

How to Use the Nutrition Care Process (NCP) & ADIME in Practice – Plus Nutrition Care Process Examples!
- February 14, 2023

Written by Olivia Farrow, RD, MHSc
Reviewed by Krista Kolodziejzyk, RD, MPH, MBA

In this article, we break down the steps of the Nutrition Care Process and ADIME charting to help you feel more confident applying them in practice. At the end, you will find Nutrition Care Process examples for 3 practice areas.
Whether you are a new dietitian, a student, or a seasoned dietitian, knowing how to utilize the Nutrition Care Process or ADIME documentation can help maintain consistency and organization in your practice.
This blog post has been developed based on information retrieved from the eNCPT electronic Nutrition Terminology Reference Manual 2023 edition.
Table of Contents
What is the nutrition care process (ncp).
The Nutrition Care Process (also known as NCP) was developed by the Academy of Nutrition and Dietetics and is recognized and used internationally. It was designed to create consistency across the steps of nutrition care, and includes terminology (the Nutrition Care Process Terminology, or NCPT), to keep the language used in documentation standardized.
The NCP is intended to be used for more than just direct client care. However, for the purpose of this article, we will be focusing on direct client care for the Nutrition Care Process examples provided.
Basically, the NCP standardizes the steps to take when providing nutrition care to patients/clients. Following the 4 main steps of the NCP can help provide dietitians with a blueprint for nutrition care.
The 4 Steps of the Nutrition Care Process
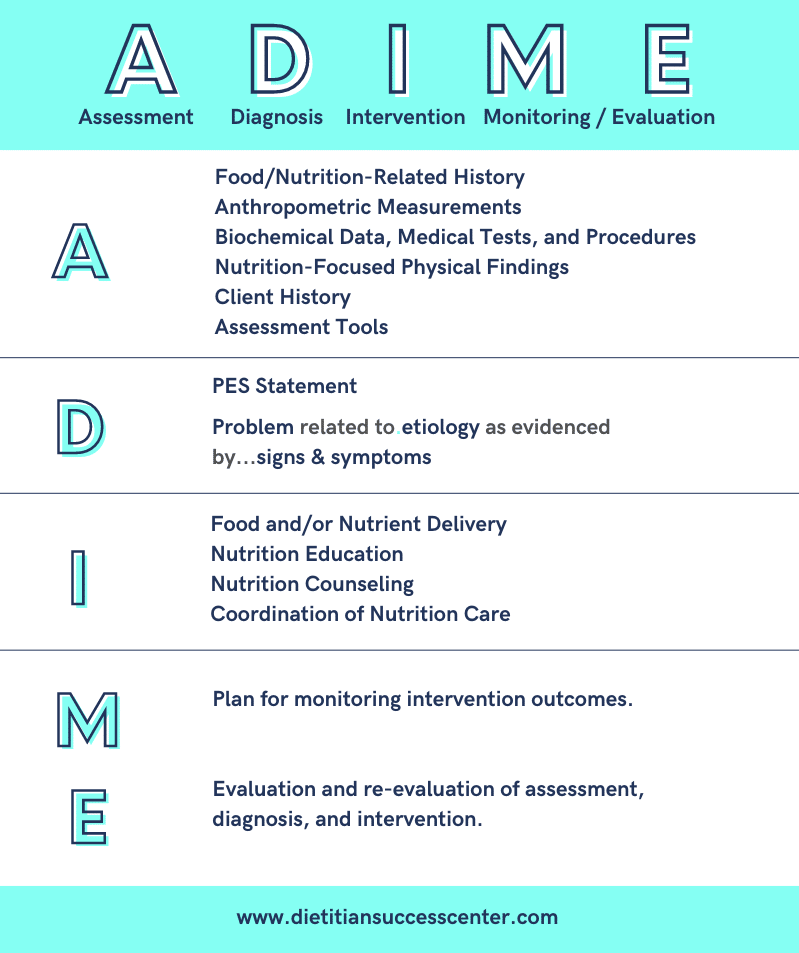
The NCP comprises 4 steps:
Nutrition Assessment
Nutrition diagnosis, nutrition intervention, nutrition monitoring/evaluation.
Let’s break down what each of these steps includes:
In the assessment stage, relevant information about the client is collected. The information collected will depend on the individual client, the reason you are providing care, and how you are obtaining the information.
For example, a dietitian working in an ICU setting will likely rely more heavily on the patient’s current medical data and the health team to collect information for a nutrition assessment. Whereas a dietitian working in an intuitive eating-focused private practice will collect mostly qualitative data from the client themselves.
How do you know what information to collect in the assessment of a client?
For the most part, it will depend on your clinical judgment, but the Nutrition Care Process Terminology (NCPT) can help by providing a list of options for assessment data to collect.
