Essay on Health Education for Students and Children
500 words essay on health education.
We all know that health education has become very important nowadays. It refers to a career where people are taught about healthcare . Professionals teach people how to maintain and restore their health. In other words, health does not merely refer to physical but also mental, social and sexual health. Health education aims to enhance health literacy and develop skills in people which will help them maintain good health.


Importance of Health Education
Health education is very essential for enhancing the condition of the overall health of different communities and people. It will also help in improving the health of the whole nation. You can also say that the economy of a country is directly proportional to health education. In other words, it means that the higher the life expectancy the better will be the standard of living.
Health education is given to people by professionals in the field known as health educators. They are qualified and certified enough to talk about these issues. Furthermore, they undergo training related to health and hygiene for educating people.
Similarly, health education is very important as it improves the health conditions of the people. It does so by teaching them ways on how to remain healthy and prevent diseases. Moreover, it also makes them responsible enough as a whole community.
The developing nations especially are in dire need of health education. It not only conveys basic knowledge about health but also shapes their habits and way of living. Most importantly, it not only focuses on physical health but also addresses other issues like mental illnesses, sexual well-being and more.
Methods to Improve Health Education
Although health education is very important, we often see how it is not given the importance it deserves. The poor condition of the prevalent health education in many countries is proof of this statement. We need to improve the state of public health education in the world, especially in developing countries.
As the developing countries have many remote areas, the necessary help does not reach there. We must emphasis more on conveying this education to such people. The villagers especially must be made aware of health education and what role it plays in our lives. We can organize these programs which will attract more audience like fares or markets, which already has a gathering.
Moreover, as most of the audience will be illiterate we can make use of visuals like plays, folk shows and more to convey the message in a clear manner. Subsequently, we must also make the most of the opportunity we get at hospitals. The patients coming in to get checked must be made conscious of their health conditions and also be properly educated on these matters.
Similarly, we must target schools and inculcate healthy habits amongst children from an early age. This way, students can spread this knowledge better to their homes and amongst their friends. Therefore, we must enhance the state of health education in the world to help people become healthier and maintain their vitality and dynamism.
FAQs on Health Education
Q.1 Why is Health Education important?
A.1 Health education is very important as it improves the health standards of the country. It further helps in preventing diseases and making people more aware of their health conditions. Most importantly, it not only focuses on physical health but also mental health and others.
Q.2 How can we improve health education?
A.2 We can improve health education by making the people of remote areas more aware. One can organize programs, camps, plays, folk shows and more plus teach it properly at schools too.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Education Improves Public Health and Promotes Health Equity
Robert a hahn, benedict i truman.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: Robert A. Hahn, Centers for Disease Control and Prevention, 1600 Clifton Road NE, MS E-69, Atlanta, GA 30333, USA. [email protected]
Issue date 2015.
Reprints and permissions: sagepub.com/journalsPermissions.nav
This article describes a framework and empirical evidence to support the argument that educational programs and policies are crucial public health interventions. Concepts of education and health are developed and linked, and we review a wide range of empirical studies to clarify pathways of linkage and explore implications. Basic educational expertise and skills, including fundamental knowledge, reasoning ability, emotional self-regulation, and interactional abilities, are critical components of health. Moreover, education is a fundamental social determinant of health – an upstream cause of health. Programs that close gaps in educational outcomes between low-income or racial and ethnic minority populations and higher-income or majority populations are needed to promote health equity. Public health policy makers, health practitioners and educators, and departments of health and education can collaborate to implement educational programs and policies for which systematic evidence indicates clear public health benefits.
Keywords: equity, disparities, social determinant, health in all policies
Education is a process and a product . From a societal perspective, the process of education (from the Latin, ducere, “to lead,” and e, “out from,” yield education, “a leading out”) intentionally engages the receptive capacities of children and others to imbue them with knowledge, skills of reasoning, values, socio-emotional awareness and control, and social interaction, so they can grow as engaged, productive, creative, and self-governing members of a society. 1 Of course, not all educational institutions achieve these goals for all children – far from it; educational institutions in the United States often fall short of goals, and too many students may be led into school failure, social dysfunction, and marginal living conditions with lifelong disadvantages.
Not all learning is acquired in a formal school setting. The process of education occurs at home, in school, and in the child’s community. Children in the United States spend a relatively small proportion of their waking hours in school – approximately 1,000 hours per year or about one fifth of their waking hours. 2 Thus there are many opportunities for informal education outside the school setting. 3 When researchers find evidence linking mental capacities, knowledge, feelings, and values with health outcomes, 4 not all consequences can be attributed to formal education.
As the product of the educational process, an education is the array of knowledge, skills, and capacities (ie, intellectual, socio-emotional, physical, productive, and interactive) acquired by a learner through formal and experiential learning. An education is an attribute of a person. And, although a person may be said to “have” a certain level of education at any particular moment, educational attainment is a dynamic, ever-evolving array of knowledge, skills, and capacities.
Although we conceive of education broadly, including both its formal and informal sources, the focus of our evidence review is the formal education that is measured in most research. Our recommendation also focuses on the formal education, from early childhood to college and beyond, that is, the subject of educational policy and, we argue, should also be the subject of public health policy.
In public health, researchers and practitioners have examined 3 principal relationships between education and health. First, health is a prerequisite for education : hungry children or children who cannot hear well, or who have chronic toothaches, eg, are hindered in their learning. 5 Second, education about health (ie, health education) occurs within schools and in many public health interventions; it is a central tool of public health. 6 Third, physical education in schools combines education about the importance of physical activity for health with promoting such activity. 7 Here we focus on 2 additional relationships between education and health. First, we propose that education as a personal attribute is a central conceptual component and essential element of health , similar to physical fitness. Second, we summarize the extensive literature demonstrating that formal education is a contributing cause of health .
We argue that education – the product and personal attribute acquired – is both a critical component of a person’s health and a contributing cause of other elements of the person’s concurrent and future health. Consistent with other definitions of health, a person who lacks basic elements of an education is not fully healthy. 8 , 9 For example, the 1978 Alma Ata International Conference on Primary Health Care defined “health” to include “a state of complete…mental and social well-being” – which we see as largely products of education. Attainment of a certain level of formal education by young adulthood affects lifelong health through multiple pathways. 8 , 10
We then argue that, because it is both an essential component and a major contributing cause of health, educational achievement broadly should be a legitimate arena for public health intervention. Thus, public health practitioners could legitimately promote educational programs to advance public health. Education should also be recognized as an essential requirement for the disruption of the cycle of poverty and inequities in health. The public health community should expand research to better understand the causal relationships between education and health, and thereby identify evidence-based educational policies that have great potential to improve public health.
A Broad Concept of Education
We propose a broad concept of education as a personal attribute, which includes not only subject-matter knowledge, reasoning, and problem-solving skills, but also awareness of one’s own emotions and those of others and control of one’s emotions (ie, “emotional intelligence”) 11 and associated abilities to interact effectively. “Education improves health because it increases effective agency, enhancing a sense of personal control that encourages and enables a healthy lifestyle. Education’s beneficial effects are pervasive, cumulative, and self-amplifying, growing across the life course.” 12
In 1983, the National Commission on Excellence in Education’s report, A Nation at Risk , launched a national conversation about the need for educational reform. 13 In 1990, the US Department of Labor initiated a program – the Secretary’s Commission on Achieving Necessary Skills – to determine critical capacities for a US workforce to be provided by the educational system. 14 The capacities proposed were based on “a three-part foundation” reflecting the broad notion of education that we propose: Basic Skills (reading, writing, arithmetic, mathematics, listening, speaking), Thinking Skills (creative thinking, decision making, problem solving, seeing things in the mind’s eye, knowing how to learn, reasoning), and Personal Qualities (responsibility, self-esteem, sociability, self-management, integrity/honesty). The project recommends as a central educational goal: “All American high school students must develop a new set of competencies and foundation skills if they are to enjoy a productive, full, and satisfying life.” 14 (p1) We would expand this list of outcomes to include a healthy life.
Education as an Element of Health
In our conception, basic education is an integral part of being healthy. A person is unhealthy if he or she lacks basic knowledge, the ability to reason, emotional capacities of self-awareness and emotional regulation, and skills of social interaction. These embodied personal attributes or mental capacities, the products of formal education as well as other learning experiences, are conceptually comparable to physical capacities of fitness and coordination – well-established components of health. “Education teaches a person to use his or her mind: Learning, thinking, reasoning, solving problems, and so on are mental exercises that may keep the central nervous system in shape the same way that physical exercise keeps the body in shape.” 8 (p738) A person is unhealthy who cannot conduct himself or herself effectively and achieve some level of “social well-being” – a critical element of the World Health Organization (WHO) conception of health, which recognized the contributions of social sectors beyond the health sector in promoting health. 9
The projects of several US and international health agencies reflect this concept of education as a component of health. For example, the US Centers for Disease Control and Prevention recognizes “cognitive health” in its Healthy Aging Program; although the focus of this program is prevention and control of Alzheimer’s disease, the “cognitive health” rubric suggests far broader considerations: “The public health community should embrace cognitive health as a priority, invest in its promotion, and enhance our ability to move scientific discoveries rapidly into public health practice.” 15 (p1) The National Institutes for Health similarly has a “healthy brain” program that recognizes cognitive as well as emotional capacities as elements of health. 16
Similar concepts are recognized internationally by the WHO, in accordance with its definition of health cited above. More recently, a WHO paper 17 included cognition and affect as 2 of 6 domains for the international comparison of health status .
Measures of Education as a Personal Attribute
Education is measured in a variety of ways. A common measure, years of schooling/educational attainment, is problematic insofar as time spent in school gives little indication of how the time is spent and what is learned. 2 School-level completion may be a better measure, but also varies in terms of the quality and quantity of what is learned. Standardized tests of subject-matter knowledge and reasoning skills may be still better for some purposes, but may offer challenges when compared across populations. 18
Some 19 , 20 have argued that teacher-assigned grades are an alternate, if not better, predictor of long-term outcomes than standardized tests because they reflect not only academic achievement, but also classroom social and learning skills that indicate abilities to learn and to interact successfully. The breadth of skills addressed by this measure better reflects the broad concept of education argued here. Subjectivity, personal preferences, and comparability are challenges with teacher-assigned grades as a measure of achievement.
Evidence of Causal Association
It may seem odd that, in the perspective developed here, education – the product and the personal attribute – is at once an element of health and a cause of health. The relationship is similar to that of physical fitness and health. Fitness is an element of health and an important cause of subsequent health – not only of physical fitness, but of other facets of health as well, including cardiac health and mental health. 21 – 23 In addition to providing extensive evidence that education is associated with health, we argue that the underlying causal process is conceptually similar to the causal relationships between physical activity or an infectious agent and health. We provide some evidence of causation, noting that the notion of causal proof in a traditional deterministic sense has been challenged. 24
Criteria to determine causality in public health developed by Sir Bradford-Hill in 1965 25 are still useful. They are:
Strength of association linking hypothetical cause and outcome (as assessed, eg, by the magnitude of relative risks)
Consistency of findings, eg, by different researchers in different settings
Specificity – the connection of specific, narrow causes to specific outcomes
Temporal sequence—the necessity of cause preceding consequence
Dose–response relationship
Plausibility in terms of current knowledge
Coherence – similar to plausibility, the fit with other contemporary knowledge
Experiment – offering the strongest support
Analogy – the comparability of postulated causality with causality in similar phenomena
Most of the Bradford-Hill criteria clearly apply when linking education to health. An obvious exception is specificity, because education itself is a broad concept including many elements, and the causal consequences of education are also numerous and heterogeneous. Bradford-Hill did not regard specificity as essential, as in the case of cigarette smoke with its multiple health consequences. As Susser has argued, “Specificity enhances the plausibility of causal inference, but lack of specificity does not negate it.” 26 (p153)
The associations presented below satisfy several standard criteria for causation. At least 3 approaches are used: 1) observational cohort studies with concurrent controls, 2) natural quasi-experiments in education policy, and 3) educational experiments. In the sections that follow, we provide samples of evidence of the causal association between education and health, assessed first by various health-related outcomes: health risk and protective behaviors, wages and income (resources for health), self-assessed health, morbidity, mortality, and life expectancy. We then provide evidence from experimental studies. The literature on these topics is extensive 4 , 8 and here we describe only a few examples, from early childhood and beyond. Evidence of the association between measures of education – the personal attribute – and other health-related outcomes is positive, strong, and consistent.
Health Risk and Protective Behaviors Are Associated With Academic Achievement
Evidence of an association between high school student grades and risk behaviors in the United States is remarkably consistent; higher average grade achievement is associated with lower rates of risk behavior ( Figure 1 ). 27 One plausible explanation is that there is causation in the reverse direction of what is proposed here, ie, that risk behavior interferes with academic achievement; such reverse causation seems reasonable, eg, for watching television and using alcohol. Also plausible is that other factors, such as strong values, promote both academic achievement and self-protective behaviors, or that academic achievement is associated with knowledge, which leads to risk avoidance. Another explanation is that underlying psychological or environmental conditions are associated with risk behavior and academic problems. Causation in both directions is likely. The consistency of a dose response for multiple behaviors is consistent with an effect of educational success on the avoidance of risky behavior.
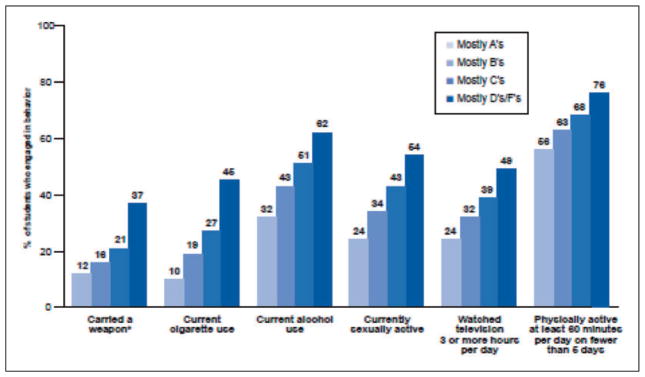
Health-risk behaviors and school grades, United States, 2009.
Source: www.cdc.gov/healthyyouth/health_and_academics/pdf/health_risk_behaviors.pdf .
There is also strong evidence of a dose response between years of education and many health-related risk and protective behaviors among US adults. Analysis of a representative survey of adults aged >25 years between 1990 and 2000 indicates that the prevalence of several risk behaviors is generally higher among those with fewer than nine years of formal education, begins to decline among those who have nine to 12 years of formal education, and continues to decline with additional years of education; this finding corresponds to the recognized importance of high school completion for subsequent health. 28 , 29
Wages and Income, Resources for Health, Are Associated With Educational Success
Wages and income are not health outcomes, but are closely linked with health outcomes because they provide access to health-related resources, such as healthy food, a safe environment, and healthcare. A recent analysis 30 of trends in US wages over more than 20 years finds higher wages consistently associated with higher educational attainment and a trend toward increasing differences in wages by educational status. In the causal chain, high educational attainment is antecedent to high wages or income. A recent study 31 linking individual kindergarten standardized achievement tests with wages at ages 25–27 years indicates a remarkable linear association accounting for 17% of the variability in the wage outcome – 20 years later ( Figure 2 ). Although high family income precedes and predicts educational success in children, controlling for such demographic characteristics of the kindergartner (including family income, household ownership, and marital status) diminishes, but by no means eliminates, the association found in this study.
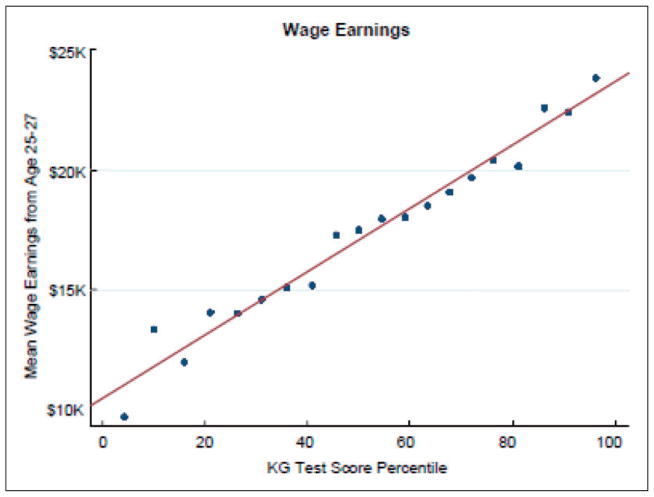
Association between kindergarten test score percentiles and mean wage earnings, ages 25–27 years, Tennessee STAR program.
Source: Chetty, 2010.
Self-Assessed Health Is Associated With Educational Attainment
Self-assessed health is a well-established index of morbidity and predictor of mortality. 32 , 33 A recent study compares the association of educational attainment with self-assessed health in US and Canadian populations. 34 , 35 Controlling for basic demographics and income, those with less than a high school education in the United States are 2.4 times as likely as high school graduates and 4.1 times as likely as those with post-secondary education to rate their health as poor. Further adjusting these ratios for risk behaviors only moderately reduces the ratios, suggesting that education is related to self-reported health due to important factors in addition to risk behaviors.
It is plausible that health status affects the likelihood of educational achievement, but it is likely that the major force of causation is in the opposite direction. Not only is educational attainment closely associated with self-rated health, but the association increases with age when measured by the number of days per week reported as free of major symptoms. With increasing age, the gap in symptom-free days increases between those with a college degree, those with a high school degree or some college, and those with less than a high school degree, suggesting that the effects of education are pervasive throughout the lifespan, and that its consequences have cumulative effects on health over time. 36
Morbidity is Associated With Educational Attainment
In the United States, although higher self-reported rates of several conditions, such as prostate cancer and sinusitis, are reported among more adults with greater levels of education, for most conditions the reverse direction of association is evident. Rates of major circulatory diseases, diabetes, liver disease, and several psychological symptoms (sadness, hopelessness, and worthlessness) show higher rates among adults with lower educational attainment. 35
Mortality and Life Expectancy Are Associated With Educational Attainment
Evidence also exists of a strong association between educational attainment and mortality from many diseases. 37 The parallel relationship for three heterogeneous groups of illness or injury again suggests an underlying connection unrelated to the specific etiologic pathways of each cause of death ( Figure 3 ). 37 In addition, the modal age for completing formal education (the mid-20 s) substantially precedes the peak age for mortality in the United States (77 years of age) by many years, consistent with another Bradford-Hill principle, ie, the precedence of cause before effect.
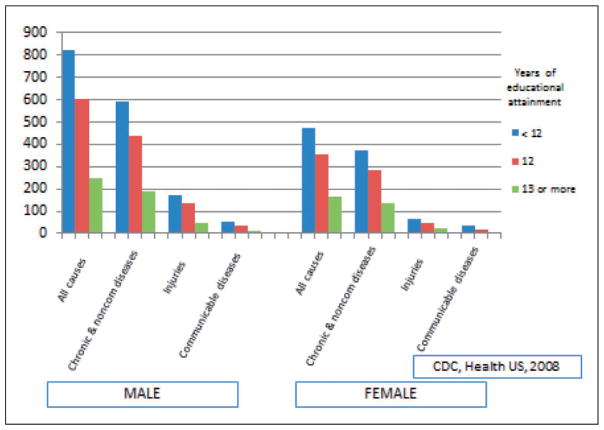
Age-adjusted death rates among persons ages 25–64 years for several condition groupings, by sex and educational attainment. Selected US states, 1994–2005.
From the perspective of life expectancy, at age 25 in 2005, a man in the United States with less than a high school education could expect to live an additional 44.2 years to age 69.2 years; a man with a graduate degree could expect to live more than 15 years longer. At age 25 years, a woman in the United States with less than a high school education could expect to live to age 74.9 years; a woman with a graduate degree could expect to live more than 11 years longer. 38
Educational Experiments and Quasi-Experiments
True experiments in the field of education are uncommon. Nevertheless, several experiments have been conducted. Groups of children, often from low-income or minority families, have been exposed, sometimes with random assignment, to different forms of education and followed over time to determine long-term outcomes, including health-related outcomes, as shown in the following 3 examples of early childhood programs.
In the early 1960s, 3- and 4-year-olds with low IQs from low-income families were randomly assigned to either the High/Scope Perry Preschool Program – an educational program including home visits – or no intervention. Home visits were designed to strengthen parental engagement in the child’s education. Participants were periodically assessed until age 40. 39 Over several follow-up assessments, intervention participants had greater levels of educational attainment, income, and health insurance, lived in safer family environments, and had lower rates of tobacco and drug use and risky driving behavior than controls. At age 40 years, however, more intervention than control participants had chronic diseases, but fewer intervention participants had died.
In 1972, healthy infants at risk of academic difficulties because of their demographic circumstances (eg, poor, minority, single parents) were randomly assigned to the Carolina Abecedarian Project or a control intervention (offered social services, nutritional supplements, and healthcare services, but no educational program). 40 The Abecedarian preschool program focused on developing cognitive, social, language, and motor skills from birth through age 5 years. Before entering kindergarten, control and experimental children were again randomized into either routine schooling or a strengthened school program complemented by home visits for parental guidance to reinforce child learning. At follow-up, both the preschool and the early schooling programs were shown to be beneficial in terms of academic achievement; the preschool program had the larger effect. By age 21 years, participants in the early childhood education intervention (combining those with and without the strengthened primary school programming) had better health behaviors and better health than those who did not receive the early childhood education intervention. 41 By their mid-30 s, those exposed to the intervention, particularly males, had substantially more favorable cardiovascular risk profiles than those exposed to the control condition. 42
Finally, though not a true experiment, the Chicago Child-Parent Center program followed two groups of poor Chicago children aged 3 and 4 years: one exposed to an early childhood program and the other not exposed. Children residing in Chicago districts with federally funded kindergarten programs were eligible and selected on a “most-in-need basis”; comparison children lived in similarly poor neighborhoods with locally funded kindergarten programs. The Chicago Child-Parent Center provided educational enrichment from prekindergarten through the third grade, required parental involvement in the classroom a half-day per week, and provided nutrition and health services. At age 24 years, in comparison with control subjects, participants had lower rates of out-of-home placement (indicating child abuse), lower rates of arrests and conviction for violent behaviors, and lower rates of disability. 43
A recent review of the effects of early childhood educational programs indicates that programs with strong instructional components and those evaluated with strong study designs have large and enduring effects on the educational, social, and health outcomes of participants. 44
Several researchers have made use of natural quasi-experiments involving education policies that rapidly change years of schooling required, to evaluate the effects of the requirement on health-related and other outcomes. When state educational requirements change from 1 year to the next from 7 to 9 years, eg, cohorts of children of a certain age in that state will receive approximately 7 years of education, while their younger siblings will receive 9 years. The state where this policy is implemented may be compared by regression discontinuity analysis from before to after the change, but also with other states that have not made this change at the same time.
In one such study, Lleras-Muney 45 uses a sample of US census data to estimate the effects on mortality of changes in compulsory education requirements in 30 states, comparing birth cohorts before and after such changes between 1915 and 1939 with long-term follow-up data. Lleras-Muney concludes that each year of additional required schooling resulted in a reduction of mortality by 3.6% over 10 years, or gain of 1.7 years to life expectancy at 35 years of age. Although these data are old, it is likely that the general effects of increased educational requirements on mortality have not changed substantially. Other researchers have used regression discontinuity analysis to estimate the effects of education on rates of crime, arrest, and incarceration in the United States 46 and on teenage births in the United States and Norway. 47 Among researchers using this design, only Arendt 48 finds equivocal evidence regarding the effects of additional years of education on self-rated health, body mass index, and smoking in the United States, Canada, and Denmark. The heterogeneity of conditions affected by educational exposure again suggests a broad, nonspecific underlying “mechanism.”
The Fallacy of the Endowment Hypothesis
Gottfredson has proposed that intelligence – innate intellectual and associated ability – rather than educational attainment is the “fundamental cause” of socioeconomic inequalities in health, a proposal referred to as the “endowment hypothesis.” 49 Several basic features distinguish Gottfredson’s notion of intelligence from the concept of education as defined in this article: intelligence is regarded as “natural, not cultural,” “context-free,” and “highly heritable” – indicating a largely innate, biological foundation, little affected by environmental variability. From this vantage, education as conceived in this article may be regarded as largely determined by intelligence insofar as those with greater intelligence are both more likely to seek education and to succeed in acquiring it.
