related data from daily life and in a clinical context. The interdisciplinary team led by Prof. Dr.-Ing. Bert Arnrich includes computer scientists and data scientists working on projects that address the whole pipeline from data collection, data preparation and analysis through statistical methods and machine learning models, up until the presentation of relevant information to clinical practitioners.
About the project partner Charité
The Surgical Clinic, Campus Charité Mitte|Campus Virchow Klinikum of the Charité - Universitätsmedizin Berlin is one of the largest surgical departments in Europe with over 5000 cases annually. Conducting more than 170 pancreatic, 350 liver, 500 intestinal and 170 esophageal and gastric surgical procedures per year, it is one of only a few surgical single centres providing a number of operations high enough for the development and evaluation of various machine learning algorithms. The challenging process of systematic data collection and digital storage throughout inpatient stays has already been introduced and continuously been optimized at the Campus Virchow Klinikum as part of the Enhanced Recovery After Surgery (ERAS ©)-program that works an holistic perioperative documentation concept.
All open positions at a glance
Current News
03.07.2024 | hpi-professor leitet programmkomitee der internationalen fachkonferenz debs.
Prof. Tilmann Rabl übernahm den Co-Vorsitz des Programmkomitees für die Konferenz zum Thema Datenverarbeitung in Lyon. > Go to article
02.07.2024 | "Ein Stipendium. Viele Gesichter"
Für sein Engagement und seine Studienleistungen hat HPI-Bachelorstudent Max Blaschke das Universitätsstipendium Potsdam … > Go to article
01.07.2024 | Prof. Ariel Dora Stern holds her inaugural lecture at HPI
In her lecture, the Humboldt Professorship awardee spoke about the transformation of digital health. > Go to article
01.01.1970 | HPI graduate Lars Masanneck receives the University of Potsdam Graduate Award
In his thesis, he investigated the usage trend of digital health technologies in clinical trials. > Go to article
25.06.2024 | HPI-Doktorand Remo Monti im American Journal of Human Genetics (AJHG)
In seinem Paper beschäftigt er sich mit der Bewertung polygener Scoring-Methoden. > Go to article
29.11.2024 | HPI Code Night 2024
Die ganze Nacht wach bleiben und coden: Das geht für alle IT-Begeisterten ab 16 Jahren zur HPI Code Night im November. > Go to article
12.05.2022 | Women in Tech Conference
HPI's Future Work Conference creates space for inspiring personalities to talk about the necessary change in the world … > Go to article
16.10.2024 | Young Women in AI Camp
Beim Young Women in AI Camp lernen Schülerinnen vom 16.-18. Oktober die Welt der künstlichen Intelligenz kennen. > Go to article
Hasso Plattner Institute Prof.-Dr.-Helmert-Straße 2-3 14482 Potsdam, Germany
- Getting there
Tel.: +49 (0)331 5509-0 Fax: +49 (0)331 5509-325 E-Mail: hpi-info(at)hpi.de
- Skip to content
- Skip to navigation

PhD Scholarship - Digital health for patients and healthcare consumers
Scholarship program.
PhD or Master of Research + PhD bundle (1+3 year program; see below)
Australian Institute of Health Innovation (AIHI), Centre for Health Informatics (CHI), Consumer Informatics team
Project name
Digital Health for Patients and Healthcare Consumers
Project description
The Centre for Health Informatics (CHI) is the longest-running health informatics research centre in Australia. The Centre's work is internationally recognised for its ground-breaking contributions in the role of digital technology to support health service innovation.
We are seeking a bright and enthusiastic candidate to join the Consumer Informatics team to undertake PhD research under the supervision of Senior Research Fellow Dr Annie Lau. Our research program focuses on the impact, design, and science of digital technology for healthcare consumers, patients and their carers.
The exact PhD topic will be determined taking into account the interests, experience and prior training of the successful candidate. Possible topics include, but are not limited to:
- understanding unmet needs of patients and consumers in everyday settings (e.g. patient work) and crisis circumstances (e.g. pandemics),
- co-designing and co-evaluating digital health with patients and consumers,
- investigating the role, benefits and unintended consequences of novel technologies for patients and consumers (e.g. artificial intelligence),
- addressing the challenges of integrating digital technologies for patients and consumers in real-life settings (e.g. homes, routine care).
The scholarship will suit an applicant with training in Human Factors, Psychology, Design methods, Computer Science, Engineering, Data Sciences, Public Health, Medicine, Health Sciences, or a Health-related field. It would also suit applicants who enjoy innovative technologies, as well as a desire to work with patients, consumers, carers and clinicians.
Other important information
This scholarship is available to eligible domestic candidates for direct entry into a 3-year PhD program. The scholarship is comprised of a Tuition Fee Offset and a Living Allowance Stipend. The value and tenure of the domestic scholarship at a full-time stipend rate is $28,092 per annum (in 2020, tax exempt for up to 3 years - indexed annually).
An additional 1-year funding is also available to support exceptional candidates who need to complete a Master by Research program before enrolling into the PhD program. Please contact Dr Annie Lau for more details.
How to apply:
Please confirm your suitability before applying by contacting Dr Annie Lau (see below).
Scholarship allocation number: 20223065
To be eligible for the scholarship, applicants are expected to have a record of excellent academic performance, relevant research experience, and preferably peer-reviewed publication record. Refer to the Rating Scholarship Applicants section for more information about these guidelines.
Specifically, applicants will need to comply with Macquarie University PhD admission and scholarship requirements:
- Completion of a Master of Research (MRes) with a grade of at least a Distinction level (75% or greater) in second year; or
- A Master of Philosophy (MPhil) ; or
- A two-year Masters degree with a major research component at Distinction level (75% or greater).
- Peer-reviewed research output may be taken into consideration for admission to the program.
Prospective candidates are encouraged to submit their applications to [email protected] .
Applications must include the following documents:
- Complete CV, including publication list, past education and training, and awards.
- Detailed academic transcripts of relevant undergraduate and Masters studies.
- 1-page summary addressing the above admission and scholarship requirements.
- 1-page research statement describing the proposed scope of the PhD and its alignment with the research of the Centre.
Applicants will need to complete the HDR Candidature and Scholarship Application Form via the Online Application System , selecting HDR Strategic Scholarship (Project or Supervisor Specific) . Applicants must also arrange for two academic referee reports to be submitted to the Higher Degree Research Office. Further information can be found on the How to Apply page.
Macquarie University will advise the successful applicant of entitlements at the time of scholarship offer.
Please quote the allocation number on your application.
Contact name
Dr Annie Lau
Contact email
Contact phone
(02) 9850 1608
Find a programme
Accounting and finance.
Find out about the University of Bristol's PhD in Accounting and Finance, including entry requirements, supervisors and research groups.
Advanced Quantitative Methods
Find out about the University of Bristol's PhD in Advanced Quantitative Methods, including entry requirements, supervisors and research groups.
Aerosol Science
Find out about the University of Bristol's PhD in Aerosol Science, including entry requirements, supervisors and research groups.
Aerospace Engineering
Find out about the University of Bristol's PhD in Aerospace Engineering, including entry requirements, supervisors and research groups.
Anthropology and Archaeology
Find out about the University of Bristol's PhD in Anthropology and Archaeology, including entry requirements, supervisors and research groups.
Biochemistry
Find out about the University of Bristol's PhD in Biochemistry, including entry requirements, supervisors and research groups.
Biological Sciences
Find out about the University of Bristol's PhD in Biological Sciences, including entry requirements, supervisors and research groups.
Cellular and Molecular Medicine
Find out about the University of Bristol's PhD in Cellular and Molecular Medicine, including entry requirements, supervisors and research groups.
Find out about the University of Bristol's PhD in Chemistry, including entry requirements, supervisors and research groups.
Civil Engineering
Find out about the University of Bristol's PhD in Civil Engineering, including entry requirements, supervisors and research groups.
Classics and Ancient History
Find out about the University of Bristol's PhD in Classics and Ancient History, including entry requirements, supervisors and research groups.
Clinical Conscious Sedation and Anxiety Management
Comparative literatures and cultures.
Find out about the University of Bristol's PhD and MPhil in Comparative Literatures and Cultures, including structure and supervisors.
Computer Science
Find out about the University of Bristol's PhD in Computer Science, including entry requirements, career prospects and research groups.
Creative Writing
Find out about the University of Bristol's PhD in Creative Writing, including entry requirements, supervisiors and research groups.
Cyber Security (Cyber Secure Everywhere)
Dds orthodontics.
Find out about the University of Bristol's Orthodontics Doctorate in Dental Surgery (DDS) research degree, including career prospects and supervisors.
DEdPsy Educational Psychology
Find out about the University of Bristol's Doctor of Educational Psychology (DEdPsy) research degree, including career prospects and supervisors.
Disability Studies
Find out about the University of Bristol's PhD in Disability Studies, including entry requirements, career prospects and research groups.
Dynamic Molecular Cell Biology (Wellcome Trust)
Find out about the University of Bristol's PhD in Dynamic Molecular Cell Biology, fully funded by the Wellcome Trust for UK students.
Earth Sciences
Find out about the University of Bristol's PhD in Earth Sciences, including entry requirements, supervisiors and research groups.
East Asian Studies
Find out about the University of Bristol's PhD in East Asian Studies, including entry requirements and key themes.
Find out about the University of Bristol's PhD in Economics, including entry requirements, supervisiors and research groups.
EdD Education: Learning, Leadership and Policy
Find out about the University of Bristol's EdD in Education: Learning, Leadership and Policy, including entry requirements, career prospects and research groups.
Find out about the University of Bristol's PhD in Education, including entry requirements, career prospects and research groups.
Electrical and Electronic Engineering
Find out about the University of Bristol's PhD in Electrical and Electronic Engineering, including entry requirements and research groups.
EngD Composites Manufacture
Engd future innovation in non-destructive evaluation, engineering biology, engineering mathematics.
Find out about the University of Bristol's PhD in Engineering Mathematics, including entry requirements, career prospects and research groups.
English Literature
Find out about the University of Bristol's PhD in English Literature, including entry requirements, supervisors and research groups.
Exercise, Nutrition and Health
Find out about the University of Bristol's PhD in Exercise, Nutrition and Health, including entry requirements, supervisors and research groups.
Film and Television
Find out about the University of Bristol's PhD in Film and Television, including entry requirements, supervisors and research groups.
Find out about the University of Bristol's PhD in French, including entry requirements, supervisors and research groups.
Geographical Sciences (Human Geography)
Find out about the University of Bristol's PhD in Geographical Sciences (Human Geography), including entry requirements, supervisors and research groups.
Geographical Sciences (Physical Geography)
Find out about the University of Bristol's PhD in Geographical Sciences (Physical Geography), including entry requirements, supervisors and research groups.
Find out about the University of Bristol's PhD in German, including entry requirements, supervisors and research groups.
Global Challenges and Transformations
Find out about the University of Bristol's PhD in Global Challenges and Transformations, including entry requirements, supervisors and research groups.
Graduate Diploma Economics
Great western four+ doctoral training partnership (nerc).
Find out about the Great Western Four+ Doctoral Training Partnership, a multidisciplinary training environment for postgraduate students in NERC sciences.
Health and Wellbeing
Find out about the University of Bristol's PhD in Health and Wellbeing, including entry requirements, supervisors and research groups.
Hispanic, Portuguese and Latin American Studies
Find out about the University of Bristol's PhD in Hispanic, Portuguese and Latin American Studies, including supervisors and research groups.
Find out about the University of Bristol's PhD in History, including entry requirements, supervisors and research groups.
History of Art
Find out about the University of Bristol's PhD in History of Art, including entry requirements, supervisors and research groups.
Innovation and Entrepreneurship
Find out about the University of Bristol's PhD in Innovation and Entrepreneurship, including entry requirements, supervisors and research groups.
Integrative Cardiovascular Science (BHF)
Find out about the University of Bristol's PhD in Integrative Cardiovascular Science (BHF), including entry requirements, funding and structure.
Find out about the University of Bristol's PhD in Italian, including entry requirements, structure and research groups.
Find out about the University of Bristol's PhD in Law, including entry requirements, structure and research groups.
Linguistics
Llm law - banking and finance law.
Find out about the University of Bristol's LLM in Banking and Finance Law, including structure, entry requirements and career prospects.
LLM Law - Commercial Law
Find out about the University of Bristol's LLM in Commercial Law, including structure, entry requirements and career prospects.
LLM Law - Company Law and Corporate Governance
Find out about the University of Bristol's LLM in Company Law and Corporate Governance, including structure, entry requirements and career prospects.
LLM Law - Employment, Work and Equality
Find out about the University of Bristol's LLM in Employment, Work and Equality Law, including structure, entry requirements and career prospects.
LLM Law - General Legal Studies
Find out about the University of Bristol's LLM in General Legal Studies, including structure, entry requirements and career prospects.
LLM Law - Health, Law and Society
Find out about the University of Bristol's LLM in Health, Law and Society, including structure, entry requirements and career prospects.
LLM Law - Human Rights Law
Find out about the University of Bristol's LLM in Human Rights Law, including structure, entry requirements and career prospects.
LLM Law - International Commercial Law
Find out about the University of Bristol's LLM in International Commercial Law, including structure, entry requirements and career prospects.
LLM Law - International Law
Find out about the University of Bristol's LLM in International Law, including structure, entry requirements and career prospects.
LLM Law - International Law and International Relations
Find out about the University of Bristol's LLM in International Law and International Relations, including structure, entry requirements and career prospects.
LLM Law - Labour Law and Corporate Governance
Llm law - law and globalisation, llm law - public law, llm law, environment, sustainability & business.
Find out about the University of Bristol's LLM in Law, Environment, Sustainability and Business, including structure, entry requirements and career prospects.
LLM Law, Environment, Sustainability and Business
Llm law, innovation & technology.
Find out about the University of Bristol's LLM in Law, Innovation and Technology, including structure, entry requirements and career prospects.
LLM Law, Innovation and Technology
Ma anthropology.
Find out about the University of Bristol's MA in Anthropology, including structure, entry requirements and career prospects.
MA Black Humanities
Ma chinese-english audiovisual translation.
Find out about the University of Bristol's MA in Chinese-English Audiovisual Translation, including structure, entry requirements and career prospects.
MA Chinese-English Translation
Find out about the University of Bristol's MA in Chinese-English Translation, including structure, entry requirements and career prospects.
MA Comparative Literatures and Cultures
Find out about the University of Bristol's MA in Comparative Literatures and Cultures, including structure, entry requirements and career prospects.
MA Composition of Music for Film and Television
Find out about the University of Bristol's MA in Composition of Music for Film and Television, including structure, entry requirements and career prospects.
MA Creative Innovation and Entrepreneurship
Find out about the University of Bristol's MA in Creative Innovation and Entrepreneurship, including structure, entry requirements and career prospects.
MA Creative Writing
Find out about the University of Bristol's MA in Creative Writing, including structure, entry requirements and career prospects.
MA English Literature
Find out about the University of Bristol's MA in English Literature, including structure, entry requirements and career prospects.
MA Environmental Humanities
Find out about the University of Bristol's MA in Environmental Humanities, including structure, entry requirements and career prospects.
MA Film and Television
Find out about the University of Bristol's MA in Film and Television, including structure, entry requirements and career prospects.
Find out about the University of Bristol's MA in History, including structure, entry requirements and career prospects.
MA History of Art
Find out about the University of Bristol's MA in History of Art, including structure, entry requirements and career prospects.
MA Immersive Arts (Virtual and Augmented Reality)
Find out about the University of Bristol's MSc, PGCert and PGDip in Immersive Arts (Virtual and Augmented Reality) including structure and career prospects.
Find out about the University of Bristol's MA in Law, including structure, entry requirements and career prospects.
MA Logic and Philosophy of Mathematics
Ma medieval studies.
Find out about the University of Bristol's MA in Medieval Studies, including structure, entry requirements and career prospects.
Find out about the University of Bristol's MA in Music, including structure, entry requirements and career prospects.
MA Philosophy
Ma philosophy and history of science, ma philosophy of biological and cognitive sciences, ma philosophy of physics, ma religion, ma translation, ma translation (online).
Find out about the University of Bristol's PhD in Management, including entry requirements, structure and research groups.
Mathematics
Find out about the University of Bristol's PhD in Mathematics, including entry requirements, structure and research groups.
Mechanical Engineering
Find out about the University of Bristol's PhD in Mechanical Engineering, including entry requirements, supervisors and research groups.
Medieval Studies
Find out about the University of Bristol's PhD in Medieval Studies, including entry requirements, supervisors and research groups.
Molecular, Genetic and Lifecourse Epidemiology (Wellcome)
Find out about the University of Bristol's PhD in Molecular, Genetic and Lifecourse Epidemiology, fully funded by the Wellcome Trust for UK students.
MRes Advanced Quantitative Methods
Find out about the University of Bristol's MRes in Advanced Quantitative Methods, including structure, entry requirements and career prospects.
MRes Economics
Find out about the University of Bristol's MRes in Economics, including structure, entry requirements and career prospects.
MRes Education
Find out about the University of Bristol's MRes in Education, including structure, entry requirements and career prospects.
MRes Global Political Economy
Mres health sciences research.
Find out about the University of Bristol's MRes in Health Sciences Research, including structure, entry requirements and career prospects.
MRes Security, Conflict and Human Rights
Mres sustainable futures.
Find out about the University of Bristol's MRes in Sustainable Futures, including structure, entry requirements and career prospects.
MSc Accounting and Finance
Find out about the University of Bristol's MSc in Accounting and Finance, including structure, entry requirements and career prospects.
MSc Accounting, Finance and Management
Find out about the University of Bristol's MSc in Accounting, Finance and Management, including structure, entry requirements and career prospects.
MSc Advanced Composites
Find out about the University of Bristol's MSc in Advanced Composites, including structure, entry requirements and career prospects.
MSc Advanced Microelectronic Systems Engineering
Find out about the University of Bristol's MSc in Advanced Microelectronic Systems Engineering, including structure, entry requirements and career prospects.
MSc Aerial Robotics
Find out about the University of Bristol's MSc in Aerial Robotics, including structure, entry requirements and career prospects.
MSc Applied Neuropsychology
Find out about the University of Bristol's MSc in Applied Neuropsychology, including structure, entry requirements and career prospects.
MSc Applied Neuropsychology (Distance Learning)
Msc applied neuropsychology (online), msc banking, regulation and financial stability.
Find out about the University of Bristol's MSc in Banking, Regulation and Financial Stability, including structure, entry requirements and career prospects.
MSc Bioinformatics
Find out about the University of Bristol's MSc in Bioinformatics, including structure, entry requirements and career prospects.
MSc Biomedical Engineering
Msc biomedical sciences research.
Find out about the University of Bristol's MSc in Biomedical Sciences Research, including structure, entry requirements and career prospects.
MSc Biorobotics
Find out about the University of Bristol's MSc in Biorobotics, including structure, entry requirements and career prospects.
MSc Business Analytics
Find out about the University of Bristol's MSc in Business Analytics, including structure, entry requirements and career prospects.
MSc Business Innovation and Entrepreneurship
Find out about the University of Bristol's MSc in Innovation and Entrepreneurship, including structure, entry requirements and career prospects.
MSc by research Global Environmental Challenges
Find out about the University of Bristol's MSc by research Global Environmental Challenges, including structure, entry requirements and career prospects.
MSc Cardiovascular Perfusion (distance learning)
Msc cardiovascular perfusion (online), msc climate change science and policy.
Find out about the University of Bristol's MSc in Climate Change Science and Policy, including structure, entry requirements and career prospects.
MSc Clinical Neuropsychology
Find out about the University of Bristol's MSc in Clinical Neuropsychology, including structure, entry requirements and career prospects.
MSc Clinical Perfusion Science
Msc clinical research methods and evidence-based medicine, msc communication networks and signal processing.
Find out about the University of Bristol's MSc in Communication Networks and Signal Processing, including structure, entry requirements and career prospects.
MSc Computer Science (Conversion)
Find out about the University of Bristol's MSc conversion programme in Computer Science, including structure, entry requirements and career prospects.
MSc Contemporary Identities
Find out about the University of Bristol's MSc in Contemporary Identities, including structure, entry requirements and career prospects.
MSc Cyber Security (Infrastructures Security)
Find out about the University of Bristol's MSc in Cyber Security (Infrastructures Security), including structure, entry requirements and career prospects.
MSc Data Science
Find out about the University of Bristol's MSc in Data Science, including structure, entry requirements and career prospects.
MSc Data Science (Distance Learning)
Msc data science (online), msc dental implantology.
Find out about the University of Bristol's MSc in Dental Implantology, including structure, entry requirements and career prospects.
MSc Development and Security
Find out about the University of Bristol's MSc in Development and Security, including structure, entry requirements and career prospects.
MSc Digital Health
Find out about the University of Bristol's MSc in Digital Health, including structure, entry requirements and career prospects.
MSc Earthquake Engineering and Infrastructure Resilience
Find out about the University of Bristol's MSc in Earthquake Engineering and Infrastructure Resilience, including structure and career prospects.
MSc East Asian Development and the Global Economy
Find out about the University of Bristol's MSc in East Asian Development and the Global Economy, including structure and career prospects.
MSc Economics
Find out about the University of Bristol's MSc in Economics, including structure, entry requirements and career prospects.
MSc Economics and Finance
Find out about the University of Bristol's MSc in Economics and Finance, including structure, entry requirements and career prospects.
MSc Economics with Data Science
Find out about the University of Bristol's MSc in Economics with Data Science, including structure, entry requirements and career prospects.
MSc Economics, Finance and Management
Find out about the University of Bristol's MSc in Economics, Finance and Management including structure, entry requirements and career prospects.
MSc Education (Education and Climate Change)
Find out about the University of Bristol's MSc in Education (Education and Climate Change), including structure, entry requirements and career prospects.
MSc Education (Inclusive Education)
Find out about the University of Bristol's MSc in Education (Inclusive Education), including structure, entry requirements and career prospects.
MSc Education (Leadership and Policy)
Find out about the University of Bristol's MSc in Education (Leadership and Policy), including structure, entry requirements and career prospects.
MSc Education (Learning, Technology and Society)
Find out about the University of Bristol's MSc in Education (Learning, Technology and Society), including structure, entry requirements and career prospects.
MSc Education (Mathematics Education)
Find out about the University of Bristol's MSc in Education (Mathematics Education), including structure, entry requirements and career prospects.
MSc Education (Neuroscience and Education)
Find out about the University of Bristol's MSc in Education (Neuroscience and Education), including structure, entry requirements and career prospects.
MSc Education (Open Pathway)
Find out about the University of Bristol's MSc in Education (Open Pathway), including structure, entry requirements and career prospects.
MSc Education (Policy and International Development)
Find out about the University of Bristol's MSc in Education (Policy and International Development) including structure, entry requirements and career prospects.
MSc Education (Teaching and Learning)
Msc engineering mathematics.
Find out about the University of Bristol's MSc in Engineering Mathematics, including structure, entry requirements and career prospects.
MSc Engineering with Management
Find out about the University of Bristol's MSc in Engineering with Management, including structure, entry requirements and career prospects.
MSc Environmental Analytical Chemistry
Msc environmental modelling and data analysis.
Find out about the University of Bristol's MSc in Environmental Modelling and Data Analysis, including structure, entry requirements and career prospects.
MSc Environmental Policy and Management
Find out about the University of Bristol's MSc in Environmental Policy and Management, including structure, entry requirements and career prospects.
MSc Epidemiology
Find out about the University of Bristol's MSc in Epidemiology, including structure, entry requirements and career prospects.
MSc Finance and Investment
Find out about the University of Bristol's MSc in Finance and Investment, including structure, entry requirements and career prospects.
MSc Financial Technology
Find out about the University of Bristol's MSc in Financial Technology, including structure, entry requirements and career prospects.
MSc Financial Technology with Data Science
Find out about the University of Bristol's MSc in Financial Technology with Data Science, including structure, entry requirements and career prospects.
MSc Gender and International Relations
Find out about the University of Bristol's MSc in Gender and International Relations, including structure, entry requirements and career prospects.
MSc Geographic Data Science and Spatial Analytics
Find out about the University of Bristol's MSc in Geographic Data Science and Spatial Analytics, including structure, entry requirements and career prospects.
MSc Global Development and Environment
Find out about the University of Bristol's MSc in Global Development and Environment, including structure, entry requirements and career prospects.
MSc Global Management
Msc global operations and supply chain management.
Find out about the University of Bristol's MSc in Global Operations and Supply Chain Management, including structure, entry requirements and career prospects.
MSc Global Wildlife Health and Conservation
Find out about the University of Bristol's MSc in Global Wildlife Health and Conservation, including structure, entry requirements and career prospects.
MSc Health Economics and Health Policy Analysis
Find out about the University of Bristol's MSc in Health Economics and Health Policy Analysis, including structure, entry requirements and career prospects.
MSc Health Professions Education
Msc health professions education (online), msc healthcare management, msc healthcare management (online), msc human geography: society and space.
Find out about the University of Bristol's MSc in Human Geography: Society and Space, including structure, entry requirements and career prospects.
MSc Human Resource Management and the Future of Work
Find out about the University of Bristol's MSc in Human Resource Management and the Future of Work, including structure and career prospects.
MSc Human-Computer Interaction (Online)
Msc image and video communications and signal processing.
Find out about the University of Bristol's MSc in Image and Video Communications and Signal Processing, including structure and career prospects.
MSc Immersive Technologies (Virtual and Augmented Reality)
Find out about the University of Bristol's MSc in Immersive Technologies (Virtual and Augmented Reality), including structure and career prospects.
MSc Innovation and Entrepreneurship
Msc international business and strategy: global challenges.
Find out about the University of Bristol's MSc in International Business and Strategy: Global Challenges), including structure and career prospects.
MSc International Development
Find out about the University of Bristol's MSc in International Development, including structure, entry requirements and career prospects.
MSc International Relations
Find out about the University of Bristol's MSc in International Relations, including structure, entry requirements and career prospects.
MSc International Security
Find out about the University of Bristol's MSc in International Security, including structure, entry requirements and career prospects.
MSc Management
Find out about the University of Bristol's MSc in Management, including structure, entry requirements and career prospects.
MSc Management (CSR and Sustainability)
Find out about the University of Bristol's MSc in Management (CSR and Sustainability), including structure, entry requirements and career prospects.
MSc Management (Digitalisation and Big Data)
Find out about the University of Bristol's MSc in Management (Digitalisation and Big Data), including structure, entry requirements and career prospects.
MSc Management (Entrepreneurship and Innovation)
Find out about the University of Bristol's MSc in Management (Entrepreneurship and Innovation), including structure, entry requirements and career prospects.
MSc Management (International Business)
Find out about the University of Bristol's MSc in Management (International Business), including structure, entry requirements and career prospects.
MSc Management (International Human Resource Management)
Find out about the University of Bristol's MSc in Management (International Human Resource Management), including structure and career prospects.
MSc Management (Marketing)
Find out about the University of Bristol's MSc in Management (Marketing), including structure, entry requirements and career prospects.
MSc Management (Project Management)
Find out about the University of Bristol's MSc in Management (Project Management), including structure, entry requirements and career prospects.
MSc Marketing
Find out about the University of Bristol's MSc in Marketing, including structure, entry requirements and career prospects.
MSc Mathematical Sciences
Find out about the University of Bristol's MSc in Mathematical Sciences, including structure, entry requirements and career prospects.
MSc Medical Statistics and Health Data Science
Find out about the University of Bristol's MSc in Medical Statistics and Health Data Science, including structure, entry requirements and career prospects.

