
- Presidential Message
- Nominations/Elections
- Past Presidents
- Member Spotlight
- Fellow List
- Fellowship Nominations
- Current Awardees
- Award Nominations
- SCP Mentoring Program
- SCP Book Club
- Pub Fee & Certificate Purchases
- LEAD Program
- Introduction
- Find a Treatment
- Submit Proposal
- Dissemination and Implementation
- Diversity Resources
- Graduate School Applicants
- Student Resources
- Early Career Resources
- Principles for Training in Evidence-Based Psychology
- Advances in Psychotherapy
- Announcements
- Submit Blog
- Student Blog
- The Clinical Psychologist
- CP:SP Journal
- APA Convention
- SCP Conference

CASE STUDY Sage (bulimia nervosa)
Case study details.
Sage is a 26-year-old doctoral candidate in English literature at the local university. She is in good standing in her program and has plans to enter the job market in the fall. In your intake, she tells you she thinks she is “fat” and has been self-conscious about her body since the sixth grade, at which time she began menstruating and developing breasts earlier than the other girls in her class. She was teased for needing a bra and remembers feeling “chubby, too big, and just wanting to be small like [her] younger sister.” She started dieting in the seventh grade, following strict rules for weeks (e.g., she recalls the grapefruit only diet), then transitioning into what she called “bad” weeks. During these times, she would stock up on candy bars and other snack foods and eat them, often in her bedroom late at night. Her parents became concerned and tried to strictly limit her dieting. This led to eating “normal” during the day and binging on those candy bars she kept hidden in her bedroom at night if she felt sad, scared, or mad. She grew into a habit of eating to feel better – relief that was only temporary, as she would feel ashamed about what she had done and resolve to not do it again. In college, her pattern of emotional eating continued, which felt more distressing to her because of the pressure to look “as pretty and thin as the other girls.” In spring of her freshman year she experimented with throwing up after the late-night eating and found that, at least in the minutes that followed, she felt like she had much more control and believed this would help her to prevent the weight gain she so dreaded. She fell into a vicious cycle of late-night binges (typically consuming about 7 candy bars in 15 minutes, during which times Sage described feeling very out of control) followed by making herself throw up. In college, she engaged in these binge-purge episodes about 6 nights/week. At present, she is having a harder time hiding the episodes because she lives with her boyfriend; she estimates that they occur about 4 nights per week. The times when she feels the most compelled to binge and purge are when she has a major presentation coming up in her doctoral program and when she gets in a fight with her boyfriend. Her BMI is in the normal range, but she says she needs to lose weight. She wants to stop binging and purging because she does not want her boyfriend to find out, but she is also afraid that if she stops, she will gain weight.
- Binges and Purging
- Emotion Dysregulation
- Disordered Eating
Diagnoses and Related Treatments
1. bulimia nervosa.
Thank you for supporting the Society of Clinical Psychology. To enhance our membership benefits, we are requesting that members fill out their profile in full. This will help the Division to gather appropriate data to provide you with the best benefits. You will be able to access all other areas of the website, once your profile is submitted. Thank you and please feel free to email the Central Office at [email protected] if you have any questions
CASE REPORT article
Case report: unexpected remission from extreme and enduring bulimia nervosa with repeated ketamine assisted psychotherapy.

- 1 Department of Psychology, University of Utah, Salt Lake City, UT, United States
- 2 Behavioral Science Department, Utah Valley University, Orem, UT, United States
- 3 Division of Public Health, University of Utah School of Medicine, Salt Lake City, UT, United States
- 4 Marriage and Family Therapy Program, Capella University, Minneapolis, MN, United States
- 5 Riverwoods Behavioral Health, Provo, UT, United States
- 6 Department of Educational Psychology, University of Utah, Salt Lake City, UT, United States
Background: Bulimia nervosa is a disabling psychiatric disorder that considerably impairs physical health, disrupts psychosocial functioning, and reduces overall quality of life. Despite available treatment, less than half of sufferers achieve recovery and approximately a third become chronically ill. Extreme and enduring cases are particularly resistant to first-line treatment, namely antidepressants and cognitive behavioral therapy, and have the highest rate of premature mortality. Here, we demonstrate that in such cases, repeated sessions of ketamine assisted psychotherapy (KAP) is an effective treatment alternative for improving symptoms.