Gottfredson’s hypothesis is explicitly evaluated by others in a study of 2 US cohorts that assesses the contributions of education, income, and intelligence to 3 health outcomes: mortality, life-threatening illness, and self-rated health. 50 The researchers posit an alternative model, in which there are underlying “background influences on [socioeconomic status] and intelligence.” In this model, intelligence affects education and income, and both of these socioeconomic status characteristics in turn affect intelligence; a summary of research on this linkage 51 indicates that a year of education is associated with a gain of between 2 and 4 IQ points. In both study cohorts, intelligence during high school is measured by standardized and validated tests, the Henmon-Nelson test and the Wechsler Adult Intelligence Scale. The researchers find generally consistent evidence of pairwise dose–response associations between levels of education, income, and intelligence with each of 3 health outcomes.
The researchers then examine the questions: what is the effect of controlling the association of education and health outcomes for intelligence; of income and health outcomes controlling for intelligence; and of intelligence and health outcomes controlling for both education and income? This assessment allows answering 2 basic questions: how much does intelligence contribute to the effects of education and of income on health, ie, what are the effects of these determinants net the contribution of intelligence? And, to what extent are the effects of intelligence on health mediated by income and education? The researchers find that separately controlling the effects of education and income on health outcomes for intelligence alters the coefficients for education and income minimally and leaves all associations statistically significant at the 0.05 level or less, indicating that little of the effect of education on health is mediated by intelligence.
The effects of controlling the effects of intelligence on health for education and income are more complex. Only 1 of the 2 surveys finds a significant effect of intelligence on mortality ( P <.05); controlling for education and income eliminates the significance of this finding. Thus, the effect of intelligence on mortality is largely mediated by income and education. Both surveys find statistically significant effects of intelligence for both life-threatening illnesses and self-rated health; however, the effect magnitudes are diminished by a mean of 69.4% and statistical significance is again eliminated for all findings except for self-rated health in one of the surveys. These findings indicate that the effects of intelligence on health outcomes are largely mediated by education and income. 50 There is thus substantial evidence that education has a strong effect on health, independent of background intelligence. Innate intelligence may be a “fundamental cause” principally insofar as it leads to higher education and income.
Causal Pathways and Evidence Linking Education and Health
Building on the work of others, 10 , 52 we constructed a model indicating the three major pathways linking education and health outcomes in adulthood and including the several facets of education – knowledge, problem solving, emotional awareness and self-regulation, values, and interactional skills ( Figure 4 ). First is the psycho-social environment, including the individual’s sense of control, social standing, and social support, which reflects and bolsters capacity and agency. Second is work, through which the individual may achieve satisfaction and income, which allows access to many health-related resources. Finally, healthy behavior may protect an individual against health risks and facilitate negotiation of the healthcare system.
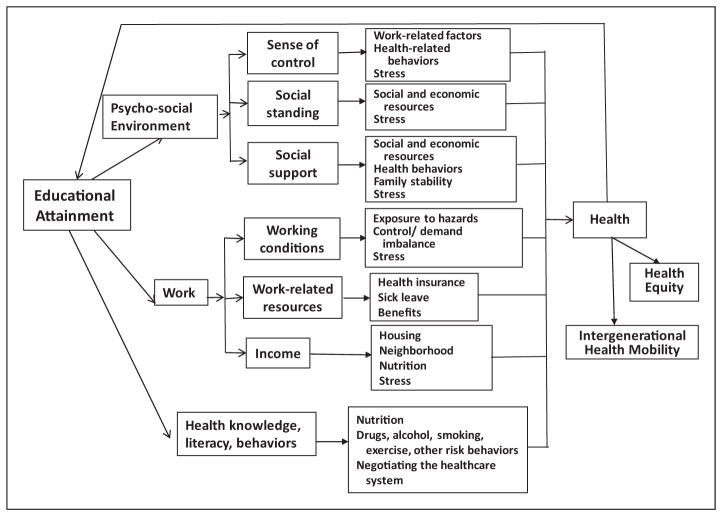
Pathways from educational attainment to health outcomes.
Ross and Wu 8 used 2 national probability samples of US adults to assess the effects of completed education on self-perceived health and reported physical functioning. They first assessed the association between education and each of three broad covariate groups – psycho-social environment; work; and health knowledge, literacy, and behaviors – that are themselves determinants of health outcomes ( Figure 4 ). 8 For each data source, they began with a model including as covariates only demographic characteristics of their samples. To the basic model, they first added employment and economic covariates, then social-psychological covariates, and finally risk behavior covariates, noting the changes in regression coefficients for educational exposures on health outcomes. This approach allowed assessment of the magnitude of each of these groups of covariates as pathways linking education to health-related outcomes. However, the relative contribution of each group of factors cannot be determined precisely, because these groups are unlikely to be causally independent, and covariate groups entered into the regression early are thus likely to show greater reductions in regression coefficients than those entered later.
In both samples, education was associated with all covariates in expected directions. The largest effect was for work-related variables, including income. Those with lower income not only had limited resources useful in maintaining health, but also may have experienced anxieties that exacerbate health problems. The effects of psycho-social resources were also statistically significant and of similar magnitude. Risk behavior and knowledge also contributed to the association between education and health by both measures. The 3 clusters of covariates together explain between 55% and 59% of the variance in self-reported health and between 46% and 71% of physical functioning in these surveys. This suggests that the smallest contribution to health outcomes is associated with health behaviors, which were entered last into the regression model. In both samples, education has a significant residual “direct” effect, independent of the three examined pathways. In summary, education’s association with improved health is attributable to greater work opportunities and rewards, a greater sense of control and social support, healthier behaviors, and a direct effect on health. Similar results are found by Cutler and Lleras-Muney, 28 who use different sources to assess associations between educational attainment, health behaviors, and mortality in the United States and Great Britain.
In a separate study, Ross and Mirowsky 53 provide evidence that the effect of higher levels of education on health is mediated principally by its contents, including values and skills imparted, and far less by means of status markers such as the diploma or the prestige of the degree-granting institution. Evidence for this conclusion derives from a regression analysis of national data including measures of years of education, receipt of diplomas, and school selectivity (based on test scores of entering freshmen). In another study, Reynolds and Ross 54 provide evidence that “the direct effect of education on well-being is greater than the direct effect of social origins, and the total effect of social origins is mediated mostly by education.” 54 (p226) Evidence derives from a regression analysis of two national data sources in which the researchers control for parental education, father’s occupation, and childhood poverty. They also find that a person’s level of education has a far greater effect on health if his or her parents were poorly educated than if they were well-educated. Unfortunately, in our society, parental and child educational levels are highly positively correlated, so that the children of parents with little education, who might benefit the most from higher levels of education, are least likely to receive that education. 55
Ross and Mirowsky 55 (pp597,598) conclude (emphasis added): “…certain policy implications follow. First, education policy is health policy. Second, health policy must address the educational opportunities of children raised by poorly-educated parents. Otherwise those children, in adulthood, will suffer the multiplicative health consequences of low parental education and low personal education…Structural amplification condemns some families to the concentration of low education with poor health across generations… Break that mediating link, and the moderating effect of higher education will suppress the health disadvantages of the socially disadvantaged origins. ”
High Societal Price in Health of Education Forgone
An estimate of the number of annual deaths attributable to lack of high school education among persons 25–64 years of age in the United States (237,410) exceeds the number of deaths attributed to cigarette smoking among persons 35–64 years of age (163,500) (Krueger et al., unpublished manuscript, 2013). 56 (The estimate of smoking-attributable mortality does not include adults younger than 35 years of age because mortality from smoking is negligible at this age.)
Several recent estimates have been made of economic costs to individuals, the government, and society of the failure of each American to achieve an optimal education. Although it may be argued that there is a moral duty to redress injustice and inequity regardless of cost, these estimates indicate the economic magnitude of this loss and the potential value of its redress.
Schoeni and colleagues 57 , 58 estimate the annual economic value of health forgone in the United States in 2006 by adults who lack a college education. For a population of 138 million aged 25 years or older with less than a college education, the economic value of the life and health forgone is US$1.02 trillion per year – 7.7% of US gross domestic product.
Levin and colleagues 59 provide an estimate of benefits to the government (in 2004 dollars) if those who did not finish high school had completed a high school education (or higher) with a diploma. Based on governmental benefits of income taxes associated with greater earnings of high school graduates and reduced costs of welfare and incarceration, Medicaid, and lifetime savings of approximately US$40,000 per capita in public health expenses, they estimated a total lifetime benefit of US$209,000 for each high school dropout if he or she had instead completed high school. They then examined the costs and benefits of 5 programs with demonstrated efficacy in improving rates of high school completion. Cost–benefit ratios range from 1.5 to 3.5, indicating substantial governmental benefit. 59
Education as a Domain of Public Health Action
Just as many areas of daily life are recognized domains of legitimate public health action – agriculture (eg, nutrition and food safety), transportation (eg, vehicle injuries, air pollution, and walking), immigration (eg, immigrant health and infection control), justice (eg, violent crime and prison health), urban design (eg, safety, walkable communities, and food deserts), and labor (eg, occupational safety and health) – so should education (beyond health education in schools) be recognized as a legitimate domain of public health action. Education is a critical component of health and, we argue, education is a major, long-term, multifaceted cause of health. In particular, education is a powerful means of breaking the cycle of poverty (which greatly affects ethnic and racial minority populations) and promoting health equity.(As this article was in press, the authors encountered an excellent paper by Cohen and Syme 60 which draws similar conclusions.)
Several federal agencies have supported “health in all policies,” 61 particularly through the National Prevention, Health Promotion and Public Health Council. 62 The US Department of Health and Human Services includes in its mission 63 to “engage multiple sectors to take actions to strengthen policies and improve practices that are driven by the best available evidence and knowledge” and in its overarching goals to “Create social and physical environments that promote good health for all.”
States and the District of Columbia have also adopted a “health in all policies” perspective. California’s “CAL Health in all Policies” 64 – 66 recognizes the potential for education as a means of moving toward health equity. “Promote efforts that demonstrate positive effects in closing the achievement gap. Collaborate on advancing strategies, addressing the major factors that inhibit the learning of all students.” Counties (eg, Los Angeles, Baltimore) also have adopted a “health in all policies” perspective. 64 , 67 , 68
The effort to pursue multi-sectoral strategies for health improvement is international, practiced in the European Union, Australia, and elsewhere. The European Union has adopted a social determinants-based approach: “Health in All Policies addresses the effects on health across all policies such as agriculture, education, the environment, fiscal policies, housing, and transport. It seeks to improve health and at the same time contribute to the well-being and the wealth of the nations through structures, mechanisms, and actions planned and managed mainly by sectors other than health.” 69 (pXVIII)
In “A Framework for Public Health Action: The Health Impact Pyramid,” 71 Frieden writes, “Interventions that address social determinants of health have the greatest potential public health benefit” and contrasts social determinants – the base of the “health impact pyramid” – with higher strata in the pyramid. 70 (p594) Among social determinants, education is fundamental, because education forms the new members of society – children and youth. Effective teachers are facilitators of long-term health benefits. Beyond school health promotion, education as a means of public health intervention is more difficult to define, to administer, to measure, and to evaluate. It is cumulative, formative, and transformative, both for the individuals who experience it and for the society it recreates and modifies. Although these features make education more challenging than some other tools of public health, such challenges must not deter the public health community from working closely with the education community to investigate and understand this form of social determinant causation, evaluate the wide array of educational program types, and mobilize for action on this powerful force for public health benefits.
Acknowledgments
Many thanks to thoughtful readers and editors Randy Elder, Catherine Ross, Barbara Rimer, Kate W. Harris, Amy Brown, Heba Athar, and Kristen Folsom.
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Biographies
Robert A. Hahn received his PhD in anthropology at Harvard University (1976) and his MPH in epidemiology from the University of Washington (1986). Since 1986, he has served as an epidemiologist at the US Centers for Disease Control and Prevention (CDC) in Atlanta and is a member of the Senior Biomedical Research Service. He is the author of Sickness and Healing: An Anthropological Perspective (1995) and co-editor of Anthropology and Public Health: Bridging Differences in Culture and Society (2008), with a second edition recently published. In 1998–1999, he worked as a Capitol Hill Fellow in the US House of Representatives Committee on Veterans Affairs and in the office of Congresswoman Louise Slaughter. He is currently coordinating scientist of systematic reviews on health equity for the CDC Guide to Community Preventive Services .
Benedict I. Truman earned his BS in chemistry and MD from Howard University and his MPH from the Johns Hopkins Bloomberg School of Public Health, where he completed a residency in preventive medicine and public health and served as chief resident. He has held scientific and leadership positions in state, local, and federal public health agencies and is the associate director for science at the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention at the US Centers for Disease Control and Prevention (CDC). In this role, he works with other scientists and program managers to ensure that the CDC’s scientific products and research ethics meet the highest standards of quality and integrity. He has published many peer-reviewed journal articles on educational interventions for health equity; prevention and control of infectious diseases and chronic noninfectious diseases; adolescent and school health; community preventive services guidelines; minority health and health disparities; employee performance and public health workforce development; and applied epidemiologic methods. He serves as the Consulting Editor for Infectious Diseases for the Journal of Public Health Management and Practice .
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
- 1. Dewey J. Democracy and Education: An Introduction to the Philosophy of Education. New York, NY: MacMillan Co; 1916. [ Google Scholar ]
- 2. Silva E. [Accessed May 9, 2014];On the clock: rethinking the way schools use time. 2007 http://www.educationsector.org/publications/clock-rethinking-way-schools-use-time .
- 3. Bandura A. Social Learning Theory. New York, NY: General Learning Press; 1977. [ Google Scholar ]
- 4. Feinstein L, Sabates R, Anderson TM, Sorhaindo A, Hammond C. What are the Effects of Education on Health?. Copenhagen, Denmark. Measuring the Effects of Education on Health and Civic Engagement: Proceedings of the Copenhagen Symposium, OECD; 2006. [ Google Scholar ]
- 5. Basch CE. Healthier Students Are Better Learners: A Missing Link in School Reforms to Close the Achievement Gap. Equity Matters. 2010 doi: 10.1111/j.1746-1561.2011.00632.x. Research Review No. 6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Peters LW, Kok G, Ten Dam GT, Buijs GJ, Paulussen TG. Effective elements of school health promotion across behavioral domains: a systematic review of reviews. BMC Public Health. 2009;9:182–195. doi: 10.1186/1471-2458-9-182. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 7. Rasberry C, Lee SM, Robin L, et al. The association between school-based physical activity, including physical education, and academic performance: a systematic review of the literature. Prev Med. 2011;52(Suppl 1):S10–S20. doi: 10.1016/j.ypmed.2011.01.027. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Ross CE, Wu CL. The links between education and health. Am Soc Rev. 1995;60(5):719–745. [ Google Scholar ]
- 9. World Health Organization. [Accessed May 9, 2014];Declaration of Alma-Ata. 1978 http://www.who.int/publications/almaata_declaration_en.pdf?ua=1 .
- 10. Egerter S, Braveman P, Sadegh-Nobari T, Grossman-Kahn R, Dekker M. Education matters for health. Educ Health. 2009;6:1–15. [ Google Scholar ]
- 11. Bradberry T, Greaves J. Emotional Intelligence 2.0. San Diego, CA: Talent Smart; 2009. [ Google Scholar ]
- 12. Mirowsky J, Ross CE. Education, learned effectiveness and health. London Rev Educ. 2005;3:205–220. [ Google Scholar ]
- 13. National Commission on Excellence in Education. A Nation at Risk. Washington DC: U.S. Government Printing Office; 1983. [ Google Scholar ]
- 14. Secretary’s Commission on Achieving Necessary Skills. A SCANS report for America. 2000. Learning a living: a blueprint for high performance. [ Google Scholar ]
- 15. CDC Healthy Aging Program. [Accessed May 9, 2014];The CDC Healthy Brain Initiative: Progress 2006–2011. 2011 http://www.cdc.gov/aging/healthybrain .
- 16. National Institutes of Health. [Accessed May 5, 2014];Healthy Brain Initiative. http://trans.nih.gov/cehp/
- 17. Sadana R, Tandon A, Murray CLJ, et al. Describing population health in six domains: comparable results from 66 household surveys. Global Programme on Evidence for Health Policy. Discussion Paper No. 43. Geneva, Switzerland: WHO; 2002. [ Google Scholar ]
- 18. U.S. Congress, Office of Technology Assessment. Testing in American Schools: Asking the Right Questions, OTA-SET-519. Washington DC: U.S. Government Printing Office; 1992. [ Google Scholar ]
- 19. Bowers A. Reconsidering grades as data for decision making: more than just academic knowledge. J Educ Admin. 2009;47:609–629. [ Google Scholar ]
- 20. Willingham W, Pollack JM, Lewis C. Grades and test scores: accounting for observed differences. J Educ Meas. 2002;39:1–37. [ Google Scholar ]
- 21. Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report. Washington, DC: U.S. Department of Health and Human Services; 2008. [ Google Scholar ]
- 22. Powell KE, Spain KG, Christenson GM, Mollenkamp MP. The status of the 1990 objectives for physical fitness and exercise. Public Health Rep. 1986;101(1):15–21. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. U.S. Department of Health and Human Services. Physical Activity and Health: a Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [ Google Scholar ]
- 24. Karhausen LR. Causation: the elusive grail of epidemiology. Med, Health Care Philos. 2000;3:59–67. doi: 10.1023/a:1009970730507. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Bradford-Hill A. The environment and disease: association or causation? Proc Royal Soc Med. 1965;58:295–300. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Susser M. Causal Thinking in the Health Sciences. Concepts and Strategies of Epidemiology. New York, NY: Oxford University Press; 1973. [ Google Scholar ]
- 27. CDC Division of Adolescent and School Health. [Accessed May 5, 2014];Health-risk behaviors and academic achievement. 2009 http://www.cdc.gov/healthyyouth/health_and_academics/pdf/health_risk_behaviors.pdf .
- 28. Cutler DM, Lleras-Muney A. Understanding differences in health behaviors by education. J Health Econ. 2010;29:1–28. doi: 10.1016/j.jhealeco.2009.10.003. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. Winkelby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–820. doi: 10.2105/ajph.82.6.816. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 30. Murnane RJ. Improving the education of children living in poverty. Future Child. 2007;17:161–182. doi: 10.1353/foc.2007.0019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Chetty R, Friedman JN, Hilger N, et al. How does your kindergarten classroom affect your earnings? Evidence from Project Star. Q J Econ. 2011;126(4):1593–1660. doi: 10.1093/qje/qjr041. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Ferraro KF, Farmer MM. Utility of health data from social surveys: is there a gold standard for measuring morbidity? Am Sociol Rev. 1999;64(2):303–315. [ Google Scholar ]
- 33. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty seven studies community. J Health Soc Behav. 1997;38:21–37. [ PubMed ] [ Google Scholar ]
- 34. Prus SG. Comparing social determinants of self-rated health across the United States and Canada. Soc Sci Med. 2011;73:50–59. doi: 10.1016/j.socscimed.2011.04.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Schiller JS, Lucas JW, Ward BW, Peregoy JA National Center for Health Statistics. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat. 2012;10(252):1–207. [ PubMed ] [ Google Scholar ]
- 36. Ross CE, Wu CL. Education, age and the cumulative advantage in health. J Health Soc Behav. 1996;37:104–120. [ PubMed ] [ Google Scholar ]
- 37. CDC National Center for Health Statistics. Health, United States, 2008. Hyattsville, MD: National Center for Health Statistics; 2009. [ Google Scholar ]
- 38. Rostron BL, Boies JL, Arias E National Center for Health Statistics. Education reporting and classification on death certificates in the United States. Vital Health Stat. 2010;2(151):1–19. [ PubMed ] [ Google Scholar ]
- 39. Muennig P, Schweinhart L, Montie J, Neidell M. Effects of a prekindergarten educational intervention on adult health: 37-year follow-up results of a randomized controlled trial. Am J Public Health. 2008;99(8):1431–1437. doi: 10.2105/AJPH.2008.148353. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 40. Ramey C, Campbell FA, Burchinal M, et al. Persistent effects of early childhood education on high-risk children and their mothers. Appl Dev Sci. 2000;4:2–14. [ Google Scholar ]
- 41. Muennig P, Robertson D, Johnson G, et al. The effect of an early education program on adult health: the Carolina Abecedarian project randomized controlled trial. Am J Public Health. 2011;101:512–516. doi: 10.2105/AJPH.2010.200063. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 42. Campbell F, Conti G, Heckman JJ, et al. Early childhood investments substantially boost adult health. Science. 2014;343(6178):1478–1485. doi: 10.1126/science.1248429. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Reynolds AJ, Temple JA, Ou SR, et al. Effects of a school-based, early childhood intervention on adult health and well-being: a 19-year follow-up of low-income families. Arch Pediatr Adolesc Med. 2007;161:730–739. doi: 10.1001/archpedi.161.8.730. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Barnett WS. Effectiveness of early educational intervention. Science. 2011;333:975–978. doi: 10.1126/science.1204534. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. Lleras-Muney A. The relationship between education and adult mortality in the United States. Rev Econ Stud. 2005;72:189–221. [ Google Scholar ]
- 46. Lochner L, Moretti R. The effect of education on crime: evidence from prison inmates, arrests, and self-reports. Am Econ Rev. 2004;94:155–189. [ Google Scholar ]
- 47. Black SE, Devereux PJ, Salvanes KG. Fast times at Ridgemont High? The effect of compulsory schooling laws on teenage births. [Accessed May 9, 2014];NBER Working Paper Series: Working Paper 10911. 2004 http://www.nber.org/papers/w10911 .
- 48. Arendt JN. Does education cause better health? A panel data analysis using school reforms for identification. Econ Educ Rev. 2005;24:149–160. [ Google Scholar ]
- 49. Gottfredson LS. Intelligence: is it the epidemiologists’ elusive fundamental cause of social class inequalities in health? J Pers Soc Psychol. 2004;86(1):174–199. doi: 10.1037/0022-3514.86.1.174. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Link BG, Phelan JC, Miech R, Westin EL. The resources that matter: fundamental social causes of health disparities and the challenge of intelligence. J Health Soc Behav. 2008;49(1):72–91. doi: 10.1177/002214650804900106. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Winship C, Korenman S. Does staying in school make you smarter: the effect of education on IQ in the Bell Curve. In: Devlin B, Fienberg SE, Resnick DP, Roeder K, editors. Intelligence, Genes, and Success. Scientists Respond to The Bell Curve. New York, NY: Springer Verlag; 1997. [ Google Scholar ]
- 52. World Health Organization. Closing the gap in a generation: health equity through action on the social determinants of health. [Accessed May 9, 2014];Final Report of the Commission on Social Determinants of Health. 2008 http://www.who.int/social_determinants/thecommission/finalreport/en/index.html .
- 53. Ross CE, Mirowsky J. Refining the association between education and health: the effects of quantity, credential, and selectivity. Demography. 1999;36:445–460. [ PubMed ] [ Google Scholar ]
- 54. Reynolds JR, Ross CE. Social stratification and health: education’s benefit beyond economic status and social origins. Soc Probl. 1998;45(2):221–247. [ Google Scholar ]
- 55. Ross CE, Mirowsky J. The interaction of personal and parental education on health. Soc Sci Med. 2011;72:591–599. doi: 10.1016/j.socscimed.2010.11.028. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Office of the Surgeon General. The Health Consequences of Smoking—50 years of Progress. A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; 2014. [ Google Scholar ]
- 57. Schoeni R, Dow WF, Miller WD, Pamuk ER. The economic value of improving the health of disadvantaged Americans. Am J Prev Med. 2011;40(1Suppl1):S67–S72. doi: 10.1016/j.amepre.2010.09.032. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Rothwell J. Metropolitan Policy Program: Brookings Institution. 2012. Housing Costs, Zoning, and Access to High-Scoring Schools. [ Google Scholar ]
- 59. Levin H, Belfield C, Muennig P, Rouse C. [Accessed September 5 2014];The Costs and Benefits of an Excellent Education for all of America’s Children. 2006 http://www.irre.org/publications/costs-and-benefits-excellent-education-all-americas-children .
- 60. Cohen AK, Syme SL. Education: a missed opportunity for public health intervention. Am J Public Health. 2013;103(6):997–1001. doi: 10.2105/AJPH.2012.300993. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Healthy People. [Accessed May 9, 2014];Social Determinants of Health. 2020 http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39 .
- 62. National Prevention Health Promotion and Public Health Council. [Accessed May 9, 2014];2010 Annual Status Report. 2010 http://www.hhs.gov/news/reports/nationalprevention2010report.pdf .
