- Español (Spanish)

HIV Overview
Hiv and aids clinical trials.
- A clinical trial is a research study in which people volunteer to help find answers to specific health questions. HIV and AIDS clinical trials help researchers find better ways to prevent, detect, or treat HIV and AIDS.
- Examples of HIV and AIDS clinical trials underway include studies of new HIV medicines, studies of vaccines to prevent or treat HIV, and studies of medicines to treat infections related to HIV and AIDS such as opportunistic infections .
- The details on the benefits and possible risks of participating in an HIV and AIDS clinical trial are explained to volunteers before they decide whether to participate in a study, through a process called an informed consent .
- Use the search feature on ClinicalTrials.gov to find HIV and AIDS studies looking for volunteer participants. Some HIV and AIDS clinical trials enroll only people who have HIV. Other studies enroll people who do not have HIV.
What is a clinical trial?
A clinical trial is a research study in which people volunteer to help find answers to specific health questions. These studies are conducted according to a plan, called a protocol, which include—
- New medicines or new combinations of medicines.
- New medical devices or surgical procedures.
- New, different ways to use an approved, existing medicine or device.
- New ways to change behaviors to improve health.
Clinical trials are conducted in several phases to determine whether new medical studies are safe and effective in people. Results from a Phase 1 Trial , Phase 2 Trial , and Phase 3 Trial are used to determine whether a new drug should be approved by the U.S. Food and Drug Administration for sale in the United States. Once a new drug is approved, researchers continue to track its safety in a Phase 4 Trial .
Interventional trial and observational trial are two main types of clinical trials:
- An interventional study tests (or tries out) an intervention—a potential drug or treatment, medical device, or procedure—in people. Interventional studies are often prospective and are specifically tailored to evaluate the direct effects of new drugs or treatments on disease.
- An observational study does not test potential treatments. Instead, researchers observe participants on their current treatment plan and track health outcomes. Observational studies (also called epidemiologic studies) are mostly retrospective .
What is an HIV and AIDS clinical trial?
HIV and AIDS clinical trials help researchers find better ways to prevent, detect, or treat HIV and AIDS. Every HIV medicine was first studied through clinical trials.
Examples of HIV and AIDS clinical trials include—
- studies of new medicines to prevent or treat HIV and AIDS.
- studies of vaccines to prevent or treat HIV.
- studies of medicines to treat infections related to HIV and AIDS, such as opportunistic infections.
Can anyone participate in an HIV and AIDS clinical trial?
Participation in a clinical trial depends on the study. Some HIV and AIDS clinical trials enroll only people who have HIV. Other studies include people who do not have HIV.
Participation in an HIV and AIDS clinical trial may also depend on other factors, such as age, gender, pregnancy, HIV treatment history, or other medical conditions.
What are the benefits of participating in an HIV and AIDS clinical trial?
Many people participate in HIV and AIDS clinical trials because they want to contribute to HIV and AIDS research. They may have HIV or know someone who has HIV.
People with HIV who participate in an HIV and AIDS clinical trial may benefit from new HIV medicines before they are widely available. HIV medicines being studied in clinical trials are called investigational drugs . To learn more, read the HIVinfo What is an Investigational HIV Drug? fact sheet.
Another benefit of participating in an HIV and AIDS clinical trial is that participants can receive regular and careful medical care from a research team that includes doctors and other health professionals. Often the medicines and medical care are free of charge.
Sometimes people get paid for participating in a clinical trial. For example, they may receive money or a gift card. They may be reimbursed for the cost of meals or transportation.
Are HIV and AIDS clinical trials safe?
Researchers try to make HIV and AIDS clinical trials as safe as possible. However, volunteering to participate in a study testing an experimental treatment for HIV can involve risks of varying degrees. Most volunteers do not experience serious side effects; however, potential side effects that may be serious or even life-threatening can occur from the treatment being studied.
Before enrolling in a clinical trial, potential volunteers learn about the study in a process called informed consent . The process includes an explanation of the possible risks and benefits of participating in the study.
The FDA believes that obtaining a research participant's written informed consent is only part of the process. Once enrolled in a study, people continue to receive information about the study through the informed consent process.
If a person decides to participate in an HIV and AIDS clinical trial, will their personal information be shared?
The privacy of study volunteers is very important to everyone involved in an HIV and AIDS clinical trial. The informed consent process includes an explanation of how a study volunteer’s personal information is protected.
How can one find an HIV and AIDS clinical trial looking for volunteer participants?
There are several ways to find an HIV and AIDS clinical trial searching for volunteer participants.
Use the find a case study search feature ClinicalTrials.gov to find HIV and AIDS studies looking for volunteer participants.
- Call a Clinicalinfo health information specialist at 1-800-448-0440 or email [email protected]
- Join ResearchMatch , which is a free, secure online tool that makes it easier for the public to become involved in clinical trials.
This fact sheet is based on information from the following sources:
From the National Institutes of Health (NIH):
- NIH Clinical Research Trials and You: The Basics
From the National Library of Medicine:
- Learn About Clinical Studies
From the Food and Drug Administration:
- Clinical Trials: What Patients Need to Know
- Informed Consent for Clinical Trials
Also see the HIV Source collection of HIV links and resources.
- Open access
- Published: 07 December 2021
The lived experience of HIV-infected patients in the face of a positive diagnosis of the disease: a phenomenological study
- Behzad Imani ORCID: orcid.org/0000-0002-1544-8196 1 ,
- Shirdel Zandi 2 ,
- Salman khazaei 3 &
- Mohamad Mirzaei 4
AIDS Research and Therapy volume 18 , Article number: 95 ( 2021 ) Cite this article
7653 Accesses
5 Citations
3 Altmetric
Metrics details
AIDS as a human crisis may lead to devastating psychological trauma and stress for patients. Therefore, it is necessary to study different aspects of their lives for better support and care. Accordingly, this study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease.
This qualitative study is a descriptive phenomenological study. Sampling was done purposefully and participants were selected based on the inclusion and exclusion criteria. Data collection was conducted, using semi-structured interviews. Data analysis was performed using Colaizzi’s method.
12 AIDS patients participated in this study. As a result of data analysis, 5 main themes and 12 sub-themes were identified, which include : emotional shock (loathing, motivation of social isolation), the fear of the consequences (fear of the death, fear of loneliness, fear of disgrace), the feeling of the guilt (feeling of regret, feeling guilty, feeling of conscience-stricken), the discouragement (suicidal ideation, disappointment), and the escape from reality (denial, trying to hide).
The results of this study showed that patients will experience unpleasant phenomenon in the face of the positive diagnosis of the disease and will be subjected to severe psychological pressures that require attention and support of medical and laboratory centers.
Patients will experience severe psychological stress in the face of a positive diagnosis of HIV.
Patients who are diagnosed with HIV are prone to make a blunder and dreadful decisions.
AIDS patients need emotional and informational support when they receive a positive diagnosis.
As a piece of bad news, presenting the positive diagnosis of HIV required the psychic preparation of the patient
Introduction
HIV/AIDS pandemic is one of the most important economic, social, and human health problems in many countries of the world, whose, extent and dimensions are unfortunately ever-increasing [ 1 ]. In such circumstances, this phenomenon should be considered as a crisis, which seriously affects all aspects of the existence and life of patients and even the health of society [ 2 ]. Diagnosing and contracting HIV/AIDS puts a person in a vague and difficult situation. Patients suffer not only from the physical effects of the disease, but also from the disgraceful consequences of the disease. HIV/AIDS is usually associated with avoidable behaviors that are not socially acceptable, such as unhealthy sexual, relations and drug abuse: So the patients are usually held guilty for their illness [ 3 ]. On the other hand, the issue of disease stigma in the community is the cause of rejection and isolation of these patients, and in health care centers is a major obstacle to providing services to these patients [ 4 ]. Studies show that HIV/AIDS stigma has a completely negative effect on the quality of life of these patients [ 5 ]. Criminal attitudes towards these patients and disappointing behavior by family, community, and medical staff cause blame and discrimination in patients [ 6 ]. HIV/AIDS stigma is prevalent among diseases, making concealment a major problem in this behavioral disease. The stigma comes in two forms: a negative inner feeling and a negative feeling that other people in the community have towards the patient [ 7 ]. The findings of a study that conducted in Iran indicated that increasing HIV/AIDS-related stigma decreases quality of life of people living with HIV/AIDS [ 8 ]. Robert Beckman has defined bad news as “any news that seriously and unpleasantly affects persons’ attitudes toward their future”. He considers the impact of counseling on moderating a person’s feeling of being important [ 9 ]. Therefore, being infected by HIV / AIDS due to the stigma can be bad news, which will lead to unpleasant emotional reactions [ 10 ]. Studies that have examined the lives of these patients have shown that these patients will experience mental and living problems throughout their lives. These studies highlight the need for age-specific programming to increase HIV knowledge and coping, increase screening, and improve long-term planning [ 11 , 12 ].
A prerequisite for any successful planning and intervention for people living with HIV/AIDS is approaching them and conducting in-depth interviews in order to discover their feelings, attitudes; their views on themselves, their illness, and others; and finally, their motivation to follow up and the participation in interventions [ 13 ]. Accordingly, the present study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease, since the better understanding of the phenomena leads to the smoother ways to help and care for these patients.
Study setting
In this study, a qualitative method of descriptive phenomenology was used to discover and interpret the lived experience of HIV-positive patients, when they face a positive diagnosis of the disease. The philosophical strengths underlying descriptive phenomenology afford a deeper understanding of the phenomenon being studied [ 14 ]. Husserl’s four steps of descriptive phenomenology were employed: bracketing, intuiting, analyzing and interpreting [ 15 ].
Participants and sampling
Sampling was done purposefully and participants were selected based on inclusion criteria. In this purposeful sampling, participants were selected among those patients who had sufficient knowledge about this phenomenon. The sample size was not determined at the beginning of the study, instead, it continued until no new idea emerged and data-saturated. Participants were selected from patients who were admitted to the Shohala Behavioral Diseases Counseling Center in Hamadan-Iran. The center has been set up to conduct tests, consultations, medical and dental services, and to distribute medicines among the patients. Additional inclusion criteria for selecting a participant are: having a positive diagnosis experience at the center, Ability to recall events and mental thoughts in the face of the first positive diagnosis of the disease, having psychological and mental stability, having a favorable clinical condition, willingness to work with the research team, and the possibility of re-access for the second interview if needed. Exclusion criteria were unwillingness to participate in the study and inability of verbal communication in Persian language.
Data collection
The interviews began with a non-structured question (tell us about your experience with a positive diagnosis) and continued with semi-structured questions. Each interview lasted 35–70 min and was conducted in two sessions if necessary. All interviews were conducted by the main investigator (ShZ) that who has experience in qualitative research and interviewing. The interview was recorded and then written down with permission of the participant.
Data analysis
The descriptive Colaizzi method was used to analyses the collected data [ 16 ]. This method consists of seven steps: (1) collecting the participants’ descriptions, (2) understanding the meanings in depth, (3) extracting important sentences, (4) conceptualizing important themes, (5) categorizing the concepts and topics, (6) constructing comprehensive descriptions of the issues examined, and (7) validating the data following the four criteria set out by Lincoln and Guba.
Trustworthiness criteria were used to validate the research, due to the fact that importance of data and findings validity in qualitative research [ 17 ]. This study was based on four criteria of Lincoln and Guba: credibility, transferability, dependability, and conformability [ 18 ]. For data credibility, prolong engagement and follow-up observations, as well as samplings with maximum variability were used. For dependability of the data, the researchers were divided into two groups and the research was conducted as two separate studies. At the same time, another researcher with the most familiarity and ability in conducting qualitative research, supervised the study as an external observer. Concerning the conformability, the researchers tried not to influence their own opinions in the coding process. Moreover, the codes were readout by the participants as well as two researcher colleagues with the help of an independent researcher and expert familiar with qualitative research. Transferability of data was confirmed by offering a comprehensive description of the subject, participants, data collection, and data analysis.
Ethical considerations (ethical approval)
The present study was registered with the ethics code IR.UMSHA.REC.1398.1000 in Hamadan University of Medical Sciences. The purpose of the study was explained and all participants’ consents were obtained at first step. All participants were assured that the information obtained would remain confidential and no personal information would be disclosed. Participants were also told that there was no need to provide any personal information to the interviewer, including name, surname, phone number and address. To gain more trust, interviews were conducted by a person who was not resident of Hamadan and was not a native of the region, this case was also reported to the participants.
Twelve HIV-infected participated in this study. The mean age of the participants was 36.41 ± 4.12 years. 58.33% of the participants were male and 41.66% were married. Of these, 2 were illiterate, 2 had elementary diploma, 6 had high school diploma and 2 had academic education. Six of them were unemployed, 5 were self-employed and 1 was an official employee. These people had been infected by this disease for 6.08 ± 2.71 years, in average (Table 1 ).
Analysis of the HIV-infected patients’ experiences of facing the positive diagnosis of the disease by descriptive phenomenology revealed five main themes: emotional shock, the fear of the consequences, the feeling of the guilt, the discouragement, and the escape from reality (Table 2 ).
Emotional shock
Emotional shock is one of the unpleasant events that these patients have experienced after facing a positive diagnosis of the disease. This experience has manifested in loathing and motivation of social isolation.
These patients stated that after facing a positive diagnosis of the disease, they developed a strong inner feeling of hatred towards the source of infection. The patients feel hatred, since they hold the carrier as responsible for their infection. “…After realizing I was affected, I felt very upset with my husband, I did not want to see him again, because it made me miserable, I even decided to divorce ….”(P3).
Motivation of social isolation
The experiences of these patients showed that after facing the incident, they have suffered an internal failure that has caused them to try to distance from other people. These patients have become isolated, withdrawing from the community and sometimes even from their families. “…After this incident, I decided to live alone forever and stay away from all my family members. I made a good excuse and broke up our engagement…” (P7).
Fear of the consequences
Fear of the consequences is one of the unpleasant experiences that these patients will face, as soon as they receive a positive diagnosis of the disease. Based on experiences, these patients feel fear of loneliness, death, and disgrace as soon as they hear the positive diagnosis.
Fear of the death
The patients said that as soon as they got the positive test results, they thought that the disease was incurable and would end their lives soon. “…When I found I had AIDS, I was very upset and moved like a dead man because I was really afraid that at any moment this disease might kill me and I would die …” (P1).
Fear of loneliness
The participants stated that one of the feelings that they experienced as soon as they received a positive diagnosis of the disease was the fear of being alone. They stated that at that moment, the thought of being excluded from society and losing their intimacy with them was very disturbing. “…The thought that I could no longer have a family and had to stay single forever bothered me a lot, it was terrifying to me when I thought that society could no longer accept me as a normal person …” (P10).
Fear of disgrace
One of the feelings that these patients experienced when faced the positive diagnosis of the disease was the fear of disgrace. They suffer from the perception that the spread of news of the illness hurts the attitudes of those around them and causes them to be discredited. “…It was very annoying for me when I thought I would no longer be seen as a member of my family, I felt I would no longer have a reputation and everyone would think badly of me …” (P2).
Feeling of the guilt
From other experiences of these patients in facing the positive diagnosis of the disease is feeling guilty. This feeling appears in patients as feeling of regret, guilty and remorse.
Feeling of regret
These patients stated that they felt remorse for their lifestyle and actions as soon as they heard the positive diagnosis of the disease, because they thought that if they had lived healthier, they would not have been infected. “…After realizing this disease, I was very sorry for my past, because I really did not have a healthy life. I made a series of mistakes that caused me to get caught. At that moment, I just regretted why I had this disaster …” (P11).
Feeling guilty
The experience of these patients has shown that after receiving a positive diagnosis of the disease, they consider themselves guilty and complain about themselves. These patients condemn their lifestyle and sometimes even consider themselves deserving of the disease and think that it is a ransom that they have paid back. “…after getting the disease, I realized that I was paying the ransom because I was hundred percent guilty, I was the one who caused this situation with a series of bad deeds, and now I have to be punished …” (P5).
Feeling of conscience-stricken
One of the experiences that these patients reported is the pangs of conscience. These patients stated that after receiving a positive diagnosis of the disease, the thought that as a carrier they might have contaminated those around them was very unpleasant and greatly affected their psyche. “…after getting the disease. It was shocked and I was just crazy about the fact that if my wife and children had taken this disease from me, what would I do, I made them hapless … and this as very annoying for me …” (P8).
Discouragement
Discouragement is an unpleasant experience that patients experienced after receiving a positive HIV test results. Discouragement in these patients appears in the suicidal ideation and disappointment.
Suicidal ideation
The patients stated that they were so upset with the positive diagnosis of the illness and they immediately thought they could not live with the fact and the best thing to do was to end their own lives. “…The news was so bad for me that I immediately thought that if the test result was correct and I had AIDS, I would have to kill myself and end this wretch life, oh, I had a lot of problem and the thought of having to wait for a gradual death was horrible to me …” (P12).
Disappointment
The experience of these patients shows that a positive diagnosis of the disease for these patients leads to a destructive feeling of disappointment. So that they are completely discouraged from their lives. These patients think that their dreams and goals are vanished and that they have reached the end and everything is over. “…It was a horrible experience, so at that moment I felt my life was over, I had to prepare myself for a gradual death, I was at marriage ages when I thought I could no longer get married, I saw life as meaningless …” (P7).
Escape from reality
The lived experience of these patients shows that after receiving a positive diagnosis of the disease, they found that this fact was difficult to accept and somehow tried to escape from the reality. This experience has been in the form of denial and trying to hide from others.
One of the experiences of these patients in dealing with the positive test result of this disease has been to deny it. In this way, patients believed that the test result was wrong or that the result belonged to someone else. For this reason, the patients referred to other laboratories after receiving the first positive diagnosis of the disease. “…After the lab told me this and found out what the disease really was, I was really shocked and said it was impossible, it was definitely wrong and it is not true … I could not believe it at all, because I was a professional athlete and this could not happen to me. So I immediately went to a bigger city and there I went to a few laboratories for further tests …” (P6).
Trying to hide
These patients stated that after receiving the first positive diagnosis of the disease, they thought that no one should notice their disease and should remain anonymous as much as possible. “…I immediately decided that no one in my city should know that I got this disease and the news should not be spread anywhere, so I discard my phone number through which our city laboratory communicated with me and I came here to do a re-examination and go to the doctor, and after all these years, I always come here again for an examination …” (P4).
In this qualitative study, we attempted to discover lived experience of HIV-infected patients in the face of a positive diagnosis of the disease. Therefore, a descriptive phenomenological method was applied. As a result of this study, based on the experiences of the HIV-infected patients, the five main themes of emotional shock, fear of the consequences, feelings of guilt, discouragement and, escape from reality were obtained.
In this study, it was shown that the confrontation of these patients with the positive diagnosis of the disease causes them to experience a severe emotional shock. In this regard, Yangyang Qiu et al. [ 19 ] argued that anxiety and depression are very common among HIV-infected patients who have recently been diagnosed with the disease. The experience of the participants has shown that this emotional shock appears in the form of loathing and the motivation of social isolation. In fact, in these patients, the feeling of the loathing is an emotional response to the primary carrier that has infected them. The study of Imani et al. [ 20 ] have shown that decrease emotional intelligence in an environment where there is an HIV carrier, other people hate him/her, because they see him/her as a risk factor for their infection. The experience of the participants has also shown that receiving a positive diagnosis will motivate social isolation in these patients. Various studies have revealed that one of the consequences of AIDS/HIV that patients will suffer from, is social isolation [ 21 , 22 ].
Another experience of the participants, according to this study is fear of the consequences. This phenomenon appears in these patients as fear of the death, fear of loneliness, and fear of disgrace. Due to the nature of the disease, these patients feel an inner fear of premature death, as soon as they receive a positive diagnosis. In this regard, the study of Audrey K Miller et al. [ 23 ] showed that death anxiety in AIDS patients is a psychological complication. the participants have stated that they are very afraid of being alone after receiving a positive diagnosis, which is a natural feeling according to Keith Cherry and David H. Smith [ 24 ]; because these patients will mainly experience some degree of loneliness. HIV-infected patients also experienced a fear of disgrace, which will go back to the nature of the disease and people’s insight; but they should be aware that, as Newman Amy states, AIDS/ HIV is a disease, not a scandal [ 25 ].
Another experience of the participants in dealing with the positive diagnosis of the disease is guilt feeling. The patients will experience feelings of regret, the feeling guilty and feeling of the conscience-stricken. The experience of the participants shows that they regret their past. Earlier studies have also revealed that regret for the past is a common phenomenon among the patients living with HIV [ 26 , 27 , 28 ]. HIV-infected feel guilty while facing the positive diagnosis of the disease and consider themselves the main culprit of the situation. They often play a direct role in their infection, and their past lifestyle for sure [ 29 ]. Our study also found that these patients feel the conscience-stricken after a positive diagnosis, because they suspect that they may have infected people around them. This disease can be easily transmitted from the carrier to others if the health protocols are not followed [ 30 , 31 , 32 ].
Another experience of HIV-infected in dealing with the receiving a positive diagnosis of the disease is discouragement. These patients are disappointed and sometimes decide to suicide. Based on the lived experience of HIV-infected, it was found that receiving a positive diagnosis of the disease, will discourage them from life and patients will be disappointed in many aspects of life. Studies have shown that AIDS/HIV, as a crisis, will greatly reduce the patients' life expectancy and that they will continue to live in despair [ 33 ]. Studies also stated that they considered suicide as a solution to relieve stress when receiving a positive diagnosis. In this regard, various studies have emphasized that among the AIDS/HIV patients, loss of self-esteem and severe stress have led to high suicide rates [ 34 , 35 , 36 ].
According to the patients, trying to escape from reality is another phenomenon that they will experience. This phenomenon will occur in patients as denial and trying to hide the disease from others. Based on the lived experience of these patients, it was found that after facing a positive diagnosis, HIV-infected tend to deny that they are infected. In this regard, various studies have shown that AIDS/HIV patients in different stages of the disease and their lives try to deny it in different ways [ 37 , 38 , 39 ]. The HIV-infected also stated that at the beginning of the positive diagnosis of the disease, did not want others to know, so they wanted to hide themselves from others in any way possible. In this regard, Emilie Henry et al. [ 40 ] have shown that a high percentage of the patients living with AIDS/HIV have tried that others do not notice that they are ill.
One of the strengths of this study is the methodology of the study, because in this study, an attempt has been made to use descriptive phenomenology to explain the lived experience of HIV-infected patients when faced with a positive diagnosis of this disease. In fact, in this study, patients' experience of this particular situation was identified, and with careful analysis, the experiences of these people became codes and concepts, each of which can be a bridge that keeps the path of modern knowledge open to help these patients. One of the limitations of this study is the generalizability of the findings because patients’ experiences in different societies that have cultural, religious, subsistence, and economic differences can be different.
The results of this study showed that patients will experience unpleasant experiences in the face of receiving a positive diagnosis of the HIV. Patients’ unpleasant experiences at that moment include emotional shock, fear of the consequences, feeling guilty, discouragement and escape from reality. Therefore, medical and laboratory centers must pay attention to the patients' lived experience, and try to support the patients through education, counseling and other support programs to minimize the psychological trauma caused by the disease.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding authors through reasonable request.
Acknowledgements
The authors would like to express their gratitude to the Hamadan Health Network, the Hamadan Shohada Behavioral Diseases Counseling Center, and the participants who helped us in this study.
The study was funded by Vice-chancellor for Research and Technology, Hamadan University of Medical Sciences (No. 9812209934).
Author information
Authors and affiliations.
Department of Operating Room, School of Paramedicine, Hamadan University of Medical Sciences, Hamadan, Iran
Behzad Imani
Department of Operating Room, Student Research Committee, Hamadan University of Medical Sciences, Hamadan, Iran
Shirdel Zandi
Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
Salman khazaei
Department of Epidemiology, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
Mohamad Mirzaei
You can also search for this author in PubMed Google Scholar
Contributions
BI designed the study, collected the data, and provide the first draft of manuscript. ShZ designed the study and revised the manuscript. SKh participated in design of the study, the data collection, and revised the manuscript. MM participated in design of the study and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Shirdel Zandi .
Ethics declarations
Ethics approval and consent to participate.
This study is the result of a student project that has been registered in Hamadan University of Medical Sciences of Iran with the ethical code IR.UMSHA.REC.1398.1000.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Imani, B., Zandi, S., khazaei, S. et al. The lived experience of HIV-infected patients in the face of a positive diagnosis of the disease: a phenomenological study. AIDS Res Ther 18 , 95 (2021). https://doi.org/10.1186/s12981-021-00421-4
Download citation
Received : 15 July 2021
Accepted : 26 November 2021
Published : 07 December 2021
DOI : https://doi.org/10.1186/s12981-021-00421-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lived experience
- Phenomenological study
AIDS Research and Therapy
ISSN: 1742-6405
- Submission enquiries: [email protected]
- Open access
- Published: 27 March 2023
A case study of HIV/AIDS services from community-based organizations during COVID-19 lockdown in China
- Jennifer Z.H. Bouey 1 , 2 ,
- Jing Han 3 ,
- Yuxuan Liu 1 ,
- Myriam Vuckovic 1 ,
- Keren Zhu 2 ,
- Kai Zhou 4 &
BMC Health Services Research volume 23 , Article number: 288 ( 2023 ) Cite this article
2125 Accesses
2 Citations
8 Altmetric
Metrics details
Introduction
People living with HIV (PLHIV) relied on community-based organizations (CBOs) in accessing HIV care and support during the COVID-19 pandemic in China. However, little is known about the impact of, and challenges faced by Chinese CBOs supporting PLHIV during lockdowns.
A survey and interview study was conducted among 29 CBOs serving PLHIV in China between November 10 and November 23, 2020. Participants were asked to complete a 20-minute online survey on their routine operations, organizational capacity building, service provided, and challenges during the pandemic. A focus group interview was conducted with CBOs after the survey to gather CBOs’ policy recommendations. Survey data analysis was conducted using STATA 17.0 while qualitative data was examined using thematic analysis.
HIV-focused CBOs in China serve diverse clients including PLHIV, HIV high-risk groups, and the public. The scope of services provided is broad, ranging from HIV testing to peer support. All CBOs surveyed maintained their services during the pandemic, many by switching to online or hybrid mode. Many CBOs reported adding new clients and services, such as mailing medications. The top challenges faced by CBOs included service reduction due to staff shortage, lack of PPE for staff, and lack of operational funding during COVID-19 lockdowns in 2020. CBOs considered the ability to better network with other CBOs and other sectors (e.g., clinics, governments), a standard emergency response guideline, and ready strategies to help PLHIV build resilience to be critical for future emergency preparation.
Chinese CBOs serving vulnerable populations affected by HIV/AIDS are instrumental in building resilience in their communities during the COVID-19 pandemic, and they can play significant roles in providing uninterrupted services during emergencies by mobilizing resources, creating new services and operation methods, and utilizing existing networks. Chinese CBOs’ experiences, challenges, and their policy recommendations can inform policy makers on how to support future CBO capacity building to bridge service gaps during crises and reduce health inequalities in China and globally.
Peer Review reports
The COVID-19 pandemic is a defining catastrophic public health event of our lifetimes.In China, the COVID-19 pandemic started with a national lockdown in 2020. After two years of conservative intervention focusing on mass testing and quarantine, COVID-19 came back in 2022 and caused millions of infections and an overwhelming death toll, which put a significant strain on China’s healthcare system and paralyzed the economic engine. How do Chinese community organizations support vulnerable populations such as HIV/AIDS patients during such disasters? What policy changes do the Chinese CBOs hope to see? Our case study strives to answer these questions.
China was the first country to encounter the novel coronavirus disease and to implement a strict, large-scale lockdown between January 23, 2020, and April 2020 to contain the virus [ 1 , 2 ]. Most of the 31 provinces in China declared the highest Emergency Level on January 23rd of 2020, enabling local governments to employ social policing mechanisms to enforce quarantine and to close public events with crowd gatherings across the country. Most highways and public transportation were shut down (January 23- February 7) [ 2 ]. All businesses and recreational facilities were closed, except for medical emergency rooms, grocery stores, and keyinfrastructure-related economic activities. In rural areas, many villages stalled traffic and set up entrance checks, whereas urban residential communities required residents to prove their residence to use the weekly grocery shopping quota [ 3 ]. After the outbreak peaked in mid-February, many prefecture-level cities switched from the stringentshutdown to semi-lockdown for another month [ 4 ]. Wuhan, the capital of Hubei province and the origin of the outbreak, experienced the longest lockdown from January 21 to April 7, 2020 [ 5 ]. COVID-19 and the stringent intervention had a profound impact on the lives of the Chinese people during this initial period of the COVID-19 pandemic [ 6 , 7 ].
China is also home to 1.05 million people living with HIV (PLHIV) who needed long-term antiviral medical treatment and care in 2020 [ 8 ]. The central government provides PLHIVs access to free antiretroviral therapy (ART) and free voluntary counseling and testing since 2003 [ 9 ]. In 2016, the new “Treatment for All’’ policy removed the requirement of low CD4 levels as a treatment qualifier. By 2020, about 978,138 PLHIV had gained access to ART, covering 92.9% of all PLHIV in China [ 8 ]. Despite this progress and updated policies, various structural, psychological, and behavioral barriers to ART adherence persist [ 10 ]. Barriers including patients’ concerns for side effects and “pill burden,” lack of effective communication between patients and health care providers, low patient self-efficacy of ART, competing priorities for patients, and depression and stigma associated with HIV [ 11 , 12 ]. Like many Community-Based Organizations (CBO) serving vulnerable populations globally, Chinese CBOs play critical roles in helping PLHIV to improve their access to HIV screening, treatment and care, and reduce stigma, especially among men who have sex with men (MSM) [ 13 , 14 , 15 , 16 ]. In China, there are two main types of CBOs providing services to PLHIV: those independently registered with the state/provincial or local government of Civil Affairs as a non-profit organization, and those affiliated with health clinics and local public health offices without an independent registry [ 17 ]. Both types of CBOs rely on government public health agencies for funding.
COVID-19 has led to unprecedented stress on health and public health systems and has intensified disruptions in HIV prevention, testing, and HIV care continuum services worldwide [ 18 ]. China is not an exception. A Chinese provincial study based on the HIV registration system found a 49% drop in HIV testing rates and a 37% drop in new HIV diagnoses during the first months of COVID-19. In addition, only half of the 475 newly diagnosed HIV patients underwent CD4 count testing and 28.6% did not receive routine linkage to care in the same time period [ 19 ].
