Our use of cookies
We use necessary cookies to make our site work. We'd also like to set optional cookies to help us measure web traffic and report on campaigns.
We won't set optional cookies unless you enable them.
Cookie settings

Mental Health
- Entry year 2024
- Duration Part time 4 - 7 years
An international first, the PhD in Mental Health meets the needs of those wishing to gain a deep and critical insight into mental health theory, research and practice and to develop or enhance research skills whilst fulfilling their existing responsibilities. The programme is offered part-time and combines innovative distance learning with face-to-face teaching at an annual autumn Academy held in Lancaster.
The programme brings together the theory and practice of mental health, including psychological models of psychological disorders, evidence-based interventions and current priorities for mental health. Whether you are based within a healthcare setting, local government, education, research or management, the PhD in Mental Health is your chance to work with world-leading academics on the production of a thesis that makes an original contribution to knowledge within your area of professional practice.
This part-time, flexible doctorate runs over a minimum of four and a maximum of seven years. The programme begins with a compulsory five-day Induction Academy in Lancaster. Each of the subsequent academic years start with a compulsory three-day autumn Academy, while the rest of the course is delivered via e-learning. Attendance at the annual academies is compulsory until students have been confirmed on the PhD programme
Years 1 and 2 consist of taught modules delivered online. In Year 1 students take a specialist module that covers the theory and practice of mental health followed by a module on research philosophy and a module on research design. Year 2 modules may include: Systematic Reviews, Data Analysis, Research Design and Practical Research Ethics.
From Year 3 onwards, students undertake an independent research study , which will conclude with the submission of a thesis that makes an original contribution to knowledge. The research project will be supervised from the University but undertaken in students’ own location or workplace. Supervision meetings take place using video conferencing software such as Skype. During the annual autumn Academy students meet with supervisors face to face.
A number of mental health research groups work from Lancaster University’s prestigious Division of Health Research. For example, the Spectrum Centre, which has attracted more than £6m in funding since its launch, is the only specialist research centre in the UK dedicated to translational research into the psychosocial aspects of bipolar disorder and associated conditions (including recurrent depression, anxiety, and psychosis), as well as developments in their treatment. Other staff research interests include mental health in people with chronic physical conditions or difficulties and ensuring positive mental health among socially marginalised groups.
Our close links to NHS mental health services in the North West of England and the voluntary sector, both regionally and nationally, combine with the current research interests of staff to inform the content of our modules. Service users will also be actively involved in the delivery of the taught component of your Doctorate.
Your department
- Division of Health Research Faculty of Health and Medicine
- Telephone +44 (0)1524 592032
Mental Health Research at Lancaster University
Professor Steve Jones introduces Mental Health research at Lancaster University, and our multi-facetted approach to understanding mental health. He discusses how the Faculty's research influences practice, changing the debate around mental health and ultimately improving outcomes.
Entry requirements
Academic requirements.
2:1 Hons degree (UK or equivalent) in an appropriate subject and relevant work experience.
We may also consider non-standard applicants, please contact us for information.
If you have studied outside of the UK, we would advise you to check our list of international qualifications before submitting your application.
Additional Requirements
As part of your application you will also need to provide a viable research proposal. Guidance for writing a research proposal can be found on our writing a research proposal webpage.
English Language Requirements
We may ask you to provide a recognised English language qualification, dependent upon your nationality and where you have studied previously.
We normally require an IELTS (Academic) Test with an overall score of at least 6.5, and a minimum of 6.0 in each element of the test. We also consider other English language qualifications .
Contact: Admissions Team +44 (0) 1524 592032 or email [email protected]
Course structure
You will study a range of modules as part of your course, some examples of which are listed below.
Information contained on the website with respect to modules is correct at the time of publication, but changes may be necessary, for example as a result of student feedback, Professional Statutory and Regulatory Bodies' (PSRB) requirements, staff changes, and new research. Not all optional modules are available every year.
The aim of this module is to provide students with an advanced introduction to the methods commonly used in health research. Students will gain knowledge and understanding of:
- How to use Moodle for distance learning and engage with peers and staff online
- Using the library as a distance learning student
- How to search the literature
- Using End Note
- How to synthesise evidence
- Standards of academic writing
- The nature of plagiarism and how to reference source material correctly
- Theoretical perspectives in health research
- The practical process of conducting research
- How to formulate appropriate questions and hypotheses
- How to choose appropriate methodology
- Quantitative and qualitative research method
- Research ethics
- Disseminating and implementing research into practice
- Programme-specific research.
e-learning distance module
Autumn Term (weeks 1-10, October – December)
Credits: 30
Mode of assessment : 3000 word essay (75%) and a poster (25%).
This module is an introduction to current topics and issues in mental health, covering theory (mechanisms underlying mental health), practice (psychosocial approaches to treating mental health problems), contemporary issues in mental health, and up-to-date research relating to these important topic areas.
Deadline: January
Spring Term (weeks 1-10, January-March)
Mode of assessment : 5000 word essay
This module explores the philosophical underpinnings of research. It begins with an introduction to epistemology, i.e. the philosophical basis of knowledge and its development. It then considers the influence of different epistemological bases on research methodology and explores the role of theory and theoretical frameworks in the research process. It also examines the nature of the knowledge that underpins evidence-based policy and practice and introduces the fundamental principles of ethics.
Deadline: April
Sunmer Term (weeks 1-10, April-June)
Mode of assessment : 5000 word assignment consisting of two 2500 word components
This module introduces a range of methods used in health research. The focus is on justifying research design choices rather than practical skills in data analysis. The starting point is the development of meaningful and feasible research questions. The module then introduces a range of quantitative research designs and quantitative approaches to data collection. Next, the module looks at qualitative research designs and their relation to different epistemological positions. How to integrate quantitative and qualitative methods into mixed methods research is being discussed next. The module also explores issues such as sampling and quality across different research designs.
Deadline: July
Spring term (weeks 1-10, January-March)
Mode of assessment : two pieces of written work (Qualitative data analysis, 2500 words; Quantitative data analysis, 2500 words)
This module is an introduction to the theory and practice of qualitative and quantitative data analysis. The module consists of two distinct parts: qualitative data analysis and quantitative data analysis. Within each part, there will be an option to take an introductory or an advanced unit.
The introductory quantitative unit covers data management and descriptive analyses and introduces students to inferential testing in general and statistical tests for comparisons between groups specifically. The advanced quantitative unit covers linear regression as well as regression methods for categorical dependent variables and longitudinal data before exploring quasi-experimental methods for policy evaluation and finally providing an opportunity to discuss more specific regression methods such count data models or duration analysis.
The introductory qualitative unit focusses on the technique of thematic analysis, a highly flexible approach and useful foundation for researchers new to qualitative data analysis. The unit takes students through the stage of a qualitative data analysis: sorting and organising qualitative data, interrogating qualitative data, interpreting the data and finally writing accounts of qualitative data. The advanced qualitative unit introduces students to alternative techniques such as narrative analysis or discourse analysis.
Summer Term (weeks 1-10, April-June)
Mode of assessment : A written assignment that includes: a) a 4000 word research proposal and b) a completed FHMREC ethics application form and supporting documents.
This module completes the taught phase of Blended Learning PhD programmes. It enables students to put everything they have learned so far together and produce a research proposal that will provide the basis for the research phase of the programme.
The first part of the module – research design – starts by discussing the components of a research proposal according to different epistemologies and research methods. It then takes students through the process of developing their own proposal, starting with the topic and epistemological framework, through to the study design and data collection methods and finally the practical details.
The second part of the module – practical research ethics – teaches students how to think about their research proposal from an ethical perspective. It covers ethical guidelines and teaches students how to identify the purpose of a guideline, to enable them to translate their proposal into an ethical review application. Finally, students will prepare a practice research ethics application using the FHMREC ethics application form.
Autumn term (weeks 1-10, October-December)
Mode of assessment : 5000 word assignment
This module provides an introduction to the principles and components of systematic reviewing. It takes students through the key steps of a systematic review. The starting point of the module is the construction of an appropriate review question. Next, the module discusses the (iterative) process of creating a search strategy that successfully identifies all relevant literature. The module then moves on to selecting appropriate methodological quality criteria, enabling students to develop their skills in critically appraising studies. After discussing how to prepare a data extraction form the module introduces a key component of a systematic review: synthesising the evidence. Finally, the module will teach students how to put everything together in a systematic review protocol.
Fees and funding
Home Fee £4,350
International Fee £11,340
General fees and funding information
There may be extra costs related to your course for items such as books, stationery, printing, photocopying, binding and general subsistence on trips and visits. Following graduation, you may need to pay a subscription to a professional body for some chosen careers.
Specific additional costs for studying at Lancaster are listed below.
College fees
Lancaster is proud to be one of only a handful of UK universities to have a collegiate system. Every student belongs to a college, and all students pay a small College Membership Fee which supports the running of college events and activities. Students on some distance-learning courses are not liable to pay a college fee.
For students starting in 2023 and 2024, the fee is £40 for undergraduates and research students and £15 for students on one-year courses. Fees for students starting in 2025 have not yet been set.
Computer equipment and internet access
To support your studies, you will also require access to a computer, along with reliable internet access. You will be able to access a range of software and services from a Windows, Mac, Chromebook or Linux device. For certain degree programmes, you may need a specific device, or we may provide you with a laptop and appropriate software - details of which will be available on relevant programme pages. A dedicated IT support helpdesk is available in the event of any problems.
The University provides limited financial support to assist students who do not have the required IT equipment or broadband support in place.
For most taught postgraduate applications there is a non-refundable application fee of £40. We cannot consider applications until this fee has been paid, as advised on our online secure payment system. There is no application fee for postgraduate research applications.
For some of our courses you will need to pay a deposit to accept your offer and secure your place. We will let you know in your offer letter if a deposit is required and you will be given a deadline date when this is due to be paid.
The fee that you pay will depend on whether you are considered to be a home or international student. Read more about how we assign your fee status .
If you are studying on a programme of more than one year’s duration, tuition fees are reviewed annually and are not fixed for the duration of your studies. Read more about fees in subsequent years .
Similar courses
Health studies.
- Clinical Psychology DClinPsy
- Dementia Studies PhD
- Health Data Science MSc
- Health Data Science PhD
- Health Economics and Policy MSc
- Health Economics and Policy PhD
- Health Research PhD
- Organisational Health and Well-Being PhD
- Palliative Care PhD
- Public Health PhD
Take an innovative approach to distance learning combining interactive lectures, webinars and online collaboration, group work and self-directed study.
Work with world-leading academics to make an original contribution to your area of professional practice.
Benefit from an international peer group that could include educators, mental health practitioners and policy-makers.
Studying by blended learning
The PhD in Mental Health is offered part-time via blended learning . Teaching and research activities are carried out through a combination of face-to-face and online interaction, allowing you to undertake the majority of study from your own location whilst fulfilling your existing responsibilities. You will benefit from being part of a UK and internationally-based peer group working across a range of sectors.
Face-to-face interactions take place at an annual residential autumn Academy while taught modules are delivered via distance learning using our virtual learning environment and include discussion forums, collaborative digital spaces and video conferencing. All students have access to a hub space that facilitates interaction with their cohort and with students on related programmes, creating a virtual information space that’s also sociable. An academic tutor will support you during the taught phase and two supervisors provide you with support in the research phase.

The Division of Health Research
The Division of Health Research have been offering blended learning postgraduate programmes since 2010. We have many successful graduates and currently around 200 continuing students on a range of programmes who have benefited in progressing their careers from the high quality postgraduate education we provide.
Our Research in Mental Health
Our mental health research covers a wide range of research areas and activities, including bipolar disorder and related conditions, chronic illness and care approaches.

The Spectrum Centre
The Spectrum Centre is the only specialist research centre in the UK dedicated to translational research into the psychosocial aspects of bipolar disorder and associated conditions.

Athena SWAN: Gender Equality at Lancaster
We hold the Athena SWAN Silver Award, recognising our commitment to advancing the careers of women in higher education and research.

Important Information
The information on this site relates primarily to 2024/2025 entry to the University and every effort has been taken to ensure the information is correct at the time of publication.
The University will use all reasonable effort to deliver the courses as described, but the University reserves the right to make changes to advertised courses. In exceptional circumstances that are beyond the University’s reasonable control (Force Majeure Events), we may need to amend the programmes and provision advertised. In this event, the University will take reasonable steps to minimise the disruption to your studies. If a course is withdrawn or if there are any fundamental changes to your course, we will give you reasonable notice and you will be entitled to request that you are considered for an alternative course or withdraw your application. You are advised to revisit our website for up-to-date course information before you submit your application.
More information on limits to the University’s liability can be found in our legal information .
Our Students’ Charter
We believe in the importance of a strong and productive partnership between our students and staff. In order to ensure your time at Lancaster is a positive experience we have worked with the Students’ Union to articulate this relationship and the standards to which the University and its students aspire. View our Charter and other policies .
Why Lancaster?

League tables and reputation
A highly-ranked university with a global reputation.

Colleges and community
Your college will be your home away from home.

Careers and employability
Career support for our students through university and beyond.

Student life
Lancaster has so much to offer. On our campus, in our city and in our community, you’ll find your place – whoever you are.

Where is Lancaster?
Lancaster is easy to get to and surrounded by natural beauty.

The campus and the city
Our campus and the surrounding area is a great place to call home.

Your global experience
Build your global community on campus and around the world.

Wellbeing and support
Services to help you fulfil your potential at Lancaster.

Alternatively, use our A–Z index

Attend an open day
PhD/MPhil Mental Health / Programme details
Year of entry: 2024
- View full page
Programme description
Our PhD/MPhil Mental Health programme enables you to undertake a research project that will improve understanding of Mental Health.
Our postgraduate research programmes in mental health are based on individually tailored projects. Applicants are specifically matched with a primary academic supervisor according to their research interest and background.
All of our postgraduate research students have more than one supervisor, and our dynamic multidisciplinary supervisory teams typically cover a wide and diverse range of academic disciplines beyond mental health and psychology, including nursing, pharmacy, epidemiology and biostatics, informatics, health economics, sociology and qualitative research.
Our academics have internationally outstanding knowledge and expertise in conducting research studies in mental health across the life course. Particular strengths include:
- severe mental disorders such as schizophrenia and bipolar disorder (including the prodromal stages of these conditions);
- depression;
- anxiety disorders;
- personality disorders;
- autism spectrum disorder;
- attachment disorders;
- self-harm and suicide;
- homicide and other forms of interpersonal violence;
- forensic mental health;
- neurobiological and imaging studies;
- mental health epidemiology;
Special features
Training and development
All of our postgraduate researchers attend the Doctoral Academy Training Programme delivered by the Researcher Development team . The programme provides key transferable skills and equips our postgraduate researchers with the tools to progress beyond their research degree into influential positions within academia, industry and consultancy. The emphasis is on enhancing skills critical to developing early-stage researchers and professionals, whether they relate to effective communication, disseminating research findings and project management skills.
Teaching and learning
Applicants are specifically matched with a Primary Supervisor and individual project based on their research interests and background.
International applicants interested in this research area can also consider our PhD programme with integrated teaching certificate .
This unique programme will enable you to gain a Postgraduate Certificate in Teaching and Learning, whilst also carrying out independent research on your chosen project.
Scholarships and bursaries
Funded programmes and projects are promoted throughout the year. Funding is available through UK Research Councils, charities and industry. We also have other internal awards and scholarships for the most outstanding applicants from within the UK and overseas.
For more information on available the types of funding we have available, please visit the funded programmes and funding opportunities pages.
What our students say
Disability support.
Welcome to the Midlands Mental Health and Neurosciences PhD Programme for Healthcare Professionals
The Midlands hosts the most innovative centres in mental health and neurosciences (MH&N), including digital mental health, clinical trials, neuroimaging, and epidemiology, serving an area of huge clinical need.
The Midlands Mental Health & Neurosciences PhD Programme is led by the University of Nottingham, in collaboration with University of Birmingham, University of Leicester, and University of Warwick, and our local NHS Trusts in the Midlands.
The Programme
In a research environment that is dynamic, socially inclusive, and supportive, our Doctoral Training Programme (DTP) will develop an excellent, multidisciplinary, multi-professional researchers and an inter-sectoral research Midlands hub, facilitating adult learning, developing research and leadership skills, independent and critical thinking, and sharing of ideas, and teamwork.
Our PhD scholars will undertake excellent challenge-led research encompassing MH&N discovery science to translational and applied health research, covering the human lifespan and taking a bio-psycho-social approach, commensurate with the complex presentations, experiences, interventions, and impact of mental ill-health.
Our PhDs are funded by the generous contribution of Wellcome in collaboration with our DTP universities.

- NHS salary for three years (based on current pay) – Employing Trusts will be paid this money to backfill the PhD student’s time on the Programme.*
- Home (UK) rate tuition fees for three years
- Generous research costs
- Generous funds for additional training
- Travel costs for research
- PhD students are permitted to undertake up to 0.2 FTE clinical work to maintain their clinical skills, which will be paid for by the Programme
*Funding for salaries is based on average NHS pay bands for different healthcare professionals, which Wellcome has used to fund this programme. We may be able to accommodate funding above the average pay bands, but this will be dealt with on a case-by-case basis.