- 63. US Department of Health and Human Services. [Accessed May 9, 2014];Healthy People 2020. 2010 http://www.healthypeople.gov/2020/default.aspx .
- 64. Fielding JE. [Accessed May 9, 2014];Health in All Policies: Lessons Learned by LA County DPH. http://publichealth.lacounty.gov/docs/Fielding%20CDC%20L2L%207.8.08%20-%20FINAL.pdf .
- 65. Gase LN, Pennotti R, Smith KD. Health in all policies: taking stock of emerging practices to incorporate health in decision making in the United States. J Public Health Manag Pract. 2013;19(6):529–540. doi: 10.1097/PHH.0b013e3182980c6e. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. National Association of County and City Health Officials. [Accessed May 9, 2014];Health in All Policies. http://www.naccho.org/topics/environmental/HiAP/
- 67. Baltimore City Health Department. [Accessed May 9, 2014];Healthy Baltimore. http://www.baltimorehealth.org/healthybaltimore2015.html .
- 68. Rudolph L, Caplan J, Ben-Moshe K, Dillon L. Health in All Policies: A Guide for State and Local Governments. Washington, DC and Oakland, CA: American Public Health Association and Public Health Institute; 2013. [ Google Scholar ]
- 69. Ståhl T, Wismar M, Ollila E, Lahtinen E, Leppo K, editors. [Accessed May 9, 2014];Health in All Policies Prospects and Potentials. 2006 http://www.euro.who.int/__data/assets/pdf_file/0003/109146/E89260.pdf .
- 70. Frieden TR. A framework for public health action: the health impact pyramid. Am J Public Health. 2010;100:590–595. doi: 10.2105/AJPH.2009.185652. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (532.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

Health and education
Education has the power to transform the lives of children and young people, and the world around them. At UNESCO, inclusive and transformative education starts with healthy, happy and safe learners. Because children and young people who receive a good quality education are more likely to be healthy, and likewise those who are healthy are better able to learn and complete their education.
Guided by the UNESCO Strategy on education for health and well-being , UNESCO works to improve the physical and mental health, well-being and education outcomes of all learners. By reducing health-related barriers to learning, such as gender-based violence, gender inequality, HIV and sexually transmitted infections (STIs), early and unintended pregnancy, bullying and discrimination, and malnutrition, UNESCO, governments and school systems empower learners to understand their rights, learn better and lead fulfilling lives.
What you need to know about education for health and well-being
Helping children learn about health and well-being
For healthy, informed and empowered learners
Supporting comprehensive sexuality education for adolescents and young people in Sub-Saharan Africa
Preventing and addressing violence in and around school
Key figures
is bullied at school every month globally
occur each year among adolescent girls aged 15–19
lack basic drinking water & almost half do not have handwashing facilities
globally – nearly half of all children in primary school – receive school meals
A foundation for life and love campaign
What does comprehensive sexuality education mean to you?
A foundation for life and love

First technical brief in a series of four.

More publications


School Success: An Opportunity for Population Health: Proceedings of a Workshop (2020)
Chapter: 2 the relationship between education and health, 2 the relationship between education and health 1.
To provide a foundation for the discussions, Steven Woolf of Virginia Commonwealth University’s Center on Society and Health gave a brief overview of why educational success matters for health. The discussion that followed was moderated by Joshua Sharfstein, Johns Hopkins Bloomberg School of Public Health. (Highlights of this session are presented in Box 2-1 .)
FACTORS THAT SHAPE HEALTH OUTCOMES
Woolf outlined five domains from the report U.S. Health in International Perspective: Shorter Lives, Poorer Health ( NRC and IOM, 2013 ) that are important to shaping health outcomes. These include health care and public health (which, he noted, account for only 10–20 percent of health outcomes); individual behaviors; the physical and social environment; social and economic factors (including education); and public policies and spending, which shape the other four domains (see Figure 2-1 ). Differences in health outcomes are related to differences in how people and communities experience each of these domains. Key factors impacting health outcomes include
___________________
1 Unless otherwise noted, as in the case of the question and answer/discussion period, this chapter represents the rapporteur’s synopsis of the presentation delivered by Steven Woolf of Virginia Commonwealth University and the statements have not been endorsed or verified by the National Academies of Sciences, Engineering, and Medicine.

- education and income (e.g., families with limited incomes cannot live in healthy neighborhoods);
- quality of housing (e.g., exposure to allergens that cause asthma, overcrowding);
- quality of food that is accessible to residents (convenient availability of fresh, nutritious foods versus unhealthy options);
- the built environment (e.g., opportunities for residents to safely exercise, walk, cycle, or play outside);
- proximity to highways, factories, and other sources of exposure to pollutants and toxic agents;
- access to primary care providers and quality hospitals;
- access to affordable and reliable public transit (for travel to jobs, health and child care, social services, etc.); and
- residential segregation or other features that isolate communities and stifle economic growth.
Education, income, and wealth are among the most powerful predictors of health outcomes, Woolf said.
EDUCATION AS A PREDICTOR OF HEALTH OUTCOMES
In the United States, the risk of dying from any cause (all-cause mortality) is directly related to educational attainment. Woolf described this relationship as a gradient: for both men and women, the more years of education an individual has, the lower the risk of death ( Ross et al., 2012 ). Similarly, people who have less educational attainment more frequently self-report fair or poor health ( Schiller et al., 2012 ). This association (between higher education and better health) is demonstrable across a range of different health outcomes, Woolf said, and he shared prevalence data by education for coronary heart disease, stroke, lung diseases, diabetes, kidney disease, and others ( Schiller et al., 2012 ).
There is a tendency in U.S. society to assume that health is primarily the result of health care, Woolf observed, but he said the assumption is incorrect. Analyzing data from Kaiser Permanente in Northern California, Woolf and colleagues found that the educational attainment–health outcome gradient persists even among patients in this integrated health system, whose members have equivalent access to health care. Factors outside of the health care system contribute to the differences in health outcomes by educational attainment.
Tremendous amounts of money are dedicated to health care in the United States, he said, but the importance of the social determinants of health, including education, is not always fully appreciated. He shared data that suggest that for every life saved by medical advances, seven
lives would be saved if all adults had the mortality rate of people with some college education ( Woolf et al., 2007 ).
Recognizing that patients who have less educational attainment are at greater risk for chronic diseases is important for clinicians, Woolf said, but there are also broader implications of this association for decision makers outside of the health sector, such as employers. A greater percentage of individuals with less educational attainment have difficulties with physical functioning—from walking, climbing steps, or handling small objects to lifting, carrying, or pushing large or heavy objects ( Schiller et al., 2012 ). An educated workforce is more capable of physically functioning in blue-collar jobs. In addition to higher productivity, a more educated employee population will experience lower health care costs, less absenteeism, and more presenteeism. 2
In a knowledge economy, it is difficult to separate the impact of education from that of income and wealth, Woolf said. People who have more education are more likely to obtain high-earning jobs and thus to have higher incomes and greater wealth. As with the education–health gradient, higher levels of income are associated with better health across a wide range of both physical and mental health outcomes ( Schiller et al., 2012 ). Woolf added that people with less educational attainment are more dramatically impacted by societal trends. For example, although life expectancy in industrialized countries has been increasing for the past century, U.S. life expectancy has decreased in recent years, and this trend has been more pronounced among adults who have not graduated from high school ( Olshansky et al., 2012 ). The factors behind this trend are complex. Woolf cited the work of Case and Deaton, who have drawn attention to the problem of “deaths of despair”: death rates from drug overdoses, alcoholism, and suicides have increased significantly since the 1990s. Case and Deaton showed that this increase was concentrated among middle-aged whites, especially among Americans with less educational attainment ( Case and Deaton, 2017 ).
UNDERSTANDING THE RELATIONSHIP BETWEEN EDUCATION AND HEALTH
Education can produce better health through multiple pathways (see Figure 2-2 ). For example, those who have more education have the ability to access more economic resources, such as better-paying jobs with health insurance benefits. Having those resources, in turn, allows them to live in healthier neighborhoods and avoid a range of health hazards, from
2 “Presenteeism” in this sense means the state of being present, as opposed to being present at work but not productive.

crime to air pollution. In what is called reverse causality, health can also influence educational outcomes. For example, proper management of conditions such as attention-deficit/hyperactivity disorder or asthma can improve a child’s academic success.
This education–health relationship is highly influenced by contextual factors, Woolf emphasized. Contextual factors are the conditions throughout a person’s life that can affect both education and health. These contextual factors, including both experiences and place, may often be the root cause of the correlation between education and health. For example, chronic stress and trauma are examples of contextual factors that can affect a child’s health trajectory and success in school. Research has shown that adverse childhood experiences can influence health throughout life, leading to higher risks of depression, substance abuse, and chronic diseases later in life ( Felitti et al., 1998 ). Place—the conditions in communities where people live—can also shape both health outcomes and educational outcomes. For example, life expectancy in Chicago varies as much as 20 years by census tract, with much lower life expectancies in Southside Chicago and similar areas. Maps reveal that the areas that tend to have lower life expectancy are also areas where educational attainment is the lowest.
In closing, Woolf noted that many efforts are under way to draw a connection between the community and a child’s experience in school.

As examples, he mentioned the Whole School, Whole Community, Whole Child model 3 that the Centers for Disease Control and Prevention developed and the Together for Healthy and Successful Schools Initiative being undertaken by Washington University in St. Louis. 4
Strength and Appreciation of the Data
Moderator Sharfstein asked about the extent to which the data on the importance of education for health are appreciated by health care leaders. Woolf responded that there has historically been a lack of awareness in the health care community about the importance of the social determinants of health. In recent years, however, health care systems have become more attentive to these issues, driven in part by health care reform. The Patient Protection and Affordable Care Act and other health reforms that
3 See https://www.cdc.gov/healthyschools/wscc/index.htm (accessed May 30, 2019).
4 See https://cphss.wustl.edu/items/healthy-schools (accessed May 30, 2019).
mandate efforts to improve population health outcomes and lower the use of health care services have emphasized the importance of addressing the social determinants of health. Although health care systems have been focusing on addressing factors such as unstable housing and food security, there is increasing interest in investing in education, including not only education for children but also skills training for adults to compete for better jobs.
The issue of correlation versus causation was raised by a participant relative to the data on the association between education and health. Woolf acknowledged the problem, noting that more prospective studies are needed to demonstrate that improvements in education will improve health outcomes. “Just giving out diplomas doesn’t save lives,” he said. That said, although arguments could be made about the magnitude of the impact, the concept that improving education will improve health outcomes has been well established by numerous examples worldwide. Woolf referred to a National Research Council (NRC) and Institute of Medicine (IOM) study comparing the health of Americans to that of people in other high-income countries ( NRC and IOM, 2013 ). The NRC and IOM committee found that life expectancy and other health outcomes in the United States were inferior to those in other high-income countries, across many different health metrics. A systematic examination of potential causes revealed differences compared to other countries across all five domains that shape health. Among these, education was a key factor: after World War II, Americans were the most educated people in the world, he said, but educational outcomes in the United States have not kept pace with progress in other high-income countries or even in some developing economies, such as South Korea. These countries have outperformed the United States in terms of their ability to educate young people and prepare them for successful careers.
Another key difference is that many other high-income countries invest more (per capita or as a proportion of their total spending) in social services, education, and other factors that improve health. From a policy perspective, Woolf said, the United States needs to shift its priorities as a way not only to improve health outcomes but also to strengthen its economic competitiveness with these other countries. If the U.S. workforce is less healthy than workers in other countries, the nation’s ability to challenge the economic performance of other countries is at risk if those kinds of investments are not made, he said.
Education and Health Inequities
Health inequities are a key health challenge in the United States, Sharfstein noted. He asked about the impact of educational challenges in
producing serious health inequities by race, location, or other key factors. The five domains that shape health outcomes also drive health inequities, Woolf responded. There are other factors that influence health inequities (e.g., the biological effects of experiencing racial discrimination and trauma), but racial and ethnic disparities in health are often mirrored by dramatic differences in educational outcomes, he said. For a variety of reasons (including racism), African Americans have, on average, a lower rate of graduation from high school and less success in obtaining 4-year degrees than white Americans. In marginalized communities, escaping the multigenerational cycle of poverty often depends on the ability of young people to get a good education. Woolf reiterated that education is important in shaping not only health outcomes but economic opportunity and social mobility. Investments are needed to address the gaps in education that often exist to a greater degree in marginalized populations, both to improve health outcomes and to end the negative economic cycle that has historically trapped these communities in a state of persistent disadvantage.
Higher Education
Sanne Magnan of the HealthPartners Research Institute asked whether young people are still being encouraged to pursue higher education the way they were after World War II and whether, given the expense of a college education, there should be more investment in craft, trade, and vocational education. Woolf agreed that a strong interest in higher education was evident after World War II, as exemplified by the GI Bill. He felt that although today’s world places a fair amount of pressure on high school students to perform well and try to get into the best schools, there are barriers to accessing a college education that prior generations did not face. He agreed that a 4-year degree was not the only way to break the cycle of poverty, adding that there is a great market demand for people who are trained in the trades and an underinvestment in vocational schools and community colleges.
Sally Kraft from Dartmouth-Hitchcock inquired about the existence of any research on whether innovative ways of delivering education at lower cost (e.g., open online courses) have the same impact on increasing educational attainment and the associated health and income outcomes. Woolf replied that although the question was a good one, he was not familiar with research on that topic.
Education and health care significantly influence well-being and health outcomes, especially throughout adolescence. In fact, doctors note that performance in school is highly reflective of a child's current and future health. Despite knowledge of this connection, pediatricians are rarely aware of their patients' school performance and have a limited understanding of the education system. Fostering collaboration and aligning efforts within the health and education sectors is a critical step towards building stronger and healthier communities.
On June 14, 2018, the National Academies convened a workshop to discuss how efforts within the health sector can support children's education from pre-kindergarten through 12th grade and to explore the barriers between these sectors. The committee also examined case examples of health-education collaboration and opportunities in policy. This publication summarizes the presentations and discussions from the workshop.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
- Open access
- Published: 06 April 2020
The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015
- Viju Raghupathi 1 &
- Wullianallur Raghupathi 2
Archives of Public Health volume 78 , Article number: 20 ( 2020 ) Cite this article
240k Accesses
185 Altmetric
Metrics details
A clear understanding of the macro-level contexts in which education impacts health is integral to improving national health administration and policy. In this research, we use a visual analytic approach to explore the association between education and health over a 20-year period for countries around the world.
Using empirical data from the OECD and the World Bank for 26 OECD countries for the years 1995–2015, we identify patterns/associations between education and health indicators. By incorporating pre- and post-educational attainment indicators, we highlight the dual role of education as both a driver of opportunity as well as of inequality.
Adults with higher educational attainment have better health and lifespans compared to their less-educated peers. We highlight that tertiary education, particularly, is critical in influencing infant mortality, life expectancy, child vaccination, and enrollment rates. In addition, an economy needs to consider potential years of life lost (premature mortality) as a measure of health quality.
Conclusions
We bring to light the health disparities across countries and suggest implications for governments to target educational interventions that can reduce inequalities and improve health. Our country-level findings on NEET (Not in Employment, Education or Training) rates offer implications for economies to address a broad array of vulnerabilities ranging from unemployment, school life expectancy, and labor market discouragement. The health effects of education are at the grass roots-creating better overall self-awareness on personal health and making healthcare more accessible.
Peer Review reports
Introduction
Is education generally associated with good health? There is a growing body of research that has been exploring the influence of education on health. Even in highly developed countries like the United States, it has been observed that adults with lower educational attainment suffer from poor health when compared to other populations [ 36 ]. This pattern is attributed to the large health inequalities brought about by education. A clear understanding of the health benefits of education can therefore serve as the key to reducing health disparities and improving the well-being of future populations. Despite the growing attention, research in the education–health area does not offer definitive answers to some critical questions. Part of the reason is the fact that the two phenomena are interlinked through life spans within and across generations of populations [ 36 ], thereby involving a larger social context within which the association is embedded. To some extent, research has also not considered the variances in the education–health relationship through the course of life or across birth cohorts [ 20 ], or if there is causality in the same. There is therefore a growing need for new directions in education–health research.
The avenues through which education affects health are complex and interwoven. For one, at the very outset, the distribution and content of education changes over time [ 20 ]. Second, the relationship between the mediators and health may change over time, as healthcare becomes more expensive and/or industries become either more, or less hazardous. Third, some research has documented that even relative changes in socioeconomic status (SES) can affect health, and thus changes in the distribution of education implies potential changes in the relationship between education and health. The relative index of inequality summarizes the magnitude of SES as a source of inequalities in health [ 11 , 21 , 27 , 29 ]. Fourth, changes in the distribution of health and mortality imply that the paths to poor health may have changed, thereby affecting the association with education.
Research has proposed that the relationship between education and health is attributable to three general classes of mediators: economic; social, psychological, and interpersonal; and behavioral health [ 31 ]. Economic variables such as income and occupation mediate the relationship between education and health by controlling and determining access to acute and preventive medical care [ 1 , 2 , 19 ]. Social, psychological, and interpersonal resources allow people with different levels of education to access coping resources and strategies [ 10 , 34 ], social support [ 5 , 22 ], and problem-solving and cognitive abilities to handle ill-health consequences such as stress [ 16 ]. Healthy behaviors enable educated individuals to recognize symptoms of ill health in a timely manner and seek appropriate medical help [ 14 , 35 ].
While the positive association between education and health has been established, the explanations for this association are not [ 31 ]. People who are well educated experience better health as reflected in the high levels of self-reported health and low levels of morbidity, mortality, and disability. By extension, low educational attainment is associated with self-reported poor health, shorter life expectancy, and shorter survival when sick. Prior research has suggested that the association between education and health is a complicated one, with a range of potential indicators that include (but are not limited to) interrelationships between demographic and family background indicators [ 8 ] - effects of poor health in childhood, greater resources associated with higher levels of education, appreciation of good health behaviors, and access to social networks. Some evidence suggests that education is strongly linked to health determinants such as preventative care [ 9 ]. Education helps promote and sustain healthy lifestyles and positive choices, nurture relationships, and enhance personal, family, and community well-being. However, there are some adverse effects of education too [ 9 ]. Education may result in increased attention to preventive care, which, though beneficial in the long term, raises healthcare costs in the short term. Some studies have found a positive association between education and some forms of illicit drug and alcohol use. Finally, although education is said to be effective for depression, it has been found to have much less substantial impact in general happiness or well-being [ 9 ].
On a universal scale, it has been accepted that several social factors outside the realm of healthcare influence the health outcomes [ 37 ]. The differences in morbidity, mortality and risk factors in research, conducted within and between countries, are impacted by the characteristics of the physical and social environment, and the structural policies that shape them [ 37 ]. Among the developed countries, the United States reflects huge disparities in educational status over the last few decades [ 15 , 24 ]. Life expectancy, while increasing for all others, has decreased among white Americans without a high school diploma - particularly women [ 25 , 26 , 32 ]. The sources of inequality in educational opportunities for American youth include the neighborhood they live in, the color of their skin, the schools they attend, and the financial resources of their families. In addition, the adverse trends in mortality and morbidity brought on by opioids resulting in suicides and overdoses (referred to as deaths of despair) exacerbated the disparities [ 21 ]. Collectively, these trends have brought about large economic and social inequalities in society such that the people with more education are likely to have more health literacy, live longer, experience better health outcomes, practice health promoting behaviors, and obtain timely health checkups [ 21 , 17 ].
Education enables people to develop a broad range of skills and traits (including cognitive and problem-solving abilities, learned effectiveness, and personal control) that predispose them towards improved health outcomes [ 23 ], ultimately contributing to human capital. Over the years, education has paved the way for a country’s financial security, stable employment, and social success [ 3 ]. Countries that adopt policies for the improvement of education also reap the benefits of healthy behavior such as reducing the population rates of smoking and obesity. Reducing health disparities and improving citizen health can be accomplished only through a thorough understanding of the health benefits conferred by education.
There is an iterative relationship between education and health. While poor education is associated with poor health due to income, resources, healthy behaviors, healthy neighborhood, and other socioeconomic factors, poor health, in turn, is associated with educational setbacks and interference with schooling through difficulties with learning disabilities, absenteeism, or cognitive disorders [ 30 ]. Education is therefore considered an important social determinant of health. The influence of national education on health works through a variety of mechanisms. Generally, education shows a relationship with self-rated health, and thus those with the highest education may have the best health [ 30 ]. Also, health-risk behaviors seem to be reduced by higher expenditure into the publicly funded education system [ 18 ], and those with good education are likely to have better knowledge of diseases [ 33 ]. In general, the education–health gradients for individuals have been growing over time [ 38 ].
To inform future education and health policies effectively, one needs to observe and analyze the opportunities that education generates during the early life span of individuals. This necessitates the adoption of some fundamental premises in research. Research must go beyond pure educational attainment and consider the associated effects preceding and succeeding such attainment. Research should consider the variations brought about by the education–health association across place and time, including the drivers that influence such variations [ 36 ].
In the current research, we analyze the association between education and health indicators for various countries using empirical data from reliable sources such as the Organization for Economic Cooperation and Development (OECD) and World Bank. While many studies explore the relationship between education and health at a conceptual level, we deploy an empirical approach in investigating the patterns and relationships between the two sets of indicators. In addition, for the educational indicators, we not only incorporate the level of educational attainment, but also look at the potential socioeconomic benefits, such as enrollment rates (in each sector of educational level) and school life expectancy (at each educational level). We investigate the influences of educational indicators on national health indicators of infant mortality, child vaccinations, life expectancy at birth, premature mortality arising from lack of educational attainment, employment and training, and the level of national health expenditure. Our research question is:
What are some key influencers/drivers in the education-health relationship at a country level?
The current study is important because policy makers have an increasing concern on national health issues and on policies that support it. The effect of education is at the root level—creating better overall self-awareness on personal health and making healthcare more accessible. The paper is organized as follows: Section 2 discusses the background for the research. Section 3 discusses the research method; Section 4 offers the analysis and results; Section 5 provides a synthesis of the results and offers an integrated discussion; Section 6 contains the scope and limitations of the research; Section 7 offers conclusions with implications and directions for future research.
Research has traditionally drawn from three broad theoretical perspectives in conceptualizing the relationship between education and health. The majority of research over the past two decades has been grounded in the Fundamental Cause Theory (FCT) [ 28 ], which posits that factors such as education are fundamental social causes of health inequalities because they determine access to resources (such as income, safe neighborhoods, or healthier lifestyles) that can assist in protecting or enhancing health [ 36 ]. Some of the key social resources that contribute to socioeconomic status include education (knowledge), money, power, prestige, and social connections. As some of these undergo change, they will be associated with differentials in the health status of the population [ 12 ].
Education has also been conceptualized using the Human Capital Theory (HCT) that views it as a return on investment in the form of increased productivity [ 4 ]. Education improves knowledge, skills, reasoning, effectiveness, and a broad range of other abilities that can be applied to improving health. The third approach - the signaling or credentialing perspective [ 6 ] - is adopted to address the large discontinuities in health at 12 and 16 years of schooling, which are typically associated with the receipt of a high school diploma and a college degree, respectively. This perspective considers the earned credentials of a person as a potential source that warrants social and economic returns. All these theoretical perspectives postulate a strong association between education and health and identify mechanisms through which education influences health. While the HCT proposes the mechanisms as embodied skills and abilities, FCT emphasizes the dynamism and flexibility of mechanisms, and the credentialing perspective proposes educational attainment through social responses. It needs to be stated, however, that all these approaches focus on education solely in terms of attainment, without emphasizing other institutional factors such as quality or type of education that may independently influence health. Additionally, while these approaches highlight the individual factors (individual attainment, attainment effects, and mechanisms), they do not give much emphasis to the social context in which education and health processes are embedded.
In the current research while we acknowledge the tenets of these theoretical perspectives, we incorporate the social mechanisms in education such as level of education, skills and abilities brought about by enrollment, school life expectancy, and the potential loss brought about by premature mortality. In this manner, we highlight the relevance of the social context in which the education and health domains are situated. We also study the dynamism of the mechanisms over countries and over time and incorporate the influences that precede and succeed educational attainment.
