Essay on Organ Donation for Students and Children
500+ words essay on organ donation.
Essay on Organ Donation – Organ donation is a process in which a person willingly donates an organ of his body to another person. Furthermore, it is the process of allowing the removal of one’s organ for its transplanting in another person. Moreover, organ donation can legally take place by the consent of the donor when he is alive. Also, organ donation can also take place by the assent of the next of kin of a dead person. There has been a significant increase in organ donations due to the advancement of medical science.


Organ Donation in Different Countries
First of all, India follows the opt-in system regarding organ donation. Furthermore, any person wishing to donate an organ must fill a compulsory form. Most noteworthy, this form is available on the website of the Ministry of Health and Family Welfare Government of India. Also, The Transplantation of Human Organs Act 1994, controls organ donation in India.
The need for organ donation in the United States is growing at a considerable rate. Furthermore, there has also been a significant rise in the number of organ donors in the United States. Most noteworthy, organ donation in the United States takes place only by the consent of the donor or their family. Nevertheless, plenty of organizations are pushing for opt-out organ donation
Within the European Union, the regulation of organ donation takes place by the member states. Furthermore, many European countries have some form of an opt-out system. Moreover, the most prominent opt-out systems are in Austria, Spain, and Belgium. In England, no consent is presumed and organ donation is a voluntary process.
Argentina is a country that has plenty of awareness regarding organ donation. Most noteworthy, the congress of Argentina introduced an opt-out organ donation policy. Moreover, this means that every person over 18 years of age will be a donor unless they or their family state their negative. However, in 2018, another law was passed by congress. Under the new law, the family requirement was removed. Consequently, this means that the organ donor is the only person who can state their negative.
Get the huge list of more than 500 Essay Topics and Ideas
Benefits of Organ Donation
First of all, organ donation is very helpful for the grieving process. Furthermore, many donor families take relief and consolation due to organ donation. This is because they understand that their loved one has helped save the life of other people. Most noteworthy, a single donor can save up to eight lives.
Organ donation can also improve the quality of life of many people. An eye transplant could mean the ability to see again for a blind person. Similarly, donating organs could mean removing the depression and pain of others. Most noteworthy, organ donation could also remove the dependency on costly routine treatments.
Organ donation is significantly beneficial for medical science research. Donated organs offer an excellent tool for conducting scientific researches and experiments. Furthermore, many medical students can greatly benefit from these organs. Most noteworthy, beneficial medical discoveries could result due to organ donation. Organ donation would also contribute to the field of Biotechnology.
To sum it up, organ donation is a noble deed. Furthermore, it shows the contribution of an individual even after death. Most noteworthy, organ donation can save plenty of lives. Extensive awareness regarding organ donation must certainly be spread among the people.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App


Organ Donation Essay

Table of Contents
Organ donation has proved to be a miracle for the society. Organs such as kidneys, heart, eyes, liver, small intestine, bone tissues, skin tissues and veins are donated for the purpose of transplantation. The donor gives a new life to the recipient by the way of this noble act. Organ donation is encouraged worldwide. The government of different countries have put up different systems in place to encourage organ donation. However, the demand for organs is still quite high as compared to their supply. Effective steps must be taken to meet this ever-increasing demand.
Fill Out the Form for Expert Academic Guidance!
Please indicate your interest Live Classes Books Test Series Self Learning
Verify OTP Code (required)
I agree to the terms and conditions and privacy policy .
Fill complete details
Target Exam ---
Long and Short Essay on Organ Donation in English
We have provided below short and long essay on organ donation in simple English for your information and knowledge.
After going through the essays you will know the significance of organ donation for someone in need, the procedure involved, under what circumstances is it illegal to donate an organ and what are safe physical criterion for organ donation.
You can use these organ donation essay in your school college events wherein you need to give a speech, write an essay or take part in debate.
Essay on Organ Donation in 200 words
Organ donation is done by both living and deceased donors. The living donors can donate one of the two kidneys, a lung or a part of a lung, one of the two lobes of their liver, a part of the intestines or a part of the pancreas. While a deceased donor can donate liver, kidneys, lungs, intestines, pancreas, cornea tissue, skin tissue, tendons and heart valves.
The organ donation process varies from country to country. The process has broadly been classified into two categories – Opt in and Opt out. Under the opt-in system, one is proactively required to register for donation of his/ her organs while in the opt-out system, every individual becomes a donor post death unless he/she opts-out of it.
There is a huge demand for organs. It is sad how several people in different parts of the world die each year waiting for organ transplant. The governments of different countries are taking steps to raise the supply of organs and in certain parts the number of donors has increased. However, the requirement of organs has simultaneously increased at a much rapid speed.
Each one of us should come forward and register to donate organs after death. “Be an organ donor, all it costs is a little love”.
Also Check: Essay on Organ Trafficking
Essay on Organ Donation in 300 words
Organ donation takes place when an organ of a person’s body is removed with his consent while he is alive or with the consent of his family member after his death for the purpose of research or transplant. Kidneys, liver, lungs, heart, bones, bone marrow, corneas, intestines and skin are transplanted to give new life to the receiver.
Organ Donation Process
- Living Donors
Living donors require undergoing thorough medical tests before organ donation. This also includes psychological evaluation of the donor to ensure whether he understands the consequences of donation and truly consents for it.
- Deceased Donors
In case of the deceased donors, it is first verified that the donor is dead. The verification of death is usually done multiple times by a neurologist. It is then determined if any of his/ her organs can be donated.
After death, the body is kept on a mechanical ventilator to ensure the organs remain in good condition. Most organs work outside the body only for a couple of hours and thus it is ensured that they reach the recipient immediately after removal.
Gap between Demand and Supply
The demand for organs is considerably higher than the number of donors around the world. Each year several patients die waiting for donors. Statistics reveal that in India against an average annual demand for 200,000 kidneys, only 6,000 are received. Similarly, the average annual demand for hearts is 50,000 while as low as 15 of them are available.
The need for organ donation needs to be sensitized among the public to increase the number of donors. The government has taken certain steps such as spreading awareness about the same by way of TV and internet. However, we still have a long way to go.
Organ donation can save a person’s life. Its importance must not be overlooked. A proper system should be put in place for organ donation to encourage the same.
Essay on Organ Donation in 400 words
Organ donation is the process of allowing organ or tissue to be removed surgically from one person to place it in another person or to use it for research purpose. It is done by the consent of donor in case he is alive or by the consent of next of kin after death. Organ donation is encouraged worldwide.
Kidneys, liver, lungs, heart, bones, bone marrow, skin, pancreas, corneas, intestines and skin are commonly used for transplantation to render new life to the recipient. Organ donation is mostly done after the donor’s death. However, certain organs and tissues such as a kidney, lobe of a lung, portion of the liver, intestine or pancreas can be donated by living donors as well.
Organ Donation Consent Process
There are two types of consents when it comes to organ donation. These are the explicit consent and the presumed consent.
- Explicit Consent: Under this the donor provides a direct consent through registration and carrying out other required formalities based on the country.
- Presumed Consent: This does not include a direct consent from the donor or the next of kin. As the name suggests, it is assumed that the donation would have been allowed by the potential donor in case consent was pursued.
Among the possible donors approximately twenty five percent of the families deny donation of their loved one’s organs.
Organ Donation in India
- Legalised by Law
Organ donations are legal as per the Indian law. The Transplantation of Human Organs Act (THOA), 1994 enacted by the government of India permits organ donation and legalizes the concept of brain death.
- Documentation and Formalities
The donor is required to fill a prescribed form. The same can be taken from the hospital or other medical facility approached for organ donation or can be downloaded from the ministry of health and family welfare government of India’s website.
In case of a deceased donor, a written consent from the lawful custodian is required in the prescribed application form.
As is the case with the rest of the world, the demand of organs in India is much higher compared to their supply. There is a major shortage of donated organs in the country. Several patients are on the wait list and many of them succumb to death waiting for organ transplant.
The government of India is making efforts to spread awareness about organ transplant to encourage the same. However, it needs to take effective steps to raise the number of donors.
Essay on Organ Donation in 500 words
Organ donation refers to the process of giving organs or tissues to a living recipient who requires a transplant. Organ donation is mostly done after death. However, certain organs can be donated even by a living donor.
The organs that are mostly used for the purpose of transplant include kidney, liver, heart, pancreas, intestines, lungs, bones and bone marrow. Each country follows its own procedure for organ donation. Here is a look at how different countries encourage and process organ donation.
Organ Donation Process – Opt In and Opt Out
While certain countries follow the organ donation opt-in procedure others have the opt-out procedure in place. Here is a look at the difference between these two processes of organ donation:
- Opt In System: In the opt-in system, people are required to proactively sign up for the donation of their organs after death.
- Opt Out System: Under this system, organ donation automatically occurs unless a person specifically makes a request to opt out before death.
Organ Donation in Different Countries
India follows the opt-in system when it comes to organ donation. Anyone who wishes to donate organs needs to fill a prescribed form available on the Ministry of Health and Family Welfare Government of India’s website.
In order to control organ commerce and encourage donation after brain death, the government of India came up with the law, The Transplantation of Human Organs Act in the year 1994. This brought about a considerable change in terms of organ donation in the country.
Spain is known to be the world leader in organ donations. It follows the opt-out system for organ donation.
- United States
The need for organs in the United States is growing at a rapid pace. Though there has been a rise in the number of organ donors, however, the number of patients waiting for the organs has increased at a much higher rate. Organ donation in the United States is done only with the consent of the donor or their family. However, several organizations here are pushing for the opt-out organ donation.
- United Kingdom
Organ donation in the United Kingdom is voluntary. Individuals who want to donate their organs after death can register for the same.
This is the only country that has been able to overcome the shortage of transplant organs. It has a legal payment system for organ donation and is also the only country that has legalized organ trade.
Organ donation is quite low in Japan as compared to other western countries. This is mainly due to cultural reasons, distrust in western medicines and a controversial organ transplant that took place in 1968.
In Columbia, the ‘Law 1805’ passed in August 2016, introduced the opt-out policy for organ donation.
Chile opted for the opt-out policy for organ donation under the, ‘Law 20,413’ wherein all the citizens above the age of 18 years will donate organs unless they specifically deny it before death.
Most of the countries around the world suffer from low organ donor rate. The issue must be taken more seriously. Laws to increase the rate of organ donation must be put in place to encourage the same.
Essay on Organ Donation in 600 words
Organ Donation is the surgical removal of a living or dead donor’s organs to place them in the recipient to render him/her a new life. Organ donation has been encouraged worldwide. However, the demand of human organs far outweighs the supply. Low rate of organ donation around the world can be attributed to various reasons. These reasons are discussed below in detail.
Teleological Issues
The moral status of the black market organ donation is debatable. While some argue in favour of it others are absolutely against the concept. It has been seen that those who donate their organs are generally from the poor section of the society and those who can afford these are quite well off. There is thus an imbalance in the trade.
It has been observed that those who can purchase the organs are taking advantage of the ones who are desperate to sell. This is said to be one of the reasons for the rising inequality of status between the rich and the poor. On the other hand, it is argued that those who want to sell their organs should be allowed to do so as preventing them from it is only contributing to their status as impoverished. Those who are in favour of the organ trade also argue that exploitation is preferable to death and hence organ trade must be legalized. However, as per a survey, later in life the living donors regret their decision of donating their organs.
Several cases of organ theft have also come forward. While those in support of the legalization of organ market say that this happens because of the black market nature of trade while others state that legalizing it would only result in the rise of such crimes as the criminal can easily state that the organ being sold has not been stolen.
Deontological Issues
These are defined by a person’s ethical duty to take action. Almost all the societies in the world believe that donating organs voluntarily is ethically permissible. Many scholars believe that everyone should donate their organs after death.
However, the main issue from the standpoint of deontological ethics is the debate over the definitions of life, death, body and human. It has been argued that organ donation is an act of causing self harm. The use of cloning to come up with organs with a genotype identical to the recipient is another controversial topic.
Xenotransplantation which is the transfer of animal organs into human bodies has also created a stir. Though this has resulted in increased supply of organs it has also received a lot of criticism. Certain animal rights groups have opposed the sacrifice of animals for organ donation. Campaigns have been launched to ban this new field of transplantation.
Religious Issues
Different religious groups have different viewpoints regarding organ donation. The Hindu religion does not prohibit people from donating organs. The advocates of the Hindu religion state that it is an individual choice. Buddhists share the same view point.
The Catholics consider it as an act of love and charity. It is morally and ethically acceptable as per them. The Christian Church, Islam, United Methodists and Judaism encourage organ donation. However, Gypsies tend to oppose it as they believe in afterlife. The Shintos are also against it as they believe that injuring a dead body is a heinous crime.
Apart from this, the political system of a country also impacts organ donation. The organ donation rate can increase if the government extends proper support. There needs to be a strong political will to ensure rise in the transplant rate. Specialized training, care, facilities and adequate funding must be provided to ensure a rise.
The demand for organs has always been way higher than their supply due to the various issues discussed above. There is a need to focus on these issues and work upon them in order to raise the number of organ donors.
Essay on Organ Donation FAQs
How do you write an organ donation essay.
To write an organ donation essay, start with an introduction explaining its importance, discuss benefits, address common concerns, and conclude with a call to action for readers to consider becoming donors.
What is a short note on organ donation?
Organ donation involves willingly giving one's organs after death to save lives. It's a selfless act that can bring hope and health to those in need.
How important is organ donation?
Organ donation is crucial as it saves lives by providing organs to individuals suffering from organ failure, offering them a chance for a healthier and longer life.
What is the aim of organ donation?
The aim of organ donation is to provide organs and tissues from willing donors to those in need, improving the quality of life and increasing survival rates for recipients.
What are the 4 types of organ donation?
The four types of organ donation include deceased donation (after death), living donation (from a living person), paired exchange (swapping organs between two donor-recipient pairs), and directed donation (to a specific person).
What is the concept of organ donation?
Organ donation is the voluntary act of giving one's organs or tissues to save or enhance the lives of others, often occurring after death or, in some cases, while the donor is still alive.
Which organ Cannot be donated?
The brain cannot be donated for transplantation. While other organs like the heart, liver, kidneys, and lungs can be donated, the brain's complex functions make it ineligible for donation.
Related content
Talk to our academic expert!
Language --- English Hindi Marathi Tamil Telugu Malayalam
Get access to free Mock Test and Master Class
Register to Get Free Mock Test and Study Material
Offer Ends in 5:00

Organ Donation: Opportunities for Action (2006)
Chapter: 1 introduction, 1 introduction.
I n the 50 years since the first successful organ transplant, thousands of recipients of a transplanted kidney, heart, pancreas, liver, or other solid organ in the United States and throughout the world have had their lives extended and their health enhanced as a result of organ transplantation.
Organ transplantation is unique among surgical procedures, in that the procedure cannot take place without the donation of an organ or a partial organ from another person. Since 1988, more than 390,000 organs have been transplanted, with approximately 80 percent of the transplanted organs coming from deceased donors. In 2005, 7,593 deceased donors provided 23,249 transplanted organs in the United States, and there were 6,896 living donors (OPTN, 2006 1 ).
The success of organ transplantation as a treatment option, the rising incidence of related or contributory medical conditions, improvements in immunosuppressive medications, and other factors have resulted in a rapid escalation in the waiting list for transplantation 2 in recent decades. In 1988, there were 16,026 individuals on the waiting list for an organ transplant; by 1995 the waiting list had increased almost 275 percent to 43,937; and it

FIGURE 1-1 Growth in the number of transplants and in the number of candidates on the transplant waiting list.
SOURCE: HRSA and SRTR (2006).
has since more than doubled so that by January 2006 the waiting list topped 90,000 individuals ( Figure 1-1 ) (IOM, 1999; OPTN, 2006). The waiting list is primarily driven by the need for kidney transplants. The statistics on the transplant waiting list are continually updated, and as of March 24, 2006, there were 91,214 transplant candidates 3 on the waiting list, of whom 65,917 individuals (approximately 70 percent of the waiting list) were candidates for kidney transplantation. In 2005, 44,619 transplant candidates were added to the waiting list (OPTN, 2006).
As the demand for organ transplants far exceeds the current supply of available organs, various efforts are under way to determine how best to reduce the gap between supply and demand. In addition to refinements in hospital processes and protocols, several proposals are being discussed that
might further enhance the system or provide incentives for more individuals or families to consent to organ donation.
In 2004, the Health Resources and Services Administration (HRSA) and The Greenwall Foundation asked the Institute of Medicine (IOM) to study the issues involved in increasing the rates of organ donation. This report is the result of a 16-month study conducted by an IOM committee composed of experts in the fields of bioethics, law, health care, organ donation and transplantation, economics, sociology, emergency care, end-of-life care, and consumer decision making.
SCOPE OF THIS REPORT
The IOM committee was charged with reviewing the current efforts and proposals to increase organ donations from deceased donors, including but not limited to educational activities, media campaigns, financial incentives, and presumed-consent laws. The committee was asked to identify ethically controversial proposals and, for those proposals, to
evaluate and address the impact that these proposals may have on existing donation efforts and public perceptions regarding organ donation;
evaluate and address the impact that these proposals may have on specific groups, such as ethnic minorities (specifically, African Americans), socioeconomically disadvantaged individuals, those likely to be disproportionately affected by the proposal, and living donors;
make recommendations about whether particular alterations can be made to various proposals to reduce ethical problems; and
provide recommendations regarding the cost-effectiveness, feasibility, and practicality of implementing such proposals.
To address its charge, the committee held five meetings and gathered information by holding a scientific workshop (see Appendix B for the workshop agenda) and two public comment sessions, talking with numerous individuals in the organ transplantation field, and conducting a literature review. The committee developed a set of perspectives and principles that guided its consideration of the complex issues that it was asked to address ( Chapter 3 ). This report benefits from the work of prior IOM committees that examined organ allocation and donation after circulatory determination of death (IOM, 1997, 1999, 2000). However, this report focuses on organ donation, not on the equally complex issues of organ allocation. Furthermore, it focuses on solid-organ donation and does not address eye and tissue donation. Finally, this report concentrates on increasing rates of deceased donation and considers living donation only briefly in Chapter 9 .
To set the context for the report, this chapter provides an overview of the history and current status of the U.S. system of organ donation and
transplantation and describes in brief some of the organ donation policies and practices of other countries. The chapter also highlights the committee’s thoughts on the evolving terminology in the field of organ donation, provides a discussion of the economic value of increasing the organ supply, and concludes with an emphasis on the benefit of preventive measures to reduce the demand for organ transplantation and minimize the rejection of transplanted organs.
OVERVIEW AND HISTORY OF THE CURRENT U.S. SYSTEM
The current U.S. system of organ donation, recovery, allocation, and transplantation has developed and evolved during the past 50 years. In 1954, the first successful U.S. transplantation involved the transplantation of a kidney between living twin brothers (Merrill et al., 1956). Immunosuppressive medications began to be used in the late 1950s, leading to the first successful transplantation of a kidney from a deceased donor in 1962 (Halloran and Gourishankar, 2001). This transplantation involved an unrelated donor and recipient and the use of the immunosuppressive drug azathioprine (Morrissey et al., 2001). Cyclosporine, discovered in 1978, provided significantly improved immunologic tolerance; and numerous subsequent pharmacologic, surgical, and clinical advances have continued to improve the rates of graft survival and reduce the potential for organ rejection. The growth and development of the field of organ transplantation and the nature of its organization and structure have been guided by state and federal laws and regulations ( Box 1-1 ).
Clarifying Criteria for Determination of Death
The early transplants were generally the result of donations of kidneys from living donors or donations of organs from deceased donors who had been declared dead following the irreversible cessation of circulatory and respiratory function (DeVita et al., 1993). In the late 1960s, improvements in mechanical ventilation and other types of medical support to sustain cardiopulmonary function highlighted the need to clarify the criteria for determining death. This led to clarification of the determination of death by circulatory criteria and to examination of the concept of determining death by neurologic criteria (Report of the Ad Hoc Committee, 1968; Guidelines for the determination of death, 1981). As a result, in addition to clarification of the criteria for the diagnosis of death by irreversible cessation of circulatory function, criteria were developed for the diagnosis of death based on the irreversible loss of function of the whole brain, including the brain stem (neurologic criteria). These criteria were incorporated into the Uniform Determination of Death Act, which was codified into state law in
various forms. For each set of criteria the diagnosis of death requires both the cessation of function and irreversibility (Guidelines for the determination of death, 1981). The use of neurologic criteria for the determination of death has gained wide medical, legal, ethical, and public acceptance in the United States, although debates continue (Bernat, 2005; Laureys, 2005).
Growth and Organization of the Transplantation Field
The increased number of transplantation operations in the 1970s and 1980s and concerns about the allocation of donated organs led to an expanded role for organ procurement organizations (OPOs), some of which had emerged in the 1960s as localized efforts. In 1972, legislation authorized Medicare coverage for kidney transplantation as a treatment for end-stage renal disease. In 1978, amendments to that legislation increased the length of availability of Medicare benefits after a successful kidney transplant from 1 year to 3 years and also increased coverage of kidney acquisition costs and home dialysis costs (Eggers, 2000). The next breakthrough in transplantation came with the advent of reliable and effective immunosuppressive medications to improve graft functioning and survival for patients posttransplantation.
The growing demand for organ transplantation, controversies regarding the allocation of organs, and concerns about payment for organs prompted congressional hearings on organ transplantation in the early 1980s. The resulting federal legislation, the National Organ Transplant Act of 1984, prohibited the sale of human organs; established a task force to address organ donation and allocation issues; and established the Organ Procurement and Transplantation Network (OPTN).
OPTN is charged with developing policies for and implementing an equitable system of organ allocation, maintaining the waiting list of potential recipients, and compiling data from U.S. transplant centers (OPTN, 2004). The United Network for Organ Sharing (UNOS), a nonprofit, private voluntary organization, has been the sole administrator of OPTN since the initial contract was awarded in 1986. Oversight for the OPTN contract is provided by the Division of Transplantation in the Health Resources and Services Administration of the U.S. Department of Health and Human Services. OPOs and transplant centers are required to participate in OPTN. OPTN’s oversight responsibilities focus on solid organ donation and transplantation from deceased donors. OPTN has limited responsibilities regarding living donation and does not have oversight responsibilities regarding tissue donation and distribution, although most OPOs recover tissue as well as solid organs, and a few OPOs are involved in tissue processing.
Currently, the organ donation and transplantation system in the United States is coordinated by 58 OPOs serving unique geographic areas (donor service areas) ( Figure 1-2 ). When a donated organ becomes available, the organ allocation algorithms developed by OPTN-UNOS identify a potential recipient on the basis of multiple factors, including severity of disease; geographic proximity; and blood, tissue, and size matches with the donor. Ongoing efforts are made to ensure impartiality in the allocation process. OPOs are charged with working with individuals, families, and hospital staff to explore consent for and facilitate organ donation; evaluating the

FIGURE 1-2 Donor service areas. Reprinted courtesy of the Association of Organ Procurement Organizations.
medical eligibility of potential donors; coordinating the recovery, preservation, and transportation of donated organs; and educating the public about organ donation (UNOS, 2006).
In addition to the OPOs, the other key organizations involved with organ donation are the donor hospital and the transplant center. Although organ donation, recovery, and transplantation may all occur in the same medical center, it is often the case that the organs are recovered in the donor hospital and are then transported to several transplant centers in the region or across the country. In 2005, 267 transplant centers were operating approximately 865 transplant programs in the United States (UNOS, 2005). This represents significant growth from the 244 transplant programs functioning in 1984 (UNOS, 2004). The number of annual organ transplants
has also significantly increased, from an estimated 7,692 in 1984 to 28,110 in 2005 (UNOS, 2004; OPTN, 2006).
Some of the challenges in further improving the organ donation system result from the heterogeneity of the OPOs, donor hospitals, and transplant centers, each of which serves populations with different demographics. Furthermore, the priorities and norms of the OPOs vary, such as in their approaches to families and their policies on donation after circulatory determination of death (Chapters 4 and 5 ). For example, there is variability in the rates at which consent is obtained for deceased organ donation in various transplant centers and OPOs ( Chapter 4 ). A 2003 study examining the variability among 190 transplant centers found that 30 centers (16 percent) had consent rates of 70 percent or higher, whereas 18 centers had consent rates below 30 percent (DHHS, 2003). This is similar to the variation of donation rates reported by OPOs, which ranged from 34.3 to 77.9 percent in 2004 (SRTR, 2005). As discussed throughout this report, efforts by OPOs and participating hospitals to increase the availability of organs for transplantation are focusing on increasing the consent rate for donation as well as on increasing the population of potential donors.
Although this report focuses on solid organ donation, many of the matters it discusses are closely tied with tissue donation. However, the tissue recovery and distribution system is quite different, particularly in the extent of private-sector commercial involvement. The resulting issues and challenges impact both the solid organ and tissue donation and recovery systems (Youngner et al., 2004).
Deceased Organ Donation
In the United States, deceased organ donation is an opt-in system in which the donation decision is made by the individual or by his or her family.
Most current U.S. transplantations from deceased donors result from deaths determined by neurologic criteria. The donor-eligible deaths determined by neurologic criteria—estimated to number between 10,500 and 16,800 per year—represent only a small fraction of the more than 2 million annual deaths in the United States (Guadagnoli et al., 2003; Sheehy et al., 2003; NCHS, 2005). For deaths determined by neurologic criteria, organ viability can be maintained through ventilatory support and thereby improve opportunities for successful transplantation. Death determined by circulatory criteria is much more common in the population at large, but, because it often occurs outside of the hospital setting, maintaining the viability of the organs presents distinct challenges ( Chapter 5 ).
The Uniform Anatomical Gift Act (UAGA) of 1968 specified that the donor’s authorization to donate is legally binding, and the subsequent
amendment of UAGA in 1987 assigned explicit priority to the donor’s intent even if his or her family objected to donation. In several states, the individual’s decision to donate is recorded on an organ donor card, on the individual’s driver’s license, or in a donor registry and is as legally binding as an advance directive regarding end-of-life care (DHHS, 2000). In practice, however, organ donation and recovery involve a complex set of circumstances and decisions.
When the individual’s wishes regarding donation are not known, discussions between the family of the deceased individual and the OPO and hospital staff focus on the opportunity for donation and the family is asked to make a decision about donation. Families often view organ donation as a way to redeem an otherwise tragic situation; as a way to honor their loved one’s life, passions, and philosophies; and as a way to help others live. Despite such positive reasons to consider organ donation, historically only 50 percent of families asked to consent to organ donation do so (JCAHO, 2004). However, progress has been made both in identifying dying patients who would be potentially suitable donors and in obtaining family consent for donation. Gortmaker and colleagues (1998), examining 1990 data, found that 27 percent of eligible patients had not been identified as potential donors or the family had not been contacted. The study found that 48 percent of the families who were asked to donate their loved one’s organs consented to the donation and that 33 percent of the deceased persons who were potential donors became actual donors. This contrasts with data collected between 1997 and 1999 by Sheehy and colleagues (2003), who found that only 16 percent of eligible patients were not identified as potential donors. Results from the latter study showed that 54 percent of the families who were asked to donate consented and that 42 percent of the potential donors became actual donors. These results suggest substantial improvements over the course of the decade, and consent rates have continued to improve in recent years. The process of organ donation is outlined in Figure 1-3 .
It is difficult to determine the uppermost potential for the number of deceased organ donors. Efforts to date have focused on estimating the number of potential deceased organ donors with neurologic determination of death. However, the potential pool also includes a large number of individuals whose deaths are determined by circulatory criteria, although estimating the number of such potential donors is a complex task (see Chapter 5 ).
Guadagnoli and colleagues (2003) estimated the number of potential deceased organ donors (neurologic determination of death) in the United States in 1998 to be 16,796; the actual number of deceased donors in 1998 was 5,793. This analysis used hospital case-mix data, hospital bed size, medical school affiliation, and status as a trauma center to estimate the

FIGURE 1-3 Process of organ donation.
SOURCE: Adapted from Delmonico et al. (2005). Reprinted with permission from Blackwell Publishing.
number of potential organ donors per hospital and then aggregated the data for each OPO. Because of variations in demographics, the number of eligible hospitals, and other factors, there is wide variation in the number of donations that a single OPO works with each year (in 2004 ranging from 13 to 387 donors) (HRSA and SRTR, 2006).
Sheehy and colleagues (2003) reviewed hospital medical records of deaths submitted by 36 OPOs from 1997 through 1999. Forms were completed for deaths occurring in hospital intensive care units for all individuals who met the neurologic criteria for death and who were 70 years of age or younger. That study estimated that each year in the United States there is a national pool of 10,500 to 13,800 potential donors for whom death is determined by neurologic criteria.
As seen in data from 2002 and 2003 ( Table 1-1 ), the annual pool of eligible donors with neurologic determination of death has numbered approximately 12,000.
In 2003, there were approximately 2.4 million deaths in the United States; of those approximately 1 million deaths were of individuals age 15 to 74 years (NCHS, 2005). Despite a number of coexisting conditions that would preclude organ donation, a comparison of the number of potential eligible donors with the number of actual donors ( Table 1-2 ) shows that there could well be a large number of additional donors if technologies and systems are developed in the future to keep organs viable. This would include an increased focus on donation after circulatory determination of death ( Chapter 5 ). Furthermore, issues regarding organs that are recovered but that are not used have yet to be fully explored ( Chapter 2 ; Delmonico et al., 2005).
TABLE 1-1 Eligible, a Actual, and Additional Donors, 2002 and 2003
TABLE 1-2 Deceased Organ Donors, Potential Versus Actual
Transplant Recipients
Transplant recipients probably know best the real value of increasing the numbers of donated organs: an extended lifetime, improved quality of life, and a chance to resume activities that would have been precluded without a transplant. A 10-year overall increase in life expectancy is reported for kidney transplant recipients compared with the life expectancy
for individuals on transplant waiting lists (Wolfe et al., 1999). Transplant recipients not only experience gains in life expectancy but also enjoy improvements in the quality of their lives. A literature review of 218 independent studies involving approximately 14,750 transplant recipients demonstrated statistically significant improvements in physical functioning, mental health, social functioning, and overall perceptions of quality of life following transplantation (Dew et al., 1997). These improvements are particularly striking when they are contrasted with the pretransplant conditions of patients requiring a transplant, such as the health complications and difficulties associated with long-term dialysis and other medical interventions. Moreover, many individuals face imminent death without a transplant. The lack or inferiority of alternative therapies should be considered when post-transplant quality-of-life data are evaluated (Whiting, 2000).
Other factors may have negative effects on a patient’s quality of life posttransplantation. The financial burden of immunosuppression therapy is thought to play a significant role in patient noncompliance with treatment regimens (Chisholm et al., 2000), which may eventually lead to rejection of the transplant and the need for other therapies or retransplantation. 4 Physical side effects and the psychological and social issues that a patient encounters following a transplantation must also be considered. Improved immunosuppression protocols and the provision of patient education and support services have been recommended as ways to promote positive outcomes and enhance the quality of life for transplant recipients (Galbraith and Hathaway, 2004).
INTERNATIONAL PERSPECTIVE
Most countries around the globe also face such problems as long waiting lists for organ transplantation and challenges with the allocation of scarce organs. In the last decade, organ donation systems, transplantation programs, and organ exchange organizations have received increasing resources and attention from governmental agencies. In some countries, such as Spain and France, the government itself operates those organizations. In other countries, such as the United Kingdom, the organ donation and allocation efforts remain in control of a nongovernmental body affiliated with the nation’s department of health. Most countries (e.g., Austria, Belgium, Denmark, Sweden, Germany, and The Netherlands) continue to operate a quasipublic system. Most organ exchange organizations operate on a na-
tional basis. However, the Eurotransplant International Foundation serves Austria, Belgium, Germany, Luxembourg, The Netherlands, and Slovenia; UK Transplant serves the United Kingdom and Ireland; and Scandiatransplant serves Denmark, Finland, Iceland, Norway, and Sweden.
Bolstering the infrastructure for organ donation and transplantation has been a major focus in a number of countries. In recent years Spain has been successful in significantly increasing its donor rates. Among the major changes instituted in Spain are an active donor detection program conducted by well-trained transplantation coordinators; an extensive transplant coordination network linking national, regional, and hospital efforts; hospital-level coordinators; increased economic reimbursement for hospitals; professional and public education efforts; systematic death audits conducted in hospitals; and a focus on expanded-criteria donors and on donation after circulatory determination of death (Matesanz, 1998, 2003, 2004).
Cross-country comparisons of donation rates are generally based on the number of donors per million population, a measure that has been criticized because of inconsistent definitions ( Box 1-2 ). According to a report by the Council of Europe, Spain had the highest number of deceased donors per million population (34.6) in 2004, with the United States having 24.1 per million population (Council of Europe, 2005) ( Figure 1-4 ). However, it is difficult to draw accurate or meaningful international comparisons, even for those countries closely aligned geographically, politically, and socioeconomically. A combination of factors influences the effective-

