- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
November 22, 2023
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source

Researchers develop 'game-changing' dental implant technology
by University of California, Los Angeles

A team of UCLA School of Dentistry researchers led by Takahiro Ogawa, D.D.S., Ph.D., has culminated a decade of dental implant research with the development of a cutting-edge technology that ensures near-perfect osseointegration, faster healing times, and significantly reduced complications for patients.
A device blasting one minute of ultraviolet (UV) light treatment on titanium implants —done chairside immediately prior to an implant procedure—has recently come to market and holds opportunities for applications beyond dentistry.
"We have entered a new era in dental implantology," said Dr. Ogawa. "This UV technology not only enhances the effectiveness of dental implants but also improves the quality of life for patients. The possibilities are limitless, and I am incredibly excited about the potential impact on oral and overall health."
Dr. Ogawa and colleagues in the Weintraub Center for Reconstructive Biotechnology team identified a key obstacle in the advancement of dental implant science, which had stagnated for three decades: A layer of hydrocarbons naturally deposited on implant surfaces called titanium pellicle, hindering the integration process. This is also associated with significant post-op complications, with peri-implantitis (gum disease around implants) occurring in 35%–40% of patients.
In response, the team developed a method to remove these hydrocarbons via UV light, which took 48 hours in early trials. Researchers gradually reduced UV treatment times to 12 minutes, but performing the procedure chair-side just before implant surgery only became feasible with their one-minute hydrocarbon removal breakthrough in late 2022. The process is chronicled in an article published in the Journal of Functional Biomaterials , authored by Dr. Ogawa and his team.
The impact of this technology is profound. UV-treated implants exhibit nearly 100% bone integration, doubling their anchoring capability and reducing bacterial susceptibility by 60% compared to untreated control implants. This means faster healing, lower risk of complications, and increased suitability for a larger portion of the patient population, including aging patients, smokers, and those with diabetes and osteoporosis among other conditions.
A follow-up journal article in which Dr. Ogawa is the primary author, published Oct. 29 in Cells , demonstrates how one-minute UV treatment induces unprecedented action of gingival (gum) cells to seal the implants, limiting bacterial invasion and reducing incidents of peri-implantitis.
"Our goal is to eradicate peri-implantitis," said Dr. Ogawa.
Additionally, the technology allows for more versatile occlusion, eliminating the need for smaller implant crowns and reducing the number of required bridge implants.
Dr. Ogawa is energized by the potential use of UV-treated implants in the broader medical world.
"Orthopedic implants like hip joint reconstruction and spine fixation show a high incidence of revision surgery and complications. I believe UV-treated implants will help mitigate them," he said.
Toshikatsu Suzumura et al, Vacuum Ultraviolet (VUV) Light Photofunctionalization to Induce Human Oral Fibroblast Transmigration on Zirconia, Cells (2023). DOI: 10.3390/cells12212542
Explore further
Feedback to editors

Combining popular diabetes drugs offers complementary heart and kidney benefits, research finds
4 hours ago

Highly accurate AI model can estimate lung function just by using chest X-rays

A research team may have discovered the neurological mechanism underlying a common eating disorder
5 hours ago

Study: Raw milk is risky, but airborne transmission of H5N1 from cow's milk is inefficient in mammals
6 hours ago

Erasing 'bad memories' to improve long term Parkinson's disease treatment

Researchers discover the role of RNF114B, a key gene in the progression and treatment of lung adenocarcinoma

Small molecules induce trained immunity, opening a new approach to fighting disease

Researchers find a common immune system mechanism between pregnancy and cancer

New research supports 'social good' as a cognitive approach to dealing with highly stressful events

Study: Americans find hospital-at-home care appealing and safe
9 hours ago
Related Stories

AI helps predict treatment outcomes for patients with diseased dental implants
May 12, 2021

Complications following dental implant therapy are common
Jun 18, 2021

Infection-resistant, 3D-printed metals developed for implants
Nov 20, 2023

Breast implant illness uncommon cause of revision surgery
Oct 14, 2022

New study identifies successful method to reduce dental implant failure
Mar 24, 2017

Advanced nanotechnology to improve success of dental implants
Jun 11, 2020
Recommended for you

Blood test measuring protein levels could provide snapshot of overall health
12 hours ago

Bio-based tool quickly detects concerning coronavirus variants
11 hours ago

Pulsed field ablation procedures found safe and effective for atrial fibrillation patients

Scientists develop bandage that measures glucose levels in sweat using microlaser technology

Researchers aim to change contraceptive technology with new iron IUDs
Jul 5, 2024

Re-engineering cancerous tumors to self-destruct and kill drug-resistant cells
Jul 4, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- World J Stem Cells
- v.15(3); 2023 Mar 26
- PMC10052340
Clinical trials using dental stem cells: 2022 update
Wen-peng song.
Department of Stomatology, Beijing Tiantan Hospital, Capital Medical University, Beijing 100070, China
Lu-Yuan Jin
Department of General Dentistry and Integrated Emergency Dental Care, Beijing Stomatological Hospital, Capital Medical University, Beijing 100050, China
Meng-Di Zhu
Deng-sheng xia.
Department of General Dentistry and Integrated Emergency Dental Care, Beijing Stomatological Hospital, Capital Medical University, Beijing 100050, China. nc.ude.umcc.liam@aixsd
Supported by the National Natural Science Foundation of China, No. 82071073 and No. 82270951 .
Corresponding author: Deng-Sheng Xia, DDS, Assistant Professor, Department of General Dentistry and Integrated Emergency Dental Care, Beijing Stomatological Hospital, Capital Medical University, No. 4 Tiantan Xili, Dongcheng District, Beijing 100050, China. nc.ude.umcc.liam@aixsd
For nearly 20 years, dental stem cells (DSCs) have been successfully isolated from mature/immature teeth and surrounding tissue, including dental pulp of permanent teeth and exfoliated deciduous teeth, periodontal ligaments, dental follicles, and gingival and apical papilla. They have several properties (such as self-renewal, multidirectional differentiation, and immunomodulation) and exhibit enormous potential for clinical applications. To date, many clinical articles and clinical trials using DSCs have reported the treatment of pulpitis, periapical lesions, periodontitis, cleft lip and palate, acute ischemic stroke, and so on, and DSC-based therapies obtained satisfactory effects in most clinical trials. In these studies, no adverse events were reported, which suggested the safety of DSC-based therapy. In this review, we outline the characteristics of DSCs and summarize clinical trials and their safety as DSC-based therapies. Meanwhile, we also present the current limitations and perspectives of DSC-based therapy (such as harvesting DSCs from inflamed tissue, applying DSC-conditioned medium/DSC-derived extracellular vesicles, and expanding-free strategies) to provide a theoretical basis for their clinical applications.
Core Tip: Since dental pulp stem cells were first isolated and identified in 2000, a variety of dental stem cells (DSCs) have been reported. DSCs have shown satisfactory clinical effects in the treatment of a variety of diseases and have great potential for clinical application. This paper will summarize DSC-based clinical trials and put forward the current limitations and perspectives to accelerate and extend the clinical application of DSCs.
INTRODUCTION
Mesenchymal stem cells (MSCs) are a population of unspecialized cells characterized by the properties of self-renewal and multidirectional differentiation[ 1 , 2 ]. Currently, MSCs are currently being explored for the treatment of many diseases, such as cardiovascular disease, neurodegenerative diseases, dental diseases, and metabolic diseases[ 1 ].
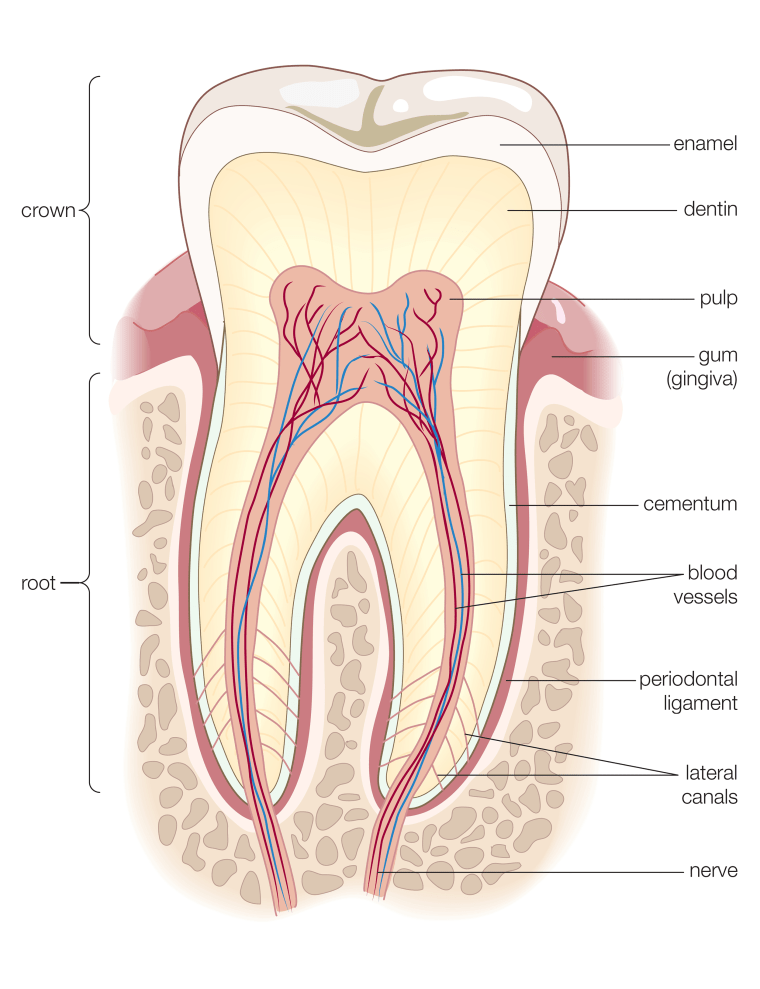
Dental SCs (DSCs) were reported to have similar features to MSCs[ 3 ]. Since dental pulp SCs (DPSCs) were first successfully isolated from the extracted third molar in 2000[ 4 ], multiple DSC types have been harvested from mature and immature teeth and their surrounding tissues, including periodontal ligament stem cells (PDLSCs), stem cells from apical papilla (SCAP), stem cells from exfoliated deciduous teeth (SHED), gingiva-derived mesenchymal SCs (GMSCs), and dental follicle progenitor cells (DFPCs)[ 5 - 7 ] (Figure (Figure1). 1 ). DSCs develop from the neural crest and express both stem cell markers and neural markers[ 8 , 9 ]. It was reported that DSCs have the potential for multipotent differentiation into osteogenic, chondrogenic, adipogenic, neurogenic, odontogenic, dentinogenic cells, and so on[ 10 ]. In addition to their self-renewal and differentiation properties, DSCs have also been reported to be involved in secretion, immunomodulation, and tumor processes[ 3 , 11 ]. Based on the characteristics of DSCs, many clinical articles and clinical trials have used DSCs in tissue regeneration and the treatment of various diseases, such as pulpitis, periapical lesions, and periodontitis[ 12 ].