We analyze country level education and health data from the OECD and World Bank for a period of 21 years (1995–2015). Our variables include the education indicators of adult education level; enrollment rates at various educational levels; NEET (Not in Employment, Education or Training) rates; school life expectancy; and the health indicators of infant mortality, child vaccination rates, deaths from cancer, life expectancy at birth, potential years of life lost and smoking rates (Table 1 ). The data was processed using the tools of Tableau for visualization, and SAS for correlation and descriptive statistics. Approaches for analysis include ranking, association, and data visualization of the health and education data.
Analyses and results
In this section we identify and analyze patterns and associations between education and health indicators and discuss the results. Since countries vary in population sizes and other criteria, we use the estimated averages in all our analyses.

Comparison of health outcomes for countries by GDP per capita
We first analyzed to see if our data reflected the expectation that countries with higher GDP per capita have better health status (Fig. 1 ). We compared the average life expectancy at birth, average infant mortality, average deaths from cancer and average potential year of life lost, for different levels of GDP per capita (Fig. 1 ).
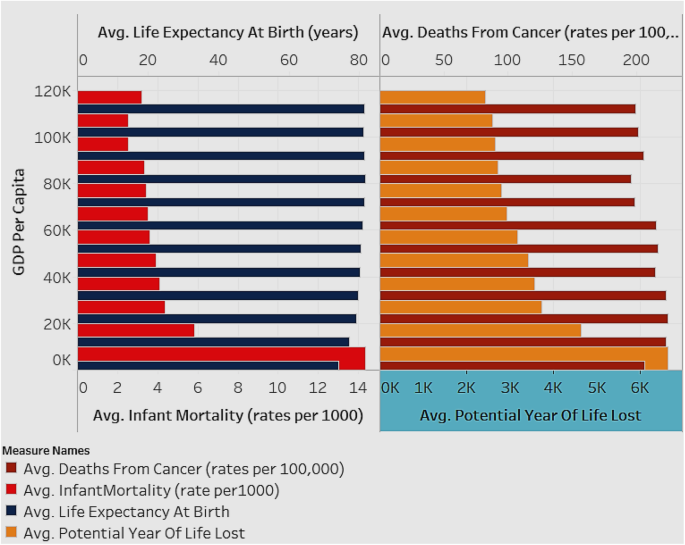
Associations between Average Life Expectancy (years) and Average Infant Mortality rate (per 1000), and between Deaths from Cancer (rates per 100,000) and Average Potential Years of Life Lost (years), by GDP per capita (for all countries for years 1995–2015)
Figure 1 depicts two charts with the estimated averages of variables for all countries in the sample. The X-axis of the first chart depicts average infant mortality rate (per 1000), while that of the second chart depicts average potential years of life lost (years). The Y-axis for both charts depicts the GDP per capita shown in intervals of 10 K ranging from 0 K–110 K (US Dollars). The analysis is shown as an average for all the countries in the sample and for all the years (1995–2015). As seen in Fig. 1 , countries with lower GDP per capita have higher infant mortality rate and increased potential year of life lost (which represents the average years a person would have lived if he or she had not died prematurely - a measure of premature mortality). Life expectancy and deaths from cancer are not affected by GDP level. When studying infant mortality and potential year lost, in order to avoid the influence of a control variable, it was necessary to group the samples by their GDP per capita level.
Association of Infant Mortality Rates with enrollment rates and education levels
We explored the association of infant mortality rates with the enrollment rates and adult educational levels for all countries (Fig. 2 ). The expectation is that with higher education and employment the infant mortality rate decreases.
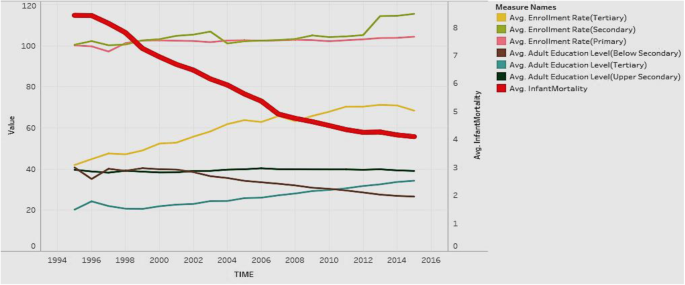
Association of Adult Education Levels (ratio) and Enrollment Rates (ratio) with Infant Mortality Rate (per 1000)
Figure 2 depicts the analysis for all countries in the sample. The figure shows the years from 1995 to 2015 on the X axis. It shows two Y-axes with one axis denoting average infant mortality rate (per 1000 live births), and the other showing the rates from 0 to 120 to depict enrollment rates (primary/secondary/tertiary) and education levels (below secondary/upper secondary/tertiary). Regarding the Y axis showing rates over 100, it is worth noting that the enrollment rates denote a ratio of the total enrollment (regardless of age) at a level of education to the official population of the age group in that education level. Therefore, it is possible for the number of children enrolled at a level to exceed the official population of students in the age group for that level (due to repetition or late entry). This can lead to ratios over 100%. The figure shows that in general, all education indicators tend to rise over time, except for adult education level below secondary, which decreases over time. Infant mortality shows a steep decreasing trend over time, which is favorable. In general, countries have increasing health status and education over time, along with decreasing infant mortality rates. This suggests a negative association of education and enrollment rates with mortality rates.
Association of Education Outcomes with life expectancy at birth
We explored if the education outcomes of adult education level (tertiary), school life expectancy (tertiary), and NEET (not in employment, education, or training) rates, affected life expectancy at birth (Fig. 3 ). Our expectation is that adult education and school life expectancy, particularly tertiary, have a positive influence, while NEET has an adverse influence, on life expectancy at birth.
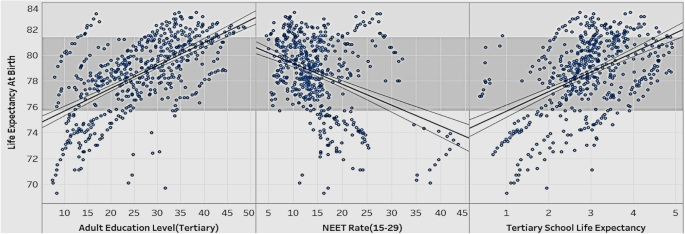
Association of Adult Education Level (Tertiary), NEET rate, School Life Expectancy (Tertiary), with Life Expectancy at Birth
Figure 3 show the relationships between various education indicators (adult education level-tertiary, NEET rate, school life expectancy-tertiary) and life expectancy at birth for all countries in the sample. The figure suggests that life expectancy at birth rises as adult education level (tertiary) and tertiary school life expectancy go up. Life expectancy at birth drops as the NEET rate goes up. In order to extend people’s life expectancy, governments should try to improve tertiary education, and control the number of youths dropping out of school and ending up unemployed (the NEET rate).
Association of Tertiary Enrollment and Education with potential years of life lost
We wanted to explore if the potential years of life lost rates are affected by tertiary enrollment rates and tertiary adult education levels (Fig. 4 ).
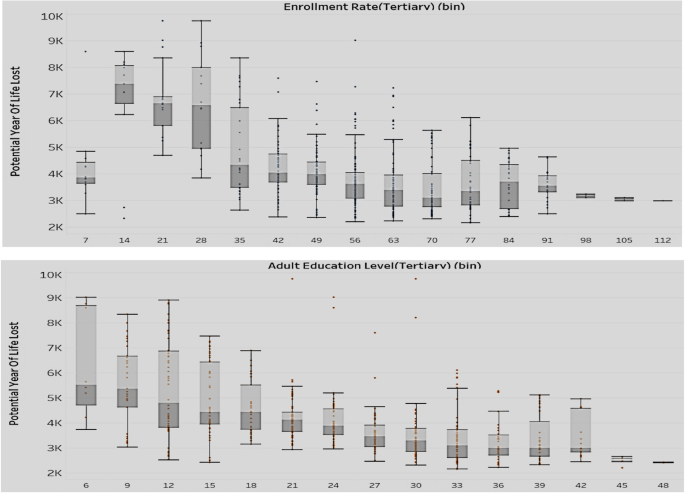
Association of Enrollment rate-tertiary (top) and Adult Education Level-Tertiary (bottom) with Potential Years of Life Lost (Y axis)
The two sets of box plots in Fig. 4 compare the enrollment rates with potential years of life lost (above set) and the education level with potential years of life lost (below set). The analysis is for all countries in the sample. As mentioned earlier, the enrollment rates are expressed as ratios and can exceed 100% if the number of children enrolled at a level (regardless of age) exceed the official population of students in the age group for that level. Potential years of life lost represents the average years a person would have lived, had he/she not died prematurely. The results show that with the rise of tertiary adult education level and tertiary enrollment rate, there is a decrease in both value and variation of the potential years of life lost. We can conclude that lower levels in tertiary education adversely affect a country’s health situation in terms of premature mortality.
Association of Tertiary Enrollment and Education with child vaccination rates
We compared the performance of tertiary education level and enrollment rates with the child vaccination rates (Fig. 5 ) to assess if there was a positive impact of education on preventive healthcare.
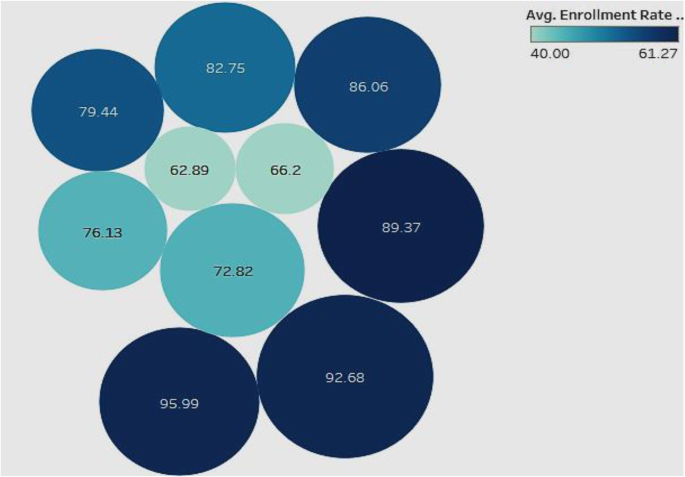
Association of Adult Education Level-Tertiary and Enrollment Rate-Tertiary with Child Vaccination Rates
In this analysis (Fig. 5 ), we looked for associations of child vaccination rates with tertiary enrollment and tertiary education. The analysis is for all countries in the sample. The color of the bubble represents the tertiary enrollment rate such that the darker the color, the higher the enrollment rate, and the size of the bubble represents the level of tertiary education. The labels inside the bubbles denote the child vaccination rates. The figure shows a general positive association of high child vaccination rate with tertiary enrollment and tertiary education levels. This indicates that countries that have high child vaccination rates tend to be better at tertiary enrollment and have more adults educated in tertiary institutions. Therefore, countries that focus more on tertiary education and enrollment may confer more health awareness in the population, which can be reflected in improved child vaccination rates.
Association of NEET rates (15–19; 20–24) with infant mortality rates and deaths from Cancer
In the realm of child health, we also looked at the infant mortality rates. We explored if infant mortality rates are associated with the NEET rates in different age groups (Fig. 6 ).
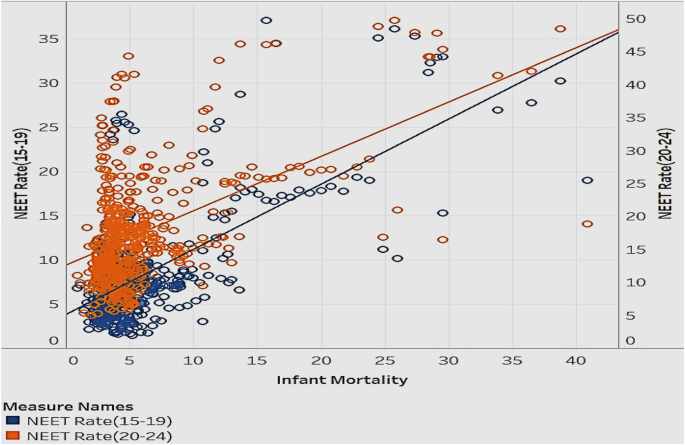
Association of Infant Mortality rates with NEET Rates (15–19) and NEET Rates (20–24)
Figure 6 is a scatterplot that explores the correlation between infant mortality and NEET rates in the age groups 15–19 and 20–24. The data is for all countries in the sample. Most data points are clustered in the lower infant mortality and lower NEET rate range. Infant mortality and NEET rates move in the same direction—as infant mortality increases/decrease, the NEET rate goes up/down. The NEET rate for the age group 20–24 has a slightly higher infant mortality rate than the NEET rate for the age group 15–19. This implies that when people in the age group 20–24 are uneducated or unemployed, the implications on infant mortality are higher than in other age groups. This is a reasonable association, since there is the potential to have more people with children in this age group than in the teenage group. To reduce the risk of infant mortality, governments should decrease NEET rates through promotional programs that disseminate the benefits of being educated, employed, and trained [ 7 ]. Additionally, they can offer financial aid to public schools and companies to offer more resources to raise general health awareness in people.
We looked to see if the distribution of population without employment, education, or training (NEET) in various categories of high, medium, and low impacted the rate of deaths from cancer (Fig. 7 ). Our expectation is that high rates of NEET will positively influence deaths from cancer.
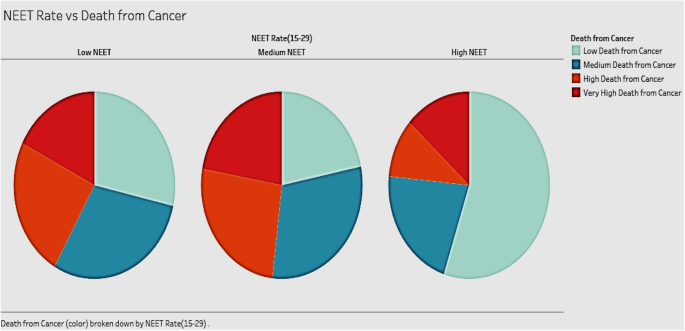
Association of Deaths from Cancer and different NEET Rates
The three pie charts in Fig. 7 show the distribution of deaths from cancer in groups of countries with different NEET rates (high, medium, and low). The analysis includes all countries in the sample. The expectation was that high rates of NEET would be associated with high rates of cancer deaths. Our results, however, show that countries with medium NEET rates tend to have the highest deaths from cancer. Countries with high NEET rates have the lowest deaths from cancer among the three groups. Contrary to expectations, countries with low NEET rates do not show the lowest death rates from cancer. A possible explanation for this can be attributed to the fact that in this group, the people in the labor force may be suffering from work-related hazards including stress, that endanger their health.
Association between adult education levels and health expenditure
It is interesting to note the relationship between health expenditure and adult education levels (Fig. 8 ). We expect them to be positively associated.
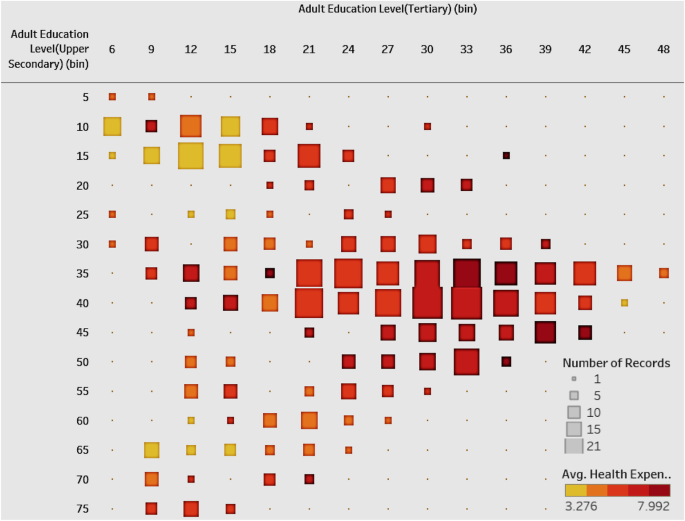
Association of Health Expenditure and Adult Education Level-Tertiary & Upper Secondary
Figure 8 shows a heat map with the number of countries in different combinations of groups between tertiary and upper-secondary adult education level. We emphasize the higher levels of adult education. The color of the square shows the average of health expenditure. The plot shows that most of the countries are divided into two clusters. One cluster has a high tertiary education level as well as a high upper-secondary education level and it has high average health expenditure. The other cluster has relatively low tertiary and upper secondary education level with low average health expenditure. Overall, the figure shows a positive correlation between adult education level and compulsory health expenditure. Governments of countries with low levels of education should allocate more health expenditure, which will have an influence on the educational levels. Alternatively, to improve public health, governments can frame educational policies to improve the overall national education level, which then produces more health awareness, contributing to national healthcare.
Association of Compulsory Health Expenditure with NEET rates by country and region
Having explored the relationship between health expenditure and adult education, we then explored the relationship between health expenditure and NEET rates of different countries (Fig. 9 ). We expect compulsory health expenditure to be negatively associated with NEET rates.
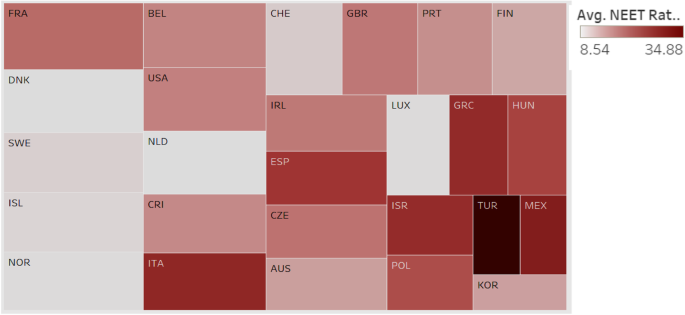
Association between Compulsory Health Expenditure and NEET Rate by Country and Region
In Fig. 9 , each box represents a country or region; the size of the box indicates the extent of compulsory health expenditure such that a larger box implies that the country has greater compulsory health expenditure. The intensity of the color of the box represents the NEET rate such that the darker color implies a higher NEET rate. Turkey has the highest NEET rate with low health expenditure. Most European countries such as France, Belgium, Sweden, and Norway have low NEET rates and high health expenditure. The chart shows a general association between low compulsory health expenditure and high NEET rates. The relationship, however, is not consistent, as there are countries with high NEET and high health expenditures. Our suggestion is for most countries to improve the social education for the youth through free training programs and other means to effectively improve the public health while they attempt to raise the compulsory expenditure.
Distribution of life expectancy at birth and tertiary enrollment rate
The distribution of enrollment rate (tertiary) and life expectancy of all the countries in the sample can give an idea of the current status of both education and health (Fig. 10 ). We expect these to be positively associated.
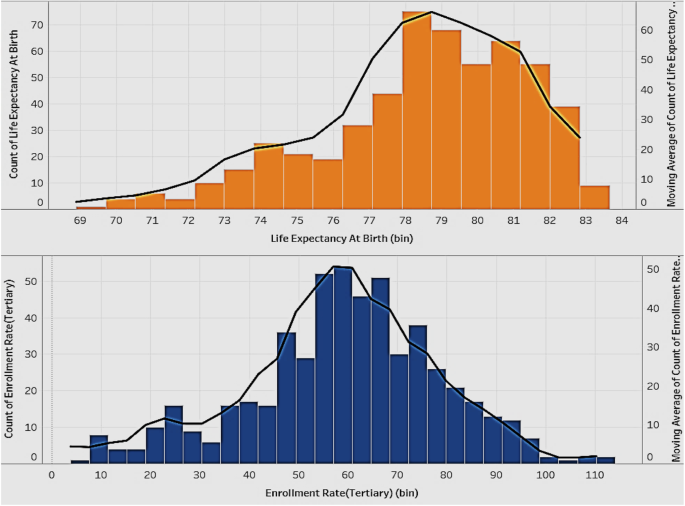
Distribution of Life Expectancy at Birth (years) and Tertiary Enrollment Rate
Figure 10 shows two histograms with the lines representing the distribution of life expectancy at birth and the tertiary enrollment rate of all the countries. The distribution of life expectancy at birth is skewed right, which means most of the countries have quite a high life expectancy and there are few countries with a very low life expectancy. The tertiary enrollment rate has a good distribution, which is closer to a normal distribution. Governments of countries with an extremely low life expectancy should try to identify the cause of this problem and take actions in time to improve the overall national health.
Comparison of adult education levels and deaths from Cancer at various levels of GDP per capita
We wanted to see if various levels of GDP per capita influence the levels of adult education and deaths from cancer in countries (Fig. 11 ).
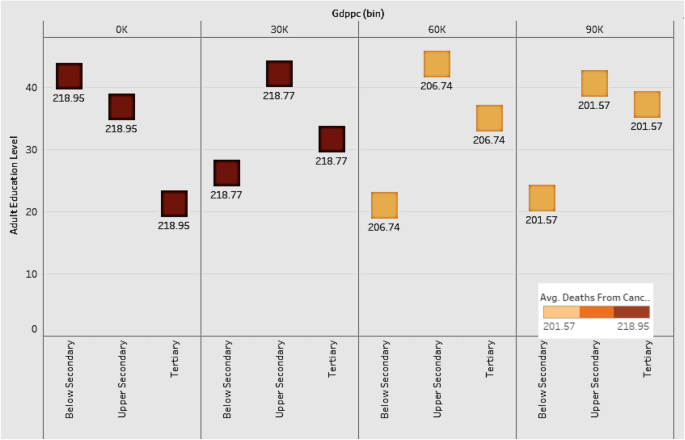
Comparison of Adult Education Levels and Deaths from Cancer at various levels of GDP per capita
Figure 11 shows the distribution of various adult education levels for countries by groups of GDP per capita. The plot shows that as GDP grows, the level of below-secondary adult education becomes lower, and the level of tertiary education gets higher. The upper-secondary education level is constant among all the groups. The implication is that tertiary education is the most important factor among all the education levels for a country to improve its economic power and health level. Countries should therefore focus on tertiary education as a driver of economic development. As for deaths from cancer, countries with lower GDP have higher death rates, indicating the negative association between economic development and deaths from cancer.
Distribution of infant mortality rates by continent
Infant mortality is an important indicator of a country’s health status. Figure 12 shows the distribution of infant mortality for the continents of Asia, Europe, Oceania, North and South America. We grouped the countries in each continent into high, medium, and low, based on infant mortality rates.
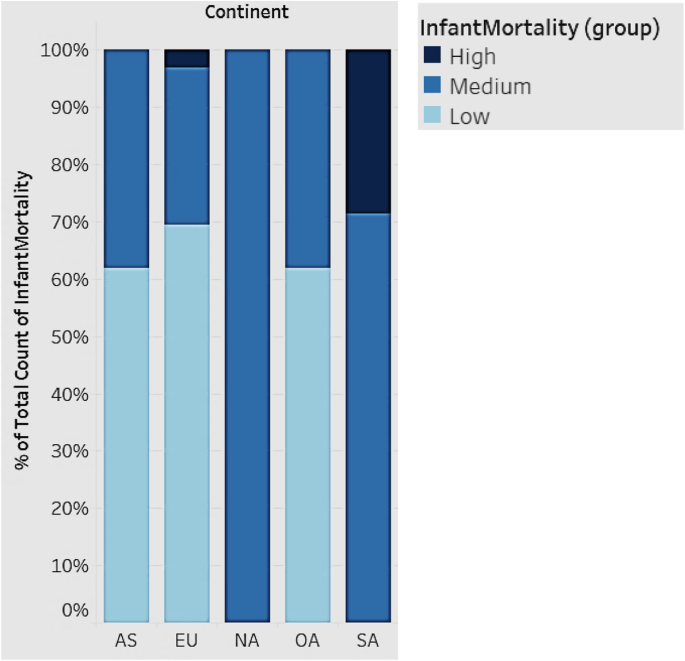
Distribution of Infant Mortality rates by Continent
In Fig. 12 , each bar represents a continent. All countries fall into three groups (high, medium, and low) based on infant mortality rates. South America has the highest infant mortality, followed by Asia, Europe, and Oceania. North America falls in the medium range of infant mortality. South American countries, in general, should strive to improve infant mortality. While Europe, in general, has the lowest infant mortality rates, there are some countries that have high rates as depicted.
Association between child vaccination rates and NEET rates
We looked at the association between child vaccination rates and NEET rates in various countries (Fig. 13 ). We expect countries that have high NEET rates to have low child vaccination rates.
