
- Presidential Message
- Nominations/Elections
- Past Presidents
- Member Spotlight
- Fellow List
- Fellowship Nominations
- Current Awardees
- Award Nominations
- SCP Mentoring Program
- SCP Book Club
- Pub Fee & Certificate Purchases
- LEAD Program
- Introduction
- Find a Treatment
- Submit Proposal
- Dissemination and Implementation
- Diversity Resources
- Graduate School Applicants
- Student Resources
- Early Career Resources
- Principles for Training in Evidence-Based Psychology
- Advances in Psychotherapy
- Announcements
- Submit Blog
- Student Blog
- The Clinical Psychologist
- CP:SP Journal
- APA Convention
- SCP Conference

CASE STUDY Victor (post-traumatic stress disorder)
Case study details.
Victor is a 27-year-old man who comes to you for help at the urging of his fiancée. He was an infantryman with a local Marine Reserve unit who was honorably discharged in 2014 after serving two tours of duty in Iraq. His fiancé has told him he has “not been the same” since his second tour of duty and it is impacting their relationship. Although he offers few details, upon questioning he reports that he has significant difficulty sleeping, that he “sleeps with one eye open” and, on the occasions when he falls into a deeper sleep, he has nightmares. He endorses experiencing several traumatic events during his second tour, but is unwilling to provide specific details – he tells you he has never spoken with anyone about them and he is not sure he ever will. He spends much of his time alone because he feels irritable and doesn’t want to snap at people. He reports to you that he finds it difficult to perform his duties as a security guard because it is boring and gives him too much time to think. At the same time, he is easily startled by noise and motion and spends excessive time searching for threats that are never confirmed both when on duty and at home. He describes having intrusive memories about his traumatic experiences on a daily basis but he declines to share any details. He also avoids seeing friends from his Reserve unit because seeing them reminds him of experiences that he does not want to remember.
- Hypervigilance
- Intrusive Thoughts
- Irritability
- Loss of Interest
- Sleep Difficulties
Diagnoses and Related Treatments
1. posttraumatic stress disorder.
Thank you for supporting the Society of Clinical Psychology. To enhance our membership benefits, we are requesting that members fill out their profile in full. This will help the Division to gather appropriate data to provide you with the best benefits. You will be able to access all other areas of the website, once your profile is submitted. Thank you and please feel free to email the Central Office at [email protected] if you have any questions
- Case Report
- Open access
- Published: 25 November 2008
A case of PTSD presenting with psychotic symptomatology: a case report
- Georgios D Floros 1 ,
- Ioanna Charatsidou 1 &
- Grigorios Lavrentiadis 1
Cases Journal volume 1 , Article number: 352 ( 2008 ) Cite this article
30k Accesses
1 Altmetric
Metrics details
A male patient aged 43 presented with psychotic symptomatology after a traumatic event involving accidental mutilation of the fingers. Initial presentation was uncommon although the patient responded well to pharmacotherapy. The theoretical framework, management plan and details of the treatment are presented.
Recent studies have shown that psychotic symptoms can be a hallmark of post-traumatic stress disorder [ 1 , 2 ]. The vast majority of the cases reported concerned war veterans although there were sporadic incidents involving non-combat related trauma (somatic or psychic). There is a biological theoretical framework for the disease [ 3 ] as well as several psychological theories attempting to explain cognitive aspects [ 4 ].
Case presentation
A male patient, aged 43, presented for treatment with complaints tracing back a year ago to a traumatic work-related event involving mutilation of the distal phalanges of his right-hand fingers. Main complaints included mixed hallucinations, irritability, inability to perform everyday tasks and depressive mood. No psychic symptomatology was evident before the event to him or his social milieu.
Mental state examination
The patient was a well-groomed male of short stature, sturdy build and average weight. He was restless but not agitated, with a guarded attitude towards the interviewer. His speech pattern was slow and sparse, his voice low. He described his current mood as 'anxious' without being able to provide with a reason. Patient appeared dysphoric and with blunted affect. He was able to maintain a linear train of thought with no apparent disorganization or irrational connections when expressing himself. Thought content centred on his amputated fingers with a semi-compulsive tendency to gaze to his (gloved) hand. The patient was typically lost in ruminations about his accident with a focus on the precise moment which he experienced as intrusive and affectively charged in a negative and painful way. He could remember wishing for his fingers to re-attach to his hand almost as the accident took place. A trigger in his intrusive thoughts was the painful sensation of neuropathic pain from his half-mutilated fingers, an artefact of surgery.
He denied and thoughts of harming himself and demonstrated no signs of aggression towards others. Hallucinations had a predominantly depressive and ego-dystonic character. He denied any perceptual disturbances at the time of the examination. Their appearance was typically during nighttime especially in the twilight. Initially they were visual only, involving shapes and rocks tumbling down towards the patient, gradually becoming more complex and laden with significance. A mixed visual and tactile hallucination of burning rain came afterwards while in the time of examination a tall stranger clad in black and raiding a tall steed would threaten and ridicule the patient. He scored 21 on a MMSE with trouble in the attention, calculation and recall categories. The patient appeared reliable and candid to the extent of his self-disclosure, gradually opening up to the interviewer but displayed a marked difficulty on describing his emotions and memories of the accident, apparently independent of his conscious will. His judgement was adequate and he had some limited Insight into his difficulties, hesitantly attributing them to his accident.
He was married and a father of three (two boys and a girl aged 7–12) He had no prior medical history for mental or somatic problems and received no medication. He admitted to occasional alcohol consumption although his relatives confirmed that he did not present addiction symptoms. He had some trouble making ends meet for the past five years. Due to rampant unemployment in his hometown, he was periodically employed in various jobs, mostly in the construction sector. One of his children has a congenital deformity, underwent several surgical procedures with mixed results and, before the time of the patient's accident, it was likely that more surgery would be forthcoming. The patient's father was a proud man who worked hard but reportedly was victimized by his brothers, they reaping the benefits of his work in the fields by manipulating his own father. He suffered a nervous breakdown attributed to his low economic status after a failed economic endeavour ending in him being robbed of the profits, seven years before the accident. There was no other relevant family history.
Before the accident the patient was a lively man, heavily involved as a participant and organizer in important local social events from a young age. He was respected by his fellow villagers and felt his involvement as a unique source of pride in an otherwise average existence. Prior to his accident, the patient was repeatedly promised a permanent job as a labourer and fate would have it that his appointment was supposedly approved immediately after the accident only to be subsequently revoked. He viewed himself as an exploited man in his previous jobs, much the same way his father was, while he harboured an extreme bitterness over the unavailability of support for his long-standing problems. His financial status was poor, being in sick-leave from his previous job for the last four months following the accident and hoping to receive some compensation. Although his injuries were considered insufficient for disability pension he could not work to his full capacity since the hand affected was his primary one and he was a manual labourer.
Given that the patient clearly suffered a high level of distress as a result of his hallucinatory experiences he was voluntary admitted to the 2nd Psychiatric Department of the Aristotle University of Thessaloniki for further assessment, observation and treatment. A routine blood workup was ordered with no abnormalities. A Rorschach Inkblot Test was administered in order to gain some insight into patient's dynamics, interpersonal relations and underlying personality characteristics while ruling out any malingering or factitious components in the presentation as suggested in Wilson and Keane [ 5 ]. Results pointed to inadequate reality testing with slight disturbances in perception and a difficulty in separating reality from fantasy, leading to mistaken impressions and a tendency to act without forethought in the face of stress. Uncertainty in particular was unbearable and adjustment to a novel environment hard. Cognitive functions (concentration, attention, information processing, executive functions) were impaired possibly due to cognitive inability or neurological disease. Emotion was controlled with a tendency for impulsive behaviour; however there was difficulty in processing and expressing emotions in an adaptive manner. There were distinct patterns of aggression and anger towards others but expressing those patterns was avoided, switching to passivity and denial rather than succumbing to destructive urges or mature competitiveness. Self-esteem was low with feelings of inferiority and inefficiency.
A neurological examination revealed a left VI cranial nerve paresis, reportedly congenital, resulting in diplopia while gazing to the extreme left, which did not significantly affect the patient. The patient had a chronic complaint of occasional vertigo, to which he partly attributed his accident, although the symptoms were not of a persisting nature.
Initial diagnosis at this stage was 'Psychotic disorder NOS' and pharmacological treatment was initiated. An MRI scan of the brain with gadolinium contrast was ordered to rule out any focal neurological lesions. It was performed fifteen days later and revealed no abnormalities.
Patient was placed on ziprasidone 40 mg bid and lorazepam 1 mg bid. He reported an immediate improvement but when the attending physician enquired as to the nature of the improvement the patient replied that in his hallucinations he told the tall raider that he now had a tall doctor who would help him and the raider promptly left (sic). Apparently, the random assignment of a strikingly tall physician had an unexpected positive effect. Ziprasidone gradually increased to 80 mg bid within three days with no notable effect to the perceptual disturbances but with the development of akathisia for which biperiden was added, 1 mg tid. Duloxetine was added, 60 mg once-daily, in a hope that it could have a positive effect to his mood but also to this neuropathic pain which was frequent and demoralising. The patient had a tough time accommodating to the hospital milieu, although the grounds were extended and there was plenty of opportunity for walks and other activities. He preferred to stay in bed sometimes in obvious agony and with marked insomnia. He presented a strong fear for the welfare of his children, which he could not reason for. Due to the apparent inability of ziprasidone to make a dent in the psychotic symptomatology, medication was switched to amisulpride 400 mg bid and the patient was given a leave for the weekend to visit his home. On his return an improvement in his symptoms was reported by him and close relatives, although he still had excessive anxiety in the hospital setting. It was decided that his leave was to be extended and the patient would return for evaluation every third day. After three appointments he had a marked improvement, denied any psychotic symptoms while his sleep pattern improved. A good working relationship was established with his physician and the patient was with a schedule of follow-up appointments initially every fifteen days and following two months, every thirty days. His exit diagnosis was "Psychotic disorder Not Otherwise Specified – PTSD". He remained asymptomatic for five months and started making in-roads in a cognitively-oriented psychotherapeutic approach but unfortunately further trouble befell him, his wife losing a baby and his claim to an injury compensation rejected. He experienced a mood loss and duloxetine was increased to 120 mg per day to some positive effect. His status remains tenuous but he retains a strong will to make his appointments and work with his physician. A case conceptualization following a cognitive framework [ 6 ] is presented in Figure 1 .
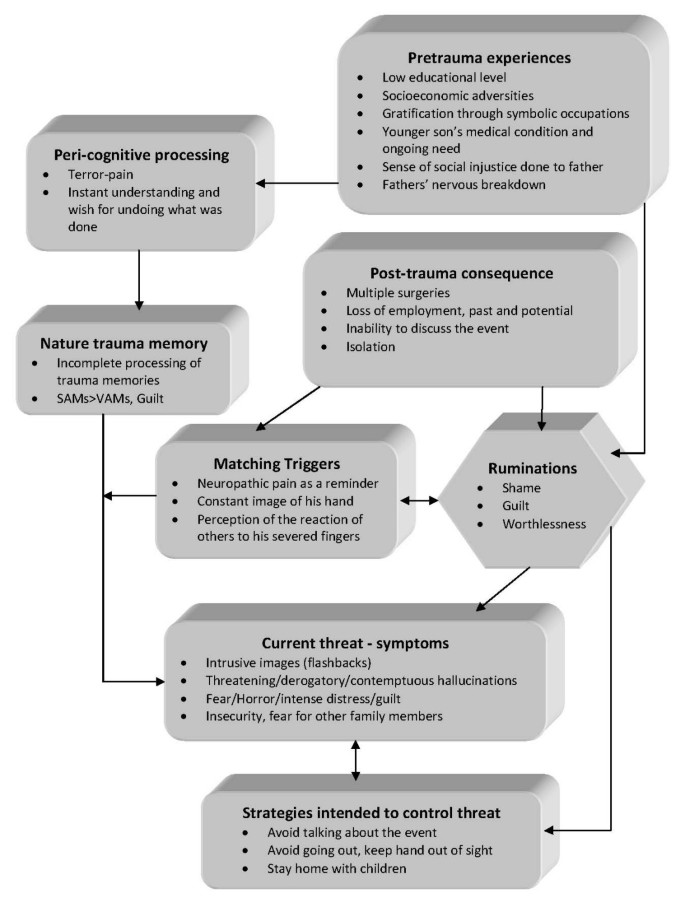
Case formulation – (Persistent PTSD, adapted from Ehlers and Clark [ 6 ] ) . Case formulation following the persistent PTSD model of Ehlers and Clark [ 6 ]. It is suggested that the patient is processing the traumatic information in a way which a sense of immediate threat is perpetuated through negative appraisals of trauma or its consequences and through the nature of the traumatic experience itself. Peri-traumatic influences that operate at encoding, affect the nature of the trauma memory. The memory of the event is poorly elaborated, not given a complete context in time and place, and inadequately integrated into the general database of autobiographical knowledge. Triggers and ruminations serve to re-enact the traumatic information while symptoms and maladaptive coping strategies form a vicious circle. Memories are encoded in the SAM rather than the VAM system, thus preventing cognitive re-appraisal and eventual overcoming of traumatic experience [ 4 ].
The value of a specialized formulation is made clear in complex cases as this one. There is a relationship between the pre-existing cognitive schemas of the individual, thought patterns emerging after the traumatic event and biological triggers. This relationship, best described as a maladaptive cognitive processing style, culminates into feelings of shame, guilt and worthlessness which are unrelated to similar feelings, which emerge during trauma recollection, but nonetheless acts in a positive feedback loop to enhance symptom severity and keep the subject in a constant state of psychotic turmoil. Its central role is addressed in our case formulation under the heading "ruminations" which best describes its ongoing and unrelenting character. The "what if" character of those ruminations may serve as an escape through fantasy from an unbearably stressful cognition. Past experience is relived as current threat and the maladaptive coping strategies serve as negative re-enforcers, perpetuating the emotional suffering.
The psychosocial element in this case report, the patient's involvement with a highly symbolic activity, demonstrates the importance of individualising the case formulation. Apparently the patient had a chronic difficulty in expressing his emotions and integrating into his social surroundings, a difficulty counter-balanced somewhat with his involvement in the local social events which gave him not only a creative way out from any emotional impasse but also status and recognition. His perceived inability to continue with his symbolic activities was not only an indicator of the severity of his troubles but also a stressor in its own right.
Complex cases of PTSD presenting with hallucinatory experiences can be effectively treated with pharmacotherapy and supportive psychotherapy provided a good doctor-patient relationship is established and adverse medication effects rapidly dealt with. A cognitive framework and a Rorschach test can be valuable in deepening the understanding of individuals and obtaining a personalized view of their functioning and character dynamics. A biopsychosocial approach is essential in integrating all aspects of the patients' history in a meaningful way in order to provide adequate help.
Patient's perspective
"My life situation can't seem to get any better. I haven't had any support from anyone in all my life. Leaving home to go anywhere nowadays is hard and I can't seem to be able to stay anyplace else for a long time either. Just getting to the hospital [where the follow-up appointments are held] makes me very nervous, especially the minute I walk in. Can't seem to stay in place at all, just keep pacing while waiting for my appointment. I am only able to open up somewhat to my doctor, whom I thank for his support. Staying in hospital was close to impossible; I was very stressed and particularly concerned for my children, not being able to be close to them. I still need to have them near-by. Getting the MRI scan was also a stressful experience, confined in a small space with all that noise for so long. I succeeded only after getting extra medication.
I hope that things will get better. I don't trust anyone for any help any more; they should have helped me earlier."
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
stands for 'Post Traumatic Stress Disorder'
for 'Verbally Accessible Memory'
for 'Situationally Accessible Memory'
Butler RW, Mueser KT, Sprock J, Braff DL: Positive symptoms of psychosis in posttraumatic stress disorder. Biological Psychiatry. 1996, 39: 839-844. 10.1016/0006-3223(95)00314-2.
Article CAS PubMed Google Scholar
Seedat S, Stein MB, Oosthuizen PP, Emsley RA, Stein DJ: Linking Posttraumatic Stress Disorder and Psychosis: A Look at Epidemiology, Phenomenology, and Treatment. The Journal of Nervous and Mental Disease. 2003, 191: 675-10.1097/01.nmd.0000092177.97317.26.
Article PubMed Google Scholar
Nutt DJ: The psychobiology of posttraumatic stress disorder. J Clin Psychiatry. 2000, 61: 24-29.
CAS PubMed Google Scholar
Brewin CR, Holmes EA: Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003, 23: 339-376. 10.1016/S0272-7358(03)00033-3.
Wilson JP, Keane TM: Assessing Psychological Trauma and PTSD. 2004, The Guilford Press
Google Scholar
Ehlers A, Clark DM: A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000, 38: 319-345. 10.1016/S0005-7967(99)00123-0.
Download references
Acknowledgements
The authors wish to acknowledge the valuable support and direction offered by the department's chair, Professor Ioannis Giouzepas who places the utmost importance in creating a suitable therapeutic environment for our patients and a superb learning environment for the SHO's and registrars in his department.
Author information
Authors and affiliations.
2nd Department of Psychiatry, Psychiatric Hospital of Thessaloniki, 196 Langada str., 564 29, Thessaloniki, Greece
Georgios D Floros, Ioanna Charatsidou & Grigorios Lavrentiadis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Georgios D Floros .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
GF was the attending SHO and the major contributor in writing the manuscript. IC performed the psychological evaluation and Rorschach testing and interpretation. GL provided valuable guidance in diagnosis and handling of the patient. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Floros, G.D., Charatsidou, I. & Lavrentiadis, G. A case of PTSD presenting with psychotic symptomatology: a case report. Cases Journal 1 , 352 (2008). https://doi.org/10.1186/1757-1626-1-352
Download citation
Received : 12 September 2008
Accepted : 25 November 2008
Published : 25 November 2008
DOI : https://doi.org/10.1186/1757-1626-1-352
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ziprasidone
- Psychotic Disorder
- Amisulpride
- Hallucinatory Experience
Cases Journal
ISSN: 1757-1626
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- June 15, 2024 | VOL. 77, NO. 2 CURRENT ISSUE pp.43-100
- March 15, 2024 | VOL. 77, NO. 1 pp.1-42
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Interpersonal Psychotherapy (IPT) for PTSD: A Case Study
- Alexandra Klein Rafaeli , Psy.D. ,
- John C. Markowitz , M.D.
New York State Psychiatric Institute, Columbia University, New York, NY.
Search for more papers by this author
Interpersonal Psychotherapy (IPT), a time-limited, evidence-based treatment, has shown efficacy in treating major depressive disorder and other psychiatric conditions. Interpersonal Psychotherapy focuses on the patient’s current life events and social and interpersonal functioning for understanding and treating symptoms. This case report demonstrates the novel use of IPT as treatment for posttraumatic stress disorder (PTSD). Preliminary evidence suggests IPT may relieve PTSD symptoms without focusing on exposure to trauma reminders. Thus IPT may offer an alternative for patients who refuse (or do not respond to) exposure-based approaches. Interpersonal Psychotherapy focuses on two problem areas that specifically affect patients with PTSD: interpersonal difficulties and affect dysregulation. This case report describes a pilot participant from a study comparing 14 weekly sessions of IPT to treatment with two other psychotherapies. We describe the session-by-session IPT protocol, illustrating how to formulate the case, help the patient identify and address problematic affects and interpersonal functioning, and to monitor treatment response.
Introduction
Interpersonal Psychotherapy (IPT) is a time-limited, evidence-based treatment that focuses on patients’ social and interpersonal functioning, affect, and current life events. It is efficacious in treating major depression, bulimia, and other conditions ( Weissman et al., 2000 ). Developed by the late Gerald Klerman, M.D., and Myrna Weissman, Ph.D., IPT stems from the theoretical work of Harry Stack Sullivan and John Bowlby and from empirical research on the psychosocial aspects of depression. Sullivan (1953) viewed interactions with others as the most profound source of understanding one’s emotions, while Bowlby (1969) considered strong bonds of affection with others the foundation for individual well being. These theorists guide IPT practitioners as they explore their patients’ affective experiences through the lens of the social and the interpersonal.
Initial evidence suggests that IPT may also benefit patients with posttraumatic stress disorder ([PTSD]; Bleiberg & Markowitz, 2005 ; Campanini et al., 2010 ; Krupnick et al., 2008 ; Ray et al., 2010 ; Robertson et al., 2004 ; Robertson et al., 2007 ). There are at least two rationales for testing IPT for this population. First, IPT does not utilize exposure to trauma reminders. Although extensive evidence supports the efficacy of exposure-based therapies for PTSD (Grey, 2008), IPT offers an alternative to patients who may refuse exposure techniques or not respond to them. A recent review article suggested that highly traumatized patients who dissociate may fare better receiving affect-focused therapy than exposure-based therapy ( Lanius et al., 2010 ). Second, IPT works by improving patients’ interpersonal functioning and emotion regulation ( Markowitz et al., 2006 , 2009 ; Markowitz, 2010 ), which are commonly impaired in PTSD (APA, 2000) and therefore, important targets for change. Social support, which IPT helps patients to mobilize, has been shown to be a key factor in preventing and recovering from PTSD ( Brewin et al., 2000 ; Ozer et al., 2003 ).
PTSD is a psychiatric illness triggered by traumatic events: experiencing a natural disaster, witnessing a death, suffering chronic abuse, or otherwise facing a threat to one’s own life or physical integrity. Although most people (50% to 90%) encounter traumas during their lifetimes, only about 8% develop full PTSD ( Kessler et al., 1995 ). Symptoms of PTSD are distressing and often significantly impair social and occupational functioning.
Many forms of psychotherapy have been employed to address PTSD. Those with the strongest evidence base are forms of cognitive behavioral therapy (CBT), which utilize controlled exposure to trauma reminders (Butler et. al., 2000). Cognitive Behavioral Therapy aims to solve problems by working towards changing patterns of irrational thinking or behavior linked to one’s negative emotions. The CBT approach involves exposure to the trauma either through imaginal confrontation of traumatic memories (Foa, 2003) or in vivo exposure to trauma reminders (Joseph, 2008).
In contrast to exposure-based CBT approaches, IPT eschews focusing on the trauma and instead concentrates on the patient’s current life events, particularly on social and interpersonal aspects ( Markowitz, 2010 ). The basic premise of IPT for PTSD is trauma shatters the patient’s sense of interpersonal safety, leading to withdrawal from interpersonal relationships and impaired ability to use social supports to process the traumatic event ( Markowitz et al., 2009 ). By withdrawing, individuals with PTSD cut off vital social supports needed when they are most vulnerable. Because they are interpersonally hypervigilant, emotionally detached or dysregulated, patients with PTSD mistrust relationships ( Bleiberg and Markowitz, 2005 ). Interpersonal Psychotherapy helps the patient to understand rather than avoid feelings, to tolerate such affects, to use them to enhance communication and effectively manage interactions with others, and thereby, to rebuild interpersonal trust. Finding ways to reconnect meaningfully to one’s surrounding world may reinstate severed social networks and reduce PTSD symptoms.
| • | (mourning the death of a significant other), | ||||
| • | (a struggle with a significant other, which the patient is inevitably losing), or | ||||
| • | (any major life change, including having suffered a traumatic event or events) ( ). | ||||
In a role transition, a life change costs the patient an old role and substitutes a new, unwanted one. Treatment helps the patient mourn the loss of the former and develop skills, interpersonal opportunities, and confidence in the latter, new role. Even an interpersonal trauma may have a silver lining.
Empirical Support
Bleiberg and Markowitz (2005) developed a manualized modification of individual IPT for PTSD. A small, open trial treating 14 patients with chronic PTSD yielded improvements across the three PTSD-DSM-IV-TR symptom clusters of hyper arousal, avoidance/numbing, and intrusive symptoms, in addition there were reductions in depression and anger and improvements in social functioning ( Bleiberg & Markowitz, 2005 ). An NIMH-funded, randomized controlled study is currently comparing three 14-week psychotherapies that employ very different mechanisms for treating chronic PTSD: 1) prolonged exposure ( Foa and Rothbaum, 1998 ); 2) IPT, focusing on interpersonal sequelae of PTSD rather than exposure to its traumatic triggers; and 3) relaxation, emphasizing reduction of anxiety through relief of physical tension ( Jacobson, 1938 ). This study will evaluate not only the efficacy of IPT for PTSD, but potential mediators and moderators of treatment outcome.
To illustrate IPT for PTSD, we present data from a pilot case that was not included in the current NIMH study, but served as a valuable training case. This patient received open IPT treatment for PTSD because his Clinician-Administered PTSD Scale (CAPS, Blake et al., 1995 ) score of 45, while indicating moderate symptom severity ( Weathers et al., 2001 ), fell below the study inclusion threshold of 50 or above. This case served as training for a therapist who was new to the study. The patient exemplifies the complex presentation of most patients who meet DSM-IV criteria for PTSD, who generally report comorbidity ( Kessler et al., 1995 ). His response to treatment illustrates the use of IPT as an alternative approach to reducing PTSD symptoms without exposure techniques.
Mr. A., a 48-year-old male, worked from home as a freelance software engineer. He held a master’s degree in computer science and had worked successfully for many years as a computer programmer, but was currently working sporadically and struggling financially. He requested psychotherapy to address current symptoms of “irritability, sleep disturbance, and interpersonal conflicts.” He reported a history of multiple traumas that he felt contributed to his current difficulties. Although he described attempting to “accept the pain and suffering these past ordeals caused” and to “move on,” he often felt resentful and unable to forgive.
Mr. A. was raised in a blue-collar suburb of Philadelphia, living with his parents and two younger sisters. He reported feeling tremendous pressure to excel, which he attributed to his father’s continual dissatisfaction with Mr. A.’s accomplishments. He had few friends growing up, but was committed and loyal to those he did call friends. He had had a few short-term relationships when younger, was once briefly married, and had a daughter, Chloe, who was currently in her twenties. He described his marriage as “agreeable,” despite feeling the couple shared no common interests and lacked any “passionate connection.” He reported being strongly attached to Chloe from her infancy until age 2. During that interval, he carried out most parental duties while his wife recuperated from a serious back injury. He described his attachment to his daughter during this time as “the most harmonious bond I ever experienced with another human being.”
Mr. A. was currently living with his girlfriend of 7 years, Diane, age 38. He referred to this as a “9/11 relationship”: their first date was in New York on the eve of September 11, 2001, and he believed that the catastrophe brought them closer and created a mutual urgency to “settle down.” Had the terrorist attacks not occurred, he believed their relationship would not have lasted.
Mr. A. exhibited ambivalence about this relationship (and any longterm commitment). He shared a home with Diane, was extremely loyal and devoted, described her with affection, respect, and warmth, and even sometimes referred to her as his fiancée. He described his love for her as strictly platonic, however. They hadn’t been sexually intimate in years, and he saw her more as a “best friend” or “soul mate” than a future wife or mother.
Mr. A.’s description of his interactions with Diane reflected several characteristic behaviors of PTSD ( Markowitz et al., 2009 ). He depicted interactions at home as tense and at times explosive, and attributed these interpersonal struggles to an overall aversion to any “intense feelings.” He would get angry at Diane for intruding on his work space or on his chance to “relax” or “meditate in solitude.” He had created a work environment void of almost all social interaction and found Diane’s presence disturbed his plan, which was to distance himself enough from others so there would be no conflict. His general mistrust in others, another characteristic behavior of PTSD, also added to his uncertainty in his relationship with Diane. For example, Mr. A. had severed ties with Diane’s father over a failed business venture, but Diane continued communicating with him. As a consequence, Mr. A. questioned her fidelity.
Mr. A. reported a shift in his sexuality that he considered the primary cause of his diminished physical attraction towards Diane. Approximately one year before starting IPT, he had become strongly attracted to transsexuals and was daily pursuing contact with the community online. Through Mr. A.’s exploration of the transsexual community, he developed a close “cyber” relationship with Jane, a transsexual living abroad, with whom he frequently e-mailed and “chatted.” Apart from posting photographs online, however, they had never seen each other. Here too, his avoidance of intense feelings seemed to preclude any intimacy. For although he and Jane had discussed setting up a webcam so they could interact more (and even planned to one day meet in person) Mr. A. always stopped short of seeing through with the plans.
Mr. A. initially considered the recent shift in his sexuality a novel curiosity. During the therapy, however, he began to consider the possibility that this attraction was not novel, but part of a longer-standing confusion about sexual orientation.
Trauma History
Mr. A. reported multiple events in his past involving intense fear and humiliation. Some were indeed traumas as defined by the DSM-IV-TR criterion A for PTSD, where others would more appropriately be categorized as subjectively distressing events. Regardless of the clinical classification, each experience Mr. A. recounted evoked vivid and frightful memories. Mr. A.’s first memory dated back to his toddler years. He was told his mother had to stay in the hospital for several weeks after giving birth due to complications, and he would stay with his aunt and uncle. He worried that his mother would die in the hospital and that he would never see her again. He then recounted experiencing additional “emotional trauma” when his aunt “humiliated” him in front of a house full of family members by forcing him to rub his nose in the diaper he had soiled. He linked this memory of shame and disgrace to problems he had in adulthood with sexual intimacy. Mr. A. also recalled the same aunt and uncle so criticizing him for eating messily that it “felt like verbal abuse” and produced a severe food phobia. Other early traumas he revealed at intake included experiencing a hurricane firsthand (age 6) and physical assault by a group of peers in middle school.
The magnitude of Mr. A.’s horrific experiences had no bearing on the impression they left behind. For example, the hurricane and physical assault hardly affected his daily routine; however, his “humiliation” by his aunt (an event not meeting PTSD criterion A) shaped him for years to come. The trauma that most profoundly affected his functioning (DSM-IV criterion A) occurred after Mr. A. and his wife separated. He initially continued to see his child regularly. After several months, however, his wife abruptly abducted Chloe to her native country. Because she left no word for Mr. A., he had no knowledge of his daughter’s well-being or whereabouts for two days. Convinced she had been abducted, he feared for her life. Eventually, he learned that she was safe with her mother, but remained unable to contact or see her.
In the ensuing two years, Mr. A. devoted his life to locating and reconnecting with his daughter. He quit his job, moved to his ex-wife’s country, and immersed himself in custody and abduction law. That Chloe’s age was similar to his when he had first been “traumatized” held great significance for him: his mother had been “taken away,” leaving him fearful and anxious. This memory deepened his need to remain close to his daughter and never to let feel abandoned. A two-year international pursuit and custody battle ensued, including at least two threats on Mr. A.’s life by his ex-father-in law and someone he believed had been hired to kill him by his ex-wife’s family.
Mr. A. underwent a profound role transition with this life trauma. He often referred to his life before and after his daughter’s abduction as if describing two separate individuals: Pretrauma, he reported always having felt “a little mistrustful of others” and acknowledged lifelong “trouble with love and affection,” but was an active, functioning adult who held a full-time job, pursued various hobbies, and even, with some effort, participated in his community. Posttrauma, he struggled to function, to self-regulate, and to find meaning and purpose in his life. His social withdrawal was worsened, and despite seeking numerous therapies and self-help, his PTSD symptoms lingered.
Presenting Complaints
Hyperarousal symptoms.