MSc Molecular Neuroscience
Find out about the University of Bristol's MSc in Molecular Neuroscience, including structure, entry requirements and career prospects.
MSc Nanoscience and Functional Nanomaterials
Msc nuclear science and engineering.
Find out about the University of Bristol's MSc in Nuclear Science and Engineering, including structure, entry requirements and career prospects.
MSc Nutrition, Physical Activity and Public Health
Find out about the University of Bristol's MSc in Nutrition, Physical Activity and Public Health, including structure, entry requirements and career prospects.
MSc Optical Communications and Signal Processing
Find out about the University of Bristol's MSc in Optical Communications and Signal Processing, including structure, entry requirements and career prospects.
MSc Optoelectronic and Quantum Technologies
Find out about the University of Bristol's MSc in Optoelectronic and Quantum Technologies, including structure, entry requirements and career prospects.
MSc Oral Medicine
Find out about the University of Bristol's MSc in Oral Medicine, including structure, entry requirements and career prospects.
MSc Orthopaedic Research Methods and Evidence-Based Medicine
Msc palaeobiology.
Find out about the University of Bristol's MSc in Palaeobiology, including structure, entry requirements and career prospects.
MSc Perfusion Science
Msc periodontology.
Find out about the University of Bristol's MSc and Postgraduate Certificate in Perfusion Science, including structure, entry requirements and career prospects.
MSc Policy Research
Find out about the University of Bristol's MSc in Policy Research, including structure, entry requirements and career prospects.
MSc Psychology (Conversion)
Msc psychology of education bps.
Find out about the University of Bristol's MSc conversion programme in Psychology of Education, accreddiated by the British Psychological Society,
MSc Public Health
Find out about the University of Bristol's MSc in Public Health, including structure, entry requirements and career prospects.
MSc Public Policy
Find out about the University of Bristol's MSc in Public Policy, including structure, entry requirements and career prospects.
MSc Public Policy Analysis (Distance Learning)
Msc reproduction and development.
Find out about the University of Bristol's MSc, PGCert and PGDip in Reproduction and Development, including structure, entry requirements and career prospects.
MSc Robotics
Find out about the University of Bristol's MSc in Robotics, including structure, entry requirements and career prospects.
MSc Science Communication for a Better Planet
Find out about the University of Bristol's MSc in Science Communication for a Better Planet, including structure, entry requirements and career prospects.
MSc Scientific Computing with Data Science
Find out about the University of Bristol's MSc in Scientific Computing with Data Science, including structure, entry requirements and career prospects.
MSc Social and Cultural Theory
Find out about the University of Bristol's MSc in Social and Cultural Theory, including structure, entry requirements and career prospects.
MSc Social Innovation and Entrepreneurship
Find out about the University of Bristol's MSc in Social Innovation and Entrepreneurship, including structure, entry requirements and career prospects.
MSc Social Science Research Methods (Management)
Find out about the University of Bristol's MSc in Social Science Research Methods (Management), including structure, entry requirements and career prospects.
MSc Social Science Research Methods (Politics)
Find out about the University of Bristol's MSc in Social Science Research Methods (Politics), including structure, entry requirements and career prospects.
MSc Social Science Research Methods (Sociology)
Find out about the University of Bristol's MSc in Social Science Research Methods (Sociology), including structure, entry requirements and career prospects.
MSc Social Work
Find out about the University of Bristol's MSc in Social Work, including structure, entry requirements and career prospects.
MSc Social Work Research
Find out about the University of Bristol's MSc in Social Work Research, including structure, entry requirements and career prospects.
MSc Society, Politics and Climate Change
Find out about the University of Bristol's MSc in Society, Politics and Climate Change, including structure, entry requirements and career prospects.
MSc Socio-Legal Studies
Find out about the University of Bristol's MSc in Socio-Legal Studies, including structure, entry requirements and career prospects.
MSc Sociology
Find out about the University of Bristol's MSc in Sociology, including structure, entry requirements and career prospects.
MSc Stem Cells and Regeneration
Msc stem cells and regeneration (online), msc strategy, change and leadership.
Find out about the University of Bristol's MSc and PGCert in Strategy, Change and Leadership, including structure, entry requirements and career prospects.
MSc Sustainable Engineering
Msc teaching and learning for health professionals, msc teaching english to speakers of other languages (tesol).
Find out about the University of Bristol's MSc in Teaching English to Speakers of Other Languages, including structure, entry requirements and career prospects.
MSc Technology Innovation and Entrepreneurship
Find out about the University of Bristol's MSc in Technology Innovation and Entrepreneurship, including structure, entry requirements and career prospects.
MSc Translational Cardiovascular Medicine
Find out about the University of Bristol's MSc, PGCert and PGDip in Translational Cardiovascular Medicine, including structure and entry requirements.
MSc Translational Cardiovascular Medicine (Online)
Msc volcanology, msc water and environmental management.
Find out about the University of Bristol's MSc in Water and Environmental Management, including structure, entry requirements and career prospects.
MSc Wireless Communications and Signal Processing
Find out about the University of Bristol's MSc in Wireless Communications and Signal Processing, including structure, entry requirements and career prospects.
Find out about the University of Bristol's PhD in Music, including entry requirements, supervisors and research groups.
Oral and Dental Sciences
Find out about the University of Bristol's PhD in Oral and Dental Sciences, including entry requirements, supervisors and research groups.
PG Certificate (Postgraduate Certificate) Clinical Neuropsychology Practice
Find out about the University of Bristol's Postgraduate Certificate in Clinical Neuropsychology Practice, including structure and career prospects.
PG Certificate (Postgraduate Certificate) Clinical Oral Surgery
Find out about the University of Bristol's Postgraduate Certificate in Clinical Oral Surgery, including structure, entry requirements and career prospects.
PG Certificate (Postgraduate Certificate) Clinical Perfusion Science
Pg certificate (postgraduate certificate) healthcare improvement, pg certificate (postgraduate certificate) healthcare improvement (online), pg certificate (postgraduate certificate) perfusion science, pg diploma (postgraduate diploma) applied neuropsychology, pg diploma (postgraduate diploma) applied neuropsychology (bristol-based), pg diploma (postgraduate diploma) applied neuropsychology (distance learning), pg diploma (postgraduate diploma) applied neuropsychology (online), pg diploma (postgraduate diploma) clinical neuropsychology.
Find out about the University of Bristol's Postgraduate Diploma in Clinical Neuropsychology, including structure, entry requirements and career prospects.
PG Diploma (Postgraduate Diploma) Orthodontic Therapy
Pg diploma (postgraduate diploma) philosophy, pg diploma (postgraduate diploma) theoretical and practical clinical neuropsycho, pg diploma (postgraduate diploma) theoretical and practical clinical neuropsychology.
Find out about the University of Bristol's PG Diploma in Theoretical and Practical Clinical Neuropsychology, including structure and entry requirements.
PGCE Education (Secondary)
Find out about the University of Bristol's PGCE in Education (Secondary) including structure, entry requirements and career prospects.
PhD Accounting and Finance
Phd advanced composites, phd advanced quantitative methods, phd aerosol science, phd aerospace engineering, phd anthropology and archaeology, phd biochemistry, phd biological sciences, phd cellular and molecular medicine, phd chemistry, phd civil engineering, phd classics and ancient history, phd comparative literatures and cultures, phd computational statistics and data science: compass, phd computer science, phd creative writing, phd cyber security (tips at scale), phd digital health and care, phd disability studies, phd dynamic molecular cell biology (wellcome trust), phd earth sciences, phd east asian studies, phd economics, phd education, phd electrical and electronic engineering, phd engineering mathematics, phd english literature, phd exercise, nutrition and health, phd film and television, phd geographical sciences (human geography), phd geographical sciences (physical geography), phd global political economy, phd great western four+ doctoral training partnership (nerc), phd health and wellbeing, phd hispanic, portuguese and latin american studies, phd history, phd history of art, phd innovation and entrepreneurship, phd integrative cardiovascular science (bhf), phd interactive artificial intelligence, phd italian, phd management, phd mathematics, phd mechanical engineering, phd medieval studies, phd molecular, genetic and lifecourse epidemiology (wellcome), phd oral and dental sciences, phd philosophy, phd physics, phd physiology, pharmacology and neuroscience, phd politics, phd population health sciences, phd psychology, phd quantum engineering, phd religion and theology, phd robotics and autonomous systems, phd russian, phd security, conflict and human rights, phd social policy, phd social work, phd sociology, phd south west biosciences doctoral training partnership (bbsrc), phd south west doctoral training partnership (esrc), phd sustainable futures, phd technology enhanced chemical synthesis, phd theatre and performance, phd translation, phd translational health sciences, phd veterinary sciences.
Find out about the University of Bristol's PhD in Philosophy, including entry requirements, supervisors and research groups.
Find out about the University of Bristol's PhD in Physics, including entry requirements, supervisors and research groups.
Physiology, Pharmacology and Neuroscience
Find out about the University of Bristol's PhD in Physiology, Pharmacology and Neuroscience, including entry requirements, supervisors and research groups.
Find out about the University of Bristol's PhD in Politics, including key themes and entry requirements.
Population Health Sciences
Find out about the University of Bristol's PhD in Population Health Sciences, including entry requirements, career prospects and research groups.
Practice-Oriented Artificial Intelligence
Quantum information science and technologies, religion and theology.
Find out about the University of Bristol's PhD in Religion and Theology, including structure, entry requirements and supervisors.
Find out about the University of Bristol's PhD in Russian, including entry requirements, supervisors and research groups.
Social Policy
Find out about the University of Bristol's PhD in Social Policy, including entry requirements, supervisors and research groups.
Social Work
Find out about the University of Bristol's PhD in Social Work, including entry requirements, supervisors and research groups.
Find out about the University of Bristol's PhD in Sociology, including entry requirements, supervisors and research groups.
Sociotechnical Futures and Digital Methods
Find out about the University of Bristol's PhD in Sociotechnical Futures and Digital Methods, including entry requirements, supervisors and research groups.
South West Biosciences Doctoral Training Partnership (BBSRC)
Find out about the University of Bristol's South West Biosciences Doctoral Training Partnership, including structure and entry requirements.
Sustainable Futures
Find out about the University of Bristol's PhD in Sustainable Futures, including entry requirements, supervisors and research groups.
Technology Enhanced Chemical Synthesis
Find out about the University of Bristol's PhD in Technology Enhanced Chemical Synthesis, including entry requirements, supervisors and research groups.
Theatre and Performance
Find out about the University of Bristol's PhD in Theatre and Performance, including entry requirements, supervisors and research groups.
Translation
Find out about the University of Bristol's PhD in Translation, including entry requirements, supervisors and research groups.
Translational Health Sciences
Find out about the University of Bristol's PhD in Translational Health Sciences, including entry requirements, supervisors and research groups.
Veterinary Sciences
Find out about the University of Bristol's PhD in Veterinary Sciences, including entry requirements, research groups and career prospects.
Digital Health
The future of health care is digital.
Taught by Harvard Medical School faculty, this Harvard Online course explores the opportunities and difficulties facing widespread adoption of digital technologies in the US health care system and explores innovative frameworks to think strategically about implementing digital transformation in your organization.
What You'll Learn
How has digital transformation influenced the health care industry?
Millions of health-related data points are captured every day, from information collected by our personal devices and doctor's office visits to public health data collection about disease prevalence and treatment outcomes. Digital technologies have transformed how we buy and listen to music and how we plan our travel. Will there be a similar digital disruption in health care?
Throughout this online digital health certificate program, you will become familiar with developments that have led to digital transformation in health care and weigh the pros and cons of digital technology in health care. You will understand the process of product development in digital health innovation by participating in a fictional hackathon, working alongside other learners to determine which digital tools to invest in.
Using a selection of real-world case studies as a starting point, you will evaluate the potential impact of digital tools on patients, physicians, payers, and future health care ecosystems. In doing so, you’ll consider the impact digital tools have on these stakeholders to understand how data tracking and digital health products can improve patient care, enhance communication between doctors and patients, increase employee benefits and happiness, and track health trends and develop solutions.
While this course emphasizes independent learning, it also provides opportunities for peer collaboration through group assignments and online discussions.
The course is part of the Harvard on Digital Learning Path and Health Care Leadership Learning Path will be delivered via HBS Online’s course platform . Learners will be immersed in real-world examples from experts at industry-leading organizations.
By the end of this digital health program you will:
- Understand how digital technologies can address critical pain points in health care
- Learn how to think about applications of collecting and using data to inform health care, and the privacy risks and analytical pitfalls unique to health care data
- Explore the opportunities and difficulties of implementing new technology in health care, such as artificial intelligence, machine learning, apps, and sensors
- Navigate the systemic barriers and often conflicting needs of health care stakeholders in bringing digital health technologies to market
- Become adept at analyzing gaps in health care that can be closed with technology and data
Continuing Medical Education Information
The Harvard Medical School is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to provide continuing medical education for physicians.
The Harvard Medical School designates this enduring material for a maximum of 14.25 AMA PRA Category 1 Credits™ . Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Upon successful completion of the course, participants will have access to claim their credits through the Harvard Medical School’s continuing education platform.
Your Instructor
Stanley Y. Shaw, MD, PhD is the Associate Dean for Executive Education at Harvard Medical School. In this role, he directs Harvard Medical School's programs for companies and individuals in the health care industry that provide insights into leadership behaviors and emerging technologies. These programs educate learners across diverse sectors of health care, such as tech, IT, biopharma, investing, and care delivery organizations. A practicing cardiologist, Dr. Shaw’s research studies how digital tools, bioinformatics, the gut microbiome, and patient-reported data can be leveraged to better assess health and disease.
Job Outlook
6x more jobs, since january 2020, there has been a significant increase in jobs in the health care industry listing “digital transformation” as a required skill., join the top 6% of the job market, there are more than 29,000 job postings looking for talent with skills including “digital transformation” and “technology entrepreneurship”, among others, while only 6% of job seekers list these skills., data: source: lightcast™, available discounts and benefits for groups and individuals.
Experience Harvard Online by utilizing our wide variety of discount programs for individuals and groups.
Past participant discounts.
Learners who have enrolled in at least one qualifying Harvard Online program hosted on the HBS Online platform are eligible to receive a 30% discount on this course, regardless of completion or certificate status in the first purchased program. Past Participant Discounts are automatically applied to the Program Fee upon time of payment. Learn more here .
Learners who have earned a verified certificate for a HarvardX course hosted on the edX platform are eligible to receive a 30% discount on this course using a discount code. Discounts are not available after you've submitted payment, so if you think you are eligible for a discount on a registration, please check your email for a code or contact us .
Nonprofit, Government, Military, and Education Discounts
For this course we offer a 30% discount for learners who work in the nonprofit, government, military, or education fields.
Eligibility is determined by a prospective learner’s email address, ending in .org, .gov, .mil, or .edu. Interested learners can apply below for the discount and, if eligible, will receive a promo code to enter when completing payment information to enroll in a Harvard Online program. Click here to apply for these discounts.
Gather your team to experience Digital Health and other Harvard Online courses to enjoy the benefits of learning together:
- Single invoicing for groups of 10 or more
- Tiered discounts and pricing available with up to 50% off
- Growth reports on your team's progress
- Flexible course and partnership plans
Learn more and enroll your team !
Learner Testimonials
The majority of digital health learners who participated in our post-course survey report: .
- They can immediately apply their learnings to upcoming projects or projects that they are currently working on.
- The most valuable aspect of the course to be the perspectives from industry leaders and Professor Stanley Shaw.
- They are likely to recommend this course to a colleague or friend.
"I am so grateful to have been able to take this course, and as a working adult with additional family responsibilities, could only have done so by its online, asynchronous nature. Dr. Shaw was an excellent presenter and is an inspiration for my own future endeavors."
Jeanne U. Dentist
"I have started a digital health company focused on provider burnout and improving efficiencies. I plan to have every employee take the course and will be providing it as an employee benefit."
Isaac C. Co-Founder/Chief Technology Officer
Who Will Benefit
Rising Leaders
Health care providers, administrators, managers, and decision-makers who are interested in implementing digital health solutions in their organizations.
Healthcare Investors and Consultants
Investors, bankers, and consultants interested in investing or working with innovative health care technologies.
Tech Entrepreneurs
Developers and entrepreneurs wanting to create tools and technologies to improve health and health care.
Real World Case Studies
Affiliations are listed for identification purposes only.

Katherine Chou
Hear from the Director of Research & Innovations at Google on using health and AI data for social good.
Marcus Osborne
Learn from the Senior Vice President of Walmart Health on using digital technologies to make health care more affordable and accessible.

Hear from the CEO of Omada Health on designing user-friendly digital tools for optimizing patient success.
Syllabus and Upcoming Calendars
Digital technologies hold great potential for enhancing health care, in terms of empowering patients, improving access and equity, and delivering better health outcomes. Yet health care’s digital transformation lags behind that of other industries. This course, Digital Health, aims to help learners unlock digital transformation in health care and improve the industry by providing a framework to enable learners to think strategically about digital health solutions, develop and deploy them in health care’s unique culture and ecosystem, and navigate the sometimes competing needs of health care’s multiple stakeholders.
Learning requirements: There are no prerequisites required to take this course. To earn a Certificate of Completion from Harvard Online, participants must thoughtfully complete modules 1 through 4.
Download Full Syllabus
Download February 2024 Calendar
Download May 2024 Calendar
- Study patient-facing solutions in the Omada Health case.
- Identify barriers to care in simulated clinical interaction, and opportunities for digital solutions to mitigate these.
- Take a patient-centric view of unmet medical needs, key metrics, and outcomes for a digital solution.
- Navigate the potential of digital solutions to improve access but also create new barriers to care.
- Study enterprise AI solutions through Google Health .
- Explore the competing needs of stakeholders for an enterprise digital solution.
- Consider physician needs and apprehensions about digital solutions.
- Evaluate the robustness and potential weaknesses of an AI development pipeline.
- Proactively anticipate how bias can arise in development and deployment of AI algorithms.
- Evaluate how well competing fictional start-ups address the themes of this module.
- Study the Evidation Health case to understand how to solve needs for patients and drug discovery.
- Compare the strengths and weaknesses of different digital business models.
- Differentiate the capabilities of different digital care management platforms.
- Consider the regulatory implications of different kinds of digital health solutions.
- Reflect on obstacles to successful pilots with care delivery organizations.
- Study the Walmart Health case to understand digital solutions in the future of health care.
- Compare health care to other sectors of the economy that are more digitally mature, as a view into the future.
- Understand the usefulness but also limitations of the “patients as consumers” analogy.
- Anticipate changes to the patient experience, culture of health care, and other stakeholder perspectives in a digitally-enabled future of health care.
- Describe the challenges of data coordination and interoperability.
- Evaluate the equity impact of a digital tool.
- Decide which fictional start-up you choose to back based on your.
Earn Your Certificate
Enroll today in Harvard Online's Digital Health course.
Still Have Questions?
What are the learning requirements? How do I list my certificate on my resume? Learn the answers to these and more in our FAQs.

Related Courses
Health care economics.
Taught by Harvard Medical School faculty, this course provides insights into the interactions between industries in the US health care sector and teaches what economic forces are shaping health care.
Data Science Principles
Data Science Principles gives you an overview of data science with a code- and math-free introduction to prediction, causality, data wrangling, privacy, and ethics.
Health Care Strategy
Learn from HBS Professor Leemore Dafny how to align the principles of business strategy with the unique challenges and structures of health care organizations to capture value, define your mission, and lead your organization to success.
Related Blogs and Learner Resources
The business of health care in the united states.
The business of health care in the United States is complicated. How can we ensure that patients have access to care while still adopting important, life-saving innovations that have the potential to improve health and health care?
How To Earn CME Credits with Harvard Online Courses On Health
Harvard University faculty guide you through topics with a focus on the current state of the US health care system and how you can apply innovative approaches to make improvements within your organization.
Best Continuing Education Courses for Health Care Professionals
In order to help you take the next step in your professional development, we have compiled a list of our top professional development courses for health care professionals.
Digital Health @ Harvard
The Digital Health @ Harvard collaboration brings together an interdisciplinary community of scholars, researchers, practitioners, and others at Harvard who have an interest and expertise in digital health issues, broadly conceived.
If you're interested in getting more involved or contributing to the series, please email [email protected]
Brown Bag Lunch Series
The brown bag lunch series features speakers from Harvard as well as collaborators and colleagues from other institutions who research the intersection between health and digital technology. The series is co-hosted by the Berkman Klein Center for Internet & Society, and the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics . The goal of the series is to discuss ongoing research in this research area, share new developments, identify opportunities for collaboration, and explore the digital health ecosystem more generally.
Lunch Series Format
The series consists of a monthly 60-minute brown bag lunch, which will take place on the last Thursday of each month throughout 2017, from 12-1pm. Specific dates are listed below.
The lunches will begin with a 15-20 minute presentation by the speaker, followed by 40-45 minutes of discussion. The host of/venue for the brown bags will rotate among the various co-hosts.
Check below to join any of our upcoming talks, or explore past events.
Our Work 07

Determining Disability
Medicaid work requirements and what the limits of digital health mean for recipients, providers, and states
This year, several states applied for and received permission from the federal government to implement work requirements in their Medicaid programs. Policy designs vary…

Health Care Costs and Transparency
featuring John Freedman, President & CEO of Freedman HealthCare
Health spending continues to outpace wages and GDP, while some new insurance designs transfer greater shares of that to patients’ own out of pocket costs. What is driving health…
Vish Viswanath, Ph.D.
This is a talk in the monthly Digital Health @ Harvard Brown Bag Lunch Series, which is co-hosted by the Petrie-Flom Center for Health Law Policy,…

Holding Hospitals Hostage
From HIPAA to Ransomware
For hospitals and healthcare providers, data protection efforts have long been driven by the Health Insurance Portability and Accountability Act. This talk will look at recent…

Using Mobile Phone Data to Map Migration and Disease
Politics, Privacy, and Public Health
Mobile phone data are providing unprecedented insights into human migration and behavior with relevance for containment of epidemics and response to natural disasters, but what…

Free Independent Health Records
featuring Adrian Gropper, MD
Free Independent Health Records are an important use-case for self-sovereign technology that links individual people with licensed practitioners and connected services. Blockchain…

- Latest news
- UCL in the media
- Services for media
- Student news
- Tell us your story

Fully-funded PhD scholarships in digital health and wellbeing
19 March 2015
Applications are invited from prospective PhD students and UCL staff for three-year fully funded PhD scholarships in digital health and wellbeing.

Bupa Global Institute for Digital Health Excellence (GLIDHE) is a new partnership between UCL and Bupa, established to develop digital health enabled solutions, evidenced by research.
The Institute will focus on the development of predictive techniques for behaviour change that are sustainable, to reduce the global burden of increasing healthcare demand.
This partnership represents a unique opportunity to significantly augment evidence and delivery with both world leading academic institutions and a global health organisation to be thought leaders in digital health.
Behaviour change
With the exponential growth in digital engagement, GLIDHE can leverage academic insight and credibility to evidence behaviour change at both the individual and population levels delivering solutions that will scale, be robust and above all, affordable.
GLIDHE will develop and disseminate an integrated suite of personalised digital behaviour change products, aimed at improving health and wellbeing using up-to-date evidence, state-of-the-art technology and appropriate theories from behaviour and computer science.
Being part of GLIDHE is an opportunity to build a community to generate exciting new ideas in digital health and wellbeing, to improve the health of the world.
Please email expressions of interest in a PhD scholarship to: Lesley Payne, GLIDHE Lead [email protected]
Useful Links
- Bupa Global Institute for Digital Health Excellence

- Weill Cornell Medicine

Institute of Artificial Intelligence for Digital Health
Our mission is to advance individualized health and healthcare with data-driven insights derived from applying artificial intelligence technologies. The institute will establish a community of experts across multiple disciplines in computational science and clinical medicine, facilitate collaborations, promote multi-disciplinary research, and engage in entrepreneurship and technology commercialization.

Institute of AI for Digital Health
402 E 67th St New York, NY 10065
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- NAM Perspect
- v.2022; 2022

The Promise of Digital Health: Then, Now, and the Future
Amy abernethy, laura adams.
National Academy of Medicine
Meredith Barrett
Christine bechtel, patricia brennan.
National Library of Medicine
San Francisco
Judith Faulkner
Epic Systems
Elaine Fontaine
Stephen friedhoff, john halamka.
Mayo Clinic
Michael Howell
Google Health
Kevin Johnson
University of Pennsylvania
Blue Shield of California
Deven McGraw
Ciitizen Corporation
Redonda Miller
Johns Hopkins Hospital
Microsoft Corporation
Jonathan Perlin
The Joint Commission
Donald Rucker
UnitedHealth Group
Lucia Savage
Yale New Haven Health System and Yale School of Medicine
Stanford University
The Scripps Research Institute
Reed Tuckson
Kristen valdes.
b.well Connected Health
June 27, 2022
Digital Health in the 21st Century
Over the past several decades, the development and accelerated advancement of digital technology has prompted change across virtually all aspects of human endeavor. The positive and negative effects of these changes have been and will remain the focus of active speculation, including the implications for human health. Application of mechanical and digital recording and capture of physical status, experiences, and narratives have set the stage for revolutionary progress in individual health and medical management, population-wide health strategies, and integrated real-time generation of new knowledge and insights. Together, these developing digitally mediated capacities are termed digital health.
Digital health has evolved as a broad term encompassing electronically captured data, along with technical and communications infrastructure and applications in the health care ecosystem. Revolutionary advances in digital health are transforming health, medicine, and biomedical science, and redefining and re-engineering the tools needed to create a healthier future. Developments such as cloud computing, artificial intelligence, machine learning, blockchain, digitally mediated diagnostics and treatment, telehealth, and consumer-facing mobile health applications are now routinely used in self-management, health care, and biomedical science. These developments promise to drive earlier diagnoses and interventions, improve outcomes, and support more engaged patients ( McGinnis et al., 2021 ).
In the mid-20th century, the newly established World Health Organization (WHO) defined the concept of health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” ( WHO, 2006 ). As an integrative concept, this definition is a vision for the planet that is at once bold and elusive, even for the United States as the world’s wealthiest nation. The WHO definition is clear that health derives from much more than medical care. Since WHO’s founding, much has been learned about how different factors, including but extending far beyond medical care, interact to shape health prospects. Indeed, research indicates that social and behavioral factors both outweigh medical care in determining health status and modulate the contributions of genetics and physical environments ( Kottke et al., 2016 ; McGovern et al., 2014 ; Schroeder, 2007 ; McGinnis et al., 2002 ).
Unfortunately, U.S. health policies and health system investments remain misaligned with these insights. In the U.S., approximately 90% of all health expenses go to disease and injury treatment rather than to addressing the predisposing factors of these illnesses and injuries. By 2020, U.S. health expenditures had grown to $4.1 trillion. Spending in the health sector is projected to increase to over $6 trillion annually and encompass 20% of the nation’s gross domestic product by 2028 ( Keehan et al., 2020 ; CMS, 2019 ). The U.S. is falling far short of the WHO vision, despite spending nearly twice as much as other high-income countries. The U.S. currently has a lower life expectancy, higher rate of death by suicide, higher chronic disease burden, higher rates of preventable hospitalizations, higher use of unnecessary expensive testing and procedures, and lower use of primary care than its peer countries ( Tikkanen and Abrams, 2020 ).
Despite important gains in the last two decades, made possible by significant investment by payers, providers, and the federal government in electronic health records (EHRs), progress toward interoperable systems, and advanced technology to coordinate care and manage disease, the promise of digital health remains illusory. The ability to use interoperable digital technology to improve the effectiveness, efficiency, equity, and continuity of care remains substantially conceptual. For example, digital interfaces in inpatient care systems are often clumsy; volumes of health data are mostly sequestered, inaccessible, and difficult to aggregate in a meaningful and actionable way, in part due to the ongoing need for evolving data standards. In addition, digital tools and data are relatively ineffective in assisting clinicians in better understanding patient and family preferences and circumstances that facilitate health progress outside of the clinic. The notion of digital tools that can be applied in widespread fashion to coordinate health care organizations and public health efforts to identify and engage those at particular risk from behavioral, social, and environmental public health risks remains rudimentary at best. The expansive vision of real-time generation of evidence in a learning health system that links datasets and analyzes them using artificial intelligence and machine learning is nascent and limited to a few pilots.
Ongoing and accelerated progress must be made to fully realize the vision of a learning health system. In the digital age, regardless of the specific barrier to the creation and support of individual and population health (e.g., COV-ID-19, staff burnout, challenging financial outlook, equity, etc.), digital health can and should act as a “force multiplier” of the interventions to combat these challenges. As active participants in advancing prospects and practices in digital health, the authors of this paper hope to:
- highlight the compelling possibilities and unresolved challenges for advancing trustworthy digital technology for the benefit of all people at every stage of their lives;
- underscore the importance of ensuring that the benefits are equally shared across society;
- identify the structural, technical, and policy preconditions for long-term progress; and
- identify critical priorities for cooperation and collaboration between policy makers, practitioners, and industry leaders to propel the development and application of best-in-class digital health tools.
This paper aims to provide a comprehensive review of digital health tools and their promise and to identify critical priorities for cooperation and collaboration among policy makers and industry leaders. The challenge is addressing both the breadth and depth of the issues, which are multifactorial and overlapping.
It is important to note that the narrative and suggestions here represent the views of the individual authors, not necessarily those of the National Academy of Medicine or the organizations with which the authors are affiliated. In developing the text, the authors have been informed by their respective roles and responsibilities in those organizations. These include various efforts in contending with the digital health challenges and opportunities of the COVID-19 pandemic. The discussion paper Digital Health COVID-19 Impact Assessment: Lessons Learned and Compelling Needs was produced in parallel to and in coordination with this work and serves as a use case of the key concepts presented here ( Lee et al., 2022 ). In addition, the development of this paper was informed by the National Academy of Medicine Leadership Consortium’s Digital Health Action Collaborative (DHAC) and DHAC’s prior work stewarding development of the international statement on Digital Health and the Learning Health System, issued collectively in 2020 by national academies of science and medicine of 14 countries ( NASEM, 2020 ).
Digital Innovation and Medical Care
Digital technology has now been developed and applied to every aspect of health and health care. Figure 1 groups the various digital health tools into a dozen application arenas, but the individual applications number in the thousands.