Case Presentation: A 21-year-old woman presented with extreme and enduring bulimia nervosa. She reported recurrent binge-eating and purging by self-induced vomiting 40 episodes per day, which proved refractory to both pharmacological and behavioral treatment at the outpatient, residential, and inpatient level. Provided this, her physician recommended repeated KAP as an exploratory and off-label intervention for her eating disorder. The patient underwent three courses of KAP over 3 months, with each course consisting of six sessions scheduled twice weekly. She showed dramatic reductions in binge-eating and purging following the first course of treatment that continued with the second and third. Complete cessation of behavioral symptoms was achieved 3 months post-treatment. Her remission has sustained for over 1 year to date.
Conclusions: To our knowledge, this is the first report of repeated KAP used to treat bulimia nervosa that led to complete and sustained remission, a rare outcome for severe and enduring cases, let alone extreme ones. Additionally, it highlights the degree to which KAP can be tailored at the individual level based on symptom severity and treatment response. While its mechanism of action is unclear, repeated KAP is a promising intervention for bulimia nervosa that warrants future research and clinical practice consideration.
Introduction
Bulimia nervosa (BN) is a disabling psychiatric disorder characterized by recurrent binge-eating (consuming objectively large amounts of food with a sense of lost control) and inappropriate compensatory behaviors (self-induced vomiting; laxative, diuretic, or medication misuse; and fasting or excessive exercise) aimed at preventing weight gain ( 1 , 2 ). Overtime, the severity of these patterns significantly disrupts physical health and psychosocial functioning, as well as impacts families and communities at large ( 3 ). Approximately 50 million people worldwide will develop BN at some point in their life ( 4 ). Moreover, studies have found BN to be associated with concomitant psychiatric comorbidity [e.g., mood disorders and substance abuse; ( 5 , 6 )] in addition to premature mortality due to medical complications ( 7 – 9 ). Death by suicide is also eight times more likely to occur among individuals with BN compared to the general population, with more than a third experiencing lifetime rates of non-suicidal self-injury ( 10 , 11 ).
While pharmacological (e.g., selective serotonin reuptake inhibitors) and behavioral (e.g., cognitive behavioral therapy) interventions are effective in managing BN ( 12 , 13 ), many individuals do not respond to first-line treatment, are unsuccessful in later attempts, and fail to change over protracted periods ( 14 , 15 ). Nearly 30% of sufferers become chronically ill as a result ( 16 ). For such chronic refractory cases, the paucity of evidence-based treatments has prompted paradigm shifts toward harm reduction and palliative care over recovery ( 17 , 18 ).
Ketamine, a non-competitive N-methyl-D-aspartate receptor (NMDAr) antagonist, is an emerging therapy for treatment-resistant mood disorders ( 19 , 20 ). Single-dose studies have consistently shown rapid antidepressant and anti-suicidal effects following ketamine treatment, though are relatively short-lived (1–4 weeks) ( 21 – 28 ). Ketamine assisted psychotherapy (KAP) has therefore been utilized to prolong ketamine's efficacy and maximize therapeutic outcomes ( 29 – 34 ). To date, few studies have used ketamine for the treatment of eating disorders, including one open-label study ( 35 ), two case reports ( 36 , 37 ), and one longitudinal case series ( 38 ), all of which administered ketamine without a psychotherapeutic component. Nonetheless, the results are encouraging. Here, we report the case of a young woman suffering from extreme and enduring BN, according to CARE (CAse REport) guidelines ( 39 ), who demonstrated remarkable symptom improvement following repeated sessions of KAP.
Case Presentation
A 21-year-old woman with BN of 9 years presented to the outpatient clinic, Forum Health. She was first diagnosed with BN, binge-eating/purging type, at 12.5 years of age to which the severity of her symptoms steadily increased overtime. On presentation, she reported alarming rates of binge-eating and purging by self-induced vomiting, averaging ~40 episodes per day for the last 12 months. Based on this frequency, her BN was categorized as “extreme” according to Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criterion (14 or more episodes per week). Clinical assessment and scoring on the Eating Disorder Examination Questionnaire [EDE-Q; ( 40 , 41 )] additionally confirmed the severity of her illness. No laxative or diuretic abuse was reported. While not active in psychiatric treatment, the patient was taking potassium chloride 20 mEq extended-release twice daily for hypokalemia as well as trazodone 100 mg once daily in the evenings for sleep. At 161.92 cm tall and 46.26 kg in weight [body mass index (BMI) = 17.6 kg per m 2 ], the patient was amenorrheic and described body image disturbances, intense fear of gaining weight, and obsessive-compulsive tendencies around food (counting calories, binging by order of food group, and inability to discard uneaten items). She further displayed pronounced bilateral parotid sialadenosis (enlargement of the salivary glands) and pseudo-idiopathic edema, otherwise known as pseudo-bartter's syndrome (PBS): a rare and painful complication of BN characterized by hyperaldosteronism, metabolic alkalosis, and hypokalemia ( 42 ). As a University student studying cognitive neuroscience, the patient was obliged to take a medical leave due functional decline. “I lost all ability to take care of myself. I could not think clearly or show up for classes. I stopped socializing and running errands. I could hardly maintain basic hygiene.”