Mr. A. reported feeling hyperalert and watchful, even when knowing there was no real need. In public settings he experienced moderate hypervigilance. He reported frequent, if brief, startle reactions. He described frequent (daily) intense anger and irritability; on most days, he took this anger out on Diane. Although able to recover relatively quickly from each anger outburst, he found his attempts to suppress anger exhausting, and he noted that the anger outbursts were damaging his relationship with Diane.
Avoidance/Numbing Symptoms
Mr. A. avoided activities, people, and places that evoked strong memories: e.g., phone calls from family members and parties where he might encounter individuals from his past. Avoidant behavior was pervasive: from the cocoon-like home environment, which permitted him to live in virtual isolation (he described choosing to work from home as “adaptive” given his history of interpersonal conflicts in work settings) to avoiding any possible reminder of Chloe’s abduction (he felt “more in control” at home, where he could carefully limit interactions with others). Although he did not meet criteria for substance abuse, he reported using marijuana three times a week and stated that he might not be able to stop using it during treatment. He also reported some loss of interest in previously enjoyable activities, such as sex and sports.
Intrusive symptoms
Although he presenting with a detached affective expression, Mr. A. became visibly upset (as though reliving experiences in the present) when reminded of past traumas or of instances when people betrayed him. Mr. A. reported intrusive daytime thoughts and occasional “bad dreams” about his traumas. The thoughts and nightmares impaired his concentration and made him anxious and uneasy “most of the day.” He described sleep as “chaotic,” compromised by his unstructured daily routine. As a consequence, he was often awake much of the night and then napped sporadically by day.
Other Symptoms
Mr. A. had concerns about his interactions with his most significant others. Although caring deeply for Diane, he worried that he could not reciprocate her romantic feelings for him. He could not imagine deepening their commitment through marriage or starting a family, and he often felt “too emotionally numb” to respond to Diane’s physical or emotional needs. Mr. A. also described considerable conflicts at home. He frequently “snapped” at Diane, and his discomfort with any physical intimacy she initiated caused constant tension between them. He spent most of his days on the computer, chatting online, or talking to his business partner by phone, and even those relatively detached interactions felt stressful.
Previous Treatments
Over the years, Mr. A. had participated in individual, group, and family therapy and had actively sought self-help solutions from books and websites. These had not relieved his ruminations about his distressing past nor helped him cope with high daily levels of anger and frustration. One psychodynamic treatment lasted several years. He also reported a briefer behavioral therapy with an exposure component, and family therapy. Exposure therapy had not helped to quell his anger and anxiety; he was only willing to share parts of his trauma narrative and had resisted any systematic in vivo or imaginal exposure techniques. Similarly, psychodynamic therapy had not reduced his symptoms. Mr. A.’s tendency to control conversations may have turned interpretations into debates. Despite participating in various psychotherapies, Mr. A. had never discussed his sexuality, focusing instead on past traumas.
An independent evaluator assessed Mr. A. using the Clinician-Administered PTSD Scale ([CAPS] Blake et al., 1995 ) and Hamilton Rating Scale for Depression ([Ham-D] Hamilton, 1967 ). Although his scores were subthreshold for the PTSD study, based on his CAPS score (CAPS = 45) ( Weathers et al., 2001 ), he warranted a diagnosis of moderate PTSD. His baseline score on the PTSD Diagnostic Scale Self Report (PSS-SR; Foa, 1993) was 25, which is considered severe ( Foa et al., 2009 ). The Life-Events Checklist ( Johnson et al, 1980 ) and Structured Clinical Interview for DSM-IV-TR Axis I Disorders (First, 1997) were also administered at intake. Mr. A. met criteria for PTSD, chronic agoraphobia without panic disorder (both lifetime and current), and specific phobia (fear of food being mixed or touching; lifetime and present). Mr. A. was admitted as a pilot IPT case.
Because Mr. A. was not a formal participant, the independent evaluator did not readminister the CAPS following treatment. However, Mr. A. did complete the PSS-SR and the Beck Depression Inventory (BDI-II) ( Beck, et al, 1996 ) pre-, mid-, and post-treatment.
Treatment Overview
Mr. A.’s long history of avoidant behaviors and interpersonal conflicts made him appear a good candidate for IPT. Interpersonal Psychotherapy differs theoretically and technically from other PTSD treatments in targeting posttrauma sequelae of impaired interpersonal functioning rather than exposure and re-processing of the traumatic events themselves ( Markowitz, 2010 ). Interpersonal Psychotherapy-PTSD (Markowitz, et al, 2009) comprises 14 weekly sessions of 50-minutes each. The clinician largely devotes the initial two to three sessions to an “interpersonal inventory,” collecting information to identify current relationships, overall patterns of interpersonal behavior, and links between relationships and symptoms. The clinician then formulates the case, linking the DSM-IV PTSD diagnosis to an interpersonal focus that emerged in the assessment, and shares this formulation with the patient. Sessions 3 to 14 focus on addressing and resolving the interpersonal problem area (e.g., role transition); the therapist provides psychoeducation about PTSD as a treatable medical illness that is not the patient’s fault, and serially monitors symptoms. The final sessions focus on termination, an important interpersonal event but one that has been anticipated from the start of the time-limited therapy.
Sessions 1 to 3: Initial phase
Goals for these sessions included exploring in detail Mr. A.’s current and past relationships to understand his interpersonal functioning, to identify interpersonal issues linked to the onset of PTSD symptoms, and to take a trauma history. The therapist first explained the IPT approach to Mr. A. He acknowledged the prominent interpersonal difficulties in his current life and expressed his eagerness r to work on changing his behaviors. The therapist then reviewed Mr. A.’s current PTSD symptoms, which were based on the PSS-SR results. She observed that his avoidance symptoms were the most prominent. She took a general history of traumas throughout Mr. A.’s life. Mr. A. noted that each trauma involved a profound sense of betrayal, which led him to mistrust people and to avoid forming close relationships.
The most important people in Mr. A.’s life were his girlfriend Diane and his daughter Chloe. He felt that his traumas negatively affected both relationships. He was irritable with Diane, and he avoided close contact with Chloe to avoid being hurt. He cited similar problems in other relationships, and reported that the “major trauma” of his life, Chloe’s abduction, unquestionably exacerbated this distancing tendency.
Mr. A. often attempted to advise and guide others, considering that he related to others best by imparting knowledge. Unfortunately, his guidance was often unsolicited and not well accepted. This behavior also arose almost immediately in IPT sessions. Mr. A. elaborated in great detail how particular computer programs worked or what he had learned in a recent self-help class. He would talk without pause for several minutes, despite the therapist’s attempts to interject. This tactic succeeded in avoiding any guidance from the therapist.
A similar process unfolded with his daughter, who had recently expressed interest in studying law. Upon hearing this, Mr. A. began telling her all of the details of his custody battle with her mother, including an enormous number of personal and confidential documents. He deemed this a supportive act; she did not.
Mr. A. admitted that his concept of relationships and his approaches to others often left him feeling distant from the very people he cared for most. At times he felt “betrayed” after doing “so much.” For example, early in his relationship with Diane, her father developed a rare illness. Mr. A. immediately took it upon himself to research extensively alternative treatments. Mr. A. felt he was instrumental in saving her father’s life, but never felt recognized for it.
After Chole and Mr. A. were reunited, he was hurt by Chloe’s decision to live with her mother rather than with him. He also still grieved his lost bond with Chloe when she was a baby, a bond defining to him the purest and most powerful of connections. Although he admitted having struggled for many years with feeling comfortable in romantic relationships and with physical intimacy, he believed this struggle worsened after the abduction.
Mr. A. had trouble accepting affection from Diane. When they met they had sex regularly, but in recent years they stopped sleeping in the same bed and had only been intimate once in recent years. He summarized a recent, deliberate attempt to rekindle passion between them as “the attempt failed.” Diane frequently desired physical closeness, and although he cared for her and wanted to reciprocate the affection for her sake, he found himself recoiling from her touch. He described her as “coming at him” too fast with a hug or a kiss, and he experienced excruciating discomfort from any physical touch.
Just as Mr. A. sought solutions for his “PTSD,” he spent time seeking an explanation for his intimacy difficulties. He began questioning his sexuality, past and present. In his past, he had felt most comfortable with female bisexual partners, and was often told he “made love like a woman.” He felt an unusual bond in his recent online relationship with Jane, a male-to-female transsexual. Extremely attracted to her, he also felt he could be more open and honest online, whereas at home he had to feign interest and affection. He wondered whether this recent attraction stemmed from an online self-help course that encouraged attunement with both his “left” and “right” brain. Attraction to a transsexual, he opined, tapped into his “middle-brain.”
Mr. A. believed yoga, meditation, and spirituality helped him to feel more “balanced.” He stated his primary goal was to become more “disciplined” and “even tempered,” “like the Dalai Lama.” Nonetheless, he continued to struggle with self-regulation in interpersonal situations. His spiritual exercises, all solitary in nature, were not aiding his quest for equilibrium; on the contrary, they enabled Mr. A. to continue avoiding interpersonal contact and any strong emotions such exchanges might evoke.
Ipt Case Formulation
The IPT formulation concisely links symptoms to the focal interpersonal problem area. The formulation, presented as feedback at the end of the initial phase, draws on information gathered from the interpersonal inventory and provides an organizing focus for the remainder of therapy:
I understand from our initial meeting that your interpersonal goals are to be closer to Chloe and to reduce disputes with Diane. I also understand that you’ve always experienced interpersonal difficulties, but that they grew much worse after your daughter’s abduction-triggered PTSD. You have clearly worked hard over the years to overcome problems you’ve had in social arenas, and you’ve tried numerous times to address the painful memories of past traumas that still live with you today .
Your PTSD symptoms still overshadow your feelings and actions. You feel overwhelmed by both your emotions and your environment. Your symptoms are also coupled with an important current life issue you say has you’ve never discussed in past treatments: your sexual identity. Through understanding yourself in relationship to others, you cam mend your social conflicts and reduce your symptoms .
You’ve discussed how hard it is to trust people, and how that has limited your social network for years. Your wife’s abduction of Chloe took away the person closest in the world to you, and has made it extremely difficult—to this day—for you to trust others, to take the risk to connect with those around you. This mistrust is very common in PTSD. Avoidance, numbing, intrusive thoughts are all symptoms of the illness. Although you say that you always had difficulty in social situations, these symptoms are not necessarily part of your character; they’re indication of an illness that you suffer from—an illness that’s treatable and not your fault. The symptoms can improve .
Your mistrust has led you to minimize social contact. You’ve discussed feeling “betrayed ” or “deceived ” after trying to help others many times over .
So you’ve been keeping your distance through “ electronic relationships ” that are more comfortable. Yet, you say you “yearn for closer, more real relationships!”
You are going through a role transition: Uncomfortable feelings about your relationships and your own sexuality have made life extremely confusing, and it’s hard for you to know what you want from whom. What we can work on in the remaining weeks of treatment is how to navigate this transition: Do you want to stay with Diane, deepen a relationship with Jane, or what? If you can understand your feelings and use them to resolve this uncertainty, not only will your life feel better, but you symptoms are likely to subside. Does that make sense to you?
Mr. A. agreed to work on this interpersonal focus.
Session 4 to 10: Middle Phase
Having agreed to focus on his role transition, Mr. A. and the therapist entered the middle phase of IPT. Mr. A. now understood that he was suffering from a treatable illness that was not his fault, with clinical symptoms related to his past traumas. He would learn to detect and monitor these symptoms in the course of therapy, but should not blame himself for having symptoms or for their impact on his relationships. In all likelihood, he would start to feel better and see the symptoms subside.
In his role transition, Mr. A.. was adjusting to changes in what and who attracted him sexually. The therapist introduced strategies to improve interpersonal communication, and helped elicit emotional responses that surfaced in the process. She supported Mr. A. in confronting and wrestling with intense (particularly negative) feelings. Mr. A. also needed to understand that his tendencies to intellectualize emotional experiences and to defend against any unpleasant moods complicated this shift. Tolerating his affects would help him become more connected with others and more open with his sexuality.
The therapist helped him to examine closely current conflicts and arguments. This would help Mr. A. determine what he wanted in these situations and explore interpersonal options, including role play to practice responses, to resolve them. Specific incidents from the week were reviewed, eliciting Mr. A.’s feelings and behaviors, and sessions offered a chance to practice and hone interpersonal skills.
“How have things been since we last met?”
This simple question starts every IPT session. It anchors both therapist and patient by focusing on current feelings and life events related to the focal problem area (role transition) and by eliciting current concrete interpersonal incidents on which to draw when discussing alternative interpersonal techniques ( Weissman et al., 2000 ). Mr. A. could seldom recall any events from his week to discuss and instead, chose to recount stories from his past. His week, after all, intentionally avoided interpersonal encounters; he thought there was little to recount. Alternatively, he would offer a detailed description of a computer program he was developing, dive into monologues about what it takes to be an effective software engineer, or return to his distant past. This parrying the opening IPT question was a fundamental challenge in the treatment.
The therapist persisted in probing each week, seeking to guide Mr. A. to the here and now and away from the distant stories indelibly fixed in his mind. Despite his cocoon-like existence, Mr. A. had interactions with others, though he may have wanted to avoid the affect attached to recent arguments with Diane, or an emotionally charged phone call with Chloe, or a negative response from an online communication.
Mr. A.’s communication style was intellectualized, emotionally detached, expressed in abstract theoretical rather than experiential verbiage. When asked a simple question like, “How did that make you feel?” he responded with an analysis of how his “left brain” was dictating his behavior, making it impossible for his creative, emotional “right brain” to respond. The therapist challenged him to explore the feelings he consistently ignored or avoided, using his vocabulary as an illustration. She suggested that such detached language contributed to his distancing himself from the real feelings situations evoked. She urged him to retell day-to-day encounters using emotional words and describing his momentary experience. Again, the focus was on everyday interactions rather than a review of his trauma experiences, which were in this case, too well rehearsed to evoke genuine emotion. The therapist would then return to the initial question: “How have things been since we last met?”
It was frustrating when, at first, Mr. A. couldn’t break old habits. The therapist felt as Chloe must have when she hoped for her father’s support but instead got a lecture, or Diane might have when trying to connect with him, only to be repeatedly rebuffed. Mr. A. clearly cared deeply about his relationships and suffered from his isolation, but he made it almost impossible to break through the veneer.
By Session 6, Mr. A. was better able to recount specific events from his week, and was willing to take greater emotional risks when feelings surfaced. He described a telephone conversation with Chloe in which they talked more openly about their current lives. He still wished he could have influenced her life decisions (e.g., career choice) and values. He also recognized that many of the feelings he often avoided or suppressed related to his daughter. His years of grieving about time lost with Chloe no longer mattered as much to him as did the importance of their current relationship. He then attributed his current qualms about having children with Diane to regrets and losses surrounding Chloe and to his generalized loss of trust in other people.
The therapist introduced role play for improving Mr. A.’s ability to communicate with his significant others. She encouraged him to limit his phone interactions and increase face-to-face meetings with his business partner. In such meetings, Mr. A. could break his isolation, better read facial and body cues, and circumvent conflict. The therapist clarified that this was not a form of exposure, rather a technique for relating to others better. Mr. A. was initially uncomfortable with this until they role-played scenarios in session.
The therapist encouraged Mr. A. to recognize when he was frustrated or angry with Diane and tell her. With practice, he gradually saw the benefit of this approach in preventing angry outbursts. Similarly, when Jane suddenly broke off on-line communication, the therapist encouraged Mr. A. to confront her rather than avoid the behavior’s meaning and the hurt feelings it evoked. The therapist validated and normalized these negative affects as useful indicators of social encounters.
The therapist used IPT’s medical model and designation of the “sick role” ( Weissman et al., 2000 ) throughout the middle phase to underscore that Mr. A.’s symptoms were not his personality or a personal failing. As Mr. A.’s PTSD symptoms had lingered for decades, he had, unsurprisingly, come to confuse the disorder with his character. He had internalized symptoms, such as avoidance, startle responses, and irritability, as if they were fixed traits he could only manage, not dissolve. With time, he began to recognize the symptoms were not his character and not his fault. Through understanding his emotions and their role in daily minor encounters, he could reduce them so that he would merely experience healthy anxiety when reminded of traumas.
Just as Mr. A. had believed initially that PTSD an intractable part of himself, he also believed that strong feelings, such as anger or sorrow, could produce only negative outcomes. The therapist supported Mr. A. in confronting, rather than avoiding, intense (particularly negative) feelings. Each time he retreated into intellectualized language, she asked him to describe how he was feeling at that moment. Acknowledging, and simply sitting with an intense emotion, was his most challenging task.
This piece of the treatment was crucial, and is central to understanding how IPT differs from other affect-based therapies. Learning to acknowledge one’s emotions and to experience them more deeply is a shared core principle. However, in IPT the patient learns to understand a particular emotion as a response in an interpersonal context and then to communicate the feeling to improve an important relationship. Mr. A. did this with his irritability: his anger outbursts resulted from avoiding or suppressing intense feelings. If he could express his fears, anxiety, or disappointments with Diane as they surfaced, he was less likely to angrily “explode.” He practiced talking with Diane about his feelings when they were at peace, using “I” statements to avoid accusing or attacking language. He also shifted his communication of his feelings during sessions. Instead of “educating” the therapist, he now was willing to verbalize emotions and to explore their interpersonal context.
As the termination phase neared, an evaluator reassessed Mr. A.’s symptoms. His PSS-SR scores improved dramatically, falling from 25 at the start of treatment to 9 by session 8, indicating that he no longer met full criteria for PTSD. His BDI score remained euthymic, falling from 7 to 6.
Early in treatment, Mr. A. had responded hesitantly to techniques the therapist suggested, hiding behind intellectualization and refusing to focus on the present. He progressed as he became more willing to leave his comfort zone and to acknowledge that negative affects are not “bad,” but that sadness, loss, anger, are all useful, socially informative feelings if tolerated. This was a profound shift. He noticed he was becoming less irritable with Diane and his business partner and was less avoidant of social situations. He came to sessions more willing to discuss recent events and resultant feelings. He said this would never come easily or “naturally,” but he saw the benefit in trying. As a result, he felt better.
Session 11-14: Termination Phase
The final sessions reviewed the treatment course and addressed Mr. A.’s progress, his developing skills, and his feelings about ending therapy. The therapist acknowledged the sadness of separation, yet focused on the gains he had made, and reviewed areas where Mr. A. felt more competent and independent to function without therapy. Together they tried to anticipate difficulties that might resurface after treatment. Mr. A. recognized his progress, but voiced disappointment that treatment was ending and wanted to discuss ways to continue. He viewed “endings” negatively, recalling his childhood separation from his parents, his marriage, and his relationship with his daughter. He feared that parting would only bring gloom and helplessness, as it had in his past.
The therapist presented termination as a potentially corrective experience: Mr. A. could work through the feelings that arose in saying goodbye, and potentially, see that not only could he tolerate such emotions, but also that he deserved a sense of completion, mastery of skills, and progress.
At termination, Mr. A. was more socially engaged and communicated more effectively. He now considered his shift in sexuality more a curiosity than a bona fide change in identity, and decided his relationship with Diane was worth nurturing. He became more affectionate with Diane, talking with her more openly about both their future and his past. Diane knew about Chloe’s abduction, but not about the related traumas that contributed to Mr. A.’s fears of intimacy and lasting relationships. She also knew about his online relationship, but their discussions had never gotten past angry, jealous exchanges, so that she had been unaware of his longer standing sexual confusion. Mr. A. also reported that he felt his relationship with his daughter had improved. They talked more and she involved him more in her daily life.
In anticipating difficulties post treatment, Mr. A. expected his “poor people skills” would never remit, and he would need to continue practicing communication skills and challenging himself to approach people. He felt more capable of tolerating negative moods and better able to bounce back from conflicts. Mr. A. reported still thinking about past traumas and the people who had been disloyal to him over the years, but this occurred less often and less intensely.
Assessment of Progress
Mr. A.’s scores on the PSS-SR remained at 9 at session 14. Thus, by the end of the protocol, he was well below the cutoff score for PTSD criteria. His reports indicated improved daily functioning. Although his work schedule continued to disturb his sleep pattern, he reported less nocturnal anxiety. He reported less anger and irritability towards Diane and less conflict at home. He cited an improved relationship with Chloe, and increased hope of restoring their past bond. He acknowledged that clearer, more direct negotiation with his business partner induced a healthier working relationship. Finally, he decreased cannabis use from at least three times a week, to “as needed,” approximately once a week.
Complicating Factors During the Course of Treatment
During this short-term treatment, several factors complicated clinical progress. Mr. A. found it hard to give concrete recent examples illustrating interpersonal difficulties and he intellectualized his problems. A second, related complication was Mr. A.’s smorgasbord of past therapy approaches. He often arrived with a list of items to discuss and had difficulty shifting focus. His rigid preparation for sessions made it hard for the therapist to structure treatment. Similarly, Mr. A.’s “teacher” role interfered with the patient role and he thus avoided affect and interpersonal closeness. Finally, although Mr. A. did not meet full criteria for substance abuse or dependence, his habitual cannabis use was maladaptive.
Treatment Implications
This IPT-PTSD case illustrates what may present a viable alternative to exposure-based treatments for this serious disorder. The patient described grappled for more than 20 years with the aftereffects of a personal trauma. Despite numerous therapies and attempts at self-help, his PTSD had persisted. Neither exposure therapy nor long term psychodynamic therapy had helped to quell his anger, anxiety, and avoidance.
Interpersonal Psychotherapy-PTSD offered Mr. A. a chance to understand himself through his feelings and relationships subsequent to the trauma. No formal exposure techniques were used; instead, IPT-PTSD focused on the patient’s feelings in current interpersonal relationships through decision and communication analyses. The PTSD symptoms appeared to diminish through the processes of understanding feelings and relationship patterns and the slow building of social support.
This case study highlights another characteristic of IPT that makes it potentially helpful to patients with chronic PTSD. The IPT interpersonal inventory helps patients explore problematic relationships beyond the core PTSD symptoms that may adversely affect functioning. Mr. A. struggled with his sexuality. The more he discussed this, the more he connected it to his relationships and PTSD symptoms. Had the therapy focused exclusively on re-exposure to trauma reminders, this key issue might never have surfaced. Yet, the interpersonal issues bordering this patient’s daily functioning were paramount to his dilemma and his progress.
Acknowledgement:
Supported in part by grant R01 MH079078 from the National Institute of Mental Health.
American Psychiatric Association . ( 2000 ). Diagnostic and Statistical Manual of Mental Disorders , Fourth Edition, Text Revision. Washington, DC, American Psychiatric Association. Google Scholar
Beck, A.T., Steer, R.A., & Brown, G.K. ( 1996 ). Manual for Beck Depression Inventory II (BDI-II). San Antonio, TX, Psychology Corporation,. Google Scholar
Blake, D. D., Weathers, F. W., Nagy, L. M., Kaloupek, D. G., Gusman, F. D., Charney, D. S., & Keane, T. M. ( 1995 ). The development of a clinician-administered PTSD scale. Journal of Traumatic Stress ,;8, 75-90. Crossref , Medline , Google Scholar
Bleiberg, K.L., Markowitz, J.C. ( 2005 ). Interpersonal psychotherapy for posttraumatic stress disorder. The American Journal of Psychiatry ; 162,181-3. Crossref , Medline , Google Scholar
Bowlby J. ( 1969 ). Attachment . New York, NY: Basic Books. Google Scholar
Brewin, C.R, Andrews, B., & Valentine, J.D. ( 2000 ). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology , 68, 748-766. Crossref , Medline , Google Scholar
Butler, A.C., Chapman, J.E., Forman, E.M., & Beck, A.T. ( 2006 ). The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical Psychology Review , 26, 7-31. Crossref , Google Scholar
Campanini, R.F., Schoedl, A.F., Pupo, M.C., Costa, A.C., Krupnick, J.L., & Melo, M.F. ( 2010 ). Efficacy of interpersonal therapy-group format adapted to post-traumatic stress disorder: an open-label add-on trial. Depression and Anxiety , 72-77. Crossref , Medline , Google Scholar
Foa, E.B., Rothbaum, B.O. ( 1998 ) Treating the Trauma of Rape: Cognitive-Behavioral Therapy for PTSD . New York, NY: Guilford Press. Google Scholar
Foa, E.B., Riggs, D.S, Dancu C.V, & Rothbaum, B.O. ( 1993 ) Reliability and validity of a brief instrument for assessing post-traumatic stress disorder . Journal of Traumatic Stress , 6, 459-473. Crossref , Google Scholar
Foa, E.B., Keane,T.M., & Friedman, M.J. ( 2009 ) Effective Treatments for PTSD: Practice Guidelines from the International . Society for Traumatic Stress Studies. Guilford Press. Google Scholar
Foa, E.B, Rothbaum, B., & Furr, J. ( 2003 ) Augmenting exposure therapy with other CBT procedures . Psychiatric Annals , 33, 47-56. Crossref , Google Scholar
Hamilton M. Development of a rating scale for primary depressive illness . ( 1967 ). British Journal of Social and Clinical Psychology 6, 278-96. Crossref , Medline , Google Scholar
Jacobson, E. ( 1938 ) Progressive Relaxation . Chicago: University of Chicago Press. Google Scholar
Johnson, J.H., McCutcheon, S.M. ( 1980 ) Life Events Checklist . Hemisphere Publishing Corporation. Google Scholar
Joseph, J.S., Gray, M.J. ( 2008 ). BAO Exposure therapy for posttraumatic stress disorder . Journal of Behavior Analysis of offender and Victim: Treatment and Prevention 1, 69-80. Crossref , Google Scholar
Kessler, R.C., Sonnega, A., Bromet, E., & Nelson, C.B. ( 1995 ). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry , 52, 1048-60. Crossref , Medline , Google Scholar
Klerman, G.L., Weissman, M.M., Rounsaville, B.J., & Chevron, E. ( 1984 ). Interpersonal psychotherapy of depression. New York, NY: Basic Books. Google Scholar
Krupnick, J.L., Green, B.L., Stockton, P., Miranda, J., Krause, E., & Mete, M. ( 2008 ) Group interpersonal psychotherapy with low-income women with posttraumatic stress disorder . Psychotherapy Research ,18, 497-507. Crossref , Medline , Google Scholar
Lanius, R.A., Vermetten, E., Loewenstein, R.J., Brand, B., Schmahl, C. Bremner, J.D., & Spiegel, D. ( 2010 ) Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype . American Journal of Psychiatry , 167, 640-647. Crossref , Medline , Google Scholar
Markowitz, J.C. : ( 2010 ) Cutting Edge: IPT and PTSD . Depression and Anxiety , 27:879-881. Crossref , Medline , Google Scholar
Markowitz, J.C., Milrod, B., Bleiberg, K.L., & Marshall, R.D. ( 2009 ) Interpersonal factors in understanding and treating posttraumatic stress disorder. Journal of Psychiatric Practice , 15, 133-140. Crossref , Medline , Google Scholar
Markowitz, J.C., Bleiberg, K.L., Christos, P., & Levitan, E. ( 2006 ) Solving interpersonal problems correlates with symptom improvement in interpersonal psychotherapy: preliminary findings . Journal of Nervous and Mental Disease , 194, 15-20. Crossref , Medline , Google Scholar
Ozer, E.J., Best, S.R., Lipsey, T.L., & Weiss, D.S. ( 2003 ) Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin , 129, 52-73. Crossref , Medline , Google Scholar
Ray, R.D., & Webster, R. ( 2010 ) Group Interpersonal Psychotherapy for veterans with posttraumatic stress disorder: a pilot study . International Journal of Group Psychotherapy , 60, 131-140. Crossref , Medline , Google Scholar
Robertson, M., Rushton, P.J., Bartrum, M.D., & Ray, R. ( 2004 ) Group-Based Interpersonal Psychotherapy for Posttraumatic Stress Disorder: Theoretical and Clinical Aspects . International Journal of Group Psychotherapy , 54, 145-175. Crossref , Medline , Google Scholar
Robertson, M., Rushton, P, Batrim, D., Moore, E., & Morris, P. ( 2007 ) Open trial of interpersonal psychotherapy for post traumatic stress disorder . Australasian Psychiatry , 15, 375-379. Crossref , Medline , Google Scholar
Sullivan, H.S. ( 1953 ). The Interpersonal Theory of Psychiatry. New York, NY: Norton. Google Scholar
Weissman, M.M., Markowitz, J.C., Klerman, G.L. ( 2000 ) Comprehensive guide to interpersonal psychotherapy . New York: Basic Books. Google Scholar
Weathers, F.W., Keane, T.M., & Davidson,J.R.T. ( 2001 ) Clinician-Administered PTSD Scale: a review of the first ten years of research. Depression and Anxiet,y 13, 132-156. Crossref , Medline , Google Scholar
- Interpersonal psychotherapy for traumatic grief following a loss due to COVID-19: a case report 29 September 2023 | Frontiers in Psychiatry, Vol. 14
- Survivor‐led relational psychotherapy and embodied trauma: A qualitative inquiry 4 October 2020 | Counselling and Psychotherapy Research, Vol. 21, No. 3
- An Illustration of Interpersonal Psychotherapy for Perinatal Depression Case Reports in Psychiatry, Vol. 2020
- The Moderating Role of Child Maltreatment in Treatment Efficacy for Adolescent Depression 21 July 2020 | Journal of Abnormal Child Psychology, Vol. 48, No. 10
- PROTOCOL: Effectiveness of interpersonal psychotherapy in comparison to other psychological and pharmacological interventions for reducing depressive symptoms in women diagnosed with postpartum depression in low and middle‐income countries: A systematic review 25 February 2020 | Campbell Systematic Reviews, Vol. 16, No. 1
- Interpersonal Psychotherapy for Gender Dysphoria in a Transgender Woman 13 December 2019 | Archives of Sexual Behavior, Vol. 49, No. 2
- Interpersonal Psychotherapy for PTSD
- Yearbook of Psychiatry and Applied Mental Health, Vol. 2013
- Treating Patients Who Strain the Research Psychotherapy Paradigm Journal of Nervous & Mental Disease, Vol. 200, No. 7
- Posttraumatic stress disorder
- interpersonal psychotherapy
- affect dysregulation
- interpersonal difficulties

EMDR Case Studies

Case Study: EMDR Treatment – Rebecca
Case Study: EMDR Treatment – Rebecca PTSD UK Supporter Rebecca initially shared her EMDR experience on her own website, but has given us permission to

Case Study: EMDR Treatment – Ranya
Case Study: EMDR Treatment – Ranya Ranya* grew up in a violent and abusive household which led to her developing PTSD. In this case study,

Case Study: EMDR Treatment for Children – AJ
Case Study: EMDR Treatment for Children – AJ After a humiliating experience at school, AJ developed PTSD. Following panic attacks and other symptoms he underwent

Case Study: EMDR Treatment – Chris
Case Study: EMDR Treatment – Chris Chris developed severe PTSD after being struck from behind by a lorry while on duty as a Police Officer.