Tissue origin, harvest, characteristics, and clinical application potential of the various populations of dental stem cells. Dental pulp stem cells and stem cells from exfoliated deciduous teeth can be isolated from the inner dental pulp of permanent teeth and deciduous exfoliated teeth, respectively. Stem cells from apical papilla can be extracted from the apical papilla; periodontal ligament stem cells can be harvested from the periodontal ligament; and dietary fiber supplementation combinations can be derived from the dental follicle. Gingiva-derived mesenchymal stem cells can be extracted from gingiva. Citation: Sharpe PT. Dental mesenchymal stem cells. Development 2016; 143: 2273-2280[ 139 ]. Copyright ©The Authors 2016. Published by The Company of Biologists Ltd. The authors have obtained the permission for figure using from the Company of Biologists Ltd ( Supplementary material ).
In this study, the current status of clinical articles and clinical trials using DSCs in the treatment of various diseases and conditions are reviewed. In addition, current limitations and perspectives, including harvesting DSCs from inflamed tissue, applying DSC-conditioned medium (CM) and DSC-derived extracellular vesicles (EVs), and expanding-free strategies, are also discussed.
CHARACTERISTICS OF DSCS
Based on their various sources, DSCs are divided into DPSCs, SHED, PDLSCs, SCAP, GMSCs, and DFPSCs (Figure (Figure1). 1 ). DSCs are known to express not only mesenchymal and embryonic stem cell markers (such as CD44, STRO-1, and Nanog) but also neuronal markers because they originate from embryonic neural crests[ 8 , 9 ] (Table (Table1). 1 ). However, they do not express CD34, CD45, or CD11b, which are defined as hematopoietic markers[ 7 ].
Characteristics of different types of dental stem cells
| DPSCs | CD13, CD29, CD44, CD59, CD73, CD90, CD105, CD146, STRO-1[ ], CD81, CD49f[ ], CD40, CD120a, CD261, CD262, CD264, CD266, CD121a, CD130, CD213a1, CD217, CDw210b[ ] | OCT-4, Nanog[ ], SSEA-1, SEEA-4[ ], SOX-2[ ] | βIII-tubulin, NFM, Nestin, CNPase[ ], S100, CD271[ ] | Osteogenic, Odontogenic[ ], Dentinogeni, Chondrogenic, Neurogenic, Myogenic, Adipogenic[ ], Hepatogenic[ ] |
| PDLSCs | CD13, CD29, CD44, CD49, CD73, CD90, CD105, CD146, CD166, CD271[ ], CD10[ ], STRO-1[ ] | SSEA-1, SSEA-3, SSEA-4, TRA-1-60, TRA-1-81, OCT-4, Nanog, SOX-2, REX1, and ALP[ ] | Nestin, OCT-4, SSEA-4[ ] CD271, SOX-10[ ], SOX-2[ ] | Osteogenic, Cementogenic, Adipogenic, Chondrogenic, Neurogenic[ ], Hepatogenic[ ], Cardiac myogenic, Endothelial-like, Islet-like, Retinal ganglion-like[ ] |
| SCAP | CD13, CD24, CD29, CD44, CD49, CD51, CD56, CD61, CD73, CD90, CD105, CD106, CD146, CD166, STRO-1, NOTCH-3[ ], CD81, CD49f[ ] | OCT-4, Nanog, SOX2[ ], CD49f[ ] | βIII-tubulin, NFM, Nestin, CNPase[ ], SOX-2[ ], Vimentin, Survivin[ ] | Osteogenic, Dentinogenic, Adipogenic[ ], Neurogenic[ ], Chondrogenic, Hepatogenic[ ] |
| SHED | CD29, CD73, CD90, CD166[ ], STRO-1, CD44[ ], CD105[ ], NOTCH-1, CD10, CD13, CD34, CD106, CD146, CD166, CD271[ ] | OCT-4, Nanog, SSEA-3[ ], SSEA-4[ ], NOTCH-1, OCT-4, SOX-2[ ] | βIII-tubulin, NFM, Nestin, CNPase, GAD, NeuN, GFAP[ ], CD271, Vimentin, OCT-4, PAX-6, NSE, MAP-2, PSA-NCAM, TH[ ] | Osteogenic, Odontogenic[ ], Dentinogenic, Chondrogenic, Neurogenic, Myogenic, Adipogenic[ ], Hepatogenic[ ] |
| DFPCs | CD13, CD29, CD59, CD90[ ], CD105, CD146[ ], CD44, CD73, NOTCH-1, STRO-1[ ] | OCT-4, Nanog[ ], NOTCH-1, SOX-2[ ] | OCT-4, SOX2[ ], Nestin, SOX-2[ ] | Osteogenic, Cementogenic, Odontogenic, Adipogenic, Chondrogenic[ ], Hepatogenic[ ] |
| GMSCs | CD13, CD29, CD44, CD73, CD90, CD105, CD146, STRO-1[ ] | SSEA-4[ ], OCT-4, Nanog[ ] | Nestin, SOX10[ ], βIII-tubulin, NFM, CNPase[ ] | Osteogenic, Adipogenic, Chondrogenic, Neurogenic, Endothelial-like, Odontogenic[ ], Myogenic[ ] |
ALP: Alkaline phosphatase; CD: Cluster of differentiation; CNPase: 2’,3’-cyclic nucleotide 3’-phosphodiesterase; GAD: Glutamic acid decarboxylase; GFAP: Glial fibrillary acidic protein; MAP-2: Microtubule associated protein 2; NeuN: Neuronal nuclei; NFM: Neurofilament medium chain; NGFR: Nerve growth factor receptor; NSE: Neuron-specific enolase; OCT: Octamer-binding transcription factor; PAX-6: Paired Box 6; PSA-NCAM: Polysialylated neural cell adhesion molecule; REX-1: RNA exonuclease 1 homolog; SOX: Sex determining region Y-box; SSEA: Stage-specific embryonic antigen; TH: Tyrosine hydroxylase; SHED: Stem cells from exfoliated deciduous teeth.
Similar to mesenchymal stem cells, DSCs showed the ability of self-renewal and multidirectional differentiation, such as osteogenic, chondrogenic, adipogenic, neurogenic, odontogenic, dentinogenic, cementogenic, and myogenic differentiation[ 13 - 16 ] (Table (Table1). 1 ). In addition, even in the undifferentiated state, DSCs were able to secrete several angiogenic and neurotrophic factors, including vascular endothelial growth factor (VEGF), ciliary neurotrophic factor (CNTF), brain-derived neurotrophic factor (BDNF), glia-derived neurotrophic factor (GDNF), and β-nerve growth factor (β-NGF), to promote angiogenesis and tissue regeneration[ 17 , 18 ].
In addition, the immunomodulatory features of DSCs have also been the focus of a number of studies. First, it was reported that DSCs, like mesenchymal stem cells, faintly express the MHC class II antigen HLA-DR and maintain low immunogenicity[ 19 - 21 ]. Second, local tissue regeneration and inflammation could be influenced by the secretome of DSCs (including the production of inflammatory and anti-inflammatory cytokines and the regulation of immune cells), which is also regulated by the local inflammatory microenvironment[ 21 - 24 ]. Finally, the inflammatory microenvironment could impact the behaviors of DSCs, such as proliferation potential, migration, homing, and differentiation[ 22 ].
Based on the characteristics of DSCs, they have been widely studied in regenerative medicine and tissue engineering and have shown an amazing therapeutic effect on oral-facial, neurologic, corneal, cardiovascular, hepatic, diabetic, renal, muscular, tenogenic, dystrophic and autoimmune conditions in both animal and human models[ 21 , 25 - 27 ]. For example, the proliferation, paracrine effect, and multidirectional differentiation potential of DSCs support the application of DSCs in regenerative medicine ( e.g. , dental pulp and bone tissue regeneration)[ 28 , 29 ]. The anti-inflammatory, immunomodulatory, and immunoevasive properties of DSCs also help in the treatment of plaque psoriasis[ 30 ] (Figure (Figure1). 1 ). DSC-based therapies have broad prospects for clinical application.
It is worth noting that the naming of mesenchymal stem cells and mesenchymal stromal cells remains controversial. Based on the position paper issued by The International Society for Cell & Gene Therapy (ISCT) Mesenchymal Stromal Cell (ISCT MSC) in 2005, mesenchymal stem cells are not equivalent or interchangeable with mesenchymal stromal cells[ 31 ]. Mesenchymal stem cells refer to progenitor cell populations with obvious self-renewal and differentiation functions, while mesenchymal stromal cells refer to large populations with significant secretion, immune regulation, and homing properties[ 32 - 34 ]. As we have just summarized, dental stem cells share some of the characteristics of both mesenchymal stem cells and mesenchymal stromal cells, and more consensus articles may be needed to further define the naming of dental stem cells.
DSC-BASED CLINICAL TRIALS FROM PUBLISHED ARTICLES
Pulpitis and pulp necrosis.
Four studies were reported to treat pulp necrosis or irreversible pulpitis using autologous DPSCs or SHED, including a randomized controlled trial (RCT), two case series, and a case report[ 28 , 35 - 37 ] (Table (Table2). 2 ). Xuan et al [ 28 ] applied SHED in the treatment of pulp necrosis caused by trauma and observed dental pulp tissue regeneration at 12 mo and 24 mo after transplantation. Meanwhile, the results also showed increased dental root length and decreased apical foramen width compared with traditional apexification treatment. Two case series reported by Nakashima et al [ 35 , 37 ] indicated that DPSCs transplanted with granulocyte colony-stimulating factor and gelatin sponges could increase pulp sensitivity and mineralization and recover the signal intensity (SI) of regenerated pulp tissue on MRI examination. Meza et al [ 36 ] transplanted DPSCs and leukocyte platelet-rich fibrin (L-PRF) harvested from autologous inflamed dental pulp and blood, respectively, to the root canal of irreversible pulpitis teeth and observed dentin bridge formation and a response to the cold test and electric pulp test.
Dental stem cell-based clinical trials from published articles
| Xuan [ ], 2018 | NCT01814436 | Pulp necrosis | RCT | Autologous deciduous pulp | Implanted into injured teeth | SHED ( = 26) | Traditional apexification treatment ( = 10) | 12 mo; 24 mo | Dental pulp tissue regeneration; no adverse events observed; the length of the root (↑); the width of the apical foramen (↓) |
| Nakashima [ ], 2022 | None | Irreversible pulpitis | Case series | Autologous dental pulp | Transplanted into the root canal | DPSCs + Gelatin sponge + G-CSF ( = 5) | None | 1, 2, 4, 12, 24, 28, 32 wk | Pulp sensibility (↑); MRI examination showed similar SI between test teeth and untreated controls |
| Nakashima [ ], 2017 | None | Irreversible pulpitis | Case series | Autologous dental pulp | Transplanted into the root canal | DPSCs + Gelatin sponge + G-CSF ( = 2) | None | 1, 4, 12, 24, and 48 wk | MRI examination showed similar SI between test teeth and untreated controls; mineralized tissue deposition (↑) |
| Meza [ ], 2019 | None | Irreversible pulpitis | A case report | Autologous inflamed dental pulp | Transplanted into the root canal | DPSCs + L-PRF ( = 1) | None | 6 mo; 3 year | Delayed response to the cold test; positive response to electric pulp testing; dentin bridge formation |
| Shiehzadeh [ ], 2014 | None | Periapical lesions | Case series | Case 1 and case 3: Autologous apical papilla; case 2: Deciduous pulp | Case 1 and Case 3: Injected from root apex to cavity; case 2: Injected into the defect a surgical approach | Case 1 and Case 3: SCAP + PEG-PLGA scaffold ( = 2); case 2: SHED + PEG-PLGA scaffold ( = 1) | None | Case 1: 30 d, 3 mo, 1 year; 2 year; case 2: 3, 6, 18 mo; case 3: 3, 6, 12, 24 mo | Developed mature apices; periapical tissue healing (↑) |
| Prasad [ ], 2017 | None | Periapical lesions | Case series | Allogeneic deciduous pulp | Transplanted into the root canal | SHED + Bioglass ( = 2) | None | 7, 30, 90, 180, 365 d | Closure of open apex; periapical tissue healing; positive response to electric pulp testing and cold testing |
| Prasad [ ], 2019 | None | Periapical lesions | A case report | Allogeneic deciduous pulp | Transplanted into the root canal and periapical area | SHED + Bioglass ( = 1) | None | 2 wk; 4, 12, 24 mo | Periapical tissue healing; positive response to electric pulp testing |
| Ferrarotti [ ], 2018 | NCT03386877 | Periodontal intrabony defects | RCT | Autologous dental pulp | Implanted into bone defect sites consisted of MIST | Pulp micrografts + Collagen sponge ( = 15) | Collagen sponge ( = 14) | 6 and 12 mo | PD (↓); CAL (↓); bone defect fill (↑); residual PD < 5 mm and CAL gain ≥ 4 mm (↑) |
| Sánchez [ ], 2020 | ISRCTN13093912 | Periodontal intrabony defects | CCT | Autologous periodontal ligament | Implanted into bone defect sites surgical approach | PDLSCs + β-TCP ( = 9) | β-TCP ( = 10) | 1, 3, 6, 9, 12 mo | CAL (-); PPD (-) |
| Feng [ ], 2010 | None | Periodontal intrabony defects | Case series | Autologous periodontal ligament | Implanted into bone defect sites surgical approach | PDLPs + HA/TCP ( = 3) | None | 3, 6, 12, 32, 42, and 72 mo | CAL (↓); PD (↓); GR (↑) |
| Chen [ ], 2016 | NCT01357785 | Periodontal intrabony defects | RCT | Autologous periodontal ligament | Implanted into bone defect sites surgical approach | PDLSCs sheets + DBBM ( = 20) | DBBM ( = 21) | 2 wk; 3, 6, 12 mo | CAL (-); PD (-); GR (-) |
| Iwata [ ], 2018 | UMIN000005027 | Periodontal intrabony defects | Case series | Autologous periodontal ligament | Implanted into bone defect sites surgical approach | PDL-derived cell sheets + β-TCP ( = 10) | None | 3, 6, 55 ± 19 mo | CAL (↓); PD (↓); bone height (↑) |
| Vandana [ ], 2015 | None | Periodontal intrabony defects | A case report | Autologous periodontal ligament | Implanted into bone defect sites via surgical approach | Periodontal ligament soft tissue + Gelatin sponge + Cementum scrapings ( = 1) | None | 1 wk; 3, 6, 12 mo | CAL (↓); PD (↓); BMD (↑) |
| Aimetti [ ], 2014 | None | Periodontal intrabony defects | A case report | Autologous dental pulp | Implanted into bone defect sites surgical approach | Pulp micrografts + Collagen sponge ( = 1) | None | 6 mo; 1 year | PPD (↓); bone fill (↑) |
| Aimetti [ ], 2018 | None | Periodontal intrabony defects | Case series | Autologous dental pulp | Implanted into bone defect sites surgical approach | Pulp micrografts + Collagen sponge ( = 11) | None | 1 year | CAL (↓); PD (↓); bone fill (↑) |
| Aimetti [ ], 2015 | None | Periodontal intrabony defects | Case series | Autologous dental pulp | Implanted into bone defect sites surgical approach | Pulp micrografts + Collagen sponge ( = 4) | None | 6, 12 mo | PD (↓); CAL (↓); bone fill (↑) |
| Hernández-Monjaraz [ ], 2018 | ISRCTN12831118 | Periodontal intrabony defects | A case report | Allogeneic dental pulp | Implanted into bone defect sites surgical approach | DPSCs + Lyophilized collagen-polyvinylpyrrolidone sponge scaffold ( = 1) | None | 3, 6 mo | PD (↓); TM (↓); bone fill (↑) |
| Barbier [ ], 2018 | EudraCT database 2014-001913-18 | Post-extraction sockets | Split-mouth RCT | Autologous dental pulp | Implanted into postextraction sockets | Pulp micrografts + collagen matrix ( = 30) | Collagen matrix ( = 30) | 6 mo | BMD (-); interdental septum height (-) |
| Cubuk [ ], 2023 | NCT04641533 | Post-extraction sockets | Split-mouth RCT | Autologous dental pulp | Implanted into postextraction sockets | Pulp micrografts + L-PRF ( = 13) | L-PRF ( = 13) | 7 d; 6 mo | PPD (-); CAL (-); vertical bone loss (-); relative bone density (-) |
| d’Aquino [ ], 2009 | None | Post-extraction sockets | Split-mouth CCT | Autologous dental pulp | Implanted into postextraction sockets | Dental pulp stem/progenitor cells + collagen sponge ( = 7) | Collagen sponge ( = 7) | 7 d; 1, 2, 3, 12 mo | Rate of mineralization (↑); levels of cortical bone (↑); CAL (↓); BMP-2, VEGF (↑) |
| Tanikawa [ ], 2020 | NCT03766217 | Cleft lip and palate | Historical control study | Autologous deciduous pulp | Placed into the alveolar defect via surgical approach | SHED + Hydroxyapatite-collagen sponge ( = 6) | rhBMP-2 + Hydroxyapatite-collagen sponge (Group I = 8); Iliac crest bone graft (Group II = 8) | 6, 12 mo | Bone filling percentage (↑, compared with Group I at the 6-mo follow-up) |
| Manimaran [ ], 2014 | None | Mandibular osteoradionecrosis | A case report | Allogeneic dental pulp | Inserted into the defect after surgical curettage | DPSCs + PRP + TCP ( = 1) | None | 2, 6 mo | Bone formation (↑) |
| Manimaran [ ], 2016 | None | Bone defect left by the resection of mandibular ameloblastoma | A case report | Autologous dental pulp | Packed inside the mesh and placed over the mandible after tumor resection | DPSCs + β-TCP + PRF + SVF ( = 1) | None | 1, 10 mo; 1.5 years | Bone regeneration (↑); no recurrence of tumor |
| Brunelli [ ], 2013 | None | Sinus lifting | A case report | Autologous dental pulp | Implanted into sinus cavity | Pulp micrografts + Collagen sponge ( = 1) | None | 4 mo | BMD (↑) |
| Koga [ ], 2022 | None | Erectile dysfunction | Case series | Allogeneic deciduous pulp | Injected into the penis | SHED-CM ( = 38) | None | After every injection | IIEF-5 score (↑) |
| Silva [ ], 2022 | NCT02728115 | Huntington’s disease with preexisting pulmonary nodule | A case report | Allogeneic deciduous pulp | Intravenous administrations | SHED ( = 1) | None | 15, 30 d; 7, 24, 32 mo | Unified Huntington’s disease rating scale (↓); not show long-term tropism or homing for the lung adenocarcinoma |
| Wang [ ], 2010 | None | Plaque psoriasis | A case report | Allogeneic gingival | Bolus injection | GMSCs ( = 1) | None | 3 years | Psoriatic lesions fully cleared; no recurrence |
| Suda [ ], 2022 | NCT04608838; JapicCTI194570 | Acute ischemic stroke | Study protocol | Allogeneic dental pulp | Intravenous administration | DPSCs | Placebo | Per 15 min (1-4 h); per 30 min (4-6 h); 12, 24 h; 2, 3, 8, 31, 91, 181, 366 d | No results |
| Nagpal [ ], 2016 | None | Chronic disability after stroke | Study protocol | Autologous dental pulp | Implanted into peri-infarct region neurosurgical procedure | DPSCs | None | 1, 6, 9, 12 mo | No results |
| Ye [ ], 2020 | ChiCTR2000031319: NCT04336254 | COVID-19 | Study protocol | Allogeneic dental pulp | Intravenous administration | DPSCs | Saline | 2 h ± 30 min; 24 h ± 30 min; 90 d ± 3 d | No results |
BMD: Bone mineral density; CAL: Clinical attachment level; CCT: Controlled clinical trials; COVID-19: Coronavirus disease 2019; DBBM: Deproteinized bovine bone mineral; GR: Gingival recession; G-CSF: Granulocyte colony stimulating factor; HA/TCP: Hydroxyapatite/tricalcium phosphate; IIEF: International index of erectile function; L-PRF: Leukocyte-platelet rich fibrin; MIST: Minimally invasive surgical technique; MRI: Magnetic resonance imaging; PD: Probing depth; PDL: Periodontal ligament; PDLPs: Periodontal ligament progenitor cells; PPD: Periodontal probing depth; PRF: Platelet rich fibrin; PRP: Platelet-rich plasma; PEG-PLGA: Poly (lactide-co glycolide)-polyethylene glycol; RCT: Random clinical trial; rh-BMP: Recombinant human bone morphogenetic protein; SI: Signal intensity; SVF: Stromal vascular fraction: TCP: Tricalcium phosphate; TM: Tooth mobility; VEGF: Vascular endothelial growth factor; SHED-CM: Stem cells from exfoliated deciduous teeth conditioned medium.
Periapical lesions
In a case report and two case series, SCAP/SHED combined with a polyethylene glycol polylactic-polyglycolic acid (PEG-PLGA) scaffold and SHED combined with bioglass were used for the treatment of periapical lesions[ 38 - 40 ] (Table (Table2). 2 ). Periapical tissue healing was found in the follow-up examinations of all three studies. It was reported a positive response in the test of dental pulp activity after SHED transplantation, suggesting the regeneration of pulp or pulp-like tissue, which does not occur in traditional root canal therapy[ 39 , 40 ].
Periodontal intrabony defects
There are two RCTs, a controlled clinical trial (CCT), three case series, and two case reports of DSC-based treatment for periodontal intrabony defects[ 29 , 41 - 46 ] (Table (Table2). 2 ). The RCT of Ferrarotti et al [ 41 ] indicated that pulp micrografts applied with collagen sponges could significantly reduce PD and CAL and promote the regeneration of bone defects when compared with collagen sponges alone. Three case series and a case report using pulp micrografts/DPSCs and collagen sponges also reported similar results of periodontal benefits[ 46 - 49 ]. It was reported a novel approach using periodontal ligament soft tissue, gelatin sponges, and cementum scrapings, which reduced the CAL and PD of periodontitis teeth in their case report[ 45 ].
Although two case series demonstrated the periodontal benefits of PDLPs and PDL-derived cell sheets[ 43 , 44 ], significant differences in periodontal indices (including PD and CAL) were not observed between the test groups and control groups in the other two CCTs that applied PDLSC and PDLSC sheets[ 29 , 42 ]. Several factors might have contributed to the lack of significant differences in the outcomes, such as satisfactory scaffold material properties and small sample sizes. In these four studies, β-TCP, HA/TCP, and deproteinized bovine bone mineral (Bio-oss ® ) were applied as scaffold materials. Although some studies reported abilities to provide support for PDLSCs on osteogenic differentiation of these scaffolds in vitro and in vivo [ 50 - 53 ], only using these scaffolds also achieved great clinical benefits in the treatment of periodontitis[ 54 - 56 ]. The excellent performance of the scaffold may have overshadowed the contribution by PDLSCs. More clinical studies at multiple centers with different amounts and types of DSCs, more follow-up time points, and larger sample sizes are necessary, and the results of such studies would be meaningful.
Bone defects caused by other conditions
In addition to periodontal intrabony defects, DSCs were also used for the treatment of post-extraction sockets, mandibular osteoradionecrosis, bone defects after ameloblastoma resection, and sinus lifting[ 57 - 61 ] (Table (Table2). 2 ). Two split-mouth RCTs reported by Barbier et al [ 57 ] and Cubuk et al [ 62 ] did not find significant differences in BD or interdental septum height between the pulp micrograft + scaffold (collagen matrix/L-PRF) group and the scaffold (collagen matrix/L-PRF) group after implantation into post-extraction sockets. However, in another split-mouth CCT designed for regenerating post-extraction sockets, DPSCs combined with collagen sponges promoted the rate of mineralization, the levels of cortical bone, and the expression of bone morphogenetic protein-2 (BMP-2) and VEGF when compared with collagen sponge treatment alone[ 58 ]. Tanikawa et al [ 63 ] reported a historical control study comparing the effects of SHED, rhBMP, and iliac crest bone grafts in treating cleft lip and palate. The SHED group showed similar satisfactory performance in bone healing compared with iliac crest bone grafts and a higher bone filling percentage compared with the rhBMP group at the 6-mo follow-up[ 63 ].
Two case reports indicated that DPSCs combined with TCP could increase the bone regeneration of bone defects caused by osteoradionecrosis and ameloblastoma[ 59 , 60 ]. A case report by Brunelli et al [ 61 ] demonstrated that pulp micrografts + collagen sponges increased the BD in newly formed bone when applied for sinus lifting.
Other conditions
Koga et al [ 64 ] reported a case series that applied SHED conditioned medium (SHED-CM) to treat erectile dysfunction. In this study, the international index of erectile function (IIEF-5), which is clinically used to screen for erectile function and to assess treatment efficacy, was increased after SHED-CM injection into the corpus cavernosum of erectile dysfunction patients[ 64 ]. A case report indicated that SHED intravenous administrations could decrease the scale of unified Huntington’s disease rating, which is designed to assess clinical performance and capacity in patients with Huntington’s disease[ 65 , 66 ]. Meanwhile, the patient with Huntington’s disease also suffered from preexisting pulmonary nodules, and SHED injection did not result in long-term tropism or homing for the patient’s lung adenocarcinoma[ 65 ]. In a case report by Wang et al [ 30 ], GMSCs were used to treat plaque psoriasis via bolus injection, and they observed fully cleared psoriatic lesions without recurrence.
Three clinical study protocols using DSCs have been published in recent years, including the treatment of acute ischemic stroke, chronic disability after stroke, and COVID-19[ 67 - 69 ].
DSC-BASED CLINICAL TRIALS FROM CLINICAL DATABASES
ClinicalTrials.gov ( https://clinicaltrials.gov/ ) and the International Clinical Trials Registry Platform (ICTRP, https://trialsearch.who.int/ ) were screened for DSC-based clinical trials.
To date, there have been 21 clinical trials registered on ClinicalTrials.gov evaluating the use of DSCs in treating periodontitis (33.3%, 7/21), post-extraction sockets (4.8%, 1/21), edentulous alveolar ridge (4.8%, 1/21), cleft lip and palate (9.5%, 2/21), knee osteoarthritis (4.8%, 1/21), dental pulp necrosis (4.8%, 1/21), liver cirrhosis (4.8%, 1/21), type 1 diabetes (4.8%, 1/21), acute ischemic stroke (4.8%, 1/21), Huntington’s disease (14.3%, 3/21), and COVID-19 (9.5%, 2/21) (Table (Table3). 3 ). In addition to the 6 studies reported in ClinicalTrials.gov, 7 clinical trials were registered on the ICTRP using DSCs in the treatment of periodontitis (57.1%, 4/7), wrinkles (28.6%, 2/7), and hair loss (14.3%, 1/7) (Table (Table4). 4 ). In all, 28 clinical trials were registered on these two platforms.
Dental stem cell-based clinical trials registered at clinicaltrials.gov
| - | NCT04983225 | Recruiting | Periodontitis | Randomized; parallel assignment; double-blind (participant, investigator) | Dental pulp | Injecting into the periodontal defect site | 36 | DPSCs (1 × 10 )/site; DPSCs (5 × 10 )/site; DPSCs (3-4 × 10 )/three or four sites; DPSCs (1 × 10 )/site; DPSCs (2 × 10 )/two sites | Saline solution | 90, 180, 360, 720 d | Phase 1 | |
| - | NCT02523651 | Unknown | Periodontitis | Randomized; parallel assignment; triple-blind (participant, investigator, outcomes Assessor) | Allogeneic dental pulp | Injecting into the periodontal defect site | 40 | DPSCs (1 × 10 ) | Saline solution | 1 year | Phase 1/2 | |
| - | NCT03386877 | Completed | Periodontitis | Randomized; parallel assignment; triple-blind (participant, investigator, outcomes assessor) | Autologous dental pulp | Delivering into intrabony defect minimally invasive surgical technique | 29 | Micrografts of DPSCs + Collagen sponge | Collagen sponge | 6, 12 mo | Not applicable | |
| - | NCT01082822 | Unknown | Periodontitis | Nonrandomized; parallel assignment; open label | Periodontal ligament | Implanted into bone defect sites surgical approach | 80 | PDLSCs sheet fragment + DBBM (Bio-oss); PDLSCs sheet pellets + DBBM (Bio-oss); DBBM (Bio-oss) | Sham comparator | 4, 12, 24 wk; 1 year | Phase 1/2 | |
| - | NCT03638154 | Completed | Periodontitis | Randomized; parallel assignment; double-blind (care provider, outcomes assessor) | Gingival | Implanted into bone defect sites surgical approach | 20 | GFs + GMSCs + β-TCP | β-TCP | 1, 3, 7, 14 d; 6 mo | Not applicable | |
| - | NCT03137979 | Unknown | Periodontitis | Randomized; parallel assignment | Gingival | Implanted into bone defect sites surgical approach | 30 | GMSCs + Collagen scaffolds; collagen scaffolds | Open flap debridement | 1, 3, 6 mo | Phase1/2 | |
| Chen [ ], 2016 | NCT01357785 | Unknown | Periodontitis | Randomized; parallel assignment; open label | Autologous periodontal ligament | 35 | None | 3-12 mo | Phase1 | |||
| Cubuk [ ], 2023 | NCT04641533 | Completed | Post-extraction sockets | Split-mouth; randomized; crossover assignment; double-blind (investigator, outcomes assessor) | Dental pulp | Placing into the extraction socket | 13 | DPSCs + L-PRF | L-PRF | 7 d; 6 mo | Not applicable | |
| - | NCT02731586 | Unknown | Edentulous alveolar ridge | Single group assignment; open label | Allogeneic dental pulp | Introducing dental pulp-derived mesenchymal stem cells during placement of dental implants | 10 | Dental pulp-derived MSCs | None | 3 mo | Early Phase 1 | |
| Tanikawa [ ], 2020; Pinheiro [ ], 2019 | NCT03766217 | Completed | Cleft lip and palate | Randomized; parallel assignment; single-blind (outcomes assessor) | Autologous deciduous pulp | Placed into the alveolar defect surgical approach | 62 | SHED + Hydroxyapatite-collagen sponge | Iliac crest autogenous bone graft | 15 d; 3, 6, 12 mo | Phase3 | |
| Tanikawa [ ], 2020 | NCT01932164 | Completed; Has results | Cleft lip and palate | Single group assignment; open label | Autologous deciduous pulp | Maxillary alveolar graft by tissue engineering | 5 | SHED + Hydroxyapatite-collagen sponge | None | 3, 6 mo | Not applicable | Percentage of bone filling at 6 mo postoperatively: 89.5% |
| - | NCT04130100 | Unknown | Knee osteoarthritis | Randomized; parallel assignment; open label | Dental pulp | Intraarticular injection | 60 | Low dose of DPSCs; high dose of DPSCs | Sodium hyaluronate | 12 mo | Early phase 1 | |
| - | NCT01814436 | Unknown | Dental pulp necrosis | Single group assignment;open label | Autologous deciduous pulp | 80 | Scaffold-free SHED-derived pellet | None | 3-12 mo | Not applicable | ||
| - | NCT03957655 | Unknown | Liver cirrhosis | Randomized; parallel assignment; single-blind (outcomes assessor) | Autologous deciduous pulp | Peripheral vein infusion | 40 | SHED (1 × 10 cells/kg body weight) | Standard medication for viral hepatitis and cirrhosis | 4, 8, 12, 16, 24 wk | Early phase 1 | |
| - | NCT03912480 | Unknown | Type 1 diabetes | Single group assignment; open label | Deciduous pulp | Intravenous drip | 24 | SHED (0.11 IU/kg body weight) + Insulin + oral hypoglycemic drugs | None | 1, 2, 6 wk; 2, 3, 6, 9, 12 mo | Early phase 1 | |
| Suda [ ], 2022 | NCT04608838 | Completed | Acute ischemic stroke | Randomized;Parallel assignment;Quadruple-blind (Participant, Care Provider, Investigator, Outcomes Assessor); | Allogeneic dental pulp | Intravenously infusion | 79 | DPSCs (JTR-161, 1 × 10 cells); DPSCs (JTR-161, 3 × 10 cells) | Placebo | 91, 366 d | Phase 1/2 | |
| - | NCT02728115 | Active, not recruiting | Nonrandomized; parallel assignment; open label | Allogeneic deciduous pulp | Intravenous administration | 6 | SHED (Cellavita HD, 1 × 10 cells); SHED (Cellavita HD, 2 × 10 cells) | None | 1, 4 years | Phase 1 | ||
| - | NCT04219241 | Active, not recruiting | Huntington’s disease | Single group assignment; open label | Allogeneic deciduous pulp | Intravenous administration | 35 | SHED (Cellavita HD, 2 × 10 cells) | None | 1, 2 years | Phase 2/3 | |
| Wenceslau [ ], 2022 | NCT03252535 | Completed | Huntington’s disease | Randomized; parallel assignment; triple-blind (participant, investigator, outcomes assessor) | Allogeneic deciduous pulp | Intravenous administration | 35 | SHED (Cellavita HD, 1 × 10 cells); SHED (Cellavita HD, 2 × 10 cells) | Physiological solution without cells | Monthly for 14 mo | Phase 2 | |
| Ye [ ], 2020 | NCT04336254 | Recruiting | COVID-19 | Randomized; parallel assignment; triple-blind (participant, investigator, outcomes assessor) | Allogeneic dental pulp | Intravenous injection | 20 | DPSCs (3 × 10 cells) | Saline | 28 d | Phase 1/2 | |
| - | NCT04302519 | Unknown | COVID-19 | Single group assignment; open label | Dental pulp | Intravenous injection | 24 | DPSCs (1 × 10 cells/kg body weight) | None | 3, 7, 14, 28, 360 d | Early phase 1 | |
DBBM: Deproteinized bovine bone mineral; GFs: Gingival fibroblast; PRF: Platelet-rich fibrin; TCP: Tricalcium phosphate; DPSCs: Dental pulp stem cells; SHED: Stem cells from exfoliated deciduous teeth.
Dental stem cell-based clinical trials registered on the International Clinical Trials Registry Platform
| - | JPRN-UMIN000042791 | Complete: Follow-up complete | Periodontitis | Randomized; parallel assignment; single-blind (participants) | Deciduous pulp | Gargle | 30 | Mouthwash containing SHED culture supernatant | Mouthwash without SHED culture supernatant | 1 mo | Not applicable | |
| - | ChiCTR2100051466 | Recruiting | Periodontitis | Randomized; parallel assignment; open label | Dental pulp | Bilateral multipoint injection on a single tooth | 96 | DPSCs (1 × 10 cells) for once; DPSCs (1 × 10 cells) for twice | Saline | 90, 180, 360 d | Phage 0 | |
| - | ChiCTR2100049178 | Pending | Periodontitis | Randomized; parallel assignment; double-blind | Dental pulp | Local injection | 36 | DPSCs (1 × 10 cells) for single injection; DPSCs (5 × 10 cells) for single injection; DPSCs (1 × 10 cells) for single injection; DPSCs (1 × 10 cells) for single injection in 2 locations; DPSCs (1 × 10 cells) for single injection in 3-4 locations | None | Phage 1 | ||
| Sánchez [ ], 2020 | ISRCTN13093912 | Completed | Periodontitis | Randomized; parallel assignment; single-blind (patients and examiners) | Dental pulp | Implanted into bone defect sites surgical approach | 20 | DPSCs (1 × 10 cells) + hydroxyapatite-collagen scaffold | Hydroxyapatite-collagen scaffold | 1, 2, 4, 12, 24, 36 wk; 12, 24, 36, 48, 60 mo | Not applicable | |
| - | JPRN-UMIN000045926 | Complete: Follow-up complete | Wrinkles | Randomized; parallel assignment; single-blind (outcomes assessor) | Dental pulp | 12 | All-in-one gel containing immortalized DPSCs-CM solution and various beauty ingredients | No treatment | 4 wk | Not applicable | ||
| - | JPRN-UMIN000043528 | Complete: Follow-up complete | Wrinkles | Randomized; parallel assignment; single-blind (outcomes assessor) | Dental pulp | 12 | All-in-one gel containing immortalized DPSC-CM solution and the latest peptide raw materials | No treatment | 4 wk | Not applicable | ||
| - | JPRN-UMIN000045897 | Complete: Follow-up continuing | Hair loss | Nonrandomized; parallel assignment; open label | Deciduous pulp | Injection | 22 | SHED-CM; after SHED-CM injection, one dose of micrografts (Rigenera) followed by another SHED-CM injection; SHED-CM injection after one dose of micrografts (Rigenera) | None | 6 mo | Not applicable | |
DPSCs: Dental pulp stem cells; SHED-CM: Stem cells from exfoliated deciduous teeth conditioned medium.
Several registered clinical trials applied two stages in one work. The most frequently appearing trial phases were phase 1 (42.9%, 12/28), followed by phase 2 (25%, 7/28), Phase 3 (7.1%, 2/28), and Phase 0 (3.6%, 1/28). There were 10 trials (35.7%) in which the phase design was not applied or not selected. One clinical trial reported the outcomes both on the registry platform and in a published article[ 63 ] ( {"type":"clinical-trial","attrs":{"text":"NCT01932164","term_id":"NCT01932164"}} NCT01932164 ), and the published articles of seven trials stated the registered ID[ 29 , 42 , 62 , 63 , 67 , 69 - 71 ], while other trials did not publish any data.
Consistent with the literature, the proportion of clinical trials using DSCs to treat periodontitis was the highest. Eleven registered clinical trials researched the effect of DSCs on periodontitis (39.3%, 11/28). In these trials, various amounts, types, and injection times of DSCs and different application modes (such as DSCs, micrografts, cell sheet pellets, and cell sheet fragments) were applied. In addition, several scaffolds were used in combination with DSCs, including collagen sponges, deproteinized bovine bone minerals, β-TCP scaffolds, and hydroxyapatite-collagen scaffolds.
SAFETY ISSUES REGARDING DSC-BASED THERAPY
Although encouraging treatment effects on diseases have been achieved, the safety issues of stem cell-based therapy remain controversial, especially in long-term follow-up[ 72 ]. At present, the limitations of stem cell-based therapy are mainly focused on non-directional differentiation, accelerating tumor progression.
In addition, uncontrolled non-directional differentiation may have a great impact on the safety of stem cell transplantation. Breitbach et al [ 73 ] found that the encapsulated structures in the infarcted areas contained calcifications and/or ossifications in myocardial infarction mice after MSC injection. In another study, unselected bone marrow cells injected directly induced significant intramyocardial calcification in acutely infarcted myocardium[ 74 ].
Similar to the regeneration of damaged tissue, tumors exert chemotactic effects on MSCs, affecting their recruitment to tumor sites[ 75 - 77 ]. Current studies have shown that MSCs have bidirectional, anti-cancer and pro-cancer, regulatory effects, which raises safety concerns for clinical application. On the one hand, MSCs are the major component of the tumor microenvironment and can be reprogrammed to the pro-tumorigenic phenotype by the tumor[ 78 ]. MSCs have been revealed to participate in the initiation, development, progression, and metastasis of multiple cancers[ 79 ]. The pro-cancer effect of stem cells may be achieved by secreting molecules that affect the phenotype of tumor cells, promoting tumor angiogenesis, cancer-associated fibroblast differentiation, cell-to-cell contact, or cell engulfment[ 76 ]. In recent studies, DPSCs and their conditioned medium were reported to promote the proliferation and carcinogenic properties of prostate cancer, oral cancer, breast cancer, and melanoma cells in vitro [ 80 - 82 ].
On the other hand, there is also evidence that MSCs can inhibit the growth of a variety of tumors, including breast cancer, Kaposi’s sarcoma, hepatoma, glioma, and melanoma[ 76 , 83 - 85 ]. DPSCs and their conditioned medium also showed a suppressive effect on the development and migration of colorectal cancer cells through mitogen-activated protein kinase pathways[ 86 ]. In fact, there are few reports of primary pulp malignancies[ 87 ]. In a genome-wide RNA-seq study, phosphatase and tensin homolog (PTEN) expression in DPSCs was higher than that in BMSCs[ 88 ]. PTEN, a phosphatase, can metabolize phosphatidylinositol 3,4,5-triphosphate and directly oppose the activation of the oncogenic PI3K/AKT/mTOR signaling network[ 89 ]. At present, the regulatory effects of stem cells on cancer are still controversial, and the difference in results may be related to cell lines, cell doses, animal models, cancer types, treatment duration time, and other factors.
In conclusion, no adverse events were reported in the published clinical articles or clinical trials using DSCs, which suggested the safety of DSC-based therapy. However, based on current concerns about the safety of stem cell therapy, more in vivo studies on the safety of DSC-based therapies are of great significance.
CURRENT LIMITATIONS AND PERSPECTIVES
Harvesting dscs from inflamed tissue.
Most studies applied stem cells extracted from healthy dental tissue for treatment, but additional surgery (such as third molar extraction) might increase patient suffering. Harvesting stem cells from inflamed dental tissue could be an alternative method, although stem cell abilities might be affected[ 36 , 90 , 91 ].
Several studies have researched the different biological properties of DPSCs derived from normal and inflamed pulps (iDPSCs), and the results are still in dispute[ 92 - 98 ]. In some studies, DPSCs showed better self-renewal ability[ 92 , 93 ] and multidirectional differentiation capacities than iDPSCs[ 92 ], while in other studies, no significant difference was observed[ 94 , 95 , 98 ]. A study by Nie et al [ 97 ] indicated that DPSCs showed higher colony-forming, proliferative, and osteo/dentinogenesis abilities, while iDPSCs demonstrated enhanced chondrogenesis, neurogenesis, angiogenesis, and adipogenesis capacities. Park et al [ 96 ] reported that iDPSCs appear to have higher osteogenic differentiation potential and lower neurogenic differentiation potential than DPSCs.
Differences in inflammation levels may explain the discrepancy in the biological properties of DPSCs and iDPSCs in various studies. Intense and rapid inflammatory stimulation irreversibly initiates pulp necrosis, while low insult levels of inflammation are able to cause reversible pulpitis and promote dentine regeneration[ 99 ]. DPSCs are a suitable source of stem cells for pulp nerve regeneration because of their neuronal differentiation potential. It was reported that acute inflammation with a high level of proinflammatory cytokines could reduce neural precursor cell (NPC) survival and inhibit the neuronal differentiation of NPCs, while chronic inflammation expressed a potentially neuroprotective phenotype and supported neuronal differentiation[ 100 ]. Meanwhile, age, sex, tooth position, and sample size are also confounding factors affecting the function of DPSCs, which should be considered in subsequent studies and clinical practice.
DSC-CM and DSC-EVs
The culture medium collected from cells in culture is known as CM. CM is applied as an alternative therapy for tissue regeneration, which is a less ethical issue because it uses cells indirectly. Koga et al [ 64 ] applied SHED-CM in the treatment of erectile dysfunction, which is the only record of its clinical use to the best of our knowledge.
DSC-CM contains a variety of cytokines associated with vascular and nerve tissue regeneration, such as VEGF, BDNF, β-NGF, GDNF and neurotrophin-3 (NT-3)[ 101 , 102 ]. To date, DSC-CM has been reported to have the potential to promote bone regeneration[ 103 ], periodontal regeneration[ 104 ], angiogenesis[ 105 ], pulp regeneration[ 106 ], and nerve protection/regeneration[ 105 , 107 - 109 ] with great possibilities for clinical application.
In addition, DSC-CM showed satisfactory anti-inflammatory and immunoregulatory effects. Several in vivo studies based on various animal models reported that intravenous injection or intranasal administration of SHED-CM improved liver fibrosis[ 110 ], acute liver failure[ 111 ], acute lung injury[ 112 ], Alzheimer’s disease, temporomandibular joint osteoarthritis[ 113 ], Sjögren’s syndrome[ 114 ], and rheumatoid arthritis[ 115 ] by exerting anti-inflammatory effects. Meanwhile, studies have also reported the effect of SHED-CM on promoting Treg cell differentiation[ 114 ] and M2-like macrophage induction[ 111 , 112 ], as well as inhibiting Th17 cell differentiation[ 114 ] and inflammatory macrophage activation[ 116 ].
In addition to DSC-CM, DSC-EVs harvested from cell-culture medium have also been deeply studied in recent years. Multiple studies have indicated the promotion effect of DSC-EVs on jawbone and calvarial bone regeneration[ 117 , 118 ], angiogenesis and cutaneous wound healing in vivo [ 119 , 120 ]. Li et al [ 121 ] also reported that DSC-EVs could alleviate cerebral ischemia-reperfusion by suppressing the inflammatory response, which is related to the inhibition of the HMGB1/TLR4/MyD88/NF-κB pathway.
The poor survival rate of implanted DSCs and host immunogenic reactions are the main drawbacks of applying DSCs directly. In some comparative studies, stem cell-derived CM showed similar and even better treatment effects on acute lung injury, Parkinsonism, and type 1 diabetes than the direct use of stem cells[ 112 , 122 , 123 ]. DSC-CM and its components (such as EVs) provide several key advantages over cell-based applications, including avoiding the risk of host immunogenic reactions, cost-effectiveness, long-term storage capacity, and simpler evaluation of safety and efficacy[ 104 , 124 ]. Accumulating evidence indicates the great potential of DSC-CM/DSC-EV-based treatment in clinical applications.
Expanding-free strategy
Despite encouraging results of differentiation and tissue regeneration, DSCs still require rigorous cell-expanding procedures to obtain a sufficient number of cells for treatment, which is costly with great technique sensitivity, often taking tens of days. The ex vivo expansion of stem cells often reduces their self-renewal and proliferation abilities[ 125 ]. Direct mechanical digestion or tissue transplantation are promising solutions to these limitations.
In recent years, using mechanical disaggregation of dental tissues instead of cell-expending procedures was successful for harvesting autologous pulp micrografts rich in progenitor cells[ 41 , 126 ]. In 2016, Monti et al [ 126 ] indicated that DSCs harvested by mechanical digestion (Rigenera ® system, HBW, Turin, Italy) were fully comparable to stem cells obtained after enzymatic digestion. In this study, mechanical digestion-obtained DPSCs showed osteogenic, adipogenic, and chondrogenic differentiation abilities in vitro and were able to increase the regeneration of post-extraction sockets in vivo when applied with the collagen sponge[ 126 ].
Pulp micrografts harvested by mechanical digestion were also applied in the treatment of sinus lifting, post-extraction sockets, and periodontal intrabony defects[ 46 , 47 , 49 , 57 , 61 , 62 ]. One clinical trial using pulp micrografts was also designed for periodontitis management ( {"type":"clinical-trial","attrs":{"text":"NCT03386877","term_id":"NCT03386877"}} NCT03386877 ), but the outcome was not reported. Different systems of mechanical disaggregation were applied in these studies, including BD Medimachine (BD Biosciences San Jose, CA, United States)[ 62 ], the Rigenera ® system (HBW, Turin, Italy)[ 46 , 57 , 61 ], and the Medimachine System (Consul TS, Orbassano, Italy)[ 47 , 49 ]. In brief, dental pulp is first collected from extracted teeth and then sent to the mechanical disaggregation system to obtain pulp micrografts. After filtration or without filtration, pulp micrografts are combined with the scaffold for transplantation.
In addition, Vandana et al [ 125 ] described a novel approach using stem cell assistance in the periodontal regeneration technique (SAI-PRT), which contained periodontal ligament soft tissue gelatin sponge scaffolds and cementum scrapings. In their research, SAI-PRT successfully bypassed in vitro culture and expanded PDLSCs, resulting in satisfactory defect filling of periodontal intrabony defects[ 125 ].
Embryonic stem cells, PSCs, and DSCs
Embryonic stem cells (ESCs) are pluripotent cells of great significance to developmental biology. They give rise to all types of germ layer cells in the embryo. The self-renewal ability and plasticity of ESCs make it possible to generate unlimited numbers of different types of cells in vitro [ 127 ]. Similar to embryonic cells, PSCs derived from different somatic cells also have the ability to immortalize and differentiate into the three germ layers[ 128 ]. The properties of these two cell types make them promising sources for stem cell-based therapy for various diseases and injuries. However, due to the limitations of ESCs and PSCs, adult stem cells (such as DSCs) still possess high application value.
First, ethical issues regarding the use of ESCs make their clinical application challenging[ 128 ]. Second, the preparation of autologous PSCs takes a long time (more than 3 mo) and has high medical cost, and the immune rejection issue of allotransplantation should be considered[ 129 ]. In addition, teratomas are germ cell tumors containing cells of two or three germ lines that always occur via uncontrollable stem cell proliferation and differentiation[ 130 , 131 ]. In experimental studies, stem cell transplants (especially ESC and PSC transplants) have been found to increase the risk of teratomas, raising safety concerns[ 131 - 133 ]. Previously, viral vector integration and contamination of animal-derived components also posed obstacles to the use of PSCs, but these problems have been addressed by innovative techniques, such as integration-free methods and xeno-free culture[ 134 - 136 ].
DSCs did not show unlimited proliferation potential and demonstrated poorer differentiation ability than PSCs and ESCs[ 137 ]. However, the advantages of DSCs over ESCs and PSCs, such as fewer ethical issues and lower teratoma risk[ 87 , 88 , 138 ], lower cost and shorter preparation period, harvesting from medical waste, and implementing therapeutic effects without gene editing, grant them greater potential for clinical applications in the future.
Many clinical articles and clinical trials of autologous and allogeneic DSCs have aimed to evaluate their therapeutic effects on various diseases, such as pulpitis, periapical lesions, periodontitis, cleft lip and palate and Huntington’s disease. In most studies, satisfactory clinical treatment results were obtained, while clinical benefits of using DSCs were not found in some research. Although safety risks exist for stem cell-based therapies, safety issues have not been reported in the clinical applications of DSCs. In the future, in addition to continuing to study the efficacy and safety of DSC-based treatment, harvesting DSCs from inflammatory tissues, expanding-free strategies, and applying DSC-CM or DSC-EVs should be studied, as they have strong research value and application potential. Taken together, DSC-based therapy is a promising tool for the treatment of various diseases and can be further promoted.
ACKNOWLEDGEMENTS
We thank our friend Han-Yi Dong for designing and drawing Figure Figure1 1 .
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: December 5, 2022
First decision: January 11, 2023
Article in press: March 8, 2023
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Collart-Dutilleul PY, France; Ventura C, Italy S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
Contributor Information
Wen-Peng Song, Department of Stomatology, Beijing Tiantan Hospital, Capital Medical University, Beijing 100070, China.
Lu-Yuan Jin, Department of General Dentistry and Integrated Emergency Dental Care, Beijing Stomatological Hospital, Capital Medical University, Beijing 100050, China.
Meng-Di Zhu, Department of General Dentistry and Integrated Emergency Dental Care, Beijing Stomatological Hospital, Capital Medical University, Beijing 100050, China.
Hao Wang, Department of Stomatology, Beijing Tiantan Hospital, Capital Medical University, Beijing 100070, China.
Deng-Sheng Xia, Department of General Dentistry and Integrated Emergency Dental Care, Beijing Stomatological Hospital, Capital Medical University, Beijing 100050, China. nc.ude.umcc.liam@aixsd .
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu
- Subscribe SciFeed
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Digitalization, technologies, new approaches, and telemedicine in dentistry and craniofacial/temporomandibular disorders.