Our vision, with inclusivity at its core, is to develop the next generation of multi-skilled research leaders amongst healthcare professionals from diverse cultural backgrounds and professions to conduct excellent research and advance knowledge in MH&N, paving the way to better patient, family, and carer care; community empowerment; and social development.
Develop the next generation of multidisciplinary clinical academics in mental health & neurosciences (MH&N)
Conduct and disseminate world-leading research
Create and sustain an ambitious Midlands-based, internationally connected, compassionate clinical-academic ecosystem, collaborating to address the key contemporary mental health challenges
Our Guiding Principles
High quality research.
We will support our scholars to undertake high-quality research, that is going to answer the key questions the scholars seek to address. Through rigorous peer review and links with experts in the field nationally and internationally, we will ensure that the PhD projects are of the highest quality.
Equality, Diversity and Inclusion (EDI)
We are committed to Advance HE’s Guiding Principles of the Race Equality Charter and Athena Swan Charter , and strive to follow their Good Practice Initiatives . We strongly encourage applications from those groups who are underrepresented in different healthcare professions and those with lived experience of mental health difficulties.
Improvement and innovation through continuous evaluation
We have several years of experience running different DTPs, but we believe in self-improvement and we want to ensure that the PhD programme is tailored to the needs to our PhD scholars. Through regular consultation with our PhD scholars, supervisors, and our PPI members, we will learn about what is considered good practice and where we need to do better.
Interdisciplinarity and Team Science
Our scholars will be addressing in their research large and complex MH&N challenges, which requires teamwork and input from different professional groups and experts in different research methods. We strongly encourage interdisciplinarity. Scholars will have the opportunity to develop their skills and research projects with the input from experts from multiple disciplines, thereby enabling innovation within their own healthcare professional group. Our Team Science approach ensures that our PhD scholars get the benefits of working as part of a team, where the contributions of each member of the team are recognised.
Patient and Public Involvement (PPI)
PPI is core to our DTP and to all our scholars’ projects. PPI offers researchers:
- An improved understanding of what is important to patients and the public about a specific area/topic
- An alternative point of view
- An early indication of whether people would want to participate in the study (or how to improve the experience of participating in a study), and
- Guidance regarding dissemination of their research findings.
PPI will be expected at every stage of the scholar’s PhD journey, from the conceptualisation of the project to the dissemination plans. Scholars may also have a PPI member as part of their advisory team.
- Accessibility Tools
- Current Students
- Postgraduate
- Postgraduate Research Programmes
- School of Health and Social Care Postgraduate Research Courses
Mental Health, Ph.D. / M.Phil.
- An introduction to postgraduate study
- Postgraduate Taught Courses
- Postgraduate scholarships and bursaries
- Contact the Postgrad Admissions team
- Scholarships and Bursaries
- Research projects
- Postgraduate Research Programmes coming soon
- How to apply for your Postgraduate Research programme
- School of Aerospace, Civil, Electrical and Mechanical Engineering Research Courses
- School of Biosciences, Geography and Physics Postgraduate Research Courses
- School of Culture and Communication Postgraduate Research Courses
- School of Engineering and Applied Sciences Postgraduate Research Courses
- Gerontology and Ageing Studies, PhD/MPhil
- Health and Wellbeing, MSc by Research
- Health Economics, PhD/MPhil/MSc by Research
- Health Policy, PhD/MPhil
- Health Sciences, PhD/MPhil
- Healthcare Management, PhD/MPhil
- Mental Health, PhD/MPhil
- Nursing, PhD/MPhil
- Public Health, PhD/MPhil
- Social Work and Social Care, PhD/MPhil
- Children and Young People, PhD/MPhil
- School of Law Postgrad Research Courses
- School of Management Postgraduate Research Courses
- School of Mathematics and Computer Science Postgraduate Research Courses
- Medical School Postgraduate Research Courses
- School of Psychology Postgraduate Research Courses
- School of Social Sciences Postgraduate Research Courses
- Fees and Funding
- How to Apply For Your Postgraduate Course
- Postgraduate Fees and Funding
- Postgraduate Open Days
- Apply Online
- Postgraduate Careers and Employability
- Accommodation
- Postgraduate Study Video Hub
- Why study at Swansea
- Academi Hywel Teifi
- Student life
- Student Services
- Information for parents and advisors
- Enrolment, Arrivals and Welcome
- Postgraduate Enquiry
- Postgraduate programme changes
- Meet our postgraduate students
- Postgraduate Prospectus
- Fast-track for current students
Are you a UK or International Student?
Develop and evaluate effective evidence-based mental health services, key course details, course overview.
Start dates: 1st October, 1st January, 1st April, 1st July.
Developing and evaluating effective evidence-based mental health services to support people at some of the most challenging times of their lives depends on high-quality research.
Studying for a PhD in Mental Health will give you the opportunity to pursue your own personal or professional research interests in this vital field while contributing to new ways of thinking about mental health care, services, and policy.
Over the course of your studies, you will develop and enhance transferable skills such as problem-solving, project management, and critical thinking that are valued in any professional setting.
As a student at our School of Health and Social Care, you will benefit from a dynamic and supportive research environment with many opportunities to make connections across disciplines and develop links with organisations and policymakers both in the UK and abroad. As such, you can be confident that your research will inform and be informed by the wider health and social care environment.
According to the most recent Research Excellence Framework in 2014-2021, over 75% of the research carried out at the school was of international or world-leading quality.
Currently, students are looking at evidence-based practices in mental health (in particular early intervention services), care co-ordination in forensic mental health care and the influence of service user participation in professional role development.
Recent research funding and collaboration partners include:
- Welsh Government
- Public Health Wales
- European Union
- Amgen Europe
- Ministry of Defence
- GlaxoSmithKline Biologicals
- British Medical Association
- National Institute for Social Care and Health Research
- Astrazeneca
- The Wellcome Trust.
You will be joining a university that was named ‘University of the Year’ and ‘Postgraduate’ runner up in the What Uni Student Choice Awards 2019.
Entry Requirements
Qualifications MPhil: Applicants for MPhil must normally hold an undergraduate degree at 2.1 level (or Non-UK equivalent as defined by Swansea University). See - Country-specific Information for European Applicants 2019 and Country-specific Information for International Applicants 2019 .
PhD : Applicants for PhD must normally hold an undergraduate degree at 2.1 level and a master’s degree. Alternatively, applicants with a UK first class honours degree (or Non-UK equivalent as defined by Swansea University) not holding a master’s degree, will be considered on an individual basis. See - Country-specific Information for European Applicants 2019 and Country-specific Information for International Applicants 2019 .
English Language IELTS 6.5 Overall (with no individual component below 6.5) or Swansea University recognised equivalent. Full details of our English Language policy, including certificate time validity, can be found here.
As well as academic qualifications, Admissions decisions may be based on other factors, including (but not limited to): the standard of the research synopsis/proposal, performance at interview, intensity of competition for limited places, and relevant professional experience.
Reference Requirement
As standard, two references are required before we can progress applications to the College/School research programme Admissions Tutor for consideration.
Applications received without two references attached are placed on hold, pending receipt of the outstanding reference(s). Please note that any protracted delay in receiving the outstanding reference(s) may result in the need to defer your application to a later potential start point/entry month, than what you initially listed as your preferred start option.
You may wish to consider contacting your referee(s) to assist in the process of obtaining the outstanding reference(s) or alternatively, hold submission of application until references are sourced. Please note that it is not the responsibility of the University Admissions Office to obtain missing reference(s) after our initial email is sent to your nominated referee(s), requesting a reference(s) on your behalf.
The reference can take the form of a letter on official headed paper, or via the University’s standard reference form. Click this link to download the university reference form .
Alternatively, referees can email a reference from their employment email account, please note that references received via private email accounts, (i.e. Hotmail, Yahoo, Gmail) cannot be accepted.
References can be submitted to [email protected] .
How you are Supervised
Find out more about some of the academic staff supervising theses in this area:
Professor Michael Coffey
Dr Ian Beech
Dr Julia Terry
Welsh Provision
Tuition fees, ph.d. 3 year full time, ph.d. 6 year part time, m.phil. 2 year full time, m.phil. 4 year part time.
Tuition fees for years of study after your first year are subject to an increase of 3%.
You can find further information of your fee costs on our tuition fees page .
You may be eligible for funding to help support your study. To find out about scholarships, bursaries and other funding opportunities that are available please visit the University's scholarships and bursaries page .
International students and part-time study: It may be possible for some students to study part-time under the Student Visa route. However, this is dependent on factors relating to the course and your individual situation. It may also be possible to study with us if you are already in the UK under a different visa category (e.g. Tier 1 or 2, PBS Dependant, ILR etc.). Please visit the University information on Visas and Immigration for further guidance and support.
Current students: You can find further information of your fee costs on our tuition fees page .
Funding and Scholarships
You may be eligible for funding to help support your study.
Government funding is now available for Welsh, English and EU students starting eligible postgraduate research programmes at Swansea University. To find out more, please visit our postgraduate loans page.
To find out about scholarships, bursaries and other funding opportunities that are available please visit the University's scholarships and bursaries page.
Academi Hywel Teifi at Swansea University and the Coleg Cymraeg Cenedlaethol offer a number of generous scholarships and bursaries for students who wish to study through the medium of Welsh or bilingually. For further information about the opportunities available to you, visit the Academi Hywel Teifi Scholarships and Bursaries page.
Additional Costs
Access to your own digital device/the appropriate IT kit will be essential during your time studying at Swansea University. Access to wifi in your accommodation will also be essential to allow you to fully engage with your programme. See our dedicated webpages for further guidance on suitable devices to purchase, and for a full guide on getting your device set up .
You may face additional costs while at university, including (but not limited to):
- Travel to and from campus
- Printing, photocopying, binding, stationery and equipment costs (e.g. USB sticks)
- Purchase of books or texts
- Gowns for graduation ceremonies
How to Apply
Details of the application process for research degrees are available here , and you can apply online and track your application status at www.swansea.ac.uk/applyonline . As part of your application you should include a research proposal outlining your proposed topic of study. Guidance on writing a research proposal is also available .
You can expect to be interviewed following your application to discuss your topic of research and to demonstrate the necessary level of commitment to your studies and training.
It is advisable that you contact us before submitting your application. This will ensure we can identify appropriate supervisors, and where necessary work with you to refine your proposal. If you would like to do this you should contact [email protected] .
If you're an international student, find out more about applying for this course at our international student web pages
Suggested Application Timings
In order to allow sufficient time for consideration of your application by an academic, for potential offer conditions to be met and travel / relocation, we recommend that applications are made before the dates outlined below. Please note that applications can still be submitted outside of the suggested dates below but there is the potential that your application/potential offer may need to be moved to the next appropriate intake window.
October Enrolment
UK Applicants – 15th August
EU/International applicants – 15th July
January Enrolment
UK applicants – 15th November
EU/International applicants – 15th October
April Enrolment
UK applicants – 15th February
EU/International applicants – 15th January
July Enrolment
UK applicants – 15th May
EU/International applicants – 15th April
EU students - visa and immigration information is available and will be regularly updated on our information for EU students page.
PhD Programme Specification
This Programme Specification refers to the current academic year and provides indicative content for information. The University will seek to deliver each course in accordance with the descriptions set out in the relevant course web pages at the time of application. However, there may be situations in which it is desirable or necessary for the University to make changes in course provision , either before or after enrolment.
Programme Summary
This PhD in Mental Health at Swansea will enable you to undertake a substantial project led by your own interests. It is a highly respected qualification which can present a career in academia or a wider scope for employment in fields such as education, government or the private sector. A thesis of 100,000 words will be submitted for assessment demonstrating original research with a substantive contribution to the subject area. The PhD is examined following an oral examination of the thesis (a viva voce examination or viva voce). You will acquire research skills for high-level work and skills and training programmes are available on campus for further support. There will be an opportunity to deliver presentations to research students and staff at departmental seminars and conferences. There may also be opportunities to develop your teaching skills through undergraduate tutorials, demonstrations and seminars.
Programme Aims
This PhD programme will provide doctoral researchers with:
- The opportunity to conduct high quality postgraduate research in a world leading research environment.
- Key skills needed to undertake advanced academic and non-academic research including qualitative and quantitative data analysis.
- Advanced critical thinking, intellectual curiosity and independent judgement.
Programme Structure
The programme comprises three key elements:
- Entry and confirmation of candidature
- Main body of research
- Thesis and viva voce
The programme comprises of the undertaking of an original research project of 3 years duration full time (6 years duration part time). Doctoral researchers may pursue the programme either full time or part time by pursuing research at the University at an external place of employment or with/at a University approved partner.
Doctoral researchers for the PhD in Mental Health are examined in two parts.
The first part is a thesis which is an original body of work representing the methods and results of the research project. The maximum word limit is 100,000 for the main text. The word limit does not include appendices (if any), essential footnotes, introductory parts and statements or the bibliography and index.
The second part is an oral examination (viva voce).
Doctoral Researcher Supervision and Support
Doctoral researchers will be supervised by a supervisory team. Where appropriate, staff from Colleges/Schools other than the ‘home’ College/School (other Colleges/Schools) within the University will contribute to cognate research areas. There may also be supervisors from an industrial partner.
The Primary/First Supervisor will normally be the main contact throughout the doctoral research journey and will have overall responsibility for academic supervision. The academic input of the Secondary Supervisor will vary from case to case. The principal role of the Secondary Supervisor is often as a first port of call if the Primary/First Supervisor becomes unavailable. The supervisory team may also include a supervisor from industry or a specific area of professional practice to support the research. External supervisors may also be drawn from other Universities.
The primary supervisor will provide pastoral support. If necessary the primary supervisor will refer the doctoral researcher to other sources of support (e.g. Wellbeing, Disability, Money Advice, IT, Library, Students’ Union, Academic Services, Student Support Services, Careers Centre).
Programme Learning Outcomes
Upon successful completion of this programme, doctoral researchers should be able to:
Knowledge & Understanding
- Demonstrate the systematic acquisition and understanding of a substantial body of knowledge which is at the forefront of research through the development of a written thesis.
- Create, interpret, analyse and develop new knowledge through original research or other advanced scholarship.
- Disseminate new knowledge gained through original research or other advanced scholarship via high quality peer reviewed publications within the discipline.
- Apply research skills and subject theory to the practice of research.
- Apply process and standards of a range of the methodologies through which research is conducted and knowledge acquired and revised.
Attitudes and values
- Conceptualise, design and implement a project aimed at the generation of new knowledge or applications within Mental Health.
- Make informed judgements on complex issues in the field of Mental Health, often in the absence of complete data and defend those judgements to an appropriate audience.
- Apply sound ethical principles to research, with due regard for the integrity of persons and in accordance with professional codes of conduct.
- Demonstrate self-awareness of individual and cultural diversity, and the reciprocal impact in social interaction between self and others when conducting research involving people.
Research Skills
- Respond appropriately to unforeseen problems in project design by making suitable amendments.
- Communicate complex research findings clearly, effectively and in an engaging manner to both specialist (including the academic community), and non-specialist audiences using a variety of appropriate media and events, including conference presentations, seminars and workshops.
- Correctly select, interpret and apply relevant techniques for research and advanced academic enquiry.
- Develop the networks and foundations for on-going research and development within the discipline.
- Implement advanced research skills to a substantial degree of independence.
- Locate information and apply it to research practice.
Skills and Competencies
- Display the qualities and transferable skills necessary for employment, including the exercise of personal responsibility and largely autonomous initiative in complex and unpredictable situations, in professional or equivalent environments.
Progression Monitoring
Progress will be monitored in accordance with Swansea University regulations. During the course of the programme, the Doctoral researcher is expected to meet regularly with their supervisors, and at most meetings it is likely that the doctoral researcher’s progress will be monitored in an informal manner in addition to attendance checks. Details of the meetings should ideally be recorded on the on-line system. A minimum of four formal supervision meetings is required each year, two of which will be reported to the Postgraduate Progression and Awards Board. During these supervisory meetings the doctoral researcher’s progress is discussed and formally recorded on the on-line system.
Learning Development
The University offers training and development for Doctoral Researchers and supervisors ( https://www.swansea.ac.uk/research/undertake-research-with-us/postgraduate-research/training-and-skills-development-programme/ ).
Swansea University’s Postgraduate Research Training Framework is structured into sections, to enable doctoral researchers to navigate and determine appropriate courses aligned to both their interest and their candidature stage.
There is a training framework including for example areas of Managing Information and Data, Presentation and Public Engagement, Leadership and working with others, Safety Integrity and Ethics, Impact and Commercialisation and Teaching and Demonstrating. There is also range of support in areas such as training needs, literature searching, conducting research, writing up research, teaching, applying for grants and awards, communicating research and future careers.
A range of research seminars and skills development sessions are provided within the School of Health and Social Care and across the University. These are scheduled to keep the doctoral researcher in touch with a broader range of material than their own research topic, to stimulate ideas in discussion with others, and to give them opportunities to such as defending their own thesis orally, and to identify potential criticisms. Additionally, the School of Health and Social Care is developing a research culture that aligns with the University vision and will link with key initiatives delivered under the auspices of the University’s Academies, for example embedding the HEA fellowship for postgraduate research students.
Research Environment
Swansea University’s research environment combines innovation and excellent facilities to provide a home for multidisciplinary research to flourish. Our research environment encompasses all aspects of the research lifecycle, with internal grants and support for external funding and enabling impact/effect that research has beyond academia.
Swansea University is very proud of our reputation for excellent research, and for the calibre, dedication, professionalism, collaboration and engagement of our research community. We understand that integrity must be an essential characteristic of all aspects of research, and that as a University entrusted with undertaking research we must clearly and consistently demonstrate that the confidence placed in our research community is rightly deserved. The University therefore ensures that everyone engaged in research is trained to the very highest standards of research integrity and conducts themselves and their research in a way that respects the dignity, rights, and welfare of participants, and minimises risks to participants, researchers, third parties, and the University itself.
In the School of Health and Social Care we are strongly focused on the translation of our research into real-life benefits for users, carers and professionals across the range of health and social care services. In doing so our staffs has long established links with a range of international networks and similar university departments in Europe and around the world, and are committed to building productive relationships with front-line policymakers and practitioners. Some senior researchers have also been embedded within the NHS to ensure healthcare and service provision is developed and informed by high quality robust research.
Alongside this we play an integral role in the Welsh Government’s research infrastructure, through the Centre for Ageing & Dementia Research, Wales School for Social Care Research and the Welsh Health Economic Support Service, increasing the volume of research taking place within Wales. While some of our PhD programmes form part of the ESRC Doctoral Training Centre for Wales, a pan-Wales collaboration to train top-level social scientists. Our funding also comes from a wide range of prestigious funders such as the Research Councils, European research programmes, Government, Ministry of Defence, professional bodies, private sector and charitable organisations, with the school securing £7.37m of funding across the last three years.
Supporting our staff and students in their research is a range of facilities including our Health and Wellbeing Academy, which provides healthcare services to the local community, a range of clinical and audiology suites and state-of-the-art research facilities. These include a high density EEG suite, a fully-fitted sleep laboratory, a social observation suite, eye-tracking, psychophysiological, tDCS and conditioning labs, a lifespan lab and baby room, and over 20 all-purpose research rooms.
Career Opportunities
Having a PhD demonstrates that graduates can work effectively in a team, formulate, explore and communicate complex ideas and manage advanced tasks. Jobs in academia (eg postdoctoral research, lecturing), education, government, management, the public or private sector are possible. Examples include administrators, counsellors, marketing specialists, and researchers.
The Postgraduate Research Office Skills Development Team offer support and a training framework for example in creating a researcher profile based upon publications and setting up your own business. The Swansea Employability Academy assists students in future career opportunities, improving CVs, job applications and interview skills.
MPhil Programme Specification
Programme Summary
This MPhil in Mental Health at Swansea will enable you to undertake a substantial project led by your own interests. It is a highly respected qualification which can present a career in academia or a wider scope for employment in fields such as education, government or the private sector. A thesis of 60,000 words will be submitted for assessment demonstrating original research with a substantive contribution to the subject area. The Masters is examined following an oral examination of the thesis (a viva voce examination or viva). You will acquire research skills for high-level work and skills and training programmes are available on campus for further support. There will be an opportunity to deliver presentations to research students and staff at departmental seminars and conferences.
This Masters programme will provide students with:
- Thesis and viva voce examination
The programme comprises of the undertaking of an original research project of 2 years duration full time (4 years duration part time). Students may pursue the programme either full time or part time by pursuing research at the University at an external place of employment or with/at a University approved partner.
Students for the Masters in Mental Health are examined in two parts.
The first part is a thesis which is an original body of work representing the methods and results of the research project. The maximum word limit is 60,000 for the main text. The word limit does not include appendices (if any), essential footnotes, introductory parts and statements or the bibliography and index.
The second part is an oral examination ( viva voce ).
Supervision and Support
Students will be supervised by a supervisory team. Where appropriate, staff from Colleges/Schools other than the ‘home’ College/School (other Colleges/Schools) within the University will contribute to cognate research areas. There may also be supervisors from an industrial partner.
The Primary/First Supervisor will normally be the main contact throughout the student journey and will have overall responsibility for academic supervision. The academic input of the Secondary Supervisor will vary from case to case. The principal role of the Secondary Supervisor is often as a first port of call if the Primary/First Supervisor becomes unavailable. The supervisory team may also include a supervisor from industry or a specific area of professional practice to support the research. External supervisors may also be drawn from other Universities.
The primary supervisor will provide pastoral support. If necessary the primary supervisor will refer the student to other sources of support (e.g. Wellbeing, Disability, Money Advice, IT, Library, Students’ Union, Academic Services, Student Support Services, Careers Centre).
Upon successful completion of this programme, doctoral researchers should be able to:
- Demonstrate the systematic acquisition and understanding of a substantial body of knowledge through the development of a written thesis.
- Create, interpret, analyse and develop new knowledge through original research or other advanced scholarship.
- Apply process and standards of a range of the methodologies through which research is conducted and knowledge acquired and revised.
- Make informed judgements on complex issues in the field of Mental Health often in the absence of complete data and defend those judgements to an appropriate audience.
- Communicate complex research findings clearly, effectively and in an engaging manner to both specialist (including the academic community), and non-specialist audiences using a variety of appropriate media.
- Correctly select, interpret and apply relevant techniques for research and academic enquiry.
- Develop the foundations for on-going research and development within the discipline.
- Implement independent research skills.
- Display the qualities and transferable skills necessary for employment, including the exercise of personal responsibility and initiative in complex situations.
Progress will be monitored in accordance with Swansea University regulations. During the course of the programme, the student is expected to meet regularly with their supervisors, and at most meetings it is likely that the student’s progress will be monitored in an informal manner in addition to attendance checks. Details of the meetings should ideally be recorded on the on-line system. A minimum of four formal supervision meetings is required each year, two of which will be reported to the Postgraduate Progression and Awards Board. During these supervisory meetings the student’s progress is discussed and formally recorded on the on-line system.
Swansea University’s Postgraduate Research Training Framework is structured into sections, to enable students to navigate and determine appropriate courses aligned to both their interest and their candidature stage.
A range of research seminars and skills development sessions are provided within the School of Health and Social Care and across the University. These are scheduled to keep the student in touch with a broader range of material than their own research topic, to stimulate ideas in discussion with others, and to give them opportunities to such as defending their own thesis orally, and to identify potential criticisms. Additionally, the School of Health and Social Care is developing a research culture that will align with the University vision and will link with key initiatives delivered under the auspices of the University’s Academies, for example embedding the HEA fellowship for postgraduate research students
Research Environment
Swansea University’s Research Environment combines innovation and excellent facilities to provide a home for multidisciplinary research to flourish. Our research environment encompasses all aspects of the research lifecycle, with internal grants and support for external funding and enabling impact/effect that research has beyond academia.
Swansea University is very proud of our reputation for excellent research, and for the calibre, dedication, professionalism, collaboration and engagement of our research community. We understand that integrity must be an essential characteristic of all aspects of research, and that as a University entrusted with undertaking research we must clearly and consistently demonstrate that the confidence placed in our research community is rightly deserved. The University therefore ensures that everyone engaged in research is trained to the very highest standards of research integrity and conducts themselves and their research in a way that respects the dignity, rights, and welfare of participants, and minimises risks to participants, researchers, third parties, and the University itself.
College of Human and Health Sciences
In the School of Health and Social Care we are strongly focused on the translation of our research into real-life benefits for users, carers and professionals across the range of health and social care services. In doing so our staff have long established links with a range of international networks and similar university departments in Europe and around the world, and are committed to building productive relationships with front-line policymakers and practitioners. Some senior researchers have also been embedded within the NHS to ensure healthcare and service provision is developed and informed by high quality robust research.
Having a Master of Philosophy degree shows that you can communicate your ideas and manage tasks. Jobs in academia, education, government, management, the public or private sector are possible.
- 1" class="nav-item" v-on:click="getDoc($event, item['0C13'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 1
- 1" class="nav-item" v-on:click="getDoc($event, item['0C14'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 2
- 1" class="nav-item" v-on:click="getDoc($event, item['0C15'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 3
- 1" class="nav-item" v-on:click="getDoc($event, item['0C16'].replaceAll(/ ]*?>/g, ''))"> Progress report - year 4
- 1" class="nav-item" v-on:click="getDoc($event, item['0C17'].replaceAll(/ ]*?>/g, ''))"> Progress report - final
1" v-html="item['0C7']">
Supervisor(s):
1">Read 's thesis online at
')" v-html="p">
Project abstract
Project aims, progress report - year 1, progress report - year 2, progress report - year 3, progress report - year 4, progress report - final year, mental health research uk, the first uk charity dedicated to raising funds for research into mental illnesses, their causes and cures., since 2008, we have ....
in scholarships
research students
research publications
Mental Health Research UK aims to make a significant improvement to the lives of people with mental illness, by funding research into causes and cures. We know it is often challenging to find resources to support PhD studentships and that is why we focus our funding on these awards, supporting mental health researchers of the future.
Although only registered with the Charity Commission in 2008, Mental Health Research UK has already made research awards; the first being funded jointly with the University of Nottingham.
Select the sub-headings below to learn more ...
What we fund
We fund research into:
- The underlying causes of mental ill health
- Treatments for mental health problems
We do not fund research into autism or dementia. Nor do we fund research that involves laboratory animals.
Mental Health Research UK has one competitive round of PhD Scholarship awards per year, launched in the spring, for submission in May, with decisions made in the autumn to start the following year. The annual timeline is as follows:
- March: Scholarships are advertised via our mailing list and listed on our website.
- Mid-May: Closing date for applications.
- July: The panel meets and shortlists applications. Those not shortlisted are informed at once. References and service user reports are organized.
- September: Deadline for the receipt of references and service user reports.
- Late September: The panel meets and selects applicants to be offered a scholarship.
- October: All applicants are notified of the outcome of their application by the end of the month.
Research topics
Mental Health Research UK makes research awards focusing on research into the causes of, or cures for, mental illnesses.
The specific research topics of interest are selected year-on-year by the Trustees. However, the Schizophrenia Research Fund John Grace QC PhD Scholarship award always focuses on Schizophrenia.
Our awards cover fees and stipend only and are based on the Medical Research Council’s minimum stipend and fees for UK students, currently as follows:
2023/24 stipend: Outside London: £18,662; Inside London: £20,622
2023/24 fees: £4,712
Funding will cease at 4 years or on submission of the PhD thesis, whichever is earlier.
The fourth year is regarded as a ‘writing up’ year and the grant will be the stipend and thesis fee only.
In the event of early submission, a brief application to retain the student for the remainder of the period within the total cost envelope will be considered. College fees will be considered, where advertised by the university as being in addition to the tuition fee.
Mental Health Research UK will consider a small grant towards travel and conference allowances, where the student is presenting, subject to prior approval. No contribution will be made towards Research Training and Support grants.
If your university fees or stipend are different from the above, we will consider these provided you advise us with your application.
MD(Res) awards
Please note that applications are not currently being considered.
The Trustees of Mental Health Research UK have, since 2018, supported the MD(Res) degree at the Institute of Psychiatry, Psychology and Neuroscience (IOPPN) at King's College, London.
Mental Health Research UK wishes to support young psychiatrists with an interest in mental health research by offering scholarships for this programme because we need to encourage more people to develop careers within academic psychiatry. We are keen to provide a supportive community within Mental Health Research UK for all our scholars, which the MD(Res) award holders will join. This will help doctors thrive in their studies and ensure progress is made towards improving the lives of people with mental health problems, through scientific advances.
Dr Gareth Owen, Chair of the MD(Res) committee, IOPPN said:
"Doctors working in mental health sometimes come to research questions later in their careers with the benefit of clinical experience and training. It is hugely important that their experience and research energy is tapped and academic awards make a real difference to enabling such innovation. These awards from MHRUK are an excellent way to bring clinical experience and high quality research supervision together to foster an exciting new cohort of clinical academics in mental health."
Eligibility
Applications for our awards need to come from UK universities. Research supervisors must be based at UK universities.
We accept one application per scholarship award from any one university. A university may apply for more than one scholarship if they wish.
Please note that we do not accept any requests for funding from individuals, including current PhD students.
User and carer involvement
Best practice will be followed to ensure that service users and carers are involved at all stages with the prioritization of research topics and the commissioning of research.
All research project applications will be peer-reviewed by service user reviewers as well as academic reviewers.
NIHR and NHS information
Mental Health Research UK is a National Institute for Health Research (NIHR) non-commercial Partner . This means the studies that we fund may be eligible to access the NIHR Study Support Service which is provided by the NIHR Clinical Research Network. The NIHR Clinical Research Network can now support health and social care research taking place in non-NHS settings, such as studies running in care homes or hospices, or public health research taking place in schools and other community settings. Read the full policy: Eligibility Criteria for NIHR Clinical Research Network Support . In partnership with your local R&D office, we encourage MHRUK award holders to involve your local NIHR Clinical Research Network team in discussions as early as possible when planning your study. This will enable you to fully benefit from the support available through the NIHR Study Support Service.
If your study involves NHS sites in England or Wales you will need to apply for Health Research Authority (HRA) and Health and Care Research Wales (HCRW) Approval .
Open Access publication of research results
Students can download our application form for open access publication of research results here .
PhD Competition 2025
Mental Health Research UK (incorporating the Schizophrenia Research Fund) is pleased to announce a competition for 2 PhD Scholarships beginning September 2025.
We are inviting applications for PhD scholarships under the theme of maternal mental health . We view this topic in its broadest sense inviting proposals that cover all aspects of mental health during pregnancy and in the first year afterwards. We are interested in proposals that aim to understand causes, risk factors, mechanisms, or treatments. MHRUK does not fund health services research.
John Grace QC scholarship 2025: Maternal mental health
The John Grace QC scholarship should focus on psychotic disorders, including puerperal psychosis.
MHRUK scholarship 2025: Maternal mental health
The second scholarship is open, and we invite applications on topics such as post-natal depression, developing post-natal family mental health interventions, factors influencing maternal mental health.
We invite applications from UK Universities for these scholarships. The deadline for applications is midnight on 27th May 2024.
The full terms and conditions can be found here .
If you have any queries regarding the application process, please read the guidance above and check our FAQs document . If this does not provide the information that you need, please contact [email protected] .
Please note that for each individual scholarship we can accept only one application per university. A university may apply for more than one scholarship if they wish.
Scholarships Awarded
Find out more about the scholarships that we have awarded..
Use the buttons below to filter the list.
1" span v-html="item['0C7']">
Select from the tags below to filter by topic:
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 09 December 2021
Nationwide assessment of the mental health of UK Doctoral Researchers
- Cassie M. Hazell 1 ,
- Jeremy E. Niven 2 ,
- Laura Chapman 3 ,
- Paul E. Roberts 4 ,
- Sam Cartwright-Hatton 3 ,
- Sophie Valeix 2 &
- Clio Berry 5
Humanities and Social Sciences Communications volume 8 , Article number: 305 ( 2021 ) Cite this article
8631 Accesses
15 Citations
106 Altmetric
Metrics details
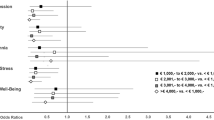
Doctoral Researchers (DRs) are an important part of the academic community and, after graduating, make substantial social and economic contributions. Despite this importance, DR wellbeing has long been of concern. Recent studies have concluded that DRs may be particularly vulnerable to mental health problems, yet direct comparisons of the prevalence of mental health problems between this population and control groups are lacking. Here, by comparing DRs with educated working controls, we show that DRs report significantly greater anxiety and depression, and that this difference is not explained by a higher rate of pre-existing mental health problems. Moreover, most DRs perceive poor mental health as a ‘normal’ part of the PhD process. Thus, our findings suggest a hazardous impact of PhD study on mental health, with DRs being particularly at risk of developing common mental health problems. This provides an evidence-based mandate for universities and funders to reflect upon practices related to DR training and mental health. Our attention should now be directed towards understanding what factors may explain heightened anxiety and depression among DRs so as to inform preventative measures and interventions.
Similar content being viewed by others