SOURCE: National Academy of Medicine. 2019. Digital Health Action Collaborative, NAM Leadership Consortium: Collaboration for a Value & Science-Driven Health System.
The authors see the potential in digital innovation in health care delivery in the following areas: advancing diagnosis and treatment, ensuring care continuity, facilitating off-site patient management through telemedicine, partnering with individuals to support self-management, and reducing error and waste in the delivery system.
Advancing Diagnosis and Treatment
Research shows that a significant proportion of health spending is attributed to chronic diseases, with individuals experiencing multiple comorbidities accounting for a disproportionate share of expenditures ( Buttorff et al., 2017 ). Although additional research is necessary, a recent review concluded that self-management as part of a treatment program for patients with chronic conditions has small-to-moderate impacts on health behaviors, health outcomes, and service utilization and should be an ongoing priority in promoting population health ( Allegrante et al., 2019 ). Thus, the market appetite and the necessity exist to facilitate diagnosis, reduce disease burden, and improve care for those who experience chronic disease. To address these problems, innovators, software vendors, payers, and government regulators are investing heavily in digital health solutions for diagnosis and treatment, with particular attention to high-need, high-cost populations ( The Commonwealth Fund, 2016 ).
An example of a diagnostic tool enhanced by digital health includes smartphone-based photoplethysmography (using a smartphone camera to capture video from the subject’s index fingertip), combined with a deep neural network, a form of artificial intelligence (AI), to detect diabetes ( Avram et al., 2020 ). While not widely adopted, such tools could be used for self-administered, low-cost, widespread screening. AI is also used in radiology and pathology to augment human interpretation of diagnostic (e.g., ocular, x-ray, or magnetic resonance imaging) and pathology slide images, supporting potentially more accurate and timely diagnosis and individualized treatment plans for various cancers and renal disease ( Barisoni et al., 2020 ). Drug researchers and manufacturers are also leveraging various forms of AI for patient recruitment, virtual engagement, and literature review, and using the technologies to assist in detecting and refining pharmaceutical targets ( Lamberti et al., 2019 ).
Treatment decisions can be augmented by clinical decision support (CDS) systems and enriched with advanced analytics. An editorial in the New England Journal of Medicine succinctly summarized the challenge: “The complexity of medicine now exceeds the capacity of the human mind” ( Eddy, 1982 ). While AI-based systems are currently unable to discern a grimace, notice sweating, or hear a tremor in a patient’s voice—skills at which humans excel—these systems offer the unique opportunity to augment clinician performance by creating order and transforming vast amounts of mostly unstructured data into clinically actionable information to support optimal care. This field, although nascent, is rapidly advancing. For example, AI has been used to improve the speed of prediction and diagnosis of sepsis ( Goh et al., 2021 ). Integrated with the care delivery workflow, these technologies could identify patterns, form linkages between disparate data sources, and suggest treatment options for clinicians to review. In addition, AI-powered CDS systems might offer opportunities for improving efficiency and mitigating clinician burnout, another potential downstream benefit.
Ensuring Care Continuity
Even the most sophisticated digital diagnostics will have little impact on clinical outcomes if they are implemented in a fragmented health care ecosystem. Regulations promulgated by the 21st Century Cures Act Final Rule (Cures Act) have the potential to address this shortcoming by promoting seamless interoperability and supporting increased control for the individual regarding their health data ( HealthIT.gov, 2020 ). The Cures Act addresses foundational standards, including technical, syntactic, and semantic issues surrounding health data interoperability and prioritizes ensuring patients have choices when managing their own health data. Further complexities associated with a robust trust framework, data accuracy, identity matching, and privacy protections of individual data managed by noncovered entities will likewise be critical to confront.
Significant progress on interoperability has occurred over the past decade with the implementation of foundational data standards such as Health Level 7 Fast Healthcare Interoperability Resources (FHIR) ( HL7 International, n.d. ), SNOMED ( SNOMED International, n.d. ), RxNorm ( NLM, 2022 ), and the United States Core Data for Interoperability (USCDI) ( HealthIT.gov, n.d. ). Still, the broad interoperability of health care data platforms is incomplete in many settings due to incomplete record availability, lack of terminology standards, and concern about bidirectional incorporation of data between health systems using different EHRs. In a 2019 study of primary care physicians in high-income countries, the Commonwealth Fund (2019) found that just over 50% of American primary care physicians surveyed were able to electronically exchange data with physicians outside of their practice. In addition, since health is not primarily produced by health care, interoperability with data outside of EHRs may add to a holistic picture of an individual and support continuity of care. However, this level of interoperability is nascent, as demonstrated by a recent review of data exchange capacity of wearables, which found limited ability to transfer data from mobile monitoring systems into medical records ( Muzney et al., 2019 ). The power of EHR systems to capture and organize clinical data allows for rapid cycle learning and organizational agility, but barriers—both technical and economic—to transmitting non-native data into the EHR limit the comprehensive view of individuals and populations needed to transform health care delivery and the health system writ large. To facilitate data interoperability, the U.S. health system must expand embedded, open-source interoperability beyond nationally regulated technologies like EHRs.
Research has documented the potential for Health Information Exchange (HIE) and interoperability to improve care coordination and reduce costs ( Walker et al., 2005 ), and will likely also benefit public health reporting. An example of HIE use to support care coordination is the delivery of near real-time dashboards to primary care and substance use disorder providers about inpatient and emergency department admissions and discharges for their patient panels, supporting post-discharge care coordination ( HealthIT.gov, 2017 ). Still, patients and providers will struggle to realize these benefits at scale as the existing reimbursement system continues to disincentivize care coordination, which results in duplicative service utilization. The ongoing transition to value-based payment can support the realignment of financial incentives and serve as a significant driver for expanding interoperability ( Biel et al., 2019 ).
In this regard, banking, which provides ubiquitous, near real-time, standardized access to account information globally, provides lessons about industry-wide information exchange that might be adopted in health care. The Society for Worldwide Interbank Financial Communications (SWIFT) established a financial transaction messaging system in the 1970s with a focus on essential transactions, a strong business case for participation, and an industry-supported oversight organization ( Glaser, 2019 ). The Office of the National Coordinator for Health IT (ONC), through the Trusted Exchange Framework and Common Agreement (TEFCA), has made inroads toward this vision with the formal recognition of an industry-supported oversight organization through the Recognized Coordinating Entity (RCE), which was awarded to the Sequoia Project in 2019 ( HealthIT.gov, 2022 ).
Facilitating Off-Site Patient Management through Telemedicine
Digital tools that collect data and support interventions outside the clinical setting offer meaningful opportunities to identify risks and engage patients. Consumer-facing apps and clinical monitors that actively or passively collect data can also serve as an early warning system for prevention and disease management. During the COVID-19 pandemic, digital contact tracing apps provided patients with notifications about potential exposure to COVID-19. Beyond COVID-19, some tools generate warnings to individuals or caregivers regarding changes in environmental risks, such as pollen or air pollution alerts, while other platforms generate alerts to patients, families, and providers in the event of disease exacerbation. Additionally, while not widely acceptable or accessible by all populations, use of remote patient monitoring (RPM) tools increased during the COVID-19 pandemic. RPM enables clinicians to assess symptoms for patients at home with mild cases of COVID-19 and observe non-COVID-19-related health outcomes in the context of daily living for patients with chronic conditions (e.g., Blue-tooth scales for patients with congestive heart failure, connected blood pressure cuffs for patients with hypertension).
Digital tools have also expanded care delivery for providers beyond the hospital or exam room. A 2020 analysis found that virtual urgent care visits could reduce the need for emergency room care by approximately 20%, and 20% of all office care, outpatient, and home health services could be delivered virtually or near-virtually ( Bestsennyy, et al., 2020 ; Cigna Newsroom, n.d. ). Non-acute care visits for many conditions were implemented virtually during the COVID-19 pandemic to reduce risk of exposure for patients and providers. Even with the sharp decline in telehealth in 2021—after the steep rise associated with COVID-19 in 2020—a review by a large payer in 2022 supported the value of virtual care ( Cigna, 2022 ).
Even acute care can be delivered outside the health care delivery setting, as witnessed during the COVID-19 pandemic when severely ill patients occupied many hospital beds ( Heller et al., 2020 ). Virtual intensive care units can deliver remote 24/7 monitoring of patients by intensivists who can manage patients in multiple locations, allowing patients to get intensive care unit-level care in community hospitals.
Partnering with Individuals to Support Self-Management
Given that most chronic disease management occurs outside of the traditional health care setting, partnering with individuals so that they can fully engage in their own care and meeting people where they are physically and mentally is essential to achieving better health outcomes, improving quality of life, and reducing health care spending ( Allegrante et al., 2019 ). However, meeting individuals on their own terms may present multiple challenges to both individuals and the delivery system. Basic knowledge gaps about anatomy and physiology are worsened by issues of language fluency, health and reading literacy, numeracy, conflicting cultural beliefs, and limitations in cognitive capacity. These same challenges may be further exacerbated by poor medication tolerance and complex clinical care plans, including polytherapy and polypharmacy ( Settineri et al., 2019 ). Access issues, including distance from the delivery system for rural residents, lack of transportation, and difficulty taking time away from work, all affect attendance at provider visits and can result in delays in seeking care. Financial barriers force individuals to choose between needed health care and medication and other household expenses, can result in not taking medicines as prescribed, including pill splitting and dose skipping ( Kearny et al., 2021 ). These barriers often lead to clinical inertia and are amplified by structural racism, furthering health disparities among underresourced communities.
By applying digital tools successfully used in other industries, such as consumer-directed, preference-based scheduling; personalized recommendations; and regular text communications, the health care system may be positioned to develop a more robust partnership between individuals, families, and providers. Data and digital health tools serve as a bonding agent in their shared understanding of the individual’s state of health and a shared health management plan. Individuals and families have grown accustomed to mobile and online tools in other aspects of their lives, such as airline booking, car services, and banking. Developing a robust partnership between individuals, families, and providers requires further adoption of systems that function the same way that these other tools do, offering patient-centric, easy, and secure two-way communication for appointment booking, self-check-in, and feedback surveys. Such tools can and should be seamlessly interoperable within health systems workflows. While patient portals support many of these functions, adoption among adults in the U.S. is below 50% ( HINTS, 2018 ). Strategies should acknowledge user comfort with technology and offer multiple communication modes, including text messaging, audio, and video, depending on the user preference ( Zachrison et al., 2021 ). These approaches also need to consider form and frequency of communication to ensure maximum engagement and understanding.
Reducing Error and Waste in the Delivery System
Extensive research indicates that health care resources are inappropriately allocated within the current system. Waste has been shown to carry consequences for quality outcomes and patient safety (e.g., medical errors and delays) and economic efficiency (e.g., unnecessary spending) ( Shrank et al., 2019 ). In the context of safety, since the Institute of Medicine’s (IOM) report titled To Err Is Human: Building a Safer Health System was published in 2000, health care providers have made progress in reducing harm in hospital settings, but that progress varies widely ( IOM, 2000 ). Equally troubling is the inability to accurately measure the harm associated with the lack of timely, standardized, and accurate information movement across systems ( Bates and Singh, 2018 ). As identified in a 2010 report from the IOM titled The Healthcare Imperative: Lowering Costs and Improving Outcomes , disruptive innovation has been foundational across sectors to reduce waste and increase efficiency, and its use as a strategy to address these issues in health care is essential ( IOM, 2010 ).
The digitization of health data has long been considered the foundation for patient safety, operational efficiency, and quality of care. It was also a driving force behind the Health Information Technology for Economic and Clinical Health (HITECH) Act, which incentivized the adoption of EHRs ( IOM, 2004 ; HealthIT.gov, 2009 ). By 2017, 80% of office-based physicians and 96% of non-federal acute care hospitals had adopted certified EHRs ( Health IT Dashboard, 2016 ). Multiple studies have documented improvements in care quality ( Atasoy et al., 2019 ; Buntin et al., 2011 ). However, in a recent survey of over 5,000 physicians across specialties, perceived EHR usability was poor. Results showed a “dose-response relationship between EHR usability and physician burnout”, which is negatively associated with patient safety ( Melnick et al., 2020 ; Panagioti et al., 2018 ). However, patient safety is improved regardless of physician experience ( Tanner et al., 2015 ). In addition, ongoing opportunities to better integrate clinical and administrative functions, streamline documentation (e.g., via voice technologies), automate quality metrics reporting, and embed AI and advanced CDS systems represent meaningful advancements that EHR vendors are pursuing as these platforms mature—either as new functionality within their platforms or by connecting to external third-party vendors, creating a “both/and” approach to maximizing efficiency.
When it is clinically appropriate to address health concerns without an exam or with good quality video or still images, telehealth can reduce delays for specialty consultations and primary care, as the constraints of a shared physical space for an exam are eliminated. Advanced analytics can also reduce waste by helping health care professionals work at the top of their licenses. Advanced analytics can improve clinical risk stratification, allowing less skilled care team members to address the needs of patients who require minimal care. Higher skilled care team members are freed up to spend additional time with patients with complex medical needs, resulting in the delivery of the right care, to the right patients, at the right time, in the right place, by the right clinical team members. Machine learning (ML) and natural language processing (NLP) algorithms have outperformed nursing staff and provided comparable levels of accuracy to skilled physicians in assessing acuity risk in emergency departments ( Ivanov et al., 2021 ). However, caution must be used because algorithms can inadvertently perpetuate significant bias ( Tanner et al., 2015 ).
Process automation is another area of opportunity to use digital health technology to improve efficiency in both ambulatory care and inpatient settings. Barcoding has been widely used in hospital pharmacies for over a decade, resulting in a reduction in adverse drug events ( Boyde and Chaffee, 2019 ). Repetitive tasks such as scheduling, billing, capacity coordination, and asset management are amenable to automation, optimizing use of system resources and creating a frictionless experience for patients. For example, health care organizations can emulate the airline industry in maximizing automation and self-service functionality in scheduling while addressing customer demand, service supply, and equipment needs ( ONC, 2020 ).
Digital Innovation and Population Health
Figure 1 also identifies various tools applicable to improving population health and drivers of health that are upstream from medical care—e.g., geospatial and environmental sensors, personal health devices, and knowledge generators and integrators. The importance of using digital tools in helping to integrate critical social services into care delivery has been clearly demonstrated by the nation’s experience with COVID-19 and the disproportionate impacts on communities of color and other economically disadvantaged and underresourced populations ( Isasi et al., 2021 ; Health IT Dashboard, 2016 ). Innovations in digital health hold the potential to help identify and address many of the barriers to achieving the vision of a healthy society. When thoughtfully designed, equitably deployed, and effectively used, digital health tools have the potential to improve the identification, measurement, and modification of the root sources of illness, health, and well-being. Without the precise analytic information possible through a robust digital infrastructure, the nation will not be able to accelerate the identification and engagement of the causes and consequences of structural racism, which plays such a perverse and pervasive role in the health disparities of far too many Americans.
As digital health tools become increasingly sophisticated and capable of capturing social, behavioral, and environmental determinants of health, clinicians and caregivers can learn more about the individual in the context of their daily lives, including individual preferences, values, interactions, and exposures, to deliver targeted preventive and acute care and to restore health after illness. This digitally enabled health ecosystem has the potential to create long-term partnerships between individuals and their care teams that support healthy behaviors. Similarly, if thoughtfully designed, equitably deployed, and effectively used, such digital health applications have the potential to help prevent, mitigate, and reduce disparities in access and care ( Craig et al., 2020 ). In such a system, health information flows freely within a trust-enabled and robust security and privacy framework across both the health care industry and nontraditional commercial entrants into the market.
Digital Innovation and the Social Determinants of Health
Kaiser Family Foundation defines the social determinants of health (SDoH) as “the conditions in which people are born, grow, live, work and age that shape health,” with these conditions including “socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care” ( Artiga and Hinton, 2018 ). Although approximately 15% of premature deaths are attributed to SDoH, these upstream drivers of health have largely been considered out of scope and not yet routinely addressed by providers or health care systems ( McGinnis et al., 2002 ).
For digital technology to have a meaningful effect on SDoH, information about nonmedical factors and services must be better collected and integrated into mobile apps and standardized, aggregated, and integrated into EHRs to promote trust and ensure secure and private management. Digital tools could play a role in screening and identifying SDoH factors that impact a patient, alerting the provider to discuss them with the patient at the next visit, and connecting the patient with relevant community services. While existing digital health tools are already capable of supporting the collection, exchange, and integration of SDoH to support risk stratification and shared care planning, the benefits of these tools have been limited by inconsistent use across care delivery settings and the significant risk of algorithmic bias ( Meyer et al., 2020 ; Lindau, 2019 ). For example, scheduling algorithms designed to identify patients who frequently miss appointments may both stigmatize people of lower socioeconomic status and distort the real issues. Many of these “no shows” cannot afford childcare or to leave work for a medical appointment, or they may have health problems that cause disability or reduced cognitive function, causing them to miss appointments ( Murray et al., 2020 ). Understanding and intervening on SDoH and systems factors could reduce missed appointments, helping patients to get needed care and reducing lost care capacity for the system. These issues highlight the need for transparency in data collection and encoding and the criticality of proactive action to mitigate unintended consequences and biases when developing algorithms.
Digital health technologies are also developing new use cases to address various environmental factors, including air pollution and climate change. Digital inhaler sensors have been used to monitor when and where patients with asthma used medications and needed adjustments to treatment plans and are associated with a reduction in rescue inhaler use, an improvement in symptom-free days for individuals, and a reduction in health care resource utilization ( Merchant et al., 2018 ; Barrett et al., 2013 ). Furthermore, “aggregated data on inhaler use, combined with environmental data, led to policy recommendations”, a community asthma notification system, community-wide improvements in asthma symptoms, and reductions in asthma-related emergency department use ( Barrett et al., 2018 ; Barrett et al., 2013 ). Consumer-facing tools also can provide smartphone alerts for heat or air pollution data at the neighborhood level, making public health efforts more efficient. The use of telehealth and HIE can also support coordinated patient care during natural disasters. Of course, none of these tools address the root causes of these environmental problems—for example, a person might be able to know that their drinking water contains lead, but the tool cannot assist in solving the underlying drinking water problem. These SDoH must be addressed at the root level to realize improved health and well-being for all.
Digital Innovation and Health Behavior
Although consumer demand for interventions that support behavior change is high, and successes have been evident in areas such as tobacco use and the consumption of foods high in saturated fat, the complexity of behavioral interventions can be vexing. Consider the case of weight management programs. The overall weight loss market in the U.S. in 2020 was estimated at $71 billion, yet many programs elicit only marginal and temporary changes in weight, with participants often experiencing weight regain ( LaRosa, 2020 ; Hall and Kahan, 2018 ). As such, interest in digital and virtual weight loss programs is mounting as an alternative ( LaRosa, 2020 ). However, while several well-controlled studies have demonstrated improved clinical outcomes when incorporating digital tools relative to usual care, most applications in the consumer marketplace are not supported by evidence, nor are they produced by subject matter experts in health behavior change ( Gordon et al., 2020 ; Pagoto and Bennett, 2020 ; Steinmetz et al., 2020 ).
This example illustrates some of the broader challenges and opportunities for digital tools to support self-management of individual health behaviors. In their ideal form, evidence-based digital health tools that focus on health behavior can improve self-awareness, provide on-demand health information and education, support improved self-efficacy, and promote accountability with social support networks, health coaches, and providers. The resulting data can also be analyzed to identify behavioral risk factors that contribute to chronic disease, resulting in real-time, personalized feedback and messaging to support health behavior change in a way that is more compelling than traditional patient education ( Shegog et al., 2020 ; Barrett et al., 2013 ). Similarly, these data can be aggregated at the community level to more accurately measure the health behaviors and activities of populations, supporting resource allocation and data-driven public health decision making at the local level ( Barrett et al., 2013 ).
Digital health tools designed to support adherence to treatment plans also present an important opportunity. Connected self-monitoring tools (e.g., glucometers), wearables, digital inhaler sensors, and SMS messages and reminder systems have shown promise in patients with a variety of conditions, including epilepsy, asthma, chronic obstructive pulmonary disease (COPD), diabetes, depression, and hypertension ( De Keyser et al., 2020 ; Kaye et al., 2020 ; Anderson et al., 2019 ; Shan et al., 2019 ; Patel et al., 2013 ). For example, objective, passive data about adherence to asthma medication treatment plans identified issues with medication-taking technique errors and presented an opportunity for intervention and education ( Anderson et al., 2019 ). Interestingly, patients with asthma and COPD who received digital support (reminders for missed medication doses and education) increased their medication adherence during the early months of COVID-19 ( Kaye et al., 2020 ).
Digital Innovation, Genomics, and Precision Health
Digital technologies are accelerating the “genomics revolution”—advances in understanding the health implications of structural and functional variations in the human genome. These are often discussed in terms of augmented abilities to target individual medical interventions more precisely. While this is certainly an important likelihood, broader scale benefits in terms of reduced mortality and morbidity are likely to result from “precision public health”—the ability to better identify populations at greater risk from certain characteristics or exposures and implement protective interventions.
Whole genome sequencing and digitally enabled risk scores generated by such sequencing will help identify individuals and groups at risk for common health conditions in their earliest stages. These data can be used to support mitigation strategies such as behavior change, medication use, or early screening to decrease the risk of sequelae from a genetic disease or gene variants. Examples of existing consumer-facing mobile health apps today draw from several data sources and partnerships, including self-reported family history data, laboratory results from personal genetics companies, and collaboration with providers, payers, or employers ( Tung et al., 2018 ). The ongoing integration of genetic or genomic data and clinical histories, accelerated by emerging AI and ML technologies, increases the feasibility of leveraging precision medicine into clinical practice ( Luchini et al., 2022 ). For example, AI is currently used in oncology, including FDA-approved AI used in support of care for breast, lung, and prostate cancers ( Luchini et al., 2022 ). Advanced computational analytics used on such datasets could ultimately be employed to deliver near real-time feedback to individuals to promote health using a voice assistant, much like a digital health coach ( Topol, 2019 ).
Digital Innovation and the Learning Health System
The application of digital technologies at scale serves as the nervous system for the continuously learning health care system: “one in which science, informatics, incentives, and culture are aligned for continuous improvement, innovation, and equity—with best practices and discovery seamlessly embedded in the delivery process, individuals and families active participants in all elements, and new knowledge generated as an integral by-product of the delivery experience” ( NAM, 2020 ). Digital health will serve a critical role, and its promise must be fully leveraged. Effectively applied, digital health tools have the potential to catalyze progress on each of the key principles for a digitally facilitated learning health system, presented below in Box 1 .
Core Principles for Stewards of the Digital Health Infrastructure and Data
Personal: Discretion on control and use of personal data resides with the individual or their designee.
Safe: Data stewardship protocols safeguard against use resulting in personal harm.
Effective: Data are collected and maintained according to validated stewardship protocols.
Equitable: Data systems are designed to identify and counter bias or disparities.
Efficient: Every digital equipment acquisition or service license enhances health system interoperability.
Accessible: Data are available when and where needed for decision-making.
Measurable: Digital health performance is continuously monitored for accuracy and interoperability.
Transparent: Personal data sources and uses are clearly indicated, including timing and context.
Adaptive: Data strategies are regularly calibrated to ensure continuity, currency, and utility.
Secure: Data sharing protocols are considered secure by users.
SOURCE: National Academy of Medicine Leadership Consortium: Collaboration for a Learning Health System. n.d. Digital Health Action Collaborative Strategic Framework.
Leveraging Big Data for Knowledge Generation
Much of the data collected in clinical care or recorded in consumer apps are available for further research and learning. Currently, the broader application of available health data is more likely to be used in service of product development rather than for learning, discovery, or continuous improvement of the health of individuals, families, or populations. There is an unrealized opportunity to share, aggregate, and analyze that data in alignment with the goals of a learning health system while also protecting and tightening the processes and procedures for unwarranted access to and use of personal data and inadvertent sharing of sensitive data, including medical records, via third-party consumer apps.
The investment, innovation, and amassing of data present important opportunities to affect not just health and the health care delivery system but also knowledge development in a learning health system. If appropriately managed and analyzed, datasets that incorporate structured and unstructured clinical data, SDoH information, genomics, digital phenotype data collected from wearables, and other data can make it possible to change baseline understandings of health and disease ( Engelhard et al., 2020 ; Jain et al., 2015 ). Statistical tools and techniques, including AI and ML, can be used to develop dataset assessment tools and to support evolving research designs that meld traditional randomized controlled trials (RCTs) with observational studies. Similarly, analytical models can be applied across at-risk populations to ensure equity in opportunities to create health and treat disease. Development of virtual health data trusts, with shared governance and individuals controlling and contributing their data to support scientific discovery, present an important opportunity to distribute the costs and maximize research output while protecting individual agency and privacy ( Baker et al., 2016 ; Ideas for Change, 2016 ; MiDATA, n.d. ). If successful, this digitally enhanced approach to research could allow multiple stakeholders, including professional societies, health care providers, patient advocacy groups, individuals, families, legal experts, medical administrators, the private sector, and governments, to share data, experiences, and research priorities.
Leveraging Big Data for Population-Level and Public Health Insights
Fully realizing the benefit of vast datasets with information collected in near real time across the health continuum promises to improve population and public health. Some noteworthy examples of these public datasets include the National Patient-Centered Clinical Research Network (PCORnet) ( PCORNet, n.d. ), the Research Data Assistance Center (ResDAC) for CMS data ( ResDAC, 2022 ), the Observational Health Data Sciences and Informatics program (OHDSI) ( OHDSI, 2022 ). This promise includes the active and passive collection of real-time data from patients’ daily living activities, gathered in clinical systems and payer systems and the analysis of that data to make well-reasoned decisions using standard analytics and AI/ML ( Singhal et al., 2020 ; Bughin et al., 2017 ). To apply analytics tools to health care will require significant investment; fortunately, the Cures Act authorized $1.5 billion over 10 years to support the NIH’s All of Us Research Program, which is designed to build and make available to researchers a secure and expansive database, including EHR, survey, and biometrics data of one million people to support medical discovery ( NIH, 2020 ). While NIH did not explicitly create the All of Us program for AI/ML, as a by-product of the program, researchers will have access to new datasets and platforms upon which they can train their models.
As health systems, payers, and community organizations collaborate and share data to serve specific populations, public health agencies are positioned to seamlessly collect data and apply advanced analytics for health surveillance and community intervention. Interoperability links health systems, community agencies, geographical information systems, and public health agencies to address medical, environmental, and SDoH ( Buckeridge, 2020 ). Interoperability can also create opportunities, via big data and precision public health, to tailor interventions to subpopulations, which will help ensure equity ( Buckeridge, 2020 ). During COVID-19, the public health sector is experiencing an opportunity to test a variety of new precision public health tools, including the use of cell phone location data, activity trackers, and sewage data to intervene early to identify outbreaks and to limit morbidity and mortality ( Rasmussen et al., 2020 ).
Requirements for the Digital Health Infrastructure
Digital technology serves as the nervous system for the learning health system and accelerates the identification and elimination of wide-scale disparities in individual, local, regional, and global health care. As individuals gain more access to their health data via application programming interfaces (APIs), and as providers use these data for critical clinical decision making using AI/ML, it is essential to consider several foundational infrastructure requirements. Figure 2 presents the essential infrastructure requirements for progress in digital health. While there has been some progress, opportunities remain in each interrelated component. Each area must be carefully reviewed and addressed to fully establish the framework to allow the benefits of digital health to be fully realized. Of particular interest for priority action are individual access and engagement, equity and ethics, privacy and identifier protocols, cybersecurity, data quality and reliability, data storage, sharing, and stewardship, interoperability, AI/ML, and workforce.