Case Study: EMDR Treatment – Rachael
Case Study: EMDR Treatment – Rachael Rachael was diagnosed with PTSD as a result of the horrific symptoms she experienced following a surgery. Unfortunately, Rachael

Case Study: EMDR Treatment – Emily
Case Study: EMDR Treatment – Emily Emily underwent EMDR treatment over Zoom to treat her PTSD following a trauma in her job as a Police

Case Study: EMDR Treatment – Alani
Case Study: EMDR Treatment – Alani After her son was hit by a distracted driver, and in ICU for 6 weeks, Alani developed PTSD. She

Case Study: EMDR Treatment – Emma
Case Study: EMDR Treatment – Emma After witnessing her husband having a terrifying seizure, Emma was diagnosed with PTSD. She underwent EMDR treatment and in

Case Study: EMDR Treatment – Jenna
Case Study: EMDR Treatment – Jenna Jenna* was diagnosed with PTSD as a result of an ‘incomplete’ miscarriage and the inconsistent and traumatic care that

Case Study: Sam’s EMDR Treatment
Case Study: Sam’s EMDR Treatment Sam underwent EMDR treatment after being diagnosed with C-PTSD following multiple and sustained traumas in childhood. Here, Sam explains more

Case Study: Jasmine’s EMDR Treatment
Case Study: Jasmine’s EMDR Treatment Jasmine underwent EMDR treatment after being diagnosed with PTSD following a trauma. Here, Jasmine explains more about her EMDR treatment,

Case Study: EMDR Treatment – Sophie
Case Study: Sophie’s EMDR Treatment Sophie* underwent EMDR treatment after being diagnosed with PTSD following a trauma. Here, Sophie explains more about her EMDR treatment,

Case Study: EMDR Treatment – Darren
Case Study: EMDR Treatment – Darren Darren* was diagnosed with PTSD as a result of a medical emergency and underwent EMDR treatment which he says

Case Study: EMDR Treatment – Claudia
Case Study: EMDR Treatment – Claudia Claudia* was diagnosed with PTSD as a result of a number of traumatic events in her life and underwent

Case Study: EMDR treatment-Melissa
Case Study: Melissa’s EMDR Treatment Melissa* underwent EMDR treatment after being diagnosed with PTSD following a medical emergency which resulted in an induced coma. Here,
Hello! Did you find this information useful?
Please consider supporting ptsd uk with a donation to enable us to provide more information & resources to help us to support everyone affected by ptsd, no matter the trauma that caused it, ptsd uk blog.
You’ll find up-to-date news, research and information here along with some great tips to ease your PTSD in our blog.

Finding Safety After Trauma – Guest Blog: Finley De Witt In this guest blog by Finley De Witt, Finley explores how to regain a sense of safety after experiencing trauma. Drawing from their experiences as a trauma practitioner and client,

Sunflower Conversations
Sunflower Conversations with PTSD UK We’re delighted to be working alongside the team at Hidden Disabilities Sunflower to raise awareness of PTSD and C-PTSD, and this month, they invited our Business development Manager, Rachel to appear on their podcast… You

PTSD Awareness Day 2024
PTSD Awareness Day 2024 This Thursday, 27th June 2024 marks International PTSD Awareness Day and we’d love for you to get involved and help us raise our voice, shout louder and drive towards our mission to help support EVERYONE affected

Rebellious Rebirth – Oran: Guest Blog
Rebellious Rebirth – Oran: Guest Blog In this moving guest blog, PTSD UK Supporter Oran shares her personal story after a traumatic event brought childhood traumas to the surface. Dealing with Complex PTSD, Oran found solace in grounding techniques and

Ralph Fiennes – Trigger Warnings Response
Guest Blog: Response to Ralph Fiennes – Trigger warnings in theatres This thought-provoking article has been written for PTSD UK by one of our supporters, Alex C, and addresses Ralph Fiennes’ recent remarks on trigger warnings in Theatre. Alex sheds

Please don’t tell me I’m brave
Guest Blog: Living With PTSD – Please don’t tell me I’m brave ‘Adapting to living in the wake of trauma can mean maybe you aren’t ready to hear positive affirmations, and that’s ok too.’ and at PTSD UK, we wholeheartedly
Treatments for PTSD
It is possible for PTSD to be successfully treated many years after the traumatic event occurred, which means it is never too late to seek help. For some, the first step may be watchful waiting, then exploring therapeutic options such as individual or group therapy – but the main treatment options in the UK are psychological treatments such as Eye Movement Desensitisation Reprogramming (EMDR) and Cognitive Behavioural Therapy (CBT).
Traumatic events can be very difficult to come to terms with, but confronting and understanding your feelings and seeking professional help is often the only way of effectively treating PTSD. You can find out more in the links below, or here .
Creating a Treatment Plan for PTSD: What to Include + Example
Experiencing trauma is, unfortunately, something that many individuals experience at some point in their lives.. Normative reactions to traumatic events include shock, fear, sadness, anxiety , difficulty sleeping, and intrusive thoughts or memories related to the events, all of which tend to resolve over time. When these symptoms are persistent, or worsen over time, the individual may have developed post-traumatic stress disorder ( PTSD ), which usually required treatment from mental health professionals. Keep reading to learn how you can create an evidence-based treatment plan for PTSD and what you should include (with an example).
The exact prevalence of PTSD is unknown because there has yet to be a survey asking every U.S. resident about their trauma history and related mental health concerns. The research we do have estimates that about 6% of the U.S. population will experience PTSD during their lifetime. It is believed that 5% of the U.S. population is living with PTSD every day, which is approximately 13 million individuals. Women are more likely to develop PTSD when compared to men who experience traumatic events. Additionally, Veterans are at a higher risk of developing PTSD when compared to civilians, especially those who are deployed to a war zone
Setting Goals and Objectives With Clients in Your PTSD Treatment Plan
When you begin thinking about PTSD treatment plan goals for your client, it is important to reflect on the information you have gathered in previous sessions. More specifically, their current symptoms and their severities, as well as how these symptoms are affecting their functioning. This will give you insight into what goals would be impactful, as well as realistic, for your client at this point in their journey. It will be important to consider the presence of other mental health concerns, including substance use disorders, depression , anxiety, dissociative disorders, and personality disorders, as these too should be addressed within a treatment plan.
Clinicians who provide treatment for PTSD tend to have a theoretical approach that they gravitate towards, which they have likely received training and supervision for. There are several evidence-based approaches that can be used for treating PTSD, some of which can be used in a group or individual setting. The following theories have clinical evidence demonstrating their effectiveness in reducing PTSD symptoms:
- Cognitive-Behavioral Therapy ( CBT )
- Eye Movement Desensitization and Reprocessing Therapy (EDMR)
- Prolonged Exposure Therapy (PE)
- Cognitive Processing Therapy (CPT)
- Acceptance and Commitment Therapy (ACT)
What to Include in a Treatment Plan for PTSD + Example
For the remainder of this resource, we will elaborate on various components of a PTSD treatment plan example that will use CPT as its treatment modality. With this, we will be craft components of a treatment plan that aligns with the following case study:
Jane is a 28-year-old female who was referred to counseling after a follow-up appointment with her primary care physician. Jane survived a car accident 4 months ago where she was hit by an impaired driver while driving her 4-door sedan. She experienced serious physical injuries, and was in her local ICU for a couple weeks to manage her conditions. After her release, she was referred to physical therapy and her primary care physician for further treatment. She has been attending physical therapy as scheduled, and feels as though she is making progress in that regard. Her primary care physician has discontinued her use of pain medications, and referred her to a mental health treatment provider for her continued psychological distress. Symptoms discussed in her intake session included intrusive thoughts and memories of the accident, flashbacks, nightmares, being startled easily, irritability, and poor concentration. Jane cannot drive because of her physical injuries, and she avoids being in cars when possible. She reported feeling more comfortable when traveling in a larger vehicle, such as an SUV or pickup truck because it is never safe to drive in cars. At this point, Jane’s symptoms have been present for over 3 months, and have significantly impacted her ability to attend appointments, focus on work, and complete day-to-day tasks. She has also reported relationship distress with her partner, noting that she does see her irritability as a common thread in their arguments.

Trauma Worksheets Bundle PDF Templates

Counseling Treatment Plan Template Editable PDF
View our Counseling treatment Plan that corresponds with this resource or view all of our Trauma Worksheets
Agencies Involved and Plans for Care Coordination
When we look at Jane’s case, it would be appropriate to be in contact with her primary care physician, as they were the referral source. Your contact could be as brief, or descriptive as you deem necessary, and Jane is comfortable with. Based on the symptoms described, Jane may be a suitable candidate for Psychotropic medications, which means that a referral to a psychiatrist may be warranted.
Example for Jane:
Other Agency : Primary Care Physician
Plan to Coordinate Services : Call XXX-XXXX to verify information reported in session, follow up as needed
Other Agency : Licensed Psychiatrist (referral)
Plan to Coordinate Services : initiate referral for evaluation based on reported PTSD symptoms
Clinical Diagnoses
Based on the information provided, it sounds as though Jane is experiencing PTSD. Her car accident was an experienced trauma which caused serious injuries, resulting in a hospital admission. She endorsed intrusive symptoms, negative cognitions, avoidance of stimuli related to the accident, and changes in arousal and reactivity.
There are a number of clinical assessments that can be used during an assessment to screen for PTSD as well as formulate a diagnosis, and track changes in symptoms, including:
- Clinician-Administered PTSD Scale (CAPS)
- PTSD Checklist for DSM-5 (PCL-5)
- Impact of Event Scale-Revised (IES-R)
- Davidson Trauma Scale (DTS)
- Post-traumatic Stress Disorder Checklist (PCL-C)
- Trauma Symptom Inventory-2 (TSI-2)
- Harvard Trauma Questionnaire (HTQ)
- Post-Traumatic Stress Disorder, 309.81
- Supporting Assessments: PCL-5 score of 56
Current Medications and Responses
At this time, Jane is not currently taking medications, as her primary physician ended her pain medication prescription recently. If you provide a referral to a psychiatrist, this area could be updated to reflect changes that occur in Jane’s medication regimen.
None at this time/ N/A/ N/A/ N/A
Presenting Problem and Related Symptoms
This area of your treatment plan will provide a detailed account of Jane’s symptoms, and the effect that they have been having on her overall level of functioning.
Client has indicated the presence of intrusive thoughts and memories, flashbacks, nightmares, being startled easily, irritability, and poor concentration, since being in a traumatic vehicle accident that resulted in serious physical injuries. Avoidance symptoms are present, as she avoids being in smaller care. Her level of functioning has been impaired, and she struggles with her concentration and focus, and is experiencing interpersonal challenges, which she attributes to her mental health.
Goals and Objectives
Identified goals often require long-term focus and commitment, which should also be realistic, attainable, and specific. Objectives are smaller, or short-term goals, that fall under the scope of overarching goals on a treatment plan. Breaking larger goals down into digestible sections can make them feel more manageable and less intimidating for clients.
Examples Jane:
Problem/Symptom : Intrusive Symptoms
Long-Term Goal : Improve ability to identify, modify, and cope with intrusive symptoms
Objective 1 : Jane will learn to identify and challenge maladaptive thoughts related to the traumatic event(s) during therapy sessions.
Objective 2 : Jane will practice using cognitive restructuring techniques to reframe intrusive memories and flashbacks, reducing their frequency and intensity.
Objective 3 : Jane will develop and implement coping strategies , such as grounding techniques or guided imagery, to manage distressing intrusive symptoms outside of therapy sessions.
Problem/Symptom : Avoidance Behaviors
Long-Term Goal : Decrease arousal resulting from triggers that cause avoidance behaviors
Objective 1 : Jane will create an avoidance hierarchy, ranking avoided situations or triggers related to the traumatic event(s) from least to most anxiety-provoking.
Objective 2 : Jane will gradually confront avoided situations or triggers in a controlled and systematic manner, using exposure techniques during therapy sessions.
Objective 3 : Jane will monitor and challenge avoidance behaviors outside of therapy sessions, gradually increasing engagement in avoided activities or situations over time.
Problem/Symptom : Negative thoughts and beliefs affecting emotions and behaviors
Long-Term Goal : Modify Negative Beliefs and Thoughts
Objective 1 : Jane will identify and record negative beliefs about themselves, others, and the world related to the traumatic event(s) during therapy sessions.
Objective 2 : Jane will critically evaluate and challenge negative beliefs using evidence-based cognitive restructuring techniques, such as examining evidence for and against the beliefs.
Objective 3 : Jane will practice adopting more balanced and adaptive beliefs about themselves, others, and the world outside of therapy sessions, reinforcing positive changes through daily journaling or self-reflection exercises.
Specific Interventions to Be Used
In Jane’s case, it is important to be mindful of evidence-based approaches for her symptoms and the goals she is working towards. This example treatment plan will utilize CPT as its therapeutic approach, with tailored interventions, specific to Jane’s needs.
Intervention/Action : Psychoeducation about trauma and PTSD
Responsible Person : Counselor A
Intervention/Action : Socratic Questioning
Intervention/Action : Use of Thought Records
Responsible Person : Jane
Intervention/Action : Decatastrophizing
Intervention/Action : Relaxation techniques including, but not limited to, deep breathing, progressive muscle relaxation, and guided imagery
Family Involvement
Social support is a common component of biopsychosocial assessments, which would allow you to identify individuals in her life that are supporting her through this challenging time in her life.
Jane wishes to involve her partner and is open to the use of joint sessions to focus on healthy communication and improving the status of their relationship.
Additional Services and Interventions
Additional services would include other interventions used to provide whole-person care. This could include support groups, or couples counseling with her partner if she was agreeable to do so.
- Provide Jane with a referral for local PTSD support group
- Provide Jane with referral to a psychiatrist for assessment of symptoms, and exploration of possible psychotropic medications
Estimation for Completion
The time frame associated with CPT falls between 12 and 16 weeks, as this is a structured and time-limited treatment approach. Counseling sessions may occur weekly or bi-weekly, and the duration of care would be dependent on the severity of Jane’s symptoms.
12 weeks; can be adjusted if needed
Aftercare Plans
Aftercare plans should be included in a treatment plan as a safety measure in case she ends her therapeutic alliance by terminating, for any reason. Aftercare plans can be updated during treatment plan review, to reflect progress and changes in symptoms.
- Referral for licensed therapist, psychologist, or psychiatrist
- Local treatment centers that specialize in PTSD treatment
- Community Mental Health Treatment Centers
- Local support groups for PTSD
Final Thoughts On Creating a Treatment Plan for PTSD
Thank you for reading this resource on creating a treatment plan for PTSD. Trauma therapists are compassionate and supportive clinicians, devoting their time to creating a safe and supportive environment promoting healing for the individuals they work with. Evidence-based treatment approaches have been proven effective, and often provide clinicians with flexibility to adjust care to fit the needs of their client. TherapyByPro provides Treatment Plan Templates that can be used with clients who have an array of mental health concerns, including PTSD.
TherapyByPro is an online mental health directory that connects mental health pros with clients in need. If you’re a mental health professional, you can Join our community and add your practice listing here . We have assessments, practice forms, and worksheet templates mental health professionals can use to streamline their practice. View all of our mental health worksheets here .
- “Post-Traumatic Stress Disorder.” National Institute of Mental Health. Accessed March 27, 2024. https://www.nimh.nih.gov/health/topics/post-traumatic-stress-disorder-ptsd .
- “PTSD: National Center for PTSD.” U.S. Department of Veteran Affairs, September 13, 2018. https://www.ptsd.va.gov/understand/common/common_adults.asp .
Author: Kayla Loibl, MA, LMHC
Kayla is a Mental Health Counselor who earned her degree from Niagara University in Lewiston, New York. She has provided psychotherapy in a residential treatment program and an outpatient addiction treatment facility in New York as well as an inpatient addiction rehab in Ontario, Canada. She has experience working with individuals living with a variety of mental health concerns including depression, anxiety, bipolar disorder, borderline personality disorder , and trauma.
Ready to Take Your Practice to the Next Level?
Explore our great partner sites to help you improve your practice:
Advertisement
SimplePractice

- Easy-to-use notes and documentation template library
- Increase client satisfaction and decrease no-shows with automated appointment reminders
- Client portal offers clients one easy place where they can schedule, complete paperwork, pay, and more
TherapyByPro Special Offer: Get up to 2 months free, No Credit Card Required

- $60 to $70 per week, billed every 4 weeks
- Receive therapy via messaging, phone, or live video
- Flexible option to cancel at any time
Take 20% off your first month

- $69 to $129 per week, billing flexible
- Psychiatric services and prescription management available
Use code 'SPACE' for $100 off your first subscription

Join Over 5000 Other Mental Health Pros
Subscribe to our TherapyByPro community to receive tips to help you better serve your clients and grow your practice.
CASE REPORT article
Case report: psychotherapy of a 10-year-old afghani refugee with post-traumatic stress disorder and dissociative absences.
Parts of this article's content have been modified or rectified in:
Erratum: Case Report: Psychotherapy of a 10-year-old Afghani refugee with post-traumatic stress disorder and dissociative absences
- Read erratum