Doctoral researchers’ mental health and PhD training satisfaction during the German COVID-19 lockdown: results from an international research sample

Prevalence of mental health symptoms and potential risk factors among Austrian psychotherapists

A cross-sectional study of the health status of Swiss primary care physicians
Introduction.
University research makes a substantial contribution to the economy (University Alliance, 2014 ). A significant part of that contribution is driven by Doctoral Researchers (DRs), also known as PhD students, who consistently produce a reliable financial return on any investment in their studies, both to their institution and to industry more widely (Casey, 2009 ; EPSRC, 2010 ; Zolas et al., 2015 ). When asked during their PhD studies, the majority of DRs want to pursue a career in research post-PhD (Cornell, 2020 ). However, in reality, subsequent to receiving their PhD, more than 70% leave academia completely (Hancock, 2020 ); instead pursuing careers in industry, government or non-profit organisations (Cornell, 2020 ). A key motivator for DRs leaving academia is to protect their mental health (Metcalfe et al., 2018 ). Therefore, the poor mental health of DRs and their subsequent exodus from academia will have implications for the volume and quality of academic research, as well as having broader social and economic impacts.
The issue of DR mental health was well evidenced in a recent international survey by Nature (Woolston, 2019 ). The survey found that 36% of current DRs reported seeking help for anxiety and/or depression (Woolston, 2019 ), with further editorials acknowledging the poor mental health of PhD students (Nature, 2019b , 2019a ; Woolston, 2020 ). A recent meta-analysis found that DRs are moderately more stressed when compared to whole population normative data (Hazell et al., 2020 ). The available research all points in the same direction: DRs are stressed and experiencing poor mental health, and may be leaving the profession as a result of this (Hazell et al., 2020 ). However, there are significant limitations and gaps in the understanding of DR mental health (Hazell et al., 2020 ). In particular, we do not know whether DRs are at a higher risk of poor mental health than individuals who chose other career pathways because studies largely did not include comparison groups.
One recent study did attempt to address this gap in the field (Levecque et al., 2017 ); employing an online survey, this study revealed that DRs reported greater psychological distress than both undergraduate students and educated employees. However, this study, along with all others in the field (Hazell et al., 2020 ), did not assess symptoms indicative of Serious Mental Illness (SMI) diagnoses. Instead, this study (Levecque et al., 2017 ) used the General Health Questionnaire 12 (GHQ12) (Goldberg et al., 1997 ), which has been widely criticised for encouraging response biases, lack of reliability, and limited clinical validity (Hankins, 2008a , 2008b ; Ye, 2009 ). Finally, to our knowledge, no studies have addressed the issue of causality. That is, whether those with existing poor mental health might be more attracted to pursuing PhD studies or whether studying for the PhD itself is the cause of mental health difficulties.
To address these limitations, we conducted a UK-based mixed-methods online survey with DRs, and a control group comprised of similarly aged, educated working professionals (WP). The central aim of our study was to determine how the prevalence of mental health problems differs between DRs and WPs. Secondary to this, we aimed to assess DRs’ perceptions of the commonality of mental health problems. Our survey employed outcomes measures with well-established clinical cut-offs and included measures that capture SMI symptoms i.e. mania and suicidality. We also controlled for pre-existing mental health problems, which allowed us to test whether our data support PhD study as causative of mental health problems.
Participants
We recruited DRs and a matched group of educated WPs. To be eligible for inclusion in the DR group, participants had to be currently studying for their PhD at a UK University. The eligibility criteria for the WP group were developed to ensure similarity between the two groups, other than PhD status. Eligibility criteria, therefore, reflected the minimum entry requirements for PhD programmes in the UK. WPs had to be aged 21 years or over and possess a university undergraduate degree of 2.1 or above. Moreover, WPs had to be working in the UK at least 3 days a week (0.6 full time equivalent (FTE)) as this matched the minimum FTE for a part-time PhD.
Recruitment
To recruit DRs, we emailed every Doctoral School in the UK ( N = 162) asking them to share details of the study with their students. To recruit WPs, we emailed the public relations departments of the top 100 graduate employers and the top 500 UK businesses. None of the graduate employers confirmed that they had disseminated the survey details. Additionally, we promoted the study via the project social media outlets, Prolific Academic and paid advertisements on Facebook. As part of the debrief information, we asked participants to share details of the survey with their personal and professional networks.
The study is an online, cross-sectional survey. We used a between-group design, comparing responses from DRs to WPs. The survey was administered using Qualtrics survey software.
We collected data using a battery of measures of mental health problems and psychological and social functioning. In the present paper, we report comparative data on prevalence and symptomatology for DRs and WPs.
Demographics
Participants were asked to self-identify as either a DR or a WP and then complete basic demographic questionnaires. DRs were asked for information about their PhD, including funding status and whether they were engaging in fieldwork. WPs were asked to classify the type of job they have and how likely they were to complete a PhD in the future.
As part of the demographic questionnaire, we asked participants about their mental health, including whether they have a mental health diagnosis, and whether they have experienced a mental health crisis. With the aim of assessing premorbid mental health, we adapted interview questions from the Composite International Diagnostic Interview (CIDI) (Kessler and Üstün, 2004 ), in which lifetime prevalence participants are asked to reflect on key milestones across the lifespan and whether they were experiencing mental health problems at that time. Using milestones to determine the onset of mental health problems is associated with increased accuracy of retrospective data (Kessler et al., 2005 ). We provided participants with a series of milestones related to their studies and work history and asked them to indicate whether they were experiencing mental health problems at that time or not, for example while at secondary school, before they started an undergraduate degree, while completing an undergraduate degree and so on.
Perceived mental health problem commonality and impact
We asked DR participants only to respond to several statements assessing DRs’ perceptions of the commonality and impact of mental health problems, for example, whether they thought it was the norm to experience mental health difficulties during a PhD, and whether they had considered or had actually taken time away from their studies in relation to mental health. These statements had the following response options: true, false, or not sure.
Patient Health Questionnaire 9 (PHQ-9)
The PHQ-9 is widely used in UK primary healthcare as a depression screening tool (Spitzer et al., 1999 ). The PHQ-9 has 9 items which are scored by participants using a 4-point Likert scale from ‘not at all’ (0) to ‘nearly every day’ (4). A higher score indicates greater depression symptoms. The scale has strong internal consistency (Cronbach’s α = 0.89) and well-established cut-off criteria delineating clinical from sub-clinical levels of depression (Kroenke et al., 2001 ). In the present sample, we also found the PHQ-9 to have good scale reliability (Cronbach’s α = 0.89).
Generalised Anxiety Disorder 7 (GAD-7)
Akin to the PHQ-9, the GAD-7 (Spitzer et al., 2006 ) is used in UK primary healthcare settings as a screening tool for anxiety/GAD. The GAD-7 has 7 items, scored by participants on a 4-point Likert scale, ranging from ‘not at all’ (0) to ‘nearly every day’ (4). A higher score indicates greater anxiety symptoms. The scale has strong internal consistency (Cronbach’s α = 0.92) with well-established cut-off scores distinguishing those with clinical and sub-clinical levels of anxiety (Spitzer et al., 2006 ). We found similar levels of scale reliability in the current sample (Cronbach’s α = 0.90).
Altman Self-Reported Mania Scale (ASRMS)
The 5-item ASRMS measures symptoms of mania (Altman et al., 1997 ). Each item has a 5-point Likert scale with unique anchor points. A higher score indicates greater mania. The scale has acceptable levels of internal consistency (Cronbach’s α = 0.65) (Altman et al., 1997 ), which was replicated in the current sample (Cronbach’s α = 0.66). The scale reliability could not be improved by removing any of the items.
Suicidal Behaviours Questionnaire-Revised (SBQ-R)
The SBQ-R (Osman et al., 2001a ) comprises four items; each captures a different facet of suicidality and all combine to provide an assessment of overall suicide risk. Each of the items has its own Likert Scale and scoring system. A higher score indicates greater suicide risk. The SBQ-R has good internal consistency (all Cronbach α s > 0.70), with a score of 7 or above amongst a general population sample indicating a high risk of suicide (Osman et al., 2001a ). The scale reliability found here exceeds that reported by Osman et al. ( 2001a , 2001b ) (Cronbach’s α = 0.81).
Participants were able to access the online survey via a weblink provided. After being presented with the participant information screen, participants were asked to provide consent by completing a ‘tick box’ form. Participants were next asked to complete an eligibility screening questionnaire. Eligible participants were then invited to complete the questionnaire battery. Because of the sensitive nature of the measures, all of the questions were optional. At the end of the survey, participants were presented with debriefing information and invited to enter a prize draw for one of two iPad minis.
This study received ethical approval from the University of Sussex Sciences and Technology Cross-Schools Research Ethics Committee (C-REC) on the 19 December 2017 (Reference: ER/CH283/9).
Analysis plan
Data analyses were conducted using SPSS version 25. We first calculated the descriptive statistics for all of the demographic items and clinical measures. Means and standard deviations are provided for continuous variables, and frequencies and percentages are given for categorical variables. Missing data were examined by performing a forced entry logistic regression with complete (complete questionnaire battery) versus missing data (demographic data present only) as the outcome variable, and key demographics entered as predictors. Specifically, we included age, and dummy codes for gender (females versus all other genders, males versus all other genders, and other gender versus male or female), ethnicity (White British versus all other ethnicities, and White versus all other ethnicities), disability (versus no disability), and profession (DRs versus WPs) as predictors. None of the sample characteristics significantly predicted whether data were missing or complete (i.e. age, female versus non-females, males versus non-male, other gender versus non-other, White British versus non-White British, White versus non-White, disabled versus not disabled, and group; all p s > 0.05).
Our research questions were tested first by calculating the frequencies and percentages of DRs that endorsed specific statements related to mental health. Second, we conducted an independent samples t -test comparing the reported age of mental health problem onset between DRs and WPs. This analysis was supplemented with chi-square tests to compare the milestone (life phase) at which symptoms reportedly emerged between DRs and WPs. Where any significant interactions were identified, these were further explored using the distribution of counts.
Finally, we performed a one-way independent-groups MANCOVA with a Bonferroni correction. Our grouping variable compared DRs and WPs. We entered four dependent variables into the model: depression (PHQ-9 total), anxiety (GAD-7 total), mania (ASMRS total), and suicidality (SBQ-R total). To control for confounding variables, we entered age, gender (dummy coded as female versus male and other; male versus female and other; and other versus female and male), disability status (reporting a disability versus not), ethnicity (White British versus all other ethnicities; and White versus non-White), and mental health history (reported a history of mental health problems versus no history) as covariates.
In total, 4608 participants were included in the analysis of whom 3352 were DRs and 1256 WPs (see Fig. 1 and Table 1 ). Based on figures from the Higher Education Statistics Agency (HESA, 2019 ), our sample represented ~3.29% of the total UK DR population. The majority of DRs agreed that developing a mental health problem during a PhD is ‘the norm’ and that most of their peers had experienced mental health problems (Table 2 ). More than a third of DRs (35.8%) had considered ending and/or taking a break from their studies due to poor mental health. Just over 14% of DRs had formally intermitted due to mental health problems.
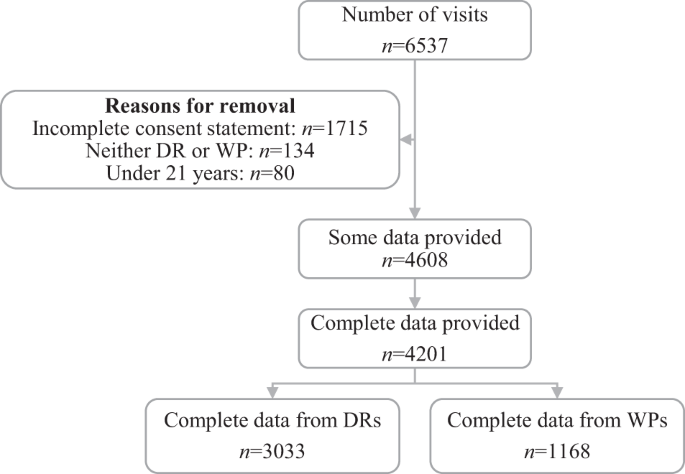
Note: Complete data here is classed as any participant where they provided some level of demographic data and complete data for at least one of the clinical outcome measures. WP working professionals, DR doctoral researchers.
Lifetime prevalence
DRs reported a greater lifetime prevalence of mental health difficulties than WPs ( χ 2 (1) = 18.39, p < 0.001; φ c = 0.06), but this difference was no longer present when considering only a history of professionally diagnosed mental health problems ( χ 2 (1) = 0.00, p = 0.99; φ c < 0.01).
Timing of symptom onset
There was no difference between DRs and WPs in terms of the age at which mental health problems began ( t (946.51) = 0.58, p = 0.56) (Table 3 ). However, there was a small significant difference between DRs and WPs in terms of the life phase at which mental health problems first emerged ( χ 2 (5) = 26.09, p < 0.001; φ c < 0.10). Compared to WPs, DRs generally had a later onset of mental health problems ( i.e . starting during or after undergraduate studies). This association remained when the analysis was replicated with participants who did ( χ 2 (5) = 14.16, p = 0.02; φ c < 0.10) or did not report having been given a formal mental health problem diagnosis ( χ 2 (5) = 12.82, p = 0.03; φ c < 0.10).
Prevalence of mental health problems
Clinical cut-offs.
The prevalence of probable depressive disorders, as assessed using the PHQ9 (Spitzer et al., 1999 ) ( χ 2 (4) = 41.74, p < 0.001; φ c = 0.10), and prevalence of probable Generalised Anxiety Disorder (GAD) ( χ 2 (3) = 98.47, p < 0.001; φ c = 0.15), as assessed using the GAD7 (Spitzer et al., 2006 ), was significantly greater amongst DRs than WPs. Moderate to severe presentations of depression and anxiety were more common amongst DRs, whereas having no or mild symptoms was more typical amongst WPs.
By contrast, the probable risk of mania, as measured by the ASRMS (Altman et al. 1997 ), was greater amongst WPs than DRs ( χ 2 (1) = 33.61, p < 0.001; φ c = 0.09). That is, a high probability of mania was more prevalent amongst WPs whereas being at no risk of mania was more common amongst DRs. There was no difference between WPs and DRs in terms of suicide risk as measured using the Suicidal Behaviours Questionnaire—Revised (SBQ-R) (Osman et al., 2001a ) ( χ 2 (1) = 1.28, p = 0.26; φ c = 0.02).
Symptom severity
When turning to mental health symptoms (as opposed to probable diagnoses), overall symptomology was significantly greater for DRs compared to WPs ( Λ = 0.98, F (4, 3737) = 22.60, p < 0.001). Specifically, the severity of depression ( F (1, 3740) = 14.97, p < 0.001; DR: EMM = 8.77, SE = 0.11; WP: EMM = 7.96, SE = 0.18) and anxiety symptoms ( F (1, 3740) = 57.58, p < 0.001; DRs: EMM = 8.47, SE = 0.10; WP: EMM = 7.08, SE = 0.16) were significantly greater for DRs compared to WPs. Conversely, symptoms of mania were greater in WPs compared to DRs ( F (1, 3740) = 27.97, p < 0.001; WPs: EMM = 3.53, SE = 0.08; DRs: EMM = 3.06, SE = 0.05), and there was no difference between the groups in terms of suicidality ( F (1, 3740) = 0.39, p = 0.53; DRs: EMM = 5.92, SE = 0.06; WPs: EMM = 5.98, SE = 0.09).
Item-level analysis of suicidality
The SBQ-R (Osman et al., 2001a ) measures overall suicide risk with individual items assessing various facets of suicidality (i.e. lifetime suicidal thoughts, recent suicidal thoughts, future suicide intent, and suicide behaviours). WPs (EMM = 1.30, SE = 0.02) were more likely to report having attempted suicide than DRs (EMM = 1.26, SE = 0.01) ( F (2, 3748) = 5.72, p = 0.02). There was no difference between DRs and WPs in terms of suicidal thoughts (lifetime or recent) or future suicide risk (lifetime suicidal thoughts: DRs: EMM = 1.85, SE = 0.02; WPs: EMM = 1.90, SE = 0.03; p = 0.16; recent suicidal thoughts: DRs: EMM = 1.82, SE = 0.02; WPs: EMM = 1.81, SE = 0.04; future suicide risk: DRs: EMM = 0.99, SE = 0.02; WPs: EMM = 0.98, SE = 0.04; p = 0.84).
We aimed to ascertain whether, compared to an educated working control group, DRs were at significantly greater risk for both common (depression and anxiety) and serious (mania and suicidality) mental health problems and whether any greater risk was explained by pre-existing differences in mental health problem proneness. We also aimed to understand DRs’ beliefs regarding the commonality and occupational impact of problems with their mental health. DRs reported significantly higher levels of depression and anxiety, and significantly lower levels of mania, than WPs. There was no main difference between DRs and WPs in reported suicidality, but our item-level exploratory analysis of facets of suicidality revealed that WPs reported greater risk for engaging in suicide behaviours. DRs widely endorsed beliefs about the normalcy of mental health problems in their peer group. Moreover, there appeared to be an impact of this poor mental health on considered and actual intermissions from PhD study.
When viewed alongside those of Levecque et al. ( 2017 ), our results suggest that mental health problems are more prevalent amongst UK-based DRs than Belgian DRs. More than half of DRs (51.1%) in Belgium met the criteria for psychological distress (Levecque et al., 2017 ); where we found that 70.9% and 74.2% of DRs reported clinically relevant (i.e. mild to severe symptoms) of depression and anxiety symptoms, respectively. The difference between these findings could reflect differences in the outcome measures employed; Levecque et al. ( 2017 ) used the General Health Questionnaire (GHQ) (Goldberg, 1972 ), whereas we used the PHQ-9 (Spitzer et al., 1999 ) and GAD-7 (Spitzer et al., 2006 ). Alternatively, this could represent genuine differences in the prevalence of mental health problems across countries, over time, or with respect to the conditions DRs experience during their PhD.
The high rates of depression and anxiety symptoms within our UK DR sample are concerning. In addition to the clear distress reported here, depression and anxiety symptoms are likely to undermine the chances of successfully completing a PhD by impairing academic performance via undermining neurocognitive functioning (Castaneda et al., 2008 ), for example through impairing executive functioning, attention, and working memory (Shackman et al., 2006 ; Rock et al., 2014 ; Shields et al., 2016 ). Supporting the mental health of DRs is important to not only improve the wellbeing of these students, but also to enable them to successfully complete their studies and ensure important contributions to the research (Levecque et al., 2017 ) and knowledge economies (Kehm, 2006 ).
The overall scores from our measure of suicidality (using the SBQ-R (Osman et al., 2001a )) yielded no significant differences between DRs and WPs. However, closer inspection of the scores reveals a worrying picture, whereby both groups reported alarmingly high levels of suicide risk. A concerning 35% of DRs (and WPs) met criteria for ‘suicide risk’, using measure thresholds derived for the general population (Osman et al., 2001b ). There have been two studies that have used the SBQ-R to assess suicidality in the general population (Castillejos et al., 2020 ). The prevalence of suicide risk in both of our samples far exceeds the prevalence observed in the general population studies of 4.6% (Polatöz et al., 2011 ; Blüml et al., 2013 ) at its highest. This high suicide risk may be a consequence of the high prevalence of depression in our sample, which could therefore be reduced by ameliorating depressive symptoms, though this relationship requires testing. Currently, national suicide data for all UK students is collected by the Higher Education Statistics Agency (HESA) and the Office for National Statistics (ONS). To help identify which students are at greatest risk of dying by suicide, we recommend these data differentiate and disaggregate by phase of study so that suicide rates are monitored amongst DRs specifically.
There was no difference in terms of the lifetime prevalence of a diagnosed mental health problem or the age of symptom onset between DRs and WPs. However, WPs generally reported mental health problems starting in an earlier life phase than did DRs. These data combined suggests that those with long-term mental health problems are not disproportionately drawn to study for a PhD and that the high prevalence of mental health problems amongst DRs does not simply represent pre-existing conditions.
Limitations
Despite efforts to recruit both those with and without mental health difficulties, our results may be skewed by a selection bias. That is, the survey may have disproportionately attracted respondents within both the DR and the educated working control group who have mental health problems (with or without diagnosis) compared to those who do not. Mental health prevalence statistics for the UK general population suggest 25% (1 in 4) (Time to Change, 2015 ) of people experience mental health problems; whereas, in the present sample, prevalence was more than double this (59.4% for DRs and 52.4% for WPs). Although this may limit the representativeness of our findings, it does in fact strengthen our conclusions. That is, even compared to a WP sample who have particularly high rate of mental health problems and which had an earlier onset, DRs still report significantly greater levels of depression and anxiety. Similarly, our findings may have limited generalisability due to the disproportionate number of White British and female participants who participated in the survey and is not necessarily being applicable beyond the UK.
Our survey used brief, self-report measures of mental health problems, which may be more likely to produce less reliable and valid results than a diagnostic interview. However, there is some suggestion that using measures such as these, particularly in an online setting, reduces social desirability (Henderson et al., 2012 ; Zhang et al., 2017 ) and therefore, our findings may actually better reflect prevalence than if we had interviewed participants face-to-face.
We must also acknowledge the limitations of our exploratory post-hoc analysis of the SBQ-R (Osman et al., 2001a ) data. Suicidality can broadly be conceptualised as thoughts (e.g. ideation) and action (e.g. planning and attempts) (Klonsky et al., 2016 ), and after examining full-scale scores we decided to carry out the additional item-level analysis. As this item level analysis was not planned a priori, the results should be interpreted with caution.
Research implications
In addition to measuring common mental health symptoms (depression and anxiety), we included measures related to more SMI conditions (mania and suicide). Yet there remains a need to explore other SMI symptoms and unusual experiences. Moreover, DRs are a heterogenous group, for example in relation to funding, area of study, and home/international status, and we did not explore associations between such characteristics and mental health problems. Furthermore, while our findings suggest that DRs generally have poorer mental health, we have not drawn any conclusions as to putative mechanisms that explain this difference. We have however begun to test predictive associations of DR mental health symptoms in a further study (Berry et al., 2021 ).
Data availability
The data are available upon reasonable request to the corresponding author.
Altman EG, Hedeker D, Peterson JL, Davis JM (1997) The Altman self-rating Mania scale. Biol Psychiatry 42:948–955. https://doi.org/10.1016/S0006-3223(96)00548-3
Article CAS PubMed Google Scholar
Berry C, Niven J, Hazell C (2021) Personal, social and relational predictors of UK postgraduate researcher mental health problems. BJPsych Open, 7:E205. https://doi.org/10.1192/bjo.2021.1041
Blüml V, Kapusta ND, Doering S et al. (2013) Personality factors and suicide risk in a representative sample of the German general population. PLoS ONE 8:1–7. https://doi.org/10.1371/journal.pone.0076646
Article CAS Google Scholar
Casey BH (2009) The economic contribution of PhDs. J High Educ Policy Manag 31:219–227. https://doi.org/10.1080/13600800902974294
Article Google Scholar
Castaneda AE, Tuulio-Henriksson A, Marttunen M et al. (2008) A review on cognitive impairments in depressive and anxiety disorders with a focus on young adults. J Affect Disord 106:1–27. https://doi.org/10.1016/j.jad.2007.06.006
Article PubMed Google Scholar
Castillejos MC, Huertas P, Martín P, Moreno Küstner B (2020) Prevalence of suicidality in the european general population: a systematic review and meta-analysis. Arch Suicide Res 0:1–19. https://doi.org/10.1080/13811118.2020.1765928
Cornell B (2020) PhD students and their careers. London, UK
Engineering & Physical Science Research Council (EPSRC) (2010) The economic impact of PhDs. Edinburgh
Goldberg DP (1972) The detection of psychiatric illness by questionnaire. Maudsley Monogr 21: Oxford University Press
Goldberg DP, Gater R, Sartorius N et al. (1997) The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 27:191–197. https://doi.org/10.1017/S0033291796004242
Hancock S (2020) The employment of PhD graduates in the UK: what do we know? Higher Education Policy Institute. https://www.hepi.ac.uk/2020/02/17/the-employment-of-phd-graduates-in-the-uk-what-do-we-know/ . Accessed 22 Oct 2020
Hankins M (2008a) Clinical Practice and Epidemiology Executive function abnormalities in pathological gamblers. Clin Pract Epidemiol Ment Health 6:1–6. https://doi.org/10.1186/1745-0179-4-Received
Hankins M (2008b) The reliability of the twelve-item general health questionnaire (GHQ-12) under realistic assumptions. BMC Public Health 8:1–7. https://doi.org/10.1186/1471-2458-8-355
Hazell CM, Chapman L, Valeix SF et al. (2020) Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis. Syst Rev 9:1–30
Henderson C, Evans-Lacko S, Flach C, Thornicroft G (2012) Responses to mental health stigma questions: the importance of social desirability and data collection method. Can J Psychiatry 57:152–160. https://doi.org/10.1177/070674371205700304
HESA (2019) Who’s studying in HE? Higher Education Statistics Agency. https://www.hesa.ac.uk/data-and-analysis/students/whos-in-he . Accessed 3 Nov 2020
Kehm BM (2006) Doctoral education in Europe and North America: a comparative analysis. In: Teichler U (ed) The formative years of scholars. Wenner-Gren International Series. Portland Press, London, UK, pp. 67–78
Kessler RC, Berglund P, Demler O et al. (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 62:593–602. https://doi.org/10.1001/archpsyc.62.6.593
Kessler RC, Üstün BB (2004) The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int. J. Methods Psychiatr. Res. 13:93–117
Klonsky ED, May AM, Saffer BY (2016) Suicide, suicide attempts, and suicidal ideation. Annu Rev Clin Psychol 12:307–330. https://doi.org/10.1146/annurev-clinpsy-021815-093204
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16:606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Article CAS PubMed PubMed Central Google Scholar
Levecque K, Anseel F, De Beuckelaer A et al. (2017) Work organization and mental health problems in PhD students. Res Policy 46:868–879. https://doi.org/10.1016/j.respol.2017.02.008
Metcalfe J, Wilson S, Levecque K (2018) Exploring wellbeing and mental health and associated support services for postgraduate researchers. Cambridge
Nature (2019a) The mental health of PhD researchers demands urgent attention. Nature 575:257–258. https://doi.org/10.1038/d41586-019-03489-1
Nature (2019b) Academia’s mental-health woes. Nature 569:307
Google Scholar
Osman A, Bagge CL, Gutierrez PM et al. (2001a) The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment 8:443–454. https://doi.org/10.1177/107319110100800409
Osman A, Bagge CL, Gutierrez PM et al. (2001b) The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment 8:443–454
Polatöz Ö, Kuğu N, Doğan O, Akyüz G (2011) The prevalence of suicidal behaviour and its correlation with certain sociodemographic variables in Sivas province. Dusunen Adam J Psychiatry Neurol Sci 24:13–23. https://doi.org/10.5350/dajpn2011240102
Rock PL, Roiser JP, Riedel WJ, Blackwell AD (2014) Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med 44:2029–2040. https://doi.org/10.1017/S0033291713002535
Shackman AJ, Sarinopoulos I, Maxwell JS et al. (2006) Anxiety selectively disrupts visuospatial working memory. Emotion 6:40–61. https://doi.org/10.1037/1528-3542.6.1.40
Shields GS, Moons WG, Tewell CA, Yonelineas AP (2016) Anxiety not anger impairs executive functionioning. Emotion 16:792–797. https://doi.org/10.1016/j.antiviral.2015.06.014.Chronic
Article PubMed PubMed Central Google Scholar
Spitzer RL, Kroenke K, Williams JBW et al. (2006) A brief measure for assessing generalized anxiety disorder. Arch Intern Med 166:1092. https://doi.org/10.1001/archinte.166.10.1092
Spitzer RL, Kroenke K, Williams JBW, Group PHQPCS (1999) Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA 282:1737. https://doi.org/10.1001/jama.282.18.1737
Time to Change (2015) Attitudes to mental illness 2014 research report. Time to Change, London
University Alliance (2014) The contribution of university research to economic growth. University Alliance, London, UK
Woolston C (2019) PhD poll reveals fear and joy, contentment and anguish. Nature 575:403–406. https://doi.org/10.1038/d41586-019-03459-7
Article ADS CAS PubMed Google Scholar
Woolston C (2020) Pandemic and panic for US graduate students. Nature 585:147–148. https://doi.org/10.1038/d41586-020-02439-6
Ye S (2009) Factor structure of the General Health Questionnaire (GHQ-12): The role of wording effects. Pers Individ Dif 46:197–201. https://doi.org/10.1016/j.paid.2008.09.027
Zhang XC, Kuchinke L, Woud ML et al. (2017) Survey method matters: online/offline questionnaires and face-to-face or telephone interviews differ. Comput Hum Behav 71:172–180. https://doi.org/10.1016/j.chb.2017.02.006
Zolas N, Goldschlag N, Jarmin R et al. (2015) Wrapping it up in a person: examining employment and earnings outcomes for Ph.D. recipients. Science (80–) 350:1367–1371. https://doi.org/10.1126/science.aac5949
Article ADS CAS Google Scholar
Download references
Acknowledgements
The authors wish to thank the Doctoral Researchers who participated in the present study, and the universities and individuals who helped to promote the U-DOC project. This research was jointly funded by Research England and the Office for Students ( https://re.ukri.org/research/postgraduate-researchers/ ).
Author information
Authors and affiliations.
School of Social Sciences, University of Westminster, 115 New Cavendish Street, London, W1W 6UW, UK
- Cassie M. Hazell
School of Life Sciences, University of Sussex, Falmer, Brighton, BN1 9QG, UK
Jeremy E. Niven & Sophie Valeix
School of Psychology, University of Sussex, Falmer, Brighton, BN1 9QJ, UK
Laura Chapman & Sam Cartwright-Hatton
Centre for Higher Education and Equity Research, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Paul E. Roberts
Brighton and Sussex Medical School, Brighton, BN1 9PH, UK
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Clio Berry .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the University of Sussex Sciences and Technology Cross-Schools Research Ethics Committee (C-REC) (Date: 19 December 2017; Reference: ER/CH283/9).
Informed consent
All individuals who took part in this study provided informed consent to participate and for their data to be used in research reports.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Hazell, C.M., Niven, J.E., Chapman, L. et al. Nationwide assessment of the mental health of UK Doctoral Researchers. Humanit Soc Sci Commun 8 , 305 (2021). https://doi.org/10.1057/s41599-021-00983-8
Download citation
Received : 04 December 2020
Accepted : 13 September 2021
Published : 09 December 2021
DOI : https://doi.org/10.1057/s41599-021-00983-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The mental labyrinth of postgraduate research: a qualitative study of postgraduate mental health and wellbeing and the impact of the supervisory relationship.
- Naomi White
- Jelena Milicev
- Maria Gardani
Higher Education (2024)
Predictors of UK postgraduate researcher attendance behaviours and mental health-related attrition intention
- Jeremy E. Niven
Current Psychology (2023)
Depression and anxiety ‘the norm’ for UK PhD students
- Chris Woolston
Nature (2021)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