Individual Access and Engagement and Equity and Ethics
To ensure digitally facilitated health for all, access to digital health writ large, supported by widespread broadband internet access, is essential across all economic strata and all regions of the U.S. Unfortunately, while COVID-19 resulted in the practical and essential application of telehealth, key gaps in consumer access to such technologies—“the digital divide”—were also exposed.
Equity in available broadband access will spur growing consumerism and engagement in health and health care. The public has routine exposure to digitally facilitated convenience, agency, transparency, and privacy based on their experience with other industries and now expects the same from the health care ecosystem ( Accenture, 2019 ). As the understanding of what creates health and well-being grows, it is imperative to engage patients, families, and communities in the design of new structures, processes, and solutions to support health and well-being. It is also essential to address systemic racism and institutional health inequities and disparities within the U.S. when designing these new structures, processes, and solutions ( Feagin and Bennefield, 2014 ). These steps are necessary to mitigate the risk that new technologies will deepen the existing digital divide or perpetuate historical mistrust in the health system.
In addition, it will be important to translate what is learned through the collection of digital health data writ large (e.g., better insight into environmental determinants of health, Barrett et al., 2013 ) into local and national policies to make these learnings applicable at the individual and population level. These improved policies should, in turn, translate into community improvements (e.g., urban planning decisions about not placing schools next to freeways, informing national air quality standards with research into the association between air pollutants and respiratory symptoms) to improve the health of those who live in that community.
Privacy and Identifier Protocols
The opportunity to share, aggregate, and analyze health data to improve individual health and to advance the learning health system is significant, as is the risk of loss of privacy for individuals sharing their most sensitive data via third-party consumer apps. Consumers have a limited but growing understanding of the risks (including loss of privacy) and benefits of sharing their health data and express a range of views about sharing health information. For example, a 2019 focus group on consumers’ perception of interoperability found that “participants overwhelmingly supported greater access to data both for health care providers and for themselves” ( The Pew Charitable Trusts, 2020 ).
In the intervening decades since the enactment of the Health Insurance Portability and Accountability Act of 1996 (HIPAA), health data systems have grown exponentially. A new industry of health-related applications was launched, giving individuals the ability to readily share their most private data with a variety of health sector and commercial actors. Some apps serve as a core communication device between individuals and their physicians and sit squarely within HIPAA. In contrast, other tools and vendors are unregulated by HIPAA, creating uneven protection and confusion for consumers. The expansion of HIPAA to redefine and protect health information outside of covered entities could mitigate risks to individuals.
Another critical area requiring progress in support of digitally facilitated health is accurately matching individuals across systems ( The Pew Charitable Trusts, 2018 ). A unique national patient identifier was envisioned as a foundational element of HIPAA, but privacy and security concerns prevented the enactment of necessary regulatory action. Promulgating such regulations remains a valuable aim to support efficient, accurate matching. In 2021, the ONC advanced efforts to accurately match patient data across systems with Project US@, which was established “to develop a unified, cross-standards, health care industry-wide specification for representing patient addresses to improve patient matching” ( HHS, 2021 ). Correctly matching an individual’s data across organizations (with sufficient gold standard matches that allow for appropriate algorithm development) remains an essential component for the learning health system to support the right care for the right person today and to support the use of AI and research to ensure the best outcomes for tomorrow.
Cybersecurity
Cybersecurity and privacy concerns are major obstacles to digital health adoption, continue to erode patient trust, and reinforce health systems’ reluctance to share data. Psychological resistance, the risk of ubiquity of data, consequences of a breach, and patchwork of local and national privacy protections—or lack thereof—have created barriers to the use of pioneering, forward-looking digital health tools, and as such, cybersecurity must not be an afterthought.
These critical challenges require technologic, governance, and legal protocols. A public-private partnership is necessary to develop a superstructure framework to ensure the safety, security, and privacy of digital health architecture. As noted earlier, the cybersecurity framework produced by the National Institute of Standards and Technology (NIST) provides such guidance ( NIST, 2018 ). Transparency and consent for consumers and patients regarding data sharing, agency, and privacy within and across platforms and stakeholders—including those not covered by HIPAA—must be simplified and standardized, including understandable consent forms and the extension of HIPAA protections to currently noncovered entities like third-party app vendors. In addition, privacy and security risks with big data and AI require special attention to avoid intentional corruption of AI/ML training datasets (training data poisoning), use of AI by attackers, or anti-privacy designs in digital health ( Hartzog, 2018 ).
Data Quality and Reliability, Storage, and Stewardship
Foundational to digital health, the standards and curation protocols for data and information (e.g., Findability, Accessibility, Interoperability, and Reusability [FAIR] principles), while best-practice, are not required by regulation. However, such standards and protocols are required to achieve uniform value between and among stakeholders. Data standards and stewardship guidelines and national cooperation are critical, while simultaneous attention must be paid to “economic, legal, philosophical, and practical issues” relating to health data ( NASEM, 2020 ). In principle, the individual, the source of health data, controls access to and use of the data derived from their health care and interaction with digital platforms. In practice, the organization collecting and managing the data has differing custody and control of the data, depending on the nature of the individual’s data and regulations to which the data’s collector and custodian is subjected. Differences among organizations concerning “data access, control, and monetization” limit the potential of digital health, and expanding structures for cooperation and exchange are essential ( NASEM, 2020 ).
The availability of patient portals in most EHR systems and consumer-facing digital health tools and the data associated with these applications represent a meaningful opportunity to improve patient care. However, significant challenges, including the digital divide, issues of systemic racism, data curation, integration into the care setting, and data sharing for research, impede progress toward realizing improved patient care.
Further, the strong drive to innovate and rapidly market mHealth tools has led to product development outpacing the capacity of regulators to establish standards and communicate clear guidance to various stakeholders, including consumers and payers. These unclear standards and lack of regulatory guidance and oversight have created a marketplace where promising digital health solutions that provide superior quality, impact, and value are difficult to distinguish from poor quality innovations and work to the disadvantage of rigorously studied digital health products. For example, emerging scientific evidence indicates that some RPM devices can predict five-year mortality in adults between 50 and 85 years and empower patients to better manage their health and participate in health care ( Halamka and Cerrato, 2020 ). Clear standards and widespread rigorous review of innovations, including the evaluation of technical design, clinical value, and usability, could increase confidence in and meaningful adoption of new consumer-facing digital health tools.
Finally, decisions will need to be made about how data are stored in cloud-based systems to advance the common good. Virtual data repositories must be structured and controlled to protect the integrity and privacy of the data through all aspects of data management - acquisition, storage, access, maintenance and release. ( NASEM, 2020 ) Simultaneously, computing power should migrate to the cloud to support this future vision, as the cloud has both sophisticated security and economies of scale. Cloud-based computing will require a paradigm shift for organizations with on-premises systems.
Interoperability
Through the work of ONC, data and interoperability standards have grown increasingly sophisticated over the past decade. While more work is needed, early progress with HIEs, APIs, and EHR integration has yielded improvements in care coordination, and recent efforts during the COVID-19 pandemic demonstrated the capacity of HIEs to deliver value by generating public health reporting ( Dixon et al., 2021 ).
In addition, interoperability standards need to extend beyond the current focus on EHRs. Existing interoperability of health care data systems neither adequately supports optimal longitudinal care delivery nor advances the nation’s health needs. The COVID-19 pandemic illuminated the needs and opportunities for digital health and transformative preparedness and response capacity. The rapid pace of the pandemic’s spread emphasized the need for a rapid learning system that relies on capturing, organizing, sharing, and analyzing large amounts of data digitally across public health, research, and clinical systems. An effective response to public health crises is highly dependent on interoperable data, without which there is an inability to understand what is needed in terms of resources and capacity and to understand the impact of interventions. While data was critical for forecasting and coordination, its collection, sharing, and aggregation were, at times, chaotic and burdensome for clinicians and administrators.
The post-COVID-19 era can help ensure the interoperability of all mediums of digital recordkeeping used to support health and deliver health care services, including labs, certified EHRs, home-grown EHRs, digital devices, consumer electronics with health features, and databases to support research and public health. Before the pandemic, the Centers for Disease Control and Prevention (CDC) had launched a data modernization initiative to undergird disease surveillance systems. The Coronavirus Aid, Relief, and Economic Security (CARES) Act allocated $500 million to the CDC to implement a “modern, interoperable, and real-time public health data and surveillance systems that will protect the American public” ( CDC, 2020 ).
Artificial Intelligence and Machine Learning
As the U.S. moves to value-based payment models, transparent and advanced analytics are needed to calculate population risk, the foundation upon which medical budgets are established in contracts between payers and providers. AI-driven predictive modeling and other sophisticated statistical techniques can be used to identify subpopulations for intense care management to prevent inappropriate emergency room use or early intervention for an acute worsening event to reduce hospital admissions. For example, in the inpatient environment, AI has been used to identify patients at risk of decompensation using data collected in the background during clinical care ( Lin et al., 2019 ). A recent literature review of AI algorithms for sepsis models found the models to be highly predictive but noted several issues with algorithmic standards ( Deng et al., 2021 ). As digital health tools incorporate increasingly disparate data into predictive models using various AI techniques, standard outcome and data definitions, bias in training datasets and final models, and frequently updated algorithms must be considered. Harnessing AI will depend on coherent data architecture and diverse training datasets, which are large, sampled adequately, and represent subgroups adequately (e.g., by gender, race, age, socioeconomic status). The Food and Drug Administration (FDA) has released guiding principles for “Good Machine Learning Practice for Medical Device Development,” which are practical and should be considered when embarking upon model development ( FDA, n.d. ). The regulatory framework for AI as a medical device is nascent and must address certification of constantly changing algorithms and maintenance of accountability of vendors to ensure reliable and valid processes. There are alternative ways to regulate AI, including principles and standards developed by multi-stakeholder collaboration that can create adaptable standards and guidelines. Components of the European Union’s proposed rules governing AI might be considered in the U.S. ( EC, 2021 ). Additional standards to consider include the International Medical Device Regulators Forum “Software as a Medical Device (SaMD): Application of Quality Management System,” FDA Center for Devices and Radiological Health “Software as a Medical Device (SaMD): Clinical Evaluation Guidance for Industry,” and “Artificial Intelligence/Machine Learning (AI/ML)Based Software as a Medical Device (SaMD) Action Plan” ( IMDRF, 2015 ; IMDRF, 2017 ; FDA, 2021 ). These strategies could work in tandem with regulations updated for rapidly changing capacities.
To support digitally enabled health in a learning health system, the workforce of the future will require a comprehensive set of skills that are currently rarely seen. Besides basic competency on core organizational applications (e.g., EHR functionality), clinicians, health system staff and management, and vendors/innovators will all require at least basic or conceptual knowledge of data management (collection, storing, normalizing), interoperability, basic statistics and data science, data governance and collaboration, ethics, process improvement, and implementation science. Finally, diversity training is critical to all engaged in supporting digitally facilitated health in the learning health system and must mitigate disparities and build awareness among all parties—especially those individuals producing AI algorithms—to the consequences of bias for vulnerable populations.
The technical workforce of the future will also need expertise in user-centered design, which seeks to involve end users throughout the product development life cycle. The earliest digital health care applications did not incorporate these principles, and as such, use cases were limited to the automation of paper processes rather than the reimagination of care delivery and payment. This issue remains a problem today, as evidenced by burnout and frustration among providers using EHRs ( Melnick et al., 2020 ). In seeking to achieve better health, better care quality, lower costs, and greater satisfaction among individuals and providers, user-centered design will be an essential ingredient of any infrastructure strategy. Particular attention to culturally appropriate design and addressing the needs of historically underrepresented populations has shown early positive effects when delivering interventions to populations in need and is another critical issue when ensuring that unintentional bias does not further the digital divide ( Schueller et al., 2019 ).
Stewarding Digital Innovation for Our Health Futures
To achieve the full potential of digital health, the health care industry and governmental leaders must collaborate, cooperate, and develop shared governance, creating a unified digital health system architecture from independently functioning infrastructure building blocks.
Key priorities must be identified and pursued within both the environmental and the technical contexts to achieve the full potential of digital health. The key priorities in the environmental context include focusing on the individual, embedding equity and transparency as first principles, reforming health system payments in support of outcomes and value, and nurturing a learning health system ethos. From the technical perspective, the priorities include establishing seamless system interoperability, ensuring cybersecurity, and expanding algorithm validation and real-world testing.
Focusing on the Individual
Fully engaging individuals in their health and well-being through digital health, responding to public demand for participation in the growing digital health ecosystem, and balancing demand for consistent, transparent protections for health data within and outside of the health care system is a priority in achieving a fully realized future for digital health. Health data are intensely personal, and unintentional or nefarious exposure of that data has the potential to upend an individual’s life. Capturing the full potential of digital health will require broad confidence in health systems and commercial ventures to protect the individual from negative outcomes.
Transparent stewardship standards are needed to ensure individual agency in using their data. A critical first step in building trust in health data governance is a public dialogue about digital health—bringing together stakeholders into the policy process to address individual rights regarding data sharing, issues of consent, transparency, secondary uses of data, common patient identifiers, consideration of health data as a public good, and regulation of AI/ML. These dialogues will build comfort levels and demands for expanded applications while also maintaining safeguards against abuse and unintended consequences.
Central to the critical priorities for fully actualized digital health is the need to promote a sector-wide culture of transparency and truthfulness without fear of retribution. Similar to how To Err Is Human called upon the health care industry to acknowledge where their practices were worsening health, a critical next step in advancing digital health is to take definitive action to ensure that people feel comfortable reporting errors without fear of punitive actions ( Shrank et al., 2019 ).
Beyond individual agency over health data, engaging consumers in their own health and health care via digital platforms will require both systems developers and health system leaders to include the customer’s voice in the development, execution and evaluation of digital health tools and platforms. A model for patient and family engagement in digital health initiatives is in development in Canada and could serve as a starting point for advancing a model in the U.S. ( Shen et al., 2021 ).
Embedding Equity and Transparency as First Principles
The rapid development and application of digital health is also accompanied by the need for vigilance on equity and equality issues that include availability and access to the benefits of digital health, racial bias in AI, and misuse of personal information in discriminatory practices. For digital health to improve health and well-being, a data-centric and patient-centric approach to developing and deploying these tools is essential, and data must reflect the diverse communities and populations across the U.S. Here again, the health system, researchers, and commercial ventures must address issues of mistrust with transparent, accountable, and unbiased protections so that the benefits of digital health are shared equally across society.
Reforming Health System Payments in Support of Outcomes and Value
COVID-19 has provided a further reminder of the systemic shortcomings of fee-for-service reimbursement, renewing the impetus for restructuring health care financing in America. Given the tremendous uptake of platforms such as telehealth and RPM during the COVID-19 pandemic, forthcoming payment reforms must account for the role of digital health writ large in driving delivery system transformation. Policy makers will also need to address concerns that extending digital technologies will increase costs and the risk of fraud and abuse or otherwise negatively impact quality or provider-patient engagement.
Furthermore, the infrastructure improvements required to advance the digital functions of a learning health system (e.g., population health management, data and analytics for risk stratification) are often unfunded activities that would benefit from additional incentives and investments such as those that accompanied HITECH.
The financial benefits of payer and provider organizations must align with the health benefits of digital tools. This alignment will require data sharing from industry, evaluations from academia and regulators, and collaboration across sectors to develop progressive payment structures across payers that allow flexibility for innovation. The path forward for value-based payment will therefore require a renewed commitment to building trust and collaboration and aligning incentives to balance the drive to innovate with stewardship of cost, quality, outcomes, and safety.
Nurturing a Learning Health System Ethos
The vision of digitally facilitated health depends on a continuously learning health system and a dramatically shortened interval between evidence generation, deployment to the field, and incorporation into standard practice. There is also a need to use real-world data (from wearables to ambulatory care to robotics) to generate real-world evidence that complements the results of randomized controlled trials, which often suffer from limited racial or socioeconomic diversity in patient recruitment. Rapid cycle learning must also be employed, as it will enable the necessary organizational agility to respond to an accelerated rate and nature of change that has become the norm.
Digital health tools must be well integrated into the health care delivery system to enable the continuously learning health system. With expanded data assets and improved interoperability, the delivery system has an opportunity to reimagine and recreate a care system that is culturally attuned, personalized, holistic, and comprehensive—one unlike our current system, which consists of specialty, sector, and system silos. New care models can be developed with an understanding of disease and digital phenotypes and envirotypes that will each have different treatment responses. Advanced analytics are needed to create cohorts of similar patients for more effective population health management to address the high prevalence of chronic disease and create a feedback loop regarding outcomes and evidence-based treatment in the care delivery system.
Establishing Seamless System Interoperability
Seamless connectivity and communication among health care-related devices are essential prerequisites for promoting optimal health. Incompatible interfaces, corrupted data written between systems, or mismatched patient data have the potential to have dire consequences, requiring collective action to ensure adherence to standards to protect data integrity. Technological advancement and national policies have made possible the vision for a digital infrastructure that can facilitate seamless interfaces and real-time interoperability of devices and data streams. Released in March 2020, the Cures Act final rules set forth penalties for information blocking and expanded the access of individuals to their health records by leveraging the FHIR specifications. Such standards allow information to be shared and processed consistently. In addition, there are several industry-led initiatives, such as the Integrating Healthcare Enterprise, Argonaut Project, and others, aimed at promoting seamless data exchange ( IHE International, 2021 ; USF Morsani College of Medicine, 2021 ). As a promising indicator, many health systems have aligned organizational priorities toward interoperability objectives.
Nonetheless, a great deal of work remains to achieve full system interoperability, as semantic interoperability is limited. Progress is uneven across the industry, with some health systems being pioneers in real-time data sharing while others are lagging. Moreover, interoperability continues to be stunted by the systemic misalignment of incentives, competitive forces, and lack of coordination.
Ensuring Cybersecurity
The rapidly evolving landscape of cyberattacks highlights the urgent need for collaboration across the government, health organizations, and consumer-facing vendors to develop consensus on security protocols and upgrade security infrastructure. Existing approaches such as multi-factor authentication, intrusion detection monitoring, etc., must be employed as we explore more advanced strategies, such as adopting blockchain technologies to share immutable records of transactions among network participants. Places to start could be expansion of HIPAA, national application of the California Consumer Protection Act, and a comprehensive privacy regime similar to the European Union’s General Data Protection Regulation to protect all types of data deemed essential for health improvement.
Expanding Algorithm Validation and Real-World Testing
There is a clear need to invest in the capacity and cooperation necessary to advance data science and AI. AI/ML and deep learning that apply transparent algorithms and decision rule architecture to large, diverse databases present the opportunity to develop increasingly precise insights for individuals and populations. Critical issues include explicit and implicit bias in the development and application of modeling, visualization, explainability, validity, and regulation ( The Lancet Digital Health, 2019 ; Buolamwini and Gebru, 2018 ). A regulatory framework must address certification of constantly changing algorithms and must hold vendors accountable for valid and reliable processes and must include codes of conduct and the development of “data science tools, …pathways, agreements, and protocols for establishing curated virtual health data trusts” ( NASEM, 2020 ). The FDA’s AI/ML-based Software as a Medical Device (SaMD) Action Plan proposes such a framework and shares valuable stakeholder feedback ( FDA, 2021 ).
The capacity to advance data science and AI is dependent on a highly skilled digital health workforce, and “the training challenge for leveraging digital health is vast—in health care, public health, and biomedical science” ( NASEM, 2020 ). In addition, as AI/ML is applied to CDS tools, it is essential to address unintended bias in algorithm creation.
Tools designed for the clinical system and providers can be evaluated on their impacts on health outcomes and costs, as well as their impact on both patient and provider satisfaction. Real-world testing across unique health systems is required to understand impacts on usability, clinical workflow, provider burden, and staff time requirements that benefit providers and patients. While time consuming, these pilots are useful and must be tied to scaling opportunities if successful. When relevant, testing of devices and AI-supported CDS must achieve FDA clearance.
While the availability of digital health tools and associated data sharing has better positioned America to face CO-VID-19 and harness opportunities for long-term preparedness and system resiliency, limitations such as the ability to aggregate data have emerged. The full potential benefits of these tools has not been realized, and the adoption and application of digital health remains uneven and subject to significant structural, technical, social, geographic, political, and economic impediments, limiting the nation’s ability to be as nimble as needed in such crisis.
Priority Near-Term Actions
The progress of digital technologies writ large is undisputed and can be observed in the millions of enthusiastic viewers who use streaming video services; the countless customers who shop online; and the growing number of consumers, patients, and clinicians who are embracing mobile health apps, AI-enabled diagnostic aids, and many other CDS tools. However, while the predictive analytics used to suggest a person’s next favorite movie may be similar to the analytics used to suggest a medical diagnosis or treatment option, one key difference remains: when a streaming service recommends a new movie, viewers may find it helpful, annoying, or even amusing—not life threatening. When algorithms are used to assist in the diagnosis of diabetic retinopathy or the recommendation of a therapeutic approach to sepsis, the stakes are much higher ( Lin et al., 2019 ). To fully realize the goal of health and well-being for every individual, these concerns must be considered as all stakeholders in the health care ecosystem make intense and sustained efforts to improve the capabilities of the health care delivery system, impact SDoH, ensure equal benefit from digital health, and establish an overarching architecture and governance framework that engages the public.
ONC has made significant inroads toward an overarching digital health blueprint for fully enabling digital health. Augmented by broader authority, continued progress on interagency collaboration, and robust public-private partnerships, this progress will ensure a digital health superstructure that:
- ensures equitable and ethical use of data;
- supports the collection, storage, protection, and seamless sharing of accurate datasets and generated insights in near-real time;
- ensures the curation of that data into actionable intelligence; and
- enables transformative advances in medical care and patient safety based on the actionable intelligence generated.
Below is a sampling of specific, actionable items for consideration within this national blueprint, with specific reference to the key priorities identified above.
- A multi-stakeholder panel should be convened to develop recommendations to meaningfully engage the diverse individual consumers of health care in all health care sectors. This panel should follow the adage “nothing about me without me” to ensure the priorities of focusing on the individual and embedding equity and transparency as a first principle.
- A multi-stakeholder panel should be convened to establish use cases and support the development of guidelines for applications laboratories to advance the learning health system ethos and expand algorithm validation and real-world testing.
- Congress should promulgate rational, right-sized, risk-based regulation, standards, and frameworks to enable the seamless flow of data while protecting privacy and ensuring transparency and accountability to advance system interoperability and cybersecurity, as well as focusing on the individual and expanding ethical and effective algorithm development, validation and real-world testing.
- ONC should develop and implement a governance infrastructure and policy framework regarding data, virtual health data trusts, privacy, and regulations to advance focus on the individual, seamless system interoperability, and cybersecurity, working collaboratively with industry to ensure broad coverage of these principles.
- CMS should lead the effort to ensure sustainable payment coverage to ensure equal access to digital health tools for all individuals and providers, regardless of private versus public payer source. In addition, CMS should significantly accelerate the move to value-based payments to support outcomes, innovation, and aligned incentives.
- ONC should ensure the timely, full implementation of standards of structure, coding, security, and common APIs, as these standards are foundational for most progress on digital health.
Envisioning and achieving a seamless, healthier future through digital innovation will require a deeper investment in evidence-based research, more clinical and field studies, and commitment from diverse stakeholders. But the potential for rewards is enormous. Validated information, curated across the health data continuum and easily shared, can deliver insight at the point of care, easing provider burden and augmenting clinical reasoning skills. An “Internet of Things” in health care serves the public’s need for accurate health advice, and a digital health ecosystem that provides high-quality, personalized, equitable care to all who need it is achievable and worthy of our best individual and collective efforts.
Acknowledgments
This paper benefited from the thoughtful input of John Glaser, Siemens Healthcare; Clement McDonald, National Library of Medicine; and Marc Overhage, Anthem.
The authors would like to recognize Paul Cerrato with the Mayo Clinic for contributing to earlier drafts of this publication and to thank Mahnoor Ahmed and Asia Williams with the National Academy of Medicine Leadership Consortium for assistance with research and fact-checking.
Funding Statement
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies.
Conflict-of-Interest Disclosures: Amy Abernethy discloses employment by Verily, an Alphabet Company; employment by the U.S. FDA while this paper was being drafted; and serving as member of the Board of Directors or EQRx. Laura Adams discloses employment as Senior Advisor to the National Academy of Medicine. Meredith Barrett discloses receiving personal fees from ResMed and Propeller Health. Atul Butte discloses receiving grants and non-financial support from Progenity; personal fees and other support from NuMedii, Personalis, Assay Depot, GNS Healthcare, uBiome, and Nuna Health; grants and personal fees from NIH and Genentech; grants from L’Oreal and Samsung; personal fees and non-financial support from Merck, Lilly, Geisinger Health, and Roche; and serving as consultant to Wilson Sonsini Goorich & Rosati, Orrick Herrington & Sutcliffe, Verinata, 10x Genomics, Pathway Genomics, Guardant Health, and Gerson Lehrman Group. Elaine Fontaine discloses employment as a consultant to the National Academy of Medicine. Stephen Friedhoff discloses employment by Anthem BC while this paper was being drafted; current employment by BCNC; serving as board member to Agape Care and Medical Review Institute of America; and advisor to Rialtic. Michael Howell discloses employment and equity in Google, an Alphabet company. Kevin Johnson discloses employment by University of Pennsylvania. Peter Lee discloses employment by Microsoft. Deven McGraw discloses employment by Invitae Corporation and Ciitizen Corporation; personal fees from Datavant and All of Us Research Program; and serving as board member for CARIN Alliance and Manifest Medex. Redonda Miller discloses employment by the Johns Hopkins University. Jonathan Perlin discloses former employment by HCA Healthcare. Donald Rucker discloses former employment by the National Coordinator for Health IT; current employment by 1up Health; and personal fees from Cync Health. Paul Tang discloses employment by IBM Watson Health. Eric Topol discloses receiving personal fees from Illumnia and serving on the board of directors at Dexcom. Kristen Valdes discloses employment by b.well Connected Health.
Contributor Information
Amy Abernethy, Verily.
Laura Adams, National Academy of Medicine.
Meredith Barrett, ResMed.
Christine Bechtel, X4 Health.
Patricia Brennan, National Library of Medicine.
Atul Butte, San Francisco.
Judith Faulkner, Epic Systems.
Elaine Fontaine, National Academy of Medicine.
Stephen Friedhoff, Inc.
John Halamka, Mayo Clinic.
Michael Howell, Google Health.
Kevin Johnson, University of Pennsylvania.
Peter Long, Blue Shield of California.
Deven McGraw, Ciitizen Corporation.
Redonda Miller, Johns Hopkins Hospital.
Peter Lee, Microsoft Corporation.
Jonathan Perlin, The Joint Commission.
Donald Rucker, 1upHealth.
Lew Sandy, UnitedHealth Group.
Lucia Savage, Inc.
Lisa Stump, Yale New Haven Health System and Yale School of Medicine.
Paul Tang, Stanford University.
Eric Topol, The Scripps Research Institute.
Reed Tuckson, LLC.
Kristen Valdes, b.well Connected Health.
Amsterdam Public Health

Digital Health
Digital Health strives to contribute to public health and the clinical healthcare domain by improving the overall health and health equity of all on the macro, meso and micro level. The research program intends to support citizens, patients and patients’ relatives as well as those caring for them. It focuses on how to provide better and more efficient prevention, care and cure; in a way that not only health and well-being, but also autonomy and self-efficacy of patients may be enhanced. Research topics include research on e-health systems and solutions focusing on providing better (preventive) care and cure tailored to person and patient; on provider and situation using digital tools and technology; on (Findable, Accessible, Interoperable, Reusable – FAIR) data science; on better use of tools such as those exploiting artificial intelligence (AI), virtual and augmented reality, simulation and applied mobile health.
Program support: Nina Zipfel Contact: [email protected]
We aim to contribute to prevent disease from happening and support those in current need of healthcare by fostering and governing research on development, evaluation and implementation of digital tools and by smart, fair and ethical use of data bringing equity for all. And by doing so, supporting current and future citizens, patients, providers and healthcare systems.
Mission and goals
The APH research program Digital Health catalyzes research in digital health and the implementation of successful findings and instruments in the public health and healthcare domain; aiming to improve health, provision of healthcare and health equity for all.
The goal of the research program is to bring together research from Amsterdam UMC and VU and UvA research partners in the affiliated research programs and institutes; to collaborate with industry, strategic partners and public initiatives focusing on – but not limiting to - the Amsterdam region; shaping the digital landscape in healthcare from both a somatic and mental health perspective. This, to examine, align and safeguard initiatives, in order to propel them and the people fostering them further. This encompasses not only initiatives within APH or the Amsterdam region, as Digital Health is a research program much about crossing regional and scientific/(multi-)disciplinary boundaries. Hence, the research program aims to align with and strengthen relevant initiatives and partnerships in the Netherlands and internationally. The scope embraces research themes in the area of e-health, digital health, (FAIR) data science, AI, virtual and augmented reality, simulation and applied mobile and blended health and care. Our mission is to position the research program, residing under APH, to help achieve the aforementioned goals. Furthermore, our mission is to raise public and scientific awareness on the theme, and build a strong community for further research developments, collaborations and partnerships.
The Digital Health research program is an overarching research program fostering, embedding and bringing together research initiatives – from fundamental to implementation science and participatory action research, from public and preventive to clinical medicine including psychiatry, in the domain of digital health for Amsterdam UMC, affiliated research programs and research institutes . Digital Health aims to contribute to smart, fair and ethical use of data and digital tools to improve both personal and societal health and wellbeing of citizens. This is key not only to futureproof healthcare in terms of access, quality and costs but also to establish a learning, connected healthcare system. Professional and public awareness is on the rise, as is the need for solid evidence on the proposed benefits and risks of 'digital health'. The body of evidence showing the importance of digital health towards health made it become an essential part of the Amsterdam UMC strategy. The movement towards a more personalized health care provision supported by digitalization is reinforced by the implementation program ‘Samen Digitaal’ of Amsterdam UMC. APH has included digitalization as one of their strategic themes, to contribute to overcoming current challenges. Use of digital health strategies may, if well researched and implemented, support the citizen, the patients and their relatives. Also, it may help healthcare professionals to provide better and more efficient care and help healthcare systems to connect with one another and to be sustainable. Impact assessment of digital interventions will be an important topic, to enable early detection of any unintended effects.
The Digital Health research program is rooted in APH and led by a 2-headed Program Leadership. The Leadership is supported by (and part of) the Program Council, with senior board members representing relevant research domains. The Program Council and senior board closely collaborate with the Junior Council and the APH support staff. The research program brings together a community of researchers to collaborate, share, and learn, in order to increase knowledge and skills to improve health and wellbeing of citizens. To this end, we intend to establish a supportive network for the participants, and to provide and support various collaboration opportunities both program-wide and in topical working groups.
Program leaders

