The Value of Critical Thinking in Nursing

- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

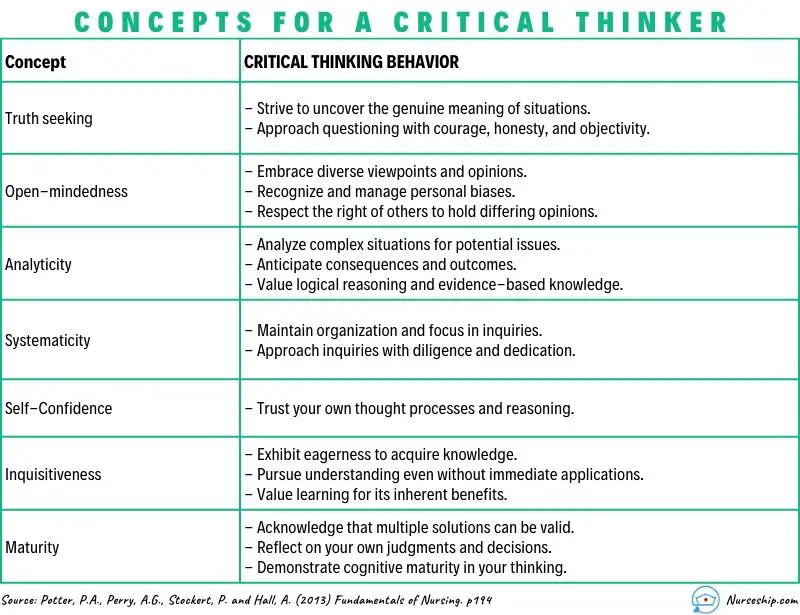
Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.

How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter, DNP, APRN, ACNS-BC, CNE
Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads, Ph.D., RN
Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan, BSN, RN, CCRN
Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.
What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.
What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

- Who We Insure
- Insurance Products
- About Berxi
Topics on this page:
The importance of critical thinking in nursing.
Topics on this page

While not every decision is an immediate life-and-death situation, there are hundreds of decisions nurses must make every day that impact patient care in ways small and large.
“Being able to assess situations and make decisions can lead to life-or-death situations,” said nurse anesthetist Aisha Allen . “Critical thinking is a crucial and essential skill for nurses.”
The National League for Nursing Accreditation Commission (NLNAC) defines critical thinking in nursing this way: “the deliberate nonlinear process of collecting, interpreting, analyzing, drawing conclusions about, presenting, and evaluating information that is both factually and belief-based. This is demonstrated in nursing by clinical judgment, which includes ethical, diagnostic, and therapeutic dimensions and research.”
Why Critical Thinking in Nursing Is Important
An eight-year study by Johns Hopkins reports that 10% of deaths in the U.S. are due to medical error — the third-highest cause of death in the country.
“Diagnostic errors, medical mistakes, and the absence of safety nets could result in someone’s death,” wrote Dr. Martin Makary , professor of surgery at Johns Hopkins University School of Medicine.
Everyone makes mistakes — even doctors. Nurses applying critical thinking skills can help reduce errors.
“Question everything,” said pediatric nurse practitioner Ersilia Pompilio RN, MSN, PNP . “Especially doctor’s orders.” Nurses often spend more time with patients than doctors and may notice slight changes in conditions that may not be obvious. Resolving these observations with treatment plans can help lead to better care.
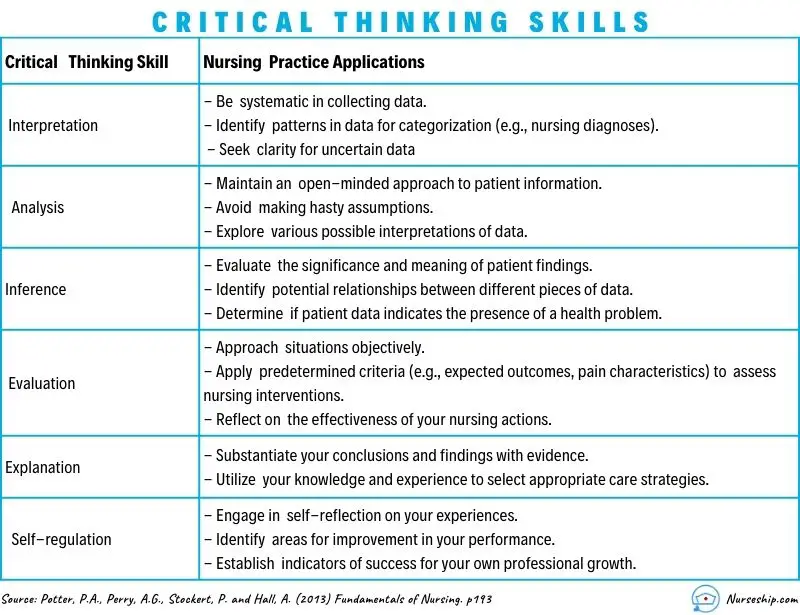
Key Nursing Critical Thinking Skills
Some of the most important critical thinking skills nurses use daily include interpretation, analysis, evaluation, inference, explanation, and self-regulation.
- Interpretation: Understanding the meaning of information or events.
- Analysis: Investigating a course of action based on objective and subjective data.
- Evaluation: Assessing the value of information and its credibility.
- Inference: Making logical deductions about the impact of care decisions.
- Explanation: Translating complicated and often complex medical information to patients and families in a way they can understand to make decisions about patient care.
- Self-Regulation: Avoiding the impact of unconscious bias with cognitive awareness.
These skills are used in conjunction with clinical reasoning. Based on training and experience, nurses use these skills and then have to make decisions affecting care.
It’s the ultimate test of a nurse’s ability to gather reliable data and solve complex problems. However, critical thinking goes beyond just solving problems. Critical thinking incorporates questioning and critiquing solutions to find the most effective one. For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health.
8 Examples of Critical Thinking in Nursing
Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Example #1: Patient Assessments
“Doing a thorough assessment on your patient can help you detect that something is wrong, even if you're not quite sure what it is,” said Shantay Carter , registered nurse and co-founder of Women of Integrity . “When you notice the change, you have to use your critical thinking skills to decide what's the next step. Critical thinking allows you to provide the best and safest care possible.”
Example #2: First Line of Defense
Often, nurses are the first line of defense for patients.
“One example would be a patient that had an accelerated heart rate,” said nurse educator and adult critical care nurse Dr. Jenna Liphart Rhoads . “As a nurse, it was my job to investigate the cause of the heart rate and implement nursing actions to help decrease the heart rate prior to calling the primary care provider.”
Nurses with poor critical thinking skills may fail to detect a patient in stress or deteriorating condition. This can result in what’s called a “ failure to rescue ,” or FTR, which can lead to adverse conditions following a complication that leads to mortality.
Example #3: Patient Interactions
Nurses are the ones taking initial reports or discussing care with patients.
“We maintain relationships with patients between office visits,” said registered nurse, care coordinator, and ambulatory case manager Amelia Roberts . “So, when there is a concern, we are the first name that comes to mind (and get the call).”
“Several times, a parent called after the child had a high temperature, and the call came in after hours,” Roberts said. “Doing a nursing assessment over the phone is a special skill, yet based on the information gathered related to the child's behavior (and) fluid intake, there were several recommendations I could make.”
Deciding whether it was OK to wait until the morning, page the primary care doctor, or go to the emergency room to be evaluated takes critical thinking.
Example #4: Using Detective Skills
Nurses have to use acute listening skills to discern what patients are really telling them (or not telling them) and whether they are getting the whole story.
“I once had a 5-year-old patient who came in for asthma exacerbation on repeated occasions into my clinic,” said Pompilio. “The mother swore she was giving her child all her medications, but the asthma just kept getting worse.”
Pompilio asked the parent to keep a medication diary.
“It turned out that after a day or so of medication and alleviation in some symptoms, the mother thought the child was getting better and stopped all medications,” she said.
Example #5: Prioritizing
“Critical thinking is present in almost all aspects of nursing, even those that are not in direct action with the patient,” said Rhoads. “During report, nurses decide which patient to see first based on the information gathered, and from there they must prioritize their actions when in a patient’s room. Nurses must be able to scrutinize which medications can be taken together, and which modality would be best to help a patient move from the bed to the chair.”
A critical thinking skill in prioritization is cognitive stacking. Cognitive stacking helps create smooth workflow management to set priorities and help nurses manage their time. It helps establish routines for care while leaving room within schedules for the unplanned events that will inevitably occur. Even experienced nurses can struggle with juggling today’s significant workload, prioritizing responsibilities, and delegating appropriately.
Example #6: Medication & Care Coordination
Another aspect that often falls to nurses is care coordination. A nurse may be the first to notice that a patient is having an issue with medications.
“Based on a report of illness in a patient who has autoimmune challenges, we might recommend that a dose of medicine that interferes with immune response be held until we communicate with their specialty provider,” said Roberts.
Nurses applying critical skills can also help ease treatment concerns for patients.
“We might recommend a patient who gets infusions come in earlier in the day to get routine labs drawn before the infusion to minimize needle sticks and trauma,” Robert said.
Example #7: Critical Decisions
During the middle of an operation, the anesthesia breathing machine Allen was using malfunctioned.
“I had to critically think about whether or not I could fix this machine or abandon that mode of delivering nursing anesthesia care safely,” she said. “I chose to disconnect my patient from the malfunctioning machine and retrieve tools and medications to resume medication administration so that the surgery could go on.”
Nurses are also called on to do rapid assessments of patient conditions and make split-second decisions in the operating room.
“When blood pressure drops, it is my responsibility to decide which medication and how much medication will fix the issue,” Allen said. “I must work alongside the surgeons and the operating room team to determine the best plan of care for that patient's surgery.”
“On some days, it seems like you are in the movie ‘The Matrix,’” said Pompilio. “There's lots of chaos happening around you. Your patient might be decompensating. You have to literally stop time and take yourself out of the situation and make a decision.”
Example #8: Fast & Flexible Decisions
Allen said she thinks electronics are great, but she can remember a time when technology failed her.
“The hospital monitor that gives us vitals stopped correlating with real-time values,” she said. “So I had to rely on basic nursing skills to make sure my patient was safe. (Pulse check, visual assessments, etc.)”
In such cases, there may not be enough time to think through every possible outcome. Critical thinking combined with experience gives nurses the ability to think quickly and make the right decisions.
Improving the Quality of Patient Care
Nurses who think critically are in a position to significantly increase the quality of patient care and avoid adverse outcomes.
“Critical thinking allows you to ensure patient safety,” said Carter. “It’s essential to being a good nurse.”
Nurses must be able to recognize a change in a patient’s condition, conduct independent interventions, anticipate patients and provider needs, and prioritize. Such actions require critical thinking ability and advanced problem-solving skills.
“Nurses are the eyes and ears for patients, and critical thinking allows us to be their advocates,” said Allen.
Image courtesy of iStock.com/ davidf
Last updated on Jan 05, 2024 .
Originally published on Aug 25, 2021 .
The views expressed in this article are those of the author and do not necessarily reflect those of Berxi™ or Berkshire Hathaway Specialty Insurance Company. This article (subject to change without notice) is for informational purposes only, and does not constitute professional advice. Click here to read our full disclaimer
Delegation in Nursing: Steps, Skills, & Solutions for Creating Balance at Work
The 7 Most Common Nursing Mistakes (And What You Can Do If You Make One)
Resource topics.

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
What are the Levels of Critical Thinking in Nursing?
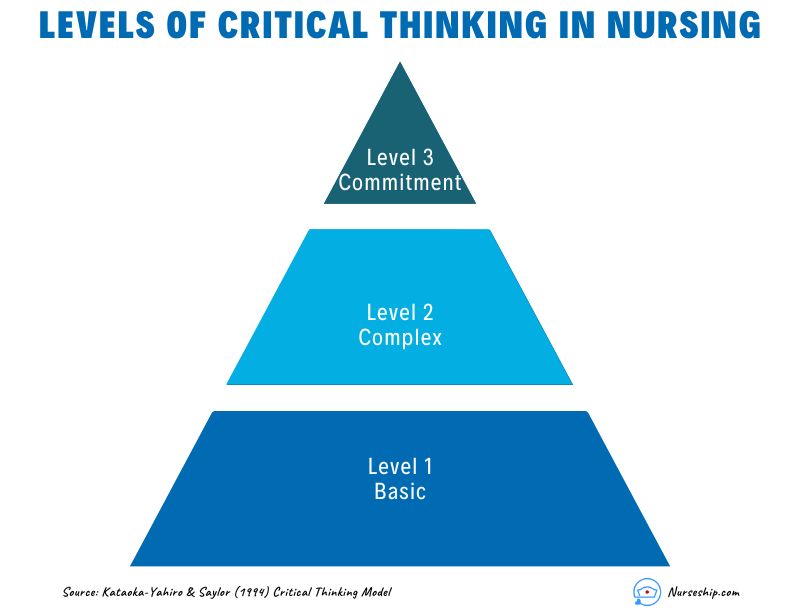
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.
Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
| Level 1: Gathering | 1. What are the common side effects of the prescribed medication? 2. When was the patient’s last bowel movement? 3. Who is the patient’s emergency contact person? 4. Describe the patient’s current level of pain. 5. What information is in the patient’s medical record? |
| 1. What would happen if the patient’s blood pressure falls further? 2. Compare the patient’s oxygen saturation levels before and after administering oxygen. 3. What other nursing interventions could be considered for wound care? 4. Infer the potential reasons behind the patient’s increased heart rate. 5. Analyze the relationship between the patient’s diet and blood glucose levels. | |
| 1. What do you think will be the patient’s response to the new pain management strategy? 2. Could the patient’s current symptoms be indicative of an underlying complication? 3. How would you prioritize care for patients with varying acuity levels in the emergency department? 4. What evidence supports your choice of administering the medication at this time? 5. Create a care plan for a patient with complex needs requiring multiple interventions. |
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.