‘You have to suffer for your PhD’: poor mental health among doctoral researchers – new research
Lecturer in Social Sciences, University of Westminster
Disclosure statement
Cassie Hazell has received funding from the Office for Students.
University of Westminster provides funding as a member of The Conversation UK.
View all partners
PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
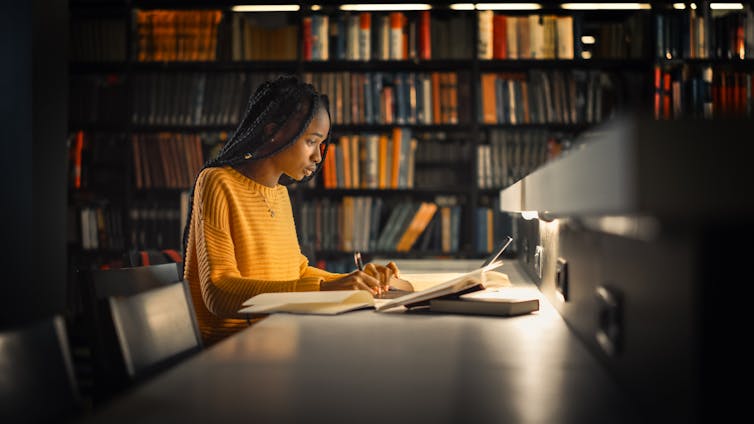
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse. If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
- Mental health
- Academic life
- PhD research

Head of School, School of Arts & Social Sciences, Monash University Malaysia

Chief Operating Officer (COO)

Clinical Teaching Fellow

Data Manager

Director, Social Policy

- About the LSE Impact Blog
- Comments Policy
- Popular Posts
- Recent Posts
- Subscribe to the Impact Blog
- Write for us
- LSE comment
Cassie M Hazell
January 12th, 2022, is doing a phd bad for your mental health.
9 comments | 77 shares
Estimated reading time: 6 minutes
Poor mental health amongst PhD researchers is increasingly being recognised as an issue within higher education institutions. However, there continues to be unanswered questions relating to the propensity and causality of poor mental health amongst PhD researchers. Reporting on a new comparative survey of PhD researchers and their peers from different professions, Dr Cassie M Hazell and Dr Clio Berry find that PhD researchers are particularly vulnerable to poor mental health compared to their peers. Arguing against an inherent and individualised link between PhD research and mental health, they suggest institutions have a significant role to play in reviewing cultures and working environments that contribute to the risk of poor mental health.
Evidence has been growing in recent years that mental health difficulties are common amongst PhD students . These studies understandably have caused concern in academic circles about the welfare of our future researchers and the potential toxicity of academia as a whole. Each of these studies has made an important contribution to the field, but there are some key questions that have thus far been left unanswered:
- Is this an issue limited to certain academic communities or countries?
- Do these findings reflect a PhD-specific issue or reflect the mental health consequences of being in a graduate-level occupation?
- Are the mental health difficulties reported amongst PhD students clinically meaningful?
We attempted to answer these questions as part of our Understanding the mental health of DOCtoral researchers (U-DOC) survey. To do this we surveyed more than 3,300 PhD students studying in the UK and a control group of more than 1,200 matched working professionals about their mental health. In our most recent paper , we compared the presence and severity of mental health symptoms between these two groups. Using the same measures as are used in the NHS to assess symptoms of depression and anxiety, we found that PhD students were more likely to meet criteria for a depression and/or anxiety diagnosis and have more severe symptoms overall. We found no difference between these groups in terms of their overall suicidality. However, survey responses corresponding to past suicidal thinking and behaviour, and future suicide intent were generally highly rated in both groups.
42% of PhD students reported that they believed having a mental health problem during your PhD is the norm
We also asked PhD students about their perceptions and lived experience of mental health. Sadly, 42% of PhD students reported that they believed having a mental health problem during your PhD is the norm. We also found similar numbers saying they have considered taking a break from their studies for mental health reasons, with 14% actually taking a mental health-related break. Finally, 35% of PhD students have considered ending their studies altogether because of their mental health.
We were able to challenge the working theory that the reason for our findings is that those with mental health difficulties are more likely to continue their studies at university to the doctoral level. In other words, the idea that doing a PhD doesn’t in any way cause mental health problems and these results are instead the product of pre-existing conditions. Contrary to this notion, we found that PhD students were not more likely than working professionals to report previously diagnosed mental health problems, and if anything, when they had mental health problems, these started later in life than for the working professionals. Additionally, we found that our results regarding current depression and anxiety symptoms remained even after controlling for a history of mental health difficulties.

