- Resume Builder
- Resume Templates
- Resume Formats
- Resume Examples
- Cover Letter Builder
- Cover Letter Templates
- Cover Letter Formats
- Cover Letter Examples
- Career Advice
- Interview Questions
- Resume Skills
- Resume Objectives
- Job Description
- Job Responsibilities
- FAQ’s

Utilization Management Nurse Resume Examples
If you are a Utilization Management Nurse looking to create a strong and effective resume, you have come to the right place! Utilization Management Nurses are responsible for performing assessments of medical care and wellness, as well as providing advocacy and recommendations to ensure quality of care. They must possess a deep understanding of patient needs, treatments, and health care processes. A successful Utilization Management Nurse resume should showcase your skills, qualifications, and experience. This guide will provide you with tips and examples on how to write an effective and persuasive Utilization Management Nurse resume that will help you stand out from the competition.
If you didn’t find what you were looking for, be sure to check out our complete library of resume examples .
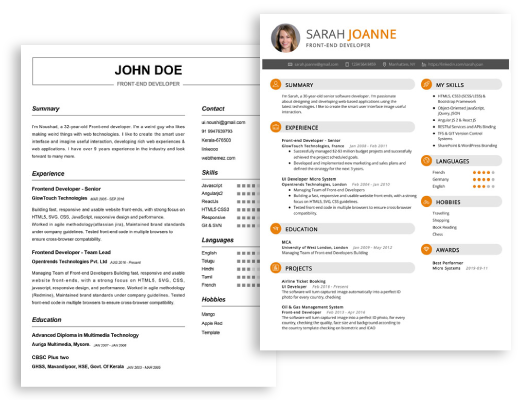
Start building your dream career today!
Create your professional resume in just 5 minutes with our easy-to-use resume builder!
Utilization Management Nurse
123 Main Street | Anytown, USA 99999 | Phone: (123) 456-7890 | Email: [email protected]
I am a highly experienced Utilization Management Nurse with over four years of clinical experience in both inpatient and outpatient settings. I have expertise in utilizing evidence- based practices to ensure the highest quality of care for patients, as well as identifying and addressing potential utilization issues. I am skillful in working with other healthcare professionals to ensure patients receive the most effective and appropriate care and I have a proven track record of success in reducing costs while maintaining quality care.
Core Skills :
- Clinical expertise in utilization management
- Knowledge of evidence- based practices
- Ability to educate and evaluate appropriate treatment plans
- Proven track record of success in reducing costs while maintaining quality care
- Excellent communication and interpersonal skills
- Proficiency in ICD- 10, CPT, and HCPCS coding
Professional Experience : Utilization Management Nurse ABC Healthcare, Florida October 2016 – Present
- Utilize evidence- based practices and current medical information to ensure the quality of care provided to patients
- Review and approve/deny requests for services or treatments in accordance with health plan criteria
- Collaborate with other healthcare professionals to ensure appropriate utilization of services and resources
- Educate patients about treatment plans and coordinate with providers to ensure continuity of care
- Monitor and analyze utilization trends to evaluate overall effectiveness of services
- Identify any potential utilization issues or gaps in care
Utilization Review Nurse XYZ Healthcare, Florida June 2015 – October 2016
- Evaluated treatment plans for appropriateness, medical necessity and coverage guidelines
- Monitored treatments to ensure adherence to plan of care and authorization criteria
- Analyzed utilization trends to evaluate overall effectiveness of services
- Assessed and reported any potential utilization issues or gaps in care
- Educated patients and providers on utilization review processes and guidelines
Education : Master of Science in Nursing University of Florida, FL 2013- 2015
Create My Resume
Build a professional resume in just minutes for free.
Utilization Management Nurse Resume with No Experience
Motivated and highly organized Utilization Management Nurse with no experience. Proven track record in providing high- level patient care, as well as experience in administrative duties. Adept at quickly assessing patient needs and formulating plans of care through communication with interdisciplinary team members.
- Critical thinking
- Attention to detail
- Computer proficiency
- Multitasking
- Excellent communication
- Problem solving
- Knowledge of medical terminology
Responsibilities
- Review medical records for accuracy and completeness
- Perform initial evaluation of patient records and make determination on appropriateness of care
- Ensure patients receive appropriate care in accordance with established standards and regulations
- Develop and implement utilization review plans for specific patient populations
- Monitor utilization patterns and identify trends that may require additional interventions
- Coordinate with physicians and other healthcare providers to ensure appropriate care is provided
- Ensure documentation is accurate and complete in the patient’s electronic medical record
- Participate in quality improvement efforts to improve the delivery of healthcare services
Experience 0 Years
Level Junior
Education Bachelor’s
Utilization Management Nurse Resume with 2 Years of Experience
Dedicated Utilization Management Nurse with 2 years of experience in the healthcare field. Skilled in assessing and monitoring the utilization of healthcare services and resources. Possess a strong ability to coordinate with providers and other healthcare professionals to ensure that patient care is cost- effective and meets the standards of quality. Adept in managing utilization review systems, interpreting and evaluating guidelines, and providing education to healthcare professionals on utilization management best practices.
- Utilization Management
- Medical Terminology
- Interdisciplinary Collaboration
- Quality Assurance
- Patient Care Coordination
- Regulatory Compliance
- Documentation
- Policy Implementation
Responsibilities :
- Coordinate clinical review activities to ensure the appropriateness and effectiveness of services provided to the patient
- Monitor and evaluate utilization review of services to ensure compliance with regulations and standards
- Analyze medical records and clinical documentation to identify potential utilization problems and recommend cost- effective solutions
- Provide education and training to healthcare professionals on utilization management best practices
- Collaborate with interdisciplinary teams to ensure that services provided to the patient meet their needs
- Ensure that all documentation is accurate and in compliance with applicable regulations and standards
- Develop and implement utilization management policies to ensure cost- effectiveness of services
Experience 2+ Years
Utilization Management Nurse Resume with 5 Years of Experience
A Utilization Management Nurse with 5 years of experience providing assessments of the appropriateness and efficacy of care provided in an inpatient setting. Extensive knowledge of risk management, patient safety, and clinical standards of care. Proven ability to analyze patient’s medical records, make clinical determinations, and provide recommendations to support cost- effective care.
- Utilization management
- Patient assessments
- Clinical decision making
- Risk management
- Patient safety
- Medical record analysis
- Cost- effective care
- Evaluated patient medical records to assess the appropriateness and efficacy of inpatient care
- Evaluated and documented medical necessity of inpatient stay
- Identified potential utilization opportunities, variances, and over/under utilization
- Monitored quality, efficiency, and effectiveness of care delivered
- Made clinical and financial determinations based on medical record analysis and medical necessity criteria
- Developed and implemented cost- effective care plans to promote patient safety and quality of care
- Collaborated with healthcare team to ensure quality patient care and compliance with government regulations
Experience 5+ Years
Level Senior
Utilization Management Nurse Resume with 7 Years of Experience
Utilization Management Nurse with 7 years of experience in managing and evaluating patient care services, providing utilization review and promoting cost- effective health care and quality patient outcomes.
- Quality Assessments
- Patient Care Management
- Medical Record Review
- Care Planning
- Health Insurance Benefits
- Critical Thinking
- Conducted utilization review of patient care services and developed individualized plans of care to ensure quality outcomes and cost effectiveness
- Assessed patients’ health status and provided appropriate guidance, counseling, and follow- up for care plan
- Reviewed inpatient and outpatient medical records to ensure compliance with all applicable regulations
- Worked collaboratively with providers and health insurance companies to maximize coverage benefits
- Developed and implemented protocols for utilization management and quality assessments
- Monitored utilization trends across multiple clinical settings and patient populations
- Evaluated medical necessity of services to ensure patient care was medically necessary and met the standards of care
- Participated in multidisciplinary team meetings to coordinate patient care and facilitate communication between physicians and other health care providers
Experience 7+ Years
Utilization Management Nurse Resume with 10 Years of Experience
Utilization Management Nurse with over 10 years of experience in healthcare. Experienced in reviewing utilization of healthcare services, identifying trends and opportunities for improvement, and increasing efficiency. Skilled in developing strategies for utilization management, overseeing quality assurance initiatives, and reviewing patient records and medical documents. Committed to providing the best possible care to patients and helping healthcare providers provide the highest quality services.
- Patient Record Review
- Medical Document Review
- Clinical Practice Guidelines
- Healthcare Compliance
- Inter- professional Collaboration
- Data Analysis
- Report Writing
- Review utilization of healthcare services and identify trends and opportunities for improvement
- Develop strategies for utilization management, such as case management protocols, guidelines, and programs
- Oversee quality assurance initiatives to ensure compliance with clinical practice guidelines and healthcare laws and regulations
- Review patient medical records and documents to evaluate the necessity and appropriateness of services
- Collaborate with interdisciplinary teams to support efficient and effective delivery of care
- Analyze data to identify areas for improvement and inform decisions related to utilization management
- Prepare reports to communicate utilization management results and recommendations to healthcare providers and other stakeholders
Experience 10+ Years
Level Senior Manager
Education Master’s
Utilization Management Nurse Resume with 15 Years of Experience
Utilization Management Nurse with 15 years of experience in utilization management, managed care, and healthcare administration. Skilled in assessing the medical necessity of admissions and claims to ensure regulatory and contractual compliance. Experienced in developing and implementing denials or pre- authorizations for inpatient and outpatient services.
- Managed care
- Health care administration
- Authorization and denials
- Regulatory and contractual compliance
- Data analysis
- Insurance guidelines
- Complex case management
- Collaboration with healthcare team
- Record keeping
- Assessed medical necessity of admissions and claims
- Developed and implemented denials or pre- authorizations for inpatient and outpatient services
- Conducted data analysis and risk management
- Developed and implemented clinical policies and procedures
- Monitored utilization trends and projected utilization
- Assisted with complex case management and insurance guidelines
- Collaborated with other healthcare team members to determine appropriate level of care
- Kept detailed and accurate records of all treatment and services provided
Experience 15+ Years
Level Director
In addition to this, be sure to check out our resume templates , resume formats , cover letter examples , job description , and career advice pages for more helpful tips and advice.
What should be included in a Utilization Management Nurse resume?
Utilization Management Nurses play a vital role in helping healthcare organizations ensure quality care and services are provided to their patients. As such, a well-crafted resume that clearly showcases your experience, knowledge, and skills can make a difference in your job search. To help you stand out from the crowd, here are some key elements that you should consider including in your Utilization Management Nurse resume:
- Professional Summary: A brief summary of your skills, experience, and qualifications as a Utilization Management Nurse.
- Education: A list of all relevant academic credentials, including certifications and licenses.
- Work Experience: A detailed list of your past roles, with a focus on the utilization management duties and responsibilities you have performed.
- Skills: The capabilities and knowledge that you have acquired in your role, such as risk assessment and case management.
- Clinical Experience: Any clinical experiences that you have that relate to utilization management, including patient education and discharge planning.
- Professional Accomplishments: Any awards, recognition, or other accomplishments you have achieved in your field.
- Relevant Volunteer Experience: If applicable, any volunteer work that you have completed that is related to utilization management.
- Professional Memberships: Any relevant professional associations that you are a member of.
By including all these elements in your Utilization Management Nurse resume, you will be sure to make a great impression to potential employers. Good luck with your job search!
What is a good summary for a Utilization Management Nurse resume?
A Utilization Management Nurse resume should include a summary which highlights the nurse’s experience in patient care, care coordination and utilization management. This summary should include details such as the nurse’s educational qualifications and certifications, their experience in utilization management, and the areas of patient care the nurse is most knowledgeable about. It should also include details about how the nurse’s utilization management skills can benefit the organization. Additionally, the summary should demonstrate the nurse’s commitment to providing quality patient care and their ability to collaborate with other healthcare professionals. Finally, the resume should include an overview of any recognition the nurse has received for their excellent performance in utilization management, such as awards or accolades.
What is a good objective for a Utilization Management Nurse resume?
A Utilization Management Nurse is responsible for helping improve patient care while managing healthcare costs. This role is key to ensuring health systems are fiscally sound while still providing quality care. To stand out when applying for this role, your resume should demonstrate your understanding of the basics of Utilization Management and show that you are a results-driven professional.
When you write your Utilization Management Nurse resume objective, be sure to include the following:
- Demonstrate an understanding of the basic principles of Utilization Management
- Demonstrate an ability to review patient records and provide accurate documentation
- Demonstrate excellent communication and problem-solving skills
- Demonstrate an ability to effectively negotiate and collaborate with healthcare providers
- Demonstrate a commitment to providing quality patient care while managing healthcare costs
- Demonstrate an ability to stay organized and meet tight deadlines
- Demonstrate a dedication to professional development and lifelong learning.
How do you list Utilization Management Nurse skills on a resume?
The role of a Utilization Management Nurse requires an extensive skill set. When creating a resume, it is important to list relevant skills to showcase your experience and abilities. Here are some potential skills you can list on a resume as a Utilization Management Nurse:
- Knowledge of health care policies and regulations
- Understanding of the principles of Utilization Management
- Ability to review and manage medical records
- Excellent problem-solving skills
- Ability to analyze data and make evidence-based decisions
- Proficiency in medical coding and billing
- Attention to detail and accuracy
- Proficiency in using electronic systems and software
- Ability to collaborate with multi-disciplinary teams
- Ability to work independently and handle multiple tasks
- Time management and organizational skills
- Commitment to patient safety and satisfaction
What skills should I put on my resume for Utilization Management Nurse?
When you are writing your resume as a Utilization Management Nurse, it is important to focus on the skills that are most relevant to the position. Utilization Management Nurses are responsible for assessing patient care plans to ensure that they are effective and cost-efficient. In order to be successful in this role, you must possess certain skills and qualifications. Here are some of the most important skills to include in your resume for a Utilization Management Nurse role.
- Knowledge of Utilization Management: A Utilization Management Nurse should have an in-depth understanding of the Utilization Management process. This includes understanding how provider networks and managed care plans function, and how to assess patient care plans and make recommendations.
- Excellent Interpersonal Skills: As a Utilization Management Nurse, you will be working closely with patients, care providers, and insurers. You must have strong interpersonal skills to be able to communicate effectively with all parties involved.
- Problem-Solving Ability: You must have the ability to think critically and analyze data in order to make informed decisions. Utilization Management Nurses must be able to identify potential issues and develop solutions to address them.
- Documentation Skills: As a Utilization Management Nurse, you need to have strong documentation skills. You must be able to accurately document patient information, care plans, and recommendations in order to ensure that the processes run smoothly.
- Computer Skills: The ability to use computers and navigate electronic medical records will be an important skill for a Utilization Management Nurse. You should also be proficient in Microsoft Office and other software programs used in healthcare.
By including these skills on your resume, you will demonstrate to potential employers that you have the qualifications and expertise to be successful in a Utilization Management Nurse role.
Key takeaways for an Utilization Management Nurse resume
When crafting a resume for an Utilization Management Nurse position, there are a few key takeaways you should keep in mind. First, include any certifications or specializations that you have acquired during your nursing career. This could include certifications in disease management, case management, utilization management, or any other relevant certifications. Additionally, be sure to list any specific experience you have in working with utilization management, such as developing protocols or handling appeals.
Secondly, emphasize any professional affiliations or volunteer work that you have participated in, as this can demonstrate your commitment to the field of utilization management. Finally, make sure to emphasize any software and analytics skills that you may have acquired. This could include working with data-driven software systems or analytics tools. With these key takeaways in mind, you can create a strong resume for an Utilization Management Nurse position.
Let us help you build your Resume!
Make your resume more organized and attractive with our Resume Builder
100+ Nursing Resume Objective Examples + How To Write