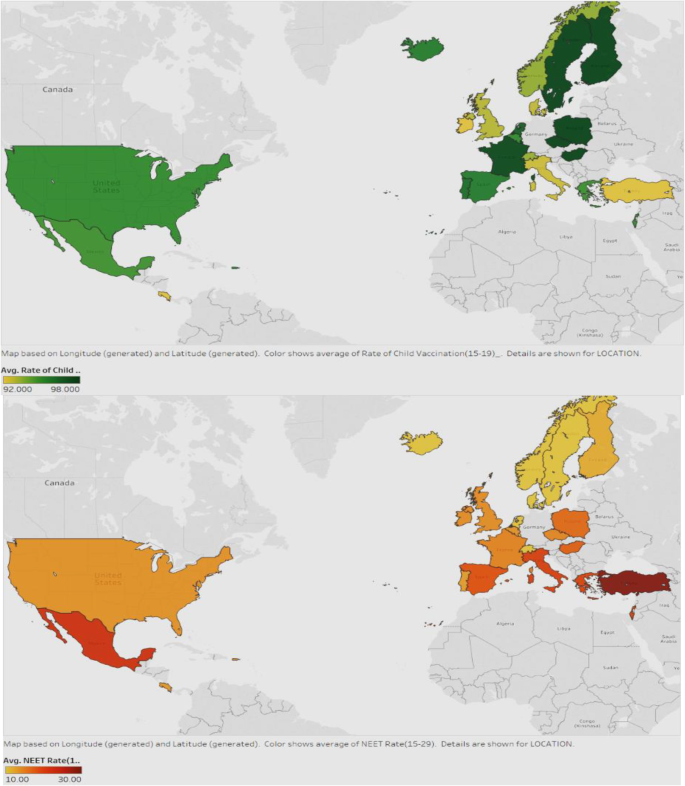
Association between Child Vaccination Rates and NEET rates
Figure 13 displays the child vaccination rates in the first map and the NEET rates in the second map, for all countries. The darker green color shows countries with higher rates of vaccination and the darker red represents those with higher NEET rates. It can be seen that in general, the countries with lower NEET also have better vaccination rates. Examples are USA, UK, Iceland, France, and North European countries. Countries should therefore strive to reduce NEET rates by enrolling a good proportion of the youth into initiatives or programs that will help them be more productive in the future, and be able to afford preventive healthcare for the families, particularly, the children.
Average smoking rate in different continents over time
We compared the trend of average smoking rate for the years 1995–201 for the continents in the sample (Fig. 14 ).
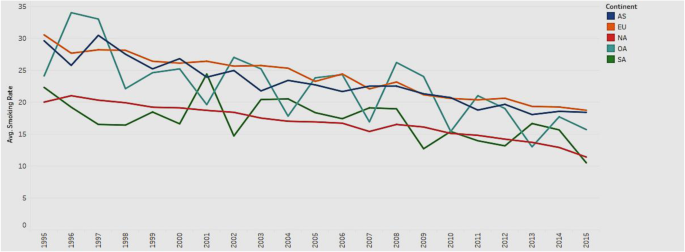
Trend of average smoking rate in different continents from 1995 to 2015
Figure 14 depicts the line charts of average smoking rates for the continents of Asia, Europe, Oceania, North and South America. All the lines show an overall downward trend, which indicates that the average smoking rate decreases with time. The trend illustrates that people have become more health conscious and realize the harmful effects of smoking over time. However, the smoking rate in Europe (EU) is consistently higher than that in other continents, while the smoking rate in North America (NA) is consistently lower over the years. Governments in Europe should pay attention to the usage of tobacco and increase health consciousness among the public.
Association between adult education levels and deaths from Cancer
We explored if adult education levels (below-secondary, upper-secondary, and tertiary) are associated with deaths from cancer (Fig. 15 ) such that higher levels of education will mitigate the rates of deaths from cancer, due to increased awareness and proactive health behavior.
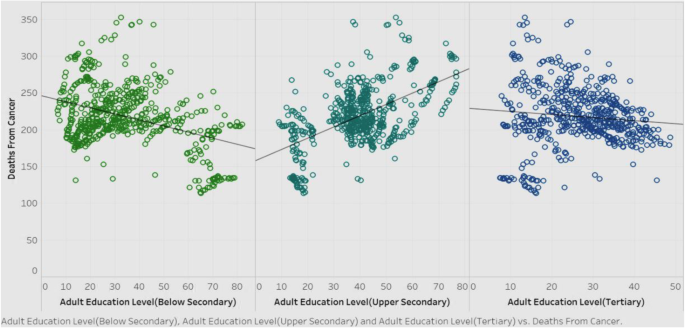
Association of deaths from cancer with adult education levels
Figure 15 shows the correlations of deaths from cancer among the three adult education levels, for all countries in the sample. It is obvious that below-secondary and tertiary adult education levels have a negative correlation with deaths from cancer, while the upper-secondary adult education level shows a positive correlation. Barring upper-secondary results, we can surmise that in general, as education level goes higher, the deaths from cancer will decrease. The rationale for this could be that education fosters more health awareness and encourages people to adopt healthy behavioral practices. Governments should therefore pay attention to frame policies that promote education. However, the counterintuitive result of the positive correlation between upper-secondary levels of adult education with the deaths from cancer warrants more investigation.
We drilled down further into the correlation between the upper-secondary education level and deaths from cancer. Figure 16 shows this correlation, along with a breakdown of the total number of records for each continent, to see if there is an explanation for the unique result.
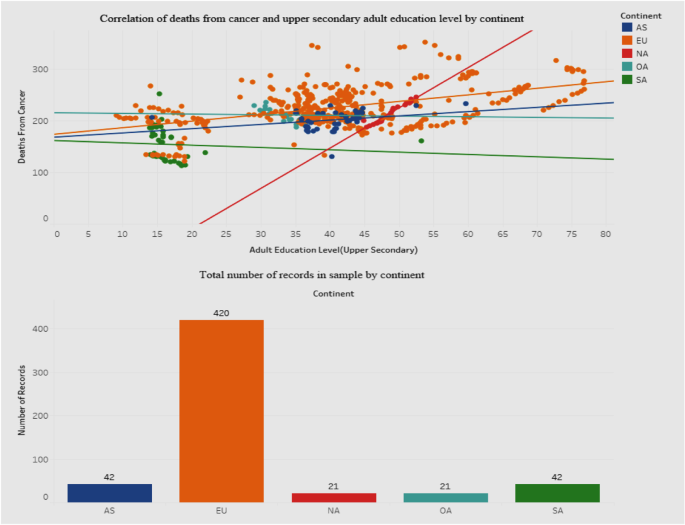
Association between deaths from cancer and adult education level-upper secondary
Figure 16 shows a dashboard containing two graphs - a scatterplot of the correlation between deaths from cancer and education level, and a bar graph showing the breakdown of the total sample by continent. We included a breakdown by continent in order to explore variances that may clarify or explain the positive association for deaths from cancer with the upper-secondary education level. The scatterplot shows that for the European Union (EU) the points are much more scattered than for the other continents. Also, the correlation between deaths and education level for the EU is positive. The bottom bar graph depicts how the sample contains a disproportionately high number of records for the EU than for other continents. It is possible that this may have influenced the results of the correlation. The governments in the EU should investigate the reasons behind this phenomenon. Also, we defer to future research to explore this in greater detail by incorporating other socioeconomic parameters that may have to be factored into the relationship.
Association between average tertiary school life expectancy and health expenditure
We moved our focus to the trends of tertiary school life expectancy and health expenditure from 1995 to 2015 (Fig. 17 ) to check for positive associations.
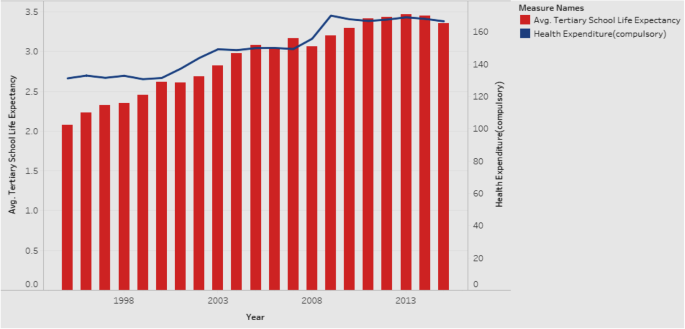
Association between Average Tertiary School Life Expectancy and Health Expenditure
Figure 17 is a combination chart explaining the trends of tertiary school life expectancy and health expenditure, for all countries in the sample. The rationale is that if there is a positive association between the two, it would be worthwhile for the government to allocate more resources towards health expenditure. Both tertiary school life expectancy and health expenditure show an increase over the years from 1995 to 2015. Our additional analysis shows that they continue to increase even after 2015. Hence, governments are encouraged to increase the health expenditure in order to see gains in tertiary school life expectancy, which will have positive implications for national health. Given that the measured effects of education are large, investments in education might prove to be a cost-effective means of achieving better health.
Our results reveal how interlinked education and health can be. We show how a country can improve its health scenario by focusing on appropriate indicators of education. Countries with higher education levels are more likely to have better national health conditions. Among the adult education levels, tertiary education is the most critical indicator influencing healthcare in terms of infant mortality, life expectancy, child vaccination rates, and enrollment rates. Our results emphasize the role that education plays in the potential years of life lost, which is a measure that represents the average years a person would have lived had he/she not died prematurely. In addition to mortality rate, an economy needs to consider this indicator as a measure of health quality.
Other educational indicators that are major drivers of health include school life expectancy, particularly at the tertiary level. In order to improve the school life expectancy of the population, governments should control the number of youths ending up unemployed, dropping out of school, and without skills or training (the NEET rate). Education allows people to gain skills/abilities and knowledge on general health, enhancing their awareness of healthy behaviors and preventive care. By targeting promotions and campaigns that emphasize the importance of skills and employment, governments can reduce the NEET rates. And, by reducing the NEET rates, governments have the potential to address a broad array of vulnerabilities among youth, ranging from unemployment, early school dropouts, and labor market discouragement, which are all social issues that warrant attention in a growing economy.
We also bring to light the health disparities across countries and suggest implications for governments to target educational interventions that can reduce inequalities and improve health, at a macro level. The health effects of education are at the grass roots level - creating better overall self-awareness on personal health and making healthcare more accessible.
Scope and limitations
Our research suffers from a few limitations. For one, the number of countries is limited, and being that the data are primarily drawn from OECD, they pertain to the continent of Europe. We also considered a limited set of variables. A more extensive study can encompass a larger range of variables drawn from heterogeneous sources. With the objective of acquiring a macro perspective on the education–health association, we incorporated some dependent variables that may not traditionally be viewed as pure health parameters. For example, the variable potential years of life lost is affected by premature deaths that may be caused by non-health related factors too. Also there may be some intervening variables in the education–health relationship that need to be considered. Lastly, while our study explores associations and relationships between variables, it does not investigate causality.
Conclusions and future research
Both education and health are at the center of individual and population health and well-being. Conceptualizations of both phenomena should go beyond the individual focus to incorporate and consider the social context and structure within which the education–health relationship is embedded. Such an approach calls for a combination of interdisciplinary research, novel conceptual models, and rich data sources. As health differences are widening across the world, there is need for new directions in research and policy on health returns on education and vice versa. In developing interventions and policies, governments would do well to keep in mind the dual role played by education—as a driver of opportunity as well as a reproducer of inequality [ 36 ]. Reducing these macro-level inequalities requires interventions directed at a macro level. Researchers and policy makers have mutual responsibilities in this endeavor, with researchers investigating and communicating the insights and recommendations to policy makers, and policy makers conveying the challenges and needs of health and educational practices to researchers. Researchers can leverage national differences in the political system to study the impact of various welfare systems on the education–health association. In terms of investment in education, we make a call for governments to focus on education in the early stages of life course so as to prevent the reproduction of social inequalities and change upcoming educational trajectories; we also urge governments to make efforts to mitigate the rising dropout rate in postsecondary enrollment that often leads to detrimental health (e.g., due to stress or rising student debt). There is a need to look into the circumstances that can modify the postsecondary experience of youth so as to improve their health.
Our study offers several prospects for future research. Future research can incorporate geographic and environmental variables—such as the quality of air level or latitude—for additional analysis. Also, we can incorporate data from other sources to include more countries and more variables, especially non-European ones, so as to increase the breadth of analysis. In terms of methodology, future studies can deploy meta-regression analysis to compare the relationships between health and some macro-level socioeconomic indicators [ 13 ]. Future research should also expand beyond the individual to the social context in which education and health are situated. Such an approach will help generate findings that will inform effective educational and health policies and interventions to reduce disparities.
Availability of data and materials
The dataset analyzed during the current study is available from the corresponding author on reasonable request.
Abbreviations
Fundamental Cause Theory
Human Capital Theory
Not in Employment, Education, or Training
Organization for Economic Cooperation and Development
Socio-economic status
Andersen RM, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc. 1973;51(1):95–124.
Article CAS Google Scholar
Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Social Behav. 1995;36(1):1–10.
Baker DP. The Schooled Society: The Educational Transformation of Global Culture. Stanford, CA: Stanford Univ. Press: 2014; 360.
Becker GS. Human capital: a theoretical and empirical analysis, with special reference to education. Chicago: Univ. Chicago Press; 1964.
Google Scholar
Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Oxford Acad J. 1979;109(2):186–204.
CAS Google Scholar
Crimmins EM, Kim JK, Vasunilashorn S. Biodemography: new approaches to understanding trends and differences in population health and mortality. Demography. 2010;47:S41–64.
Article Google Scholar
Spence M. Job market signalling. The Quarterly J Econ. 1973;87:355–79.
Cutler DM, Lleras-Muney A. Education and Health: Evaluating Theories and Evidence: NBER Working Papers; 2006. p. 12352.
Feinstein L. What are the effects of education on health? OECD Proceedings of the Copenhagen Symposium; 2006 . .
Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J Health Soc Behav. 1980;21(3):219–39.
Freedman VA, Martin LG. The role of education in explaining and forecasting trends in functional limitations among older Americans. Demography. 1999;36(4):461–73.
Freese J, Lutfey K. Fundamental causality: challenges of an animating concept for medical sociology. In: Pescosolido BA, Martin JK, McLeod JD, Rogers A, editors. Handbook of the Sociology of Health, Illness, and Healing: a blueprint for the 21st century. New York: Springer; 2011. p. 67–81.
Chapter Google Scholar
Fouweather T, Gillies C, Wohland P, Van Oyen H, Nusselde W, Robine J, Cambois E, Jagger C. Comparison of socio-economic indicators explaining inequalities in healthy life years at age 50 in Europe: 2005 and 2010. Eur J Pub Health. 2015;25:978–83.
George LK, Gwyther LP. Caregiver Weil-being: a multidimensional examination of family caregivers of demented adults. Gerontologist. 1986;26(3):253–9.
Goldman D, Smith JP. The increasing value of education to health. Soc Sc Med. 2011;72(10):1728–37.
Harper AC, Lambert LJ. The health of populations: an introduction. New York: Springer Publishing Company; 1994.
Health 2020: Education and health through the life-course. WHO Europe Sector Brief on Education Health; 2015. http://www.euro.who.int/__data/assets/pdf_file/0007/324619/Health-2020-Education-and-health-through-the-life-course-en.pdf?ua=1 .
Kino S, Bernabé E, Sabbah W. The role of healthcare and education systems in co-occurrence of health risk behaviours in 27 European countries. Eur J Public Health. 2018;28(1):186–92.
Landerman LR, Burns BJ, Swartz MS, Wagner HR, George LK. The relationship between insurance coverage and psychiatric disorder in predicting use of mental health services. Am J Psychol. 1994;151(12):1785.
Lynch SM. Cohort and life-course patterns in the relationship between education and health: a hierarchical approach. Demography. 2003;40(2):309–31.
Mackenbach J, Kunst A. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med. 1997;44(6):757–71. https://doi.org/10.1016/S0277-9536(96)00073-1 .
Article CAS PubMed Google Scholar
Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982-1994. Natl Acad Sci. 1997;94(6):2593–8.
Mirowski J, Ross CE. Education, learned effectiveness and health. London Rev Edu. 2005;3(3):205–20.
Montez JK, Berkman LF. Trends in the educational gradient of mortality among US adults aged 45 to 84 years: bringing regional context into the explanation. Am J Pub Health. 2014;104(1):e82–90.
Montez JK, Zajacova A. Trends in mortality risk by education level and cause of death among US white women from 1986 to 2006. Am J Pub Health. 2013;103:473–9.
Olshansky SJ, Antonucci T, Berkman L, Binstock RH, Boersch-Supan A, Cacioppo JT, Carnes BA, Carstensen LL, Fried LP, Goldman DP, Jackson J, Kohli M, Rother J, Zheng Y, Rowe J. Differences in life expectancy due to race and educational differences are widening, and many may not catch up. Health Aff. 2012;31(8):1803–13.
Pamuk ER. Social-class inequality in infant mortality in England and Wales from 1921 to 1980. Eur J Popul 1988; 4 , 1–21, https://doi.org/10.1007/BF01797104.
Phelan JC , Link BG , Tehranifar P . Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications . J Health Soc Behav 2010 ; 51 : S28 S40 . doi : 10.1177/0022146510383498.
Renard F, Devleesschauwer B, Speybroeck N, Deboosere P. Monitoring health inequalities when the socio-economic composition changes: are the slope and relative indices of inequality appropriate? Results of a simulation study. BMC Public Health 2019; 19: 662. https://doi.org/10.1186/s12889-019-6980-1.
Ro A, Geronimus A, Bound J, Griffith D, Gee G. Educational gradients in five Asian immigrant populations: do country of origin, duration and generational status moderate the education-health relationship? Prev Med Rep. 2016;4:338–43.
Ross CE, Wu CL. The links between education and health. Am Soc Rev. 1995;60(5):719–45.
Shiels MS, Chernyavskiy P, Anderson WF, Best AF, Haozous EA. Diverging trends in premature mortality in the U.S. by sex, race, and ethnicity in the 21st century. Lancet. 2017;389:1043–54.
Tsou MT. Association of Education, health behaviors, concerns, and knowledge with metabolic syndrome among urban elderly in one medical Center in Taiwan. Int J Gerontology. 2017;11(3:138–43.
Wheaton B. Stress, personal coping resources, and psychiatric symptoms: an investigation of interactive models. J Health Soc Behav. 1983;24(3):208–29.
Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Ann Rev Soc. 1995;21:349–86.
Zajacova A, Lawrence EM. The relationship between education and health: reducing disparities through a contextual approach. Ann Rev Pub Health. 2018;39:273–89.
Zimmerman EB, Woolf SH. Understanding the relationship between education and health. Discussion Paper, Inst Med. Washington DC; 2014. https://nam.edu/wp-content/uploads/2015/06/BPH-UnderstandingTheRelationship1.pdf .
Zhong H. An over time analysis on the mechanisms behind the education–health gradients in China. China Econ Rev. 2015;34(C):135–49.
Download references
Acknowledgements
Not applicable.
Author information
Authors and affiliations.
Koppelman School of Business, Brooklyn College of the City University of New York, 2900 Bedford Ave, Brooklyn, NY, 11210, USA
Viju Raghupathi
Gabelli School of Business, Fordham University, 140 W. 62nd Street, New York, NY, 10023, USA
Wullianallur Raghupathi
You can also search for this author in PubMed Google Scholar
Contributions
Both authors contributed equally to all parts of the manuscript.
Corresponding author
Correspondence to Viju Raghupathi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raghupathi, V., Raghupathi, W. The influence of education on health: an empirical assessment of OECD countries for the period 1995–2015. Arch Public Health 78 , 20 (2020). https://doi.org/10.1186/s13690-020-00402-5
Download citation
Received : 16 October 2019
Accepted : 26 February 2020
Published : 06 April 2020
DOI : https://doi.org/10.1186/s13690-020-00402-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Education level
- Enrollment rate
- Life expectancy
- Potential years of life lost
- Infant mortality
- Deaths from cancer
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
Health Education and Health Promotion: Key Concepts and Exemplary Evidence to Support Them
- First Online: 09 October 2018
Cite this chapter

- Hein de Vries 8 ,
- Stef P. J. Kremers 8 &
- Sonia Lippke 9
3614 Accesses
14 Citations
Health is regarded as the result of an interaction between individual and environmental factors. While health education is the process of educating people about health and how they can influence their health, health promotion targets not only people but also their environments. Promoting health behavior can take place at the micro level (the personal level), the meso level (the organizational level, including e.g. families, schools and worksites) and at the macro level (the (inter)national level, including e.g. governments). Health education is one of the methods used in health promotion, with health promotion extending beyond just health education.
Models and theories that focus on understanding health and health behavior are of key importance for health education and health promotion. Different classes of models and theories can be distinguished, such as planning models, behavioral change models, and diffusion models. Within these models different topics and factors are relevant, ranging from health literacy, attitudes, social influences, self-efficacy, planning, and stages of change to evaluation, implementation, stakeholder involvement, and policy changes. Exemplary health promotion settings are schools, worksites, and healthcare, but also the domains that are involved with policy development. Main health promotion methods can involve a variety of different methods and approaches, such as counseling, brochures, eHealth, stakeholder involvement, consensus meetings, community ownership, panel discussions, and policy development. Because health education and health promotion should be theory- and evidence-based, personalized interventions are recommended to take empirical findings and proven theoretical assumptions into account.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Similar content being viewed by others

Health Promotion Practice

Theory and Fundamentals of Health Promotion for Children and Adolescents
Aarts, H., Paulussen, T., & Schaalma, H. (1997). Physical exercise habit: On the conceptualization and formation of habitual health behaviours. Health Education Research, 12 (3), 363.
Article PubMed Google Scholar
Abraham, C., & Michie, S. (2008). A taxonomy of behavior change techniques used in interventions. Health Psychology, 27 (3), 379–387.
Abraham, C., & Sheeran, P. (2003). Acting on intentions: The role of anticipated regret. The British Journal of Social Psychology, 42 (Pt 4), 495–511.
Abraham, C., & Sheeran, P. (2005). The Health Belief Model. In M. Conner & P. Norman (Eds.), Predicting health behaviour (pp. 28–80). Berkshire: Open University Press.
Google Scholar
Abroms, L. C., & Maibach, E. W. (2008). The effectiveness of mass communication to change public behavior. Annual Review of Public Health, 29 , 219–234.
Adams, J., & White, M. (2003). Are activity promotion interventions based on the transtheoretical model effective? A critical review. British Journal of Sports Medicine, 37 (2), 106–114.
Article PubMed PubMed Central Google Scholar
Ajzen, I. (1988). Attitudes, personality, and behavior . Chicago: Dorsey Press.
Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50 (2), 179–211.
Article Google Scholar
Ajzen, I., & Fishbein, M. (1980). Understanding attitudes and predicting social behavior . Englewood Cliffs: Prentice-Hall.
Aldana, S. G., Merrill, R. M., Price, K., Hardy, A., & Hager, R. (2005). Financial impact of a comprehensive multisite workplace health promotion program. Preventive Medicine, 40 (2), 131–137.
Alderman, M. H., & Schoenbaum, E. E. (1975). Detection and treatment of hypertension at the work site. The New England Journal of Medicine, 293 (2), 65–68.
Armitage, C. J. (2009). Is there utility in the transtheoretical model? British Journal of Health Psychology, 14 (2), 195–210.
Armitage, C. J. (2004). Evidence that implementation intentions reduce dietary fat intake: A randomized trial. Health Psychology, 23 (3), 319.
Armitage, C. J., & Conner, M. (2001). Efficacy of the theory of planned behaviour: A meta-analytic review. The British Journal of Social Psychology, 40 (Pt 4), 471–499.
Armstrong, N., & Powell, J. (2008). Preliminary test of an Internet-based diabetes self-management tool. Journal of Telemedicine and Telecare, 14 (3), 114–116.
Asch, S. E. (1956). Studies of independence and conformity: I. A minority of one against a unanimous majority. Psychological Monographs, 70 (9), 1.
Ashford, S., Edmunds, J., & French, D. P. (2010). What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. British Journal of Health Psychology, 15 (Pt 2), 265–288.
Ausems, M., Mesters, I., van Breukelen, G., & De Vries, H. (2004). Effects of in-school and tailored out-of-school smoking prevention among Dutch vocational school students. Health Education Research, 19 (1), 51–63.
Austin, J. T., & Vancouver, J. B. (1996). Goal constructs in psychology: Structure, process, and content. Psychological Bulletin, 120 (3), 338.
Aveyard, P., Massey, L., Parsons, A., Manaseki, S., & Griffin, C. (2009). The effect of Transtheoretical Model based interventions on smoking cessation. Social science and medicine, 68 (3), 397–403.