The findings from this paper and our other work on the U-DOC project has highlighted that PhD students seem to be particularly vulnerable to experiencing mental health problems. We found several factors to be key predictors of this poor mental health ; specifically not having interests and relationships outside of PhD studies, students’ perfectionism, impostor thoughts, their supervisory relationship, isolation, financial insecurity and the impact of stressors outside of the PhD .
the current infrastructure, systems and practices in most academic institutions, and in the wider sector, are increasing PhD students’ risk of mental health problems and undermining the potential joy of pursuing meaningful and exciting research
So, does this mean that doing a PhD is bad for your mental health? Not necessarily. There are several aspects of the PhD process that are conducive to mental health difficulties, but it is absolutely not inevitable. Our research (and our own experiences!) suggests that doing a PhD can be an incredibly positive experience that is intellectually stimulating, personally satisfying, and gives a sense of meaning and purpose. We instead believe a more appropriate conclusion to draw from our work is that the current infrastructure, systems and practices in most academic institutions, and in the wider sector, are increasing PhD students’ risk of mental health problems and undermining the potential joy of pursuing meaningful and exciting research.
Reducing this issue to the common rhetoric that “PhD studies cause mental health problems” is problematic for several reasons: Firstly, it ignores the many interacting moving parts at work here that variably increase and reduce risk of poor mental health across people, time, and place. Secondly, it does not acknowledge the pockets of incredibly good practice in the sector we can learn from and implement more widely. Finally, it reinforces the notion that poor mental health is the norm for PhD students which then becomes a self-fulfilling prophecy- and itself ignores the joy of pursuing a thesis in something potentially so personally meaningful. Nonetheless, a significant paradigm shift is needed in academia to reduce the current environmental toxins so that studying for a PhD can be a truly enjoyable and fulfilling process for all.
Note: This article gives the views of the author, and not the position of the Impact of Social Science blog, nor of the London School of Economics. Please review our Comments Policy if you have any concerns on posting a comment below.
Image Credit: Geralt via Pixabay.

About the author

Dr Cassie M Hazell (she/her) is a lecturer in Social Sciences at the University of Westminster. Her research is on around mental health, with a special interest in implementation science. She is the co-founder of the international Early Career Hallucinations Research (ECHR) group and Early-Mid Career representative on the Research Council at her institution.

Dr Clio Berry is a Senior Lecturer in Healthcare Evaluation and Improvement in the Brighton and Sussex Medical School. She is interested in the application of positive and social psychology approaches to mental health problems and social outcomes for young people and students. Her work spans identification of risk and resilience factors in predicting mental health and social problems and their outcomes, and in the development and evaluation of clinical and non-clinical interventions.
- Pingback: Is doing a PhD bad for your mental health? | Thinking about Digital Publishing
My own experience of doing a PhD (loneliness, the lack of routine, imposter syndrome) has led to my discouraging my daughter, who has a history of mental health issues, from considering it at the moment, despite her having the academic aptitude and even a topic. I would hazard a guess that the problems are worse in the humanities than in the applied sciences, where most PhD students tend to work as part of research teams and be well supported in more structured environments.
- Pingback: What can universities do to support the well-being and mental health of postgraduate researchers? | Impact of Social Sciences
Fascinating research… I had a terrible PhD, but most of the mental health issues arose after the fact. If you ever conducted another survey it would be interesting to include those who had recently finished a PhD.
Looking at your follow up BJPsyche paper, I noticed you haven’t gone into the correlation between subject and mental health. I’d be interested to know how sciences vs humanities compared.
I see that your work is very restrained in discussing the causes of mental health issues, and I’m sure you have plenty of hypothesis. In my experience, a key factor is that there is no mechanism to hold supervisors to account for the quality of their supervision. (Linking to the point above, I believe in the sciences supervisors with poor outcomes do suffer repetitional damage – not so in the humanities.)
I’d also add that the UK’s Viva system, which I believe is unique globally, is a recipe for disaster – years of work evaluated over the course of just a couple of hours by examiners who, again, are not held accountable in any way.
I wrote my experience up here: https://medium.com/the-faculty/i-had-a-brutal-phd-viva-followed-by-two-years-of-corrections-here-is-what-i-learned-about-vivas-5e81175aa5d
- Pingback: The benefits of getting involved with the LSESU as a PhD student | Students@LSE
- Pingback: “Am I ready for a PhD?” - The Undercover Academic
- Pingback: #AcWriMo & online writing communities for off-campus PGRs – UoB PGR Development
- Pingback: Psychische Herausforderungen während der juristischen Promotion › JuWissBlog
- Pingback: What To Expect When You’re PhDing - Völkerrechtsblog
Leave a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Notify me of follow-up comments by email.
What can universities do to support the well-being and mental health of postgraduate researchers? February 1st, 2022
Related posts.

Is peer review bad for your mental health?
April 19th, 2018.

Book Review: Being Well in Academia: Ways to Feel Stronger, Safer and More Connected by Petra Boynton
February 27th, 2021.
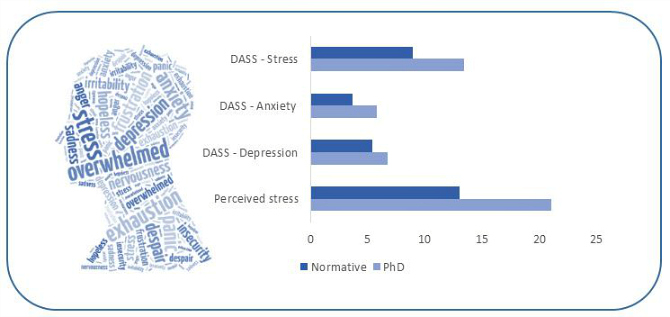
Mental health risks in research training can no longer be ignored
June 25th, 2018.

The neurotic academic: how anxiety fuels casualised academic work
April 17th, 2018.

Visit our sister blog LSE Review of Books
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Research disruption during PhD studies and its impact on mental health: Implications for research and university policy
Contributed equally to this work with: Maria Aristeidou, Angela Aristidou
Roles Conceptualization, Data curation, Formal analysis, Methodology, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Institute for Educational Technology, The Open University, Milton Keynes, Buckinghamshire, United Kingdom
Roles Conceptualization, Investigation, Resources, Writing – original draft, Writing – review & editing
Affiliation UCL School of Management, London, United Kingdom
- Maria Aristeidou,
- Angela Aristidou