Research themes
This overarching theme is dedicated to advance research on e-health, digital tools, platforms, structures and instruments to support, citizens, patients, their significant others and healthcare professionals. Applications of information and communication technology are developed, tested, implemented, and evaluated to be scaled-up both in healthcare and preventive medicine.
Data science
In this theme the capture, processing, and fair application of data, the legal, ethical, societal and scientific insights to support this, and semantic and mathematic algorithms to discover new knowledge from data are researched to advance healthcare provision. This includes research into approaches, methods, and techniques to establish FAIR data and services.
Utilizing Artificial intelligence (AI)
Within this theme, research will contribute to the study of artificial intelligence (and its subsets machine learning, deep learning, and knowledge representation) in healthcare. Research covers advancing and modernizing patient and healthcare professional experiences through the design and application of AI-based tools to optimally utilize medical data and to perform prediction while considering the key aspects of trust and explainability.
Virtual- and augmented reality
This theme concerns research on the use of virtual, mixed and augmented reality within healthcare to support patients and/or healthcare professionals in the clinical and preventive domain. Also, developments in the Metaverse, relating to clinical and educational context of health and healthcare are part of this theme.
In this theme the wide range of activities that may contribute to the improvement of safety, effectiveness and efficiency of healthcare provision and training of healthcare professionals individually and / or in teams will be researched.
Mobile health
This theme concerns research on a the use of a wide range of mobile and wireless devices, and technologies that can be connected using e.g., WiFi , Bluetooth or 4/5G networks in healthcare including Ecological Momentary Assessment strategies.
Program council
The Program Leaders of the Digital Health research program chair the Program Council. This Program Council consists of a selection of renowned senior researchers, being professor or PI with own research lines active in the digital health domain. The Program Council meets -at least twice a year - to help implement or update the research program-specific strategy, to foster and help build the program and its initiatives and to discuss anticipatory or reactive response to external events.
| Program council members | |
|---|---|
| Dr. Christine Dedding | Prof. Henk Marquering |
| Prof. dr. Michèle van Vugt | Prof. dr. Heleen Riper |
| Prof. dr. Mark Hoogendoorn | Dr. Paul Elbers |
Junior council
The Digital Health research program has installed a Junior Council. Ambitious post-docs and PhD-candidates foreseeing a future in digital health provide the Program Leaders and Program Council with solicited and unsolicited advice, may initiate independent activities under the umbrella of Digital Health after consultation of and in good collaboration with Program Leaders to form a strong network; and help in organizing research program-specific activities and events.
| Junior council members | |
|---|---|
| Boris Janssen | David Neal |
| Marketa Ciharova | Thomas Engelsma |
| Franciscus Bennis | Ruben Boyd |
| Yvonne Blokland | Susan Oudbier |

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Open access
- Published: 29 June 2024
Recommendations to advance digital health equity: a systematic review of qualitative studies
- Sarah Wilson ORCID: orcid.org/0000-0001-7803-3978 1 ,
- Clare Tolley 1 ,
- Ríona Mc Ardle 2 ,
- Lauren Lawson ORCID: orcid.org/0000-0003-0433-5214 1 ,
- Emily Beswick 3 ,
- Nehal Hassan ORCID: orcid.org/0000-0002-8302-5769 1 ,
- Robert Slight 4 &
- Sarah Slight 1 , 4
npj Digital Medicine volume 7 , Article number: 173 ( 2024 ) Cite this article
78 Accesses
9 Altmetric
Metrics details
- Public health
- Social sciences
The World Health Organisation advocates Digital Health Technologies (DHTs) for advancing population health, yet concerns about inequitable outcomes persist. Differences in access and use of DHTs across different demographic groups can contribute to inequities. Academics and policy makers have acknowledged this issue and called for inclusive digital health strategies. This systematic review synthesizes literature on these strategies and assesses facilitators and barriers to their implementation. We searched four large databases for qualitative studies using terms relevant to digital technology, health inequities, and socio-demographic factors associated with digital exclusion summarised by the CLEARS framework (Culture, Limiting conditions, Education, Age, Residence, Socioeconomic status). Following the PRISMA guidelines, 10,401 articles were screened independently by two reviewers, with ten articles meeting our inclusion criteria. Strategies were grouped into either outreach programmes or co-design approaches. Narrative synthesis of these strategies highlighted three key themes: firstly, using user-friendly designs, which included software and website interfaces that were easy to navigate and compatible with existing devices, culturally appropriate content, and engaging features. Secondly, providing supportive infrastructure to users, which included devices, free connectivity, and non-digital options to help access healthcare. Thirdly, providing educational support from family, friends, or professionals to help individuals develop their digital literacy skills to support the use of DHTs. Recommendations for advancing digital health equity include adopting a collaborative working approach to meet users’ needs, and using effective advertising to raise awareness of the available support. Further research is needed to assess the feasibility and impact of these recommendations in practice.
Similar content being viewed by others
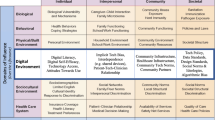
A framework for digital health equity

Barriers and facilitators to utilizing digital health technologies by healthcare professionals
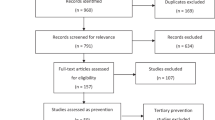
Preventive digital mental health interventions for children and young people: a review of the design and reporting of research
Introduction.
The World Health Organisation (WHO) advocates Digital Health Technologies (DHTs) to advance population health 1 . Digital health can be defined as the use of information and communication technologies within healthcare to provide healthcare users with services relating to the prevention, detection, diagnosis and management of diseases and other health conditions 2 , 3 , 4 . Examples of DHTs include smartphone applications and wearable monitoring devices that can empower people to better manage their own conditions, such as keeping track of symptoms or remotely monitoring their condition(s) over time 2 , 3 , 4 . DHTs can pick up signs of deterioration in healthcare users’ symptoms longitudinally and provide real-time data to healthcare professionals to help support tailored clinical decision making 4 . DHTs can also enable individuals with mobility issues and those living in rural areas to access healthcare. Digital health has gained global momentum due to its potential to contribute to personalised health care for patients, improved quality of care, and lower healthcare costs 5 , 6 .
However, there are growing concerns that DHTs may not lead to health benefits in all populations, with underserved groups (i.e., those typically left out of research or experience inadequate access to healthcare) at particular risk 7 . One possible factor contributing to this is digital exclusion, denoting disparities in motivation, access and use of DHTs across different demographic groups 8 . Digital exclusion can potentially create a barrier for various underserved groups, such as those who are on a low income, are not fluent in English, or homeless, thus exacerbating health inequities for these groups 9 . Individuals with visual impairment may also find on-screen reading challenging and many older adults with hearing impairments have expressed low motivation to use phone calls as a remote option to access healthcare due to their disability 10 .
Technology has advanced rapidly over recent years, with some DHTs (e.g., telehealth services, mobile phones, wearable devices, smartphone apps and other software) having greater relevance to the direct inequities underserved groups face compared to other DHTs. For example, DHTs designed to be solely used by healthcare professionals (e.g., electronic patient records) are less likely to directly impact healthcare service users, and so it is prudent to focus on DHTs that underserved groups may be asked to use. Qualitative studies gathering rich in-depth experiences from those whose voices are rarely heard (i.e., underserved groups) 11 , 12 will provide valuable insights into the facilitators and barriers regarding access, motivated and/or use of DHTs.
The WHO Bellagio eHealth Evaluation Group (2019) recognised the need to mitigate digital exclusion 13 , with organisations such as NICE (National Institute for Health and Care Excellence) requiring evidence that health inequities have been considered in the design of DHTs 2 . This includes important aspects of design, development or implementation of a DHT that support digital inclusivity, such as strategies to increase an individual’s access to suitable devices or connectivity, and educational support in digital literacy to increase DHT use 14 . To support the development of such strategies, it is vital to understand the needs of underserved groups as well as their experiences and perspectives of these strategies to identify what does and does not support digital inclusivity. However, there is currently no qualitative systematic review of key strategies conducted in this area; a key knowledge gap in the literature. To advance digital health equity, we aimed to systematically synthesise the literature on what key strategies have been used to promote digital inclusivity, and assess the facilitators and barriers to implementing and adopting these in practice based on underserved groups’ experiences and perspectives.
Study descriptions
Our search yielded 13,216 results. After removing duplicates ( n = 2815), titles ( n = 10,401) abstracts ( n = 1224) and full-texts ( n = 143) were screened. Ten papers met our inclusion criteria (Fig. 1 ). Inter-reviewer reliability was high with 99.33% agreement at title stage, 99.43% at abstract stage, and 97.89% at full-text stage. All included studies were found to have moderate- to high-quality levels (Supplementary Tables 7 and 8 ). None of the included studies measured or reported any participants’ health literacy.

A PRIMSA flow chart detailing our search and selection process applied during the article screening process.
Included studies incorporated a range of participants at risk of digital exclusion, including those from different cultural backgrounds (ethnic diversity, languages and religion) ( n = 8) 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , those with limiting conditions (visual and hearing impairments) ( n = 2) 21 , 22 , low educational attainment ( n = 4) 15 , 19 , 20 , 21 , aged over 65 ( n = 4) 16 , 20 , 21 , 22 , homeless ( n = 2) 19 , 24 , and those who had low socioeconomic status ( n = 5) 15 , 16 , 17 , 18 , 21 (Supplementary Table 9 ). All 10 studies used interviews 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , with two studies also conducting focus groups with participants 18 , 21 . (Supplementary Table 10 ). Inclusive digital health strategies were grouped into either outreach programmes providing educational support and/or access to devices ( n = 2) 19 , 22 , or co-designing DHTs with underserved groups ( n = 8) to gain feedback on the usability and acceptability of DHT to enhance inclusivity in future versions of the DHT (Table 1 ) 15 , 16 , 17 , 18 , 20 , 21 , 23 , 24 .
Our narrative thematic synthesis generated three overarching themes; user-friendly designs (e.g., software and website design elements that promoted inclusivity), infrastructure (e.g., access to DHTs) and educational support (e.g., training to develop digital literacy skills required to use DHTs) (Supplementary Table 10 ). Facilitators and barriers to the adoption of these themes are embedded in the discussion below and summarised in Fig. 2 .
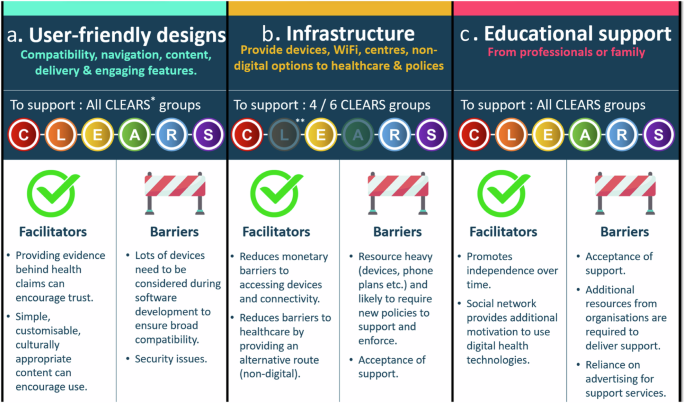
Summary of the key facilitators and barriers to strategies to support digital health equity (using a user-friendly design, providing infrastructure and providing educational support) alongside the specific CLEARS groups the strategy will support.
User-friendly designs
User-friendly designs were a key theme supporting access and use of DHTs across seven studies 15 , 16 , 20 , 21 , 22 , 24 . Health-related software and websites needed to be compatible across different digital platforms, operating systems and devices including smartphones and desktops, and assistive technologies (e.g., screen reading software) to accommodate the needs of ethnically and linguistically diverse groups 17 , 18 , 22 , individuals with limiting conditions (visual and hearing impairments) 20 , 21 , older adults (+65 years) 20 , 22 , those with low educational attainment and low socioeconomic status 17 , 18 . For example, Yeong et al. noted how older adults with visual impairments and of low socioeconomic status needed websites to be compatible with different magnification levels and assistive technologies (e.g., iOS Voiceover [Apple Inc]; a screen reading software) to aid visibility 21 . The authors also noted how certain features aided navigation and minimised scrolling to help the user find information, such as tables of contents, drop-down menus, and ‘jump to top’ buttons 21 . Older adults with limiting conditions (visual or hearing) also suggested that navigation features, such as search bars and hyperlinks, needed to be of high contrast (compared to the rest of the screen) to improve visibility 20 , 21 . Yeong et al. emphasised how search features should be designed in a similar way to commonly visited search engines, like Google, to improve usability and reduce confusion 21 .
Older adults, homeless, ethnically diverse individuals and those with visual impairments all described how digital messages on software, health related websites or text messages should be simple, concise, and presented in a logical manner without time restrictions 18 , 20 , 21 , 24 . For example, older adults with visual impairments described how they did not have enough time to read the information when presented on a timed loop (i.e., rotating between different screens with information), and suggested that the user be able to manually control the timing of this loop 21 . Older adults interviewed in another study described how it would be useful if they could change the font size to improve the visibility of the text, and provide alternative languages for those who are not fluent in English 22 . Personalising information, such as allowing users to choose content that they are interested in, was felt to be one way of increasing the motivation to use health related websites and software amongst those with visual impairments 21 and ethnically diverse individuals 18 . Additionally, providing evidence that supported the key messages in healthcare information, such as the importance of reducing alcohol intake to reduce the risk of developing chronic health conditions, enhanced trust amongst ethnically diverse individuals 18 . Kramer et al. also emphasised how any communication should be culturally appropriate and avoid reinforcing stereotypes, especially for ethnically and linguistically diverse users 18 . For example, the language used to categorise different ethnicities on DHTs should avoid generic terms such as ‘men of colour’ as some ethnically diverse men found this offensive; they felt it defined them based on their skin colour and not their ethnic background. Instead, specific terminology should be used that accurately represented their ethnicities (e.g., African American for individuals with an African and American descent) 18 . Any imagery should also be inclusive to all cultural groups 18 .
It was felt that the overall user friendliness and engagement of health related software could be improved with the addition of engaging features 15 , 18 , 20 , 22 , 24 . This included interactive quiz elements 20 , notifications encouraging behavioural changes 18 , reminders about upcoming appointments (particularly for homeless individuals as this they may not have access to other reminders, like letters) 24 , ability to order a repeat prescription and schedule specific appointments (e.g., physiotherapy) 22 . Older adults of Jewish faith also suggested simplifying security features, as many found flicking between a text message with the password reset information and the screen (where the information should be entered) challenging 22 .
Infrastructure
Five studies described the need for supportive infrastructure, such as access to devices and connectivity (i.e., Wi-Fi) to support homeless individuals, ethnically and linguistically diverse groups, and individuals of low socioeconomic status 15 , 17 , 19 , 23 , 24 . For example, Howell et al. explained how community nurses in the UK provided homeless individuals with temporary access to smartphones during the pandemic so as to enable them to access vital digital healthcare support 19 . In the United States (US), homeless individuals were provided with phones (the Obama phone), credit and data plans financed through a government programme 24 . However, Asgary et al. found that some of these homeless individuals using the Obama phone plan often exceeded their limits when put on hold to schedule medical appointments 24 . They subsequently turned to friends and family for financial support to purchase credit 24 . Other homeless individuals were hesitant to accept this government support, with the authors reflecting on how this may have been due to the homeless experiencing a lack of government financial aid in the past 24 .
Homeless individuals 19 , ethnically and linguistically diverse groups 15 , 17 , 23 , and those of low educational attainment and low socioeconomic status 15 , 17 , 19 reported relying heavily on free Wi-Fi to be able to access healthcare. This included accessing free Wi-Fi in public spaces and transport systems, fast-food restaurants, clinics and families’ houses. However, they often experienced barriers to this connectivity with time limits set by the specific organisations (e.g., opening hours) 15 or restrictions placed on using shared devices (e.g., computer keyboards due to the risk of coronavirus spreading) 19 . Many participants suggested creating dedicated centres for digital health services with suitable devices and free Wi-Fi that would also include some private areas 15 . Access to these private spaces was felt to be important for some ethnic and linguistically diverse groups with low educational attainment and socioeconomic status, as they were concerned about being overheard when discussing/looking at confidential health information 17 . Many groups suggested that they would like the choice between both digital and non-digital access to healthcare, as this would help mitigate the risk of possibly excluding those with poor digital literacy skills, those who would prefer in-person consultations, or those who lack the resources to access digital healthcare 15 , 18 , 19 , 23 .
To complement infrastructural changes, ethnically diverse adults based in the US advocated for more resources to be provided by local government 15 . This included the introduction of new policies, such as reduced payment plans and regulations on the price of DHTs for lower income earners to make them affordable 15 . Older adults of Jewish faith and ethnically diverse adults with a low educational attainment and socioeconomic status also suggested that financial incentives could help promote greater access to DHTs and encourage motivation to use DHTs 15 , 22 . Alkureishi et al. highlighted how different organisations, such as hardware and Wi-Fi companies, might need to collaborate to ensure that these different components (e.g., devices, connectivity, financial aid) are jointly available to support successful implementation 15 .
Educational support
Provision of educational support was important for ethnically diverse individuals and older adults to enable their use of DHTs in five studies 15 , 16 , 19 , 20 , 22 . Ethnically diverse individuals with lower educational attainment and low socioeconomic status, and older adults of Jewish faith commonly reported asking family members to remain close during video healthcare consultations in case of technical issues 15 , or for their guidance with accessing online health information 22 . Mizrachi et al. found this support promoted independence over time as older adults’ digital skills developed through learning and they were further motivated to use DHTs on hearing positive experiences from their family and friends 22 .
Some individuals relied on educational support from professional services to use DHTs 19 . It was felt that in-person educational support from community workers or health care professionals with supplementary materials (e.g., videos and written information) would be beneficial prior to attending virtual appointments to support ethnically diverse adults (both above and below 65 years) from a low socioeconomic status and low educational attainment 15 , 16 Alternatively, Alkureishi et al. noted some participants expressed preference for accessing training classes at healthcare sites (e.g., hospitals) and community centres, where support was provided by ‘technology champions and coaches’ 15 . However, older adults of Jewish faith highlighted how advertisements to promote awareness of support services would be unlikely to reach individuals in their community and those who were socially isolated and arguably most in need of support 22 . Some studies also highlighted how certain groups (e.g., ethnically diverse adults with low socioeconomic status and low educational attainment, and older adults of Jewish faith) might also be reluctant to accept this educational support due to concerns around burdening others, feeling helpless, and/or reaffirming how they are unable to do something independently 15 , 22 .
This systematic review synthesises strategies that promote digital inclusivity and assess the barriers and facilitators to adopting these in practice. Our findings highlighted three key themes relating to user-friendly designs, supportive infrastructure, and provision of educational support. Barriers to adopting these strategies included a lack of acceptance amongst some underserved groups to receive such support, whilst facilitators included promoting trust amongst ethnically diverse groups by providing lay term friendly evidence that supports health claims.
Our findings highlighted how health-related software and websites must be interoperable across different devices to accommodate the needs of underserved groups. This form of user-friendly design is advocated by national healthcare providers and government bodies; for example, the UK and US have legislation in place which mandates that websites and software in the public sector be ‘perceivable, operable, understandable and robust’ to ensure that those with visual and hearing impairments, low reading ability (reading age of 9) and/or those who are not fluent in English can access and understand the information provided 25 , 26 . However, a recent study reported that public health authority websites in only three countries (UK, Italy, China) out of a total of 24 actually adhered to these accessibility standards when checked 27 . Additionally, the wider literature supports our findings on how the use of appropriate language and imagery can improve end-user satisfaction 18 , 28 . National bodies, such as the US National Institute of Health (NIH), have developed the ‘National Culturally and Linguistically Appropriate Services (CLAS) Standards’ to assist developers and researchers in developing culturally and linguistically appropriate services 29 . The wider literature also suggests co-designing DHTs with underserved groups at the earliest stages to help ensure that they meet the needs of all end-users 30 . This involves co-designing security features that are easy-to-use and align with the UK government ‘ secure by design principles’ , to help overcome any potential future barriers to usage 31 , 32 .
Our results also highlighted the need for supportive infrastructure to facilitate access and use of DHTs. Government schemes in high-income countries are already available; for example, the ‘Obama phone’ in the USA and the Emergency Broadband Benefits and social tariffs (reduced payment phone plans) in the UK, to support those on a low income to access smartphones and phone plans 24 , 33 . However, implementing supportive infrastructure might not be viable for low to middle income countries as they may have less suitable centres to provide devices and free public Wi-Fi spots, which high income countries already have access to 34 . Some charity organisations, such as the Good Things Foundation, have started to repurpose donated corporate IT devices and deliver them to those who are digitally excluded 35 . However, better promotion of the support available and a collaborative working environment is needed, especially by healthcare professionals, social services, and charities. Free phone numbers would also help to facilitate access to healthcare services. Some underserved groups would like the option of accessing healthcare via non digital means, thus questioning the temptation to always use technology to potentially address healthcare challenges 36 . Researchers need to consider whether a new DHT will provide an equitable solution to the healthcare problem and whether other means of accessing healthcare should also be provided within healthcare systems 37 .
This systematic review also underlined the importance of providing educational support, from family or professional services, to encourage motivation and capability to use DHTs. There is a need for effective advertising of this support to groups at particular risk of both digital and social exclusion, such as older adults and homeless individuals, in order to increase their awareness 38 . A systematic review conducted by Ige et al. 39 suggested using a combination of two or more strategies to reach socially isolated individuals, including referrals from relevant agencies (e.g., GPs, pharmacists etc), as this might be a more effective approach than relying solely on public facing methods 39 .
Previous recommendations to promote digital health equity have centred around guidance for behavioural and social science researchers with limited insight to the facilitators and barriers to implementing strategies into society and appear limited to research settings 40 . Previous reviews have applied the socioeconomic model to inform recommendations to promote digital health equity, such as providing devices (individual level support), educational support (relationship/interpersonal level support), access to connectivity infrastructure (community level support) and implementing policies (societal level support) 41 , 42 . However, there has been little consideration given to those individuals who belong to two or more underserved groups at risk of digital exclusion. Our systematic review considered this intersectionality and provides practical recommendations that focus on two main areas: collaborative working and effective advertising (Fig. 3 ). Collaborative working between the DHT developer, healthcare professionals, policy-makers, voluntary sectors, patients and public members of underserved groups is vital to help improve the co-design of DHTs and provision of support and should be embedded from the very beginning of the design and development process 30 . Effective advertising strategies are also vital to raise public awareness and ensure that those who are, or know of an individual, at risk of digital exclusion are made aware of in-person support that is available and how to access it. DHT developers and researchers should also be aware of the accessibility and inclusivity standards (e.g., government legislation and CLAS) and on how to use them to support digital health equity.

Summary of the two key recommendations to advance digital health equity, centring around adopting a collaborative working environment and using effective advertisement.
This review used a comprehensive and systematic approach to identify relevant literature. Included studies were published within the last decade to remain relevant to the current digital healthcare landscape. We opted to focus on qualitative research to gather rich detailed information on the facilitators and barriers to each strategy. Despite no geographical restrictions being placed on this search, we found that all included studies were conducted in high-income countries, which may limit the applicability of these findings to low- and middle-income countries; this also highlights the importance of further work in this area. Representation of the different religious groups and languages was limited, highlighting a gap in the literature and a need for greater diverse inclusion in research. None of the included studies reported on participants’ health literacy, which has previously been suggested to overlap with low digital literacy 43 ; this information would have aided our understanding of whether the participants included in the qualitative studies were truly representative of the groups that they were intended to represent. Future research should incorporate a standardised health literacy measure, such as the Newest Vital Sign (NVS) 44 or the Health Literacy Questionnaire (HLQ) 45 , into their methodology to provide greater detail on the participants in their study.
The appropriateness of recommendations from this systematic review could be further explored using an established framework, such as the APEASE criteria (Affordability, Practicability, Effectiveness, Acceptability, Size effects/safety, and Equity) 46 . This would involve seeking the perspectives of CLEARS demographic groups’ and relevant stakeholders’ (e.g., policy makers and community workers) on the practicalities of implementing these different strategies and recommendations to further advance this important area of digital health equity. The facilitators and barriers to implementing government-issued public health website accessibility standards should also be explored to further understand how to encourage use of these standards.
This systematic review identified three key themes relating to digital inclusivity, associated facilitators and barriers, and recommendations for advancing digital health equity. This information will guide individuals when designing, developing and implementing digital health interventions to ensure it is done in a digitally inclusive manner. This review also highlighted the need for further work to explore the feasibility and acceptance of implementing different strategies and recommendations to support digital health equity amongst those at risk of digital exclusion.
Identification of key groups at risk of digital exclusion
We conducted a scoping review of the literature to identify the sociodemographic factors that could put an individual at risk of digital exclusion. Based on the findings published in peer-reviewed articles 24 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , systematic reviews 61 , 62 , 63 , 64 , government reports 8 , 65 , and regulatory organisation documents 66 , we identified a number of sociodemographic factors that we complied into six groups, relating to Culture (ethnicity, language, and religion) 8 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 62 , Limiting conditions (visual and hearing impairments) 6 , 54 , 66 , Education (at or below United Kingdom (UK) government mandated level or equivalent) 52 , 55 , 56 , 66 , Age (over 65 years) 51 , 54 , 55 , 56 , 62 , 66 , Residence (rural or deprived areas [based on consensus data within a country], or homeless) 8 , 24 , 51 , 60 , and Socioeconomic status (low income [earns less than 60% of the median household annual income within a country] and unemployed individuals) 8 , 52 , 55 , 56 , 62 , 65 , 66 abbreviated to CLEARS (Fig. 4 ). These factors often intersect (i.e. intersectionality), placing an individual at even greater risk of digital exclusion 8 , 64 , 65 , 66 .