Babbin, S. F., Harrington, M., Burditt, C., Redding, C., Paiva, A., Meier, K., Oatley, K., McGee, H., & Velicer, W. F. (2011). Prevention of alcohol use in middle school students: Psychometric assessment of the decisional balance inventory. Addictive Behaviors, 36 (5), 543–546.
Bagozzi, R. P. (1992). The self-regulation of attitudes, intentions, and behavior. Social Psychology Quarterly, 55 (2), 178.
Bagozzi, R. P., & Dholakia, U. (1999). Goal setting and goal striving in consumer behavior. Journal of Marketing, 63 , 19–32.
Baker, D. W., Parker, R. M., Williams, M. V., & Clark, W. S. (1998). Health literacy and the risk of hospital admission. Journal of General Internal Medicine, 13 (12), 791–798.
Bandura, A. (1977). Social learning theory . New York: General Learning Press.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory . Englewood Cliffs: Prentice-Hall.
Bandura, A. (1989). Human agency in social cognitive theory. American Psychologist, 44 (9), 1175–1184.
Bandura, A. (1993). Perceived self-efficacy in cognitive development and functioning. Educational Psychologist, 28 (2), 117–148.
Bandura, A. (1997). Editorial. American Journal of Health Promotion, 12 (1), 8–10.
Bargh, J. A. (2005). Bypassing the will: Toward demystifying the nonconscious control of social behavior. In R. R. Hassin, J. S. Uleman, & J. A. Bargh (Eds.), The new unconscious (pp. 37–58). New York: Oxford University Press.
Bartholomew, L. K., Parcel, G. S., Kok, G., & Gottlieb, N. H. (2001). Intervention-mapping: Designing theory and evidence-based health promotion programs . Mountain View: Mayfield.
Bartholomew, L. K., Parcel, G. S., Kok, G., Gottlieb, N. H., & Fernández, M. E. (2011). Planning health promotion: An intervention mapping approach (3rd ed.). San Francisco: Jossey Bass.
Bentz, C. J., Bruce Bayley, K., Bonin, K. E., Fleming, L., Hollis, J. F., Hunt, J. S., LeBlanc, B., McAfee, T., Payne, N., & Siemienczuk, J. (2007). Provider feedback to improve 5A’s tobacco cessation in primary care: A cluster randomized clinical trial. Nicotine & Tobacco Research, 9 (3), 341–349.
Berkman, L. F., & Syme, S. L. (1979). Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. American Journal of Epidemiology, 109 (2), 186–204.
Beyer, J. M., & Trice, H. M. (1978). Implementing change: Alcoholism policies in work organization . New York: Free Press.
Blissmer, B., & McAuley, E. (2002). Testing the requirements of stages of physical activity among adults: The comparative effectiveness of stage-matched, mismatched, standard care, and control interventions. Annals of Behavioral Medicine, 24 (3), 181–189.
Bodenheimer, T., Lorig, K., Holman, H., & Grumbach, K. (2002). Patient self-management of chronic disease in primary care. JAMA, 288 (19), 2469–2475.
Boer, H., & Seydel, E. R. (1996). Protection motivation theory. In M. Conner & P. Norman (Eds.), Predicting health behavior (pp. 95–120). Buckingham: Open University Press.
Bolman, C., Arwert, T. G., & Vollink, T. (2011). Adherence to prophylactic asthma medication: Habit strength and cognitions. Heart & Lung, 40 (1), 63–75.
Bonfadelli, H. (2002). Medieninhaltsforschung: Grundlagen, Methoden, Anwendungen . Konstanz: UVK.
Borland, R., Balmford, J., Segan, C., Livingston, P., & Owen, N. (2003). The effectiveness of personalized smoking cessation strategies for callers to a Quitline service. Addiction, 98 (6), 837–846.
Botvin, G. J., Eng, A., & Williams, C. L. (1980). Preventing the onset of cigarette smoking through life skills training. Preventive Medicine, 9 (1), 135–143.
Botvin, G. J., & Griffin, K. W. (2004). Life skills training: Empirical findings and future directions. The Journal of Primary Prevention, 25 (2), 211.
Bracht, N. (1990). Community organization principles in health promotion: A five-stage model. In N. Bracht & L. Kingsbury (Eds.), Health promotion at the community level . Thousand Oaks: Sage.
Bracht, N. (1999). Health promotion at the community level: New advances . Thousand Oaks: Sage.
Brewer, N. T., Weinstein, N. D., Cuite, C. L., & Herrington, J. E. (2004). Risk perceptions and their relation to risk behavior. Annals of Behavioral Medicine, 27 (2), 125.
Brewer, N. T., Brewer, N. T., & Fazekas, K. I. (2007). Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine: An International Journal Devoted to Practice and Theory, 45 (2–3), 107.
Brinn, M. P., Carson, K. V., Esterman, A. J., Chang, A. B., & Smith, B. J. (2010). Mass media interventions for preventing smoking in young people. Cochrane Database of Systematic Reviews, 11 , CD001006.
Britt, E., Hudson, S. M., & Blampied, N. M. (2004). Motivational interviewing in health settings: A review. Patient Education and Counseling, 53 (2), 147–155.
Brodie, M., Flournoy, R. E., Altman, D. E., Blendon, R. J., Benson, J. M., & Rosenbaum, M. D. (2000). Health information, the Internet, and the digital divide. Health Affairs (Millwood), 19 (6), 255–265.
Brouwer, W., Oenema, A., Raat, H., Crutzen, R., de Nooijer, J., de Vries, N. K., & Brug, J. (2010). Characteristics of visitors and revisitors to an Internet-delivered computer-tailored lifestyle intervention implemented for use by the general public. Health Education Research, 25 (4), 585–595.
Brown, T., & Summerbell, C. (2009). Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: An update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obesity Reviews, 10 (1), 110–141.
Brug, J., Lechner, L., & De Vries, H. (1995). Psychosocial determinants of fruit and vegetable consumption. Appetite, 25 (3), 285.
Brug, J., Steenhuis, I., van Assema, P., & de Vries, H. (1996). The impact of a computer-tailored nutrition intervention. Preventive Medicine, 25 (3), 236–242.
Brug, J., Steenhuis, I. H. M., Van Assema, P., Glanz, K., & De Vries, H. (1999). The impact of two computer tailored nutrition education interventions. Health Education Research, 14 , 249–256.
Brug, J., Conner, M., Harré, N., Kremers, S., McKellar, S., & Whitelaw, S. (2005). The transtheoretical model and stages of change: A critique. Observations by five commentators on the paper by Adams, J., & White, M. (2004). Why don’t stage-based activity promotion interventions work? Health Education Research, 20 (2), 244.
Bruvold, W. H. (1993). A meta-analysis of adolescent smoking prevention programs. American Journal of Public Health, 83 (6), 872.
Bryan, A., Fisher, J. D., & Fisher, W. A. (2002). Tests of the mediational role of preparatory safer sexual behavior in the context of the theory of planned behavior. Health Psychology, 21 (1), 71–80.
Campbell, M. K., Demark-Wahnefried, W., Symons, M., Kalsbeek, W. D., Dodds, J., Cowan, A., Jackson, B., Motsinger, B., Hoben, K., Lashley, J., Demissie, S., & McClelland, J. W. (1999). Fruit and vegetable consumption and prevention of cancer: The Black Churches United for Better Health project. American Journal of Public Health, 89 (9), 1390–1396.
Chaiken, S., Liberman, A., & Eagly, A. H. (1989). Heuristic and systematic information processing within and beyond the persuasion context. In J. S. Uleman & J. A. Bargh (Eds.), Unintended thought . New York: The Guilford Press.
Charles, C., Whelan, T., & Gafni, A. (1999). What do we mean by partnership in making decisions about treatment? BMJ, 319 (7212), 780–782.
Chinn, M. D., & Fairlie, R. W. (2007). The determinants of the global digital divide: A cross-country analysis of computer and internet penetration. Oxford Economic Papers, 16 , f-44.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98 (2), 310.
Collins, J. L. (1982, March). Self-efficacy and ability in achievement behavior. Paper presented at the annual meeting of the American Educational Research Association, New York.
Conner, M., & Norman, P. (2005). Predicting health behaviour: Research and practice with social cognition models . Maidenhead: Open University Press.
Conner, M., & Armitage, C. J. (1998). Extending the theory of planned behavior: A review and avenues for further research. Journal of Applied Social Psychology, 28 (15), 1429.
Conner, M., Godin, G., Sheeran, P., & Germain, M. (2013). Some feelings are more important: Cognitive attitudes, affective attitudes, anticipated affect, and blood donation. Health Psychology, 32 (3), 264.
Coster, S., & Norman, I. (2009). Cochrane reviews of educational and self-management interventions to guide nursing practice: A review. International Journal of Nursing Studies, 46 (4), 508–528.
Cramer, J. A. (2004). A systematic review of adherence with medications for diabetes. Diabetes Care, 27 (5), 1218–1224.
Cranney, M., Warren, E., Barton, S., Gardner, K., & Walley, T. (2001). Why do GPs not implement evidence-based guidelines? A descriptive study. Family Practice, 18 (4), 359–363.
Cutrona, S. L., Choudhry, N. K., Stedman, M., Servi, A., Liberman, J. N., Brennan, T., Fischer, M. A., Alan Brookhart, M., & Shrank, W. H. (2010). Physician effectiveness in interventions to improve cardiovascular medication adherence: A systematic review. Journal of General Internal Medicine, 25 (10), 1090–1096.
de Bruijn, G. J., Kremers, S. P., De Vries, H., Van Mechelen, W., & Brug, J. (2007). Associations of social-environmental and individual-level factors with adolescent soft drink consumption: Results from the SMILE study. Health Education Research, 22 (2), 227–237.
de Meij, J. S., Chinapaw, M. J., Kremers, S. P., Jurg, M. E., & Van Mechelen, W. (2010). Promoting physical activity in children: The stepwise development of the primary school-based JUMP-in intervention applying the RE-AIM evaluation framework. British Journal of Sports Medicine, 44 (12), 879–887.
de Nooijer, J., Lechner, L., & de Vries, H. (2002). Early detection of cancer: Knowledge and behavior among Dutch adults. Cancer Detection and Prevention, 26 (5), 362–369.
de Vet, E., de Nooijer, J., de Vries, N. K., & Brug, J. (2008a). Testing the transtheoretical model for fruit intake: Comparing web-based tailored stage-matched and stage-mismatched feedback. Health Education Research, 23 (2), 218–227.
de Vet, E., De Nooijer, J., De Vries, N. K., & Brug, J. (2008b). Do the transtheoretical processes of change predict transitions in stages of change for fruit intake? Health Education & Behavior, 35 (5), 603–618.
de Vet, E., Gebhardt, W. A., Sinnige, J., Van Puffelen, A., Van Lettow, B., & de Wit, J. B. (2011). Implementation intentions for buying, carrying, discussing and using condoms: The role of the quality of plans. Health Education Research, 26 (3), 443–455.
de Vries, H., & Backbier, E. (1994). Self-efficacy as an important determinant of quitting among pregnant women who smoke: The phi-pattern. Preventive Medicine, 23 (2), 167–174.
de Vries, H., & Brug, J. (1999). Computer-tailored interventions motivating people to adopt health promoting behaviours: Introduction to a new approach. Patient Education and Counseling, 36 (2), 99–105.
de Vries, H., & van Dillen, S. (2002). Prevention of Lyme disease in Dutch children: Analysis of determinants of tick inspection by parents. Preventive Medicine, 35 (2), 160–165.
de Vries, H., & van Dillen, S. (2007). I PLAN: Planning the prevention of Lyme disease, a health promotion approach. In P. van Nitch (Ed.), Research on Lyme disease . New York: Nova Science.
de Vries, H., Dijkstra, M., & Kuhlman, P. (1988). Self-efficacy: The third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health Education Research, 3 (3), 273.
de Vries, H., Backbier, E., Kok, G., & Dijkstra, M. (1995). The impact of social influences in the context of attitude, self-efficacy, intention and previous behavior as predictors of smoking onset. Journal of Applied Social Psychology, 25 , 237–257.
de Vries, H., Mudde, A. N., Dijkstra, A., & Willemsen, M. C. (1998). Differential beliefs, perceived social influences, and self-efficacy expectations among smokers in various motivational phases. Preventive Medicine, 27 (5 Pt 1), 681–689.
de Vries, H., Mudde, A., Leijs, I., Charlton, A., Vartiainen, E., Buijs, G., Clemente, M. P., Storm, H., González Navarro, A., Nebot, M., Prins, T., & Kremers, S. (2003). The European Smoking Prevention Framework Approach (EFSA): An example of integral prevention. Health Education Research, 18 (5), 611–626.
de Vries, H., Lezwijn, J., Hol, M., & Honing, C. (2005). Skin cancer prevention: Behaviour and motives of Dutch adolescents. European Journal of Cancer Prevention, 14 (1), 39–50.
de Vries, H., Candel, M., Engels, R., & Mercken, L. (2006). Challenges to the peer influence paradigm: Results for 12–13 year olds from six European countries from the European Smoking Prevention Framework Approach study. Tobacco Control, 15 (2), 83–89.
de Vries, H., van’t Riet, J., Panday, S., & Reubsaet, A. (2007). Access point analysis in smoking and nonsmoking adolescents: Findings from the European Smoking Prevention Framework Approach study. European Journal of Cancer Prevention, 16 (3), 257–265.
de Vries, H., Kremers, S., Smeets, T., & Reubsaet, A. (2008a). Clustering of diet, physical activity and smoking and a general willingness to change. Psychology & Health, 23 (3), 265.
de Vries, H., van’t Riet, J., Spigt, M., Metsemakers, J., van den Akker, M., Vermunt, J. K., & Kremers, S. (2008b). Clusters of lifestyle behaviors: Results from the Dutch SMILE study. Preventive Medicine, 46 (3), 203–208.
de Vries, H., Kremers, S. P. J., Smeets, T., Brug, J., & Eijmael, K. (2008c). The effectiveness of tailored feedback and action plans in an intervention addressing multiple health behaviors. American Journal of Health Promotion, 22 (6), 417–425.
Dean, A. J., Walters, J., & Hall, A. (2010). A systematic review of interventions to enhance medication adherence in children and adolescents with chronic illness. Archives of Disease in Childhood, 95 (9), 717–723.
Della Mea, V. (2001). What is e-Health (2): The death of telemedicine? Journal of Medical Internet Research, 3 (2), e22.
Dempsey, A. R., Johnson, S. S., & Westhoff, C. L. (2011). Predicting oral contraceptive continuation using the transtheoretical model of health behavior change. Perspectives on Sexual and Reproductive Health, 43 (1), 23–29.
Dictionary, O. E. (2010). “Mass media, n.”, Oxford University Press.
Dijk, F., & de Vries, H. (2009). Smoke alert: A computer-tailored smoking-cessation intervention for Dutch adolescents. Documentation of a FCHE workshop held in Berlin, 18–19 September 2008. Research and Practice of Health Promotion, 14 , 34–46.
Dijkstra, A. (2005). Working mechanisms of computer-tailored health education: Evidence from smoking cessation. Health Education Research, 20 (5), 527–539.
Dijkstra, A., & De Vries, H. (1999). The development of computer-generated tailored interventions. Patient Education and Counseling, 36 (2), 193–203.
Dijkstra, A., & De Vries, H. (2000). Subtypes of precontemplating smokers defined by different long-term plans to change their smoking behavior. Health Education Research, 15 (4), 423–434.
Dijkstra, A., Bakker, M., & De Vries, H. (1997). Subtypes within a sample of precontemplating smokers: A preliminary extension of the stages of change. Addictive Behaviors, 22 (3), 327–337.
Dijkstra, A., De Vries, H., Roijackers, J., & van Breukelen, G. (1998). Tailored interventions to communicate stage-matched information to smokers in different motivational stages. Journal of Consulting and Clinical Psychology, 66 (3), 549–557.
Dijkstra, A., Conijn, B., & De Vries, H. (2006). A match–mismatch test of a stage model of behaviour change in tobacco smoking. Addiction, 101 (7), 1035–1043.
DiMatteo, M. R. (2004). Social support and patient adherence to medical treatment: A meta-analysis. Health Psychology, 23 (2), 207–218.
Dlamini, S., Taylor, M., Mkhize, N., Huver, R., Sathiparsad, R., de Vries, H., Naidoo, K., & Jinabhai, C. (2009). Gender factors associated with sexual abstinent behaviour of rural South African high school going youth in KwaZulu-Natal, South Africa. Health Education Research, 24 (3), 450–460.
Dunton, G. F., Lagloire, R., & Robertson, T. (2009). Using the RE-AIM framework to evaluate the statewide dissemination of a school-based physical activity and nutrition curriculum: “Exercise Your Options”. American Journal of Health Promotion, 23 (4), 229–232.
Dusenbury, L., Brannigan, R., Falco, M., & Hansen, W. B. (2003). A review of research on fidelity of implementation: Implications for drug abuse prevention in school settings. Health Education Research, 18 (2), 237–256.
Epstein, S. (1994). Integration of the cognitive and the psychodynamic unconscious. The American Psychologist, 49 (8), 709–724.
Etter, J. F. (2009). Comparing computer-tailored, internet-based smoking cessation counseling reports with generic, untailored reports: A randomized trial. Journal of Health Communication, 14 (7), 646–657.
Evans, R. I. (1976). Smoking in children: Developing a social psychological strategy of deterrence. Preventive Medicine, 5 (1), 122–127.
Evans-Whipp, T., Beyers, J. M., Lloyd, S., Lafazia, A. N., Toumbourou, J. W., Arthur, M. W., & Catalano, R. F. (2004). A review of school drug policies and their impact on youth substance use. Health Promotion International, 19 (2), 227.
Eysenbach, G. (2005). The law of attrition. Journal of Medical Internet Research, 7 (1), e11.
Faggiano, F., Vigna-Taglianti, F. D., Versino, E., Zambon, A., Borraccino, A., & Lemma, P. (2008). School-based prevention for illicit drugs use: A systematic review. Preventive Medicine, 46 (5), 385–396.
Farquhar, J. W., Fortmann, S. P., Flora, J. A., Taylor, C. B., Haskell, W. L., Williams, P. T., Maccoby, N., & Wood, P. D. (1990). Effects of communitywide education on cardiovascular disease risk factors. The Stanford Five-City Project. JAMA, 264 (3), 359–365.
Fazio, R. H. (1990). Multiple processes by which attitudes guide behaviour: The MODE model as an integrative framework. In M. P. Zanna (Ed.), Advances in experimental social psychology (pp. 75–109). San Diego: Academic Press.
Feifer, C., Ornstein, S. M., Jenkins, R. G., Wessell, A., Corley, S. T., Nemeth, L. S., Roylance, L., Nietert, P. J., & Liszka, H. (2006). The logic behind a multimethod intervention to improve adherence to clinical practice guidelines in a nationwide network of primary care practices. Evaluation & the Health Professions, 29 (1), 65–88.
Festinger, L. (1954). A theory of social comparison processes. Human Relations, 7 , 117.
Fishbein, M., & Ajzen, I. (1975). Belief, attitude, intention, and behavior: An introduction to theory and research . Reading: Addison-Wesley.
Fishbein, M., & Ajzen, I. (2010). Predicting and changing behavior: The reasoned action approach . New York: Taylor & Francis Group.
Fletcher, A., Bonell, C., & Hargreaves, J. (2008). School effects on young people’s drug use: A systematic review of intervention and observational studies. The Journal of Adolescent Health, 42 (3), 209–220.
Fleuren, M., Wiefferink, K., & Paulussen, T. (2004). Determinants of innovation within health care organizations: Literature review and Delphi study. International Journal for Quality in Health Care, 16 (2), 107–123.
Floyd, D. L., Prentice-Dunn, S., & Rogers, R. W. (2000). A meta-analysis of research on protection motivation theory. Journal of Applied Social Psychology, 30 (2), 407–429.
Fox, M. P. (2009). A systematic review of the literature reporting on studies that examined the impact of interactive, computer-based patient education programs. Patient Education and Counseling, 77 (1), 6–13.
Fransen, G. A. J., Mesters, I., Janssen, M. J. R., Knottnerus, J. A., & Muris, J. W. M. (2009). Which patient-related factors determine self-perceived patient adherence to prescribed dyspepsia medication? Health Education Research, 24 (5), 788–798.
Gaglio, B., Shoup, J. A., & Glasgow, R. E. (2013). The RE-AIM framework: A systematic review of use over time. American Journal of Public Health, 103 (6), e38–e46.
Gagne, C., & Godin, G. (2000). The theory of planned behavior: Some measurement issues concerning belief-based variables. Journal of Applied Social Psychology, 30 (10), 2173–2193.
Glanz, K., Rimer, B. K., & Viswanath, K. (2008). Health behavior and health education: Theory, research, and practice . San Francisco: Jossey-Bass.
Glasgow, R. E., Vogt, T. M., & Boles, S. M. (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89 (9), 1322–1327.
Glasgow, R. E., Lichtenstein, E., & Marcus, A. C. (2003). Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health, 93 (8), 1261–1267.
Glynn, T. J. (1989). Essential elements of school-based smoking prevention programs. The Journal of School Health, 59 (5), 181–188.
Godin, G., & Conner, M. (2008). Intention-behavior relationship based on epidemiologic indices: An application to physical activity. American Journal of Health Promotion, 22 (3), 180–182.
Godin, G., & Kok, G. (1996). The theory of planned behavior: A review of its applications to health-related behaviors. American Journal of Health Promotion, 11 (2), 87–98.
Goebbels, A. F., Goebbels, A. F. G., Nicholson, J. M., Walsh, K., & De Vries, H. (2008). Teachers’ reporting of suspected child abuse and neglect: Behaviour and determinants. Health Education Research, 23 (6), 941–951.
Goetzel, R. Z., & Ozminkowski, R. J. (2008). The health and cost benefits of work site health-promotion programs. Annual Review of Public Health, 29 , 303–323.
Gollwitzer, P. M. (1990). Action phases and mind-sets. In E. T. Higgins & R. M. Sorrentino (Eds.), Handbook of motivation and cognition: Foundations of social behavior (Vol. 2, pp. 53–92). New York: Guilford Press.
Gollwitzer, P. M. (1999). Implementation intentions: Strong effects of simple plans. American Psychologist, 54 (7), 493.
Gollwitzer, P. M., & Sheeran, P. (2006). Implementation intentions and goal achievement: A Meta-analysis of effects and processes. Advances in Experimental Social Psychology, 38 , 69–119.
Grant, R. W., Wald, J. S., Poon, E. G., Schnipper, J. L., Gandhi, T. K., Volk, L. A., & Middleton, B. (2006). Design and implementation of a web-based patient portal linked to an ambulatory care electronic health record: Patient gateway for diabetes collaborative care. Diabetes Technology & Therapeutics, 8 (5), 576–586.
Green, L. W. (1980). Health education planning: A diagnostic approach . Palo Alto: Mayfield.
Green, L. W., & Kreuter, M. W. (1991). Health promotion planning: An educational and environmental approach . Mountain View: Mayfield.
Green, L. W., & Kreuter, M. (1999). Health promotion planning: An educational and ecological approach . Mountain View: Mayfield.
Green, L. W., & Kreuter, M. W. (2005). Health program planning: An educational and ecological approach . New York: McGraw-Hill.
Grilli, R., Ramsay, C., & Minozzi, S. (2002). Mass media interventions: Effects on health services utilisation. Cochrane Database of Systematic Reviews, 1 , CD000389.
Groeneveld, I. F., Proper, K. I., Van der Beek, A. J., & Van Mechelen, W. (2010). Sustained body weight reduction by an individual-based lifestyle intervention for workers in the construction industry at risk for cardiovascular disease: Results of a randomized controlled trial. Preventive Medicine, 51 (3-4), 240–246.
Grol, R., & Jones, R. (2000). Twenty years of implementation research. Family Practice, 17 (Suppl 1), S32–S35.
Grube, J. W., Morgan, M., & McGree, S. T. (1986). Attitudes and normative beliefs as predictors of smoking intentions and behaviours: A test of three models. The British Journal of Social Psychology, 25 (Pt 2), 81–93.
Hagger, M. S., Lonsdale, A. J., Hein, V., Koka, A., Lintunen, T., Pasi, H., Lindwall, M., Rudolfsson, L., & Chatzisarantis, N. L. D. (2011). Predicting alcohol consumption and binge drinking in company employees: An application of planned behaviour and self-determination theories. British Journal of Health Psychology, 17 (2), 379–407.