- Published: October 18, 2023
- https://doi.org/10.1371/journal.pone.0291555
- Reader Comments
Research policy observers are increasingly concerned about the impact of the disruption caused by the Covid-19 pandemic on university research. Yet we know little about the effect of this disruption, specifically on PhD students, their mental health, and their research progress. This study drew from survey responses of UK PhD students during the Covid-19 pandemic. We explored evidence of depression and coping behaviour (N = 1780) , and assessed factors relating to demographics, PhD characteristics, Covid-19-associated personal circumstances, and significant life events that could explain PhD student depression during the research disruption (N = 1433) . The majority of the study population (86%) reported a negative effect on their research progress during the pandemic. Results based on eight mental health symptoms (PHQ-8) showed that three in four PhD students experienced significant depression. Live-in children and lack of funding were among the most significant factors associated with developing depression. Engaging in approach coping behaviours (i.e., those alleviating the problem directly) related to lower levels of depression. By assessing the impact of research disruption on the UK PhD researcher community, our findings indicate policies to manage short-term risks but also build resilience in academic communities against current and future disruptions.
Citation: Aristeidou M, Aristidou A (2023) Research disruption during PhD studies and its impact on mental health: Implications for research and university policy. PLoS ONE 18(10): e0291555. https://doi.org/10.1371/journal.pone.0291555
Editor: Yadeta Alemayehu, Mettu University, ETHIOPIA
Received: January 23, 2023; Accepted: August 31, 2023; Published: October 18, 2023
Copyright: © 2023 Aristeidou, Aristidou. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The raw dataset on PhD students' patient health questionnaire scale and coping mechanisms is available from the Open Research Data Online (ORDO) database: https://doi.org/10.21954/ou.rd.22794203 .
Funding: This work was supported by the Institute of Educational Technology at The Open University (MA) and the University College London (UCL) School of Management (AA). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
The abrupt outbreak in January 2020 and the global proliferation of a novel virus (Covid-19) has created a crisis for many sectors, including the international higher education (HE) sector [ 1 ] that continues during the ‘post-pandemic’ period. A point of particular alarm for HE leaders, policy observers, and governments is the disruption to the typical flow and pace of university research activity. While research related to Covid-19 is still in overdrive, other research was slowed or stopped due to worldwide physical distancing measures to contain the virus’ spread (e.g., sudden campus and laboratory closures, mobility restrictions, stay-at-home orders) [ 2 ]. The resulting ‘drop in research work’ is suggested to have a detrimental impact on the HE sector on the ‘research and innovation pipeline’ [ 3 ], and on ‘research capacity, innovation and research impact’ [ 4 ].
As research and university policies internationally are being (re)shaped at a rapid pace in efforts to meet the challenge of university research disruption [ 5 ], we contribute to academic and policy conversations by examining the effect of the research disruption on the mental health of PhD students. A considerable body of research acknowledges the role of PhD students in the innovation process, in knowledge creation and diffusion (e.g., [ 6 ]) and further posits that the period of one’s PhD program is key to early career success and research productivity (e.g., [ 7 ]). These outcomes, which matter to research policy, have been linked to PhD student mental health [ 8 – 10 ]. In those times of relative stability, research had additionally demonstrated the higher prevalence of mental health issues amongst the PhD student population across research disciplines, as compared to other students within academia [ 9 ] and the general population [ 9 , 11 , 12 ]. In the period since Covid-19 disrupted our social and economic lives, depression levels in the general population have been exacerbated globally [ 13 , 14 ]. These trends suggested that the already high prevalence of poor mental health in PhD students is likely to be further exacerbated during the pandemic. Indeed, as reported in early studies on research students’ experience of the Covid-19 pandemic (e.g., [ 15 ]) and the post-pandemic period (e.g., [ 16 ]) the impact on students’ mental wellbeing has been significant, with students suggesting a number of support measures at institutional and national level.
Ignoring, at this critical moment, the increased likelihood of poor mental health in PhD students may jeopardize research capacity and HE competitiveness for years to come. Therefore, there is a pressing need to identify–within the PhD student population–those whose mental health is more affected by the research disruption, so that policies and assistance can be timelier and more targeted. Additionally, by understanding more clearly the factors that may contribute to poor mental health, and their interrelationships (presented in Methods), policymakers and HE leaders may be better placed to tackle, and ultimately overcome, this and future research disruptions.
Motivated by the current lack of an empirical basis for insights into PhD students’ mental health during the pandemic-induced disruption, we collected survey data contemporaneously during July 2020. Our 1780 survey respondents are PhD students in 94 UK Universities, across the natural and social sciences and across PhD stages. Our study has three objectives: first, to explore mental health prevalence (depression) and coping behaviour in a large-scale representative sample of PhD students in the UK (O1); second, to evaluate the relationships among mental health prevalence and coping behaviour (O2); third, to identify factors that increase the likelihood of poor PhD student mental health during the period of research disruption (O3). Our study extends previous research on mental health in the HE sector by considering the dynamics of severe disruption, as opposed to the dynamics of relative stability, on PhD students’ mental health, performance satisfaction, and coping behaviours.
Background and literature review
Uk phd students’ mental health in times of disruption.
In the UK, there are approximately 100,000 postgraduate students completing doctoral research [ 17 ]. Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students’ mental health [ 18 ]. Still, with the exception of Byrom et al. [ 11 ], published research on PhD students’ mental health in the UK exhibits the same limitations as the international research: It reflects discipline- or institution-related specificity (e.g., [ 19 ]) or utilizes samples of early career researchers in general (e.g., [ 20 ]).
Early findings on postgraduate research students’ wellbeing during the pandemic showed that only a small proportion of them are in good mental health wellbeing (28%) while the rest demonstrate possible or probable depression or anxiety [ 15 ]. Goldstone and Zhang [ 15 ] further highlight the differences among student groups with, for example, students with disabilities or caring responsibilities or female students having lower levels of mental wellbeing. The post-pandemic findings have been more promising, as only about one in four students were at risk of experiencing mental health issues [ 16 ].
In response to the Covid-19 research disruption, substantive actions have been taken by the HE sector and the UK Government to disseminate approaches deployed by UK universities to support student mental health (e.g., [ 18 ]) and to update mental health frameworks for UK universities (e.g., [ 4 ]), but so far, mitigation activities have been targeting mental health for UK university students broadly, not UK PhD students specifically.
Overcoming the paucity of evidence on UK PhD students’ mental health during the pandemic is a crucial first step to drawing strong conclusions on the prevalence and determinants of mental health issues and ways to mitigate them specific to the PhD population. For example, policy recommendations by UK postgraduate respondents during the pandemic [ 15 ] focused mainly on financial support, such as extensions to their funded period of study and tuition and visa fee support (including waivers to fees). To develop an overarching framework specific to the Objectives of our study, we synthesize insights from the international literature on PhD student mental health conducted in the period before the research disruption.
International research on PhD student mental health in times of relative stability
In the international literature examining mental health specifically for PhD students (see the systematic review in [ 21 ], the issue of mental health for PhD students is acknowledged to be multidimensional and complex [ 10 ]. In this growing research area, some address mental health as an aspect of the broader ‘health’ of the PhD students (e.g., [ 22 ]), some focus on psychological distress [ 23 ], while others take depression as a specific manifestation of distress [ 9 , 24 ]. The latter is particularly interesting because depression within the PhD population in these studies is often assessed with standardised questionnaires (e.g., PHQ, see below) that allow for developing comparative insights. It is also the approach adopted by the only global survey of PhD students’ mental health by Evans et al. [ 12 ], showing that 39% of PhD students report moderate-to-severe depression, significantly more than the general population.
Literature on PhD student’s mental health determinants in times of relative stability
Past literature on PhD students’ mental health offers insights into the determinants of PhD students’ mental health in times of stability, which may help understand the relationships we want to examine between PhD mental health, performance satisfaction and coping in times of research disruption.
First, past studies evidence the influence of PhD students’ personal lives on poor mental health. PhD students with children or with partners are less likely to have or develop psychological distress [ 9 ]. The normalcy of family roles is a much-needed antidote to the known pressures of a PhD program [ 25 ] and might even protect against mental health problems [ 22 , 26 ]. Other aspects of PhD students’ personal lives, such as significant life events (e.g., severe problems in personal relationships or severe illness of the student or someone close to them), have been linked to dissatisfaction with their research progress [ 24 ]. Research progress is defined as students’ perception of their progress in the completion of their degree [ 27 ] and is linked to their mental health. Dissatisfaction is tied to negative outcomes, such as attrition and delay [ 28 ], but also to lower productivity and mental health problems, such as worry, anxiety, exhaustion, and stress [ 29 ]. Related to this, Levecque and colleagues [ 9 ] observed that PhD students expressing a high interest in an academic career are in better mental health than those with no or little interest in remaining in academia.
Second, gender was the key personal factor that emerged as a determinant for mental health in past studies: PhD students who self-identify as female report greater clinical [ 9 , 30 ] and non-clinical problems with their mental health [ 23 , 31 ]. This is explained through the additional pressure women report on their professional and personal lives [ 23 ].
Third, past studies argue that each PhD phase presents PhD students with specific sets of challenges and should thus be explored discreetly in relation to mental health [ 32 ]. Still, the evidence on the link between the PhD phase (or the year of study as a proxy for the PhD phase) and mental health is inconclusive. Barry et al.’s [ 33 ] survey reports no connection between the PhD phase and depression levels in an Australian PhD population. However, Levecque et al. [ 9 ] report high degrees of depression in the early PhD stage of students in Belgium, and a global survey of PhD students across countries and disciplines shows that depression likelihood increases as the PhD program progresses [ 32 ].
Fourth, past research offers strong evidence that financial concerns impact PhD students’ mental health negatively. In a study by El-Ghoroury et al. [ 34 ], 63.9% of PhD students cited debt or financial issues as a cause for poor wellbeing and cited financial constraints as the major barrier to improving their wellness (through social interactions, outside-PhD activities, etc). Even uncertainty about funding was shown to predict poor mental health [ 9 ]. To this end, Geven et al. [ 35 ] explored packages of reforms in a pre-pandemic graduate school programme, including an extension of the grant period, and indicated that such policies can increase students’ completion rates to up to 20%.
Finally, age is not shown to be associated with mental health [ 9 ], but numerous studies found that having children, particularly for female PhD students and in Science-Technology-Engineering-Maths (STEM) disciplines [ 36 ], consistently corresponds with heightened stress [ 37 ]. However, a specific examination of the relationship between children and mental health indicates that PhD students with one or more children in the household showed significantly lower odds of having or developing a common psychiatric disorder [ 9 ]. Further, parenting and, in particular, motherhood during doctorate studies contribute to the development of students’ coping mechanisms that allows them to succeed in a balance in both worlds [ 38 ].
Past research insights into PhD mental health and coping
Past research explored how PhD students may “cope” with stressors and thus mitigate poor mental health [ 39 ]. Studies identify the importance of social interactions (e.g., [ 22 ]); balancing life demands (e.g., [ 16 ]), reaching out for social support (e.g., [ 40 ]) sometimes through peer relationships (e.g., [ 10 , 39 ]); and ‘planning’ (e.g., [ 22 ]); As invaluable as these insights are, drawing comparisons between these findings is difficult because often the identification of coping styles or strategies was not the focus of these studies, making it difficult to draw fine-grained conclusions as to their effect on PhD students’ mental health.
There is, however, a long tradition of research on coping for physiological wellbeing that provides standardised measures for individuals’ coping and their link to mental health [ 41 ]. The most widely used measurement instrument in the literature reviewed is the COPE Inventory, which allows researchers to assess how people cope in a variety of stressful situations, including in HE for students [ 42 – 44 ], making it particularly relevant to the context and sample under investigation in our study of PhD students. Additionally, COPE allows for the identification of consistent ways of coping, which provides predictive validity across a range of situations. Predictive validity is desired when examining the role of coping in relation to mental health. Indeed, multiple studies have linked the COPE measurement to mental health outcomes (e.g., [ 45 , 46 ]), including depression [ 43 ], which is a focus of our study.
Data and methods
Participants.
For the current study, we recruited participants that were active PhD students from March to July 2020 at any stage of their research to take part in an online survey. The survey ran between the 31st of July and the 23rd of August 2020, with the aim of capturing the potential impact of the Covid-19 disruption during the first lockdown on their research progress and mental health. The use of online surveys to assess the scope of mental health problems is particularly appropriate during the Covid-19 outbreak [ 47 ]. The current study has been reviewed by, and received a favourable opinion, from The Open University Human Research Ethics Committee (reference number: HREC/3605/Aristeidou), http://www.open.ac.uk/research/ethics/ . For the recruitment of a diverse audience, we followed a snowball sampling method, forwarding our invitation to PhD student groups in a number of UK-based universities, but also exploited the reach of PhD social media channels and online PhD groups, and we invited academics and respondents to recruit other participants. Vouchers were provided as an incentive for participation to the first 300 respondents. Before completing the survey, the respondents were provided with an online information sheet and were asked to provide their written consent through a digital consent form. They reported their email addresses to be identifiable and contactable for validation, consent issues, potential withdrawal, and incentive processing. The dataset was anonymized on the 30th of August 2020, prior to initiating data analysis.
Exclusion criteria included survey respondents who ‘straight-lined’ (chose the same answer option repeatedly), gave inconsistent responses to similar questions, or did not use their institution emails (rendering them unidentifiable). Finally, there were 1790 PhD students in the study from 94 different HE institutions across all four UK nations (England, Scotland, Northern Ireland and Wales). The majority of the study population (86%) reported that their research progress had been impacted in a negative way. The dataset [ 48 ] included 44.4% male and 55.4% female participants, while the doctoral students in the UK consist of 51% male and 49% female students [ 17 ]. Weighting adjustments were made to correct the sample representativeness. The majority of the survey respondents were 25–34 years old (80.4%), with live-in children (71%). Most respondents (86.7%) were conducting their PhDs full-time, and almost two-thirds (64.4%) were funded by a research council or a charitable body in the UK. At the time of the survey, a large proportion of the survey respondents were in the ‘executing’ phase of their research (i.e., data collection/analysis). Finally, a natural science-related PhD was being pursued by slightly over two-thirds of the respondents (68.8%). According to data sourced from HESA [ 17 ], the likelihood of individuals embarking on a research postgraduate degree at a younger age (such as 18–20) appears to be relatively low. This is evident from the fact that only 90–130 students within this age group register for such programs each year. More details on the demographics and characteristics of the sample can be found in Table 1 and below.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0291555.t001
Variables and instruments
Brief cope inventory (bci)..
The BCI [ 49 ] is a 28-item self-report questionnaire designed to measure effective and ineffective ways to cope with a stressful life event, and it is the abbreviated version of the original 60-item COPE inventory developed by [ 42 ]. The BCI has a 4-point Likert scale with options on each item ranging from 0 (I usually do not do this at all) to 3 (I usually do this a lot). Coping in this study is categorised in two overarching coping behaviours, as per Eisenberg et al. [ 50 ]: (a) the approach behaviours that attempt to reduce stress by alleviating the problem directly, which include 12 items related to active coping, positive reframing, planning, acceptance, seeking emotional support, and seeking informational support; and (b) the avoidant coping behaviours that attempt to reduce stress by distancing oneself from the problem, which include 12 items related to denial, substance use, venting, behavioural disengagement, self-distraction, and self-blame. Items that belong to neither overarching behaviour are coping related to humour and religion. These were included in the overall coping score but excluded from the analysis based on the two overarching behaviours. A higher score indicates frequent use of that coping behaviour. Cronbach’s alpha for the BCI was .88. Further, both the approach and avoidant scales have shown very good internal consistency in this sample, with Cronbach’s alpha equal to 0.83 and 0.80, respectively.
Patient health questionnaire eight-item depression scale (PHQ-8).
PHQ-8 [ 57 ] is an eight-item version of the Patient Health Questionnaire (PHQ-9). PHQ is a popular measure for assessing depression and is frequently used for PhD mental health (e.g., [ 12 , 51 ]), making it an ideal choice for our study. PHQ-9 has been validated as both a diagnostic and severity measure [ 52 , 53 ] in population-based settings [ 54 ] and self-administered modes [ 55 , 56 ], and it was recently used in a global survey of PhD students’ depression prevalence [ 12 ]. PHQ-8 omits the ninth question that assesses suicidal or self-injurious thoughts, and it was deemed more appropriate for our research because researchers in web-based interviews/surveys are unable to provide adequate interventions remotely. The PHQ-8 items employ a 4-point Likert scale with options on each item ranging from 0 (not at all) to 3 (nearly every day). Then, the scores are summed to give a total score between 0 and 24 points, where 0–4 represent no significant depressive symptoms, 5–9 mild depressive symptoms, 10–13 moderate, 15–19 moderately severe, and 20–24 severe [ 55 ]. Evidence from a large-scale validation study [ 57 ] indicates that a PHQ-8 score ≥ 10 represents clinically significant depression. In this study, Cronbach’s alpha for the PHQ-8 was 0.71, indicating a good internal consistency.
Performance satisfaction.
Performance satisfaction is an 8-item self-report scale designed to measure the students’ self-perceived progress in their PhD research, their confidence in being able to finish on time, and their satisfaction. The scale was successfully used in a PhD student well-being study at the university of Groningen [ 24 ] prior to the Covid-19 pandemic. The performance satisfaction 5-point Likert scale responses range from 1 (completely disagree) to 5 (completely agree). The score for each respondent equals the mean score of the 8-item responses. A reliability analysis was carried out on the performance satisfaction scale. Cronbach’s alpha showed the scale to reach acceptable reliability, α = 0.86.
Significant life events Significant Life events is a questionnaire designed to capture whether PhD students had experienced any significant life events in the 12 months prior to the survey. This was successfully used in studying PhD students’ mental health at the university of Groningen [ 24 ] prior to the Covid-19 pandemic research disruption. Events include the death of someone close, severe problems in personal relationships, financial problems, severe illness of oneself or someone close, being in the process of buying a house, getting married, expecting a child, none of these events, and prefer not to say. Significant life events were used as an incident control variable in this study.
Statistical analyses
SPSS (Version 25) was used for statistical analysis. In the first phase, descriptive statistics were used to describe the PHQ-8 Depression and coping behaviours of the sample and the distribution of these three variables among demographics, PhD characteristics, and Covid-19-related circumstances (O1). We used a weighting adjustment for gender to correct the survey representativeness for descriptive analysis; females were given a ‘corrective’ weight of 0.88 and males of 1.15.
In relation to O2, Spearman rank correlations were used to examine the degree of association between all of the 28 coping behaviours and PHQ-8 Depression scores. This finding contributed to our understanding of how individual coping behaviours could relate to lower or higher depressive symptoms.
To assess whether the behaviours significant to our study (i.e., those with a negative or the strongest positive PHQ-8 Depression association) were used more frequently by students of a particular demographic group (O2), we used independent-samples t-test and ANOVA. Before assessing the relationship between our variables, outliers, and groups with a sample size smaller than 15 for each group were removed from the tests (e.g., Gender = other; Funding = partially funded; Likelihood in HE = already employed in academia).