- Login / FREE TRIAL

‘Nursing is on the front line in times of war and elections’
STEVE FORD, EDITOR
- You are here: Archive
Thinking your way to successful problem-solving
13 September, 2001 By NT Contributor
VOL: 97, ISSUE: 37, PAGE NO: 36
Jacqueline Wheeler, DMS, MSc, RGN, is a lecturer at Buckinghamshire Chilterns University College
Problems - some people like them, some do not think they have any, while others shy away from them as if they were the plague. Opportunities, in the form of problems, are part of your life.
The most difficult decision is deciding to tackle a problem and implement a solution, especially as it is sometimes easier to ignore its existence. Problem-solving takes time and effort, but once a problem has been addressed the nurse can feel satisfied that the issue has been resolved and is therefore less likely to re-emerge.
Nurses make clinical decisions using two different approaches. The first is the rationalist approach, which involves an analysis of a situation so that subsequent actions are rational, logical and based on knowledge and judgement. The second approach is based on a phenomenological perspective, where a fluid, flexible and dynamic approach to decision-making is required, such as when dealing with an acutely ill patient.
Types of problems
Problems come in different guises and the solver can perceive them either as a challenge or a threat. One of the most common types of problem is when the unexpected happens. As a nurse you plan and implement care for a patient based on your knowledge and experience, only to find that the patient’s reaction is totally different from that expected but without any apparent reason.
Another type of problem is an assignment where others set a goal or task. Throughout your working life you will be required to undertake duties on behalf of other people. For some this is difficult as they feel unable to control their workload. Others see it as an opportunity to develop new skills or take on additional responsibilities. Opportunities can be perceived as problems by those who fear failure.
A third type of problem is when a dilemma arises. This is when it is difficult to choose the best solution to a problem because the nurse is confronted with something that challenges his or her personal and/or professional values.
Diagnosing problems
The sooner a problem is identified and solutions devised, the better for all involved. So try to anticipate or identify problems when they occur through continuously monitoring staff performance and patient outcomes.
Listening to and observing junior staff will help you to detect work or organisational concerns, because when there are problems staff are likely to behave in an unusual or inconsistent manner.
Initial analysis
Remember that people view things differently, so what you perceive as a problem may not be one to anyone else. So before you begin thinking about what to do - whether to keep it under surveillance, contain it or find a solution - you should undertake an initial analysis. This will help you to understand the problem more clearly.
An analysis will also enable you to prioritise its importance in relation to other problems as problems do not occur one at a time.
Routine problems often need little clarification, so an initial analysis is recommended for non-routine problems only. Even then, not all problems justify the same degree of analysis. But where it is appropriate, an initial analysis will provide a basis from which to generate solutions.
Perception is also important when dealing with patients’ problems. For example, if a patient gives up reading because he or she cannot hold the book (objective), the nurse may assume it is because the patient has lost interest (subjective, one’s own view).
Generating solutions
It is essential for the problem-solver to remember that, where possible, solutions must come from those connected with the problem. If it is to be resolved, agreement must be owned by those involved as they are probably the best and only people who can resolve their differences. The manager should never feel that he or she must be on hand to deal with all disputes.
To solve a problem you need to generate solutions. However, the obvious solution may not necessarily be the best. To generate solutions, a mixture of creative and analytical thinking is needed (Bransford, 1993).
Creativity is about escaping from preconceived ideas that block the way to finding an innovative solution to a problem. An effective tool for assisting in this process is the technique of lateral thinking, which is based largely on the work of Edward de Bono, who regards thinking as a skill.
There are several ways to encourage creative decision-making. One method that works best for specific or simple problems is brainstorming. If the ground rules of confidentiality and being non-judgemental are applied, it will produce a free flow of ideas generated without fear of criticism (Rawlinson, 1986).
Time constraints and staff availability may make it difficult for all those involved in a problem to meet. In such cases an adaptation of brainstorming - where a blank piece of paper is given to those involved and each writes down four solutions to the problem - may be the answer. A similar technique is the collective notebook, where people are asked to record their thoughts and ideas about a problem for a specified period.
An alternative is where one person writes down a list of solutions in order of priority, which is then added to by others. This helps to prioritise the ideas generated. All these methods produce data that can then be analysed by the problem-solver.
When the problem affects people in different geographical areas, solutions can be generated by obtaining the opinion of experts through the use of a questionnaire, which is known as the Delphi technique (McKenna, 1994).
When an apparently insurmountable problem presents itself, it is often useful to divide it into smaller pieces. This is known as convergent thinking. Using divergent thinking - where you consider a problem in different ways to expand your view - may also help.
A final alternative is the stepladder technique, which is time-consuming but effective if the issue is stirring up strong feelings. This requires the people involved in the problem to be organised into groups. First, two people try to solve the problem, then a third member is drawn in, to whom the solution reached by the first two is presented. All three then try to agree a solution. More people are added to the group, if necessary, in a similar way, until there is agreement of all involved. Provided the individuals are motivated to solve the problem, this technique creates ownership and commitment to implementing the agreed solution.
Analytical thinking, which follows a logical process of eliminating ideas, will enable you to narrow the range down to one feasible solution.
Although someone has to make the ultimate decision on which solution to implement, there are advantages to group decision-making: a greater number of possible solutions are generated and conflicts are resolved, resulting in decisions being reached through rational discussion.
This does, however, require the group to be functioning well or the individuals involved may feel inhibited in contributing to the decision-making. One individual may dominate the group or competition between individuals may result in the need to win taking precedence over deciding on an agreed practical solution.
As nursing becomes less bureaucratic individuals are being encouraged to put forward their own ideas, but social pressures to conform may inhibit the group. We do not solve problems and make decisions in isolation, but are influenced by the environment in which we work and the role we fulfil in that environment. If group members lack commitment and/or motivation, they may accept the first solution and pay little attention to other solutions offered.
Making a decision
There are three types of decision-making environments: certain, risk and uncertain. The certain environment, where we have sufficient information to allow us to select the best solution, is the most comfortable within which to make a decision, but it is the least often encountered.
We usually encounter the risk environment, where we lack complete certainty about the outcomes of various courses of action.
Finally, the uncertain environment is the least comfortable within which to make decisions as we are almost forced to do this blind. We are unable to forecast the possible outcomes of alternative courses of action and, therefore, have to rely heavily on creative intuition and the educated guess.
Taking this into consideration, you should not contemplate making a decision until you have all the information needed. Before you make your decision, remind yourself of the objective, reassess the priorities, consider the options and weigh up the strengths, weaknesses, opportunities and threats of each solution.
An alternative is to use the method that Thomas Edison used to solve the problem of the electric light bulb. Simply focus on your problem as you drift off to sleep, and when you wake up your subconscious mind will have presented you with the answer. But bear in mind that this is not a scientific way of solving problems - your subconscious can be unreliable.
If you are not sure about your decision, test the solution out on others who do not own the problem but may have encountered a similar dilemma. Once you have made your choice stick to it, or you may find it difficult to implement because those involved will never be sure which solution is current. They will also be reluctant to become involved in any future decision-making because of your uncertainty.
The next step is to ensure that all the people involved know what decision has been made. Where possible, brief the group and follow this up with written communication to ensure everyone knows what is expected of them. You may need to sell the decision to some, especially if they were not involved in the decision-making process or the solution chosen is not theirs.
Implementing the solution
Finally, to ensure the solution is implemented, check that the people involved know who is to do what, by when and that it has happened. Review the results of implementing your solution (see Box) and praise and thank all those involved.
- Part 1 of this series was published in last week’s issue: Wheeler, J. (2001) How to delegate your way to a better working life. Nursing Times; 97: 36, 34-35.
Next week. Part three: a step-by-step guide to effective report writing.
- Add to Bookmarks
Related articles
Christmas prize gave winner a head start in her studies
As we announce the winner of the Nursing Times Christmas Competition for 2017, we…
Competition winner goes the extra mile to put patients at ease
In December, Nursing Times invited readers to nominate a nurse who makes a real…

Inter-professional education: if we are working together, shouldn’t we be learning together?
As nurses, no matter what our field of practice, we always work…

Special recognition for nurses who treated terror attack victims
Nurses from the hospital trusts that treated the victims of this year’s…
Have your say
Sign in or Register a new account to join the discussion.
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Solving problems together
Chapter 3 Solving problems together Objectives 1. Define mutuality in nurse–client relationships 2. Discuss the use of face work and politeness theory in approaching clients 3. Discuss mutual problem solving to involve the client in the implementation of the nursing process 4. Complete exercises to practice a mutual problem-solving approach to the nursing process 5. Examine the steps in making contracts with clients 6. Participate in exercises to build skills in solving problems with clients We must not talk to them, or at them, but with them. Florence Nightingale [on partnership with clients] ( Atwell , 2010) Moments of Connection . . . Setting Goals Together A nurse was called to a client’s room to discuss her therapy options for cancer treatment. As they talked, the client began to clearly understand that this disease was going to be what claimed her life. The client cried the most deep, painful, gut-level crying the nurse had ever experienced with an adult. The nurse held her hand and cried with her. They began to talk when the client relaxed. They set goals of her leaving the hospital and experiencing her next Christmas. The nurse said she felt good that she was able to take the time to let the client cry. Mutuality in nurse–client relationships Mutuality, a concept grounded in research, is an essential element in building relationships with the client, although it is not always easy to achieve ( Berg , 2005; Chalmers , 2005; Geanellos , 2005; Jack , 2005; Porr , 2005; Zoffmann , 2005). Mutuality is characterized by empathy, collaboration, equality, and interdependency ( Jeon , 2004). Mutuality is “the experience of real or symbolic commonalities of visions, goals, sentiments, or characteristics, including shared acceptance of difference that validates the person’s world-view” ( Hagerty et al, 1993, p. 294). Responsive relationships between the nurse and client are based on respect, trust, and mutuality that reflect both personal moral knowledge and ethical nursing knowledge ( Tarlier , 2004). Mutuality is a sharing of collective knowledge ( McCance et al, 2008). An ongoing sharing of knowledge between healthcare professionals and shared decision making help ensure patient satisfaction ( Cerda et al, 2010). Face work and politeness theory The outcome of the client–nurse interaction depends on the nurse’s ability to engage the client in decision making and share the control and power in the relationship ( Roberts et al, 1995; Spiers , 1998). Nurses build their communication skills by study and practice of techniques, trial and error, observation of role models, experience, and achievement of comfort with the use of their own intuition. Face work and politeness theory point to the need to consider the client’s and nurse’s “sense of self-esteem, autonomy, and solidarity in conversation” ( Spiers , 1998). We speak of “saving face” or helping the other “save face” and mean the preservation of dignity so that each party continues to be willing to invest in the interaction without experiencing any threat. Consider a patient stepping up on the scale to be weighed. Clients want to preserve or manage their image of self or “face.” How the nurse handles this situation can influence the client’s willingness to problem solve if the weight is “face threatening,” that is, not what the person wanted or expected ( Pillet-Shore , 2006). If the client is discouraged, the nurse might offer, “We all have things to work on. If your weight is not what you desire just now, we can work together to meet your goals.” In the complex process of problem solving with the client to promote health, many factors can present barriers, including perceptions and negotiations about the rules, norms, expectations, and boundaries that can distort both information and interpersonal intent ( Cauce and Srebnik, 1990). Nurses must “negotiate a mutually acceptable and satisfying level of distance or intimacy, self-disclosure, privacy, and information exchange with a context of power differences, a need for help, and a right to act” ( Spiers , 1998). Each party wants to maintain a sense of personal competency and control. Attacks on these or on the person’s poise or sense of belonging or being liked are called face threats. Consider the actions of the nurse in assessment: questioning about the client’s behavior, a physical assessment, and assessment of and intervention in spiritual needs. These actions are invasive. Polite behavior, which is more than just our notion of the conduct traditionally required by mothers and is a part of the consideration of face theory, refers to ways in which nurses ease the interaction to help decrease fear, embarrassment, and anger. Polite behaviors lessen the threat of the intimate nature of nursing interventions. Nurses may gently and indirectly encourage the client’s participation in problem solving, whereas a direct order in such a situation would be considered impolite and inappropriate. When discussing a potentially embarrassing situation such as safe sex, the nurse is careful about the language used and asks questions gently to help the client save face. Because of the complicated balance between considerations of face work and politeness and the necessity for client involvement, further research is required to identify methods to supplement successful intuitive strategies, which are difficult to teach. Nurses understand the importance of tact in engaging the client’s participation. Nursing research validates the concept that treating the client as a unique individual and actively engaging the client in problem solving are associated with increased client satisfaction, an important quality indicator ( Roberts et al, 1995). Defining the difference between problem solving and mutual problem solving in nursing Problem solving: the nursing process In Chapter 1 we identified a five-step model of the nursing process, the problem-solving process: 1. Assessment 2. Diagnosis 3. Planning 4. Implementation 5. Evaluation The mutual problem-solving process in nursing Validation Validation signifies the difference between problem solving for clients and mutual problem solving with clients. Incorporating validation keeps us focused on the rights and obligations of clients to make their own decisions about their health. The important activity of validation must be incorporated at each step of the problem-solving process in nursing. Validation means consciously seeking out our clients’ opinions and feelings at each phase of the nursing process. Validation means unearthing any questions or concerns our clients have about plans for their healthcare and securing their understanding and willingness to proceed to the next step. Incorporating validation into our problem solving stops us from moving too quickly and alienating our clients. It ensures that we obtain complete agreement and commitment from our clients about the plans for nursing care being considered for their particular health problems. A mutual problem-solving process in nursing looks like this ( Iyer et al, 1995): I Assessment A Collecting data regarding the client, client–family system, or community B Identifying needs, problems, concerns, or human responses II Diagnosis A Analyzing data B Validating the interpretation of data with the client C Identifying nursing diagnoses D Validating the nursing diagnoses with the client III Planning A Setting priorities for resolution of identified problems with the client B Determining expected and desired outcomes of nursing actions in collaboration with the client C Writing nursing interventions to achieve these outcomes in collaboration with the client IV Implementation A Implementing nursing actions with assistance from the client B Encouraging client participation in carrying out nursing actions to achieve the outcomes C Continuing to collect data about the client’s condition and interaction with the environment V Evaluation A Evaluating the outcomes of nursing care in consultation with the client B Ongoing evaluation to revise the nursing care plan Including validation in the nursing process does not necessarily increase the time or energy required to carry out nursing care. Much of the checking can be done quickly and naturally while interacting with clients. Ensuring that clients understand and agree with each step of the nursing process increases the probability that they will do their part to comply with treatment. Clients who have a clear understanding of their health problems, as well as what they and their nurses can do about them, expend less energy worrying and more energy doing something constructive. Clearly understanding their nursing diagnoses and having a say in how best to respond to them enable clients to maintain a sense of control. Validation invites the collaboration that is essential for successful client change. The trust developed from working together is likely to increase the accuracy and validity of the database and thus enrich the foundation for the rest of the nursing process. The trust growing out of mutuality provides the clients with an anchor, giving them the support they need to risk changing health behaviors. Collaboration ensures the benefits of two heads working on a health problem; this is essential because nursing cannot exist in a vacuum. We cannot strive for excellence without including the full participation of our clients. Nurse researchers report that “recognition of the client as a unique person and encouragement of active client participation in the nursing encounter are highly associated with client satisfaction, one important indicator of quality care” ( Roberts et al, 1995). “Nursing interactions characterized as task oriented and that disregard the client as an equal participant have been related to acts of resistance” by clients ( Hallberg et al, 1995). Many of today’s healthcare customers are speaking up, asking questions, seeking second opinions, demanding alternative healthcare options, and forming their own self-help groups to take action. Their assertiveness and independence reflect the true meaning of the label “client,” designating those who claim the rights and privileges of partnership in healthcare. The client contracts for services with a qualified healthcare provider. This relationship is a negotiated partnership in which the client implicitly agrees to comply with the plan they generate together. The proliferation of advanced nurse practitioners in response to the demands for cost-effective care in a managed care environment demonstrates such a partnership from a holistic perspective. Advanced nurse practitioners identify collaboration with clients and other healthcare professionals as part of their nursing philosophy ( Grando , 1998). C. Everett Koop, former U.S. surgeon general, emphasized that clear communication between clients and physicians could prevent serious medical problems. He reported results from a Louis Harris poll indicating that of 1000 clients questioned, 25% admitted a hesitancy to talk with their physicians because the physician seemed rushed or distracted or because the client was embarrassed ( Koop , 1998). Nurses can build working relationships among nurses, clients, and physicians by assisting with collaborative communication. Not all healthcare customers think of themselves as active, responsible partners in their care. Some do what healthcare professionals tell them, living out the definition of the label “patient.” The passive nature of this role creates an imbalance between the power of the nurse and that of the client. The passivity of this stance creates an inequitable relationship between nurses and others. As nurses, we can help reverse this apathy and listlessness by encouraging our clients to be partners in their own healthcare ( Cooper and Powell, 1998). This means appreciating the worth of our clients and calling on their strengths. We can transform our nursing care into a mutual problem-solving process when we invite, even request, the full participation of our partners, the clients. Earlier in this century patients were more satisfied with a system of illness care that focused on disease eradication. As the influence of science and technology on healthcare has increased, discontent has emerged, along with resentment of chauvinistic, “all-knowing,” healthcare professionals. Clients have begun demanding more influence in their healthcare and requesting more individualized care. Evidence of this movement was seen as early as 1972, with the publication of the Patient’s Bill of Rights (presented by the American Hospital Association). This document describes the expectations for respect, knowledge, privacy, and confidentiality, and access to any information essential for adequate treatment. Nurses need to focus on the individual’s responsibility for healthcare along with his or her rights. It is important to emphasize what clients can do to take care of themselves, as well as to safeguard their right to quality, informed care. The notion of clients as consumers of healthcare that arose in the 1970s has evolved into the idea of clients and their families as customers. In addition to providing informed care, nurses must now give attention to customers’ expectations of service. Decreased hospital stays, outpatient surgery, and the movement toward home healthcare make the need for problem solving even more essential because clients and their families and significant others play a more active role. Because clients are frequently discharged from the hospital before they are able to care for themselves, much client education and care must be done in the home. Clients need to be able to make informed decisions about their choices for insurance. Nurses need to be informed about the differences in the choices of providers and services covered by managed care organizations to assist clients in the selection of and in the proper procedures for reimbursement. The standards set forth in Standards of Clinical Nursing Practice by the American Nurses Association (2004)—quality of care, diagnosis, outcome identification, planning, implementation, and evaluation—provide support for a mutual problem-solving approach with clients. The following statements are taken from two of the standards of nursing practice. Standard IV: planning. Within the measurement criteria for standard IV we find: “The plan is developed with the patient, family, and health care providers, as appropriate.” This standard demands that clients, family, and significant others be kept informed about the patient’s current health status, changes in health status, total health care plan, nursing care plan, roles of healthcare personnel, and healthcare resources. Clients, family, and significant others must be provided with the information needed to make decisions and choices about promoting, maintaining, and restoring health; seeking and utilizing appropriate healthcare personnel; and maintaining and using healthcare resources. Standard VI: evaluation. Within the measurement criteria for standard VI we find: “The patient, family, and other health care providers are involved in the evaluation process, as appropriate.” Clients are an essential part of the comprehensive and intelligent determination of the impact of nursing on the patient’s health status. Clients, family, significant others, and healthcare providers evaluate nursing actions and goal achievement. Incorporation of validation into the nursing process The example given in the following subsections illustrates suggested methods for ensuring maximum client participation in a mutual problem-solving approach. Validating the interpretation of collected data. From the time clients enter our nursing care, we start asking them questions about their health problems. As we receive information about their situations from the answers they give us, the way they answer our questions, and objective data from laboratory tests and physical assessment, we start to piece together a meaningful picture. That picture is our interpretation of the data. It starts off as fuzzy and develops into a clear explanation of our clients’ health problem(s). Nurses are not the only ones who crave a clear picture of what is going on—clients are usually eager to know as well. Put yourself in the following clinical nursing situation: Mrs. Cook is 48 years old and has been referred to a home healthcare agency by her family physician to help establish control of her adult-onset diabetes. She has been on oral hypoglycemic agents for the past 2 years. Her most recent blood glucose level was 350 mg/dl. Mrs. Cook: “Oh, don’t worry about me. I’ll be fine. You won’t need to visit me. I can’t be worrying my husband. He wants a healthy wife!” As you talk, you learn that Mrs. Cook has little knowledge about what special care she must take, how to monitor her nutritional intake, how to pay careful attention to skin care, and how to check her urine daily for glucose. You learn that sickness is “unacceptable” in her family. She has two sisters who are “perfectly healthy” and a husband she calls a “fitness fanatic.” All her life Mrs. Cook has received verbal and nonverbal messages from her parents and husband that she must be a perfect wife and homemaker and that sickness is not tolerated. When the symptoms of hyperglycemia first occurred, Mrs. Cook tried to ignore them and pretend nothing was wrong. Her neighbor insisted that Mrs. Cook see a doctor when her symptoms of increased thirst and appetite were accompanied by diminished strength and weight loss. You want to share with Mrs. Cook your assessment that she appears to have little knowledge about how to manage her diabetes to prevent complications. You suspect she has never really learned much about diabetes in an attempt to be “healthy” so as to live up to her parents’ and husband’s expectations. It was easier to pretend she was healthy than to admit she had a chronic illness. You sense that she may mistakenly assume that she will not be able to live an active and full life as a diabetic. You validate this interpretation of the information with the following statements: You: “Mrs. Cook, I know you are eager to feel better, and I have some concerns about your ability to continue to feel healthy without learning more about taking care of yourself and managing your diabetes. From what you’ve told me, I know it is important to you and your husband that you be healthy. It is my experience that if people exercise proper self-care, diabetes doesn’t have to stop them from doing anything they want, but to accomplish this you must accept the fact that you have diabetes. You can do things to be healthy. Tell me what you think about that.” This validation respectfully lets your client know your assessment of her health situation. Your ending allows Mrs. Cook to argue, disagree, or ask questions about your interpretation of her situation.

Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Expressing opinions
- Spirituality
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

- Get new issue alerts Get alerts
- Submit your manuscript
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Relationship Between the Problem-Solving Skills and Empathy Skills of Operating Room Nurses
AY, Fatma 1* ; POLAT, Şehrinaz; KASHIMI, Tennur
1 PhD, RN, Assistant Professor, Faculty of Health Sciences, Department of Midwifery, Istanbul University-Cerrahpaşa, Turkey
2 PhD, RN, Directorate of Nursing Services, Hospital of Faculty of Medicine, Istanbul University, Turkey
3 MS, RN, Director, Operating Room, Hospital of Faculty of Medicine, Istanbul University, Turkey.
Accepted for publication: January 21, 2019
*Address correspondence to: Fatma AY, No.25, Dr. Tevfik Saglam Street, Dr. Zuhuratbaba District, Bakirkoy, Istanbul 34147, Turkey. Tel: +90 212 4141500 ext. 40140; Fax: +90 212 4141515; E-mail: [email protected]
The authors declare no conflicts of interest.
Cite this article as: Ay, F., Polat, Ş., & Kashimi, T. (2019). Relationship between the problem-solving skills and empathy skills of operating room nurses. The Journal of Nursing Research , 28 (2), e75. https://doi.org/10.1097/jnr.0000000000000357
This is an open access article distributed under the Creative Commons Attribution License 4.0 (CCBY) , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background
The use of empathy in problem solving and communication is a focus of nursing practice and is of great significance in raising the quality of patient care.
Purpose
The purposes of this study are to investigate the relationship between problem solving and empathy among operating room nurses and to explore the factors that relate to these two competencies.
Methods
This is a cross-sectional, descriptive study. Study data were gathered using a personal information form, the Interpersonal Problem Solving Inventory, and the Basic Empathy Scale ( N = 80). Descriptive and comparative statistics were employed to evaluate the study data.
Results
Age, marital status, and career length were not found to affect the subscale scores of cognitive empathy ( p > .05). A negative correlation was found between the subscale scores for “diffidence” and “cognitive empathy.” Moreover, the emotional empathy scores of the graduate nurses were higher than those of the master's/doctorate degree nurses to a degree that approached significance ( p = .078). Furthermore, emotional empathy levels were found to decrease as the scores for insistent/persistent approach, lack of self-confidence, and educational level increased ( p < .05). The descriptive characteristics of the participating nurses were found not to affect their problem-solving skills.
Conclusions/Implications for Practice
Problem solving is a focus of nursing practice and of great importance for raising the quality of patient care. Constructive problem-solving skills affect cognitive empathy skills. Educational level and career length were found to relate negatively and level of self-confidence was found to relate positively with level of cognitive empathy. Finally, lower empathy scores were associated with difficult working conditions in operating rooms, intense stress, and high levels of potential stress-driven conflicts between workers in work settings.
Introduction
Healthcare institutions are where individuals seek remedies to their health problems. These institutions face problems, which relate to both employees and care recipients. These problems may occur spontaneously and require immediate solution. Moreover, these problems require that the preferred remedies be adapted to address the unique nature of both organizational circumstances and individual requirements. Therefore, it is important that nurses, who are a major component of the healthcare system, have problem-solving skills.
Operating rooms are complex, high-risk environments with intense levels of stress that require rapid judgment making and fast implementation of appropriate decisions to increase patients' chances of survival ( Kanan, 2011 ; Jeon, Lakanmaa, Meretoja, & Leino-Kilpi, 2017 ). Furthermore, aseptic principles may never be compromised, and a high level of coordination and cooperation among team members should be maintained in these areas ( Kanan, 2011 ; Sandelin & Gustafsson, 2015 ). The members of a surgical team may vary in the operating room ( Sandelin & Gustafsson, 2015 ; Sonoda, Onozuka, & Hagihara, 2018 ). Under these difficult conditions, time management and workload are important stress factors for nurses ( Happell et al., 2013 ; Suresh, Matthews, & Coyne, 2013 ). At the same time, operating room nurses are legally responsible for the nature and quality of the healthcare service received by patients before, during, and after their surgical intervention ( Kanan, 2011 ). The American Nurses Association defines a nurse as “the healthcare professional establishing, coordinating and administering the care while applying the nursing process in an aim to meet the identified physiological, psychological, sociocultural and spiritual needs of patients who are potentially at the risk of jeopardized protective reflexes or self-care ability because of surgery or invasive intervention” ( Association of periOperative Registered Nurses, 2015 ).
Problem solving is the most critical aspect of the nursing practice. The fact that nursing requires mental and abstract skills, such as identifying individual needs and finding appropriate remedies, was first stated in 1960s. In 1960s, the nursing theorists Abdellah, Orem, and Levin emphasized the mental aspect of nursing. They argued that the most critical requirement of nurses in the clinical field is the ability to decide on and plan the right action and that nursing care should be founded on a sound knowledge base ( Taşci, 2005 ).
The World Health Organization has stated that “taking measures and applying a problem-solving approach to provide appropriate care is one of the compulsory competencies of nurses” ( Taşci, 2005 ). Thus, enhancing the problem-solving skills of nurses is of great importance in raising the quality of patient care ( Taylor, 2000 ; Yu & Kirk, 2008 ). On the other hand, Bagnal (1981) argued that people with problem-solving skills need to be equipped with personal traits including innovation, clear manifestation of preferences and decisions, having a sense of responsibility, flexible thinking, courage and adventurousness, ability to show distinct ideas, self-confidence, a broad area of interest, acting rationally and objectively, creativity, productivity, and critical perspective (as cited in Çam & Tümkaya, 2008 ).
To provide the best surgical care to a patient, team members must work together effectively ( Sonoda et al., 2018 ). One of the most important factors affecting the quality of healthcare service delivery is effective communication between healthcare professionals and healthcare recipients, with empathy forming the basis for effective communication.
Because of the intrinsic nature of the nursing profession, nurses should have empathy skills. Thus, empathy is the essence of the nursing profession ( Fields et al., 2004 ; Vioulac, Aubree, Massy, & Untas, 2016 ). A review of resources in the literature on problem solving reveals that gathering problem-related data is the first major step toward determining the root causes of a problem. In this respect, empathy is an important skill that helps properly identify a problem. On the basis of the definition of empathy, sensing another person's feelings and thoughts and placing oneself in his or her position or feeling from within his or her frame of reference should work to improve one's problem-solving skills, particularly those skills related to social problem solving ( Taşci, 2005 ; Topçu, Baker, & Aydin, 2010 ; Vioulac et al., 2016 ). It is possible to explain empathic content emotionally as well as cognitively. Emotional empathy (EE) means feeling the emotions of another person and providing the most appropriate response based on his or her emotional state. This is very important in patient–nurse communications. Cognitive empathy (CE) is the ability to recognize the feelings of another without experiencing those feelings yourself ( de Kemp, Overbeek, de Wied, Engels, & Scholte, 2007 ).
Gender, age, level of education, marital status, years of work, duration working at current institution, and problem-solving situations have been shown in the literature not to affect the problem-solving or empathy skills of nurses ( Abaan & Altintoprak, 2005 ; Kelleci & Gölbaşi, 2004 ; Yu & Kirk, 2008 ). Empathy is especially critical to the quality of nursing care and is an essential component of any form of caring relationship. The findings in the literature regarding empathy among nurses are inconsistent ( Yu & Kirk, 2008 ), and no findings in the literature address the relationship between problem-solving skills and empathy skills in operating room nurses.
Today, the healthcare system demands that nurses use their professional knowledge to handle patient problems and needs in flexible and creative ways. Problem solving is a primary focus of the nursing practice and is of great importance to raising the quality of patient care ( Kelleci & Gölbaşi, 2004 ; Yu & Kirk, 2008 ). Enhancing the problem-solving and empathy skills of nurses may be expected to facilitate their identification of the sources of problems encountered during the delivery of healthcare services and their resolution of these problems.
The purposes of this study are to investigate the relationship between problem solving and empathy in operating room nurses and to explore the factors related to these two competencies.
Study Model and Hypotheses
This study is a cross-sectional and descriptive study. The three hypotheses regarding the relationships between the independent variables are as follows:
- H1: Sociodemographic characteristics affect problem-solving skills.
- H2: Sociodemographic characteristics affect level of empathy.
- H3: Problem-solving skills are positively and significantly correlated with empathy.
Study Population and Sample
The study was conducted during the period of May–June 2015 at three hospitals affiliated with Istanbul University. The study population consisted of 121 nurses who were currently working in the operating rooms of these hospitals. The study sample consisted of the 80 nurses who volunteered to participate and answered all of the questions on the inventory.
Data Collection Tool
Study data were gathered using a personal information form, the Interpersonal Problem Solving Inventory (IPSI), and the Basic Empathy Scale.
Personal information form
This questionnaire, created by the researchers, is composed of 10 questions on the age, gender, educational background, organization and department, position, and organizational and professional functions of the respondent.
Interpersonal problem solving inventory
The IPSI, developed and validated by Çam and Tümkaya (2008) , was used in this study. The Cronbach's α internal consistency coefficients of the IPSI subscales were previously evaluated at between .67 and .91. The IPSI includes 50 items, all of which are scored on a 5-point Likert scale, with 1 = strictly inappropriate and 5 = fully appropriate . The lack of self-confidence (LSC) subscale assesses lack of confidence in problem solving. The constructive problem solving (CPS) subscale assesses emotions, thoughts, and behaviors that contribute to the effective and constructive solution of interpersonal problems. The negative approach to the problem subscale assesses intensely the negative emotions and thoughts such as helplessness, pessimism, and disappointment that are experienced when an interpersonal problem is encountered. The abstaining from responsibility subscale assesses failure to take responsibility for solving the problem. The persistent approach (PA) subscale assesses self-assertive/persistent thoughts and behaviors in solving problems encountered in interpersonal relationships. A high score on a subscale indicates a high interpersonal-problem-solving capability for that subscale category ( Çam & Tümkaya, 2008 ). A high score on the negative approach to the problem subscale indicates a higher likelihood of experiencing intense negative feelings and thoughts such as helplessness, pessimism, and sadness when encountering a problem. A high score on CPS indicates that the respondent will show more of the emotions, thoughts, and behaviors that contribute to the problem in an effective and constructive way. A low level of self-confidence indicates that the respondent will exhibit low self-confidence toward effectively resolving a problem. A high score on the abstaining from responsibility subscale indicates a high inclination to assume responsibility to resolve a problem ( Table 1 ). The high level of insistent approach indicates that the participant is more willing to solve problems ( Çam & Tümkaya, 2008 ). In this study, the Cronbach's α reliability coefficients were .901, .899, .763, .679, and .810, respectively.

Basic empathy skill scale
The Basic Empathy Skill Scale was developed by Jolliffe and Farrington (2006) and validated by Topçu et al. (2010) in Turkish. It is a 5-Likert scale (1 = s trictly disagree and 5 = strictly agree ) consisting of 20 items, of which nine measure CE and 11 measure EE. The Cronbach's α coefficients that were calculated for the reliability study range between .76 and .80. The lowest possible scores are 9 and 45 and the highest possible scores are 11 and 55 for the CE and EE subscales, respectively. A high score on the CE subscale indicates that the CE level is high, and a high score on the EE subscale indicates that the EE level is high ( Topçu et al., 2010 ). The two subscales of the Basic Empathy Skill Scale have been found to be highly reliable. The Cronbach's α reliability coefficients in this study were .782 for the CE subscale and .649 for the EE subscale.
Data Collection
The study was conducted between May and June 2015 at three hospitals affiliated with Istanbul University. The researcher explained the study to those nurses who agreed to participate. The questionnaire form was distributed to the participants, the purpose of the investigation was clarified, and permission to use participant data was obtained. The participants completed the questionnaire on their own, and the completed questionnaires were collected afterward. The time required to complete the questionnaire was 15–20 minutes in total.
Evaluation of Data
Number Cruncher Statistical System 2007 (Kaysville, UT, USA) software was used to perform statistical analysis. To compare the quantitative data, in addition to using descriptive statistical methods (mean, standard deviation, median, frequency, ratio, minimum, maximum), the Student t test was used to compare the parameters with the regular distribution in the two groups and the Mann–Whitney U test was used to compare the parameters without normal distribution in the two groups. In addition, a one-way analysis of variance test was used to compare three or more groups with normal distribution, and a Kruskal–Wallis test was used to compare three or more groups without normal distribution. Pearson's correlation analysis and Spearman's correlation analysis were used to evaluate the relationships among the parameters. Finally, linear regression analysis was employed to evaluate multivariate data. Significance was determined by a p value of < .05.
Ethical Considerations
Ethical conformity approval was obtained from the Non-Interventional Clinical Research Ethics Board at Istanbul Medipol University (108400987-165, issued on March 30, 2015). Written consent was obtained from the administrations of the participating hospitals. Furthermore, the informed consent of nurses who volunteered to participate was obtained. Permission to use the abovementioned scales that were used in this study as data collection tools was obtained via e-mail from their original authors.
Eighty nurses (97.5% female, n = 78; 2.5% male, n = 2) were enrolled as participants. The age of participants ranged between 24 and 64 (mean = 37.56 ± 8.12) years, mean years of professional nursing experience was 15.84 ± 8.30, and mean years working in the current hospital was 13.19 ± 8.23. Other descriptive characteristics for the participants are provided in Table 2 .