Around the world,PLHIV and high-risk populations rely on CBOs for their rich local knowledge, operational flexibility, and direct contact to people in need, to provide humanitarian aid during a crisis [ 20 ]. Facing challenges due to quarantine requirements and transportation service requirements, CBOs in many countries responded by moving their services online and utilizing technology-driven solutions to promote access to HIV counseling, testing, and treatment [ 21 ]. Global [ 22 , 23 ] and China-specific [ 24 ] studies have shown that CBOs promoting community connectedness among MSM resulted in higher HIV testing rates during COIVD-19. However, CBOs themselves are not immune to the negative impact of COVID-19. Preliminary studies in the U.S. have found that the COVID-19 pandemic presents multifaceted challenges to CBOs providing HIV services, including but not limited to structural inequality, resources shortages, and disruption to patient-centered services provision [ 25 , 26 ].
Clearly, more in-depth studies among CBOs are necessary to understand COVID-19’s impact among CBOs serving PLHIV in China. Although several studies in China highlighted the challenges to PLHIV [ 19 , 27 , 28 , 29 ] and healthcare workers [ 30 , 31 ], few looked at the implications for Chinese CBOs during the lockdowns. Only one stakeholder study published in English included 17 CBO workers in the interviews and found that CBOs could assist HIV care among PLHIV in multiple ways during COVID-19 [ 13 ].
In this study, a team of CBO leaders, clinicians, and public health researchers try to answer the following questions using data collected from a mixed-method study (survey and focus group): What challenges did PLHIV face during the first pandemic lockdown in China? What were the challenges to the CBOs and how did they cope? What innovation came out of the crisis? What gaps in CBOs’ capacity were revealed and how to build better preparedness for future emergencies? The study provides critical information on how best to prepare and utilize community organization services on HIV care during a public health emergency or a disaster.
Study design and participants
The study research team included HIV specialists of a large infectious disease hospital in Beijing, their affiliated and long-term CBO partner “Home of Red Ribbon (HRR),” staff of the Joint United Nations Programme on HIV/AIDS (UNAIDS) Beijing office, and global health researchers from Georgetown University and the RAND Corporation, an American think tank that develops solutions to public policy challenges. HRR was founded in 1999 to serve local PLHIV. In 2019, HRR founded the “Beijing Red Ribbon Alliance,” a national platform with 60 + CBO members serving PLHIV. In this study, CBO participants were recruited by HRR from the Alliance. They come from all seven geographic regions of China and were considered reliable information sources based on previous collaborations with HRR. Organizations participating in the study had to meet the following criteria: (a) established Chinese CBOs providing HIV prevention and treatment services; (b) delivered services from January 20, 2020, to April 29, 2020; and (c) would like to provide informed consent for the study. Among survey invitations to 32 qualified CBOs, 29 CBOs responded. Three CBOs have multiple branch offices that completed the survey, yielding a 90% response rate.
Data collection
Both qualitative and quantitative data on service provision and needs during the COVID-19 pandemic were collected from the participating CBOs. A 20-minute online survey with both closed- and open-ended questions was first disseminated and collected between November 10 and November 23, 2020, and a virtual focus group interview was conducted on November 13, 2020. In addition to the survey data, detailed notes from the focus group interview were used for theme analysis. All data collection followed the principles of confidentiality and voluntary participation. There were no consequences if a participant withdrew from the study. The study protocol was approved by the Ditan Hospital Internal Research Board (IRB number: KY2020-019).
The online survey questionnaire was designed by the research team staff from Beijing Ditan Hospital with HRR. A Chinese online survey platform “Wen-Juan-Xing’’ was used to host the survey, which was then disseminated to the invited participants through the social media app WeChat. The CBO organizations that completed the online survey received RMB 800 (approximately USD 125) for their participation. The questionnaire contained nineteen close-ended multiple-choice questions and eleven open-ended short-answer questions to cover the following three domains:
CBO routine operational characteristics
questions obtained information on the CBO’s location of operation, operational years, registration status, number of full-time and part-time staff and volunteers, presence of PLHIV among staff and volunteers, CBO’s social media platform usage, target client populations and routine services provided.
Service provision during COVID-19
questions included CBO’s operational modes during COVID-19, presence of operation interruptions during the pandemic, CBO’s target client populations during the pandemic, types of services requested and provided during the pandemic. The survey also asked about the ways clients contacted CBOs during the COVID-19 lockdown.
If CBOs reported unresolved requests or an interruption in service provision during COVID-19 lockdowns, they were asked to provide follow-up information on the types of such requests in open-ended short answers, whether service provision had resumed, and whether there was staff loss. Finally, the CBOs were asked to rate their satisfaction on their collaborations with government agencies and other CBOs during the pandemic.
Needs and organizational capacity building
questions started with a description of the CBO’s operational advantages and challenges during COVID-19, including short answers on CBOs’ most urgent needs, the relative advantages of their organizations compared to other CBOs, and whether their services were better recognized and expanded during COVID-19. They also estimated whether COVID-19 was helpful or not, in terms of future prospects of the organization.
Focus group interview
While the survey focused on the challenges CBOs faced during the lockdown, a focus group interview was set up to help researchers contextualize the findings of the survey and to collect policy recommendations to support CBOs’ work in future outbreaks. All 29 survey participants were invited to the focus group interviews and eighteen CBOs (62%) participated through Tencent Meeting (an online meeting platform in China) after they completed the survey. The focus group interview was led by a Ditan Hospital HIV specialist and an HRR staff following a semi-structured question guide. The semi-structured question guide was developed to capture the following themes: (a) what services delivery challenges they encountered during COVID-19 in 2020; (b) which special groups of patients (e.g., elderly, people with disability etc.) came to their service during the COVID-19 lockdown; (c) what innovation and lessons they have learned from providing services for PLHIV during the COVID-19 pandemic; and (d) what policy recommendations do they have to enhance CBOs’ service delivery in future pandemics.The online focus group interview lasted two hours until data saturation was achieved. Detailed field notes were used for data analyses.
Data analysis
Online survey data was collected and managed through the online service platform Wen-Juan-Xing and analyzed using STATA 17.0 [ 32 ]. We first provided descriptive statistics to summarize the characteristics of the CBOs operations, services, and clients during COVID-19 with multiple choice questions. We then used thematic analysis to analyze and explore potential themes of the open-ended questions. Two independent researchers followed the analytic process recommended for thematic analysis [ 33 ]: (a) familiarizing themselves with the data; (b) generating-e initial themes and codes; (c) coding the open-ended answers according to the themes; (d) discussing the differences, obtaining consensus, and finalizing the name of the themes; and (e) producing the report for the results section. The same approach was used to summarize additional themes from the notes of the focus group interview. Quotations were used to highlight the findings. Both survey and focus group scripts were analyzed in Chinese and translated to English for the report. Back translations were used to check for translation accuracy.
Characteristics of CBOs
29 CBOs participated in the study and their characteristics aree summarized in Table 1 . More than half (55.2%) were registered with the Chinese government as a civil organization, while 13 CBOs (44.8%) were affiliated with hospitals or the local public health agencies. More than one third of the CBOs (41.4%) in the study were located in the North or Northeast Region of China, about another third (34.5%) were from Eastern or Southern China, and seven (24.1%) CBOs were from West China. Number of staff was another measurement of the operation scale: 41.4% (n = 12) of CBOs reported more than 50 staff, while only two (6.9%) reported having less than 10 staff (Table 1 ). 69.0% of CBOs employed PLHIV, and all organizations reported having PLHIV among their volunteers.
CBOs’ new services during the COVID-19 lockdown
Even before COVID-19, Chinese CBOs often served a diverse client population. In our study, the majority (96.4%) of CBOs reported providing services to MSM, 80% catered to PLHIV, 60.7% provided services to adolescents at risk, and others facilitated services to migrants (28.6%), female commercial sex workers (25%), substance users (7.1%), children affected and orphaned by AIDS (14.3%), and the general public (25%) before the COVID-19 pandemic (Table 2 ). During COVID-19 lockdowns, almost all CBOs reported providing new services to non-local clients seeking HIV related services when they could not go back to their routine medical services (n = 28, 96.6%), and to their regular clients who got stranded in other cities (n = 26, 89.7%), in addition to their regular local clients. These new services were requested through various channels, including peer referrals, online platforms and group chats, hospitals and clinics, and through CBOs’ pre-pandemic services.
The scope of CBO services also changed during the COVID-19 lockdown period. While most CBOs reported continued provision of regular services, they had to add services unique to the lock-down period, including mailing ART medicines and post-exposure prophylaxis (PEP), supporting family notification of PLHIV’s HIV status, and peer support (Table 2 ).
Not only did the service requests intensify during the COVID-19 lockdown, but many CBOs also had to switch their on-site services to phone- and online-based when the travel restrictions hit. All participating CBOs reported using one or more new platforms such as WeChat, TikTok, etc. for services during this period (Table 2 ). Meanwhile, most CBOs still maintained on-site services except for five who stopped providing in-person services.
To cope with the challenges brought by the pandemic, many CBOs turned to innovative communication strategies and digital technology to secure medicine supplies. One CBO said: “There are 10 internet volunteers to promote online, and 5 volunteers to make appointments for testing, so that you can ensure access to various HIV supplies via the internet without having to come to the office.” (Medium CBO, 5–9 yrs of operation, independent, large city in the West). Six CBOs also attributed human-centered care and respect for PLHIV, their rapport with marginalized clients, and their ability to operate at the grass-roots level as key factors in their success. As one CBO put it: “Government agencies work according to rules and regulations, while friends of the community work more on the basis of their enthusiasm and human feelings for the community.” (Large CBO,10–14 yrs of operation, independent, small city in the Northeast/North).
Challenges and coping strategies during COVID-19
While many CBOs successfully carried out services for PLHIV, challenges still mounted during the unexpected lockdowns. In the survey, most CBOs (90%) reported unmet needs from their clients during the pandemic, especially on access to ART (41%), referral to health care (24%), and HIV testing and confirmation (21%). About a third of CBOs reported that their services were disrupted by the pandemic, particularly their in-person services (31.0%). Among the services most impacted were in-person HIV testing (27.6%), in-person counseling (10.3%), in-person volunteering (3.4%) and outreach (3.4%). After the lockdown, all CBOs resumed their services. However, 33.3% of organizations reported losing staff.
When asked about the top three challenges during the COVID-19 lockdown, 18 CBOs identified limited service provision modes as their main challenge, followed by shortage of personal protective equipment (PPE) for staff (51.7%), lack of funding (37.9%), staff shortages and loss of staff and volunteers (17.2%), limited or slow HIV testing services (10.3%), lack of support from other sectors and society at large (3.4%), limited medical resources (3.4%), and hard to obtain and deliver medication (13.8%). CBOs also mentioned short-term funding shortfalls, weak Wi-Fi, and inaccessibility of office space as challenges.
One additional challenge CBOs reported was the lack of mail courier services, especially in remote areas and to college students who live on locked-down campuses. One CBO observed: “Some patients stop taking their medication when they can’t even get to the courier company in places where transportation is inconvenient.” (Medium CBO, 5–9 yrs of operation, civil governance registered, medium city in the West). Another said: “It is difficult to give medication to students because the school is very strict, no deliveries to campus for 8 months, and security checks to enter school, risking exposure of privacy.” (Medium CBO, 5–9 yrs of operation, independent, small city in the West).
Another common challenge was associated with HIV testing and confirmation tests: “There has been no opportunity to confirm and then start treatment for infected persons with positive initial screening due to the lockdown and home isolation…. Someone tested positive in July and it took three months to confirm.” (Medium CBO, 5–9 yrs of operation, independent, small city in the West).
Finally, several CBOs mentioned that they could not meet clients’ needs in gaining peer support, resolving financial issues and how to navigate other barriers.
An important coping strategy among the CBOs was building collaboration with various government agencies, including local CDC (86.2%), hospitals (86.2%), the Ministry of Public Security (10.3%), and local government organizations or other agencies (10.3%). On a scale from 0 to 10, most organizations were very satisfied with their collaborations during the pandemic (24 CBOs > 8), four CBOs were somewhat satisfied (ratings of 5–7), and only one CBO was completely unsatisfied (rating of 0). Almost 80% of CBOs reported collaborations with other non-governmental organizations, mostly with similar organizations in the same region (e.g., provincial and municipal sister agencies). Such collaboration helped relieve shortages of service, medicine, and PPEs.
CBO’s sustainability and capacity building needs
When asked about the top three areas of needs, 15 CBOs named funding and personnel as their top need (51.72%). Other top needs included technical assistance, supplies, organizational capacity building, and collaboration among CBOs and with other sectors. While the second and third needs varied, organizational capacity building was mentioned seven times (24.14%), demonstrating its significance for the CBOs. Only two CBOs did not report any external needs.
Many organizations felt that the capacity needed during the pandemic were better coordination and communication skills (27.6%), flexibility (20.7%), and good service provision (13.8%). Six CBOs also emphasized that the ability to provide online consultation and telemedicine services were useful skills during a pandemic. A large network and emergency response training were also desirable capacities reported by the CBOs.
Despite the many challenges faced by the participating CBOs and their clients during the COVID-19 pandemic, most of the CBOs felt that they had gained popularity during the pandemic, and many mentioned thank-you-notes from their clients. They were also able to build a larger network with requests from other organizations (34.5%), received media coverage (20.7%), and additional project funding (31.0%) during the pandemic. About half of the CBOs considered the COVID-19 pandemic beneficial to their organization’s development.
Policy recommendations from the CBOs
The focus group interview helped confirm capacity-building needs. More importantly participating CBOs also offered the following recommendations during the focus group discussion, which expand on the needs expressed in the survey. We summarized the policy recommendations in the following:
Create regional CBO service alliance networks : “Alliances can be formed between community organizations, and a directory of information on local drug assistance, etc., can be produced and sent to patients so that they can refer to the directory for targeted help.” (Large CBO, 5–9 yrs of operation, independent, mega city in the Northeast/North).
Strengthen multisectoral cooperation between CBOs, hospitals, the CDC, community level government and community health centers from different regions: “… the local CDC alone may not be able to get the job done. There is a need for the creation of a network of emergency support services in the event of an emergency.” (Large CBO, 14 yrs + of operation, civil governance registered, large city in the Northeast/North).
Develop standardized emergency response operational manuals/guidelines (including recruitment). One CBO talked about preparing both CBOs and their clients by establishing guidelines: “There should be guidelines for patients, but also for community organizations, including what community organizations can do, how to do it, how to do risk assessment (e.g. group lending, mutual aid lending), and what are the channels for obtaining supplies; for patients, it is a manual for self-management of infected persons in case of emergency.” (Large CBO, 14 yrs + of operation, civil governance registered, large city in the Northeast/North).
Support PLHIV community resilience building . Many CBOs discussed ways to build resilience among PLHIV during emergencies, including on ART: “Infected people need to be better guided and educated about treatment adherence.” (Small CBO, 5–9 yrs of operation, independent, medium city in the East/South).
Optimize medicine access during a crisis . CBOs identified access to medicine as the top challenge during COVID-19 and the necessity of flexible policy on longer-term prescriptions: “It would be better for the infected to be prepared when something like this happens again, and to have peace of mind, if they are advised by the agency that dispenses the drugs.” (Large CBO,5–9 yrs of operation, independent, medium city in the East/South).
Build a larger volunteer pool to offset staff shortage during a crisis : “Policies are needed to involve volunteers in the fight against the pandemic and AIDS.” (Medium CBO, 5–9 yrs of operation, independent, small city in the West).
COVID-19 posed unprecedented challenges to global health and reversed decades of hard-earned progress on health [ 34 ]. Our study was one of the first to survey and interview frontline CBO staff that serve PLHIV around China in the first year of the pandemic. The CBOs in our study varied in their operational size and their affiliations status with the CDC and clinics. While some work in urban centers with advanced economic development, others are located in rural districts. In both the survey and the focus group interview, the common themes were the challenges they faced unexpectedly when COVID-19 hit and how the strict lockdown added to their service scope and forced them to change service methodology. Our survey findings add to the growing literature on resilience of communities during a natural disaster and highlight the importance of networking, digital platforms, and operational flexibility among grass-root community organizations. The focus group interview with the CBOs further explained the mechanisms of coping and provided a much-needed reflection on the need for capability building for future pandemics or disasters.
Our study found that CBOs serving people living with HIV in China often had at least 5–10 years of experience working with local PLHIV and generally have good working knowledge and close collaborations with local public health agencies and medical institutions. This type of three-in-one network has proven to improve performance metrics on disease testing and detections among high-risk populations [ 35 ]. The community organizations also serve a diverse population, including PLHIV as well as people at higher risk for HIV, such as MSM and female sex workers, and routinely carry out services including health promotion, peer support, and treatment coordination. Many CBOs have volunteers from the local PLHIV or high-risk population, which enables them to conduct targeted outreach and build trust with their clients. This finding validates a community resilience theory [ 36 ] that named four primary sets of adaptive capacities as critical to community resilience: social capital, economic development, information and communication, and community competence. The social capital, community competency, and communication skills of the CBOs have helped the organizations to achieve high efficiency in HIV control with flexible working venues and low operating costs.
During emergencies, to build collective resilience, communities must create organizational linkages, boost and protect social supports, and plan for not having a plan – which requires flexibility, decision-making skills, and trusted sources of information that function in the face of unknowns [ 36 ]. Our study found that CBOs that can provide PLHIV with wider organizational connections and mobilize social support through flexible operation plans, had a pivotal role in building community resilience during COVID-19. For example, despite the fact that the National Center for AIDS/STD Control and Prevention of China’s CDC issued a special policy to facilitate ART treatment continuity among PLHIV at the early stage of the COVID-19 pandemic [ 37 ], travel restrictions under the COVID-19 lockdown still had a significant impact on PLHIV’s access to and the CBO’s ability to provide services, such as ART, testing, and other medical care [ 13 ]. Since the lockdown happened at Chinese New Year, a time when internal migration is at its peak and a large population visits their family away from where they work, many PLHIV found themselves stuck in places away from their routine care. Many who had to quarantine with their parents found themselves having to forgo privacy and to disclose to their parents and families for the first time that they needed HIV care [ 27 , 38 ]. Meanwhile, most of the local staff at public health stations were redeployed to respond to COVID-19. CBOs found significant workload increase with new clients stranded in their location in need of HIV care, new demands to coordinate HIV treatment continuity and testing, and additional requests on peer support in this time of crisis. In response, many CBOs had to make quick decisions to switch their service online and to seek new connections with fellow organizations and new government agencies– with varying success as our survey showed. Similar to our study’s findings, a 2020 China AIDS Fund for NGOs and UNAIDS’s CBO survey found that 87% of community organizations set up their own hotlines and implemented flexible working hours for volunteers during the COVID-19 epidemic from February to April 2020, to provide AIDS-related services. Nearly half added express mailing services for delivery of HIV self-testing kits and medicine to their services [ 39 ].
The same UNAIDS survey revealed that some CBOs encountered difficulties in HIV/AIDS services during the peak of the pandemic during February and March of 2020. The main reasons for the service interruption were urban traffic control (86%) and CDC staff who were unable to support AIDS prevention work (51%) because of their participation in the prevention and control of the COVID-19 epidemic. By the end of April 2020, about 53% of community organizations had fully restored their services, and 42% had restored some services [ 39 ]. Our findings are in line with the scenario described in the UNAIDS report and found the most critical challenges to the CBOs to be a lack of funding, limited service provision methods, shortage of staff and PPE, limited medical resources, testing and medication delivery capacities, and lack of support and understanding from society at large. All these factors contributed to CBOs’ service disruption, in addition to the reasons identified by the UNAIDS survey.
Paton (2000) defined community resilience as the capacity to bounce back and use physical and economic resources effectively to aid recovery following exposure to hazards [ 40 ]. In an earlier report for UNAIDS, we found that as a vulnerable population, PLHIV faced unique challenges during the unexpected COVID-19 lockdowns [ 41 ]. However, they had better resiliency resources – the CBOs that had already served their community before the pandemic – compared to other vulnerable populations, such as migrant workers and people with disabilities in China [ 41 ]. To build stronger resilience in the face of future disaster situations, the CBOs in our study offered multiple suggestions that we can summarize into four recommendations: First, enhance CBOs network building both horizontally and vertically: horizontally among CBOs with similar missions across different geographic areas so that when PLHIV travel, they can rely on the network for the continuation of support; vertically between CBOs and multiple hierarchies of government and healthcare facilities for resource coordination. Such collaborations should be included in government-level emergency response plans and policies to ensure the continuation of support for PLHIVs.
Secondly, funding agencies should consider supporting CBOs’ capacity building in communication and technology upgrades so that CBOs can expand their digital direct service platforms and mobilize resources during a crisis.
Thirdly, CBOs should consider strengthening their volunteer base and building a workforce reserve for their community-based services to prepare for staff shortages during emergencies. CBOs can mobilize these local talents from various groups. One way is to empower PLHIV to become peer supporters/volunteers during emergencies. Their presence in an emergency response would benefit the utilization of community-based services, and reduce PLHIV’s unease to disclose their status and seek help. Another way to engage more talents to grassroot community governance is to provide CBO-based internships for college students and professional training institutes (e.g., to students of public health, medicine, sociology, or other related fields). Efforts should also be made to cultivate professional talent serving grassroot communities, adjust policies and incentive mechanisms, and encourage more experts to provide intellectual support for community governance. Encouraging the public to participate in grassroots social governance can also help empower community members and generate increased cohesion and community resilience.
Finally, the CBOs’ capacity building should include a community-level emergency response plan. Education on disaster prevention and mitigation at the community level should be strengthened, and communities with excellent emergency response and disaster relief operations should be promoted as models, so their experiences can be shared. Bureaucratically and institutionally, the division of labor in emergency response and community governance should be further clarified, and community staff should receive training in emergency planning and response, to provide speedy and efficient public service when faced with future uncertainties and emergencies.
The findings of this study should be viewed in the context of several limitations. First, the study survey was cross-sectional. Therefore, causal inference could not be established, and the results can only reflect the situation of CBOs during a certain period during the pandemic. Second, the study only analyzed 29 responses from different CBOs and their operational branches, utilizing the connections of HRR. The limited number of participants and the recruitment method may have led to biased results, as the selected CBOs might not be representative of the population. Third, all information in the study was self-reported by one manager of each CBO, thus is subject to risk of bias.
Risks and vulnerabilities induced by pandemics and other natural hazards and disasters are on the rise globally. Some emergencies, such as COVID-19, have severe and widespread destructive impacts on health, the economy, social development, and global supply chains. In this context, community resilience to disasters is critical for government hazard mitigation and recovery planning [ 36 , 42 ]. Our case study showed that CBOs serving a highly stigmatized and vulnerable population before the crisis were instrumental in building resilience in the community. They were able to quickly mobilize resources, set up new business platforms/models, and expand their network to meet unprecedented challenges. They also identified key areas for capacity building for future crisis preparedness. Their experience and reflections may help governments, communities, and international organizations when considering how to reduce health inequity and how to serve those who need long-term healthcare during an unexpected natural or manmade crisis.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Molefi M, Tlhakanelo JT, Phologolo T, Hamda SG, Masupe T, Tsima B, et al. The impact of China’s Lockdown Policy on the incidence of COVID-19: an interrupted Time Series Analysis. Biomed Res Int. 2021;2021:9498029.
Article PubMed PubMed Central Google Scholar
Full, Text. Fighting COVID-19: China in Action [Internet]. [cited 2022 Apr 12]. Available from: http://www.scio.gov.cn/zfbps/32832/Document/1681809/1681809.htm
Ren X. Pandemic and lockdown: a territorial approach to COVID-19 in China, Italy and the United States. Eurasian Geogr Econ. 2020 Sep;61(2):423–34.
Leung K, Wu JT, Liu D, Leung GM. First-wave COVID-19 transmissibility and severity in China outside Hubei after control measures, and second-wave scenario planning: a modelling impact assessment. The Lancet. 2020 Apr25;395(10233):1382–93.
Pan A, Liu L, Wang C, Guo H, Hao X, Wang Q, et al. Association of Public Health Interventions with the epidemiology of the COVID-19 outbreak in Wuhan, China. JAMA. 2020 May;19(19):1915–23.
Jia P, Liu L, Xie X, Yuan C, Chen H, Guo B et al. Changes in dietary patterns among youths in China during COVID-19 epidemic: The COVID-19 impact on lifestyle change survey (COINLICS). Appetite. 2021 Mar 1;158:105015.
Ren X, Huang W, Pan H, Huang T, Wang X, Ma Y. Mental Health during the Covid-19 outbreak in China: a Meta-analysis. Psychiatr Q. 2020 Dec;91(4):1033–45.
He N. Research Progress in the Epidemiology of HIV/AIDS in China.China CDC Wkly. 2021 Nov26;3(48):1022–30.
Wu Z, Chen J, Scott SR, McGoogan JM. History of the HIV Epidemic in China. Curr HIV/AIDS Rep. 2019;16(6):458–66.
Zhou G, Li X, Qiao S, Zhou Y, Shen Z. Psychological and behavioral barriers to ART adherence among PLWH in China: role of self-efficacy. AIDS Care. 2017 Dec;29(12):1533–7.
Zhou G, Li X, Qiao S, Shen Z, Zhou Y. Influence of Side Effects on ART Adherence Among PLWH in China: The Moderator Role of ART-Related Knowledge. AIDS Behav. 2018 Mar 1;22(3):961–70.
Chen W-T, Shiu C, Yang JP, Chuang P, Zhang L, Bao M, et al. A structural equation model of patient-healthcare provider relationships and HIV-infected patient outcomes in chinese populations. AIDS Care. 2018 Mar;30(3):383–90.
Sun Y, Zhan Y, Li H, Yuan T, Gao Y, Liang B, et al. Stakeholder efforts to mitigate antiretroviral therapy interruption among people living with HIV during the COVID-19 pandemic in China: a qualitative study. J Int AIDS Soc. 2021 Sep;24(9):e25781.
Yan H, Zhang M, Zhao J, Huan X, Ding J, Wu S, et al. The increased effectiveness of HIV preventive intervention among men who have sex with men and of follow-up care for people living with HIV after “task-shifting” to community-based organizations: a “cash on service delivery” model in China. PLoS ONE. 2014;9(7):e103146.
Tao J, Li M, Qian H-Z, Wang L-J, Zhang Z, Ding H-F, et al. Home-based HIV testing for men who have sex with men in China: a novel community-based partnership to complement government programs. PLoS ONE. 2014;9(7):e102812.
Cheng W, Cai Y, Tang W, Zhong F, Meng G, Gu J et al. Providing HIV-related services in China for men who have sex with men. Bull World Health Organ. 2016 Mar 1;94(3):222–7.
Liu L, Wang D, Qin X, Hu Z, Chen R. The impact of social capital on civil society organizations delivering voluntary counseling and testing HIV/AIDS service: a cross-sectional study in China.Biosci Trends. 2020 Jul17;14(3):182–91.
Ogunbodede OT, Zablotska-Manos I, Lewis DA. Potential and demonstrated impacts of the COVID-19 pandemic on sexually transmissible infections.Curr Opin Infect Dis. 2021 Feb1;34(1):56–61.
Shi L, Tang W, Hu H, Qiu T, Marley G, Liu X et al. The impact of COVID-19 pandemic on HIV care continuum in Jiangsu, China. BMC Infect Dis. 2021 Aug 7;21(1):768.
Han J, Su Y, Zhou Z, Wang K, Yu Y, Huang H, et al. Analysis of antiretroviral medicine availability to people living with HIV from different designated medical institutions during the COVID-19 pandemic. Chin J AIDS STD. 2020;26(07):698–700.
Google Scholar
Harsono D, Deng Y, Chung S, Barakat LA, Friedland G, Meyer JP et al. Experiences with Telemedicine for HIV Care During the COVID-19 Pandemic: A Mixed-Methods Study. AIDS Behav. 2022.
Painter TM, Song EY, Mullins MM, Mann-Jackson L, Alonzo J, Reboussin BA, et al. Social support and other factors associated with HIV testing by Hispanic/Latino gay, bisexual, and other men who have sex with men in the U.S. South. AIDS Behav. 2019 Oct;23(Suppl 3):251–65.
Grover E, Grosso A, Ketende S, Kennedy C, Fonner V, Adams D, et al. Social cohesion, social participation and HIV testing among men who have sex with men in Swaziland. AIDS Care. 2016;28(6):795–804.
Article PubMed Google Scholar
Lyu H, Zhou Y, Dai W, Zhen S, Huang S, Zhou L, et al. Solidarity and HIV Testing willingness during the COVID-19 epidemic: a Study among Men who have sex with men in China. Front Public Health. 2021 Dec;9:9:752965.
Pinto RM, Park S. COVID-19 pandemic disrupts HIV Continuum of Care and Prevention: implications for research and practice concerning community-based Organizations and Frontline Providers. AIDS Behav. 2020;24(9):2486–9.
Robillard AG, Julious CH, Smallwood SW, Douglas M, Gaddist BW, Singleton T. Structural inequities, HIV Community-Based Organizations, and the end of the HIV Epidemic. Am J Public Health. 2022 Mar;112(3):417–25.
Sun Y, Li H, Luo G, Meng X, Guo W, Fitzpatrick T, et al. Antiretroviral treatment interruption among people living with HIV during COVID-19 outbreak in China: a nationwide cross-sectional study. J Int AIDS Soc. 2020 Nov;23(11):e25637.
Sun S, Hou J, Chen Y, Lu Y, Brown L, Operario D. Challenges to HIV Care and Psychological Health during the COVID-19 pandemic among people living with HIV in China. AIDS Behav. 2020 Oct;24(10):2764–5.
Booton RD, Fu G, MacGregor L, Li J, Ong JJ, Tucker JD et al. The impact of disruptions due to COVID-19 on HIV transmission and control among men who have sex with men in China. J Int AIDS Soc. 2021 Apr 6;24(4):e25697.
Yang X, Zeng C, Tam CC, Qiao S, Li X, Shen Z et al. HIV Service Interruptions During the COVID-19 Pandemic in China: The Role of COVID-19 Challenges and Institutional Response from Healthcare Professional’s Perspective. AIDS Behav. 2021 Oct 6
Qiao S, Yang X, Sun S, Li X, Mi T, Zhou Y, et al. Challenges to HIV service delivery and the impacts on patient care during COVID-19: perspective of HIV care providers in Guangxi, China. AIDS Care. 2021 May;33(5):559–65.
StataCorp. Stata Statistical Software: Release 17. College Station. TX: StataCorp LLC; 2021.
Nowell LS, Norris JM, White DE, Moules NJ. Thematic Analysis: Striving to Meet the Trustworthiness Criteria. International Journal of Qualitative Methods. 2017 Dec 1;16(1):1609406917733847.