Whether you are a new nurse graduate or a nurse with years of experience, applying for a new nursing job can feel a little overwhelming. One of the most important things you can do is prepare a great resume. If you plan to create a resume, you may have wondered, “What are some great nursing resume objective examples?” Nursing resume objectives are important parts of resumes. In this article, I will share 100+ great nursing resume objective examples + how to write them.
What Exactly is a Nursing Resume Objective?
When should you include an objective on your nursing resume, 5 reasons why a great nursing resume objective makes a difference.
1. A great nursing resume objective gives nurses the opportunity to make a good first impression. 2. A well-written objective on a nursing resume helps demonstrate your written communication skills, which are vital for nursing success. 3. A nursing resume objective can show prospective employers how you have cultivated your career. 4. Resume objectives are an excellent way to briefly showcase your experience. 5. Great Nursing resume objectives offer excellent opportunities to show confidence in your knowledge and skills.
How to Write a Great Nursing Resume Objective?
1. keep it simple:, 2. tell how many years of experience you have:, 3. state the position you want:, 4. mention the facility:, 5. describing yourself:, 6. action verbs are important:, 7. mention hard skills:, 8. mention the type of patients you hope to work with:, 9. mention personal goals which clarify your love for nursing and the role for which you are applying:, 10. mention your degrees/title:, nursing resume objective examples by level of experience, entry-level nursing examples, intermediate-level nursing examples, senior-level nursing examples, nursing resume objective examples by job title, crna examples, clinical nurse specialist examples, er nurse examples, nicu nurse examples, nurse practitioner examples, or nurse examples, pacu nurse examples, aesthetic nurse examples, charge nurse examples, director of nursing examples, flight nurse examples, float nurse examples, home health nurse examples, hospice nurse examples, icu nurse examples, interventional radiology nurse examples, labor and delivery nurse examples, med surg nurse examples, nurse case manager examples, nurse educator examples, nurse manager examples, nurse midwife examples, nursing informatics examples, nursing leadership examples, nursing supervisor examples, oncology nurse examples, pediatric nurse examples, plastic surgery nurse examples, psychiatric nurse examples, school nurse examples, staff nurse examples, stepdown nurse examples, telemetry nurse examples, travel nurse examples, utilization review nurse examples, nursing resume objective examples by situation, nursing internship, career change to nursing, nurse moving to a new geographic area, nurse seeking an advancement, nurse restarting career after a break, 10 bad examples of nursing resume objectives, 1. bad example:, what makes it bad:, 2. bad example:, 3. bad example:, 4. bad example:, 5. bad example:, 6. bad example:, 7. bad example:, 8. bad example:, 9. bad example:, 10. bad example:, my final thoughts, frequently asked questions answered by our expert, 1. what is the difference between nursing resume objective and resume summary, 2. for a nursing job, what is more important, a resume objective or a resume summary, 3. where do i put an objective on my nursing resume, 4. how long should my objective for nursing resume be, 5. do i need a different resume objective for each nursing job i apply to, 6. how often should i update my objective for nursing resume, 7. how much time does it take to write a great objective for nursing resume, 8. how do i submit my nursing resume objective, 9. is it okay if i don’t write an objective for nursing resume.

Career Advice > Job Search > Resumes and Cover Letters > Utilization Review Nurse Resume Writing Tips and Sample
Utilization Review Nurse Resume Writing Tips and Sample
Search resource center.

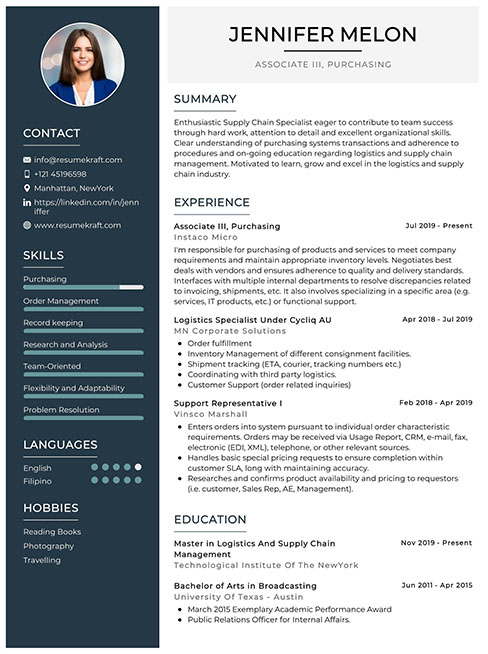
As a utilization review nurse , you’re a silent architect of healthcare, working behind the scenes to ensure resources are used efficiently and patients receive the care they deserve. These nurses are all about finding that perfect balance between resourcefulness and top-notch care, nurturing the hospital’s sustainable growth, and ensuring continuous improvement in patient care. Note that this position is often available as a remote job .
In order to get into this field, you need a strong utilization review nurse resume and cover letter . A great resume is key to standing out and earning the opportunity for an interview . Don’t forget to check out our resume sample for an extra boost of inspiration.
Tips for Writing Utilization Nurse Resumes
1. prioritize important information.
Have you ever heard about the elevator pitch ? If you were to meet the employer of your dreams in an elevator and only had 30 seconds to showcase your qualifications, what would you say? Think about what sets you apart and make it stand out. Employers scanning through hundreds of resumes won’t have time to uncover your hidden talents in the sea of words. Put your strengths in your resume summary to get the reader’s attention.
2. Quantify Your Experience
It’s beneficial to back up everything you say in your resume with numbers. Saying, “I am an exceptional nurse,” is less informative than stating, “I am a registered nurse with 10 years of experience.” Therefore, support statements with concrete evidence whenever possible. How many years of experience do you have? What is your typical patient load? How many times have you been promoted?
3. Use Similar Wording
Here’s the deal — many companies use computer programs to scan resumes for matching keywords. If you don’t pass that screening, the hiring manager may not even see your resume. To pass this test, customize your resume by using keywords from the job posting. If they’re seeking a utilization review nurse, stick to the term “utilization review,” not “UR nurse.”
4. Personalize Your Resume
Many people think resumes are generic — you create one and mass-send it to all employers out there. But the truth is, generic resumes often go unnoticed. Use those keywords we talked about to customize your resume for each job by adding a personal touch — small adjustments can make a big difference.
Utilization Review Nurse Resume Sample
Dinah roven, rn, hum.
Mountain Street, CA | [email protected] | 444-444-4444
Dedicated and skilled utilization review nurse with over 10 years of experience. Proven track record of efficiently managing and optimizing healthcare resources to ensure quality patient care.
Key Qualifications
- Proven track record in utilization review and case management.
- Clinical expertise as a registered nurse in acute care and med-surg settings.
- In-depth understanding of healthcare regulations and compliance, and proficient in insurance guidelines and reimbursement processes.
- Proficient in working with EHR systems to maintain accurate and detailed patient records.
Mountain University , San Diego, CA, 20XX
Bachelor of Science in Nursing
Professional Experience
Reputable Hospital, Utilization Review Nurse, 20XX–present
- Conducted comprehensive reviews of medical records to assess the appropriateness and necessity of healthcare services.
- Evaluate medical documentation for compliance with regulatory requirements and insurance guidelines.
- Develop and implement care plans based on individual patient needs and available resources.
- Provide recommendations for improving care delivery processes and cost-effectiveness.
Great Hospital, Float Pool Nurse, 20XX–20XX
- Provided expert care to patients in the 150-bed critical care hospital, managing a high caseload.
- Worked in various departments, including medical-surgical, critical care, and emergency.
- Administered life-saving interventions, such as advanced cardiac life support (ACLS) and trauma care.
- Maintained accurate and detailed medical records in compliance with regulatory standards.
- Utilization review and case management
- Clinical assessment and documentation
- Healthcare regulations and compliance
- Strong analytical and problem-solving skills
- Language comprehension: English, Russian, and German
- Software proficiency: Cortex, PowerChart, Epic, Cerner, WebPT
Certifications and Licenses
- Basic life support (BLS)
- Advanced cardiovascular life support (ACLS)
- Registered nurse (RN)
- Health utilization management (HUM)
Utilization Review Nurse Salary
Wondering what utilization review nurses typically earn? The average salary for a utilization review RN in the U.S. is $90,700 per year.
Looking for the highest-paying states for nurses? These states have some of the most competitive salaries in the country:
Ready to Use Your Utilization Review Nurse Resume?
Well done! You’ve conquered the challenges of becoming a nurse and writing a top-notch resume. Now, let IntelyCare help with the rest. Explore the latest utilization review nurse jobs and find the ones that match your skills and interests.
Latest Jobs
Medical assistant – endocrinology clinic at fairview health services, registered nurse rn – medical oncology office at ascension, wound care coordinator rn full time at scionhealth, pre-op/pacu rn – full time at surgery partners, registered nurse iii special procedures (per diem) at valley hospital medical center, related articles, pmhnp resume writing tips and sample, nurse educator cover letter writing tips and sample, nurse educator resume writing tips and sample, home health nurse resume writing tips and sample, pcu nurse resume writing tips and sample, related jobs.
- Software Developer
- Quality Assurance
- Software Teacher
- Software Nurse
- Software Accountant
- Software Marketing Specialist
Utilization Review Nurse Resume Example & Writing Guide
Share this page
Utilization review nurse resume sample, professional summary.
Diligent Utilization Review Nurse with 5 years of experience reviewing medical records to ensure compliance with insurance standards, while promoting the most effective use of healthcare resources. Demonstrated ability to communicate with interdisciplinary healthcare teams to develop and implement care plans that meet patient needs, improve outcomes and reduce costs.
Utilization Review Nurse
ABC Healthcare, Anytown USA
May 2020 - Present
- Conducted utilization review of medical records for inpatient and outpatient services to assess and evaluate quality and effectiveness of care
- Collaborated with interdisciplinary healthcare teams to create and implement care plans that meet patient needs, improve outcomes and reduce costs
- Communicated with insurance providers to confirm approvals, resolve denials, and ensure appropriate patient care
- Educated healthcare providers on utilization management procedures, compliance with insurance standards, and medical necessity criteria
Registered Nurse
XYZ Hospital, Anytown USA
August 2015 - May 2020
- Monitored and assessed patient conditions, administered medications, and assisted with activities of daily living
- Collaborated with interdisciplinary healthcare teams to develop and implement care plans that meet patient needs and improve outcomes
- Educated patients and families on discharge instructions and self-care to support optimal recovery
- Documented patient care and outcomes in electronic health records
Bachelor of Science in Nursing
State University, Anytown USA
Graduated May 2015
Keep It Concise
Recruiters spend an average of 6 seconds reviewing an individual resume. Keep yours concise and to the point. Aim for one to two pages maximum for most jobs.
Utilization Review Nurse Resume Writing Guide
Introduction:.
If you are looking to apply for the position of a utilization review nurse, then it is important to have a well-crafted resume that highlights your skills, education, and experience. This type of nursing job is competitive, so putting together the best résumé possible is essential in order to stand out from other applicants.
1. Create a Professional Summary:
The first section of your resume should be a professional summary that outlines your skills, experience, and career objective. Keep this section brief, but make sure to include any relevant information that will help you stand out from other applicants.
- Highlight your nursing qualifications and certifications
- Include your areas of expertise
- Outline any relevant work experience
- Explain your goals and what makes you the ideal candidate for the job
2. List your Professional Experience:
The next section of your resume should list your professional experience. This includes your work history as a utilization review nurse, or any other similar nursing experience that would be relevant to the job. Be sure to include the following:
- The name of your previous employer and job title
- Your start and end dates of employment
- Key responsibilities and duties for each job
- Any relevant achievements or accomplishments
3. Highlight your Skills:
List your skills in a separate section of your resume. Utilization review nursing requires a blend of skills and knowledge, so be sure to highlight the ones that make you an excellent candidate:
- Strong analytical and critical thinking skills
- Effective communication skills
- Attention to detail and organizational skills
- Good time management skills to work under strict deadlines
- Ability to work both independently and as part of a team
- Knowledge of electronic medical records (EMRs) and medical terminology
- Familiarity with CMS guidelines, medical coding, and regulations
4. Include your Education and Certifications:
The final section of your resume should list your education and relevant certifications. This should include:
- The name of the universities or institutions you have attended
- Your degree type and major
- Your GPA (if you are a recent graduate)
- Any relevant certifications that you have received, such as Certified Professional Utilization Review Nurse (CPUR) or Certification in Healthcare Quality (CHC)
Conclusion:
A well-written resume is essential for getting noticed by hiring managers and landing a job as a utilization review nurse. Highlighting your skills and experience using the tips outlined above, will help you create a compelling resume that showcases your professional strengths and makes you stand out from other candidates.
Common Resume Writing Mistake
Typos and grammatical errors.
These types of errors indicate a lack of attention to detail and might give an impression of carelessness. Always proofread your resume multiple times and consider having someone else review it as well.
Resume Examples You May Interested