A comparison of scale subdimension scores revealed a negative and statistically significant correlation at a level of 22.3%. Statistical significance was reached only between the LSC subscale and the CE subscale ( r = −.223, p = .047; Table 3 ). Thus, a higher LSC score was associated with a lower CE score.

Comparisons between participants' descriptive characteristics and subdimension scores on the problem-solving skill scale revealed no significant differences. Thus, demographic characteristics such as age, educational background, and career length were found to have no influence on problem-solving skills ( p > .05; Table 4 ).

Age, marital status, and professional career length were not found to affect the CE and EE subscale scores, with no statistically significant correlations found between the two subscales ( p > .05; Table 4 ). However, the EE scores of undergraduate nurses were found to be higher than those of postgraduate nurses, at a level that approached statistical significance ( p = .078). In addition, the average CE scores of nurses who had worked for 1–10 and 11–20 years were higher than those of nurses who had worked for 21 years or more, at a level that approached statistical significance ( p = .066).
A statistically significant difference was found between mean years working in the current hospital and educational background, respectively, and CE scores ( p = .027 and p = .013; Table 4 ). On the basis of paired comparison analysis, the CE scores of participants with 1–10 years of working experience at their current hospital were higher than those with ≥ 21 years of working experience at their current hospital ( p = .027). Also on the basis of paired comparison analysis, the CE score of participants educated to the undergraduate level was found to be higher at a statistically significant level than those educated to the master's/doctorate degree level ( p = .013).
The comparison of problem-solving skill scores by descriptive characteristics revealed no statistically significant difference between subscale scores and the variables of age, marital status, length of professional and organizational career, or educational background ( p > .05). Thus, the descriptive characteristics of the participants did not affect their problem-solving skills.
Regression Analysis of Risk Factors Affecting Cognitive and Empathy Skills
Variables found after univariate analysis to have significance levels of p < .01 were subsequently modeled and evaluated. A regression analysis was conducted to determine the effect on CE skills of educational level, duration of institutional work, CPS level, and self-insecurity level. The explanatory power of this model was 29.9% ( R 2 = .299), and the model was significant ( p < .001). As a result of the analysis, CPS ( p = .006), educational status of graduate ( p < .001), and working for the current hospital for a period of more than 20 years ( p = .004) were found to have a significant and positive influence on the CE score.
A 1-unit increase in the CPS score was found to increase CE skills by 0.139 points (β = 0.139, 95% CI [0.041, 0.237], p < .01). For education, graduate education was found to decrease the CE score by 4.520 points (β = −4.520, 95% CI [−6.986, −2.054], p < .001). For duration working for the current hospital, working for the same institution for a period exceeding 20 years was found to decrease the CE score by 3.429 points (β = −3.429, 95% CI [−5.756, −1.102], p < .05). In addition, a 1-unit increase in the LSC score was found to decrease the CE score by 0.114 points, which did not achieve statistical significance (β = 0.114, 95% CI [−0.325, 0.096], p > .05).
Regression analysis was used to evaluate the effects of education, PA, and LSC on the risk factors affecting EE. As a result of this evaluation, the explanatory power of the model was determined as 15.3% ( R 2 = .153), which was significant despite the low level ( F = 3.388, p = .001). The effects of PA ( p = .021) and educational status ( p = .015) on the EE score were shown through analysis to be statistically significant ( Table 5 ). A 1-unit increase in PA score was found to increase the EE score by 0.323 points (β = 0.323, 95% CI [0.049, 0.596], p < .05). For education, having a graduate education was found to decrease the EE score by 3.989 points (β = −3.989, 95% CI [−7.193, −0.786], p < .05). Moreover, the LSC score was found to be 0.119 points lower than the EE score. However, this result was not statistically significant (β = −0.193, 95% CI [−0.467, 0.080], p > .05). Dummy variables were used in the regression analysis of sociodemographic characteristics (educational status and years working for the current hospital).

This study found that age, marital status, educational background, years of professional working experience, and years working for the current hospital did not affect the problem-solving skills of the participants. In the literature, the findings of several studies indicate that characteristics such as age, educational background, department of service, and career length do not affect the problem-solving skills of nurses ( Abaan & Altintoprak, 2005 ; Kelleci & Gölbaşi, 2004 ; Yu & Kirk, 2008 ), whereas other studies indicate that these variables do affect these skills ( Ançel, 2006 ; Watt-Watson, Garfinkel, Gallop, Stevens, & Streiner, 2000 ; Yu & Kirk, 2008 ). However, beyond these characteristics, some studies have reported a positive correlation between the problem-solving skills of nurses and their educational level, with this correlation mediated by the physical conditions of the workplace, good relationships with colleagues, and educational background ( Yildiz & Güven, 2009 ). These findings suggest that factors affecting the empathy and problem-solving skills of nurses working in operating rooms differ from known and expected factors.
Operating room nurses deliver dynamic nursing care that requires attention and close observation because of the fast turnover of patients. In addition to the problem-solving skills that they use during the patient care process, these nurses must use or operate a myriad of lifesaving technological devices and equipment ( AbuAlRub, 2004 ; Özgür, Yildirim, & Aktaş, 2008 ). The circumstances in which nurses employ their problem-solving skills are generally near-death critical conditions and emergencies. Furthermore, operating rooms are more isolated than other areas of the hospital, which affects nurses who work in operating rooms and intensive care units ( AbuAlRub, 2004 ; Özgür et al., 2008 ).
Communication is a critical factor that affects the delivery of healthcare services. Communication does not only take place between a service recipient and a provider. To establish a teamwork philosophy between employees, it is essential to build effective communication ( Sandelin & Gustafsson, 2015 ). Empathic communication helps enhance the problem-solving skills of nurses as they work to learn about individual experiences ( Kumcağiz, Yilmaz, Çelik, & Avci, 2011 ). Studies in the literature have found that nurses who are satisfied with their relationships with colleagues, physicians, and supervisors have a high level of problem-solving skills ( Abaan & Altintoprak, 2005 ; Kumcağiz et al., 2011 ) and that higher problem-solving skills are associated with a higher level of individual achievement ( Abaan & Altintoprak, 2005 ; Chan, 2001 ). Another finding of this study is that CPS increases the cognitive emphatic level. This may be attributed to constructive problem-solving skills increasing CE, as these skills are associated with feelings, thoughts, and behaviors that contribute to problem resolution.
A review of the literature on empathy and communication skills revealed, as expected, that these skills increased with level of education ( Kumcağiz et al., 2011 ; Vioulac et al., 2016 ). However, a number of studies have reported no significant correlation between age, marital status, and professional working experience and empathy skills or communication abilities in nurses ( Kumcağiz et al., 2011 ; Yu & Kirk, 2008 ).
EE is assumed to be a more intuitive reaction to emotions. Factors that affect EE are nurses working with small patient groups, frequent contact with patient groups, and long periods spent accompanying or being in close contact with patient groups ( Vioulac et al., 2016 ). Studies in the literature have reported no correlation between the empathy skills of nurses and demographic characteristics ( Vioulac et al., 2016 ). This study supports this finding, with the empathy skills of operating room nurses found to be close to the peak value of the scale.
Studies in the literature reveal a positive correlation between empathy and career length ( Watt-Watson et al., 2000 ; Yu & Kirk, 2008 ) as well as a correlation between increased professional experience and lower empathy ( Yu & Kirk, 2008 ). This study found an association between longer periods working for the same hospital and higher levels of education with lower empathy scores. This may be attributed to the difficult working conditions in operating rooms, intense stress, and high level of potential stress-driven conflicts between employees in work settings.
Stress is a major factor that affects the empathy skills and relationship-building abilities of nurses ( Vioulac et al., 2016 ). Nurses are exposed to a wide variety of stressors such as quality of the service, duration of shifts, workload, time pressures, and limited decision-making authority ( Patrick & Lavery, 2007 ; Shimizutani et al., 2008 ; Vioulac et al., 2016 ). In particular, environments evoking a sense of death (e.g., operating rooms) is another factor known to elevate perceived stress ( Ashker, Penprase, & Salman, 2012 ). High stress may lead to negative consequences such as reduced problem-solving abilities ( Zhao, Lei, He, Gu, & Li, 2015 ). Both having a long nursing career and working in stressful environments such as operating rooms may negatively affect empathy and problem-solving skills. However, this study revealed that working for a long period at the current hospital had no influence on problem-solving skills. The low reliability of the scales means that the variance may be high in other samples that are drawn from the same main sample, with the resultant data thus not reflecting the truth.
Low reliability coefficients reduce the significance and value of the results obtained by increasing the standard error of the data ( Şencan, 2005 ). The Cronbach's α of the EE scale used in the study was between .60 and .80 and is highly trustworthy. However, the Cronbach's α value is close to .60 (i.e., .649). This result may elicit suspicion in regression analysis estimates that are done to determine the variables that affect EE. In the correlation analysis, a statistically significant weak correlation was found only between the LSC subdimension and CE. However, the fact that the subscales of empathy and problem-solving skills are significantly related to the regression models may also be related to the reliability levels of the scales.
According to the results of the regression analysis, all of the variables remaining in Model A affected level of low for the CE ( R 2 = .299). Having constructive problem-solving skills ( p = .006), having a high level of education ( p < .001), and working for the current hospital for over 20 years ( p = .004) were found to be significantly related to CE.
Other variables were found to have no significant effect. According to the results of the regression analysis, all of the remaining variables in Model B accounted for a relatively low portion of the EE ( R 2 = .153). When the t test results for the significance of the regression coefficients were examined, it was determined that PA ( p = .021) and educational status ( p = .015) were significant predictors of EE. Other variables had no significant effect ( Table 5 ). The increase in the level of education of nurses may have increased their cognitive and emotional development. Thus, working in the same hospital for over 20 years was found to increase the levels of CE and EE. This result may be because of greater professional experience and regular experience handling numerous, different problems. In addition, the low explanatory power of the models may also be because of the fact that many other arguments that may affect empathy were not modeled. When constant values are fixed and the value of the independent variables entering the regression formula is zero, constant value is the estimated value of the dependent variable. According to findings of this study, sociodemographic characteristics and problem-solving abilities did not affect empathy level, although the CE value was 31.707 and the EE value was 37.024. Repeating this research in larger and different nurse groups may be useful to verify these research results.
Conclusions
The following results were derived from this study: First, constructive problem-solving skills affect CE skills. EE is adversely affected by the PA and LSC. Second, no correlation was found between the demographic characteristics of nurses and their problem-solving skills. Third, as level of education increases, cognitive and emotional levels of empathy decrease.
Duration of time spent working at one's current healthcare institution and educational level were both found to correlate negatively with the CE score. The higher the educational level and PA and the lower the self-confidence of the participants, the lower their EE levels. Finally, higher constructive problem-solving scores were associated with higher CE skills.
Limitations
The major limitation of the study is that it was conducted in the affiliated hospitals of one healthcare organization. The study data were obtained from operating room nurses who currently worked in these hospitals and who volunteered to participate. The conditions of nurses who did not participate in the study cannot be ascertained. A second important limitation is that the data reflect the subjective perceptions and statements of the participants. A third important limitation is that participant characteristics such as trust in management, trust in the institution, burnout, and communication skills were not assessed. For this reason, the effects of these variables on problem-solving and empathy skills remain unknown.
Author Contributions
Study conception and design: SP
Data collection: TK
Data analysis and interpretation: FA, SP
Drafting of the article: FA
Critical revision of the article: FA
- Cited Here |
- Google Scholar
operating room; critical thinking; surgery; cognitive; emotional
- + Favorites
- View in Gallery
Readers Of this Article Also Read
Effectiveness of a patient safety incident disclosure education program: a..., the relationship between critical thinking skills and learning styles and....
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Healthcare (Basel)