Conflicts of Interest
- Alqahtani, J.; Alhemaid, G.; Alqahtani, H.; Abughandar, A.; AlSaadi, R.; Algarni, I.; AlSharif, W.; Al-Harbi, S.; Burwaih, R.; Hasan, A.; et al. Digital Diagnostics and Orthodontic Practice. J. Healthc. Sci. 2022 , 2 , 112–117. [ Google Scholar ] [ CrossRef ]
- Joda, T.; Ferrari, M.; Gallucci, G.O.; Wittneben, J.; Brägger, U. Digital Technology in Fixed Implant Prosthodontics. Periodontology 2000 2017 , 73 , 178–192. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Khurshid, Z. Digital Dentistry: Transformation of Oral Health and Dental Education with Technology. Eur. J. Dent. 2023 , 17 , 943–944. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Çin, V.; İzgi, A.D.; Kale, E.; Yilmaz, B. Marginal and Internal Fit of Monolithic Zirconia Crowns Fabricated by Using Two Different CAD-CAM Workflows: An In Vitro Study. Prosthesis 2023 , 5 , 35–47. [ Google Scholar ] [ CrossRef ]
- Tallarico, M.; Cuccu, M.; Meloni, S.M.; Lumbau, A.I.; Baldoni, E.; Pisano, M.; Fiorillo, L.; Cervino, G. Digital Analysis of a Novel Impression Method Named the Biological-Oriented Digital Impression Technique: A Clinical Audit. Prosthesis 2023 , 5 , 992–1001. [ Google Scholar ] [ CrossRef ]
- D’Ambrosio, F.; Giordano, F.; Sangiovanni, G.; Di Palo, M.P.; Amato, M. Conventional versus Digital Dental Impression Techniques: What Is the Future? An Umbrella Review. Prosthesis 2023 , 5 , 851–875. [ Google Scholar ] [ CrossRef ]
- Yuzbasioglu, E.; Kurt, H.; Turunc, R.; Bilir, H. Comparison of Digital and Conventional Impression Techniques: Evaluation of Patients’ Perception, Treatment Comfort, Effectiveness and Clinical Outcomes. BMC Oral Health 2014 , 14 , 10. [ Google Scholar ] [ CrossRef ]
- Subramanian, A.K.; Chen, Y.; Almalki, A.; Sivamurthy, G.; Kafle, D. Cephalometric Analysis in Orthodontics Using Artificial Intelligence℄A Comprehensive Review. Biomed. Res. Int. 2022 , 2022 , 1880113. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Silva, T.P.; Hughes, M.M.; Menezes, L.D.S.; de Melo MD, F.B.; Freitas, P.H.L.D.; Takeshita, W.M. Artificial Intelligence-Based Cephalometric Landmark Annotation and Measurements According to Arnett’s Analysis: Can We Trust a Bot to Do That? Dentomaxillofac. Radiol. 2022 , 51 , 20200548. [ Google Scholar ] [ CrossRef ]
- Gokdeniz, S.T.; Kamburoğlu, K. Artificial Intelligence in Dentomaxillofacial Radiology. World J. Radiol. 2022 , 14 , 55–59. [ Google Scholar ] [ CrossRef ]
- Duran, G.S.; Gökmen, Ş.; Topsakal, K.G.; Görgülü, S. Evaluation of the Accuracy of Fully Automatic Cephalometric Analysis Software with Artificial Intelligence Algorithm. Orthod. Craniofacial Res. 2023 , 26 , 481–490. [ Google Scholar ] [ CrossRef ]
- Kılınç, D.D.; Kırcelli, B.H.; Sadry, S.; Karaman, A. Evaluation and Comparison of Smartphone Application Tracing, Web Based Artificial Intelligence Tracing and Conventional Hand Tracing Methods. J. Stomatol. Oral Maxillofac. Surg. 2022 , 123 , e906–e915. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Görürgöz, C.; İçen, M.; Kurt, M.; Aksoy, S.; Bakırarar, B.; Rozylo-Kalinowska, I.; Orhan, K. Degenerative Changes of the Mandibular Condyle in Relation to the Temporomandibular Joint Space, Gender and Age: A Multicenter CBCT Study. Dent. Med. Probl. 2023 , 60 , 127–135. [ Google Scholar ] [ CrossRef ]
- Lombardo, G.; Signoriello, A.; Marincola, M.; Bonfante, E.A.; Díaz-Caballero, A.; Tomizioli, N.; Pardo, A.; Zangani, A. Five-Year Follow-Up of 8 and 6 mm Locking-Taper Implants Treated with a Reconstructive Surgical Protocol for Peri-Implantitis: A Retrospective Evaluation. Prosthesis 2023 , 5 , 1322–1342. [ Google Scholar ] [ CrossRef ]
- Ortu, E.; Di Nicolantonio, S.; Mummolo, A.; Cattaneo, R.; Pietropaoli, D.; Monaco, A. Use of Tens in the Diagnosis of Functional Mandibular Lateral Deviation. Appl. Sci. 2023 , 13 , 13258. [ Google Scholar ] [ CrossRef ]
- Barayan, M.A.; Qawas, A.A.; Alghamdi, A.S.; Alkhallagi, T.S.; Al-Dabbagh, R.A.; Aldabbagh, G.A.; Linjawi, A.I. Effectiveness of Machine Learning in Assessing the Diagnostic Quality of Bitewing Radiographs. Appl. Sci. 2022 , 12 , 9588. [ Google Scholar ] [ CrossRef ]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Di Blasio, M.; Isola, G.; Cicciù, M. Conservative Treatment of Temporomandibular Joint Condylar Fractures: A Systematic Review Conducted According to PRISMA Guidelines and the Cochrane Handbook for Systematic Reviews of Interventions. J. Oral Rehabil. 2023 , 50 , 886–893. [ Google Scholar ] [ CrossRef ]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Almeida, L.E.; Ronsivalle, V.; Cicciù, M. Prevalence of Temporomandibular Disorders (TMD) in Obesity Patients: A Systematic Review and Meta-analysis. J Oral Rehabil 2023 , 50 , 1544–1553. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Inchingolo, A.M.; Inchingolo, A.D.; Settanni, V.; De Leonardis, N.; Campanelli, M.; Garofoli, G.; Benagiano, S.; Malcangi, G.; Minetti, E.; Palermo, A.; et al. Correlation between Temporomandibular Disorders and Tinnitus and Possible Treatment Strategies: Comprehensive Review. Appl. Sci. 2023 , 13 , 8997. [ Google Scholar ] [ CrossRef ]
- Minervini, G.; Franco, R.; Marrapodi, M.M.; Di Blasio, M.; Ronsivalle, V.; Cicciù, M. Children Oral Health and Parents Education Status: A Cross Sectional Study. BMC Oral Health 2023 , 23 , 787. [ Google Scholar ] [ CrossRef ]
- Ceylan, G.; Eken, M.O.; Yuruk, S.; Emir, F. Examining the Influence of Self-Esteem and Digital Literacy on Professional Competence Factors in Dental Education: A Cross-Sectional Study. Appl. Sci. 2023 , 13 , 9411. [ Google Scholar ] [ CrossRef ]
- Ortu, E.; Di Nicolantonio, S.; Cova, S.; Pietropaoli, D.; De Simone, L.; Monaco, A. Efficacy of Elastodontic Devices in Temporomandibular Disorder Reduction Assessed by Computer Aid Evaluation. Appl. Sci. 2024 , 14 , 1651. [ Google Scholar ] [ CrossRef ]
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Franco, R.; Minervini, G. Digitalization, Technologies, New Approaches, and Telemedicine in Dentistry and Craniofacial/Temporomandibular Disorders. Appl. Sci. 2024 , 14 , 5871. https://doi.org/10.3390/app14135871
Franco R, Minervini G. Digitalization, Technologies, New Approaches, and Telemedicine in Dentistry and Craniofacial/Temporomandibular Disorders. Applied Sciences . 2024; 14(13):5871. https://doi.org/10.3390/app14135871
Franco, Rocco, and Giuseppe Minervini. 2024. "Digitalization, Technologies, New Approaches, and Telemedicine in Dentistry and Craniofacial/Temporomandibular Disorders" Applied Sciences 14, no. 13: 5871. https://doi.org/10.3390/app14135871
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