Create resume online now to take the first step towards career success
CVBLADE developed by hiring professionals. With our resume builder, applying for your dream job is easy and fast.
- ResumeBuild
- Utilization Review Nurse
5 Amazing utilization review nurse Resume Examples (Updated 2023) + Skills & Job Descriptions

Build your resume in 15 minutes
Utilization review nurse: resume samples & writing guide, employment history.
- Participate in quality assurance activities
- Monitor patient care for quality and appropriateness of services
- Develop and maintain utilization review policies and procedures
- Review medical records to ensure that services are medically necessary
- Document all utilization review activities in accordance with regulations
- Facilitate discharge planning and coordinate care transitions
- Collaborate with physicians, case managers, and other members of the healthcare team
- Evaluate the need for continued care and recommend appropriate changes
Do you already have a resume? Use our PDF converter and edit your resume.
- Educate providers and other staff on utilization review processes
- Develop utilization review plans and ensure compliance with regulations
- Verify insurance coverage and authorization for services
Professional Summary
- Provide clinical expertise in the review of medical services
- Perform concurrent and retrospective review of medical services
- Analyze and interpret utilization data to identify trends and cost savings opportunities
- Communicate findings and recommendations to appropriate parties
Not in love with this template? Browse our full library of resume templates

Table of Content
- Introduction
- Resume Samples & Writing Guide
- Resume Example 1
- Resume Example 2
- Resume Example 3
- Resume Example 4
- Resume Example 5
- Jobs Description
- Jobs Skills
- Technical Skills
- Soft Skills
- How to Improve Your Resume
- How to Optimize Your Resume
- Cover Letter Example
utilization review nurse Job Descriptions; Explained
If you're applying for an utilization review nurse position, it's important to tailor your resume to the specific job requirements in order to differentiate yourself from other candidates. Including accurate and relevant information that directly aligns with the job description can greatly increase your chances of securing an interview with potential employers. When crafting your resume, be sure to use action verbs and a clear, concise format to highlight your relevant skills and experience. Remember, the job description is your first opportunity to make an impression on recruiters, so pay close attention to the details and make sure you're presenting yourself in the best possible light.
utilization review nurse
- Review individual records and conduct utilization reviews for precertification, continued stay and discharge.
utilization review nurse Job Skills
For an utilization review nurse position, your job skills are a key factor in demonstrating your value to the company and showing recruiters that you're the ight fit for the role. It's important to be specific when highlighting your skills and ensure that they are directly aligned with the job requirements, as this can greatly improve your chances of being hired. By showcasing your relevant skills and experience, you can make a compelling case for why you're the best candidate for the job.
How to include technical skills in your resume:
Technical skills are a set of specialized abilities and knowledge required to perform a particular job effectively. Some examples of technical skills are data analysis, project management, software proficiency, and programming languages, to name a few. Add the technical skills that will get hired in your career field with our simple-to-use resume builder. Select your desired resume template, once you reach the skills section of the builder, manually write in the skill or simply click on "Add more skills". This will automatically generate the best skills for your career field, choose your skill level, and hit "Save & Next."
- Medical Terminology
- Clinical Documentation
- ICD-10 Coding
- Medical Record Review
- Clinical Assessment
- Utilization Management
- Quality Assurance
- Disease Management
- HIPAA Compliance
- Chart Auditing
- Computer Proficiency
- Regulatory Compliance
- Risk Management
- Healthcare Regulations
- Medical Billing
- Claims Processing
- Patient Advocacy
- Healthcare Reimbursement
- Insurance Verification.
How to include soft skills in your resume:
Soft skills are non-technical skills that relate to how you work and that can be used in any job. Including soft skills such as time management, creative thinking, teamwork, and conflict resolution demonstrate your problem-solving abilities and show that you navigate challenges and changes in the workplace efficiently. Add competitive soft skills to make your resume stand-out to recruiters! Simply select your preferred resume template in the skills section, enter the skills manually or use the "Add more skills" option. Our resume builder will generate the most relevant soft skills for your career path. Choose your proficiency level for each skill, and then click "Save & Next" to proceed to the next section.
- Communication
- Interpersonal
- Time Management
- Problem Solving
- Decision Making
- Critical Thinking
- Adaptability
- Organization
- Public Speaking
- Negotiation
- Conflict Resolution
- Attention to Detail
- Self-Motivation
- Stress Management
- Collaboration
- Strategic Thinking
- Emotional Intelligence
- Flexibility
- Reliability
- Professionalism
- Computer Literacy
- Data Analysis
- Project Management
- Customer Service
- Presentation
- Written Communication
- Social Media
- Troubleshooting
- Supervisory
- Database Management
- Documentation
- Financial Management
- Visualization
- Business Acumen
- Process Improvement
- Relationship Management.
How to Improve Your utilization review nurse Resume
Navigating resume pitfalls can mean the difference between landing an interview or not. Missing job descriptions or unexplained work history gaps can cause recruiters to hesitate. Let's not even talk about the impact of bad grammar, and forgetting your contact info could leave your potential employer hanging. Aim to be comprehensive, concise, and accurate.
Unexplained Year Gaps and Missing Job Experiences are a No-no
Gaps in your resume can prevent recruiters from hiring you if you don't explain them..
- It's okay to have gaps in your work experience but always offer a valid explanation instead of just hiding it.
- Use the gap to talk about positive attributes or additional skills you've learned.
- Be honest and straightforward about the gap and explain it using a professional summary.
How to Optimize Your utilization review nurse Resume
Keep an eye out for these resume traps. Neglecting to detail your job roles or explain gaps in your career can lead to unnecessary doubts. Grammar blunders can reflect negatively on you, and without contact information, how can employers reach you? Be meticulous and complete.
- Facilitate discharge planing, and coordiante care transtions.
- Perform concurrent, and retrospective review of medical servies.
- Verfiy insurance coverage, and authoriztion for servies.
- Perform concurrent and retrospectiv review of medical services
- Educate providers and other staff on utilizaiton review processes
- Proivde clinical expertise in the review of medical services
- Evaluate the need for continued care, and recommend appropriate changs.
- Facillitate discharge planning, and co-ordinate care transitions.
- Develop utilisation review plans, and ensurre compliance with regulatons.
Avoid Spelling Mistakes and Include your Contact Information
Missing contact information prevents recruiters from understanding you're the best fit for the position..
- Make sure you're not missing contact information on your resume. That should include your full name, telephone number and email address.
- Make sure to use a professional email address as part of your contact information.
- Highlight your contact information and double check that everything is accurate to help recruiters get in touch with you.
utilization review nurse Cover Letter Example
A cover letter can be a valuable addition to your job application when applying for an utilization review nurse position. Cover letters provide a concise summary of your qualifications, skills, and experience, also it also gives you an opportunity to explain why you're the best fit for the job. Crafting a cover letter that showcases your relevant experience and enthusiasm for the Accounts Payable role can significantly improve your chances of securing an interview.
To the Hiring Team at NYU Langone Health
I am excited to apply for the Chief Utilization Review Nurse position at NYU Langone Health. As a highly skilled Utilization Review Nurse with 7 years of experience in the Medical field, I am confident that I can contribute significantly to your organization.
My life experiences have taught me the importance of hard work, dedication, and collaboration. Whether it was on the work, or just personally, I have always been committed to pursuing my goals with passion and tenacity. I am confident that throughout all of these years I have gained the skills and expertise necessary to succeed in this role and be a great asset for NYU Langone Health. I am eager to join a team that shares my values and work towards a common goal.
I cannot stress enough how thrilled I am about the chance to join a team of like-minded individuals who share my values and passion for this amazing field. Thank you for considering my application and I hope for the chance to work together.
Showcase your most significant accomplishments and qualifications with this cover letter. Personalize this cover letter in just few minutes with our user-friendly tool!
Related Resumes & Cover Letters
Contemporary
Professional
Looking to explore other career options within the Medical field?
Check out our other resume of resume examples.
- Psychiatrist Resume
- Psychologist Resume
- Nurse Resume
- Lab Assistant Resume
- Medical Assistant Resume
- Medical Technologist Resume
- Dental Assistant Resume
- Dentist Resume
FIND EVERYTHING YOU NEED HERE.
IF YOU HAVE QUESTIONS, WE HAVE ANSWERS.

4 Ways a Career Test Can Jump-Start Your Future (and Help Your Resume)
If you’re looking for a fresh path or a new passion, a career test could help you find it. You can take these tests online, in the comfort of your...

Avoid These 3 Resume Mistakes at All Costs
Your resume is your first impression for a prospective employer. The way you present yourself in that little document can make or break you – it can clinch you an...

Resume Design Tips and Tricks
Creating a resume that stands out from the rest doesn’t have to be rocket science. With just a few tips and tricks, you can make your professional resume a shining...