Factors Influencing Problem-Solving Competence of Nursing Students: A Cross-Sectional Study
Eunhee choi.
1 Department of Nursing, Korean Bible University, 32 Dongil-ro(st) 214-gil, Nowon-gu, Seoul 01757, Korea; moc.revan@1029iohci
Jaehee Jeon
2 Department of Nursing, Gangneung-Wonju National University, Gangneung-si 26403, Korea
Associated Data
Not applicable.
Problem-solving ability is an important competency for nursing students to enable them to solve various problems that occur in dynamic clinical settings. The purpose of this cross-sectional study was to identify the factors that affect the problem-solving ability of nursing students. The subjects of this study were 192 nursing college students in their second year or beyond. The research tool consisted of an online questionnaire, with a total of 91 items regarding general characteristics, metacognition, and communication competence. Data collection was conducted from 10 to 30 March 2022. An online survey link was uploaded to the student group of a social network service from two nursing colleges that permitted data collection. Subjects who agreed to participate directly accessed and responded to the online survey. The collected data were analyzed using descriptive statistics, and the factors associated with the problem-solving ability of nursing students were examined using hierarchical multiple regression analysis. The subjects’ mean problem-solving ability score was 3.63 out of 5. Factors affecting problem-solving ability were age, communication competence, and metacognition, among which metacognition had the greatest influence. These variables explained 51.2% of the problem-solving ability of nursing students. Thus, it is necessary to provide guidance to improve metacognition and to develop educational methods to improve communication competence in curricular and non-curricular courses to improve the problem-solving ability of nursing students.
1. Introduction
Nurses must have the ability to develop individual problem-solving methods to satisfy their patients’ diverse and high-level health needs [ 1 ]. However, the medical field is characterized by uncertainty, instability, and unpredictability; thus, it is not easy for nurses to apply or utilize the knowledge learned within controlled situations in schools, and therefore, it is often difficult for nurses to address the health needs of patients [ 2 ]. The problem-solving ability required in such situations is an essential skill that college students majoring in nursing must have in order to effectively perform their assigned nursing tasks after graduation, while successfully adapting in order to practice in a rapidly changing medical field [ 3 ]. Therefore, strategies to improve the problem-solving ability of nursing students should be applied in their education.
This study aimed to examine the relationship between metacognition, communication competency, and the problem-solving ability of nursing students, and to identify factors that affect nursing students’ problem-solving ability. The results represent basic data that could help inform the development of educational strategies to improve the communication skills of nursing students.
Problem solving involves recognizing the difference between the problem solver’s current state and the goal state to be reached, and resolving the obstacles that prevent them from achieving the goal [ 4 ]. Acquiring problem-solving ability based on judgment and critical thinking is an important element of nursing education [ 5 ]. Furthermore, the use of effective problem-solving strategies based on professional knowledge is a competency that a professional nurse should possess [ 3 ].
Recently, metacognition has been recognized in psychology and pedagogy as a central element of the understanding, self-learning, communication, and problem-solving processes. Metacognition is the ability to think about one’s own thinking [ 6 ], as expressed by the individual knowing and controlling their thought processes and applying previously acquired knowledge, skills, and experiences using appropriate strategies [ 7 ]. In particular, metacognition is an important variable for learning and problem-solving. It is the knowledge related to the selection of an appropriate strategy for the task; the establishment, selection, and application of problem-solving measures; evaluation of the effectiveness of the applied measures; and checking and adjusting the performance process [ 6 , 7 ]. Accordingly, interest in metacognition is increasing in the field of nursing, with emphasis on the problem-solving ability of nursing students [ 8 ].
Metacognition affects problem solving by cultivating the learner’s active attitude, linking existing knowledge with new knowledge, and fostering the development of practical cognitive strategies that can be used for problem solving [ 7 ]. Previous studies on learners’ metacognition have observed that a higher level of metacognition leads to an improvement in the problem-solving process, as metacognition has a significant effect on goal setting and problem-solving performance [ 9 ]. Thus, metacognition and problem-solving ability are closely related; furthermore, metacognition is a key strategic aspect in the problem-solving process [ 10 ]. Although metacognition is a powerful predictor of learning outcomes and problem-solving success, it is not clear how metacognition works regarding cognitive strategies and learning outcomes [ 11 ]. A study of adolescent metacognition-related cognition (learning strategies and problem-solving strategies) and how metacognition affects various types of learning performance confirmed that problem solving is the only mediator between general metacognition and learning performance [ 11 ]. Metacognition plays a major role in improving learning and work ability, and the appropriate use of metacognition when performing nursing tasks can improve the personal lives of nurses [ 12 ]. Therefore, it is necessary to assess the influence of metacognition and problem-solving ability on nursing education.
Communication competence is a major factor that affects problem-solving ability [ 13 ]. It is essential for smoothly maintaining professional relationships with medical personnel, patients, and guardians in diverse and complex medical environments [ 14 ]. Since communication competence is an important aspect of problem solving, it can affect the quality of nursing and the satisfaction of the patient [ 15 ]. There is an urgent need to improve communication competence, as various issues that arise during the clinical process can be solved through communication between medical staff and patients, and nurses are responsible for much of the continuous communication with patients and their guardians [ 16 ]. However, a lack of communication competence among nurses may lead to miscommunication, and thereby, poor outcomes, even if nurses possess good problem-solving methods [ 13 ].
While previous studies have revealed the relationship between communication competence and the problem-solving ability of nursing students [ 13 , 17 ], there is a lack of research regarding the relationship between metacognition, communication competence, and problem-solving ability. Through this research, we confirmed the relationship between the metacognition and problem-solving ability of nursing college students, the relationship between communication ability and problem-solving ability, and finally, examined the factors that affect variables associated with problem-solving ability, including metacognition.
2. Materials and Methods
2.1. design.
This study used quantitative methods to investigate the relationship between the metacognition, communication ability, and problem-solving ability of nursing students and to identify factors that affect problem-solving ability.
2.2. Participants and Procedures
The subjects of this study were nursing students enrolled in two nursing colleges in the same city and region. Since data collection was conducted in March, second-year, third-year, and fourth-year students, with college life experience, were targeted. The required number of study subjects was calculated using the G-Power 3.1.9.7 program, which determined a significance level of 0.05, an effect size of 0.15, a power of 0.90, and 11 predictors, for multiple regression analysis. The minimum sample size was 152. In consideration of the dropout rate, 170 was set as the target number of subjects.
Data collection was conducted from 10 to 30 March 2022. The survey was conducted online. Consent for participation in the study was obtained by the individual reading the explanation of the purpose of the study and checking a consent box, which was displayed on the first screen of the online survey. The study subjects were redirected to the questionnaire completion page after providing their consent. It required approximately 10 min to complete the questionnaire. A total of 200 participants accessed and completed the questionnaire; 192 questionnaires were used for analysis after excluding 8 questionnaires that were determined to have been completedinccurately.
2.3. Instruments
The tools of this study consisted of a total of 91 items, including 9 items regarding general characteristics, 20 metacognition items, 15 items dealing with communication competencies, and 45 regarding problem-solving skills.
The items regarding the general characteristics of the subjects included age, sex, academic level, interpersonal relationships, satisfaction with major, problem based learning (PBL) experience, number of related experiences, clinical practice experience (yes or no), and number of weeks of clinical practice experience.
Metacognition was assessed using the state metacognitive inventory developed by O’Neil Jr et al. [ 18 ], as modified and supplemented by Joo [ 19 ]. It consists of a total of 20 items that assess the four sub-factors of metacognition: cognition, cognitive strategy, plan, and monitoring, using a 5-point Likert scale ranging from 1 point, for ‘not at all’, to 5 points, for ‘strongly agree’. The Cronbach’s α measure of the reliability of the tool was 0.86 at the time of development and 0.89 in the study of Joo [ 19 ]. The value in the current study was 0.91.
Communication competence was measured using a comprehensive interpersonal communication competence scale developed by Rubin [ 20 ], as modified and supplemented by Hur [ 21 ] to fit Korean culture. This tool consists of 15 items related to communication, such as self-exposure, cross-exposure, social tension relief, assertiveness, and concentration. Each item is assessed on a 5-point Likert scale ranging from 1 point, for ‘not at all’, to 5 points, for ‘strongly agree’. The Cronbach’ α reliability measure at the time of development was 0.72, and the value in this study was 0.84.
Problem-solving ability was assessed via a life-skills measurement tool developed by the Korea Educational Development Institute [ 22 ]. This tool considers 5 problem factors (clarification, cause analysis, alternative development, plan and implementation, and performance evaluation) and 9 sub-factors (problem recognition, information collection, analysis ability, divergent thinking, decision making, planning ability, execution and risk taking, evaluation, and feedback), and thus consists of 45 items in total. Each item is assessed on a 5-point Likert scale ranging from 1 point, for ‘very rarely’, to 5 points, for ‘very often’, with higher scores indicating better problem-solving skills. The reliability at the time of tool development was indicated by a Cronbach’s α value of 0.95, whereas in this study, the Cronbach’s α value was 0.90.
2.4. Statistical Analysis
Statistical analyses were performed using SPSS (ver. 25) statistical software (IBM). The subjects’ general characteristics, metacognition, communication competence, and problem-solving ability were analyzed by number and percentage, as well as mean and standard deviation. To test the normality of all variables, skewness and kurtosis were assessed. In general, when the absolute value of skewness is less than 2 or the absolute value of kurtosis is less than 7, there are no problems associated with deviations in the variable distributions from normality [ 23 ]. In this study, skewness ranged between −0.002 and 0.435, with absolute values less than 2, and kurtosis ranged between −0.204 to 1.580, with absolute values less than 7, thus indicating that the variables satisfied the assumption of univariate normality. Differences in metacognition, communication competence, and problem-solving ability according to the general characteristics of the subjects were analyzed by mean, standard deviation, independent t-test, and one-way ANOVA, followed by Scheffé’s post hoc analysis. The correlation between metacognition, communication competence, and problem-solving ability of the participants was analyzed using Pearson’s correlation coefficient. Factors affecting the subject’s problem-solving ability were analyzed using hierarchical multiple regression.
2.5. Ethical Considerations
Before the study was conducted, the research proposal and questionnaire were approved by the Institutional Review Board of Gangneung–Wonju National University (No: GWNUIRB-2022-1). The tools used in the study were used after obtaining the consent of the original author. When explaining the purpose of the study, it was emphasized that the participants had the right to withdraw from the study at any time, that the anonymity and confidentiality of the survey results were guaranteed, and that the study results would not be used for other purposes. Participants were provided with a small gift to motivate participation.
3.1. General Characteristics
Table 1 illustrates that the participants’ mean age was 21.56 ± 1.99. Most participants were women (81.3%).
General Characteristics of Participants (N = 192).
| Variable | Categories | N | % |
|---|---|---|---|
| Sex | Male | 36 | 18.7 |
| Female | 156 | 81.3 | |
| Age (years) | <21 | 62 | 32.3 |
| 21~<23 | 84 | 43.8 | |
| ≥23 | 46 | 24.0 | |
| Mean ± SD | 21.56 ± 1.99 | ||
| Academic level | Sophomore | 63 | 32.8 |
| Junior | 64 | 33.3 | |
| Senior | 65 | 33.9 | |
| Interpersonal relationships | Very good | 29 | 15.1 |
| Good | 118 | 61.5 | |
| Moderate | 45 | 23.4 | |
| Satisfaction with major | Very satisfied | 30 | 15.6 |
| Satisfied | 100 | 52.1 | |
| Moderately satisfied | 47 | 24.5 | |
| Dissatisfied | 15 | 7.8 | |
| PBL experience | Yes | 130 | 68.2 |
| No | 62 | 31.8 | |
| Number of PBL experiences | 0 | 62 | 32.3 |
| 1~2 | 29 | 15.1 | |
| 3~6 | 55 | 28.6 | |
| ≥7 | 46 | 24.0 | |
| Clinical practice experience | Yes | 104 | 50.2 |
| No | 88 | 46.8 | |
| Weeks of clinical practice experience | 0 | 88 | 45.9 |
| 1~6 | 54 | 28.1 | |
| ≥7 | 50 | 26.0 |
† SD, standard deviation; ‡ PBL, problem-based learning.
3.2. Scores for Metacognition, Communication Competence, and Problem-Solving Ability
Table 2 illustrates that the average score of the subjects’ metacognition was 3.86 ± 0.47 (out of 5). Among the sub-domains, cognitive strategy showed the highest score of 4.03 ± 0.45, followed by monitoring, with 3.90 ± 0.59. The average for communication competence was 3.92 ± 0.42 points (out of 5 points). The average for problem-solving ability was 3.63 ± 0.35 (out of 5), and among the sub-domains, problem clarification was the highest at 3.83 ± 0.52, and cause analysis was the lowest at 3.28 ± 0.36.
Scores for metacognition, communication competence, and problem-solving ability. (N = 192).
| Variables | Categories | M ± SD | Range | Min | Max | Skewness | Kurtosis |
|---|---|---|---|---|---|---|---|
| Cognition | 3.87 ± 0.54 | 1–5 | 2.00 | 5.00 | −0.405 | 0.616 | |
| Cognitive strategy | 4.03 ± 0.45 | 1–5 | 2.80 | 5.00 | −0.002 | −0.204 | |
| Planning | 3.66 ± 0.59 | 1–5 | 2.00 | 5.00 | −0.234 | 0.449 | |
| Monitoring | 3.90 ± 0.59 | 1–5 | 2.20 | 5.00 | −0.366 | 0.364 | |
| 3.86 ± 0.47 | 1–5 | 2.35 | 5.00 | −0.214 | 0.607 | ||
| 3.92 ± 0.42 | 1–5 | 2.60 | 4.93 | 0.025 | 0.582 | ||
| Problem clarification | 3.83 ± 0.52 | 1–5 | 1.80 | 5.00 | −0.508 | 1.288 | |
| Cause analysis | 3.28 ± 0.36 | 1–5 | 2.50 | 5.00 | 0.435 | 1.171 | |
| Alternative development | 3.64 ± 0.47 | 1–5 | 2.20 | 5.00 | 0.285 | 0.989 | |
| Planning/implementation | 3.63 ± 0.51 | 1–5 | 1.50 | 5.00 | −0.203 | 1.580 | |
| Performance evaluation | 3.65 ± 0.39 | 1–5 | 2.60 | 5.00 | 0.351 | 1.205 | |
| 3.63 ± 0.35 | 1–5 | 2.53 | 4.64 | 0.243 | 1.253 | ||
3.3. Differences in Problem-Solving Ability According to General Characteristics
The problem-solving ability according to the general characteristics of the subjects was as follows ( Table 3 ): age (F = 4.32, p = 0.015), academic level (F = 10.17, p < 0.001), interpersonal relationships (F = 9.47, p < 0.001), satisfaction with major (F = 3.73, p = 0.012), PBL experience (F = 3.73, p = 0.012), number of PBL experiences (F = 3.20, p = 0.025), and practical experience (F = 2.74, p = 0.007). There was a significant difference in problem-solving ability accorfing to the number of training weeks (F = 4.46, p = 0.013). Scheffé’s post hoc analysis indicated that participants older than 23 years old and younger than 20 years old, as well as fourth-year students, were more dissatisfied than were second-year students. In other cases, interpersonal relationships were very good. Additionally, satisfaction with the major was more than satisfactory. Problem-solving ability was statistically significantly higher for those with more than 7 weeks of practice, and there was no case of not having more than 7 weeks of practice.
Differences in metacognition, communication competence, and problem-solving ability according to nursing students’ general characteristics (N = 192).
| M ± SD | t/F( ) | M ± SD | t/F( ) | M ± SD | t/F( ) | ||
| Age (years) | <21 | 3.75 ± 0.48 | 2.83 (0.061) | 3.87 ± 0.38 | 0.84 (0.433) | 3.54 ± 0.32 | 4.32 (0.015) a < c |
| 21–<23 | 3.92 ± 0.47 | 3.95 ± 0.42 | 3.64 ± 0.37 | ||||
| ≥23 | 3.92 ± 0.44 | 3.96 ± 0.47 | 3.73 ± 0.31 | ||||
| Sex | Male | 3.92 ± 0.42 | 0.68 (0.409) | 3.95 ± 0.41 | 0.30 (0.584) | 3.70 ± 0.35 | 1.81 (0.181) |
| Female | 3.85 ± 0.49 | 3.92 ± 0.42 | 3.61 ± 0.34 | ||||
| Academic level | Sophomore | 3.72 ± 0.59 | 5.59 (0.004) a < c | 3.80 ± 0.43 | 4.58 (0.011) a < c | 3.51 ± 0.29 | 10.17 (<0.001) a < c |
| Junior | 3.89 ± 0.47 | 3.96 ± 0.35 | 3.60 ± 0.32 | ||||
| Senior | 3.99 ± 0.45 | 4.01 ± 0.44 | 3.77 ± 0.37 | ||||
| Interpersonal relationships | Very good | 4.07 ± 0.54 | 5.79 (0.004) a > c | 4.38 ± 0.40 | 40.71 (<0.001) c < b < a | 3.78 ± 0.48 | 9.47 (<0.001) b, c < a |
| Good | 3.88 ± 0.44 | 3.92 ± 0.32 | 3.66 ± 0.29 | ||||
| Moderate | 3.70 ± 0.48 | 3.63 ± 0.39 | 3.46 ± 0.33 | ||||
| Satisfaction with major | Very satisfied | 4.09 ± 0.43 | 7.21 (<0.001) d < b, c < a | 4.19 ± 0.48 | 7.70 (<0.001) c, d < a | 3.76 ± 0.38 | 3.73 (0.012) d < a, b |
| Satisfied | 3.92 ± 0.45 | 3.94 ± 0.38 | 3.66 ± 0.33 | ||||
| Moderately satisfied | 3.71 ± 0.50 | 3.77 ± 0.40 | 3.53 ± 0.35 | ||||
| Dissatisfied | 3.55 ± 0.37 | 3.77 ± 0.31 | 3.52 ± 0.23 | ||||
| PBL experience | Yes | 3.93 ± 0.47 | 2.92 (0.004) | 3.98 ± 0.40 | 2.74 (0.007) | 3.68 ± 0.36 | 3.06 (0.003) |
| No | 3.72 ± 0.47 | 3.81 ± 0.43 | 3.52 ± 0.28 | ||||
| Number of PBL experiences | 0 | 3.72 ± 0.47 | 2.87 (0.038) | 3.81 ± 0.43 | 2.47 (0.063) | 3.52 ± 0.28 | 3.20 (0.025) |
| 1~2 | 3.92 ± 0.51 | 3.97 ± 0.47 | 3.66 ± 0.42 | ||||
| 3~6 | 3.95 ± 0.47 | 3.98 ± 0.38 | 3.70 ± 0.36 | ||||
| ≥7 | 3.91 ± 0.44 | 3.98 ± 0.38 | 3.68 ± 0.32 | ||||
| Clinical practice experience | Yes | 3.93 ± 0.42 | 2.40 (0.019) | 3.97 ± 0.38 | 1.58 (0.115) | 3.69 ± 0.32 | 2.74 (0.007) |
| No | 3.78 ± 0.52 | 3.91 ± 0.44 | 3.56 ± 0.36 | ||||
| Weeks of clinical practice experience | 0 | 3.78 ± 0.52 | 3.02 (0.051) | 3.87 ± 0.46 | 1.58 (0.208) | 3.56 ± 0.36 | 4.46 (0.013) a < c |
| 1~6 | 3.96 ± 0.40 | 3.93 ± 0.35 | 3.66 ± 0.29 | ||||
| ≥7 | 3.91 ± 0.44 | 4.00 ± 0.41 | 3.73 ± 0.35 | ||||
† Scheffé test; ‡ PBL, problem based learning.
3.4. Relationship beetween Metacognition, Communication Competence, and Problem-Solving Ability
There was a strong, significantly positive correlation between metacognition and problem-solving ability (r = 0.672, p < 0.001), and communication competence and problem-solving ability (r = 0.542, p < 0.001). There was also a strong, significantly positive correlation between metacognition and communication competence (r = 0.557, p < 0.001; Table 4 ).
Relationships between metacognition, communication competence, and problem-solving ability (N = 192).
| Variables | Metacognition | Communication Competence | Problem-Solving Ability |
|---|---|---|---|
| r ( ) | r ( ) | r ( ) | |
| Metacognition | 1 | ||
| Communication competence | 0.557 (<0.001) | 1 | |
| Problem-solving ability | 0.672 (<0.001) | 0.542 (<0.001) | 1 |
3.5. Factors Influencing Problem-Solving Ability
Among general characteristics, variables were converted into dummy variables as needed to confirm their effect on the problem-solving ability of nursing students (e.g., age, 23 years or older = 1; academic level, third year = 1; interpersonal relationships, very good = 1; satisfaction with major, more than satisfied = 1; the number of PBL experiences, 3–6 times = 1; and the number of training weeks, 7 weeks or more = 1). A hierarchical stepwise multiple regression analysis was then performed, inputting communication ability followed by metacognition, which were significantly correlated.
The Durbin–Watson value was 1.96 (close to 2), which confirmed that there was no autocorrelation between the independent variables. The variance inflation factor was 1.013 to 4.999; as all value were less than 10, there were no problems with multicollinearity between independent variables.
General characteristics that showed a significant difference with problem-solving ability in univariate analyses were first input to Model 1, namely age, academic level, interpersonal relationships, and satisfaction with major. This model explained 8.1% of the variance in problem-solving ability. When PBL experience and frequency, clinical practice, and number of weeks were added to Model 1 (Model 2), the variance explained was 12.5%, namely an increased of 4.4% compared to Model 1. When communication competence and metacognition were additionally added to Model 2 (Model 3), the variance explained was 51.2%, which is an increase of 38.7% compared to Model 2. Finally, age (β = 0.11, p = 0.048), communication competence (β = 0.24, p = 0.001), and metacognition (β = 0.52, p = 0.023) were significantly related to problem-solving ability. These variables exhibited an explanatory power of 51.2% (F = 21.01, p < 0.001) regarding job satisfaction; the most influential variable was metacognition ( Table 5 ).
Factors influencing problem-solving ability (N = 192).
| Variables | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | β | t | B | β | t | B | β | t | |
| Age (R = ≥23) | 0.13 | 0.16 | 2.29 * | 0.10 | 0.13 | 1.77 | 0.09 | 0.11 | 1.99 * |
| Academic level (R = Junior) | −0.06 | −0.09 | −1.22 | −0.23 | −0.31 | −2.71 * | −0.12 | −0.17 | 1.91 |
| Interpersonal relationships (R = Very good) | 0.16 | 0.17 | 2.41 * | 0.14 | 0.15 | 2.11 * | −0.19 | −0.02 | −0.33 |
| Satisfaction with major (R = Satisfied) | 0.13 | 0.17 | 2.40 * | 0.11 | 0.15 | 2.10 * | −0.01 | −0.02 | −0.35 |
| PBL experience | −0.25 | −0.34 | −2.25 * | −0.09 | −0.11 | −1.01 | |||
| Number of PBL experiences (R = 3–6) | 0.14 | 0.19 | 1.66 | 0.14 | 0.18 | 2.13 * | |||
| Clinical practice experience | 0.11 | 0.16 | 1.16 | 0.11 | 0.16 | 1.16 | |||
| Weeks of clinical practice experience (R = ≥7) | −0.00 | −0.004 | −0.03 | 0.09 | 0.12 | −0.03 | |||
| Communication competence | 0.19 | 0.24 | 3.42 * | ||||||
| Metacognition | 0.38 | 0.52 | 8.22 * | ||||||
| Adj R = 0.081, F = 5.20, = 0.001 | Adj R = 0.125, F = 4.42, < 0.001 | Adj R = 0.512, F = 21.01, < 0.001 | |||||||
† Dummy variables; ‡ Reference; ¶ PBL, problem-based learning; * p < 0.05.
4. Discussion
In this study, the mean problem-solving ability score of nursing students was 3.63 out of 5, which is similar to the 3.56 points reported in a study targeting third- and fourth- year students in the department of nursing [ 24 ]. However, the current value is higher than the 3.44 points reported in a study targeting first- and second-year students [ 13 ]. Participants in these studies were nursing students in the second, third, and fourth years of study in this paper, in the third and fourth years in the study done by Kim et al. [ 24 ]; and in the first and second grades in the study by Ji et al. [ 13 ]. Problem-solving ability can be developed under the influence of various factors; those identified in previous studies include communication ability [ 13 ], critical thinking ability [ 12 , 25 ], metacognition [ 11 ], and self-directed learning [ 2 ]. These factors are continuously improved through various interpersonal relationships formed while learning and studying liberal arts and other major subjects, rather than existing as innate abilities [ 26 ]. Therefore, the degree of problem-solving ability was rather high in the study targeting the upper grades. Problem-solving ability in various unexpected situations is essential for working as a nurse [ 27 ]. In the current study, the problem-solving ability score of nursing students approximated the 72.6 percentile of the full 100-point scale. Although this score is relatively high, it is nevertheless necessary to improve problem-solving ability; given the nature of the nurse’s job, this ability represents a very important competency. Therefore, it is necessary to improve the problem-solving ability level of nursing students in Korea. The results of this study showed that factors affecting nursing students’ problem-solving ability were metacognition, communication competence, and age. It is necessary to establish a strategy that considers these factors to improve the problem-solving ability of nursing students.
The participants’ average metacognitive score was 3.86 out of 5, which was slightly higher than the 3.61 observed in a study conducted using the same tools for second-year nursing students [ 12 ]. While direct comparison using other tools is difficult, the metacognitive level of 72.3 obtained by Kim [ 28 ] for all grades in the nursing department was lower than the 77.2 points (out of 100 points) obtained in this study. According to Sternberg and Sternberg [ 29 ], the problem-solving phase includes problem identification, problem expression, strategy formulation, information construction, resource allocation, supervision, and evaluation. For health science students, metacognitive instruction has been shown to have a positive effect on students’ problem-solving ability and in improving academic achievement [ 30 ]. That is, metacognition is a key factor in predicting learning outcomes in the problem-solving domain [ 31 ]. These results were replicated in this study, which showed that a higher metacognitive level of nursing students indicated a significantly higher problem-solving ability. The subjects of this study were second-, third-, and fourth-year nursing students, and it is thought that their metacognitive level was improved compared to students in earlier phases of education, as a result of the curriculum of the nursing department. Educational programs and strategies to improve metacognition will be needed to improve the problem-solving ability of nursing students. The components of metacognition are thinking deeply in the planning stage, establishing possible strategies, undertaking regulating and monitoring activities to carry out the strategy, and revising and regulating to ensure that the solution is progressing in an appropriate direction to achieve the goal [ 32 ]. Therefore, a professor who instructs and checks nursing students is necessary to enable them to set their own goals in the curricular and non-curricular programs as they advance through the course, plan and implement strategies to achieve their goals through deep thinking, and conduct their own monitoring and control processes.
The average communication competence score of the subjects was 3.92 out of 5. Previous studies targeting students in various years of the course at the department of nursing found that the communication competence of nursing students also improved as they progressed through the course, with values reported of 3.58 points [ 33 ] and 3.56 points [ 34 ].
In previous studies, communication competence was a factor affecting nursing students’ problem-solving ability [ 13 ]. However, the current study is valuable because it additionally revealed that the level of problem-solving ability significantly increased according to the level of communication competence. Case-based education is suggested as a strategy to simultaneously improve communication competence and problem-solving skills in nursing student education [ 17 ]. This is because it is difficult to solve problems through integrative thinking and effective communication in a clinical environment, such as a hospital, with only theoretical knowledge of nursing subjects. Thus, the PBL method is applied to theoretical education in nursing colleges [ 35 , 36 ]. The results of this study showed that the presence or absence of PBL education had a significant effect on the problem-solving ability of nursing students; this ability improved when the PBL factor was added to Model 2. Therefore, it is necessary for nursing professors to practice and improve the communication competence of their students through case-based education in various subjects beginning in the first year to improve the problem-solving abilities of the students.
Additionally, the age of the subjects was also a factor influencing the problem-solving ability. Stewart, Cooper, and Moulding [ 37 ] reported that metacognitive levels increase with age. The study revealed that the communication competence of nursing students improved through various experiences [ 38 ]. Age may have had a similar influence.
Previous studies identified critical thinking disposition, empathy, nursing professional intuition, self-leadership [ 24 ], learning motivation [ 17 ], and communication competence [ 13 ] as examples of factors that affect nursing students’ problem-solving ability. However, this study demonstrated that metacognition also significantly affects the problem-solving ability of nursing students. In particular, metacognition and communication competence are considered key concepts, as they explained 51.2% of nursing students’ problem-solving ability. Therefore, it is necessary to consider and continuously apply educational strategies to improve metacognition and communication competence in the education of nursing students in the future.
This study is limited by the small number of nursing colleges that were included in the sampling, as this hinders the generalizability of the results.
5. Conclusions
This was a descriptive research study that identified the degree of and correlations between metacognition, communication competence, and problem-solving ability of nursing students, and identified factors that affect problem-solving ability. The results demonstrated that age, communication competence, and metacognition were the factors that most significantly affected the problem-solving ability of nursing students. Among these factors, metacognition had the greatest influence. Therefore, to improve the problem-solving ability of nursing students, an educational strategy is needed to improve communication competence through case-based learning in the curriculum, and development and application of activities such as PBL. In addition, the guidance of professors is needed to enable nursing students to improve their metacognition.
Since this study revealed that metacognition is a factor that influences the problem-solving ability of nursing students, we recommend conducting a study to check whether it affects actual problem-solving by developing and applying a metacognitive improvement curriculum in the future.
Acknowledgments
We would like to thank the nursing students who participated in the study.
Funding Statement
This study was supported by the research fund of Korean Bible University in 2021.
Author Contributions
Conceptualization, E.C. and J.J.; methodology, E.C. and J.J.; validation, E.C.; formal analysis, E.C.; investigation, E.C. and J.J.; resources, E.C. and J.J.; data curation, E.C.; writing—original draft preparation, E.C.; writing—review and editing, J.J.; supervision, E.C.; project administration, E.C. and J.J.; funding acquisition, E.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of Gangneung–Wonju National University (No. GWNUIRB-2022-1).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