Current Research in Dentistry
Aims and scope.
Current Research in Dentistry cover articles on evaluation, diagnosis, prevention, and treatment of diseases, disorders and conditions of the soft and hard tissues of the jaw, the oral cavity, maxillofacial area and the adjacent and associated structures and their impact on the human body. Current Research in Dentistry is an international, peer reviewed journal publish two times a year.
It is with great pleasure that we announce the SGAMR Annual Awards 2020. This award is given annually to Researchers and Reviewers of International Journal of Structural Glass and Advanced Materials Research (SGAMR) who have shown innovative contributions and promising research as well as others who have excelled in their Editorial duties.
This special issue "Neuroinflammation and COVID-19" aims to provide a space for debate in the face of the growing evidence on the affectation of the nervous system by COVID-19, supported by original studies and case series.
The SGAMR Editorial Board is pleased to announce the inauguration of the yearly “SGAMR Young Researcher Award” (SGAMR-YRA). The best paper published by a young researcher will be selected by a journal committee, from the Editorial Board.
- Recently Published
- Most Viewed
- Most Downloaded
The next revolution in dental care is about to begin
From fluoride toothpaste to dental sealants, science has brought all sorts of tools for fighting tooth decay — and yet 91% of Americans between 20 and 64 years of age are affected by dental caries.
But provocative new research suggests that cell-stimulating medications can “trick” teeth into repairing themselves. If these “small molecule” drugs work as well as scientists think they will, we may be on the cusp of a new era in which dental tissue and even entire teeth can be regrown .
And this is only one of several new approaches that hold promise for tooth regeneration.
Stem cells to the rescue
Right now, when dentists spot caries, they drill out the decayed material and fill the hole with a cement-like substance called amalgam. But amalgam can fail or even fall out. That can bring more discomfort and a trip back to the dentist.
This could all change. The research shows the drugs can coax stem cells within the dental pulp — the soft material deep within teeth that’s filled with nerves and blood vessels — into regrowing enough bony tissue (dentin) to fill the cavity.
Researchers are especially excited about Tideglusib , a low-cost experimental drug with an established safety record. They think it could be fast-tracked through clinical trials for use to stop tooth decay (Tideglusib is currently being tested for use against Alzheimer’s disease).
“The dentin produced by stimulating stem cells with Tideglusib integrates itself completely within the tooth so there’s no risk of the filling coming out, which is a big problem with the current methods, which haven’t changed much in the past 100 years,” says Dr. Paul Sharpe, professor of stem biology at Kings College London and leader of the research. “There’s a big need for biology to impact upon dentistry and drag it out of the 19th century.”
So far Tideglusib has been studied only in rats, but Sharpe expects to start human trials within the next year. He hopes that it can eventually replace amalgam, which contains mercury. “Mercury works and it lasts for a long time, but having that in your mouth is a concern,” Sharpe says.
Maybe lasers
Meanwhile, scientists at the University at Buffalo in New York are exploring an even more radical way to regrow teeth. A team led by Dr. Praveen Arany, assistant professor of oral biology at the university, is testing the use of low-power laser light to stimulate tooth regeneration .