Fenner R, Cernev T. The implications of the Covid-19 pandemic for delivering the Sustainable Development Goals. Futures. 2021 Apr;128:102726.
Zhang D, Lu H, Zhuang M, Wu G, Yan H, Xu J et al. Enhancing HIV Testing and Treatment among Men Who Have Sex with Men in China: A Pilot Model with Two-Rapid Tests, Single Blood Draw Session, and Intensified Case Management in Six Cities in 2013. PLoS One. 2016 Dec 1;11(12):e0166812.
Norris FH, Stevens SP, Pfefferbaum B, Wyche KF, Pfefferbaum RL. Community Resilience as a Metaphor, Theory, Set of Capacities, and Strategy for Disaster Readiness. Am J Community Psychol. 2008;41(1–2):127–50.
National Center for AIDS/STD Control and Prevention, Chinese Center for Disease Control and Prevention. Notice on guaranteeing the free HIV antiretroviral treatment drugs supply for stranded people living with HIV - Notice - Chongqing Network for HIV/AIDS Communication and Education [Internet]. [cited 2022 Apr 12]. Available from: http://www.cqaidsw.com/index php?m=content&c=index&a=show&catid=58&id=4389
Mi T, Li X, Zhou G, Qiao S, Shen Z, Zhou Y. HIV Disclosure to Family Members and Medication Adherence: role of social support and self-efficacy. AIDS Behav. 2020 Jan;24(1):45–54.
UNAIDS. Research | The impact of the COVID-19 pandemic on CBOs. ’ HIV prevention and treatment services [Internet]. WeChat. [cited 2022 Apr 12]. Available from: http://mp.weixin.qq.com/s?__biz=MzA3OTgxODkwNA==&mid=2649756780&idx=1&sn=99f89e502150e931386347ca2d2948d0&chksm=87a90d9bb0de848db8760a36e4e2358d150f1e9081f6a4eb6ccb6f554accba23b749251584e0#rd
Paton D. Emergency planning: integrating community development, community resilience and hazard mitigation. J Am Soc Prof Emerg Managers. 2000 Jan;1:7:109–18.
Guo W, Wen H L, Bai H, Liu J, Wei X N, Zhou K, Sande A. Quick community survey on the impact of COVID-19 outbreak for the healthcare of people living with HIV. Chinese J Epidemiol. 2020 May;41(5):662–666.
Rose A. Defining and measuring economic resilience to disasters. Disaster Prevention and Management: An International Journal. 2004 Jan 1;13(4):307–14.
Download references
Acknowledgements
Thanks to all community organizations serving HIV patients and people who are at high risk for HIV in China, who participated in the survey and focus group discussion. Special thanks to the House of Red Ribbon that coordinated interviews and focus groups, and to UNAIDS China Office for providing support on information and data analysis.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Department of Global Health, School of Health, Georgetown University, 3700 Reservoir Road NW, Washington, DC, 20057, USA
Jennifer Z.H. Bouey, Yuxuan Liu & Myriam Vuckovic
RAND Corporation, Santa Monica, CA, USA
Jennifer Z.H. Bouey & Keren Zhu
Ditan Infectious Disease Hospital, Beijing, China
UNAIDS China, Beijing, China
Home of Red Ribbon, Beijing, China
You can also search for this author in PubMed Google Scholar
Contributions
Jing Han, Jennifer Bouey designed the study and manuscript, Jing Han and Ye Su. collected data, Yuxuan Liu, Myriam Vuckovic conducted data analysis, Jennifer Bouey, Yuxuan Liu, Myriam Vuckovic drafted the manuscript., Keren Zhu and Kai Zhou participated in drafting and editing.
Corresponding author
Correspondence to Jennifer Z.H. Bouey .
Ethics declarations
Ethical approval.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The study protocol was approved by the Ditan Hospital Internal Research Board (IRB number: KY2020-019).
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Not applicable.
Competing interests
The authors have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bouey, J.Z., Han, J., Liu, Y. et al. A case study of HIV/AIDS services from community-based organizations during COVID-19 lockdown in China. BMC Health Serv Res 23 , 288 (2023). https://doi.org/10.1186/s12913-023-09271-4
Download citation
Received : 02 August 2022
Accepted : 10 March 2023
Published : 27 March 2023
DOI : https://doi.org/10.1186/s12913-023-09271-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- HIV/AIDS care
- Community-based Organizations
- Telemedicine
- Community capacity building
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 November 2021
A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data
- Shobhit Srivastava ORCID: orcid.org/0000-0002-7138-4916 1 ,
- Shekhar Chauhan ORCID: orcid.org/0000-0002-6926-7649 2 ,
- Ratna Patel ORCID: orcid.org/0000-0002-5371-7369 3 &
- Pradeep Kumar ORCID: orcid.org/0000-0003-4259-820X 1
Scientific Reports volume 11 , Article number: 22841 ( 2021 ) Cite this article
11k Accesses
7 Citations
11 Altmetric
Metrics details
- Health care
- Health services
- Public health
Acquired Immunodeficiency Syndrome caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. This study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with the change in awareness level on HIV-related information among adolescents over the period. Data used for this study were drawn from Understanding the lives of adolescents and young adults, a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh. The present study utilized a sample of 4421 and 7587 unmarried adolescent boys and girls, respectively aged 10–19 years in wave-1 and wave-2. Descriptive analysis and t-test and proportion test were done to observe changes in certain selected variables from wave-1 (2015–2016) to wave-2 (2018–2019). Moreover, random effect regression analysis was used to estimate the association of change in HIV awareness among unmarried adolescents with household and individual factors. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2 to 39.1% between wave-1 & wave-2. With the increase in age and years of schooling, the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV. Adolescent boys' paid work status was inversely associated with HIV awareness [Coef: − 0.01; p < 0.10]. Use of internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness with reference to their counterparts. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups, as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents.
Similar content being viewed by others

Predictors of never testing for HIV among sexually active individuals aged 15–56 years in Rwanda
Awareness and use of HIV pre-exposure prophylaxis and factors associated with awareness among MSM in Beijing, China

Identification of adolescent girls and young women for targeted HIV prevention: a new risk scoring tool in KwaZulu Natal, South Africa
Introduction.
Acquired Immunodeficiency Syndrome (AIDS) caused by Human Immunodeficiency Virus (HIV) poses a severe challenge to healthcare and is a significant public health issue worldwide. So far, HIV has claimed almost 33 million lives; however, off lately, increasing access to HIV prevention, diagnosis, treatment, and care has enabled people living with HIV to lead a long and healthy life 1 . By the end of 2019, an estimated 38 million people were living with HIV 1 . More so, new infections fell by 39 percent, and HIV-related deaths fell by almost 51 percent between 2000 and 2019 1 . Despite all the positive news related to HIV, the success story is not the same everywhere; HIV varies between region, country, and population, where not everyone is able to access HIV testing and treatment and care 1 . HIV/AIDS holds back economic growth by destroying human capital by predominantly affecting adolescents and young adults 2 .
There are nearly 1.2 billion adolescents (10–19 years) worldwide, which constitute 18 percent of the world’s population, and in some countries, adolescents make up as much as one-fourth of the population 3 . In India, adolescents comprise more than one-fifth (21.8%) of the total population 4 . Despite a decline projection for the adolescent population in India 5 , there is a critical need to hold adolescents as adolescence is characterized as a period when peer victimization/pressure on psychosocial development is noteworthy 6 . Peer victimization/pressure is further linked to risky sexual behaviours among adolescents 7 , 8 . A higher proportion of low literacy in the Indian population leads to a low level of awareness of HIV/AIDS 9 . Furthermore, the awareness of HIV among adolescents is quite alarming 10 , 11 , 12 .
Unfortunately, there is a shortage of evidence on what predicts awareness of HIV among adolescents. Almost all the research in India is based on beliefs, attitudes, and awareness of HIV among adolescents 2 , 12 . However, few other studies worldwide have examined mass media as a strong predictor of HIV awareness among adolescents 13 . Mass media is an effective channel to increase an individuals’ knowledge about sexual health and improve understanding of facilities related to HIV prevention 14 , 15 . Various studies have outlined other factors associated with the increasing awareness of HIV among adolescents, including; age 16 , 17 , 18 , occupation 18 , education 16 , 17 , 18 , 19 , sex 16 , place of residence 16 , marital status 16 , and household wealth index 16 .
Several community-based studies have examined awareness of HIV among Indian adolescents 2 , 10 , 12 , 20 , 21 , 22 . However, studies investigating awareness of HIV among adolescents in a larger sample size remained elusive to date, courtesy of the unavailability of relevant data. Furthermore, no study in India had ever examined awareness of HIV among adolescents utilizing information on longitudinal data. To the author’s best knowledge, this is the first study in the Indian context with a large sample size that examines awareness of HIV among adolescents and combines information from a longitudinal survey. Therefore, this study intends to examine the change in the awareness level of HIV among adolescents. Furthermore, this study examined the factors associated with a change in awareness level on HIV-related information among adolescents over the period.
Data and methods
Data used for this study were drawn from Understanding the lives of adolescents and young adults (UDAYA), a longitudinal survey on adolescents aged 10–19 in Bihar and Uttar Pradesh 23 . The first wave was conducted in 2015–2016, and the follow-up survey was conducted after three years in 2018–2019 23 . The survey provides the estimates for state and the sample of unmarried boys and girls aged 10–19 and married girls aged 15–19. The study adopted a systematic, multi-stage stratified sampling design to draw sample areas independently for rural and urban areas. 150 primary sampling units (PSUs)—villages in rural areas and census wards in urban areas—were selected in each state, using the 2011 census list of villages and wards as the sampling frame. In each primary sampling unit (PSU), households to be interviewed were selected by systematic sampling. More details about the study design and sampling procedure have been published elsewhere 23 . Written consent was obtained from the respondents in both waves. In wave 1 (2015–2016), 20,594 adolescents were interviewed using the structured questionnaire with a response rate of 92%.
Moreover, in wave 2 (2018–2019), the study interviewed the participants who were successfully interviewed in 2015–2016 and who consented to be re-interviewed 23 . Of the 20,594 eligible for the re-interview, the survey re-interviewed 4567 boys and 12,251 girls (married and unmarried). After excluding the respondents who gave an inconsistent response to age and education at the follow-up survey (3%), the final follow-up sample covered 4428 boys and 11,864 girls with the follow-up rate of 74% for boys and 81% for girls. The effective sample size for the present study was 4421 unmarried adolescent boys aged 10–19 years in wave-1 and wave-2. Additionally, 7587 unmarried adolescent girls aged 10–19 years were interviewed in wave-1 and wave-2 23 . The cases whose follow-up was lost were excluded from the sample to strongly balance the dataset and set it for longitudinal analysis using xtset command in STATA 15. The survey questionnaire is available at https://dataverse.harvard.edu/file.xhtml?fileId=4163718&version=2.0 & https://dataverse.harvard.edu/file.xhtml?fileId=4163720&version=2.0 .
Outcome variable
HIV awareness was the outcome variable for this study, which is dichotomous. The question was asked to the adolescents ‘Have you heard of HIV/AIDS?’ The response was recorded as yes and no.
Exposure variables
The predictors for this study were selected based on previous literature. These were age (10–19 years at wave 1, continuous variable), schooling (continuous), any mass media exposure (no and yes), paid work in the last 12 months (no and yes), internet use (no and yes), wealth index (poorest, poorer, middle, richer, and richest), religion (Hindu and Non-Hindu), caste (Scheduled Caste/Scheduled Tribe, Other Backward Class, and others), place of residence (urban and rural), and states (Uttar Pradesh and Bihar).
Exposure to mass media (how often they read newspapers, listened to the radio, and watched television; responses on the frequencies were: almost every day, at least once a week, at least once a month, rarely or not at all; adolescents were considered to have any exposure to mass media if they had exposure to any of these sources and as having no exposure if they responded with ‘not at all’ for all three sources of media) 24 . Household wealth index based on ownership of selected durable goods and amenities with possible scores ranging from 0 to 57; households were then divided into quintiles, with the first quintile representing households of the poorest wealth status and the fifth quintile representing households with the wealthiest status 25 .

Statistical analysis
Descriptive analysis was done to observe the characteristics of unmarried adolescent boys and girls at wave-1 (2015–2016). In addition, the changes in certain selected variables were observed from wave-1 (2015–2016) to wave-2 (2018–2019), and the significance was tested using t-test and proportion test 26 , 27 . Moreover, random effect regression analysis 28 , 29 was used to estimate the association of change in HIV awareness among unmarried adolescents with household factors and individual factors. The random effect model has a specific benefit for the present paper's analysis: its ability to estimate the effect of any variable that does not vary within clusters, which holds for household variables, e.g., wealth status, which is assumed to be constant for wave-1 and wave-2 30 .
Table 1 represents the socio-economic profile of adolescent boys and girls. The estimates are from the baseline dataset, and it was assumed that none of the household characteristics changed over time among adolescent boys and girls.
Figure 1 represents the change in HIV awareness among adolescent boys and girls. The percentage of adolescent boys who had awareness regarding HIV increased from 38.6% in wave-1 to 59.9% in wave-2. Among adolescent girls, the percentage increased from 30.2% in wave-1 to 39.1% in wave-2.
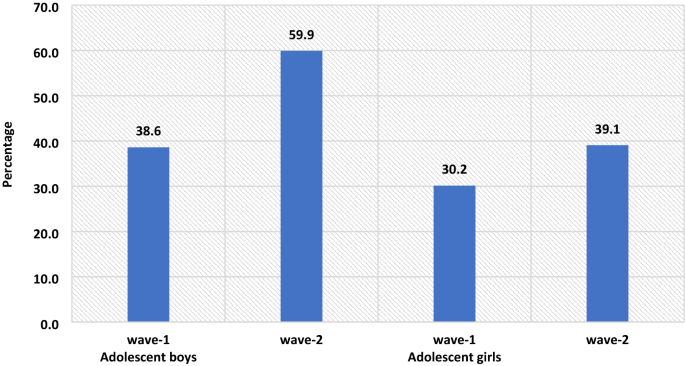
The percenate of HIV awareness among adolescent boys and girls, wave-1 (2015–2016) and wave-2 (2018–2019).
Table 2 represents the summary statistics for explanatory variables used in the analysis of UDAYA wave-1 and wave-2. The exposure to mass media is almost universal for adolescent boys, while for adolescent girls, it increases to 93% in wave-2 from 89.8% in wave-1. About 35.3% of adolescent boys were engaged in paid work during wave-1, whereas in wave-II, the share dropped to 33.5%, while in the case of adolescent girls, the estimates are almost unchanged. In wave-1, about 27.8% of adolescent boys were using the internet, while in wave-2, there is a steep increase of nearly 46.2%. Similarly, in adolescent girls, the use of the internet increased from 7.6% in wave-1 to 39.3% in wave-2.
Table 3 represents the estimates from random effects for awareness of HIV among adolescent boys and girls. It was found that with the increases in age and years of schooling the HIV awareness increased among adolescent boys ([Coef: 0.05; p < 0.01] and [Coef: 0.04; p < 0.01]) and girls ([Coef: 0.03; p < 0.01] and [Coef: 0.04; p < 0.01]), respectively. The adolescent boys [Coef: 0.06; p < 0.05] and girls [Coef: 0.03; p < 0.05] who had any mass media exposure were more likely to have an awareness of HIV in comparison to those who had no exposure to mass media. Adolescent boys' paid work status was inversely associated with HIV awareness about adolescent boys who did not do paid work [Coef: − 0.01; p < 0.10]. Use of the internet among adolescent boys [Coef: 0.18; p < 0.01] and girls [Coef: 0.14; p < 0.01] was positively associated with HIV awareness in reference to their counterparts.
The awareness regarding HIV increases with the increase in household wealth index among both adolescent boys and girls. The adolescent girls from the non-Hindu household had a lower likelihood to be aware of HIV in reference to adolescent girls from Hindu households [Coef: − 0.09; p < 0.01]. Adolescent girls from non-SC/ST households had a higher likelihood of being aware of HIV in reference to adolescent girls from other caste households [Coef: 0.04; p < 0.01]. Adolescent boys [Coef: − 0.03; p < 0.01] and girls [Coef: − 0.09; p < 0.01] from a rural place of residence had a lower likelihood to be aware about HIV in reference to those from the urban place of residence. Adolescent boys [Coef: 0.04; p < 0.01] and girls [Coef: 0.02; p < 0.01] from Bihar had a higher likelihood to be aware about HIV in reference to those from Uttar Pradesh.
This is the first study of its kind to address awareness of HIV among adolescents utilizing longitudinal data in two indian states. Our study demonstrated that the awareness of HIV has increased over the period; however, it was more prominent among adolescent boys than in adolescent girls. Overall, the knowledge on HIV was relatively low, even during wave-II. Almost three-fifths (59.9%) of the boys and two-fifths (39.1%) of the girls were aware of HIV. The prevalence of awareness on HIV among adolescents in this study was lower than almost all of the community-based studies conducted in India 10 , 11 , 22 . A study conducted in slums in Delhi has found almost similar prevalence (40% compared to 39.1% during wave-II in this study) of awareness of HIV among adolescent girls 31 . The difference in prevalence could be attributed to the difference in methodology, study population, and study area.
The study found that the awareness of HIV among adolescent boys has increased from 38.6 percent in wave-I to 59.9 percent in wave-II; similarly, only 30.2 percent of the girls had an awareness of HIV during wave-I, which had increased to 39.1 percent. Several previous studies corroborated the finding and noticed a higher prevalence of awareness on HIV among adolescent boys than in adolescent girls 16 , 32 , 33 , 34 . However, a study conducted in a different setting noticed a higher awareness among girls than in boys 35 . Also, a study in the Indian context failed to notice any statistical differences in HIV knowledge between boys and girls 18 . Gender seems to be one of the significant determinants of comprehensive knowledge of HIV among adolescents. There is a wide gap in educational attainment among male and female adolescents, which could be attributed to lower awareness of HIV among girls in this study. Higher peer victimization among adolescent boys could be another reason for higher awareness of HIV among them 36 . Also, cultural double standards placed on males and females that encourage males to discuss HIV/AIDS and related sexual matters more openly and discourage or even restrict females from discussing sexual-related issues could be another pertinent factor of higher awareness among male adolescents 33 . Behavioural interventions among girls could be an effective way to improving knowledge HIV related information, as seen in previous study 37 . Furthermore, strengthening school-community accountability for girls' education would augment school retention among girls and deliver HIV awareness to girls 38 .
Similar to other studies 2 , 10 , 17 , 18 , 39 , 40 , 41 , age was another significant determinant observed in this study. Increasing age could be attributed to higher education which could explain better awareness with increasing age. As in other studies 18 , 39 , 41 , 42 , 43 , 44 , 45 , 46 , education was noted as a significant driver of awareness of HIV among adolescents in this study. Higher education might be associated with increased probability of mass media and internet exposure leading to higher awareness of HIV among adolescents. A study noted that school is one of the important factors in raising the awareness of HIV among adolescents, which could be linked to higher awareness among those with higher education 47 , 48 . Also, schooling provides adolescents an opportunity to improve their social capital, leading to increased awareness of HIV.
Following previous studies 18 , 40 , 46 , the current study also outlines a higher awareness among urban adolescents than their rural counterparts. One plausible reason for lower awareness among adolescents in rural areas could be limited access to HIV prevention information 16 . Moreover, rural–urban differences in awareness of HIV could also be due to differences in schooling, exposure to mass media, and wealth 44 , 45 . The household's wealth status was also noted as a significant predictor of awareness of HIV among adolescents. Corroborating with previous findings 16 , 33 , 42 , 49 , this study reported a higher awareness among adolescents from richer households than their counterparts from poor households. This could be because wealthier families can afford mass-media items like televisions and radios for their children, which, in turn, improves awareness of HIV among adolescents 33 .
Exposure to mass media and internet access were also significant predictors of higher awareness of HIV among adolescents. This finding agrees with several previous research, and almost all the research found a positive relationship between mass-media exposure and awareness of HIV among adolescents 10 . Mass media addresses such topics more openly and in a way that could attract adolescents’ attention is the plausible reason for higher awareness of HIV among those having access to mass media and the internet 33 . Improving mass media and internet usage, specifically among rural and uneducated masses, would bring required changes. Integrating sexual education into school curricula would be an important means of imparting awareness on HIV among adolescents; however, this is debatable as to which standard to include the required sexual education in the Indian schooling system. Glick (2009) thinks that the syllabus on sexual education might be included during secondary schooling 44 . Another study in the Indian context confirms the need for sex education for adolescents 50 , 51 .
Limitations and strengths of the study
The study has several limitations. At first, the awareness of HIV was measured with one question only. Given that no study has examined awareness of HIV among adolescents using longitudinal data, this limitation is not a concern. Second, the study findings cannot be generalized to the whole Indian population as the study was conducted in only two states of India. However, the two states selected in this study (Uttar Pradesh and Bihar) constitute almost one-fourth of India’s total population. Thirdly, the estimates were provided separately for boys and girls and could not be presented combined. However, the data is designed to provide estimates separately for girls and boys. The data had information on unmarried boys and girls and married girls; however, data did not collect information on married boys. Fourthly, the study estimates might have been affected by the recall bias. Since HIV is a sensitive topic, the possibility of respondents modifying their responses could not be ruled out. Hawthorne effect, respondents, modifying aspect of their behaviour in response, has a role to play in HIV related study 52 . Despite several limitations, the study has specific strengths too. This is the first study examining awareness of HIV among adolescent boys and girls utilizing longitudinal data. The study was conducted with a large sample size as several previous studies were conducted in a community setting with a minimal sample size 10 , 12 , 18 , 20 , 53 .
The study noted a higher awareness among adolescent boys than in adolescent girls. Specific predictors of high awareness were also noted in the study, including; higher age, higher education, exposure to mass media, internet use, household wealth, and urban residence. Based on the study findings, this study has specific suggestions to improve awareness of HIV among adolescents. There is a need to intensify efforts in ensuring that information regarding HIV should reach vulnerable sub-groups as outlined in this study. It is important to mobilize the available resources to target the less educated and poor adolescents, focusing on rural adolescents. Investment in education will help, but it would be a long-term solution; therefore, public information campaigns could be more useful in the short term.
WHO. HIV/AIDS . https://www.who.int/news-room/fact-sheets/detail/hiv-aids (2020).
Singh, A. & Jain, S. Awareness of HIV/AIDS among school adolescents in Banaskantha district of Gujarat. Health Popul.: Perspect. Issues 32 , 59–65 (2009).
Google Scholar
WHO & UNICEF. adolescents Health: The Missing Population in Universal Health Coverage . 1–31 https://www.google.com/search?q=adolescents+population+WHO+report&rlz=1C1CHBF_enIN904IN904&oq=adolescents+population+WHO+report&aqs=chrome..69i57.7888j1j7&sourceid=chrome&ie=UTF-8 (2018).
Chauhan, S. & Arokiasamy, P. India’s demographic dividend: state-wise perspective. J. Soc. Econ. Dev. 20 , 1–23 (2018).
Tiwari, A. K., Singh, B. P. & Patel, V. Population projection of India: an application of dynamic demographic projection model. JCR 7 , 547–555 (2020).
Troop-Gordon, W. Peer victimization in adolescence: the nature, progression, and consequences of being bullied within a developmental context. J. Adolesc. 55 , 116–128 (2017).
PubMed Google Scholar
Dermody, S. S., Friedman, M., Chisolm, D. J., Burton, C. M. & Marshal, M. P. Elevated risky sexual behaviors among sexual minority girls: indirect risk pathways through peer victimization and heavy drinking. J. Interpers. Violence 35 , 2236–2253 (2020).
Lee, R. L. T., Loke, A. Y., Hung, T. T. M. & Sobel, H. A systematic review on identifying risk factors associated with early sexual debut and coerced sex among adolescents and young people in communities. J. Clin. Nurs. 27 , 478–501 (2018).
Gurram, S. & Bollampalli, B. A study on awareness of human immunodeficiency virus among adolescent girls in urban and rural field practice areas of Osmania Medical College, Hyderabad, Telangana, India. (2020).
Jain, R., Anand, P., Dhyani, A. & Bansal, D. Knowledge and awareness regarding menstruation and HIV/AIDS among schoolgoing adolescent girls. J. Fam. Med. Prim Care 6 , 47–51 (2017).
Kawale, S., Sharma, V., Thaware, P. & Mohankar, A. A study to assess awareness about HIV/AIDS among rural population of central India. Int. J. Commun. Med. Public Health 5 , 373–376 (2017).
Lal, P., Nath, A., Badhan, S. & Ingle, G. K. A study of awareness about HIV/AIDS among senior secondary school Children of Delhi. Indian J. Commun. Med. 33 , 190–192 (2008).
CAS Google Scholar
Bago, J.-L. & Lompo, M. L. Exploring the linkage between exposure to mass media and HIV awareness among adolescents in Uganda. Sex. Reprod. Healthcare 21 , 1–8 (2019).
McCombie, S., Hornik, R. C. & Anarfi, J. K. Effects of a mass media campaign to prevent AIDS among young people in Ghana . Public Health Commun. 163–178 (Routledge, 2002). https://doi.org/10.4324/9781410603029-17 .
Sano, Y. et al. Exploring the linkage between exposure to mass media and HIV testing among married women and men in Ghana. AIDS Care 28 , 684–688 (2016).
Oginni, A. B., Adebajo, S. B. & Ahonsi, B. A. Trends and determinants of comprehensive knowledge of HIV among adolescents and young adults in Nigeria: 2003–2013. Afr. J. Reprod. Health 21 , 26–34 (2017).
Rahman, M. M., Kabir, M. & Shahidullah, M. Adolescent knowledge and awareness about AIDS/HIV and factors affecting them in Bangladesh. J. Ayub. Med. Coll. Abbottabad 21 , 3–6 (2009).
Yadav, S. B., Makwana, N. R., Vadera, B. N., Dhaduk, K. M. & Gandha, K. M. Awareness of HIV/AIDS among rural youth in India: a community based cross-sectional study. J. Infect. Dev. Countries 5 , 711–716 (2011).
Alhasawi, A. et al. Assessing HIV/AIDS knowledge, awareness, and attitudes among senior high school students in Kuwait. MPP 28 , 470–476 (2019).
Chakrovarty, A. et al. A study of awareness on HIV/AIDS among higher secondary school students in Central Kolkata. Indian J. Commun. Med. 32 , 228 (2007).
Katoch, D. K. S. & Kumar, A. HIV/AIDS awareness among students of tribal and non-tribal area of Himachal Pradesh. J. Educ. 5 , 1–9 (2017).
Shinde, M., Trivedi, A., Shinde, A. & Mishra, S. A study of awareness regarding HIV/AIDS among secondary school students. Int. J. Commun. Med. Public Health https://doi.org/10.18203/2394-6040.ijcmph20161611 (2016).
Article Google Scholar
Council, P. UDAYA, adolescent survey, Bihar and Uttar Pradesh, 2015–16. Harvard Dataverse https://doi.org/10.7910/DVN/RRXQNT (2018).
Kumar, P. & Dhillon, P. Household- and community-level determinants of low-risk Caesarean deliveries among women in India. J. Biosoc. Sci. 53 , 55–70 (2021).
Patel, S. K., Santhya, K. G. & Haberland, N. What shapes gender attitudes among adolescent girls and boys? Evidence from the UDAYA Longitudinal Study in India. PLoS ONE 16 , e0248766 (2021).
CAS PubMed PubMed Central Google Scholar
Fan, C., Wang, L. & Wei, L. Comparing two tests for two rates. Am. Stat. 71 , 275–281 (2017).
MathSciNet Google Scholar
Kim, T. K. T test as a parametric statistic. Korean J. Anesthesiol. 68 , 540–546 (2015).
PubMed PubMed Central Google Scholar
Bell, A., Fairbrother, M. & Jones, K. Fixed and random effects models: making an informed choice. Qual. Quant. 53 , 1051–1074 (2019).
Jarrett, R., Farewell, V. & Herzberg, A. Random effects models for complex designs. Stat. Methods Med. Res. 29 , 3695–3706 (2020).
MathSciNet CAS PubMed PubMed Central Google Scholar
Neuhaus, J. M. & Kalbfleisch, J. D. Between- and within-cluster covariate effects in the analysis of clustered data. Biometrics 54 , 638–645 (1998).
CAS PubMed MATH Google Scholar
Kaur, G. Factors influencing HIV awareness amongst adolescent women: a study of slums in Delhi. Demogr. India 47 , 100–111 (2018).
Alene, G. D., Wheeler, J. G. & Grosskurth, H. Adolescent reproductive health and awareness of HIV among rural high school students, North Western Ethiopia. AIDS Care 16 , 57–68 (2004).
CAS PubMed Google Scholar
Oljira, L., Berhane, Y. & Worku, A. Assessment of comprehensive HIV/AIDS knowledge level among in-school adolescents in eastern Ethiopia. J. Int. AIDS Soc. 16 , 17349 (2013).
Samkange-Zeeb, F. N., Spallek, L. & Zeeb, H. Awareness and knowledge of sexually transmitted diseases (STDs) among school-going adolescents in Europe: a systematic review of published literature. BMC Public Health 11 , 727 (2011).
Laguna, E. P. Knowledge of HIV/AIDS and unsafe sex practices among Filipino youth. in 15 (PAA, 2004).
Teitelman, A. M. et al. Partner violence, power, and gender differences in South African adolescents’ HIV/sexually transmitted infections risk behaviors. Health Psychol. 35 , 751–760 (2016).
Oberth, G. et al. Effectiveness of the Sista2Sista programme in improving HIV and other sexual and reproductive health outcomes among vulnerable adolescent girls and young women in Zimbabwe. Afr. J. AIDS Res. 20 , 158–164 (2021).
DeSoto, J. et al. Using school-based early warning systems as a social and behavioral approach for HIV prevention among adolescent girls. Preventing HIV Among Young People in Southern and Eastern Africa 280 (2020).
Ochako, R., Ulwodi, D., Njagi, P., Kimetu, S. & Onyango, A. Trends and determinants of Comprehensive HIV and AIDS knowledge among urban young women in Kenya. AIDS Res. Ther. 8 , 11 (2011).
Peltzer, K. & Supa, P. HIV/AIDS knowledge and sexual behavior among junior secondary school students in South Africa. J. Soc. Sci. 1 , 1–8 (2005).
Shweta, C., Mundkur, S. & Chaitanya, V. Knowledge and beliefs about HIV/AIDS among adolescents. WebMed Cent. 2 , 1–9 (2011).