In order to continue enjoying our site, we ask that you confirm your identity as a human. Thank you very much for your cooperation.
The Nursing Process
The common thread uniting different types of nurses who work in varied areas is the nursing process—the essential core of practice for the registered nurse to deliver holistic, patient-focused care. Assessment An RN uses a systematic, dynamic way to collect and analyze data about a client, the first step in delivering nursing care. Assessment includes not only physiological data, but also psychological, sociocultural, spiritual, economic, and life-style factors as well. For example, a nurse’s assessment of a hospitalized patient in pain includes not only the physical causes and manifestations of pain, but the patient’s response—an inability to get out of bed, refusal to eat, withdrawal from family members, anger directed at hospital staff, fear, or request for more pain mediation.
Diagnosis The nursing diagnosis is the nurse’s clinical judgment about the client’s response to actual or potential health conditions or needs. The diagnosis reflects not only that the patient is in pain, but that the pain has caused other problems such as anxiety, poor nutrition, and conflict within the family, or has the potential to cause complications—for example, respiratory infection is a potential hazard to an immobilized patient. The diagnosis is the basis for the nurse’s care plan.
Outcomes / Planning Based on the assessment and diagnosis, the nurse sets measurable and achievable short- and long-range goals for this patient that might include moving from bed to chair at least three times per day; maintaining adequate nutrition by eating smaller, more frequent meals; resolving conflict through counseling, or managing pain through adequate medication. Assessment data, diagnosis, and goals are written in the patient’s care plan so that nurses as well as other health professionals caring for the patient have access to it.
Implementation Nursing care is implemented according to the care plan, so continuity of care for the patient during hospitalization and in preparation for discharge needs to be assured. Care is documented in the patient’s record.
Evaluation Both the patient’s status and the effectiveness of the nursing care must be continuously evaluated, and the care plan modified as needed.
Item(s) added to cart