mach Dogs can't speak human. Here's the tech that could change that.
When decay reaches the pulp, dentists perform a root canal. This involves removing the bulk of the tooth and then filling what’s left with amalgam. The tooth is then sealed with an artificial cap, but this can fail over time as a result of the stresses of chewing.
Arany has found that shining laser light directly on the remaining pulp can stimulate stem cells in the pulp to produce new dentin. This would still need to be capped, but is likely to be far more resilient.
“By regenerating the tooth so the pulp is coated in natural dentin again, it doesn’t have the same risk of material failure,” Arany says. “Our bodies have the ability to heal our tissues through their own stem cells, so figuring out how to kick-start this process is a dramatically different and more effective way of doing dentistry.”
Growing back entire teeth
The holy grail for dental researchers is the ability to regrow an entire missing tooth. Sharpe has done this in mice, but doing the same in humans raises ethical and legal concerns. It would involve the creation of a so-called tooth primordium (a tooth in its earliest stage of development) and implanting it in the jaw where the missing tooth had been. To create a tooth primordium, it’s necessary to harvest stem cells from human embryos — which bumps up against U.S. law .
“Embryos have the only cells we know of that can make a tooth,” Sharpe says. “Our adult mouths don’t make teeth. These cells are no longer present.”
But if regrowing entire teeth is impractical now, scientists believe they will make it happen one day. “We need to find another way which doesn’t involve cells from embryos,” Sharpe says. “That’s going to take a lot of research and more time. I believe it can happen, but it’s not going to be in the next few years.”
FOLLOW NBC NEWS MACH ON TWITTER , FACEBOOK , AND INSTAGRAM .
A dental crown, also sometimes referred to as a “cap,” is a type of dental restoration that fits over the remains of a tooth to restore the appearance of the natural tooth or to protect it from further damage.
Radicular Cysts
Tartar causes, importance of pharmacology in dentistry, feature articles, hard tissue lasers in dentistry, what is nanodentistry, wisdom teeth removal, (how to) make your own toothpaste, are genes involved in tooth decay and gum disease, what is dental informatics, what is dental public health, what is pediatric dentistry, what is dentin / dentine, what is dentin hypersensitivity, what is tooth enamel, what is dental pulp, dental implant risks, dental implant techniques, medical uses of dental implants, history of dental implants, dental abscess causes and prevention, what is a dental abscess, dental abscess symptoms, what are dental braces, procedure for dental braces, risks of dental braces, types of dental braces, history of dental braces, taking care of your teeth with braces, what is a dental bridge, types of dental bridges, dental bridge procedure, dental bridges - advantages and disadvantages, uses for a dental bridge, dental crown complications, dental crown uses, procedure for dental crowns, advantages and disadvantages of dental crowns, recovery after a dental crown procedure, patient care for dental crowns, tooth erosion causes, reasons for a dental extraction, procedure for dental extraction, types of dental extraction, dental filling procedure, what are dental fillings, flossgate & the importance of preventative oral hygiene, what are dentures, latest dentistry news and research.
Gene mutation explains heart defects in children
A new groundbreaking study sheds light on a medical question scientists have long wondered: why do 40 per cent of children with the rare neurodevelopmental disorder KBG syndrome have heart defects? The research now points to a critical link between the heart and the brain.