Build your Resume in 15 minutes
- ResumeBuilderPro
- Resume Examples
- Utilization Review Nurse
Utilization Review Nurse resume examples
A modern resume example for a Utilization Review Nurse position. Based on the best resume writing practices.
- No experience
- Specialized
Average Utilization Review Nurse Salary
What is the pay by experience level for utilization review nurse, career paths.
Explore the most common career paths for Utilization Review Nurse. Thickness and color of lines indicates popularity of movement from one job to the next. Visit our career path planner to research other job paths.
- Licensed Practical Nurse (LPN) View salaries
- Utilization Management (UM) Nurse Reviewer View salaries
- Registered Nurse (RN), Utilization Review (UR) View salaries
Try our resume builder today!
Save time with our easy 3-step resume builder. No more writer’s block or formatting difficulties in Word. Rapidly make a perfect resume employers love.
Pro guidelines and recommendations for a successful Utilization Review Nurse job curriculum vitae.
Overcome each of the rivals with your properly relevant resume. Include all of the applicable details relating to your skills in the sphere and shape it with important and action phrases. Make use of the pro advice on Utilization Review Nurse CV displayed on our web page to inevitably acquire the employment in Healthcare.
Dominant Key Skills and Action Verbs for Utilization Review Nurse
Do you know the top specifics helping a Healthcare CV differentiate itself from the rest? Certainly, the firm's human resources professional will analyze your Utilization Review Nurse CV as reported by the overview of professional capabilities and employment aims you demonstrate in the resume. For that reason, spend some time to develop the best description of your skills - a few examples of most common experience and achievements and are accessible in our forms: mental health, intravenous therapy, acute care expertise. patient care plans, parkinson's disease knowledge, acute rehabilitation.
Key Skills & Proficiencies
Action verbs, utilization review nurse curriculum vitae phrases to adopt.
If you are planning to have the job of a Utilization Review Nurse, be prepared to invest a regular time to your own resume. In most cases, the more connected to the position an applicant's competencies are, the more odds they'll have the job. Look at all possibly practical skills to include in the resume that keep to the job standards - several most beneficial key words and capabilities for your CV are given in our list: data entry, managed care, scheduling.
Phrases To Use
Best utilization review nurse resume objective examples.
To maximize the percentages of attaining the employment as a Utilization Review Nurse, describe all of the skill sets and qualities in relation to the industry of Healthcare you've obtained and add the statement at the beginning of your ideal job CV.
How To Use Resume Examples To Create A Job-winning Resume
Introduction.
It is no longer news that you need to submit a professional resume if you want to improve your chances of getting the job you crave. In this article, you will find out how resume examples can help you with this challenging task. Over the years, statistics have shown that many job seekers find the act of resume writing difficult. Creating resumes that can win you the job you desire can be challenging, especially if you are writing your first resume. However, thanks to the emergence of information technology, you can now say goodbye to the struggles that come with crafting a resume from scratch. Now, there are a wide variety of tested and proven job-winning online resume samples on different resume builders available for you to choose from. This makes it much easier for you to write resumes that will convince hiring managers to give you the job. As you keep reading this article, you will find answers to the following questions:
- What are Resume Examples?
How do I create my own resume with Resume Examples?
How do professional resume examples work, why do we suggest using resume examples, what are the things i should pay attention to when searching for a resume example, can i edit resume examples according to my needs.
Let's get right into the details!
What are Resume Samples?
As the name implies, they are ideal examples of what resumes in different industries look like. For instance, they provide you with suitable resume structures and recommended details to include in your resume. Additionally, they also show you the most effective way to portray your skills and experience to your potential employer. With the aid of these samples, you can create your resume faster and boost your chances of getting the job that you crave. This is why we have gone all out to show you how you can use them to edge out your competition (other job seekers). You will also discover some key details about resumes. Read on!
If you want to prove to your potential employers that you are the perfect fit for a vacant position, you need to create a perfect resume or cover letter. However, there is good news. You don't need to rack your brain to write a job-winning resume. All you have to do is visit a reliable online resume builder, follow a few simple steps, and best. These resume builders give you access to many ideal examples of industry-related resumes you can easily refer to when creating yours. Resume samples provide you with the perfect guide you need to craft a readable and relevant resume. Here is how you can use them to create your own resume:
- Choose samples with resume formats suitable for a specific job or industry.
- Observe how the names and contact information are included and follow suit
- Include your resume objective or summary, following the pattern
- Take a look at how the skills are highlighted and do the same
- Get keywords from the sample and use them in your own resume
- Mention your education using the structure in the example
- Pay attention to the font style and use the same when creating your resume
- Make sure you proofread your resume to confirm if it aligns with the sample you used
After doing this, you can rest assured that you have created a professional resume.
Before explaining how these examples work, let's clear air. They should not be mistaken for resume templates that are ready-made document format designed to help job-seekers portray their career achievements, skills, education, and work experience to their potential employers in an organized and attractive way. Now, the purpose of an example is to provide you with sufficient context, general best practices, and insight on what a resume for a specific industry looks like. Once you have an idea about how writing a specific or targeted resume works, you can improve the way you write your resume. This is how they work in helping you achieve your goals of writing a job-winning resume.
Here's why we recommend you use them:
- Makes writing a top-notch resume Easier
Most of them are written by resume experts
- Helps you to avoid the mistakes most job seekers make
Saves you time
Makes writing a top-notch resume easier.
Writing a professional resume is easier when you use a resume example. It's no longer a hidden secret that some job seekers know little to nothing about creating a resume or cover letter. If you fall under this category, that's no problem at all. Not everyone is great at putting words on paper. So, don't feel bad because you struggle with this aspect. It isn't all doom and gloom.
Here's what you can do to make things better:
Look for samples of resumes related to the industry or position you are applying for and use them as a guide when writing yours. This will improve your ability to write a job-winning resume quickly.
When you use them, you are simply following a laid-down blueprint on the right way to write a resume suitable for any industry. This is because the options you will find on resume builders are crafted by resume experts. These experts possess vast knowledge about the do's and don'ts when it comes to writing a resume. They understand perfectly well what hiring managers look out for when they screen job resumes. For this reason, they ensure that the examples they make available to you on the resume builders are easy to read and well-formatted. They make it possible for you to draw the attention of any employer to your skills, experiences, and accomplishments. You can be sure that writer's block is a thing of the past when you use them as your guide. And the best part is this — you will be able to create a resume that will leave a lasting impression on your potential employers.
Helps you to avoid the mistakes that most job seekers make
One way to avoid the mistakes that most job seekers make is to use a guide for writing resumes. According to experts' opinions, most job seekers make spelling and grammatical errors. In the eyes of your potential employers, these mistakes are red flags that can prevent you from getting the job you crave. Using examples to create your own resume can help you cut out mistakes because you need to pay attention to every detail. By doing this, you can avoid the errors your competitors will likely make in their resumes. This gives you the upper hand.
Writing a resume from scratch takes a lot of time. But it gets better when you use samples because you get to save yourself a few minutes or hours of brain-racking. All you have to do is find a resume ideal for the industry of your choosing and use it to your advantage. Besides saving you time, you won't need to go through as much stress as you would have if you had to start from scratch.
Making a decision to use examples when crafting your resume is one step in the right direction. But before you settle for an example, here are a few things you should consider during your search:
- Ensure they are industry-related resume
- The resume format (Chronological, Functional, or Combination Resume Format). Make sure it is the perfect fit for the position you are applying for.
When it comes to resume writing, you control the situation completely. It is up to you to create a great resume that is well-suited to a particular position or industry. You can use this opportunity to transform your previous job experience into a sensation and catch the eye of your potential employers. If you want to pull this off easily, you can edit samples of resumes. The sole purpose of an example is to provide you with the right context required to craft a resume for a certain industry or job title. Every tip, resume format, or phrase you will find is designed to help you target industries specifically and show your worth. It helps you to prove to your employers that you are a professional who understands the demands of a position and the goal of the company. With the aid of this guide, you can easily draw the attention of the company's management to your skills, dedication, knowledge, and expertise. Regardless of the industry, you plan to begin or continue your career in, there is an example available for you to use. This implies that if you want to impress employers in industries like Information Technology, Real Estate Management, Accounting, and many others, there is one for you to edit according to your needs. No one is left out.
Final Words
So far, we have shared with you all you need to know when using these helpful tools to create your resume. It's now up to you to use all we have shown and explained to you to your advantage. Remember, although writing a great resume can be tasking, you can rest assured that if you use samples on industry-related resumes the writing experience will be much easier. We wish you success in your job hunting.
Targeting other Healthcare? See one of our examples:
- Veterinary Receptionist
- Wound Care Nurse
- ABI Companion
- Activities Assistant
- Activity Aide
- Acupuncturist
Most popular Resume Examples:
Learn from people who have succeeded in their job hunt
- Proofreader
- Software Engineering Manager
- Software Architect
- Commercial Real Estate Broker
- Lab Assistant
- Surgical Technologist
- Clinical Assistant
- Geriatric Nurse
- Home Care Provider
- Orthopedic Surgeon
- Education and Training
- Community and Public Service
Explore Jobs
- Jobs Near Me
- Remote Jobs
- Full Time Jobs
- Part Time Jobs
- Entry Level Jobs
- Work From Home Jobs
Find Specific Jobs
- $15 Per Hour Jobs
- $20 Per Hour Jobs
- Hiring Immediately Jobs
- High School Jobs
- H1b Visa Jobs
Explore Careers
- Business And Financial
- Architecture And Engineering
- Computer And Mathematical
Explore Professions
- What They Do
- Certifications
- Demographics
Best Companies
- Health Care
- Fortune 500
Explore Companies
- CEO And Executies
- Resume Builder
- Career Advice
- Explore Majors
- Questions And Answers
- Interview Questions

Utilization Review Nurse resume examples for 2024
A strong utilization review nurse resume should highlight the ability to verify medical records and authorization requests, conduct clinical reviews, and manage patient care documentation. It's also important to showcase experience with various medical codes and criteria, such as Interqual and CPT. As seen in the examples, a utilization review nurse resume should also demonstrate the ability to interact with patients, medical professionals, and insurance providers, while maintaining knowledge of community resources and HIPAA regulations.

Utilization Review Nurse resume example
How to format your utilization review nurse resume:.
- Use the job title 'Utilization Review Nurse' on your resume to match the application.
- Tailor your work experience to emphasize achievements that demonstrate your ability to determine medical necessity, utilize InterQual criteria, and improve processes.
- Limit your resume to one page, focusing on relevant experience and accomplishments that showcase your expertise as a Utilization Review Nurse.
Choose from 10+ customizable utilization review nurse resume templates
Choose from a variety of easy-to-use utilization review nurse resume templates and get expert advice from Zippia’s AI resume writer along the way. Using pre-approved templates, you can rest assured that the structure and format of your utilization review nurse resume is top notch. Choose a template with the colors, fonts & text sizes that are appropriate for your industry.