FIGURE 1-4 Numbers of deceased donors per million population for various countries, 2004.
SOURCE: Council of Europe (2005).
ness of a given country’s response to organ donation and transplantation: history; political philosophy; social, legal, and cultural factors; economics; and medical professional practices.
In many countries, explicit consent is needed for organ donation. Countries with opt-in policies include the United States, Canada, United Kingdom, Germany, The Netherlands, and New Zealand (Abadie and Gay, 2004).
An alternative approach used by a number of countries is a presumed-consent or an opt-out approach, in which the default policy is that citizens are presumed to be organ donors unless they have expressly opted out of the system ( Chapter 7 ). Opt-out or presumed-consent structures enable either verbal or computer registration of an individual’s objection to organ donation. This is applied with various degrees of strictness. Some countries follow a strict or strong presumed-consent model with little to no role for the family in the organ donation decision-making process. Other countries have a presumed-consent law, but in practice the donor family is involved in the consent process. For example, this is the case in Belgium, Bulgaria, Croatia, Spain, Italy, France, and Sweden (Abadie and Gay, 2004).
Ethical, Social, and Cultural Issues
The ethical issues surrounding transplantation have come under close scrutiny in most countries, and legislation has gradually been introduced to
regulate the transplantation process and to protect donors. Trust in a country’s medical establishment is crucial, however. For example, the relatively low rate of donation in Brazil has been attributed, in part, to distrust of the medical community. Brazil has a large underclass with poor access to health care, and the quality of health care varies greatly. When a new policy of presumed consent was established, Brazilians reported difficulties, even obstacles, in registering as nondonors, further fueling fears that the healthcare system authorities were not to be trusted (McDaniels, 1998). The presumed-consent statute was subsequently repealed.
There are wide differences in the policies and statutes regarding living donation among various countries. For example, Iran has a government-regulated program that compensates and monitors living unrelated kidney donors (Ghods, 2004), whereas many other countries prohibit the exchange of money for transplantable organs.
Cultures vary in the extent to which people are willing to donate their own organs and the organs of their deceased relatives (Sanner et al., 1995). Repeated surveys in Sweden have shown that about 66 percent of the public supports donation, but only 40 percent would consent to removal of a relative’s organs if the wishes of the deceased were not known (Sanner, 1994). A common problem across cultures, however, is that few individuals have informed their families of their wishes, and where donor cards are available, even fewer have signed them (Sanner et al., 1995).
Cultures have different views and traditions about death, and there have been significant debates about the determination of death by neurologic criteria. In Denmark in the 1980s and Germany in the 1990s, many believed that prolonged public debates over the determination of death by neurologic criteria led to declines in organ donation rates (Matesanz, 1998). In Japan, cultural and religious beliefs, particularly those associated with the wholeness of nature and of the human body, have played a role in resistance to the determination of death by neurologic criteria. Under a law adopted in 1997 in Japan, death is pronounced by neurologic criteria only in cases of organ donation and only for those who consented, while they were alive, to organ donation and to the use of brain-based criteria (Veatch, 2000). The next of kin must also give their consent to organ procurement and agree to the pronouncement of death (Fitzgibbons, 1999).
Cultural and religious traditions and beliefs about the treatment of the dead body, beliefs about life after death, and fears of mutilation can also influence decisions about organ donation. The major tenets of nearly all religious traditions, however, are compatible with the practice of organ donation ( Chapter 2 ). Yet, religious beliefs are often invoked in expressing resistance to organ donation, perhaps in part reflecting differences between official religious policies and folk beliefs and practices.
TERMINOLOGY
Because the concepts and processes of organ donation are so closely intertwined with emotional issues of death and dying, it is of utmost importance to the committee, as it is to the transplantation community, that the terminology used to describe and discuss all aspects of organ transplantation be both as accurate and as sensitive as possible. Terminology in this field has had both positive and negative connotations. On the one hand, some terms have played a role in creating or propelling myths, have led to increased misconceptions and fears about organ and tissue donation, or have bred mistrust of the system in general. Other terms have a more positive role in the healing process of a hurting family and in motivating the public to agree to donation. The National Donor Family Council and numerous recipient and donor family organizations have been active in addressing terminology.
Some terms that have seemed descriptive or useful in the past are now being reconsidered in favor of terms that are sensitive to the donor family and that affirm the value of individual human life (see Table S-1 in the Summary ). In the past, the term donor did not require any specificity. Today, as more people choose to become living donors, there is a need to distinguish between living and deceased donors. The term cadaveric has been used in the past but has an impersonal connotation (a dead body intended for dissection). The term deceased donor is preferred because it conveys a more positive message and also denotes that it is a donation by an individual human being.
Although the medical community has used the term harvest , it has agricultural and impersonal connotations for the general public. Similarly, the word retrieval suggests the reclamation of an object and can be quite unpalatable, especially to donor families. The preferred word, recovery , helps people to understand that the removal of a loved one’s organs for transplantation is a respectful surgical procedure. The word receive might even be more appropriate because it highlights the gift relationship. Even though the term procure is widely used, it is also receiving close scrutiny. This term, similar to retrieve , has an impersonal connotation that does not fit with the intensely personal and emotional decisions regarding the end of a human life.
The term life support can be a confusing term for a family who has been notified that their loved one is dead. When death occurs, there is no support that can make the individual alive again. After the declaration of death by neurologic criteria, if there is consent for organ donation, the organs may be perfused with oxygen for several hours through mechanical support. Mechanical support and ventilated support are appropriate terms for the support given a deceased person’s organs in the event of organ donation.
Further confusing to families in times of crisis are the terms brain death and cardiac death . To some, these terms imply that certain organs have died but do not convey that this is a final determination of death. In order to avoid such confusions, the committee recommends use of the word death , adding either circulatory determination of death or neurologic determination of death where it is important to have greater specificity. Instead of donation after cardiac death and donation after brain death , the committee believes it would be clearer to use the phrases donation after circulatory determination of death (DCDD) and donation after neurologic determination of death (DNDD). Even though these phrases are more cumbersome, they better convey the finality of death and provide additional information on how that death was declared.
As terms continue to evolve, the committee urges all who are involved in organ transplantation to use words and phrases that clarify rather than mystify the process of organ transplantation and that affirm the value of each individual human life.
It is also important at the outset of this report to clarify the measures of deceased donation that the committee used. The consent rate is defined as the number of patients for whom consent is granted for organ donation (permission may be granted by the individual donor while he or she is alive or by the donor’s family after death) per the total number of patients eligible to be donors. The donation rate (also termed the conversion rate ) is the number of actual donors (i.e., the organs are removed for transplantation) per the total number of individuals eligible to be donors. The consent rate can be slightly higher than the donation (or conversion) rate, since after consent is obtained it might be determined that the organs are not suitable for recovery. Both of these measures have focused on donation after neurologic determination of death. As the measures are currently defined, the denominator for each excludes patients who are eligible for donation after circulatory determination of death. The implications of this approach are further discussed in Chapter 5 .
U.S. EFFORTS TO INCREASE ORGAN DONATION
Current efforts in the United States to increase rates of organ donation involve the collective work of numerous governmental and private-sector organizations. This section provides a brief overview of ongoing efforts. The chapters that follow provide further insights into the many parties that enable, facilitate, and promote organ donation.
HRSA is a major federal funder of research and initiatives to increase organ donation rates in the United States. HRSA’s Division of Transplantation is responsible for administering the federal contracts for OPTN and for the Scientific Registry of Transplant Recipients, which collects and analyzes
data on solid-organ transplant recipients. In addition to this operational role, HRSA works to increase organ donation rates through three major avenues: an extramural grants program, which funds model interventions, including social and behavioral, media-based, and clinical interventions ( Appendix E ); the Organ Donation Breakthrough Collaboratives, an ongoing initiative that emphasizes quality improvement and that focuses on improving hospital and OPO collaborations and encouraging best practices in organ donation ( Chapter 4 ); and additional Gift of Life initiatives, including efforts in workplaces, schools, and driver’s education centers, as well as model donor card, donor registry, and similar projects ( Chapter 6 ). In recent years, the level of funding for HRSA’s Division of Transplantation has decreased, with a significant reduction encountered in fiscal year 2006 ( Table 1-3 ). The potential impact of these budget reductions on organ donation efforts is of concern.
The National Institutes of Health (NIH) funds grants for organ transplantation research that primarily focus on biomedical studies of improvements in surgical techniques for transplantation, understanding immune-related processes, and improving graft survival. Additionally, and to a more limited extent, NIH funds have been applied to behavioral research on organ donation. In fiscal year 2005, the National Institute of Diabetes & Digestive & Kidney Diseases (NIDDK) supported research grants primarily aimed at raising awareness of organ donation in minority communities and improving the role of healthcare professionals in encouraging donation. In addition to these grants, NIDDK and the National Center on Minority Health and Health Disparities support the National Minority Organ and Tissue Transplant Education Program ( Chapter 6 ).
The Centers for Medicare & Medicaid Services (CMS) has the regulatory authority to certify OPOs and hospitals that perform transplantations
TABLE 1-3 Funding History, HRSA Division of Transplantation
for participation in Medicare. CMS administers the End-Stage Renal Disease Program and is active in ensuring quality improvements in transplantation programs.
States play an important role in promoting organ donation through legislative action (e.g., anatomical gift acts and the criteria used for the determination of death), the funding and implementation of organ donor registries ( Chapter 6 ), drivers’ license registration options for organ donation, and other programs (Gilmore et al., 2001). Some states have mandated that information on organ donation be provided as a part of high school driver’s education curriculum.
One of the key responsibilities of OPOs is “educating the public about the critical need for organ donation” (UNOS, 2006). OPOs work closely with donor families, transplant recipients, and others in a range of donation efforts.
In addition, numerous voluntary health organizations focus on public education about organ donation and the provision of support for donor families, living donors, and transplant recipients. For example, the Coalition on Donation is a not-for-profit alliance of national organizations and local coalitions across the United States that have joined forces to educate the public about organ, eye, and tissue donation (Coalition on Donation, 2004). The National Kidney Foundation and similar organizations that focus on relevant diseases and organ systems also support research and efforts for public and professional education. Other organizations, such as the National Donor Family Council, support the needs of donor families, assist the healthcare professionals who work most closely with these families, and raise public awareness.
The Joint Commission on Accreditation of Healthcare Organizations has promoted organ donation efforts by incorporating policies and procedures on the identification and referral of potential donors into hospital accreditation standards.
Professional organizations, including the Association of Organ Procurement Organizations, the American Society of Transplantation, the American Society of Transplant Surgeons, and the Organization for Transplant Professionals, are active in professional education and also work to promote organ donation through advocacy and public education efforts.
THE ECONOMIC VALUE OF INCREASING THE ORGAN SUPPLY
Numerous clinical studies have documented the benefit to patients of organ transplantation in terms of life expectancy and quality of life. Increasing the rates of organ donation would provide these benefits to more patients and would reduce the waiting time for many transplant recipient candidates. Policies that increase the organ supply also entail monetary and
nonmonetary costs. In deciding whether to pursue these policies, it is helpful to know whether the benefits to patients in terms of life expectancy and quality of life outweigh the costs and whether the cost per unit of health gained is low (or, alternatively, the “value” is high) compared with the value of other policies that are implemented to improve health.
The literature on the cost-effectiveness of transplantation provides indirect evidence of the economic value of increasing the organ supply. Kidney transplantation has been estimated to be highly cost-effective compared with the cost of dialysis (Winkelmayer et al., 2002) and is probably cost saving (Matas and Schnitzler, 2003; Whiting et al., 2004). Estimates of the cost-effectiveness of nonrenal transplantation are more variable (Ramsey et al., 1995; Cope et al., 2001; Sagmeister et al., 2002; Longworth et al., 2003; Ouwens et al., 2003). Most of these studies find that the cost per life year gained is less than commonly cited estimates of the value of a life year (Richardson, 2003), although cost data are often incomplete and, for studies based on transplants occurring in European countries, may not be generalizable to the United States. Most of these studies find that the cost per year of life gained is less than $100,000, although the data required for cost-effectiveness studies of nonrenal transplantation are often incomplete.
Several studies have directly addressed the economic value of increasing organ donation. Matas and Schnitzler (2003) estimate that every additional kidney donation from a living donor reduces total spending by more than $90,000. Mendeloff and colleagues (2004) used published estimates of the costs of and quality-adjusted life years gained from kidney, liver, and heart transplants to calculate the monetary value to society of a deceased organ donor, assuming that each donation results in 1.55 kidney transplants, 0.37 heart transplants, and 0.76 liver transplants. They estimated that a deceased organ donor is associated with a gain to transplant recipients of 13 quality-adjusted life years (summed across the transplanted organs) and a $200,000 increase in healthcare spending, although that figure is based on a conservative value of the cost savings from kidney transplantation (Schnitzler et al., 2005a). If it is assumed that a life year is worth $100,000, their “central” estimate is that each donor is worth $1,086,000 to society, or $1,800,000 when their best-case estimates of cost savings and life years gained are used.
Interpretation of the findings of these studies requires one note of caution, however, in that they are based on historical outcomes data, and the patients who would gain access to transplantation as a result of an increased organ supply may differ systematically from patients who currently receive a transplant. For example, in the case of liver transplantation, in which organs are allocated according to a “sickest first” priority rule, an increased supply would allow physicians to perform transplantations for healthier patients, who, under current supply constraints, must wait until
their health declines before they reach the top of the waiting list. Because the cost-effectiveness of transplantation varies widely by age group (Jassal et al., 2003, Schnitzler et al., 2003), primary diagnosis (Longworth et al., 2003; Groen et al., 2004), and other factors, knowledge of the characteristics of the patients who will receive additional organs is important for estimation of the impact of efforts to increase the organ supply. Schnitzler and colleagues (2005b) have made progress on this front by measuring the life years gained from transplantation on the basis of the pretransplantation death rates of patients near the top of each organ-specific waiting list. They have found that an additional deceased organ donor yields a gain of 30.8 life years for these patients (summed across the transplanted organs), assuming that each donation results in 1.4 kidney transplants, 0.80 liver transplants, 0.20 lung transplants, and 0.30 heart transplants. For the case of livers, an analysis by Gibbons and colleagues (2003) suggests that urgent patients (status 1, under the old classification system) derive a greater benefit from transplantation than nonurgent patients.
An increase in the organ supply will increase the number of patients who receive transplants, but even when the number of transplantations is held fixed, an increase in the supply will reduce the waiting times for patients who would eventually receive a transplant anyway. A number of studies indicate that longer waiting times are associated with worse outcomes (Everhart et al., 1997; Howard, 2000; Meier-Kriesche and Kaplan, 2002). It may be possible, however, to provide transplants to patients too early in the course of their disease, in the sense that the benefit of the reduced waiting time is outweighed by the immediate risk of postoperative mortality (Kim and Dickson, 2000; Alagoz et al., 2004).
A number of secondary effects of increasing the organ supply should be considered when the value of increasing donation rates is assessed, although these have not been well documented. If the organ supply increases, providers may place more patients on the waiting list, particularly those who are less likely to benefit from transplantation. Physicians may also become reluctant to use low-quality organs (Howard, 2002).
In evaluating the payoffs from increasing the organ supply, it is important to remember that cost-effectiveness studies are approximations and that some nonmonetary costs and benefits are not easily quantified. Moreover, policies that are implemented to increase the supply of organs must be compared with other opportunities to improve the length and quality of life through public policy. In a country in which so many people have limited access to effective health care, many unexploited opportunities to obtain quality-adjusted life years at a low cost probably exist. Nevertheless, with these caveats in mind, the committee concludes that the available data suggest that well-designed policies to increase deceased and living organ donation are potentially cost-effective and even cost saving.
EMPHASIS ON PREVENTION
In considering the total picture of organ transplantation, it is helpful to step back and examine each of the points at which interventions and initiatives could make a difference in equalizing the supply and the demand for organs for transplantation. The focus of the committee’s task—and thus, the focus of this report—is on increasing the supply of donated organs. However, reducing the demand for organ transplantation would be even more effective, because it would mean that greater numbers of healthier individuals have not reached the point of needing an organ transplant. In general, transplantation should be seen as a rescue technology; it is an invaluable resource and option when it is needed, but prevention measures leading to improved health status are the first line of defense to avoid, where possible, the need for transplantation. The committee recognizes that not all causes of organ deterioration and failure can be prevented; however, for those cases in which prevention could make a difference, it is important to begin to implement preventive interventions at the earliest time possible and to minimize the rejection of the transplanted organ(s).
Transplantation occurs at the end of a continuum of symptoms, diagnoses, treatments, and interventions. The prevention framework of public health, with insights from the Haddon matrix (a model originally developed to address injury prevention), provides a context for considering the numerous points at which interventions could improve health status and reduce the demand for transplantation ( Table 1-4 ).
If transplantation is considered the event, then pre-event measures and interventions could focus on efforts to prevent the onset of disease or minimize its outcomes so that it will not reach the point of requiring transplantation. Examples of pre-event interventions include education on healthy lifestyles and screenings for stroke, diabetes, and high blood pressure. Event interventions focus on high-quality care for the patient during transplantation and the provision of support to the patient and family so that they understand the transplantation procedures and the necessity for follow-up. In the third phase—the post-event phase—the focus is on restoring lost function and former quality of life, with particular attention to access to immunosuppressive therapies and ensuring that the donated and transplanted organ is fully maintained so that retransplantation is not necessary.
The goal, of course, is to minimize the need for organ transplantation by preventing the underlying disease risk factors that lead to organ deterioration and failure. Although not all the medical conditions necessitating organ transplantation can be prevented, preventive interventions and the treatment of contributory diseases as early as possible have the potential to reduce significantly the demand for organ transplantation.
TABLE 1-4 Organ Transplantation Prevention Matrix
ON THE HORIZON
A variety of technological advances in development might improve organ viability or diminish the need for living or deceased organ donation. Ongoing research on organ preservation and organ culture is examining methods to improve organ function and viability. Nanotechnology offers the potential for the insertion of implantable devices that would restore organ function or serve as an organ replacement. For example, mechanical devices such as the left ventricular assist device currently serve as a bridge for those waiting for a heart transplant, but refinements or reengineering
may permit them to be used as a long-term alternative to or replacement for transplantation. Xenotransplantation (transplantation of an organ between two different species) has been an ongoing area of research and has some current clinical applications (e.g., heart valve transplants from pigs). However, the use of organs or tissues from other species continues to encounter biological barriers regarding immunosuppression, organ rejection, and disease transmission as well as the psychosocial concerns of some individuals regarding the use of organs from animals. Stem cell research offers the promise of repairing or restoring organ function in the near future.
Other technologic developments are raising new ethical questions. Organs such as the face and the ovary have been transplanted with some success and raise ethical concerns about identity and reproductive lineage. It is too early to determine if and how public attitudes regarding these developments will impact rates of organ donation.
Until the time that preventive measures diminish the need for transplantation or alternative approaches offer an effective option, numerous families, healthcare and transplantation professionals, and many others continue to make extraordinary efforts each day to ensure that organs are donated and are successfully transplanted with the goal of improving the quality of life and the length of life for transplant recipients.
OVERVIEW OF THIS REPORT
The large gap between the supply and the demand for solid organs has prompted the need to carefully examine a variety of policy, organizational, and institutional changes that might be made to increase rates of organ donation. As discussed in Chapter 2 and throughout the report, a variety of factors influence an individual’s or a family’s decision making regarding organ donation.
This report examines a range of proposals for increasing deceased organ donation ( Table 1-5 ) and briefly discusses some ethical concerns raised by living donation. The committee’s framework—perspectives and principles—for considering these proposals is provided in Chapter 3 . The subsequent chapters examine changes in the organization, processes, and interactions of hospitals and OPOs ( Chapter 4 ); expanding the pool of potential organ donors through donation after circulatory determination of death ( Chapter 5 ); and individual decision making, public education, and research ( Chapter 6 ). Opt-out policies, particularly presumed consent, are discussed in Chapter 7 , and Chapter 8 focuses on financial and nonfinancial incentives. Living donation is discussed in Chapter 9 , and the report concludes in Chapter 10 with a synopsis of the opportunities for action to increase organ donation.
TABLE 1-5 Several Approaches to Increasing Deceased Organ Donation, Issues Examined in This Report
Abadie A, Gay S. 2004. The Impact of Presumed Consent Legislation on Cadaveric Organ Donation: A Cross Country Study. [Online]. Available: http://ksghome.harvard.edu/~aabadie/pconsent.pdf [accessed March 15, 2006].
Alagoz A, Maillart LM, Schaefer AJ, Roberts M. 2004. The optimal timing of living-donor liver transplantation. Management Science 50(10):1420–1430.
Bernat JS. 2005. The concept and practice of brain death. Progress in Brain Research 150: 369–379.
Chisholm MA, Vollenweider LJ, Mulloy LL, Jagadeesan M, Wynn JJ, Rogers HE, Wade WE, DiPiro JT. 2000. Renal transplant patient compliance with free immunosuppressive medications. Transplantation 70(8):1240–1244.
Coalition on Donation. 2004. Who We Are. [Online]. Available: http://www.shareyourlife.org/contact_who.html [accessed August 9, 2005].
Cope JT, Kaza AK, Reade CC, Shockey KS, Kern JA, Tribble CG, Kron IL. 2001. A cost comparison of heart transplantation versus alternative operations for cardiomyopathy. Annals of Thoracic Surgery 72(4):1298–1305.
Council of Europe. 2005. International figures on organ donation and transplantation. Transplant Newsletter 10(1).
Delmonico FL, Sheehy E, Marks WH, Baliga P, McGowan JJ, Magee JC. 2005. Organ donation and utilization in the United States, 2004. American Journal of Transplantation 5(4 Pt 2):862–873.
DeVita MA, Snyder J, Grenvik A. 1993. History of organ donation by patients with cardiac death. Kennedy Institute of Ethics Journal 3(2):113–129.
Dew MA, Switzer GE, Goycoolea JM, Allen AS, DiMartini A, Kormos RL, Griffith BP. 1997. Does transplantation produce quality of life benefits? A quantitative analysis of the literature. Transplantation 64(9):1261–1273.
DHHS (U.S. Department of Health and Human Services), Office of the Assistant Secretary for Planning and Evaluation. 2000. Analysis of State Actions Regarding Donor Registries. Prepared by The Lewin Group, Inc. [Online]. Available: http://www.organdonor.gov/aspehealth.html [accessed April 3, 2006].
DHHS, Office of the Inspector General. 2003. Variation in Organ Donation Among Transplant Centers. OEI-01-02-00210. Washington, DC: DHHS.
Eggers PW. 2000. Medicare’s end stage renal disease program. Health Care Financing Review 22(1):55–60.
Everhart JE, Lombardero M, Detre KM, Zetterman RK, Wiesner RH, Lake JR, Hoofnagle JH. 1997. Increased waiting time for liver transplantation results in higher mortality. Transplantation 64(9):1300–1306.
Fitzgibbons SR. 1999. Cadaveric organ donation and consent: A comparative analysis of the United States, Japan, Singapore, and China. ILSA Journal of International and Comparative Law 6:73.
Galbraith CA, Hathaway D. 2004. Long-term effects of transplantation on quality of life. Transplantation 77(9):S84–S87.
Ghods AJ. 2004. Changing ethics in renal transplantation: Presentation of Iran model. Transplantation Proceedings 36(1):11–13.
Gibbons RD, Duan N, Meltzer D, Pope A, Penhoet E, Dubler N, Francis C, Gill B, Guinan E, Henderson M, Ildstad S, King PA, Martinez-Maldonado M, Mclain GE, Murray J, Nelkin D, Spellman MW, Pitluck S. 2003. Waiting for organ transplantation: Results of an analysis by an Institute of Medicine committee. Biostatistics 4:207–222.
Gilmore L, Matthews T, McBride VA. 2001. State Strategies for Organ and Tissue Donation: A Resource Guide for Public Officials. Rockville, MD: Health Resources and Services Administration.
Gortmaker SL, Beasley CL, Sheehy E, Lucas BA, Brigham LE, Grenvik A, Patterson RH, Garrison N, McNamara P, Evanisko MJ. 1998. Improving the request process to increase family consent for organ donation. Journal of Transplant Coordination 8(4): 210–217.
Groen H, van der Bij W, Koeter GH, TenVergert EM. 2004. Cost-effectiveness of lung transplantation in relation to type of end-stage pulmonary disease. American Journal of Transplantation 4(7):1155–1162.
Guadagnoli, E, Christiansen CL, Beasley CL. 2003. Potential organ-donor supply and efficiency of organ procurement organizations. Health Care Financing Review 24(4): 101–110.
Guidelines for the determination of death. 1981. Report of the medical consultants on the diagnosis of death to the President’s Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Journal of the American Medical Association 246(19):2184–2186.
Halloran PF, Gourishankar S. 2001. Historical overview of pharmacology and immunosuppression. In: Norman DJ, Turka LA, eds. Primer on Transplantation , 2nd ed. Mt. Laurel, NJ: American Society of Transplantation. Pp. 73–75.
Howard DH. 2000. The impact of waiting time on liver transplant outcomes. Health Services Research 35(5):1117–1134.
Howard DH. 2002. Why do transplant surgeons turn down organs? A model of the accept/ reject decision. Journal of Health Economics 21(6):931–1094.
HRSA (Health Resources and Services Administration) and SRTR (Scientific Registry of Transplant Recipients). 2005. 2004 Annual Report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1994–2003 . [Online]. Available: http://www.optn.org/AR2004/default.htm [accessed March 30, 2006].
HRSA and SRTR. 2006. 2005 Annual Report of the U.S. Organ Procurement and Transplantation Network and the Scientific Registry of Transplant Recipients: Transplant Data 1995–2004 . [Online]. Available: http://www.optn.org/AR2005/default.htm [accessed March 3, 2006].
IOM (Institute of Medicine). 1997. Non-Heart-Beating Organ Transplantation: Medical and Ethical Issues in Procurement. Washington, DC: National Academy Press.
IOM. 1999. Organ Procurement and Transplantation: Assessing Current Policies and the Potential Impact of the DHHS Final Rule. Washington, DC: National Academy Press.
IOM. 2000. Non-Heart-Beating Organ Transplantation. Practice and Protocols. Washington, DC: National Academy Press.
Jassal SV, Krahn MD, Naglie G, Zaltzman JS, Roscoe JM, Cole EH, Redelmeier DA. 2003. Kidney transplantation in the elderly: A decision analysis. Journal of the American Society of Nephrology 14(1):187–196.
JCAHO (Joint Commission on Accreditation of Healthcare Organizations). 2004. Health Care at the Crossroads: Strategies for Narrowing the Organ Donation Gap and Protecting Patients. [Online]. Available: http://www.jointcommission.org/NR/rdonlyres/E4E7DD3F-3FDF-4ACC-B69E-AEF3A1743AB0/0/organ_donation_white_paper.pdf [accessed March 30, 2006].
Kim WR, Dickson ER. 2000. Timing of liver transplantation. Seminars in Liver Disease 20(4):451–464.
Laureys S. 2005. Science and society: Death, unconsciousness and the brain. Nature Reviews. Neuroscience 6(11):899–909.
Longworth L, Young T, Buxton MJ, Ratcliffe J, Neuberger J, Burroughs A, Bryan S. 2003. Midterm cost-effectiveness of the liver transplantation program of England and Wales for three disease groups. Liver Transplantation 9(12):1295–1307.
Matas AJ, Schnitzler M. 2003. Payment for living donor (vendor) kidneys: A cost-effectiveness analysis. American Journal of Transplantation 4(2):216–221.
Matesanz R. 1998. Cadaveric organ donation: Comparison of legislation in various countries of Europe. Nephrology Dialysis Transplantation 13(7):1632–1635.
Matesanz R. 2003. Factors influencing the adaptation of the Spanish model of organ donation. Transplant International 16(10):736–741.
Matesanz R. 2004. Factors that influence the development of an organ donation program. Transplantation Proceedings 36(3):739–741.
McDaniels A. 1998 (January 16). Brazil mandates organ “donation” for transplants. Christian Science Monitor. p. 1.
Meier-Kriesche HU, Kaplan B. 2002. Waiting time on dialysis as the strongest modifiable risk factor for renal transplant outcomes: A paired donor kidney analysis. Transplantation 74(10):1377–1381.
Mendeloff J, Ko K, Roberts MS, Byrne M, Dew MA. 2004. Procuring organ donors as a health investment: How much should we be willing to spend? Transplantation 78(12): 1704–1710.
Merrill JP, Murray JE, Harrison JH, Guild WR. 1956. Successful homotransplantation of the human kidney between identical twins. Journal of the American Medical Association 160(4):277–282.
Morrissey PE, Madras PN, Monaco AP. 2001. History of kidney and pancreas transplantation. In: Norman DJ, Turka LA, eds. Primer on Transplantation , 2nd ed. Mt. Laurel, NJ: American Society of Transplantation. Pp. 411–413.
NCCUSL (National Conference of Commissioners on Uniform State Laws). 2005. A Few Facts About the Anatomical Gift Act (1987). [Online]. Available: http://www.nccusl.org/Update/uniformact_factsheets/uniformacts-fs-aga87.asp [accessed April 13, 2006].
NCHS (National Center for Health Statistics). 2005. Deaths: Preliminary data for 2003. National Vital Statistics Reports 53(15). Hyattsville, MD: National Center for Health Statistics.
OPTN (Organ Procurement and Transplantation Network). 2004. OPTN Charter. [Online]. Available: http://www.optn.org/ContentDocuments/OPTN_CHARTER_II_-_NOV_04.pdf [accessed January 20, 2006].
OPTN. 2006. National Data Reports. [Online]. Available: http://www.optn.org/latestData/step2.asp? [accessed March 29, 2006].
Ouwens JP, van Enckevort PJ, TenVergert EM, Bonsel GJ, van der Bij W, Haagsma EB, Rutten FF, Slooff MJ, Koeter GH. 2003. The cost effectiveness of lung transplantation compared with that of heart and liver transplantation in The Netherlands. Transplant International 16(2):123–127.
Ramsey SD, Patrick DL, Albert RK, Larson EB, Wood DE, Raghu G. 1995. The cost-effectiveness of lung transplantation. A pilot study. University of Washington Medical Center Lung Transplant Study Group. Chest 108(6):1594–1601.
Report of the Ad Hoc Committee of the Harvard Medical School to Examine the Definition of Brain Death. 1968. A definition of irreversible coma. Journal of the American Medical Association 205(6):85–88.
Richardson VE. 2003. Coverage does matter: The value of health forgone by the uninsured. In: Institute of Medicine. Hidden Costs, Value Lost: Uninsurance in America. Washington DC: The National Academies Press. Pp. 129–169.
Roels L. 2005 (June 20). International Perspective. Presentation at the Institute of Medicine Workshop on Increasing Rates of Organ Donation. Washington, DC. Institute of Medicine Committee on Increasing Rates of Organ Donation.
Sagmeister M, Mullhaupt B, Kadry Z, Kullak-Ublick GA, Clavien PA, Renner EL. 2002. Cost-effectiveness of cadaveric and living-donor liver transplantation. Transplantation 73(4):616–622.
Sanner M. 1994. A comparison of public attitudes toward autopsy, organ donation, and anatomic dissection. A Swedish survey. Journal of the American Medical Association 271(4):284–288.
Sanner MA, Hedman H, Tufveson G. 1995. Evaluation of an organ-donor-card campaign in Sweden. Clinical Transplantation 9(4):326–333.
Schnitzler MA, Whiting JF, Brennan DC, Lin G, Chapman W, Lowell J, Boxerman S, Hardinger KL, Kalo Z. 2003. The expanded criteria donor dilemma in cadaveric renal transplantation. Transplantation 75(12):1940–1945.
Schnitzler MA, Lentine KL, Burroughs TE. 2005a. The cost effectiveness of deceased organ donation. Transplantation 80(11):1636–1637.
Schnitzler MA, Whiting JF, Brennan DC, Lentine KL, Desai NM, Chapman W, Abbott KC, Kalo Z. 2005b. The life-years saved by a deceased organ donor. American Journal of Transplantation 5(9):2289–2296.
Sheehy E, Conrad SL, Brigham LE, Luskin R, Weber P, Eakin M, Schkade L, Hunsicker L. 2003. Estimating the number of potential organ donors in the United States. New England Journal of Medicine 349(7):667–674.
SRTR, 2005. National Reports: National Summary by OPO by Table, Table 3 (Measures of Donation Rates). [Online]. Available: http://www.ustransplant.org/csr/current/nats.aspx [accessed December 19, 2005].
UNOS (United Network for Organ Sharing). 2004. UNOS Celebrates 20th Anniversary. [Online]. Available: http://www.unos.org/news/newsDetail.asp?id=317 [accessed December 13, 2005].
UNOS. 2005. About Transplant Centers. [Online]. Available: http://www.unos.org/whoWeAre/transplantCenters.asp [accessed December 13, 2005].
UNOS. 2006. Who We Are. [Online]. Available: http://www.unos.org/whoWeAre/OPOs.asp [accessed January 20, 2006].
Veatch RM. 2000. Transplantation Ethics. Washington, DC: Georgetown University Press.
Whiting JF. 2000. Standards for economic and quality of life studies in transplantation. Transplantation 70(7):1115–1121.
Whiting JF, Kiberd B, Kalo Z, Keown P, Roels L, Kjerulf M. 2004. Cost-effectiveness of organ donation: Evaluating investment into donor action and other donor initiatives. American Journal of Transplantation 4(4):569–573.
Winkelmayer WC, Weinstein MC, Mittleman MA, Glynn RJ, Pliskin JS. 2002. Health economic evaluations: The special case of end-stage renal disease treatment. Medical Decision Making 22(5):417–430.
Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, Held PJ, Port FK. 1999. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. New England Journal of Medicine 341(23):1725–1730.
Youngner S, Anderson M, Shapiro R, eds. 2004. Transplanting Human Tissue: Ethics, Policy, and Practice. New York: Oxford University Press.
This page intially left blank
Rates of organ donation lag far behind the increasing need. At the start of 2006, more than 90,000 people were waiting to receive a solid organ (kidney, liver, lung, pancreas, heart, or intestine). Organ Donation examines a wide range of proposals to increase organ donation, including policies that presume consent for donation as well as the use of financial incentives such as direct payments, coverage of funeral expenses, and charitable contributions. This book urges federal agencies, nonprofit groups, and others to boost opportunities for people to record their decisions to donate, strengthen efforts to educate the public about the benefits of organ donation, and continue to improve donation systems. Organ Donation also supports initiatives to increase donations from people whose deaths are the result of irreversible cardiac failure. This book emphasizes that all members of society have a stake in an adequate supply of organs for patients in need, because each individual is a potential recipient as well as a potential donor.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
Switch between the Original Pages , where you can read the report as it appeared in print, and Text Pages for the web version, where you can highlight and search the text.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Organ Donation and Transplantation - Current Status and Future Challenges
Organ Donation and Transplantation: “Life after Death”
Submitted: 13 November 2017 Reviewed: 03 April 2018 Published: 25 July 2018
DOI: 10.5772/intechopen.76962
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Organ Donation and Transplantation - Current Status and Future Challenges
Edited by Georgios Tsoulfas
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
2,123 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Organ donation is defined as giving an organ or part of an organ to be transplanted into another person. Organ transplantation is the only option to save lives in patients affected by terminal organ failures and improve their quality of life. However, there is a disparity exists between the supply and demand of donated organs, leads to a loss of many lives. The number of organ transplantation have gradually increased in the last two decades and provide excellent results in children and young adults, and are challenging by the growing proportion of elderly transplant patients with co morbidity. The results of organ transplantation continue to improve, as a consequence of the innovations and the improvements in peri-operative management. This chapter describes organ donation and transplantation and its trends and challenges.
- organ donation
- psychosocial
Author Information
Kanmani job *.
- Amrita College of Nursing, Amrita Vishwa Vidyapeetham, Kochi, India
Anooja Antony
*Address all correspondence to: [email protected]
1. Introduction
Organ donation is defined as giving an organ or part of an organ to be transplanted into another person. Organ transplantation is the only option to save lives in patients affected by terminal organ failures and improve their quality of life. However, there is a disparity exists between the supply and demand of donated organs, leads to a loss of many lives. The number of organ transplantation have gradually increased in the last two decades and provide excellent results in children and young adults, and are challenging by the growing proportion of elderly transplant patients with co morbidity. The results of organ transplantation continue to improve, as a consequence of the innovations and the improvements in peri-operative management.
Organ transplantation currently depends on the availability of human organs. Their scarcity means that there is a waiting list of almost 63,000 in the European Union, and over 100,000 people in the United States according to the recent survey. The process of obtaining organs for donation and transplantation purely depends on the resources of health services and by health professionals’ performance in potential donor identification and management tasks. However, in accordance with the current legislation it is mainly subjected to a personal or family decision, strongly mediated by psychosocial processes. Therefore, the need to analyze and intervene both in the practices of the professionals involved in the process of organ generation and in the attitudes of the general population need to stressed and addressed [ 1 , 2 , 3 , 4 , 5 ].
2. Organ transplantation and organ donation: an overview
Organ transplantation involves the surgical implantation of an organ or section of an organ into a person whose own organ is failing. The donor organ may come from both deceased individual as well as from a living donor. The patients psychological and behavior aspect as well their emotional response and mental health and adherence to medical regimen should be assessed before and after organ transplantation. The living donor’s psychological response towards organ donation (most commonly for kidney and liver segment transplantation) is an important aspect to consider in the transplantation process.
Organ donation is defined as “giving an organ or part of an organ to be transplanted into another person” (Organ procurement of Transplant Network (OPTN), 2015), organ donation has the potential to save lives. The organs donated from one single donor can save up to eight lives. Organ transplantation may be one of the options left to sustain someone’s life. However, the disparity that exists between the supply and demand of donated organs, leads to a loss of many lives. Based on recent OPTN data, approximately 21 people will die each day while waiting for a transplant in the United States (US). Currently, 123, 358 people are awaiting organs and on the transplant list in the US with this number growing and the number of donated organs declining.
Asian Indians are more likely to have higher rates of having obesity and diabetes when compared with other Asian subgroups which make them at an increased risk of needing a donated organ [ 35 ]. These conditions can lead one to develop coronary artery disease and hypertension which then can lead to chronic kidney disease and other chronic illnesses. Patients who suffer from chronic kidney disease need regular dialysis which can ultimately lead them to organ transplantation to improve one’s quality of life. Also, conditions such as diabetes and obesity can be detrimental to one’s life and can lead to fatty liver disease which can lead to chronic liver disease requiring liver transplantation if the liver decompensates.
The development of organ transplantation in the second half of the 20th century has been a remarkable achievement. Recently; organ transplantation is one of the most effective options for those with an end-stage organ failure. Its success has been basically dependent on public awareness, support and active participation. Without these factors, the efficiency of organ transplantation and the consequent saving or extension of lives would have undoubtedly suffered adversely.
The number of patients in need of organ transplantation has increased at a rapid pace; in contrast, the number of available organs has increased only slightly. Expanded criteria for donor selection, such as older age, have resulted in more people who meet the criteria for brain death becoming organ donors although fewer organs are transplanted from each donor. Improvements in automobile and highway safety, as well as increased enforcement of gun control laws, have also contributed to a plateau in the number of young, healthy donors. Public education efforts that encourage organ donation may be effective in getting more people to sign organ donor cards, but most individuals who do so will never be in a position to become organ donors.
Faced with increasing numbers of patients who need transplantation, deaths on the waiting list, and a fixed number of available organs, some transplant programs are working to increase the number of transplants from living donors. Although living donation has always been an option for some types of transplants, many programs have been reluctant to promote it, as living donation requires invasive surgery on a healthy person with associated risks of morbidity and mortality. For example, since dialysis is an option for patients with end-stage renal disease, surgery on a healthy donor may be difficult to justify, despite the dialysis patient’s diminished quality of life.
The most important in organ donation is to maximize the psychological status and well-being of the donors before and after transplantation has become the foremost goal of all transplantation centres. The psychological issues that mainly concern with the living organ donation includes prevention of psychological harm, ensuring the donors are fully informed and decide to donate without coercion, monitoring donor psychosocial outcomes are intimately linked to the factors that historically served as barriers to use of organs from living donors. These barriers can be overcome by the motivating of the public and creating awareness and responsibility among oneself.
Organs that can be transplanted from the living donor includes one kidney, part of intestine, pancreas, islets of Langerhans, bone, part of liver, one testis, bone marrow and blood. The organ that can be transplanted from the deceased donor are heart, kidney, pancreas, stomach, hand, skin, blood vessels, lungs, liver, intestine, testis, cornea and heart valve.
Autograft: Transplanting a person’s tissues from one site and use it in another site of his body and is called autograft. For example, removal of skin from the legs and using it for damaged skin face or other exposed part.
Allograft: Transplant of an organ between two genetically non identical individuals, it is called allograft. Due to the genetic difference, the donor’s organ will be treated as foreign by the recipient and will try to destroy it. This is called s rejection.
Isograft: Transplant of organ/tissue from a donor to genetically identical recipient is called isograft. There will not be any immune response hence no transplant rejection.
Xenograft: Transplantation of organ/tissues forms one species to another species. For example, the heart valve of pig is transplanted successfully to human.
Split transplant: An organ like liver retrieved from the deceased donor can be divided between two recipients, usually an adult and a child.
Domino transplant: When the lungs are to be transplanted, surgically it is easier to replace them along with the heart. If the recipient’s original heart is healthy, it can be transplanted into another recipient in the need of one.
ABO incompatible transplantation: The immune system of young children aged below 12 months might have developed fully. They can receive organs from incompatible donors.
Live donors: A living person, mentally and physically healthy can donate one of a paired organ, part of an organ or a tissue. The organs donated are kidneys, part of live, one of the lung, part of small intestine, skin, bone marrow, one of the testis and one of the ovaries. Live donor can either be related or unrelated.
Unrelated donors: For altruistic reasons, a person can donate one of his organs to an unrelated donor. According to TOHO act, the unrelated donor should be known to the recipient and have some obligation to him. It has to be established that there is no monetary transaction between them. But in many other countries, even a stranger can donate one of his organs to a needy person on altruistic grounds.
Deceased donors: Organs are harvested from brain dead person whose respiration and circulation are maintained artificially. Brain dead has to be certified by a team of doctors nominated by Government I every organ retrieval centers.
Paired exchange: When a living donor is not compatible with the related recipient, but may be compatible for another recipient. That second recipient related donor is compatible to the first recipient, then permission can be granted for transplantation. The surgery for all four donors and recipient are conducted simultaneously and anonymity is kept until after the transplant.
Spousal donation: A spouse can donate an organ to the partner. It has to be recorded that the couple is legally married.
3. Current scenario: trends