- Adult Nursing
- Critical Care Nursing
- Family Nursing
- Holistic Nursing
- Home Health Nursing – visiting nurse
- Neonatal Intensive Care Nursing
- Pediatric Nursing
- Perinatal Nursing
- Psychiatric and Mental Health Nursing
- Public Health or Community Nursing
- Rehabilitation Nursing
- Faye Abdellah
- Phil Barker
- Dr. Patricia Benner
- Helen C. Erickson
- Katie Eriksson
- Lydia E. Hall
- Virginia Henderson
- Dorothy E. Johnson
- Imogene King
- Katharine Kolcaba
- Madeleine Leininger
- Myra Estrine Levine
- Ramona Mercer
- Betty Neuman
- Margaret A. Newman
- Florence Nightingale
- Ida Jean Orlando
- Dorothea E. Orem
- Rosemarie Rizzo Parse
- Nola Pender
- Hildegard Peplau
- Isabel Hampton Robb
- Martha E. Rogers
- Nancy Roper
- Sister Callista Roy
- Henry Stack-Sullivan
- Joyce Travelbee
- Jean Watson
- Ernestine Wiedenbach
- Alfred Adler
- Lawrence Kohlberg
- Robert R. Carkhuff
- Albert Bandura
- Carl O. Helvie
- Dr. Joyce Fitzgerald
- Clarissa Harlowe Barton
- Mary Ann Bickerdyke
- Mary Carson Breckinridge
- Dorothea Lynde Dix
- Sarah Emma Edmonds
- Helen Fairchild
- Eddie Bernice Johnson
- Mary Todd Lincoln
- Mary Eliza Mahoney
- Malinda Ann Judson Richards
- Dr. Lauranne Sams
- Margaret Higgins Sanger
- Dame Cicely Mary Saunders
- Mary Jane Seacole
- Susie King Taylor
- Lillian D. Wald
- Alyce Faye Wattleton
- Walt Whitman
- National Nurses Week
- First Annual Travel Nurse Day
- AACN Synergy Model
- Trans-Cultural Nursing
- Evidence-Based Nursing
- Modern Nursing
- Nursing Techniques
- Methods of Nursing
- Nursing Theories and a Philosophy of Nursing
- Nursing Mentors
- Nursing Leaders
- How to Study and Pass the NCLEX
- How to Study in Nursing School
- Pain Scale 1-10
- Nursing Clinicals and Nursing Theories
- Nursing Program
- Nursing Theory Definition
- Nursing Ethics and the Nursing Process
- History of Nursing
- Definition of Nursing
- The Nursing Process
- Nursing Care Plans in Action
- Nursing Technology
- Nursing Home Jobs and Getting Qualified
- Standards and Criteria Used by the NLNAC
- How Much Does Nursing School Cost
- Unsubsidized Nursing Student Loans
- A Statistical Look at Patient-Centered Care
- Being A Nurse At Christmas
- Nemours Brings Nursing Opportunities to Central Florida
- How Have the Sequester Cuts Affected Nursing and Health Care
21 Nursing Problems by Faye Abdellah
The Twenty-One Nursing Problems Theory was developed by Faye Glenn Abdellah . Her model of nursing was progressive for the time in that it refers to a nursing diagnosis during a time in which nurses were taught that diagnoses were not part of their role in health care.
There are specific characteristics identifiable in the Twenty-One Nursing Problems. The theory has interrelated the concepts of health, nursing problems, and problem-solving. Problem-solving is an activity that is inherently logical in nature. The framework focuses on nursing practice and individual patients.
The twenty-one nursing problems identified in the nursing theory are comprised of ten steps used to identify the patient’s problems and eleven skills used in developing a treatment typology or nursing care plan .
The ten steps to identify the patient’s problems are:
- Learn to know the patient
- Sort out relevant and significant data
- Make generalizations about available data in relation to similar nursing problems presented by other patients
- Identify the therapeutic plan
- Test generalizations with the patient and make additional generalizations
- Validate the patient’s conclusions about his nursing problems
- Continue to observe and evaluate the patient over a period of time to identify any attitudes and clues affecting his behavior
- Explore the patient’s and family’s reaction to the therapeutic plan and involve them in the plan
- Identify how the nurses feel about the patient’s nursing problems
- Discuss and develop a comprehensive nursing care plan
The eleven nursing skills in the theory are:
- observation of health status
- skills of communication
- application of knowledge
- teaching of patients and families
- planning and organization of work
- use of resource materials
- use of personnel materials
- problem-solving
- direction of work of others
- therapeutic use of the self
- nursing procedure
The twenty-one nursing problems fall into three categories: physical, sociological, and emotional needs of patients; types of interpersonal relationships between the patient and nurse; and common elements of patient care.
The needs of patients are divided into four categories: basic to all patients, sustenal care needs, remedial care needs, and restorative care needs.
Needs that are basic to all patients are to maintain good hygiene and physical comfort; promote optimal activity, including exercise, rest and sleep; promote safety through the prevention of accidents, injury or other trauma and through the prevention of the spread of infection; and maintain good body mechanics and prevent or correct deformity.
Sustenal care needs facilitate the maintenance of a supply of oxygen to all body cells; facilitate the maintenance of nutrition of all body cells; facilitate the maintenance of elimination; facilitate the maintenance of fluid and electrolyte balance; recognize the physiological responses of the body to disease conditions; facilitate the maintenance of regulatory mechanisms and functions; and facilitate the maintenance of sensory function.
Remedial care needs identify and accept positive and negative expressions, feelings, and reactions; identify and accept the interrelatedness of emotions and organic illness; facilitate the maintenance of effective verbal and non-verbal communication; promote the development of productive interpersonal relationships; facilitate progress toward achievement of personal spiritual goals; create and maintain a therapeutic environment; and facilitate awareness of the self as an individual with varying physical, emotional, and developmental needs.
Restorative care needs include the acceptance of the optimum possible goals in light of limitations, both physical and emotional; the use of community resources as an aid to resolve problems that arise from illness; and the understanding of the role of social problems as influential factors in the case of illness.
According to the Twenty-One Nursing Problems model, patients are described as having physical, emotional, and sociological needs. People are also the only justification for the existence of nursing. That is, without people, nursing would not be a profession since they are the recipients of nursing.
Patient-centered approaches to nursing health are described as a state mutually exclusive of illness. Abdellah does not provide a definition of health, but speaks to “total health needs” and “a healthy state of mind and body” in her description of nursing.
In this nursing model , society is included in “planning for optimum health on local, state, national, and international levels.” However, the focus of nursing is the individual. The environment is the home or community from which the patient comes.
Nursing is a helping profession. Nursing care is doing something for or to the patient or giving the patient information with the goals of meeting needs, increasing or restoring self-help ability, or alleviating impairments. The role of the nurse is to help the patient achieve goals to reach optimum health.
Abdellah explained nursing as a comprehensive service, which includes:
- Recognizing the nursing problems of the patient
- Deciding the appropriate course of action to take in terms of relevant nursing principles
- Providing continuous care of the individual’s total needs
- Providing continuous care to relieve pain and discomfort and provide immediate security for the individual
- Adjusting the total nursing care plan to meet the patient’s individual needs
- Helping the individual to become more self-directing in attaining or maintaining a healthy state of body and mind
- Instructing nursing personnel and family to help the individual do for himself that which he can within his limitations
- Helping the individual to adjust to his limitations and emotional problems
- Working with allied health professions in planning for optimum health on local, state, national, and international levels
- Carrying out continuous evaluation and research to improve nursing techniques and to develop new techniques to meet people’s health needs
The twenty-one problems can be applied to the nursing process . In the assessment phase, the nursing problems provide guidelines for data collection. The results of data collection determines the patient’s specific problems, which leads to the nursing diagnosis. The statements of nursing problems resemble goal statements, so once the patient has been diagnosed, nursing goals have already been established. The goals can be used as a framework to develop a plan and nursing interventions. In terms of evaluation, the nurse’s progress or lack of progress toward the achievement of stated goals is the appropriate evaluation. The theory provides a basis for determining and organizing nursing care, as well as a basis for organizing nursing strategies.
Nurse Selection Criteria + Example Responses
- Careers & Specialisations
- Wages, Salaries & Pay Rates
- Types of Nursing Courses
- ATAR for Nursing
- Scholarships
- Resume Tips & Template
- Nursing Cover Letter
- Interview Questions & Answers
- Selection Criteria Examples
- Tertiary Admissions Centres
- Nursing Agencies
- Nursing Jobs
When it comes to nursing positions, education and experience are important, but they are not the only factors employers take into consideration. Employers also look for certain key selection criteria that demonstrate a candidate’s ability to perform the role effectively. As with any interview, it’s often recommended that you follow the STAR method when provding a response. The STAR method is a structured manner of responding to behavioral-based interview questions by providing the specific Situation, Task, Action, and Result of the particular scenario. This article will go beyond education and experience, and provide insight into the key selection criteria for nursing positions, along with example STAR responses.
1. Communication & Interpersonal Skills
Effective communication and interpersonal skills are critical in the nursing profession. You need to be able to communicate with patients, their families, and other healthcare professionals in a clear and concise manner. Additionally, being able to form strong relationships with others is important in building trust and providing the best care for your patients. Employers will be looking for evidence of your communication and interpersonal skills during the interview.
Example response:
- Situation: During my time working as a nurse in a hospital, I was faced with a patient who was non-verbal and unable to communicate their needs.
- Task: I needed to assess their condition and administer medication.
- Action: I used non-verbal communication techniques, such as gestures and facial expressions, to understand their needs and communicate with them effectively. I also formed a rapport with the patient, by talking to them in a calm and reassuring tone.
- Result: The patient was able to receive the necessary treatment and was much more comfortable with the process. The patient and their family also expressed their gratitude for my compassionate and empathetic approach.
2. Compassion & Empathy
Compassion and empathy are key traits for nurses as they must be able to understand and connect with their patients. This requires an ability to listen, understand, and respond to the emotional and physical needs of patients. Nurses must be able to show compassion and empathy towards their patients and provide comfort and support.
Employers are looking for nurses who can demonstrate their compassion and empathy skills and show that they are able to connect with and understand their patients. They want to see that you have a genuine concern for the well-being of your patients and are able to provide comfort and support. They also want to know that you are able to maintain a professional demeanor and provide care in a respectful and empathetic manner.
By demonstrating your compassion and empathy skills, you show that you are a caring and empathetic nurse who is able to understand and connect with your patients. You also show that you are able to provide comfort and support to your patients, which is essential for providing high-quality patient care. Your compassion and empathy skills demonstrate your commitment to providing patient-centered care and helping your patients feel supported and understood.
- Situation: I was working in a hospice where a patient was in their final stages of life.
- Task: The patient was in a lot of pain and their family was upset and worried.
- Action: I listened to the patient’s concerns and provided comfort and reassurance to both the patient and their family. I also kept in close communication with the patient’s physician to ensure that their pain was managed appropriately.
- Result: The patient was able to pass away peacefully, and the family felt comforted knowing that their loved one was not alone. They also expressed their appreciation for my compassionate and empathetic approach.
3. Teamwork
Nursing is a team-oriented profession, and it is important to be able to work well with others. This involves being able to collaborate with other healthcare professionals, such as physicians and nursing assistants, to provide the best care for your patients. Nurses must be able to work towards a common goal and support their colleagues, while also being able to take initiative and lead when necessary.
Employers are looking for nurses who can demonstrate their teamwork skills and show that they are able to collaborate effectively with others. They want to see that you have a positive attitude, are supportive of your colleagues, and can work well under pressure. They also want to know that you have the ability to take initiative and lead when necessary, as this is essential for providing high-quality patient care.
By demonstrating your teamwork skills, you show that you are a collaborative and supportive nurse who is able to work well with others. You also show that you have the ability to take initiative and lead when necessary, which is essential for providing high-quality patient care. You demonstrate your commitment to teamwork and collaboration, which is essential for ensuring the best outcomes for your patients and the success of the healthcare team.
- Situation: I was working on a busy medical-surgical unit where the staff was stretched thin.
- Task: I needed to ensure that all of my patients received the care they needed in a timely manner.
- Action: I worked closely with my fellow nurses and nursing assistants to prioritize patient care, delegate tasks, and provide support when needed. I also kept open communication with the physician to ensure that everyone was on the same page.
- Result: We were able to provide the best care for our patients and maintain a positive and productive work environment. The unit received positive feedback from patients and their families for our teamwork and collaboration.
4. Quality Improvement
Quality improvement is an essential aspect of the nursing profession as it helps to ensure that patients receive the best care possible. It involves identifying areas for improvement and implementing changes to improve the quality of care. This could include improving patient outcomes, reducing errors, increasing patient satisfaction, or improving efficiency.
Quality improvement requires a systematic approach, collaboration, and an ongoing commitment to continuous improvement. Nurses play a vital role in this process as they are often on the front lines, working with patients and providing care. By being involved in quality improvement initiatives, nurses can make a positive impact on patient outcomes and contribute to the overall success of the healthcare organisation.
Employers will be looking for evidence of your ability to identify areas for improvement, implement changes, and monitor the results during the interview. They want to see that you have a commitment to providing the best care for your patients and are proactive in seeking ways to improve the quality of care.
- Situation: I was working in a hospital where the discharge process was taking longer than it should.
- Task: I needed to find a solution to improve the discharge process for patients.
- Action: I analyzed the current process, identified areas for improvement, and made suggestions for changes. I also collaborated with the rest of the nursing staff and physicians to implement the changes and monitor the results.
- Result: The discharge process was streamlined, and patients were able to be discharged faster, which improved their experience and satisfaction. The hospital also received positive feedback from patients and their families for the improved discharge process.
5. Continuous Professional Development (CPD)
Continuous professional development is important for nurses, as it helps them to stay up-to-date with the latest developments in the field and maintain their competency. Employers are looking for nurses who are committed to their ongoing professional development and have a strong desire to learn and grow in their careers. By demonstrating a commitment to CPD, nurses show that they are dedicated to providing the best care for their patients and are interested in staying current in their field.
- Situation: I was working as a nurse and wanted to further my knowledge in a specific area of nursing.
- Task: I needed to find ways to continue my professional development.
- Action: I researched and attended conferences, workshops, and courses related to my area of interest. I also sought out mentorship opportunities with experienced nurses.
- Result: I was able to expand my knowledge and skills in my area of interest, which helped me provide better care for my patients. I also received recognition from my peers and supervisors for my commitment to continuous professional development.
6. Problem-Solving
Problem-solving is a crucial skill for nurses as they often face complex and challenging situations in their daily work. It requires critical thinking, effective communication, and the ability to identify and analyse problems and find solutions. Nurses must be able to make informed decisions, prioritise tasks, and work effectively under pressure.
Employers are looking for nurses who can demonstrate their problem-solving skills and show that they can handle challenging situations in a calm and effective manner. They want to see that you can think creatively and come up with innovative solutions to problems. They also want to know that you have the ability to make decisions that benefit your patients, your team, and the organisation.
By demonstrating your problem-solving skills, you show that you are a competent nurse who can handle complex and challenging situations and make informed decisions. You also show that you have the ability to think critically and creatively, which is essential for providing high-quality patient care.
- Situation: I was working as a nurse in a busy emergency room where a patient was in critical condition.
- Task: I needed to find a solution to provide the best care for the patient in a limited amount of time.
- Action: I assessed the patient’s condition, gathered relevant information, and considered multiple options for treatment. I then collaborated with the physician to determine the best course of action.
- Result: The patient received the necessary treatment, and their condition stabilized. The patient and their family also expressed their gratitude for my quick thinking and effective problem-solving skills.
7. Legal Understanding
Legal understanding is an important aspect of nursing as nurses must be aware of and adhere to the laws and regulations that govern their practice. This includes understanding the laws and regulations related to patient privacy, informed consent, and medical ethics. Nurses must also be aware of the legal implications of their actions and understand how to handle difficult and complex legal situations.
Employers are looking for nurses who have a good understanding of the laws and regulations that govern their practice and who can demonstrate their ability to apply this knowledge in their daily work. They want to see that you have a commitment to upholding the ethical and legal standards of the nursing profession and are able to make informed decisions that are in line with these standards.
By demonstrating your legal understanding, you show that you are a responsible and ethical nurse who is committed to providing high-quality care to your patients. You also show that you are aware of the laws and regulations that govern your practice and have the ability to handle difficult and complex legal situations in a professional and responsible manner.
- Situation: I was working as a nurse and was faced with a situation where a patient’s privacy was in question.
- Task: I needed to ensure that the patient’s privacy was protected.
- Action: I consulted the relevant laws and regulations, and determined the appropriate course of action. I also kept the patient informed of the situation and their rights.
- Result: The patient’s privacy was protected, and the hospital was able to comply with the relevant laws and regulations. The patient also expressed their appreciation for my understanding of their rights and protection of their privacy.
In conclusion, education and experience are important factors when it comes to nursing positions, but they are not the only factors that employers take into consideration. Employers also look for evidence of key selection criteria such as communication and interpersonal skills, compassion and empathy, teamwork, quality improvement, continuous professional development, problem-solving, and legal knowledge.
It is essential for nursing candidates to understand these criteria and be able to provide examples of how they demonstrate them during the interview. By following the STAR method and being able to articulate your experiences and accomplishments, you can show the interviewer that you possess the skills and qualities necessary for a successful nursing career.
So, when preparing for a nursing interview , take the time to reflect on your experiences and think about how you can demonstrate these key selection criteria. Show the interviewer that you are a well-rounded and competent nurse who is committed to providing the best care for your patients. Good luck!
More information
- Nursing Schools
- Find Courses
- Diploma of Nursing
- Bachelor of Nursing
- Master of Nursing
- CPD Courses
- Nursing Courses Sydney
- Nursing Courses Melbourne
- Nursing Courses in QLD
- Nursing Courses Brisbane
- Nursing Courses Perth
- Nursing Courses Online
- Nursing Courses in Tasmania
- Nursing Courses in Darwin NT
- Nursing Courses in Adelaide SA
- Nursing Courses in Canberra ACT
The Ultimate Guide to Nursing Diagnosis in 2024
What is a nursing diagnosis.
- NANDA Nursing Diagnosis
- Classification
NANDA Nursing Diagnosis List
Writing a nursing diagnosis.
- Nursing Diagnosis vs Medical Diagnosis
- American vs International