A framework which encompasses sociodemographic factors associated with digital exclusion and recognises the role of intersectionality.
Search strategy
This systematic review was registered with PROSPERO (CRD42022378199) and followed PRISMA guidelines 67 . The search string utilised terms from two relevant scoping reviews 8 , 68 , with additional relevant terms included when searching four large online databases (Medline, Embase, PsycINFO and Scopus) (Supplementary Tables 1 – 4 ). The search focused on words associated with digital technology, health inequities, and CLEARS (Table 2 ).
Eligibility criteria
The eligibility criteria followed the Population, Intervention, Comparison, Outcomes and Study design (PICOS) framework, recommended by the Cochrane Handbook for Systematic Reviews 69 , and provided an organising framework to list the main concepts in the search. The Population criteria included any group represented by our CLEARS framework (see above). The Intervention criteria focused on inclusive digital health strategies, which we defined as an action designed to alleviate the digital exclusion of individuals by promoting access, motivation, and/or use of information and communication technologies 2 , 3 , 4 , 5 . Articles needed to have discussed the facilitators or barriers associated with the inclusive digital health strategy (outcome criteria) to be included. This allowed the researchers to reflect on what currently worked or did not work to inform key recommendations. Only qualitative studies that provided rich in-depth experiences from CLEARS groups were included to aid our understanding of how a complex phenomenon, i.e., intersectionality, can affect digital exclusion 11 , 12 . Quantitative studies were excluded as they are designed to test a hypothesis or enumerate events or phenomena 11 , 12 , which was not aligned with the aim of this review. Only peer-reviewed articles published between 2012 and 2022 in the English language were included; this ensured only the latest advancements in digital technologies were considered.
Study selection
Results from each database were exported into EndNote (version 20.5, Clarivate, International) and duplicates removed. Remaining articles were uploaded to Rayyan (Qatar Foundation, State of Qatar) 70 , where titles, abstracts, and full-texts were screened independently by two reviewers (SW, LL, EB) to minimise bias. The lead author (SW) screened all articles, acting as a constant throughout the process. Disagreements were resolved by a third reviewer (RMA). The reasons for excluding full text articles were recorded (Fig. 1 ).
Data extraction and synthesis
The lead author (SW) developed a data-extraction sheet with the research team to extract and record specific study details, including participant demographics and a description of the inclusive digital health strategy under investigation (Supplementary Tables 5 and 6 ). Any measure used to record participants’ health literacy in the included studies, such as the Newest Vital Sign (NVS) 44 or the Health Literacy Questionnaire (HLQ) 45 , was also extracted. A quality assessment was carried out on the included studies using the Critical Appraisal Skills Programme (CASP) Qualitative Review Checklist 71 . Quality was measured by reporting the frequency of ‘yes’ (denoting the study met the criteria on the checklist) (Supplementary Tables 7 and 8 ).
The lead author (SW) performed a narrative thematic synthesis of the included studies. Firstly, the authors began by developing a preliminary synthesis of findings from included studies to identify the key strategies and list the facilitators and barriers to implementation. We then considered the factors that might explain any commonalities and differences in the successful implementation of these digital inclusive strategies across included studies. This involved exploring the directly reported verbatim quotations obtained from particular CLEARS groups and seeking to draw descriptive and explanatory conclusions around key themes 72 , 73 . All data management and analysis was carried out within N-Vivo (version 1.6.1, QSR International). Discussions with co-authors (SPS, RM, CT) were conducted at several stages throughout the analysis to discuss, refine and define themes to ensure a coherent narrative that reflected the data. Detailed descriptions and contextual material from the included studies was kept throughout the analysis to ensure that the trustworthiness was upheld 74 , 75 . Ethics approval was not required for this systematic review.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All relevant data used for the study has been included in the manuscript and supplementary information.
World Health Organization. Digital Health. URL: https://www.who.int/health-topics/digital-health#tab=tab_3 (2020).
National Institute for Health and Clinical Excellence. Evidence standards framework for digital health technologies. URL: https://www.nice.org.uk/corporate/ecd7/resources/evidence-standards-framework-for-digital-health-technologies-pdf-1124017447605 (2022).
Arora, S. et al. Detecting and monitoring the symptoms of Parkinson’s disease using smartphones: A pilot study. Parkinsonism Relat. Disord. 21 , 650–653 (2015).
Article CAS PubMed Google Scholar
Yao, R. et al. Inequities in Health Care Services Caused by the Adoption of Digital Health Technologies: Scoping Review. J. Med. Internet Res. 24 , e34144 (2022).
Article PubMed PubMed Central Google Scholar
Berwick, D. M., Nolan, T. W. & Whittington, J. The triple aim: care, health, and cost. Health Aff. 27 , 759–769 (2008).
Article Google Scholar
Espay, A. J. et al. Technology in Parkinson’s disease: challenges and opportunities. Mov. Disord. 31 , 1272–1282 (2016).
National Institute for Health Research. Improving inclusion of under-served groups in clinical research: Guidance from include project. URL: https://www.nihr.ac.uk/documents/improving-inclusion-of-under-served-groups-in-clinical-research-guidance-from-include-project/25435 (2022).
Honeyman, M., Maguire, D., Evans, H. & Davies, A. Digital technology and health inequalities: a scoping review (Public Health Wales NHS Trust, 2020).
Mitchell, C. et al. Underserved ‘Deep End’ populations: a critical analysis addressing the power imbalance in research. Br. J. Gen. Pract. 73 , 326–329 (2023).
Kaihlanen, A. M. et al. Towards digital health equity—a qualitative study of the challenges experienced by vulnerable groups in using digital health services in the COVID-19 era. BMC Health Serv. Res. 22 , 188 (2022).
Patton, M. Q. Alternative Evaluation Research Paradigm (University of North Dakota, 1975).
Sofaer, S. Qualitative methods: what are they and why use them? Health Serv. Res. 34 , 1101 (1999).
CAS PubMed PubMed Central Google Scholar
World Health Organization. WHO guideline: recommendations on digital interventions for health system strengthening (World Health Organization, 2019).
NHS England. Supporting digital inclusion in general practice: 10 top tips. Available from: https://www.england.nhs.uk/long-read/supporting-digital-inclusion-in-general-practice-10-top-tips/#:~:text=For%20NHS%20patients%2C%20digital%20inclusion,confidently%20to%20access%20NHS%20services (2023). (Accessed 29 October 2023).
Alkureishi, M. A. et al. Digitally disconnected: qualitative study of patient perspectives on the digital divide and potential solutions. JMIR Hum. Factors 8 , e33364 (2021).
Choxi, H., VanDerSchaaf, H., Li, Y. & Morgan, E. Telehealth and the digital divide: Identifying potential care gaps in video visit use. J. Med. Syst. 46 , 58 (2022).
Kim, H. & Zhang, Y. Health information seeking of low socioeconomic status Hispanic adults using smartphones. Aslib J. Inf. Manag. 67 , 542–561 (2015).
Kramer, J. et al. Black men’s experiences with health care: individuals’ accounts of challenges, suggestions for change, and the potential utility of virtual agent technology to assist black men with health management. Qualitative Health Res. 31 , 1772–1785 (2021).
Howells, K. et al. Remote primary care during the COVID-19 pandemic for people experiencing homelessness: a qualitative study. Br. J. Gen. Pract. 72 , e492–e500 (2022).
Maidment, D. W. et al. Evaluating a theoretically informed and co-created mobile health educational intervention for first-time hearing aid users: qualitative interview study. JMIR mHealth uHealth 8 , e17193 (2020).
Yeong, J. L., Thomas, P., Buller, J. & Moosajee, M. A newly developed web-based resource on genetic eye disorders for users with visual impairment (Gene. Vision): usability study. J. Med. Internet Res. 23 , e19151 (2021).
Mizrachi, Y., Shahrabani, S., Nachmani, M. & Hornik, A. Obstacles to using online health services among adults age 50 and up and the role of family support in overcoming them. Isr. J. Health Policy Res. 9 , 1–10 (2020).
Wikaire, E. et al. Reducing healthcare inequities for Māori using telehealth during COVID-19. NZ Med. J. 135 , 112–117 (2022).
Google Scholar
Asgary, R. et al. Perceptions, attitudes, and experience regarding mHealth among homeless persons in New York City shelters. J. Health Commun. 20 , 1473–1480 (2015).
Public Sector Bodies (Websites and Mobile Applications) (No. 2) Accessibility Regulations https://www.legislation.gov.uk/uksi/2018/952/contents (2018).
Checklist of requirements for federal websites and digital services. Accessibility and Section 508. https://digital.gov/resources/checklist-of-requirements-for-federal-digital-services/ (2018).
Alajarmeh, N. Evaluating the accessibility of public health websites: an exploratory cross-country study. Univers. Access Inf. Soc. 21 , 771–789 (2022).
Article PubMed Google Scholar
Brach, C. & Fraserirector, I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Med. Care Res. Rev. 57 , 181–217 (2000).
U.S. Department of Health and Human Services, Office of Minority Health. National Standards for Culturally and Linguistically Appropriate Services in Health and Health Care: Compendium of State-Sponsored National CLAS Standards Implementation Activities. Washington, DC: U.S. Department of Health and Human Services (2016).
Slattery, P., Saeri, A. K. & Bragge, P. Research co-design in health: a rapid overview of reviews. Health Res. Policy Syst. 18 , 1–3 (2020).
Central Digital and Data Office (CDDO). Secure by design principles. URL: https://www.security.gov.uk/guidance/secure-by-design/principles/#4-design-usable-security-controls (2024).
Central Digital and Data Office (CDDO). Understanding business objectives and user needs. URL: https://www.security.gov.uk/guidance/secure-by-design/activities/understanding-business-objectives-and-user-needs (2024).
UK Government. Low cost broadband and mobile phone tariffs. URL: https://www.gov.uk/government/news/low-cost-broadband-and-mobile-phone-tariffs (2022).
Verhagen, L. M. et al. COVID-19 response in low-and middle-income countries: Don’t overlook the role of mobile phone communication. Int. J. Infect. Dis. 99 , 334–337 (2020).
Article CAS PubMed PubMed Central Google Scholar
National Device Bank: Donate unused corporate IT equipment. URL: https://www.goodthingsfoundation.org/national-device-bank/ (2023).
IJsselsteijn, W., Tummers-Heemels, A. & Brankaert, R. Warm technology: A novel perspective on design for and with people living with dementia. In HCI and Design in the Context of Dementia , 33–47 (2020).
Shull, J. G. Digital health and the state of interoperable electronic health records. JMIR Med. Inform. 7 , e12712 (2019).
Landeiro, F., Barrows, P., Musson, E. N., Gray, A. M. & Leal, J. Reducing social isolation and loneliness in older people: a systematic review protocol. BMJ Open 7 , e013778 (2017).
Ige, J., Gibbons, L., Bray, I. & Gray, S. Methods of identifying and recruiting older people at risk of social isolation and loneliness: a mixed methods review. BMC Med. Res. Methodol. 19 , 1–10 (2019).
Article CAS Google Scholar
Jaworski, B. K. et al. Advancing digital health equity: Directions for behavioral and social science research. Transl. Behav. Med. 13 , 132–139 (2023).
McCall, T. et al. A socio-ecological approach to addressing digital redlining in the United States: a call to action for health equity. Front. Digital Health 4 , 897250 (2022).
Richardson, S., Lawrence, K., Schoenthaler, A. M. & Mann, D. A framework for digital health equity. NPJ Digital Med. 5 , 119 (2022).
Stone, E., Nuckley, P. & Shapiro, R. Digital inclusion in health and care: lessons learned from the NHS Widening Digital Participation Programme (Good Things Foundation, 2020).
Weiss, B. D. et al. Quick assessment of literacy in primary care: the newest vital sign. Ann. Fam. Med. 3 , 514–522 (2005).
Osborne, R. H. et al. The grounded psychometric development and initial validation of the Health Literacy Questionnaire (HLQ). BMC Public Health 13 , 7 (2013).
Michie, S., Atkins, L. & West, R. The behaviour change wheel. A guide to designing interventions (Silverback Publishing, 2014).
Boonya-Ananta, T. et al. Monte Carlo analysis of optical heart rate sensors in commercial wearables: the effect of skin tone and obesity on the photoplethysmography (PPG) signal. Biomed. Opt. Express 12 , 7444–7457 (2021).
Mitchell, U. A., Chebli, P. G., Ruggiero, L. & Muramatsu, N. The digital divide in health-related technology use: The significance of race/ethnicity. Gerontologist 59 , 6–14 (2019).
Diao, J. A. et al. Clinical implications of removing race from estimates of kidney function. JAMA 325 , 184–186 (2021).
Levey, A. S. et al. Kidney disease, race, and GFR estimation. Clin. J. Am. Soc. Nephrol. 15 , 1203–1212 (2020).
Dilmaghani, M. Religiosity and the digital divide in Canada. Commun. Rev. 21 , 181–211 (2018).
Jamil, S. From digital divide to digital inclusion: Challenges for wide-ranging digitalization in Pakistan. Telecommun. Policy 44 , 102206 (2021).
Bix, A. S. Remember the Sabbath’: a history of technological decisions and innovation in Orthodox Jewish communities. Hist. Technol. 36 , 205–239 (2020).
Harris, J. The use, role and application of advanced technology in the lives of disabled people in the UK. Disability Technol. 80–127 (2017).
Estacio, E. V., Whittle, R. & Protheroe, J. The digital divide: examining socio-demographic factors associated with health literacy, access and use of internet to seek health information. J. Health Psychol. 24 , 1668–1675 (2019).
Alvarez-Galvez, J. et al. The persistence of digital divides in the use of health information: A comparative study in 28 European countries. Int. J. Public Health 65 , 325–333 (2020).
Elena-Bucea, A. et al. Assessing the role of age, education, gender and income on the digital divide: Evidence for the European Union. Inf. Syst. Front. 23 , 1007–1021 (2021).
Yao, Y. et al. Bridging the digital divide between old and young people in China: challenges and opportunities. Lancet Healthy Longev. 2 , e125–e126 (2021).
Holgersson, J. & Söderström, E. Bridging the gap: Exploring elderly citizens’ perceptions of digital exclusion. In 27th European Conference on Information Systems (ECIS) (Association for Information Systems, 2019).
Rhoades, H. et al. No digital divide? Technology use among homeless adults. J. Soc. Distress Homeless 26 , 73–77 (2017).
Saeed, S. A. & Masters, R. M. Disparities in health care and the digital divide. Curr. Psychiatry Rep. 23 , 1–6 (2021).
Reiners, F. et al. Sociodemographic factors influencing the use of eHealth in people with chronic diseases. Int. J. Environ. Res. Public Health 16 , 644 (2019).
Almathami, H. K., Win, K. T. & Vlahu-Gjorgievska, E. Barriers and facilitators that influence telemedicine-based, real-time, online consultation at patients’ homes: systematic literature review. J. Med. Internet Res. 22 , e16407 (2020).
Husain, L. et al. Desperately seeking intersectionality in digital health disparity research: narrative review to inform a richer theorization of multiple disadvantage. J. Med. Internet Res. 24 , e42358 (2022).
Gov.uk. Ethnicity facts and figures: People in low-income households. URL: https://www.ethnicity-facts-figures.service.gov.uk/work-pay-and-benefits/pay-and-income/people-in-low-income-households/latest (2022).
Ofcom. Digital exclusion: A review of Ofcom’s research on digital exclusion among adults in the UK. URL: https://www.ofcom.org.uk/__data/assets/pdf_file/0022/234364/digital-exclusion-review-2022.pdf (2022).
Page, M. J. et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int. J. Surg. 88 , 105906 (2021).
Budhwani, S. et al. Challenges and strategies for promoting health equity in virtual care: findings and policy directions from a scoping review of reviews. J. Am. Med. Inform. Assoc. 29 , 990–999 (2022).
Tacconelli, E. Systematic reviews: CRD’s guidance for undertaking reviews in health care. Lancet Infect. Dis. 10 , 226 (2010).
Rayyan: AI powered tool for Systematic Literature Reviews. Available from: https://www.rayyan.ai/ (2023).
Critical Appraisal Skills Programme. CASP Qualitative Studies Checklist. URL: https://casp-uk.net/images/checklist/documents/CASP-Qualitative-Studies-Checklist/CASP-Qualitative-Checklist-2018_fillable_form.pdf (2023). (Accessed 30 April 2023).
Pope, C. & Mays, N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 311 , 42–45 (1995).
Popay, J., Rogers, A. & Williams, G. Rationale and standards for the systematic review of qualitative literature in health services research. Qualitative Health Res. 8 , 341–351 (1998).
Wertz, F. J. Five ways of doing qualitative analysis: Phenomenological psychology, grounded theory, discourse analysis, narrative research, and intuitive inquiry , 228 (Guilford Press, 2011).
Lucas, P. J., Baird, J., Arai, L., Law, C. & Roberts, H. M. Worked examples of alternative methods for the synthesis of qualitative and quantitative research in systematic reviews. BMC Med. Res. Methodol. 7 , 1–7 (2007).
Download references
Acknowledgements
We would like to thank the social sciences librarian, Karen Crinnion, at Philip Robinson Library, Newcastle University, for her help and advice regarding the search strategy, choice of databases and search keywords for this systematic review. This work has been supported by the Early Detection of Neurodegenerative diseases (EDoN) research initiative, funded by Alzheimer’s Research UK with support from Gates Ventures and the Alzheimer’s Drug Discovery Foundation through its Diagnostic Accelerator Project. This project is also funded by the NIHR, (NIHR205190). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. Ríona Mc Ardle is funded by the National Institute for Health Research (NIHR) (NIHR 301677) and the NIHR Newcastle Biomedical Research Centre (BRC) based at The Newcastle upon Tyne Hospital National Health Service (NHS) Foundation Trust; Newcastle University; and the Cumbria, Northumberland and Tyne and Wear (CNTW) NHS Foundation Trust. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care.
Author information
Authors and affiliations.
School of Pharmacy, Newcastle University, Newcastle Upon Tyne, UK
Sarah Wilson, Clare Tolley, Lauren Lawson, Nehal Hassan & Sarah Slight
Translational and Clinical Research Institute, Newcastle University, Newcastle Upon Tyne, UK
Ríona Mc Ardle
Trinity College Dublin, Dublin, Ireland
Emily Beswick
The Newcastle upon Tyne Hospitals NHS Foundation Trust, Newcastle Upon Tyne, UK
Robert Slight & Sarah Slight
You can also search for this author in PubMed Google Scholar
Contributions
S.W. (Lead author): Conception and design of the work. Methodology. Literature search and data acquisition, analysis and interpretation of the data. Drafting (writing original draft) and revising. Visualisations. Completion of version. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. S.S. (Corresponding author): Conception of the work. Funding acquisition. Methodology. Revising the work (providing feedback) and supervision of lead author. Final approval of the completed version. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. C.T.: Conception of the work. Methodology. Revising the work (providing feedback) and supervision of lead author. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. R.M.A.: Conception of the work. Methodology. Revising the work (providing feedback) and supervision of lead author. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. R.S.: Conception of the work. Methodology. Revising the work (providing feedback) and supervision of lead author. Accountability for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. N.H.: Revising the work (providing feedback). E.B.: Data acquisition (second check of the articles). Revising the work (providing feedback). L.L.: Data acquisition (second check of the articles). Revising the work (providing feedback).
Corresponding author
Correspondence to Sarah Slight .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wilson, S., Tolley, C., Mc Ardle, R. et al. Recommendations to advance digital health equity: a systematic review of qualitative studies. npj Digit. Med. 7 , 173 (2024). https://doi.org/10.1038/s41746-024-01177-7
Download citation
Received : 24 January 2024
Accepted : 21 June 2024
Published : 29 June 2024
DOI : https://doi.org/10.1038/s41746-024-01177-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Find an expert
- Media contacts
Student links
- How to log in to University systems
- Class timetables
- Our rankings
- Faculties and schools
- Research centres
- Campus locations
- Find a staff member
- Careers at Sydney
- Find an event
- Emergencies and personal safety
- Accessibility
- Website feedback
- Johns Hopkins University Human Resources
- Benefits & Worklife
- Our Health & Life Offerings
- Student & Learner Health Benefits
PhD Benefits Overview
The following benefits are available to PhDs at Johns Hopkins University.
PhDs are auto-enrolled into individual medical coverage. The plan is administered by Wellfleet and utilizes the Cigna PPO network of providers. Prescription coverage is included in the medical plan. For more information about the plan, please visit: Wellfleet Medical Plan – JHU Human Resources
To enroll dependents into medical coverage, please visit: https://students.care26.com/login
PhDs are auto-enrolled into individual level dental coverage. The plan is offered in partnership with Delta Dental and utilizes the Delta Dental PPO + Primer network of providers. For more information about the dental plan, please visit: Delta Dental Plan – JHU Human Resources
To enroll dependents into dental coverage, please visit: https://students.care26.com/login
PhDs are auto-enrolled into individual level vision coverage through EyeMed on the Insight Network. For more information about the vision plan, please visit: EyeMed Vision Plan – JHU Human Resources
PhDs at the University are required to re-enroll their dependents each semester (Fall/Spring) or each Term (Term 1, Term 2, Term 3, and Term 4) for BSPH.
Effective 8/15/2024 , PhDs are eligible to be reimbursed for their dependent premiums if they enrolled a child or spouse/domestic partner that is not eligible to work in the US and does not have other insurance coverage. To complete the application for reimbursement, please follow this link.
PhDs submitting for reimbursement must do so within 90 days of payment and will need to upload a copy of their receipt for the student benefits office to review here .
As a PhD student, you can participate in a voluntary benefits program to purchase a discounted legal services plan. You can enroll during annual enrollment (7/1 – 9/15 each year).
The MetLife Legal Plan gives you access to a nationwide network of more than 12,000 attorneys, to help you and your dependents with vital legal matters such as estate planning, financial, and support with reproductive issues. You can receive a consultation over the phone or in person.
To enroll, please visit: phd.jhuvoluntarybenefits.com
As a PhD student, you can participate in a voluntary benefits program to purchase Pet Insurance. You can enroll in the program at any time.
Nationwide pet insurance helps you cover veterinary expenses so you can provide your pets with the best care possible without worrying about the cost.
For more information and to enroll into pet insurance, please visit: phd.jhuvoluntarybenefits.com
As a PhD student, you can participate in a voluntary benefits program to purchase Identity Protection. You can enroll in the program at any time.
With Allstate Identity Protection Pro Plus, you’ll get access to: identity and credit monitoring, dark web monitoring, social medical reputation monitoring, financial threshold monitoring, digital wallet storage and monitoring, data breach notification, and more.
For more information and to enroll, please visit: phd.jhuvoluntarybenefits.com
PhD students are eligible to be reimbursed for bus passes purchased through the MTA All Access College Program or through the U-Pass program. PhDs can be reimbursed for 2 passes at one time. Each pass is valid for 31 days. Reimbursement for passes will be processed through concur and must be submitted within 90 days of payment.
PhDs must opt-in to have their information shared with the MTA / U-Pass for discounted bus passes. To Opt-In, PhDs must complete this form.
To submit your receipt to Concur, please visit: https://login.johnshopkins.edu/concur
PhDs in full-time resident status will receive child subsidies of $4,500 per child per fiscal year for eligible children under the age of six (6) or $3,000 per child aged six (6) to eighteen (18), with a maximum of $12,000 per family per year.
Must be eligible dependents under the Student Health Benefits Plan (SHBP).
PhDs with adult dependents as defined by Section 152 of the Internal Revenue Code will qualify for this benefit at a rate of $3,000 per dependent per fiscal year.
Dependents are defined as anyone for whom you provided more than 50% of the financial support for the year, as defined in Section 152 of the Internal Revenue Code, and who resides in your home at least one-half of the taxable year.
The subsidies will be paid in installments over the course of the fiscal year.
To apply for the PhD Dependent Subsidy, please complete the online application.
At the end of the application, you will be required to upload copies of your dependent verification documents (child’s birth certificate or passport that shows their date of birth, copy of J-2 visa with dependents name and date of birth, or copy of marriage certificate with spouse’s name and date of birth). Please upload dependent verification documents here .
Student Health & Well-Being (SHWB) Primary Care consists of three clinic locations (Homewood, East Baltimore, and Washington DC) that provide a variety of medical services for the evaluation and treatment of an illness or injury, preventive health care and health education to the Johns Hopkins University student and trainee population. For more information or to schedule an appointment, please visit: Primary Care (jhu.edu)
Mental Health Services supports the diverse community of Johns Hopkins University students and trainees through the provision of accessible, high-quality and compassionate mental healthcare resources. We are committed to diversity, equity, inclusion, and justice and prioritize these values in our approach to clinical care as well as every aspect of the work we do. For more information or to schedule an appointment, please visit: Mental Health Services (jhu.edu)
PhD students are eligible to receive no less than 8 weeks of fully-paid new child accommodations. For more information please visit: New Child Accommodations for Full Time Graduate Students and Postdoctoral Trainees (jhu.edu)
The following benefits are administered by JHU Benefits & WorkLife.
Locate Search Child Care by the Maryland Family Network (eligible at any time)
Child Care Voucher Program (eligible as of the date of appointment, application required annually)
Child Care Scholarships to JHU Partner Centers (eligible as of the date of appointment, application required annually)
Please contact 410-516-2000, [email protected] or [email protected] if you have questions about these programs.
- Career Advice
- Carpe Careers
How Your Ph.D. Prepares You to Be an Entrepreneur
You can deploy skills you develop as a grad student and postdoc in a variety of careers, including working for a start-up or founding your own, Chris Smith writes.
By Chris Smith
You have / 5 articles left. Sign up for a free account or log in.

Yutthana Gaetgeaw/iStock/Getty Images Plus
Innovation has become a hot topic in economic circles over the past few years. In March 2022, the United States’ National Science Foundation created its first new directorate in over 30 years : Technology, Innovation and Partnerships , or TIP. The passing of the CHIPS and Science Act of 2022 helped fund the directorate, the mission of which is to “advance U.S. competitiveness and societal impact by nurturing partnerships that drive and accelerate diverse innovation ecosystems, technology translation and development, and workforce development.” The U.S. is investing heavily in research and innovation—which you can take advantage of as a Ph.D. researcher working in academia or beyond.
Graduate students and postdoctoral scholars already contribute much to research and innovation in the United States through their work on a variety of projects supported by the federal government and industry partners. But despite that fact, few consider a career focused on the leading edge of innovation: entrepreneurship.
Being willing to push the boundaries of human knowledge and forge new ideas into products is essential for entrepreneurs. And to secure backing, entrepreneurs must also work to articulate the value they and their products bring to individuals, organizations and the nation. Fortunately, plenty of resources are available to assist in those efforts, although many graduate students and postdocs may not be aware of them.
To encourage more technology commercialization and entrepreneurship, in the latter half of the 20th century the federal government established two funding programs for academics and others seeking to either move full-time to a start-up company or obtain funding to develop and commercialize new technologies. The Small Business Innovation Research program supports the growth of start-up companies, while the Small Business Technology Transfer program is aimed at technology commercialization.
Both the National Institutes of Health and NSF fund grants from both programs, and both offer a variety of other mechanisms to foster an innovation and entrepreneurial ecosystem in the United States. In addition, NIH provides numerous resources to educate people about entrepreneurship and special programs like the Small Business Transition Grant for New Entrepreneurs (see a webinar on the program here ), which helps researchers interested in transitioning to entrepreneurship via a mentor.
American universities also offer an increasing number of programs that either focus on training Ph.D.s for careers in the technology transfer space or assist them in learning how to commercialize technological and other innovations coming from their research work, as our Innovation Postdoctoral Fellowship here at Virginia Tech seeks to do. In addition, NSF’s Innovation Corps (I-Corps) provides a seven-week experiential training program that prepares scientists and engineers to extend their focus beyond the university laboratory and toward commercialization by engaging in customer discovery and other activities. Such programs can be a bridge between traditional academic research and exploring an entrepreneurial career or employment in the innovation and entrepreneurial ecosystem.
Many academics may mistakenly believe that entrepreneurial skills are only relevant if one is planning to run a start-up company. Yet most faculty members running research groups at large universities are effectively leading small businesses inside their institutions. They must articulate a value proposition to get hired and ultimately secure funding for their research. In addition, most faculty leaders or principal investigators are in charge of hiring those who work in their labs and must manage these individuals and their projects toward a larger, common goal. A faculty leader must create a vision for their group and think strategically about how the various projects align toward both short- and long-term goals. This is entrepreneurship in an academic research context.
And just as an entrepreneurial mindset is essential to a successful academic career, it is also extremely useful for any scholar looking to create their own company, independent of their institution.
Entrepreneurial Skills From Your Ph.D. or Postdoc
Ph.D. training offers graduate students and postdocs many experiences to help them navigate entrepreneurship and/or working in a start-up company, such as the following.
- Project planning and management. Completing a doctoral dissertation involves extensive project planning and management skills, from ideation to execution and dissemination. This directly translates to the ability to plan and manage large projects as an entrepreneur.
- Independent work. Ph.D. students, and especially postdocs, often work independently with minimal oversight, building the drive and accountability needed to accomplish tasks without rigid external deadlines—a crucial skill for entrepreneurs.
- Networking and collaboration. Entrepreneurs thrive on networking. Similarly, Ph.D. students and postdocs benefit from building strong connections—engaging with industry professionals, attending conferences and collaborating across disciplines to enhance their network. Such connections can lead to job opportunities, collaborations and funding.
Editors’ Picks
- DEI Ban Prompts Utah Colleges to Close Cultural Centers, Too
- Supreme Court Decision Weakens Education Department
- The Only Certainty Is Uncertainty
- Thirst for knowledge. A core requirement for a Ph.D. is an insatiable desire to learn and expand one’s knowledge base. Entrepreneurs must constantly step out of their comfort zones and learn new skills, making this thirst for learning invaluable for Ph.D.s and postdocs looking to focus on entrepreneurship as a career.
- Research skills. Doctoral training equips individuals with the ability to seek out, evaluate and synthesize quality information from various sources—a vital skill when navigating the unfamiliar territories of entrepreneurship.
- Curiosity about the big questions. Starting a business requires asking and answering big questions about target audiences, value propositions and strategic direction. Ph.D.s are trained to take disparate information and craft cohesive narratives to address complex inquiries. Successful entrepreneurs do the same.
- Problem-solving. Overcoming research obstacles and failed experiments hones problem-solving abilities in Ph.D.s and postdocs. As entrepreneurs constantly face new challenges, this skill is indispensable for finding innovative solutions.
- Resilience and adaptability. Entrepreneurship involves risk-taking and overcoming failures. Ph.D. students and postdocs learn resilience by navigating setbacks. This adaptability prepares them for a dynamic marketplace for their products and ideas and the post-Ph.D. job market itself, where flexibility and the ability to pivot are critical.
In essence, the rigorous training and self-driven nature of doctoral programs and postdoc positions cultivate skills like project management, working both independently and collaboratively, learning agility, strategic thinking and problem-solving—all of which are invaluable assets for successful entrepreneurship. The key to honing these skills is taking increased agency in your projects so that you learn all aspects of the process of identifying a gap in knowledge or application, scoping out the current landscape of that area and working toward a solution. It is certainly not easy work, but it can help you in graduate school, postdoctoral training and beyond.
In sum, by embracing an entrepreneurial mindset in your job search, you identify opportunities in industry, start-ups, government or nonprofits or create your own position through entrepreneurship. And even if you don’t decide to go that direction, innovative thinking and treating one’s career development like a start-up can propel you to professional growth and success. The fact that cultivating the entrepreneurial skills I’ve described can also be significantly helpful for an academic researcher means leaning into them is a win-win for any graduate student or postdoc.
Chris Smith is the postdoctoral affairs program administrator at Virginia Tech. He serves on the National Postdoctoral Association’s Board of Directors and is a member of the Graduate Career Consortium—an organization providing an international voice for graduate-level career and professional development leaders.