Utilization Review Nurse resume format and sections
1. add contact information to your utilization review nurse resume.
Utilization Review Nurse Resume Contact Information Example # 1
Dhruv Johnson
[email protected] | 333-111-2222 | www.linkedin.com/in/dhruv-johnson
2. Add relevant education to your utilization review nurse resume
Your resume's education section should include:
- The name of your school
- The date you graduated ( Month, Year or Year are both appropriate)
- The name of your degree
If you graduated more than 15 years ago, you should consider dropping your graduation date to avoid age discrimination.
Optional subsections for your education section include:
- Academic awards (Dean's List, Latin honors, etc. )
- GPA (if you're a recent graduate and your GPA was 3.5+)
- Extra certifications
- Academic projects (thesis, dissertation, etc. )
Other tips to consider when writing your education section include:
- If you're a recent graduate, you might opt to place your education section above your experience section
- The more work experience you get, the shorter your education section should be
- List your education in reverse chronological order, with your most recent and high-ranking degrees first
- If you haven't graduated yet, you can include "Expected graduation date" to the entry for that school
Check More About Utilization Review Nurse Education
Utilization Review Nurse Resume Relevant Education Example # 1
Master's Degree In Nursing 2000 - 2001
Grand Canyon University Phoenix, AZ
Utilization Review Nurse Resume Relevant Education Example # 2
Bachelor's Degree In Nursing 2003 - 2006
Miami Dade College Miami, FL
3. Next, create a utilization review nurse skills section on your resume
Your resume's skills section should include the most important keywords from the job description, as long as you actually have those skills. If you haven't started your job search yet, you can look over resumes to get an idea of what skills are the most important.
Here are some tips to keep in mind when writing your resume's skills section:
- Include 6-12 skills, in bullet point form
- List mostly hard skills ; soft skills are hard to test
- Emphasize the skills that are most important for the job
Hard skills are generally more important to hiring managers because they relate to on-the-job knowledge and specific experience with a certain technology or process.
Soft skills are also valuable, as they're highly transferable and make you a great person to work alongside, but they're impossible to prove on a resume.
Example of skills to include on an utilization review nurse resume
The branch of secondary healthcare which is responsible for giving short-term care to patients recovering from severe injuries or urgent medical problems is known as acute care. Acute care comprises multiple domains like; emergency care, urgent care, short-term stabilization, pre-hospital care, critical care, and trauma care.
Another name for utilization review is utilization management. It is the process of ensuring that healthcare services are used in a suitable manner. Utilization review is a critical component of adding value to the health care system. Mostly, UR is carried out by healthcare insurance companies, but hospitals and other healthcare providers also perform the process. Utilization review has three types of assessment namely: concurrent, prospective, and retrospective.
Community resources are a set of resources that are used in the day to day life of people which improves their lifestyle in some way. People, sites or houses, and population assistance can come under the services offered by community resources.
Clinical knowledge is defined as the complete body of information about diseases, pathology, treatments, drugs, mechanisms, pathogenesis, therapies, interactions, contraindications, and interpretation of lab tests and reports which is helpful in devising a diagnosis and treatment plan for a given patient.
Patient care entails the diagnosis, recovery, and control of sickness as well as the maintenance of physical and emotional well-being through the use of healthcare providers' services. Patient care is described as services provided to patients by health practitioners or non-professionals under guidance.
CPT is a medical term that stands for Current Procedural Terminology. Whenever a procedure like surgery or diagnosis occurs or some other medical service is rendered to a patient, it is reported to the concerned physician, insurance company, or organization. The aforementioned practice is widely referred to as CPT.
Top Skills for a Utilization Review Nurse
- Medical Necessity , 9.0%
- Patients , 7.4%
- Acute Care , 7.4%
- Discharge Planning , 7.2%
- Other Skills , 69.0%
4. List your utilization review nurse experience
The most important part of any resume for a utilization review nurse is the experience section. Recruiters and hiring managers expect to see your experience listed in reverse chronological order, meaning that you should begin with your most recent experience and then work backwards.
Don't just list your job duties below each job entry. Instead, make sure most of your bullet points discuss impressive achievements from your past positions. Whenever you can, use numbers to contextualize your accomplishments for the hiring manager reading your resume.
It's okay if you can't include exact percentages or dollar figures. There's a big difference even between saying "Managed a team of utilization review nurses" and "Managed a team of 6 utilization review nurses over a 9-month project. "
Most importantly, make sure that the experience you include is relevant to the job you're applying for. Use the job description to ensure that each bullet point on your resume is appropriate and helpful.
- Facilitated delivery of evidence-based nursing care in the Northern Virginia Region.
- Researched/recommended alternative items to contracts.
- Promoted learning environment for all team members and maintained standards of efficiency and cost effectiveness.
- Led training for new hire nurses to the phone triage call center for monthly hires between 2-12 nurses.
- Assigned all UM NCQA standards for internal auditing and preparation of our NCQA 3rd submission for accreditation.
- Managed three NIH funded studies including development and design of educational interventions for patients and caregivers.
- Provided HIV and STD counseling, testing, and treatment.
- Reviewed protocols submitted to OCR to determine if a PRA was required.
- Reviewed study protocols for financial and resource feasibility.
- Analyzed VINCI database to determine progression of diabetes.
- Established successful account relationships with physicians and pharmacist; building rapport and maintaining consistent communication.
- Ensured HIPAA compliance and also, schedule doctors appointments for patients.
- Communicated residents' concerns with doctors and facilitated resolution of these issues.
- Provided excellence in customer service with internal and external customers resulting in heightened customer satisfaction.
- Answered multiple phone lines and triage patient calls.
- Assisted the Investigator in the conduct of research in accordance with the statement of Investigator (Form FDA 1572/Investigator Agreement).
- Obtained clinical information using IRB protocol standards and consulted with the principal investigator regarding the study.
- Worked with investigators and coordinators in completing regulatory files.
- Mentored a team of seven Innovation Project Managers located across the country.
- Acted as Field Clinical Engineer at implant procedures and follow-up visits in the absence of the assigned FCE.
5. Highlight utilization review nurse certifications on your resume
Specific utilization review nurse certifications can be a powerful tool to show employers you've developed the appropriate skills.
If you have any of these certifications, make sure to put them on your utilization review nurse resume:
- Certified Case Manager (ACM)
- Legal Nurse Consultant Certified (LNCC)
- Medical Assistant
- Certified Nurse Assistant (CNA)
- Certified Nurse Technician (CNT)
- Certified Managed Care Nurse (CMCN)
- Certified Gastroenterology Licensed Vocational/Practical Nurse (LPN/LVN)
- Medical-Surgical Nursing (RN-BC)
- Certified Nurse Educator (CNE)
- Family Nurse Practitioner
6. Finally, add an utilization review nurse resume summary or objective statement
A resume summary statement consists of 1-3 sentences at the top of your utilization review nurse resume that quickly summarizes who you are and what you have to offer. The summary statement should include your job title, years of experience (if it's 3+), and an impressive accomplishment, if you have space for it.
Remember to emphasize skills and experiences that feature in the job description.
Common utilization review nurse resume skills
- Medical Necessity
- Discharge Planning
- Utilization Management
- Utilization Review
- Community Resources
- Outpatient Services
- Clinical Knowledge
- Home Health
- Patient Care
- Medical Directors
- Clinical Judgment
- Medical Care
- Clinical Review
- Chart Review
- Proactive Planning
- Social Work
- Concurrent Review
- Health Care Services
- Inpatient Admissions
- Health Plan
- Interqual Criteria
- Retrospective Reviews
- Clinical Documentation
- Excellent Interpersonal
- Data Collection
- Medical Services
- Rehabilitation
- Strong Computer
- Medical Policy
- Physician Review
- Medical Claims
- Clinical Criteria
- Clinical Guidelines
Utilization Review Nurse Jobs
Links to help optimize your utilization review nurse resume.
- How To Write A Resume
- List Of Skills For Your Resume
- How To Write A Resume Summary Statement
- Action Words For Your Resume
- How To List References On Your Resume
Utilization Review Nurse resume FAQs
What are the responsibilities of a utilization review nurse, what is utilization in nursing, what nursing skills should be listed on a resume, search for utilization review nurse jobs.
Updated June 25, 2024
Editorial Staff
The Zippia Research Team has spent countless hours reviewing resumes, job postings, and government data to determine what goes into getting a job in each phase of life. Professional writers and data scientists comprise the Zippia Research Team.
- Zippia Careers
- Healthcare Practitioner and Technical Industry
- Utilization Review Nurse
- Utilization Review Nurse Resume
Browse healthcare practitioner and technical jobs
Utilization Review Nurse Resume Sample
The resume builder.
Create a Resume in Minutes with Professional Resume Templates
Work Experience
- Refers treatment plans/plan of care to peer clinical reviewers in accordance with established criteria/guidelines and does not issue medical necessity non-certifications
- Current active unrestricted license or certification to practice as a health professional within the scope of licensure in the State of TN required
- Conducts pre-certification, inpatient, retrospective, out of network and appropriateness of treatment setting reviews within scope of licensure by utilizing appropriate medical policies and clinical guidelines in compliance with department guidelines and consistentwith the member's eligibility, benefits and contract
- Applies clinical knowledge to work with facilities and providers for care-coordination
- Current active unrestricted license or certification to practice as a health professional within the scope of licensure in the State of VA or TN required
- Plans, directs, assigns, and evaluates the work of subordinates engaged in utilization review activities
- Plans, develops, and implements procedures to fulfill the requirements and guidelines for an effective and timely utilization review system
- Confers with physicians, administrative personnel, and other disciplines in the hospital to coordinate the work of the unit, obtain information, answer questions concerning the necessity for utilization review, and develop review procedures
- Determines need for and conducts in-service training to improve quality of admission and continued stay reviews, and to disseminate information concerning new or revised procedures
- Works with Professional Standards Review Organization representative to orient new staff to Federal laws and regulations pertaining to Medicare and Medi-Cal reimbursement
- Analyzes cases for referral to the physician advisor to ensure that the admission or continued stay is being questioned based upon appropriate screening criteria and standards; serves as the liaison with the physician advisor for the referral of unusual questionable cases, on referred cases for reconsideration, and to obtain authorization for the issuance of denial letters
- Reviews, retrospectively, utilization review records for completeness, use of appropriate codes, correctness of primary reason for admission and certified hospital days, and inclusion of all relevant supporting medical information
- Develops procedures for the compilation of information from medical charts concerning particular diagnoses, problems, procedures, or practitioner categories as directed for medical care evaluation studies
- Prepares and analyzes reports on number and status of reviews, physician advisor referrals, and type of physician advisor determinations to determine if improvement in procedures or additional staff training is needed, and to make recommendations on potential areas for medical care evaluation studies
- Attends Utilization Review Committee meetings to inform the committee of new or revised utilization review requirements, the impact of the requirements, and procedures to be implemented for compliance, as needed
- As a unit supervisor at the LAC-USC Medical Center
- Has immediate responsibility for organizing, assigning, and evaluating the work of at least seven Utilization Review Nurses
- Acts as a technical resource person to subordinate staff concerning Federal regulations pertaining to Medicare and Medi-Cal reimbursement, aspects of medical treatment for unusual illnesses and diseases, and interpretation of review procedures and standards
- Participates in the formulation of and changes in utilization review procedures by assessing the effectiveness of the review system and providing information on the policies and procedures within the assigned medical areas
- Provides input for the in-service training program by identifying areas of deficiency in staff knowledge or experience
- Analyzes cases for referral to the physician advisor to ensure that the admission or continued stay is being questioned based upon appropriate screening criteria and standards; serves as the liaison with the physician advisor for follow up on referrals
- Compiles data on number and status of reviews, physician advisor referrals, and type of physician advisor determinations
- Maintains effective working relationships with unit physicians to facilitate the execution of the utilization review system
- Participates in the work performed by subordinates
- Work retro Medicaid and prebill accounts efficiently and effectively obtaining authorizations for entire length of stay
- Evaluates clinical documentation on multiple patient accounts and escalates issues through the established chain of command
Professional Skills
- Excellent prioritization and organizational skills; effectively manage competing priorities and multiple deadlines
- Strong organizational skills and able to proactively prioritize needs and effectively manage resources
- Experience with clinical applications/systems. Excellent analytic, research, and problem solving skills
- Excellent organizational, written, and interpersonal skills and the ability to anticipate and solve problems and communicate clearly and effectively
- Excellent communication, organization, and interpersonal skills. Car and valid driver’s license required
- PC Skills– demonstrates advanced proficiency in Microsoft Office applications and others data mining software
- Possesses strong mentoring skills
How to write Utilization Review Nurse Resume
Utilization Review Nurse role is responsible for interpersonal, computer, clinical, organization, basic, medical, facilitation, microsoft, analytical, leadership. To write great resume for utilization review nurse job, your resume must include:
- Your contact information
- Work experience
- Skill listing
Contact Information For Utilization Review Nurse Resume
The section contact information is important in your utilization review nurse resume. The recruiter has to be able to contact you ASAP if they like to offer you the job. This is why you need to provide your:
- First and last name
- Telephone number
Work Experience in Your Utilization Review Nurse Resume
The section work experience is an essential part of your utilization review nurse resume. It’s the one thing the recruiter really cares about and pays the most attention to. This section, however, is not just a list of your previous utilization review nurse responsibilities. It's meant to present you as a wholesome candidate by showcasing your relevant accomplishments and should be tailored specifically to the particular utilization review nurse position you're applying to. The work experience section should be the detailed summary of your latest 3 or 4 positions.
Representative Utilization Review Nurse resume experience can include:
- Strong computer skills including the ability to rapidly learn and use new applications
- Strong experience in chart review and discharge planning, ER and ICU experience
- Prior clinical experience preferably in an acute care, skilled or rehabilitation clinical setting
- Strong experience in chart review, discharge planning, Med Surg and ICU
- Strong experience in chart review, discharge planning, Med Surge and ICU
- Computer skills and typing expertise
Education on an Utilization Review Nurse Resume
Make sure to make education a priority on your utilization review nurse resume. If you’ve been working for a few years and have a few solid positions to show, put your education after your utilization review nurse experience. For example, if you have a Ph.D in Neuroscience and a Master's in the same sphere, just list your Ph.D. Besides the doctorate, Master’s degrees go next, followed by Bachelor’s and finally, Associate’s degree.
Additional details to include:
- School you graduated from
- Major/ minor
- Year of graduation
- Location of school
These are the four additional pieces of information you should mention when listing your education on your resume.
Professional Skills in Utilization Review Nurse Resume
When listing skills on your utilization review nurse resume, remember always to be honest about your level of ability. Include the Skills section after experience.
Present the most important skills in your resume, there's a list of typical utilization review nurse skills:
- Excellent time management and problem solving-skills
- Demonstrated knowledge of pathophysiology with application of critical thinking skills
- Three years prior nursing experience in a hospital required with previous utilization review experience required
- Excellent analytic, research, and problem solving skills
- Strong organization skills, self-directed, flexible, able to adapt to rapidly changing regulatory requirements
- Solid analytical, assessment and documentation skills
List of Typical Experience For an Utilization Review Nurse Resume
Experience for utilization review nurse auditor resume.
- Proficient in MS word and excel applications. Previous experience working in an electronic medical record system
- Demonstrates excellence in communications to ensure customer satisfaction and retention
- Utilizes nationally recognized evidenced based guidelines to make medical necessity decisions
- Completing concurrent reviews for caseload to extend clients’ length of stay
- Participates in coordinating on-going education for Case Management staff regarding government and payor regulatory and outcomes
- Work assigned accounts in eRequest to resolve outstanding issues
- Report insurance denial trends identified during daily operational assignments
- Adhere to all policies and procedures, including, attendance, phone and internet usage, break utilization, etc
Experience For RN Utilization Review Nurse Bedford, Texas Resume
- Participate in education and training as needed
- Serves as the primary contact for all payors regarding utilization review and management issues
- Assess the needs for a Medicare IM, delivers admission notice if not already done so by admitting
- Collaborates with the third party payers to anticipate denial of payment and proactively addresses issues contributing to a potential denial
- Contacts the attending physician to notify him/her of all decisions to issue a notice of non-coverage for all payers
- Maintains productivity and meets all UR performance standards according to department policies and procedures
- Attends education sessions each year for internal and external customers regarding utilization management
- Graduate of an accredited practical/vocational or professional nursing program
Experience For Utilization Review Nurse Supervisor Resume
- Handles complex, high acuity cases, and/or account sensitive cases involving largest reserves
- Current/active Nursing License - needs to be licensed in Georgia and Alabama- strictly telephonic
- Provide assistance to physicians and hospital staff with discharge planning to expedite hospital discharge
- Support orientation program for UR staff by acting as primary mentor for review nurse and physician reviewers
- Conducts service connection reviews using Quadramed and also assists with clinical reviews as directed by the CBO: i.e., The Combat Vet Project
- Responsible/accountable for professional development and maintaining licensure
- Function as subject matter expert for Wyoming Disability Determination reviews as well as complete additional utilization management specialty reviews
- Perform accurate and timely documentation of all review activities based on policy and procedure
Experience For Telephonic Utilization Review Nurse Onsite Resume
- Contact facilities, physicians’ offices and/or insurance companies to resolve denials/appeals if needed
- Demonstrates knowledge of regulatory requirements, Ethics and Compliance policies, and quality initiatives; monitors self-compliance and implements process changes to ensure compliance to such regulations and quality initiatives