A nursing diagnosis is a part of the nursing process and is a clinical judgment that helps nurses determine the plan of care for their patients. These diagnoses drive possible interventions for the patient, family, and community. They are developed with thoughtful consideration of a patient’s physical assessment and can help measure outcomes for the nursing care plan .
In this article, we'll explore the NANDA nursing diagnosis list, examples of nursing diagnoses, and the 4 types.
Some nurses may see nursing diagnoses as outdated and arduous. However, it is an essential tool that promotes patient safety by utilizing evidence-based nursing research.
According to NANDA-I, the official definition of the nursing diagnosis is:
“Nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable.”
What is The Purpose of a Nursing Diagnosis?
According to NANDA International , a nursing diagnosis is “a judgment based on a comprehensive nursing assessment.” The nursing diagnosis is based on the patient’s current situation and health assessment, allowing nurses and other healthcare providers to see a patient's care from a holistic perspective.
Proper nursing diagnoses can lead to greater patient safety, quality care, and increased reimbursement from private health insurance, Medicare, and Medicaid.
They are just as beneficial to nurses as they are to patients.
NANDA Nursing Diagnosis
NANDA diagnoses help strengthen a nurse’s awareness, professional role, and professional abilities.
Formed in 1982, NANDA is a professional organization that develops, researches, disseminates, and refines the nursing terminology of nursing diagnosis. Originally an acronym for the North American Nursing Diagnosis Association, NANDA was renamed to NANDA International in 2002 as a response to its broadening worldwide membership.
According to its website, NANDA International’s mission is to:
- Provide the world’s leading evidence-based nursing diagnoses for use in practice and to determine interventions and outcomes
- Contribute to patient safety through the integration of evidence-based terminology into clinical practice and clinical decision-making
- Fund research through the NANDA-I Foundation
- Be a supportive and energetic global network of nurses, who are committed to improving the quality of nursing care and improvement of patient safety through evidence-based practice
NANDA members can be found worldwide, specifically in Brazil, Colombia, Ecuador, Mexico, Peru, Portugal, Germany, Austria, Switzerland, Netherlands, Belgium, and Nigeria-Ghana.
NANDA Classification of Nursing Diagnoses
NANDA-I adopted the Taxonomy II after consideration and collaboration with the National Library of Medicine (NLM) in regards to healthcare terminology codes. Taxonomy II has three levels: domains, classes, and nursing diagnoses.
There are currently 13 domains and 47 classes:
- Health Awareness
- Health Management
- Urinary Function
- Gastrointestinal Function
- Integumentary Function
- Respiratory Function
- Activity/Exercise
- Energy Balance
- Cardiovascular-Pulmonary Responses
- Orientation
- Sensation/Perception
- Communication
- Self-concept
- Self-esteem
- Caregiving Roles
- Family Relationships
- Role Performance
- Sexual Identity
- Sexual Function
- Reproduction
- Post-trauma Responses
- Coping Response
- Neuro-Behavioral Stress
- Value/Belief Action Congruence
- Physical Injury
- Environmental Hazards
- Defensive Processes
- Thermoregulation
- Physical Comfort
- Environmental Comfort
- Social Comfort
- Development
This refined Taxonomy is based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Furthermore, the NLM suggested changes because the Taxonomy I code structure included information about the location and the level of the diagnosis.
NANDA-I nursing diagnoses and Taxonomy II comply with the International Standards Organization (ISO) terminology model for a nursing diagnosis.
The terminology is also registered with Health Level Seven International (HL7), an international healthcare informatics standard that allows for nursing diagnoses to be identified in specific electronic messages among different clinical information systems.
A full list of NANDA-I-approved nursing diagnoses can be found here .
Additional examples include:
- Dysfunctional ventilatory weaning response
- Impaired transferability
- Activity intolerance
- Situational low self-esteem
- Risk for disturbed maternal-fetal dyad
- Impaired emancipated decision-making
- Risk for impaired skin integrity
- Risk for metabolic imbalance syndrome
- Urge urinary incontinence
- Risk for unstable blood pressure
- Impaired verbal communication
- Acute confusion
- Disturbed body image
- Relocation stress syndrome
- Ineffective role performance
- Readiness for enhanced sleep
Examples of Nursing Diagnoses
The three main components of a nursing diagnosis are as follows.
- Problem and its definition
- Defining characteristics or risk factors
Examples of proper nursing diagnoses may include:
>> Related: What is the Nursing Process?
NANDA Nursing Diagnosis Types
There are 4 types of nursing diagnoses according to NANDA-I. They are:
- Problem-focused
- Health promotion
Popular Online RN-to-BSN Programs

Enrollment: Nationwide

At Purdue Global, discover a faster, more affordable way to earn your Nursing degree. Purdue Global is committed to keeping your tuition costs as low as possible and helping you find the most efficient path to your degree.
Enrollment: Nationwide, but certain programs have state restrictions. Check with Purdue for details.
- RN-to-BSN - ExcelTrack

Pursue Your Dream of Becoming a Nurse! Our 3-Year BSN Program is designed with one goal – to prepare you for a successful career as a BSN-prepared registered nurse. We combine classroom teaching, hands-on simulations, and clinicals in real-world healthcare environments to give you the skills you need.
Enrollment: On-Campus in AZ, FL, MI, MO, NV, OH, TX, UT, VA
- BS in Nursing (RN Not Required)
- RN to BSN - Global Studies

1. Problem-focused diagnosis
A patient problem present during a nursing assessment is known as a problem-focused diagnosis. Generally, the problem is seen throughout several shifts or a patient’s entire hospitalization. However, it may be resolved during a shift depending on the nursing and medical care.
Problem-focused diagnoses have three components.
- Nursing diagnosis
- Related factors
- Defining characteristics
Examples of this type of nursing diagnosis include:
- Decreased cardiac output
- Chronic functional constipation
- Impaired gas exchange
Problem-focused nursing diagnoses are typically based on signs and symptoms present in the patient. They are the most common nursing diagnoses and the easiest to identify.
2. Risk nursing diagnosis
A risk nursing diagnosis applies when risk factors require intervention from the nurse and healthcare team prior to a real problem developing.
- Risk for imbalanced fluid volume
- Risk for ineffective childbearing process
- Risk for impaired oral mucous membrane integrity
This type of diagnosis often requires clinical reasoning and nursing judgment.
3. Health promotion diagnosis
The goal of a health promotion nursing diagnosis is to improve the overall well-being of an individual, family, or community.
- Readiness for enhanced family processes
- Readiness for enhanced hope
- Sedentary lifestyle
4. Syndrome diagnosis
A syndrome diagnosis refers to a cluster of nursing diagnoses that occur in a pattern or can all be addressed through the same or similar nursing interventions.
Examples of this diagnosis include:
- Decreased cardiac output
- Decreased cardiac tissue perfusion
- Ineffective cerebral tissue perfusion
- Ineffective peripheral tissue perfusion
Possible nursing diagnosis
While not an official type of nursing diagnosis, possible nursing diagnosis applies to problems suspected to arise. This occurs when risk factors are present and require additional information to diagnose a potential problem.
Nursing Diagnosis Components
The three main components of a nursing diagnosis are:
- Etiology or risk factors
1. The problem statement explains the patient’s current health problem and the nursing interventions needed to care for the patient.
2. Etiology, or related factors , describes the possible reasons for the problem or the conditions in which it developed. These related factors guide the appropriate nursing interventions.
3. Finally, defining characteristics are signs and symptoms that allow for applying a specific diagnostic label. Risk factors are used in the place of defining characteristics for risk nursing diagnosis. They refer to factors that increase the patient’s vulnerability to health problems.
>> Show Me Online Nursing Programs
Problem-focused and risk diagnoses are the most difficult nursing diagnoses to write because they have multiple parts. According to NANDA-I , the simplest ways to write these nursing diagnoses are as follows:
PROBLEM-FOCUSED DIAGNOSIS
Problem-Focused Diagnosis related to ______________________ (Related Factors) as evidenced by _________________________ (Defining Characteristics).
RISK DIAGNOSIS
The correct statement for a NANDA-I nursing diagnosis would be: Risk for _____________ as evidenced by __________________________ (Risk Factors).
Nursing Diagnosis vs Medical Diagnosis
While all important, the nursing diagnosis is primarily handled through specific nursing interventions while a medical diagnosis is made by a physician or advanced healthcare practitioner.
The nursing diagnosis can be mental, spiritual, psychosocial, and/or physical. It focuses on the overall care of the patient while the medical diagnosis involves the medical aspect of the patient’s condition.
A medical diagnosis does not change if the condition is resolved, and it remains part of the patient’s health history forever. A nursing diagnosis, however, generally refers to a specific period of time.
Examples of medical diagnosis include:
- Congestive Heart Failure
- Diabetes Insipidus
Collaborative problems are ones that can be resolved or worked on through both nursing and medical interventions. Oftentimes, nurses will monitor the problems while the medical providers prescribe medications or obtain diagnostic tests.
History of Nursing Diagnoses
- 1973: The first conference to identify nursing knowledge and a classification system; NANDA was founded
- 1977: First Canadian Conference takes place in Toronto
- 1982: NANDA formed with members from the United States and Canada
- 1984: NANDA established a Diagnosis Review Committee
- 1987: American Nurses Association (ANA) officially recognizes NANDA to govern the development of a classification system for nursing diagnosis
- 1987: International Nursing Conference held in Alberta, Canada
- 1990: 9th NANDA conference and the official definition of the nursing diagnosis established
- 1997: Official journal renamed from “Nursing Diagnosis” to “Nursing Diagnosis: The International Journal of Nursing Terminologies and Classifications”
- 2002: NANDA changes to NANDA International (NANDA-I) and Taxonomy II released
- 2020: 244 NANDA-I approved diagnosis
American vs International Nursing Diagnosis
There is currently no difference between American nursing diagnoses and international nursing diagnoses. Because NANDA-I is an international organization, the approved nursing diagnoses are the same.
Discrepancies may occur when the translation of a nursing diagnosis into another language alters the syntax and structure. However, since there are NANDA-I offices around the world, the non-English nursing diagnoses are essentially the same.
What is an example of a nursing diagnosis?
- A nursing diagnosis is something a nurse can make that does not require an advanced provider’s input. It is not a medical diagnosis. An example of a nursing diagnosis is: Excessive fluid volume related to congestive heart failure as evidenced by symptoms of edema.
What is the most common nursing diagnosis?
- According to NANDA, some of the most common nursing diagnoses include pain, risk of infection, constipation, and body temperature imbalance.
What is a potential nursing diagnosis?
- A potential problem is an issue that could occur with the patient’s medical diagnosis, but there are no current signs and symptoms of it. For instance, skin integrity breakdown could occur in a patient with limited mobility.
How is a nursing diagnosis written?
- Nursing diagnoses are written with a problem or potential problem related to a medical condition, as evidenced by any presenting symptoms. There are 4 types of nursing diagnoses: risk-focused, problem-focused, health promotion-focused, or syndrome-focused.
What is the clinical diagnosis?
- A clinical diagnosis is the official medical diagnosis issued by a physician or other advanced care professional.
Find Nursing Programs

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. You may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

IMAGES
VIDEO
COMMENTS
Problem-solving in nursing is the vital foundation that makes up a nurse's clinical judgment and critical thinking skills. Having a strong problem-solving skillset is pertinent to possessing the ability and means to provide safe, quality care to a variety of patients. Nurses must rely on their clinical judgment and critical thinking skills to ...
Nurses can implement the original nursing process to guide patient care for problem solving in nursing. These steps include: Assessment. Use critical thinking skills to brainstorm and gather information. Diagnosis. Identify the problem and any triggers or obstacles. Planning. Collaborate to formulate the desired outcome based on proven methods ...
For example: Ask questions. Gather information. Implement a strategy. Evaluate the results. Consider another point of view. These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
s, and problem-solving, which requires analysis. Decision-makingfree flow of ideas is essential to problem-solving and decision-making becaus. it helps prevent preconceived ideas from controlling the process. Many decisions in healthcare are arrived at by group or teams rather than by the in. vidual, and this type of decision-making requ.
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
One example of critical thinking in nursing is interpreting these changes with an open mind. Make impartial decisions based on evidence rather than opinions. ... Problem-solving skills. Practicing your problem-solving skills can improve your critical-thinking skills. Analyze the problem, consider alternate solutions, and implement the most ...
Nurse leaders perceive their role as a problem-solver, which is a necessary step in advocacy. 27 Problem-solving is a process that contains the elements of decision-making and critical thinking. 28. The theory that emerged from the core categories explicitly focused on the central phenomenon of LHV in the nursing work environment.
For example, treating immediate symptoms may temporarily solve a problem, but determining the underlying cause of the symptoms is the key to effective long-term health. 8 Examples of Critical Thinking in Nursing. Here are some real-life examples of how nurses apply critical thinking on the job every day, as told by nurses themselves.
Problem solving for nurses is essential to quality patient care. Explore problem-solving examples in nursing and devise effective strategies.
Step 2: Analyze the Problem. Break down the problem to get an understanding of the problem. Determine how the problem developed. Determine the impact of the problem. Step 3: Develop Solutions. Brainstorm and list all possible solutions that focus on resolving the identified problem. Do not eliminate any possible solutions at this stage.
By thinking outside the box and exploring innovative approaches, nurses develop adaptable problem-solving skills that can be applied to complex patient care challenges. Example. Brainstorming creative approaches to comfort a distressed pediatric patient empowers a nurse to find innovative methods beyond routine interventions. 16.
Promotes Problem-Solving: Nurses encounter complex patient issues that require effective problem-solving. Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient. Drives Creativity: Nursing care is not always straightforward.
This paper analyses the role of problem solving in nursing practice including the process, acquisition and measurement of problem-solving skills It is argued that while problem-solving ability is acknowledged as critical if today's nurse practitioner is to maintain effective clinical practice, to date it retains a marginal place in nurse education curricula Further, it has attracted limited ...
Conclusion. The influencing factors of clinical nurses' problem-solving dilemma are diverse. Hospital managers and nursing educators should pay attention to the problem-solving of clinical nurses, carry out a series of training and counselling of nurses by using the method of situational simulation, optimize the nursing management mode, learn to use new media technology to improve the ...
To solve a problem you need to generate solutions. However, the obvious solution may not necessarily be the best. To generate solutions, a mixture of creative and analytical thinking is needed (Bransford, 1993). Creativity is about escaping from preconceived ideas that block the way to finding an innovative solution to a problem.
Chapter 3 Solving problems together Objectives 1. Define mutuality in nurse-client relationships 2. Discuss the use of face work and politeness theory in approaching clients 3. Discuss mutual problem solving to involve the client in the implementation of the nursing process 4. Complete exercises to practice a mutual problem-solving approach to the nursing process 5.
Problem solving is a focus of nursing practice and of great importance for raising the quality of patient care. Constructive problem-solving skills affect cognitive empathy skills. ... The study sample consisted of the 80 nurses who volunteered to participate and answered all of the questions on the inventory. Data Collection Tool.
Background. Problem solving involves recognizing the difference between the problem solver's current state and the goal state to be reached, and resolving the obstacles that prevent them from achieving the goal [].Acquiring problem-solving ability based on judgment and critical thinking is an important element of nursing education [].Furthermore, the use of effective problem-solving ...
Problem-solving - when the nurse applies critical thinking skills to the issue at hand; ... The best way to understand critical thinking in nursing is through the use of examples. The following is ...
Care is documented in the patient's record. Evaluation. Both the patient's status and the effectiveness of the nursing care must be continuously evaluated, and the care plan modified as needed. Learn more about the nursing process, including its five core areas (assessment, diagnosis, outcomes/planning, implementation, and evaluation).
Problem-solving is an activity that is inherently logical in nature. The framework focuses on nursing practice and individual patients. The twenty-one nursing problems identified in the nursing theory are comprised of ten steps used to identify the patient's problems and eleven skills used in developing a treatment typology or nursing care plan .
This article will go beyond education and experience, and provide insight into the key selection criteria for nursing positions, along with example STAR responses. 1. Communication & Interpersonal Skills ... Problem-Solving. Problem-solving is a crucial skill for nurses as they often face complex and challenging situations in their daily work ...
A patient problem present during a nursing assessment is known as a problem-focused diagnosis. Generally, the problem is seen throughout several shifts or a patient's entire hospitalization. However, it may be resolved during a shift depending on the nursing and medical care. Problem-focused diagnoses have three components. Nursing diagnosis