Understanding the role of vaccination in mitigating long COVID brain fog
Since the outset of the COVID-19 pandemic, 10 to 30 per cent of the general population has experienced some form of virus-induced cognitive impairment, including trouble concentrating, brain fog or memory loss.

UT Health San Antonio researcher wins NIH grant to investigate alcohol-associated liver disease
Liver transplants associated with alcohol-related disease are growing at a rapid pace, shifting research to address pathologies behind the ailments in light of a limited supply of organ donors.

Research finds causal evidence tying cerebral small-vessel disease to Alzheimer’s, dementia
Research led by in part by The University of Texas Health Science Center at San Antonio (UT Health San Antonio) finds that the most common cerebral small-vessel disease feature seen in brain magnetic resonance imaging is a primary vascular factor associated with dementia risk.

Evaluation of serum tumor markers as adjuncts in NSCLC management
A new research paper was published in Oncotarget's Volume 15 on June 13, 2024, entitled, "Assessment of serum tumor markers CEA, CA-125, and CA19-9 as adjuncts in non-small cell lung cancer management."


Is coffee good or bad? Genetic study investigates health correlations
Coffee drinking is a heritable habit, and one that carries a certain amount of genetic baggage.

Study reveals anesthetic injections as biggest stress factor in teen dental patients
Children are very stressed by anesthetics injected into the mouth before tooth extraction, in connection with orthodontic treatment.

Low-sodium alternatives could have a positive impact on the Indonesian health
Excess sodium intake and a lack of potassium are major contributing factors towards high blood pressure in Indonesia, prompting calls for low-sodium potassium-rich salt substitutes (LSSS) to be readily available to improve health and curb health costs.

Patient perspectives highlight urgent need for research on smell and taste disorders
Researchers and patient advocates from the Monell Chemical Senses Center, Smell and Taste Association of North America (STANA), and Thomas Jefferson University came together during the COVID-19 pandemic to incorporate patient voices in efforts to prioritize research areas focused on improving care for people with smell and taste disorders.

New research reveals hidden challenges faced by people with tooth loss and dentures
The hidden challenges faced by people with tooth loss and dentures has been identified by new research from the University of Sheffield.

New method provides a more accurate way to predict dementia up to nine years before diagnosis
Researchers at Queen Mary University of London have developed a new method for predicting dementia with over 80% accuracy and up to nine years before a diagnosis.

Goethe University Frankfurt's Student Polyclinic marks its tenth anniversary
On June 3, Goethe University Frankfurt's Student Polyclinic, part of the Frankfurt Health Department, marked its tenth anniversary.

Older individuals with multimorbidity at increased risk of hospitalization during hot weather
Australians are no strangers to long, hot summers, but new Griffith University research has looked at the impact of hot weather on patients with pre-existing chronic diseases and how it increases their risk of being hospitalized.
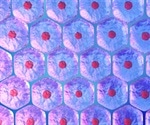
From ancient remedies to modern medicine: Inorganic materials offer new hope for tissue regeneration
For centuries, civilizations have used naturally occurring, inorganic materials for their perceived healing properties.

Understanding the long-term effects and safety of testosterone therapy in transgender men
Transgender individuals often face unique challenges in aligning their physical bodies with their true gender identity.

New dentists may face NHS service requirement under new government plans
Newly-qualified dentists could be required to deliver NHS care for several years after they graduate under a government consultation being launched today.

Improved animal model captures full picture of periodontal disease progression
Periodontal disease, represented by periodontitis, is the leading cause of tooth loss and affects close to one in five adults worldwide.

Matcha green tea powder may help keep gum disease bacteria at bay
Periodontitis is an inflammatory gum disease driven by bacterial infection and left untreated it can lead to complications including tooth loss.

Continuous long-term ketogenic diet may induce cellular senescence in multiple organs
A strict "keto-friendly" diet popular for weight loss and diabetes, depending on both the diet and individual, might not be all that friendly.

Study reveals association between ribosomal DNA copy number and disease risk
Ribosomal DNA (rDNA) is present in hundreds of copies in the genome, but has not previously been part of genetic analyses.
- Trending Stories
- Latest Interviews
- Top Health Articles

Pioneering Live Cell Imaging - Yokogawa's Impact and Innovations
In this interview, NewsMedical speaks with Kevin Jan from Yokogawa about the future of live cell imaging technologies.

Revolutionizing Life Science: An Interview with SCIEX on ASMS, the SCIEX 7500+ System, and AI-Driven Quantitation
Jose Castro-Perez and Chris Lock, SCIEX
In our latest interview, News Medical speaks with SCIEX, a global leader in life science analytical technologies, about their exciting announcements at ASMS, the SCIEX 7500+ System, and how they utilize AI quantitation software to streamline solutions.

From Discovery Biology to ELRIG Chair
Melanie Leveridge
In this interview, we speak with Melanie Leveridge, Vice President of Discovery Biology at AstraZeneca and Chair of the Board for ELRIG UK, to discuss her extensive career in the pharmaceutical industry, her role in fostering scientific innovation, and her vision for ELRIG's future.

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback
- Member Login
Groundbreaking dental research

The ADA Science & Research Institute, LLC (ADASRI) conducts cutting-edge studies that advance dental technology and care.
The ADA Health Policy Institute (HPI) is a thought leader for critical policy knowledge about the U.S. dental care system.

The Dental Quality Alliance (DQA) develops performance measures to improve oral health care and patient safety.
The ADA Dental Experience and Research Exchange™ (DERE) is the first data registry open to all practices.
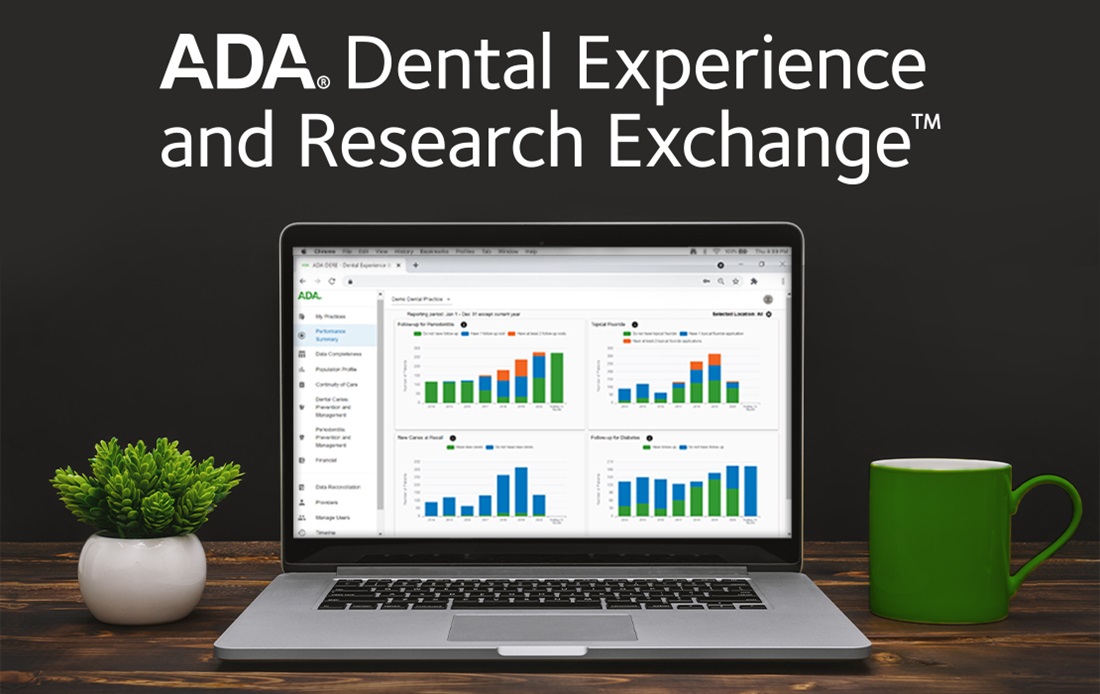
- New Dentist News
- Member Login
by Mary Beth Versaci
June 12, 2022
Original Article
Pathways to dentistry: Researchers move dental profession forward
Contributions have lasting impact on oral health care.
Editor's note: This is the third article in a series that celebrates the diversity of career paths in dentistry and the Association's efforts in supporting dentists' career choices in the profession.
From examining the connections between oral and overall health to evaluating the behavior of materials used in dentistry, researchers ask the questions and do the work to inform how dentists care for their patients every day.
"Dentistry is an amazing profession that has offered so many of us the opportunity to improve patients' lives. It is critical that we continue to evolve and expand our understanding of the diseases and conditions that affect our patients and continue to work to optimize the treatments that they receive," said Mia Geisinger, D.D.S., professor and director of the Advanced Education Program in Periodontology at the University of Alabama at Birmingham School of Dentistry. "My goal in research is always to change the way that we treat patients for the better, and while the pace of scientific discovery may be incremental, we continually strive to improve oral and overall health for all."
The American Dental Association recognizes the importance of research — like Dr. Geisinger's on the impact of periodontal disease and treatment on overall health — to the practice of dentistry. One of its core values is to be a science- and evidence-based organization, a goal that is supported by the ADA Science & Research Institute, which conducts research and produces evidence-based resources for dentists.
"Scientific research is so important to the health and advancement of the dental profession. That's why I'm really proud of the work ADASRI does," said Marcelo Araujo, D.D.S., Ph.D., chief science officer of the ADA and CEO of ADASRI. "At ADASRI, our work runs the gamut of scientific research — everything from basic science, like the creation of novel dental materials, to applied science that tests and refines dental materials, to clinical and translational research that communicates that basic and applied science in a way that is easy to implement chairside. As a whole, the work of ADASRI’s researchers, and really the work of all dental researchers, has a profound impact on improving dentistry."
The ADA also has two scientific journals: The Journal of the American Dental Association and JADA Foundational Science.
"The ADA continues to demonstrate its strong commitment to the health sciences through many avenues, including the dissemination of basic, translational and clinical research through its journals and other media offerings," said Jack L. Ferracane, Ph.D., editor-in-chief of JADA Foundational Science. "It all boils down to creating new and better pathways to oral health, and we all find it exciting and gratifying to play our different roles in the process that links discovery to successful clinical care."
A New Day for Dentistry, a campaign launched by ADA President Cesar R. Sabates, D.D.S., celebrates the ADA’s diverse community of dentists by recognizing their personal differences and the varied career paths they have chosen within the profession.
"Researchers are essential members of the dental workforce," Dr. Sabates said. "Clinicians strive to provide the best care they can to their patients, and researchers provide the evidence they need to make informed decisions. Their work also helps to expand dentistry’s knowledge base, driving innovation and advancement in our profession. The contributions of researchers have a lasting impact on all facets of oral health care."

For dentists who choose to pursue research as part of their career, a natural curiosity is key.
"I was exposed to research and science when I was in high school, and ever since, I was always interested in learning the underlying mechanisms of diseases," said Hatice Hasturk, D.D.S., Ph.D., director of the Center for Clinical and Translational Research and senior member of the staff at the Forsyth Institute. "I believe that without knowing what is really involved in tissues or structures we are working with, we cannot provide an effective and long-lasting solution."
Dr. Hasturk, who won the ADA’s 2020-21 Norton M. Ross Award for Excellence in Clinical Research and serves on the ADA Council on Scientific Affairs, teaches at the Boston University Henry M. Goldman School of Dental Medicine and Harvard School of Dental Medicine and practices once a week as a staff dentist/periodontist at the Forsyth Faculty Associates Clinic. Her research focuses on periodontology and immunology.
Dr. Hasturk's studies have shown that changing the body's response to infections and diseases can reduce the oral disease it is experiencing, provide better stability and lead the body to produce more beneficial molecules that can help improve its defense system against other infections and diseases.
"As a dentist/periodontist, my goal is to provide the best prevention and best treatment to my patients," Dr. Hasturk said. "As a researcher, this goal drives me to better understand health and disease, not only to improve oral health, but also overall health."