Despite advances in medicine and technology, and increased awareness of organ donation and transplantation, the gap between supply and demand continues to widen. Each year, the number of people in the waiting list is increasing in both donor and transplant. The donation statistics according to OPTN Annual report shows that in 2016, total of 41,335 organs were donated. It can be either deceased or living and four out of five donations came from deceased donors and four out of ten from living donors. According to the report by OTPN 2018, 115,033 people need life-saving organ transplant, of those 74,926 people are the active waiting list candidates.
The real reason behind a living person’s interest in donating one’s organ is important to determine but it is often difficult. Now days, money has become the motivation for donation. The relationships also have played a great role in increasing donation rates. The shortage of available organs can be reduced if; people choose to donate their organs after they die. If more people did that the issue regarding organ shortage can be minimized.
The trend is expected to accelerate each year. Many organ procurement and the Joint Commission on Accreditation of Healthcare Organizations actively participate to increase the donation rates. The organizations take various to steps against traditional social taboos.
The approach, known as “donation after cardiac death” (DCD), usually involves patients who have suffered brain damage, such as from a car accident or a stroke. After family members have made the difficult decision to discontinue a ventilator or other life-sustaining treatment, organ-bank representatives talk to them about donation. Sometimes, the donor is suffering from an incurable disease also end up with the decision of organ donation.
According to U.S Department of Health and Human Services, more than 1,23,000 men, women and children currently needed life-saving organ transplants every 10 minutes and another name is added to the national organ transplant waiting list. In 2014, more than 8500 deceased donors made possible approximately 24,000 organ transplants. In addition, there were nearly 6000 transplants from living donors. In India, nationally with a population of 1.2 billion people, the statistics stands 0.08 persons as organ donor populations. Mrithasanjeevani, Kerala network of organ sharing which began in 2012, also states that the need for organ transplantation is high as the patients in waiting list is increasing day by day who requires organ transplantation.
The need for organ has gone up substantially all over the world. India also suffers from acute organ shortage with little to no solution for this issue. It is estimated that every year 1.5 lakh people suffer from renal failure out of which only 3000 people get donors. Similarly, every year around 2 lakh people die of liver failure or cancer and rarely get any help in the form of organ donors. It is the same for heart patients, for every 50,000 heart attack patients there are only 15 hearts available for transplant. Therefore, there is an urgent need for widespread campaigns to spread awareness about organ donation in India and to bridge the gap between supply and demand. The numbers that are mentioned here are estimates and real numbers could be far more than this, it is scary because this means very few people get relief and get a second chance in life.
The main reasons for organ shortage in India are mainly ignorance and lack of knowledge. People are not well informed enough about the benefits of organ donation. Today social media and so many other forums can promote the positives of organ donation and how it will save so many lives if more people register themselves for organ donation. The reason for organ shortage is myth and superstition. Many people do not want to donate their organs even after death because of so many myths and superstition they are instilled with. People with existing medical condition or old people, who wish to donate, do not donate thinking they are not fit or eligible. Almost everyone can donate some part or the other unless you have any extreme medical condition.
The need for organ donation is necessary because out of the 1.5 lakh people who need kidney in India only 3000 people receive them, only 1 out of 30 people receive kidney and 90% of people in the waiting list die without getting any donor. Around 70% liver transplants are dependent on a live donor but 30% dependent on cadaver (corpse) donations. Hence, there is an urgent need to increase the organ donation rates and give a person a second chance in their life.
4. Challenges in organ donation
As far as the challenges concerned it includes mainly donor’s motives for donation, the predominant ways in which donors arrive at the decision to donate, and the donors’ psychological status and its relationship to their fitness as donors.
4.1. Pre-donation challenges
4.1.1. donor’s motives.
Most donors are likely to be motivated by multiple factors. These factors include intrinsic factors (e.g., desires to relieve the suffering of another or to act in according to the religious convictions) and extrinsic factors (e.g., the social pressures or perceived norms) that may operate simultaneously. The particular combination of motivational forces will also differ depending on whether and how the donor is related to the recipient.
Among living related donors, it has long been assumed that family members or emotional partners are motivated primarily for saving the lives of their loved ones. Such motives are indeed the most commonly expressed feelings, as noted in a variety of studies over the past 30 years. Among nondirected living donors (individuals donating to unrelated patients whom the donors did not select)(NDLDs), it was identified as the altruistic/humanitarian motives, along with beliefs that the donor’s self-worth would be improved, and feelings of moral and religious obligation or self- identity.
4.1.2. Donor’s decision-making
The motivation for the organ donation is purely on the donor’s decision of organ donation and it may be influenced by many factors including the relationship to the recipients. Decision-making swiftness may indicate the type of decision being made. There appear to be two decision-making approaches that include the moral decision making and the rational decision making. “Moral decision-making” involves awareness that one’s actions can affect another; ascription of responsibility to oneself; acceptance of the social/moral norm governing the behavior; and taking action consistent with that norm. Because moral decision-making does not involve the costs and benefits of a given behavior but, instead, is based on perceived norms governing that behavior, it is likely to lead to non- deliberative, instantaneous decisions. In contrast, “rational” decision-making includes various steps that focus on gathering relevant information, evaluating alternatives, selecting an alternative, and implementing the decision.
4.1.3. Support
It includes mainly the assessment of the donor’s available physical, financial and emotional support. It is necessary to identify whether the donor have someone to provide care in the recovery period, have sufficient financial support and so on. This important to avoid distress if the donor develops any complications. Finally, does the donor have the support of significant others for being a donor, or is he or she choosing to donate over the objections of persons who have a legitimate interest in the outcome of an autonomous decision.
4.1.4. Family attitudes toward donation
Spouse and family attitudes about donation should also be explored. Collateral interviews with significant others is necessary, especially those who will be providing tangible support to the donor during the recovery period, should be conducted whenever possible. Conflicts between potential donors and significant others should be addressed and, ideally, resolved prior to surgery itself in order to avoid conflicts later. Family members should provide a good understanding of the donor’s wishes and motives, even if they agree to disagree to the donor’s decision.
4.1.5. Behavioral and psychological health
The behavioral and psychological health of the donor should also be considered before donation. It is important to identify donor’s lifestyle is sufficiently healthy to reduce unnecessary risk for both donor and recipient. Many potential donors may have some unhealthy behaviors, such as moderate obesity or smoking. It is necessary to identify that there is sufficient time for the donor to reduce risks (e.g., lose weight, stop smoking). Moreover, it needs to be taken care of that the donor is emotionally stable to cope with stresses which may come up before, during, and after the donation. Hence it is important to identify psychological and behavioral status of the donor or else it may affect the quality of life.
4.1.6. Donor-recipient relationship
The relationship between the donor and recipient is a complex matter. Even when both parties are agree for donation and transplant, family dynamics may be complicated, and other family members may assertively involve themselves in the decision-making process. The donor may have unrealizable expectations that transplant will alter his or her relationship with the recipient. The health care team should not expect an ideal relationship in which all interactions between donor and recipient are harmonious. However, obvious tensions and overt psychological issues should be addressed. Joint interviews, involving both donor and recipient, should be avoided early in the evaluation process in order to preserve privacy and give the potential donor the opportunity to express reservations or “opt out” gracefully.
4.1.7. Diversity issues
Non directed donors may have diversity concerns that may affect the organ donation. The potential donors should be assessed for comfort with donation to recipients of different genders, races, religions, sexual orientations, nationalities, ages, underlying diseases, and lifestyles. Donors who express objections, fears, or concerns about who might receive their organ may need to be deferred until they can receive counseling.
4.1.8. Psychological status of potential donors
The potential donor’s psychological status is of greatest concern for donation and transplantation. Concerns have been particularly high in case of unrelated donation (either directed to a specific patient, or NDLD): the willingness or desire to donate to a stranger has been historically viewed with suspicion and as likely to reflect significant psychopathology. There is no doubt that some potential donors will be psychologically poor candidates to serve as donors.
4.1.9. Post-donation challenges
The donors’ perceptions of their physical functional, psychological, and social well-being were found to be either nonsignificantly different from or significantly better than levels reported in the general population. The post challenges mainly includes recipient death or graft loss, donor medical complications, donor history of mood or other psychiatric problems, and poor donor relationships with recipient or family. The other factor is that it may affect the donor’s quality of life if any complication arises.
The post transplantation challenges are many which include minimizing rejection risks, immunosuppression, organ shortage, handling of the stressors of transplantation, psychosocial adaptation and psychological disorders and so on.
4.1.10. Minimizing rejection risks
The twin conditions of antibody sensitization and antibody-mediated rejection remain challenging and frustrating to treat. The recent drugs which are used to desensitize patients or reverse antibody-mediated rejection, especially chronic antibody mediated rejection is totally unsatisfactory. Development of therapies those are more effective and less toxic should be made available. Recent regimens used for antibody desensitization and reversal of antibody-mediated rejection include plasmapheresis, immunoglobulin (IVIG), and rituximab, an anti-chimeric, anti-CD20 antibody. Recently, the proteasome inhibitor Velcade has also been reported to reverse refractory antibody rejection. Eculizumab, a humanized anti-C5 monoclonal antibody appears to protect the renal allograft despite the presence of donor-specific antibodies (DSA). None of these agents have been tested in rigorous studies.
4.1.11. Immunosuppression
This is one of the major challenges after organ transplantation. Many studies have suggested that most of the late graft loss occurs because of immunologic reasons, frequently antibody-mediated. So the approach of minimizing immunosuppression is necessary with the present drugs to reduce toxicities may actually be helpful in the long-term survival of the graft. The toxicities are minimized by allowing more grafts to be rejected by immune mechanisms. Hence, development of effective agents that lack long-term toxicities so that we can maintain optimum immunosuppression over the long-term.
4.1.12. Stressors after transplantation
In the perioperative period, the focus is on the patient’s physical recovery, with possible rejection episodes and other medical complications causing anxiety and emotional strain. Within the first days after transplantation, a postoperative delirium can occur. The patient can present with symptoms of mental confusion, language disturbances, and occasional hallucinations and delusions are often a frightening experience to patients and their families. Acute brain dysfunction can occur in intensive care patients and patients after surgery. The corticosteroids which are administered for immunosuppression cause these problems. Some of the patients experience problems in accepting the new organ from another individual and suffer with feeling of guilt towards the donor which, in turn, can increase psychological stress and nonadherence [ 6 , 7 , 8 , 9 , 10 , 11 ].
In the long-term postoperative period, medication side effects and associated comorbidities become central stressors impeding patient’s life quality. Most common comorbidities seen are infections, diabetes mellitus, hypertension, lipometabolic disorders, adipositas, cardiovascular diseases, oncological diseases, osteoporosis, and chronic kidney failure [ 12 , 13 ]. Furthermore, psychiatric symptoms (e.g., depression, anxiety, agitation, psychosis) and neurological symptoms (e.g., sleep disturbances, cognitive impairment, delirium) can occur as neurotoxic side effects in patients receiving immunosuppressive drugs.
Faced with the multiple health risks, patients often continue to experience anxiety and worries regarding possible retransplantation, serious comorbidities, and death. Even patients in good physical health are confronted with severe challenges, for example, regaining their previously lost or restricted social roles as family members and partners (including sexual activity) and returning to work or taking up other meaningful activities. Financial constraints and legal disputes with health or pension insurance agencies constitute other possible sources of psychological strain.
5. Psychosocial adaptation and psychological disorders
After the transplantation, the psychosocial burden more severe in preoperative period than postoperative period. Nevertheless, patients themselves have to demonstrate considerable coping skills. In the best case, transplant patients learn to adapt to their new situation, often by reevaluating life goals and by focusing on more positive consequences, for example, personal growth. On the other hand, unsuccessful readjustment can lower the quality of life and psychiatric morbidity. The most common psychological disorders among patients before and after transplantation are affective and anxiety disorders.
The literature review shows that prevalence of depression in 20–25% of cases before and after kidney transplantation. Less information is available concerning patients receiving other organs. Prior to and following lung transplantation, depression seems to be prevalent in approximately 30% of patients. Hence these show that the depression is a major challenge after transplantation. These issues can be reduced by personal and social resources (resilience factors), that is, favorable coping skills, self-efficacy, sense of coherence, optimism, and social support.
6. Factors affecting donor’s motivation
There are many factors affecting donor’s motivation which includes feelings of love and responsibility, spiritual motives, and greater success rate of organ donation.
6.1. Feelings of love and responsibility
Motives for donating organ to their relative patients were that they tended to do something for their loved ones. In fact, they feel responsible for their problems. They do not treat others’ problems with indifference and attempted to do whatever they could for resolving the problems experienced by transplant recipients. It is considered as their own responsibilities to help them to get rid of their problems. The feel like they are the ones who need to support their patients.
6.2. Close and constant companionship
Another factor affecting the participants’ feeling of responsibility for donation to their family members was close and constant companionship with recipients. This close and constant companionship made the participants to clearly understand the recipients’ conditions and hence, it had resulted in their decision on organ donation in order to alleviate recipients’ problems. This close and constant companionship with patients help family members understand patients’ problems well and increase their degree of commitment to do something for patient’s pain and discomfort. They also noted that this had made them experience deeper shared emotions with their patients and hence, required them to feel responsible for minimizing their patient’s problems.
6.3. Inability to tolerate recipient’s discomfort
Another motive for organ donation was one’s difficulty in tolerating recipient’s discomfort. Love for their sick family members had made the participants feel responsible and decide on doing something for solving their patient’s problems. Their patient’s pain, suffering and discomfort cause a great inconvenience and irritation which lead them to the decision of organ donation. They hoped that organ donation alleviate their patient’s problems [ 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 36 ].
6.4. Spiritual motives for donation
Religious beliefs played a significant role in motivating to organ donation. Some of them believed that donation was a way for expiating their past sins. They referred to faith in God, reliance on Him, and hope for a successful transplant as the important motives for organ donation. Some of them even accused themselves of causing their family members to develop organ failure and believed that donation was a way for alleviating their feelings of guilt. Such a practice was particularly common among the parents of sick children. Some of them considered donation as a God-approved practice, and noted that God has helped them donate their organs. They noted that they donated their organs for gratifying God and believed that he sees it and help them in all bad situations.
6.5. Greater success rate of organ transplantation
The category is the greater success of organ transplantation. In other words, obtaining information and realizing the greater benefits of organ transplantation had motivated the participants to opt for organ donation. Some of them reported that they had never thought about donation until obtaining information from their patient’s physicians. However, after obtaining adequate information, they had made an irreversible decision about organ donation. Accordingly, a major motive for organ donation was the lower likelihood of organ rejection.
7. Measures to overcome challenges for organ donation
The decisions regarding organ donation based on the personal beliefs (religious, cultural, family, social and body integrity) levels of knowledge about organ donation and previous interaction with the health care team. Many maintained positive attitudes to organ donation despite significant reservations about the organ donation process. Resistance to organ donation found to be less in the case of living donation for family.
There are some religious beliefs that can have both positive and negative influences, these often stemmed from uncertainty or misrepresentation of religious edicts. One solution would be to actively engage religious leaders in the transplant community, especially when it has been reported that, across the major religions, there are very few cases where organ donation can be seen to be inconsistent with religious beliefs. Religious leaders should be made available in hospitals and other transplantation setting to assist families in making decisions regarding organ donation and potentially to remove the misperceptions. Staff members who are involved in approaching families to request consent for donation should be part of the awareness programs and resources about religious concerns. Similarly, cultural sensitivity to issues such as apprehensiveness to discuss death among certain groups or individuals and the importance to many of death rituals may improve dialog regarding organ donation.
Studies have shown that engaging some minority groups in the health care system and creating a sense of belonging and ownership can improve compliance with organ donation. As a consequence, more efforts should be made to create positive interactions within the health care team members, especially for minority groups, to improve the organ donation rates. Although many of the studies have showed that higher socio-economic status and education were associated with a stronger willingness to be an organ donor. Some of the strong reservations held, even among those with generally positive views towards donation, such as concerns that agreeing to donation would discourage doctors from caring so much about saving their lives in case of an emergency or that it would result in the premature removal of their organs or indeed prevent them from having an open coffin at their funerals, are examples of very real barriers that can be readily addressed through information. Through a proper awareness and motivation the donation rates can be improved which can save many lives.
7.1. Psychological care
Psychological consultation is essential for all disease stages enabling patients to better cope with their extraordinarily stressful situation. A need for psychological care was found in up to 50% of transplant patients. Educational and supportive therapies are of utmost importance but also cognitive-behavioral interventions including relaxation techniques can also be considered. Less common methods like hypnotherapy and “Quality of Life Therapy” have also been utilized for overcoming the challenges.
Moreover, family members as well as caregivers of transplant patients show increased psychological strain before and after transplantation. Family counseling, and psychotherapeutic support, can help reduce psychological strain, thus also maintaining the valuable social support provided by care givers and family members of the transplant patient. Henceforth, the family and care givers should also be considered in psychosocial evaluation to overcome the problems.
7.2. Alternative methods to increase donation
In view of ethical, legal and political issues, it was deemed important to obtain some opinion about alternative methods to increase organ donation rates. Financial incentives were given to increase organ donation. Many in both donor and non-donor groups were given a reasonable incentive. Education and dissemination of information about donation and transplantation was important to increase organ donation rates. There was nearly universal agreement that implied consent (presumed consent) should not be tried. The use of financial incentives was not markedly opposed (some accepted the idea of funeral expense reimbursement), although there was not strong support either. In general, methods to increase organ donation had not been well thought out by either donors or nondonors indicating, perhaps, that the assumption of altruism or motivation is the best way to increase the donation rates.
8. Responsibilities of nurses in organ donation and transplantation
Organ and tissue transplant nurses need comprehensive and scientific knowledge. They include the evaluation and management of deceased donors, transplant recipients, potential donors or live donors, teaching and counseling of transplant recipients and live donors related to self-care management, healthy life and a peaceful death when this is imminent. This is important in order to improve the posttransplant quality of life.
Nurses have important role in the development of a successful transplantation program. They are key members of the team that works to deliver care to patients and relatives, through the use of technological, logistic and human resources, with a view to coordination, care, education and research on organ and tissue donation and transplantation. Therefore, the nurses need adequate knowledge on the principles of good ethical principles and should have resources available for them to assess patient’s risks and social issues related to organ transplants and donation. The researchers hope that the future studies will encourage further researches on the role and responsibilities of nurses.
9. Conclusion
The organ donation decision is a complex one, based strongly on personal beliefs. There are some factors, such as religious and cultural beliefs, that are seemingly intractable and are often cited as reasons for a refusal to donate. In this chapter, it is shown that these have often been found to be tied in with more complex issues such as a distrust of the medical system, misunderstandings about religious stances and ignorance about the donation process. Interventions to better engage the community, including disadvantaged and minority groups, to foster trust and provide information represent promising opportunities of promoting organ donation in the future.
Donor motives directly contribute to their decision to donate, is not uniform and is influenced by multiple factors. Majority of the donors were relationship oriented donor, whose major motives were desires to relieve the suffering & save the life of their loving ones. Creating awareness to the organ donation will directly influence the donor motives and willingness. By deriving the motives many more intervention to improve the willingness to be a living organ donor can be evolved. Recruitment of living donors represents a medical and moral responsibility. The possibility of organ removal from healthy donor to a recipient needs great inner motivation. Saving one’s life is divine.
The psycho social assessment must be made as a routine part of the nursing process. These assessments are meant to identify patients at risk for poor outcomes, provide guidelines for their management and improve the post-transplant quality of life [ 6 ]. “Because donated organs are a severely limited resource, the best potential, recipients should be identified. The probability of a good outcome must be highly emphasized to achieve the maximum benefit for all transplants” (OPTN/UNOS Ethics committee General Considerations in Assessment for Transplant Candidacy White paper-2010).
- 1. United Network for Organ Sharing. 1999 Annual Report of the U. S. Scientific Registry of Transplant Recipients and the Organ Procurement and Transplantation Network.: Transplant Data 1989–1998. Richmond, Va: US Department of Health and Human Services, Health Research Services Administration, Office of Sponsored Projects, Division of Transportation, and United Network for Organ Sharing; 2000
- 2. Alexander JW, Zola JC. Expanding the donor pool: Use of marginal donors for solid organ transplantation. Clinical Transplantation. 1996; 10 :1-19
- 3. Kumar A, Mandhani A, Verma BS, et al. Expanding the living related donor pool in renal transplantation: Use of marginal donors. Journal of Urology. 2000a; 163 :33-36
- 4. Mandal AK, Kalligonis AN, Ratner LE. Expanded criteria donors: Attempts to increase the renal donor transplant pool. Advances in Renal Replacement Therapy. 2000a; 7 :117-113
- 5. Simmons RG et al. Gift of Life: The Social and Psychological Impact of Organ Transplantation. NY: Wiley; 1977. Reprinted with additions, Brunswick, NJ: Transaction Books, 1987
- 6. Corley MC et al. Attitude, self-image, and quality of life of living kidney donors. Nephrology Nursing Journal. 2000; 27 (1):43-52
- 7. Goldman LS. Liver transplantation using living donors: Preliminary donor psychiatric outcomes. Psychsomatics. 1993; 34 (3):235-240
- 8. Pradel FG et al. Exploring donors’ and recipients’ attitudes about living donor kidney transplantation. Progress in Transplantation. 2003; 13 (3):203-210
- 9. Fellner CH. Renal transplantation and the living donor. Decision and consequences. Psychother Psychosomat. 1976/77; 27 :139-143
- 10. Toronyi E et al. Attitudes of donors towards organ transplantation in living related kidney transplantations. Transplant International. 1998; 11 (Suppl 1):S481-S483
- 11. Henderson AJZ et al. The living anonymous kidney donor: Lunatic or saint? American Journal of Transplantation. 2003; 3 :203-213
- 12. Jacobs CL et al. Twenty-two nondirected kidney donors: An update on a single center’s experience. American Journal of Transplantation. 2004; 4 :1110-1116
- 13. Matas AJ et al. Nondirected donation of kidneys from living donors. The New England Journal of Medicine. 2000; 343 (6):433-436
- 14. Olbrisch ME et al. Psychological, Social and Behavioral Characteristics of Living Donor Candidates for Adult Liver Transplantation. Biennial Meeting on Psychiatric, Psychosocial and Ethical Issues in Organ Transplantation. Santa Monica, CA; February, 2005
- 15. Crowley-Matoka M et al. Long-term quality of life issues among adult-to-pediatric living donors: A qualitative exploration. American Journal of Transplantation. 2004; 4 :744-750
- 16. Karliova M et al. Living-related liver transplantation from the view of the donor: A 1-year follow-up survey. Transplantation. 2002; 73 (11):1799-1804
- 17. De Graaf Olson W, Bogetti-Dumlao A. Living donors’ perception of their quality of health after donation. Progress in Transplantation. 2001; 11 (2):108-115
- 18. Beavers KL et al. The living donor experience: Donor health assessment and outcomes after living donor liver transplantation. Liver Transplant. 2001; 7 (11):943-947
- 19. Lennerling A et al. Becoming a living kidney donor. Transplantation. 2003; 76 :1243-1247
- 20. Pradel FG. Exploring donor’s and receipient’s attitudes about living door kidney transplantation. Progress in Transplantation. 2003; 13 (3):203-210
- 21. Smith MD. Living related kidney donors. A multicenter study of donor education, socioeconomic adjustment and rehabilitation. American Journal of Kidney Diseases. 1986; 8 (4):223-233
- 22. Jacobs CL. Expanding living donor options. Minnesota Medicine. 2001; 84 :46-48
- 23. Switzer GE. Understaning donor;s motivations. A study of unrelated bone arrow donors. Social Science & Medicine. 1999; 45 (1):137-147
- 24. Rosenthal JT. Expanded criteria for cadaver organ donation in renal transplant. The Urologic Clinics of North America. 1994; 21 :283-292
- 25. Shiel AGR. Transplantation and society. In: Ginns LC, Cosimi A, Morris PJ, editors. Transplantation. Malden, MA: Blackwell Science; 1999. pp. 897-913
- 26. Callender CO, Bay AS, Miles PV, Yeager CL. A national minority organ/tissue transplant education program: The first step in the evolution of a national minority strategy and minority transplant equity in the USA. Transplantation Proceedings. 1995; 27 :1441-1443
- 27. Surman OS et al. Live organ donation: Social context, clinical encounter, and the psychology of communication. Psychosomatics. 2005; 46 :1-6
- 28. Papachristou C et al. Motivation for living-donor liver transplantation from the donor’s perspective: An in-depth qualitative research study. Transplantation. 2004; 78 :1506-1514
- 29. Haljamäe U. Remaining experiences of living kidney donors more than 3 yr after early recipient graft loss. Clinical Transplantation. 2003; 17 :503-510
- 30. Hamburger J, Crosnier J. Moral and ethical problems in transplantation. Rapaport F, Daussert J. Human Transplantation. NY: Grune & Stratton; 1968. pp. 68
- 31. Sadler HH et al. The living, genetically unrelated, kidney donor. Seminars in Psychiatry. 1971; 3 :86-101
- 32. Walter M et al. Psychosocial outcome of living donors after living donor liver transplantation: A pilot study. Clinical Transplantation. 2002; 16 :339-344
- 33. Fukunishi I et al. Psychiatric disorders before and after living-related transplantation. Psychosomatics. 2001; 42 (4):337-343
- 34. Crowley-Matoka M, Switzer G. Nondirected living donation: A survey of current trends and practices. Transplantation. 2005; 79 (5):515-519
- 35. Boparai J, Davila H, Chandalia M. Cardiovascular disease in Asian Indians living in the United States. Current Cardiovascular Risk Reports. 2011; 5 :240-245
- 36. Ji WR, Frederick B, Hsin CY. Trends in prevalence of Type 2 diabetes in Asians Versus Whites results from the United States National Health Interview Survey 1997-2008. Diabetes Care. Feb 2011; 34 (2):353-357
© 2018 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Organ donation and transplantation.
Published: 25 July 2018
By Bulang He, Xiuwu Han and Michael A. Fink
2414 downloads
By Félix Cantarovich
1959 downloads
By Alyssa Green, Peter G. Thomas, Rebecca Wilde-Onia,...
1214 downloads
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Family Med Prim Care
- v.8(1); 2019 Jan
Organ donation – “attitude and awareness among undergraduates and postgraduates of North-East India”
Raktim pratim tamuli.
1 Department of Forensic Medicine and Toxicology, Gauhati Medical College and Hospital, Guwahati, Assam, India
Smritimala Sarmah
2 Department of Physics, B. Borooah College, Guwahati, Assam, India
Bishwajeet Saikia
3 Department of Anatomy, NEIGRIHMS, Shillong, Meghalaya, India
Background:
Organ donation is defined as “When a person allows an organ of theirs to be removed, legally, either by consent while the donor is alive or after death with the assent of the next of the kin.” Common transplantations after organ donations include kidney, heart, liver, pancreas, intestines, lungs, bones, bone marrow, skin, and cornea. Although some organs such as kidney and tissues like part of the liver, pancreas, lungs, and intestines can be donated while the donor is alive, most of the donations occur only after the donor's death. In India, the legislative foundation for brain death and organ donation was officially established, under Transplantation of Human Organs Act, 1994 amended in 2011. It provided a much-needed legal and transparent system for organ donation. India's organ donation rate (ODR) stands at an abysmal 0.34 per million populations (PMP) when compared with donation rate of 36 PMP in countries like Spain. While in the rest of the country, states like Tamil Nadu, Maharashtra, Andhra Pradesh, and Gujarat have made efforts to ramp up their ODR, by facilitating public and private health sector activities, such vision is still a far cry for the states in the North-Eastern part of India.
Materials and Methods:
This study on awareness of organ donation was conducted in one of the premiere educational institutes at Guwahati. A predesigned performa (questionnaire) was used to collect data from 360 individual, of which 180 participants were undergraduate students and 180 participants were faculties having postgraduate degree.
The results show that 79.17% (285) of participants were aware about organ donation, and out of all participants, families of only three have donated organ in the past 5 years. A total number of 12 (3.33%) participants have signed up for organ donation. A significant portion of the study population (12.5%) opined that there might be some religious beliefs which are preventing certain strata of local population from donating or accepting organs. More than half (186) (51.67%) of the study group opined that there is lack of awareness among people which may be one of the reasons for low rates of organ donation.
Conclusion:
Organ donation programs are at a very primordial stage in India and are almost negligible in its North-Eastern region. It is high time for the policy makers and other stake holders of a global giant like India to understand the magnitude of the benefits from these programs. Making tangible policies that are reflected nationally, emphasizing attention to both the organ donors and recipients, is the need of the hour.
Introduction
Organ donation is when a person allows an organ of theirs to be removed, legally, either by consent while the donor is alive or after death with the assent of the next of kin. Common transplantations include kidneys, heart, liver, pancreas, intestines, lungs, bones, bone marrow, skin, and corneas. Some organs and tissues can be donated by living donors, such as a kidney or part of the liver, part of the pancreas, part of the lungs, or part of the intestines. Even though possible while living, most donations occur only after the donor's death.[ 1 ] A significant number of deaths due to organ failure can be prevented by timely donation and transplantation of organs. However, when it comes to India, the country is beset with a monumental deficit of organs available for transplants. India's organ donation rate (ODR) stands at an abysmal 0.34 per million populations (PMP), while countries like Spain are having a donation rate of 36 PMP.[ 2 ] In 1994, the legislative foundation for brain death and organ donation, amended in 2011, was officially established in India, under Transplantation of Human Organs Act (THOA).[ 3 ] It provided a much-needed legal and transparent system for organ donation. Yet again in 2015, the health ministry in India announced a policy mechanism to facilitate cadaver organ donation to further address institutional roadblocks.[ 2 ]
Brain death and organ donation
It has been quite a long time now that the deceased organ donation/brain death has been popularized worldwide. Maintenance of circulation and respiration becomes possible with the advent of mechanical ventilator and other sophisticated instruments, even if the person's brain is damaged irreversibly. These are known as brain-stem death persons or beating cadavers.[ 4 ] Organs can be harvested or retrieved from them for transplantation. Harvesting organs for transplantation purposes from such persons is known as cadaver transplantation . Recently, determination of brain death has assumed importance for two reasons:
- Counseling relatives of the deceased for organs’ donation
- Timely declaration of brain death can reduce prolonged unnecessary hospital stay and cut short hospital bills.
In India, THOA, 1994 amended in 2011 regulates the removal, storage, and transplantation of human organs/tissues for therapeutic purposes and prevents the commercial dealings of human organs.[ 3 ]
Organ donation in India
Data from 2015 show that as against the demand for 1.75 lakhs of kidney transplants, there were only 5000 transplants done. Similarly, of 50,000 people dying of end-stage liver disease, only 1000 got their liver transplanted. Statistics are distressingly poor in case of transplantation of heart or lung.[ 2 ] Transplant rates for cornea are 1 in 25,000 when compared with 1 in 199 and 1 in 14,000 for the United States and Brazil, respectively.[ 5 ]
Only 0.08% of Indians donate their organs when compared with 70%–80% of Spaniards and Belgians.[ 6 ] About 0.5 million people in India die every year due to nonavailability of organs.[ 7 ]
There are two systems for organ donation practiced worldwide, the family consent system and the presumed consent system . Countries like the United States, United Kingdom, Germany, and Netherlands follow family consent system where people sign up as organ donors, and their family's consent is required. ODR in these countries averages between 10 and 30 PMP. The more aggressive presumed consent system is adopted by countries like Singapore, Belgium, and Spain. This system permits organ donation by default unless the donor has explicitly opposed it during his or her lifetime. This system does not require family's consent. It is seen that the ODR in countries adopting presumed consent is double than the countries who have adopted family consent, averaging between 20 and 40 PMP.[ 7 ] Inspired by this outcome, the doctors of All India Institute of Medical Sciences, New Delhi, have recently suggested starting “Presumed Consent” in India too, especially in cases of accidental fatalities.[ 8 ]
State-wise organ donation status in India
Organ donation from deceased donors is slowly gaining momentum in India. In the year 2000, MOHAN Foundation took the lead in setting up an organ sharing network, the Indian Network for Organ Sharing in the state of Tamil Nadu. This network facilitated the retrieval of 1033 organs and tissues.[ 9 ]
Many other states are also following Tamil Nadu with robust “Deceased organ donation and transplantation program.” According to 2014 data, Puducherry has got highest ODR in India with 10.4 organ donation PMP, followed by Chandigarh with an ODR of 5.7 PMP.[ 9 ] In terms of number of deceased organ donors, Tamil Nadu holds the number one spot with 136 donations during that year.[ 9 ] Programs such as “Jeevandan” in Andhra Pradesh[ 10 ] and “Zonal Transplant Coordination Center” in Maharashtra[ 11 ] are already working for facilitating organ transplantation in these states. MOHAN Foundation has been spearheading efforts in Delhi NCR (National Capital Region) and Chandigarh with encouraging results. Kerala government has set up “Mrithasanjeevani” and the Kerala Network for Organ Sharing,[ 12 ] which have been running successfully since 2012. The Government of Rajasthan initiated the movement on organ donation with the setting up of the Rajasthan Network for Organ Sharing.[ 13 ] They have successfully retrieved 12 organs (liver and kidney) from five deceased donor within a period of 7 months since its inception in December 2014.
Scenario of organ donation North-Eastern part of India
Organ transplantations were being performed in a few occasions in North-Eastern India, but the numbers are very nominal to talk about. Although a few local nongovernment organizations (NGOs) are being reported to be working toward generating awareness for organ donation, overall administrative negligence which can be summed up to lack of basic infrastructure, lack of trained individuals, and lack of government approved centers is probably putting the issue of organ donation to a state of dire straits in this region. It must be noteworthy to mention here that nothing substantial has been heard from the authorities of any of the seven North-Eastern states for adapting policies to facilitate organ donation till now. Thus, hundreds of patients still have to leave this region for transplantation every year. Raising awareness of organ donation in the present healthcare scenario in North-East India emerges as a challenge where even the basic health facilities are a far cry.
Aims and objectives
- To determine awareness and knowledge of educated [undergraduate (UG) students and postgraduate (PG) degree holders] population toward organ donation
- To find out factors impeding the organ donation program in this part of the country
- To observe differences between findings of UG students and PG degree holders (faculty).
Materials and Methods
Guwahati, the gateway to North-East India, is the largest city in this region, serving a population of around 1 million. This study was conducted in one of the premiere educational institutes of Guwahati. A predesigned questionnaire was used to collect data from 360 individuals with n = 360, 180 UG students, and 180 faculties having PG degree. Data collected were analyzed using Microsoft Excel, which were tabulated and figured accordingly. Comparison between findings was analyzed using Chi-square test (χ 2 ) test, and P value was calculated. P value <0.005 was regarded as significant.
Results and Observation
Awareness about organ donation.
The results showed that 285 (79.17%) subjects were completely aware about organ donation, 60 (16.67%) were partially aware, and 15 subjects were totally unaware about organ donation. Comparison between UG students and PG degree holders showed significant difference; data show that all UG students were either partially or completely aware about organ donation, whereas 8.33% (15) of PG degree holders are completely unaware about it [ Table 1 ].
Awareness about organ donation among undergraduate students and postgraduate degree holders
UG: Undergraduate; PG: Postgraduate
Family members donating organ in the past 5 years
Family member of only three subjects (UG students) had donated organ in the past 5 years.
Response about organs which can be donated
Most of the subjects, 297 (82.5%) of 360, believed that only eye (cornea) and kidney are the organs available for donation. About one-third people, 129 (35.83%), knew about liver and heart transplantation. Only few, 42 (11.67%), were aware about donation of organs such as lungs, pancreas, and intestine. The results showed significant difference between findings of UG students and PG degree holders [ Table 2 ].
Response about various organs that can be donated
Ideal organ donor and response of participants
More than one-third, 38.33% (138) subjects, knew that organ can be donated both during life and after death, whereas most of them were uncertain about it. This finding also shows significant difference between both study groups [ Table 3 ].
Response about who can actually donate organs
Participants signing up for organ donation
Of the total study participants, it was observed that only 12 (3.33%) individuals had signed up for organ donation programs. Among them, nine (5%) were PG degree holders. This finding was not statistically significant with P value 0.078when compared between UG and PG study groups.
Interest in becoming an organ donor
More than half of the participants, 205 (57%), were willing to become a potential donor [ Figure 1 ]. This finding also shows significant difference between the study groups ( P = 0.0014), with UG students showing more interest in becoming a potential donor.