In relation to O3, a binary logistic regression analysis was performed to examine whether Covid-19-related circumstances explain significant depression in PhD students, while controlling for demographics, PhD characteristics, and external incidents. Prior to performing the regression analysis, PHQ-8 Depression score outliers, as well as groups with fewer than 10 events per variable (e.g., gender = other; age = 55–64; Impact reason = mental health), were detected and excluded from the dataset. The dichotomous dependent variable was calculated based on PHQ-8 Depression scores smaller than 10 for non-significant depression, and equal or larger than 10 for significant depression. Associations between Depression in PhD students and the independent variables in our dependency model were estimated using odds ratios (ORs) as produced by the logistic regression procedure in SPSS (Version 25). The ORs were used to explain the strength of the presence or absence of significant depression. Wald tests were used to assess the significance of each predictor. A test of the full model against a constant only model was statistically significant, indicating that the predictors as a set reliably distinguished between PhD students who are having or developing significant depression and those who are not ( Χ 2 (25) = 405.258, p < . 001 ). A Nagelkerke R 2 of .798 indicated a good to substantial relationship between prediction and grouping (68% of variance explained by the proposed model in completion rates). Table 2 presents response percentages about the categorical variables entered in the model, including the two dependent variables (significant depression and non-significant depression).
https://doi.org/10.1371/journal.pone.0291555.t002
Exploring depression prevalence and coping behaviours
The average PHQ-8 Depression score was 10.13 ( SD = 3.23) on a scale of 0–24 (weighted cases). Importantly, this highlights that the majority of survey respondents are facing moderate depression symptoms ( Fig 1 ). The PHQ-8 item with the highest score, in a range of 0–4, was ‘having trouble to concentrate on things, such as reading the newspaper or watching television’ ( M = 1.45; SD = 0.84), and the item with the lowest score was ‘moving or speaking so slowly that other people could have noticed; or the opposite–being so fidgety or restless that have been moving around a lot more than usual’ ( M = 1.10; SD = 0.75). Of the study population, 75% self-reported significant depression (moderate, moderately severe, or severe major).
https://doi.org/10.1371/journal.pone.0291555.g001
The coping behaviours that the majority of PhD students used in a medium or large amount to overcome the Covid-19 disruption were “accepting the reality of the fact that it has happened” (84%), followed by “thinking hard about what steps to make” (76%) ( Fig 2 ). Both are approaching coping behaviours. Other coping behaviours used to a great extent were “praying or meditating” (73%) , “blaming myself for things that happened” (avoidant) (71%) , and “expressing my negative feelings” (avoidant) (69%). On the other hand, coping behaviours that were used the least were all avoidant ones: “giving up attempting to cope” ( 13%) , “refusing to believe that it has happened” (15%) , “using alcohol or other drugs to make myself feel better” (17%) , and “giving up trying to deal with it” (17%) . Overall, approach coping behaviours were used to a greater extent ( M = 26.43, SD = 5.15) than avoidant coping behaviours ( M = 23.97, SD = 4.90).
https://doi.org/10.1371/journal.pone.0291555.g002
The Spearman correlations between coping behaviours and PHQ-8 scores ( Table 3 ), which included outliers, suggested that only two items have significant negative (very weak) associations with depression: Item 15, “getting comfort and understanding from someone” ( r s (1780) = -.107, p < .01); and Item 7, “taking action to try to make the situation better” ( r s (1762) = -.077, p < .01). The majority of the coping behaviours had a significant positive relationship with higher scores in depressive symptoms. The coping behaviours with the largest effect and a moderate to strong association were Item 13, “criticizing myself” ( r s (1762) = .452, p < .01), followed by Item 11 “using alcohol or other drugs to help me go through it” ( r s (1762) = .387, p < .01).
https://doi.org/10.1371/journal.pone.0291555.t003
Table 4 shows the relationship among approach and avoidant coping behaviours, and demographics. Our analyses indicated that both approach and avoidant coping behaviours had been significantly used to a greater extent by the female over male PhD students, by students without a live-in partner than those with a live-in partner, and by those without live-in children than those with live-in children. There is no evidence that the students of a particular age group were using avoidant coping more than those of another age group. However, students aged 25–34 were using approach coping behaviours less than other groups, and those aged 45–54 more ( Table 5 ).
https://doi.org/10.1371/journal.pone.0291555.t004
https://doi.org/10.1371/journal.pone.0291555.t005
Our analyses indicated that female PhD students, who had significantly lower PHQ-8 Depression scores, were using Table 3 ‘s Items 15 ( t [1778] = 14.61, p < .001) and Item 7 ( t [480] = 15.11, p < .001) significantly more than male students. Also, those without live-in partners were getting comfort and understanding from someone to a significantly greater extent than those without ( t [702] = 20.09, p < .001). PhD students without live-in children were taking action to try to make the situation better significantly more than those who have them ( t [894] = 25.21, p < .001).
Predictors of depression and relative influence
Covid-19-related circumstances (receiving an extension, impact reasons, and impact results), performance satisfaction, and coping behaviours (approach and avoidant) were entered together as predictors of depression. Demographics (gender, age, live-in partner, and live-in children), PhD characteristics (discipline, PhD phase, PhD mode, funding, interest in HE, and likelihood in HE) and external incidents were used as control variables. Table 6 reports the findings of the analyses.
https://doi.org/10.1371/journal.pone.0291555.t006
Prediction success overall was 95.3% (83.1% for not significant depression and 98.0% for significant depression). The Wald criterion demonstrated that not having an extension ( p = .014), having caring responsibilities ( p < .001), and using approach ( p < .001) or avoidant ( p < .001) coping behaviours made significant contributions to prediction. The OR value indicated that in the case that PhD students were not receiving an extension amid the Covid-19 disruption, or they did not know whether they were receiving one yet, they were 5.4 times more likely to experience significant depression. For the impact reason, our findings showed that–compared to those who experienced personal illness–PhD students who had caring responsibilities (e.g., childcare or other) showed slightly lower depressive symptoms (OR = 0.10). The OR for approach and avoidant coping behaviours were 0.13 and 43.73, respectively. This finding indicates that when approach coping is raised by one unit (e.g., +1 to the score), we see evidence for better mental health, while when avoidant coping is raised by one unit, a PhD student is very likely (44 times) to experience significant depression.
Turning to our control variables, PhD students with children in the household and with live-in partners showed significantly higher odds (about 14 and 7 times more, respectively) of having or developing depressive symptoms than those without. The latter can be explained by the fact that 88% of the participants with live-in partners also reported having live-in children. Also, male students were slightly more likely than female students to experience significant depression (with a borderline p-value), but this might be explained by the significantly increased use of coping approaches by female students. This gender-related finding that shows nearly no difference between the two categories slightly differs from Goldstone and Zhang’s model [ 15 ] which highlights a difference between female and male participants’ mental wellbeing. This difference can be explained by the fact that the research instruments used in the two studies were different, as well as the survey period.
Some PhD characteristics that made significant contributions to prediction were the discipline of PhD studies and the interest of students to remain in academia after finishing their PhD projects. The risk of experiencing significant depression in PhD students in social sciences (OR = 9.68) was lower than in students conducting a PhD in natural sciences. In contrast to findings by Levecque et al. [ 9 ], we observed that PhD students expressing a high interest in an academic career were 3.5 times more likely to develop depressive symptoms than those with no or only little interest in remaining in academia. Further, those considering having a high likelihood of remaining in academia were slightly more depressed (OR = 3.73), as well as those who were in the executing phase of their PhD research (OR = 3.33). No differences between funded and self-funded students were detected. Finally, the OR for the external incident variable was 6.13, indicating that for each incident unit (e.g., one more incident), we see evidence for depressive symptoms that are six times worse.
Our study contributes new empirical data and new insights needed to develop knowledge on the effect of university research disruption on the PhD student population. In turn, new knowledge may provide the evidence base for university and research policy.
Exploring mental health and coping behaviours
Our first contribution is to provide empirical estimates for the performance satisfaction, prevalence of mental health problems, and coping behaviours of PhD students during the pandemic-induced research disruption, on the basis of representative data across disciplines and across universities in the UK.
Our findings show that most UK PhD students across universities and disciplines report that their research progress has been affected negatively (86%). By contrast, in pre-pandemic periods, 79% of UK PhD students across Universities and disciplines had indicated excellent research progress [ 11 ]. This shift within the same population is important to reveal because of its potential implications for PhDs’ careers and university research capacity and innovation, as we know that dissatisfaction about the PhD trajectory is tied to negative outcomes such as attrition and delay [ 24 , 28 ], but also to lower productivity [ 58 ].
We found that during the period of severe research disruption caused by the Covid-19 pandemic, 75% of the UK students surveyed from 94 universities and across disciplines self-reported in the moderate-severe range for depression. This is at least three times more compared to the reported prevalence of depression among the general population internationally during the Covid-19 outbreak (16–28%, [ 59 ]). Our findings are also in line with findings in Goldstone and Zhang’s study [ 15 ] on UK postgraduate students’ mental wellbeing during the pandemic, in which 72% of the surveyed students were found to demonstrate possible or probable depression or anxiety.
By adopting widely used standardised questionnaires, our findings provide an accessible benchmark for the comparison with studies that took place among PhD student populations in periods of HE stability (pre-2020), thereby providing the empirical basis to accurately estimate the issue of poor mental health among PhD students during a period of research disruption. Using the same questionnaire as in our survey (PHQ-9) and drawing on a sample of PhD students from multiple universities and across research disciplines, a pre-pandemic global survey reported that 39% of PhD students scored in the moderate-severe range for depression [ 12 ]. Pre-pandemic national surveys of PhD students across institutions and disciplines report similar rates of depression, between 32% (in Belgium, Levecque et al. [ 9 ] and 38% (in the Netherlands, Van der Weijden et al. [ 60 ]. In a pre-pandemic (2018–2019) survey of UK PhD students across 48 universities and disciplines, only 25% reported levels that would indicate probable depression or anxiety [ 11 ]. These comparisons indicate that the prevalence of depression among the UK PhD student population of our study during the pandemic-induced period of research disruption is two-to-three times more than that which was reported in periods of stability for the UK PhD student population, for PhD student populations of other countries, and the global PhD population.
Our findings on PhD students’ mental health and PhD students’ coping advance past literature [ 22 , 23 , 34 ] in two significant ways. First, by using a highly reliable coping measure (COPE), we are able to demonstrate the relationship between coping styles and mental health outcomes in PhD students in a way that allows for comparisons and to build further research in this area. Second, we identify specific coping behaviours amongst the UK PhD students that are associated with lower depression scores and some that have a negative association with depression (i.e., getting comfort and understanding from someone and taking action to try to make the situation better ). Both are ‘coping approach’ behaviours (i.e., attempts to reduce stress by alleviating the problem directly; [ 50 ]). Studies using COPE in other populations have also linked coping-approach behaviours to fewer symptoms of psychological distress [ 45 ], more physical and psychological well-being at work [ 46 ], and an absence of anxiety and depression [ 61 ].
Factors explaining PhD students’ depression
Our second contribution is to explain–within the UK PhD population–whose mental health is more affected by the pandemic-induced research disruption. We find that several factors have a significant impact on PhD students to have or develop mental health issues during a period of research disruption.
Consistent with past research on PhD students’ mental health, our findings reveal the significant influence of their personal lives on poor mental health. The relationships we observed during a period of research disruption, however, differ from those suggested in studies conducted in periods of stability (e.g., [ 9 , 22 , 25 , 26 , 62 ]). We found that PhD students with live-in children or with a live-in partner and PhDs with caring responsibilities are more likely to have or develop significant depression compared to those without. This difference can be explained by the closure of schools that resulted in parents home-schooling their children, a greater demand for devices and the internet in households, and parents going through emotional hardship [ 63 ]. We additionally find six times worse depressive symptoms for each ‘external life incident’ (e.g., childbirth, moving home) that occurred in the PhD students’ lives. A larger number of external incidents were found to be associated with students with live-in partners and students with live-in children, which may explain these as reinforcing negative effects. These new insights explain that–although most of these realities in PhD students’ personal lives existed besides the research disruption—when combined with the research disruption, their mental health can spiral downward.
Our findings also address the role of structural PhD characteristics (PhD discipline and PhD phase) in predicting whether a student might present mental health issues in times of research disruption. We find that in a period of research disruption, the risk of significant depression is higher in the execution phase of the PhD compared to the beginning or extension phases, contrary to Levecque and colleagues’ findings [ 9 ]. Because there is very limited research on the PhD stage and mental health, our findings contribute insights to a broader community of scholars who advocate for the further study of the challenges in each PhD stage discreetly (e.g., [ 32 ]). Furthermore, we find that the risk of experiencing significant depression in PhD students in social sciences was lower than students conducting a PhD in natural sciences. Our survey respondents offered explanations on the role of PhD discipline in mental health during the pandemic in the open text responses. These converge on the fact that natural sciences often require being physically in a laboratory, which is probably unfeasible when university facilities are closed.
In tune with past research on finances and mental health in PhD students [ 9 , 64 ], we found those without funded extensions are more likely to have or develop significant depression (moderate, moderately severe, and severe) compared to those with them. We reveal the size of this association (about 5.5 times more) and link PhD funding extensions to standardized assessments of depression prevalence, thus uniquely providing new evidence for policy scholars.
Implications for research and higher education policy
Our findings show an alarming increase in self-reported depression levels among the UK PhD student population. The long-term mental health impact of Covid-19 may take years to become fully apparent, and managing this impact requires concerted effort not just from the healthcare system at large [ 59 ] but also from the HE sector specifically. With mental illness a cause for PhD student attrition, loss of research capacity and productivity, data from our survey should prompt consideration of immediate intervention strategies.
For research and education policy scholars, our findings contribute directly to the development of evidence-based research and university policies on support for targeted groups of PhD students in times of disruption. Specifically, our findings show that institutional and funder support should not only be in the form of PhD-funded extensions–which are nevertheless shown in our study and other studies (e.g., [ 15 ]) to be very significant. But also, in the form of providing expedited alternatives to the changes evoked by the pandemic for PhD students, such as new and adjusted policies that explicitly consider those PhDs with caring responsibilities, since 77% of our respondents reported that childcare and other caring responsibilities are the reason for dissatisfaction with their PhD progress. If not, the Covid-19 research disruption could erase decades of progress towards equality in academia [ 65 ].
Our main contribution is that we offer insights into how to mitigate mental health consequences for PhD students in times of research disruption. Individual-driven coping behaviours are suggested to be of equal importance to those promoted by the PhD students’ institutions [ 66 ]. In this study, approach coping behaviours were found to associate with lower depression levels, which may eventually contribute to PhD completion. The importance of developing coping mechanisms has also been highlighted in pre-pandemic studies, with, for instance, mothers finding ways to combine academic work and family responsibilities and succeed in both roles [ 38 ]. Still, institutions may play a crucial role in offering training for PhD students on coping and wellbeing through, for instance, a virtual platform to comply with social distancing policies. Such efforts may include mental health support and coping behaviour guidance, so that students are guided on how to successfully deal with disruptions (for example, to avoid avoidant coping behaviours that may lead them to higher levels of depression). Pre-pandemic reforms have previously shown that a well-structured programme and well-timed financial support can facilitate and uphold PhD completion, alongside student efforts [ 35 ]. As the future generation of academics, PhD students would be better equipped to handle the current and future disruptions and better cope with other disruptions in their academic journeys.
Limitations and implications for further research
Although our study has gone some way towards enhancing our understanding of Covid-19-related effects on UK PhD students’ mental health, it is plausible that a number of limitations could have influenced the results obtained. First, while our research attracted a representative number of students from different age groups, PhD modes, phases and funding, there was a very strong presence of students in natural sciences [ 17 ]. Second, as this was a cross-sectional study, we did not follow the UK PhD population longitudinally, and we may not offer insights into the trajectory of the relationships we articulate in our findings. Nevertheless, our adoption of standardized questionnaires allows for a platform for comparisons with past and future research efforts. Third, findings in this survey are based on self-report and may be subject to unconscious biases (e.g., PhD students assessing themselves or the situation inaccurately). Fifth, the research undertaken employed the PHQ-8 with a specific emphasis on assessing aspects related to depression. It is important to acknowledge that while these questionnaires offer valuable insights into depression, they may not comprehensively encompass the broader spectrum of general mental health. Therefore, the findings of the study should be interpreted within the context of its targeted focus on depression, recognizing the potential existence of other dimensions of mental health that were not directly addressed within this research framework. Finally, despite the high percentage of prediction in our findings (80%), additional factors may likely explain variabilities in our study outcomes, such as leadership factors or supervision styles in the 94 UK Universities whose PhD students participated in our survey.
As our study strongly demonstrates, juxtaposing findings from studies conducted during periods of relative HE stability with those conducted during periods of disruption is a fruitful approach for advancing research and university policy. By identifying which insights that would have been invaluable during periods of stability are less so during a period of disruption, scholars can provide significant advancements to existing research and new insights for policy, research and HE leadership.
Conclusions
Our study extends previous research on mental health in the HE sector by considering the dynamics of a severe disruption as opposed to the dynamics of relative stability in PhD mental health and coping behaviours. Drawing on our insights into these interrelationships, we suggest extensions to the literature on PhD students’ mental health, research and university policy. With our findings, HE leaders and policymakers may be better placed to tackle and ultimately overcome this and future research disruptions.
Acknowledgments
The authors would like to thank all the PhD students who committed time for taking part in this study and their responses informed the writing of this paper.
- View Article
- Google Scholar
- 3. O’Malley B. 180 congressmen support call for US$26bn research support. University World News [Internet]. 2020 [cited 2023 Jan 15]; Available from: https://www.universityworldnews.com/post.php?story=20200502080814674
- PubMed/NCBI
- 39. Drake KL. Psychology Graduate Student Well-being: The Relationship between Stress, Coping, and Health Outcomes. University of Cincinnati; 2010.
- 40. Pychyl T. Personal projects, subjective well-being and the lives of doctoral students. | CURVE [Internet]. Carleton University; 1995 [cited 2023 Jan 15]. Available from: https://curve.carleton.ca/d330c15c-eeaa-459c-afea-4bf841b7daa0
- 48. Aristeidou M, Aristidou A. PhDMentalHealth_UKDataset [Internet]. The Open University; 2023 [cited 2023 May 10]. Available from: https://ordo.open.ac.uk/articles/dataset/PhDMentalHealth_UKDataset/22794203/0 .
- 65. Malisch JL, Harris BN, Sherrer SM, Lewis KA, Shepherd SL, McCarthy PC, et al. Opinion: In the wake of COVID-19, academia needs new solutions to ensure gender equity [Internet]. Vol. 117, Proceedings of the National Academy of Sciences of the United States of America. National Academy of Sciences; 2020 Jul [cited 2023 Jan 15]. Available from: https://www.pnas.org/lookup/suppl/doi:10.1073/pnas.2010636117/-/DCSupplemental .