Anwar, M., Sulaiman, S. A. S., Ahmadi, K. & Khan, T. M. Awareness of school students on sexually transmitted infections (STIs) and their sexual behavior: a cross-sectional study conducted in Pulau Pinang, Malaysia. BMC Public Health 10 , 47 (2010).
Cicciò, L. & Sera, D. Assessing the knowledge and behavior towards HIV/AIDS among youth in Northern Uganda: a cross-sectional survey. Giornale Italiano di Medicina Tropicale 15 , 29–34 (2010).
Glick, P., Randriamamonjy, J. & Sahn, D. E. Determinants of HIV knowledge and condom use among women in madagascar: an analysis using matched household and community data. Afr. Dev. Rev. 21 , 147–179 (2009).
Rahman, M. Determinants of knowledge and awareness about AIDS: Urban-rural differentials in Bangladesh. JPHE 1 , 014–021 (2009).
Siziya, S., Muula, A. S. & Rudatsikira, E. HIV and AIDS-related knowledge among women in Iraq. BMC. Res. Notes 1 , 123 (2008).
Gao, X. et al. Effectiveness of school-based education on HIV/AIDS knowledge, attitude, and behavior among secondary school students in Wuhan, China. PLoS ONE 7 , e44881 (2012).
ADS CAS PubMed PubMed Central Google Scholar
Kotecha, P. V. et al. Reproductive health awareness among urban school going adolescents in Vadodara city. Indian J. Psychiatry 54 , 344–348 (2012).
Dimbuene, T. Z. & Defo, K. B. Fostering accurate HIV/AIDS knowledge among unmarried youths in Cameroon: do family environment and peers matter?. BMC Public Health 11 , 348 (2011).
Kumar, R. et al. Knowledge attitude and perception of sex education among school going adolescents in Ambala District, Haryana, India: a cross-sectional study. J. Clin. Diagn. Res. 11 , LC01–LC04 (2017).
ADS PubMed PubMed Central Google Scholar
Tripathi, N. & Sekher, T. V. Youth in India ready for sex education? Emerging evidence from national surveys. PLoS ONE 8 , e71584 (2013).
Rosenberg, M. et al. Evidence for sample selection effect and Hawthorne effect in behavioural HIV prevention trial among young women in a rural South African community. BMJ Open 8 , e019167 (2018).
Gupta, P., Anjum, F., Bhardwaj, P., Srivastav, J. & Zaidi, Z. H. Knowledge about HIV/AIDS among secondary school students. N. Am. J. Med. Sci. 5 , 119–123 (2013).
Download references
This paper was written using data collected as part of Population Council’s UDAYA study, which is funded by the Bill and Melinda Gates Foundation and the David and Lucile Packard Foundation. No additional funds were received for the preparation of the paper.
Author information
Authors and affiliations.
Ph.D. Research Scholar, Department of Survey Research & Data Analytics, International Institute for Population Sciences, Mumbai, India
Shobhit Srivastava & Pradeep Kumar
Ph.D. Research Scholar, Department of Family and Generations, International Institute for Population Sciences, Mumbai, India
Shekhar Chauhan
Ph.D. Research Scholar, Department of Public Health and Mortality Studies, International Institute for Population Sciences, Mumbai, India
Ratna Patel
You can also search for this author in PubMed Google Scholar
Contributions
Conception and design of the study: S.S. and P.K.; analysis and/or interpretation of data: P.K. and S.S.; drafting the manuscript: S.C., and R.P.; reading and approving the manuscript: S.S., P.K., S.C. and R.P.
Corresponding author
Correspondence to Pradeep Kumar .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Srivastava, S., Chauhan, S., Patel, R. et al. A study of awareness on HIV/AIDS among adolescents: A Longitudinal Study on UDAYA data. Sci Rep 11 , 22841 (2021). https://doi.org/10.1038/s41598-021-02090-9
Download citation
Received : 05 June 2021
Accepted : 29 September 2021
Published : 24 November 2021
DOI : https://doi.org/10.1038/s41598-021-02090-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Case study of a patient with HIV-AIDS and visceral leishmaniasis co-infection in multiple episodes
Affiliation.
- 1 Postgraduate Course of Biology applied to Health, Federal University of Pernambuco, PE, Brazil, [email protected], [email protected].
- PMID: 24213197
- PMCID: PMC4105092
- DOI: 10.1590/S0036-46652013000600010
Abstract in English, Portuguese
Report of a 45-year-old male farmer, a resident in the forest zone of Pernambuco, who was diagnosed with human immunodeficiency virus (HIV) in 1999 and treated using antiretroviral (ARV) drugs. In 2005, the first episode of visceral leishmaniasis (VL), as assessed by parasitological diagnosis of bone marrow aspirate, was recorded. When admitted to the hospital, the patient presented fever, hepatosplenomegaly, weight loss, and diarrhea. Since then, six additional episodes of VL occurred, with a frequency rate of one per year (2005-2012, except in 2008). In 2011, the patient presented a disseminated skin lesion caused by the amastigotes of Leishmania, as identified by histopathological assessment of skin biopsy samples. In 2005, he was treated with N-methyl-glucamine-antimony and amphotericin B deoxycholate. However, since 2006 because of a reported toxicity, the drug of choice was liposomal amphotericin B. As recommended by the Ministry of Health, this report emphasizes the need for HIV patients living in VL endemic areas to include this parasitosis in their follow-up protocol, particularly after the first infection of VL.
RESUMO: Relato de caso de paciente masculino de 45 anos, agricultor, residente na zona da mata do Estado de Pernambuco, diagnosticado com HIV em 1999 e em uso de ARV. Em 2005 foi registrada a primeira ocorrência de LV através do diagnóstico parasitológico a partir do aspirado da medula óssea. À admissão no hospital apresentava-se com febre, hepatoesplenomegalia, perda de peso e diarréia. Desde então houve a ocorrência de mais sete episódios de LV, tendo ocorrido em media, um evento a cada ano (2005-2012 exceto em 2008). O paciente apresentou, em 2011, um quadro cutâneo disseminado, sendo realizada biopsia de pele que evidenciou formas amastigotas de Leishmania no exame histopatológico. Em 2005, o tratamento foi realizado com antimoniato de N-metil-glucamina e anfotericina B desoxicolato, mas desde 2006, devido à toxicidade, o medicamento de escolha foi a anfotericina B lipossomal. Como recomendado pelo Ministério da Saúde, esse relato reforça a necessidade de que os casos de HIV residentes em área endêmica de LV deverão ter inserido em seu protocolo de acompanhamento essa parasitose, principalmente após o primeiro episódio.
Publication types
- Case Reports
- Research Support, Non-U.S. Gov't
- AIDS-Related Opportunistic Infections / diagnosis*
- AIDS-Related Opportunistic Infections / parasitology
- Leishmaniasis, Visceral / diagnosis*
- Middle Aged
- Clinical Ethics Services
- Ethical AI Services
- Custom Workshops
- Medical Student Education
- In the News
- Impact Videos and Stories
- Frequently Asked Questions
- Policies, Disclosures and Reports

Confidentiality in the Age of AIDS: A Case Study in Clinical Ethics
Print this case study here: Case Study – Confidentiality in the Age of AIDS
The Journal of Clinical Ethics, Fall 1993
Martin L Smith, STD, is an Associated in the Department of Bioethics, Cleveland Clinic Foundation, Cleveland, Ohio.
Kevin P Martin, MD is a Child and Adolescent Psychiatrist in the Department of Mental Health, Kaiser Permanente, Cleveland.
INTRODUCTION
AIDS (acquired immunodeficiency syndrome), now in pandemic proportions, presents formidable challenges to health-care professionals. The human immunodeficiency virus (HIV) infection and its related diseases have also raised a number of thorny ethical questions about government and social policy, health-care delivery systems, and the very nature of the physician-patient relationship. This article presents the case of an HIV-positive patient who presented the treating physician, a psychiatrist, with an ethical dilemma. We provide the details of the case, identify the ethical issues it raises, and examine the ethical principles involved. Finally, we present a case analysis that supports the physician’s decision. Our process of ethical analysis and decision making is a type of casuistry,1 which involves examining the circumstances and details of the case, considering analogous cases, determining which maxim(s) should rule the case and to what extent, and weighing accumulated arguments and considerations for the options that have been identified. The goal of this method is to arrive at a reasonable, prudent moral judgement leading to action.
The patient, Seth, is a 32-year-old, HIV-positive, gay, white male whose psychiatric social worker had referred him to a community-mental-health-center psychiatrist for evaluation. He had a history of paranoid schizophrenia that went back several years. He had been functioning well for the last two years as an outpatient on antipsychotic medications and was working full time, socializing actively, and sharing an apartment with a female roommate.
The social worker described a gradual deterioration over several months. Seth had become less compliant with his medication and with his appointments at the mental-health center, had lost his job, had been asked to leave his apartment, and was living on the streets. He was described as increasingly disorganized and paranoid. His behavior was increasingly inappropriate, and he had only limited insight into his condition.
On examination, Seth was thin, casually dressed, slightly disheveled, and with poor hygiene. His speech was spontaneous, not pressured, and loose with occasional blocking. [That is, he spoke spontaneously, he could be interrupted, and his speech was unfocused with occasional interruption of thought sequence.] His psychomotor activity was labile [unstable]. His affect was cheerful and inappropriately seductive, and he described his mood as ”mellow.” He denied having hallucinations, systematized delusions and suicidal or homicidal ideation. He admitted having ideas of reference [incorrect interpretation of casual incidents and external events as having direct reference to himself], was clearly paranoid, and at times appeared to be internally stimulated. He made statements such as: “They’re blaming me for everything,” and “I’m scared all the time,” although he was too guarded or disorganized to provide more detail. His cognitive functioning was impaired, and testing was difficult given his distracted, disorganized state. His judgement was significantly impaired, and his insight was quite limited.
At the time of the evaluation, Seth indiscriminately revealed his HIV-positive status to the staff and other patients. He claimed he had been HIV positive for five years, and he denied that he had developed any symptoms of disease or taken any HIV-related medications. He was not considered reliable, and the staff sought confirmation. After he provided the location and approximate date of his most recent HIV test, the physician confirmed that the patient had been HIV positive at least since the test, about a year earlier.
When asked, Seth stated that the was not currently in a relationship. He appeared to be disorganized and could not name his most recent sexual partner(s). He could not remember whether he had been practicing safer sex and whether he had informed his partners of his HIV positive status.
In addition to the information he obtained during the evaluation, the psychiatrist, by chance, had limited personal knowledge of the patient. Through his own involvement as a member of the local gay community, the psychiatrist had briefly met the patient twice – once while attending an open discussion at the lesbian-gay community center, and later, at a worship service in a predominantly lesbian-gay church. The physician recalled that Seth had seemed to be functioning quite adequately, at least superficially. He was somewhat indiscriminately flirtatious, his behavior was otherwise appropriate, and he did not appear to be psychotic or disorganized in his thinking. He was not overtly paranoid and did not publicly reveal his HIV-positive status.
Through the church, the psychiatrist had also become acquainted with Maxwell and Philip, who were partners in a primary sexual relationship. Before Seth’s decompensation [deterioration of existing defenses, leading to an exacerbation of pathologic behavior], but after he was known to have tested HIV positive, Seth and Maxwell had been lovers. Maxwell left Philip and moved in with Seth for about two months, but then left Seth and returned to Philip around the time of Seth’s decompensation.
The psychiatrist was not privy to details of Maxwell and Seth’s or Maxwell and Philip’s sexual practices. He did not know of the HIV status of Maxwell or Philip, or whether either had ever been tested. In addition, he was unaware of whether Maxwell or Philip know of Seth’s HIVpositive status at the time of Maxwell’s relationship with Seth, or at any time thereafter. During the evaluation, Seth did not recall having met the psychiatrist, nor did he mention his relationship with Maxwell.
Seth agreed to enter a crisis stabilization unit and to resume treatment with antipsychotic medications. Free to come and go at will during daylight hours, he left the unit on day two, failed to return, and was lost to follow-up. His mental status had not changed significantly before he left the crisis unit.
In this case, the physician’s duty to maintain physician-patient confidentiality conflicts with his duty as a psychiatrist to warn third parties at risk. Clearly, a patient’s status as HIV positive is a matter of confidentiality between doctor and patient. Just as clear is the risk for third parties to whom the patient may pass the virus via sexual intercourse. It is unknown whether everyone infected with HIV will develop AIDS, or how many months or years may intervene between infection and the appearance of full-blown AIDS. However, once AIDS develops it is always fatal.2 Therefore, there is a potentially lethal risk to a person having intercourse, particularly without employing safer sex-practices, with another infected with the HIV virus.
This ethical conflict raises two questions. Is it permissible to violate confidentiality to warn a third party at risk? Is there a duty to violate confidentiality to warn a third party at risk? The potential benefit to the third parties must be considered, as well as the strength of the principle of confidentiality in the patient-physician relationship. There is also wider societal consideration as to how breaches of confidentiality, even for good reasons, will affect voluntary testing and seeking of prophylactic treatment by HIV-positive persons. This societal consideration must be weighed against the benefit to the individual third party of knowing the risk and then choosing to be tested and treated and choosing to be tested and treated and choosing to take precautions against infecting others.
In this case, another issue arises from the fact that the physicians of at least one third party who may have been placed at risk possibly without his knowledge, was obtained through personal knowledge, outside the professional relationship. Is it appropriate to bring this information into the clinical setting, particularly because it is so central to the primary ethical issue? Does the physician have an obligation to act on this information?
Finally, two additional sets of issues complicate this case. First, the patient’s decompensation and disappearance necessitate the physician’s choosing a course of action without patient consent or cooperation, and with patient-supplied information that is incomplete and probably unreliable. Second, a breach of confidentiality could greatly damage the physician’s position as a psychiatrist and a trusted member of the gay community, offering assistance directly to some and referral to many others. Given these issues, what should the physician do?
BACKGROUND DISCUSSION
Some background information will be useful in analyzing the ethical issues of the case. This information includes basic ethical values and norms, and legal mandates and opinions about confidentiality, the duty to warn, and HIV/AIDS reporting.
Whether privacy is viewed as a derivative value from the principle of autonomy or as a fundamental universal need with its own nature and importance,3 privacy, and the associated issue of confidentiality, is generally accepted as essential to the relationship between physician and patient. The purpose of confidentiality is to prevent unauthorized persons from learning information shared in confidence.4 Stated more positively, confidentiality promotes the free flow of communication between doctor and patient, thereby encouraging patient disclosure, which in turn should lead to more accurate diagnosis, better patient education, and more effective treatment.
The Hippocratic Oath is evidence of the long-standing tradition of confidentiality in Western though: “What I may see or hear in the course of treatment… I will keep to myself, holding such things shameful to be spoken about.” More recently, the American Medical Association,6 the American Psychiatric Association,7 the American College of Physicians, and the Infectious Diseases Society of America8 have reaffirmed the right of privacy and confidentiality, specifically for HIV-positive patients. Without the informed consent of the patient, physicians should not disclose information about their patient. The Center for Disease Control also recommends that patient confidentiality be maintained, because the organization believes that a successful response to the HIV epidemic depend on research and on the voluntary cooperation of infected persons.9That is, the interests of society seem best served if the trust and cooperation of those at greatest risk can be obtained and maintained.10
Within the complexities of clinical care, should patient confidentiality be regarded as absolute, never to be breached under any circumstances (as claimed by the World Medical Association in its 1949 International Code of Medical Ethics11)? Or should confidentiality be regarded as a prima facie duty? (That is, should it be binding on all occasions unless it is in conflict with equal or higher duties?12)
Most commentators and codes conclude that patient confidentiality is not absolute and, therefore, it could – and even should – be overridden under come conditions.13 In other words, in a specific situation in which patient confidentiality is one value at stake, the health-care provider’s actual duty is determined by weighing the various competing prima facie duties and corresponding values, including confidentiality. (As might be expected, not all authors accept this conditional view of confidentiality and argue for its absolute quality.14) There is less unanimity about the circumstances under which patient confidentiality can be justifiably breached. More specifically for HIV-positive patients, the controversy revolves around the premise that some circumstances might create a duty to warn endangered third parties, even at the expense of confidentiality. The potential for harm to HIV-positive patients through breaches of confidentiality is great. Discrimination, isolation, hospitality, and stigmatization are all too real for these patients when their HIV-positive status has become known to others.15 Further, societal harm is possible if these patients – who might ordinarily seek medical attention voluntarily – refrain from doing so, knowing that professional breaches of confidentiality may ensue. Without ignoring this potential societal harm, the majority opinion of professional codes and of ethical and legal experts16 foresee the possibility of a duty to warn through discrete disclosure, especially if others are in clear and imminent danger if the patient cannot be persuaded to change hi behaviors or to notify those at risk of exposure.
Public health regulations often reflect the same conclusion – that confidentiality can be compromised under certain circumstances – and therefore mandate reporting HIV-positive and AIDS patients to public health authorities. Patient confidentiality is not to be upheld so strictly that it obviates an ethically justified (and usually legally mandated) duty to report such cases to authorized health agencies. Those who support such public policies view society’s right to promote its health and safety, and the need for accurate epidemiological information, to be at least as important as an individual’s right to privacy and confidentiality.
In trying to balance patient confidentiality with other professional values, the California Supreme Court decision in Tarasoff v. Regents of the University of California17 has become a guideline for other courts and health-care professionals (although technically this decision applies to only one state and specifically addresses a unique set of circumstances). In this famous and controversial case heard before the California Supreme Court in 1976, the majority opinion held that the duty of confidentiality in psychotherapy is outweighed by the duty to protect an intended victim from a serious danger of violence. The court explained the legal obligation to protect and the potential duty to warn as follows:
When a therapist determines, or pursuant to the standards of his profession should determine that his patient presents a serious danger of violence to another, he incurs an obligation to use reasonable care to protect the intended victim against such danger. The discharge of this duty may require the therapist to take one or more various steps, depending upon the nature of the case. Thus, it may call for him to warn the intended victim or others likely to apprise the victim of the danger, to notify the police, or to take whatever steps are reasonably necessary under the circumstances.18
Regarding the limits placed on confidentiality under these conditions, the court stated: “The protective privilege ends where the public peril begins.” This “Tarasoff Tightrope” identifies for the professional the dual duties of promoting the well-being and interests of the patient and protecting public and private safety.
Given the general jurisdictional autonomy of each state, the duty to protect and the potential duty to warn as adopted in California has been applied differently in different states.20 Although most commentators assume that Tarasoff is relevant for sorting out the issue of confidentiality relative to HIV-positive patients, this assumption is not universally accepted.21
Without a state statute or court case that specifically addresses the tension between patient confidentiality and the right of others to know whether they may have been exposed to HIV infection, and given the conundrum of legal principles relating to AIDS confidentiality, it is unclear as to who must be warned and under what circumstances.22 This lack of clarity is in indication that, in practice, the professional duty to warn is not absolute but always conditioned by the circumstances of the case (that is, the duty to warn is a prima facie value).
The above paragraphs describe an emerging consensus among health-care professionals who face confidentiality dilemmas, although universal agreement has not been fully achieved. Further, this emerging consensus and its contributing principles by no means provide easy answers to ethical quandaries. Each case, with its own specific set of relevant circumstances, must be analyzed and judged individually. Such an analysis of the presented case now follows.
AN ANALYSIS
Seth’s case, perceived as a dilemma by the psychiatrist, could be brushed aside easily if the information obtained outside the therapeutic relationship was simply ignored. But the lethality of HIV infection makes it difficult to dismiss the information either as irrelevant or inadmissible for serious consideration. Had the information been obtained by unethical means (for example, by coercion or deception), a stronger justification for not using the information might be made. Such is not the situation. Without reason to ignore this information, the psychiatrist must incorporate this “data of happenstance” into his decision. To do so, of course, places him precisely at the crossroads of the dilemma: to uphold confidentiality, to warn the third party, or to create an option that supports the values behind these apparently conflicting duties.
Several factors ethically support both a breach of confidentiality and the physician’s duty to warn and protect the third party: the emerging professional consensus that confidentiality is not absolute; the known identity of a third party who stands in harm’s way; the risk to unknown and unidentified sexual partners of the third party; and the deadliness of AIDS. Such a combination of factors is what the professional statements noted above23 have tried to address in their allowance for limits to patient confidentiality. In this case, the risk to the known third party has already been established, but other people may be at risk, including sexual partners of the patient and those of the third party. Individuals infected and unaware will not benefit from prophylactic therapies.
An additional reason for the psychiatrist to warn the third part is the patient’s mental status, which probably renders him incapable of informing his sexual partner(s) or of consenting to the physician’s informing them. On admission, he was not able to name his partner(s), and he was lost to follow-up without significant change in his mental status. Without the decision-making capacity of the likelihood of action on the part of the patient, any warning to the third party would have to come from the physician or through public health officials notified by the physician.
But the duty to warn, incidental information, and mental status are not the only factors that need to be considered here. Patients are subject to the risks of discrimination when their HIV status is disclosed. But for a patient who has indiscriminately revealed his own HIV-positive status, the physician’s contribution to this risk of discrimination through discreet disclosure to one person may be minimal.
Also, to be considered is the societal risk that testing and prophylactic treatment of HIV-positive persons will decrease if confidentiality is not upheld. Members of the lesbian and gay community are often mistrusting of medical and mental health professionals,24 perhaps with valid reason. Mistrust, fear, and nonparticipation in voluntary programs may increase if confidentiality cannot be assured. Persons will be less likely to come forward voluntarily for education, testing, or other assistance if their well-being is threatened as a result. In Tarasoff, the court declared that protective privilege ends where social peril begins. In this case, overriding the protective privilege of the individual could lead to greater societal peril. Trust in this physician by members of the lesbian and gay community benefits individuals and the community as a whole, by improving access to medical and mental health services. A breach of confidentiality, if it became known, could damage this trust, as well as the physician’s reputation, reducing his professional contributions to the community. This professional loss would be significant.
Also, to be considered is the general knowledge of the higher risk among gay and bisexual men for HIV infection, as well as the information in the gay community as to what constitutes high risk behavior and what precautions can decrease risk of infection. Thus, we can reasonably assume that a gay or bisexual male is already aware of his risk and that of his sexual partner(s) for carrying the HIV virus. Warning a probably knowledgeable third party about the HIV-positive status may be of little benefit to the third party, while it risks the greater individual, societal, and professional harms discussed above. Regarding the risk to unknown sexual partners of the patient, whatever their number, the physician is powerless to change their fate precisely because they are unknown to him.
The duty to maintain patient confidentiality and the duty to warn third parties at risk can both be viewed as prima facie duties. In clinical situations such as the one described here, when one duty must be weighed against another to arrive at an ethically supportable solution, the weighing should take place only in the context of the given case. In this case, we found no solution that upholds all the duties; thus, a choice must be made between the two duties.
We submit that, although there is support for the physician to warn the third party, there is greater support for upholding confidentiality in this case. The individual risk of discriminatory harm from disclosure is possible, although admittedly small. Further, it is reasonable to presume the third party’s awareness of his risk and of the risk to his sexual partner(s) of carrying the HIV virus, and thus, his awareness of the need for appropriate precautions.
Even more persuasive is the peril to the local gay community and the wider society if a breach of confidentiality increases mistrust of the healthcare system and decreases the effectiveness of this particular psychiatrist to provide quality professional care. In this case, the confidentiality of the physician-patient relationship should be maintained.
What has been presented here can serve as a model for ethical decision making within the complexities of clinical care. As cases and their accompanying ethical questions arise, the details of each case should be gathered. Any tendency to label the case prematurely as a particular type (for example, a duty-to-warn case) should be resisted. Such a label can divert attention from relevant details that make each case unique. In examining the facts of the case and judging their significance, the values and duties at stake can be identified. If necessary and practical, background material and analogous cases should be researched. Ethical dilemmas present persons with hard choices. While several solutions may have some ethical support, few can be labeled as perfect solutions. Often, choosing one solution over another leaves behind an ethically significant value and regrettably may even produce harm. The circumstances described here presented the psychiatrist with a hard choice and no easy answer. We have suggested an ethically supported solution, but we found no perfect solution for the dilemma.
1. A.R. Jonsen, “Casuistry as Methodology in Clinical Ethics,” Theoretical Medicine 12 (1991): 295-307. 2. J.W. Curran, H.W. Jaffee, A.M. Hardy, et al., “Epidemiology of HIV Infection and AIDS in the United States,” Science 239 (1988): 610-16. 3. T.L. Beauchamp and J.F. Childress, Principles of Biomedical Ethics (New York: Oxford University Press, 1983). 4. W.J. Winslade, “Confidentiality,” in Encyclopedia of Bioethics, ed. W.T. Reich (New York: Free Press, 1978). 5. L. Walters, “Ethical Aspects of Medical Confidentiality,” in Contemporary Issues in Bioethics,3rd edition, ed. T.L. Beauchamp and L. Walters (Belmont, Calif.: Wadsworth, 1989). 6. Council on Ethical and Judicial Affairs of the American Medical Association, “Ethical Issues Involved in the Growing AIDS Crisis,” Journal of the American Medical Association 259 (1988): 1360-61. 7. American Psychiatry Association, “AIDS Policy: Confidentiality and Disclosure,” American Journal of Psychiatry 145 (1988): 541-42. 8. Health and Public Policy Committee of the American College of Physicians, and lnfectious Diseases Society of America, “A quired Immunodeficiency Syndrome,” Annals of Internal Medicine 104 (1986): 575-81. 9. Centers for Disease Control, “Additional Recommendations to Reduce Sexual and Drug-Related Transmission of Human T-Lymphotropic Virus Type I I1/L y mph adenopathy-Associated Virus,” Morbidity and Mortality Weekly Report 35 (1986a): 152-55. 10. R. Gillan, “AIDS and Medical Confidentiality,” in Contemporary lssues in Bioethics. Code of Ethics, 1949 World Medical Association,” in Encyclopedia of Bioethics. 11. W.O. Ross, The Foundations of Ethics (Oxford, England: Clarendon Press, 1939). 12. Beauchamp and Childress, Principles of Biomedical Ethics; Winslade, “Confidentiality”; Walters, “Ethical Aspects of Medical Confidentiality”; AMA, “Report on Ethical Issues”; APA, “AIDS Policy”; American College of Physicians and Infectious Diseases Society of America, “Acquired Immunodeficiency Syndrome”; S. Bok, “The Limits of Confidentiality,” Hastings Center Re port 13 (February 1983): 24- 31; H.E. Emson, “Confidentiality: A Modified Value,” Journal of Medical Ethics 14 (1988): 87-90. 13. M.H. Kottow, “Medical Confidentiality: An Intransigent and Absolute Obligation,” Journal of Medical Ethics 12 (1986):117-22. 14. R.J. Blendon and K. Donelan, “Discrimination against People with AIDS,” New England Journal of Medicine 319 (1988): 1022-26; L.O. Gostin, “The AIDS Litigation Project: A National Review of Court and Human Rights Commission Decisions, Part II: Dis crimination,” Journal of American Medical Association 263 (1990): 2086-93. 15. G.J. Annas, “Medicolegal Di lemma: The HIV-Positive Patient Who Won’t Tell the Spouse,” Medical Aspects of Human Sexuality 21 (1987):16; T.A. Brennan, “AIDS and the Limits of Confidentiality: The Physician’s Duty to Warn. Contacts of Seropositive Individuals,” Journal of General Internal Medicine 4 (1989): 242-46: B.M. Dickens, “Legal Limits of AIDS, Confidentiality,” Journal of the American Medical Assoclarion 259 (1988):3449-?1; S.L. Lentz. ”Confidentiality and lnformed Consent and the Acquired Immunodeficiency. Syndro111e. Epidemic,” . Archives of Pathology, & Laboratory Medicine 114 (1990):304 8; D. Seiden, “HIV ·Seropositive Patients and Confidentiality,” Clinical Ethics Report (1987): 1-8H.Zomina, “Warning Third 16. Tarasoff v. Regents of the University of California, 11Cat.3d 425,551 P 2d ht (1,976) 17. Ibid. 18. R.D. Mackay, “Dangerous. Patients: Third Party Safety and Psychiatrists’ Duties: Walking the Tarasoff Tightrope,” Medicine, Science & the Law 3Q (1990): 52-56, 19. LA. Gray and A.R. Harding, “Confidentiality Limits with Clients Who Have the AIDS Virus,” Journal of Counseling and Development 6 (1988):219-23. 20. S. Perry, “Warning Third ‘Parties at Risk of AIDS: APA’s Policy is a Barrier to Treatment,” Hospital and Community Psychiatry 40 {1989):’ i5.8-6I. 21. L.O Gostin, The AIDS Litigation Project: A National Review of Court and Human Rights Commission Decisions. Part 1: The Social Impact of AIDS,” Journal of the American Medical Association 263 (1990), ‘961-7Q 22. AMA; “Report on Ethical Issues”; APA, “AIDS Policy”; American College of Physics and Infectious Diseases Society of America” Acquired lmmunodeficiency Syndrome.” 23. L. Dardick and KE Grady, “Openness between·:Gay Persons and Health Professionals,” Annals of Internal Medicine 93 -(1 80): 115-.19; T.A. DeCrescenzo, Homophobia: A Study of the Attitudes of Mental Health Professionals toward Homosexuality. Journal of Social Work and Homosexuality 2 (198):.84): 115-36.
Print this case study here: Case Study – Gathering Information and Casuistic Analysis
Gathering Information and Casuistic Analysis
Journal of Clinical Ethics By Athena Beldecos and Robert M. Arnold
Athena Beldecos is a graduate student in medical ethics in the Department of History and Philosophy of Science, University of Pittsburgh.
Robert M. Arnold, MD is an Assistant Professor of Medicine, and the Associate Director for Education, Center for Medical Ethics, University of Pittsburgh.
In their article, “Confidentiality in the Age of AIDS,” Martin L. Smith and Kevin P. Martin present a complex case in clinical ethics. Their analysis examines a physician’s quandary when treating a mentally incompetent HIV-positive patient: whether to uphold physician-patient confidentiality or to violate this confidentiality by warning a third party. Out critique focuses on the way the problem is conceptualized and the analytic methods used to resolve the case, rather than on the solution itself. We believe that several problems in the authors’ analysis arise from a misinterpretation of the casuistic method. Furthermore, we argue that Smith and Martin present a case that is insufficiently detailed, thereby precluding the identification of all of the moral problems in the case and the development of creature solutions to the problem(s) identified. We note several reasons why there is a need to gather more information prior to determining the appropriate ethical response. Finally, we suggest ways in which similar problems in clinical ethics might be avoided in the future.
IS THIS CASUISTRY?