- 1 Child and Adolescent Psychiatry Service, Lausanne University Hospital, Lausanne, Switzerland
- 2 Department of Psychiatry, Lausanne University Faculty of Biology and Medicine, Lausanne, Switzerland
- 3 Department of Child and Adolescent Psychiatry, New York University Grossman School of Medicine, New York, NY, United States
Violence-related post-traumatic stress disorder (PTSD) in the context of war and terrorism has become an increasingly pressing public health issue relevant to refugee children and families. PTSD and related psychopathology in children can adversely affect all domains of development and, in particular, interfere with learning and socialization. When the experience of violent trauma and related loss is shared with the entire family, resulting impairment and distress may prevent caregivers from being psychologically available to process their traumatized children’s emotional communication and otherwise meet their children’s developmental needs. When children suffer from PTSD, it may be impossible to put their experience and related thoughts and feelings into words, let alone a coherent narrative. The latter difficulty can be even more pronounced when the child displays dissociative symptoms, possibly signaling a dissociative subtype of PTSD. Thus, the narrative within the child’s play during psychotherapy becomes all the more important as an indicator of the child’s internal world. This case report is an example both of evaluation and of psychotherapy that is both psychodynamic and trauma-informed with a 10-year-old Afghani boy who suffered the violent loss of his father at age of 3 years, leading to his immigration to Switzerland. This paper addresses the question of how the psychotherapist can accompany the child through the elaboration of his trauma and how the therapist can contribute to the co-construction of a coherent narrative of the child’s experience and to the restoration of an intersubjective connection between the traumatized child and caregiver.
Introduction
Children are exposed to war, terrorism, and other forms of interpersonal violence worldwide. Psychological and developmental sequelae can be particularly noxious when any form of violence leads to parental loss. Post-traumatic stress disorder (PTSD) affects all domains of children’s social-emotional development, resulting often in disruptive behavior, heightened vigilance, and dissociative symptoms that ensue to protect the child from overwhelming threat, yet when generalized after the threat has passed, can interfere with learning and socialization. When multiple family members suffer from violence-related PTSD, their respective symptoms may prevent them from responding sensitively to each other’s suffering and developmental needs ( 1 ). It may be impossible for traumatized children to communicate their experiences, depending on their capacity for symbolization and verbal expression. Even if verbal, if the child has PTSD and, in particular, manifests a dissociative subtype of PTSD with prominent emotional numbing, derealization, and depersonalization ( 2 ), a coherent narrative about traumatic experiences may be extremely challenging. Play, especially for young children, becomes the primary means of communication. The more helpless and alone children feel in a violent environment, the more they try to control traumatic memories and related emotional dysregulation beyond their control through solitary play repeatedly reenacting the events (a.k.a. “post-traumatic play”) ( 3 ). One often neglected “side-effect” of post-traumatic play, is that it can trigger PTSD symptoms in the surviving family members, impairing the surviving parent’s emotional availability and ability to connect intersubjectively with their child ( 4 ).
In a trauma-informed psychodynamic psychotherapy model, the psychotherapist plays the role of a “mentalizing third” ( 5 ) who is an individual observer and not being part of the relational system of the two individuals coming for consultation—such as a mother-child dyad. This mentalizing third expressly thinks about and holds in mind the parent’s and child’s thoughts, feelings, and intentions, while also taking their perspective and potential biases into account. So, how can a psychotherapist—within that specific model of psychotherapy—endorse the function of that mentalizing third so that the parent and child can internalize or integrate that kind of metacognitive monitoring into their exchanges about their shared traumatic experiences—such as sudden loss—even in the absence of the psychotherapist?
Case description
In this article, we will present a case report of the therapy that is both psychodynamic and trauma-informed, of Mustafa 1 a 10-year-old Afghani immigrant to Switzerland referred for psychotherapy in the context of being assigned to a therapeutic school because of scholastic and behavioral problems. His teachers wondered whether he suffered from Attention-Deficit/Hyperactivity disorder (ADHD). During his first session, his therapist noted a lot of anxiety, which appeared to trigger his externalizing symptoms. Mustafa displayed multiple fears of injury and aggression triggered by ordinary loud sounds (e.g., pencils rolled in their aluminum box) or by peers (e.g., anger outbursts), and when asked about his mental “absences” Mustafa said—believing he was asleep— “I had a nightmare.” This curious symptom observed both in the classroom, in therapy sessions, and at home by his family contained elements of derealization (seems like a “nightmare”) and depersonalization (Mustafa saw himself “sleeping” as if being outside himself and sleeping at the same time). Further history revealed that Mustafa who is of Hazara ethnicity was forced to leave Afghanistan with his family in 2015 at 4 years old due to persecution of the Hazara and the murder of his father by the Taliban. He was shot at close range as he attempted to protect Mustafa’s older brother. Mustafa—who did not likely witness that—was in earshot, with his aunt rushing him to safety next door. After the murder, Mustafa, his mother, older brother, and sister left Afghanistan and arrived in Switzerland after a 3-month journey. His sister described their immigration as long, difficult, and triggering persistent fears of loss. It was fraught with the uncertainty of difficult passages in secret across mountainous regions in which there was a risk of further attacks within Afghanistan. They were unsure of whether they would have enough food and water, or if they would ever be able to return for their belongings as they were only able to take what they could carry in a small backpack. They did not know if they would ever again see the family whom they left behind. Subsequently, the family faced placement and resettlement in settlement camps where they feared illness, maltreatment, and met the uncertainty of not knowing where they would be sent next, if they would be able to stay together, and if they would be able to remain where they were sent and to thrive. Moreover, when the family finally arrived in Switzerland, they were left on their own, with very little information given about where they were, where they could get food, where they will be next and how long it would take to complete the immigration legal process.
Diagnostic assessment
During his first school year in Switzerland, the patient presented with motor restlessness, difficulty concentrating and impulsive behavior, emotional dysregulation, as well as recurrent disruptive behavior in class including aggression toward his peers. For that reason, he was transferred to a therapeutic school (with fewer students and more teaching staff). There, the patient presented additional, transient “absences” during which the patient did not seem to hear the adults speaking to him and appeared to stare and to be internally preoccupied. He also displayed startle responses to abrupt sounds or agitation by his peers. After being startled, he seemed disorganized. At that time, he admitted having intrusive, frightening images of faceless men fighting, holding weapons, women and children crying, and nightmares of intruders, monsters. The patient also exhibited avoidance and emotional numbing during verbal and physical conflicts between classmates as well as hypervigilance and irritability. He complained of fatigue due to awakening in the night, worries about his mother and other people in Afghanistan, and fears that something bad would happen again to him and his family. Re-experiencing, avoidance, hyperarousal, and negative cognition symptoms according to the DSM-5—strongly suggested a diagnosis of PTSD related to early experiences in civil war-torn Afghanistan. Moreover, the patient’s symptoms involving the moments of absences—not consistent with any neurological difficulties, but rather feeling as if he was in a dream or movie and looking at himself and his classmates from afar (i.e., derealization and depersonalization), pointed toward the specific subtype of PTSD—called dissociative PTSD—which is characterized by abnormally high activation of several brain regions associated with emotional regulation and arousal modulation ( 2 ). We did not feel that Mustafa’s dissociative symptoms were pervasive enough to say that he had a dissociative disorder independent of PTSD of a dissociative subtype.
The patient’s clinical picture at the time could have also suggested complicated bereavement. However, given that Mustafa was only 3-year-old at the time of his father’s murder by the Taliban, he would not yet have been developmentally able to comprehend cognitively the finality of death—a cognitive milestone that only occurs around the average age of 7 years. Another differential diagnosis came to the professional’s mind: ADHD. Indeed, aside from the agitation and poor focus capacities, the patient was particularly absent during the play in therapy. Nevertheless, this can be understood by the fact that the symbolic play done during the psychotherapy sessions involved re-experiencing the traumatic events surrounding his father’s murder. The patient would present dissociative symptoms as mentioned above that can easily be confused with an attentional disorder. At the beginning of the therapy, we put this diagnosis of ADHD on hold as a pending treatment of the patient’s PTSD, knowing that the two disorders may be comorbid. However, in our opinion, the PTSD symptoms were more prominent, distressing, and troublesome at the time of assessment. However, after 2 years of therapy, while the PTSD symptoms were improving (fewer dissociative episodes, less conflict with peers, and hypervigilance), the patient was still having difficulty concentrating in the class as well as learning disabilities. Therefore, we decided to screen him for ADHD, which confirmed this co-morbid diagnosis.
Course of psychotherapy
During the first 4-month-long phase of treatment, Mustafa was agitated, inattentive, and hypervigilant (e.g., abruptly looking at the door if he heard someone in the hall). He presented dissociative symptoms, such as those described above and also in the form of what could have been considered a hallucination if Mustafa had not been able to test reality just after the odd perception: while looking at a toy he said, “I thought it was a severed head [but I knew it was not].” Although he remained compliant, Mustafa’s play was disorganized, without significant interactions between characters ( 1 ). One character emerged in every session: an all-powerful monster—represented by a vampire—who repeatedly killed a “man,” a “sister,” or a “brother.” The killings that Mustafa staged were brutal, without escape, and the therapist felt like a helpless onlooker as Mustafa—with his back turned toward her—ignored and refused any help or participation in the play. During that phase, the mother was reluctant to see her son’s new therapist. Indeed, during the first interview at her son’s new school, she was asked to tell her story. Following this interview, Mustafa’s mother stated that she “did not want to answer any more questions about Afghanistan.”
During the second phase of psychotherapy, lasting 6 months, Mustafa repeated battle-scenes between a little boy, a sister, and a brother trying to escape a monster that came to harm, abduct, or kill them. As the therapeutic alliance strengthened, Mustafa allowed the therapist to join in his play and to insert a trustworthy policeman who restored justice. The combat and killing in his play decreased in intensity and frequency; the monster became less powerful or at least, easier to capture. The father’s character remained absent from the play: “He’s dead” or “There is no father,” declared Mustafa when his therapist asked him about the presence of his father. This shows how avoidant Mustafa had been concerning his father’s memory. His behavior mirrored the avoidance he experienced at home. His sister told the therapist that there were no pictures or mention of their father in the house. In addition, when Mustafa asked the therapist if she thought that he had “the same hair as my father,” she responded by asking him if his mother would know. Mustafa responded: “Mom says that she cannot tell how he [his father] looked,” “I think he looked like nothing.” Mustafa was thus very afraid to activate his mother’s PTSD symptoms. We speculate that Mustafa would not thereafter speak about his father or play out scenarios that he did during therapy, at home. During that time, the mother came for an interview. The therapist—seeing that she was very defensive and gaze-avoidant—said that “she does not have to repeat her story.” She encouraged the mother to talk about her son to create a safe place and positive alliance before eliciting the trauma narrative.
It would not be until after the summer, during the 2nd year and third phase of psychotherapy, that Mustafa spontaneously talked about his father. One day, he brought a drawing to his session—a school assignment to tell the story of a family member. Mustafa said, “It’s for my father, but he cannot receive it because he is dead.” Then, while mimicking pointing the gun at his head, he said, “He (my father) was shot by the Taliban in the dark.” Mustafa asked his therapist: “Is your father dead too?” to which she responded: “No, but I would be very sad and angry if he was.” Psychotherapy thus offered Mustafa a safe place with an emotionally present therapist with whom he could experience the existence of his father.
Since then, Mustafa’s play changed: a father-figure appeared and fought the monster with the boy. Turning passive to active, Mustafa could avert tragedy in play that he could not in life. The monster weakened and failed to kill more people. Subsequently transformed as a “teddy-bear-monster.” Mustafa described him as “the little boy’s new friend,” “a part of the family.” Fewer dissociative episodes were reported along with less agitation at school.
After 18 months into therapy, the United States Army exited Afghanistan, leaving it in the hands of the Taliban. Innocent people were hurt, killed, and forced to leave. This was extremely stressful for Mustafa and his family—because of their relatives and friends there. It triggered renewed helplessness in Mustafa’s post-traumatic play: the monster returned ferociously, and the father became a weaker character. The boy became “the hero of the story” who could save everybody. Mustafa described the mother as “going crazy because she’s too stressed.” She was left aside, unable to fight the monster “because she’s too tired.” Mustafa presented characters who were dismembered, echoing news that a cousin’s hands were “chopped off” by the Taliban. At that time, the therapist saw the mother again. She appeared depressed, fearful for her brother in Afghanistan, and described his condition there: “He has to hide from the Taliban, they come into people’s home and kill and mutilate them.” Nevertheless, Mustafa’s mother was less defensive than previously. The therapist was able to tell her that her son “had lived really difficult things and that he is traumatized and that he needs therapy to speak about that trauma.” She listened tearfully. The mother then said of Mustafa playing at home: “He makes up stories in French, which I cannot understand.” When the therapist asked her if Mustafa was speaking about Afghanistan at home, she replied that her son “never speaks about Afghanistan at home … maybe he thinks that it can make me sad.” At that moment, the therapist, seeing that the alliance was positive and that the mother would speak about her and her son’s trauma, said to the mother: “You are both in your own pain and I think it will be less frightening if you come together. My role is to accompany you both in that.” To which the mother replied: “Ok, when can I see you again?”
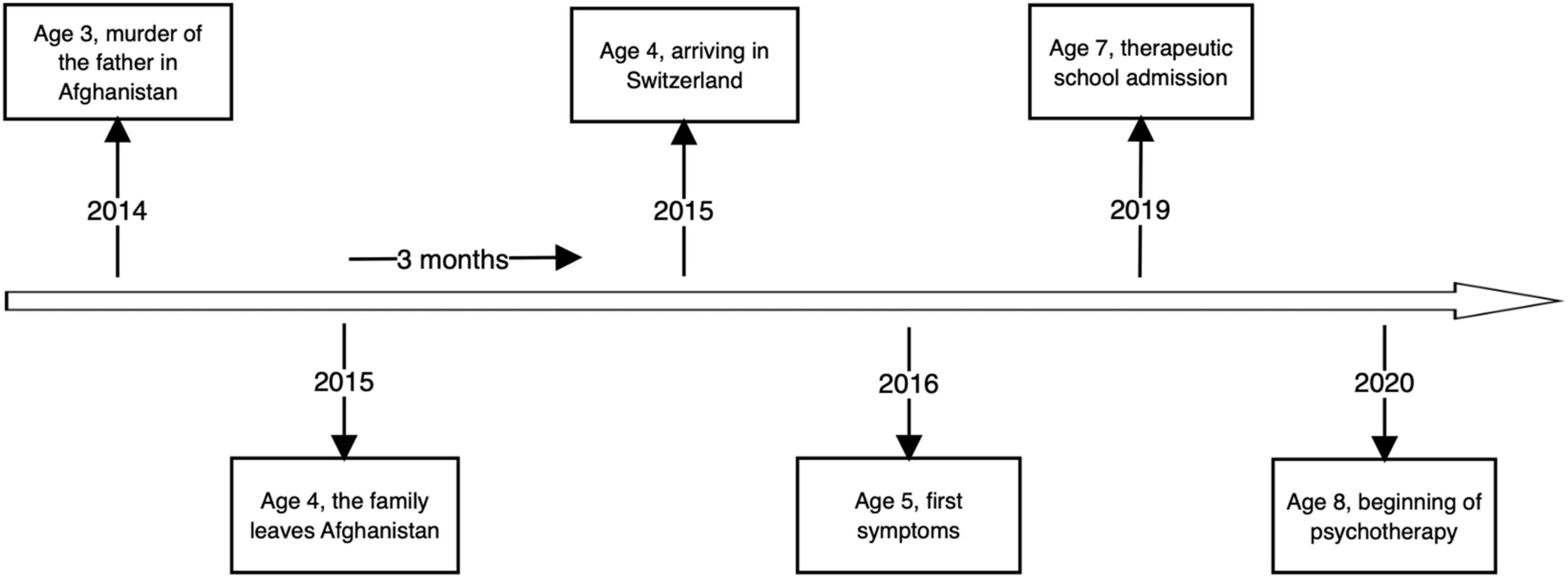
This report presented the case of a 10-year-old Afghani refugee boy who at the age of 3 years, experienced the murder of his father in the context of civil war, and then the stress of immigration and loss of his homeland. Post-traumatic play therapy following these experiences, that is to say, both psychodynamic and trauma-informed allows for imaginal exposure to traumatic memory traces, memory recontextualization, and reconsolidation with help of the therapist’s mentalizing stance (mentalizing third). In this psychotherapy, the therapist helped the patient clarify the Taliban’s murder of his father and loss of homeland that Mustafa had experienced as a helpless preschool-age child. Mustafa could, during the course of psychotherapy at the age of 10 years, form a more coherent trauma narrative, rediscover earlier memories of shared experiences while his father was still alive, and also confront and attribute meaning to the pain of his and his mother’s losses, she having also likely suffered from complicated bereavement. Mustafa’s empowerment through the restoration of justice in his play with the help of his therapist allowed what had been frozen in the compulsive repetition of post-traumatic play to evolve, while simultaneously distinguishing Mustafa’s safe, present context in Switzerland from his dangerous, past context in Afghanistan. The connection between the child and the therapist permitted the sharing of an intersubjective field that had been foreclosed in his relationship with his traumatized mother who could not intersubjectively join with him despite their shared traumatic experiences because of her own complicated bereavement, PTSD symptoms, and depressive state that ensued. The authors assert that mutative effects were enhanced in the treatment by the psychotherapist who played the role of a mentalizing, emotionally regulating third ( 5 ), who helped explicitly to link memory traces, affects, and behaviors related to Mustafa’s traumatic experiences that had been dissociated from one another. During the course of this 2-year long psychotherapy, the patient and the family’s avoidance of traumatic and non-traumatic memories of the lost father diminished and the patient’s PTSD and dissociative symptoms remitted, and his functioning improved both scholastically, socially, and with respect to his relationship with his deeply traumatized mother.
Patient perspective
At the beginning of the psychotherapy—as described above—it was difficult if not impossible for the therapist to talk about the trauma with the patient. Gradually, the therapist was able to bounce back and forth on the elements brought into the trauma play by the patient and name the difficult events the patient had experienced. For example: “This little boy in the story looks very scared. Have you ever been very scared like the little boy?” To which the patient would respond, “Yes, for example in Afghanistan.” Following these brief inclusions during the sessions, the therapist was able to name the patient’s trauma: “You experienced difficult events when you were a child, in Afghanistan, and here you can talk about them so that they do not come back to you all of a sudden, during the day, at times when you do not want them to come back and where they can scare you.” The trauma named clearly in the therapy, gave the patient the possibility to talk about it spontaneously in the game or by revealing his worries: “Are there Taliban in Switzerland?”
Similar work could be done with the patient’s sister and mother. During the first few meetings, it was impossible to talk about the trauma. Mustafa’s mother refused to talk about Afghanistan and the trip to Switzerland, and the sister denied that the patient could remember anything at all, given his young age. As the therapeutic alliance strengthened, the therapist was able to reveal elements of the sessions to his family: “He makes up a lot of stories about people fighting, about children using guns, and he tells me that he remembers that in Afghanistan young children have guns. He is also very afraid of loud noises [that sound like gunfire]. Does this sound familiar?” To which the family responds, “ In Afghanistan there are sounds of shooting and bombs often. Maybe he remembers that.” From that point on, it was easier for the family to accept the patient’s psychotherapy because they could understand its importance in making sense of Mustafa’s early experience of the trauma and loss of war and subsequent displacement.
Data availability statement
The datasets for this article are not publicly available due to concerns regarding participant/patient anonymity. Requests to access the datasets should be directed to the corresponding author.
Ethics statement
Ethics review and approval/written informed consent was not required as per local legislation and institutional requirements.
Author contributions
OS: scientific contribution. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Open access funding was provided by the University of Lausanne.
Acknowledgments
We would like to thank Prof. Schuyler Henderson, Associate Clinical Professor of Child and Adolescent Psychiatry, NYU Grossman School of Medicine, United States for his helpful comments on an earlier manuscript.
- ^ Fictitious name.
1. Schechter DS, Zygmunt A, Coates SW, Davies M, Trabka KA, McCaw J, et al. Caregiver traumatization adversely impacts young children’s mental representations on the MacArthur story stem battery. Attach Hum Dev. (2007) 9:187–205. doi: 10.1080/14616730701453762
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, et al. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry. (2010) 167:640–7. doi: 10.1176/appi.ajp.2009.09081168
3. Terr LC. “Forbidden games”: post-traumatic child’s play. J Am Acad Child Psychiatry. (1981) 20:741–60. doi: 10.1097/00004583-198102000-00006
4. Schechter DS. And then there was intersubjectivity: addressing child self and mutual dysregulation during traumatic play: in memory of Louis sander. Psychoanal Inq. (2019) 39:52–65. doi: 10.1080/07351690.2019.1549911
CrossRef Full Text | Google Scholar
5. Ogden TH. The analytic third: implications for psychoanalytic theory and technique. Psychoanal Q. (2004) 73:167–95. doi: 10.1002/j.2167-4086.2004.tb00156.x
Keywords : post-traumatic stress disorder (PTSD), dissociation, refugee mental health, psychotherapy, post-traumatic play, intersubjectivity
Citation: Junod N, Sidiropoulou O and Schechter DS (2022) Case Report: Psychotherapy of a 10-year-old Afghani refugee with post-traumatic stress disorder and dissociative absences. Front. Psychiatry 13:940862. doi: 10.3389/fpsyt.2022.940862
Received: 10 May 2022; Accepted: 27 June 2022; Published: 22 July 2022.
Reviewed by:
Copyright © 2022 Junod, Sidiropoulou and Schechter. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nastia Junod, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Nursing Case Study for (PTSD) Post Traumatic Stress Disorder
Watch More! Unlock the full videos with a FREE trial
Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mr. Bryant is a 32-year-old male who presents to the emergency room brought by law enforcement for what they describe as possible public drug or alcohol intoxication along with erratic and aggressive behavior. He was outside a local bar and patrons called 911. Law enforcement officers (LEOs) seek medical clearance before proceeding any further and present a Veteran Health Care ID card identifying Mr. Bryant. The patient is resisting officers and saying he has to, “…save my buddies. They are down range and there’s explosions and gunfire. Can’t you hear it? Let me go so I can help them!” He also points at the LEOs and whispers to the nurse, “These guys captured me. They’re not on our side.”
What assessments and initial check-in activities should the nurse perform to best assist the patient and law enforcement?
- The priority for this patient and staff is SAFETY. First, place the patient in a gown, removing all potential dangers; this step is vital for security and safety, and it also helps the nurse to begin a full head-to-toe assessment which is the first step of the nursing process. He should be screened for suicide and asked specifically if he has a plan. Signs of injury or hints to the patient’s history can guide the plan of care and next interventions. Determining his veteran status may help with obtaining medical history as well as to guide nursing interactions to help alleviate the paranoia he seems to be exhibiting. Next, asking LEOs to leave the room will afford the patient his right to privacy and protection of his personal health information to which he is entitled. LEOs may remain nearby (i.e. outside of the room)
What orders does the nurse expect the provider to give?
- Psychiatric precautions like placing in a gown, removing personal items, searching for weapons, suicide/harm screening should be expected. Diagnostics to rule out medical issues like vital signs, urine drug screen/blood alcohol level, blood work, and IV start are all orders to anticipate. The IV may be needed for urgent/STAT med orders. Further diagnostics (i.e. radiology, etc.) might be anticipated only after initial screening gives data. For example, high HR and BP may warrant an EKG. Signs of trauma may warrant an XRay or CT scan. Similarly, referrals may be necessary, but not initially.
After screening and assessing the patient, the nurse has the following data:
Patient is able to follow instructions after LEOs step out of the room. He removes his clothing with assistance to be placed in a gown and on a monitor. He voids unassisted, but supervised, for a urine sample. Offers no resistance to IV placement and blood draw.
He frequently looks around and seems hyperalert. He is unable to articulate his exact location, only saying, “I’m at a hospital.” PERRLA, moves all extremities. Multiple military-themed tattoos are visible on his arms, chest, back, and legs.
No potential weapons noted. No signs or symptoms of physical assault, skin is intact with no bruising. The patient is wearing military-issued dog tags on a long chain beneath his clothing. Personal items placed in a belongings bag and secured per protocol. He indicates he has not slept for several days due to being out of his medication and says, “I can’t do it anymore. I can’t take the nightmares, so I don’t want to sleep. I just can’t make it.” He denies a medical or psychiatric history only saying, “I go to the VA hospital. They give me meds and therapy, though.”
PRN medications ordered: Lopressor 5 mg IV bolus given over 2 minutes, PRN Normal Saline 0.9% 1000 mL rapid IV bolus, PRN Naloxone 0.4-2 mg IV/IM/SC; may repeat q2-3min PRN; not to exceed 10 mg Lorazepam 1 mg IV, may repeat PRN; not to exceed 4 mg
BP 180/90 SpO2 98% on Room Air HR 112 bpm and regular Ht 182 cm RR 28 bpm Wt 99.8 kg Temp 37.9°C
Prioritize the top nursing interventions. What are some vital interventions and why are they performed in this order?
- Making sure the patient and staff stay SAFE is the priority right now. Placing him in a gown and checking for dangerous items take precedence PRIOR to obtaining labs or monitoring. Reassuring the patient and remaining calm throughout is needed at this time as well. Putting him on a monitor for continuous monitoring is important in case there are sudden changes so that happens 2nd since his initial triage vital signs are outside of parameters but not emergent. Obtaining samples to rule out medical/metabolic concerns vs intoxication is 3rd. Further examining the patient’s statements with therapeutic communication can happen concurrently with medical interventions and help foster a healthy nurse-patient relationship. Based on assessment findings, the nurse could also use a reliable and valid PTSD screening tool like the five-item Primary Care PTSD Screen for the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders. Please note: restraints are not mentioned and should be avoided if the patient is SAFE. If orders for restraints are placed, the provider MUST document as either medical or behavioral. This is not within a nurse’s scope of practice.
Should the nurse administer the PRN medications written by the provider now or question other medication orders? Why or why not?
- No. Firstly, ALL PRN orders need parameters to proceed. I.e. Answer Lopressor IV 5 mg bolus over 2 minutes FOR stated HR and/or BP. These orders do not have any parameters provided. It is beyond a nurse’s scope of practice to administer without the prescriber’s guidance. None of these PRN orders have parameters provided. Also, for each med: For the Lopressor, there is no indication this is a cardiac issue and no frequency/max provided either. For the IVF there is no indication that he is dehydrated, and cardiac status is not known so the nurse should be concerned for possible fluid overload. Also, there is no scientific evidence that NS can impact the alcohol intoxication this patient appears to have. For the naloxone, UDS shows the patient did not ingest an overdosage of opioids and his V/S do not indicate respiratory depression or opioid intoxication (even without labs to prove it). For the Lorazepam, there is no seizure activity and giving this medication may impair the psychiatric screening needed to further assess the situation.
Are there other orders the nurse might anticipate and/or suggest?
- Placing him on suicide precautions would be a good start as it is not harmful and can always be discontinued after further observation/assessments. Obtaining medical records to determine PTSD treatment and/or other conditions would be helpful. Also, seeking expert consultation in the form of a psychiatric consult is in the patient’s best interest.
Are there past medical history concerns specific to this patient and his background that may aid in the plan of care?
- Research indicates that many who suffer from PTSD also have a history of traumatic brain injury and/or other combat trauma. Determining his TBI status may help in obtaining consults (i.e. neurology, occupational therapy, etc.) as well as guiding further diagnostics (does he need a head CT? For example). TBI-related issues may be the root cause of his current behavior but if they are not then psychiatric concerns would be more likely. Finding out all you can about his current treatment plan will help in the present.
After determining the patient is not a harm to himself or others, LEOs release him to the medical treatment facility. A records request produces a brief patient history and treatments he is receiving from the local VA hospital. Records do not indicate any history of physical combat trauma, no traumatic brain injury (TBI). The medication list is available to review and, since some time has passed and the patient has been cooperative and calm, he is conversing appropriately. He concurs with his medications verbally.
Regarding patient medications, what process is necessary for the nurse to perform and why?
- A medication reconciliation should be completed on ALL patients per Joint Commission. From the National Patient Safety Goal literature: “NPSG.03.06.01 Maintain and communicate accurate patient medication information. –Rationale for NPSG.03.06.01– There is evidence that medication discrepancies can affect patient outcomes. Medication reconciliation is intended to identify and resolve discrepancies—it is a process of comparing the medications a patient is taking (or should be taking) with newly ordered medications. The comparison addresses duplications, omissions, and interactions, and the need to continue current medications. The types of information that clinicians use to reconcile medications include (among others) medication name, dose, frequency, route, and purpose. Organizations should identify the information that needs to be collected in order to reconcile current and newly ordered medications and to safely prescribe medications in the future.”
What patient education topics would need to be covered? When? Is this only the nurse’s responsibility?
- Once the patient is determined to be no harm to himself and AA&O enough to participate in self-care (by assessment and provider determination) then staff can provide education with a focus on medication regimen adherence with rationales (i.e. sudden discontinuation of antidepressants may cause sleep disturbances and they should not be taken with alcohol either). Resources for him to seek out if he has suicidal ideation (this should be simple and clearly explained – avoid medical jargon) or thoughts of self-harm. Ensuring he has a support system and the resources to follow up with appropriate parties should be part of the interactive education process. Case management may need to assist in discharge/follow-up recommendations. His family/support system should be included in discharge planning as well. There may be literature or web sources to give to the patient as well so he can participate in self-care.
After sleeping for a few more hours, the patient remains appropriate, cooperative, and calm. HR, BP, RR all decreased. His spouse arrives to take him home. They both verbally acknowledge discharge plans for him to return home with particular emphasis on follow-up with the VA psychiatric team. Mr. Bryant states very clearly that he has no plans to harm himself or others. The nurse documents he is fully alert and oriented x 4 after assessing one more time.
What does oriented x 4 mean? Why is this important?
- Oriented x 4 means oriented to person (who are you? name?), place (where are you? specific), time (time/day/date), and situation (what is going on?) This is vital for this patient because initially, he presented as disoriented. In order for him to be discharged to self-care and able to follow up as directed he must be fully awake and oriented so as not to pose a threat to himself, others, or his future care. This also allows staff to accurately document the level of consciousness at discharge.
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
References:
View the full transcript, nursing case studies.

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions

Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Case Studies PTSD and Post-Traumatic Stress Disorder
Written by Roland Bal
These case studies of PTSD are mostly from people I have worked with over the years, with some fictitious elements added or parts omitted, simply to highlight the mechanisms and dissociation processes of trauma.
- Surgery - Car accident - Rape - Falling accident - Grief/Bereavement - Birth/cesarean
Case Study PTSD #1: Surgery
I’d consider surgery to be one of the medical wonders of this day and age. Unfortunately, as with many things, it has become big business. Rather than being carefully skeptical and hesitant about surgery, it has become the norm to undergo it, in some countries at least, even for minor issues that can easily be treated by non-invasive therapies.
John is a middle-aged man who recently went through an open-heart bypass procedure. Full anesthetic was administered, and the operation itself went well. From John’s perspective, however, it is a different story. Towards the end of the operation, John’s anesthetic started to wear off. Although he wasn't able to feel physical pain, he did regain consciousness. The last 20 minutes of the operation, when they cleaned and stitched him up, he went through agony. John didn't experience pain, but was overwhelmed by feelings of helplessness as he was unable to move or let the medical staff know that he had become conscious.
The experience left him traumatized. Subsequently, his sleep was severely disturbed with repeated flashbacks of the alarming "wake up" during surgery. His blood pressure remained high. He was very snappy, agitated, and irritated. When asked about it, he admitted that he was very angry with the medical staff for not acknowledging that something like this could happen, and for not administering the right dose of anesthetic. His wife said that sadly, John is not the same man that he used to be.
Case Study PTSD #2: Car Accident
Ella is in her thirties, ambitious and active in life. On a wintry evening, while driving back home from work, she lost control of her car while negotiating a bend in the road. The car spun and came to a halt after it crashed into a tree. She was taken to the hospital, unconscious, with fractured ribs, a torn spleen, and concussion. Ella had no memory of the event after losing control of the car; however, months after the accident and her release from the hospital, she suffered from anxiety and fatigue accompanied by chronic pain. She managed to work only part time, but forced herself to drive again.
Case Study PTSD #3: Rape
Jane is married and has two children. Outwardly they seem to be a happy, normal family. She sought treatment as she had frequent outbursts of anger, often for little things and against her children. She also had difficulties with intimate contact with her husband, and always needed some kind of background noise, like music or television, or some kind of occupation. As we progressed in our work, it came to light that Jane was raped by a friend of the family at a young age. Her shame and pain about what happened was covered up by anger, which expressed itself in her family surroundings.
Case Study PTSD #4: Falling Accident
Doug fell in the basement after having a verbal fight with his partner. Though he didn't hurt his head, he’d hurt his back and the stiffness and dull pain didn't go away even though it had been there for some time now. He continued to take prescription drugs for pain and inflammation, which upset his digestion and made him feel nausea from time to time. He angrily blamed himself for losing his footing. This is a clear case where the anger of an argument was coupled with and projected onto the fall, and was then internalized through self-reproach. The persistence of back pain turned out to be the psychosomatic holding on to anger. Although Doug didn't suffer the usual PTSD symptoms, this is still a post-traumatic stress condition!
Case Study PTSD #5: Grief/Bereavement
Karen lost her son in a motorcycle accident. She’s retired, widowed, and lived on her own. She smoked heavily, suffered from insomnia, and admitted that she was overcome by grief, and often felt lonely and depressed. She was able to positively identify that her condition was related to the death of her son, but was not able to let go of her attachment to him.
Case Study PTSD #6: Cesarean Birth
Kelly initially visited me to let me have a look at her little girl, who was just a few weeks old. She was very concerned because the baby cried herself to exhaustion before succumbing to sleep. Doing the routine intake/checklist questions I discovered that the birth had been anything but normal, and had turned into an emergency cesarean.
The pregnancy had gone very well with the baby in the right position. Karen was taken to the hospital once the contractions had started. After some hours of labor, with very little cervix dilation, the doctor opted for emergency cesarean surgery, as the baby had descended and it had been stuck for too long with the head in the base of the mother’s pelvis. Kelly and her husband had no time to take in and consider the situation, and went along with the decision of the doctor.
Dealing with Helplessness
Looking back, Karen realized that she felt out of control and overwhelmed by the suddenness of the changed circumstances. She was severely frustrated with how things turned out, and felt angry with the medical staff. Rationally, she understood that the doctor did the right thing. Emotionally, she felt a sense of helplessness for having had to give in to the "rules" of surgery and medical practice. Finally, what emerged was that she had trouble accepting her child due to her desire for a natural birth; again, the anger and resentment towards the medical intervention were masking her sense of helplessness, and her frustration was coupled with and projected onto her non-acceptance of the child, which resulted in the crying and misery of the little one.
- Do you want to reduce anxiety, hyper-vigilance, and being “ON” alert constantly?
- Do you want to move out of a dissociated, fatigued and depressed state?
- Do you want to work with anger and reestablishing boundaries?
- Are you interested in sleeping better, having better relationships, and being able to live a normal life?
I have created The Trauma Care Audio Guided Meditations which address the most fundamental insights into the processes of trauma and dissociation and how you can work through them.
Share this article if you think it could be helpful to someone:.
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to email a link to a friend (Opens in new window)
Related Articles
Emotional Coping & PTSD: Learn 2 Strategies for Recovery
PTSD Insomnia & The Desire for Peaceful Sleep
PTSD and Why You Gain Weight
Oh man, that last one with the birth process changed.
This makes me wonder how differently my own mother treated me, as I was her first kid after a miscarriage.
rape was down to a T .. as im sure the others
Session expired
Please log in again. The login page will open in a new tab. After logging in you can close it and return to this page.
Module 5: Obsessive Compulsive Disorder and Stressor Related Disorders
Case studies: ocd and ptsd, learning objectives.
- Identify OCD and PTSD in case studies
Case Study: Mauricio

Case Study: Cho

Possible treatment considerations for Cho may include CBT or eye movement desensitization and reprocessing (EMDR). This could also be coupled with pharmaceutical treatment, such as anti-anxiety medication or anti-depressants to help alleviate symptoms. Cho will need a trauma therapist who is experienced in working with adolescents. Other treatment that may be helpful is starting family therapy as well to ensure everyone is learning to cope with the trauma and work together through the painful experience.
Link to Learning
To read more about the ongoing issues of PTSD in violent-prone communities, read this article about a mother and her seven-year-old with PTSD .
Think It Over
If you were a licensed counselor working in a community that experienced a high rate of violent crimes, how might you treat the patients that sought therapeutic help? What might be some of the challenges in assisting them?
- Case Studies. Authored by : Christina Hicks for Lumen Learning. Provided by : Lumen Learning. License : Public Domain: No Known Copyright
- Desk top. Located at : https://www.pickpik.com/desk-top-desk-notebook-keyboard-desktop-shallow-116155 . License : Public Domain: No Known Copyright
- Lightning strike. Authored by : John Fowler. Located at : https://www.flickr.com/photos/snowpeak/3761397491 . License : CC BY: Attribution