Person interested in becoming organ donor
Awareness about beating heart donor
Almost 56% (201) participators were unaware about beating heart donor (or brain death) [ Figure 2 ]. Both UG and PG groups do not show any significant difference regarding their perception with a P value of 0.3395.

Role of religion in donating or accepting organs
About 45 (12.5%) of the participants from the study population believed that religious beliefs do prevent individuals from donating or accepting organs; however, 113 participants (31.37%) were doubtful about it. The differences in the two groups in this regard were not significant statistically [ Table 4 ].
Role of religion in organ donation
Reason behind a poor level of organ donation
About 186 (51.67%) of participants opined that lack of awareness among common people was the prime factor responsible for such sparse state of organ donation in this part of India. Both study groups showed significant difference regarding their views about this low level of organ donation [ Table 5 ].
Reasons for infancy level of organ donation
OD: Organ donation; UG: Undergraduate; PG: Postgraduate
Even though a very few articles were available for evaluation, the findings of our study can be compared with a survey published in the popular Indian English Daily, the Times of India (TOI), which conducted a survey for organ donation in eight major cities of the country.[ 14 ] High level of awareness or consciousness is usually associated with a higher rate of organ donation. A good percentage of study population, 79.17% (285), was aware about organ donation, and 15 (4.17%) were completely unaware about it. The TOI survey reported a higher rate of awareness (94%) than our study. The reasons may be a difference in level of both education and social awareness between the two populations.
While carrying out a research at Andhra Medical College, Deepthi et al . found that 97.6% of students were aware about organ donation, 87% could tell the definition, and 56.9% show complete knowledge about every aspect of organ donation.[ 15 ] Sucharitha et al .[ 16 ] in their study observed that 77% of the participants strongly approve organ donation. This study was conducted in the state of Tamil Nadu, which is the forerunner of organ donation in India. It reported a better result with participants of their study claimed to have had a history of organ donation in the family (6.6%). In our study, the majority of the participants (90.6%) agreed that organ donation should also be promoted. With the level of awareness being comparable (79.17%) with the studies conducted by TOI (94%) and Deepthi et al . (97.6%), the rate of organ donation was much better with Deepthi (6.6%) when compared with our study (0.83%).
Lack of infrastructure, higher cost of transplantation, and dearth of facilitating organizations are the probable reasons for the poor state of organ donation in North-East India. Voluntary organ donation after brain death necessitates an organ bank for harvesting of retrieved organs. Till now, no such bank is established in the entire North-Eastern part of India. NGOs and people working on promotion of organ donation must compel government on such issues. Only after establishment of such facilities, we can think about intensifying the movement on cadaver organ donation.
People of almost entire Indian subcontinent still believe that the eye and kidney are the only organs available for donation. Almost 80% participants of our study were aware about eye (82.5%) and kidney (77.5%) donation. Few of them knew about donations of liver (35.83%) and heart (35.83%). Only 11.67% believed that most of the organs can be donated. Similar results were reflected in the TOI survey, according to which 91%, 87%, 63%, and 38% participants know about donation of organs such as eye, kidney, heart, and liver, respectively. In contrary to our study, the TOI survey got a worse response (7%) when participants were enquired about possible donation of almost all organs. Compared with our study and the TOI survey, Deepthi et al . got better results where 26% of students correctly named the organs available for donation. Saleem et al . in their study at Karachi, Pakistan, also found a similar result; 26.2% of participants of their study knew about multiple-organ transplantation.[ 17 ] Almost similar to our study, 66.2% of study population of Saleem et al . and 95.4% of participants of A. Soubhanneyaz et al .[ 18 ] were aware about kidney donation programs.
Who can actually donate organ; during life, after brain death, or only young and healthy individuals? In response to this question, 38.33% of participants of our study say that it can be donated both during and after life. Another 12.5% believe that organ can only be donated after death. Just like our study, in the TOI survey, 46% individuals were aware that organ can be donated both during life and after death. In contrary to our study, they found a higher response (45%) regarding only deceased organ donation. In Sucharitha et al .,11.3% of participants were aware that organ donation can be done both while living and after death.[ 16 ] Regarding age of the donor, 19.2% of participants of Sucharitha et al . and 47.2% of Deepthi et al . opined that the donor can be of any age. In a study conducted by Sahu RK et al .[ 19 ] on 342 participants, they found that 218 (63.7%) participants thought that organ can only be donated by living persons, while 4.09% were aware that organ can be retrieved from both living and cadaver. About 50% of participants (50.1%) of Saleem et al . say that organ for donation can come from cadavers, while 36.5% knew about living organ donation.[ 17 ] In this study, 23% responded that organs can be donated both during life and after death.
Only 12 (3.33%) of 360 participants have signed up for organ donation till now. This finding is almost consistent with the TOI survey, where barely 5% finally took the step to register as organ donors. Sahu et al . reported a better scenario; 10.6% participants of this study have already signed up the organ donation form (89.4% have not filled up any pledge on organ/body donation). A collective approach with political and administrative will with sensitization campaigns in print/electronic/social media and active involvement of stakeholders from health sectors including doctors might help increase the number of people signing for these organ donation programs.
More than half participants of our study (57%) are interested in becoming a potential donor. Similarly, 53.5% of participants of Sucharitha et al . responded positively to pledge their organs for donation after death. Deepthi et al . found that about 50% of students are willing to donate their own organs and 61% show willingness to donate their family member's organs after their death. A better response is obtained in the TOI survey with 69% participants nodding their head for potential organ donation. In contrary to these studies, Sahu et al . observed that only 44.1% of participants are keen to donate their body for organ donation after death. Abdulrahman Soubhanneyaz et al . in their study conducted in Saudi Arabia found that 73.5% of participants are interested in becoming an organ donor.[ 18 ] About 62.3% of participants of Saleem et al . were seen motivated to donate their organs. A study from Nigeria shows a poor response, where only 30% respondents expressed their willingness to donate their organs.[ 20 ] Better results were shown in studies from Ohio[ 21 ] and Brazil[ 22 ] with 96% and 87% participants, respectively, showing willingness to donate. Almost similar to our study, 57.9% of study population of Hamed et al . was willing to donate their organs.[ 23 ] H. Schauenburg and A. Hildebrandt conducted a study catering citizens of Germany and Spain on Public Knowledge and Attitudes on Organ Donation . They found that 17.71% of participants were seriously thinking (much thought) and 54.5% were somewhat thinking to donate organs.[ 24 ] Lack of sensitization, family refusal, and fear of mutilation of the body after death are a few possible factors responsible for not getting enough organ donors from this part of the country. Cumbersome official paper works or insufficient knowledge about the procedure might be some of the other pertinent factors.
Our study shows that 44.17% of participants were aware about beating heart donor (brain-stem death). Compared with this, very less percentage (11.7%) of participants from Hamed et al . were aware about brain-stem death. With such a good level of awareness about beating heart donor, a better status of organ donation in North-Eastern India can be expected. Nongovernment agencies along with medico organizations must work together to sensitize common people about the concept of brain death and organ donation. We can expect a more number of potential donors from North-Eastern part of India, once people are fully sensitized.
Religion does prevent someone from donating or accepting organs; 12.5% participants have opined like that and 31.37% are doubtful about it. Similarly, 12% of students of Deepthi et al . think religion as possible barrier. Sahu et al . and the TOI survey found almost equal results in this regard with 5.5% and 5% of responses. In Suchiritha ST et al ., 64.3% individuals mentioned that their religion allows organ donation. Just like the TOI survey, 5% participants of Abdulrahman Soubhanneyaz et al . believe that religion is an important factor in donating organs. In Saleem et al ., almost 30% (29.6) of participants say that before donating any organ they would consider religion of the recipient. Hamed et al . found religious prohibition as a cause of refusal to donate organs in 19% of participants.
About 52% of participants of our study think that lack of awareness among common people is the factor responsible for such poor state of organ donation in this part of India. Whereas 95.9% of participants of Deepthi et al . thought that there is need to create awareness in the public to promote organ donation. Sensitization of common people and involvement of different agencies and media are a must to do to for a better outcome.
Limitations of the study
- The study carried out in one of the premiere educational institutes of Guwahati might not exactly be representing the scenario of organ donation in India, but it is definitely highlighting a few important factors that need to be addressed at this point of time
- A bigger sample size would reflect a better picture of the research issue.
With a rate of about 10 transplants per year, Gauhati Medical College and Hospital is one of the leading institutes in North-East India catering organ transplant procedures.[ 25 ] Such low rates in the region make North-East India lag much far behind the rest of the country in organ donation and transplantation programs. Be it lack of resources in the form of medical facilities and expertise or lack of awareness due to negligible promotion in the public domain, this miserable state of affair is unacceptable and should be attended by the authorities in precedence. While recently it was seen that efforts are being made by some NGOs for creating awareness toward organ donation,[ 26 , 27 ] such programs need more participation from the learned section of the society. This is where the healthcare providers can contribute in a significant way through mass education. Thus, apart from revealing the perception of the educated strata of our society toward organ donation, this study also attempts to make efforts for raising awareness of the same.
Even though provisions for organ donation are available under regulations provided by the government in this part of the country, a more organized and proactive approach by the policy makers is need of the hour.
Implications to the policy makers for organ donation
- Establishment of organ banks with facilitating speedy transport and harvesting of organs
- Promotion of the concept of brain death, mandatory declaration of brain death, and henceforth promotion of organ donation among the common people
- Minimal charges for organ donation (retrieval) and transplantation
- Offering incentives in the form of educational and financial support to dependent children of donors
- Implementation of “presumed consent” for harvesting organs in cases of accidental deaths
- Convenient and donor-friendly official paper works.
Implications to nongovernmental stakeholders
- The NGOs along with healthcare providers should start awareness programs on organ donation in a more intensive way, involving print/social and electronic media.
There is a long way to traverse, but there is still hope to achieve what we seek.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Acknowledgement
The authors thank the students and faculties of Girijananda Choudhury Institute of Management and Technology, Azara, Guwahati.
93 Organ Donation Essay Topic Ideas & Examples
🏆 best organ donation topic ideas & essay examples, ⭐ good research topics about organ donation, 👍 interesting topics to write about organ donation, ❓ organ donation research questions.
- Importance of Organ Donation Considering the huge number of people in need of different body organs today, and the many that are dying each day due to organ problems, a socially upright member of our society should not consider […]
- Organ Donation: Willingness to Donate Organ Among Medical Students In conclusion, organ donation is a vital and life-changing procedure that can help save lives and improve the quality of life for those in need.
- The COVID-19 Impact on Organ Donation The official statistics of the United States government also support the idea that with the onset of the pandemic, the number of organ transplantation procedures has decreased. The pandemic appears to be the main cause […]
- The Organ Donation Legislation Critique She expresses outrage and condemnation of the current organ donation legislation and the politicians who drafted it. If the global majority accepts such a perspective, it will lead to a worldwide spike of violence and […]
- Researching of Xenograft and Organ Donation Doctors have been searching for methods to save lives all along, and xenograft has shown to be one of the most reliable, particularly when it comes to organ replacement. A xenograft is fraught with dangers, […]
- Organ Donation: Donor Prevalence in Saudi Arabia Donating organs does not pose a threat to the life of the donor; however, it can save the lives of many other people who need organ transplants.
- Organ Donation Registry Beginning 16th February 2010 through to the 18th the Ypsilanti Lions club organized the organ donation registry table whose main purpose was to invite people from all walks of life to literally give a piece […]
- Organ Donation: Postmortem Transplantation The ethicality of such actions has been questioned, as this procedure may be ambiguously perceived by the relatives of the deceased patient and the recipient of organs.
- The Issue of Compensation for Organ Donation Nevertheless, in spite of the fact that proponents of the compensation for the organ donation indicate obvious advantages of using this approach for the healthcare system, opponents emphasize the unethical character of such approaches.
- Organ Donation: Ethical and Legal Considerations The other approach is by requesting the family of the deceased to give consent for the donation in a case where the deceased did not permit earlier on.
- Organ Donation in Saudi Arabia: Survey Results A total of 27 participants answered the questions that were asked in the survey. The problems that are behind the ambiguity that people have over this issue are some of their limitations and perceptions.
- Organ Donation: Ethical Dilemmas An example of an ethical dilemma surrounding the procedure is the case of rich man vs.poor man, or rather, the case of a person who can afford to buy an organ on the black market […]
- Ethics of Organ Donation After Human Death In reference to this case, the ethical dilemma is related to the fact that the hospital administrator needs to disregard the necessity of informed consent for organ donation.
- Medical Ethics of Child’s Organ Donation Obviously, the parents are the only people who represent the wishes of the patient in the case. The above-mentioned position seems to be viable when it comes to the concept of the greatest good used […]
- Gene Patenting and Organ Donation Profitability is the key to violating the law, and that is the reason for the lack of transparency in the tissue market.
- Organ Donation and Transplantation Medicine Although money and financial support will be a major factor in the process of body transplant that Canavero expects to take two years, pegging human life on money is unethical.
- Organ Donation Myths: Critical Thought This essay is aimed at subverting three of the most common myths about the subject matter by considering the facts closely, relating them to the values concerning the organ donation, and isolating the issues related […]
- Organ Donation: Importance Information Because of the improved and advanced technology, the practice of organ transplant is becoming more popular and acceptable in the society.
- Organ and Blood Donation However, ethical and legal issues, and unwillingness of many potential donors to provide consents have slowed down the rate of organ and blood donation in the county.
- Ethical Issues in Organ Donation According to the authors of the study, death is defined as, “the irreversible loss of the integrated and coordinated life of the person as a single living organism”.
- The Ethics of Organ Donation in Modern World The patient is referred to a transplant center and is to their “dismay” put on a national waiting list, after a “series of interviews, physical and medical tests” to determine the suitability of the recipient […]
- Pros and Cons of Paying for Organ Donation: Arguments for Prohibition Although the potential of people to purchase organs might bring in profits to health care and increase supply and demand of transplanted organs, the fact of increased supply rates is doubtful because recent surveys prove […]
- The Nebraska Laws on Organ Donation in the United States
- Factors Influencing Organ Donation Among African Americans
- Pros and Cons of a New Opt-Out System of Organ Donation
- An Argument in Favor of Encouraging Organ Donation After Death for Transplantation Opportunities
- Beneficence Justice Malfeasance and Autonomy in Organ Donation
- The Cases of Brain Death and Organ Donation in Children and Adults
- Comparison of the Organ Donation in the U.S. and Sweden
- Compensation for Organ Donation: The Sale of Organs
- Could Death Row Inmates Be a Viable Source for Organ Donation
- Overview of the Dutch and Belgium Organ Donation Acts
- Donation of the Organs and Their Harmful Effects on the Society
- Knoweldge and Attitudes of Health Professionals on Organ Donation
- Financial Compensation for Organ Donation
- Analyzing the Importance of the Organ Donation
- The Benefits and Shotrcomes of Organ Donation
- Improving Organ Donation Through Clarification and Education
- Increasing Organ Donation via Changes in the Default Choice or Allocation Rule
- Organ Donation: Why Everyone Should Be a Donor
- Legal and Ethical Issues Regarding Organ Donation
- Mandatory Organ Donation: Ethical or Unethical
- Organ Donation: How Recipients Are Chosen and Should Donors Be Compensated
- The Discussion of the Legalization of Organ Donation
- Effects of the Organ Donation on the Lives of Thousands of Recipients
- Ethical Issues Surrounding Organ Donation
- Why Cash for Kidneys Is Better Than Organ Donation
- Organ Donation Issues and Laws: Federal and California State
- Social Madia Initiative May Help Increase Organ Donation
- Organ Donation: Life That You May Have the Power to Save
- The Best Ways to Decrease the Shortage of Organs for Transplantation
- Public Policies in the Question of Consent for Organ Donation
- Organ Donation: Keeping the Gift of Life Alive
- Description of the Commercial Market for Organ Donation
- The Controversy Associated With the Opt-Out Organ Donation
- The Life Saving Benefits of Organ Donation
- Comparing Organ Donation Programmes Across the World
- The Global Need for Organ Donations
- Why Organ Donation Should Be Encouraged
- Organ Donation: Two Deaths or One Life
- Neonatal and Pediatric Organ Donation: Ethical Perspectives and Implications
- Organ Donation and Forest Depletion Depicted in Fitzhugh’s “The Organ Grinders”
- Is There a Black Market for Organ Donation?
- What Are the Advantages and Disadvantages of Organ Donation?
- How Is Organ Donation a Lucrative Business?
- Why Do Muslims Disagree With Organ Donation?
- Is Organ Donation Against God and Nature?
- What Are the Ethical Issues in Organ Donation?
- Is the US Opt-in or Opt-Out for Organ Donation?
- Why Is Organ Donation a Moral Issue?
- How Does the Process of Organ Donation Work?
- What Ethical Theory Is Against Organ Donation?
- Does Islam Support the Concept of Organ Donation After Death?
- What Is the Most Complicated Organ Donation?
- Are Organ Donations Compulsory in China?
- Why Can’t Organ Donation Be Mandatory?
- Is There an Age Limit for Organ Donation?
- What Do Religions Think About Organ Donation?
- Why Is Organ Donation in Exchange for Money Illegal?
- Is an Opt-in or Opt-Out More Effective for Organ Donation?
- What Are the Disadvantages of Organ Donation After Death?
- Are Religious Beliefs Keeping Organ Donations From Going Mainstream?
- What Cultures Don’t Believe in Organ Donation?
- Why Is Organ Donation Uncommon in India?
- Should Presumed Consent for Organ Donation Be Used in the US?
- What Are the Laws Behind Organ Donation?
- How Does the Debate on Deontology vs. Consequentialism Stand When It Comes to Organ Donation?
- What Are the Emotional Tolls of Organ Donation for the Donor?
- How Do Living Organ Donations Compare to Deceased Organ Donations in the United States?
- What Are the Challenges of Organ Donation?
- Are There Barriers to Organ Donation in the US?
- Why Are Donated Organs Sometimes Rejected?
- Cardiovascular Diseases Titles
- Ethical Dilemma Titles
- Genetic Engineering Topics
- Healthcare Reform Essay Ideas
- Nursing Theory Questions
- Bureaucracy Paper Topics
- Fundraising Topics
- Stem Cell Essay Titles
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 2). 93 Organ Donation Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/organ-donation-essay-topics/
"93 Organ Donation Essay Topic Ideas & Examples." IvyPanda , 2 Mar. 2024, ivypanda.com/essays/topic/organ-donation-essay-topics/.
IvyPanda . (2024) '93 Organ Donation Essay Topic Ideas & Examples'. 2 March.
IvyPanda . 2024. "93 Organ Donation Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/organ-donation-essay-topics/.
1. IvyPanda . "93 Organ Donation Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/organ-donation-essay-topics/.
Bibliography
IvyPanda . "93 Organ Donation Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/organ-donation-essay-topics/.
My Portfolio
Andrew duffy.
- Literacy Narrative
- Image Analysis Essay
Argument Research Essay
- Other Works About My Writing
- Final Reflective Essay
The medical field utilizes a variety of techniques to save lives everyday. One way is to perform an organ transplant by replacing a patient’s failing organ with a working one. The problem with this is that working organs are very hard to come by, and when they do, it is not guaranteed that the organ can be transplanted. One way to obtain a transplantable organ is through donation. Organs can be donated by both living and deceased people, but very little people donate that it makes the waiting list long. One debate that is currently going on in the medical field is whether or not an opt-out system (A system where all citizens would be registered organ donors, and would have to manually opt out) should be implemented over our current opt-in system. However, there are arguments against this, stating that it would be easier to focus on smaller problems, because one giant system alone will not increase donation numbers. The best approach to increasing the number of organ donors is to improve the process by compensating donors, providing adequate support, and enact laws which strengthen the organ donation centers.
One way to increase the number of organ donors is to properly compensate donors. A big reason why people may feel hesitant to donate is because many fear that they have neither the time or the money to donate. Organ donation is not simply an appointment you make where you show up, give them a kidney, and be on your way. It is a process that takes up to three months to recover from (Thiessen C, Jaji Z, Joyce M, et al, 2017) Many are hesitant because they fear that they will be bedridden for a few month, and as a result, fear being unable to support themselves and their families. Some fear they will not be able to pay rent or even keep their job if they donate due to the healing process. Hospitals do not compensate nearly enough for most donors to live comfortably.
A fix to this problem would be to compensate fully for a person’s cost of living during their recovery, and also work with employers to give donors rights to their job. Since donation is a very rare event to begin with, the government would not suffer financing these people’s lives for a short amount of time.The government could receive the funds for donors by accepting monetary donation, and by cutting into the healthcare sector and setting aside more money for donors in these scenarios. Financial support could also be offered to help support funeral costs of deceased donors, to encourage more families to allow their loved one’s organs to be donated. If this problem were to be fixed, people might feel eager or better about donating in general. This could lead to more donations.
Another way to increase the number of organ donors is to provide adequate support for donors. One conflict that arises is that of a deceased’s wishes vs what their family wants. While someone can register themselves as a donor, it is ultimately up to their family to decide once they are deceased. As a result, many families choose not to have them donate, mostly due to what they do not know, or what they think will happen. Others feel obligated to either donate or have the deceased donated just because they believe it is moral. The problem here is that if organ donation has a reputation for guilt-tripping, less people will want to register.
The way to fix the inadequate support is to simply expand organ transplant centers, both by increasing the number of workers, and the number of educational resources. Educating the hesitant can lead to less of these ‘uncertain’ moments where they either feel obligated to make a decision that they do not have the information to make. There are a few ways to provide education, but one simple one would be to hire professionals to teach people the pros and cons of donating, the facts … etc. They could provide pamphlets that answer simple questions, and could even offer classes and a hotline for potential donors. By investing more money into professionals who can properly teach everything about organ donation, the support for donors would increase, and as a result, more would be informed enough to make the best decision for them.
By improving the process, more people may feel comfortable with either donating or not. Even in cases where donors decide to not donate, resources must be made available in order to decrease negative feelings of guilt. One study showed that most donors would prefer an alibi to break news to whoever needed a donation that they were not getting what they needed. While only a small sample of people, it still proves that many people can feel guilty by denying their receiver. These are the emotions that need to be eliminated if people are going to feel completely comfortable with donating.
The last way to increase the number of organ donations is to enact laws which strengthen organ donation centers. A problem found by a UK task force in 2008 found that one problem with organ transplantation is that the centers do not have a very tight network (Rudge C, Buggins E, 2012) Because Organ donation is a rare occurrence, and many cannot donate even if they are registered, organ donation centers are rather small (Not much is put into them) This means that these centers aren’t running as efficiently as they could be. Organs have to be properly retrieved within a certain time frame to still be usable. If the centers don’t work efficiently and cooperatively, the already small number of organs to use decreases. This applies to the U.S. as well since both countries have an opt in system, and neither have, or had the most money, or resources going into their centers. It only makes sense that if it works in the UK, it can work in the U.S. (
The way to fix this was based on the Task Force’s findings. They recommended that changes be made based on establishing official organizations that specialize in organ donation, and resolving ethical and legal issues. By doing this, the UK saw a 25% increase in deceased organ donors over three years. This suggests that if the U.S. improves its infrastructure in organ donation centers the number of donations will increase.
While the opt-out system does have its supporters, it is just not logical to enact this system over an opt-in one (By itself). While, yes, countries with this system do have a higher correlation of donations, there are a misconceptions. The best known example of a country with a opt-out system is Spain. Unsurprisingly, Spain has the highest rate of donations and donors. However, what some do not understand is that the numbers that increased were not just because of their switch to this system, Spain also improved their donation network and made access to donation easier around the same time. Over a decade, numbers started to rise, which means that the opt-out system alone is not enough to increase donation numbers.
While an opt-out system does have its benefits, it does not outweigh the benefits of improving the current system. Evidence has shown that by compensating donors, decreasing uneasiness about donating, and strengthening donation centers, donation numbers will increase. Despite the debate about which will do more, it is still important to remember that both want improvement. The issue at hand is increasing donor numbers, and more specifically, improving how to improve the number of usable organs. Neither side is wrong, and a compromise can certainly be met to synergize with each other. It is important that everyone works together in order to solve an issue as big, as timely, and as costly as organ donation is.
References Page
Henderson, M. L., & Gross, J. A. (2017). Living Organ Donation and Informed Consent in the United States: Strategies to Improve the Process. Journal of Law, Medicine & Ethics , 45 (1), 66–76. https://doi.org/10.1177/1073110517703101
Oh, T. (2015, January). Organ donation: how to increase the donor pool. Anaesthesia & Intensive Care , pp. 12–13.
Organ Donation and Transplantation Statistics. (2014, August 12). Retrieved October 31, 2017, from https://www.kidney.org/news/newsroom/factsheets/Organ-Donation-and-Transplantation-Stats
Rudge, C. J., & Buggins, E. (2012). How to Increase Organ Donation: Does Opting Out Have a Role? Transplantation , 93 (2), 141–144. https://doi.org/10.1097/TP.0b013e31823a2411
Thiessen, C., Jaji, Z., Joyce, M., Zimbrean, P., Reese, P., Gordon, E. J., & Kulkarni, S. (2017). Opting out: a single-centre pilot study assessing the reasons for and the psychosocial impact of withdrawing from living kidney donor evaluation. Journal of Medical Ethics , 43 (11), 756–761. https://doi.org/10.1136/medethics-2016-103512
Wilkinson, K., & Peet, D. (2014). Organ donation. InnovAiT , 7 (2), 109–116. https://doi.org/10.1177/1755738013506565