The authors conceive of their “process of ethical analysis and decision making” as a “type of casuistry.” Although we agree that casuistry, as outlined by A.R. Josen,1 is a potentially fruitful technique for practical ethical decision making, we believe that certain essential features of such casuistic reasoning are not clearly present in Smith and Martin’s analysis.
The power and scope of casuistry are derived not only from attention to details and careful identification of circumstances in the presentation of individual cases, but – more importantly – from the process of case comparison. Using this method, a case under moral consideration is situated in a family of related cases, whereby the casuist examines the similarities and differences between the cases at hand. The context of an individual case and how its conflicting maxims appear within that particular context are the raw materials of the case-comparison method. The relative weight of conflicting maxims in an individual case is ascertained by comparison to analogous cases. With casuistry, moral judgement does not involve a more traditional retreat to the weighing of conflicting duties or general principles. Rather, moral guidance is provided by an ever-growing body of paradigm cases that represent unambiguous instances in which moral consensus is easily obtained. It is crucial that the casuist place the case under consideration in its proper taxonomic context(s) and that she or he identify the most appropriate paradigm, whether it be real or hypothetical.
The authors do identify a paradigm case, but their analysis departs from casuistry on several interrelated points. The authors do not proceed by analogical reasoning. Had they done so, they might have discovered that their chosen paradigm is inappropriate, due to significant dissimilarities with Seth’s case. Finally, their insufficiently detailed case precludes a thorough measurement of the similarities and differences between the cases at hand. For it is in the details that an individual case may differ from a paradigm case.
The authors’ analytic method has more in common with principle-based ethics2 than casuistry. They do not use a variety of similarly situated cases to point out and balance the relevant moral maxims instead, they extract the conflicting duties and principles from their paradigm, the Tarasoff case,3 and apply them directly to Seth’s case. The authors weigh one prima facie duty “against another to arrive at an ethically supportable solution.” Furthermore, the weighing takes place “only in the context of the given case.” Thus, case comparison, an intrinsic element of casuistry, is not performed. Instead, the authors’ major goal seems to be finding and applying a sufficiently modified principle regarding confidentiality to resolve the case at hand.
WHY TARASOFF IS PROBLEMATIC AS A PARADIGM CASE
By using Tarasoff as a paradigm case in their analysis, Smith and Martin situate their case in the family of “duty-to-warn” (prevention-of-harm) cases. It is reasonable that they identify this particular taxonomy as a starting point for their analysis. However, they do not test the appropriateness of the paradigm by systematically comparing and contrasting it with Seth’s case. The authors note the uniqueness of the circumstances of the Tarasoff case and its limited applicability but nonetheless proceed to use it as a paradigm. Casuistry, however, seeks closest-match paradigms. The use of analogical reasoning would have illuminated the similarities and differences between the two cases and would have helped the authors to determine which morally relevant features a paradigm case should minimally share with its analogous cases.
In the Tarasoff case, the court held that a psychotherapist, to whom a patient had confided a murderous intent, had a duty to protect the intended victim from harm.4 This duty includes warning the third party at risk, among other interventions. The unique circumstances of Tarasoff include the imminence of fatal harm to an identified, yet unsuspecting, individual. Although the authors are correct in noting the precedent-setting value of Tarasoff, the dissimilarities between Tarasoff and Seth’s case are so numerous as to suggest the selection of another paradigm.
First, a critical aspect in Tarasoff is the prevention of future fatal harm. Based on the circumstances of the case, there is no evidence of preventable fatal harm to Maxwell. For this condition to be satisfied, the psychiatrist would have to be assured of Maxwell’s seronegativity and have evidence of a current or an intended sexual relationship between Maxwell and Seth. The preventable harm to Maxwell consists of not allowing him the opportunity to institute early anti-viral therapy or to reconsider his life goals in the face of a fatal disease. A casuist would need to assess, using a series of cases, the moral difference between the fatal harm in Tarasoff and the lesser harms in the case of Seth.
Second, Tarasoff involves a person maliciously intending to harm another person. However, there is no evidence suggesting that Seth intended to harm Maxwell. Here, a casuist might begin the analysis using a paradigm case in which a physician is aware of his HIV-positive patient’s malicious intention to infect a third party from that point, one could progressively change the variables of the case to approach the degree of moral ambiguity and complexity shown in Seth’s case. This process would culminate in a case involving sexual relationship between a patient and his partner.
Third, the notion of harm with respect to HIV transmission is quite different from the harm to be prevented in Tarasoff . One might argue that fatal harm to others is averted by informing Maxwell of his risk for HIV positivity. He can subsequently alter his sexual practices and, thus, prevent the future spread of the virus. Herein lies the problem. In Tarasoff the person warned of the harm is also the person at risk of being harmed. In the case under discussion, however, warning Maxwell might prevent harm to other, yet unnamed individuals. A case analogous to Seth’s should describe a situation in which the possible harm has already occurred and the future harm to be avoided consists of preventing future transmission. An analogous case might involve issues of confidentiality in regard to the (vertical) transmission of a fatal genetic disease that manifests itself after sexual maturity. Imagine, for example, a young man afflicted with a severe and incurable genetic disease who has proceeded to start a family without disclosing his genetic status to his wife. Does his personal physician have a duty to uphold confidentiality in this case, or should he notify the spouse so that she can make informed reproductive decisions?
Fourth, in Tarasoff , the victim was presumably unaware of the intended harm. In Seth’s case, one can argue that Maxwell knows (or can be reasonably expected to know) the potential risk of having sexual relations with a homosexual. The authors mention this factor but do not provide a way to assess its importance. To test the importance of this morally relevant fact, a series of cases in which the third party is more (or less) responsible for knowing about the possibility of risk could be used for comparison. For example, how would our intuitions about physician disclosure in this case differ if Seth were a bisexual male who did not inform his wife of his unprotected extramarital affairs with gay and bisexual men?
Fifth, Seth was reported to have publicly announced his HIV-positive status, whereas the patient in Tarasoff disclosed his intent to kill within a protected doctor-patient relationship. Does the fact that “Seth indiscriminately revealed his HIV-positive status to the staff and other patients” at a community-mental-health-center make it easier for the psychiatrist to justify a violation of confidentiality in the name of protecting potential victims? Unfortunately, there is insufficient information to determine whether Seth’s public disclosure qualifies as a fair warning to potential victims and sanctions a violation of confidentiality. This point is potentially an important difference between Tarasoff and Seth’s case. The authors, however, would need to gather additional information concerning the circumstances of Seth’s public disclosures (when they began, to whom they were addressed, and so forth) before evaluating the weight of this morally relevant feature by comparison to a similar case.
Sixth, Tarasoff does not address the issue of how the duty to uphold confidentiality might be affected when a patient’s mental competence is in question. Seth’s case involves a mentally incompetent patient presumed to be “incapable of informing his sexual partner(s) [of his HIV positivity] or of consenting to the physician’s informing them.” The circumstances of this case raise the question: Does Seth’s physician have the same obligation to respect his patient’s confidences as he would have if Seth were a mentally competent adult patient? Central to this analysis is an understanding of how the underlying justifications for respecting the confidences of incompetent patients might differ from those of competent patients. Although the authors briefly discuss the implications of Seth’s impaired mental status, they could have profitably expanded their analysis of the ethical significance of a patient’s competency in regard to the physician’s duty to maintain confidentiality. The authors neglect to discuss, for example, how the selection of a surrogate to speak on Seth’s behalf might influence the case’s resolution.
Identifying which should be the determining factor(s) in deciding Seth’s case is a difficult moral problem. However, the first step is any casuistic analysis is to determine where the case fits in relation to other cases. Without this basic first step, it is too easy to neglect factors that may be critical in determining the proper course of action or to reply upon ad hoc, intuitive decisions.
THE NEED FOR A RICHLY DETAILED CASE
The casuistic method to which Smith and Martin supposedly subscribe, demands attention to the context of the particular case at hand, so that it may be compared to and contrasted with paradigm cases in which the ethical analysis is clear. A casuist needs sufficiently detailed information to be able to identify all of the moral issues and, thereby, situate an individual case in its appropriate taxonomy.
In Seth’s case, the authors seem to decide prematurely on the ethical issue, inappropriately hindering the search for future data. In the rush to identify and resolve the presumed ethical conflict, the ethicist may neglect to collect critical information.5 Without adequate information, the ethicist is unable to determine accurately what kind of case it is. While obtaining more information might be less interesting than theoretical analysis, often the most prudent course of action is to gather more information from the sources available in order to clarify and embellish the initial facts. Prior to leading the psychiatrist through a philosophical analysis of how to resolve the conflict between the duty to warn and the duty to uphold confidentiality, the authors should have urged the psychiatrist to obtain more information.
It is difficult, for example, to weigh the impact of Seth’s mental incompetency against the duty to maintain confidentiality because of a lack of sufficient information. Information regarding the severity of Seth’s mental illness and the chances of its reversibility would be useful in determining whether Seth should be viewed as only temporarily or permanently incompetent. If Seth is incompetent, it is not clear who should assess the harm done to Seth by a breach of confidentiality. We know too little about Seth’s life to determine who would most appropriately serve as his surrogate. Furthermore, it is not clear that violating Seth’s confidentiality would result in the social harms the authors forecast. In order to make this point, the authors would need to identify a case analogous to Seth’s, in which violating an incompetent person’s confidences is ill-advised because it might lead competent patients to mistrust or fear the health-care system.
In the previous section, we identified a variety of morally relevant factors in Seth’s case and suggested how they might affect one’s analysis. Determining the importance of the various factors in this case, however, requires the ethicist to obtain information concerning the following: the efficacy of antiviral treatment in HIV-positive persons, Seth and Maxwell’s sexual practices, the probability that Maxwell knows of Seth’s seropositivity, the degree to which Maxwell can reasonably be expected to know the risk of homosexual encounters, Seth’s previous comments regarding confidentiality, who is best situated to serve as Seth’s surrogate, and the degree to which violating an incompetent patient’s confidentiality will lead other patients to lose trust in physicians and thus avoid the health-care system. Some of this information might be obtained from Seth’s social worker. Other data, however, can be obtained only by reviewing the empirical literature. We admit that much of this information may be unobtainable. Knowing the limits of one’s knowledge, however, will allow an honest appraisal of how uncertainty regarding various factors affects one’s moral decision making. This is preferable to not attempting to ascertain the information at all.
CREATIVE SOLUTIONS
The failure to gather sufficient information often leads to an impoverished understanding of the ethical issues that a case raises. In Seth’s case, the authors present the case as though there were one question: Is it permissible/obligatory to violate Seth’s confidentiality to warn Maxwell? Asked this way, there appears to be only two resolutions to the case: either a physician protects Seth’s confidentiality by failing to warn Maxwell o the risk, or he violates Seth’s confidentiality by warning Maxwell. Upon collection of sufficient data, one might discover ways to resolve the case that would allow all relevant values to be promoted. In some cases, additional information may provide the ethicist with an “end run” around the presumed ethical problem. For instance, if the ethicist learns that Maxwell is already aware of Seth’s seropositivity, then the ethical quandary vanishes. There is strong pedagogical justification for the authors to provide us with sufficient information to conclude that the quandary could have been resolved by seeking additional information and to help us develop innovative solutions that might promote the competing values.
Even if more information does not allow one to avoid the ethical conflict, it may prove useful in determining how best to resolve the case. It is simplistic to view the outcome of ethical analysis as a hierarchical ranking of two competing values or principles. Intermediate solutions often exist, which allow one to respect both competing values. Even in those cases where it is justified to promote one value over another, one is nevertheless obligated to consider alternative courses of action that respect, as much as possible, the other value. The authors neglect an important step in ethical problem solving – attempting to develop creative solutions that, if they cannot perfectly respect all values, at least cause as little damage as possible. This approach, known in American law as “the least restrictive alternative,”6 recognizes that solutions can be more or less respectful of ethical principles. Thus, for example, one might decide that the risk to Maxwell is sufficiently high so that some violation of Seth’s confidentiality is permissible. A variety of options would still be open. (1) The psychiatrist could call Maxwell (or have the public health department do so) and inform him that he may have been exposed to the HIV virus and thus, he should be tested. (2) The psychiatrist could call Maxwell, identify himself as Seth’s physician, and attempt to ascertain what Maxwell knows about Seth’s serostatus and what the nature of their sexual relationship was. That evidence could then be used to determine whether further actions are in order. (3) The psychiatrist could call Maxwell and tell him that he is Seth’s physician, hat he knows of Maxwell and Seth’s sexual relationship, and that Seth is HIV positive. He could then urge Maxwell to be tested. A similar range of alternatives could be developed if one decides that respecting Seth’s confidentiality is the most important value.
PREVENTIVE ETHICS
A final question is simply why this problem arose. If we assume, as the authors do, that “choosing one solution [in an ethical dilemma] over another leaves behind an ethically significant value and regrettably may even produce harm,” we should attempt to prevent ethical dilemmas from occurring.7 However, typically, case discussions focus on how to “solve” the problem at hand without determining how and why the problem arose, and how it might be avoided in the future. As E. Haavi Morreim points out: “Our moral lives are comprised, not of terrible hypotheticals from which there are no escapes, but of complex situations whose constituent elements are often amenable to considerable alterations.”8 The psychiatrist in this case may not have been able to anticipate Seth’s disappearance, but perhaps he could have asked additional questions on his initial encounter to prevent the resulting ethical quandary. For instance, it would have been useful if the psychiatrist had gathered information about Seth’s values and desires prior to his decompensation. Furthermore, if the physician had asked Seth for permission to talk to his friends, whether others knew of his seropositivity, whether the doctor could release this information to Seth’s sexual partners. or to identify his moral surrogate, this additional information could have ameliorated the quandary that subsequently arose.
In the final analysis, we may well agree with Smith and Martin about how the psychiatrist should handle this case. In this article we have tried to criticize not the answer, but the process by which the answer was reached. We urge ethicists who are dealing with a challenging case to use the process of case comparison in their analysis, examining a variety of analogous cases; to seek sufficient information to be able to identify all the moral issues in a case and situate the case in its proper taxonomic family; to attempt to develop creative, “least-restrictive” alternatives to ethical dilemmas; and to determine if there are ways that the ethical problem can be prevented in the future. Close attention to these points is likely to improve ethical decision making in the clinical setting and ethical analyses of cases presented in the bioethics literature.
ACKNOWLEDGMENTS
We would like to thank our friends and colleagues for their helpful comments on this paper: Lisa Parker, PhD; Joel Frader, MD; Peter Ubel, MD; and Shawn Wright. JD, MPH.
1. A.R. Jonsen, “Casuistry as Methodology in Clinical Ethics,” Theoretical Medicine 12 (1991): 295-307.
2. T.L Beauchamp and J.F. Childress, Principles of Biomedical Ethics (New York: Oxford University Press, 1989).
3. 3c. Tarasoff v. Regents of the University of California, 17 Cal. 3d 425. 551 P.2d 334 (1976}.
5. N. Whitman, Creative Medical Teaching (SaIt Lake City: University of Utah School of Medicine, 1990).
6. Lake v. Cameron. 364 F. 2d 657 (D.C. Cir. 1966).
7. L. Forrow R.M. Arnold and L.S. Parker, “Preventive Ethics: Expanding the Horizons of Clinical Ethics:· The Journal of Clinical Ethics (forthcoming).
8. E.H. Morreim, “Philosophy Lessons from the Clinical Sening.” Theoretical Medicine 7 (1986): 47-63.
TARASOFF: Discussion Questions
1. Traditionally, the Tarasoff case pits two goods or values against each other: confidentiality between therapist and patient vs. protection of an intended victim. Why is each a value?
2. Confidentiality is not only a value, but it has been called a duty which is incumbent on health care professionals to maintain secrecy about information gained in the course of interaction with a patient or client. Confidentiality derives from the more fundamental value of autonomy, the right each person has to be one’s own self-decider, one’s own intentional agent.
Protection of an intended victim likewise becomes a duty. To discharge that duty, the court argued, the therapist is obliged to warn the intended victim or others, to notify the police, or to take steps which are reasonably necessary to guard the intended victim.
Formulate an argument that supports the duty of confidentiality over the duty to warn an intended victim. Then formulate an argument which supports the duty to warn over the duty to protect confidentiality. (Being able to make good cases for each of the values shows the ambiguity involved here. Bring into your arguments the issue of the foreseeability of violence (is violence clearly foreseeable, probably foreseeable or unforseeable?) and the element of control over the patient by the therapist.)
3. One can easily use the Tarasoff decision to show the two principal ways of argument, consequentialist and non-consequentialist. Formulate an argument from a utilitarian (consequentialist) perspective, i.e., emphasize risk over benefit in arguing for safety and again, in arguing for confidentiality.
Next, consider confidentiality and the right to be protected as goods in themselves, regardless of consequences. Show how each value is tied to the meaning of being human and indicate how such a value can be argued for without consideration of consequences.
4. Notice how the arguments being proposed by the committee deny the absolute nature of either value. Rather, the committee is attempting to justify an action that is indicated in favor of one value over another, while acknowledging that both values are human goods. How would one attempt to argue when faced with the position that confidentiality or protection were absolute values?
Further Readings
Beauchamp, Tom and LeRoy Walters (eds.) 1994. “The Management of Medical Information” in Contemporary Issues in Bioethics. Fourth Edition. Belmont, CA: Wadsworth:123-186.
Kleinman, Irwin. 1993. “Confidentiality and the Duty to Warn.” Canadian Medical Association Journal 149: 1783-1785.
Perlin, Michael L. 1992. “Tarasoff and the Dilemma of the Dangerous Patient: New Directions for the 1990’s.” Law and Psychology Review 16: 29-63.
Loading metrics
Open Access
Peer-reviewed
Research Article
Process evaluation of the HIV+D intervention for integrating the management of depression in routine HIV care in Uganda
Roles Conceptualization, Formal analysis, Methodology, Writing – original draft
* E-mail: [email protected]
Affiliation Medical Research Council/Uganda Virus Research Institute & London School of Hygiene and Tropical Medicine Uganda Research Unit, Mental Health Research Unit, Entebbe, Uganda
Roles Validation, Writing – review & editing
Roles Methodology, Project administration
Roles Methodology, Supervision, Writing – review & editing
Affiliations Medical Research Council/Uganda Virus Research Institute & London School of Hygiene and Tropical Medicine Uganda Research Unit, Mental Health Research Unit, Entebbe, Uganda, Butabika National Referral Mental Hospital, Kampala, Uganda
Roles Investigation, Supervision, Writing – review & editing
Roles Conceptualization, Supervision
Affiliation Mental Health Division, Ministry of Health, Kampala, Uganda
Roles Conceptualization, Funding acquisition, Resources
Roles Conceptualization, Resources, Supervision
Affiliation Department of Global Health and Social Medicine, Harvard Medical School, Boston, Massachusetts, United States of America
Roles Conceptualization, Funding acquisition, Project administration, Supervision, Validation
- Joshua Ssebunnya,
- Rutakumwa Rwamahe,
- Richard Mpango,
- Leticia Kyohangirwe,
- Christine Tusiime,
- Hafsa Sentongo,
- Pontiano Kaleebu,
- Vikram Patel,
- Eugene Kinyanda

- Published: June 4, 2024
- https://doi.org/10.1371/journal.pmen.0000009
- Peer Review
- Reader Comments
HIV/AIDS continues to be one of the leading global health challenges, having claimed over 40 million lives so far. People infected with HIV are more likely to develop depression, leading to several negative behavioural and clinical outcomes. Studies have reported exceptionally high prevalence of depressive symptoms among people living with HIV/AIDS (PLWHA), making a case for integrating mental healthcare in routine HIV care. The HIV+D program was implemented in Uganda as an intervention model for integrating the management of depression in HIV care. Process evaluation was carried out to understand the contextual factors and explain the outcomes of the intervention. This was a qualitative study, conducted in 28 out of the 40 public health facilities in 3 districts, where the intervention was undertaken. A total of 82 participants, including the implementers and beneficiaries of the intervention were purposively selected for key informant interviews and focus group discussions. Conventional content analysis was done focusing on 6 aspects including reach, effectiveness, acceptability, implementation fidelity, maintenance (sustainability) and contextual factors that affected the intervention. The intervention was well received and believed to address a real need of the intended beneficiaries; many of whom described it as a program for helping the depressed PLWHA to deal with their depression. The implementers were said to have adhered to the intervention protocol, without major program adaptations, suggesting strong implementation fidelity. The respondents cited several positive health outcomes that resulted from the intervention, for both the beneficiaries and the implementers. Several contextual factors affected the implementation. Although it met the beneficiaries’ approval, and was considered relevant and acceptable, they expressed uncertainty over sustainability of the intervention in a health system characterized by understaffing, resource constraints and several other challenges. The intervention was generally implemented as intended, resulting in several positive health outcomes.
Citation: Ssebunnya J, Rwamahe R, Mpango R, Kyohangirwe L, Tusiime C, Sentongo H, et al. (2024) Process evaluation of the HIV+D intervention for integrating the management of depression in routine HIV care in Uganda. PLOS Ment Health 1(1): e0000009. https://doi.org/10.1371/journal.pmen.0000009
Editor: Justus Uchenna Onu, Nnamdi Azikiwe University, NIGERIA
Received: December 11, 2023; Accepted: March 17, 2024; Published: June 4, 2024
Copyright: © 2024 Ssebunnya et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: De-identified data from which this manuscript has been produced will be made available upon request, but the full data set may not be shared due to the qualitative and potentially identifiable nature of the raw data (eg, transcripts). Request for data access should be made to the UVRI – REC Chairperson: Mr. Tom Lutalo, [email protected] and committee member, Mr. Wilber Ssembajjwe, [email protected] .
Funding: The study was supported by an unrestricted grant from the Wellcome Trust through a Senior Research Fellowship in Public Health and Tropical Medicine to EK, reference number 205069/Z/16/Z. The funders had no influence on the design or conduct of the study and were not involved in data collection or analysis, in the writing of the manuscript, or in the decision to submit it for publication.
Competing interests: The authors have declared that no competing interests exist.
Introduction
HIV/AIDS is one of the most devastating illnesses that humans have ever suffered. It remains a major public health issue impacting communities all over the world, having claimed over 40 million lives so far, and with an estimated 39 million people living with HIV globally, as at the end of 2022 [ 1 ]. Eastern and Southern Africa, an under-resourced region with significant health system constraints [ 2 ], remains the region most heavily affected, with an estimated 20.6 million people living with HIV [ 1 , 3 ]. Several studies have shown that depression is one of the most common comorbid conditions in people infected with HIV, with approximately 8–50% of persons living with HIV reported to have suffered from depressive disorders [ 4 – 8 ]. In Uganda, a recent meta-analysis found a pooled depression prevalence of 28.2% among people living with HIV/AIDS (PLWHA), nearly ten times higher than the prevalence estimates in the general population [ 9 ].
Depression in PLWHA worsens the existing disease states, as it not only affects the quality of life [ 10 ], but has been associated with poorer health outcomes such as hastening the progression to AIDS [ 11 – 13 ], poor adherence to HIV treatment, risky sexual behaviour and increased utilization of health facilities [ 14 – 16 ] and elevated risk of mortality [ 5 , 17 ]. Although an estimated 76% of the PLWHA globally are on antiretroviral (ARV) treatment, the majority of HIV care providers in sub-Saharan Africa do not routinely provide mental health services to address the problem of depression [ 3 ]. However, there is growing evidence of specific treatments for depression among PLWHA, associated with anti-retroviral therapy (ART) adherence and reduced HIV disease progression [ 18 – 20 ]. This makes a case for integrating such treatments in routine HIV care [ 21 – 23 ].
With an estimated 1.4 million people living with HIV/AIDS in Uganda, studies have reported exceptionally high prevalence of depressive symptoms among PLWHA, posing a major challenge in HIV care, despite the success in the scale up of anti-retroviral therapy. This consequently increases mortality [ 14 , 24 ]. To address the absence of mental health care in HIV programs, the Uganda National HIV and AIDS Strategic Plan (2020/21–2024/25) called for the integration of mental health and other chronic conditions in HIV care so as to further improve the quality of care and treatment. In a similar vein, the 2016 Ministry of Health policy initiative and guidelines called for the assessment and management of depression in PLWHA [ 25 ].
In response to the above calls, the Mental Health Section of the Medical Research Council (MRC)/Uganda Virus Research Institute (UVRI) & London School of Hygiene and Tropical Medicine (LSHTM) Uganda Research Unit, in partnership with the STD/AIDS Control Program of the Ministry of Health, Uganda Implemented the HIV+D intervention model. This was a 5 year project implemented in 3 districts within Uganda. The intervention model consisted of psychoeducation, Behavioural Activation, antidepressant medication and referral to mental health workers; delivered in a stepped care fashion. The therapies have previously been shown to be effective against depression in primary care settings including in HIV care [ 26 – 29 ].
Process evaluation, which is carried out during or after the intervention to evaluate and explain the outcomes has become a dominant part of clinical trials [ 30 ]. It focuses on how and why the intervention works or does not work in the context of the trial [ 31 , 32 ]. Process evaluation is critical for interpreting the outcomes of trials of complex interventions and aids in the understanding of contextual factors associated with intervention and implementation effectiveness; which can influence potential replication in different settings as well as scale up [ 33 , 34 ].
It is on this basis that we set out to conduct a process evaluation for the HIV+D intervention.
The aim of the study therefore was to assess and report results of the process evaluation of the HIV+D intervention. This was deemed necessary so as to understand whether the intervention was implemented as intended and received similarly across all sites; and to understand the variation in outcomes, breadth and depth in effectiveness; thereby differentiating intervention failure from implementation failure. The process evaluation would justify any variability in the intervention outcomes and inform strategies to integrate the management of depression in HIV care.
Overview of the intervention
The HIV + D intervention model was based on therapies that have been shown to be effective against depressive disorder in primary care settings including in HIV care, namely: psychoeducation, behavioural activation-the Healthy Activity Program (HAP) [ 29 ] and antidepressant medications [ 27 ]. These were delivered in a stepped care format and overseen by an HIV counsellor (Lay Health Worker). Recruitment of participants in the study started on Monday 3rd May 2021 and ended on Friday 31st December 2021.
Recruitment would start with a health talk about depression, given by a trained Lay Health Worker (LHW) to PLWHs sitting in the triage area of the participating Public Health Care Facilities. Thereafter, consecutive attenders would be approached and requested to be screened for the study. The screening would be done by the trained LHW using the PHQ-2 (a two-item questionnaire that assess for ‘depressed mood’ and ‘loss of interest in typically pleasurable activities’). Those screening positive (PHQ-2 score ≥ 3) would be invited for further evaluation by the trained LHW for trial eligibility and consent. The eligibility assessment would include confirmation of depressive symptoms using the PHQ-9 tool [ 35 ]. The eligible respondents would be recruited into the intervention. Those with suicidal ideation (endorsing item 9 on the PHQ-9) would immediately be referred to the supervisor for further assessment and then referral to a mental health specialist (Psychiatric Clinical Officer) for further management.
The intervention was delivered in 4 steps. Step 1: (initiation of treatment), patients with PHQ-9 scores of 10–19 would be told of their scores and offered psychoeducation by a LHW. Step 2: (management of moderate to severe cases), patients who remained symptomatic at follow up (PHQ-9 score ≥ 5 after 4 weeks) would be offered Behavioural Activation (BA); 4–10 bi-weekly sessions) by a LHW. Step 3: (monitoring outcomes), if after 6 sessions of BA, one still scored 10 and above on PHQ-9, they would continue BA sessions to completion and add antidepressant medication (Fluoxetine 20 mg/day for 6 months), initiated by the HIV clinician. Step 4: (referral to mental health worker), if there was no improvement (PHQ-9 ≥ 5) after step 3 or at eligibility assessment PHQ-9 ≥ 20, or if someone had a moderate to high suicide risk (based on suicide risk assessment by the supervisor), they would continue all existing treatment and be referred to a mental health worker. This is summarized in the appended CONSORT flow diagram ( S1 Fig ) and CONSORT checklist ( S1 Checklist ).
The interventions were delivered to the recruited PLWHA in the intervention sites, while those in the control sites received enhanced usual care following mental health Gap Action Plan (mhGAP) treatment guidelines. Full details of the intervention are described elsewhere in the HIV+D protocol paper, appended as supporting information ( S1 Text ) [ 36 ].
Conceptual framework for implementation outcomes
The process evaluation was designed in line with the MRC guidelines for process evaluations [ 30 ]; specifically using the RE-AIM framework [ 37 ]. This is a framework that guides planning and evaluation of programs, focusing on 5 key dimensions: (i) reach (the extent to which the intervention was received by the targeted group), (ii) efficacy/effectiveness (effects of the intervention on health outcomes), (iii) acceptability (extent to which participants found the intervention relevant, acceptable and satisfactory), (iv) implementation fidelity (extent to which the intervention was delivered as planned), (v) maintenance (extent to which the intervention can be integrated within the existing structure and sustained over time). Thus, in this paper, we report on the above 5 implementation outcomes, which formed the basis of our process evaluation. Although not part of the framework, we also report on context (environmental aspects of the intervention setting) as an additional dimension that has been acknowledged as a key dimension [ 32 ].
The specific objectives of the study were thus:
- To assess and determine the extent to which the intervention reached the target group.
- To document the effects of the intervention on the health outcomes in the target population.
- To determine the extent to which the participants found the intervention relevant and satisfactory.
- To determine the extent to which the intervention was implemented as intended across the different intervention sites.
- To explore the perceived sustainability and integration of the intervention within the existing HIV care system
- To describe the contexts in which the intervention was delivered and explore contextual factors that have influenced the delivery and outcomes of the intervention.
The HIV+D program was implemented in 40 public health facilities, which were randomly selected across the 3 study districts of Wakiso and Masaka (semi-urban and rural), and Kalungu (predominantly rural). These are all in central Uganda. All the facilities were running active HIV/AIDS clinics. This process evaluation was a qualitative study, conducted in 28 of the 40 public health facilities (14 intervention sites and 14 control sites) between June 2021 and April 2022.
Study participants and sampling
We set out to conduct the process evaluation in all the 40 health facilities and involve purposively selected participants who could provide in-depth and detailed information on the topic under investigation. These included the health workers who delivered the intervention, the study data collectors, lay health workers, persons living with HIV/AIDS and carers (treatment supporters). However, the data collection went on until we reached saturation and further data collection was deemed redundant; after covering 28 health facilities, with a total of 82 participants.