- Establish and maintain relationships with all customers
- Seeks assistance from immediate supervisor when in situations which are unclear or ambiguous
- Performs concurrent payor reviews for medical appropriateness for patients placed in outpatient observation or in an inpatient setting according to payor guidelines, rules and regulations
- Contacts the scheduling provider to get the correct status order for the scheduled procedure and/or secure documentation to support an ordered status or level of care
- Ensures inpatient vs. outpatient scheduling criteria is met in accordance with the payor and CMS requirements (inpatient only procedures)
- Establishes and maintains professional, collaborative working relationships with the Business Office Registration Department, Revenue Cycle Department and other key departments to facilitate processes to ensure timely and appropriate reimbursement for services provided
Experience For Utilization Review Nurse LPN Resume
- Initiates and coordinates the payor appeal process for all concurrent denials including arranging a scheduled time for the attending physician and payor Medical Director to discuss the clinical situation
- Completes an initial screen of all patients within 24 hours of admission utilizing specific criteria to identify needs related to utilization management
- Conducts retrospective medical appropriateness review as identified by internal and external audit and/or payor denials
- Meets Initial Clinical Review URAC Standards below
- Evaluates patients for appropriateness of admission type and setting, utilizing a combination of clinical information, screening criteria and third party information
- Appropriately uses Interqual criteria for leveling of care
- Completes CERME assessment, daily
- Ensures appropriate physician admission orders and level of care documentation by the physician
- Monitors physician compliance with the CMS 2 midnight rule
Experience For Utilization Review Nurse RN Resume
- Conducts concurrent admission and continued stay reviews based on appropriate utilization criteria, established standards, procedures and policies
- Documents authorization numbers, days approved data, and denial data as outlined in the departmental policy and procedures
- On a daily basis, identifies cases that fail to meet criteria and promptly reviews the case with the patient’s physician to resolve the issue
- Proactively follows and intervenes on open cases to include concurrent appeals of denials
- Educates staff and physicians about managed care principles, observation status, reimbursement rules and range of patient care setting beyond observation, intensive care and acute hospitals
- Delivers second IM notice to Medicare recipients if appropriate, facilitating appeal if needed
Experience For Network Utilization Review Nurse Resume
- Works collaboratively with all Revenue Cycle departments to ensure accurate, timely communication regarding changes in patient status information
- Attends required education to maintain competency with CERME and other UR systems
- Collaborates with members of the multidisciplinary team to facilitate the case management and care coordination processes for the assigned caseload
- Consults with medical staff as needed to facilitate accurate documentation and to assure an appropriate timely discharge. Monitors and ensures physician compliance with the CMS 2 midnight rule
- Monitors patient progress and plan of care with the aid of internal and external utilization guidelines
- Contributes in a positive manner to the development of the UR department
- Communicates information in a clear and timely manner
- Participates in quality improvement and evaluation processes related to the CM practice
- Participates in the development of procedures, roles, systems and structures related to the UR practice
Experience For Pre-certification / Utilization Review Nurse Resume
- Interacts with patients, families, colleagues and external contacts with respect, sensitivity and attentiveness to promote teamwork and cooperation
- Adheres to UR department specific and organizational policies and standards such as TJC, Dept of Health, etc
- UR’s are on site and available seven days a week
- Conducts pre-certification, inpatient, retrospective, out of network and appropriateness of treatment setting reviews within scope of licensure by utilizing appropriate medical policies and clinical guidelines in compliance with department guidelines and consistent with the members eligibility, benefits and contract
- Educates the member about plan benefits and contracted physicians, facilities and healthcare providers. Refers treatment plans/plan of care to peer clinical reviewers in accordance with established criteria/guidelines and does not issue medical necessity non-certifications
- A current, valid Michigan license to practice as a Registered Nurse without any conditions, limitations or restrictions
Experience For Associate Utilization Review Nurse, LPN Resume
- Applies worker’s compensation regulations, state laws and guidelines to case management activity in assigned territories
- Coordinates level of service justification directly with physician and communicates directly with third party payer to obtain approval
- Interact with social worker, community agencies to identify alternate delivery of services
- Reviews and/or coordinates requests for authorization of specialty services with external consultants, and Physician Advisors; Uses his/her own discretion in determining if submitted medical information needs a consultant’s review
- Educates external providers about HPHC’s utilization management guidelines for specialty services
Experience For Licensed Utilization Review Nurse Resume
- Licensed Practical Nurse (LPN) with current state license
- Communicating with the insurance department if a client does not have coverage or there are limitations on client’s policy that becomes available as case is opened with insurance company
- Working with clinical and client care team to communicate insurance case manager’s request for specific treatment, follow ups, and individualized care
- Participates in Contracting and Provider Relations activities as necessaryto develop and maintain provider networks. Identify and report when provider’s gaps in contracts are identified
- Refers all cases that are denied by the payor to the Concurrent Appeal URN or Physician Advisor
List of Typical Skills For an Utilization Review Nurse Resume
Skills for utilization review nurse auditor resume.
- Excellent verbal and written communication, organization and interpersonal skills
- Excellent communication (both written and verbal), organization and interpersonal skills
- Basic computer skills including word processing and spread sheets
- Nursing experience with one (1) year experience in Utilization Management
- Experience in acute long-term care, acute rehabilitation or skilled nursing facilities
- One year of care management, utilization management experience, clinical documentation or clinical auditing experience
- Utilization Review experience at a Managed Care plan or Provider Organization; 5+ years of Healthcare experience
- Develop leadership skills and to serve as a role model for clinical staff
- Demonstrates effective communication with adolescents, adults and older adults
Skills For RN Utilization Review Nurse Bedford, Texas Resume
- Documented experience in collecting, compiling, and performing preliminary analysis of data
- Experience with assisting with Discharge and Transition of Care Planning
- Documented experience assessing and interpreting clinical information from client records
- Documented experience consulting with physicians and other health team members regarding plan of care
- Recent clinical nursing experience in an acute-care hospital setting and/or payer case management
- Reviews and conducting special eligibility validation reviews including SC, Agent Orange, Combat Vet, etc
- Previous experience in an Acute Care, Hospital and/or Clinical setting
- Knowledge and experience in diverse Patient Care settings, including Inpatient Care
- Clinical experience in acute setting
Skills For Utilization Review Nurse Supervisor Resume
- Two or more years of experience in coding or a patient care acute facility, preferably at a tertiary care medical center
- Documented experience collaborating with various disciplines and/or areas within an organization
- Documented experience communicating information with outside entities, patients/families/assigned representatives, and/or staff
- Documented experience reviewing client medical records/charts
- Documented experience communicating information with outside agencies
- Documented experience discussing information with patients, families and/or assigned representatives
- Knowledge of CPT, ICD-10, and/or HCPC codes or coding experience
- Utilization Review experience
Skills For Telephonic Utilization Review Nurse Onsite Resume
- Previous Appeals / Denials experience
- Attention to detail with ability to prioritize, problem solve and multi-task
- Establish priorities, meet deadlines and maintain productivity standards in the management of the work assignment
- Perform utilization reviews to ensure that members receive necessary medical care in a timely and cost-effective manner
Skills For Utilization Review Nurse LPN Resume
- 6+ months of Concurrent / Utilization Review experience
- Demonstrate appropriate network utilization in accordance with regulatory requirements
- Proficient in computer technology and experience with Microsoft Office product Excel, Outlook, Word, Skype, etc
- Experience with clinical applications/systems
- Utilization Review experience for at least 1 year
- Acute care clinical experience
- Ensure full collection of clinical information prior to rendering a decision including contacting hospital providers for additional information as necessary
- Arrange alternative care services and maintain communication with acute long term care, acute rehabilitation or skilled nursing facilities
Skills For Utilization Review Nurse RN Resume
- Reports issues and system barriers to efficient and effective discharge planning to department leadership
- Lifting 50 lbs. (maximum) with frequent lifting and/or carrying of objects weighing up to 25 lbs
- Customer Orientation– establishes and maintains long term customer relationships, building trust and respect by consistently meeting and exceeding expectations
- Participate in company meetings, training activities and continuing education requirements
- Exp working in utilization mngt department (UR, UM, Discharge Planning, CM, Retrospective Review, Concurrent Review)
Skills For Network Utilization Review Nurse Resume
- Two (2) years Utilization Management and/or Hospital discharge planning in the acute care setting within the past four (4) years
- Conduct reviews using clinical assessment and established screening criteria
- Coordinates activities with other medical managmeent departments as needed, including making referrals to Case Managment and Behavioral Health
- Clinical practice in an acute care setting
- Quickly analyze and interpret data and write reports using standard medical terminology
- 1500 Spring Garden St
Skills For Pre-certification / Utilization Review Nurse Resume
- Assist in developing medical policies and procedures that directly impact member utilization of benefits
- 1000 S. Sterling Street
- DCS policies, procedures, and current State Federal and local laws governing AHCCCS/Medicaid health plan operations and requirements
- Proficient in using MS Word, MS Excel, and MS Outlook
- Background working with Medicare and Medicaid population
- BA/BS and nursing diploma. Current employees grandfathered (5/14)
Skills For Associate Utilization Review Nurse, LPN Resume
- Current, unrestricted RN license in the state of Wyoming
- Successful work history in a clinical setting and/or health insurance environment
- Accurately and completely documents in file using standard documentation format(s)
- Coordinate discharge planning to create member’s post-inpatient plan
- Evaluate the need for case management and transition of care services following inpatient stay
Skills For Licensed Utilization Review Nurse Resume
- Coordinate transportation with contracted vendors following inpatient stay
- Facilitate member’s transfers within contract facilities for ongoing inpatient stays
- Escalate cases not meeting criteria to Division PA
- Communicate with physicians regarding patient status, level of care. Medical necessity, utilization of resources, and denials
- Communicate lack of medical necessity and/or responder criteria being met to the facility Case Manager
- Ensure the member is at the appropriate level of care, in the appropriate setting, at the appropriate time through utilization review
List of Typical Responsibilities For an Utilization Review Nurse Resume
Responsibilities for utilization review nurse auditor resume.
- Documented skill in effective communication skills and professional behaviors that promote cooperation and teamwork
- Excellent personal computer skills (MS Outlook, MS Office, Midas, Meditech, OnBase DOS based and other related software)
- Excellent personal computer skills (MS Outlook, MS Office, Midas, Meditech, OnBase DOS based and other related software) required
- Three to five years clinical experience in a health care environment, with supervisory experience; Managed care experience desired
- Communicates effectively with other health care providers, patients, families, other hospital personnel and visitors
- Position requires candidates with determined and assertive communication skills
Responsibilities For RN Utilization Review Nurse Bedford, Texas Resume
- Behavioral health experience strongly desired
- Facilitates cost effective and quality patient care by effective communication with physicians, providers and members
- Solid understanding of Peer Review Organization criteria and standards, purpose and requirements needed; working knowledge of DRG payment system helpful
- Clinical nursing experience on an orthopedic/neurology nursing unit
- Ensures authorized services are performed in the most cost effective appropriate setting
Responsibilities For Utilization Review Nurse Supervisor Resume
- Educate providers about inpatient and outpatient cost-effectiveness, alternative placement and quality management
- Proven ability to work independently, with attention to detail and accuracy
- Evaluates effectiveness of care and facilitates coordination of care toward specific outcomes criteria
- Worker’s compensation or Occupational Medicine or Rehab experience desirable
- Experience in managed care, case managementd required
- HMO or managed care experience
- Current/valid State of Florida Registered Nurse licensure
Responsibilities For Telephonic Utilization Review Nurse Onsite Resume
- Case Management experience in an acute care setting
- Experience in a leadership role such as a manager, charge nurse, team leader, etc
- Acute care LPN experience
- Initiates the payor appeal process for all concurrent denials following the department guidelines for documentation and escalation
- Perform admission reviews, on in scope populations, utilizing InterQual within 24 hours of admission
- Professional conduct in all situations including clinical department meetings is required
- Documents clinical appropriateness reviews and care management activities in managed care operating systems
- Coordinate discharge planning activities for inpatient level of care services and facilitate referral to care management programs
Responsibilities For Utilization Review Nurse LPN Resume
- Based on case work and departmental reporting, ability to identify and report trends and/or areas of opportunities to department management and peers.
- Understand and investigate billing issues, claims and other plan benefit information.
- Assist with monitoring, inquiries, and audit activities as needed
- Provides insight and direction to management on any compliance concerns regarding products, company policies and procedures and/or client specifications
- Work rotating weekends and holidays
- Provide care coordination of members who are transitioning from one level of care to another
Responsibilities For Utilization Review Nurse RN Resume
- Participates in process performance improvement activities related to utilization management
- LVN with current state licensure
- Plans, implements, and evaluates appropriate health care services in conjunction with the physician treatment plan
- Utilizes clinical skills to assess, plan, implement, coordinate, monitor and evaluate options and services in order to facilitate appropriate healthcare outcomes for members
- Performs prospective, concurrent, and retrospective reviews for inpatient acute care, rehabilitation, referrals, and select outpatient services. Manages own caseload and coordinates all assigned cases
Responsibilities For Network Utilization Review Nurse Resume
- Acts as a resource to others
- Active and unrestricted RN or LVN license in state of New Jersey
- Collaborates with the Case Manager, Social Worker, attending physician, and other healthcare team members to ensure medical appropriateness criteria, to develop an action plan to avert reductions in care or denials and to obtain all payor information that influence discharge planning activities
- Refers all cases that are denied by the payor to the Concurrent Appeal Nurse or Physician Advisor
- Serves as an educational resource for other Case Management staff, other internal departments, physicians, nursing staff and others concerning utilization management strategies essential in meeting the organization's quality, utilization, financial and customer satisfaction objectives
- Validate the patient’s status is correct (Inpatient vs Outpatient) based on physician’s order, take action to correct status if incorrect or no order is present. Document actions
Responsibilities For Pre-certification / Utilization Review Nurse Resume
- Perform initial admission clinical summary reviews within 24 hours or per payor contract on payors with an authorization process
- Perform continued stay clinical summary reviews as per payor contract on payors with an authorization process
- Review and manage concurrent denials per FWD Centralized Utilization Review policy
- Documentation to take place, per HCA and FWD guidelines, in Midas in the Care Enhance Review Manager Enterprise (CERME), Midas Certification Entry, Midas Concurrent Review Entry and the Avoidable Denied Days module
- Registered Nurse, licensed in Massachusetts
- Identify placement settings that offer the lowest level of restriction and greatest level of autonomy for the members based upon medical necessity
- Monitor quality of care and collect and analyze utilization data
- Serve as a resource and liaison between the health plan, behavioral providers, facilities, member and families
- Provide and review member intakes and initial evaluations
Responsibilities For Associate Utilization Review Nurse, LPN Resume
- Comply with performance measures in regards to denials, higher level of care admission certifications and concurrent review timeliness
- Develop and maintain collaborative relationships with providers and educate on levels of care
- Interact with physicians, social workers, providers, case managers, and internal staff to develop discharge plans and oversee their implementation
- Authorize and/or review utilization of mental health and substance abuse services provided in inpatient and intermediate care settings. Assure appropriate levels of care and medical necessity in a manner that supports the recovery process
- Perform quality utilization review through the use of acquired knowledge and application of evidenced based guidelines for Medical Bill Reviews, TX Plans, IMEs, Peer Review reports, correspondences, addendums and/or supplemental reviews
- Utilize evidence-based guidelines (Interqual) and collaborates with hospital case managers, social workers, Primary Care Physicians, attending physicians, internal team and medical directors on a daily basis
- Manage all transitions of care related to a hospital stay through patient interviews, effective planning, and collaboration with facility personnel and client teams to prevent unplanned transitions and re-admissions through proven interventions
Responsibilities For Licensed Utilization Review Nurse Resume
- Knowledgeable about member benefits and assists member to maximize their individual benefit plan
- Facilitate authorizations for post-acute care services or medications
- Review cases for quality of care concerns
- Documents authorizations and case management activities in software applications
- Assumes leadership role in POD/IPA related meetings and shares knowledge and information
- Participates in process improvement activities and all STAR-related initiatives
- Obtains or ensures acquisition of appropriate pre-certifications/authorizations from third party payers and placement to appropriate level of care prior to hospitalization utilizing medical necessity criteria and third party payer guidelines. (30%)
- Obtains or facilitates acquisitions of urgent/emergent authorizations, continued stay authorizations, and authorizations for post-acute services as needed and with compliance with all regulatory and contractual requirements. (30%)
Related to Utilization Review Nurse Resume Samples
Nurse auditor resume sample, nurse case manager resume sample, utilization management nurse resume sample, care nurse resume sample, nurse, rn resume sample, surgery nurse resume sample, resume builder.
Utilization Review Nurse Resume Examples
Writing a great utilization review nurse resume is important because it is one of the first things a potential employer will see when they are considering you for a position. It is your opportunity to make a good first impression and sell yourself as the best candidate for the job.
Create your resume Select from 7 professional resume templates
If you're looking for inspiration when it comes to drafting your own utilization review nurse resume, look no further than the samples below. These resumes will help you highlight your experience and qualifications in the most effective way possible, giving you the best chance of landing the utilization review nurse job you're after.