Hall, K. L., & Rossi, J. S. (2008). Meta-analytic examination of the strong and weak principles across 48 health behaviors. Preventive Medicine, 46 (3), 266–274.
Hallfors, D., & Godette, D. (2002). Will the ‘principles of effectiveness’ improve prevention practice? Early findings from a diffusion study. Health Education Research, 17 (4), 461–470.
Handley, M., MacGregor, K., Schillinger, D., Sharifi, C., Wong, S., & Bodenheimer, T. (2006). Using action plans to help primary care patients adopt healthy behaviors: A descriptive study. Journal of American Board of Family Medicine, 19 (3), 224–231.
Hansen, W. B. (1992). School-based substance abuse prevention: A review of the state of the art in curriculum, 1980–1990. Health Education Research, 7 (3), 403–430.
Harakeh, Z., Scholte, R. H., Vermulst, A. A., de Vries, H., & Engels, R. C. (2004). Parental factors and adolescents’ smoking behavior: An extension of the theory of planned behavior. Preventive Medicine, 39 (5), 951–961.
Harden, A., Peersman, G., Oliver, S., Mauthner, M., & Oakley, A. (1999). A systematic review of the effectiveness of health promotion interventions in the workplace. Occupational Medicine (London), 49 (8), 540–548.
Harting, J., Rutten, G. M., Rutten, S. T., & Kremers, S. P. (2009). A qualitative application of the diffusion of innovations theory to examine determinants of guideline adherence among physical therapists. Physical Therapy, 89 (3), 221–232.
Hawkins, R. P., Kreuter, M., Resnicow, K., Fishbein, M., & Dijkstra, A. (2008). Understanding tailoring in communicating about health. Health Education Research, 23 (3), 454–466.
US Department of Health and Human Services. (1991). Healthy people 2000: National health promotion and disease prevention objectives and healthy schools. Journal of School Health, 61 (7), 298–328.
Heckhausen, H. (1991). Motivation and action . New York: Springer.
Book Google Scholar
Helmink, J. H., Meis, J. J., de Weerdt, I., Visser, F. N., de Vries, N. K., & Kremers, S. P. (2010). Development and implementation of a lifestyle intervention to promote physical activity and healthy diet in the Dutch general practice setting: The BeweegKuur programme. International Journal of Behavioral Nutrition and Physical Activity, 7 , 49.
Henderson, V. (1966). The nature of nursing . New York: Macmillan.
Hendriksen, E. S., Pettifor, A., Lee, S. J., Coates, T. J., & Rees, H. V. (2007). Predictors of condom use among young adults in South Africa: The Reproductive Health and HIV Research Unit National Youth Survey. American Journal of Public Health, 97 (7), 1241–1248.
Herzog, T. A., & Blagg, C. O. (2007). Are most precontemplators contemplating smoking cessation? Assessing the validity of the stages of change. Health Psychology, 26 (2), 222.
Hettema, J., Steele, J., & Miller, W. R. (2005). Motivational interviewing. Annual Review of Clinical Psychology, 1 , 91–111.
Hochbaum, G. M. (1971). Measurement of effectiveness of health education activites. International Journal of Health Education, 2 , 54–59.
Hoffman, D. L., & Novak, T. P. (1998). Bridging the racial divide on the Internet. Science, 280 , 390–391.
Hofmann, W., Friese, M., & Wiers, R. W. (2008). Impulsive versus reflective influences on health behavior: A theoretical framework and empirical review. Health Psychology Review, 2 , 111–137.
Holm, K., Kremers, S. P., & de Vries, H. (2003). Why do Danish adolescents take up smoking? European Journal of Public Health, 13 (1), 67–74.
Horowitz, S. M. (2003). Applying the transtheoretical model to pregnancy and STD prevention: A review of the literature. American Journal of Health Promotion, 17 (5), 304–328.
Hoving, E. F., Mudde, A. N., & de Vries, H. (2006). Smoking and the O pattern; predictors of transitions through the stages of change. Health Education Research, 21 (3), 305–314.
Hovland, C. I., Janis, I. L., & Kelley, H. H. (1953). Communication and persuasion: Psychological studies of opinion change . New Haven: Yale UP.
Huver, R. M. E., Engels, R. C. M. E., & de Vries, H. (2006). Are anti-smoking parenting practices related to adolescent smoking cognitions and behavior? Health Education Research, 21 (1), 66–77.
Huver, R. M., Engels, R. C. M. E., Vermulst, A. A., & de Vries, H. (2007). Is parenting style a context for smoking-specific parenting practices? Drug and Alcohol Dependence, 89 (2-3), 116–125.
Hyman, H. H., & Sheatsley, P. B. (1947). Some reasons why information campaigns fail. Public Opinion Quarterly, 11 , 412–423.
Ito, K. E., & Brown, J. D. (2010). To friend or not to friend: Using new media for adolescent health promotion. North Carolina Medical Journal, 71 (4), 367–372.
PubMed Google Scholar
Jackson, C., Lawton, R., Knapp, P., Raynor, D. K., Conner, M., Lowe, C., & Closs, S. J. (2005). Beyond intention: Do specific plans increase health behaviours in patients in primary care? A study of fruit and vegetable consumption. Social Science & Medicine, 60 (10), 2383.
James, S., Reddy, P., Ruiter, R. A., McCauley, A., & Borne, B. V. D. (2006). The impact of an HIV and AIDS life skills program on secondary school students in KwaZulu-Natal, South Africa. AIDS Educ Prev, 18 (4), 281–294.
Janis, I. L., & Mann, L. (1977). Decision making: A psychological analysis of conflict, choice, and commitment . New York: Free Press.
Janssen, E., van Osch, L., de Vries, H., & Lechner, L. (2011). Measuring risk perceptions of skin cancer: Reliability and validity of different operationalizations. British Journal of Health Psychology, 16 (Pt 1), 92–112.
Janssen, E., van Osch, L., Lechner, L., Candel, M., & de Vries, H. (2012). Thinking versus feeling: Differentiating between cognitive and affective components of perceived cancer risk. Psychology & Health, 27 (7), 767–783.
Janssen, E., van Osch, L., de Vries, H., & Lechner, L. (2013). Examining direct and indirect pathways to health behaviour: The influence of cognitive and affective probability beliefs. Psychology & Health, 28 (5), 546–560.
Janz, N. K., & Becker, M. H. (1984). The Health Belief Model: A decade later. Health Education Quarterly, 11 (1), 1–47.
Johnson, C. E., Mues, K. E., Mayne, S. L., & Kiblawi, A. N. (2008). Cervical cancer screening among immigrants and ethnic minorities: A systematic review using the Health Belief Model. Journal of Lower Genital Tract Disease, 12 (3), 232–241.
Joosten, E. A., DeFuentes-Merillas, L., De Weert, G. H., Sensky, T., Van Der Staak, C. P. F., & de Jong, C. A. (2008). Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychotherapy and Psychosomatics, 77 (4), 219–226.
Jurg, M. E., Kremers, S. P., Candel, M. J., Van der Wal, M. F., & Meij, J. S. D. (2006). A controlled trial of a school-based environmental intervention to improve physical activity in Dutch children: JUMP-in, kids in motion. Health Promotion International, 21 (4), 320.
Kamarck, T. W., Manuck, S. B., & Jennings, J. R. (1990). Social support reduces cardiovascular reactivity to psychological challenge: A laboratory model. Psychosomatic Medicine, 52 (1), 42.
Kemp, R., Kirov, G., Everitt, B., Hayward, P., & David, A. (1998). Randomised controlled trial of compliance therapy. 18-month follow-up. The British Journal of Psychiatry, 172 , 413–419.
King, E. S., Rimer, B. K., Seay, J., Balshem, A., & Engstrom, P. F. (1994). Promoting mammography use through progressive interventions: Is it effective? American Journal of Public Health, 84 (1), 104–106.
Kirby, D. B., Laris, B. A., & Rolleri, L. A. (2007). Sex and HIV education programs: Their impact on sexual behaviors of young people throughout the world. The Journal of Adolescent Health, 40 (3), 206–217.
Knai, C., Pomerleau, J., Lock, K., & McKee, M. (2006). Getting children to eat more fruit and vegetables: A systematic review. Preventive Medicine: An International Journal Devoted to Practice and Theory, 42 (2), 85.
Kok, G., Lo, S. H., Peters, G. J. Y., & Ruiter, R. A. (2011). Changing energy-related behavior: An intervention mapping approach. Energy Policy, 39 , 5280–5286.
Kolbe, L. J. (1985). Why school health education? An empirical point of view. Health Education, 16 (2), 116–120.
Kremers, S. P. (2010). Theory and practice in the study of influences on energy balance-related behaviors. Patient Education and Counseling, 79 (3), 291–298.
Kremers, S. P., & Brug, J. (2008). Habit strength of physical activity and sedentary behavior among children and adolescents. Pediatric Exercise Science, 20 (1), 5–14. Discussion 14-7.
Kremers, S. P. J., Mudde, A. N., & de Vries, H. (2001). Subtypes within the precontemplation stage of adolescent smoking acquisition. Addictive Behaviors, 26 (2), 237.
Kremers, S. P., De Bruijn, G. J., Visscher, T. L., Van Mechelen, W., De Vries, N. K., & Brug, J. (2006). Environmental influences on energy balance-related behaviors: A dual-process view. International Journal of Behavioral Nutrition and Physical Activity, 3 , 9.
Kreuter, M. W., & Strecher, V. J. (1996). Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial. Health Education Research, 11 (1), 97–105.
Kreuter, M. W., Farrell, D. W., Olevitch, L. R., & Brennan, L. K. (2000). Tailoring health messages: Customizing communication with computer technology . Mahwah: Lawrence Erlbaum Associates.
Kroeze, W., Werkman, A., & Brug, J. (2006). A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Annals of Behavioral Medicine, 31 (3), 205–223.
Kruger, S. (1991). The patient educator role in nursing. Applied Nursing Research, 4 (1), 19–24.
Kwak, L., Kremers, S. P., van Baak, M. A., & Brug, J. (2007). Formation of implementation intentions promotes stair use. American Journal of Preventive Medicine, 32 (3), 254.
Latham, G. P., & Locke, E. A. (2006). Enhancing the benefits and overcoming the pitfalls of goal setting. Organizational Dynamics, 35 (4), 332–340.
Lazarus, R. S. (1966). Psychological stress and the coping process . New York: McGraw-Hill.
Leung, L. (2008). Internet embeddedness: Links with online health information seeking, expectancy value/quality of health information websites, and Internet usage patterns. Cyberpsychology & Behavior, 11 (5), 565–569.
Leventhal, H. (1970). Findings and theory in the study of fear communications. In L. Berkowitz (Ed.), Advances in experimental social psychology . New York: Academic Press.
Leventhal, H., & Cameron, L. (1987). Behavioral theories and the problem of compliance. Patient Education and Counseling, 10 (2), 117.
Leventhal, H., Nerenz, D. R., & Steele, D. J. (1984). Illness representation and coping with health threats . In A. Baum, S. E. Taylor, & J. E. Singer (Eds.), Handbook of psychology and health (pp. 219–252). Hillsdale: Lawrence Erlbaum Associates.
Lewis, B. A., Williams, D. M., Neighbors, C. J., Jakicic, J. M., & Marcus, B. H. (2010). Cost analysis of Internet vs. print interventions for physical activity promotion. Psychology of Sport and Exercise, 11 (3), 246–249.
Lippke, S., & Plotnikoff, R. C. (2012). Testing two principles of the health action process approach in individuals with type 2 diabetes. Health Psychology .
Lippke, S., & Ziegelmann, J. P. (2008). Theory-based health behavior change: Developing, testing, and applying theories for evidence-based interventions. Applied Psychology, 57 (4), 698–716.
Lippke, S., Ziegelmann, J. P., & Schwarzer, R. (2004). Initiation and maintenance of physical exercise: Stage-specific effects of a planning intervention. Research in Sports Medicine, 12 (3), 221.
Lippke, S., Ziegelmann, J. P., & Schwarzer, R. (2005). Stage-specific adoption and maintenance of physical activity: Testing a three-stage model. Psychology of Sport and Exercise, 6 , 585–603.
Lippke, S., Schwarzer, R., Ziegelmann, J. P., Scholz, U., & Schüz, B. (2010). Testing stage-specific effects of a stage-matched intervention: A randomized controlled trial targeting physical exercise and its predictors. Health Education & Behavior, 37 (4), 533–546.
Liu, L. L., & Park, D. C. (2004). Aging and medical adherence: The use of automatic processes to achieve effortful things. Psychology and Aging, 19 (2), 318–325.
Locke, E. A., & Latham, G. P. (2002). Building a practically useful theory of goal setting and task motivation. A 35-year odyssey. The American Psychologist, 57 (9), 705–717.
Lotrean, L. M., Dijk, F., Mesters, I., Ionut, C., & De Vries, H. (2010). Evaluation of a peer-led smoking prevention programme for Romanian adolescents. Health Education Research, 25 (5), 803.
Luszczynska, A., & Schwarzer, R. (2003). Planning and self-efficacy in the adoption and maintenance of breast self-examination: A longitudinal study on self-regulatory cognitions. Psychology & Health, 18 (1), 93–108.
MacGregor, K., Handley, M., Wong, S., Sharifi, C., Gjeltema, K., Schillinger, D., & Bodenheimer, T. (2006). Behavior-change action plans in primary care: A feasibility study of clinicians. The Journal of the American Board of Family Medicine, 19 , 215–223.
Marks, R., Allegrante, J. P., & Lorig, K. (2005). A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part II). Health Promotion Practice, 6 (2), 148–156.
Marlatt, G. A., & George, W. H. (1984). Relapse prevention: Introduction and overview of the model. British Journal of Addiction, 79 (3), 261–273.
Marshall, S. J., & Biddle, S. J. (2001). The transtheoretical model of behavior change: A meta-analysis of applications to physical activity and exercise. Annals of Behavioral Medicine, 23 (4), 229–246.
Martinez, M. (2008). High attrition rates in e-learning: Challenges, predictors, and solutions (p. 15). Santa Rosa: The E-Learning Developers’ Journal.
Mays, D., Streisand, R., Walker, L. R., Prokhorov, A. V., & Tercyak, K. P. (2012). Cigarette smoking among adolescents with type 1 diabetes: Strategies for behavioral prevention and intervention. Journal of Diabetes and its Complications, 26 (2), 148–153.
McGuire, W. J. (1985). Attitudes and attitude change. In G. Lindzey & E. Aronson (Eds.), Handbook of social psychology (Vol. II). New York: Lawrence Erlbaum Associates.
McKenzie, J. F., & Smeltzer, J. L. (2001). Planning, implementing and evaluating health promotion programs . Boston: Allyn and Bacon.
McLean, S. M., Burton, M., Bradley, L., & Littlewood, C. (2010). Interventions for enhancing adherence with physiotherapy: A systematic review. Manual Therapy, 15 (6), 514–521.
McLeroy, K. R., Bibeau, D., Steckler, A., & Glanz, K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15 (4), 351–377.
Mercken, L., Snijders, T. A., Steglich, C., & de Vries, H. (2009). Dynamics of adolescent friendship networks and smoking behavior: Social network analyses in six European countries. Social Science & Medicine, 69 (10), 1506.
Mercken, L., Candel, M., Van Osch, L., & De Vries, H. (2010). No smoke without fire: The impact of future friends on adolescent smoking behaviour. British Journal of Health Psychology, 16 (Pt 1), 170–188.
Milgram, S. (1963). Behavioral study of obedience. Journal of Abnormal Psychology, 67 , 371–378.
Miller, W. R., & Rollnick, S. (2002). Motivational interviewing: Preparing people to change (2nd ed.). New York: Guilford Press.
Milne, S., Sheeran, P., & Orbell, S. (2000). Prediction and intervention in health-related behavior: A meta-analytic review of protection motivation theory. Journal of Applied Social Psychology, 30 (1), 106.
Milne, S., Orbell, S., & Sheeran, P. (2002). Combining motivational and volitional interventions to promote exercise participation: Protection motivation theory and implementation intentions. British Journal of Health Psychology, 7 (Pt 2), 163–184.
Montaño, D. E., & Kasprzyk, D. (2008). Theory of reasoned action, theory of planned behavior and the integrated behavioral model. In K. Glanz, B. K. Rimer, & K. Viswanath (Eds.), Health behavior and health education (4th ed.). San Francisco: Jossey-Bass.
Moritz, S. E., Feltz, D. L., Fahrbach, K. R., & Mack, D. E. (2000). The relation of self-efficacy measures to sport performance: A meta-analytic review. Research Quarterly for Exercise and Sport, 71 (3), 280–294.
Morrison, V., & Bennett, P. (2008). An introduction to health psychology (2nd ed.). London: Pearson Publishing.
Mulvaney, S. A., Rothman, R. L., Wallston, K. A., Lybarger, C., & Dietrich, M. S. (2010). An internet-based program to improve self-management in adolescents with type 1 diabetes. Diabetes Care, 33 (3), 602–604.
Newman, I. M., Martin, G. L., & Ang, J. (1982). The role of attitudes and social norms in adolescent cigarette smoking. The New Zealand Medical Journal, 95 (715), 618–621.
Ni Mhurchu, C., Aston, L. M., & Jebb, S. A. (2010). Effects of worksite health promotion interventions on employee diets: A systematic review. BMC Public Health, 10 (62), 1.
Nichols, J., Schutte, N. S., Brown, R. F., Dennis, C. L., & Price, I. (2009). The impact of a self-efficacy intervention on short-term breast-feeding outcomes. Health Education & Behavior, 36 (2), 250–258.
Nigg, C. R., Albright, C., Williams, R., Nichols, C., Renda, G., Stevens, V. J., & Vogt, T. M. (2010). Are physical activity and nutrition indicators of the checklist of health promotion environments at worksites (CHEW) associated with employee obesity among hotel workers? Journal of Occupational and Environmental Medicine, 52 (Suppl. 1), S4–S7.
Noar, S. M., & Harrington, N. G. (2012). eHealth applications . New York: Routledge.
Noar, S. M., Benac, C. N., & Harris, M. S. (2007). Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin, 133 (4), 673–693.
Noar, S. M., Black, H. G., & Pierce, L. B. (2009). Efficacy of computer technology-based HIV prevention interventions: A meta-analysis. AIDS, 23 (1), 107.
Noar, S. M., Webb, E. M., Van Stee, S. K., Redding, C. A., Feist-Price, S., Crosby, R., & Troutman, A. (2011). Using computer technology for HIV prevention among African-Americans: Development of a tailored information program for safer sex (TIPSS). Health Education Research, 26 (3), 393–406.
Norman, G. J., Velicer, W. F., Fava, J. L., & Prochaska, J. O. (2000). Cluster subtypes within stage of change in a representative sample of smokers. Addictive Behaviors, 25 (2), 183.
Norman, P., Boer, H., & Seydel, E. R. (2005). Protection motivation theory. In M. Conner & P. Norman (Eds.), Predicting health behavior (pp. 81–126). London: Open University Press.
Norris, S. L., Engelgau, M. M., & Narayan, K. V. (2001). Effectiveness of self-management training in type 2 diabetes a systematic review of randomized controlled trials. Diabetes Care, 24 (3), 561–587.
Norris, S. L., Lau, J., Smith, S. J., Schmid, C. H., & Engelgau, M. M. (2002). Self-management education for adults with type 2 diabetes a meta-analysis of the effect on glycemic control. Diabetes Care, 25 (7), 1159–1171.
O’Leary, A. (1985). Self-efficacy and health. Behaviour Research and Therapy, 23 (4), 437.
Oei, T. P., & Burrow, T. (2000). Alcohol expectancy and drinking refusal self-efficacy: A test of specificity theory. Addictive Behaviors, 25 (4), 499–507.
Oenema, A., Brug, J., & Lechner, L. (2001). Web-based tailored nutrition education: Results of a randomized controlled trial. Health Education Research, 16 (6), 647–660.
Oostveen, T., Knibbe, R., & de Vries, H. (1996). Social influences on young adults’ alcohol consumption: Norms, modeling, pressure, socializing, and conformity. Addictive Behaviors, 21 (2), 187–197.
Orbell, S., & Sheeran, P. (1998). ‘Inclined abstainers’: A problem for predicting health-related behaviour. The British Journal of Social Psychology, 37 (Pt 2), 151–165.
Panday, S., Reddy, S. P., Ruiter, R. A., Bergström, E., & de Vries, H. (2005). Determinants of smoking cessation among adolescents in South Africa. Health Education Research, 20 (5), 586–599.
Parcel, G. S., Eriksen, M. P., Lovato, C. Y., Gottlieb, N. H., Brink, S. G., & Green, L. W. (1989). The diffusion of school-based tobacco-use prevention programs: Project description and baseline data. Health Education Research, 4 (1), 111.
Parker, R. M., & Jacobson, T. A. (2000). The role of health literacy in narrowing the treatment gap for hypercholesterolemia. The American Journal of Managed Care, 6 (12), 1340–1342.
Pelletier, K. R. (2009). A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: Update VII 2004–2008. Journal of Occupational and Environmental Medicine, 51 (7), 822–837.
Perry, C. L., Kelder, S. H., & Klepp, K. I. (1994). Community-wide cardiovascular disease prevention in young people: Long-term outcomes of the class of 1989 study. European Journal of Public Health, 4 (3), 188–194.
Perry, C. L., Williams, C. L., Veblen-Mortenson, S., Toomey, T. L., Komro, K. A., Anstine, P. S., McGovern, P. G., Finnegan, J. R., Forster, J. L., Wagenaar, A. C., & Wolfson, M. (1996). Project Northland: Outcomes of a communitywide alcohol use prevention program during early adolescence. American Journal of Public Health, 86 (7), 956–965.
Peters, L. W., Wiefferink, C. H., Hoekstra, F., Buijs, G. J., ten Dam, G. T., & Paulussen, T. G. (2009). A review of similarities between domain-specific determinants of four health behaviors among adolescents. Health Education Research, 24 (2), 198–223.
Peterson, A. V., Jr., Kealey, K. A., Mann, S. L., Marek, P. M., & Sarason, I. G. (2000). Hutchinson Smoking Prevention Project: Long-term randomized trial in school-based tobacco use prevention – Results on smoking. Journal of the National Cancer Institute, 92 (24), 1979–1991.
Petty, R. E., & Cacioppo, J. T. (1986). Communication and persuasion, central and peripheral routes to attitude change . New York: Springer.
Pinto, A. M., Heinberg, L. J., Coughlin, J. W., Fava, J. L., & Guarda, A. S. (2008). The Eating Disorder Recovery Self-Efficacy Questionnaire (EDRSQ): Change with treatment and prediction of outcome. Eating Behaviors, 9 (2), 143.
Plotnikoff, R. C., Lippke, S., Courneya, K. S., Birkett, N., & Sigal, R. J. (2008). Physical activity and social cognitive theory: A test in a population sample of adults with type 1 or type 2 diabetes. Applied Psychology, 57 (4), 628–643.
Plotnikoff, R. C., Lippke, S., Johnson, S. T., & Courneya, K. S. (2010a). Physical activity and stages of change: A longitudinal test in types 1 and 2 diabetes samples. Annals of Behavioral Medicine, 40 (2), 138–149.
Plotnikoff, R. C., Lippke, S., Trinh, L., Courneya, K. S., Birkett, N., & Sigal, R. J. (2010b). Protection motivation theory and the prediction of physical activity among adults with type 1 or type 2 diabetes in a large population sample. British Journal of Health Psychology, 15 (Pt 3), 643–661.
Pomp, S., Lippke, S., Fleig, L., & Schwarzer, R. (2010). Synergistic effects of intention and depression on action control: Longitudinal predictors of exercise after rehabilitation. Mental Health and Physical Activity, 2 , 78–84.
Presson, C. C., Chassin, L., Sherman, S. J., Olshavsky, R., Bensenberg, M., & Corty, E. (1984). Predictors of adolescents’ intentions to smoke: Age, sex, race, and regional differences. The International Journal of the Addictions, 19 (5), 503–519.
Elders, M. J. (1994). Preventing tobacco use among young people. A report of the Surgeon General. Executive summary. MMWR – Recommendations and Reports, 43 (RR-4), 1–10.
Price, V., & Zaller, J. (1993). Who gets the news? Alternative measures of news reception and their implications for research. Public Opinion Quarterly, 57 (2), 133.
Prochaska, J. O., & DiClemente, C. C. (1983). Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51 (3), 390–395.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change. American Journal of Health Promotion, 12 (1), 38–48.