The NCPT for nutrition assessment is combined with monitoring and evaluation, but the main categories relevant for assessment include:
- This includes food and nutrition intake, nutrition supplements, nutrition knowledge and beliefs, food availability, physical activity, quality of life, etc.
- Height, weight, BMI, weight changes, etc.
- Labs and tests that are relevant for your nutritional assessment of the client.
- Physical appearance, swallowing ability, physical signs of nutrient deficiencies, etc.
- Relevant information obtained about the client’s personal, social, or medical history.
- Results from assessment tools, such as a validated malnutrition tool.
Once you’ve collected all relevant information and data, you will compare the data to normal values, nutrient requirements, or what would be considered appropriate for the client’s condition.
Assessment doesn’t just happen once, but will require reassessment at different stages of the nutrition care relationship.
At this stage, you will take all that you have learned about the client from your assessment and choose a main nutritional “problem” (or diagnosis) that you will be addressing. A nutritional diagnosis is not the same as a medical diagnosis.
To communicate a nutrition diagnosis, PES statements are used. PES statements communicate the nutrition-related problem that can be improved or resolved by nutrition intervention. They help to summarize your nutrition assessment and give justification for the next steps of the nutrition intervention.
A PES statement has three components: A nutrition-related problem, the etiology (the cause or origin of the problem), and the signs and symptoms. These sections are combined in a structured sentence by the phrases “related to” and “as evidenced by,” as below:
The PROBLEM related to ETIOLOGY as evidenced by SIGNS and SYMPTOMS
PES Statement Examples
Increased nutrient needs pes statement.
Increased protein and energy needs related to increased demand for wound healing as evidenced by non healing stage 3 pressure injury and unintentional weight loss of 8% in 3 months.
PES Statement for Cancer
Inadequate oral intake related to nausea and vomiting secondary to chemotherapy treatment as evidenced by consuming <50% of energy needs for the past 4 weeks and unintentional weight loss of 5% in one month.
Learn more about PES statements and how to write them here .
The nutrition diagnosis can help you prioritize the main nutritional concern and focus on what you, as the nutrition professional, can actually address.
The nutrition intervention is the plan for resolving or improving the nutrition problem identified in Step #2.
The NCPT breaks down some categories for the nutrition intervention, including:
- Modifying the diet, texture, nutrients, or eating/feeding environment.
- Providing education to the client on a particular nutritional or lifestyle topic.
- Using certain counseling skills or theoretical models to help the client implement changes.
- This could include referring to another professional or collaborating with a community partner to support the client.
For a complete list of Nutrition Interventions, check this resource .
The nutrition intervention should include the plan or goal for the client as well as the steps you are going to take to implement the plan.
Take the time to ensure that your intervention is client-centered and collaborative, including:
- Their needs and values
- The interdisciplinary team as necessary
You’ll also want to ensure that the intervention is realistic with the timeline, urgency, and level of follow-up possible.
Once the plan has been developed for nutrition care, monitoring and evaluation is next.
The first part of the stage is crafting a plan for how you will determine the progress being made on the goals for the client identified in Step #3. You can look at the nutrition diagnosis and intervention and create strategies for monitoring those specifically.
Monitoring and evaluation will likely include:
- Making an initial plan for what data will be collected at the next interaction with the client to be used for monitoring.
- Collecting any relevant assessment data pertinent to the evaluation of the client.
- Monitoring how the intervention is impacting the client.
- Comparing the information you collect to past data, to determine whether changes need to be made to your diagnosis and intervention plan.
Consider how often you can interact with the client to monitor their progress. Evaluation of how the client is doing nutritionally should be a part of each interaction with the client.
Examples of the NCP steps 1-4 combined can be found below.
ADIME Documentation
To simplify your chart notes and documentation of the NCP, you can utilize the ADIME documentation method. ADIME is just one charting format, but it works well with the NCP, we think you’ll see why.
ADIME stands for
- Intervention
So.. ADIME is the steps of the Nutrition Care Process!

Nutrition Care Process Examples
Now that we’ve covered the overall process, let’s walk through a few Nutrition Care Process examples using the ADIME structure.
These three examples represent different areas of practice that each have their own toolkits on DSC . Many DSC video courses also include case studies so you can walk through these steps with even more specific practical examples.
For these examples, we will walk through how to go through the steps of the NCP and utilize ADIME documentation for:
- Celiac Disease
- Polycystic Ovary Syndrome (PCOS)
- Nutrition Support – Enteral Nutrition
Nutrition Care Process Example 1 – Celiac Disease New Diagnosis
Nutrition Care Process Step #1 – Nutrition Assessment
The nutritional assessment for a client newly diagnosed with celiac disease might include obtaining data related to:
- Normal food intake (could be determined with a 3-day food record or 24-hour recall)
- Knowledge, beliefs, attitudes related to celiac disease and their diagnosis
- Relevant eating behaviors (how many meals and snacks they normally eat, what their eating schedule looks like, where and how they obtain food, etc.)