Data collection
Data was collected through key informant interviews (KIIs) and focus group discussions (FGDs) to understand the context and process, characteristics of the intervention, effectiveness, facilitating factors and challenges from the perspective of different stakeholders. An interview guide with items covering these aspects was developed for this purpose. A total of 58 KIIs and 6 FGDs were conducted with the different stakeholders, as summarized in Table 1 below. All interviews and FGDs were audio-recorded. The interviews with health workers and data collectors were conducted in English, while those with the LHWs, PLWHA and carers were conducted in Luganda (the local language) and translated during the transcription. The transcription and translation were done by the first author and one of the research assistants, both being very conversant with the 2 languages, and having strong experience in qualitative data collection methods.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmen.0000009.t001
Data analysis
After the transcription, conventional content analysis was done by the 2 researchers who have expertise in qualitative research and data analysis, to ensure rigour. They subjectively interpreted the content of the transcripts through coding and identifying themes [ 38 , 39 ]. The initial coding of the transcripts was undertaken by the first author, guided by predefined themes and sub-themes derived from the study objectives. These were amended along the way based on the transcription data. The coded transcripts were shared with the first co-author for common interpretation, improvement and consensus. A data analysis matrix sheet was then used to generate a concise summary of the key results.
Ethical considerations
Ethical approval was obtained from the UVRI Research and Ethics Committee (07 th April, 2020), the LSHTM Ethics Committee (17 th September, 2020) and the Uganda National Council for Science and Technology (ethical clearance number: HS645ES) (07 th July, 2020). All study participants gave written informed consent to participate in the study.
The results are presented below, under 5 themes: effectiveness, acceptability, implementation fidelity, maintenance (sustainability) and contextual factors that affected the intervention. Given the study design, it was not possible to meaningfully assess “reach”.
Acceptability
The key implementers for the program at the primary health care facilities included health workers (clinical staff), lay health workers (members of the Village Health Teams), data collectors. Some of the respondents could not give a very precise description of the program, but indicated that it was a program for treating depressed PLWHA. The non-health care professionals (LHWs and data collectors) termed it as “a program for helping PLWHA who were depressed to deal with their depression, as part of their HIV treatment program, so as to live positively.”
It emerged that the counselling provided in the routine HIV clinics mostly focused on the importance of adherence to treatment (taking ARVs), rarely addressing the clients’ psychosocial concerns and depressive feelings. However, the PLWHA reiterated that under the HIV+D intervention, they received a kind of counselling they had never received before, which helped them dealing with their psychosocial problems; although many did not know that depression is an illness; and its term in the local language was not familiar to them.
Aspects of acceptability included the respondents’ level of interest in the HIV+D program and perceptions about its relevance and usefulness as well as the level of satisfaction. The intervention and its content met the respondents’ approval, and was generally considered relevant and acceptable. The participating health workers and supervisors commented on the appropriateness of the intervention, affirming that the program addressed a real need of the target population and was much needed, given the agony, health and socio-economic challenges associated with being HIV positive. They further reported having a sense of contentment that the intervention provided for helping the depressed PLWHA more meaningfully. On the other hand, some of the PLWHA admitted that at the time of this intervention, they were still struggling to come to terms with their HIV status; and the program had greatly helped them in this aspect. There were reports of increased awareness and recognition of depression as a common health problem among PLWHA, for which they ought to seek help. One PLWHA stated:
“… Before , it was like I was in my own world , because of my HIV status . I had nothing to do to earn some money . It also seems there was another disease , inside me and I had so many thoughts … so many questions … || … I was taking the medicine (ARVs) but it wasn’t working for me … and that was mentioned by the health workers , that if you have so many thoughts , the medicine you’re taking will not work for you . Personally , I was depressed and doing badly ” (KII 40, PLWHA, Busawamanze HC III).
A health worker affirmed:
“… at first they did not even know that depression is an illness , some would tell us : ‘Nurse I did not know that to feel like this , it’s an illness . Someone can have problems , move with them every day but does not know that it is an illness’ . So patients got to know that there is a solution to those problems and one does not have to be depressed .” (FGD 06, health workers, Busawamanze HCIII).
The respondents across the different health facilities gave reports indicating high levels of patient satisfaction with the service. For example, one supervisor said:
“… Someone comes and say “nurse you have helped me a lot . Those things sessions that been through have helped me understand myself , I feel better . It means that the patient is appreciative and feels helped , I am satisfied and feel it ” (Respondent 1, FGD 02, Supervisors).
Patient satisfaction was further confirmed by the fact that some of the PLWHA and carers identified and referred fellow PLWHA in their communities, whom they believed to be depressed, for recruitment into the program. Similarly, the health workers at the facilities offering the intervention reported an increase in the number of clients seeking treatment at these facilities, attracted by the program.
Implementation fidelity
According to the protocol, the implementation would start with a health talk on depression, delivered by a lay health worker, followed by screening for depressive symptoms. The screen positive would be further subjected to an eligibility assessment to confirm the depressive symptoms before consenting for enrollment. In their accounts, most respondents affirmed that screening for depressive symptoms would be done using the PHQ-9, followed by testing for eligibility before recruitment into the program. The screen positives would initially receive psychoeducation and those whose symptoms persisted be recruited to receive Behavioural Activation therapy, which was the main intervention for the program. These would attend bi-weekly BA sessions until full remission of the symptoms. At the control sites, they would assess for depression and any other physical condition such as high blood pressure and then give medication accordingly; though not giving the clients much time, as was the case at intervention sites. However, there were some variations and confusion in some of the respondents’ description of the intervention design and components, as they seemed to confuse the procedure and order of the steps and to confuse the initial health talk that would be given, with psychoeducation which was offered as part of the therapy.
It was noted that at all health facilities, the implementers duly adhered to the intervention protocol, conducting the activities according to the plan, without major program adaptations or alterations of any critical components relating to the content, activities or delivery of the program. The process evaluation thus revealed strong implementation fidelity.
Effect of the intervention on health outcomes of the target population
The intervention was said to have been delivered with excellent facilitation skills, enthusiasm and positive attitude across the implementation sites, which resulted in positive outcomes. It was noted that the intervention resulted in increased awareness and recognition of depression as a health problem, awakening the health workers’ awareness to focus beyond presenting complaints and symptoms while handling patients.
Apparently many of the PLWHA with depressive symptoms did not know that they were having a health problem that warranted clinical intervention. The health workers on the other hand confessed that they were previously not offering adequate help because they were less confident in assessing for depression, and did not give it consideration, as reflected in the quote below:
“… we the health workers did not know these symptoms . We were not assessing the clients for depression because we did not have that knowledge … and we did not know it was important anyway ” (KII 46, Health facility manager/supervisor)
The intervention was reported to have resulted in increased competence and confidence to detect and treat depression associated with HIV or any other causes. Similarly, the health workers appreciated the importance of giving the patients more time and conducting a detailed assessment to inquire about patients’ psychosocial problems.
“… What I observed in this study if you have not talked to the person you cannot know what they are going through but when you talk with them at length , you discover that people have problems . You watch the person coming in to the clinical room as usual things seem normal but if you start a conversation with that person and give him/her time , you find that they are depressed ” (Respondent 2, FGD 01, study supervisors).
Another health worker echoed:
“… even us health workers in ART clinic , we were not emphasizing depression treatment so much . We would only ask them about how many tablets the patient is left with . And if one is not the taking medicine , we only asked “why” , but we could not go deep to find out whether the client is depressed or not ” (KII 44, Health worker)
It was reported that by design, the intervention strengthened the bond between the health workers and PLWHA, resulting in improved Patient-Health worker relationship, empathy and compassion. The improved relationship was said to have contributed to increased disclosure by the PLWHA to the health workers as well as the family members, for those who were living in denial or struggling to keep their HIV status a secret, resulting in increased adherence to treatment. This is reflected in the voices below:
“… Before [the intervention] , we would come to the facility but never got a chance to sit with a health worker to talk like we are doing now . O . k the nurse would ask whether you have anything bothering you , whether you are taking the medicine …. but doing so in a rush . You could see that she is after clearing the long queue . So , it would be hard to disclose important information ” (KII 054, PLWHA, Mpugwe HCIII).
One health worker also affirmed:
“… So , because of the good relationship we have now , they don’t miss on their appointments . And sometimes a client comes just to greet you . But before [the intervention] , that could not happen for a patient to come and say “nurse I have this problem” the moment you give them medicine , they would just walk away . Sometimes this patient may be going through hardships and you the health worker can never know about it unless the patient discloses ” (Respondent 01, FGD 06, PHC workers)
The PLWHA anticipated that the improved relationship they developed with the health workers in the course of the program would be an opportunity to leverage on and serve as a potential buffer against likely psychosocial problems long after the project.
The health workers at various health facilities reported an increase in prescription and consumption of the anti-depressant medication, which would previously expire at some of the facilities. Consequently, there was a reduction in the depressive symptoms among the beneficiaries. This was further exemplified by the significant drop in the clients’ PHQ-9 scores on the subsequent visits.
One of the remarkable outcomes reported was the improvement in adherence to treatment and positive living. Some of the PLWHA confessed that they previously deliberately defaulted on treatment and could not see the point in continuing with medication that would not lead to absolute healing. However, they had resumed taking their ARVs following the intervention.
“… before this program , I would come pick the medicine , but I was not taking it … would just keep it home waiting for death …. || … when I came and had a health talk with the health worker , I went home picked the tins of medicine and brought them back to the health facility . I confessed that I was not taking the medicine . Actually some tins had expired , so they were thrown away . But now , am taking the medicine and have not skipped even a day ” (KII 054, PLWHA, Mpugwe HCIII).
It emerged that for some PLWHA, defaulting on taking their ARV medication was driven by their suicidal ideation, wishing they could die in the process. Indeed, some of them shared testimonies indicating how they had contemplated suicide at some point, because of their HIV status and how they had deliberately defaulted on ARV medication, hoping it would be an easy gateway to death without having to use the more obvious means of committing suicide. There were reports of several PLWHA who were previously very depressed and contemplating suicide, but had improved tremendously following the intervention.
Another key outcome proving the efficacy of the intervention relates to the reported noticeable increase in viral load suppression among PLWHA at several health facilities. The health workers reported on several cases of PLWHA who had failed to suppress the viral load despite taking their ARVs for some time, but were able to achieve the suppression in the course of this intervention.
The respondents also cited some noteworthy unintended effects of the intervention. One such effect was the gain in terms of capacity building for the lay health workers who were trained in delivering BA intervention. They affirmed that delivering the intervention was in some way a learning experience for them as well, having acquired more knowledge and skills in counselling in the process, which could potentially enable sustainability of the intervention.
One such effect was the reported improvement in the welfare of some PLWHA, attributable to the small financial support they received as transport refund whenever they attended therapy sessions. One respondent revealed:
“… There are some two women in their 50s who said they had given up on life . One of them said ‘this money they give us , now I was able to buy a hoe or shoes . Because previously , I was walking bare-footed . I was even able to buy cups and plates for the home . Previously , one would have to take tea and wash the cup so that another one can also take . We did not have enough cups and plates . We would get maize from the garden , cook it and put on banana leaves and take water as soup . But you have helped us a lot . Now everyone has a plate and a cup’ . So , you realize that the program has helped this person financially ”. (KII 028, Expert Client, Kyanamukaaka HCIV).
Sustainability
The health workers were optimistic that the intervention could be adopted and incorporated into the existing HIV/AIDS care system. However, they expressed uncertainty over continuity of the intervention and sustainability of the gains, due to challenges such as understaffing and resource constraints. The PLWHA and carers too were skeptical that the quality of service would remain the same under the mainstream health care system, given the resource requirements. They thus maintained that adoption of such an intervention would necessitate scaling up of the staffing in light of the fact that the intervention entails health workers giving patients adequate time. The health workers further expressed willingness to continue delivering the intervention even after the end of the trial.
Contextual factors
The context and mode of operation at all the health facilities was generally the same, save for some difference in the staffing levels. However, several contextual factors relating to health worker’s attitude and skills, resources, organizational norms etc affected the implementation and the outcomes.
The respondents affirmed that the intervention addressed an actual need and was long overdue. The PLWHA and carers specifically commented on the humility, compassion and the positive attitude of the health workers who delivered the intervention as key facilitating factors that enabled smooth running of the intervention. The warm patient-health worker relationship has been key in fostering adherence and recovery. This was further backed by teamwork and a good working relationship that the implementers exhibited.
According to the health workers, the training they received to deliver the intervention was thorough, backed by close supervision by other project staff, which enabled them to appreciate the intervention well. In addition, they showed commitment towards the work, and were motivated by the incentive; thereby giving the program adequate time.
The transport refund given to the PLWHA recruited into therapy was also cited as a major motivating factor for patients’ attendance. Apparently, many of them previously did not show interest to turn up for the counseling sessions in the routine HIV care. Relatedly, it was reported that the beneficiaries of the intervention (PLWHA) had high expectations, in terms of material support at the time of recruitment. This was believed to have influenced their compliance and consistence in attending the therapy sessions.
There were also a few contextual factors that negatively affected implementation. Most notable of these was the nearly 2 years of Covid-19 lockdown characterized by high levels of anxiety, restriction of movement and disruption of work and people’s lives. Implementation was mostly around that timing, and necessitated conducting some of the therapy sessions on phone.
Like in any study setting, there was a limit on the number of clients to recruit at the health facilities, to a maximum of 30 PLWHA. According to some of the respondents, the limit meant leaving out some other potentially depressed clients who would actually have benefited from the service.
One major challenge in the implementation of the intervention was to do with the screening and testing clients for eligibility. It emerged that by design, the program involved too much paperwork right from assessment of individuals for eligibility, recruitment into therapy and other processes. This was considered to be practically cumbersome if the intervention is to be replicated or rolled out under normal circumstances (outside a research study context).
“… we talked about the long questionnaires … time . Some of the patients would get impatient . And our patients would always want their visits to coincide with the day for picking their drugs . Time was a major concern ” (FGD 02, Health workers, Bukakata HC III)
Related to the above, there was a possible risk of some of the PLWHA answering questions just for the sake, when already tired of the so many questions, thereby giving wrong information. Furthermore, some of the lay health workers and expert clients thought the idea of using screening tools in recruiting clients into therapy was superficial, arguing that all PLWHA have psychosocial problems and ideally should benefit from the service.
The HIV+D process evaluation findings indicated that the intervention reached the target population and was generally implemented and received as intended. Most stakeholders described the intervention as “a program for helping PLWHA who were depressed to deal with their depression”; an indicator that they were clear about the goal of the intervention and the target population. Importantly, the PLWHA acknowledged the fact that they received a form of counselling quite different from the usual HIV counselling delivered in the HIV clinics. The fact that most of them initially did not consider depression to be an illness is of particular concern, as it has implications on the likelihood of seeking help.
The intervention received approval from the implementers (health workers) as well as the recipients (PLWHA and carers); who considered it to be acceptable and very necessary. Importantly, several respondents, including health workers believed that all PLWHA would ideally benefit from the intervention in light of the fact that acquiring HIV can be a serious psychological trauma, predisposing one to psychological distress and different mental disorders [ 40 , 41 ]. This was further confirmed by health workers who cited several examples of PLWHA who earlier on seemed to be doing well, but turned out to be harboring serious distressing problems which were unearthed during the therapy sessions, much to the surprise of the health workers. This could be one reason why at the time of this evaluation, most respondents wished for continuity of the program and expressed disappointment to learn of its impending closure.
Fidelity was a function of the implementers and encompassed both the quality and quantity of delivery [ 42 ]. As earlier noted, not all respondents could accurately describe the intervention and give a perfect narration of how it was implemented from the onset. However, their summative description indicated that the health workers endeavoured to comply with the procedure and activities as set out in the intervention protocol, with no significant adaptations.
It is worth noting that both the implementers and recipients of the intervention expressed concern over the much paperwork involved, especially in the screening and recruitment process. While this was a procedural requirement as per the design of the intervention, and also important for scientific rigor (for the research aspect), it may be rather cumbersome and not practically viable in the normal clinical setting. Indeed, this emerged as one of the challenges encountered during the implementation, and would need to be considered critically while making arrangements for scaling up the intervention.
Some of the health workers cited some examples of PLWHA who disclosed during the therapy sessions that they had earlier contemplated suicide because of their HIV status, but had not responded affirmatively to the suicide item during the assessment. Several earlier studies have asserted that suicidal behaviours are much more pronounced in PLWHA [ 43 – 46 ], citing the relationship between HIV-related stigma, depression and suicidal ideation among PLWHA [ 47 ]. This therefore speaks to the likely concealment of the suicidal ideation during the screening and the need for thorough assessment so as to respond and intervene appropriately. One of the striking findings was the revelation by some of the PLWHA, that they deliberately defaulted on their ARV medication, with the ulterior motive of dying in the process. Several studies have found PLWHA to have a higher likelihood of suicidal ideation due to a significant burden of disease they have to contend; often mediated by several psychosocial variables such as high perceived stigma, low self-esteem, social support and resilience [ 48 – 50 ].
The findings further alluded to effectiveness of the intervention. According to the respondents, the intervention resulted in several positive treatment outcomes (both direct and indirect), demonstrating the importance of giving PLWHA in therapy adequate time to assess their psychosocial wellbeing and understand their plight. The intervention was thus considered a success despite being implemented during the difficult times of Covid-19 lockdown, associated with numerous challenges causing distress to communities. The observed efficacy is in support of other earlier studies that have reported on the effectiveness of Behaviour Activation therapy in treating depression, even though little is known about its working mechanisms [ 51 , 52 ]. The beneficiaries appreciated the intervention, as it apparently gave them something beyond what they ordinarily received under the usual HIV care system; illustrating the effectiveness of psychological treatments for depression.
Several contextual factors were reported to have affected the implementation of the intervention. It should be noted that both the implementers (health workers) and the beneficiaries (PLWHA and their carers) overemphasized the facilitation in terms of transport refund as having been key to their participation and consistence. Given the high poverty levels, some would even endure walking the long distances, so as to save the money and support their financial needs.
This seems to suggest that many of them were mostly driven by some extrinsic motivation, instead of their underlying condition; implying that their attendance and consistence would probably have been difficult if there was not such facilitation, as a motivating factor. This casts doubt on the sustainability of the intervention at health facility level under the current health system, characterized by inadequate staffing and resource constraints. Nevertheless, the health system ought to devise strategies for scaling up or integrating the intervention in the mainstream HIV care in light of its potential positive effects.
In light of the above findings, we reasonably conclude that the intervention was generally implemented as planned, and considered acceptable and satisfactory by the implementers and beneficiaries. All respondents concurred with the fact that the intervention was beneficial and feasible; calling for its integration into the mainstream HIV/AIDS care system.
Lessons learnt and recommendations
Some of the lessons learnt in the course of the implementation, which could potentially inform the scale up of the intervention include:
- The importance of a warm patient-health worker relationship and its potential impact on treatment outcomes.
- The importance of supervising the implementers very closely when rolling out such an intervention
- The role played by stigma and discrimination in non-adherence to treatment and loss to follow up among PLWHA.
- Poverty is a strong mediating factor leading to depression among the PLWHA.
In light of the above, we make the following recommendations:
- The need to prioritize training of all health workers involved in HIV care in mental healthcare, to be able to assess for, detect and manage the less obvious psychosocial problems and their manifestation among PLWHA.
- While there were reports of stigma and discrimination against the PLWHA, the participants’ revelations apparently pointed towards more of self-perceived (internalizing stigma). Interventions for PLWHA should therefore not overlook this problem.
- The need for special consideration of the PLWHA who are socio-economically disadvantaged, prioritizing them in economic support programs such as the Social Assistance Grants for Empowerment (SAGE) program.
Limitations of the study
The intervention had to go on during the COVID-19 pandemic. The lock-down that ensued and the associated restrictions certainly reduced activity and participation rates; implying that the overall impact of the intervention could have been more significant had it not been the disruptions by the COVID-19 pandemic. However, the process evaluation did not assess for the effect of the pandemic on the programme.
One other limitation of the study is the fact that we relied on qualitative measurements, collecting data from a relatively small sample of individuals, which may affect the generalization of the findings. Furthermore, we did not do any quantitative assessment of the intervention outputs; making it hard to assess and demonstrate rigour.
Supporting information
S1 checklist. spirit checklist (consort checklist)..
Standards of how the HIV+D trial was designed, analyzed and interpreted.
https://doi.org/10.1371/journal.pmen.0000009.s001
S1 Fig. HIV+D Consort flow diagram.
Visual representation of the steps involved (progress and phases) for the HIV+D trial.
https://doi.org/10.1371/journal.pmen.0000009.s002
S1 Text. HIV+D protocol paper.
Article about the HIV+D study, highlighting the rationale and objectives of the study, methodology, data management and analysis.
https://doi.org/10.1371/journal.pmen.0000009.s003
- 1. UNAIDS. IN DANGER: UNAIDS Global AIDS Update 2022 [Internet]. Geneva: Joint United Nations Programme on HIV/AIDS; 2022 July 27 [cited 2023 July 16]. 376p. Report. https://www.unaids.org/sites/default/files/media_asset/2022-global-aids-update_en.pdf .
- View Article
- PubMed/NCBI
- Google Scholar
- 24. Uganda AIDS Commission [Internet]. Kampala: Uganda AIDS Commission; 2022. Facts on HIV and AIDS in Uganda, 2022 [cited 2023 October 11]. https://uac.go.ug/media/attachments/2023/01/12/hiv-aids-factsheet-2022.pdf .
- 25. Uganda AIDS Commission [Internet]. Kampala: Uganda AIDS Commission; 2015. The Uganda National HIV and AIDS Strategic Plan 2015/2016–2019/2020 [cited 2023 June 19]. http://library.health.go.ug/publications/service-delivery-diseases-control-prevention-communicable-diseases/hivaids/national-h-1 .

Featured Resource
Why hiv prevention, we are not on track..
Despite progress in several countries, we are still not on track to end the AIDS epidemic by 2030. In 2022, about 4000 adults and children acquired HIV each day — a total of 1.3 million new HIV infections. Lifesaving antiretroviral therapy can also prevent HIV by suppressing the virus in a person’s blood to an untransmissible level, but 9.2 million people living with AIDS did not receive ART in 2022.
Intensive effort is needed to reach the global target of fewer than 370,000 new HIV infections annually by 2025.
Accelerating progress in HIV prevention is particularly important in the GPC focus countries where three out of four new HIV infections occur.
Learn About the GPC
1.3 million new HIV infections
39 million people living with hiv, 630,000 people died of aids related illnesses, global search.

Assess HIV prevention efforts in your country
The Global HIV Prevention Coalition and partners in HIV prevention have developed tools to facilitate country-led planning of prevention programmes. Tools are available for use in GPC and non-GPC countries for each of the thematic “pillars” of HIV prevention.
Upcoming Events
South-to-south learning network webinar: sexual and reproductive health and prevention of mother-to-child transmission, south-to-south learning network webinar: hiv prevention self-assessment tools, global key populations hiv prevention pre-conference.
- Case Report
- Open access
- Published: 27 May 2024
A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient
- Wei Fu 1 , 2 na1 ,
- Zi Wei Deng 3 na1 ,
- Pei Wang 1 ,
- Zhen Wang Zhu 1 ,
- Zhi Bing Xie 1 ,
- Yong Zhong Li 1 &
- Hong Ying Yu 1
BMC Infectious Diseases volume 24 , Article number: 533 ( 2024 ) Cite this article
330 Accesses
1 Altmetric
Metrics details
Hepatitis B virus (HBV) infection can cause liver failure, while individuals with Acquired Immunodeficiency Virus Disease (AIDS) are highly susceptible to various opportunistic infections, which can occur concurrently. The treatment process is further complicated by the potential occurrence of immune reconstitution inflammatory syndrome (IRIS), which presents significant challenges and contributes to elevated mortality rates.
Case presentation
The 50-year-old male with a history of chronic hepatitis B and untreated human immunodeficiency virus (HIV) infection presented to the hospital with a mild cough and expectoration, revealing multi-drug resistant pulmonary tuberculosis (MDR-PTB), which was confirmed by XpertMTB/RIF PCR testing and tuberculosis culture of bronchoalveolar lavage fluid (BALF). The patient was treated with a regimen consisting of linezolid, moxifloxacin, cycloserine, pyrazinamide, and ethambutol for tuberculosis, as well as a combination of bictegravir/tenofovir alafenamide/emtricitabine (BIC/TAF/FTC) for HBV and HIV viral suppression. After three months of treatment, the patient discontinued all medications, leading to hepatitis B virus reactivation and subsequent liver failure. During the subsequent treatment for AIDS, HBV, and drug-resistant tuberculosis, the patient developed disseminated cryptococcal disease. The patient’s condition worsened during treatment with liposomal amphotericin B and fluconazole, which was ultimately attributed to IRIS. Fortunately, the patient achieved successful recovery after appropriate management.
Enhancing medical compliance is crucial for AIDS patients, particularly those co-infected with HBV, to prevent HBV reactivation and subsequent liver failure. Furthermore, conducting a comprehensive assessment of potential infections in patients before resuming antiviral therapy is essential to prevent the occurrence of IRIS. Early intervention plays a pivotal role in improving survival rates.
Peer Review reports
HIV infection remains a significant global public health concern, with a cumulative death toll of 40 million individuals [ 1 ]. In 2021 alone, there were 650,000 deaths worldwide attributed to AIDS-related causes. As of the end of 2021, approximately 38 million individuals were living with HIV, and there were 1.5 million new HIV infections reported annually on a global scale [ 2 ]. Co-infection with HBV and HIV is prevalent due to their similar transmission routes, affecting around 8% of HIV-infected individuals worldwide who also have chronic HBV infection [ 3 ]. Compared to those with HBV infection alone, individuals co-infected with HIV/HBV exhibit higher HBV DNA levels and a greater risk of reactivation [ 4 ]. Opportunistic infections, such as Pneumocystis jirovecii pneumonia, Toxoplasma encephalitis, cytomegalovirus retinitis, cryptococcal meningitis (CM), tuberculosis, disseminated Mycobacterium avium complex disease, pneumococcal pneumonia, Kaposi’s sarcoma, and central nervous system lymphoma, are commonly observed due to HIV-induced immunodeficiency [ 5 ]. Tuberculosis not only contributes to the overall mortality rate in HIV-infected individuals but also leads to a rise in the number of drug-resistant tuberculosis cases and transmission of drug-resistant strains. Disseminated cryptococcal infection is a severe opportunistic infection in AIDS patients [ 6 ], and compared to other opportunistic infections, there is a higher incidence of IRIS in patients with cryptococcal infection following antiviral and antifungal therapy [ 7 ]. This article presents a rare case of an HIV/HBV co-infected patient who presented with MDR-PTB and discontinued all medications during the initial treatment for HIV, HBV, and tuberculosis. During the subsequent re-anti-HBV/HIV treatment, the patient experienced two episodes of IRIS associated with cryptococcal infection. One episode was classified as “unmasking” IRIS, where previously subclinical cryptococcal infection became apparent with immune improvement. The other episode was categorized as “paradoxical” IRIS, characterized by the worsening of pre-existing cryptococcal infection despite immune restoration [ 8 ]. Fortunately, both episodes were effectively treated.
A 50-year-old male patient, who is self-employed, presented to our hospital in January 2022 with a chief complaint of a persistent cough for the past 2 months, without significant shortness of breath, palpitations, or fever. His medical history revealed a previous hepatitis B infection, which resulted in hepatic failure 10 years ago. Additionally, he was diagnosed with HIV infection. However, he ceased taking antiviral treatment with the medications provided free of charge by the Chinese government for a period of three years. During this hospital visit, his CD4 + T-cell count was found to be 26/μL (normal range: 500–1612/μL), HIV-1 RNA was 1.1 × 10 5 copies/ml, and HBV-DNA was negative. Chest computed tomography (CT) scan revealed nodular and patchy lung lesions (Fig. 1 ). The BALF shows positive acid-fast staining. Further assessment of the BALF using XpertMTB/RIF PCR revealed resistance to rifampicin, and the tuberculosis drug susceptibility test of the BALF (liquid culture, medium MGIT 960) indicated resistance to rifampicin, isoniazid, and streptomycin. Considering the World Health Organization (WHO) guidelines for drug-resistant tuberculosis, the patient’s drug susceptibility results, and the co-infection of HIV and HBV, an individualized treatment plan was tailored for him. The treatment plan included BIC/TAF/FTC (50 mg/25 mg/200 mg per day) for HBV and HIV antiviral therapy, as well as linezolid (0.6 g/day), cycloserine (0.5 g/day), moxifloxacin (0.4 g/day), pyrazinamide (1.5 g/day), and ethambutol (0.75 g/day) for anti-tuberculosis treatment, along with supportive care.