For Rajesh Lalla, B.D.S., Ph.D., professor of oral medicine and associate dean for research at the University of Connecticut School of Dental Medicine, his favorite part of being a researcher is the ability to create new knowledge.
"It is extremely satisfying to be able to go through the process of having an idea, designing a study to test that hypothesis and determining what the truth really is," said Dr. Lalla, who studies the oral side effects of radiation therapy and chemotherapy used in the treatment of cancer.
His research team is working to publish results from a multicenter clinical study that enrolled more than 500 patients undergoing radiation therapy for head and neck cancer.
"One of the novel findings is that the radiation treatment led to a striking increase in gingival recession," said Dr. Lalla, who is the immediate past president of the Multinational Association of Supportive Care in Cancer — the first dentist to hold the role. "It was known that these patients tend to get cervical caries after radiation therapy, but the reasons were not clear. Our finding indicates that exposure of the cervical areas of teeth due to gingival recession may explain the increased risk for cervical caries."
At the University of Connecticut, Dr. Lalla developed the dental school’s course on evidence-based decision making, which emphasizes the importance of evidence to the practice of dentistry.
"Dentistry is a scientific profession. The care we provide for our patients must be evidence based," said Dr. Lalla, who won the ADA’s 2020 Evidence-Based Dentistry Accomplished Faculty Award. "Research provides that evidence, so research is the very foundation of our profession."

With a background in engineering, Nathaniel Lawson, D.M.D., Ph.D., performs applied dental materials research at the University of Alabama at Birmingham School of Dentistry, where he is an associate professor, director of the biomaterials residency program and director of the division of biomaterials. He and his team devise testing equipment and protocols to evaluate dental materials to best predict their clinical performance, and they are perhaps most well known for performing wear testing. His lab is currently testing the wear of new 3D-printed materials being developed for dentures, crowns and occlusal guards.
"There are many different types of dental research. Many dentists may think of the incredible scientific work conducted by basic and translational scientists who are working to develop new treatments, materials and drugs to treat dental and oral conditions," said Dr. Lawson, who won the ADA's 2016 John W. Stanford New Investigator Award. "However, there is still research needed to evaluate the materials that are already in clinical use in order to determine the best uses of these materials. This information can help the clinician better perform work in their office."
Dr. Lawson began conducting research when he was applying to dental school at the University of Alabama. After a brief stint in clinical practice following graduation, his dental school research adviser asked if he would be interested in returning to his alma mater for an academic position performing research and teaching.
"Within a couple years of working in the position, I realized that I really loved what I was doing," Dr. Lawson said. "I really enjoy thinking of clinical problems, performing a study to try to better understand the best clinical treatment, trying what I learned in practice and then sharing that information through teaching."
Dr. Geisinger, too, was initially unsure of her career path and thought she would go into private practice until she began volunteering as a faculty member at a dental school.
"When I thought about the opportunity to make an exponential impact on our profession through education, research and service, I knew that I had to try to make the biggest impact I could on the oral health of patients and communities," she said. "And it is the research part of that mission that allows me to have the widest reach — impacting the global delivery of dental care through incremental discovery."
Dr. Geisinger, who is a member of the ADASRI Board of Directors and secretary-treasurer of the American Academy of Periodontology, is currently involved in a project examining best practices for delivering oral hygiene care to people with dementia in skilled nursing facilities, as well as the impact of periodontal health on the development and progression of dementia.
The research dentists perform has a lasting impact on not only the profession but public health as well.
"Dentists are an integral part of health care, and as an important health care provider, we need to base what we do on science and biology in order to offer evidence-based, scientifically proven and solid approaches to our patients," Dr. Hasturk said. "They are hungry to learn from us to do better at home and in their lives and to be examples to their children and young generations. We can only be better prepared for the future with proper education, and proper education is a result of research."
Most Read View More
Recommended content.

Arginine and the Healthy Oral Microbiome

Leveraging artificial intelligence to improve clinical outcomes

Enhance clear aligner oversight with CandidMonitoring™

The Hall Technique for Modern Pediatric Caries Management
Join the ADA
Elevate your career, your life and your momentum with resources and benefits from the nation’s leading dental association
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
Rapamycin may slow aging. here's one way the drug will be tested.

Allison Aubrey
Anti-aging drug Rapamycin to prevent gum disease

A generic drug that's used to treat transplant patients has been shown to extend the life span of some animals. Guido Mieth/Getty Images hide caption
A few years back, Matt Kaeberlein was diagnosed with a frozen shoulder. “It was really bad,” he recalls. He wasn’t sleeping well and couldn’t throw a ball due to the pain. His doctor recommended physical therapy, and told him that it may take a year to get better.
Feeling frustrated, he decided to try rapamycin. In recent years, some high-profile longevity scientists have started taking the drug in hopes of fending off age-related health problems. So far, it’s untested in people taking it for anti-aging, but rapamycin has been shown to extend the lifespan of mice .
“I decided to try it,” Kaeberlein says. It was his "first foray into biohacking,” and he was very pleased with what happened next. “Within two weeks, 50% of the pain was gone,” he says. And by the end of 10 weeks, he had regained range of motion and the pain was completely gone.
“And it hasn’t come back,” he says.
Kaeberlein is no stranger to rapamycin. He’s a biologist and co-founded the Dog Aging Project to study how rapamycin influences dogs’ healthspans. He’s also the former director of the Healthy Aging and Longevity Research Institute at the University of Washington.
Rapamycin was first approved by the FDA for use in transplant patients in the late 1990s. At high doses it suppresses the immune system. At low doses, Kaeberlein says it seems to help tamp down inflammation. It works by inhibiting a signaling pathway in the body called mTOR — which seems to be a key regulator of lifespan and aging.

Shots - Health News
Scientists can tell how fast you're aging. now, the trick is to slow it down.
The drug is not approved for pain or anti-aging, but some physicians prescribe rapamycin off-label with the aim of fending off age-related conditions. Kaeberlein and his colleagues surveyed about 300 of these patients, who take low doses, and many report benefits.
But anecdotes are no replacement for science. To figure out the risks and benefits of a drug, research is needed. And that's where a dentist comes in.
Dr. Jonathan An , at the University of Washington, has been granted FDA approval to test rapamycin in patients with gum disease — a common condition that tends to accelerate with age. When he treats patients with gum disease, he says there’s not much he can do beyond cleaning and removing the plaque — a buildup of bacteria. “All we’re doing is putting a bandage on,” he says. His goal is to find and treat the underlying cause of the disease.
There’s already some evidence from transplant patients that rapamycin may help improve oral health. And as part of the study, An and his collaborators will also measure changes in participants’ microbiomes and their biological clocks.
The study will enroll participants over the age of 50 who have gum disease. They will take the drug, at various doses, intermittently for 8 weeks. Then, An will be able to determine if the drug is safe and effective.
If rapamycin has a beneficial effect he says, it will help demonstrate that it’s possible to target the root cause of the disease. “It really comes down to targeting the biology of aging,” he says.
Dr. An thinks gum disease may be a kind of canary in the coalmine of age-related diseases. For instance, gum disease is linked to a higher risk of heart disease, and maybe dementia, too . Scientists say it’s possible that bacteria in the mouth linked to periodontal disease causes inflammation, which may cause a “cascade” of damage to blood vessels, leading to problems in the heart or brain.
“If we can target that underlying biology, we predict that it might address a lot of these other underlying conditions,” An says.
Rapamycin is a generic drug, so pharmaceutical companies have little incentive to fund new research. An and his collaborators have received a grant to conduct the trial, which could open the door to further studies to determine whether rapamycin can help prevent or slow down other age-related diseases.
Eric Verdin , a physician who heads the Buck Institute for Research on Aging, says his group is fundraising for more research on rapamycin. He says there are a lot of unanswered questions, for example “what is the effect of different concentrations in a single dose?” And he wants to look for a “molecular signature” in people taking rapamycin. He wants to know more about doses and intervals, since many doctors prescribing it off-label recommend cycling on and off the drug.
Researchers are also working on other drugs that may work in similar ways, and there’s a push for new drugs — or other interventions that target biological aging. There’s a new $100 million XPRIZE Healthspan competition , aimed at accelerating the research in the field supported by Hevolution and other funders.
For now, XPRIZE founder Peter Diamandis, a physician who writes about longevity, says he takes rapamycin. “I do six milligrams every Sunday night, so once a week," for three months, he explains. Then he takes a month off. "I believe that rapamycin — in the way I'm utilizing it — is safe and has more upside potential than downside,” he says.
Diamandis constantly monitors his body with many health metrics, and he acknowledges it’s hard to determine the effect of rapamycin given all the other things he does to stay healthy, including eating well, eliminating sugar, working out every day and prioritizing sleep.
His plan is to continue with healthy lifestyle habits while supporting research into interventions and strategies that can help people add more healthy years to their life.

A cheap drug may slow down aging. A study will determine if it works
Find Allison Aubrey on Instagram at @allison.aubrey and on X @AubreyNPR .
This story was edited by Jane Greenhalgh
Could Stem Cells Eventually Repair Your Cavity With ‘Living Fillings?’
- Rowan Lynam
Featured Experts
- Stem Cells for 'Living Fillings'
Cavity Repair Now
The future of dentistry.
- 'Living Fillings' are Science Fiction for Now
Our teeth can’t repair themselves…but what if they could? The future of dentistry lies in the captivating field of regenerative medicine, where stem cell research is diving deep into the potential to repair damaged teeth with “living fillings.” But how far are we from ditching fillings for specialized tooth restoration? While the research is science fact, getting a “living filling” from your dentist is still science fiction…for now.
- Victoria Veytsman, DDS is a cosmetic dentist based in New York
- Salvator La Mastra, DDS is a cosmetic dentist based in Dallas, TX
Stem Cells for ‘Living Fillings’
“I find this field really fascinating,” says New York cosmetic dentist Victoria Veytsman, DDS. “The field of tissue engineering and regenerative medicine in dentistry is really at the forefront of where healthcare is going.”
Stem cells are those super useful specialized cells (found in adult body tissues and in embryos) that can be guided towards becoming many different cell types and can self-replicate. That makes them immensely useful in regenerative medicine, where the goal is to get the body’s repair processes engaged to handle damaged, diseased or otherwise unwell tissues. According to the California Institute for Regenerative Medicine , the most commonly used stem cell-based therapy is for bone marrow transplants.
“When it comes to filling a cavity with them, stem cells alone aren’t enough to complete the process of tooth restoration,” explains Dallas, TX cosmetic dentist Salvator La Mastra, DDS. “They would need a framework of some kind in order to form in the correct manner.”
Dr. Veytsman explains that current research is focused on creating that framework, creating a kind of “living filling.”
“We don’t want enamel to grow in a petri dish; we want it to grow on your tooth,” Dr. Veytsman says. “So the process requires a scaffold or matrix to support that growth.”
When a tooth develops a cavity, the first step is to remove the decay and stop the process of damage. “Cavities are caused by bacteria,” Dr. La Mastra explains. “That acid producing bacteria is what causes the cavitation of the tooth, which is the cavity itself and the decay. It’s basically necrotic tissue that we have to drill out.”
Then, you have to fill in what’s lost. “We do things like crowns and fillings to replace the chief structure that was lost or decayed,” Dr. Veytsman explains. “It’s called restorative dentistry because we’re trying to restore what’s been lost.”
Those fillings are made of amalgam (a mixture of metals) or composite resin filling materials (made from polymers and glass particles), and we know they’re safe, functional and that they won’t decay in the future. That’s something we can’t say about these “living fillings.”
“One thing about our current implants and fillings is that we know they won’t develop cavities down the line,” La Mastra says. “There are complications that could arise from the regenerative method that could cause more than just aesthetic consequences; your bite can also be impacted.”
“I think we’re just at the beginning of this technology,” Dr. Veytsman says. “But it definitely has the potential to change the way we approach cavities in the years to come.”
Stem cells could also be utilized outside of “living fillings” to benefit oral health. Aside from repairing enamel, stem cells could be used to encourage the growth of dentin, restore pulp, even regenerate lost gum tissues.
“You’re seeing the rise of stem cell banking now for these purposes,” Dr. Veytsman explains. “Harvesting and banking stem cells for future applications and to use as a preventative measure are growing in popularity.”
‘Living Fillings’ are Science Fiction for Now
“I think we’re multiple decades away from a changeover to regenerative medicine in dentistry,” La Mastra says. “I already have patients who ask me if they can just regrow their tooth, and we are nowhere near being able to do that.”
While “living fillings” aren’t going to enter your dentist’s office in the immediate future, there’s still reason to be excited.
“The advent of AI technologies is really accelerating this research,” Dr. Veytsman says. “And it’s letting us ask a ton of questions about possible applications. Can regenerative medicine deal with prevention? Can it help stop decay in the very early stages? We’re still so early in this process, but AI and regenerative medicine are really at the forefront of healthcare right now.”
Related Posts
It's personal.
At NewBeauty, we get the most trusted information from the beauty authority delivered right to your inbox
Find a Doctor
Find a NewBeauty "Top Beauty Doctor" Near you
Give the Gift of Luxury
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Integration of Primary and Oral Health Care—An Unrealized Opportunity
- 1 Division of General Internal Medicine and Primary Care, Department of Medicine, Brigham and Women’s Hospital, Boston, Massachusetts
- 2 Harvard Medical School, Boston, Massachusetts
- 3 School of Dental Medicine, Stony Brook University, Stony Brook, New York
Primary care is the central component of a high-functioning and equitable health system. However, there is a shortage of primary care clinicians, and the time required to complete all recommended prevention services and counseling for a typical primary care panel is prohibitive. One solution is to use a team-based approach where a variety of professionals collaborate to meet patient needs. In 2021, the National Academies of Sciences, Engineering, and Medicine released a consensus report on implementing high-quality primary care, which emphasized the adoption of interprofessional teams and the use of nontraditional care settings to improve the quality and breadth of primary care in the US. 1 In this spirit, dentists are an important resource; they are medically trained and have longitudinal relationships with patients, who may not be seen by primary care clinicians.
Read More About
Simon L , Lamster I. Integration of Primary and Oral Health Care—An Unrealized Opportunity. JAMA Intern Med. Published online June 24, 2024. doi:10.1001/jamainternmed.2024.2267
Manage citations:
© 2024
Artificial Intelligence Resource Center
Best of JAMA Network 2022
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Articles on Dental hygiene
Displaying all articles.