or download as PDF
Essential Components of a Utilization Review Nurse Resume
A well-crafted resume is a critical tool for a Utilization Review Nurse, highlighting their expertise, experience, and qualifications in the field. It provides employers with a concise overview of the candidate's capabilities, demonstrating their proficiency in delivering quality patient care while effectively managing healthcare expenditures.
An effective resume must include certain key elements that underscore the nurse's proficiency in utilization review and general nursing acumen.
The following sections will delve into the essential components of a Utilization Review Nurse resume, explaining the significance of each and offering guidance on how to optimize them for maximum impact.
1. Contact Information
At the forefront of your resume should be your contact information, as it is the primary means for potential employers to initiate communication. Ensure accuracy and visibility.

Begin with your full name, prominently displayed, followed by your professional title, "Utilization Review Nurse." Include your city and state if relevant, and provide a professional-sounding email address and phone number. If applicable, add links to your LinkedIn profile or digital portfolio to showcase your professional background.
- Place these details at the top of your resume for easy access.
- Double-check for accuracy to avoid missing potential opportunities.
2. Professional Summary or Objective Statement
The Professional Summary or Objective Statement serves as your professional introduction, succinctly presenting your skills, experiences, and career goals. Tailor this section to the Utilization Review Nurse role, emphasizing your expertise in clinical review, case management, healthcare policies, patient advocacy, and medical documentation.
A compelling summary or objective can capture an employer's attention by illustrating your potential contributions to their organization. Whether you have extensive experience or are new to the field with transferable skills, this section should position you as the ideal candidate for a Utilization Review Nurse position.
Related : Top Utilization Review Nurse Resume Objective Examples
3. Nursing License and Certification Details
Include your nursing license and any relevant certifications to establish your legal qualification to practice as a nurse. Detail your RN license, any multi-state licenses, and certifications from organizations like the ACMA or CCMC, which underscore your specialization in utilization review.
Highlight additional certifications such as CPHQ or CCS, and mention any in-progress certifications to show your commitment to professional growth.
Ensure all listed licenses and certifications are current and valid to maintain credibility with potential employers.
4. Relevant Work Experience in Utilization Review
Detailing relevant work experience is crucial. Outline your previous roles, emphasizing specific responsibilities and achievements, such as identifying cost-saving measures without compromising patient care quality. Include experience with EHR systems and data analysis software, and quantify your accomplishments to provide a clear picture of your impact.
This section should not only showcase your expertise in utilization review but also suggest how you could enhance efficiency and reduce costs for the employer.
5. Skills and Competencies
The Skills and Competencies section is vital, demonstrating your suitability for the role. List essential skills such as clinical knowledge, analytical abilities, communication proficiency, attention to detail, decision-making, understanding of healthcare laws, computer literacy, time management, interpersonal skills, and ethical practice.
Highlighting these skills can convince potential employers of your fit for the Utilization Review Nurse role.
Related : Utilization Review Nurse Skills: Definition and Examples
6. Education and Training Background
Your educational background is fundamental, showcasing your foundational nursing education and any advanced degrees or specialized training in utilization review. List your degrees, certifications, and any additional training that enhances your qualifications for the role, such as CCM or CPUR certifications.
Include the institutions from which you obtained your qualifications to provide a complete educational history.
7. References or Referees
While not always included on the resume, having a prepared list of references is essential. Select individuals who can attest to your nursing skills and professional character, such as former supervisors or colleagues. Ensure their consent and provide accurate contact information.
Inform your references about the positions you are applying for so they can tailor their recommendations accordingly.
Remember, the right references can significantly influence the hiring decision by endorsing your qualifications and experience.
In summary, a well-prepared list of references is a crucial component of your job application process as a Utilization Review Nurse, even if it is not directly included on your resume.
Related Resume Examples
- Document Review Attorney
- Nurse Case Manager
- Nurse Anesthetist
- Nurse Assistant
- Nurse Clinician
Resume Builder
- Resume Experts
- Search Jobs
- Search for Talent
- Employer Branding
- Outplacement
- Resume Samples
Rn-utilization Review Resume Samples
The guide to resume tailoring.
Guide the recruiter to the conclusion that you are the best candidate for the rn-utilization review job. It’s actually very simple. Tailor your resume by picking relevant responsibilities from the examples below and then add your accomplishments. This way, you can position yourself in the best way to get hired.
Craft your perfect resume by picking job responsibilities written by professional recruiters
Pick from the thousands of curated job responsibilities used by the leading companies, tailor your resume & cover letter with wording that best fits for each job you apply.
Create a Resume in Minutes with Professional Resume Templates
- Works in conjunction with Clinical Documentation Improvement nurses to identify the Working DRG for patients admitted as inpatients and ensure the Working DRG is entered into the Cerner UM Module in order to calculate the GMLOS
- Ensures prior authorizations are entered into the UM Module for those services requiring prior authorization from the patient’s third-party payer. Enters approved hospital days into the UM Module when received by the patient’s payer
- Participates in daily departmental planning meetings and meets with the clinical team to guide the patient’s discharge plan
- Refers to the Utilization Review Physician Advisor all cases that do not meet established guidelines for admission or continued stay consistent with the arrangement with the Physician Advisor
- Performs concurrent review of acute and sub-acute services, as well as precertification review for all services following the plans authorization guidelines
- Licensed as a Registered Nurse
- Knowledge of Medicare and Medicaid payment rules, policies and regulations
- At the request of third party payers, Provides concurrent and retrospective reviews in an effort to extend authorized days and ensure reimbursement due for services provided
- Serves as resource for case management and social service professionals with regard to managed care contract interpretation
- Provides information to CIC staff regarding medical record coding
- Educates staff with updates in Medicare Medicaid and Managed care initiatives
- Initiates and Coordinates orientation for all new case management professionals to the department
- Completes quality monitoring of the case management professionals documentation to the department standards on a weekly basis using a tool designated to measure compliance to standards of practice. Provides feedback to leadership and individuals in a professional manner
- Completes data collection, tracks and trends information on denials related to medical necessity. Identifies performance improvement opportunities and collaborates with all levels of staff to develop and implement process improvements
- Collaborate with other health care givers in reviewing actual and proposed medical care
- Manage network participation and transfers to alternative levels of care using your knowledge of benefit plan design
- Communicate with providers regarding necessary adjustments to proposed care plans based on established criteria
- Active RN license in the state of TX with no restrictions
- Reside in the state of TX
- History of meeting or exceeding productivity metrics
- Manage network participation, care with specialty networks, care with DME providers and transfers to alternative levels of care using your knowledge of benefit plan design
- Working knowledge of Microsoft Office Suite, including Excel, and ability to develop and mine databases
- Ability to interact professionally with case management staff, physicians and payers
- Knowledge of case management, working of Medicare, Medicaid and private insurance
- Demonstrates a commitment to service, organization values and professionalism through appropriate conduct and demeanor at all times
- Basic understanding of computer application
- Case Management experience nice to have
- Demonstrated ability to manage complex management and clinical situations. Ability to work within a function independently exercising judgement to reach resolutions to issues
- Extensive clinical expertise - ICU, Medical
- Adheres to and exhibits our core values
15 Rn-utilization Review resume templates