Search form
Latest posts, text widget.
These widgets are displayed because you haven't added any widgets of your own yet. You can do so at Appearance > Widgets in the WordPress settings.
© 2024 My Portfolio — Powered by WordPress
Original theme by Anders Noren | Adapted by ITS — Up ↑
Talk to our experts
1800-120-456-456
- Speech on Organ Donation

Introduction
Organ donation is a legal process through which the healthy organs and the tissues of one person are transplanted to another person. The person who donates his or her organs is known as a donor and the person who receives the organs is known as the organ receiver. Organ donation takes place by the consent of the donor when he or she was alive or by the consent of the family members of the donors. Organ donation is a noble act that can save millions of lives and sadly many people don't know the impact it has on other people’s lives. Even after death, a donor could bring joy to the life of the receiver.
Here we have provided a long and short speech on organ donation and along with that we have also given 10 line pointers about the organ donation speech.
Long Speech on Organ Donation
Good morning to everyone present here. Today I have been given the opportunity to give a speech on organ donation. I will try my best to make sure that everybody understands the importance of organ donation and how it could save millions of lives.
Organ donation is a process by which a person allows his or her organ to be removed and transplanted to another person in a legal manner either with the permission of the donor while he or she is alive or by the consent of close family members. So why is organ donation so important? and why is it talked about so much?.
Organ donation is a social act and it’s considered to be an honor. Organ donation can happen from a brain-dead owner or a living donor. A few of the common transplants include kidneys, liver, intestines, heart, bone marrow, and lungs. It is not required that the donor should be dead to donate an organ. In a few cases, the organs and the tissues can be donated by the living donors such as a part of the liver if the blood group of the donor and the recipient match. Similarly, part of the lungs, pancreas, and intestines can also be donated.
In India, we follow an opt-in system of organ donation. You may be thinking, what is an opt-in system?. In an opt-in system, the person who is on the death bed is presumed to have given consent to be a donor before his or her death unless they had made a specific request not to donate the organs. Organ donation in India is controlled by the Human Organ Act 1994. The legal forms for the people who are willing to donate their organs are given by India’s Ministry of health and family Welfare Government website.
Every year around 6 lakh people die in India due to the shortage or the unavailability of organs. The organ donation rate in a western country is as high as 36 million in the United States as in India it is 0.3 million which is very low. When it comes to Mumbai, it has the best organ donation rates in the country with almost 48 donations happening in the year 2019 and almost 51 donations happening in the year 2020.
Organ donation is a helpful act by the donor that can help in saving a life of a person and also could help in improving the quality of life for many individuals. Imagine if eye transplantation is done via opt-in organ donation, it could help a blind person to view this beautiful world again. The organs donated to hospitals could be used for scientific research and experiments. The donor organs are also used by medical students to learn about the anatomy of the human body. Thousands of patients wait for organ transplants as many have different organ failures such as a liver, kidney , and even heart and during those harsh times, an organ donor after his or her sad demise could become a ray of hope for the patients.
Many people believe that a brain-dead person cannot donate any organs, that is not. By brain death, one means permanent loss of brain and brain stem functions. The only activity the body can carry after the brain death is the beating of the heart, not even breathing. As long as the heart is beating the organ transplantation procedure could be carried out. Organ donation is a systematic and legal process and is governed by the government both at the national and the state level. National Organ and Tissue Transplant Organisation (NOTTO) is a national-level organization set up under the government of India that foresees all the organ donation procedures all over the country. A nonprofit organization by the name of Zonal Transplant Coordination Centre (ZTCC) which is set up in Mumbai is working every day to promote organ donation. A brain-dead person can save up to seven lives. Lives that have been suffering for many years due to organ failures. There are many inspirational stories of people who donated their organs when they were near the death door. I request every one of you to read those stories and make a note of how donating organs after death can save the lives of people who are in need.
To conclude this speech I want to say that death is inevitable and no one has escaped it.The greatest rulers who have lived before us have seen death and a newborn child who hasn’t experienced life has also witnessed death due to some circumstances. Organ donation is a noble act, a deed that could be done to save the lives of people even after the donor is dead. On this day, let us come forward and fulfill one more duty of ours as true Indian Citizens by pledging our organs which can save many lives after we leave this planet. The first step of willingness to donate an organ is to have a donor card. A donor card is an expression of a person’s willingness to be a donor. It is also important to make everyone aware of the importance of organ donation so please spread the word and help in saving lives. Thank you.
Short Organ Donation Speech
Good morning to everyone present here. Today I have been given an opportunity to give a small speech on organ donation. I hope that this speech will help everyone to spread the word about the importance of organ donation and how it can save lives.
Organ donation is a process by which a person allows his or her organ to be removed legally depending on his or her will or the consent of his family members to save the life of a person who is in need of that particular organ.
Every year around 5 lakh people die due to organ failures in India. This could be due to accidents or the failure of specific organs. Organ transplantation can help in saving the life of people who have been fighting to survive. Organ transplantation is one of the greatest achievements that modern science has been able to accomplish. Many lives could be saved and significant deaths could be avoided if organ donation is done at the right time.
Organ donation is a social act and it can be done by a living donor or a person who is brain dead. A few of the common organ transplantations include the Liver, intestines, kidneys, heart, and bone marrow. Organs are mostly donated after the death of the owner, however, many people are unaware of the noble act.
To conclude this speech I want to say that death is a mystery concept which many people don't understand. Death cannot be avoided and no one can run away from death. Organ donation is a noble act that could give a ray of hope to another person’s life who is suffering through many years because of the failure of a particular organ or organ. Be part of this noble act and have a donor card that shows the willingness of a person to donate an organ after his or her death. I wish you to live a happy life full of joy. A life in which you get a chance to impact many lives and when death knocks on your door I wish you are content with your life but also will make an impact through organ donation you give a chance for another person to live a happy life on this planet. Thank you for listening to everyone.
10 Lines About the Speech on Organ Donation
Organ donation is a legal transfer of healthy organs from the donor to the receiver.it is considered to be a good deed as a person is saving the life of another.
A person donating the organs is known as a donor and by the consent of the donor or family members, the process of organ donation takes place.
The donation of organs can happen before the death of the person or after the death of the person.
In India, we follow an opt-in system for organ donation. In the opt-in system of organ donation, the donor has given his consent for organ donation before his death.
Various organ transplantation takes place such as kidneys, lungs, liver, and bone marrow.
The transplantation of the kidney is the most common organ transplantation which occurs throughout the world.
Every year almost 5 lakh people die in India due to organ failure. Organ donation can help in saving the life of such people.
Organ donation requires detailed testing of the donor’s body. The blood group and the compatibility of the donor and the receiver are also matched before the organ is transplanted.
Organ donation provides a second chance to people who have suffered for years because of the failure of organs such as kidneys etc.
Some people also donate their entire bodies for research and medical science.
Different Types of Organ Donation:
Autograft : Autograft is the process of transplanting a person's tissues from one part of his body to another part of his body. For example, skin from the legs might be removed and used to repair damaged skin on the face or other exposed areas.
Allograft : Allograft refers to the transplantation of an organ between two genetically dissimilar persons. Because of the genetic difference, the receiver will regard the donor's organ as alien and attempt to kill it. This is referred to as s rejection.
Isograft : Isograft refers to the transplantation of an organ or tissue from a donor to a genetically identical recipient. There will be no immunological reaction, which means there will be no transplant rejection.
Xenograft : Xenograft refers to the transplantation of organs or tissues from one species to another. The heart valve of a pig, for example, has been successfully transplanted into a person.
Split Transplant : A deceased donor's organ, such as the liver, can be split between two recipients, generally an adult and a youngster.
Domino Transplant : When the lungs are to be transplanted, it is easier to replace them together with the heart surgically. If the original heart of the recipient is in good condition, it can be transplanted into another person who needs one.
ABO-incompatible transplantation : The immune systems of infants and toddlers under the age of 12 months may not have fully formed. They are able to get organs from donors who are incompatible with them.

FAQs on Speech on Organ Donation
1. What is organ donation?
Giving an organ or a portion of an organ to be transplanted into another person is known as organ donation. Organ transplantation is the only way to preserve patients' lives and enhance their quality of life who are suffering from terminal organ failure. However, there is a mismatch between supply and demand for donated organs, resulting in the death of many people. Organ transplantation has steadily expanded during the last two decades, with great success in adolescents and young adults. However, the rising proportion of older transplant patients with associated morbidity poses a challenge. As a result of innovations and advancements in perioperative treatment, the outcomes of organ transplantation continue to improve.
2. Who can be an organ donor?
Anyone, regardless of age, race, or medical history, can be a potential donor. Medical specialists examine your medical history to see whether you are eligible to donate. More people can donate now than ever before thanks to recent advancements in transplantation.
Adults can also make living donations, which means they can choose to donate an organ, such as a kidney, or a portion of an organ, such as a liver, to someone who is in need.
3. Why is there a need for organ donation?
Organ donation is required since only 3000 individuals out of 1.5 lakh people in India who require a kidney obtain one, just 1 out of every 30 people receives a kidney, and 90% of those on the waiting list die without receiving a donor. Around 70% of liver transplants require a living donor, with the remaining 30% relying on cadaver (dead) donors. As a result, there is a pressing need to raise organ donation rates and provide people a second shot at life.
4. What is the situation of organ donation in India?
Organ transplantation is in high demand all across the world. India is likewise experiencing a severe organ scarcity, with little hope of finding a solution. Every year, it is estimated that 1.5 lakh people suffer from renal failure, with just 3000 receiving a transplant. Similarly, over 2 lakh individuals die each year from liver failure or cancer, and organ donors are rarely available to save them. It is the same with heart patients: there are only 15 hearts available for transplant for every 50,000 heart attack sufferers. As a result, massive programs to raise awareness about organ donation and close the gap between supply and demand are urgently needed in India.
5. Where can I get an essay on organ donation?
Vedantu provides an essay on organ donation. It goes through the importance of organ donation, different types of organ donation, the current situation of organ donation in India, and more. Professional educators create content that is easy for students to learn and remember. Vedantu also offers study materials and a variety of competitive exams to students in grades 1 through 12. The contents contain notes, important topics and questions, revision notes, and other things. On Vedantu, you may access all of these resources for free. To access any of these resources, students must first register on the Vedantu website. You may also sign up using the Vedantu smartphone app.
Organ Donation Essay
Organ donation is a noble act of transplanting healthy organs from a donor to a patient receiver. Human body organs and tissues that function properly are collected and transplanted into patients’ bodies to save their lives. In most cases, organ donations are performed after the donor’s death. But some organs can be donated even when the donors are alive. Kids learning activities like organ donation essays will help them attain more scientific knowledge and better their academic performances.
Superheroes are not born; they are made by society. By participating in activities like organ donations, people can save lives and turn themselves into real superheroes. The following short essay in English on the necessity of performing organ donation in society will help kids improve their basic knowledge about the human body. BYJU’S importance of organ donation essay for kids will also help develop social consciousness and humanity in their minds.

Table of Contents
What is organ donation, necessity of organ donation in the society.
Organ donation can be defined as the process of transplanting an organ or tissue from one person to another person through surgical methods. The recipient performs the transplantation because of organ failure or damage caused by disease or injury. Organ donation marks the advancement of science in the medical sector.
People of all ages can perform organ donation. Organ donations are completely voluntary actions, and people cannot be compelled to engage in these activities. Illiteracy, lack of proper guidance, lack of awareness, the fright of surgery, etc., are some of the major reasons that stop a person from engaging in such charity practices. People hesitate to donate organs because of their misunderstandings related to organ donation procedures. Myths and misconceptions about organ donation have to be cleared from people’s minds. Teachers can direct their students to visit online resources like BYJU’S essay on health education to learn more about human health.
The kidney, eyes, liver, heart, skin tissues, small intestines, and lungs are some of the organs that people commonly donate. Participation in organ donation is a great form of charity and social service. It marks the contribution of individuals after death. We all should pledge to donate our organs to save lives and promote the importance of organ donation by participating in various campaigns.
World Organ Donation Day is observed annually on August 13. It is celebrated by people worldwide to raise awareness about the necessity of organ donation in society. The World Health Organisation and other health organisations conduct live classes on health-related topics to educate people. Essay writing activities on topics like the necessity of organ donation in society and organ donation essay are excellent tools for teaching the little ones about the process and importance of organ donations. For more essays, worksheets and stories , visit BYJU’S website.
Frequently Asked Questions
What is organ donation.
Organ donation is the practice of surgically transplanting an organ or tissue from one person to another person.
When is World Organ Donation Day?
August 13 is observed as World Organ Donation Day.
What do children learn from BYJU’S organ donation essay?
BYJU’S organ donation essay provides an opportunity for kids to attain knowledge of the human organ system. Practising essay writing activities will help them perform well in their academics and score good marks.
Related Links
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.
Home — Essay Samples — Nursing & Health — Medical Ethics — Informative Speech For Organ Donation
Informative Speech for Organ Donation
- Categories: Medical Ethics
About this sample

Words: 581 |
Published: Mar 13, 2024
Words: 581 | Page: 1 | 3 min read
Table of contents
Importance of organ donation, the process of donation, misconceptions about organ donation, impact of organ donation.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1229 words
1 pages / 642 words
5 pages / 2049 words
2 pages / 863 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Medical Ethics
Lollo, Amanda. 'The Ethical and Legal Issues of Surrogacy: A Case Study of Gestational Surrogacy.' Journal of Medical Ethics, vol. 44, no. 6, 2018, pp. 387-392.Blyth, Eric, et al. 'Surrogate mothers 10 years on: A longitudinal [...]
The Ariel case study presents a complex and multifaceted scenario that requires a deep understanding of various business concepts and principles. This essay aims to provide a comprehensive analysis of the Ariel case study, [...]
Ultrasound technology has revolutionized the field of healthcare in recent decades, providing a non-invasive and detailed imaging method that has become integral in the diagnosis and treatment of various medical conditions. As [...]
The Tuskegee Experiment, also known as the Tuskegee Study of Untreated Syphilis in the Negro Male, is considered one of the most notorious instances of unethical conduct in the history of medical research. The study, which began [...]
Medical Terminology is mostly originated from the Latin and Greek languages. When the Romans conquered Greece, around 400, the knowledge and language of both cultures merged, resulting in new medical concepts regarding disease [...]
They’re numerous controversial opinions about human and animal subjects. Is it fundamental in psychological research? For us to understand why we are the way we are, we must use human subjects to comprehend how we behave a [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Skip to main content
- Skip to secondary menu
- Skip to primary sidebar
- Skip to footer

ReadingJunction
Ultimate hub of educational content (Essay, Speech, Debate, Festivals, Events)
Essay on Organ Donation for Students and Children in 1000 Words
March 2, 2020 by ReadingJunction Leave a Comment
In this article, read an essay on organ donation for students and children in 1000 words. It includes meaning, celebration of organ donation day, process, demand, and black market of organ donation.
Table of Contents
Essay on Organ Donation (1000 Words)
Organ donation is a significant donation. It is also said a “reward for life” in other words. By doing this, we can give life to many people.
Nowadays, many prostitutes help in donating organs, encourage it. Nowadays, organs like kidneys, eyes, liver, heart, small intestine, skin tissue are in high demand.
Thousands of people die in an accident in the country every day whose organ donation gives life to other people. Most of the extracted organs are transplanted within 6 to 72 hours. One donor can save eight lives. Donations of liver, kidney, lungs, pancreas, and intestine can be made while alive.
Also read: Essay on Corruption Free India
What is organ donation?
Organ donation is a process in which healthy organs and tissues are taken from a human being (dead and sometimes even alive). Then these organs are transplanted to another needy person. In this way, the life of another person can be saved with organ donation. Organ Donation by One Person Donation made by one person can help 50 needy people.
Organ Donation in India
In India, the percentage of organ donation is deficient according to the population. Every year 5 lakh people in the country die due to lack of organs at the right time. In this, 2 lakh people die due to liver disease. Fifty thousand people die due to vision sickness.
Organ Donation Day Celebration
Organ donation day is celebrated on 13 August every year in government, non-governmental organizations. Institutions such as Gift Ek Jeevan, Mohan Foundation, Gift Your Organ Foundation, Dadhichi Dehdaan Samiti help in organ donation. Tamil Nadu, Maharashtra, Gujarat, Karnataka, Andhra Pradesh, Kerala, Delhi NCR, Punjab are the most donating states in the country.
Major Organs to Donate
Kidney, liver, intestine, blood vessel, intoxication, skin, bones, ligaments (ligaments) heart, pancreas, heart valves (soft bone), blood, platelets, tissue, the cornea (cornea), tendons.
Problems In Organ Donations
The rule is that in the event of a road accident, only those who died in the hospital can be taken part of their logo. Many people die at the accident site. In such a situation, no part can be found from them.
People are not aware yet. Consider it wrong. Many people do not even register to donate organs during their lifetime. People suffering from cancer, AIDS, infection, sepsis, or any serious illness cannot give an organ.
Organ donation process
A. living organ donor.
Comprehensive medical investigations are required before donating organs to living donors. It also includes the psychological evaluation of the donor to ensure that he or she understands the consequences of the donation and wants to consent to it.
b. Dead donor
With deceased donors, it is first verified whether or not the donor is dead. Death is usually confirmed many times by neuro physicians when it is determined that any part of it can be donated.
After death, they placed the body on a mechanical ventilator to ensure that the organ remains in good condition. Most organs function outside the body for only a few hours and thus ensure that they reach the recipient immediately after removal from the body.
Difference between demand and supply
The need for physical organs is much higher than the number of donors around the world. Every year many patients die while waiting for donors.
Statistics show that the average annual kidney demand in India is two lakhs, while only 6 thousand kidneys are received. Similarly, the average annual market for the heart is 50 thousand, whereas only 15 are available.
I order to increase the number of donors for organs; there is a need to create awareness among the public for donating organs.
Towards this end, the government has also taken some steps like spreading awareness through TV and the Internet, though we still have a long way to go to bridge the gap between demand and supply.
The black market of organs selling
On the one hand, where we are promoting organ donation, its theft has also happened a lot. Nowadays, the theft and black marketing of organs has increased in India.
In government-private hospitals, patients’ kidneys (kidneys), and other organs are being stolen from the nexus of the doctors.
Fake Organization
Many such organizations are active in many states who steal the organs of innocent spears. Such theft is done during the operation.
The organs are sold in foreign patients at high prices. A case of fraud continues to be exposed every day. Weak, vulnerable sections become the most victims of it.
People with plentiful money are ready to pay any cost to the limbs to save their lives. Doctors also keep stealing organs by being lured by money. Thousands of foreign patients come to our country every year, which has some part or two.
Flexibility in Law
Taking advantage of the flexible law of organ transplantation in the country, such people gain organs corruptly. Some poor patients sell their organs for money, but some are fraudulently removed.
Price of organs in the black market
Kidney – 5 to 10 lakhs Bone marrow – 2.5 million Surrogacy (rental womb) – 10 to 20 lakhs Lever – 5 to 10 lakh Heart – above 20 lakhs Cornea – 1.5 million One inch skin – according to 42 thousand rupees
What happens to organs?
Doctors quickly transplant these organs into any patients who have already needed them. Organ transplant hospitals have a waiting list. According to him, the organ is put in the patient whose number is there.
The blood group and many other tests are done for matching while performing the organ. If everything is fine, then the organ is put in, and if the match is not there, then it is matched with the next patient on the waiting list.
Time Duration for Transplant
- The liver should be transplanted within 6 hours of removal.
- The kidney should be taken within 12 hours.
- Eyes should be installed within three days.
Organ donation can save a person’s life. Its importance should not be ignored. A proper system should be encouraged to donate the organ. I hope you will like this essay on organ donation.
Reader Interactions
Leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Copyright Protection
All articles on this website are Copyright Protected. Copying or Using any material in any form is a serious offense.
Important Links
- Privacy Policy
- Terms and Conditions


Essay on Organ Donation
Students are often asked to write an essay on Organ Donation in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Organ Donation
What is organ donation.
Organ donation is when a person allows their organs to be given to someone who needs them after they die. The organs can be the heart, kidneys, liver, lungs, pancreas, or intestines. Giving an organ can save the life of someone with a sick organ that doesn’t work well.
Who Can Donate?
Almost anyone can be an organ donor. Adults and, with parent’s permission, children can choose to donate. Doctors check if the donor’s organs are healthy enough to be given to another person.
The Process of Donating
When a person dies, doctors see if they can donate. If yes, the organs are taken out carefully and quickly given to patients who need them. The donor’s family does not have to pay for this.
The Need for Donors
Many people are waiting for an organ, but there aren’t enough donors. More donors mean more people can get the help they need. It’s important to talk with your family about your choice to donate.
Organ donation is a kind act that can save lives. If you decide to be a donor, you could help someone else live a longer, healthier life after you’re gone.
Also check:
- Speech on Organ Donation
250 Words Essay on Organ Donation
Organ donation is when a person allows their organs to be given to someone else who needs them after they die. Sometimes, living people can also give one of their kidneys or a part of their liver to help another person.
Why is Organ Donation Important?
Organ donation is very important because it can save lives. Many people are sick with organs that do not work well, and they need new ones to become healthy again. Without new organs, these people might not live for very long.
Almost anyone can be an organ donor. It does not matter how old you are or what your background is. The most important thing is that the organs are healthy. Doctors check this very carefully before they put the organs into another person’s body.
How to Become a Donor
To become an organ donor, you can sign up on a special list or tell your family about your wish to donate. This way, if something happens to you, the doctors will know that you want to give your organs to help others.
Respect and Care
When organs are taken from a donor, doctors treat the donor with a lot of respect and care. The donor’s family is also given support during this tough time.
In summary, organ donation is a generous act that can give someone a second chance at life. It is a simple process to sign up, and it shows a big heart to help others in need.
500 Words Essay on Organ Donation
Organ donation is a kind act where a person allows their organs to be moved into another person’s body. When someone’s organ, like their heart or kidney, stops working well, they might need a new one. Organ donation is a way to give them a healthy organ. This can save their lives or help them feel better.
Almost anyone can choose to donate their organs. It doesn’t matter how old you are or what your background is. When a person decides to donate their organs, doctors will check to make sure the organs are healthy and can help someone else. There are two times when a person can donate: when they are still alive or after they pass away. Living people can donate parts of their liver, one kidney, or a piece of their lung. After a person dies, they can donate many organs if they said yes to donation before.
Organ donation is very important because it can save lives. Many people are waiting for an organ, and sometimes they have to wait a long time. Without a new organ, these people might not survive. By donating organs, you can help them live longer and enjoy life with their families and friends.
How Do You Become a Donor?
To become an organ donor, you need to tell others that you want to donate. You can do this by signing up on a special list or telling your family about your choice. It’s also a good idea to carry a card in your wallet that says you are a donor. This way, if something happens to you, doctors will know that you want to give your organs to help others.
The Process of Donation
If a person who wants to donate their organs passes away, doctors will check if their organs are still healthy. If they are, the organs are carefully taken out and kept in a special way so they stay healthy. Then, the organs are quickly taken to the person who needs them. Doctors will do an operation to put the new organ in the person’s body.
Concerns and Myths
Some people are worried about donating their organs. They might think that doctors won’t try to save their lives if they are donors, but this isn’t true. Doctors always work hard to save every person’s life. Another worry is about how the body will look after donation. The truth is, doctors are very careful, and the body will look the same as before.
Organ donation is a very special choice that can make a big difference in someone’s life. It’s a way to show kindness and help others even after you’re gone. By learning about organ donation and talking to your family, you can decide if it’s right for you. Remember, your choice to donate your organs could be the reason someone else gets to live a longer and happier life.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Oral Communication
- Essay on Human Heart
- Essay on Obesity Cause And Solution
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