Children and Young People's Mental Health

- UCL Wellcome 4-year PhD in Mental Health Science
- UCL-Birkbeck MRC Doctoral Training Programme
- ESRC/BBSRC Soc-B Centre for Doctoral Training
- ESRC UCL, Bloomsbury and East London Doctoral Training Partnership
- Doctorate in Child and Adolescent Psychotherapy
- Doctorate in Clinical Psychology
London School of Hygiene & Tropical Medicine
The London School of Hygiene & Tropical Medicine is one of the world's leading public health universities.
Our vision is to help create a more healthy, sustainable and equitable world for everyone, because we believe our shared future depends on our shared health.
How AI and microscopes can help fight infection

Inaugural Lecture of Professor Ambrose Agweyu

Corporate group discount
LSHTM is offering a 25% discount for any organisations sponsoring four or more staff members to study the Health in Humanitarian Crises programme by distance learning.
Discover what it's like to study with us via our open days, virtual tours and study visits
staff working in over 100 countries across the world
Our world-leading teaching and research activities share a collective purpose to improve health worldwide. If you're curious and passionate about public and global health, join our student community.

Discover ways to support the School
LSHTM Scholarship Fund
With your help, we can widen access to education at LSHTM through the provision of scholarships. Scholarships are transformational, have the capacity to change the lives of the students who receive them, and alleviate the financial burden of study for talented and motivated recipients.
Annual research income for LSHTM
in the world for public health (Shanghai Ranking 2023)
We are home to many cross-institution networks of researchers, collaborating and innovating to address major global health challenges.


IMAGES
VIDEO
COMMENTS
The UCL Wellcome 4-year PhD in Mental Health Science is an opportunity for students to train in a wide range of fields relevant to mental health research. This programme, funded in 2019, is the first of its kind in the UK, representing an investment of over £5m by the Wellcome Trust.
SHPS Doctoral Enquiries. +44 (0) 20 7040 5972. [email protected]. Help us to improve this page. A PhD/MPhil in Mental Health at City, University of London offers you the opportunity to carry out research that will make a real difference to people's lives.
An international first, the PhD in Mental Health meets the needs of those wishing to gain a deep and critical insight into mental health theory, research and practice and to develop or enhance research skills whilst fulfilling their existing responsibilities. The programme is offered part-time and combines innovative distance learning with face ...
PhD/MPhil Mental Health. Take the first steps towards your chosen career by undertaking your postgraduate training in a world leading research environment. Home; Study; ... PhD (full-time) UK students (per annum): Standard £4,786, Low £11,000, Medium £17,500, High £23,000
See: King's PhD Programme in Mental Health Research for Health Professionals. ... You can get in touch with us by email at [email protected] in case you have any further questions. Closing date. Thursday 1st December 2022. Interviews. w/c 8 May 2023 . Study at King's. View a prospectus.
The UCL Division of Psychiatry is a world-leading interdisciplinary centre for research into mental health and illness. We offer a broad range of possible PhD supervisors to help you gain the skills you will need for a career in mental health research - from bench and biology to neuroscience, psychology and applied clinical research.
The Wellcome-UCL 4 year PhD Programme in Mental Health Science provides a platform for interdisciplinary research necessary for effective translation of findings from work on mechanisms and risk factors into novel treatments and prevention strategies. Its ultimate objective is to train scientists and policy leaders for whom interdisciplinary ...
Programme description. Our PhD/MPhil Mental Health programme enables you to undertake a research project that will improve understanding of Mental Health. Our postgraduate research programmes in mental health are based on individually tailored projects. Applicants are specifically matched with a primary academic supervisor according to their ...
The Midlands hosts the most innovative centres in mental health and neurosciences (MH&N), including digital mental health, clinical trials, neuroimaging, and epidemiology, serving an area of huge clinical need. The Midlands Mental Health & Neurosciences PhD Programme is led by the University of Nottingham, in collaboration with University of ...
Start dates: 1st October, 1st January, 1st April, 1st July. Developing and evaluating effective evidence-based mental health services to support people at some of the most challenging times of their lives depends on high-quality research. Studying for a PhD in Mental Health will give you the opportunity to pursue your own personal or ...
04 March 2022. Prospective students are invited to apply for this Mental Health Research UK funded PhD scholarship based at the ESRC Centre for Society and Mental Health, King's College London. This will be a 4-year full-time PhD starting in October 2022. The scholarship will cover tuition fees and a stipend.
The PhD supervisors have also been selected across departments from King's campuses, for their expertise in core areas of relevance to mental health. Collectively, the supervisor pool - comprised of health professional and fundamental scientists - provides knowledge in translational neuroscience, digital mental health and social science and ...
A new King's College London PhD programme will provide mental health research training fellowships to doctors, nurses, psychologists and allied health professionals. The eight-year programme, offering 25 fellowships, has been funded by a grant of £7.8m from Wellcome Trust, with additional funding or support from a number of partners.
University of Reading School of Psychology & Clinical Language Sciences. I invite applications to ([email protected]) for self-funded students for PhD proposals in an area relating to nutrition, metabolism, cognitive function, mental health and the gut-brain axis. Read more. Supervisor: Dr D Lamport.
PhD Competition 2025 Mental Health Research UK (incorporating the Schizophrenia Research Fund) is pleased to announce a competition for 2 PhD Scholarships beginning September 2025. We are inviting applications for PhD scholarships under the theme of maternal mental health. We view this topic in its broadest sense inviting proposals that cover ...
The results don't prove that pursuing a PhD directly contributes to mental-health problems, says study co-author Clio Berry, a research psychologist at Brighton and Sussex Medical School, UK.
Mental health prevalence statistics for the UK general population suggest 25% (1 in 4) (Time to Change, 2015) of people experience mental health problems; whereas, in the present sample ...
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
Sadly, 42% of PhD students reported that they believed having a mental health problem during your PhD is the norm. We also found similar numbers saying they have considered taking a break from their studies for mental health reasons, with 14% actually taking a mental health-related break. Finally, 35% of PhD students have considered ending ...
UK PhD students' mental health in times of disruption. In the UK, there are approximately 100,000 postgraduate students completing doctoral research [].Since 2018, significant government funding has been targeted at developing insights into supporting UK PhD students' mental health [].Still, with the exception of Byrom et al. [], published research on PhD students' mental health in the ...
UCL leads PhD training programmes relevant to child and adolescent mental health, including the Wellcome 4-year PhD in Mental Health Science and the UK's largest clinical psychology doctoral training programme. UCL also hosts and participates in several funded PhD programmes relevant to child and adolescent mental health, supported by UK research councils and Wellcome, including one for ...
Improving health worldwide. The London School of Hygiene & Tropical Medicine is one of the world's leading public health universities. Our vision is to help create a more healthy, sustainable and equitable world for everyone, because we believe our shared future depends on our shared health. Discover more about us.