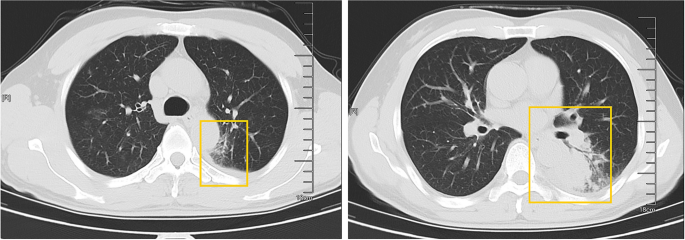
The patient’s pulmonary CT scan shows patchy and nodular lesions accompanied by a small amount of pleural effusion, later confirmed to be MDR-PTB
Unfortunately, after 3 months of follow-up, the patient discontinued all medications due to inaccessibility of the drugs. He returned to our hospital (Nov 12, 2022, day 0) after discontinuing medication for six months, with a complaint of poor appetite for the past 10 days. Elevated liver enzymes were observed, with an alanine aminotransferase level of 295 IU/L (normal range: 0–40 IU/L) and a total bilirubin(TBIL) level of 1.8 mg/dL (normal range: 0–1 mg/dL). His HBV viral load increased to 5.5 × 10 9 copies/ml. Considering the liver impairment, elevated HBV-DNA and the incomplete anti-tuberculosis treatment regimen (Fig. 2 A), we discontinued pyrazinamide and initiated treatment with linezolid, cycloserine, levofloxacin, and ethambutol for anti-tuberculosis therapy, along with BIC/TAF/FTC for HIV and HBV antiviral treatment. Additionally, enhanced liver protection and supportive management were provided, involving hepatoprotective effects of medications such as glutathione, magnesium isoglycyrrhizinate, and bicyclol. However, the patient’s TBIL levels continued to rise progressively, reaching 4.4 mg/dL on day 10 (Fig. 3 B). Suspecting drug-related factors, we discontinued all anti-tuberculosis medications while maintaining BIC/TAF/FTC for antiviral therapy, the patient’s TBIL levels continued to rise persistently. We ruled out other viral hepatitis and found no significant evidence of obstructive lesions on magnetic resonance cholangiopancreatography. Starting from the day 19, due to the patient’s elevated TBIL levels of 12.5 mg/dL, a decrease in prothrombin activity (PTA) to 52% (Fig. 3 D), and the emergence of evident symptoms such as abdominal distension and poor appetite, we initiated aggressive treatment methods. Unfortunately, on day 38, his hemoglobin level dropped to 65 g/L (normal range: 120–170 g/L, Fig. 3 A), and his platelet count decreased to 23 × 10 9 /L (normal range: 125–300 × 10 9 /L, Fig. 3 C). Based on a score of 7 on the Naranjo Scale, it was highly suspected that “Linezolid” was the cause of these hematological abnormalities. Therefore, we had to discontinue Linezolid for the anti-tuberculosis treatment. Subsequently, on day 50, the patient developed recurrent fever, a follow-up chest CT scan revealed enlarged nodules in the lungs (Fig. 2 B). The patient also reported mild dizziness and a worsening cough. On day 61, the previous blood culture results reported the growth of Cryptococcus. A lumbar puncture was performed on the same day, and the cerebrospinal fluid (CSF) opening pressure was measured at 130 mmH 2 O. India ink staining of the CSF showed typical encapsulated yeast cells suggestive of Cryptococcus. Other CSF results indicated mild leukocytosis and mildly elevated protein levels, while chloride and glucose levels were within normal limits. Subsequently, the patient received a fungal treatment regimen consisting of liposomal amphotericin B (3 mg/kg·d −1 ) in combination with fluconazole(600 mg/d). After 5 days of antifungal therapy, the patient’s fever symptoms were well controlled. Despite experiencing bone marrow suppression, including thrombocytopenia and worsening anemia, during this period, proactive symptom management, such as the use of erythropoietin, granulocyte colony-stimulating factor, and thrombopoietin, along with high-calorie dietary management, even reducing the dosage of liposomal amphotericin B to 2 mg/kg/day for 10 days at the peak of severity, successfully controlled the bone marrow suppression. However, within the following week, the patient experienced fever again, accompanied by a worsened cough, increased sputum production, and dyspnea. Nevertheless, the bilirubin levels did not show a significant increase. On day 78 the patient’s lung CT revealed patchy infiltrates and an increased amount of pleural effusion (Fig. 2 C). The CD4 + T-cell count was 89/μL (normal range: 500–700/μL), indicating a significant improvement in immune function compared to the previous stage, and C-reactive protein was significantly elevated, reflecting the inflammatory state, other inflammatory markers such as IL-6 and γ-IFN were also significantly elevated. On day 84, Considering the possibility of IRIS, the patient began taking methylprednisolone 30 mg once a day as part of an effort to control his excessive inflammation. Following the administration of methylprednisolone, the man experienced an immediate improvement in his fever. Additionally, symptoms such as cough, sputum production, dyspnea, and poor appetite gradually subsided over time. A follow-up lung CT showed significant improvement, indicating a positive response to the treatment. After 28 days of treatment with liposomal amphotericin B in combination with fluconazole, liposomal amphotericin B was discontinued, and the patient continued with fluconazole to consolidate the antifungal therapy for Cryptococcus. Considering the patient’s ongoing immunodeficiency, the dosage of methylprednisolone was gradually reduced by 4 mg every week. After improvement in liver function, the patient’s anti-tuberculosis treatment regimen was adjusted to include bedaquiline, contezolid, cycloserine, moxifloxacin, and ethambutol. The patient’s condition was well controlled, and a follow-up lung CT on day 117 indicated a significant improvement in lung lesions (Fig. 2 D).
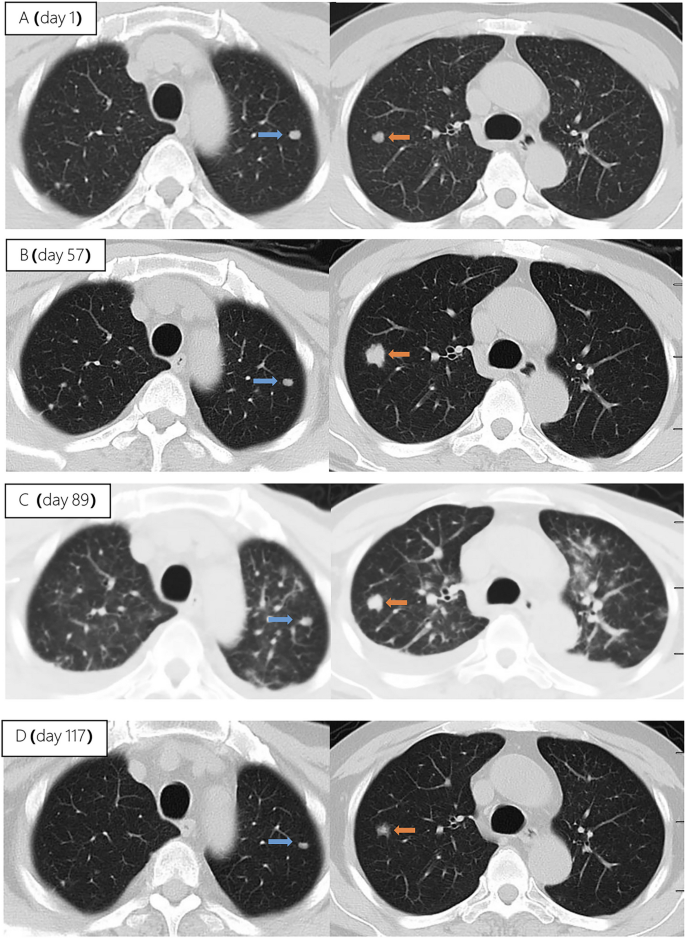
Upon second hospitalization admission ( A ), nodular lesions were already present in the lungs, and their size gradually increased after the initiation of ART ( B , C ). Notably, the lung lesions became more pronounced following the commencement of anti-cryptococcal therapy, coinciding with the occurrence of pleural effusion ( C ). However, with the continuation of antifungal treatment and the addition of glucocorticoids, there was a significant absorption and reduction of both the pleural effusion and pulmonary nodules ( D )
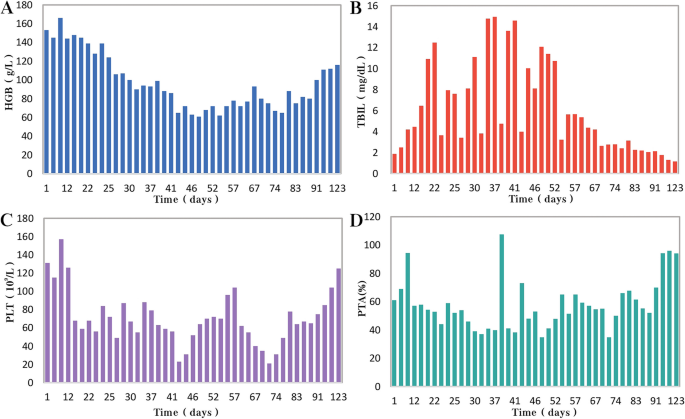
During the patient's second hospitalization, as the anti-tuberculosis treatment progressed and liver failure developed, the patient’s HGB levels gradually decreased ( A ), while TBIL levels increased ( B ). Additionally, there was a gradual decrease in PLT count ( C ) and a reduction in prothrombin activity (PTA) ( D ), indicating impaired clotting function. Moreover, myelosuppression was observed during the anti-cryptococcal treatment ( C )
People living with HIV/AIDS are susceptible to various opportunistic infections, which pose the greatest threat to their survival [ 5 ]. Pulmonary tuberculosis and disseminated cryptococcosis remain opportunistic infections with high mortality rates among AIDS patients [ 9 , 10 ]. These infections occurring on the basis of liver failure not only increase diagnostic difficulty but also present challenges in treatment. Furthermore, as the patient’s immune function and liver function recover, the occurrence of IRIS seems inevitable.
HIV and HBV co-infected patients are at a higher risk of HBV reactivation following the discontinuation of antiviral drugs
In this case, the patient presented with both HIV and HBV infections. Although the HBV DNA test was negative upon admission. However, due to the patient’s self-discontinuation of antiretroviral therapy (ART), HBV virologic and immunologic reactivation occurred six months later, leading to a rapid increase in viral load and subsequent hepatic failure. Charles Hannoun et al. also reported similar cases in 2001, where two HIV-infected patients with positive HBsAg experienced HBV reactivation and a rapid increase in HBV DNA levels after discontinuing antiretroviral and antiviral therapy, ultimately resulting in severe liver failure [ 11 ]. The European AIDS Clinical Society (EACS) also emphasize that abrupt discontinuation of antiviral therapy in patients co-infected with HBV and HIV can trigger HBV reactivation, which, although rare, can potentially result in liver failure [ 12 ].
Diagnosing disseminated Cryptococcus becomes more challenging in AIDS patients with liver failure, and the selection of antifungal medications is significantly restricted
In HIV-infected individuals, cryptococcal disease typically manifests as subacute meningitis or meningoencephalitis, often accompanied by fever, headache, and neck stiffness. The onset of symptoms usually occurs approximately two weeks after infection, with typical signs and symptoms including meningeal signs such as neck stiffness and photophobia. Some patients may also experience encephalopathy symptoms like somnolence, mental changes, personality changes, and memory loss, which are often associated with increased intracranial pressure (ICP) [ 13 ]. The presentation of cryptococcal disease in this patient was atypical, as there were no prominent symptoms such as high fever or rigors, nor were there any signs of increased ICP such as somnolence, headache, or vomiting. The presence of pre-existing pulmonary tuberculosis further complicated the early diagnosis, potentially leading to the clinical oversight of recognizing the presence of cryptococcus. In addition to the diagnostic challenges, treating a patient with underlying liver disease, multidrug-resistant tuberculosis, and concurrent cryptococcal infection poses significant challenges. It requires considering both the hepatotoxicity of antifungal agents and potential drug interactions. EACS and global guideline for the diagnosis and management of cryptococcosis suggest that liposomal amphotericin B (3 mg/kg·d −1 ) in combination with flucytosine (100 mg/kg·d −1 ) or fluconazole (800 mg/d) is the preferred induction therapy for CM for 14 days [ 12 , 14 ]. Flucytosine has hepatotoxicity and myelosuppressive effects, and it is contraindicated in patients with severe liver dysfunction. The antiviral drug bictegravir is a substrate for hepatic metabolism by CYP3A and UGT1A1 enzymes [ 15 ], while fluconazole inhibits hepatic enzymes CYP3A4 and CYP2C9 [ 16 ]. Due to the patient's liver failure and bone marrow suppression, we reduced the dosage of liposomal amphotericin B and fluconazole during the induction period. Considering the hepatotoxicity of fluconazole and its interaction with bictegravir, we decreased the dosage of fluconazole to 600 mg/d, while extending the duration of induction therapy to 28 days.
During re-antiviral treatment, maintaining vigilance for the development of IRIS remains crucial
IRIS refers to a series of inflammatory diseases that occur in HIV-infected individuals after initiating ART. It is associated with the paradoxical worsening of pre-existing infections, which may have been previously diagnosed and treated or may have been subclinical but become apparent due to the host regaining the ability to mount an inflammatory response. Currently, there is no universally accepted definition of IRIS. However, the following conditions are generally considered necessary for diagnosing IRIS: worsening of a diagnosed or previously unrecognized pre-existing infection with immune improvement (referred to as “paradoxical” IRIS) or the unmasking of a previously subclinical infection (referred to as “unmasking” IRIS) [ 8 ]. It is estimated that 10% to 30% of HIV-infected individuals with CM will develop IRIS after initiating or restarting effective ART [ 7 , 17 ]. In the guidelines of the WHO and EACS, it is recommended to delay the initiation of antiviral treatment for patients with CM for a minimum of 4 weeks to reduce the incidence of IRIS. Since we accurately identified the presence of multidrug-resistant pulmonary tuberculosis in the patient during the early stage, we promptly initiated antiretroviral and anti-hepatitis B virus treatment during the second hospitalization. However, subsequent treatment revealed that the patient experienced at least two episodes of IRIS. The first episode was classified as “unmasking” IRIS, as supported by the enlargement of pulmonary nodules observed on the chest CT scan following the initiation of ART (Fig. 2 A). Considering the morphological changes of the nodules on the chest CT before antifungal therapy, the subsequent emergence of disseminated cryptococcal infection, and the subsequent reduction in the size of the lung nodules after antifungal treatment, although there is no definitive microbiological evidence, we believe that the initial enlargement of the lung nodules was caused by cryptococcal pneumonia. As ART treatment progressed, the patient experienced disseminated cryptococcosis involving the blood and central nervous system, representing the first episode. Following the initiation of antifungal therapy for cryptococcosis, the patient encountered a second episode characterized by fever and worsening pulmonary lesions. Given the upward trend in CD4 + T-cell count, we attributed this to the second episode of IRIS, the “paradoxical” type. The patient exhibited a prompt response to low-dose corticosteroids, further supporting our hypothesis. Additionally, the occurrence of cryptococcal IRIS in the lungs, rather than the central nervous system, is relatively uncommon among HIV patients [ 17 ].
Conclusions
From the initial case of AIDS combined with chronic hepatitis B, through the diagnosis and treatment of multidrug-resistant tuberculosis, the development of liver failure and disseminated cryptococcosis, and ultimately the concurrent occurrence of IRIS, the entire process was tortuous but ultimately resulted in a good outcome (Fig. 4 ). Treatment challenges arose due to drug interactions, myelosuppression, and the need to manage both infectious and inflammatory conditions. Despite these hurdles, a tailored treatment regimen involving antifungal and antiretroviral therapies, along with corticosteroids, led to significant clinical improvement. While CM is relatively common among immunocompromised individuals, especially those with acquired immunodeficiency syndrome (AIDS) [ 13 ], reports of disseminated cryptococcal infection on the background of AIDS complicated with liver failure are extremely rare, with a very high mortality rate.
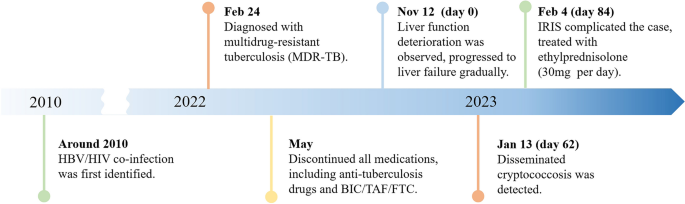
A brief timeline of the patient's medical condition progression and evolution
Through managing this patient, we have also gained valuable insights. (1) Swift and accurate diagnosis, along with timely and effective treatment, can improve prognosis, reduce mortality, and lower disability rates. Whether it's the discovery and early intervention of liver failure, the identification and treatment of disseminated cryptococcosis, or the detection and management of IRIS, all these interventions are crucially timely. They are essential for the successful treatment of such complex and critically ill patients.
(2) Patients who exhibit significant drug reactions, reducing the dosage of relevant medications and prolonging the treatment duration can improve treatment success rates with fewer side effects. In this case, the dosages of liposomal amphotericin B and fluconazole are lower than the recommended dosages by the World Health Organization and EACS guidelines. Fortunately, after 28 days of induction therapy, repeat CSF cultures showed negative results for Cryptococcus, and the improvement of related symptoms also indicates that the patient has achieved satisfactory treatment outcomes. (3) When cryptococcal infection in the bloodstream or lungs is detected, prompt lumbar puncture should be performed to screen for central nervous system cryptococcal infection. Despite the absence of neurological symptoms, the presence of Cryptococcus neoformans in the cerebrospinal fluid detected through lumbar puncture suggests the possibility of subclinical or latent CM, especially in late-stage HIV-infected patients.
We also encountered several challenges and identified certain issues that deserve attention. Limitations: (1) The withdrawal of antiviral drugs is a critical factor in the occurrence and progression of subsequent diseases in patients. Improved medical education is needed to raise awareness and prevent catastrophic consequences. (2) Prior to re-initiating antiviral therapy, a thorough evaluation of possible infections in the patient is necessary. Caution should be exercised, particularly in the case of diseases prone to IRIS, such as cryptococcal infection. (3) There is limited evidence on the use of reduced fluconazole dosage (600 mg daily) during antifungal therapy, and the potential interactions between daily fluconazole (600 mg) and the antiviral drug bictegravir and other tuberculosis medications have not been extensively studied. (4) Further observation is needed to assess the impact of early-stage limitations in the selection of anti-tuberculosis drugs on the treatment outcome of tuberculosis in this patient, considering the presence of liver failure.
In conclusion, managing opportunistic infections in HIV patients remains a complex and challenging task, particularly when multiple opportunistic infections are compounded by underlying liver failure. Further research efforts are needed in this area.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
Hepatitis B virus
Acquired immunodeficiency virus disease
Immune reconstitution inflammatory syndrome
Human immunodeficiency virus
Multi-drug resistant pulmonary tuberculosis
Bronchoalveolar lavage fluid
Bictegravir/tenofovir alafenamide/emtricitabine
Cryptococcal meningitis
World Health Organization
Computed tomography
Total bilirubin
Cerebrospinal fluid
European AIDS Clinical Society
Intracranial pressure
Antiretroviral therapy
Prothrombin activity
Bekker L-G, Beyrer C, Mgodi N, Lewin SR, Delany-Moretlwe S, Taiwo B, et al. HIV infection. Nat Rev Dis Primer. 2023;9:1–21.
Google Scholar
Data on the size of the HIV epidemic. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/data-on-the-size-of-the-hiv-aids-epidemic?lang=en . Accessed 3 May 2023.
Leumi S, Bigna JJ, Amougou MA, Ngouo A, Nyaga UF, Noubiap JJ. Global burden of hepatitis B infection in people living with human immunodeficiency virus: a systematic review and meta-analysis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71:2799–806.
Article Google Scholar
McGovern BH. The epidemiology, natural history and prevention of hepatitis B: implications of HIV coinfection. Antivir Ther. 2007;12(Suppl 3):H3-13.
Article CAS PubMed Google Scholar
Kaplan JE, Masur H, Holmes KK, Wilfert CM, Sperling R, Baker SA, et al. USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus: an overview. USPHS/IDSA Prevention of Opportunistic Infections Working Group. Clin Infect Dis Off Publ Infect Dis Soc Am. 1995;21 Suppl 1:S12-31.
Article CAS Google Scholar
Bamba S, Lortholary O, Sawadogo A, Millogo A, Guiguemdé RT, Bretagne S. Decreasing incidence of cryptococcal meningitis in West Africa in the era of highly active antiretroviral therapy. AIDS Lond Engl. 2012;26:1039–41.
Müller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M, et al. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:251–61.
Article PubMed PubMed Central Google Scholar
Haddow LJ, Easterbrook PJ, Mosam A, Khanyile NG, Parboosing R, Moodley P, et al. Defining immune reconstitution inflammatory syndrome: evaluation of expert opinion versus 2 case definitions in a South African cohort. Clin Infect Dis Off Publ Infect Dis Soc Am. 2009;49:1424–32.
Obeagu E, Onuoha E. Tuberculosis among HIV patients: a review of Prevalence and Associated Factors. Int J Adv Res Biol Sci. 2023;10:128–34.
Rajasingham R, Govender NP, Jordan A, Loyse A, Shroufi A, Denning DW, et al. The global burden of HIV-associated cryptococcal infection in adults in 2020: a modelling analysis. Lancet Infect Dis. 2022;22:1748–55.
Manegold C, Hannoun C, Wywiol A, Dietrich M, Polywka S, Chiwakata CB, et al. Reactivation of hepatitis B virus replication accompanied by acute hepatitis in patients receiving highly active antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2001;32:144–8.
EACS Guidelines | EACSociety. https://www.eacsociety.org/guidelines/eacs-guidelines/ . Accessed 7 May 2023.
Cryptococcosis | NIH. 2021. https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/cryptococcosis . Accessed 6 May 2023.
Chang CC, Harrison TS, Bicanic TA, Chayakulkeeree M, Sorrell TC, Warris A, et al. Global guideline for the diagnosis and management of cryptococcosis: an initiative of the ECMM and ISHAM in cooperation with the ASM. Lancet Infect Dis. 2024;10:S1473-3099(23)00731-4.
Deeks ED. Bictegravir/emtricitabine/tenofovir alafenamide: a review in HIV-1 infection. Drugs. 2018;78:1817–28.
Article CAS PubMed PubMed Central Google Scholar
Bellmann R, Smuszkiewicz P. Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection. 2017;45:737–79.
Shelburne SA, Darcourt J, White AC, Greenberg SB, Hamill RJ, Atmar RL, et al. The role of immune reconstitution inflammatory syndrome in AIDS-related Cryptococcus neoformans disease in the era of highly active antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2005;40:1049–52.
Download references
Acknowledgements
We express our sincere gratitude for the unwavering trust bestowed upon our medical team by the patient throughout the entire treatment process.
This work was supported by the Scientific Research Project of Hunan Public Health Alliance with the approval No. ky2022-002.
Author information
Wei Fu and Zi Wei Deng contributed equally to this work.
Authors and Affiliations
Center for Infectious Diseases, Hunan University of Medicine General Hospital, Huaihua, Hunan, China
Wei Fu, Pei Wang, Zhen Wang Zhu, Ye Pu, Zhi Bing Xie, Yong Zhong Li & Hong Ying Yu
Department of Tuberculosis, The First Affiliated Hospital of Xinxiang Medical University, XinXiang, Henan, China
Department of Clinical Pharmacy, Hunan University of Medicine General Hospital, Huaihua, Hunan, China
Zi Wei Deng
You can also search for this author in PubMed Google Scholar
Contributions
WF and ZWD integrated the data and wrote the manuscript, YHY contributed the revision of the manuscript, PW and YP provided necessary assistance and provided key suggestions, ZWZ, YZL and ZBX contributed data acquisition and interpretation for etiological diagnosis. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Hong Ying Yu .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethics Committee of the Hunan University of Medicine General Hospital (HYZY-EC-202306-C1), and with the informed consent of the patient.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fu, W., Deng, Z.W., Wang, P. et al. A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient. BMC Infect Dis 24 , 533 (2024). https://doi.org/10.1186/s12879-024-09431-9
Download citation
Received : 30 June 2023
Accepted : 24 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12879-024-09431-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Liver failure
- Disseminated cryptococcal disease
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Res Policy Syst
- v.9(Suppl 1); 2011

The impact of HIV and AIDS research: a case study from Swaziland
Alan whiteside.
1 Director and Professor, Health Economics and HIV/AIDS Research Division University of KwaZulu-Natal, Durban
Fiona E Henry
2 Visiting Fellow, Health Economics and HIV/AIDS Research Division University of KwaZulu Natal, Durban
Swaziland is experiencing the world’s worst HIV and AIDS epidemic. Prevalence rose from four percent of antenatal clinic attendees in 1992 to 42.6 percent in 2004. The Report ‘Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era’ published in 2007 bought together social and economic indicators. It built a picture of the epidemic as a humanitarian emergency, requiring urgent action from international organisations, donors, and governments. Following a targeted communications effort, the report was believed to have raised the profile of the issue and Swaziland - a success story for HIV and AIDS research.
Keen to understand how, where and why the report had an impact, Health Economics and HIV/AIDS Research Division commissioned an assessment to track and evaluate the influence of the research. This tapped into literature on the significance of understanding the research-to-policy interface. This paper outlines the report and its impact. It explores key findings from the assessment and suggests lessons for future research projects.
The paper demonstrates that, although complex, and not without methodological issues, impact assessment of research can be of real value to researchers in understanding the research-to-policy interface.
Only by gaining insight into this process can researchers move forward in delivering effective research.
HIV and AIDS Research in Swaziland
The hiv and aids epidemic.
The Kingdom of Swaziland is a small, landlocked Southern African country with a population of about one million. In the 1980’s it experienced a significant upturn in investment and growth, benefiting from a regional advantage due to war in Mozambique and apartheid in South Africa. This was combined with relative political stability, sound macroeconomic policies, and a cheap and productive workforce, and resulted in significant inflows of foreign direct investment. Between 1985 and 1999 the growth rate was 6% and the well-being of the Swazi’s was on a modest upward trajectory [ 1 ]. Since 2000 these gains have been reversed, largely due to the impact of HIV and AIDS.
Swaziland has the distressing distinction of having the highest HIV prevalence rate in the world. Its epidemic spread with exceptional speed, from four percent of antenatal clinic attendees in 1992 to 42.6 percent in 2004 [ 2 ]. The 2006 data seemed to offer some hope with a decline to 39.2 percent, but the 2008 survey recorded a rise to 42 percent [ 3 ]. Mortality rose and life expectancy fell from 60 years in 1997 to 31.3 years in 2004, the world’s lowest [ 4 ]. Swaziland is additionally handicapped because the economic success of the 1980s and early 1990s mean it is categorised as a middle-income country, and cannot access international support available to low-income countries.
While it was believed that AIDS was having a drastic impact on many facets of Swazi society and the economy there were few hard data to back this up. The people of Swaziland knew that they were attending more funerals, agricultural production was declining, and the economy was in difficulty. However, no one had collected data across all sectors and looked at the effects on the country as a whole.
In early 2007 the terms of reference for a study to assess the impact of the AIDS epidemic across the nation were drawn up. The ideas were developed primarily by Dr Derek Von Wissell, Head of the National Emergency Response Council on HIV/AIDS in Swaziland (NERCHA) and Professor Alan Whiteside, Director of the Health Economics and HIV/AIDS Research Division (HEARD) at the University of KwaZulu-Natal. The research was partly funded by HEARD and led by Amy Whalley, a former Overseas Development Institute Fellow who had worked with NERCHA and the Ministry of Health and guided by Whiteside and staff at NERCHA. Whalley’s task was to gather and analyse information on what was going on across the nation using available data sets; to compare Swaziland’s situation with other countries and thus build advocacy material for use inside the country and with the international community. The write up was primarily by Whalley with major input by Whiteside. In October 2007 the report, ‘Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era’, (here after called ‘Reviewing Emergencies’) was published [ 5 ], distributed and disseminated. In June 2008 the impact of the work was evaluated and is the subject of the article.
Reviewing Emergencies Report
Reviewing Emergencies used key socio-economic indicators from many sources to build a holistic and multidimensional picture of impact of HIV/AIDS in Swaziland. Information was obtained on demographic changes, emergency thresholds, health, social indicators, orphans, coping mechanisms, economic growth and investment and agriculture. These were tracked over time. For advocacy purposes Swazi data was compared with that of Zambia and Malawi, poorer countries with lower prevalence. The report painted a bleak picture showing that Swaziland is experiencing a humanitarian crisis comparable to countries besieged by conflict or struggling in the wake of a severe natural disaster. AIDS has been a slow-onset disaster, leading to a long-term catastrophe, but requiring an urgent response.
The report spoke to two audiences. For Swazi’s it confirmed that AIDS was indeed having a devastating effect on their nation. The same message was aimed at the international community. However it also urged the latter to re-examine the HIV and AIDS epidemic. It sought to broaden the traditional consensus on what constitutes an emergency to include ‘long-wave emergencies’. Effective interventions require both an immediate emergency response but also have to build capacity for long-term programmes [ 5 ]. In the course of the research the country’s classification emerged as an important issue. As a lower-middle income country Swaziland is not eligible for international development assistance (IDA) grants from the World Bank, and concessional-lending [ 6 ]. The report challenged the use of GDP per capita as an indicator to set the status of a country and its access to support in the face of a generalised AIDS epidemic. It noted the global perception of ‘middle-income countries’ is that they need less support and are somehow ‘less deserving’. (Figure (Figure1 1 )

Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era
Assessing the impact: The research to policy interface
Much of SRH and HIV and AIDS research, particularly in the development arena, aims to influence policy, it is “research committed to improvement” [ 7 ]. Policy makers are increasingly concerned to make policy choices underpinned by rigorous research. The research-to-policy interface is a fast growing area of study, particularly in the SRH and HIV and AIDS research communities. The purposes are two fold: accountability of a research organisation, demonstrating achievement and value for money for funders; and as a learning exercise, developing a better understanding of the research impact process in order to enhance future impact [ 8 ]. HEARD is an applied research organisation aiming to mobilise evidence for interventions in health and HIV in the region [ 9 ]. Only by identifying where change has transpired as a result of its research, where it has not, and the reasons for this, can it deliver effective research.
Impact assessment is an underdeveloped field of study, in part due to the complex and dynamic nature of research impacts and the consequent difficulty in measuring them. Sumner, Perkins and Lindstrom (2008, unpublished) identify a number of significant problems when attempting to track the impact of research: difficulty in determining conceptual influence (on opinion, attitudes and thinking); identifying research users, timing of assessment; attributing impact in the context of other drivers; and using qualitative and subjective data [ 10 ]. Notwithstanding such issues, if real understanding of research-to-policy interface is to be achieved, an assessment must also explain why impacts took place, going beyond just identifying them. Difficult as it may be, there are good reasons for attempting to evaluate the impact of policy research [ 11 ]. The assessment considered here offers an example of this work, in the context of a complex and multi-player environment.
Methodology and issues
It seemed that the Reviewing Emergencies report had been effective in influencing policymakers. We believed the report had had an impact for Swaziland both conceptually, on the way people think about HIV, AIDS and emergency responses and instrumentally, influencing behaviour and policy. In mid 2008, the decision was taken to carry out an assessment of the impact of the report to determine the validity of this claim and understand what ‘worked’ and what ‘didn’t’. Fiona Henry, who was awarded a fellowship by the University of Edinburgh to work with HEARD, was tasked with leading the assessment.
The specific objectives were to:
• Document the creation and dissemination of the report;
• Identify and explain its impact;
• Identify any barriers and/or limitations to its impact;
• Draw lessons for maximising the impact of future research.
This article was developed from the assessment assisted by a presentation given at the meeting of DFID funded Research Programme Consortia on ‘Strengthening the research to policy and practice interface: Exploring strategies used by research organisations working on Sexual and Reproductive Health and HIV and AIDS’ held in Liverpool in May 2009; and through peer review. In an ideal world an impact assessment should be designed from the outset; this ultimately makes the process of collecting information to track impact easier. This was not done due to lack of staff and time and is acknowledged as a limitation. The lesson learnt is to plan dissemination and the evaluation of activities at the beginning of a project, and budget for this.
Forward-tracking and attribution
Two broad categories exist for impact assessments; forward-tracking, from research to outcome, and backwards-tracking, from decisions taken to potential research influence. Our impact assessment wanted to track from publication to outcome. However, forward-tracking approaches can have serious limitations [ 12 ]. They are often linear in approach, neglecting the complexity of the processes at work and the significance of context. The policy environment is influenced by socio-cultural, political and economic factors and these must be acknowledged in order to understand why an impact took place. Taking this into account, the assessment attempts to put identified ‘impacts’ into a relevant context.