Caring for older Americans’ teeth and gums is essential, but Medicare generally doesn’t cover that cost
Frank Scannapieco , University at Buffalo and Ira Lamster , Stony Brook University (The State University of New York)

No, it’s not just sugary food that’s responsible for poor oral health in America’s children, especially in Appalachia
Daniel W. McNeil , West Virginia University and Mary L. Marazita , University of Pittsburgh

How did people clean their teeth in the olden days?
Jane Cotter , Texas A&M University
Related Topics
- Curious Kids US
- Dental care
- Dental health
- Dental insurance
- History of medicine
- Oral health
- Periodontitis
Top contributors
SUNY Distinguished Professor of Oral Biology, University at Buffalo
Clinical Professor of Periodontics and Endodontics, Stony Brook University (The State University of New York)
Assistant Professor of Dental Hygiene, Texas A&M University
Director, Center for Craniofacial and Dental Genetics; Professor of Oral Biology and of Human Genetics, University of Pittsburgh
Eberly Distiniguished Professor Emeritus, Clinical Professor Emeritus of Dental Public Health & Professional Practice, West Virginia University
- X (Twitter)
- Unfollow topic Follow topic
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Book review
- Published: 30 June 2022
INNOVATIONS IN PREVENTIVE DENTISTRY
- Peter Folly 1
BDJ Student ( 2022 ) Cite this article
643 Accesses
Metrics details
Christian Splieth (editor)
2021; Quintessence
eISBN 9783868675627
Preventive dentistry is a constantly changing and developing field: As new research emerges, some practices that had once been revolutionary are abandoned, while others continue to withstand the test of time. This book discusses new developments and innovations in preventive dentistry, from primary prevention to secondary prevention by inactivating initial lesions, and on to tertiary prevention to avoid subsequent progression and complications of manifest oral disease.
The book relies on a sound evidence base and instructs readers how this can be translated into clinical dental practice - what changes should be made to how we practice and why they should be made. Topics include caries and periodontal disease, orthodontic problems, diagnostic approaches, diet and oral health, oral hygiene, oral disease patterns, caries treatment, fluoride guidelines, risk management, sealants, and probiotics.
Further information
Go to http://www.bda.org/ebooks to see our selection of dental ebooks or to https://www.bda.org/library/student-services to view our range of student services.
Any questions or comments? Email [email protected] or call 020 7563 4545.
Author information
Authors and affiliations.
British Dental Association, London, UK
Peter Folly
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Peter Folly .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Folly, P. INNOVATIONS IN PREVENTIVE DENTISTRY. BDJ Student (2022). https://doi.org/10.1038/s41406-022-0324-9
Download citation
Published : 30 June 2022
DOI : https://doi.org/10.1038/s41406-022-0324-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
WVU School of Pharmacy professor receives Governor’s highest honor
West Virginia Governor Jim Justice presented Dr. Elizabeth Scharman, professor emerita at the West Virginia University School of Pharmacy, with the 2024 Distinguished Mountaineer Award. This award is the highest honor the Governor can bestow upon a non-native West Virginian.
Dr. Scharman, who retired last month, served as the executive director of the West Virginia Poison Center for 32 years. During her tenure, she led operations such as the West Virginia DHHR Coronavirus Hotline, managed the Emergency Line, provided toxicology information during the 2014 Water Crisis, and worked across the state on poison prevention and toxicology education and treatment. Additionally, she played a key role as the deputy strategic national stockpile coordinator, contributing significantly to emergency preparedness planning within the state.

Dr. Scharman holds certifications as a board-certified delegate of the American Board of Applied Toxicology and as a board-certified pharmacotherapy specialist. She previously chaired the Kanawha/Putnam Emergency Planning Committee and has been involved in various committees and editorial boards. Her scholarly contributions include numerous published articles and chapters in pharmacy textbooks. Among her many accolades are the WVU Health Sciences Women in Science and Health Advanced Career Excellence Awards in 2015, the American Academy of Clinical Toxicology's 2012 Distinguished Service Award, and the WVU School of Pharmacy's Outstanding Service Award in 2022.
Governor Justice's framed proclamation reads, “Scharman is a caring and giving person, and her dedication and commitment to her career and the great state of West Virginia have set an outstanding example for us all.”
- Search Menu
Sign in through your institution
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- Why Submit?
- About Public Opinion Quarterly
- About the American Association for Public Opinion Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

ANTI-SEMITIC ATTITUDES OF THE MASS PUBLIC: ESTIMATES AND EXPLANATIONS BASED ON A SURVEY OF THE MOSCOW OBLAST
- Article contents
- Figures & tables
- Supplementary Data
JAMES L. GIBSON, RAYMOND M. DUCH, ANTI-SEMITIC ATTITUDES OF THE MASS PUBLIC: ESTIMATES AND EXPLANATIONS BASED ON A SURVEY OF THE MOSCOW OBLAST, Public Opinion Quarterly , Volume 56, Issue 1, SPRING 1992, Pages 1–28, https://doi.org/10.1086/269293
- Permissions Icon Permissions
In this article we examine anti-Semitism as expressed by a sample of residents of the Moscow Oblast (Soviet Union). Based on a survey conducted in 1920, we begin by describing anti-Jewish prejudice and support for official discrimination against Jews. We discover a surprisingly low level of expressed anti-Semitism among these Soviet respondents and virtually no support for state policies that discriminate against Jews. At the same time, many of the conventional hypotheses predicting anti-Semitism are supported in the Soviet case. Anti-Semitism is concentrated among those with lower levels of education, those whose personal financial condition is deteriorating, and those who oppose further democratization of the Soviet Union. We do not take these findings as evidence that anti-Semitism is a trivial problem in the Soviet Union but, rather, suggest that efforts to combat anti-Jewish movements would likely receive considerable support from ordinary Soviet people.
American Association for Public Opinion Research members
Personal account.
- Sign in with email/username & password
- Get email alerts
- Save searches
- Purchase content
- Activate your purchase/trial code
- Add your ORCID iD
Institutional access
Sign in with a library card.
- Sign in with username/password
- Recommend to your librarian
- Institutional account management
- Get help with access
Access to content on Oxford Academic is often provided through institutional subscriptions and purchases. If you are a member of an institution with an active account, you may be able to access content in one of the following ways:
IP based access
Typically, access is provided across an institutional network to a range of IP addresses. This authentication occurs automatically, and it is not possible to sign out of an IP authenticated account.
Choose this option to get remote access when outside your institution. Shibboleth/Open Athens technology is used to provide single sign-on between your institution’s website and Oxford Academic.
- Click Sign in through your institution.
- Select your institution from the list provided, which will take you to your institution's website to sign in.
- When on the institution site, please use the credentials provided by your institution. Do not use an Oxford Academic personal account.
- Following successful sign in, you will be returned to Oxford Academic.
If your institution is not listed or you cannot sign in to your institution’s website, please contact your librarian or administrator.
Enter your library card number to sign in. If you cannot sign in, please contact your librarian.
Society Members
Society member access to a journal is achieved in one of the following ways:
Sign in through society site
Many societies offer single sign-on between the society website and Oxford Academic. If you see ‘Sign in through society site’ in the sign in pane within a journal:
- Click Sign in through society site.
- When on the society site, please use the credentials provided by that society. Do not use an Oxford Academic personal account.
If you do not have a society account or have forgotten your username or password, please contact your society.
Sign in using a personal account
Some societies use Oxford Academic personal accounts to provide access to their members. See below.
A personal account can be used to get email alerts, save searches, purchase content, and activate subscriptions.
Some societies use Oxford Academic personal accounts to provide access to their members.
Viewing your signed in accounts
Click the account icon in the top right to:
- View your signed in personal account and access account management features.
- View the institutional accounts that are providing access.
Signed in but can't access content
Oxford Academic is home to a wide variety of products. The institutional subscription may not cover the content that you are trying to access. If you believe you should have access to that content, please contact your librarian.
For librarians and administrators, your personal account also provides access to institutional account management. Here you will find options to view and activate subscriptions, manage institutional settings and access options, access usage statistics, and more.
Short-term Access
To purchase short-term access, please sign in to your personal account above.
Don't already have a personal account? Register
| Month: | Total Views: |
|---|---|
| November 2016 | 1 |
| January 2017 | 3 |
| March 2017 | 1 |
| August 2017 | 2 |
| February 2018 | 1 |
| March 2018 | 1 |
| August 2018 | 2 |
| October 2018 | 1 |
| November 2018 | 2 |
| December 2018 | 1 |
| June 2019 | 1 |
| October 2019 | 1 |
| November 2019 | 1 |
| January 2020 | 2 |
| February 2020 | 1 |
| March 2020 | 2 |
| June 2020 | 1 |
| August 2020 | 2 |
| October 2020 | 1 |
| November 2020 | 1 |
| December 2020 | 1 |
| August 2021 | 1 |
| November 2021 | 1 |
| February 2022 | 1 |
| December 2022 | 1 |
| January 2023 | 1 |
| April 2023 | 1 |
| June 2023 | 2 |
| August 2023 | 1 |
| October 2023 | 1 |
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1537-5331
- Copyright © 2024 American Association for Public Opinion Research
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Rights and permissions
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

COMMENTS
Evaluation of the effects of temperature and centrifugation time on elimination of uncured resin from 3D-printed dental aligners. Ji-Eun Kim. Utkarsh Mangal. Sung-Hwan Choi. Research Open Access ...
Latest research on periodontal diseases. Information on a broad range of dental health topics, including dental implants, cosmetic dentistry, and general dental health.
Effects of post-COVID-19 vaccination in oral cavity: a systematic review. Anubhuti Sood. Sreevatsan Raghavan. Harsh Priya. Research 16 May 2024 Evidence-Based Dentistry. P: 1-5.
A team of UCLA School of Dentistry researchers led by Takahiro Ogawa, D.D.S., Ph.D., has culminated a decade of dental implant research with the development of a cutting-edge technology that ...
Research 06 Mar 2024 Evidence-Based Dentistry Volume: 25, P: 111-112 The effect of aromatherapy with Lavender-Neroli oil and music in management of pediatric dental anxiety: a randomized control trial
Abstract. The digital transformation in dental medicine, based on electronic health data information, is recognized as one of the major game-changers of the 21st century to tackle present and upcoming challenges in dental and oral healthcare. This opinion letter focuses on the estimated top five trends and innovations of this new digital era ...
Journal of Dental Research (JDR) is a peer-reviewed scientific journal dedicated to the dissemination of new knowledge and information, encompassing all areas of clinical research in the dental, oral and craniofacial sciences. Average time from submission to first decision: 17 days View full journal description
Abstract. For nearly 20 years, dental stem cells (DSCs) have been successfully isolated from mature/immature teeth and surrounding tissue, including dental pulp of permanent teeth and exfoliated deciduous teeth, periodontal ligaments, dental follicles, and gingival and apical papilla. They have several properties (such as self-renewal ...
In dental research and practice, all eyes are on artificial intelligence's (AI) promise for patients. AI has made its arrival in dental care around the world, largely thanks to a swell of early adopters who have embraced the newest assistive technologies that could lead to earlier diagnosis of oral diseases and put more informative tools in the hands of patients.
Sage discipline hubs. Explore the content from across our disciplines, including the latest journal articles, special issues, and related books and digital library content. Advances in Dental Research publishes supplements to the Journal of Dental Research (JDR) . A subscription to JDR grants you access to the articles in Adv...
In recent years, the dental and craniofacial healthcare sectors have witnessed significant advancements driven by the integration of digitalization, new technologies, and telemedicine. These innovations have transformed diagnostic and therapeutic approaches, enhancing precision, efficiency, and patient outcomes.
Lab-made monomers and polymers capable of switching physicochemical properties in response to pH variations in oral environments could become a new class of dental restoratives. | By Han Byul Song, Xiaohong Wang, Sara Orski, Kathryn Beers, and Jirun Sun. Physicochemical, Mechanical, and Antimicrobial Evaluation of Novel Bioactive Resin (2020)
Digital systems now offer the opportunity to avoid conventional, analogue impressions, including traditional impression materials, time, and handling limitations associated with them. Intraoral scanners have the potential to offer excellent accuracy with a more comfortable patient experience and more efficient workflow for the dental practice.
Current Research in Dentistry cover articles on evaluation, diagnosis, prevention, and treatment of diseases, disorders and conditions of the soft and hard tissues of the jaw, the oral cavity, maxillofacial area and the adjacent and associated structures and their impact on the human body. Current Research in Dentistry is an international, peer ...
By David Cox. From fluoride toothpaste to dental sealants, science has brought all sorts of tools for fighting tooth decay — and yet 91% of Americans between 20 and 64 years of age are affected ...
News-Medical is your trusted source of Dentistry news, articles and research for doctors, patients, and families. ... A new research paper was published in Oncotarget's Volume 15 on June 13, 2024 ...
The ADA Science & Research Institute, LLC (ADASRI) conducts cutting-edge studies that advance dental technology and care. Stay on top of ADASRI clinical research guiding best-in-class dental care and delivery. Meet our team of leaders in oral health sciences that drive innovation in dental care.
Research 21 Jun 2024 Evidence-Based Dentistry. P: 1-9. Fifteen-year recall period on zirconia-based single crowns and fixed dental prostheses. A prospective observational study. Shahnawaz ...
A New Day for Dentistry, a campaign launched by ADA President Cesar R. Sabates, D.D.S., celebrates the ADA's diverse community of dentists by recognizing their personal differences and the varied career paths they have chosen within the profession. "Researchers are essential members of the dental workforce," Dr. Sabates said.
Here's how it'll be tested in humans : Shots - Health News Longevity researchers are taking a generic drug they think may help extend people's lives. Now a dentist is testing if rapamycin stops ...
While the research is science fact, getting a "living filling" from your dentist is still science fiction…for now. Featured Experts. Victoria Veytsman, DDS is a cosmetic dentist based in New ...
research news Tools of UB dental professor's bitemark research included in Smithsonian exhibition The biting apparatus created by UB alumnus Kyle Thorsrud in the lab of Mary Bush, forensic dentist and associate professor of restorative dentistry in School of Dental Medicine, is one of the pieces included in the Smithsonian exhibition ...
A common infection-causing bacteria was much less likely to evolve antibiotic resistance when treated with a mixture of antimicrobial peptides rather than a single peptide, making these mixtures a ...
Dentists have a long-standing history of successfully screening for and counseling about health behaviors associated with worse oral health outcomes, such as tobacco use disorder and diets high in processed foods; in one survey, more than 90% of dentists reported screening for tobacco use. 2 More ambitious efforts have also been successful. In the Kaiser Pacific Northwest health care system ...
Clinical Professor of Periodontics and Endodontics, Stony Brook University (The State University of New York) Jane Cotter Assistant Professor of Dental Hygiene, Texas A&M University
Christian Splieth (editor) 2021; Quintessence. 399 pages. eISBN 9783868675627. Preventive dentistry is a constantly changing and developing field: As new research emerges, some practices that had ...
In April, P3 student pharmacist Anna Lumadue from the West Virginia University School of Pharmacy, along with Assistant Professor Sabina Nduaguba from the Department of Pharmaceutical Outcomes and Policy, had the unique opportunity to present their research at the American Association for Cancer Research (AACR) Annual Meeting.
We are grateful to several agencies for support for this research, including the National Science Foundation (SES-9003868), the College of Social Sciences and the Limited-Grant-in-Aid program at the University of Houston, the Dresser Foundation, the American Jewish Committee, and the USSR Academy of Sciences. ... New issue alert. Receive ...
Elektrostal Weather Forecasts. Weather Underground provides local & long-range weather forecasts, weatherreports, maps & tropical weather conditions for the Elektrostal area.
In what follows, we will measure the magnetic eld strength in units of Bc (1) and take the electron mass m, the Compton wavelength of the electron = ~=mc 3:86 10 11 cm, and its ratio to the speed of light =c 1:29 10 21 s as the units of mass, length, and time, respectively. Formally, this means that ~ = = c = 1.