Student Wellness Tip: First-Year Workshops Promote Health and Wellness
Champlain College launched a 10-week curricular program to build students’ skills in transition, t
Share This Article
More from carpe careers.

STEM Trainees Must Master Writing Skills
Articulating discoveries, gaining funding and forging connections all require the ability to convey ideas, write Mabe

The Power of Confident and Impactful Communication
Scholars must convey complex concepts in ways that make an impression, write Diane A.

A Graduate Student’s Guide to Managing Change
Dinuka Gunaratne and Roshni Rao offer advice for handling all the new academic demands and social dynamics, so you ca
- Become a Member
- Sign up for Newsletters
- Learning & Assessment
- Diversity & Equity
- Career Development
- Labor & Unionization
- Shared Governance
- Academic Freedom
- Books & Publishing
- Financial Aid
- Residential Life
- Free Speech
- Physical & Mental Health
- Race & Ethnicity
- Sex & Gender
- Socioeconomics
- Traditional-Age
- Adult & Post-Traditional
- Teaching & Learning
- Artificial Intelligence
- Digital Publishing
- Data Analytics
- Administrative Tech
- Alternative Credentials
- Financial Health
- Cost-Cutting
- Revenue Strategies
- Academic Programs
- Physical Campuses
- Mergers & Collaboration
- Fundraising
- Research Universities
- Regional Public Universities
- Community Colleges
- Private Nonprofit Colleges
- Minority-Serving Institutions
- Religious Colleges
- Women's Colleges
- Specialized Colleges
- For-Profit Colleges
- Executive Leadership
- Trustees & Regents
- State Oversight
- Accreditation
- Politics & Elections
- Supreme Court
- Student Aid Policy
- Science & Research Policy
- State Policy
- Colleges & Localities
- Employee Satisfaction
- Remote & Flexible Work
- Staff Issues
- Study Abroad
- International Students in U.S.
- U.S. Colleges in the World
- Intellectual Affairs
- Seeking a Faculty Job
- Advancing in the Faculty
- Seeking an Administrative Job
- Advancing as an Administrator
- Beyond Transfer
- Call to Action
- Confessions of a Community College Dean
- Higher Ed Gamma
- Higher Ed Policy
- Just Explain It to Me!
- Just Visiting
- Law, Policy—and IT?
- Leadership & StratEDgy
- Leadership in Higher Education
- Learning Innovation
- Online: Trending Now
- Resident Scholar
- University of Venus
- Student Voice
- Academic Life
- Health & Wellness
- The College Experience
- Life After College
- Academic Minute
- Weekly Wisdom
- Reports & Data
- Quick Takes
- Advertising & Marketing
- Consulting Services
- Data & Insights
- Hiring & Jobs
- Event Partnerships
4 /5 Articles remaining this month.
Sign up for a free account or log in.
- Sign Up, It’s FREE
More From Forbes
What digital health can learn from big pharma.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Dr. Jeff Wessler (MD MPhil FACC) is a virtual cardiologist, the Founder of Heartbeat Health , and on clinical faculty at Northwell Health.

Imagine if new drugs were developed the way Silicon Valley startups make their products. A few scrappy entrepreneurs would concoct a compound in a rented garage, then try to get as many people as possible to try it.
Nobody would put up with that, of course, at least not after patients were hurt (or worse) by “bugs” in the new drug. We expect, and the government requires, a much higher standard for medical products than we do for our gadgets and online services.
This is a distinction that most companies that build digital health products have missed, which may contribute to why the industry is struggling to raise capital and why some startups struggle to find a profitable business model. I believe the digital health community has adopted too much of our playbook from technology and not enough from healthcare.
Since 2010, companies have raised billions of dollars with a mission to use technology to reinvent how health conditions are diagnosed and treated. Billions more poured into the sector in 2020 and 2021, as investors were likely betting that the Covid-19 pandemic would launch digital healthcare into the mainstream.
‘The First Descendant’ Servers Remain Offline During A Rough Day Two
Fed chair powell issues ‘critical’ warning, sparking sudden $60,000 bitcoin price and crypto crash, samsung issues update warning for galaxy smartphones as google confirms new threat.
It did not. So far, I haven’t seen the emergence of any company that is even beginning to disrupt healthcare delivery the way Uber shook up transportation and Netflix reorganized television.
Investors, meanwhile, seem to be disillusioned. Venture investments into digital health fell to $4.6 billion in 2023 from $17.7 billion in 2021. As of June 10, 2024, S&P’s index of digital health stocks is down 70% from its peak in January 2021. (In this context, digital health companies are those that use technology to prevent or treat health conditions in their patients. There are many companies that have found success selling technology that improves the operations of healthcare providers.)
Some explain the digital health industry’s woes as the inevitable result of the Covid bubble. Bessemer, for example, recently suggested that the sector is following the “hype cycle” so common in other technology markets where the “trough of disillusionment” follows the “peak of inflated expectations.”
As an entrepreneur running a digital health company, it’s clear to me that digital health faces deeper problems than the fickle fancies of investors.
I think we've modeled ourselves too much on Silicon Valley, with its move-fast-and-break-things, fake-it-till-you-make-it style. We’ve built slick apps and sleek devices, but they have resulted in few significant advances in the outcomes that matter: helping people stay well or get better.
Digital health companies could be better off emulating the methodical approach of the pharmaceutical industry. It conducts excellent science because it invests significantly in research and development. Further, it understands its market well enough to identify what will pay off on the business side.
Yes, there are legitimate criticisms of Big Pharma’s pricing and marketing strategies, but these don’t undercut the real value that the industry has created for patients and investors.
Before a new drug is approved, it is tested in vitro and in animal models before undergoing testing for safety and efficacy in humans.
In the United States, the Food and Drug Administration also regulates most medical devices, including some software and mobile apps . Some devices are exempt from FDA review "if they are extremely low risk or very similar to existing devices." Those that "are very important to health or sustaining life," like pacemakers, must prove their safety and effectiveness.
The offerings of digital health companies, however, don’t always fit into these narrow regulatory categories. They often weave together devices (for testing or therapies), apps and digital access to clinicians into protocols meant to treat a particular condition.
Many digital health companies do only the most rudimentary testing on these protocols before bringing products to market. Very few have published double-blind, placebo-controlled studies in top-tier, peer-reviewed journals.
My company, Heartbeat Health, has worked hard to collect data and study our care model. But we’ve been in the cardiology telehealth business for eight years, and frankly, we should have done much more safety and effectiveness research sooner.
Instead, like many other digital health companies, we followed the Silicon Valley playbook, where success is measured by how fast you can bring on new customers and increase revenue.
But now it’s time for all of us in the sector to admit that this land rush approach hasn’t worked. Everyone involved—entrepreneurs, investors and especially health insurers and other payers—could benefit from adopting two concepts that are standard in the pharmaceutical industry:
1. Agreed-Upon Standards For Safety And Effectiveness
Everyone likes to complain about regulation, but in many industries, such as pharmaceuticals, strictly enforced standards and a level playing field make for good business and good customer outcomes.
That said, I’m not sure the right answer here is for the FDA to regulate every aspect of digital treatment protocols. Another option is that the industry could develop a certification program for digital health services. One existing model is the V3 standard for validating sensor-based digital health technology created by the nonprofit Digital Medicine Society.
2. A Longer Timeframe
More testing and higher standards mean it will take longer to get digital health products to market. But there is already a useful model for that: biotech. It can take a decade or more for a startup with an innovative new drug, therapy or device to get it to market. Investors provide capital, understanding they will need to wait for a return. Thankfully, it should take less time to refine and validate most digital health products than it does a complex genetically engineered therapy or pharmaceutical.
I’m sure that some other digital health companies and their backers will object to these ideas as unneeded restraints. It’s true that trading Big Tech’s free-for-all garage for Big Pharma’s meticulous laboratory will slow innovation and encourage some entrepreneurs and investors to seek more amenable markets.
Ultimately, though, raising the bar may be the only way that digital health can achieve its promise. Long-term investors could see returns precisely because patients will receive treatments proven to improve their health.
Forbes Business Council is the foremost growth and networking organization for business owners and leaders. Do I qualify?

- Editorial Standards
- Reprints & Permissions
Still accepting applications for online and hybrid programs!
- Skip to content
- Skip to search
- Accessibility Policy
- Report an Accessibility Issue
- Alumna transitions from pandemic frontlines to inspiring instructor
Elizabeth Levin-Sparenberg, MPH ’07, PhD ’16
Instructor, online mph in population and health sciences.
May 28, 2024
The University of Michigan School of Public Health has, for some time, built up a bustling virtual community, one that much of the residential student body has yet to experience.
If they had, like most of the graduate students in the online Master of Public Health (MPH) program, they’d be aware of a much loved presence in the online space: an instructor whose journey embodies the spirit of resilience, adaptability and unwavering commitment to public health.
Elizabeth Levin-Sparenburg, MPH ’07, PhD ’16, has been teaching exclusively in the online MPH program for two years. She’s become an inspiring figure among the online graduate cohorts and known for her compassion.
Her professional journey took an unexpected turn when the world was grappling with the challenges of the COVID-19 pandemic. With four young children at home, Levin-Sparenberg found herself at a crossroads. As the pandemic swept across the globe, she felt a calling to contribute her expertise to the frontline efforts.
Despite the immense challenges and uncertainties, Levin-Sparenberg made the decision to become a full-time epidemiologist, working tirelessly to combat the spread of the virus.
“Suddenly, we were in a worldwide pandemic and I thought, ‘This is what I've been training for my whole career,’” said Levin-Sparenberg, who has a Master of Public Health in Epidemiology and a PhD in Epidemiologic Science from Michigan Public Health. “I've got to get involved.”
Her transition to the frontline was met with both challenges and rewards.
Levin-Sparenberg found herself navigating the complexities of public health policymaking, community outreach and the delicate balance between science and public perception.
“We were all just working around the clock trying to kind of tame the spread and the effects of the pandemic,” she said.
I think everybody that was on the frontlines of the pandemic can tell you, the burnout is real.
Amidst the fog of the pandemic, an unexpected opportunity arose. A former professor reached out to Levin-Sparenberg with an offer to join the faculty at Michigan Public Health, teaching in the online MPH program.
For Levin-Sparenberg, it felt like a lifeline. Two years into the pandemic, the stress of the pandemic was taking its toll.
“I think everybody that was on the frontlines of the pandemic can tell you, the burnout is real,” she said.
The offer was a chance to shift her focus from crisis management to education, and so she went from the frontline to the classroom.
“While I was glad to put all my public health training in practice, it was stressful,” Levin-Sparenberg said. “Going from what were sometimes hostile interactions with the public—with COVID-19 being so politicized—and moving into a situation where everybody was on the side of public health, it was such a positive thing. The students are just eager to learn about public health and to go out and to make a difference.”
As an alumna of the Department of Epidemiology, Levin-Sparenberg was able to bring a unique perspective to her teaching, drawing from her own experiences as a student and graduate student instructor (GSI), and as a practitioner in the field.
Her journey from student to instructor has come full circle, allowing her to mentor and inspire the next generation of public health leaders.
“It's been interesting to see how the experience has evolved since I was a student,” she said. “And especially in teaching in the online classroom, it is just so different from when I did my studies.”
One of the hallmarks of Levin-Sparenberg’s teaching philosophy is her emphasis on work-life balance—a lesson she learned firsthand as a working mother juggling the demands of career and family.
Teaching exclusively online allows Levin-Sparenberg to integrate her personal life into her professional role. Her children often make cameo appearances during her lectures, offering students a glimpse into her world outside the classroom.
“I like my children to see that mommy is a scientist, that mommy works," Levin-Sparenberg said. “I want my students to see that my family is important to me, just like their families are important to them.
This job has allowed me to have a good work-life balance. I want my students to have that too.
“This job has allowed me to have a good work-life balance. I want my students to have that too. Especially if we believe in public health; we should care about our employees, our students— their whole package, their whole life.”
Levin-Sparenberg’s approach to teaching is rooted in empathy, understanding and flexibility. She recognizes that her students are not just learners but also professionals with diverse backgrounds and commitments. She strives to create a supportive learning environment where students feel valued, heard and empowered to succeed.
“It feels like I was in their shoes not very long ago,” she said. “I was so stressed out during my master’s and PhD programs. I always think, how can I make this enjoyable rather than stressful?”
“I want my students to learn, to build passion for public health and to feel supported every step of the way. If there's something causing unnecessary stress, I want to remove it. I want my students to thrive, not just survive.”
Levin-Sparenberg teaching in the virtual classroom.
In the online MPH program, Levin-Sparenberg supported the growth of a community of like-minded individuals dedicated to making a difference in the world. Through her teaching, she hopes to foster connections, facilitate learning and inspire positive change in the field of public health.
“These students are just so impressive with their knowledge, their ideas, how they’ve been involved in their own communities, their level of passion and activism,” she said. “They’re all doing so many amazing things and I get to learn and live vicariously through each one of them.”
As Levin-Sparenberg continues her journey as an instructor, she remains committed to her mission of building public health capacity, one student at a time. In an evolving landscape of public health, her story serves as a testament to the transformative power of education, the necessary resilience of those who serve others, and the enduring impact of community - however you access it.
- Learn more about the Online MPH program .
- Read more stories about students, alumni, faculty, and staff .
- Support research and engaged learning at the School of Public Health .
- Epidemiology
- Professional Development
Recent Posts
- Connecting with community through human-centered, public health lens
- Physical therapist aims for healing on a larger scale with online MPH
- Nurse practitioner overcomes burnout with public health education
What We’re Talking About
- Adolescent Health
- Air Quality
- Alternative Therapies
- Biostatistics
- Breastfeeding
- Child Health
- Chronic Disease
- Community Partnership
- Computational Epidemiology and Systems Modeling
- Disaster Relief
- Diversity Equity and Inclusion
- Engaged Learning
- Entrepreneurship
- Environmental Health
- Epidemiologic Science
- Epigenetics
- Field Notes
- First Generation Students
- Food Policy
- Food Safety
- General Epidemiology
- Global Health Epidemiology
- Global Public Health
- Graduation 2019
- HMP Executive Masters
- Health Behavior and Health Education
- Health Care
- Health Care Access
- Health Care Management
- Health Care Policy
- Health Communication
- Health Disparities
- Health Informatics
- Health for Men
- Health for Women
- Heart Disease
- Hospital Administration
- Hospital and Molecular Epidemiology
- Industrial Hygiene
- Infectious Disease
- Internships
- LGBT Health
- Maternal Health
- Mental Health
- Mobile Health
- Occupational and Environmental Epidemiology
- Pain Management
- Pharmaceuticals
- Precision Health
- Reproductive Health
- Scholarships
- Sexual Health
- Social Epidemiology
- Social Media
- Student Organizations
- Urban Health
- Urban Planning
- Value-Based Care
- Water Quality
- What Is Public Health?
Information For
- Prospective Students
- Current Students
- Alumni and Donors
- Community Partners and Employers
- About Public Health
- How Do I Apply?
- Departments
- Findings magazine
Student Resources
- Career Development
- Certificates
- The Heights Intranet
- Update Contact Info
- Report Website Feedback
Don't miss tomorrow's healthcare industry news
Let Healthcare Dive's free newsletter keep you informed, straight from your inbox.
- Daily Dive M-F
- Payer Weekly Every Wednesday
- IT Weekly Every Thursday

Digital health funding continues to stabilize in Q1: PitchBook
Startups raised $1.1 billion across 77 deals in the first quarter — far lower than pandemic-era highs, but consistent with recent quarters.

Dive Brief:
- Venture capital funding for digital health companies has stabilized after a major drop in investment coming out of the COVID-19 pandemic, according to a PitchBook report.
- Startups raised $1.1 billion across 77 deals in the first quarter, similar to the previous three quarters, according to the market research and data firm. However, deal value in the quarter declined nearly 27% year over year, while deal count fell more than 9%.
- Some sectors are still in flux. Digital therapeutics developers have struggled to receive reimbursement for their products, while Optum and Walmart have recently closed their telehealth businesses, Pitchbook said.
Dive Insight:
Digital health funding soared during the COVID-19 pandemic, with investors pouring a record $21 billion into startups in 2021 , according to venture capital firm and advisory Rock Health.
However, the sector began to cool down the following year, and investment fell back to pre-pandemic levels in 2023. Some digital health companies — even those that raised large amounts of capital , including through public offerings — shut down.
PitchBook’s latest report finds funding in the space has evened out at far lower levels compared with pandemic highs.
Digital health funding collapsed coming out of the COVID-19 pandemic
Down rounds, when a startup raises money at a lower valuation than previous rounds, haven’t been widely reported, according to the research firm. However, the sector has seen a rise in silent raises, or unlabeled rounds with existing investors.
Fewer than 20% of startups have reported a priced round within the past 18 months, so digital health valuations “should be considered outdated to an extent,” according to PitchBook.
The sector has also seen few digital health exits. The drought of initial public offerings continued in the first quarter, though the space did see some movement this summer with healthcare payments firm Waystar and precision medicine company Tempus AI going public.
However, these IPOs might not signal an immediate flood of digital health companies entering the public markets.
“Heading into 2024, we believed several digital health IPOs could be forthcoming; however, we now expect the highest quality startups to wait until 2025, as these companies often have balance sheets strong enough to weather the storm and may be comfortable letting others test the public markets first,” the report says.
Another exception to the exit drought in the first quarter was mental health app maker Twill, which was acquired by public chronic condition management company DarioHealth.
That type of deal — wherein a digital platform buys complementary assets to create a consolidated offering — is likely to continue going forward, according to PitchBook.
Consolidation among digital therapeutics companies, which have so far faced challenges building a stable reimbursement structure for their products, could be another driver of M&A, PitchBook said.
Some digital therapeutics developers have shut down, while Akili, which offers a video game treatment for ADHD, recently said it would go private — leaving no publicly traded digital therapeutics companies in the U.S.
Virtual care has also seen turbulence in recent months, with Walmart and Optum shuttering their telehealth businesses. Major public telehealth players like Teladoc Health and Amwell have seen their stock market performance wane as they struggle to boost their bottom lines.
“Still, there is meaningful evidence that telehealth has an overall positive impact on healthcare costs, and we still see a positive investment case for the next evolution of telehealth services with a focus on specialty telemedicine, [business-to-business] platforms, and hybrid-care models,” the report’s authors wrote.
Recommended Reading
- Healthcare payments firm Waystar plans $1B IPO By Emily Olsen • May 30, 2024
- ‘Hope is not a strategy’: Health startups short on cash staring down consolidation, investors say By Rebecca Pifer • Oct. 11, 2023
Healthcare Dive news delivered to your inbox
Get the free daily newsletter read by industry experts
- Select Newsletter: Daily Dive M-F
- Select Newsletter: Payer Weekly Every Wednesday
- Select Newsletter: IT Weekly Every Thursday
- Select user consent: By signing up to receive our newsletter, you agree to our Terms of Use and Privacy Policy . You can unsubscribe at anytime.

Editors' picks
How the spread of Catholic-owned healthcare facilities may complicate access to reproductive care
Catholic facilities must follow ethical and religious directives that say they can’t provide abortion or sterilization services and may not "promote or condone" contraceptives.
Almost half of nation's OB-GYN residents train in states poised to ban abortion
Physicians warn that the Supreme Court ruling will have a dire impact on training, ultimately affecting patient care.
Company Announcements

- Data breach at Geisinger may have exposed data from 1.2M patients By Emily Olsen
- Inside AI-driven medical coding
- Health tech startup Fabric acquires Walmart’s telehealth business By Emily Olsen
- Amwell to implement reverse stock split to avoid delisting By Emily Olsen

Graduate School of Business
- MBA in Health
- MBA Standard
- Middle Managers MBA
- Ateneo-Regis MBA
- Master in Entrepreneurship
- Master in Corporate Entrepreneurship
- Master in Entrepreneurship (Social Enterprise Development)
- Academic Policies
- General FAQ
About the Program
Designed for leaders of health service organizations who would like to explore new paradigms for taking on the opportunities and challenges of a rapidly transforming public and private health sector
The increasing demands of our rapidly expanding population, the growing complexities of health care services, and the challenges of globalization have made it even more critical for us to develop a new brand of leadership for health care institutions, both public and private.
This new leader/manager should be equipped with the appropriate managerial skills and attitudes to efficiently and effectively direct scarce resources to help build a health care delivery system that is responsive to the needs of our people in terms of availability, accessibility, and affordability.
The MBA in Health program is designed for leaders of health service organizations who find themselves managing their organizations without having had the benefit of previous formal management training. This degree program offers a new model for training leaders for the health care industry by providing them not just with the necessary business frameworks and tools, but also a broad understanding of the challenges and opportunities posed by this rapidly transforming sector.
Students enrolled in the program cover a broad spectrum of professional and educational backgrounds, including physicians, nurses and allied health professionals, as well as accountants and engineers. Its interactive and student-centered program design enables students to learn from each other as well as from a faculty lineup that includes many distinguished medical and business practitioners as well as senior academics.

APPLY NOW
Distinctive Features
- Specialized program providing management education to professionals who would like to pursue careers leading to top management positions in health care organizations
- Modular approach, with specified daily learning outcomes, activities and assignment
- Focused not just on theories and techniques but also on values and personal transformation
- Requires a total of 14 courses (42 units in total) made up of 12 core courses and 2 electiveS
- Non-thesis program, with an integrating Strategic Management paper as the terminal requirement
Program Delivery
- Cohort-based part-time program designed for working professionals
- The program follows a trimestral schedule and the entire program can be completed in seven trimesters of 14 weeks each, or a total of two years and 4 months.
- Each student takes two classes per trimester; each class meets three hours per week for a total of 14 weeks All classes are delivered on Saturdays
- Student-centered focus requires students to take greater responsibility for their own learning
- Workplace-based approach will require students to draw on their personal and professional experiences, and apply their learnings to their work even as they undergo the program
- Faculty are facilitators of learning rather than lecturers
- Maximum of 25 students per class
- The MBA in Health Program is offered at our main campus in Rockwell Center, Makati City, and our satellite campus in Clark Field, Pampanga

The MBA in Health Program Curriculum
General Description
- The MBA in Health is offered on a trimestral basis. Class work is one (1) day a week (Saturdays) with two courses of three hours each per session for fourteen (14) sessions per trimester.
- The program is completed in seven (7) consecutive trimesters or a total of twenty eight (28) months. Students with a fixed load of six (6) units per trimester are able to complete the academic requirements within this period. Students who develop their strategic management paper early during their course work can graduate by the last (7th) trimester.
- The maximum load per trimester is two (2) courses. Additional load requires approval from the director of MBAH.
| Major Course | 12 units |
| Core Courses in Management | 21 units |
| Electives | 6 units |
| Integrating Course | 3 units |
- The required health care core courses serve as foundation and context by which the student is challenged to understand and apply the structure and operation of health care systems. The major MBA courses give the student a solid mastery of management fundamentals.
- Attendance in all courses is required. Absence from class for a total of 20% of sessions per course may be considered as excused absences.
- Provide factual and practical knowledge of the health care field
- Strengthen the student’s faculties of analysis, problem-solving, and decision-making
- Challenge the student’s initiative and self-discipline
- Encourage independent thought, intensity of purpose, freedom from bias, thoroughness of inquiry, originality and creativity
- Promote group interaction and cooperation, and
- Foster a high sense of professional responsibility.
| Principles and Concepts in Health and Development | MHPCHDEV | 3 |
| Managerial Epidemiology | MBEPIDEM | 3 |
| Health, Culture, and Society | MHCULSOC | 3 |
| Health Economics for Managers | MBHEAECO | 3 |
| Ethics in Health Care | MBETHICS | 3 |
| Dynamics of Leadership | MHDYLEAD | 3 |
| Principles and Dynamics of Management | MHMANPRI | 3 |
| Marketing Management | MBMARKMA | 3 |
| Financial Management | MHFINMAN | 3 |
| Operations Management | MHOPEMAN | 3 |
| Human Resource Management | MBHUMRES | 3 |
| 3. Electives (choose 2) | ||
| Health Informatics | MBHINFO | 3 |
| MBENTREP | 3 | |
| 4. Integrating Course | ||
| Strategic Management | MBSTRAMA | 3 |
The MBA in Health Program Course Sequence