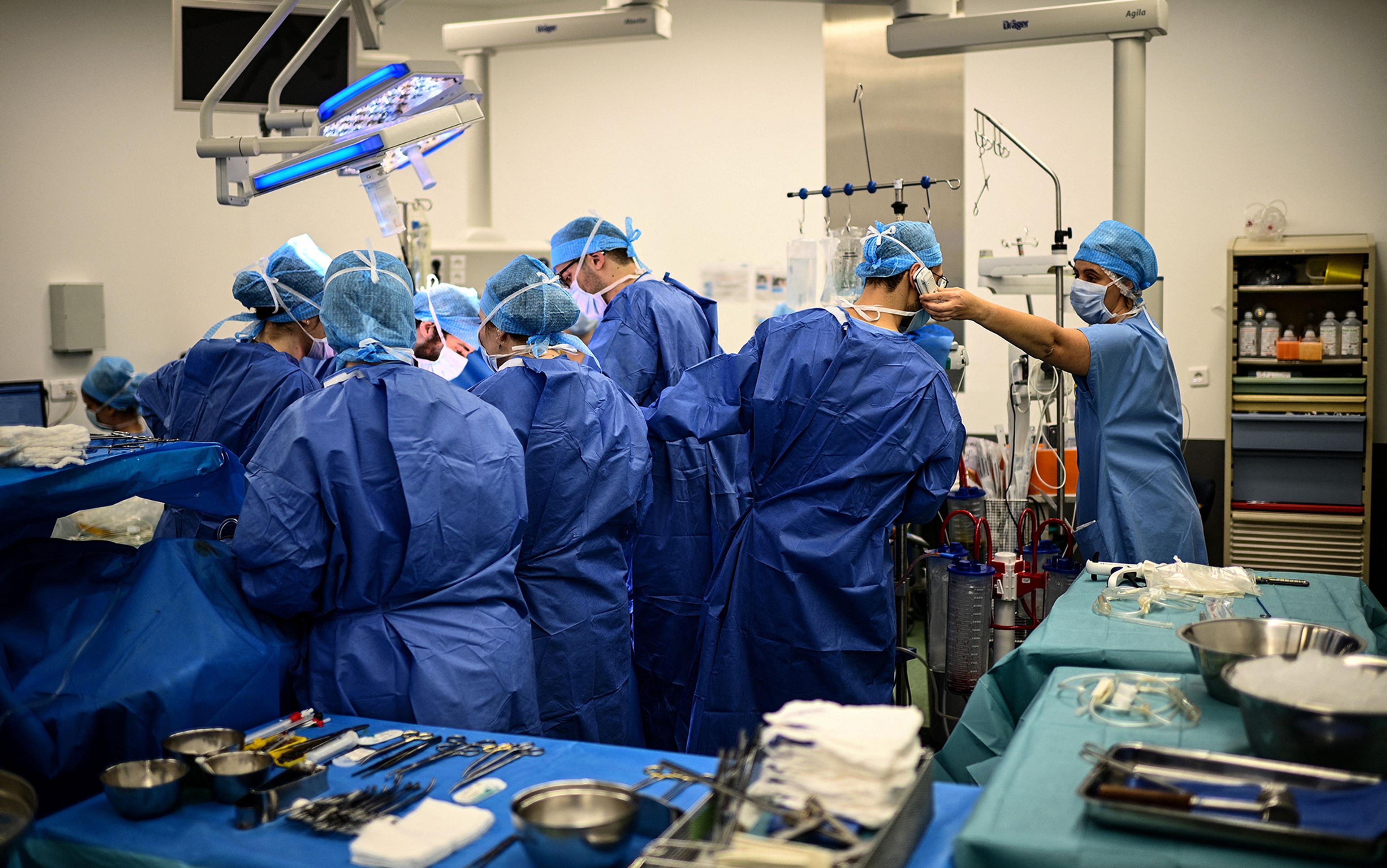
After assessing the lungs of a deceased patient, the thoracic surgeon Thomas Charrier (second from right) gives the green light for transplantation to his colleagues on the phone at the Foch hospital in Suresnes, Paris. This and all photos below taken on 9 December 2022 by Christophe Archambault/AFP. Courtesy Getty Images
Last hours of an organ donor
In the liminal time when the brain is dead but organs are kept alive, there is an urgent tenderness to medical care.
by Ronald W Dworkin + BIO
My patient was dead before I even saw her. She had been in a car accident. Now she was scheduled for organ donation.
She was called an ‘ASA 6’. To estimate operative risk, the American Society of Anesthesiologists (ASA) has a classification system built around how sick a patient is, ranging from a healthy ASA 1 to a moribund ASA 5, the latter meaning someone is not expected to live 24 hours. When the system was created in the mid-20th century, a sixth class for dead people seemed pointless. Death was known to the dead only, and life to the living only, and between the two there had been no bridge. When the definition of death changed in the late 1960s, making it possible for a person to be ‘brain dead’ but with organs still very much alive and available for donation, a bridge appeared and a sixth class was created in the early 1980s. Since 1988, when officials started collecting organ transplant data, almost a million organ transplants have been performed in the United States. Most of the organs have come from brain-dead donors. In 2021 alone, the US had almost 10,000 such donors.
When told of my upcoming case, I had mixed feelings. On the one hand, being in perfect health, unaccustomed to suffering and therefore easily disconcerted by the thought of death, I was horrified. My attitude toward death was like that of a young person standing blindfolded and tied to a post, awaiting a volley from a firing squad. The whole concept made my blood run cold. Yet the case also aroused in me a feeling of relief. Simply put, there was no risk of malpractice, as my patient was already dead. Many anaesthesiologists have such self-centred thoughts when taking care of ASA 6 patients.
I n her early 30s, she had a youthful face, without the traces of severe illness that ICU patients typically have. With her hair wrapped inside a bright, polka-dotted kerchief, she gave off an expression of almost pleasant, good-humoured cheeriness.
Who was this young person whose life had been tragically snuffed out? I jabbed into every crack of her medical record to find out. But little had been written down. Both her life and death seemed simple enough to be chronicled in a few lines. Something had happened inside her brain with the car accident, and the end came.
We wheeled her toward the operating room. Before departing, I pulled the sheet over her exposed feet. Why? I had an objection to her being dead, but I had an even more serious objection to her being undignified. With my patient still partly in the world of the living, I wanted to keep a place for her in the part that pretends to be genteel.
Six hours she had been officially dead. Now she had re-entered the world of the living
When we arrived in the operating room, something turned over inside me, sank, and went cold. After all, she was dead. The day before, she was as whole as me – and now look. She would never rise again.
After we moved her from the gurney to the operating table, the doctors and nurses, so used to taking care of living patients, stared at one another stupidly, as if not knowing why they had come together or why they stood around the table. For a brief moment, each one of us likely had the same supernatural vision, how for the past six hours, after being declared brain dead, this woman had lain under the measureless power of death. Six hours she had been officially dead. Six times had the hour hand on the clock moved – and she had lain dead. Now she had re-entered the world of the living. I would support her blood pressure and pulse. I would make her blood bright red with oxygen. Indeed, she might even wake up and look at us, I fantasised. She might be raised from the dead.

Ghoulish thinking, yet I do not write about this case to be ghoulish. Nor am I trying to stake out a new position in the bioethics debate. My purpose is more practical. Today, artificial intelligence (AI) looms over medical practice. Although unlikely to replace doctors completely, AI makes some medical activities especially ripe targets for takeover, including the harvesting of organs from brain-dead donors. And why not? Bedside manner and the common touch cease to be concerns. Using AI machines rather than doctors to harvest organs also promises to save money.
Yet this impersonal, nonhuman method of organ retrieval may discourage people from becoming organ donors , or from letting dead relatives become so, thereby exacerbating the current organ shortage. People will see pictures of organ retrieval being carried on all around by inanimate machinery in a room completely abandoned by human beings. Bodies will be brought in and sent out, while the invisible, sleepless work of the machines goes on. ‘Please, tell me this is not my end,’ people will fret privately. And they will resist consenting to organ donation.
O rgan retrieval can take place at odd hours because the time between retrieval and transplantation must be minimised. A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer. Because donation and transplantation must be synched perfectly, surgical teams must be allowed to work at any hour of the day.
Although donors are dead, managing their anaesthesia can be tricky. To keep their organs healthy, their physiology must be carefully attended to, yet brain death affects each organ system differently. High intracranial pressure can lead to an enormous outpouring of adrenaline, which can injure the heart and other organs as circulation fails. Brain death can cause pulmonary oedema (fluid in the lungs), making it hard to oxygenate the blood, thereby damaging the organs by a second route. Brain death also wreaks havoc on the body’s endocrine system, causing vital hormone levels to fall and damaging organs by a third route.
My patient lay stretched out on the table. The room was silent, as I had not yet placed any vital sign monitors on her body. It was a sinister silence. The monitors typically emit sounds that resemble the unconcerned twitter of birds. In an operating room, they symbolise life. Their absence suggests that a patient is not alive. In fact, mine wasn’t.
Nature will never permit anyone to know the exact point where brain death becomes real death
Ready to cut, the surgeon spoke through his headphones to surgeons in other cities waiting for the organs. The rest of us said nothing as he gave them an estimated time of arrival. The team had a real need for a stout word in these last few moments before the operation began. Sensing the mood, the surgeon said some dignified things about how our patient was giving other people a chance to live. Everyone nodded in agreement. He seemed thankful and sincere, yet he had to be that way for, at such a moment, anyone with even a modicum of intelligence would have felt anything else as an affront.

The surgeon cut into the patient’s chest. Almost immediately the patient’s heart rate and blood pressure jumped. It resembled the powerful surge of life that comes during a period when a person’s very existence and survival are at stake. The jump originated in a spinal reflex that stimulated the woman’s sympathetic nervous system below the level of the brain. Still, it seemed a manifestation of her will to live. Even more so when her hand moved – a sure sign of life! But that, too, was mediated through a spinal reflex.
I gave the patient some anaesthetic gas. I also gave her some opioids. Why the latter? After all, a dead patient doesn’t feel pain. In part because opioids help to lower heart rate and blood pressure directly, but also, I must admit, because I thought my patient might still be a ‘little alive’, whatever that means, and therefore in pain. Irrational on my part, yes, but the secret of life, including the definition of life, still remains the deepest and most mysterious one. Here Nature permits no eavesdroppers; never will she permit anyone to know the exact point where brain death becomes real death. At this, she draws a veil. I wanted to hedge my bets.
The woman’s blood pressure soon dropped too low. I poured fluid into her intravenous line. In the meantime, the surgeon moved hurriedly to extract her heart, clamping the large blood vessels leading both to and from it. Our fast pace betrayed another incongruence. Speed is thought to be a bit unrefined in an operating room. True, it is needed to save money, but ideally the operating room is an ordered world with calm transitions, a world without haste, except during an emergency to save a patient’s life. The visibly hasty fashion in which I and the surgeon worked made it seem like one of those urgent situations. In fact, I was trying to keep her circulation going long enough for the surgeon to tear her heart out.
I transfused a unit of blood, as excessive blood clotting, common after brain death, had made her dangerously anaemic. I turned on the warming mattress lying underneath her to keep her body temperature from dropping below 36 degrees Celsius. Brain death interferes with the body’s ability to regulate temperature, and the resulting hypothermia poses a risk to the organs. Finally, I gave her insulin to control her blood sugar level, as brain death often causes blood sugar to rise. All of these are routine lifesaving measures. In the past, I had used them to fight off death in my sickest patients, but here I had to remind myself that my patient was already dead.
T he surgeon removed her heart. The irrevocable instant had come. It was as when a train starts with a violent jerk, as if to overcome a disinclination to change its state of inertia. For many in the operating room, this was the moment when the woman’s life really ended.
A minute before, I had heard the melodies of the electrocardiogram (EKG) and pulse oximeter without really thinking about them. An anaesthesiologist’s ear is so capable of adapting itself that a continuous din, like the noise of a street or the rushing sound of a river, adjusts itself completely to their consciousness. But the unexpected halt in the sounds startled me into listening – and looking. I stared over the ether screen into the woman’s now-vacant chest cavity. It was shameful and terrible to gaze upon. Part of me felt as if I had abetted a murder around the corner.
I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate
The surgeon injected the heart with cold preservative and put it in a box. His next target was the lungs. He asked me to manually give the woman one last deep breath so that he could confirm that all parts of her lungs had been expanded before their removal. The breath I gave her was slow and gentle, like a sigh. Indeed, medically speaking, it was a sigh. On ventilators, there is a function labelled ‘sigh’ which, when pressed, gives a patient a single sustained deep breath to open up the lung’s small air sacs. Almost proudly, I imagined the sigh I gave this woman to be more human than what a machine could give. Compressing the anaesthesia bag with my hand, I imagined how she might have sighed in the past, on her own, in the face of some bitter reality, some trick or force of fate, crushing her heart but also uplifting her. I tried to make this last sigh worthy of the moment, a sigh that only another human being could replicate, a deep breath that begins with disappointment, passes into resignation, and ends in acceptance. I crafted that last sigh as if it were the epilogue to a tragedy.
When the woman exhaled her last bit of sigh, I removed her breathing tube. The surgeon took out her lungs and stapled her windpipe shut. At this point, there was little for me to do, and my inactivity plunged me into a sense of nothingness. I felt I was going to gag on my thoughts if I didn’t do something. I walked away from my patient to look inside a cupboard. I opened a few drawers. Then I felt badly for doing so. Although one of us was dead, still there seemed to be two of us here. It’s as if the woman and I were friends and I didn’t want to leave my friend. I went back and stood by her head.
The surgical team removed the rest of her organs and the case finished. Here the woman and I reached a parting of the ways. I stared at her face seriously and fixedly as though I wanted to look my fill and imprint forever on my memory her image. I cannot recall for how long I looked. Great moments are always outside of time.
Our relationship proved significant. Nothing is more characteristic of the total lack of spiritual connection between myself and other patients than the fact that I have forgotten most of their names and faces. But this woman’s name and face I remember. And when I speak of memory, I do not mean something akin to a register kept in a well-ordered office, a place in which documents are laid away in store. I mean something submerged in the rushing stream of my blood, memory as a living organ in which every feeling experienced that day retains its natural essence, its original intensity, its primary historical form.

M y patient lived longer than what her death certificate says. She lived in my mind during the organ retrieval and continues to live in my memory because I do not want to forget her, and because I cannot forget her. Although I know only her general outlines, our connection satisfies some deep law of harmony underlying all life, in which every person must enter into communion with another person in order fully to live. By that standard, my patient lived past her official time of death.
When AI replaces the anaesthesiologist during organ retrievals, you, the organ donor, will not live any longer than what’s listed on your death certificate. The air inside the operating room is already cold, dry and unpleasant. Various monitors will sit on the top shelf of the anaesthesia machine, regulated by AI. Their special melodic rings will no longer be necessary, as their data will be sent along to AI in silence. Care will be delivered without the mediation of human minds, senses or hands.
Before your lungs are removed, the machine’s ventilator bellows will go up, down, up, down. Capable only of whooshing and not ringing, the bellows will seem to call sadly through the cold air to the monitors sitting above, waiting fruitlessly for a response. What a simple, insignificant movement: up, down, up, down, never getting away from the same place. It will be the only activity surrounding your head amid the metal machines, with their cold, menacing gleam. Nobody will be sitting next to you to wonder about what you were like, or about the things that distinguished your personality and made it special. A vision of the future arises: similarly deserted operating rooms with AI machines all moving automatically, while the people who used to work in them have gone off somewhere to sit dreamily on the grass beneath the sky.
Medicine has tapped a new source of organs in the form of donation after circulatory death
It seems a decidedly unpleasant environment in which to meet one’s end, and enough to discourage those on the fence from becoming potential organ donors. Rather than live a bit longer in the mind of another person, rather than have that person think about you and wonder about you, entertain irrational imaginary concerns about you, slip a little extra narcotic into your intravenous line ‘just in case’, engage in metaphysical speculations about your breathing pattern, and imagine you a friend, you will be alone on the table, and your surgery will more closely resemble a bandit raid. The machines will be determined to take everything, every organ. Reduced to financial terms, it will be as if you were left penniless.
Worse, a new danger will come to overlie the chilling sense of emptiness, scaring even more people away from becoming organ donors. Because there are already too few brain-dead donors – each year, more than 8,000 people in the US die while on the waiting list for organs – medicine has tapped a new source of organs in the form of donation after circulatory death (DCD). These organ donors are not brain dead, although many of them are unconscious. Instead, they lack circulatory or respiratory activity after being disconnected from artificial life-support systems. Without such activity after a few minutes of so-called ‘no touch’, they are declared dead, and their organs become available for donation. Their numbers have been growing over the past two decades. Today, they account for about 10 per cent of transplanted organs in the US.
The problem is that certain medicines necessarily given to these donors before death, but in expectation of death, may hasten their death. The medicines are given for the sole purpose of making their organs more viable for transplantation. Heparin, for example, prevents blood clotting, while phentolamine dilates blood vessels and improves blood flow to the organs. Yet heparin also increases the chances of bleeding into the brain, while phentolamine may lower blood pressure to the degree that a person goes into shock. Although these patients are near death for other reasons, the medicines may become their actual cause of death. This makes doctors uneasy; hence the rule not to give these medicines to donors prone to bleeding or with low blood pressure.
Y et the rule risks driving away potential donors, who will naturally think: ‘Doctors won’t give you these medicines to kill you; on the other hand, they won’t give you these medicines to help you. At some point, doctors aren’t really on your side. But when?’ As the number of brain-dead donors drops, medicine will increasingly rely on DCD donors to compensate. Already sensitised by the image of surrendering their organs to machines in a metallic desert, potential donors will fear being herded into the ‘imminent death’ category to meet some organ quota, a fear only heightened when word gets out that doctors are not always their advocates.
Currently, doctors in the US must get consent before declaring people DCD donors, but another model, called the ‘presumed consent model’, already operates in other countries and allows the recovery of organs without prior authorisation. A cascade of events threatens to turn organ retrieval into a kind of science-fiction nightmare, where organ shortages lead to medicines being given to people to preserve their organs while possibly hastening their death, all without telling them the plan or asking for their permission.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines
Whenever people start to think about becoming an organ donor, they immediately make a leap to their own precious person. Who am I, what am I, what am I without my organs, and so forth. It is part and parcel of being a human being. That some people are willing to surrender their organs after death suggests that, to feel oneself human, they need more than merely having a whole body; they also need an atmosphere of simple humanity. To feel human, people need to feel that they occupy space in the thoughts and feelings of others. It is why they consider becoming organ donors in the first place. They imagine helping others by giving up a part of themselves in the future. In exchange, they imagine the recipients thinking from time to time about what they, their donors, were like. In that way, the donors feel a connection with whomever those recipients might be, and feel somehow fulfilled.

I’d like to think that caring for my brain-dead patient satisfied some small part of this need to feel human, whether on the part of my patient before she died and who perhaps lived in expectation of becoming a donor one day, or on the part of her relatives who gave their consent to the procedure after she was declared brain dead. Either way, I connected with her or with her family.
My experience in the operating room serves as a warning to those eager to cut corners and replace doctors with AI machines willy-nilly. You don’t satisfy people’s urge to feel human by making the bridge to the next world a totally inhuman one.
The lesson extends far beyond organ donation. AI promises to make healthcare quicker, more precise, and error-free. To the degree that it replaces doctors and nurses, it portends a massive shift in medicine that seems to come every 30 years, when people are so overwhelmed by the burden of their own technological creations, they need every iota of their strength to adjust. Once again, with the advent of AI, advancements promise to put healthcare on an entirely new footing and, once again, the inevitable backlash will be there. So it was in the 1960s, when new medical technologies and procedures, such as home dialysis machines and coronary artery bypass surgery, improved life, and yet, during this same period, the medical profession’s reputation plummeted, as patients complained that doctors had grown cold and impersonal. So it was in the 1990s, when the rise of managed care promised greater efficiency at less cost, and a ‘win-win’ strategy anchored in preventive medicine, led to a patient rebellion against being treated like cattle, including their inability to choose their own doctor, and rushed visits to practitioners ‘on the plan’.
Now, in the 2020s, the stage is set for outrage, yet again. AI promises to elevate healthcare; but, to the degree that it replaces doctors and nurses, it also threatens to depersonalise patients and to wash off their distinctive colours until everyone has the same drab tint. In the crucible that looms, patients are going to rebel. And it is in the arena of organ donation, where they face death by machine, that they are likely to baulk loudest, and first.
Quantum theory
Quantum dialectics
When quantum mechanics posed a threat to the Marxist doctrine of materialism, communist physicists sought to reconcile the two
Jim Baggott

Nations and empires
A United States of Europe
A free and unified Europe was first imagined by Italian radicals in the 19th century. Could we yet see their dream made real?
Fernanda Gallo

Stories and literature
On Jewish revenge
What might a people, subjected to unspeakable historical suffering, think about the ethics of vengeance once in power?
Shachar Pinsker

Building embryos
For 3,000 years, humans have struggled to understand the embryo. Now there is a revolution underway
John Wallingford

Design and fashion
Sitting on the art
Given its intimacy with the body and deep play on form and function, furniture is a ripely ambiguous artform of its own
Emma Crichton Miller

Learning to be happier
In order to help improve my students’ mental health, I offered a course on the science of happiness. It worked – but why?
How America’s organ transplant system can be improved

Ali Rogin Ali Rogin
Kaisha Young Kaisha Young
Leave your feedback
- Copy URL https://www.pbs.org/newshour/show/how-americas-organ-transplant-system-can-be-improved
Nearly 115,000 people are currently waiting for a new organ. But the shortage crisis is nothing new, as 5,600 people die each year waiting for an organ. Ali Rogin spoke with Barry Friedman, the former executive director of the AdventHealth Transplant Institute, about what can be done to revamp the nation’s organ donation and transplant process.
Read the Full Transcript
Notice: Transcripts are machine and human generated and lightly edited for accuracy. They may contain errors.
Laura Barron-Lopez:
Last week, a Massachusetts man who was the first person to receive a genetically modified pig kidney transplant died. The hospital where he underwent the surgery did not find any indication that his death was linked to the transplant.
But his case again put a spotlight on the organ transplant system and the extraordinary measures being taken to make up for its shortfalls. Ali Rogin has the latest on what can be done to revamp the nations organ transplant process.
Kidneys topped the list of the most needed organs in the US. Nearly 115,000 people are currently waiting for a new organ. But the shortage crisis is nothing new. Last year, more than 46,000 organ transplants were performed. But 5,600 people still die each year waiting for an organ.
Barry Friedman is the former executive director of the AdventHealth Transplant Institute. A hospital specializing in organ donation and transplant. He's now a part of Guidry and East, an organ transplant consulting firm. Barry, thank you so much for being here. What's driving the organ transplant backlog in the US?
Barry Friedman, Chief of Strategy, Guidry and East Transplant Consulting: Currently, our wait lists continue to grow. And as those wait lists grows, we have to ensure that the organs that we are recovering are utilized properly.
In this country right now, the way we distribute organs across the country, we try to get it to the right patient at the right time. So this may mean putting kidneys on commercial airplanes or charter aircraft to get those kidneys to the patient. And there truly has been some challenges and delays in getting that done. We are becoming more efficient. We're trying to create longer preservation times for these organs so that we can either keep them on controlled ice or machine perfusion.
And there's a lot of technology that has really helped us to improve that. And I think we'll beginning to see a change in ensuring that we're getting these kidneys transplanted.
And the procurement numbers, though, in this country, don't seem to line up very much with those in other parts of the western world. In 2020, more than 20 percent of procured kidneys were not transplanted. So the kidneys were there, but they just didn't make it into bodies. And those numbers are way higher than those of other countries, particularly in Europe. So I wonder what explains that disparity.
Barry Friedman:
When we look at the year 2020 and then the COVID coming on board with kidney allocation, it's critical that we're able to get the right kidney to the right patient. And we've done a tremendous job increasing the number of organs that are donated in this country, and we're grateful for those donor families and for the staff that work there.
However, we're not able at all times to match the exact kidney to the right patient. We're getting better at that and some of these kidneys because we really do want to achieve the most number of transplants.
So would you say that is mainly a geographical issue? I mean, the United States is a big country, and logistically it can be hard to get these organs from point A to point B in a timely manner.
That's part of the challenge. We need to move those organs efficiently, and we got to ensure that we are using the right transportation mode, whether it's commercial aircraft or charter aircraft or even occasionally government aircraft, to help support getting these vital organs to the correct hospitals and transplant patients.
There is also a growing body of research and industry opinion that says that the U.S. is actually discarding imperfect organs that still might work well in a transplant. What do you make of that?
Again, putting this in the hands of the capable physicians and surgeons that care for these patients is critical. The challenge that we see is getting the right kidney to the right patient, and we're making better changes in our organ allocation. We have a very collaborative society in the United States for the 250 plus transplant centers that are equipped to do these organ transplants.
And there is still a learning curve that we're trying to achieve as we see more technology and how we perfuse these organs, how we package these organs until we can get them into the transplant recipient. So we are making great progress.
And as you mentioned, there are still more reforms to come. The Biden administration has announced plans to modernize the current transplant system. They want to break up the responsibilities held by the nonprofit United Network for Organ Sharing, or UNOS, which is the only government contractor to ever operate the US transplant system. Are those efforts going to help fix things?
I believe they are, and it's time for improvement. And I'm hopeful that the lessons we've learned over the last 40 years with the united Network of Organ Sharing, that will take those lessons and incorporate it and bring in the new technologies that are so important. And the Biden administration, the previous administration, both have been very supportive.
This is a bipartisan issue, and this is one of the areas where I feel our government has done a good job in helping to help fund the necessity of increasing the number of transplants.
What does need to change, in your view? You said that there was, you know, a lot of margin for improvement.
So I think as we continue to learn how we can best allocate those organs and get them to the right patient. What's unique in organ transplant is the physicians and surgeons that have dedicated their careers to doing this. And this is a fairly young procedure that we're doing. It really began in the 1960s with kidneys seventies. We're making tremendous headway in how we can ensure we can get the right kidney to the right patient.
We're doing a much better job in 2024. Obviously, we still have to work on that number of organs that we're not using. We try to get away from using the word discard because these families have graciously donated those organs and we're unable to use them, is what we're now saying.
I want to ask also about the racial disparities that seem to persist in kidney donation. In particular, black people are over three times more likely. Hispanic people are 1.3 times more likely to have kidney failure than white people. But white Americans are more likely to have a kidney transplant than either black or Hispanic Americans. Why is this and what needs to change?
Obviously, we try to match the genetics. It's not just the kidney itself. It's the blood type and the genetic tissue typing that we do, and we try to match that up. The more blacks, the more Asians, the more that from a racial perspective, we're able to get those kidneys in the pool. I think we'll see an increase.
We've also learned over the years, as technology has changed, how we diagnose, say, what kidney is acceptable for what patient. And we're trying to adjust that so we give more points to patients that may be disadvantaged.
That is organ transplant specialist Barry Friedman, thank you so much for joining us.
Thank you, Ali.
Listen to this Segment

Watch the Full Episode
Ali Rogin is a correspondent with the PBS NewsHour and PBS News Weekend.
Kaisha Young is a general assignment producer at PBS News Weekend.
Support Provided By: Learn more
More Ways to Watch
- PBS iPhone App
- PBS iPad App
Educate your inbox
Subscribe to Here’s the Deal, our politics newsletter for analysis you won’t find anywhere else.
Thank you. Please check your inbox to confirm.
- Share full article
Advertisement
Supported by
Patient Dies Weeks After Kidney Transplant From Genetically Modified Pig
Richard Slayman received the historic procedure in March. The hospital said it had “no indication” his death was related to the transplant.

By Virginia Hughes
Richard “Rick” Slayman, who made history at age 62 as the first person to receive a kidney from a genetically modified pig, has died about two months after the procedure.
Massachusetts General Hospital, where Mr. Slayman had the operation, said in a statement on Saturday that its transplant team was “deeply saddened” at his death. The hospital said it had “no indication that it was the result of his recent transplant.”
Mr. Slayman, who was Black, had end-stage kidney disease, a condition that affects more than 800,000 people in the United States, according to the federal government, with disproportionately higher rates among Black people.
There are far too few kidneys available for donation. Nearly 90,000 people are on the national waiting list for a kidney.
Mr. Slayman, a supervisor for the state transportation department from Weymouth, Mass., had received a human kidney in 2018. When it began to fail in 2023 and he developed congestive heart failure, his doctors suggested he try one from a modified pig.
“I saw it not only as a way to help me, but a way to provide hope for the thousands of people who need a transplant to survive,” he said in a hospital news release in March.
His surgery, which lasted four hours, was a medical milestone. For decades, proponents of so-called xenotransplantation have proposed replacing ailing human organs with those from animals. The main problem with the approach is the human immune system, which rejects animal tissue as foreign, often leading to serious complications.
Recent advances in genetic engineering have allowed researchers to tweak the genes of the animal organs to make them more compatible with their recipients.
The pig kidney that was transplanted into Mr. Slayman was engineered by eGenesis, a biotech company based in Cambridge, Mass. Scientists there removed three genes and added seven others to improve compatibility. The company also inactivated retroviruses that pigs carry and could be harmful to humans.
“Mr. Slayman was a true pioneer,” eGenesis said in a statement on social media on Saturday. “His courage has helped to forge a path forward for current and future patients suffering from kidney failure.”
Mr. Slayman was discharged from the hospital two weeks after his surgery, with “one of the cleanest bills of health I’ve had in a long time,” he said at the time.
In a statement published by the hospital, Mr. Slayman’s family said he was kind, quick-witted and “fiercely dedicated to his family, friends and co-workers.” They said they had taken great comfort in knowing that his case had inspired so many people.
“Millions of people worldwide have come to know Rick’s story,” they said in the statement. “We felt — and still feel — comforted by the optimism he provided patients desperately waiting for a transplant.”
Virginia Hughes is an editor on the Health and Science desk. More about Virginia Hughes
The ESAIC is dedicated to supporting professionals in anaesthesiology and intensive care by serving as the hub for development and dissemination of valuable educational, scientific, research, and networking resources.
About Esaic

The ESAIC hosts the Euroanaesthesia and Focus Meeting congresses that serve as platforms for cutting-edge science and innovation in the field. These events bring together experts, foster networking, and facilitate knowledge exchange in anaesthesiology, intensive care, pain management, and perioperative medicine. Euroanaesthesia is one of the world’s largest and most influential scientific congresses for anaesthesia professionals. Held annually throughout Europe, our congress is a contemporary event geared towards education, knowledge exchange and innovation in anaesthesia, intensive care, pain and perioperative medicine, as well as a platform for immense international visibility for scientific research.
Upcoming scientific events
Euroanaesthesia 2024
25 - 27 May 2024 Munich
Euroanaesthesia 2025
25 - 27 May 2025 Lisbon
Professional Growth
The ESAIC's mission is to foster and provide exceptional training and educational opportunities. The ESAIC ensures the provision of robust and standardised examination and certification systems to support the professional development of anaesthesiologists and to ensure outstanding future doctors in the field of anaesthesiology and intensive care.
Education & Training
Esaic programmes, upcoming education, training & exam events.
Post operative pulmonary complications
04 Jun 2024
BCSAC 2024 – Weekend 1
08 - 09 Jun 2024
Registration Period for EDAIC Part I 2024
18 Mar - 10 Jun 2024
The ESAIC aims to advance patient outcomes and contribute to the progress of anaesthesiology and intensive care evidence-based practice through research. The ESAIC Clinical Trial Network (CTN), the Academic Contract Research Organisation (A-CRO), the Research Groups and Grants all contribute to the knowledge and clinical advances in the peri-operative setting.
Learn more about the ESAIC Clinical Trial Network (CTN) and the associated studies.