Prochaska, J. O., Velicer, W. F., Rossi, J. S., Goldstein, M. G., Marcus, B. H., Rakowski, W., Fiore, C., Harlow, L. L., Redding, C. A., Rosenbloom, D., & Rossi, S. R. (1994). Stages of change and decisional balance for 12 problem behaviors. Health Psychology, 13 (1), 39–46.
Prochaska, J. O., Velicer, W. F., Redding, C., Rossi, J. S., Goldstein, M., DePue, J., Greene, G. W., Rossi, S. R., Sun, X., & Fava, J. L. (2005). Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammograms. Preventive Medicine, 41 (2), 406–416.
Prochaska, J. J., Spring, B., & Nigg, C. R. (2008). Multiple health behavior change research: An introduction and overview. Preventive Medicine, 46 (3), 181–188.
Puska, P. M., Puska, P. M. J., Barrueco, M., Roussos, C., Hider, A., & Hogue, S. (2005). The participation of health professionals in a smoking-cessation programme positively influences the smoking cessation advice given to patients. International Journal of Clinical Practice, 59 (4), 447–452.
Quinlan, K. B., & McCaul, K. D. (2000). Matched and mismatched interventions with young adult smokers: Testing a stage theory. Health Psychology, 19 (2), 165.
Rahimi, B., Timpka, T., Vimarlund, V., Uppugunduri, S., & Svensson, M. (2009). Organization-wide adoption of computerized provider order entry systems: A study based on diffusion of innovations theory. BMC Medical Informatics and Decision Making, 9 (1), 52.
Rakowski, W., Ehrich, B., Goldstein, M. G., Rimer, B. K., Pearlman, D. N., Clark, M. A., Velicer, W. F., & Woolverton III, H. (1998). Increasing mammography among women aged 40–74 by use of a stage-matched, tailored intervention. Preventive Medicine, 27 (5 Pt 1), 748–756.
Renner, B., Kwon, S., Yang, B.-H., Paik, K.-C., Kim, S. H., Roh, S., Song, J., & Schwarzer, R. (2008). Social-cognitive predictors of dietary behaviors in South Korean men and women. International Journal of Behavioral Medicine, 15 (1), 4–13.
Resnicow, K., & Vaughan, R. (2006). A chaotic view of behavior change: A quantum leap for health promotion. International Journal of Behavioral Nutrition and Physical Activity, 3 , 25.
Resnicow, K., DiIorio, C., Soet, J. E., Borrelli, B., Hecht, J., & Ernst, D. (2002). Motivational interviewing in health promotion: It sounds like something is changing. Health Psychology, 21 (5), 444.
Rigotti, N. A., Munafo, M. R., & Stead, L. F. (2008). Smoking cessation interventions for hospitalized smokers: A systematic review. Archives of Internal Medicine, 168 (18), 1950–1960.
Riper, H., Kramer, J., Smit, F., Conijn, B., Schippers, G., & Cuijpers, P. (2008). Web-based self-help for problem drinkers: A pragmatic randomized trial. Addiction, 103 (2), 218.
Rivis, A., & Sheeran, P. (2003). Descriptive norms as an additional predictor in the theory of planned behaviour: A meta-analysis. Current Psychology: Developmental, Learning, Personality, Social, 22 , 218–233.
Rogers, R. W. (1975). A protection motivation theory of fear appeals and attitude change. Journal of Psychology: Interdisciplinary and Applied, 91 (1), 93.
Rogers, R. W. (1983). Cognitive and physiological processes in fear appeals and attitude change: A revised theory of protection motivation. In J. T. Cacioppo & R. E. Petty (Eds.), Social psychophysiology . New York: Guilford Press.
Rogers, R. W. (2003). Diffusion of innovations (5th ed.). New York: Free Press.
Rohrbach, L. A., Grana, R., Sussman, S., & Valente, T. W. (2006). Type II translation: Transporting prevention interventions from research to real-world settings. Evaluation & the Health Professions, 29 (3), 302–333.
Rosenstock, I. (1974). Historical origins of the Health Belief Model. Health Education Monographs, 2 (4), 336.
Rosseel, J. P., Hilberink, S. R., Jacobs, J. E., Maassen, I. M., Plasschaert, A. J. M., & Grol, R. P. T. M. (2010). Are oral health complaints related to smoking cessation intentions? Community Dentistry and Oral Epidemiology, 38 (5), 470–478.
Ruiter, R. A., Kessels, L. T., Jansma, B. M., & Brug, J. (2006). Increased attention for computer-tailored health communications: An event-related potential study. Health Psychology, 25 (3), 300–306.
Rutter, D. R., Steadman, L., & Quine, L. (2006). An implementation intentions intervention to increase uptake of mammography. Annals of Behavioral Medicine, 32 (2), 127–134.
Salpeter, S. R., Buckley, N. S., Ormiston, T. M., & Salpeter, E. E. (2006). Meta-analysis: Effect of long-acting beta-agonists on severe asthma exacerbations and asthma-related deaths. Annals of Internal Medicine, 144 (12), 904–912.
Sarafino, E. P. (1994). Health psychology: Biopsychosocial interactions (2nd ed.). New York: Wiley.
Sarkar, U., Karter, A. J., Liu, J. Y., Adler, N. E., Nguyen, R., López, A., & Schillinger, D. (2011). Social disparities in internet patient portal use in diabetes: Evidence that the digital divide extends beyond access. Journal of the American Medical Informatics Association, 18 (3), 318–321.
Say, R. E., & Thomson, R. (2003). The importance of patient preferences in treatment decisions – Challenges for doctors. BMJ, 327 (7414), 542–545.
Schaalma, H., Kok, G., & Peters, L. (1993). Determinants of consistent condom use by adolescents: The impact of experience of sexual intercourse. Health Education Research, 8 (2), 255.
Schoenmakers, T., Wiers, R. W., & Field, M. (2008). Effects of a low dose of alcohol on cognitive biases and craving in heavy drinkers. Psychopharmacology, 197 (1), 169–178.
Schwarzer, R. (Ed.). (1992). Self-efficacy: Thought control of action . Washington, DC: Hemisphere.
Schwarzer, R. (2008a). Modeling health behavior change: The Health Action Process Approach (HAPA) . Available from: http://www.hapa-model.de/
Schwarzer, R. (2008b). Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology. An International Review, 57 (1), 1.
Schwarzer, R., Schüz, B., Ziegelmann, J. P., Lippke, S., Luszczynska, A., & Scholz, U. (2007). Adoption and maintenance of four health behaviors: Theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Annals of Behavioral Medicine, 33 (2), 156.
Schwarzer, R., Luszczynska, A., Ziegelmann, J. P., Scholz, U., & Lippke, S. (2008). Social-cognitive predictors of physical exercise adherence: Three longitudinal studies in rehabilitation. Health Psychology, 27 (Suppl. 1), S54.
Schwarzer, R., Lippke, S., & Luszczynska, A. (2011). Mechanisms of health behavior change in persons with chronic illness or disability: The Health Action Process Approach (HAPA). Rehabilitation Psychology, 56 (3), 161.
Segaar, D., Willemsen, M. C., Bolman, C., & De Vries, H. (2007a). Nurse adherence to a minimal-contact smoking cessation intervention on cardiac wards. Research in Nursing & Health, 30 (4), 429–444.
Segaar, D., Bolman, C., Willemsen, M. C., & De Vries, H. (2007b). Identifying determinants of protocol adoption by midwives: A comprehensive approach. Health Education Research, 22 (1), 14–26.
Senge, P. (1990). The fifth discipline: The art and practice of the learning organization . New York: Currency Doubleday.
Sheeran, P., & Orbell, S. (2000). Using implementation intentions to increase attendance for cervical cancer screening. Health Psychology, 19 (3), 283–289.
Sheeran, P., Webb, T. L., & Gollwitzer, P. M. (2005). The interplay between goal intentions and implementation intentions. Personality and Social Psychology Bulletin, 31 (1), 87–98.
Sherif, M. (1935). A study of some social factors in perception. Archives of Psychology, 187 .
Simonds, S. K. (1978). Health education: Facing issues of policy, ethics, and social justice. Health Education Monographs, 6 (Suppl. 1), 18–27.
Skår, S., Sniehotta, F. F., Molloy, G. J., Prestwich, A., & Araujo-Soares, V. (2011). Do brief online planning interventions increase physical activity amongst university students? A randomised controlled trial. Psychology & Health, 26 (4), 399–417.
Skinner, C. S., Sykes, R. K., Monsees, B. S., Andriole, D. A., Arfken, C. L., & Fisher, E. B. (1998). Learn, share, and live: Breast cancer education for older, urban minority women. Health Education & Behavior, 25 (1), 60–78.
Slovic, P. (1987). Perception of risk. Science, 236 (4799), 280–285.
Slovic, P., & Peters, E. (2006). Risk perception and affect. Current Directions in Psychological Science, 15 (6), 322–325.
Smeets, T., Brug, J., & de Vries, H. (2008). Effects of tailoring health messages on physical activity. Health Education Research, 23 (3), 402–413.
Smerecnik, C., Quaak, M., van Schayck, C. P., van Schooten, F. J., & de Vries, H. (2011). Are smokers interested in genetic testing for smoking addiction? A socio-cognitive approach. Psychology & Health, 26 (8), 1099–1112.
Sniehotta, F. F. (2009). Towards a theory of intentional behaviour change: Plans, planning, and self-regulation. British Journal of Health Psychology, 14 (2), 261.
Sniehotta, F. F., Scholz, U., Schwarzer, R., Fuhrmann, B., Kiwus, U., & Völler, H. (2005). Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. International Journal of Behavioral Medicine, 12 (4), 244–255.
Sniehotta, F. F., Scholz, U., & Schwarzer, R. (2006). Action plans and coping plans for physical exercise: A longitudinal intervention study in cardiac rehabilitation. British Journal of Health Psychology, 11 (Pt 1), 23–37.
Snyder, L. B., Hamilton, M. A., Mitchell, E. W., Kiwanuka-Tondo, J., Fleming-Milici, F., & Proctor, D. (2004). A meta-analysis of the effect of mediated health communication campaigns on behavior change in the United States. Journal of Health Communication, 9 (Suppl. 1), 71–96.
Soler, R. E., Leeks, K. D., Razi, S., Hopkins, D. P., Griffith, M., Aten, A., Chattopadhyay, S. K., Smith, S. C., Habarta, N., & Goetzel, R. Z. (2010). A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. American Journal of Preventive Medicine, 38 (2 Suppl), S237–S262.
Stock, J., & Cervone, D. (1990). Proximal goal-setting and self-regulatory processes. Cognitive Therapy and Research, 14 (5), 483–498.
Strack, F., & Deutsch, R. (2004). Reflective and impulsive determinants of social behavior. Personality and Social Psychology Review, 8 (3), 220.
Strecher, V. J. (1999). Computer-tailored smoking cessation materials: A review and discussion. Patient Education and Counseling, 36 (2), 107–117.
Strecher, V. J., & Rosenstock, I. M. (1997). The Health Belief Model. In A. Baum et al. (Eds.), Cambridge handbook of psychology, health and medicine . Cambridge: Cambridge University Press.
Strecher, V. J., McEvoy DeVellis, B., Becker, M. H., & Rosenstock, I. M. (1986). The role of self-efficacy in achieving health behavior change. Health Education Quarterly, 13 (1), 73–92.
Strecher, V. J., Kreuter, M., Den Boer, D. J., Kobrin, S., Hospers, H. J., & Skinner, C. S. (1994). The effects of computer-tailored smoking cessation messages in family practice settings. The Journal of Family Practice, 39 (3), 262–270.
Strecher, V. J., Shiffman, S., & West, R. (2005). Randomized controlled trial of a web-based computer-tailored smoking cessation program as a supplement to nicotine patch therapy. Addiction, 100 (5), 682–688.
Strecher, V. J., McClure, J. B., Alexander, G. L., Chakraborty, B., Nair, V. N., Konkel, J. M., Greene, S. M., Collins, L. M., Carlier, C. C., & Wiese, C. J. (2008). Web-based smoking-cessation programs: Results of a randomized trial. American Journal of Preventive Medicine, 34 (5), 373–381.
Suissa, S., & Ernst, P. (2001). Inhaled corticosteroids: Impact on asthma morbidity and mortality. The Journal of Allergy and Clinical Immunology, 107 (6), 937–944.
Sutton, S. (2000). Interpreting cross-sectional data on stages of change. Psychology and Health, 15 (2), 163–171.
Swinburn, B., Egger, G., & Raza, F. (1999). Dissecting obesogenic environments: The development and application of a framework for identifying and prioritizing environmental interventions for obesity. Preventive Medicine, 29 (6 Pt 1), 563–570.
Taylor, S. E., Falke, R. L., Shoptaw, S. J., & Lichtman, R. R. (1986). Social support, support groups, and the cancer patient. Journal of Consulting and Clinical Psychology, 54 (5), 608–615.
Te Poel, F., Bolman, C., Reubsaet, A., & de Vries, H. (2009). Efficacy of a single computer-tailored e-mail for smoking cessation: Results after 6 months. Health Education Research, 24 (6), 930–940.
Thomas, R. (2002). School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews, 4 , CD001293.
Thomas, R., & Perera, R. (2013). School-based programmes for preventing smoking. Cochrane Database of Systematic Reviews, 4 , CD001293.
Thurstone, L. L. (1931). Measurement of social attitudes. Journal of Abnormal and Social Psychology, 26 , 249–269.
Tichenor, P. J., Donohue, G. A., & Olien, C. N. (1970). Mass media flow and differential growth in knowledge. Public Opinion Quarterly, 34 .
Tu, H. T., & Cohen, G. R. (2008). Striking jump in consumers seeking health care information. Tracking Report, 20 , 1–8.
Turner, J. C. (1991). Social influence . Belmont: Wadsworth Publishing.
Tyler-Smith, K. (2006). Early attrition among first time eLearners: A review of factors that contribute to drop-out, withdrawal and non-completion rates of adult learners undertaking eLearning programmes. Journal of Online Learning and Teaching, 2 , 73–85.
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of Behavioral Medicine, 29 (4), 377.
USDHHS. (1980). Promoting health/preventing disease: Objectives for the nation . Washington, DC: US Government Printing Office.
USDHHS. (1990). The health benefits of smoking cessation. A report of the Surgeon General’s Office on Smoking and Health . Rockville: U.S. Govt. Printing Office.
Valente, T. W. (2002). Evaluating health promotion programs . New York: Oxford University Press.
van der Velde, F. W., Hooykaas, C., & van der Pligt, J. (1996). Conditional versus unconditional risk estimates in models of AIDS-related risk behaviour. Psychology & Health, 12 (1), 87.
van Keulen, H. M., Mesters, I., Ausems, M., Van Breukelen, G., Campbell, M., Resnicow, K., Brug, J., & De Vries, H. (2011). Tailored print communication and telephone motivational interviewing are equally successful in improving multiple lifestyle behaviors in a randomized controlled trial. Annals of Behavioral Medicine, 41 (1), 104–118.
van Osch, L., Reubsaet, A., Lechner, L., & de Vries, H. (2008a). The formation of specific action plans can enhance sun protection behavior in motivated parents. Preventive Medicine, 47 (1), 127–132.
van Osch, L., Reubsaet, A., Lechner, L., Candel, M., Mercken, L., & De Vries, H. (2008b). Predicting parental sunscreen use: Disentangling the role of action planning in the intention-behavior relationship. Psychology and Health, 23 (7), 829–846.
van Osch, L., Lechner, L., Reubsaet, A., & De Vries, H. (2010). From theory to practice: An explorative study into the instrumentality and specificity of implementation intentions. Psychology & Health, 25 (3), 351–364.
van Stralen, M. M., Kok, G., de Vries, H., Mudde, A. N., Bolman, C., & Lechner, L. (2008). The Active plus protocol: Systematic development of two theory-and evidence-based tailored physical activity interventions for the over-fifties. BMC Public Health, 8 (1), 399.
Vartiainen, E., Puska, P., Koskela, K., Nissinen, A., & Toumilehto, J. (1986). Ten-year results of a community-based anti-smoking program (as part of the North Karelia Project in Finland). Health Education Research, 1 (3), 175–184.
Vassallo, M., Saba, A., Arvola, A., Dean, M., Messina, F., Winkelmann, M., Claupein, E., Lähteenmäki, L., & Shepherd, R. (2009). Willingness to use functional breads. Applying the Health Belief Model across four European countries. Appetite, 52 (2), 452.
Velicer, W. F., Diclemente, C. C., Rossi, J. S., & Prochaska, J. O. (1990). Relapse situations and self-efficacy: An integrative model. Addictive Behaviors, 15 (3), 271–283.
Velicer, W. F., Prochaska, J. O., Bellis, J. M., DiClemente, C. C., Rossi, J. S., Fava, J. L., & Steiger, J. H. (1993). An expert system intervention for smoking cessation. Addictive Behaviors, 18 (3), 269–290.
Velicer, W. F., Prochaska, J. O., & Redding, C. A. (2006). Tailored communications for smoking cessation: Past successes and future directions. Drug and Alcohol Review, 25 (1), 49–57.
Vernon, S. W. (1999). Risk perception and risk communication for cancer screening behaviors: A review. Journal of the National Cancer Institute. Monographs, 25 , 101–119.
Verplanken, B., & Faes, S. (1999). Good intentions, bad habits, and effects of forming implementation intentions on healthy eating. European Journal of Social Psychology, 29 (5-6), 591.
Vries, H. D., & Mudde, A. N. (1998). Predicting stage transitions for smoking cessation applying the attitude-social influence-efficacy model. Psychology and Health, 13 (2), 369–385.
Wagner, T. H., Bundorf, M. K., Singer, S. J., & Baker, L. C. (2005). Free internet access, the digital divide, and health information. Medical Care, 43 (4), 415–420.
Webb, T. L., & Sheeran, P. (2006). Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychological Bulletin, 132 (2), 249–268.
Webb, T. L., Joseph, J., Yardley, L., & Michie, S. (2010). Using the internet to promote health behavior change: A systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of Medical Internet Research, 12 (1), e4.
Weinstein, N. D. (1988). The precaution adoption process. Health Psychology, 7 (4), 355–386.
Weinstein, N. D., & Sandman, P. M. (1992). A model of the precaution adoption process: Evidence from home radon testing. Health Psychology, 11 (3), 170–180.
Weinstein, N. D., Lyon, J. E., Sandman, P. M., & Cuite, C. L. (1998). Experimental evidence for stages of health behavior change: The precaution adoption process model applied to home radon testing. Health Psychology, 17 (5), 445.
WHO. (1978). Declaration of Alma-Ata . International conference on Primary Health Care, Alma-Ata, USSR, 6–12 September. Geneva: WHO.
WHO. (1985). Prerequisites for health. In WHO Regional Office of Europe (Ed.), Targets for all: Targets in support of the European regional strategy for health for all . Copenhagen: WHO Regional Office of Europe.
WHO. (1986). Ottawa charter of health promotion . In Health promotion I , Ottawa.
U.S. Department of Health and Human Services. (2000). Healthy people 2010: Understanding and improving health (2nd ed.). Washington, DC: U.S. Government Printing Office.
WHO. (2013). In J. M. Pelikan, I. Kickbusch, F. Apfel, & A. D. Tsouros (Eds.), Health literacy; solid facts .
WHO, [WHO definition of Health]. (1946). Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference , New York, 19–22 June 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no. 2, p. 100) and entered into force on 7 April 1948.
Wielm, A. G. (2004). Digital Nation: Towards an inclusive information society (pp. 133–134). Cambridge, MA: MIT Press.
Wiers, R. W., Bartholow, B. D., van den Wildenberg, E., Thush, C., Engels, R. C. M. E., Sher, K. J., Grenard, J., Ames, S. L., & Stacy, A. W. (2007). Automatic and controlled processes and the development of addictive behaviors in adolescents: A review and a model. Pharmacology, Biochemistry, and Behavior, 86 (2), 263–283.
Wiers, R. W., Rinck, M., Kordts, R., Houben, K., & Strack, F. (2009). Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction, 105 (2), 279–287.
Wilde, M. H., & Garvin, S. (2007). A concept analysis of self-monitoring. Journal of Advanced Nursing, 57 (3), 339–350.
Wilson, M. G., Holman, P. B., & Hammock, A. (1996). A comprehensive review of the effects of worksite health promotion on health-related outcomes. American Journal of Health Promotion, 10 (6), 429–435.
Winett, L. B., & Wallack, L. (1996). Advancing public health goals through the mass media. Journal of Health Communication, 1 (2), 173–196.
Ziegelmann, J. P., Lippke, S., & Schwarzer, R. (2006). Adoption and maintenance of physical activity: Planning interventions in young, middle-aged, and older adults. Psychology & Health, 21 (2), 145–163.
Ziegelmann, J. P., Luszczynska, A., Lippke, S., & Schwarzer, R. (2007). Are goal intentions or implementation intentions better predictors of health behavior? A longitudinal study in orthopedic rehabilitation. Rehabilitation Psychology, 52 (1), 97.
Download references
Author information
Authors and affiliations.
Department of Health Promotion, Maastricht University, Maastricht, The Netherlands
Hein de Vries & Stef P. J. Kremers
Department of Psychology and Methods, Bremen International Graduate School of Social Sciences, Jacobs University Bremen, Bremen, Germany
Sonia Lippke
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hein de Vries .
Editor information
Editors and affiliations.
Department of Health Behavior, Gillings School of Global Public Health, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA
Edwin B. Fisher
Psychological Sciences, University of California, Merced, Merced, CA, USA
Linda D. Cameron
Department of Psychological and Brain Sciences and Department of Internal Medicine, The University of Iowa, Iowa City, IA, USA
Alan J. Christensen
Department of Clinical Psychology and Psychotherapy, University of Zurich, Zürich, Switzerland
Ulrike Ehlert
School of Public Health, Peking University Health Science Center, Beijing, China
Melbourne School of Population and Global Health, University of Melbourne, Melbourne, Australia
Brian Oldenburg
Departments of Medical Psychology, Academic Medical Center (AMC) and VU University Medical Center (VUMC), Amsterdam, The Netherlands
Frank J. Snoek
Rights and permissions
Reprints and permissions
Copyright information
© 2018 Springer Science+Business Media LLC
About this chapter
de Vries, H., Kremers, S.P.J., Lippke, S. (2018). Health Education and Health Promotion: Key Concepts and Exemplary Evidence to Support Them. In: Fisher, E., et al. Principles and Concepts of Behavioral Medicine. Springer, New York, NY. https://doi.org/10.1007/978-0-387-93826-4_17
Download citation
DOI : https://doi.org/10.1007/978-0-387-93826-4_17
Published : 09 October 2018
Publisher Name : Springer, New York, NY
Print ISBN : 978-0-387-93825-7
Online ISBN : 978-0-387-93826-4
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

COMMENTS
Professionals teach people how to maintain and restore their health. In other words, health does not merely refer to physical but also mental, social and sexual health. Health education aims to enhance health literacy and develop skills in people which will help them maintain good health.
This article describes a framework and empirical evidence to support the argument that educational programs and policies are crucial public health interventions. Concepts of education and health are developed and linked, and we review a wide range of empirical studies to clarify pathways of linkage and explore implications.
Health Education is the education that health professionals impart for healthcare. Health education is very crucial in limiting the spread of diseases. Health educators promote hygiene and healthy diet by organising campaigns.
Health and education. For healthy, happy and thriving learners. Education has the power to transform the lives of children and young people, and the world around them. At UNESCO, inclusive and transformative education starts with healthy, happy and safe learners.
How is education a social determinant of health? Explore how Tulane University’s Master of Public Health prepares graduates to address factors impacting health.
Education and health care significantly influence well-being and health outcomes, especially throughout adolescence. In fact, doctors note that performance in school is highly reflective of a child's current and future health.
Reducing health disparities and improving citizen health can be accomplished only through a thorough understanding of the health benefits conferred by education. There is an iterative relationship between education and health.
While health education is the process of educating people about health and how they can influence their health, health promotion targets not only people but also their environments.
Health education is the process of teaching people about their health and how to protect it. Health education can take many different forms, from teaching people about diseases and health risks to providing information on healthy eating and lifestyles.
Education is strongly associated with life expectancy, morbidity, health behaviours, and educational attainment plays an important role in health by shaping opportunities, employment, and income. In this issue of The Lancet Public Health, two research Articles emphasise the lifelong impact of education on health.