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Interpersonal Psychotherapy (IPT) for PTSD: A Case Study
Alexandra klein rafaeli.
* New York State Psychiatric Institute, Columbia University, New York, NY
JOHN C. MARKOWITZ
# NYS Psychiatric Institute, Room 1051 Riverside Drive, Room 4803 Unit/Box: 129, 1051 Riverside Drive, New York, NY 10032
Interpersonal Psychotherapy (IPT), a time-limited, evidence-based treatment, has shown efficacy in treating major depressive disorder and other psychiatric conditions. Interpersonal Psychotherapy focuses on the patient’s current life events and social and interpersonal functioning for understanding and treating symptoms. This case report demonstrates the novel use of IPT as treatment for posttraumatic stress disorder (PTSD). Preliminary evidence suggests IPT may relieve PTSD symptoms without focusing on exposure to trauma reminders. Thus IPT may offer an alternative for patients who refuse (or do not respond to) exposure-based approaches. Interpersonal Psychotherapy focuses on two problem areas that specifically affect patients with PTSD: interpersonal difficulties and affect dysregulation. This case report describes a pilot participant from a study comparing 14 weekly sessions of IPT to treatment with two other psychotherapies. We describe the session-by-session IPT protocol, illustrating how to formulate the case, help the patient identify and address problematic affects and interpersonal functioning, and to monitor treatment response.
INTRODUCTION
Interpersonal Psychotherapy (IPT) is a time-limited, evidence-based treatment that focuses on patients’ social and interpersonal functioning, affect, and current life events. It is efficacious in treating major depression, bulimia, and other conditions ( Weissman et al., 2000 ). Developed by the late Gerald Klerman, M.D., and Myrna Weissman, Ph.D., IPT stems from the theoretical work of Harry Stack Sullivan and John Bowlby and from empirical research on the psychosocial aspects of depression. Sullivan (1953) viewed interactions with others as the most profound source of understanding one’s emotions, while Bowlby (1969) considered strong bonds of affection with others the foundation for individual well being. These theorists guide IPT practitioners as they explore their patients’ affective experiences through the lens of the social and the interpersonal.
Initial evidence suggests that IPT may also benefit patients with posttraumatic stress disorder ([PTSD]; Bleiberg & Markowitz, 2005 ; Campanini et al., 2010 ; Krupnick et al., 2008 ; Ray et al., 2010 ; Robertson et al., 2004 ; Robertson et al., 2007 ). There are at least two rationales for testing IPT for this population. First, IPT does not utilize exposure to trauma reminders. Although extensive evidence supports the efficacy of exposure-based therapies for PTSD (Grey, 2008), IPT offers an alternative to patients who may refuse exposure techniques or not respond to them. A recent review article suggested that highly traumatized patients who dissociate may fare better receiving affect-focused therapy than exposure-based therapy ( Lanius et al., 2010 ). Second, IPT works by improving patients’ interpersonal functioning and emotion regulation ( Markowitz et al., 2006 , 2009 ; Markowitz, 2010 ), which are commonly impaired in PTSD ( APA, 2000 ) and therefore, important targets for change. Social support, which IPT helps patients to mobilize, has been shown to be a key factor in preventing and recovering from PTSD ( Brewin et al., 2000 ; Ozer et al., 2003 ).
PTSD is a psychiatric illness triggered by traumatic events: experiencing a natural disaster, witnessing a death, suffering chronic abuse, or otherwise facing a threat to one’s own life or physical integrity. Although most people (50% to 90%) encounter traumas during their lifetimes, only about 8% develop full PTSD ( Kessler et al., 1995 ). Symptoms of PTSD are distressing and often significantly impair social and occupational functioning.
Many forms of psychotherapy have been employed to address PTSD. Those with the strongest evidence base are forms of cognitive behavioral therapy (CBT), which utilize controlled exposure to trauma reminders (Butler et. al., 2000). Cognitive Behavioral Therapy aims to solve problems by working towards changing patterns of irrational thinking or behavior linked to one’s negative emotions. The CBT approach involves exposure to the trauma either through imaginal confrontation of traumatic memories ( Foa, 2003 ) or in vivo exposure to trauma reminders ( Joseph, 2008 ).
In contrast to exposure-based CBT approaches, IPT eschews focusing on the trauma and instead concentrates on the patient’s current life events, particularly on social and interpersonal aspects ( Markowitz, 2010 ). The basic premise of DPT for PTSD is trauma shatters the patient’s sense of interpersonal safety, leading to withdrawal from interpersonal relationships and impaired ability to use social supports to process the traumatic event ( Markowitz et al., 2009 ). By withdrawing, individuals with PTSD cut off vital social supports needed when they are most vulnerable. Because they are interpersonally hypervigilant, emotionally detached or dysregulated, patients with PTSD mistrust relationships ( Bleiberg and Markowitz, 2005 ). Interpersonal Psychotherapy helps the patient to understand rather than avoid feelings, to tolerate such affects, to use them to enhance communication and effectively manage interactions with others, and thereby, to rebuild interpersonal trust. Finding ways to reconnect meaningfully to one’s surrounding world may reinstate severed social networks and reduce PTSD symptoms.
Interpersonal Psychotherapy defines an interpersonal crisis and helps the patient to resolve it. For PTSD, IPT reviews the following problem areas:
- grief (mourning the death of a significant other),
- role dispute (a struggle with a significant other, which the patient is inevitably losing), or
- role transition (any major life change, including having suffered a traumatic event or events) ( Markowitz, et al, 2009 ).
In a role transition, a life change costs the patient an old role and substitutes a new, unwanted one. Treatment helps the patient mourn the loss of the former and develop skills, interpersonal opportunities, and confidence in the latter, new role. Even an interpersonal trauma may have a silver lining.
EMPIRICAL SUPPORT
Bleiberg and Markowitz (2005) developed a manualized modification of individual IPT for PTSD. A small, open trial treating 14 patients with chronic PTSD yielded improvements across the three PTSD-DSM-IV-TR symptom clusters of hyper arousal, avoidance/numbing, and intrusive symptoms, in addition there were reductions in depression and anger and improvements in social functioning ( Bleiberg & Markowitz, 2005 ). An NIMH-funded, randomized controlled study is currently comparing three 14-week psychotherapies that employ very different mechanisms for treating chronic PTSD: 1) prolonged exposure ( Foa and Rothbaum, 1998 ); 2) IPT, focusing on interpersonal sequelae of PTSD rather than exposure to its traumatic triggers; and 3) relaxation, emphasizing reduction of anxiety through relief of physical tension ( Jacobson, 1938 ). This study will evaluate not only the efficacy of IPT for PTSD, but potential mediators and moderators of treatment outcome.
To illustrate IPT for PTSD, we present data from a pilot case that was not included in the current NIMH study, but served as a valuable training case. This patient received open IPT treatment for PTSD because his Clinician-Administered PTSD Scale (CAPS, Blake et al., 1995 ) score of 45, while indicating moderate symptom severity ( Weathers et al., 2001 ), fell below the study inclusion threshold of 50 or above. This case served as training for a therapist who was new to the study. The patient exemplifies the complex presentation of most patients who meet DSM-IV criteria for PTSD, who generally report comorbidity ( Kessler et al., 1995 ). His response to treatment illustrates the use of IPT as an alternative approach to reducing PTSD symptoms without exposure techniques.
Mr. A., a 48-year-old male, worked from home as a freelance software engineer. He held a master’s degree in computer science and had worked successfully for many years as a computer programmer, but was currently working sporadically and struggling financially. He requested psychotherapy to address current symptoms of “irritability, sleep disturbance, and interpersonal conflicts.” He reported a history of multiple traumas that he felt contributed to his current difficulties. Although he described attempting to “accept the pain and suffering these past ordeals caused” and to “move on,” he often felt resentful and unable to forgive.
Mr. A. was raised in a blue-collar suburb of Philadelphia, living with his parents and two younger sisters. He reported feeling tremendous pressure to excel, which he attributed to his father’s continual dissatisfaction with Mr. A.’s accomplishments. He had few friends growing up, but was committed and loyal to those he did call friends. He had had a few short-term relationships when younger, was once briefly married, and had a daughter, Chloe, who was currently in her twenties. He described bis marriage as “agreeable,” despite feeling the couple shared no common interests and lacked any “passionate connection.” He reported being strongly attached to Chloe from her infancy until age 2. During that interval, he carried out most parental duties while his wife recuperated from a serious back injury. He described his attachment to his daughter during this time as “the most harmonious bond I ever experienced with another human being.”
Mr. A. was currently living with his girlfriend of 7 years, Diane, age 38. He referred to this as a “9/11 relationship”: their first date was in New York on the eve of September 11, 2001, and he believed that the catastrophe brought them closer and created a mutual urgency to “settle down.” Had the terrorist attacks not occurred, he believed their relationship would not have lasted.
Mr. A. exhibited ambivalence about this relationship (and any long-term commitment). He shared a home with Diane, was extremely loyal and devoted, described her with affection, respect, and warmth, and even sometimes referred to her as his fiancée. He described his love for her as strictly platonic, however. They hadn’t been sexually intimate in years, and he saw her more as a “best friend” or “soul mate” than a future wife or mother.
Mr. A.’s description of his interactions with Diane reflected several characteristic behaviors of PTSD ( Markowitz et al., 2009 ). He depicted interactions at home as tense and at times explosive, and attributed these interpersonal struggles to an overall aversion to any “intense feelings.” He would get angry at Diane for intruding on his work space or on his chance to “relax” or “meditate in solitude.” He had created a work environment void of almost all social interaction and found Diane’s presence disturbed his plan, which was to distance himself enough from others so there would be no conflict. His general mistrust in others, another characteristic behavior of PTSD, also added to his uncertainty in his relationship with Diane. For example, Mr. A. had severed ties with Diane’s father over a failed business venture, but Diane continued communicating with him. As a consequence, Mr. A. questioned her fidelity.
Mr. A. reported a shift in his sexuality that he considered the primary cause of his diminished physical attraction towards Diane. Approximately one year before starting IPT, he had become strongly attracted to transsexuals and was daily pursuing contact with the community online. Through Mr. A.’s exploration of the transsexual community, he developed a close “cyber” relationship with Jane, a transsexual living abroad, with whom he frequently e-mailed and “chatted.” Apart from posting photographs online, however, they had never seen each other. Here too, his avoidance of intense feelings seemed to preclude any intimacy. For although he and Jane had discussed setting up a webcam so they could interact more (and even planned to one day meet in person) Mr. A. always stopped short of seeing through with the plans.
Mr. A. initially considered the recent shift in his sexuality a novel curiosity. During the therapy, however, he began to consider the possibility that this attraction was not novel, but part of a longer-standing confusion about sexual orientation.
Trauma History
Mr. A. reported multiple events in his past involving intense fear and humiliation. Some were indeed traumas as defined by the DSM-IV-TR criterion A for PTSD, where others would more appropriately be categorized as subjectively distressing events. Regardless of the clinical classification, each experience Mr. A. recounted evoked vivid and frightful memories. Mr. A.’s first memory dated back to his toddler years. He was told his mother had to stay in the hospital for several weeks after giving birth due to complications, and he would stay with his aunt and uncle. He worried that his mother would die in the hospital and that he would never see her again. He then recounted experiencing additional “emotional trauma” when his aunt “humiliated” him in front of a house full of family members by forcing him to rub his nose in the diaper he had soiled. He linked this memory of shame and disgrace to problems he had in adulthood with sexual intimacy. Mr. A. also recalled the same aunt and uncle so criticizing him for eating messily that it “felt like verbal abuse” and produced a severe food phobia. Other early traumas he revealed at intake included experiencing a hurricane firsthand (age 6) and physical assault by a group of peers in middle school.
The magnitude of Mr. A.’s horrific experiences had no bearing on the impression they left behind. For example, the hurricane and physical assault hardly affected his daily routine; however, his “humiliation” by his aunt (an event not meeting PTSD criterion A) shaped him for years to come. The trauma that most profoundly affected his functioning (DSM-IV criterion A) occurred after Mr. A. and his wife separated. He initially continued to see his child regularly. After several months, however, his wife abruptly abducted Chloe to her native country. Because she left no word for Mr. A., he had no knowledge of his daughter’s well-being or whereabouts for two days. Convinced she had been abducted, he feared for her life. Eventually, he learned that she was safe with her mother, but remained unable to contact or see her.
In the ensuing two years, Mr. A. devoted his life to locating and reconnecting with his daughter. He quit his job, moved to his ex-wife’s country, and immersed himself in custody and abduction law. That Chloe’s age was similar to his when he had first been “traumatized” held great significance for him: his mother had been “taken away,” leaving him fearful and anxious. This memory deepened his need to remain close to his daughter and never to let feel abandoned. A two-year international pursuit and custody battle ensued, including at least two threats on Mr. A.’s life by his ex-father-in law and someone he believed had been hired to kill him by his ex-wife’s family.
Mr. A. underwent a profound role transition with this life trauma. He often referred to his life before and after his daughter’s abduction as if describing two separate individuals: Pretrauma, he reported always having felt “a little mistrustful of others” and acknowledged lifelong “trouble with love and affection,” but was an active, functioning adult who held a full-time job, pursued various hobbies, and even, with some effort, participated in his community. Posttrauma, he struggled to function, to self-regulate, and to find meaning and purpose in his life. His social withdrawal was worsened, and despite seeking numerous therapies and self-help, his PTSD symptoms lingered.
Presenting Complaints
Hyperarousal symptoms.
Mr. A. reported feeling hyperalert and watchful, even when knowing there was no real need. In public settings he experienced moderate hypervigilance. He reported frequent, if brief, startle reactions. He described frequent (daily) intense anger and irritability; on most days, he took this anger out on Diane. Although able to recover relatively quickly from each anger outburst, he found his attempts to suppress anger exhausting, and he noted that the anger outbursts were damaging his relationship with Diane.
Avoidance/Numbing Symptoms
Mr. A. avoided activities, people, and places that evoked strong memories: e.g., phone calls from family members and parties where he might encounter individuals from his past. Avoidant behavior was pervasive: from the cocoon-like home environment, which permitted him to live in virtual isolation (he described choosing to work from home as “adaptive” given his history of interpersonal conflicts in work settings) to avoiding any possible reminder of Chloe’s abduction (he felt “more in control” at home, where he could carefully limit interactions with others). Although he did not meet criteria for substance abuse, he reported using marijuana three times a week and stated that he might not be able to stop using it during treatment. He also reported some loss of interest in previously enjoyable activities, such as sex and sports.
Intrusive symptoms
Although he presenting with a detached affective expression, Mr. A. became visibly upset (as though reliving experiences in the present) when reminded of past traumas or of instances when people betrayed him. Mr. A. reported intrusive daytime thoughts and occasional “bad dreams” about his traumas. The thoughts and nightmares impaired his concentration and made him anxious and uneasy “most of the day.” He described sleep as “chaotic,” compromised by his unstructured daily routine. As a consequence, he was often awake much of the night and then napped sporadically by day.
Other Symptoms
Mr. A. had concerns about his interactions with his most significant others. Although caring deeply for Diane, he worried that he could not reciprocate her romantic feelings for him. He could not imagine deepening their commitment through marriage or starting a family, and he often felt “too emotionally numb” to respond to Diane’s physical or emotional needs. Mr. A. also described considerable conflicts at home. He frequently “snapped” at Diane, and his discomfort with any physical intimacy she initiated caused constant tension between them. He spent most of his days on the computer, chatting online, or talking to his business partner by phone, and even those relatively detached interactions felt stressful.
Previous Treatments
Over the years, Mr. A. had participated in individual, group, and family therapy and had actively sought self-help solutions from books and websites. These had not relieved his ruminations about his distressing past nor helped him cope with high daily levels of anger and frustration. One psychodynamic treatment lasted several years. He also reported a briefer behavioral therapy with an exposure component, and family therapy. Exposure therapy had not helped to quell his anger and anxiety; he was only willing to share parts of his trauma narrative and had resisted any systematic in vivo or imaginal exposure techniques. Similarly, psychodynamic therapy had not reduced his symptoms. Mr. A.’s tendency to control conversations may have turned interpretations into debates. Despite participating in various psychotherapies, Mr. A. had never discussed his sexuality, focusing instead on past traumas.
An independent evaluator assessed Mr. A. using the Clinician-Administered PTSD Scale ([CAPS] Blake et al., 1995 ) and Hamilton Rating Scale for Depression ([Ham-D] Hamilton, 1967 ). Although his scores were subthreshold for the PTSD study, based on his CAPS score (CAPS = 45) ( Weathers et al., 2001 ), he warranted a diagnosis of moderate PTSD. His baseline score on the PTSD Diagnostic Scale Self Report (PSS-SR; Foa, 1993 ) was 25, which is considered severe ( Foa et al., 2009 ). The Life-Events Checklist ( Johnson et al, 1980 ) and Structured Clinical Interview for DSM-IV-TR Axis I Disorders (First, 1997) were also administered at intake. Mr. A. met criteria for PTSD, chronic agoraphobia without panic disorder (both lifetime and current), and specific phobia (fear of food being mixed or touching; lifetime and present). Mr. A. was admitted as a pilot IPT case.
Because Mr. A. was not a formal participant, the independent evaluator did not readminister the CAPS following treatment. However, Mr. A. did complete the PSS-SR and the Beck Depression Inventory (BDI-II) ( Beck, et al, 1996 ) pre-, mid-, and post-treatment.
Treatment Overview
Mr. A.’s long history of avoidant behaviors and interpersonal conflicts made him appear a good candidate for IPT. Interpersonal Psychotherapy differs theoretically and technically from other PTSD treatments in targeting posttrauma sequelae of impaired interpersonal functioning rather than exposure and re-processing of the traumatic events themselves ( Markowitz, 2010 ). Interpersonal Psychotherapy-PTSD ( Markowitz, et al, 2009 ) comprises 14 weekly sessions of 50-minutes each. The clinician largely devotes the initial two to three sessions to an “interpersonal inventory,” collecting information to identify current relationships, overall patterns of interpersonal behavior, and links between relationships and symptoms. The clinician then formulates the case, linking the DSM-IV PTSD dia gnosis to an interpersonal focus that emerged in the assessment, and shares this formulation with the patient. Sessions 3 to 14 focus on addressing and resolving the interpersonal problem area (e.g., role transition); the therapist provides psychoeducation about PTSD as a treatable medical illness that is not the patient’s fault, and serially monitors symptoms. The final sessions focus on termination, an important interpersonal event but one that has been anticipated from the start of the time-limited therapy.
Sessions 1 to 3: Initial Phase
Goals for these sessions included exploring in detail Mr. A.’s current and past relationships to understand his interpersonal functioning, to identify interpersonal issues linked to the onset of PTSD symptoms, and to take a trauma history. The therapist first explained the IPT approach to Mr. A. He acknowledged the prominent interpersonal difficulties in his current life and expressed his eagerness r to work on changing his behaviors. The therapist then reviewed Mr. A.’s current PTSD symptoms, which were based on the PSS-SR results. She observed that his avoidance symptoms were the most prominent. She took a general history of traumas throughout Mr. A.’s life. Mr. A. noted that each trauma involved a profound sense of betrayal, which led him to mistrust people and to avoid forming close relationships.
The most important people in Mr. A.’s life were his girlfriend Diane and his daughter Chloe. He felt that his traumas negatively affected both relationships. He was irritable with Diane, and he avoided close contact with Chloe to avoid being hurt. He cited similar problems in other relationships, and reported that the “major trauma” of his life, Chloe’s abduction, unquestionably exacerbated this distancing tendency.
Mr. A. often attempted to advise and guide others, considering that he related to others best by imparting knowledge. Unfortunately, his guidance was often unsolicited and not well accepted. This behavior also arose almost immediately in IPT sessions. Mr. A. elaborated in great detail how particular computer programs worked or what he had learned in a recent self-help class. He would talk without pause for several minutes, despite the therapist’s attempts to interject. This tactic succeeded in avoiding any guidance from the therapist.
A similar process unfolded with his daughter, who had recently expressed interest in studying law. Upon hearing this, Mr. A. began telling her all of the details of his custody battle with her mother, including an enormous number of personal and confidential documents. He deemed this a supportive act; she did not.
Mr. A. admitted that his concept of relationships and his approaches to others often left him feeling distant from the very people he cared for most. At times he felt “betrayed” after doing “so much.” For example, early in his relationship with Diane, her father developed a rare illness. Mr. A. immediately took it upon himself to research extensively alternative treatments. Mr. A. felt he was instrumental in saving her father’s life, but never felt recognized for it.
After Chole and Mr. A. were reunited, he was hurt by Chloe’s decision to live with her mother rather than with him. He also still grieved his lost bond with Chloe when she was a baby, a bond defining to him the purest and most powerful of connections. Although he admitted having struggled for many years with feeling comfortable in romantic relationships and with physical intimacy, he believed this struggle worsened after the abduction.
Mr. A. had trouble accepting affection from Diane. When they met they had sex regularly, but in recent years they stopped sleeping in the same bed and had only been intimate once in recent years. He summarized a recent, deliberate attempt to rekindle passion between them as “the attempt failed.” Diane frequently desired physical closeness, and although he cared for her and wanted to reciprocate the affection for her sake, he found himself recoiling from her touch. He described her as “coming at him” too fast with a hug or a kiss, and he experienced excruciating discomfort from any physical touch.
Just as Mr. A. sought solutions for his “PTSD,” he spent time seeking an explanation for his intimacy difficulties. He began questioning his sexuality, past and present. In his past, he had felt most comfortable with female bisexual partners, and was often told he “made love like a woman.” He felt an unusual bond in his recent online relationship with Jane, a male-to-female transsexual. Extremely attracted to her, he also felt he could be more open and honest online, whereas at home he had to feign interest and affection. He wondered whether this recent attraction stemmed from an online self-help course that encouraged attunement with both his “left” and “right” brain. Attraction to a transsexual, he opined, tapped into his “middle-brain.”
Mr. A. believed yoga, meditation, and spirituality helped him to feel more “balanced.” He stated his primary goal was to become more “disciplined” and “even tempered,” “like the Dalai Lama.” Nonetheless, he continued to struggle with self-regulation in interpersonal situations. His spiritual exercises, all solitary in nature, were not aiding his quest for equilibrium; on the contrary, they enabled Mr. A. to continue avoiding interpersonal contact and any strong emotions such exchanges might evoke.
IPT Case Formulation
The IPT formulation concisely links symptoms to the focal interpersonal problem area. The formulation, presented as feedback at the end of the initial phase, draws on information gathered from the interpersonal inventory and provides an organizing focus for the remainder of therapy:
I understand from our initial meeting that your interpersonal goals are to be closer to Chloe and to reduce disputes with Diane. I also understand that you’ve always experienced interpersonal difficulties, but that they grew much worse after your daughter’s abduction-triggered PTSD. You have clearly worked hard over the years to overcome problems you’ve had in social arenas, and you’ve tried numerous times to address the painful memories of past traumas that still live with you today.
Your PTSD symptoms still overshadow your feelings and actions. You feel overwhelmed by both your emotions and your environment. Your symptoms are also coupled with an important current life issue you say has you’ve never discussed in past treatments: your sexual identity. Through understanding yourself in relationship to others, you cam mend your social conflicts and reduce your symptoms.
You’ve discussed how hard it is to trust people, and how that has limited your social network for years. Your wife’s abduction of Chloe took away the person closest in the world to you, and has made it extremely difficult—to this day—for you to trust others, to take the risk to connect with those around you. This mistrust is very common in PTSD. Avoidance, numbing, intrusive thoughts are all symptoms of the illness. Although you say that you always had difficulty in social situations, these symptoms are not necessarily part of your character; they’re indication of an illness that you suffer from—an illness that’s treatable and not your fault. The symptoms can improve.
Your mistrust has led you to minimize social contact. You’ve discussed feeling “betrayed” or “deceived” after trying to help others many times over. So you’ve been keeping your distance through “electronic relationships” that are more comfortable. Yet, you say you “yearn for closer, more real relationships!”
You are going through a role transition: Uncomfortable feelings about your relationships and your own sexuality have made life extremely confusing, and it’s hard for you to know what you want from whom. What we can work on in the remaining weeks of treatment is how to navigate this transition: Do you want to stay with Diane, deepen a relationship with Jane, or what? If you can understand your feelings and use them to resolve this uncertainty, not only will your life feel better, but you symptoms are likely to subside. Does that make sense to you?
Mr. A. agreed to work on this interpersonal focus.
Session 4 to 10: Middle Phase
Having agreed to focus on his role transition, Mr. A. and the therapist entered the middle phase of IPT. Mr. A. now understood that he was suffering from a treatable illness that was not his fault, with clinical symptoms related to his past traumas. He would learn to detect and monitor these symptoms in the course of therapy, but should not blame himself for having symptoms or for their impact on his relationships. In all likelihood, he would start to feel better and see the symptoms subside.
In his role transition, Mr. A., was adjusting to changes in what and who attracted him sexually. The therapist introduced strategies to improve interpersonal communication, and helped elicit emotional responses that surfaced in the process. She supported Mr. A. in confronting and wrestling with intense (particularly negative) feelings. Mr. A. also needed to understand that his tendencies to intellectualize emotional experiences and to defend against any unpleasant moods complicated this shift. Tolerating his affects would help him become more connected with others and more open with his sexuality.
The therapist helped him to examine closely current conflicts and arguments. This would help Mr. A. determine what he wanted in these situations and explore interpersonal options, including role play to practice responses, to resolve them. Specific incidents from the week were reviewed, eliciting Mr. A.’s feelings and behaviors, and sessions offered a chance to practice and hone interpersonal skills.
“How have things been since we last met?”
This simple question starts every IPT session. It anchors both therapist and patient by focusing on current feelings and life events related to the focal problem area (role transition) and by eliciting current concrete interpersonal incidents on which to draw when discussing alternative interpersonal techniques ( Weissman et al., 2000 ). Mr. A. could seldom recall any events from his week to discuss and instead, chose to recount stories from his past. His week, after all, intentionally avoided interpersonal encounters; he thought there was little to recount. Alternatively, he would offer a detailed description of a computer program he was developing, dive into monologues about what it takes to be an effective software engineer, or return to his distant past. This parrying the opening IPT question was a fundamental challenge in the treatment.
The therapist persisted in probing each week, seeking to guide Mr. A. to the here and now and away from the distant stories indelibly fixed in his mind. Despite his cocoon-like existence, Mr. A. had interactions with others, though he may have wanted to avoid the affect attached to recent arguments with Diane, or an emotionally charged phone call with Chloe, or a negative response from an online communication.
Mr. A.’s communication style was intellectualized, emotionally detached, expressed in abstract theoretical rather than experiential verbiage. When asked a simple question like, “How did that make you feel?” he responded with an analysis of how his “left brain” was dictating his behavior, making it impossible for his creative, emotional “right brain” to respond. The therapist challenged him to explore the feelings he consistently ignored or avoided, using his vocabulary as an illustration. She suggested that such detached language contributed to his distancing himself from the real feelings situations evoked. She urged him to retell day-to-day encounters using emotional words and describing his momentary experience. Again, the focus was on everyday interactions rather than a review of his trauma experiences, which were in this case, too well rehearsed to evoke genuine emotion. The therapist would then return to the initial question: “How have things been since we last met?”
It was frustrating when, at first, Mr. A. couldn’t break old habits. The therapist felt as Chloe must have when she hoped for her father’s support but instead got a lecture, or Diane might have when trying to connect with him, only to be repeatedly rebuffed. Mr. A. clearly cared deeply about his relationships and suffered from his isolation, but he made it almost impossible to break through the veneer.
By Session 6, Mr. A. was better able to recount specific events from his week, and was willing to take greater emotional risks when feelings surfaced. He described a telephone conversation with Chloe in which they talked more openly about their current lives. He still wished he could have influenced her life decisions (e.g., career choice) and values. He also recognized that many of the feelings he often avoided or suppressed related to his daughter. His years of grieving about time lost with Chloe no longer mattered as much to him as did the importance of their current relationship. He then attributed his current qualms about having children with Diane to regrets and losses surrounding Chloe and to his generalized loss of trust in other people.
The therapist introduced role play for improving Mr. A.’s ability to communicate with his significant others. She encouraged him to limit his phone interactions and increase face-to-face meetings with his business partner. In such meetings, Mr. A. could break his isolation, better read facial and body cues, and circumvent conflict. The therapist clarified that this was not a form of exposure, rather a technique for relating to others better. Mr. A. was initially uncomfortable with this until they role-played scenarios in session.
The therapist encouraged Mr. A. to recognize when he was frustrated or angry with Diane and tell her. With practice, he gradually saw the benefit of this approach in preventing angry outbursts. Similarly, when Jane suddenly broke off on-line communication, the therapist encouraged Mr. A. to confront her rather than avoid the behavior’s meaning and the hurt feelings it evoked. The therapist validated and normalized these negative affects as useful indicators of social encounters.
The therapist used IPT’s medical model and designation of the “sick role” ( Weissman et al., 2000 ) throughout the middle phase to underscore that Mr. A.’s symptoms were not his personality or a personal failing. As Mr. A.’s PTSD symptoms had lingered for decades, he had, unsurprisingly, come to confuse the disorder with his character. He had internalized symptoms, such as avoidance, startle responses, and irritability, as if they were fixed traits he could only manage, not dissolve. With time, he began to recognize the symptoms were not his character and not his fault. Through understanding his emotions and their role in daily minor encounters, he could reduce them so that he would merely experience healthy anxiety when reminded of traumas.
Just as Mr. A. had believed initially that PTSD an intractable part of himself, he also believed that strong feelings, such as anger or sorrow, could produce only negative outcomes. The therapist supported Mr. A. in confronting, rather than avoiding, intense (particularly negative) feelings. Each time he retreated into intellectualized language, she asked him to describe how he was feeling at that moment. Acknowledging, and simply sitting with an intense emotion, was his most challenging task.
This piece of the treatment was crucial, and is central to understanding how IPT differs from other affect-based therapies. Learning to acknowledge one’s emotions and to experience them more deeply is a shared core principle. However, in IPT the patient learns to understand a particular emotion as a response in an interpersonal context and then to communicate the feeling to improve an important relationship. Mr. A. did this with his irritability: his anger outbursts resulted from avoiding or suppressing intense feelings. If he could express his fears, anxiety, or disappointments with Diane as they surfaced, he was less likely to angrily “explode.” He practiced talking with Diane about his feelings when they were at peace, using “I” statements to avoid accusing or attacking language. He also shifted his communication of his feelings during sessions. Instead of “educating” the therapist, he now was willing to verbalize emotions and to explore their interpersonal context.
As the termination phase neared, an evaluator reassessed Mr. A.’s symptoms. His PSS-SR scores improved dramatically, falling from 25 at the start of treatment to 9 by session 8, indicating that he no longer met full criteria for PTSD. His BDI score remained euthymic, falling from 7 to 6.
Early in treatment, Mr. A. had responded hesitantly to techniques the therapist suggested, hiding behind intellectualization and refusing to focus on the present. He progressed as he became more willing to leave his comfort zone and to acknowledge that negative affects are not “bad,” but that sadness, loss, anger, are all useful, socially informative feelings if tolerated. This was a profound shift. He noticed he was becoming less irritable with Diane and his business partner and was less avoidant of social situations. He came to sessions more willing to discuss recent events and resultant feelings. He said this would never come easily or “naturally,” but he saw the benefit in trying. As a result, he felt better.
Session 11–14: Termination Phase
The final sessions reviewed the treatment course and addressed Mr. A.’s progress, his developing skills, and his feelings about ending therapy. The therapist acknowledged the sadness of separation, yet focused on the gains he had made, and reviewed areas where Mr. A. felt more competent and independent to function without therapy. Together they tried to anticipate difficulties that might resurface after treatment. Mr. A. recognized his progress, but voiced disappointment that treatment was ending and wanted to discuss ways to continue. He viewed “endings” negatively, recalling his childhood separation from his parents, his marriage, and his relationship with his daughter. He feared that parting would only bring gloom and helplessness, as it had in his past.
The therapist presented termination as a potentially corrective experience: Mr. A. could work through the feelings that arose in saying goodbye, and potentially, see that not only could he tolerate such emotions, but also that he deserved a sense of completion, mastery of skills, and progress.
At termination, Mr. A. was more socially engaged and communicated more effectively. He now considered his shift in sexuality more a curiosity than a bona fide change in identity, and decided his relationship with Diane was worth nurturing. He became more affectionate with Diane, talking with her more openly about both their future and his past. Diane knew about Chloe’s abduction, but not about the related traumas that contributed to Mr. A.’s fears of intimacy and lasting relationships. She also knew about his online relationship, but their discussions had never gotten past angry, jealous exchanges, so that she had been unaware of his longer standing sexual confusion. Mr. A. also reported that he felt his relationship with his daughter had improved. They talked more and she involved him more in her daily life.
In anticipating difficulties post treatment, Mr. A. expected his “poor people skills” would never remit, and he would need to continue practicing communication skills and challenging himself to approach people. He felt more capable of tolerating negative moods and better able to bounce back from conflicts. Mr. A. reported still thinking about past traumas and the people who had been disloyal to him over the years, but this occurred less often and less intensely.
ASSESSMENT OF PROGRESS
Mr. A.’s scores on the PSS-SR remained at 9 at session 14. Thus, by the end of the protocol, he was well below the cutoff score for PTSD criteria. His reports indicated improved daily functioning. Although his work schedule continued to disturb his sleep pattern, he reported less nocturnal anxiety. He reported less anger and irritability towards Diane and less conflict at home. He cited an improved relationship with Chloe, and increased hope of restoring their past bond. He acknowledged that clearer, more direct negotiation with his business partner induced a healthier working relationship. Finally, he decreased cannabis use from at least three times a week, to “as needed,” approximately once a week.
COMPLICATING FACTORS DURING THE COURSE OF TREATMENT
During this short-term treatment, several factors complicated clinical progress. Mr. A. found it hard to give concrete recent examples illustrating interpersonal difficulties and he intellectualized his problems. A second, related complication was Mr. A.’s smorgasbord of past therapy approaches. He often arrived with a list of items to discuss and had difficulty shifting focus. His rigid preparation for sessions made it hard for the therapist to structure treatment. Similarly, Mr. A.’s “teacher” role interfered with the patient role and he thus avoided affect and interpersonal closeness. Finally, although Mr. A. did not meet full criteria for substance abuse or dependence, his habitual cannabis use was maladaptive.
TREATMENT IMPLICATIONS
This IPT-PTSD case illustrates what may present a viable alternative to exposure-based treatments for this serious disorder. The patient described grappled for more than 20 years with the aftereffects of a personal trauma. Despite numerous therapies and attempts at self-help, his PTSD had persisted. Neither exposure therapy nor long term psychodynamic therapy had helped to quell his anger, anxiety, and avoidance.
Interpersonal Psychotherapy-PTSD offered Mr. A. a chance to understand himself through his feelings and relationships subsequent to the trauma. No formal exposure techniques were used; instead, IPT-PTSD focused on the patient’s feelings in current interpersonal relationships through decision and communication analyses. The PTSD symptoms appeared to diminish through the processes of understanding feelings and relationship patterns and the slow building of social support.
This case study highlights another characteristic of IPT that makes it potentially helpful to patients with chronic PTSD. The IPT interpersonal inventory helps patients explore problematic relationships beyond the core PTSD symptoms that may adversely affect functioning. Mr. A. struggled with his sexuality. The more he discussed this, the more he connected it to his relationships and PTSD symptoms. Had the therapy focused exclusively on re-exposure to trauma reminders, this key issue might never have surfaced. Yet, the interpersonal issues bordering this patient’s daily functioning were paramount to his dilemma and his progress.
Acknowledgments
Supported in part by grant R01 MH079078 from the National Institute of Mental Health.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [ Google Scholar ]
- Beck AT, Steer RA, Brown GK. Manual for Beck Depression Inventory II (BDI-II) San Antonio, TX: Psychology Corporation; 1996. [ Google Scholar ]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995; 8 :75–90. [ PubMed ] [ Google Scholar ]
- Bleiberg KL, Markowitz JC. Interpersonal psychotherapy for posttraumatic stress disorder. The American Journal of Psychiatry. 2005; 162 :181–3. [ PubMed ] [ Google Scholar ]
- Bowlby J. Attachment. New York, NY: Basic Books; 1969. [ Google Scholar ]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology. 2000; 68 :748–766. [ PubMed ] [ Google Scholar ]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: a review of meta-analyses. Clinical Psychology Review. 2006; 26 :7–31. [ PubMed ] [ Google Scholar ]
- Campanini RF, Schoedl AF, Pupo MC, Costa AC, Krupnick JL, Melo MF. Efficacy of interpersonal therapy-group format adapted to post-traumatic stress disorder: an open-label add-on trial. Depression and Anxiety. 2010:72–77. [ PubMed ] [ Google Scholar ]
- Foa EB, Rothbaum BO. Treating the Trauma of Rape: Cognitive-Behavioral Therapy for PTSD. New York, NY: Guilford Press; 1998. [ Google Scholar ]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. Journal of Traumatic Stress. 1993; 6 :459–473. [ Google Scholar ]
- Foa EB, Keane TM, Friedman MJ. Society for Traumatic Stress Studies. Guilford Press; 2009. Effective Treatments for PTSD: Practice Guidelines from the International. [ Google Scholar ]
- Foa EB, Rothbaum B, Furr J. Augmenting exposure therapy with other CBT procedures. Psychiatric Annals. 2003; 33 :47–56. [ Google Scholar ]
- Hamilton M. Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology. 1967; 6 :278–96. [ PubMed ] [ Google Scholar ]
- Jacobson E. Progressive Relaxation. Chicago: University of Chicago Press; 1938. [ Google Scholar ]
- Johnson JH, McCutcheon SM. Life Events Checklist. Hemisphere Publishing Corporation; 1980. [ Google Scholar ]
- Joseph JS, Gray MJ. BAO Exposure therapy for posttraumatic stress disorder. Journal of Behavior Analysis of Offender and Victim: Treatment and Prevention. 2008; 1 :69–80. [ Google Scholar ]
- Kessler RC, Sonnega A, Bromet E, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995; 52 :1048–60. [ PubMed ] [ Google Scholar ]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron E. Interpersonal psychotherapy of depression. New York, NY: Basic Books; 1984. [ Google Scholar ]
- Krupnick JL, Green BL, Stockton P, Miranda J, Krause E, Mete M. Group interpersonal psychotherapy with low-income women with posttraumatic stress disorder. Psychotherapy Research. 2008; 18 :497–507. [ PubMed ] [ Google Scholar ]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, Spiegel D. Emotion modulation in PTSD: clinical and neurobiological evidence for a dissociative subtype. American Journal of Psychiatry. 2010; 167 :640–647. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Markowitz JC. Cutting Edge: IPT and PTSD. Depression and Anxiety. 2010; 27 :879–881. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Markowitz JC, Milrod B, Bleiberg KL, Marshall RD. Interpersonal factors in understanding and treating posttraumatic stress disorder. Journal of Psychiatric Practice. 2009; 15 :133–140. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Markowitz JC, Bleiberg KL, Christos P, Levitan E. Solving interpersonal problems correlates with symptom improvement in interpersonal psychotherapy: preliminary findings. Journal of Nervous and Mental Disease. 2006; 194 :15–20. [ PubMed ] [ Google Scholar ]
- Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychological Bulletin. 2003; 129 :52–73. [ PubMed ] [ Google Scholar ]
- Ray RD, Webster R. Group Interpersonal Psychotherapy for veterans with posttraumatic stress disorder: a pilot study. International Journal of Group Psychotherapy. 2010; 60 :131–140. [ PubMed ] [ Google Scholar ]
- Robertson M, Rushton PJ, Bartrum MD, Ray R. Group-Based Interpersonal Psychotherapy for Posttraumatic Stress Disorder: Theoretical and Clinical Aspects. International Journal of Group Psychotherapy. 2004; 54 :145–175. [ PubMed ] [ Google Scholar ]
- Robertson M, Rushton P, Batrim D, Moore E, Morris P. Open trial of interpersonal psychotherapy for post traumatic stress disorder. Australasian Psychiatry. 2007; 15 :375–379. [ PubMed ] [ Google Scholar ]
- Sullivan HS. The Interpersonal Theory of Psychiatry. New York, NY: Norton; 1953. [ Google Scholar ]
- Weissman MM, Markowitz JC, Herman GL. Comprehensive guide to interpersonal psychotherapy. New York: Basic Books; 2000. [ Google Scholar ]
- Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD Scale: a review of the first ten years of research. Depression and Anxiety. 2001; 13 :132–156. [ PubMed ] [ Google Scholar ]
- Open access
- Published: 25 June 2024
A network meta-analysis of psychological interventions for children and adolescents after natural and man-made disasters
- Xiang Zhu 2 ,
- Lijun Wang 1 ,
- Zhendong Wan 1 ,
- Jiyu Yang 3 ,
- Chen Su 1 ,
- Shuyu Duan 1 ,
- Chenxi Xu 1 &
- Binbin Kan 4
BMC Psychiatry volume 24 , Article number: 468 ( 2024 ) Cite this article
292 Accesses
Metrics details
Introduction
Children and adolescents, after natural and man-made disasters, often exhibit various psychological, emotional, and behavioral issues, showing a range of clinical symptoms related to post-traumatic stress disorder (PTSD) and depression. This review used a network meta-analysis (NMA) approach to compare and rank psychological interventions for PTSD and depression in children and adolescents after exposure to natural and man-made disasters.
Randomized studies of psychosocial interventions for PTSD and depression in children and adolescents exposed to natural and man-made disasters were identified. PTSD and depression symptoms at postintervention and 1–12 month follow-up are the outcomes. The standardized mean differences (SMDs) between pairs of interventions at postintervention and follow-up were pooled. Mean effect sizes with 95% credible intervals (CI) were calculated, and the ranking probabilities for all interventions were estimated using the surface under the cumulative ranking curve. Study quality was assessed with version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2).
In total, 26 studies with 4331 participants were included in this NMA. Eye movement desensitization and reprocessing therapy (EMDR) (SMD = − 0.67; 95% CI − 1.17 to − 0.17), exposure therapy (ET) (SMD = − 0.66; 95% CI − 1.11 to − 0.22), and cognitive behavioral therapy (CBT) (SMD = − 0.62; 95% CI − 0.90 to − 0.34) were significantly more effective for PTSD at postintervention than inactive intervention. EMDR (SMD = − 0.72; 95% CI − 1.11 to − 0.33) and ET (SMD = − 0.62; 95% CI − 0.97 to − 0.27) were associated with a higher reduction in PTSD symptoms at follow-up than inactive intervention. EMDR (SMD = − 0.40; 95% CI − 0.78 to − 0.03) and play therapy (PT) (SMD = − 0.37; 95% CI − 0.62 to − 0.12) were significantly more effective for depression at postintervention than inactive intervention. For all psychological interventions in reducing depression symptoms at follow-up compared with inactive intervention, the differences were not significant.
EMDR appears to be most effective in reducing PTSD and depression in children and adolescents exposed to natural and man-made disasters. In addition, ET and CBT are potentially effective in reducing PTSD symptoms at postintervention, while PT is beneficial in managing depression symptoms at the treatment endpoint.
Peer Review reports
Natural and man-made disasters, such as earthquakes, cyclones, tsunamis, floods, war, and terrorist attacks, are mostly unpredictable, which often lead to severe consequences, such as environmental loss, displacement of the family, property damage, physical injury, and even death of a loved one [ 1 ]. Disasters and social and economic losses leave victims in despair, fear, shock, and maladjustment [ 2 ]. The victims of these traumatic experiences often display psychological, emotional, and behavioral issues. They show many clinical symptoms of post-traumatic stress disorder (PTSD) and depression. In particular, children and adolescents are particularly vulnerable after exposure to disasters because they lack psychological preparedness for disasters and coping skills for traumatic experiences [ 3 ]. A cross-sectional study found that the prevalence of PTSD and depression in adolescents six months after exposure to an earthquake was 58.3% and 16.8% [ 4 ]. Natural and man-made disasters might negatively impact mental health outcomes in childhood and influence psychological symptoms into adulthood. Experiencing a disaster at a young age is a risk factor for adult mental health disorders [ 5 ]. Therefore, psychological interventions for children and adolescents should be given a greater emphasis besides socioeconomic support following a disaster.
Given the psychological impact of natural and man-made disasters, a variety of psychological interventions, including cognitive behavioral therapy (CBT), eye movement desensitization and reprocessing therapy (EMDR), and narrative exposure therapy, among others, have been provided by or under the supervision of psychologists or psychiatrists. Children and adolescents can benefit from these psychological interventions, which could significantly promote their mental health and well-being. Various psychological intervention programs in terms of theoretical background, methodology, content, and duration were proposed. Several studies have been conducted to evaluate effective interventions. Previous systematic reviews and meta-analyses have aggregated the results from these studies of interventions in children and adolescents exposed to disasters, finding psychological interventions efficacious at reducing PTSD symptoms [ 6 , 7 , 8 ].
The previous meta-analyses have two shortcomings. First, the previous meta-analyses mainly target PTSD as the primary outcome of natural and man-made disasters, estimating the effectiveness of psychological interventions for reducing PTSD symptoms. Although depression was often found to co-occur with PTSD in children and adolescents after traumatic events, the symptoms or mechanisms of these mental disorders differed, making psychological intervention effects on PTSD and depression inconsistent. Further extending this work, the current meta-analysis was conducted to explore not only the effect sizes of psychological intervention on PTSD but also on depression. Second, the existing meta-analyses used standard meta-analytic techniques and evaluated effect sizes based on direct evidence, which limits the comparison of each psychological intervention’s effectiveness to others. In addition, psychologists or psychiatrists need to choose the most effective programs for children and adolescents after disasters, among numerous psychological interventions. However, traditional meta-analysis cannot provide the first choice of intervention and the possible rank for each psychological intervention.
Network meta-analysis (NMA) is a mixed treatment comparison meta-analysis and multiple treatment comparison meta-analysis. NMA is developed from classical meta-analysis, extending the standard meta-analysis that only deals with two interventions to a method that simultaneously compares several interventions with each other and performs comprehensive ranking. This means that NMA could estimate the relative effects of multiple interventions based on indirect evidence and rank the effectiveness of a particular outcome to select the most appropriate treatment plan [ 9 ]. This meta-analysis was conducted to estimate the relative effectiveness of psychological interventions for PTSD and depression in children and adolescents after exposure to natural and man-made disasters using NMA.
Protocol and registration
The study protocol for the current NMA was registered in the International Prospective Register of Systematic Reviews (PROSPERO) on May 6, 2023. The registration number is CRD42023421304. The design and reporting of the study followed the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) guidelines [ 10 ].
Literature search
Searches were conducted in the following electronic databases in June 2023: MEDLINE, PubMed, Web of Science, PsycINFO, and EMBASE. Articles were identified by using the following terms: (disaster* or mass trauma or earthquake* or tsunami* or flood* or hurricane* or terroris*) and (intervent* or counsel* or support* or treatment or therapy) and (randomized controlled trials or randomized control trial or random*) and (child* or adolescent* or youth or teen*). Searches were limited to children and adolescents (under 18 years) and English publications. In addition, five systematic reviews on relevant topics were identified, and the reference lists of these reviews were examined for potential studies [ 6 , 7 , 8 , 11 , 12 ].
Inclusion criteria
Studies included in this NMA were required to meet the following inclusion criteria: (1) randomized controlled trials (RCTs), (2) children or adolescents exposed to natural and man-made disasters, (3) assessed the efficacy of at least a psychological intervention, (4) compared the psychological intervention with inactive intervention or other interventions, (5) reported validated measurement of PTSD or depression, and (6) reported the mean score and standard deviation (SD) or provided other related information to estimate effect sizes. If one data set were published in a journal article and a book simultaneously, we would include the journal article.
The authors (YX and CS) independently examined the articles for eligibility, and any disagreements were resolved through discussion. Online supplemental material outlines the reasons for the exclusion of full-text articles. After assessing the full text of articles for eligibility, 26 studies were included in the current review.
Data extraction
NMA outcomes included PTSD symptoms and depression symptoms, which were measured on relative rating scales. The authors (YX and SD) collected these outcomes’ mean scores and SD at the treatment endpoint and follow-up. The scores obtained nearest to the end of the intervention are identified as postintervention scores, while those assessed at least one month after the intervention’s completion are identified as follow-up scores. When multiple scales are used to assess symptoms of PTSD or depression, all scores were extracted and analyzed together. If studies failed to report SD, we calculated SD from other related information, such as standard errors, confidence intervals, t-values, or p-values [ 13 ]. In addition, we extracted data from the included studies. This data consisted of author, year, type of trauma, intervention, comparison, number of participants in each group, average age, female percentage, level of intervention, PTSD measurement, and depression measurement.
Quality assessment
The authors (SD and CX) performed the quality assessment of these included studies using version 2 of the Cochrane risk-of-bias tool for randomized trials (RoB 2) [ 14 ]. The risk of bias for each study was assessed in five domains, including randomization, deviations from intended interventions, missing data, outcome measurement, and selection of reported results. Overall, studies were regarded as high risk of bias if one domain of RoB 2 was found to be at high risk. Studies were determined as low risk of bias if all domains of RoB 2 were judged to be at low risk. All other cases were judged to be of some concern.
Statistical analysis
The current NMA was conducted with the mvmeta package in Stata14.0 and OpenBUGS [ 15 , 16 ]. The standardized mean differences (SMDs) between pairs of interventions at postintervention and follow-up were pooled to synthesize outcomes because the included studies used different rating scales to report PTSD and depression symptoms. Interventions belonging to a similar theory were combined into a single group. Mean effect sizes with 95% credible intervals (CI) were calculated for each analysis. In addition, the ranking probabilities for all interventions were estimated using the surface under the cumulative ranking curve (SUCRA), which was a percentage of the effectiveness of each intervention that would be ranked first [ 17 ]. The heterogeneity across the comparisons was estimated in the network [ 18 ]. Subgroup analyses by level of intervention (individual vs. group intervention), profession treatment provider (psychologist/psychiatrist vs. teacher/counselor), and country income (HICs vs. LMICs) were conducted.
These psychological interventions belonging to the same theory or technique were combined into a single node. Cognitive Behavioral Therapy (CBT) is a relatively broad category of psychological interventions, and any intervention that employs cognitive behavioral techniques is classified under this category. Exposure techniques such as narrative, writing, and imaginal reliving were classified together as Exposure Therapy (ET). Psychological interventions that employ mindfulness techniques or theories are classified under Mindfulness Based Therapy (MBT). Treatment as usual (TAU) primarily consists of general support measures, such as routine courses and training methods. Waiting list (WL) and no treatment (NT) were combined. Eye Movement Desensitisation and Reprocessing (EMDR), Trauma and Grief Component Therapy (TGCT), Building Resilience Intervention (BRI), and Play Therapy (PT), which cannot be classified into the aforementioned categories, form a category of their own.
Consistency in a network of interventions refers to the similarity between direct and indirect evidence in comparisons [ 19 , 20 ]. The inconsistency test was performed by comparing direct and indirect evidence in the closed loop of nodes [ 21 , 22 ] and assessing the goodness of fit for the NMA model [ 23 ]. In addition, the possible inconsistency was investigated using a side-splitting approach between direct and indirect evidence. The likelihood-ratio test was conducted to examine the consistency model.
Publication bias was evaluated for each comparison by conducting global funnel plot analyses. The symmetry of funnel plots was visually inspected to distinguish publication bias [ 24 ]. Sensitivity analyses were performed by excluding studies with high bias risk. In addition, we assessed the certainty of evidence using Confidence in NMA ( https://cinema.ispm.unibe.ch/ ). This web application evaluates the confidence of findings for NMA [ 25 ].
Characteristics of included studies
The flow diagram of study selection is presented in Fig. 1 . After removing duplicates, 877 articles were included in the initial title and abstract screening, 102 of which were selected for full-text assessment. Seventy-six articles failed to meet the criteria for the current NMA, leaving 26 eligible articles that reported at least one outcome of interest.