- Overall lifestyle and physical activity details
- Stress level
- Any relevant family or social history
- Any history of dieting or elimination diets
- Any supplements or medications they might be taking that could impact their nutritional status
- Food access and ability to purchase gluten-free foods
- Height, weight, and weight history if weight change is a concern for the client
- Celiac diagnosis (serology screen, biopsy performed)
- Concurrent conditions
- Lab Values (CBC, Iron, Folate, Vitamin B12, Calcium, Albumin, Phosphate, ALP, Vitamin D, Vitamin B6, Copper, Zinc)
- Any other confirmed allergies, intolerances (ie. lactose)
- Any other relevant or concurrent medical conditions (Type-1 Diabetes, Inflammatory Bowel Diseases, Arthritis, etc.)
- Loose stool
- Constipation
- Abdominal pain
Once this data is obtained, you could assess for:
- Sources of gluten in the diet
- Sources of gluten cross-contact
- Client readiness and motivation for change
- Overall dietary quality and nutrient intake (ex: adequate Fiber, Calcium, Vitamin D, Iron, Vitamin B12, Folate)
Nutrition Care Process Step #2 – Nutrition Diagnosis
The diagnosis would be individualized to the unique client and whether there is something that comes up in your assessment as a problem that needs to be addressed first.
If the main issue is that the client is completely new to the concept of celiac disease and a gluten-free diet, a nutrition diagnosis with a “limited food and nutrition knowledge” problem might make the most sense here such as in the example below:
Limited food and nutrition-related knowledge related to newly diagnosed celiac disease as evidenced by 3-day food record showing consumption of foods containing gluten and client report of lack of celiac-disease related knowledge.
For help with building your PES statement, check out our FREE PES Statement Cheat Sheet .
Nutrition Care Process Step #3 – Nutrition Intervention
If the main problem is a knowledge deficit, nutrition education would be the main nutrition intervention. In this case, education may be around:
- The identification of gluten-containing foods
- Label reading
- Gluten cross-contamination
- Gluten-free food choices
Depending on the client’s dietary intake, education on maintaining an overall nutritionally adequate diet with fiber and micronutrients and correcting any nutrient deficiencies may also be necessary.
For a client who does not have a knowledge deficit but is having difficulty maintaining a gluten-free diet, nutrition counseling, such as motivational interviewing, may be ideal as an intervention.
Nutrition Care Process Step #4 – Nutrition Monitoring and Evaluation
A monitoring plan for a client newly diagnosed with celiac disease may include food tracking, which could be used to assess compliance to a gluten-free diet, nutritional adequacy, and diet quality at future appointments.
Other considerations for monitoring may include changes in digestive symptoms, changes in lab values including nutrient deficiencies, changes in motivation level, or personal factors that may impact diet compliance.
Nutrition Care Process Example 2 – Polycystic Ovary Syndrome (PCOS)
This example will show how to go through the steps of the NCP with a client who has PCOS.
The nutritional assessment for a client with PCOS might include obtaining data related to:
- Weight concerns, cravings, fatigue, stress, subfertility
- Intake (3-day food record / 24-hour recall)
- Client concerns
- Knowledge/beliefs/attitudes related to food
- Eating behaviors
- Readiness/motivation to change
- Access to food
- Lifestyle / physical activity
- Medications or supplements
- Height, weight, weight history
- Commonly elevated: Total Testosterone, Free Testosterone, DHEA-S, Fasting Glucose
- Commonly deficient: Zinc, Vitamin D, Magnesium, Vitamin B12
- Relevant medical history or history of concurrent conditions (ex. diabetes)
- Lab values:
- Client concerns of acne, hirsutism, digestive issues, etc.
- Relevant family history of PCOS
- Fertility concerns
- Glycemic index of the majority of carbohydrates eaten
- Overall fiber intake
- Zinc, Vitamin D, Magnesium, Vitamin B12 (if deficient or suspected deficiency)
- Anti-inflammatory vs. pro-inflammatory foods
- Fluid intake (sugar-sweetened beverages, alcohol)
- Meal and snack frequency
- Macronutrient distribution
Your nutrition diagnosis would be individualized to the unique client and any pertinent concerns the client may have.
In an outpatient setting, it can sometimes be tricky to choose a main problem to focus on. Considering the client’s needs and desires and practical interventions may be helpful in choosing a problem to focus on first.
For example, if the client you are seeing could benefit from eating more fiber and this is a goal your client is eager to achieve, it may make sense to start here.
PES statement example:
Inadequate fiber intake related to low intake of whole grains, fruits, vegetables, and legumes as evidenced by 3-day food record, postprandial hyperglycemia trends on CGM, and client concerns of feeling hungry shortly after meals.