EU Projects
The ESAIC is actively involved as a consortium member in numerous EU funded projects. Together with healthcare leaders and practitioners, the ESAIC's involvement as an EU project partner is another way that it is improving patient outcomes and ensuring the best care for every patient.

Patient Safety
The ESAIC aims to promote the professional role of anaesthesiologists and intensive care physicians and enhance perioperative patient outcomes by focusing on quality of care and patient safety strategies. The Society is committed to implementing the Helsinki Declaration and leading patient safety projects.
Upcoming Patient Safety events
ESAIC Advanced Patient Safety Course – London
01 - 02 Jul 2024 London
Patient Safety and Quality Masterclass
25 - 27 Nov 2024 Amsterdam
Sustainability
To ESAIC is committed to implementing the Glasgow Declaration and drive initiatives towards greater environmental sustainability across anaesthesiology and intensive care in Europe.
More interesting links

Partnerships
The ESAIC works in collaboration with industry, national societies, and specialist societies to promote advancements in anaesthesia and intensive care. The Industry Partnership offers visibility and engagement opportunities for industry participants with ESAIC members, facilitating understanding of specific needs in anaesthesiology and in intensive care. This partnership provides resources for education and avenues for collaborative projects enhancing science, education, and patient safety. The Specialist Societies contribute to high-quality educational opportunities for European anaesthesiologists and intensivists, fostering discussion and sharing, while the National Societies, through NASC, maintain standards, promote events and courses, and facilitate connections. All partnerships collectively drive dialogue, learning, and growth in the anaesthesiology and intensive care sector.
Upcoming external & endorsed events
ASA NSC 2024
06 - 09 Sep 2024 Darwin
69th Brazilian Congress of Anaesthesiology (CBA)
13 - 16 Nov 2024 Belo Horizonte
Guidelines play a crucial role in delivering evidence-based recommendations to healthcare professionals. Within the fields of anaesthesia and intensive care, guidelines are instrumental in standardizing clinical practices and enhancing patient outcomes. For many years, the ESAIC has served as a pivotal platform for facilitating continuous advancements, improving care standards and harmonising clinical management practices across Europe.

Publications
With over 40 years of publication history, the EJA (European Journal of Anaesthesiology) has established itself as a highly respected and influential journal in its field. It covers a wide range of topics related to anaesthesiology and intensive care medicine, including perioperative medicine, pain management, critical care, resuscitation, and patient safety.
Latest EJA publications

Becoming a member of ESAIC implies becoming a part of a vibrant community of nearly 8,000 professionals who exchange best practices and stay updated on the latest developments in anaesthesiology, intensive care and perioperative medicine. ESAIC membership equips you with the tools and resources necessary to enhance your daily professional routine, nurture your career growth, and play an active role in advancing anaesthesiology, intensive care and perioperative medicine.
Membership opportunities at the ESAIC

Congress Newsletter 2024
Ethical Controversies in Organ Donation Persist in the Twenty-First Century
Advancements in surgical techniques and the availability of effective immunosuppressive medications have made life-saving organ transplantation a reality for thousands of individuals whose medical conditions lead to end-stage organ failure. Intensive care doctors and anesthetists, who play a key role in managing potential organ donors and streamlining the transplantation process, must navigate guidelines, institutional protocols, and ethical issues that are inherent in the process of human organ donation.
At this year’s Euroanaesthesia congress, attendees will have the opportunity to improve their understanding of what constitutes a diagnosis of death and learn more about the ethical issues surrounding the donation of human tissues and organs. During Saturday’s symposium titled “Organ donation in the 21st century – A journey of hope or a road to dystopia?”, speakers will discuss current methods of defining death and their deficiencies, the ethical implications of organ donation after euthanasia, and other emerging ethical concerns related to organ transplantation.
After a century of medical progress, organ transplantation remains fraught with ethical dilemmas, according to Dutch anesthetist Jan Albert Maria Bollen, MD, who will tackle the ethical debate on organ donation after euthanasia during Saturday’s session. Bollen’s research on euthanasia through living organ donation 1 , under the supervision of Professor Walther van Mook, MD, PhD, at the Maastricht University Medical Center, helped to raise awareness about the ethical, legal, and medical challenges of the procedure combining medical assistance in dying with organ donations after the circulatory determination of death. A protocol that is now implemented in Dutch hospitals provides a framework for the removal and transplantation of viable organs immediately after euthanasia.
While organ donation after physician-assisted death resides in an ethical gray area, transplant tourism has been denounced as a violation of human rights and a public health risk by international medical organizations. Nevertheless, this phenomenon has continued to grow in response to a shortage of viable organs, becoming an integral part of the burgeoning medical tourism industry.
“In Europe and the United States, people who need an organ are waiting on transplant lists – or you can fly to the Philippines or Malaysia and buy an organ,” said Robert L. Klitzman, MD, a Professor of Psychiatry at Columbia University Irving Medical Center in New York, NY. Klitzman, who also serves as Director of the Masters of Bioethics Program at Columbia, will discuss the ethical implications of organ markets during the symposium.
“In the United States, there is a major debate about making the purchase and sale of organs legal,” the speaker added. “It would be wealthy people buying organs from poor people.” Organ markets catering to wealthy foreign nationals are an established practice in the Philippines and Malaysia, with brokerage companies facilitating connections across the borders. The donors ultimately pay the price, Klitzman said, noting that the money they receive is almost always insufficient to lift them and their families out of poverty and that donors experience poorer health and increased financial burdens over time. Donor exchanges have recently emerged as an alternative to transplant tourism in developed countries. Known as domino transplants, these directed donations from relatives who are not compatible donors for their loved ones may provide an ethical solution to the donor shortage.
When it comes to transplantations involving deceased donors, the process relies on the accurate determination of death. Dale Gardiner, MD, an intensive care consultant at Nottingham University Hospital in Nottingham, United Kingdom, and chair of the Nottingham University Hospital’s Ethics of Clinical Practice Committee, will discuss the different sets of criteria used to diagnose death in the clinical setting, as well as the efforts to reach consensus about the notion of human death in the context of organ transplantation. Gardiner is the co-author of an international collaborative statement on expanding controlled donation after the circulatory determination of death. 2 The statement was conceived to encourage the creation of deceased-donor programs worldwide and help countries become self-sufficient in terms of organ transplantation. In addition to describing the process of determining a prognosis that justifies the withdrawal of life-sustaining treatment and establishing the permanent cessation of circulation to the brain as the standard for determining death by circulatory criteria, the statement also attempts to draw a clear line between the determination of death and any consideration of organ donation. Following the necessary steps in the process of deceased organ donation is key to converting potential donors into actual donors, thus increasing the number of organs available for transplantation.
References:
- Bollen JAM, Shaw D, de Wert G, et al . Euthanasia through living organ donation: Ethical, legal, and medical challenges. J Heart Lung Transplant 2019;38(2):111-113.
- Domínguez-Gil B, Ascher N, Capron AM, et al . Expanding controlled donation after the circulatory determination of death: statement from an international collaborative. Intensive Care Med 2021;47(3):265-281.
Related news
The Ethics Police – Untangling the Thread of Human Research Ethics

Is an anaesthesiologist required on board during mission to Mars?

More science, more networking, more knowledge
Can Animal Organ Transplants Save Thousands of Dying People?
Bmc’s kidney transplant director discusses mass general’s landmark pig kidney operation.

Rick Slayman died after receiving a pig kidney for his end-stage kidney failure, but his Massachusetts General Hospital caregivers said the transplant was not the cause of his death. Photo by Massachusetts General Hospital
Rich Barlow
An average of 17 people waiting for organ transplants die each day in the United States. Might patients and doctors have a life-saving workaround in animal organs?
The tantalizing prospect follows the transplant at Massachusetts General Hospital in March of a pig kidney into a 62-year-old with end-stage kidney failure. The patient, Rick Slayman, died almost two months later, although the hospital says it has no indication that his death was related to the transplant. The kidney had been genetically edited to purge harmful pig genes and add human ones.
BU Today asked Jean Francis , an associate professor of medicine at Boston University’s Chobanian & Avedisian School of Medicine, about the state of the field. Francis is medical director of the kidney transplantation program at Boston Medical Center (the medical school’s teaching hospital and New England’s largest safety net hospital) and medical director of the pancreas transplant program at Boston’s Brigham and Women’s Hospital.
This interview was edited for clarity and brevity.
with Jean Francis
Bu today: which organs—and from which animals—show the most promise for successful transplantation into humans are any of these animal organ transplants in clinical trials.
Francis: As of now, very limited trials have occurred, using organs from pigs only. The organs trialed are the heart and kidneys. Two patients underwent heart transplants at the University of Maryland under an extremely strict immunosuppressant regimen. One heart transplant lasted a bit above 40 days and the other close to two months. Both hearts ended up being rejected (although this is still debatable), but both patients died after the transplant failed. This was one of the first trials showing the feasibility of such transplants and giving clinicians some ideas about what to expect regarding complications. A program in New York City transplanted two potentially [terminal] patients on life support with pig kidneys, connected to the radial arteries in the forearm, for two days before withdrawing support on those patients. Both kidneys showed no signs of rejection, produced urine, and as a proof of concept, they were able to show that no super-acute rejection would happen if such transplants are performed in the future. Those trials encouraged the MGH group to move forward recently with the first swine-to-human kidney transplant on a patient who has been on dialysis for a couple of years, after losing his first kidney transplant from a deceased human donor. As of now, the only animal that has the potential to be an organ transplant donor for humans is the pig. Those animals are genetically engineered to make them human-compatible. Further refinements of those modifications are always being revised. More than 100,000 patients are currently on the kidney transplant list [in the United States], and close to 5,000 patients die yearly while waiting for kidney donors. If the modified pig kidney proves its efficacy, it will eliminate the organ shortage and the waiting time. Before widespread use of those organs, a well-organized, large, multicenter trial is needed to support the benefit of such a procedure.
BU Today: At the moment, what are the medical obstacles to successful animal-to-human transplants?
Francis: The main obstacles are genetic compatibility. Without genetic manipulation of the pig kidneys, we will reject them automatically upon transplant. We have to make those kidneys human-compatible by removing or eliminating some antigens expressed on the inner layers of the blood vessels of those pig organs. Humans have preformed antibodies against those antigens, and they will trigger acute rejections. Those antigens are eliminated by genetic manipulation. Other modifications are needed to render those organs less able to induce clotting, and also make those organs more resistant to the potent immune system humans have, which we call the complement system. Complement activity needs to be controlled to prevent injury to swine grafts. Those swine organs are protected from the complement injury with special medications given at time of transplant. Also, the genetic modifications on those swine organs render them more resistant to the complement attack and injury. Last, those swine organs come to us with endogenous viruses that are part of the pig genetic material. Genetic engineering has been able to remove some of the swine retroviruses, but we don’t know if others are still there. So, close monitoring for transmitted infections from swine to human recipients is also of concern, although the data support safety so far on those very limited cases.
I am very optimistic that swine transplant will become available for a lot of patients with no other options. I feel this is the future, the moonshot of transplant. Jean Francis
BU Today: Does Mr. Slayman’s death affect your optimism about swine organ transplants?
The unfortunate passing of Mr. Slayman should not affect our determination to move forward with xenotransplantation , especially given that as of now there is no indication that his passing is attributed in any way to his pig kidney. This is based on what has been released from the treating team. Mr. Slayman was determined to be the first candidate to receive such a kidney in the hope of helping advance the field. I am very confident that Mr. Slayman [would] not want his passing to stop us from achieving his desired wish of making xenotransplantation possible. Definitely, every caution should be taken to prevent any future complications. This is going to be a long process until we fully grasp all the issues related to xenotransplantation, but we should be determined for the sake of our patients to keep advancing this field until it becomes available for many patients. I am very optimistic that swine transplant will become available for a lot of patients with no other options. I feel this is the future, the moonshot of transplant. This will come only after rigorous studies supporting safety, patients’ and organ survival, and after optimization of those engineered organs. Stay tuned.
Explore Related Topics:
- Chobanian & Avedisian School of Medicine
- Share this story
- 0 Comments Add
Senior Writer