The PRISMA diagram
Table 1 shows the characteristics of the included studies. The number of participants was 4331, while their mean age was 12.69 years (ranging from 8.40 to 16.30 years). The mean sample size of the included studies was 166.58, ranging from 26 to 1220. One study included only females, and the other had only males. In the remaining studies, the average percentage of females was 54.93, varying from 34.67 to 74.12. Seven studies were conducted in high-income countries (HICs), and nineteen in low/middle-income countries (LMICs). Eleven studies were carried out by psychologists or psychiatrists, and fifteen studies were carried out by teachers or counselors. Twenty-three studies recruited participants with measurements of PTSD symptoms using the CPSS, the CPTS-RI, the CRI, the CRIES, the HTQ, the PSS, the RI, the TGIC, the UCLA Grief Inventory, and the UCLA PTSD Index. Fifteen studies recruited participants with measurements of depression symptoms using the APAI, the BDS, the CDI, the CES-D, the DSRS, the MDI, the SCARED, and the SSRS. Twelve studies compared a psychological intervention with WL, and eight employed NT as the control condition. Twenty-four psychological interventions were included in the current research, including BRI, CBT, CP, CT, EMDR, EMDR-GP/C, ET, GSI, IPT-G, KIDNET, MBSGP, MED-RELAX, m-WET, NET, OT, PBT, PS, PY, SBT, SSET, TAU, TF-CBT, TGCT, TRT, and WR.
Risk of bias assessment
All 26 included studies were assessed for risk of bias using RoB 2. Two studies were at high risk of bias, thirteen were at low risk of bias, and eleven had some concerns. Each risk of bias item, presented as percentages across all included studies, is shown in Fig. 2 , and each risk-of-bias item for each included study is provided in online supplemental material. Combined with the risk of bias judgments, the certainty of evidence is shown in Fig. 3 .

Risk of bias across all included studies
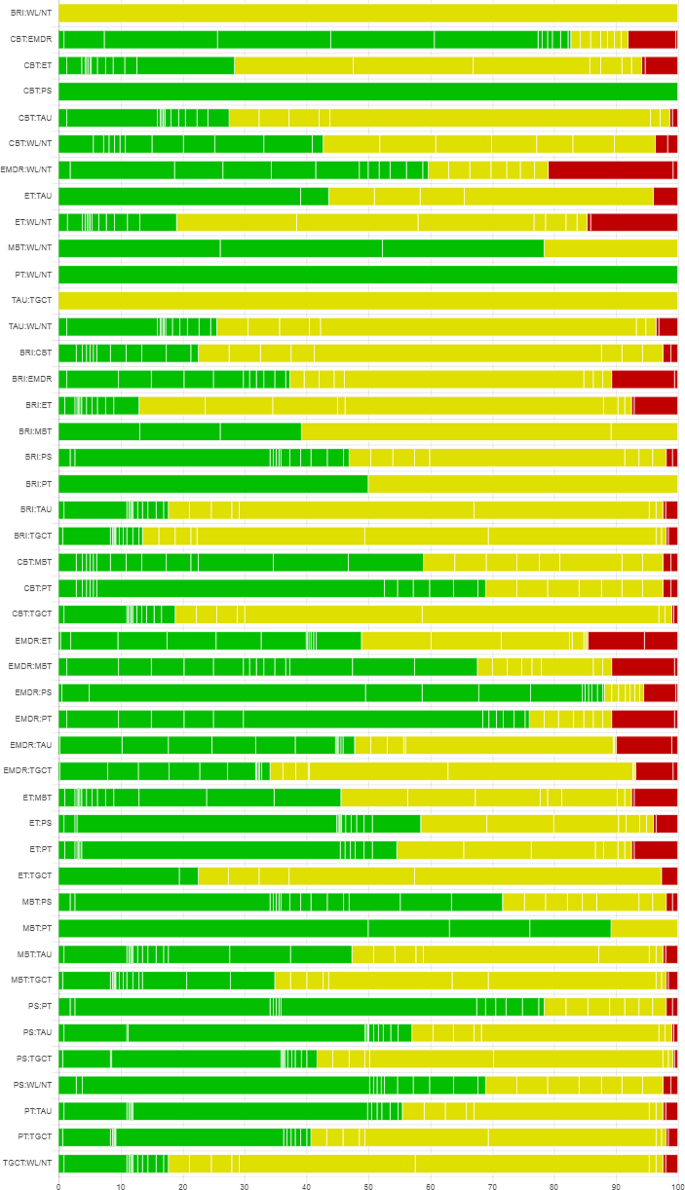
Risk of bias bar chart for the comparison of psychological interventions
PTSD symptoms at postintervention
Figure 4 presents the network plot of psychological interventions for the PTSD symptoms at postintervention, Table 2 shows the results of each analysis, and Fig. 5 illustrates the forest plots of head-to-head comparisons. EMDR (SMD = − 0.67; 95% CI − 1.17 to − 0.17), ET (SMD = − 0.66; 95% CI − 1.11 to − 0.22), and CBT (SMD = − 0.62; 95% CI − 0.90 to − 0.34) were significantly more effective than inactive intervention. For the other comparisons, the differences were not significant. The heterogeneity of pairwise comparisons was not found, except for one comparison (CBT versus inactive intervention, I 2 = 90.6). The design-by-treatment test was P = 0.960, indicating that the overall incoherence was not substantial. Loop-specific heterogeneity results were not significant for all five loops. There was no statistical disagreement between direct and indirect evidence for each comparison. The mean rank of each psychological intervention was estimated, indicating that EMDR and ET were ranked best according to the SUCRA and cumulative probability plots (online supplemental material). Results of sensitivity analyses confirmed that EMDR had the best performance compared with other interventions.

Network plots of evidence for PTSD and depression symptoms at postintervention and follow-up

Forest plots of head-to-head comparisons for PTSD symptoms at postintervention
PTSD symptoms at follow-up
Figure 4 presents the network plot of psychological interventions for PTSD symptoms at follow-up, Table 2 shows the results of each analysis, and Fig. 6 illustrates the forest plots of head-to-head comparisons. EMDR (SMD = − 0.72; 95% CI − 1.11 to − 0.33) and ET (SMD = − 0.62; 95% CI − 0.97 to − 0.27) were significantly more effective than the inactive intervention. The differences were insignificant for other psychological interventions compared with the inactive intervention. The heterogeneity of pairwise comparisons was not found. The design-by-treatment test was P = 0.178, suggesting that overall incoherence was not significant. Significant loop-specific heterogeneity emerged for one loop involving ET, CBT, and TAU ( Z = 2.265, P < 0.05). No evidence of statistical disagreement between direct and indirect evidence for each comparison was found, except for the comparison between CBT and TAU ( P < 0.05). The mean rank of each psychological intervention was estimated, indicating that EMDR was ranked best according to the SUCRA and cumulative probability plots (online supplemental material).

Forest plots of head-to-head comparisons for PTSD symptoms at follow-up
Depression symptoms at postintervention
Figure 4 presents the network plot of psychological interventions for depression symptoms at postintervention, Table 2 shows the results of each analysis, and Fig. 7 illustrates the forest plots of head-to-head comparisons. EMDR (SMD = − 0.40; 95% CI − 0.78 to − 0.03) and play therapy (PT) (SMD = − 0.37; 95% CI − 0.62 to − 0.12) were significantly more effective than the inactive intervention. The differences were insignificant for other psychological interventions compared with the inactive intervention. The heterogeneity of pairwise comparisons was not found. The design-by-treatment test was P = 0.175, suggesting that overall incoherence was not significant. Intra-loop incoherence was not substantial for all three loops. No evidence of statistical disagreement between direct and indirect evidence for each comparison was found, except for the comparison between CBT and WL/NT ( P < 0.05). The mean rank of each psychological intervention was estimated, indicating that EMDR was ranked best according to the SUCRA and cumulative probability plots (online supplemental material).

Forest plots of head-to-head comparisons for depression symptoms at postintervention
Depression symptoms at follow-up
Figure 4 presents the network plot of psychological interventions for depression symptoms at follow-up, Table 2 shows the results of each analysis, and Fig. 8 illustrates the forest plots of head-to-head comparisons. The differences were not significant for all psychological interventions compared with inactive interventions. The heterogeneity of pairwise comparisons was not found. The design-by-treatment test was P < 0.01, suggesting overall incoherence. Significant loop-specific heterogeneity emerged for one loop involving CBT, TAU, and WL/NT ( Z = 2.353, P < 0.05). There was no statistical disagreement between direct and indirect evidence for each comparison except for two comparisons (WL/NT and TAU, P < 0.001; CBT and TAU, P < 0.001). The mean rank of each psychological intervention was estimated, indicating that EMDR was ranked best according to the SUCRA and cumulative probability plots (online supplemental material).