Read our complete resume writing guides
How to tailor your resume, how to make a resume, how to mention achievements, work experience in resume, 50+ skills to put on a resume, how and why put hobbies, top 22 fonts for your resume, 50 best resume tips, 200+ action words to use, internship resume, killer resume summary, write a resume objective, what to put on a resume, how long should a resume be, the best resume format, how to list education, cv vs. resume: the difference, include contact information, resume format pdf vs word, how to write a student resume, utilization review rn-northeast region resume examples & samples.
- Manage network participation,
- Analyze clinical protocols and identify potentially unnecessary services and care delivery settings, and recommend alternatives if appropriate by analyzing
- Utilize screening criteria to examine clinical programs and identify members for specific case management and / or disease management activities or interventions
- Experience with chart review for medical necessity
- Insurance or managed care experience
- Medicare/Medicaid Experience a plus
- Previous experience in utilization review
- Up to 5% travel for potential training purpose
Utilization Review RN Resume Examples & Samples
- Establishes and maintains efficient methods of ensuring the medical necessity and appropriateness of all hospital admissions. Communicates patient admission status information to business operations staff in a timely manner such that patients obtain timely and appropriate care in the hospital setting as required by their clinical conditions
- Assure the RN Care Coordinator assigned to the patient is aware of the self-pay status of patients and make necessary referrals to financial counselors and/or hospital’s contracted financial counseling agencies, members of the healthcare team regarding target length of stay (LOS), acute care criteria, pay requirements, resource utilization, and care options to meet patient needs
- Develops and maintains relationships with third-party payers necessary to coordinate the appropriate utilization of hospital resources and meet the clinical needs of assigned patients
- Acts as a liaison with the RN Care Coordinators and Care Coordination Social Workers to facilitate the appropriate utilization of hospital resources and timely discharge. Tracks and reports trends of inappropriate utilization of resources to the Utilization Review Manager
- Minimum of 3 years nursing experience prior to care coordination required
- Ability to evaluate medical records and other health care data
- Ability to exercise good judgment and tact in relating to third-party payers, physicians and patients
- Ability to maintain confidentiality in all tasks performed
RN Telephonic Utilization Review Resume Examples & Samples
- Minumum 3 years adult acute care experience
- Strong assessment skills and proven ability using critical thinking to determine appropriateness of services
- Experience utilization criteria such as Interqual or Milliman
- Strong computer skills, ability to learn new programs quickly
RN Telephonic Utilization Review Post-acute Resume Examples & Samples
- Strong assessment skills
- Excellend computer and communication skills
Rn-utilization Review Resume Examples & Samples
- Subject matter expert regarding clinical appropriateness and level of care for CIC staff as well as Patient Access Services and Patient Financial Services staff. Reviews on referral cases to assist in determination of clinical appropriateness for level of care and Medicare/Medicaid and Managed Care related issues
- Reviews all patient documentation in response to letters of denial for reimbursement. Assess individual situations and makes appropriate referrals to physician advisor. Implements appeal process
- Completes data collection, analysis and project development for Medicare/Medicaid and managed care initiatives. Identifies performance improvement opportunities and collaborates with all levels of staff to develop and implement process improvements
Weekend RN Utilization Review Resume Examples & Samples
- Examine clinical programs information to identify members for specific disease management activities or interventions by utilizing established screening criteria
- Available to work Thurs - Sun each week
- Strong assessment skills and familiarity conducting reviews for medical necessity and appropriate level of care
- Good communication and computer skills
Utilization Review Rn-post-acute Team-central Region Resume Examples & Samples
- Working on UM cases for skilled nursing facilities, transition of care, skilled nursing and acute
- Prior clinical experience preferably in post acute care
- Previous case management, utilization review and/or discharge planning experience as a nurse
- 3+ years nursing experience prior to care coordination required
- Written and verbal communication skills
- Work as a part of a team
- Maintain confidentiality in all tasks performed
- Deal with problems involving several concrete variables in standardized situations
RN Utilization Review Manager Resume Examples & Samples
- Knowledge of Medicaid and Medicare healthcare practices and policies
- Knowledge of Medicare regulations related to utilization management turnaround times and billing rules
- High level of proficiency using InterQual and the ability to provide education and guidance to staff
- Strong written and verbal communication skills in order to effectively communicate with members, physicians, providers, plan leadership and staff members
RN Dir Utilization Review Days Resume Examples & Samples
- Bachelor's degree in nursing, health services administration or equivalent experience
- RN with extensive and varied clinical experience
- MA or MS or applicable graduate degree preferred
RN Utilization Review PRN Resume Examples & Samples
- Perform admission InterQual as per Plan contract or within 24 hours on all Non-Medicare Inpatients and document in Midas
- Ensure the patient’s status is correct (Inpatient vs Outpatient)
- Review concurrent denials and work with facility, physician and Plan to overturn the denial, document in Midas Denied Days screens
- Communicate denial status to the facility and physician
- Follow X-Code process as per HCA policy
- Communicate with physicians regarding patient status
Utilization Review Rn-weekends Resume Examples & Samples
- Prior clinical experience preferably in an acute care clinical setting
- Comfortable with Microsoft Office products including Word, Outlook and Excel
- Desire and ability to work at home in a safe and private environment, as outlined in WAH policy
- Positive disposition
- Previous experience with Milliman (MCG)
- Previous virtual work experience
Rn-utilization Review Specialist Resume Examples & Samples
- The Utilization Review (UR) Specialist has well-developed knowledge and skills in areas of utilization management (UM), medical necessity, and patient status determination. This individual supports the UM program by developing and/or maintaining effective and efficient processes for determining the appropriate admission status based on the regulatory and reimbursement requirements of various commercial and government payers
- This individual is responsible for performing a variety of concurrent and retrospective UM-related reviews and functions and for ensuring that appropriate data is tracked, evaluated, and reported. This individual monitors the effectiveness/outcomes of the UM program, identifying and applying appropriate metrics, evaluating the data, reporting results to various audiences, and designing and implementing process improvement projects as needed
- This individual identifies, develops, and provides orientation, training, and competency development for appropriate staff and colleagues on an ongoing basis. This individual leads and/or actively participates in process improvement initiatives, working with a variety of departments and multi-disciplinary staff
- This individual maintains current and accurate knowledge regarding commercial and government payers and Joint Commission regulations/guidelines/criteria related to UM. This role is responsible for ensuring that the UM program maintains documented, up-to-date policies and procedures and ensures and that all UM key processes have valid outcome measures that are monitored for compliance and reported to a variety of audiences
- The UR Specialist effectively and efficiently manages a diverse workload in a fast-paced, rapidly-changing regulatory environment. The UR Specialist is a member of and provides support to the hospital’s UR Committee. He/she collaborates with multiple leaders at various levels throughout UW Health, including directors and vice presidents, for the purpose of supporting and improving the UM program. The UR Specialist is responsible to the Medicare/Medicaid UR Program Manager
- Three (3) years relevant clinical nursing experience
- Recent experience as an inpatient or outpatient utilization review nurse or UM coordinator
- RN license in the State you will be working from
- Excellent interpersonal communication, problem-solving, and conflict resolution skills
- Computer skills in word processing, database management, and spreadsheet desirable
- Knowledge in areas of: Medicare and Medicaid UM regulations, McKesson InterQual, Medicare Inpatient Only List, RAC, QIO, MAC, and Denial Management
Supervisor Utilization Management Review, RN Resume Examples & Samples
- Required Registered Nurse graduated from an accredited Diploma, Associate’s Degree or Bachelor’s Degree program required. (Master’s degree preferred)
- Required minimum 3-5 years progressively responsible experience in a clinical environment
- Required 1-2 years utilization management/case managment
- Required solid PC skills required (Word, Excel and PowerPoint); ability to analyze and interpret data
- Required 3 years of current and progressive supervisory level experiences to include team leader or charge nurse
- Required valid driver’s license required (and reliable transportation for requested offsite work related activities
- Highly Preferred knowledge of discharge planning, outpaient clinical reviews transition care
- Preferred Managed care or Commercial Insurance
- Screens selected medical records in accordance with contractual agreements and departmental policies for appropriateness of admission; performing initial, continued stay, and retrospective reviews if applicable
- Submits initial reviews and updates using established criteria and communicates with payers as appropriate, using established processes
- Utilize established processes with the Physician Advisors to manage second level and peer to peer reviews
- Ensure patient status and levels of care are appropriate on admission and prior to discharge
- Makes timely contact with payers and provides information as appropriate
- Documents all utilization review outcomes and activities appropriately in the medical record
- Complies with all applicable payer, state and federal regulations as well as The Joint Commission requirements regarding Care Management and Utilization Review processes
- Acts as resource for and provides updates to the care management staff and care team for issues related to utilization review processes
- Engages providers with concerns regarding medical necessity and appropriateness of services
- Escalate concerns related to medical necessity and appropriateness of services to the Physician Advisors
- Works collaboratively with the Denials Specialist and Physician Advisors to manage retrospective appeals and documents according to established policy
- Reviews admissions and service requests within assigned unit for prospective, concurrent and retrospective medical necessity and/or compliance with reimbursement policy criteria. Provides case management and/or consultation for complex cases
- Assists departmental staff with issues related to coding, medical records/documentation, precertification, reimbursement and claim denials/appeals
- Three years of clinical experience required
- Previous case management, UR, billing, reimbursement and revenue cycle preferred
RN, Utilization Review Resume Examples & Samples
- Participates in designated committees and task forces according to the UM Program and at the direction of the Sr. Director of Medical Management. Coordinates with the utilization review, case management, discharge planning staff within network facilities
- Coordinates with Medical Director/Associate Medical Directors on case-specific issues
- Coordinates with Claims, Member Services, Grievance Coordinator and other operational departments regarding case management issues
- Conducts Utilization Management review for Inpatient, Outpatient, or Skilled Nursing cases
- Current license to practice as a Registered Nurse in the State of Ohio
- Minimum of 5-7 years of clinical nursing experience with at least 2 years' experience in utilization review, discharge planning, case management, or medical social work experience required. Nursing experience in an HMO insurance company setting
- Conducts admission review to assure that the hospitalization is warranted based on established criteria. Reviewing may be both concurrent or Post Discharge
- Carries out hospital programs and principles of utilization review in compliance with hospital policies and external regulatory agencies Peer Review Organization (PRO), Joint Commission, and multiple payer defined criteria for eligibility
- Engages in discussion with the Attending physician for clarification and/or status correction
- Engages second level physician review as indicated to support the appropriate status
- Ensures timely communication with Social Work staff for all concurrent status changes
- Administers Notice of Status Change to the patient/family when indicated. Provides education and information for the patient/family for clarification of the change
- Documents in the progress notes accurately to reflect the appropriate admission criteria and appropriate status along with any communications
- Ensures timely notification to Admitting of status of change or status discrepancies identified
- Reviews the records on admission for status orders present addressing CMS rules and guidelines around admission status
- Provides clinical information as requested from the insurance payer via telephone or fax in a timely manner to prevent technical denials
- Enters authorization, approvals and denials into the chart and communicates pertinent changes to Case Management
- Engages the attending physician to advocate and communicate via Peer to Peer Review for discussion with insurance for admission, continued stay or status when required
- Reviews denial letters/faxes received in and direct to Conifer CRC for appeals
- Collaborates in monitoring and addressing observation outliers and status discrepancies with HIM and Admitting
- Current licensure as a registered nurse of Iowa and five years clinical nursing experience. BSN or degree in healthcare related field preferred
- Knowledge of eligibility requirements for insurance coverage with respect to health care services: inpatient adult and child/adolescent, partial hospitalization, and Intensive Outpatient levels of care
Utilization Review Rn-bradley Resume Examples & Samples
- Two years of relevant progressive work experience in clinical psychiatric healthcare preferred
- Strong professional, organizational, and interpersonal skills required for effective and creative leadership in working with all levels of the organization, including physicians, committees as well as patients and their families
- Ability to communicate with outside agencies, third party payors, and regulators
- Possess good analytical and problem solving skills
- Ability to work with computerized clinical information systems. Initiative, flexibility, integrity, and diplomacy
- Licensed Registered Nurse
RN Utilization Review Case Manager Resume Examples & Samples
- Educates patient, families and other members of the care team about the financial out of
- Communicates pertinent information to the appropriate members of the patient care team both effectively and professionally. Takes responsibility to identify and eliminate barriers to effective patient stay management and promotes improvements in work processes within department, hospital, and community
- Provides consultation to professional staff and physicians on level of care determinations, CMS regulations and payer specific guidelines. Accurately and completely documents clinical reviews in accordance with documentation standards, policies, procedures and/or guidelines
- Associates degree from an accredited RN program
- Current license to practice as registered nurse in the State of Ohio
- Minimum of 3-5 years recent clinical experience in an acute care setting, case management or utilization review experience
Acute Onsite Rn-utilization Review Resume Examples & Samples
- Prior clinical experience in an acute care setting
- Valid driver's license and/or dependable transportation necessary (variable by region)
- Previous Medicare Experience
- Strongly Prefer Previous experience in utilization review
Optum Field Based Utilization Review Rn-maricopa County Resume Examples & Samples
- Perform utilization management, utilization review, or concurrent review (on - site or telephonic inpatient care management)
- Determine medical appropriateness of inpatient and outpatient services following evaluation of medical guidelines and benefit determination
- Identify solutions to non - standard requests and problems
- Current, unrestricted RN license in the state of residence
- 3+ years of experience in an acute care setting
- Knowledge of utilization management, quality improvement, discharge planning with transitions of care
- MCG certification, if does not have certification, must obtain within 3 years of hire
- Experience working with Medicare members
- MCG utilization management experience
- Working knowledge of hospice and palliative care
- Graduate degree in related field
- Working knowledge of SNF & LTAC facilities
- Bachelor’s degree in nursing (BSN)
- Experience using EMR, utilization management and / or prior authorization systems
Related Job Titles

IMAGES
VIDEO
COMMENTS
A right resume objective for an utilization review nurse should illustrate a strong commitment to patient care, while a wrong resume objective could focus more on the potential career advancement opportunities in the field. ... She has a background in corporate recruiting and human resources and has been writing resumes for over 10 years ...
What is a good objective for a Utilization Review Nurse resume? A Utilization Review Nurse (URN) is a registered nurse who is responsible for ensuring the quality and cost-effectiveness of patient care. The URN performs assessments of patient care and utilization of health care services to ensure they are appropriate, necessary and cost-effective.
Discover top Utilization Review Nurse resume objective examples to make your application stand out. Get hired faster with these expert tips. ... Here are a few sample resume objectives: 1. Medical professional seeking Utilization Review Nurse position with ABC Company utilizing problem solving, critical thinking, and communication skills, as ...
What is a good objective for a Utilization Management Nurse resume? A Utilization Management Nurse is responsible for helping improve patient care while managing healthcare costs. This role is key to ensuring health systems are fiscally sound while still providing quality care.
Diligent Utilization Review Nurse ensuring that patients get the appropriate level of medical care. Adept at efficiently allocating medical resources while ensuring that each patient is treated fairly. Specialize in finding a balance between the fiscal needs of the hospital or medical facility and the care needs of each patient.
Utilization Review Nurse Examples 1. Registered Nurse experienced in utilization review seeking position as Utilization Review nurse at Castelle Medical Center. Experience performing case reviews, collaborating with patients and healthcare providers, and identifying the appropriateness of prescribed care based on up-to-date data and research. 2.
As a utilization review nurse, you're a silent architect of healthcare, working behind the scenes to ensure resources are used efficiently and patients receive the care they deserve.These nurses are all about finding that perfect balance between resourcefulness and top-notch care, nurturing the hospital's sustainable growth, and ensuring continuous improvement in patient care.
Diligent Utilization Review Nurse with 5 years of experience reviewing medical records to ensure compliance with insurance standards, while promoting the most effective use of healthcare resources. ... The first section of your resume should be a professional summary that outlines your skills, experience, and career objective. Keep this section ...
utilization review nurse Job Descriptions; Explained. If you're applying for an utilization review nurse position, it's important to tailor your resume to the specific job requirements in order to differentiate yourself from other candidates. Including accurate and relevant information that directly aligns with the job description can greatly increase your chances of securing an interview with ...
Best Utilization Review Nurse Resume Objective Examples. To maximize the percentages of attaining the employment as a Utilization Review Nurse, describe all of the skill sets and qualities in relation to the industry of Healthcare you've obtained and add the statement at the beginning of your ideal job CV. ... Creating resumes that can win you ...
Create a Utilization Review Nurse resume using existing templates with skills, summary, education, experience, certifications, and contacts. Learn what should be included on a Utilization Review Nurse resume based on tips and professional advice.
Sabrina Thomas. 1637 Lady Bug Drive. Colorado Springs, CO 80903 (555)-555-5555 [email] Career Objective To obtain a position as an Utilization Review Nurse where my special skills can be used to their fullest potential to help improve the hospital.. Summary of Qualifications: Remarkable experience in geriatric nursing, renal, cardiac and endocrinology
Utilization Review Nurse Resume Samples and examples of curated bullet points for your resume to help you get an interview. ... utilization, financial and customer satisfaction objectives 3-5 years of clinical experience and/or case management, utilization review, and/or discharge planning experience in an acute care setting, insurance company ...
What is a utilization review nurse? Utilization review (UR) nurses conduct reviews for in-house patients in a hospital and patients who've been admitted to contracted facilities, including skilled nursing facilities and drug rehab programs. UR nurses collaborate with physicians on clinical reviews and keep them appraised of clinical criteria.
Find and customize career-winning Utilization Review Nurse resume samples and accelerate your job search. All utilization review nurse resume samples have been written by expert recruiters. ... utilization, financial and customer satisfaction objectives; Validate the patient's status is correct (Inpatient vs Outpatient) based on physician's ...
Utilization Review Nurse Resume. Summary : Dedicated registered nurse (RN) with specialty experience in cardiac/medical surgical nursing.Developed a strong knowledge of cardiac nursing. Reliable, an ethical healthcare provider with the ability to stay calm and intervene during crises, and to collaborate on multidisciplinary teams.
An effective resume must include certain key elements that underscore the nurse's proficiency in utilization review and general nursing acumen. The following sections will delve into the essential components of a Utilization Review Nurse resume, explaining the significance of each and offering guidance on how to optimize them for maximum impact. 1.
Conducts Utilization Management review for Inpatient, Outpatient, or Skilled Nursing cases Current license to practice as a Registered Nurse in the State of Ohio Minimum of 5-7 years of clinical nursing experience with at least 2 years' experience in utilization review, discharge planning, case management, or medical social work experience ...
Apply now for Nursing jobs with Humana - a leader in health.