The assessment cannot claim to fully understand the influence of other ‘drivers’ on outcomes. Policy research is only one of many sources of information used in decision making or to form opinion. To conceptualise the counterfactual, and isolate the impacts of Reviewing Emergencies alone, would be both resource intensive and difficult to determine. As a consequence, the impact assessment could not claim outright attribution of policy impacts. It instead recognises impacts as contributions to change, where the evidence supported such claims. This difficult methodological issue of attributing outcomes can result in a ‘shying away’ from impact assessments [ 10 ]. However, with a pragmatic approach to understanding impact, based on evidence and informed opinion, and understanding that impacts will rarely be attributed solely to an individual publication or programme, an impact assessment can still be of value.
Conceptualising ‘impact’: A temporal approach
‘Impact’ is used interchangeably with terms such as ‘influence’, ‘outcomes’, ‘use’ and ‘uptake’, and a number of definitions exist in the literature [ 10 ]. In the assessment of the Reviewing Emergencies impact is defined temporally, referring to ‘initial impact’, ‘long-term impact’ and ‘potential impact’. This is important. Firstly, initial impact refers to the ‘sticky messages’ of the report: what strikes the reader instantly about the report and its findings and the key messages that they come away with. Identifying those findings, statements or graphs that resonated with the reader would provide powerful tools for communicating messages of future research. Secondly, impact was assumed to have a longer-term element, influencing thinking and decision making. This constituted the main body of the assessment. ‘Long-term impacts’ are those conceptual and instrumental impacts that change understanding and attitudes or contribute to a change in policy or behaviour. As the assessment took place about a year after the launch of Reviewing Emergencies, ‘potential impact’ considered the possibility of impact in the future. With continued advocacy, and changes to the policy environment, potential impact outlines the ‘capability’ of the report’s findings. It highlights areas in which to focus advocacy efforts in the future.
Research users
Policy research can be used for multiple, often unforeseen, purposes [ 11 ]. Tracking a research contribution, especially one that seeks conceptual change, is difficult. Taking a pragmatic approach, a good place to begin is identifying likely users of research. The impact assessment chose five sectors for analysis to try to encompass key actors. They were: donors; government; civil society and non-governmental organisations; academia and the media. Identifying them helped to structure the analysis and understand the different ‘uptake’ of the research. The categories were purposefully broad in recognition of the broad array of policy players, and to enable flexibility in analysis; crossing national boundaries and disciplines. Lessons from Swaziland, we believed, would be applicable elsewhere in the region, especially in Lesotho, Namibia and Botswana as these are all defined as lower-middle-income countries; have similar prevalence levels; and are members (with South Africa) of the Southern African Customs Union. It was also important as Ministries of Health are often weak and in many African countries donor policies have a disproportionate influence on health.
Data and measurement
‘Measuring’ impact posed some difficulty. Changes to thinking and decisions are particularly hard to quantify. For this reason a qualitative approach was used, asking how and why people believed the report had altered their approach to the Swazi epidemic, and what impact they believed the report had. Anecdotal evidence and substantive examples were key to supporting such beliefs in the absence of quantitative evidence. Impact was ultimately considered against the aims of the report: determining what was achieved as intended, what was not achieved, and any unintended impacts.
The methods consisted first of a literature review, to develop understanding of the background and terms of reference for the study. Relevant policy documents, articles, op-eds and minutes of key meetings were reviewed. A questionnaire with questions relating to influence to date, potential influence and barriers to influence across sectors was distributed to 50 individuals, in the five sectors. Questions asked the respondents to rank how influential they thought the report had been in different areas, from ‘no influence’ to a ‘very large influence’ (including a ‘don’t know’ option). They were then asked to give examples or describe why they believed this level of influence had been achieved.
Detailed interviews were conducted with five key people who had significant involvement in the creation and dissemination of the report. Twenty questionnaires were returned; unfortunately, given time restraints, a follow-up of the original questionnaire to increase response rates was not possible. In analysing feedback from questionnaires, the percentage of answers for each ranking were calculated. Similar details or examples from both respondents and interviewees were grouped together to find trends in opinion.
We recognised a positive bias could exist. Firstly, the writing of the assessment assumed an impact had occurred. To mitigate this problem, a ‘no influence’ option was included in the questionnaire. Secondly, the respondents that worked on creating the report, or those in close partnership with the writers, may give optimistic estimates of the report’s impact to validate their own work. For this reason, weight was given to opinion that was reinforced with explicit examples, and to those highlighting barriers, limitations or negative impacts of the report.
Results and discussion
Key findings.
In the assessment the three elements (initial, long-term, and potential) of impact were discussed for each of the five sectors, providing a specific and detailed account of ‘impact’ [ 13 ]. See Figure Figure2 2 for an overview of these findings. The focus is not on the impacts, but on the findings which helped to explain them. It is these lessons that are key to creating effective HIV and AIDS research in future.

A Summary of ‘Impacts’ from ‘Assessing the Impact of ‘Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era’
The significance of communication
The questionnaire asked, “What is the single most striking aspect of the report (e.g. a graph, a statistic, a statement)?” The graphs were singled out by respondents. Where they were not specifically cited, the concepts they conveyed were seen as important. One respondent answered, “A combination of statistics, graphical illustrations and words are used effectively to convey the message”, illustrating the clear use of these tools in the original report.
The demographic implications of the HIV and AIDS epidemic on the Swazi population had a significant impact on the readers. In particular respondents cited ‘Figure 8: Swaziland Population Pyramids’, in Whiteside and Whalley 2007 (shown below) and the concept that a permanent alteration of the structure of Swazi society has occurred. (Figure (Figure3) 3 ) [ 14 ]

Swaziland Population Pyramids 2000, 2025 and 2050
The application of Swaziland’s HIV prevalence rate to western countries, in Table 2 (page 8) of the report ‘stuck’ with some. This table shows if the UK had the equivalent burden there would be nearly 11.5 million British citizens infected. When presenting these data, it would be tailored to the audience – for example talking in Sweden the presenter said ‘Swaziland’s prevalence would be equivalent to 1.75 million Swedes being infected’.
It is unsurprising that such dramatic predictions of the effects of the epidemic on the structure of the population would strike the reader. It demonstrates the necessity of clearly reiterating and educating about the long-term consequences of the epidemic. Shortly after the publication of Reviewing Emergencies the government released preliminary data from the national 2007 census showing a decline in the population - 17, 489 fewer Swazis than in 1997 [ 15 ]. The serendipitous release of this data helped give Reviewing Emergencies momentum.
Successful dissemination was crucial, but wide dissemination is not the same as wide impact, and it cannot be assumed that the former naturally or inevitably leads to the latter [ 8 ]. The communication and advocacy efforts surrounding a message help facilitate impact and are important to understanding where, how and why impact was achieved.
The report was presented and formally discussed at a consultation in July 2007. It was available in print from October 2007, and a core set of power point slides was developed and presented to a range of organisations inside and beyond Swaziland. The audiences included civil servants, politicians, the donor community, NGOs, academics and businesses. Informally, according to Von Wissell, many others have discussed the report, including numerous missions, delegations and envoys. The report was made accessible online by HEARD [ 5 ] and NERCHA as well as UNAIDS [ 16 ], Relief Web [ 17 ], Food, Agriculture and Natural Resources Policy Analysis Network [ 18 ] and Aidsportal. (Table (Table1 1 )
The Dissemination of “Reviewing ‘Emergencies’ for Swaziland”, July 2007 to April 2008
Presentations in bold were conducted by Dr. Derek Von Wissell, Director of NERCHA, and those in italics by Professor Alan Whiteside of HEARD.
HEARD and NERCHA co-ordinated their efforts in communicating the findings. The delivery of the message itself was particularly significant. It had a coherence achieved by using the same slide set – presenters were ‘singing from the same song sheet.’ However, presentations were tailored to the audiences; Von Wissell presented to Swazi audiences in SiSwati; in Scandinavia the importance of donors was stressed.
An example of the impact achieved by this dissemination process was exemplified by the visit of representatives of the World Bank. In November 2007, the Human Development Vice President and Country Director from the World Bank visited Swaziland to assess first-hand the country’s situation in human development and HIV and AIDS. They met with key government officials including the Minister of Finance, and Von Wissell. It was here that Von Wissell presented Reviewing Emergencies. One World Bank official described the effect of this by saying, “It was NERCHA’s presentation that brought home the gravity of the HIV/AIDS situation in Swaziland”, and subsequently the World Bank sent a mission to Swaziland to explore next steps for the Bank. The presentation of the report’s findings was critical to this decision.
Engagement, timing and credibility
The work built on a long-term engagement of Whiteside and HEARD with Swaziland. This historical background is particularly important to both locate the research and the response to it. The timeline below shows the progression of HIV/AIDS in Swaziland through significant events and statistics, simultaneous to key examples of research conducted on the epidemic by HEARD and associates. As the timeline shows, Reviewing Emergencies built on three major reports in 1994, 2003 and 2006, which illustrated there was something going seriously wrong. Its message was credible - based on a history of research and evidence. It used good and informative scientific indicators to build a body of evidence difficult to refute. Furthermore, it was it was written at a critical time in Swaziland: with unusual levels of death; increasing numbers of orphans; and tuberculosis emerging as a major killer, the grim predictions of previous publications were no longer speculative, but reality [ 5 ]. (Figure (Figure4 4 )

HIV and AIDS in Swaziland and Key HEARD (or associated) Research 1986-2008
The timeline illustrates the progression of HIV/AIDS from Stage 1 to Stage 5 in less than 20 years using the concept idea of ‘Stages of the HIV/AIDS epidemic’ developed by Barnett and Whiteside (2002) [ 19 ]. As one interviewee reflected, “While, in many ways, Swaziland’s response has been admirable and unique, it is clear that the HIV prevention programmes have not worked thus far, and more importantly, that the social and economic implications of the epidemic have not been adequately thought through.” Reviewing Emergencies tried to explain the significance of the latter, hence filling a crucial gap in the research arena.
Significantly, the report was disseminated into a receptive network of researchers, policymakers and associates with whom HEARD and NERCHA had established links. As one respondent commented, “The wide network of individuals, organisations and donors with whom HEARD and NERCHA are affiliated were key to its wide reception”. The effectiveness of historic relationships such as these, built on both individual and institutional credibility cannot be underestimated. For example Whiteside had served on a UN Commission with the Deputy President of the World Bank, and is a Governor of a school in Swaziland; Von Wissell held the position of Minister of Trade and Industry and Minister of Health in previous governments. The message was delivered by people driven to see change and who could speak with authority. Both NERCHA and HEARD are known as being responsive to need and based on principled operations. In addition, the involvement of NERCHA - a Swazi based and Swazi run body - created an ‘ownership’ of the research and a further credibility to its message.
Terminology
The specific terminology used in research can both help and hinder the impact of a message. In Reviewing Emergencies the term and concept of a ‘long-wave emergency’ was particularly significant. A media respondent explained the term ‘emergency’ acted as a “hook”, giving journalists an attention-grabbing story, substantiated by genuine and shocking statistics. Titles such as ‘‘Swaziland: Declare HIV/AIDS a “humanitarian emergency”’ [ 20 ] and “When is HIV/AIDS a disaster?” [ 21 ] exemplify how the term renewed interest in the epidemic in Swaziland.
Conversely however, concerns over the term ‘emergency’ were discussed at length at the Low-Middle-Income Countries meeting hosted by HEARD in February 2008. One respondent explained, “There is some reluctance on the part of donors/NGOs/civil society/government to call HIV/AIDS an ‘emergency’ because there seems to be fear that terming it so will result in short-term funding for a long-term problem. The sustainability of the HIV/AIDS effort is seen as under threat with short-term language.” This meeting concluded there was a need to marry the urgency of the crisis with a long-wave understanding of the future impact of HIV/AIDS on the country, and that ‘emergencies’ may not be the best term to represent this [ 22 ]. A key message of the report is the long-wave nature of HIV and its impacts should be included in a new kind of thinking on emergencies. This debate will continue.
Barriers and tensions
Our assessment identified five key limitations: the role of government was not addressed; using Malawi and Zambia as comparator countries had mixed results; issues around timing; the status of AIDS (and Swaziland) on the international agenda; and finally the calls for radical change may not be achievable.
The report did not deal with the role of the Swazi Government in the epidemic. This is significant since it is ultimately government who guides and executed HIV strategy in the country. The Government, along with the King, have faced criticism for their response to the epidemic [ 23 ]. One respondent reminded us, the crisis “cannot be fixed with more funding alone.” Another discussed the structural difficulties in addressing the crisis, including the ‘vertical’ response, exemplified by a separate AIDS response council (NERCHA) which, it was claimed, failed to join up a national response.
The historic and legal relationship between HEARD, NERCHA and the Swazi Government restrained the report’s ability to criticise. Prescribing how Swaziland should respond to the crisis was never the intention of the paper. Whiteside argued that attempting to change the behaviour of the Swazi Government was beyond the scope of what a researcher from outside of the country should attempt: “That is for the people of Swaziland to do.” Working with the government in a ‘strategic alliance’, rather than against is more productive. Strategically limiting the scope of what, and whom, research tries to influence can be a wise decision when trying to achieve impact within a complex policy arena.
The report made comparisons between Swaziland and Zambia and Malawi, in order to demonstrate the scale of the emergency facing Swaziland. Despite the comparison having the desired effect of emphasising the scale of the Swazi’s crisis - some respondents referenced these comparative graphs as a striking and influential tool - it also had unintended consequences. Zambia and Malawi are both countries that, like Swaziland, compete for the attention of donors and development aid. By focusing all attention on Swaziland, the report appeared to belittle the issues faced by both Malawians and Zambians.
‘Time’ is no doubt a barrier to the impact of the report, since research is usually most influential when first published. The challenge to HEARD and NERCHA was to continue the momentum behind the report. One respondent warned that the report “may lack academic credibility if it is not followed up by further research that is able to collect primary data.” The report aimed for both an immediate awareness of Swaziland’s epidemic, and a longer-term discussion on emergencies and low-middle income classifications. It is the latter of these in particular that needs to be worked at or risk a ‘fizzling out’ as time marches on.
A number of significant international barriers threatened the impact of the report and indeed the issue of HIV/AIDS throughout Sub-Saharan Africa. Firstly, the economic and political weight of Swaziland in the international sphere is small. One frustrated interviewee described that “Swaziland is just not on the list”, as it is considered as insignificant by larger countries. Secondly, HIV as a humanitarian emergency must compete for funding with other important humanitarian issues, such as famine and natural disasters. One respondent described a ‘shift’ in global priorities to issues such as climate change, terrorism and the rising price of food. Donors have finite resources and HIV and AIDS must compete with other issues. HIV and AIDS was the global health issue receiving the most attention and funding but this will change, already a gap exists between pledges and funding [ 3 ].
Finally, the report called for a change within the framework that international organisations use to identify countries’ level of development - that of income classification. It further calls for a shift in the paradigm of thinking on emergencies. “Effectively what this report says is that it can’t be business as usual”. Changing entrenched ways of thinking is a major task [ 24 ].
Conclusions
‘Reviewing ‘Emergencies’ for Swaziland’ argued that socio-economic indicators show that the Swazi population is experiencing a humanitarian crisis comparable to countries besieged by conflict or struggling in the wake of a severe natural disaster. In the short-term, the report aimed to focus attention on Swaziland and what AIDS was doing to the country. It contributed to raising the profile of the plight of the Swazi people amongst donors and policy makers, described by one interviewee as a “catalyst for re-engagement”. In the medium-term, the report aimed to influence debate on the classification of low-middle income countries. This has proved more difficult. In the long-term, the report has seen some success in opening the debate on HIV/AIDS as a ‘long-wave emergency’. Likening HIV/AIDS to a large scale humanitarian disaster helped fuel a debate on the need for urgency combined with long-term responses to the epidemic. Donors, academics and NGOs have all engaged with the debate, but further advocacy and research is necessary to continue this, and see a shift in the current paradigm of thinking on what constitutes an ‘emergency.’
Developing a better understanding of the relationship between research and policy impact is vital to advancing the influence of SRH and HIV and AIDS research. Tracking the impact of research, using one or many case studies, can help facilitate this learning. Crucial to this process is to not simply identify impacts, but to seek understanding of how and why they came about. Of particular use for developing effective research in the future is identifying where intended impact has not been achieved and why. The assessment of the impact of Reviewing Emergencies attempted to do exactly this.
Drawing from the assessment, the following lessons may help inform future SRH and HIV/AIDS research. Communication is critical. The original work - collecting existing data to tell one clear story - is a striking way to demonstrate the reach and scale of disease impact; the demographic implications of AIDS powerfully communicated the severity of the epidemic; a targeted, tailored and cohesive dissemination effort helped facilitate the impact of research; sustained advocacy which is vital in keeping momentum for a message, should be reflected in planning and resources; further publications validating and extending a message are a good way to do this; and terminology can help or hinder the impact of a message.
Context and timing may be beyond the control of researchers but can significantly influence the uptake of research. These include world events, developments within the policy arena, and specifically within the topic area. If these conditions align in the favour of the research the impact may be much greater, therefore awareness of this, and careful timing of publications and advocacy efforts could maximise impact.
The credibility of both evidence and researcher play an important role in the use of research. Historical integrity of the evidence and an established researcher (or institution) can foster confidence in the use of research and increase the likelihood of it being used to inform policy. Established relationships and networks between individuals and institutions can guarantee an audience and encourage a dialogue on the findings. ‘Ownership’ of research, by the people it affects, is a powerful way to ensure both credibility and drive behind the message.
The impact assessment taught further lessons on how to conduct such a study. An assessment should ideally be planned in advance, facilitating the process of ‘tracking’ and information gathering; careful attention should be paid to the measurement and analysis process – if basing the study on qualitative data, how will this be analysed and how will the effects of bias be mitigated; the ‘net should be cast wide’ when considering areas of potential impact, recognising both the multiplicity of policy players and the potential for unintended impacts; understand that impacts may also change over time; and ultimately, to understand why an impact took place, the socio-cultural, political and economic context must be considered.
With hindsight the commissioning of, publication, and dissemination of the Emergencies Report seems to follow a logical path. The sense of frustration and the need to provide evidence led to this innovative work. It is our belief that it achieved many of its goals and spurred an international dialogue around the issues. The evaluation taught us additional lessons, which can be applied to help maximise the impact of research in the future.
Competing interests
This article critically reflects on a research project in which the authors have been involved.
Authors’ contributions
AW conceptualised the paper, and was co-author to the original study entitled ‘Reviewing ‘Emergencies’ for Swaziland’ (2007). AW also edited the manuscript. FH drafted the manuscript, with input from AW. FH was the author of the study ‘Assessing the Impact of ‘Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era’ (2008). Both authors read and approved the final manuscript.
Authors information
AW is Director of the health economics and HIV/AIDS Research Division (HEARD) at the University of KwaZulu-Natal. He has an MA from the School of Development Studies at the University of KwaZulu-Natal and a D Econ from the University of Natal.
FH has an MSc Development Management at the Department of International Development from the London School of Economics and MA Economics and Politics from Edinburgh University. She was a visiting fellow to HEARD in 2008.
Acknowledgements and funding
This work was supported by the DFID Research Partner’s Consortium (ABBA) and the donors of the Joint Funding Arrangement. The generous support of the staff of NERCHA is acknowledged. The responsibility for the contents and interpretation of the data remains with the authors.
This article has been published as part of Health Research Policy and Systems Volume 9 Supplement 1, 2011: Strengthening the research to policy and practice interface: exploring strategies used by research organisations working on sexual and reproductive health and HIV/AIDS. The full contents of the supplement are available online at http://www.health-policy-systems.com/supplements/9/S1 .
- Basu A, Srinivasan K. Foreign Direct Investment in Africa - Some Case Studies. Washington DC: IMF; 2002. [ Google Scholar ]
- Ministry of Health and Social Welfare. 10th Round of National HIV SeroSurveillance in Women Attending Antenatal Care. Mdabane: Government of Swaziland; 2006. [ Google Scholar ]
- Whiteside A. HIV/AIDS: A Very Short Introduction. Oxford: Oxford University Press; 2008. [ Google Scholar ]
- UNDP. Human Development Report 2006: Beyond Scarcity, power, poverty and the global water crisis. New York: United Nations; [ Google Scholar ]
- Whiteside A, Whalley A. Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era. Durban: HEARD; 2007. [ Google Scholar ]
- World Bank Development Indicators 2007. http://www.worldbank.org
- Molterberg E, Bergstrøm C. Our Common Discourse: Diversity and Paradigms in Development Studies (paper 1 of 2) Noragric, Working Paper Number 20. 2000.
- Davies H, Nutley S, Walter S. Approaches to assessing the non-academic impacts of social science research: Report of the ERSC symposium on assessing the non-academic impact of research. University of St. Andrews; 2005. [ Google Scholar ]
- Annual Report. Durban; 2008. Health Economics and HIV/AIDS Research Division. [ Google Scholar ]
- Sumner A, Perkins N, Lindstrom J. Multiple perspectives on research influence: does development research make a difference? A review. 2008. Unpublished.
- Islam Y, Garrett J. IFPRI and the abolition of the wheat flour ration shops in Pakistan: A case study on policymaking and the use and impact of research. Impact Assessment Discussion Paper Number One. Washington DC: IFPRI; 1997. [ Google Scholar ]
- Henry F. Assessing the Impact of ‘Reviewing ‘Emergencies’ for Swaziland: Shifting the Paradigm in a New Era. Durban: HEARD; 2008. [ Google Scholar ]
- US Census Bureau International Database 2007. http://www.census.gov/ipc/www/idb/
- CSO. 2006-2007 Swaziland Demographic and Health Survey. Mbabane: Government of Swaziland; 2007. [ Google Scholar ]
- UNIADS. http://data.unaids.org/pub/Report/2007/swaziland%20emergency%20report_final%20pdf_en.pdf
- Relief Web. http://www.reliefweb.int/rw/RWB.NSF/db900SID/KKAA-78W7DT?OpenDocument
- FANRPAN. http://www.fanrpan.org/documents/d00423/
- Barnett T, Whiteside A. AIDS in the 21st Century: Disease and Globalisation. Basingstoke: Palgrave; 2002. [ Google Scholar ]
- IRIN News. Swaziland: Declare HIV/AIDS a "humanitarian emergency". 2007. http://www.irinnews.org/Report.aspx?ReportId=75165
- Plus News. When is HIV/AIDS a Disaster? 2008. http://www.plusnews.org/Report.aspx?ReportId=78966
- Low-Middle-Income Countries Meeting. Minutes of the Meeting. Durban: HEARD; 2008. [ Google Scholar ]
- BBC. Swazi girls burn sex-ban tassles. 2005. http://news.bbc.co.uk/1/hi/world/africa/4175854.stm
- Gladwell M. The tipping point: how little things can make a big difference. Boston: Little, Brown and Company; 2002. [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Based on this case study and literature review, it is evident that co-infection presents typical clinical, diagnostic, and therapeutic features, and can be observed in the prognosis of the disease. Therefore, prospective studies are required to clarify gaps such as the efficacy of secondary prophylaxis and need for clinical and laboratory ...
This case was presented at the 11th Annual Workshop on Advanced Clinical Care-AIDS in Durban, South Africa, organized by Drs. Henry Sunpath and Mahomed-Yunus S. Moosa (Infectious Diseases Unit ...
CASE STUDY. A 35-year-old HIV-positive man was admitted to our hospital with intermittent fever for several months and chronic diarrhea. He was diagnosed HIV-positive 4 years earlier and had subsequently developed several AIDS-defining diseases such as Pneumocystis carinii pneumonia and CMV retinitis. Three months before admission the patient ...
This case is being presented as a case study which shows the potential of effective social rehabilitation and exploring utilisation of HIV-positives as a resource in our fight against this medico-social epidemic of HIV/AIDS. A case report on process involved in rehabilitation of HIV-positive children was reported in 2006 by Verma et al. 5
In two U.S. studies of PrEP use in persons 15 to 22 ... is considered on a case-by-case basis. ... the Division of HIV-AIDS Prevention, National Center for HIV-AIDS, Viral Hepatitis, Sexually ...
Zidovudine, a nucleoside reverse-transcriptase inhibitor used in the Pediatric AIDS Clinical Trials Group Protocol 076 study, was the first antiretroviral agent shown to reduce perinatal ...
HIV/AIDS is a pandemic condition—an epidemic of diseases that spreads across large areas like multiple continents or even worldwide . The first time AIDS was recognized was in the year 1981 by the United States Center for Disease Control and Prevention (CDC). Since the reported case of an individual who had successfully undergone a stem cell ...
Learn about the types, benefits, risks, and how to find HIV and AIDS clinical trials. These studies evaluate new medicines, vaccines, and other approaches to prevent, detect, or treat HIV and AIDS.
AIDS as a human crisis may lead to devastating psychological trauma and stress for patients. Therefore, it is necessary to study different aspects of their lives for better support and care. Accordingly, this study aimed to explain the lived experience of HIV-infected patients in the face of a positive diagnosis of the disease. This qualitative study is a descriptive phenomenological study.
In light of the increasing global burden of new HIV infections, growing financial requirements, and shifting funding landscape, the global health community must accelerate the development and delivery of an HIV cure to complement existing prevention modalities. An effective curative intervention could prevent new infections, overcome the limitations of antiretroviral treatment, combat stigma ...
Human immunodeficiency virus (HIV) is an infection that attacks the body's immune system. Acquired immunodeficiency syndrome (AIDS) is the most advanced stage of the disease. HIV targets the body's white blood cells, weakening the immune system. This makes it easier to get sick with diseases like tuberculosis, infections and some cancers.
Dugas and his family were vilified for years 2. But an analysis of HIV using decades-old blood serum samples exonerates the French Canadian, who died in 1984. The paper 3, published on 26 October ...
This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of an award (grant number U1OHA49824) totaling $1,700,000 with 0% financed with non-governmental sources.
JASL. Jamaica is home to both a generalized and concentrated HIV epidemic (27), with 1.3% of adults living with HIV in 2022 (28). Progress in the HIV response in Jamaica has stagnated, with only a 17% reduction in new HIV infections from 2010 and 2022 and a 4% increase in AIDS related deaths during this period (28).
Introduction People living with HIV (PLHIV) relied on community-based organizations (CBOs) in accessing HIV care and support during the COVID-19 pandemic in China. However, little is known about the impact of, and challenges faced by Chinese CBOs supporting PLHIV during lockdowns. Methods A survey and interview study was conducted among 29 CBOs serving PLHIV in China between November 10 and ...
Data. Data used for this study were drawn from Understanding the lives of adolescents and young adults (UDAYA), a longitudinal survey on adolescents aged 10-19 in Bihar and Uttar Pradesh 23.The ...
Interview with Dr. Anthony Fauci on progress made during the past four decades of the HIV/AIDS pandemic and ongoing efforts to end this threat. 18m 44s Download. The dramatic saga of the acquired ...
CNN —. On June 5, 1981, a curious report appeared in the Center for Disease Control's weekly public health digest: Five young, gay men across Los Angeles had been diagnosed with an unusual ...
ommunity. We assessed whether a modified Project Bridge model was effective for increasing rates of HIV treatment engagement, antiretroviral therapy receipt, and adherence for community-dwelling individuals supervised on probation and parole. Setting: Baltimore, Maryland Methods: In this study, the 18-month outcomes of a randomized controlled trial in which PLWH were also on probation or ...
DOI: 10.1590/S0036-46652013000600010. Abstract. in English, Portuguese. Report of a 45-year-old male farmer, a resident in the forest zone of Pernambuco, who was diagnosed with human immunodeficiency virus (HIV) in 1999 and treated using antiretroviral (ARV) drugs. In 2005, the first episode of visceral leishmaniasis (VL), as assessed by ...
The study research team included HIV specialists of a large infectious disease hospital in Beijing, their affiliated and long-term CBO partner "Home of Red Ribbon (HRR)," staff of the Joint United Nations Programme on HIV/AIDS (UNAIDS) Beijing office, and global health researchers from Georgetown University and the RAND Corporation, an ...
This article presents the case of an HIV-positive patient who presented the treating physician, a psychiatrist, with an ethical dilemma. We provide the details of the case, identify the ethical issues it raises, and examine the ethical principles involved. In their article, "Confidentiality in the Age of AIDS," Martin L. Smith and Kevin P. Martin present a complex case in clinical ethics.
An HIV vaccine candidate elicited trace levels of HIV broadly neutralizing antibodies and high levels of other key immune cells in an early-stage clinical trial. This immune response is an important signal that, if antibody levels can be further amplified, the vaccination strategy might be able to prevent HIV.
HIV/AIDS continues to be one of the leading global health challenges, having claimed over 40 million lives so far. People infected with HIV are more likely to develop depression, leading to several negative behavioural and clinical outcomes. Studies have reported exceptionally high prevalence of depressive symptoms among people living with HIV/AIDS (PLWHA), making a case for integrating mental ...
In this case-control study involving 199 individuals living with HIV-1 and 200 HIV-uninfected controls, we conducted genotyping of IL-6/IL-6R SNPs using TaqMan real-time PCR assays. Soluble IL-6 levels were measured using ELISA. No associations were found between the investigated SNPs and HIV infection.
Despite progress in several countries, we are still not on track to end the AIDS epidemic by 2030. In 2022, about 4000 adults and children acquired HIV each day — a total of 1.3 million new HIV infections. Lifesaving antiretroviral therapy can also prevent HIV by suppressing the virus in a person's blood to an untransmissible level, but 9.2 ...
From the initial case of AIDS combined with chronic hepatitis B, through the diagnosis and treatment of multidrug-resistant tuberculosis, the development of liver failure and disseminated cryptococcosis, and ultimately the concurrent occurrence of IRIS, the entire process was tortuous but ultimately resulted in a good outcome (Fig. 4 ...
Background. Swaziland is experiencing the world's worst HIV and AIDS epidemic. Prevalence rose from four percent of antenatal clinic attendees in 1992 to 42.6 percent in 2004. The Report 'Reviewing 'Emergencies' for Swaziland: Shifting the Paradigm in a New Era' published in 2007 bought together social and economic indicators.
The events marked the release of, Adolescents in a changing world - The case for urgent investment, a landmark report which finds that failure by stakeholders to increase investments in programmes targeted at improving adolescent well-being would result in staggering social and economic costs.The report, commissioned by PMNCH, working with Victoria Institute of Strategic Economic Studies ...
The 1,701-square-foot West House is the only Case Study House in the neighborhood oriented to capture ocean views. "When people walk in the door, their jaws drop," says Doe.