Forest plots of head-to-head comparisons for depression symptoms at follow-up
Subgroup analyses
Subgroup analyses by level of intervention, profession of treatment provider, and country income level were performed (online supplemental material). For level of intervention, overall incoherence on PTSD and depression symptoms at postintervention and follow-up emerged. For individual interventions, EMDR ranked best on PTSD symptoms for both postintervention and follow-up. Regarding the profession of treatment provider, no overall incoherence was found between professionals and lay counselors on PTSD symptoms at postintervention. In the psychologist/psychiatrist category, ET showed the most favorable outcomes, and CBT showed the greatest improvement in the teacher/counselor category according to the mean SUCRA and cumulative probability plots. EMDR showed the greatest improvement in the psychologist/psychiatrist category on PTSD symptoms at follow-up, and PT showed the most favorable outcomes in the teacher/counselor category on depression symptoms at postintervention. For country income level on PTSD symptoms at postintervention, no overall incoherence between HICs and LMICs groups emerged. ET ranked best in LMICs, and EMDR ranked best in HICs according to the mean SUCRA and cumulative probability plots. For PTSD symptoms at follow-up, ET ranked best in LMICs. The remaining subgroup analyses were not performed due to unavailability of pairs of interventions with both direct and indirect comparisons.
Publication bias
Global funnel plots for outcomes were performed, as documented in the online supplemental material. There was potential publication bias for PTSD symptoms at postintervention, while there was no potential publication bias for PTSD symptoms at follow-up. No evidence of potential publication bias was shown for depression symptoms, either post-intervention or at follow-up. Visual inspections of funnel plots for subgroups were also conducted and are presented in the online supplemental material.
The current NMA comprised results from 26 studies on 4331 children and adolescents exposed to natural or man-made disasters, estimating the relative intervention effects of psychological interventions for participants with PTSD symptoms and depression symptoms. The rank probability for each psychological intervention was calculated to evaluate the most effective interventions at postintervention and 1–12 month follow-up. Overall, the results showed some psychological interventions to be effective for PTSD and depression symptoms compared to control groups.
In these included studies, EMDR, ET, and CBT were found to reduce PTSD symptoms significantly at postintervention. Similar results were obtained at follow-up, with EMDR and ET appearing to be effective interventions. Compared with inactive intervention, the results for other interventions were inconclusive because 95% CI of effects crossed the line of effect. EMDR was found at the top of the hierarchy, suggesting it to be the most effective intervention for reducing PTSD symptoms in children and adolescents with PTSD at postintervention and follow-up. Based on the included studies in this NMA, EMDR was found to have the greatest effectiveness at postintervention and follow-up and should be recommended. Although CBT had a slightly lower effect size than EMDR and ET, CBT was the most represented psychological intervention, suggesting that the evidence is more robust. However, the evidence of CBT’s long-term effectiveness is limited due to the insignificant effect size. The results of this NMA were consistent with previous reviews that used standard meta-analysis techniques. Brown and colleagues found CBT, EMDR, narrative exposure therapy for children (KIDNET), and classroom-based interventions have similar efficacy [ 6 ]. A meta-analysis conducted by Newman et al. also showed the significant effect sizes of psychological intervention on reducing PTSD symptoms in children and adolescents after disasters, finding that EMDR, ET, and Strict CBT appeared to have the largest effect sizes [ 7 ]. In line with previous meta-analyses, EMDR, ET, and CBT are effective at reducing PTSD symptoms in children and adolescents affected by natural and man-made disasters.
Our analysis also found that EMDR and PT may effectively treat depression in children and adolescents post-disaster at postintervention. However, all psychological interventions failed to show significant effect sizes at follow-up. Previous meta-analyses of intervention studies in children and adolescents exposed to disasters have found a range of results, from no effects on depression [ 12 , 52 ] to minimal effects [ 53 ]. Consistent with previous studies, most psychological interventions showed no effect in the current review. Even though EMDR and PT significantly reduced depression symptoms at postintervention, the effect sizes were small. PTSD is the most prevalent mental disorder in children and adolescents exposed to natural and man-made disasters. Most psychological interventions were designed to treat PTSD rather than depression. Therefore, the effectiveness of depression interventions is relatively limited. One study that employed a short-term group PT substantially reduced depression and anxiety in children after the earthquake [ 50 ]. In addition, we also tried to explore the effect of intervention on anxiety, but the analysis failed due to insufficient studies.
EMDR effectively reduces PTSD and depression in children and adolescents affected by disasters, grounded in the Adaptive Information Processing (AIP) model [ 54 ]. This model posits that humans have a natural system for integrating new experiences into adaptive memory networks, linking experiences to thoughts, images, emotions, and sensations. Disorders arise when information is improperly processed, leading to maladaptive storage in these networks, re-triggering traumatic memories through similar stimuli. The AIP model suggests that proper processing of these memories, especially using EMDR’s bilateral stimulation such as eye movements, can alleviate symptoms and promote healing. During EMDR therapy, children and adolescents concentrate on the worst images in their traumatic memories while also following the therapist’s fingers with rhythmic, bilateral, pulsating eye movements. This dual attention task can process traumatic memories, thereby alleviating symptoms of PTSD and depression [ 55 ]. In contrast to conventional psychological interventions, EMDR surpasses the limitations inherent in traditional talk therapy modalities. It obviates the need for children and adolescents to engage in deep, focused contemplation of their traumatic experiences. Rather, through the process of eye movements, it facilitates the association and integration of targeted traumatic memories via associative pathways.
Some imitations should be accounted for when interpreting these NMA results. First, the number of studies included in this review was relatively low. Considering the quality of the studies, we selected studies that employed RCTs. Many researchers were urged to provide immediate intervention for children and adolescents following natural and man-made disasters. In many cases, it is impossible to have a group of participants with inactive interventions such as WL or NT conditions to control for spontaneous symptom remission due to ethical concerns [ 33 ]. Limiting studies to those published in English-language, peer-reviewed journals could increase the risk of publication bias. Second, the number of direct comparisons between active psychological interventions was also relatively low. Most of the findings were based on comparisons of indirect treatments, which are more likely to have biases. Moreover, the original studies did not adequately report the results at follow-up, which led to poorly connected networks. Third, subgroup and sensitivity analyses cannot fully interpret the statistical heterogeneity detected in some comparisons. Many aspects could impact heterogeneity, such as the number of participants in each group, the mean age of participants, outcome measures, sessions of interventions, and time since disasters. Overall coherence, the key statistical manifestation of transitivity, appeared accepted in most analyses. Four, WL and NT were combined into one group because they were inactive, and keeping them together was more appropriate than other active interventions. WL was found to be less effective than NT because participants in WL would be aware that they can receive interventions after the study period is over and are likely to retain mental disorder symptoms. In contrast, participants in NT may be more active in relieving symptoms of PTSD and depression [ 56 ]. It is therefore recommended to use this NMA’s findings with caution.
Implications
The implications of this NMA are profound for the field of psychological interventions for children and adolescents exposed to natural or man-made disasters. The evidence suggests that EMDR stands out as the most effective intervention, based on the hierarchy of interventions; this indicates that it should be prioritized as a treatment option in the immediate aftermath of traumatic events. While the current NMA offers valuable insights into the immediate benefits of psychological interventions for disaster-affected youths, it also calls for a more in-depth and nuanced approach to research and treatment. Stakeholders, including clinicians, researchers, and policymakers, should take these findings into account when designing, implementing, and funding interventions for this vulnerable population.
This NMA revealed that EMDR appears to be most efficacious in reducing PTSD and depression symptoms in children and adolescents exposed to natural and man-made disasters. In addition, ET and CBT are potentially effective in reducing PTSD symptoms at postintervention, while PT is effective in managing depression symptoms at the treatment endpoint. Other psychological interventions fail to affect this population. Further study is needed to support the results of the current NMA, as the evidence of findings was very limited. Moreover, more research is required to examine interventions’ long-term effectiveness in children and adolescents, particularly for depression symptoms.
Data availability
The datasets generated in this review are available from the corresponding author on reasonable request.
Makwana N. Disaster and its impact on mental health: a narrative review. J Family Med Prim Care. 2019;8(10):3090.
Article PubMed PubMed Central Google Scholar
Hackbarth M, Pavkov T, Wetchler J, Flannery M. Natural disasters: an assessment of family resiliency following Hurricane Katrina. J Marital Fam Ther. 2012;38(2):340–51.
Article PubMed Google Scholar
Peek L. Children and disasters: understanding vulnerability, developing capacities, and promoting resilience—An introduction. Child Youth Environ. 2008;18(1):1–29.
Article Google Scholar
Marthoenis M, Ilyas A, Sofyan H, Schouler-Ocak M. Prevalence, comorbidity and predictors of post-traumatic stress disorder, depression, and anxiety in adolescents following an earthquake. Asian J Psychiatry. 2019;43:154–9.
Maclean JC, Popovici I, French MT. Are natural disasters in early childhood associated with mental health and substance use disorders as an adult? Soc Sci Med. 2016;151:78–91.
Brown RC, Witt A, Fegert JM, Keller F, Rassenhofer M, Plener PL. Psychosocial interventions for children and adolescents after man-made and natural disasters: a meta-analysis and systematic review. Psychol Med. 2017;47(11):1893–905.
Article CAS PubMed Google Scholar
Newman E, Pfefferbaum B, Kirlic N, Tett R, Nelson S, Liles B. Meta-analytic review of psychological interventions for children survivors of natural and man-made disasters. Curr Psychiatry Rep. 2014;16:1–10.
Pfefferbaum B, Nitiéma P, Newman E, Patel A. The benefit of interventions to reduce posttraumatic stress in youth exposed to mass trauma: a review and meta-analysis. Prehosp Disaster Med. 2019;34(5):540–51.
Bhatnagar N, Lakshmi PVM, Jeyashree K. Multiple treatment and indirect treatment comparisons: an overview of network meta-analysis. Perspect Clin Res. 2014;5(4):154.
Moher D, Liberati A, Tetzlaff J, Altman DG. Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41.
Fu C, Underwood C. A meta-review of school-based disaster interventions for child and adolescent survivors. J Child Adolesc Mental Health. 2015;27(3):161–71.
Pfefferbaum B, Nitiéma P, Newman E. A meta-analysis of intervention effects on depression and/or anxiety in youth exposed to political violence or natural disasters. Child Youth Care Forum. 2019;48:449–77.
Altman DG, Bland JM. Detecting skewness from summary information. BMJ. 1996;313(7066):1200.
Article CAS PubMed PubMed Central Google Scholar
Higgins JPT, Thomas J, Chandler J, editors. Cochrane. Handbook for Systematic Reviews of Interventions., 2020.
White IR. NMA Stata J. 2015;15:951–85.
White IR. Multivariate random-effects meta-analysis. Stata J. 2009;9(1):40–56.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Lu G, Ades AE. Combination of direct and indirect evidence in mixed treatment comparisons. Stat Med. 2004;23(20):3105–24.
Jansen JP, Cope S. Meta-regression models to address heterogeneity and inconsistency in network meta-analysis of survival outcomes. BMC Med Res Methodol. 2012;12:1–16.
Veroniki AA, Vasiliadis HS, Higgins JP, Salanti G. Evaluation of inconsistency in networks of interventions. Int J Epidemiol. 2013;42(1):332–45.
Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta-analysis of randomized controlled trials. J Clin Epidemiol. 1997;50(6):683–91.
Krahn U, Binder H, König J. A graphical tool for locating inconsistency in network meta-analyses. BMC Med Res Methodol. 2013;13(1):1–18.
Higgins JPT, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi‐arm studies. Res Synthesis Methods. 2012;3(2):98–110.
Article CAS Google Scholar
Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, Higgins. J. P. recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ (2011): 343.
Salanti G, Del Giovane C, Chaimani A, Caldwell DM, Higgins JP. Evaluating the quality of evidence from a network meta-analysis. PLoS ONE. 2014;9(7):e99682.
Ahmadi SJ, Musavi Z, Samim N, Sadeqi M, Jobson L. Investigating the feasibility, acceptability and efficacy of using modified-written exposure therapy in the aftermath of a terrorist attack on symptoms of posttraumatic stress disorder among Afghan adolescent girls. Front Psychiatry. 2022;13:826633.
Amin R, Nadeem E, Iqbal K, Asadullah MA, Hussain B. Support for students exposed to trauma (SSET) program: an approach for building resilience and social support among flood-impacted children. School Mental Health. 2020;12(3):493–506.
Bahar Z, ÖZtürk M, Beşer A, Baykara A, Eker G, Cakaloz B. Evaluation of interventions based on depression sign scores of adolescents. Social Behav Personality: Int J. 2008;36(1):123–34.
Banoğlu K, Korkmazlar Ü. Efficacy of the eye movement desensitization and reprocessing group protocol with children in reducing posttraumatic stress disorder in refugee children. Eur J Trauma Dissociation. 2022;6(1):100241.
Barron I, Abdallah G, Heltne U. Randomized control trial of teaching recovery techniques in rural occupied Palestine: effect on adolescent dissociation. J Aggress Maltreatment Trauma. 2016;25(9):955–73.
Baum NL, Cardozo BL, Pat-Horenczyk R, Ziv Y, Blanton C, Reza A, Brom D. Training teachers to build resilience in children in the aftermath of war: a cluster randomized trial. Child Youth Care Forum. 2013;42:339–50.
Bolton P, Bass J, Betancourt T, Speelman L, Onyango G, Clougherty KF, Verdeli H. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA. 2007;298(5):519–27.
Catani C, Kohiladevy M, Ruf M, Schauer E, Elbert T, Neuner F. Treating children traumatized by war and tsunami: a comparison between exposure therapy and meditation-relaxation in North-East Sri Lanka. BMC Psychiatry. 2009;9:1–11.
Chemtob CM, Nakashima J, Carlson JG. Brief treatment for elementary school children with disaster-related posttraumatic stress disorder: a field study. J Clin Psychol. 2002;58(1):99–112.
Chen Y, Shen WW, Gao K, Lam CS, Chang WC, Deng H. Effectiveness RCT of a CBT intervention for youths who lost parents in the Sichuan, China, earthquake. Psychiatric Serv. 2014;65(2):259–62.
Dawson K, Joscelyne A, Meijer C, Steel Z, Silove D, Bryant RA. A controlled trial of trauma-focused therapy versus problem-solving in islamic children affected by civil conflict and disaster in Aceh, Indonesia. Australian New Z J Psychiatry. 2018;52(3):253–61.
de Roos C, Greenwald R, den Hollander-Gijsman M, Noorthoorn E, van Buuren S, De Jongh. A. A randomised comparison of cognitive behavioural therapy (CBT) and eye movement desensitisation and reprocessing (EMDR) in disaster-exposed children. Eur J Psychotraumatology. 2011;2(1):5694.
Dhital R, Shibanuma A, Miyaguchi M, Kiriya J, Jimba M. Effect of psycho-social support by teachers on improving mental health and hope of adolescents in an earthquake-affected district in Nepal: a cluster randomized controlled trial. PLoS ONE. 2019;14(10):e0223046.
Gordon JS, Staples JK, Blyta A, Bytyqi M, Wilson AT. Treatment of posttraumatic stress disorder in postwar kosovar adolescents using mind-body skills groups: a randomized controlled trial. J Clin Psychiatry. 2008;69(9):1469.
Jordans MJ, Komproe IH, Tol WA, Kohrt BA, Luitel NP, Macy RD, De Jong JT. Evaluation of a classroom-based psychosocial intervention in conflict-affected Nepal: a cluster randomized controlled trial. J Child Psychol Psychiatry. 2010;51(7):818–26.
Kalantari M, Yule W, Dyregrov A, Neshatdoost H, Ahmadi SJ. Efficacy of writing for recovery on traumatic grief symptoms of Afghani refugee bereaved adolescents: a randomized control trial. OMEGA-Journal Death Dying. 2012;65(2):139–50.
Layne, C. M., Saltzman, W. R., Poppleton, L., Burlingame, G. M., Pašalić, A., Duraković,E., … Pynoos, R. S. Effectiveness of a school-based group psychotherapy program for war-exposed adolescents: A randomized controlled trial. Journal of the American Academy of Child & Adolescent Psychiatry (2008) 47(9): 1048–1062.
Mohammadi M-GJ, Yasami MR, Ali MT, Naderi RN, F., Moftakhari O. The effects of a short-term cognitive behavioral group intervention on bam earthquake related PTSD symptoms in adolescents. Iran J Psychiatry. 2009;4:79–84.
Google Scholar
McMullen J, O’callaghan P, Shannon C, Black A, Eakin J. Group trauma-focused cognitive‐behavioural therapy with former child soldiers and other war‐affected boys in the DR Congo: a randomised controlled trial. J Child Psychol Psychiatry. 2013;54(11):1231–41.
Ooi CS, Rooney RM, Roberts C, Kane RT, Wright B, Chatzisarantis N. The efficacy of a group cognitive behavioral therapy for war-affected young migrants living in Australia: a cluster randomized controlled trial. Front Psychol. 2016;7:1641.
Pityaratstian N, Piyasil V, Ketumarn P, Sitdhiraksa N, Ularntinon S, Pariwatcharakul P. Randomized controlled trial of group cognitive behavioural therapy for post-traumatic stress disorder in children and adolescents exposed to tsunami in Thailand. Behav Cogn Psychother. 2015;43(5):549–61.
Qouta SR, Palosaari E, Diab M, Punamäki RL. Intervention effectiveness among war-affected children: a cluster randomized controlled trial on improving mental health. J Trauma Stress. 2012;25(3):288–98.
Ronan KR, Johnston DM. Behaviourally-based interventions for children following volcanic eruptions: an evaluation of effectiveness. Disaster Prev Management: Int J. 1999;8(3):169–76.
Ruf M, Schauer M, Neuner F, Catani C, Schauer E, Elbert T. Narrative exposure therapy for 7-to 16‐year‐olds: a randomized controlled trial with traumatized refugee children. J Trauma Stress. 2010;23(4):437–45.
Shen YJ. Short-term group play therapy with Chinese earthquake victims: effects on anxiety, depression and adjustment. Int J Play Therapy. 2002;11(1):43.
Zhu, Z., Wang, R., Kao, H. S., Zong, Y., Liu, Z., Tang, S., … Lam, S. P. Effect of calligraphy training on hyperarousal symptoms for childhood survivors of the 2008 China earthquakes. Neuropsychiatric Disease and Treatment (2014): 977–985.
Purgato, M., Gross, A. L., Betancourt, T., Bolton, P., Bonetto, C., Gastaldon, C.,… Barbui, C. Focused psychosocial interventions for children in low-resource humanitarian settings: a systematic review and individual participant data meta-analysis. The Lancet Global Health (2018) 6(4): e390-e400.
Morina N, Malek M, Nickerson A, Bryant RA. Psychological interventions for post-traumatic stress disorder and depression in young survivors of mass violence in low-and middle-income countries: meta-analysis. Br J Psychiatry. 2017;210(4):247–54.
Shapiro F. EMDR, adaptive information processing, and case conceptualization. J EMDR Pract Res. 2007;1:68–87.
Landin-Romero R, Moreno-Alcazar A, Pagani M, Amann BL. How Does Eye Movement Desensitization and Reprocessing Therapy Work? A Systematic Review on Suggested Mechanisms of Action. Front. Psychol (2018) 9:1395.
Furukawa TA, Noma H, Caldwell DM, Honyashiki M, Shinohara K, Imai H, Churchill R. Waiting list may be a nocebo condition in psychotherapy trials: a contribution from network meta-analysis. Acta Psychiatrica Scandinavica. 2014;130(3):181–92.
Download references
This study was funded by Anhui Province Philosophy and Social Science Planning Project (Grant No. AHSKQ2020D128).
Author information
Authors and affiliations.
School of Educational Science, Anhui Normal University, Wuhu, China
Yu Xie, Lijun Wang, Zhendong Wan, Chen Su, Shuyu Duan & Chenxi Xu
School of Computer and Information, Anhui Normal University, Wuhu, China
Office of Scientific Research, XuanCheng Vocational & Technical College, Xuancheng, China
School of Educational Science, Jiangsu Second Normal University, Nanjing, China
You can also search for this author in PubMed Google Scholar
Contributions
YX and BK were involved in the design, searching strategy, analysis and review of the article, report, and manuscript writing. YX, BK and XZ were involved in the revision of the manuscript. JY, LW, and ZW made contributions to the interpretation of the results. YX and CS were involved in the data extraction. SD and CX made contributions to the quality assessment of the included studies. All authors participated in and approved the final manuscript.
Corresponding author
Correspondence to Binbin Kan .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Xie, Y., Zhu, X., Wang, L. et al. A network meta-analysis of psychological interventions for children and adolescents after natural and man-made disasters. BMC Psychiatry 24 , 468 (2024). https://doi.org/10.1186/s12888-024-05924-8
Download citation
Received : 11 October 2023
Accepted : 20 June 2024
Published : 25 June 2024
DOI : https://doi.org/10.1186/s12888-024-05924-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Network meta-analysis
- Post-traumatic stress disorder
- Intervention
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
The relationship between childhood trauma, PTSD symptoms, and perceived leadership competence: have we protected our future leaders?
- Published: 06 July 2024
Cite this article

- Stanley Kam Ki Lam ORCID: orcid.org/0000-0002-6544-795X 1 ,
- Hong Wang Fung ORCID: orcid.org/0000-0002-4606-2173 2 &
- Vincent Wan Ping Lee ORCID: orcid.org/0000-0003-4574-636X 3
Leadership is an important competency across different fields and is a key to socio-economic development. Although leadership involves various social-emotional competencies that can be profoundly affected by childhood trauma, it remains unknown about the potential relationship between childhood trauma and leadership. This study examined whether childhood trauma and complex post-traumatic stress disorder (PTSD) symptoms would be negatively associated with leadership competence. A convenience sample of N = 411 Hong Kong adults (Age: M = 38.6, SD = 12.9) completed self-report measures of the studied variables in an online survey. Hierarchical multiple regression showed that childhood betrayal trauma (β = − 0.140, p =.008) but not non-betrayal trauma (β = 0.035, p =.491) was significantly, negatively associated with perceived leadership competence, even after controlling for covariates. When symptoms of complex PTSD were added into the model, disturbances in self-organization (DSO) symptoms were also a significant factor associated with perceived leadership competence (β = − 0.454, p <.001). This study is the first to show that childhood betrayal trauma and its major mental health consequences (i.e., complex PTSD symptoms) are negatively associated with perceived leadership competence. The findings expand our limited understanding of the socio-economic correlates of childhood trauma and point to the social and economic importance of child protection. If we make efforts to prevent childhood trauma, we may possibly protect our future leaders.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or Ebook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Data availability
Data that support the findings of this study are available from the corresponding authors upon reasonable request.
Abraham, P. J. (2011). Developing nurse leaders: A program enhancing staff nurse leadership skills and professionalism. Nursing Administration Quarterly , 35 (4), 306–312.
Article PubMed Google Scholar
Baird, A. M., & Parayitam, S. (2019). Employers’ ratings of importance of skills and competencies college graduates need to get hired. Education + Training , 61 (5), 622–634. https://doi.org/10.1108/ET-12-2018-0250 .
Article Google Scholar
Bertule, M., Sebre, S. B., & Kolesovs, A. (2021). Childhood abuse experiences, depression and dissociation symptoms in relation to suicide attempts and suicidal ideation. Journal of Trauma & Dissociation , 22 (5), 598–614. https://doi.org/10.1080/15299732.2020.1869652 .
Can, S. H., Hendy, H. M., Berkay, E., & Can, M. (2017). A pilot study to develop the police transformational Leadership Scale (PTLS) and examine its associations with psychosocial well-being of officers. Journal of Police and Criminal Psychology , 32 (2), 105–113. https://doi.org/10.1007/s11896-016-9204-y .
Chan, C. K. Y. (2021). Leadership competency . University of Hong Kong. https://www.have.hku.hk/leadership .
Google Scholar
Chan, C. K. Y., & Luk, L. Y. Y. (2021). Development and validation of an instrument measuring undergraduate students’ perceived holistic competencies. Assessment & Evaluation in Higher Education , 46 (3), 467–482. https://doi.org/10.1080/02602938.2020.1784392 .
Chan, C., Fung, H. W., Choi, T. M., & Ross, C. A. (2017). Using online methods to develop and examine the Hong Kong Chinese translation of the dissociative experiences Scale. Journal of Evidence-Informed Social Work , 14 (2), 70–85. https://doi.org/10.1080/23761407.2017.1298073 .
Cheung, C. T., Cheng, C. M. H., Lee, V. W. P., Lam, S. K. K., He, K. L., Ling, H. W. H., & Fung, H. W. (2024). Could family well-being moderate the relationship between adverse childhood experiences and somatoform dissociation? A preliminary investigation. Journal of Trauma & Dissociation , 25 (2), 153–167.
Cloitre, M., Cohen, L. R., Ortigo, K. M., Jackson, C., & Koenen, K. C. (2020). Treating survivors of childhood abuse and interpersonal trauma: STAIR Narrative Therapy (2nd ed.). The Guilford Press.
Cloitre, M., Hyland, P., Prins, A., & Shevlin, M. (2021). The international trauma questionnaire (ITQ) measures reliable and clinically significant treatment-related change in PTSD and complex PTSD. European Journal of Psychotraumatology , 12 (1), 1930961.
Article PubMed PubMed Central Google Scholar
Cummings, G., Lee, H., Macgregor, T., Davey, M., Wong, C., Paul, L., & Stafford, E. (2008). Factors contributing to nursing leadership: A systematic review. Journal of Health Services Research & Policy , 13 (4), 240–248. https://doi.org/10.1258/jhsrp.2008.007154 .
Cummings, G. G., Lee, S., Tate, K., Penconek, T., Micaroni, S. P. M., Paananen, T., & Chatterjee, G. E. (2021). The essentials of nursing leadership: A systematic review of factors and educational interventions influencing nursing leadership. International Journal of Nursing Studies , 115 , 103842. https://doi.org/10.1016/j.ijnurstu.2020.103842 .
Day, D. V., & Dragoni, L. (2015). Leadership development: An outcome-oriented review based on time and levels of analyses. Annual Review of Organizational Psychology and Organizational Behavior , 2 (1), 133–156. https://doi.org/10.1146/annurev-orgpsych-032414-111328 .
Day, D. V., Fleenor, J. W., Atwater, L. E., Sturm, R. E., & McKee, R. A. (2014). Advances in leader and leadership development: A review of 25years of research and theory. The Leadership Quarterly , 25 (1), 63–82. https://doi.org/10.1016/j.leaqua.2013.11.004 .
Dehghan Manshadi, Z., Neshat-Doost, H. T., & Jobson, L. (2024). Cognitive factors as mediators of the relationship between childhood trauma and depression symptoms: The mediating roles of cognitive overgeneralisation, rumination, and social problem-solving. European Journal of Psychotraumatology , 15 (1), 2320041.
Dong, C., Xu, R., & Xu, L. (2021). Relationship of childhood trauma, psychological resilience, and family resilience among undergraduate nursing students: A cross-sectional study. Perspectives in Psychiatric Care , 57 (2), 852–859.
Font, S. A., & Berger, L. M. (2015). Child maltreatment and children’s developmental trajectories in early to middle childhood. Child Development , 86 (2), 536–556. https://doi.org/10.1111/cdev.12322 .
Freyd, J. J. (2008). Betrayal trauma. In G. Reyes, J. D. Elhai, & J. D. Ford (Eds.), Encyclopedia of psychological trauma . Wiley.
Fung, H. W., Chung, H. M., & Ross, C. A. (2020). Demographic and mental health correlates of childhood emotional abuse and neglect in a Hong Kong sample. Child Abuse & Neglect , 99 , 104288. https://doi.org/10.1016/j.chiabu.2019.104288
Fung, H. W., Chien, W. T., Ling, H. W., Ross, C. A., & Lam, S. K. K. (2022). The mediating role of post-traumatic stress disorder symptoms in the relationship between childhood adversities and depressive symptoms in two samples. Child Abuse & Neglect, 131 , 105707. https://doi.org/10.1016/j.chiabu.2022.105707
Fung, H. W., Chien, W. T., Chan, C., & Ross, C. A. (2023). A cross-cultural investigation of the Association between Betrayal Trauma and dissociative features. Journal of Interpersonal Violence , 38 (1–2), 1630–1653. https://doi.org/10.1177/08862605221090568 .
Fung, K., Hung, S. S. L., Lai, D. W. L., Shum, M. H. Y., Fung, H. W., & He, L. (2023b). Access to information and communication technology, digital skills, and perceived well-being among older adults in Hong Kong. International Journal of Environmental Research and Public Health , 20 (13), 6208. https://doi.org/10.3390/ijerph20136208 .
Glass, D. C., Kelsall, H. L., Slegers, C., Forbes, A. B., Loff, B., Zion, D., & Fritschi, L. (2015). A telephone survey of factors affecting willingness to participate in health research surveys. Bmc Public Health , 15 , 1017. https://doi.org/10.1186/s12889-015-2350-9 .
Gloria, N. I., Zeaghe, K. Y., Tutu, N. O., Mbe, M., & Ermeco, S. A. (2022). The nexus between childhood trauma and the emergence of leadership. Open Journal of Leadership , 11 (4), 335–355. https://doi.org/10.4236/ojl.2022.114018 .
Goldberg, L. R., & Freyd, J. J. (2006). Self-reports of potentially traumatic experiences in an adult community sample: Gender differences and test-retest stabilities of the items in a brief betrayal-trauma survey. Journal of Trauma & Dissociation , 7 (3), 39–63. https://doi.org/10.1300/J229v07n03_04 .
Gruzdev, M. V., Kuznetsova, I. V., Tarkhanova, I. Y., & Kazakova, E. I. (2018). University graduates’ soft skills: The employers’ opinion. European Journal of Contemporary Education , 7 (4), 690–698. https://doi.org/10.13187/ejced.2018.4.690 .
Hall, S. L., Scott, F., & Borsz, M. (2008). A constructivist case study examining the leadership development of undergraduate students in campus recreational sports. Journal of College Student Development , 49 (2), 125–140. https://doi.org/10.1353/csd.2008.0010 .
Harms, P., Credé, M., Tynan, M., Leon, M., & Jeung, W. (2017). Leadership and stress: A meta-analytic review. The Leadership Quarterly , 28 (1), 178–194. https://doi.org/10.1016/j.leaqua.2016.10.006 .
Ho, G. W., Karatzias, T., Cloitre, M., Chan, A. C., Bressington, D., Chien, W. T., & Shevlin, M. (2019). Translation and validation of the Chinese ICD-11 International Trauma Questionnaire (ITQ) for the Assessment of Posttraumatic Stress Disorder (PTSD) and Complex PTSD (CPTSD). European Journal of Psychotraumatology , 10 (1), 1608718.
Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., & Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health , 2 (8), e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4 .
Hughes, D. J., Lee, A., Tian, A. W., Newman, A., & Legood, A. (2018). Leadership, creativity, and innovation: A critical review and practical recommendations. The Leadership Quarterly , 29 (5), 549–569. https://doi.org/10.1016/j.leaqua.2018.03.001 .
Karagianni, D., & Jude Montgomery, A. (2018). Developing leadership skills among adolescents and young adults: A review of leadership programmes. International Journal of Adolescence and Youth , 23 (1), 86–98. https://doi.org/10.1080/02673843.2017.1292928 .
Liu, J., Shahwan, S., Abdin, E., Vaingankar, J. A., Basu, S., Tang, C., & Subramaniam, M. (2022). Adverse childhood experiences and positive psychotic symptoms: A nationally representative study in Singapore. Child Abuse & Neglect , 131 , 105778. https://doi.org/10.1016/j.chiabu.2022.105778 .
Loya, R. M. (2015). Rape as an economic crime: The impact of sexual violence on survivors’ employment and economic well-being. Journal of Interpersonal Violence , 30 (16), 2793–2813. https://doi.org/10.1177/0886260514554291 .
McKay, M. T., Cannon, M., Chambers, D., Conroy, R. M., Coughlan, H., Dodd, P., & Clarke, M. C. (2021). Childhood trauma and adult mental disorder: A systematic review and meta-analysis of longitudinal cohort studies. Acta Psychiatrica Scandinavica , 143 (3), 189–205. https://doi.org/10.1111/acps.13268 .
Miscenko, D., Guenter, H., & Day, D. V. (2017). Am I a leader? Examining leader identity development over time. The Leadership Quarterly , 28 (5), 605–620. https://doi.org/10.1016/j.leaqua.2017.01.004 .
Nijenhuis, E. R. S., & Van der Hart, O. (2011). Defining dissociation in trauma. Journal of Trauma & Dissociation , 12 (4), 469–473. https://doi.org/10.1080/15299732.2011.570599 .
Ortigo, K. M., Bauer, A., & Cloitre, M. (2020). Chapter 18 - Skills Training in Affective and Interpersonal Regulation (STAIR) Narrative Therapy: Making meaning while learning skills. In M. T. Tull & N. A. Kimbrel (Eds.), Emotion in Posttraumatic Stress Disorder (pp. 513–543). Academic Press. https://doi.org/10.1016/B978-0-12-816022-0.00018-1 .
Chapter Google Scholar
Pandey, J. (2018). Factors affecting job performance: An integrative review of literature. Management Research Review , 42 (2), 263–289. https://doi.org/10.1108/MRR-02-2018-0051 .
Pearson-Goff, M., & Herrington, V. (2013). Police leadership: A systematic review of the literature. Policing: A Journal of Policy and Practice , 8 (1), 14–26. https://doi.org/10.1093/police/pat027 .
Schwab-Reese, L. M., Hovdestad, W., Tonmyr, L., & Fluke, J. (2018). The potential use of social media and other internet-related data and communications for child maltreatment surveillance and epidemiological research: Scoping review and recommendations. Child Abuse & Neglect , 85 , 187–201. https://doi.org/10.1016/j.chiabu.2018.01.014
Su, S., Jimenez, M. P., Roberts, C. T., & Loucks, E. B. (2015). The role of adverse childhood experiences in cardiovascular disease risk: A review with emphasis on plausible mechanisms. Current Cardiology Reports , 17 (10), 88.
Sullivan, W. P. (2016). Leadership in social work: Where are we? Journal of Social Work Education, 52(1): S51-S61.. https://doi.org/10.1080/10437797.2016.1174644 .
Thai, T. T., Cao, P. L. T., Kim, L. X., Tran, D. P., Bui, M. B., & Bui, H. H. T. (2020). The effect of adverse childhood experiences on depression, psychological distress and suicidal thought in Vietnamese adolescents: Findings from multiple cross-sectional studies. Asian Journal of Psychiatry , 53 , 102134. https://doi.org/10.1016/j.ajp.2020.102134 .
Tian, L., Jiang, Y., & Yang, Y. (2022). CEO childhood trauma, social networks, and strategic risk taking. The Leadership Quarterly , 101618. https://doi.org/10.1016/j.leaqua.2022.101618 .
World Health Organization. (2019). The ICD-11 classification of Mental and behavioral disorders. Clinical description and diagnostic guidelines . Author.
Yasin, B., & Mustafa, F. (2020). The correlation between school principal leadership competence and teachers’ social behaviours. Indonesian Research Journal in Education| IRJE , 4 (1), 151–170. https://doi.org/10.22437/irje.v4i1.9093 .
Yuan, Y., Lee, H., Eack, S. M., & Newhill, C. E. (2023). A systematic review of the association between early childhood trauma and borderline personality disorder. Journal of Personality Disorders , 37 (1), 16–35.
Zacharatos, A., Barling, J., & Kelloway, E. K. (2000). Development and effects of transformational leadership in adolescents. The Leadership Quarterly , 11 (2), 211–226. https://doi.org/10.1016/S1048-9843(00)00041-2 .
Download references
Acknowledgements
The second author received The RGC Postdoctoral Fellowship Scheme 2022/2023 from the Research Grants Council (RGC), Hong Kong.
Author information
Authors and affiliations.
Nethersole School of Nursing, Faculty of Medicine, The Chinese University of Hong Kong, Shatin, Hong Kong
Stanley Kam Ki Lam
School of Nursing and Health Studies, Hong Kong Metropolitan University, Ho Man Tin, Hong Kong
Hong Wang Fung
Department of Social Work, Hong Kong Baptist University, Kowloon, Hong Kong
Vincent Wan Ping Lee
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hong Wang Fung .
Ethics declarations
Ethical considerations.
This study obtained ethical approval at the Chinese University of Hong Kong. All participants provided online written informed consent before participation.
Conflict of interest
Additional information, publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Lam, S.K.K., Fung, H.W. & Lee, V.W.P. The relationship between childhood trauma, PTSD symptoms, and perceived leadership competence: have we protected our future leaders?. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06269-x
Download citation
Accepted : 13 June 2024
Published : 06 July 2024
DOI : https://doi.org/10.1007/s12144-024-06269-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Childhood trauma
- Betrayal trauma
- Psychosocial correlates of maltreatment
- Find a journal
- Publish with us
- Track your research
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- Wunderkinds Nomination
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
Turning a ‘no’ vote into progress: How to advance MDMA-assisted psychotherapy for PTSD
By Andrew D. Forsyth , Mallory O. Johnson , and Jae M. Sevelius June 25, 2024