Rich Barlow is a senior writer at BU Today and Bostonia magazine. Perhaps the only native of Trenton, N.J., who will volunteer his birthplace without police interrogation, he graduated from Dartmouth College, spent 20 years as a small-town newspaper reporter, and is a former Boston Globe religion columnist, book reviewer, and occasional op-ed contributor. Profile
Comments & Discussion
Boston University moderates comments to facilitate an informed, substantive, civil conversation. Abusive, profane, self-promotional, misleading, incoherent or off-topic comments will be rejected. Moderators are staffed during regular business hours (EST) and can only accept comments written in English. Statistics or facts must include a citation or a link to the citation.
Post a comment. Cancel reply
Your email address will not be published. Required fields are marked *
Latest from BU Today
To do today: knit & crochet night at fenway community center, boston university removes the myles standish name from dorm, pov: remembering charlie pohonich, a final look back at bu’s 151st commencement, how to make the most of memorial day weekend in boston, did you win the free furiosa: a mad max saga tickets for tonight, karen antman stepping down as bu’s medical school dean and medical campus provost, a bu class tackles the massachusetts housing crisis, zesty potato salad, my reflections on the last four years of college: why small life events matter, exploring bu’s vibrant asian student communities for aapi heritage month, photo essay: behind the scenes at a bu commencement, how three class of 2024 grads landed jobs before graduating, protests unfold in and around nickerson field during bu’s 151st commencement, quotes, comments, and cheers from bu’s 151st commencement, sights and sounds from boston university’s 151st commencement, “i’m excited to embark on this journey we call life”, bu celebrates 7,600 graduates at buoyant 151st commencement, “we are called, my friends, to be peacemakers,” rev. walter e. fluker tells boston university’s baccalaureate audience.
Fr. Romanus Cessario, S.T.D.
B.A., Philosphy, St. Stephen’s College; M.A., Philosophy, St. Stephen’s College; S.T.L., Sacred Theology, Dominican House of Studies; S.T.B., Sacred Theology, Dominican House of Studies; S.T.D., Sacred Theology, University de Fribourg; S.T.M., The Order of Preachers, Santa Sabina, Rome
- Christian Satisfaction in Aquinas . Washington, DC: University Press of America, 1982. [Reviews: New Blackfriars 64 (1983); Ciencia Tomista 111 (1984); Divus Thomas n.1–2 (1984); Zeitschrift für Katholische Theologie 104 (1982); Scripta Theologica 18 (1986); Rassegna di Letteratura Tomistica 18 (1982); The Thomist 51 (1987)].
- The Godly Image: Christ and Salvation in Catholic Thought from Anselm to Aquinas . Studies in Historical Theology VI. Petersham, MA: St. Bede's Publications, 1990. [Reviews: Nova et Vetera 65 (1990); Ephemerides Theologicae Lovanienses 67 (1991); Theological Studies 53 (1992); Nouvelle Revue Théologique 8 (1992); Tijdschrift voor Theologie 32 (1992); Freiburger Zeitschrift für Philosophie und Theologie 40 (1993); Revue des Sciences Philosophiques et Théologiques 77 (1993); The Thomist 58 (1994)].
- Meeting Christ in the Sacraments by Colman E. O’Neill, O.P., and revised by Romanus Cessario, O.P. New York: Alba House, 1991.
- The Moral Virtues and Theological Ethics. Notre Dame/London: University of Notre Dame Press, 1991. [Reviews: Studium 31 (1991); The Priest October 1991; America 18 April 1992; New Blackfriars 73 (1992); The Thomist 56 (1992); Revue Thomiste 92 (1992); Theological Studies 53 (1992); Homiletic & Pastoral Review February 1992; Salesianum 54 (1992); Horizons 19 (1993); Theology Digest 39 (1992); The Journal of Religion 73 (1993); Crisis February 1993; Modern Theology 9 (1993); Tijdschrift voor Theologie 33 (1993); New Oxford Review December 1993].
- Le Virtù . Volume 19 of Manuali di Teologia Cattolica (AMATECA), Sezione sesta: La persona umana. Milan: Editoriale Jaca Book, 1994. Spanish edition: Las virtudes. Valencia: Edicep, 1998. English edition: Virtues , or the Examined Life. New York: Continuum, 2002. [Reviews: Catholic Library World December 2002; The Thomist 67 (2003); Theology Digest 50 (2003); First Things November 2003; Theological Book Review 15 (2003); Josephinum Journal of Theology 11 (2004); Theological Studies 65 (2004); Nova et Vetera (Eng. ed.) 2 (2004)]. Croatian edition: Kreposti. Zagreb: Kršćanska sadašnjost, 2007.
- Perpetual Angelus. As the Saints Pray the Rosary. New York: Alba House, 1995. [Reviews: The National Catholic Register 71 (1995); The Priest 51 (1995); The Homiletic & Pastoral Review 1995; The Catholic Faith 2 (1996); Miles Immaculatae 32 (1996)].
- Christian Faith and the Theological Life. Washington, DC: The Catholic University of America Press, 1996. [Reviews: Crisis April 1997; National Catholic Register 73 (1997); The Dunwoodie Review 20 (1997); Homiletic & Pastoral Review July 1997; First Things August/September 1997; FCS Quarterly Summer 1997; Revue Thomiste 97 (1997); L’Osservatore Romano (No. 39 English Weekly Edition) 24 September 1997; New Oxford Review November 1997; The Thomist 62 (1998); Studia Moralia 35 (1997); Theological Studies 59 (1998); Nouvelle Revue Théologique 14 (1998); Pro Ecclesia 8 (1999); Scripta Theologica 57 (1999)].
- A Love That Never Ends. A Key to the Catechism of the Catholic Church . With J.A. DiNoia, B.G. O’Donnell, P.J. Cameron. Huntington, IN: Our Sunday Visitor Press, 1996.
- Jean Capreolus en son temps (1380-1444) . (Mémoire Dominicaine, numéro spécial, 1). Edited with Guy Bedouelle and Kevin White. Paris: Les Éditions du Cerf, 1997. [Reviews: Speculum 73 (1998); Medievalia et Humanistica New Series, No. 25 (1998); The Thomist 68 (2004)].
- Veritatis Splendor and the Renewal of Moral Theology . Studies by Ten Outstanding Scholars . Edited with J. A. DiNoia, O.P. Chicago: Midwest Theological Forum, 1999. [Review: The Thomist 65 (2001)].
- Le thomisme et les thomistes . Paris: Les Éditions du Cerf, 1999. [Reviews: New Blackfriars 80 (1999); Angelicum 77 (2000); International Philosophical Quarterly 41 (2001); Revue Thomiste 100 (2000); Bulletin, Association Internationale Cardinal Henri de Lubac 3 (2000); The Thomist 65 (2001); Revue Philosophique de Louvain 99 (2001); Studia Monastica 43 (2001); Doctor Angelicus 1 (2001); Nouvelle Revue Théologique 124 (2002)]. English edition: A Short History of Thomism (Washington, DC: The Catholic University of America Press, 2005) [Reviews: Theology Digest 52 (2005); Commonweal 13 January 2006; Christian Scholar’s Review 35 (2006); The Modern Schoolman 83 (2005); Journal of Ecclesiastical History 57 (2006); First Things June/July 2006; Christian Scholar’s Review Winter 2006; Nova et Vetera (Eng. ed.) 4 (2006); Logos 9.4 (2006); The Catholic Historical Review 93 (2007); The Thomist 72 (2008)].
- John Capreolus (1380–1444): Treatise on the Virtues . Edited and Introduction with Kevin White. Washington, DC: The Catholic University of America Press, 2001. [ Theology Digest 48 (2001); Choice March 2002; First Things April 2002; Religious Studies Review July 2002; International Philosophical Quarterly 42 (2002); Theological Studies 64 (2003); Bijdragen 64 (2003); Pro Ecclesia 12 (2003); Revue Thomiste 104 (2004); The Thomist 68 (2004); The Heythrop Journal 46 (2005)].
- Introduction to Moral Theology. Washington, DC: The Catholic University of America Press, 2001. [ First Things August/September 2002; Choice September 2002; Homiletic & Pastoral Review October 2002; The Thomist 66 (2002); Theology Digest Fall 2002; Catholic Library World 73 (2002); Crisis January 2003; Nova et Vetera (Eng. ed.) 1 (2003); Indian Journal of Family Studies 1 (2003); Pro Ecclesia 12 (2003); Book symposium in Nova et Vetera (Eng. ed.) 2 (2004); Theological Book Review 16 (2004); Australian Catholic Record 83 (2006); Studies in Christian Ethics 33 (2020)].
- Boston’s Cardinal. Bernard Law, the Man and His Witness . Edited with a Biographical Essay by Mary Ann Glendon. Lanham, MD: Lexington Books, 2002. [ The Patriot Ledger (Quincy, MA) 18 May 2002; First Things June/July 2002].
- The Moral Virtues and Theological Ethics. Second Edition. Notre Dame, IN: University of Notre Dame Press, 2008. [ The Heythrop Journal 51 (2010)]. Reprint of Chapter Four, “Prudence,” in Virtue , Readings in Moral Theology, no. 16, ed. Charles E. Curran and Lisa A. Fullham (New York: Paulist Press, 2011), 211–26.
- The Seven Last Words of Jesus . Paris/New York: Magnificat, 2009. Chinese edition, trans. Phyllis Chang. Taiwan: Catholic Window Press, 2010.
- The Seven Joys of Mary . Paris/New York: Magnificat, 2011. French edition, trans. Guy Bedouelle, O.P., 2013. Chinese edition, trans. Phyllis Chang. Taipei, Taiwan: Kuangchi Cultural Group, 2015.
- Philosophical Virtues and Psychological Strengths . Edited with Craig Steven Titus and Paul C. Vitz. Introduction. Manchester, NH: Sophia Institute Press, 2013. [ New Oxford Review November (2013); Nova et Vetera (Eng. ed.) 14 (2016)].
- Introduction to Moral Theology. Revised Edition . Washington, DC: The Catholic University of America Press, 2013.
- The Seven Sorrows of Mary . Paris/New York: Magnificat, 2014. French edition, trans. Catherine Mas–Mézéran, 2017. Spanish edition, trans. Pablo Cervera Barranco, 2017. Chinese edition, trans. Phyllis Chang. Taipei, Taiwan: Kuangchi Cultural Group, 2019.
- Theology and Sanctity , ed. Cajetan Cuddy, O.P., Ave Maria, FL: Sapientia Press, 2014. [ Studies in Christian Ethics 29 (2016); New Blackfriars 97 (2016)].
- Compassionate Blood: Catherine of Siena on the Passion . Paris/New York: Magnificat, 2016.
- Thomas and the Thomists: The Achievement of Thomas Aquinas and His Interpreters , with Cajetan Cuddy, O.P. Minneapolis: Fortress Press, 2017. [ First Things April 2018; Wisconsin Bookwatch September 2017; New Blackfriars 100 (2019); Sedes Sapientiae 146 (2018); Nova et Vetera (Eng. ed) 17 (2019); Espíritu 157 (2019); Revue Thomiste 119 (2019); Journal of the Society of Christian Ethics 39 (2019)]. Spanish edition: Tomás Y Los Tomistas: El Logro de Tomás De Aquino y sus intérpretes. Toledo: Ediciones Cor Iesu, 2021.
- The Grace to Be a Priest . Cluny Media, 2017. [ The Catholic World Report http://www.catholicworldreport.com/2018/04/18/dominican-theologian-the-goal-of-the-priesthood-is-to-get-people-to-heaven/ accessed 18 April 2018].
- The Godly Image. Christian Satisfaction in Aquinas . Washington, DC: The Catholic University of America, 2020.
- Sanctifying Truth: Thomas Aquinas on Christian Holiness . Paris/New York: Magnificat, 2021.
- The Seven Sacraments of the Catholic Church . Grand Rapids, MI: Baker Academic, 2023.
- “Theology at Fribourg,” The Thomist 51 (1987): 325–366.
- “The Meaning of Virtue in Catholic Moral Life: Its Significance for Human Life Issues,” The Thomist 53 (1989): 173–96.
- “Casuistry and Revisionism: Structural Similarities in Method and Content,” in “Humanae Vitae”: 20 Anni Dopo. Atti del II Congresso Internazionale di Theologia Morale , vol. III (Milano: Edizioni Ares, 1990): 385–409.
- “Christian Satisfaction and Sacramental Reconciliation,” Communio 16 (1989): 186–196. Reprinted in Rediscovering Aquinas and the Sacraments: Studies in Sacramental Theology , ed. M. Levering and M. Dauphinais (Chicago: Hillenbrand Books, 2009), pp. 65–75.
- “Aquinas on Nature and Grace” in Catholicism and Secularization in America , ed. David L. Schindler (Notre Dame, IN: Communio Books, 1990): 207–10.
- “La tradition thomiste et l’oeuvre de l’Esprit: les dons d’intelligence et de science,” Nova et Vetera 65 (1990): 259–267.
- “Christ and Reconciliation,” Faith & Reason 17 (1991): 15-50.
- “Lacordaire et les États-Unis,” in Lacordaire, son pays, ses amis et la liberté des ordres religieux en France , ed. Guy Bedouelle (Paris: Les Éditions du Cerf, 1991): 333–347.
- “A Thomist Interpretation of Faith: The Gifts of Understanding and Knowledge,” in Novitas et Veritas Vitae. Aux Sources du Renouveau de la Morale Chrétienne . Mélanges offerts au Professeur Servais Pinckaers à l’occasion de son 65e anniversaire, ed. Carlos–Josaphat Pinto de Oliveira (Fribourg: Editions Universitaires, 1991): 67–102.
- “Incarnate Wisdom and the Immediacy of Christ’s Salvific Knowledge,” in Problemi teologici alla luce dell'Aquinate ( Atti del IX Congresso Tomistico Internazionale ). Studi Tomistici 44 (Città del Vaticano: Libreria Editrice Vaticana, 1991): 334–340.
- “St. Thomas Aquinas on Satisfaction, Indulgences, and Crusades,” Medieval Philosophy & Theology 2 (1992): 74–96.
- “Virtue Theory and the Present Evolution of Thomism,” in The Future of Thomism , ed. Deal W. Hudson and Dennis Wm. Moran (Notre Dame, IN: American Maritain Association, 1992): 291–299.
- “An Observation on Robert Lauder’s Review of G.A. McCool, S.J.,” The Thomist 56 (1992): 701–710.
- “Lacordaire and the United States,” The Catholic Historical Review 78 (1992): 197–206.
- “Boethius, Christ, and the New Order,” Carmina Philosophiae 1 (1992): 53-64. Reprinted in New Directions in Boethian Studies , ed. Noel Harold Kaylor, Jr. and Philip Edward Philips, Studies in Medieval Culture XLV (Kalamazoo: Medieval Institute Publications, 2007), 157–168.
- “Is Aquinas’s Summa Only About Grace,” in Ordo Sapientiae et Amoris . Hommage au Professeur Jean-Pierre Torrell OP à l’occasion de son 65e anniversaire, ed. Carlos–Josaphat Pinto de Oliveira (Fribourg: Editions Universitaires, 1993): 197–209. Reprinted in Reason and the Rule of Faith , ed. Christopher J. Thompson and Steven A. Long (Lanham, MD: University Press of America, 2011), 43–53.
- “Moral sexual christiana dentro de una estructura más amplia,” AnáMnesis 3 (1993): 5–25.
- “Le Père Garrigou-Lagrange (1877-1964),” Sources 20 (1994): 206–208.
- “Early Dominican Confessional Practice,” New Blackfriars 75 (1994): 425–428. [French translation: “Les Premiers Dominicains et la confession,” Mémoire Dominicaine 5 (1994): 283–286.]
- “The Church, Higher Education, and Global Concerns,” Josephinum Journal of Theology 2 (1995): 25–33.
- “Moral Absolutes in the Civilization of Love” in The Splendor of Truth and Health Care, Proceedings of the Fourteenth Workshop for Bishops , Dallas, Texas, ed. Russell E. Smith, (Braintree, MA: The Pope John XXIII Medical-Moral Research and Education Center, 1995): 43–57. Reprinted in Crisis 13 (May, 1995): 18–23.
- “Boèce, le Christ et la civilisation européenne,” Pierre d’angle 1 (1995): 51–60.
- “Toward Understanding Aquinas’ Theological Method: The Early Twelfth–Century Experience” in Studies in Thomistic Theology , ed. Paul Lockey (Notre Dame, IN: Center for Thomistic Studies, 1995): 17–89.
- “ Epieikeia and the Accomplishment of the Just” in Aquinas and Empowerment: Classical Ethics for Ordinary Lives , ed. G. Simon Harak (Washington, DC: Georgetown University Press, 1996): 170–205.
- “The Spirituality of St. Thomas Aquinas,” Crisis 14 (July/August 1996): 14–16.
- “Evangelization and Our Present Circumstances: In Praise of Virtue” in The Church’s Mission of Evangelization , ed. William E. May, (Steubenville, OH: Franciscan University Press, 1996): 129–152.
- “Éloge des vertus chrétiennes pour un temps de crise,” Pierre d’angle 2 (1996): 53–71.
- “Saint Thomas, Durand de Saint-Pourçain et Capreolus: Le Débat sur la foi” in Jean Capreolus en son temps (1380-1444) , ed. Guy Bedouelle, Romanus Cessario, and Kevin White ( Paris: Les Éditions du Cerf, 1997): 159–164.
- “Christian Virtue and Public Morality,” Rivista Teologica di Lugano 2 (1997): 27–42.
- “À nos lecteurs: sur le paradoxe de l’existence chrétienne entre foi et modernité. La foi comme Dieu l'a révélée,” Pierre d’angle 3 (1997): 18–26.
- “On Bad Actions, Good Intentions, and Loving God: Three Much-Misunderstood Issues about the Happy Life that St. Thomas Clarifies for Us,” Logos 1.2 (1997): 100–124.
- Encyclopedia of Catholic Doctrine , ed. Russell Shaw (Huntington, IN: Our Sunday Visitor Publishing Division, 1997), s. vv. “Assent and Dissent,” “Atheism,” “Bishop,” “Celibacy, Priestly,” “Deacon,” “Holy Orders,” “Ministry,” “Modernism,” “Priest,” and “Priesthood of Christ.”
- “Theological Literacy and Theological Science” in Boston Theological Institute Newsletter , vol. 27, no. 24 (18 Mar 1998): 1–2.
- “More Good News,” Catholic Dossier 4.2 (March-April 1998): 54–55.
- “The Holy Spirit, Spirit of Truth, Person of Love,” Catholic International 9 (May 1998): 220–224.
- Dizionario di Mistica , ed. L. Borriello, et al. (Città del Vaticano: Libreria Editrice Vaticana, 1998), s. vv. “Tommaso D’Aquino (santo)” and “Garrigou-Lagrange, Reginald.”
- “The D.E.S. Motto and the Benedictine Tradition: A Thomistic Connection,” Delta Epsilon Sigma Journal 43 (1998): 88–90.
- “St. Therese, Seminarians, and the Future,” Catholic Dossier 4.6 (November-December 1998): 14–16.
- “John Poinsot: On The Gift of Counsel” in The Common Things: Essays on Thomism and Education, ed. Daniel McInerny (Mishawaka: American Maritain Association, 1999): 163–178.
- “The Reason for Reason: Fides et Ratio ,” Crisis 17 (January 1999): 16–19.
- “Thomas Aquinas: A Doctor for the Ages,” First Things (March 1999): 27–32. Reprinted in The Second One Thousand Years. Ten People Who Defined the Millennium , ed. Richard John Neuhaus (Grand Rapids, MI: William B. Eerdmans Publishing Co., 2001): 28–39.
- “Reply to Professor Gilbert Morris,” First Things (June/July 1999): 7.
- “ Fides et Ratio . Un appel à la vérité et à la réconciliation,” Pierre d’angle 5 (1999): 32–38.
- “What the Angels See at Twilight,” Communio 26 (Fall 1999): 583–594. [French translation: “Ce que les anges voient au crépuscule,” Communio 25 (nov.–déc. 2000): 41–51.]
- “Custodia Condicional de la Vida Humana. Un principio moral de Juan Pablo II” in El Dios y Padre de Nuestro Señor Jesucristo , ed. José Luis Illanes et al., (Pamplona: Servicio de Publicaciones de la Universidad de Navarra, 2000): 427–432.
- “Infallible Teaching and the Gift of Divine Truth,” Catholic Dossier 6.3 (May- June 2000): 5–8.
- “Un “salut civil”? Vie et famille dans la doctrine catholique,” Pierre d’angle 6 (2000): 185–97.
- “Sacramental Confession and Addictions” in Addiction and Compulsive Behaviors, Proceedings of the Seventeenth Workshop for Bishops , Dallas, Texas, ed. Edward J. Furton (Boston, MA: The National Catholic Bioethics Center, 2000): 125–139.
- New Catholic Encyclopedia, Jubilee Volume: The Wojtya Years , s.v. “Schönborn, Christoph.”
- “Towards an Adequate Method for Catholic Bioethics,” The National Catholic Bioethics Quarterly 1 (2001): 51–62.
- The Dictionary of Historical Theology , ed. Trevor A. Hart (Grand Rapids, MI: William B. Eerdmans Publishing Company, 2001), s.v. “Gilson, Étienne (1884–1978).”
- “En partant d’une chanson de Gershwin...,” Pierre d’angle 7 (2001): 41–47.
- “Duplex ordo cognitionis,” Doctor Communis II, n.s., Atti della II Sessione Plenaria, 22-24 Giugno 2001 (Vatican City: Pontificia Academia Sancti Thomae Aquinatis, 2002): 102–109; 141–142.
- “The Theological Virtue of Hope (IIa IIae qq. 17-22)” in The Ethics of Aquinas , ed. Stephen J. Pope (Washington, DC: Georgetown University Press, 2002), pp. 232–243.
- “The Sacramental Mediation of Divine Friendship and Communion,” Faith & Reason 27 (2002): 7-41.
- New Catholic Encyclopedia , 2 nd ed., vol. 4, s.v. “Consequentialism.”
- New Catholic Encyclopedia , 2 nd ed., vol. 3, s.v. “Casuistry,” with E. Hamel.
- “Mary in the Dominican Tradition,” Nova et Vetera, English Edition, 1 (2003): 27–42.
- “Entendre les Mystères. Musique liturgique et foi théologale,” with Jonathan Gaspar, Pierre d’angle 9 (2003): 135–50.
- “Cooperation, Veritatis splendor , and the Luminous Mysteries” in Walk as Children of Light: The Challenge of Cooperation in a Pluralistic Society: Proceedings of the Nineteenth Workshop for Bishops , Dallas, Texas, ed. Edward J. Furton (Boston, MA: The National Catholic Bioethics Center, 2003): 47–67.
- “Life and Family as Themes in Catholic Social Thought” in Indubitanter ad Veritatem. Studies Offered to Leo J. Elders, S.V.D. in Honor of the Golden Jubilee of his Ordination to the Priesthood , ed. Jörgen Vijgen (Budel: Damon, 2003), pp. 69–79.
- “Aquinas on Christian Salvation” in Aquinas on Doctrine. A Critical Introduction , ed. Thomas Weinandy, Daniel Keating, John Yocum (London: T&T Clark International, 2004), pp. 117–37.
- “Response” in Book Symposium, Nova et Vetera , English Edition, 2 (2004): 208–10.
- “Mel Gibson and Thomas Aquinas: How the Passion Works,” ZENIT, 9 April 2004. Available from [email protected] , INTERNET. [German translation: “Wie die Passion Christi die Erlösung bewirkt–Mel Gibson und Thomas von Aquin,” Una Voce–Korrespondenz 34 (2004): 131–38.]
- “Conditional Stewardship of Life: A Moral Principle of John Paul II” in Moral Issues in Catholic Health Care , ed. Kevin T. McMahon (Overbook, PA: Saint Charles Borromeo Seminary, 2004), pp. 120–38.
- “Sex, Lies, and Freud,” Logos 7.3 (2004): 47–59.
- “Mel Gibson et saint Thomas d’Aquin: Un regard théologique sur La Passion du Christ ,” Pierre d’angle 10 (2004): 185–94.
- “Why Aquinas Locates Natural Law within the Sacra Doctrina ,” in St. Thomas Aquinas and the Natural Law Tradition. Contemporary Perspectives , ed. John Goyette, Mark S. Latkovic, and Richard S. Myers (Washington, DC: The Catholic University of America Press, 2004), pp. 79–93.
- “The Light of Tabor: Christian Personalism and Adoptive Friendship,” Nova et Vetera , English Edition, 2 (2004): 237–47. Reprinted in L’Antropologia della Teologia Morale Secondo L’Enciclica “Veritatis Splendor.” Atti del Simposio promosso dalla Congregazione per la Dottrina della Fede, Roma, settembre 2003 (Città del Vaticano: Libreria Editrice Vaticana, 2006), pp. 92–101.
- “Mel Gibson’s Movie & Thomas Aquinas’s Modes: How the Passion of the Christ Works,” Saint Austin Review 4 (2004): 27–32. [Dutch translation: “Mel Gibson en Thomas van Aquino over de Passie van Christus” in Doctor Humanitatis , vol. 1, De actualiteit van Sint-Thomas van Aquino , ed. Jörgen Vijgen (Hoofddorp: Uitgeverij Boekenplan, 2005).] “Mel Gibson’s ‘Passion’ & Aquinas’s Five Modes: How the Passion of Christ Works,” The Premier International Fan Website, Mel Gibson’s “The Passion of the Christ.” Available here , INTERNET.]
- “Walk According to the Light. An Illustration from North America” in Camminare nella Luce. Prospettive della teologia morale a partire da ‘Veritatis splendor ,’” ed. Livio Melina and José Noriega (Rome: Lateran University Press, 2004), pp. 401–07.
- “Capreolus on Faith and the ‘Theologal’ Life” in: Essays in Medieval Philosophy and Theology in Memory of Walter H. Principe, CSB: Fortresses and Launching Pads, ed. James R. Ginther and Carl N. Still (Aldershot, Hants; Burlington, VT: Ashgate Publishing, 2005), pp. 135–141.
- “ Duplex Ordo Cognitionis ” in Reason and the Reasons of Faith , ed. Paul J. Griffiths and Reinhard Hütter (New York: T&T Clark, 2005), pp. 327–338.
- “‘Worthy of the Temple’: Liturgical Music and Theologal Faith,” with Jonathan Gaspar, Nova et Vetera , English Edition 3 (2005): 673–688.
- “Catholic Hospitals in the New Evangelization,” The National Catholic Bioethics Quarterly 5 (2005): 675–686.
- “Person & Being: Theological and Psychological Considerations,” Doctor Communis , Atti della IV Sessione Plenaria, 25–27 Giugno 2004 (Vatican City: Pontificia Academia Sancti Thomae Aquinatis, 2006): 75–84.
- “‘Circa res ...aliquid fit’ ( Summa theologiae II-II, q. 85, a. 3, ad 3): Aquinas on New Law Sacrifice,” Nova et Vetera , English Edition 4 (2006): 295–312.
- “The Sacred, Religion, and Morality,” Doctor Communis VII, n.s., Atti della V Sessione Plenaria, 24-26 Giugno 2005 (Vatican City: Pontificia Academia Sancti Thomae Aquinatis, 2006): 173–186.
- “Johannes Capreolus” in Thomistenlexikon , ed. David Berger & Jörgen Vijgen (Bonn: Nova & Vetera Verlag, 2006), pp. 302–311.
- “The Sacred, Religion, and Morality,” Logos 9.4 (2006): 16–32.
- “Catholic Considerations on Palliative Care,” The National Catholic Bioethics Quarterly 6 (2006): 639–650.
- “Moral Theology on Earth: Learning from Two Thomases,” Studies in Christian Ethics 19 (2006): 305–322.
- “Hommage au Père Servais-Théodore Pinckaers, OP. The Significance of His Work,” Nova et Vetera , English Edition, 5 (2007): 1–16.
- “The Theological Heritage of Pope Benedict XVI,” Nova et Vetera , English Edition, 5 (2007): 267–270.
- “Moral Realism and Christian Values” in The Person and the Polis. Faith and Values within the Secular State , ed. Craig Steven Titus (Arlington, VA: The Institute for the Psychological Sciences Press, 2007), pp. 153–73.
- “ Tanquam spiritualis pulchritudinis amatores . The Consecrated Vocation of Matthew Lamb” in Wisdom and Holiness, Science and Scholarship . Essays in Honor of Matthew L. Lamb , ed. Michael Dauphinais & Matthew Levering (Naples, FL: Sapientia Press, 2007), pp. 17–45.
- “Saint Thomas and the Enculturation of the Natural Law: Doing Moral Theology on Earth,” Doctor Communis , Atti della VI Sessione Plenaria, 23–25 Giugno 2006 (Vatican City: Pontificia Academia Sancti Thomae Aquinatis, 2007): 41–53.
- “Reply to Edward T. Oakes, S.J.,” First Things (October 2007): 8–9.
- “Thomas d’Aquin, apôtre du sens commun,” Pierre d’angle 13 (2007): 49–56.
- “Sonship, Sacrifice, and Satisfaction: The Divine Friendship in Aquinas and the Renewal of Christian Anthropology,” Letter & Spirit 3 (2007): 71–93.
- “In Honor of Avery Cardinal Dulles, S.J.: Priest, Scholar, and Living Memory,” Nova et Vetera , English Edition, 6 (2008): 245–246.
- “The Sacraments of the Church” in Vatican II. Renewal Within Tradition , ed. Matthew L. Lamb & Matthew Levering (Oxford: Oxford University Press, 2008), pp. 129–146.
- “On Moral Theology” in Love Alone Is Credible: Hans Urs von Balthasar as Interpreter of the Catholic Tradition , ed. David L. Schindler, vol. 1 (Grand Rapids, MI: William B. Eerdmans Publishing Company, 2008), pp. 297–302.
- “Scholarship and Sanctity,” Second Spring 10 (2008): 13–20.
- “Love, Friendship, and Beauty: On the Twenty-fifth Anniversary of a Magisterial Document about Religious Life and the Apostolate, Logos 11.4 (2008): 147–163.
- “The Quarry Workers,” Nova et Vetera , English Edition, 6 (2008): 669–674.
- “ Humanae Vitae , the Maritains, and Maurice Sachs,” Nova et Vetera , English Edition, 6 (2008): 711–730.
- “Freedom and Satisfaction” in The Human Person and a Culture of Freedom , ed. Peter A. Pagan & Terese Auer, O.P., (Washington, DC: American Maritain Association, 2009), pp. 207–225.
- “O que os anjos vêem: natureza e graça,” Lumen Veritatis 2, N○ 5 (2008): 121–25.
- “On the Place of Servais Pinckaers († 7 April 2008) in the Renewal of Catholic Theology,” The Thomist 73 (2009): 1–27.
- New Catholic Encyclopedia Supplement 2009 . 2 vols. (Detroit: Gale, 2009), 1: 191–193, s. v. “Consequentialism.”
- “Hommage au Père Servais Pinckaers, O.P.: L’importance de son oeuvre” in Renouveler toutes choses en Christ. Vers un renouveau thomiste de la théologie morale , ed. Michael S. Sherwin, O.P., and Craig Steven Titus, Etudes d’éthique chrétienne, NS 5 (Fribourg: Academic Press, 2009), pp. 6–19.
- “Saint Thomas Aquinas: ‘The Apostle of Common Sense,’” Nova et Vetera , English Edition, 7 (2009): 563–68.
- “Realismo Morale E Legge Naturale,” in Come insegnare Teologia Morale? Prospettive di rinnovamento nelle recenti proposte di esposizione sistematica , ed. Livio Melina & Stephan Kampowski, Studie sulla persona e la famiglia, Atti 3 (Siena: Edizioni Cantagalli, 2009), pp. 91–105.
- “Maurice Sachs et les Maritain,” Pierre d’angle 15 (2009): 127–144.
- “Aquinas on the Priest: Sacramental Realism and the Indispensable and Irreplaceable Vocation of the Priest,” Nova et Vetera , English Edition, 8 (2010): 1–15.
- “Scholarship and Sanctity: A Lesson Aquinas Teaches the Priest and Seminarian,” Nova et Vetera , English Edition, 8 (2010): 233–49.
- New Catholic Encyclopedia Supplement 2010 . 2 vols. (Detroit: Gale, 2010), 1: 205–208, s. v. “Cardinal Virtues.”
- “Remarks on Sin and Indulgence,” Nova et Vetera , English Edition, 9 (2011): 99–108.
- “Blessed John Henry Newman (1801–1890), Sermon Preached at the Toronto Oratory, October 3, 2010,” Nova et Vetera , English Edition, 9 (2011): 261–66.
- “Seek Out the Harmonies between Faith and Reason,” The Catholic Social Science Review 16 (2011): 331–37.
- “Organ Donation and the Beatific Vision: Thomist Moral Theology Confronts the Tide of Relativism” in The Ethics of Organ Transplantation , ed. Steven J. Jensen (Washington, DC: The Catholic University of America Press, 2011), pp. 195–216.
- “The Trinitarian Imprint on the Moral Life” in The Oxford Handbook of the Trinity , ed. Gilles Emery, O. P., and Matthew Levering (Oxford: Oxford University Press, 2011), pp. 487–92.
- “Witness to Faith: George Weigel, Blessed John Paul II, and the Theological Life,” with Cajetan Cuddy, O.P., Nova et Vetera , English Edition, 10 (2012): 1–13.
- “The Grace St. Dominic Brings to the World: A Fresh Look at Dominican Spirituality,” Logos 15.2 (2012): 84–100.
- “Mary in the Thomist Commentatorial Tradition” in Sapienza e libertá. Studi in Onore del Prof. Lluís Clavell , ed. Miguel Pérez de Laborda (Rome: Edusc Srl, 2012), pp. 81–88.
- “Scripture as the Soul of Moral Theology: Reflections on Vatican II and Ressourcement Thomism,” The Thomist 76 (2012): 165–88.
- After Virtue , Thirty Years After: Laudatio for Alasdair MacIntyre,” Nova et Vetera , English Edition, 10 (2012): 895–900.
- “Sacramental Causality: Da capo !,” Nova et Vetera , English Edition, 11 (2013): 307–316.
- New Catholic Encyclopedia Supplement 2012–13: Ethics and Philosophy . Ed. Robert L. Fastiggi. 4 vols. (Detroit: Gale, 2013), 3: 1276–77, s. v. “Prudence [Addendum].”
- New Catholic Encyclopedia Supplement 2012–13: Ethics and Philosophy . Ed. Robert L. Fastiggi. 4 vols. (Detroit: Gale, 2013), 3: 1025–26, s. v. “Moral Skepticism.”
- “Morals and Sacraments: Themes in the Catechism that Aquinas Helps Clarify,” Doctor Communis , The Proceedings of the XII Plenary Session, 29 June–1 July 2012 (Vatican City: Pontificia Academia Sancti Thomae Aquinatis, 2013), pp. 143–49.
- “ Miscere colloquia : On the Authentic Renewal of Catholic Spirituality,” Nova et Vetera , English Edition, 11 (2013): 627–47.
- “Molina and Aquinas” in A Companion to Luis de Molina , ed. A. Aichele & M. Kaufmann (Leiden: Brill, 2013), pp. 291–323.
- “Premotion, Holiness, and Pope Benedict XIII (1724-30): Some Historical Retrospects on Veritatis Splendor ,” Nova et Vetera , English Edition, 11 (2013): 1115–35.
- “Culture and Contemplation: Catholicism in the Twenty-First Century,” The Thomist 77 (2013): 453–71.
- “The Importance of Steven A. Long’s Analogia Entis within Contemporary Catholic Thought,” Nova et Vetera , English Edition, 12 (2014): 971–974.
- “God the Son: Trinitarian Christology. Markers in the Thomist Tradition,” Nova et Vetera , English Edition, 12 (2014): 1233–1255.
- “Thomas Aquinas and Vocational Discernment,” Religious Life Review 54 (2015): 69–86.
- “Le goût du monde,” Nova et Vetera , English Edition, 14 (2016): 1–13.
- “Sacrifice, Social and Sacramental: The Witness of Louis Billot, S.J.,” Nova et Vetera , English Edition, 14 (2016): 127–149.
- “ Ego Sapientia . The Mariology of Laval Thomism” in Theology Needs Philosophy , ed. Matthew L. Lamb (Washington, DC: Catholic University of America Press, 2016), 227–239.
- “Ricezione e Prospettive negli Stati Uniti e in Australia” in Deus Caritas Est. Porta di Misericordia. Atti del Simposio internazionale nel decimo anniversario dell’Enciclica , ed. M. Graulich & R. Weimann (Rome: Libreria Editrice Vaticana, 2016): 235–249.
- “Religion and Christian Life: Religion and the Gifts of the Holy Spirit,” Doctor Communis , The Proceedings of the XV Plenary Session, 19–21 June 2015 (Vatican City: Pontificia Academia Sancti Thomae Aquinatis, 2016), pp. 119–32.
- “Charity, Mortal Sin, and Parish Life,” Logos 19.4 (2016): 86–100.
- “Ave Maria! The Grace of Predestination” in Thomism & Predestination. Principles and Disputations , ed. S. Long et al. (Ave Maria, FL: Sapientia Press, 2016): 226–238.
- “Mercy in Aquinas: Help from the Commentatorial Tradition,” with Cajetan Cuddy, O.P., The Thomist 80 (2016): 329–339.
- Nuovo Dizionario di Mistica , ed. L. Borriello, et al. (Città del Vaticano: Libreria Editrice Vaticana, 2016), s.vv. “Tommaso D’Aquino (santo)” and “Garrigou-Lagrange, Reginald.”
- “Holy Teaching, Holy Preaching: Thomas, Thomists, and the Province of Saint Joseph,” The Thomist 80 (2016): 601–622).
- “Le goût du monde” in Colloque Guy Bedouelle. Une libre intelligence chrétienne , ed. Michel Jacquet (Angers: Frémur editions, 2017): 189–220.
- “Religion and the Gifts of the Holy Spirit,” Nova et Vetera , English Edition, Vol. 15 (2017): 983–998.
- “ In memoriam. Pierre d’Angle ou les racines du présent. Hommage au frére Guy Bedouelle,” with Daniel Bourgeois, Pierre d’angle 18 (2017): 5–20.
- “Creation as a Norm for Moral Action,” Logos 21.2 (2018): 109–122. Also in Dio creatore e la creazione come casa commune , ed. S.–T. Bonino & G. Mazzotta (Vatican City: Urbaniana University Press, 2018), pp. 237–50.
- “Sacrifice and Priesthood. Maritain’s Still Untrammeled Approaches ” in The Things That Matter. Essays Inspired by the Later Work of Jacques Maritain , ed. Heidi M. Giebel (Washington, D.C.: American Maritain Association, 2018), pp. 197–208.
- “Aquinas on Virginity and Celibacy” in San Tomasso. Il Marimonio e la Familiga , ed. S.–T. Bonino & G. Mazzotta (Vatican City: Urbaniana University Press, 2019), pp. 195–207.
- “Anointing of the Sick: The Sanctification of Human Suffering,” Nova et Vetera , English Edition, Vol. 17 (2019): 1–11.
- “Human Emotion within the Theologal Life,” in Le Emozioni secondo san Tommaso , ed. S.–T. Bonino & G. Mazzotta (Vatican City: Urbaniana University Press, 2019), pp. 189–199.
- “Katholieke priesters: onontbeerlijk en onvervanbaar,” Communio , Dutch edition, Vol. 44, nr. 2 (2019): 142–154.
- “Satisfaction, a Reprise for Catholic Theology,” in San Tommaso e la salvezza , ed. S.–T. Bonino & G. Mazzotta (Vatican City: Urbaniana University Press, 2020), pp. 243–253.
- “Benedict Ashley, O.P., Theologies of the Body 1995,” in Grande opere del Tomismo nel Novecento , ed. S.–T. Bonino (Vatican City: Urbaniana University Press, 2020), pp. 203–209.
- “Sanctified Thought and Affection in Aquinas’s Teaching on Nature and Grace,” The Thomist 84 (2020): 467–80.
- “Sixteenth–Century Reception of Aquinas by the Council of Trent and Its Main Authors, in The Oxford Handbook of the Reception of Aquinas , ed. Matthew Levering & Marcus Plested (Oxford: Oxford University Press, 2021), pp. 159–172.
- “An Exercise in Christian Philosophy: The Intellectual Daring of Giuseppe Abbà,” Salesianum 83 (2021): 706–717.
- “Purgatory: A Place of Christian Satisfaction,” in Hope & Death. Christian Responses , ed. M.A. Dauphinais & R.W. Nutt (Steubenville, OH: Emmaus Academic, 2022), pp. 165–178.
- “The Priest and the Friend: Notes on Priestly Formation and on Christian Life in General,” Analecta of the UCU: Theology 9 (2022): 115–128.
- “Mary in Catholic Higher Education,” in Thomas Aquinas as Spiritual Teacher , ed. M.A. Dauphinais, Andrew Hofer, OP, & R.W. Nutt (Ave Maria, FL: Sapientia Press, 2023), pp. 245–257.
Research and Publications

Sanctifying Truth: Thomas Aquinas on Christian Holiness
These insightful reflections from Father Cessario explore the riches of thought that have become known as Thomist theology in a way that makes them accessible to anyone interested in growing closer to the Divine Wisdom that permeates all creation.

The Seven Sacraments of the Catholic Church
This book examines why participation in the sacramental life of the Church is required for the believing Christian and helps readers understand the role the sacraments play in the sanctification of the world.

The Godly Image: Christian Satisfaction in Aquinas
Ecumenical work requires a proper understanding of the place that satisfaction holds in Christian theology. Various factors operative since the sixteenth century have worked to displace satisfaction almost entirely from reformed practice and theology.

THE GRACE TO BE A PRIEST
In this text, Father Cessario explains how the vocation to the priesthood comes to a man as both gift and mystery. God chooses priests to serve as both instruments of his will and spiritual fathers for his people.

GO AHEAD AND APPLY!
Sunny skies, warm temperatures, a beautiful campus. What more could you want? How about a community-like atmosphere, quality instructors who care about your success, a wealth of spiritual activities, expert career guidance… and that’s only the beginning. Imagine your future at AMU. It all starts by filling out our free application today.

5050 Ave Maria Blvd., Ave Maria, FL 34142
- Deposit Enrollment Fee
- Campus Store
- My.AveMaria
- Self-Service
- IT Helpdesk
- Registration and Records
- Campus Safety
- Accreditation
- FCC Public Notice of Filing
- RFP - Lawn Care Services

IMAGES
COMMENTS
500+ Words Essay on Organ Donation. Essay on Organ Donation - Organ donation is a process in which a person willingly donates an organ of his body to another person. Furthermore, it is the process of allowing the removal of one's organ for its transplanting in another person. Moreover, organ donation can legally take place by the consent of ...
Introduction. The act of organ donation stands as a powerful testament to human solidarity and compassion, offering the gift of life to those in dire need. ... However, despite its critical importance, there persists a significant gap in awareness and understanding surrounding organ donation. This essay embarks on a journey to shed light on the ...
To those that have in one way or the other received or given their body organs, they portray a good heroic example of human acts since, for example, one organ from one person can save up to 50 people (MedlinePlus, 2009). This can lead to saving many lives that would otherwise have been lost. In Michigan, a positive attitude towards organ ...
500+ Words Essay on Organ Donation. Organ donation is a noble cause, and by doing this, you can give life to many people. In the current scenario, organs like the small intestine, kidney, eyes, liver, heart, and skin tissues are in great demand. Every year, thousands of people die due to accidents, and their organs give life to different people ...
Essay on Organ Donation in 200 words. Organ donation is done by both living and deceased donors. The living donors can donate one of the two kidneys, a lung or a part of a lung, one of the two lobes of their liver, a part of the intestines or a part of the pancreas. While a deceased donor can donate liver, kidneys, lungs, intestines, pancreas ...
Organ and tissue donation is more important than many of us realize—for society and for the individuals it directly affects. Today, there are nearly 118,000 individuals waiting for an organ transplant to live healthier, more productive lives (Unpublished data, Organ Procurement and Transplantation Network [OPTN], April 2013).
Although kidney donation is not practiced in the United States, it has been found to be effective in other nations. For example, Iran pays its residents up to $1,200 for kidney donations, but the recipients must be Iranian nationals and get long-term medical attention (Monday & Ogugua, 2020). There should be discussions regarding possible ...
Organ donation essay topics are on verge of medicine and ethics and may take the form of a range of discursive questions: 1. What is the best way to decrease the shortage of organs for transplantation? 2. Should the legislature concerning organ transplantation be changed? 3.
Exploring the topic of organ donation through essays can lead to a deeper understanding of the ethical, medical, and societal issues surrounding this life-saving practice. ... Introduction Organ donation is a medical marvel that saves countless lives each year, offering a ray of hope to those in dire need of organ transplants. However, beneath ...
Organ transplantation is unique among surgical procedures, in that the procedure cannot take place without the donation of an organ or a partial organ from another person. Since 1988, more than 390,000 organs have been transplanted, with approximately 80 percent of the transplanted organs coming from deceased donors.
Organ donation is defined as giving an organ or part of an organ to be transplanted into another person. Organ transplantation is the only option to save lives in patients affected by terminal organ failures and improve their quality of life. However, there is a disparity exists between the supply and demand of donated organs, leads to a loss of many lives. The number of organ transplantation ...
organ donation, the act of giving one or more organs (or parts thereof), without compensation, for transplantation into someone else. Organ donation is a very personal yet complex decision, intertwined with medical, legal, religious, cultural, and ethical issues. Today organ donation, strictly defined, encompasses the donation and transplantation of the heart, intestines, kidneys, liver, lungs ...
Introduction. Organ donation is when a person allows an organ of theirs to be removed, legally, either by consent while the donor is alive or after death with the assent of the next of kin. Common transplantations include kidneys, heart, liver, pancreas, intestines, lungs, bones, bone marrow, skin, and corneas.
Organ and Blood Donation. However, ethical and legal issues, and unwillingness of many potential donors to provide consents have slowed down the rate of organ and blood donation in the county. We will write. a custom essay specifically for you by our professional experts. 809 writers online.
Argument Research Essay. The medical field utilizes a variety of techniques to save lives everyday. One way is to perform an organ transplant by replacing a patient's failing organ with a working one. The problem with this is that working organs are very hard to come by, and when they do, it is not guaranteed that the organ can be transplanted.
Speech on Organ Donation. Organ donation is a legal process through which the healthy organs and the tissues of one person are transplanted to another person. The person who donates his or her organs is known as a donor and the person who receives the organs is known as the organ receiver. Organ donation takes place by the consent of the donor ...
Organ donation is a noble act of transplanting healthy organs from a donor to a patient receiver. Human body organs and tissues that function properly are collected and transplanted into patients' bodies to save their lives. In most cases, organ donations are performed after the donor's death. But some organs can be donated even when the ...
Informative Speech for Organ Donation. Organ donation is a topic that is often overlooked in our society, yet it holds immense importance for those in need of life-saving transplants. In this essay, we will explore the various aspects of organ donation, including its significance, the process of donation, misconceptions, and the impact of organ ...
Essay on Organ Donation (1000 Words) Organ donation is a significant donation. It is also said a "reward for life" in other words. By doing this, we can give life to many people. Nowadays, many prostitutes help in donating organs, encourage it. Nowadays, organs like kidneys, eyes, liver, heart, small intestine, skin tissue are in high demand.
Organ Donation Essay Examples 🗨️ More than 20000 essays Find the importance of organ donation essay to get real academic results at college! ... Introduction Organ donation can be described as the act of giving away an organ to save or improve the life of someone who needs a transplant. Organs like the kidney and part of the liver can be ...
Organ donation is a kind act where a person allows their organs to be moved into another person's body. When someone's organ, like their heart or kidney, stops working well, they might need a new one. Organ donation is a way to give them a healthy organ. This can save their lives or help them feel better.
And they will resist consenting to organ donation. Organ retrieval can take place at odd hours because the time between retrieval and transplantation must be minimised. A donor heart or lungs can last only four to six hours outside the body. A kidney, liver or pancreas can last a bit longer.
Paper Type: 1400 Word Essay Examples. Pros and Cons of Paying for Organ Donation The purpose of this essay is to further reinstate the claim that financial incentives should not be permitted in order to encourage organ donation. Research mainly consisted of searching through UOW databases, including summon.
Ali Rogin has the latest on what can be done to revamp the nations organ transplant process. Kidneys topped the list of the most needed organs in the US. Nearly 115,000 people are currently ...
Richard "Rick" Slayman, who made history at age 62 as the first person to receive a kidney from a genetically modified pig, has died about two months after the procedure. Massachusetts General ...
Euthanasia through living organ donation: Ethical, legal, and medical challenges. J Heart Lung Transplant 2019;38(2):111-113. Domínguez-Gil B, Ascher N, Capron AM, et al. Expanding controlled donation after the circulatory determination of death: statement from an international collaborative. Intensive Care Med 2021;47(3):265-281.
Further refinements of those modifications are always being revised. More than 100,000 patients are currently on the kidney transplant list [in the United States], and close to 5,000 patients die yearly while waiting for kidney donors. If the modified pig kidney proves its efficacy, it will eliminate the organ shortage and the waiting time.
2 Introduction Clinical organ transplantation has been known as one of the most fascinating medical developments of the century as it offers a way of giving the gift of life to patients ... In this essay, ... & Oniscu, G. C. (2021). Organ donation and transplantation: a multi-stakeholder call to action. Nature Reviews Nephrology, 17(8), 554 ...
Edited and Introduction with Kevin White. Washington, DC: The Catholic University of America Press, 2001. ... Edited with a Biographical Essay by Mary Ann Glendon. Lanham, MD: Lexington Books, 2002. [The Patriot Ledger (Quincy, MA) 18 May 2002; First Things June/July 2002]. ... "Organ Donation and the Beatific Vision: ...
Pregnancy after organ transplantation is considered high-risk and requires supervision in specialized centers. The impact of immunosuppression on the developing fetus is still the subject of research. It has been shown that it affects lymphocyte populations in the first year of life. For this reason, researchers suggest postponing mandatory infant vaccinations. The aim of the study was to ...