Depending on the unique needs of the client, the intervention may focus on education related to:
- Choosing higher fiber or lower glycemic index foods
- Meal and snack timing and frequency
- Mindful eating
- Anti-inflammatory foods
- Blood glucose management
Or, focusing on nutrient supplementation, including:
- Addressing any nutrient deficiencies determined from lab value or intake assessment
Intervention may also be counseling related, with a focus on goal setting or motivational interviewing.
A monitoring plan for a client with PCOS may focus on the client’s self-tracking of their food intake, a food and mood diary, changes in lab values or blood glucose management, and/or physical findings (ex. weight changes) if that was a focus of the intervention.
Evaluation will depend significantly on the client’s goals. In the case of the diagnosis of inadequate fiber intake, and a planned intervention to address that, the evaluation may be related to assessing the client’s food records for changes to the estimated intake of fiber.
Nutrition Care Process Example 3 – Nutrition Support (Enteral Nutrition)
This final example will show how to go through the steps of the NCP with a client who has been referred to the dietitian for an enteral nutrition plan.
The nutritional assessment for a client referred for enteral nutrition might include obtaining data related to:
- Nutrition and intake history (per OS intake or days NPO)
- Current body weight
- Usual body weight
- Biochemical data related to enteral feeding
- Clinical or medical data related to enteral feeding
- Any nutrient deficiencies on labs
- Current medications
- Any past or planned surgeries or procedures
- Physical appearance
- Skin fold thickness and mid-arm circumference
- Swallowing ability
- Digestive capabilities (ex. bowel sounds)
- Any nausea, vomiting, diarrhea concerns
- Any relevant family, social, or personal history
- Financial means to afford enteral formula
- Results from a malnutrition screening tool
Your assessment will also include the client’s energy, protein, and fluid needs.
In a clinical setting, where enteral nutrition is recommended or considered, the nutrition diagnosis is often related to intake. For a diagnosis related to intake, the intervention of enteral nutrition will address this problem. Diagnosis related to inadequate or inappropriate enteral or parenteral nutrition may also be considered if the client is already prescribed nutrition support and is in need of a change of formula or delivery method.
Clinical status, including involuntary weight loss, may also be considered the main problem.
Example PES statement:
Inadequate oral intake related to swallowing difficulties as evidenced by abnormal swallow study, unintentional weight loss of 6% in 1 month, low mid-arm circumference, and low hemoglobin levels.
Compared to the previous examples, where education and counseling were the most logical interventions, in this situation “Food and/or Nutrient Delivery” will be the category of intervention to address.
Your intervention may be related to some or all of the following:
- Determining feeding access
- Determining the feeding schedule
- Calculating energy, protein and fluid requirements
- Determining the formula and total amount required to meet needs
- Determining the feeding rate to meet goal
- Determining the risk of refeeding
- Calculating water flushes
From this, the final enteral prescription will be the main intervention, along with any goals for weight gain and education required. Referral to community supports may also be a part of the intervention.
Monitoring enteral tolerance will include looking at:
- Energy, protein, and fluid intake
- Gastrointestinal symptoms and changes
- Blood work changes
- Weight changes
- Tube placement
- Medication changes
- “Ins and Outs” (nutritional intake and bladder and bowel outputs)
Evaluation of any changes in nutrition indicators may require future interventions related to transitioning to bolus feeds prior to discharge to improve normalcy, ensuring enteral formula is covered for home use, trialing oral intake if possible, weaning off of enteral nutrition, and collaborating with community supports.
Key Takeaways for Dietitians
- The Nutrition Care Process (NCP) involves 4 steps: assessment, diagnosis, intervention, and monitoring and evaluation.
- Dietitians can use the NCP as a consistent methodology to guide nutritional care.
- ADIME charting incorporates the steps of the NCP into a documentation style.
- Nutrition Care Process Terminology (NCPT) can be used as part of the NCP to communicate the assessment, diagnosis, intervention, monitoring & evaluation.
Looking for more practical education designed for Registered Dietitians and nutrition practitioners? DSC is home to hundreds of online courses, ready-to-use client handouts, and practitioner resources designed to save you time while expanding your skills & knowledge. Become a DSC member today to access all of our toolkits and learn more about topics like celiac disease, polycystic ovary syndrome, enteral nutrition, and many more!
Quick Links
Related articles.

© 2024 Dietitian Success Center
Terms & Conditions
Privacy Policy
Learn more about the membership
Dietitian Success Center is your one-stop-shop to access affordable, evidence based nutrition courses & resources, plus business building tools without the price tag of a high-ticket business coach.
Student or Intern? Learn about our student rate .
Already a member?
" * " indicates required fields
FREE PES Statement Cheat Sheet
Fill-out details below to download the file

The price for DSC’s Membership will increase on November 22, 2024. Join now to lock in your membership rate.
We look forward to seeing you in the dsc community.