M any people have interpreted as a setback the “no” vote by an advisory committee to the Food and Drug Administration on Lykos Therapeutics’ new drug application for MDMA-assisted psychotherapy for post-traumatic stress disorder. We believe it is an opportunity to build upon Lykos’ success and rally support for better-funded, well-controlled clinical trials to determine the safety and efficacy of a promising PTSD treatment.
Upon reviewing the FDA’s and Lykos’ briefing documents, the Psychopharmacologic Drugs Advisory Committee deemed the study data insufficient to approve the application, and it determined that the company’s risk evaluation and mitigation strategy did not fully address potential harms of this therapy.
advertisement
The committee’s concerns about study design and data limitations are not uncommon in clinical trials, especially those on psychedelics. However, Lykos’ reliance on philanthropy and donations may have limited its capacity to ensure the rigor needed to meet the agency’s evidentiary standards , particularly in neglecting to properly investigate and quantify the specific contributions of the psychotherapy component. These issues raise the possibility that better study planning and coordination , enabled by more extensive funding, may have mitigated these challenges.
The potential of MDMA-assisted psychotherapy for PTSD treatment
As the FDA noted in its briefing documents , PTSD is a condition affecting an estimated 13 million Americans that may arise following intensely distressing life events, such as threats of death, severe injury, or sexual violence. Besides intrusive memories, hyperarousal, and avoidant behavior, persons with PTSD have a higher risk of suicidal ideation and behavior. Although 60% respond to FDA-approved medications such as sertraline and paroxetine, only 20% to 30% achieve remission, underscoring a vast unmet need for effective PTSD treatments, particularly for those most likely to experience trauma (e.g., combat veterans, women, racial, sexual, and gender minorities).
Related: The inside story of how Lykos’ MDMA research went awry
First synthesized in the early 1900s, MDMA gained notoriety as the 1980s street drug ecstasy before being banned as a Schedule I substance . It resurfaced in the 1990s when clinical researchers noted its capacity to facilitate profound empathy and compassion toward self and others, making it a promising adjunct to psychotherapy . Of relevance to PTSD and other avoidance-based disorders is MDMA’s capacity to diminish fear responses and facilitate lasting shifts from avoidance to acceptance behaviors.
By reducing the aversiveness of unpleasant thoughts and emotions, MDMA enables greater tolerance of traumatic memories and enhances empathetic acceptance.
Understanding the MDMA trials and the committee’s decision
Lykos submitted data from two Phase 3 clinical trials, known as MAPP1 and MAPP2 , which compared the effects of MDMA-assisted psychotherapy for severe and at least moderate PTSD versus inactive placebo plus psychotherapy. Three cycles of treatment for each participant, provided over four months, consisted of preparatory sessions, an eight-hour medication session, and integrative therapy. Endpoints measured changes in symptoms and functional impairment at 18 weeks.
Both studies reported significant improvement with MDMA-assisted psychotherapy and limited evidence of adverse events.
After careful deliberation, the Psychopharmacologic Drugs Advisory Committee endorsed several concerns raised in the FDA’s briefing documents :
First, committee members were concerned that many participants guessed correctly their assignment to the MDMA-assisted and placebo conditions, which may have affected patient-reported outcomes. No additional analyses were reported to examine this possibility.
Second, the committee pointed out missing lab tests and underreported drug reactions like euphoria and elation, which are essential for assessing side effects and abuse potential.
Related: Oral ketamine tablets effective for treating depression, new study finds
Third, the panelists shared FDA’s concerns that there were insufficient safeguards to protect patients from coercion, misconduct, and injury following improper discharge after MDMA dosing sessions.
Fourth, the committee concluded that the proposed strategies to mitigate potential harms needed more provisions for therapist training and potential misconduct, external monitoring, on-site medical supervision, and ways for patients to report issues.
A need for improved clinical trials infrastructure
The MAPP1 and MAPP2 data exhibit many common shortcomings of clinical trials on psychedelics that make it challenging to be sure that the findings reflect unbiased estimates of the underlying phenomena, namely that MDMA-assisted psychotherapy for PTSD, as implemented by Lykos Therapeutics, is safe and effective.
Given the methodological noise, the reported findings suggest a promising signal that is hard to decipher. While acknowledging the challenges raised by these studies, the committee’s “no” vote does not discourage research on MDMA-assisted psychotherapy for PTSD. Rather, in line with the National Academies of Sciences, Engineering, and Medicine’s recommendations , it suggests the need for public sector collaboration and investment to support more rigorous clinical trials to advance knowledge and translate findings into new tools for mental health.
Two examples of such public investment are noteworthy. First, the National Institutes of Health’s HIV Clinical Trials Networks models how to support high-quality clinical research worldwide, with coordinated leadership and operations, laboratory, and statistical and data management centers collaborating with advocates, government, academia, industry, and nongovernmental organizations. These networks develop and test novel HIV treatments and cure strategies with state-of-the-science protocol development, research design, and data safety and monitoring.
A second example is the U.S. Department of Veterans Affairs’ National Center for PTSD , which seeks to improve clinical care for military veterans through interdisciplinary research on stress-related disorders. Recently, the VA issued its first request for applications since the 1960s to study psychedelic compounds for treating PTSD and depression. This initiative aligns with extant NIH efforts to establish a psychedelic science and medicine interest group , co-sponsor workshops , and a $7.3 million portfolio of predominantly preclinical psychedelic studies. Although the VA’s investments primarily benefit veterans, they highlight the potential for federal investment in clinical trials to identify safe and effective PTSD treatments.
Sign up for Morning Rounds
Understand how science, health policy, and medicine shape the world every day
A call to action
The Psychopharmacologic Drugs Advisory Committee’s vote on Lykos Therapeutics’ new drug application is a call to action for advocates, academics, political leaders, funding agencies, foundations, and the scientific community. Public investment is driven by affected communities advocating for their needs and resources to address morbidity and mortality risks. In the 1990s, HIV advocates in the U.S. drastically increased federal and state investment in HIV science, shortened NIH funding cycles, and accelerated access to experimental drugs, bringing control of the global pandemic within reach. Advocates for those with PTSD should follow their lead in pushing for the rapid development of safe and effective new therapies for a persistent threat to well-being.
The time is right. There is a receptive audience in Washington, D.C., for public investment in psychedelic-assisted psychotherapy: the bipartisan Congressional Psychedelics Advancing Clinical Treatments (PACT) Caucus , led by Reps. Lou Correa (D-Calif.) and Jack Bergman (R-Mich.), which aims to fund research on the safety, efficacy, and durability of these treatments to address the national mental health crisis. In the footsteps of Australia and the Netherlands , the U.S. must redouble its efforts to fund more rigorous clinical trials to determine the safety and efficacy of a promising PTSD treatment for those who stand to benefit from it.
Andrew D. Forsyth, Ph.D., is an independent consultant and former NIH program officer based in Berkeley, Calif. Mallory O. Johnson, Ph.D., is a professor of medicine and nursing at the University of California, San Francisco. Jae M. Sevelius, Ph.D., is a professor of medical psychology in the Department of Psychiatry at New York Presbyterian/Columbia University Irving Medical Center.
LETTER TO THE EDITOR
Have an opinion on this essay submit a letter to the editor here ., about the authors reprints, andrew d. forsyth, mallory o. johnson, jae m. sevelius.
psychedelics
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

My stalled relay race to get access to ALS drugs in development

President Biden needs a full medical evaluation. Voters deserve to know the results

STAT Plus: Ascension is racing to unload hospitals as execs work to stem losses

STAT Plus: How controversial was the decision by FDA’s Peter Marks to approve Sarepta’s gene therapy? Check its footnotes

STAT Plus: The biotech scorecard for the third quarter: 19 stock-moving events to watch
Environmental Science: Nano
Overlooked impact of surface hydroxylation on the solubility of less-soluble compounds: a case study of ceo 2 †.

* Corresponding authors
a Lomonosov Moscow State University, Department of Chemistry, Leninskie Gory 1/3, 119991 Moscow, Russia E-mail: [email protected]
b Kurnakov Institute of General and Inorganic Chemistry of the Russian Academy of Sciences, Leninskii prosp. 31, 117901 Moscow, Russia
c National Research Centre “Kurchatov Institute”, Akademika Kurchatova pl. 1, 123182 Moscow, Russia
d Max Planck Institute for Solid State Research, Heisenbergstraße 1, 70569 Stuttgart, Germany
e National Research University Higher School of Economics, Myasnitskaya st. 20, 101000 Moscow, Russia
Unexpectedly, the solubility of CeO 2 nanoparticles (NPs) at 25 °C does not depend on particle size, but is significantly affected by the sample's thermal pre-treatment. The classical interpretation of NPs' solubility proposed by the Gibbs–Thompson or Kelvin equations fails to describe the experimental data on CeO 2 solubility obtained in this study. Thermal treatment did not change the samples' morphological characteristics, while slightly affecting NP hydroxylation and local crystallinity. The differences in the solubility of dried and non-treated CeO 2 particles were most noticeable at pH < 4, and dissolved cerium concentration was much lower in the case of the dried sample. After prolonged storage (up to 4.5 years) of CeO 2 NPs in aqueous media, the solubility of dried samples gradually increased, while for non-treated samples it remained unchanged. Based on the example of CeO 2 , the dissolution laws of other less soluble nanomaterials should be reconsidered.

Supplementary files
- Supplementary information PDF (1514K)
Article information
Download citation, permissions.
Overlooked impact of surface hydroxylation on the solubility of less-soluble compounds: a case study of CeO 2
T. V. Plakhova, A. Yu. Romanchuk, A. D. Konyukhova, I. F. Seregina, A. E. Baranchikov, R. D. Svetogorov, M. W. Terban, V. K. Ivanov and S. N. Kalmykov, Environ. Sci.: Nano , 2024, Advance Article , DOI: 10.1039/D4EN00014E
To request permission to reproduce material from this article, please go to the Copyright Clearance Center request page .
If you are an author contributing to an RSC publication, you do not need to request permission provided correct acknowledgement is given.
If you are the author of this article, you do not need to request permission to reproduce figures and diagrams provided correct acknowledgement is given. If you want to reproduce the whole article in a third-party publication (excluding your thesis/dissertation for which permission is not required) please go to the Copyright Clearance Center request page .
Read more about how to correctly acknowledge RSC content .
Social activity
Search articles by author.
This article has not yet been cited.
Advertisements

Knowing when to call it quits takes courage and confidence - 3 case studies
Professor of Political Science, Trinity College
Chairperson and Associate Professor of Law, College of Staten Island, CUNY
Disclosure statement
Michael Paris occasionally volunteers with Democratic organizations.
Kevin J. McMahon does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Trinity College provides funding as a member of The Conversation US.
View all partners
After President Joe Biden’s disastrous performance at the June 27, 2024, debate, many Democrats have raced to ring the alarm bell, proclaiming that it’s time for him to step aside, time to let someone else take the reins in hopes of defeating Donald Trump in November.
With that in mind, as political scientists with a side interest in sports, we recount three moments from history when men and women faced the difficult decision to stay or go. We hope they will help inform the current discussion.
We begin with two who worked at the highest levels of power in the U.S.:
President Lyndon Johnson, 1968
On the final night of March 1968, President Lyndon B. Johnson, known universally as “LBJ,” spoke to the nation from the Oval Office to say that the United States would unilaterally halt nearly all its bombing in North Vietnam.
But as his address came to a close, he had something more to say:
Shocking his audience, LBJ added : “I shall not seek, and I will not accept, the nomination of my party for another term as your president.”
Johnson was 59 years old. Three-and-a-half years earlier, he had scored one of the greatest landslides in American history, winning 61% of the vote and 44 states in the 1964 presidential election .
A scant few individuals so aptly defined the term “political animal” as LBJ. He had come to Washington as a young man bursting with ambition and succeeded like few others.
Indeed, since becoming president after John F. Kennedy’s 1963 assassination , Johnson had ushered through Congress an avalanche of progressive legislation , including the historic 1964 Civil Rights and 1965 Voting Rights acts. With the possible exception of Franklin D. Roosevelt, no other president had achieved so much legislatively.
But on that March day in 1968, at a time of growing antiwar protests and the accelerating pull of rival candidates for the Democratic nomination, he understood that he now led a country coming apart at the seams. Despite having declared his candidacy for reelection, seeking another term might make things worse.
It was time for someone else to have a turn.
Justice Ruth Bader Ginsburg, 2013
As one of us recounts in his book, “ A Supreme Court Unlike Any Other: The Deepening Divide Between the Justices and the People ,” President Barack Obama invited Justice Ruth Bader Ginsburg for a private lunch at the White House in the summer of 2013.
Obama wanted to nudge Ginsburg into retirement. The 80-year-old justice was a two-time survivor of pancreatic cancer, one of the deadliest of all cancers. She had already served on the high court for two decades and had carved out a legacy as a staunch liberal and champion of women’s equality.
Additionally, Obama was concerned about the upcoming midterm elections. If the Democrats lost the Senate, he would not be able to replace her with a like-minded justice, because a GOP-run Senate would not confirm such a nominee.
Ginsburg didn’t take Obama’s hint.

Soon after the lunch, she noted, “ I think one should stay as long as she can do the job .” She added shortly after , “There will be a president after this one, and I’m hopeful that that president will be a fine president.”
That next president was Donald Trump.
Ginsburg died in mid-September 2020, just weeks before Joe Biden would oust Trump from the White House. But significantly, Trump had sufficient time to fill Ginsburg’s seat with the conservative Amy Coney Barrett .
In 2022, Barrett provided the fifth and decisive vote in the Dobbs decision, which overturned Roe v. Wade’s federal protection of abortion rights .
Deciding when to step away or stay may have deep consequences in the political world.
The consequences are big in sports, as well, but at a more personal level.
Philadelphia Eagle Jason Kelce, 2024
Skeptics said he was too small to play among the giants on an offensive line in the NFL. Not strong enough. Not tough enough. A former walk-on who had been drafted in 2011 in the sixth round .
But in a short space of time, Jason Kelce redefined the position of center and helped guide his team to its first-ever Super Bowl win.
In 2024, Kelce’s team, the Philadelphia Eagles, was still one of the best in the NFL. It had been to the Super Bowl just a year earlier, and Kelce was still considered to be playing near the top of his game.
But Kelce had had enough. It was time for him to end his playing days.
Sitting before a packed room of reporters and family members, the bare-armed and burly-chested 36-year-old Kelce set out to say goodbye .

But before he could even get a sentence out, his emotions took over, forcing him to pause for several moments. He held his head in his hands, sobbing, sniffling, snorting, taking deep breaths. Tears streamed down his face throughout the news conference. Repeatedly, he had to stop and wipe them away with a washcloth someone tossed to him.
As he struggled to get through his statement, listeners could hear him motivate himself several times with the phrase, “Come on.”
The ‘courage to call it quits’
Kelce’s retirement announcement is both difficult and extraordinarily captivating to watch. During those 40 minutes, he displays the courage it takes to call it quits when there is still something to be gained.
The picture was of a man coming to terms with his fate. Not because of injury or lack of skill, but because he believed it was necessary to take this step before those things forced him out.
Are there moments when we can judge for another when it is time to bow out? Most assuredly, there are. Hopefully, we do so with compassion and gratitude, but there are simply times when conscience demands an honest reckoning and unflinching truth-telling.
- Lyndon Baines Johnson
- Voting Rights Act
- US Constitution
- Political conventions
- US presidency
- Mental ageing
- 25th Amendment
- Philadelphia Eagles
- Civil Rights Act
- Ruth Bader Ginsburg
- US democracy

Sydney Horizon Educators – Faculty of Engineering (Targeted)

Dean, Faculty of Education

Lecturer in Indigenous Health (Identified)

Social Media Producer

PhD Scholarship

IMAGES
VIDEO
COMMENTS
Philip, a 60-year-old who was in a traffic accident (PDF, 294KB) This case example from the European Journal of Psychotraumatology details an assisted self-study application of cognitive therapy for PTSD. Philip developed PTSD and comorbid major depression following a traffic accident. He was treated in six sessions of cognitive therapy with ...
Case Study Details. Victor is a 27-year-old man who comes to you for help at the urging of his fiancée. He was an infantryman with a local Marine Reserve unit who was honorably discharged in 2014 after serving two tours of duty in Iraq. His fiancé has told him he has "not been the same" since his second tour of duty and it is impacting ...
Monson, C. M. & Shnaider, P. (2014). Treating PTSD with cognitive-behavioral therapies: Interventions that work. Washington, DC: American Psychological Association. Updated July 31, 2017. Date created: 2017. This case example explains how Jill's therapist used a cognitive intervention with a written worksheet as a starting point for engaging in ...
The first case example about Terry documents the treatment of PTSD using Prolonged Exposure. The second is an example of in-session imaginal exposure with a different client. Prolonged Exposure is strongly recommended by the APA Clinical Practice Guideline for the Treatment of PTSD. Download case study (PDF, 107KB).
Two Stories of PTSD. Maria was only 15 when she was attacked by a group of men on the way home from school. They took turns screaming abuse at her and then they each raped her. Finally, they tried ...
Literature regarding post-traumatic stress disorder (PTSD) related to the Covid-19 pandemic is accruing rapidly, but this diagnosis is not plausible in this case, given that the DSM-5 criteria for ...
Case formulation - (Persistent PTSD, adapted from Ehlers and Clark []).Case formulation following the persistent PTSD model of Ehlers and Clark [].It is suggested that the patient is processing the traumatic information in a way which a sense of immediate threat is perpetuated through negative appraisals of trauma or its consequences and through the nature of the traumatic experience itself.
David M. Lawson. This article presents an overview of complex trauma and a case study describing the evidence-informed treatment of a 25-year-old woman with chronic complex trauma symptoms resulting from childhood sexual, physical, and psychological abuse from a caregiver. Treatment followed a relationship-based, cognitive behavior therapy ...
The Journal of Child and Family Studies states that there have been more mass shootings within the last 18 years than in the entire 20th century combined, with 77% carried out by adolescents. This case study aims to evaluate the clinical presentation of post-traumatic stress disorder (PTSD) in an adolescent by highlighting the clinical course of a school shooting survivor.
To illustrate IPT for PTSD, we present data from a pilot case that was not included in the current NIMH study, but served as a valuable training case. This patient received open IPT treatment for PTSD because his Clinician-Administered PTSD Scale (CAPS, Blake et al., 1995 ) score of 45, while indicating moderate symptom severity ( Weathers et ...
Background. Research has demonstrated that Cognitive Therapy for PTSD (CT-PTSD), a version of trauma-focused cognitive-behavioural therapy developed by Ehlers and Clark's group (2000), is effective and feasible when offered in weekly and intensive daily formats. It is unknown whether patients with post-traumatic stress disorder (PTSD) could engage in and benefit from self-study assisted ...
Starting treatment for PTSD can be daunting, but we've gathered case studies about people who've been through treatment to help you understand the process more. At first, CBT (cognitive behavioural therapy) treatment for PTSD can be tricky to understand and so some people are scared to try it, or simply don't believe it can effectively ...
This case study follows a 7-year-old boy who presented with symptoms of posttraumatic stress disorder (PTSD) following exposure to domestic violence beginning at a very young age.
EMDR Case Studies. Starting treatment for PTSD can be daunting, but we're gathering case studies about people who've been through treatment to help you understand the process more. At first, EMDR treatment for PTSD can be tricky to understand and so some people are scared to try it, or simply don't believe it can effectively treat PTSD ...
Example for Jane: 12 weeks; can be adjusted if needed. Aftercare Plans. Aftercare plans should be included in a treatment plan as a safety measure in case she ends her therapeutic alliance by terminating, for any reason. Aftercare plans can be updated during treatment plan review, to reflect progress and changes in symptoms. Example for Jane:
Robert Baral*COUNSELING*case study-Post Traumatic Stress Disorder*3/14/2004 AD**p 3 I. PRESENTATION OF THE PATIENT We are presented with a 40 plus year old male presently seeking therapy complaining of anxiety with his home and work lives, which was initiated by his spouse. The patient is a Vietnam War veteran.
Instead of feeling shame and guilt, he said, "I can carry the memory with pride.". Case presentation written by Drs. E.C. Hurley, Louise Maxfield, and Roger M. Solomon. This is a case example for the treatment of PTSD using Eye Movement Desensitization and Reprocessing (EMDR) therapy.
Violence-related post-traumatic stress disorder (PTSD) in the context of war and terrorism has become an increasingly pressing public health issue relevant to refugee children and families. PTSD and related psychopathology in children can adversely affect all domains of development and, in particular, interfere with learning and socialization.
Hi everyone. My name is Abby, and we're going to go through a case study for PTSD together, also known as post-traumatic stress disorder. In this scenario, Mr. Bryant is a 32-year-old male. He presents to the ED after being brought in by law enforcement for possible drug and alcohol intoxication, as well as for displaying erratic and aggressive ...
Case Study PTSD #2: Car Accident. Ella is in her thirties, ambitious and active in life. On a wintry evening, while driving back home from work, she lost control of her car while negotiating a bend in the road. The car spun and came to a halt after it crashed into a tree. She was taken to the hospital, unconscious, with fractured ribs, a torn ...
Case Study: Mauricio. As a teenager, Mauricio had always tried to live up to every standard (academic, religious, familial) that was placed upon him. Before every exam, he lined up his pencils, erasers, and notebooks exactly the same way, each two fingers apart. He felt a strong urge to complete this task because if he didn't, he would fail ...
To illustrate IPT for PTSD, we present data from a pilot case that was not included in the current NIMH study, but served as a valuable training case. This patient received open IPT treatment for PTSD because his Clinician-Administered PTSD Scale (CAPS, Blake et al., 1995 ) score of 45, while indicating moderate symptom severity ( Weathers et ...
It will have been a long break, but we had a bloke who injured his back, he was off for a year and came back good as new. Mine's not that different really. Just happens to be my head instead of my back. Flashbacks and an increasingly short temper made 20-year infantry veteran Mick think he might have an issue with posttraumatic stress.
Case Study #7: Veteran with PTSD. Presenter: Kate Placzek, PhD. Dr. Placzek reviews "Jack," who is a 48-year-old veteran suffering from PTSD. Jack is struggling with depression and sleep problems. He has many severe symptoms. Related Resources. Case Study #1: Pre-Menopausal Female. Case Study #2: "Burned Out" Male.
Children and adolescents, after natural and man-made disasters, often exhibit various psychological, emotional, and behavioral issues, showing a range of clinical symptoms related to post-traumatic stress disorder (PTSD) and depression. This review used a network meta-analysis (NMA) approach to compare and rank psychological interventions for PTSD and depression in children and adolescents ...
CASE STUDY. "Tom" is a 23-year-old, single, white male who present- ed for treatment approximately 1 year after a traumatic event that occurred during his military service in Iraq. Tom received CPT while on active duty in the Army. Background. Tom was born the third of four children to his parents. He described his father as an alcoholic ...
This study examined whether childhood trauma and complex post-traumatic stress disorder (PTSD) symptoms would be negatively associated with leadership competence. A convenience sample of N = 411 Hong Kong adults (Age: M = 38.6, SD = 12.9) completed self-report measures of the studied variables in an online survey.
A second example is the U.S. Department of Veterans Affairs' National Center for PTSD, which seeks to improve clinical care for military veterans through interdisciplinary research on stress ...
Unexpectedly, the solubility of CeO 2 nanoparticles (NPs) at 25 °C does not depend on particle size, but is significantly affected by the sample's thermal pre-treatment. The classical interpretation of NPs' solubility proposed by the Gibbs-Thompson or Kelvin equations fails to describe the experimental data on CeO 2 solubility obtained in this study.
After President Joe Biden's disastrous performance at the June 27, 2024, debate, many Democrats have raced to ring the alarm bell, proclaiming that it's time for him to step aside, time to let ...