Course Descriptions
- Principles and Concepts in Health and Development (MHPCHDEV) This is a core course in the MBA-Health program that grounds the students on the Philippine health system. Students are introduced to the concepts of health and development and to the workings of the health system. Elements of the health system are analyzed and stakeholders identified. Students are asked to look at how these elements and stakeholders interact, either in synergy or in opposition to each other, as the health system moves towards improving the health of the people.The course stresses the need for a more rational, coherent and enlightened understanding of the workings of the health system so that the fragmentation and disconnectedness that pervade the current system can be reformed by influencing the way people think, feel and behave about health.Students are also asked to confront the roles they play, as health professionals representing various sectors and disciplines, in this process of transformation. The end goal of the course is to provide the students with a relevant context for the application of the competencies they will learn as leaders and managers in the health sector.
- Managerial Epidemiology (MBEPIDEM) This course is an introduction to the use of epidemiology in management and decision-making for the graduate student. The student will learn to use an epidemiological model for the delivery of health care services, methods for measuring need and health, analytic approaches to decision-making when evaluating the impacts of health care programs and policies, and how to apply epidemiology in program planning and selected specialty areas.
- Health, Culture and Society (MHCULSOC) The course will introduce perspectives from the social sciences and their possible applications for health care, particularly the development of cultural competence. Using a cross-cultural survey of different medical systems- with emphases on those found in the Philippines-the course will underscore the need to look at the diversity of meanings, beliefs, symbols and rituals around health care, both “western” and “non-western”. The course will also look at the ways different societies organize themselves for health care in the popular, folk and professional sectors, often in response to challenges posed by the environment. Finally, the course will look at how macro structures and institutions- locally and globally-shape health care systems in different social and historical settings.
- Health Economics for Managers (MBHEAECO) The course is an introduction to health economics or the use of economics in the health sector. There are two branches of health economics: micro and macro. The former focuses on economic behavior of individuals and firms while the latter focuses on system structure and complex interactions between the structural components that affect national health system outcomes. Both branches are important in understanding health care policies and management decisions and the course will cover both.Economic theory and analysis influence health decision-making and the course will provide the students with an economic framework to understand how the Philippine health system is structured. The course will also deal with the issue of allocation of limited health care resources. Further, the conduct of economic evaluation of healthcare interventions will be deliberated in class.
The course will discuss the foundations of ethics in general and of health care ethics in particular. It will also attempt to help students improve their ethical decision making by presenting a model for ethical reasoning that may be used in analyzing dilemmas confronting health care managers.
- Dynamics of Leadership (MHDYLEAD) This course aims to introduce the students to a depth of thinking about individuals and collective patterns of leadership practices called for in this Master’s program. Designed as an interactive and reflective course, the learning interventions will focus on guiding the students to reflectively process or understand leadership patterns and dynamics as applied in their personal and professional lives. Reflective/critical thinking and ethics based reasoning and decision-making are emphasized.
- Principles and Dynamics of Management (MHPRIMAN) The course provides learners with an understanding of the role of management and the analytical tools to competently cope with the challenges facing today’s management. Business enterprises and non-profit organizations operate within a complex and rapidly changing global environment. The field of management is undergoing a revolution. Globalization, economic deregulation, trade liberalization, technological advancement and the widening of the urban poor have created new threats and opportunities confronting managers. This course is designed to familiarize learners with the accepted management standards, procedures and techniques employed by corporate, business and functional level managers.
- Marketing Management (MBMARKMA) The course is designed to provide learners with a formal training on the fundamental concepts and practices of Marketing in the context of the new economy. It will also focus on the formulation and implementation of marketing strategies in the areas of research, products and services, pricing, distribution, advertising and promotion, market analysis, alternative approaches to competition, brand building, and revenue-generating activities. These strategies, to serve their purpose, are best aligned to the business environment, hyper competition, digitalized technologies, the empowered consumer, and the country’s widening base of the poor. This course will likewise help learners gain a good understanding of administrative processes where marketing plays a central role in the game of demand creation and customer satisfaction. Finally, everyone will get to appreciate, by the latter part of the 15 sessions, that Marketing is indeed a powerful contributor to nation building.
- Financial Management (MHFINMAN) This course deals with decision making under uncertainty for corporate financial management designed particularly for health care institutions. Critical evaluation of concepts is emphasized to assess their usefulness in practical business situations. Problem-solving methodology is used to illustrate the theories and tools in financial decision making including the use of health demographics to help with the financial evaluation studies.More importantly, this course tackles the ethical issues and dilemmas faced by the financial manager in his day-to-day work as chief financial officer for a healthcare institution with a very important primary mission of service to its patients. The students will be taught how to resolve these ethical dilemmas.
- Operations Management (MHOPEMAN) The course covers in-depth discussion/study of specific Operations Management (OM) philosophies, concepts, trends, tools and techniques to highlight the importance of OM in a manufacturing or service organization’s pursuit of strategic goals and objectives. It focuses on strategic and tactical issues covering quality management, process management, and supply chain management.While providing students with technical and quantitative tools, it will focus more on the managerial aspect of operations, as well as on the ethical and social implications of OM decisions.
- Human Resource Management (MBHUMRES) Management is generally about making other people produce the results that one desires. An organization’s human resources is therefore of paramount value, being responsible for producing the outputs and outcomes that the organization is designed to do. The course emphasizes the need for the alignment of human resource management policies, practices, and programs with the goals, strategies, and values of the organization. It presents tools for enabling the learner to understand the most vital resource of the organization-its people.It provides a fresh perspective on the role of Human Resource Management and the function of the Human Resource Management Officer as an agent of change, in partnership with top management. The course describes how, together, they can build one of the most critical sources of sustainable competitive advantage-an organization whose design, culture, and people are aligned with strategy and values.It addresses the need for functional, if not high performing human resource management systems, such as recruitment and selection, induction, compensation and benefits, performance management, rewards and incentives, learning and development, retention, and work-force relationships from a strategic perspective. A discussion on the need to build a culture that will encourage high levels of productivity is also included.
- Health Informatics (MBHINFO) The course will provide students concepts and tools in managing technology in health. The management of information has become a key competitive advantage among healthcare enterprises. New technologies such as the Internet and mobile have given rise to new channels of delivery.In comparison to other health informatics courses, this course was developed particularly with a management perspective. This course will provide an overview of health informatics, public health informatics. Key concepts in hospital information systems such as electronic health records and clinical decision support will also discussed.
- Entrepreneurship (MBENTREP) Entrepreneurship has traditionally been understood as simply starting up a new business outside of the corporate setting. The course addresses the problem that a start-up entrepreneur faces – having a business just like a hundred other businesses that are competing for a shrinking market. At the same time, the heads of big businesses, awash with cash and basking in past success think nothing can go wrong with a new venture, become lax, only to find their sales and cash flow diminishing.The course focuses not only on new businesses, but also on existing businesses that are faced with a changing or changed environment where industries change, customer needs and demands change, and the tide of the economy can also turn against the business. The entrepreneur must know how to rejuvenate products, processes, markets, and the way one does business.
- Strategic Management (MBSTRAMA) The course serves as the capstone course for the MBA program. It aims to enable the learners develop and implement strategic cross-functional decisions towards the attainment of their organizations’ vision, mission and objectives using strategic management principles and integrating knowledge and skills acquired by the learners from the other MBA courses.The learners will apply the strategic management process consisting of strategy formulation, strategy implementation and strategy evaluation, as well as the various analytical frameworks and strategy formulation tools that can aid them in strategic decision making. Through this course, the learners’ strategic thinking capability is expected to be strengthened as they are made to critically analyze and integrate information about their companies’ external and internal environment in the local and global context, and to use this in formulating and implementing innovative strategies that can help their companies build a sustainable competitive advantage. The learners will likewise be made to understand the different strategy choices and to evaluate strategic management issues and concepts that are important to managing in today’s global environment. This course also aims to promote among its learners ethical business decisions, the practice of corporate social responsibility and making a contribution towards nation building.
Contact Details
- Director: Ayedee Ace M. Domingo, II, MD, MBA (8899.7691 – 96 loc. 2209) [email protected]
- Contact Person: Andrew Ferrer (8899.4589, 8899.7691 -96 loc. 2211) [email protected]
Ateneo de Manila Graduate School of Business
Ateneo de Manila University Rockwell Campus
#20 Rockwell Drive, Barangay Poblacion
1201 Makati City
Philippines
Telephone +63 2 8899 7691 ext 2206 / 2207
+63 919 078 8565 (Admissions)
Modal title

- For the Media
- Open Records
- Division of Marketing & Communications

Samsung, UGA to develop new digital health experience

Samsung’s upcoming Galaxy Watch combines data from UGA study and AI technologies
Why do we feel tired and sluggish one day and filled with energy the next?
While there are many factors when it comes to measuring energy levels, users of the upcoming Galaxy Watch may come closer to answering these questions based on their personalized Energy Score, a collaborative measurement developed by Samsung and the University of Georgia.
To improve the digital health care experience, Samsung Research collaborated with Patrick O’Connor, a professor in the Mary Frances Early College of Education’s Department of Kinesiology, to design a new measurement that records energy as a daily score .
While creating an objective measurement of energy is difficult, O’Connor’s extensive research into exercise and psychobiology provides a foundation for identifying relationships between cognitive and physical capacity—two concepts factored into calculating the Energy Score.
Energy is required to sustain both physical and mental activities, and while most existing measurements of energy rely solely on physical aspects, Samsung’s Energy Score also factors in assessments that can influence mental performance such as the amount of sleep an individual obtains at night, as well as its quality based on sensors in the watch.
“The decision on what factors to include in the energy score was influenced by the accuracy of watch sensors combined with findings of our team’s research conducted with the watch and a careful consideration of which variables have been adequately linked to mental or physical performance in the scientific literature,” said O’Connor.
For the study, O’Connor’s team looked at not only cognitive and physical performance in correlation to energy, but also quantified daily variations in several metrics measured by the Galaxy Watch, including physical activity, sleep, heart rate and heart rate variability—all of which are considered when calculating the Energy Score. Heart rate variability measures variation in the time between heart beats, measured in milliseconds.
His research team conducted experiments that included cognitive tests as well as energy and fatigue symptom self-reports, which found a significant correlation between the Energy Scores generated by Samsung’s models and clinical data collected by O’Connor’s team.
“From a scientific perspective, the Energy Score reflects predicted variation in the ability to perform brief cognitive tests of attention across a day based on objective information obtained from the smart device sensors across multiple prior days,” said O’Connor.
The energy score estimates the amount of activity one can sustain relative to a person’s total capacity, both physically and mentally. If people substantially exceed their typical physical or mental load on one day, their energy is reduced in the short term.
For instance, if a person typically exercises at low intensity for 30 minutes daily but decides to engage in moderate intensity for more than an hour one day, the wearer’s Energy Score is expected to drop the following day.
However, regular exercise with appropriate rest can gradually enhance overall capacity, potentially resulting in a higher Energy Score for the same workout intensity over time.
In contrast, sleep data primarily contributes to mental capacity and is measured by the duration, timing and consistency of sleep and wake times, as well as how quickly watch wearers fall asleep.
Heart rate during sleep and heart rate variability during sleep can reflect both physical and mental capacities and can forecast energy by comparing recent measurements to long-term data trends, with the precision of predictions enhanced by analyzing both stable heart rate and heart rate variability during sleep.
In addition to UGA’s research, Samsung employed AI technologies that use factors like age and gender to determine optimal weights for an individual Energy Score. Ultimately, brief daily health suggestions are provided to users based on each day’s Energy Score.
O’Connor’s research — along with Samsung’s AI technologies — aims to enhance the accuracy of each individual Energy Score.
“Through our collaboration with professor O’Connor, we were able to address this challenge in a scientifically meaningful way,” said Lee Yunsu, head of the data intelligence team at Samsung Research. “We will continue to devote our efforts to developing data and AI technologies to ensure that Samsung’s various devices are used more extensively to enhance users’ healthy lives.”
You may also like

Medical student learned to overcome the odds

UGA named best value college by The Princeton Review

Morehead Honors College named No. 1 in the nation

Multidrug-resistant fungi found in commercial soil…

Experience UGA wins 2024 ITGA Presidential Excellence…

Graduate Certificate in Crisis, Risk, and Disaster…

- FlashLine Login
- Phone Directory
- Maps & Directions
- About Overview
- Dean's Message
- Mission & Goals
- Touch Point Online Magazine
- 750+ Clinical Partners
- Simulation Lab
- #IAmKentNursing Blog
- Academics Overview
- Accelerated Second Degree BSN (ABSN)
- Mission, Goals, & Program Outcomes
- LPN & Allied Health to BSN Program
- Nursing - M.S.N.
- Financial Aid
- RN-to-BSN Online Program
- Request Information
- MSN-MBA Dual Degree
- Post-Master's Certificates
- Doctor of Nursing Practice (DNP)
- Doctor of Philosophy in Nursing (Ph.D.)
- Online Degrees & Certificates
- Information Webinars & Sessions
- Students Overview
- Why Nursing?
- Student Advisors
- Student Handbooks
- Nursing Library Guide
- Activities and Organizations
- Study Abroad
- Career Resources and Opportunities
- Apply for Graduation
- BSN Convocation/Pinning
- Graduate Convocation/Pinning
- Faculty & Staff Overview
- Faculty & Staff Directory
- Emeriti Faculty
- Faculty Handbook
- Become a Preceptor
- Nursing Research Overview
- Nursing Research Interest Form
- Areas of Expertise
- Our Researchers & Scholars
- Resource Guide for Nurse Researchers
- CNR News & Events
- About the Center for Nursing Research
- Support the College
Spring 2024 Publications, Presentations and Recognitions
- Share on Facebook
- Share on Twitter
- " class="social-sharing-google" title="Share on Google+"> Share on Google+
- Share on LinkedIn
- Share by Email
The College of Nursing is proud to recognize the achievements of our talented alumni, students, faculty and staff. From college innovations and presentation to new grant awards and published articles, the past few months have been very busy. Please join us in congratulating the following individuals on their recent accomplishments.
Faculty Recognitions
Versie Johnson-Mallard , PhD, RN, FAAN, served as invited speaker for the Health Committee of the Florida A&M University National Alumni Association, Tampa Chapter which will host the National Convention in Tampa in June.
Stacy Miner , PhD, RN, CCRP, was recently nominated for the 2023-2024 Excellence in Research Mentoring Award given by the Kent State Office of Student Research.
Stacy Miner , PhD, RN, CCRP, was recognized by University Hospitals (UH) for her contributions to clinical research as part of UH’s Diversity Month and National Minority Health Month #FacesOfResearchUH initiative.
Amy Petrinec , PhD, RN, was recently nominated for the 2023-2024 Excellence in Research Mentoring Award given by the KSU Office of Student Research.
Janet Reed, PhD, RN, CMSRN, had her abstract, Students’ Fears of the Nursing Profession Through AI-Generated Artis-tic Images , selected as a Distinguished Abstract for the Midwest Nursing Research Society (MNRS) 2024 Annual Research Conference.
Pam Stephenson , PhD, RN, and Dana Hansen , PhD, APRN, ACHPN, FPCN, were interviewed for the article, “Patients Want Spiritual Support—But Can Clinicians Provide It?” published in Medical Ethics Advisor, 30 (2), 29-30. https://www.reliasmedia.com/articles/patients-want-spiritual-support-bu…
Pam Stephenson , PhD, RN, and Dana Hansen , PhD, APRN, ACHPN, FPCN, were interviewed in a recent article published in Nurse Journal titled , “Study: Nursing Student Beliefs About Death and Dying Can Affect End-of-Life Care.” _ https://nursejournal.org/articles/nursing-stu-dents-end-of-life-care/
Cindy Wilk , PhD, APRN-CNS, CCRN, CNE, was recently named a Non-Tenure Track Provost’s Advisory Council (NPAC) Winebrenner Professional Development Excellence Award recipient.
Scientific & Scholarly Presentations
Dodson, T., & Reed, J. M. (2024, March). Expert modeling videos for use in nursing curriculum . Poster presentation for the Ohio League for Nursing Education Summit, Columbus, OH.
Johnson-Mallard, J . (2024, April). What research dollars really matter ? Keynote address for the School of Nursing Research Day, University of Nevada, Las Vegas (UNLV).
Hansen, D. (2024, Feb). Comfort and confidence in communication and collaboration in nursing and medical students: A convergent mixed methods study . Presentation for the Midwest Nursing Research Society Annual Research Conference, Minneapolis, MN.
Petrinec, A., Hansen, D. , & Hebeshy, M. (2024, Feb). Post-intensive care syndrome-family symptoms during the COVID Pandemic: Comparison of two web-based recruitment methods. Presentation for the Midwest Nursing Research Society Annual Research Conference, Minneapolis, MN.
Reed, J. M. (2024, Jan). Generative AI images for use in patient storytelling in pre-simulation . Presentation for the International Meeting on Simulation in Healthcare (IMSH), Society for Simulation in Healthcare, San Diego, CA.
Reed, J. M. (2024, March) . Generative artificial intelligence for image creation as a pedagogical strategy. Podium presentation for the Ohio League for Nursing Education Summit, Columbus, OH, March 22, 20224.
Reed, J. M. (2024, Feb). Student fears of the nursing profession through AI-generated artistic images . Presentation for the Midwest Nursing Research Society (MNRS) 2024 Annual Research Conference. Minneapolis, MN.
Reed, J. M. (2024, March). Using AI image generators to imagine and visualize in education . Presentation for E2 Elevated: Tech Forward Virtual Conference, Kent State University, Kent, OH.
Wang, Y ., Chuang, H., Tien, H., & Chang, C. (2024, Feb). Demographics, disease characteristics, and caregiver resource-fulness for children with type 1 diabetes . Poster discussion session and poster presentation for the 48th Annual Re-search Conference of the Midwest Nursing Research Society, Minneapolis, MN.
Wilk, C. , Cummins, M., & Plata, A. (2024, March). Paving an innovative path for the CNS intern: Bridging the gap between education and practice. Presentation for the National Association of Clinical Nurse Specialists 2024 Annual Conference, New Orleans, LA.
Faculty Publications
Cleveland, K. , Rudisill, P., Vander Horst, A., & Benson, L. (April 2024). Getting nurses on boards: Why health care organizations should consider adding nurses to their boards. American Hospital Association Trustee Insights .
Eades-Brown, N.T., Oguntoye, A.O., Aldossary, D., Ezenwa, M.O., Duckworth, L., Dede, D., Johnson-Mallard, V. , Yao, Y., Gallo, A., and Wilkie, D.J., 2023. Adherence to a reproductive health intervention for young adults with sickle cell. Journal of the American Association of Nurse Practitioners , 10-1097. doi:10.1097/JXX.0000000000000997. [online ahead of print]
Kosar, C., & Cleveland, K. (2024). NCPD Tests: Navigating the litigation experience. Orthopaedic Nursing 43 (2), E7. doi.10.1097/NOR.0000000000001021
Woo, J, Kim, J. W., Jarzembak, J., James, A., Biggs, J., Clements, R., Dunlosky, J., & Kim, K. (2024). Comparative design and analysis of multimodal VR simulations for IV needle insertion training.
Reed, J. M. (2024). Students’ fears of the nursing profession through AI-generated artistic images. Western Journal of Nursing Research, 46 (1), suppl, 1S-57S. https://doi.org/10.1177/01939459241233357
Reed, J. M. , Ferdig, R. E., Karpinksi, A. C., & Zsido, A. (2024). A short form for measuring anxiety in nursing education. Journal of Nursing Measurement . doi.10.1891/JNM-2022-0131 [online ahead of print]
Wilk, C., & Petrinec, A. (2024). Psychometric evaluation of the Family Willingness for Caregiving Scale (FWCS). American Journal of Critical Care, 33(3), 192-201. https://doi.org/10.4037/ajcc2024809
New Grant Awards
Drs. Janet Reed, Tracy Dodson, Joel Hughes, and Amy Petrinec received a LaunchPad Award for their project, HARMONEE- Harnessing AI Resources for Mental Health Outcomes and Nurturing Empathy in Education , from the Kent State Healthy Communities Research Institute.
Dr. Janet Reed is part of the research team (Kenne, D. (PI), Laurene, K. (PI), Clements, R., Gandolfi, E, Reed, J., & Arrington, S.) awarded a Bettering Communities Grant Award by the Kent State University Research Council, the Anti-Racism and Equity Institute, the Environmental Sci-ence and Design Research Institute, and the Healthy Com-munities Research Institute for their project, Creating an Augmented Reality Digital Health Hub to Improve HIV/AIDS Resource Support for LGBTQ+ Individuals in Akron, Ohio .
Student Research
DNP Defenses: The following students defended their scholarly projects and graduated with their DNP:
Santhi Avula , Compassion Fatigue and Satisfaction Among Nurses at a State Psychiatric Hospital: An Opportunity to Edu-cate. (Dr. Andrea Warner Stidham, Chair; Drs. Debra Cifani and James Tudhope, committee members)
Alisha Lickwar , Screening for Gestational Diabetes at the First Prenatal Visit: A Quality Improvement Project (Dr. Marilyn Nibling, Chair; Drs. Karen Mascolo and Denise Pacholski, committee members)
Jessica Miller , Enhancing Perioperative Care: Elevating Anesthesia Providers' Knowledge and Implementation of Multi- Modal Therapy for Post-operative Nausea and Vomiting (PONV) Management in High-Risk Patients (Dr. Karen Mascolo, Chair; Drs. Jo Dowell and Lisa Onesko, committee members).
Jennifer Ramsey , Barriers to Care: A Quality Improvement Project to Increase Attendance to the Developmental Follow-Up Clinic (Dr. Marilyn Nibling, Chair; Drs. Lisa Onesko and Gina Severino, committee members)
BSN Honors Student Defenses
Wayne Nieh defended his Honors thesis, Family Presence During Resuscitation: A Descriptive Study of Nursing Students. Wayne was mentored by Dr. Amy Petrinec.
Mary Grace Vavruska defended her Honors thesis, Food Allergies in College Students: Knowledge, Symptom Management, and Response Times . Mary was mentored by Dr. Jo Dowell .
Student Presentations
Ramsey, J. (2023, October). A quality improvement project to increase attendance to the developmental follow-up clinic. Poster presentation for the American Academy of Pediatrics National Conference, Washington, D. C.
Nieh, W. (2024, April). Family presence during resuscitation: A descriptive study of nursing students. Poster presentation for the 132nd Ohio Academy of Science Annual Meeting, Kent State University, Kent, OH.
Nieh, W. (2024, April). Family presence during resuscitation: A descriptive study of nursing students. Presentation for Sigma Theta Tau Collaboration with Case Western Re-serve University, Ursuline College, Kent State University, and the University of Akron, Kent, OH.
Nieh, W., & Petrinec, A. ( 2024, February). Family presence during resuscitation: A descriptive study of nursing students. Poster presentation for the Mid-west Nursing Research Society Annual Research Conference, Minneapolis, MN.
The following students gave poster presentations for the Undergraduate Research Symposium on Research, Scholarship and Creative Endeavors, April 5, 2024:
**First-place award**: Wayne Nieh , Family presence during resuscitation: A descriptive study of nursing students. Mentor: Dr. Amy Petrinec
Cunion, Mallory. , Graves, A., Bennett, T., Apple, J., Toby Gbloguidi, T., & Bennett, R. The better bathroom: Ensuring safety & accountability. Mentor: Denmarie Fairbanks
Vavruska, Mary Grace . Food allergies in college students: Knowledge, symptom management, and response times. Mentor: Dr. Jo Dowell
The following students gave presentations for the National Association of Clinical Nurse Specialists 2024 Annual Conference, New Orleans, LA in March:
Plata, A. CNS Intern: Leading the way to becoming part of the next generation of CNSs. [left]
Plata, A. CNS Intern + EBP + Lean Six Sigma = Nurse Driven Telemetry Discontinuation Protocol
Wilk, C., Cummins, M., & Plata, A. Paving an Innovative Path for the CNS Intern: Bridging the Gap Between Education and Practice
Shafer, K. Use Of Visual Management to Improve Pain Reassessment by Medical/Surgical Nurses: A Quality Improvement Project
Alumni Loni Adams , MSN, MBA, RN, CCRN, CCTC and Jennifer Katlen, MEd, MSN, APRN, ACNS-BC, CCRN, GERO-BC, gave two podium presentations: Understanding the Pharmacology of Lung Transplant Patients and Implementing CNS-Led Ethics Rounds to Build Moral Resiliency and Address Healthcare Disparities.
- College of Nursing
- Center for Nursing Research
Related Articles
Street address, mailing address.
- 330-672-3000
- [email protected]
- Latest News
- Kent State Kent Campus - linkedin
- Kent State Kent Campus - snapchat
- Kent State Kent Campus - pinterest
- Kent State Kent Campus - facebook
- Kent State Kent Campus - twitter
- Kent State Kent Campus - youtube
- Kent State Kent Campus - instagram
- Accessibility
- Annual Security Reports
- Emergency Information
- For Our Alumni
- For the Media
- Health Services
- Jobs & Employment
- Privacy Statement
- HEERF CARES/CRRSAA/ARP Act Reporting and Disclosure
- Website Feedback
- Moscow Oblast
- »
- Elektrostal
State Housing Inspectorate of the Moscow Region
Phone 8 (496) 575-02-20 8 (496) 575-02-20
Phone 8 (496) 511-20-80 8 (496) 511-20-80
Public administration near State Housing Inspectorate of the Moscow Region

COMMENTS
A hub for digital health research and teaching across academia, industry, health systems, and government agencies. It aims to harness digital technologies to improve health and health care, especially in primary care and public health.
Learn how to apply your research skills to digital health, a field that uses technology to enhance healthcare and medicine. Explore the course structure, admission requirements, career pathways and interdisciplinary networks at RMIT.
Digital health refers to the development and use of digital technologies—which includes m/eHealth, health informatics, telemedicine, data analytics, big data, artificial intelligence—utilized in and throughout health systems to improve health. ... DrPH, PhD). This certificate is brought to you by the Center for Global Digital Health ...
Secure AI-enhanced Policy Framework for Digital Health Data. Kingston University Faculty of Engineering, Computing and the Environment. This proposal is part of the Data-mdapps project which is a collaboration between Kingston University and the WHO European Office for the Prevention and Control of Noncommunicable Diseases (NCD Office) and ...
Join our Digital Health and Care PhD programme to become part of a new generation of innovators involved in building and developing apps, wearables, smart homes and other digital technologies. Together, these technologies are helping to support health professionals in their decision-making and empowering patients in managing their own health ...
Learn how digital technologies can address critical pain points in health care and explore the opportunities and difficulties of bringing them to market. This online course is offered by Harvard Business School Online and Harvard Medical School and can be taken for credit or verification.
Doctoral Student (Ph.D.) in Digital Health: Machine Learning in Medical Care May 2021 - April 2024. We are looking for a highly motivated computer science Master's graduate to fill the project-funded open position on the development and application of machine learning methods in medical care.
This scholarship is available to eligible domestic candidates for direct entry into a 3-year PhD program. The scholarship is comprised of a Tuition Fee Offset and a Living Allowance Stipend. The value and tenure of the domestic scholarship at a full-time stipend rate is $28,092 per annum (in 2020, tax exempt for up to 3 years - indexed annually).
MSc Digital Health. Find out about the University of Bristol's MSc in Digital Health, including structure, entry requirements and career prospects. ... PhD Digital Health and Care. Modes of study Full-time Awards available PhD. Research postgraduate programme. PhD Disability Studies. Modes of study Full-time, Part-time
Digital Health Design & Clinical Informatics. Under the aegis of the Center for Healthcare Innovation and Delivery Science, the Healthcare Innovation Bridging Research, Informatics, and Design (HiBRID) Lab at NYU Langone assesses how digital health innovation can be used to improve healthcare delivery and patient care.
The future of health care is digital. Taught by Harvard Medical School faculty, this Harvard Online course explores the opportunities and difficulties facing widespread adoption of digital technologies in the US health care system and explores innovative frameworks to think strategically about implementing digital transformation in your ...
The series is co-hosted by the Berkman Klein Center for Internet & Society, and the Petrie-Flom Center for Health Law Policy, Biotechnology, and Bioethics. The goal of the series is to discuss ongoing research in this research area, share new developments, identify opportunities for collaboration, and explore the digital health ecosystem more ...
Being part of GLIDHE is an opportunity to build a community to generate exciting new ideas in digital health and wellbeing, to improve the health of the world. Please email expressions of interest in a PhD scholarship to: Lesley Payne, GLIDHE Lead [email protected] Useful Links. Bupa Global Institute for Digital Health Excellence
Institute of AI for Digital Health. 402 E 67th St. New York, NY 10065. [email protected]. Follow @WCM_AIDH on Twitter. Our Location.
Advancing Diagnosis and Treatment. Research shows that a significant proportion of health spending is attributed to chronic diseases, with individuals experiencing multiple comorbidities accounting for a disproportionate share of expenditures (Buttorff et al., 2017).Although additional research is necessary, a recent review concluded that self-management as part of a treatment program for ...
Junior council . The Digital Health research program has installed a Junior Council. Ambitious post-docs and PhD-candidates foreseeing a future in digital health provide the Program Leaders and Program Council with solicited and unsolicited advice, may initiate independent activities under the umbrella of Digital Health after consultation of and in good collaboration with Program Leaders to ...
Fundamentals of Digital Health is a fully-online credential exploring the intersection between health and technology. You'll be kept up-to-date with the latest technology and digital trends in healthcare, and discover how to apply them in your workplace. It's designed specifically for clinicians, allied health practitioners, technicians or ...
The World Health Organisation (WHO) advocates Digital Health Technologies (DHTs) to advance population health 1.Digital health can be defined as the use of information and communication ...
Graduate Certificate in Digital Health and Data Science. Back to search. MADIHDSC1000. What you'll study. Our Master of Digital Health and Data Science is co-designed and co-taught by the School of Computer Science in the Faculty of Engineering, and Biomedical Informatics and Digital Health in the Faculty of Medicine and Health. ...
Find the list of all universities for PHD Studies with our interactive university search tool. Use the filter to list universities by subject, location, program type or study level. ... Gender and Diversity Finance Finance Food Science General Business Genetics Geography Geology Geophysics Health/Healthcare Healthcare History Hospitality and ...
As a PhD student, you can participate in a voluntary benefits program to purchase a discounted legal services plan. You can enroll during annual enrollment (7/1 - 9/15 each year). The MetLife Legal Plan gives you access to a nationwide network of more than 12,000 attorneys, to help you and your dependents with vital legal matters such as ...
You can deploy skills you develop as a grad student and postdoc in a variety of careers, including working for a start-up or founding your own, Chris Smith writes. Innovation has become a hot topic in economic circles over the past few years. In March 2022, the United States' National Science Foundation created its first new directorate in over 30 years: Technology, Innovation and ...
Venture investments into digital health fell to $4.6 billion in 2023 from $17.7 billion in 2021. As of June 10, 2024, S&P's index of digital health stocks is down 70% from its peak in January 2021.
Liz Levin-Sparenberg is an instructor, and alumna, at the University of Michigan School of Public Health, who transitioned from the pandemic frontlines to teaching in the online MPH program. Learn how her personal experiences helped shape her unique approach to education, fostering a supportive community of future public health leaders in the digital classroom.
Digital health funding soared during the COVID-19 pandemic, with investors pouring a record $21 billion into startups in 2021, according to venture capital firm and advisory Rock Health.
Principles and Concepts in Health and Development (MHPCHDEV) This is a core course in the MBA-Health program that grounds the students on the Philippine health system. Students are introduced to the concepts of health and development and to the workings of the health system. Elements of the health system are analyzed and stakeholders identified.
To improve the digital health care experience, Samsung Research collaborated with Patrick O'Connor, a professor in the Mary Frances Early College of Education's Department of Kinesiology, to design a new measurement that records energy as a daily score.
Please join us in congratulating the following individuals on their recent accomplishments.Faculty RecognitionsVersie Johnson-Mallard, PhD, RN, FAAN, served as invited speaker for the Health Committee of the Florida A&M University National Alumni Association, Tampa Chapter which will host the National Convention in Tampa in June.Stacy Miner ...
State Housing Inspectorate of the Moscow Region Elektrostal postal code 144009. See Google profile, Hours, Phone, Website and more for this business. 2.0 Cybo Score. Review on Cybo.
Top Dzerzhinsky Landmarks: See reviews and photos of sights to see in Dzerzhinsky, Russia on Tripadvisor.