Her psychiatric history included an adolescent sexual assault by a treating physician (13 years of age [2011]); a suicide attempt by cut throat injury at the level of the hyoid bone, which required emergency transportation and thyroid cartilage repair as well as inpatient hospitalization (13 years of age [2011]); a second suicide attempt by drug overdose involving mixed opioids, barbiturates, and antidepressants that resulted in emergency room hospitalization (15 years of age [2013]); and a blitz rape (surprise attack) by an unknown assailant (19 years of age [2017]). The patient's history also contained reports of major depression, general anxiety, and obsessive-compulsive disorder. There was no family history of eating disorders, including BN.
As an outpatient, she was treated with various pharmacotherapies (fluoxetine 40 mg once daily, citalopram 20 mg once daily, and naltrexone 50 mg twice daily), behavioral interventions (cognitive behavioral therapy, mindfulness-based stress reduction, and eye movement desensitization and reprocessing), and nutritional counseling (dietary modification and time-based feeding). She additionally was prescribed spironolactone 25 mg twice daily, a potassium-sparing diuretic, on multiple occasions to treat PBS following attempts at purging cessation. However, the patient's binge-purge patterns continued. Finally, she received inpatient, residential, and intensive-outpatient eating disorder care (15–16 years of age [2013–2014]), which the patient described as a “traumatic experience” that resulted in immediate relapse upon discharge.
“My parents pulled me out of class and dropped me off at a center, leaving me there for almost 10 months. It was like being in prison. I was completely cut off from my friends and family. I was forced to eat unreasonable amounts of food at each meal. And I learned new [eating disorder] tricks from other patients that I tried later on. It was not a place conducive to recovery, at least for me. It just made my condition worse.”
Her medical history detailed emergency room hospitalizations for hypokalemia (16, 19, and 20 years of age [2014, 2017, 2018]), gastroesophageal reflux disorder (17–21 years of age [2015–2019]), gastric and duodenal ulcers (19 and 21 years of age [2017, 2019]), hypothyroidism (20–21 years of age [2018–2019]), and adrenocortical insufficiency (20–21 years of age [2018–2019]). Porcelain-laminate veneers were also placed on 10 of her teeth due to dental caries and enamel erosion from chronic purging (21 years of age [2019]).
Given the patient's extreme and chronic refractory state, her physician recommended repeated KAP, with the understanding it constituted an exploratory and off-label intervention for her eating disorder. She consented to treatment following a comprehensive medical evaluation and in-depth review of the procedures, risks, and possible side effects. A signed consent form was obtained. Prior to treatment, she met with a clinical psychologist to establish rapport and therapeutic alliance. The patient then underwent one course of repeated KAP, consisting of six sessions scheduled twice weekly for 3 weeks, with a minimum interval between sessions of 48 h ( Figure 1 ). Each KAP session involved guided psychotherapy combined with racemic ketamine hydrochloride (0.5 mg per kg bodyweight suspended in 0.9% normal saline) administered intravenously over 40 min. The drug regimen was standard practice in the clinic for sub-anesthetic ketamine infusions, which is most commonly used for treating psychiatric disorders and is supported by a substantial body of literature ( 43 , 44 ). A person-centered, humanistic approach to psychotherapy was employed to facilitate the process of self-actualization and therapeutic change. KAP sessions were preceded by 30 min of preparatory psychotherapy and delivered in a private room with dimmed lights, ambient music, and textile art on the ceiling. The intervention components and ketamine regimen remained the same for all five consecutive sessions; and blood pressure, heart rate, and oxygen saturation were continuously monitored. Due to the severity of her eating disorder, however, the patient returned to the clinic 1 month later for a second course of repeated KAP and then again 1 month later for a third.
Figure 1 . Timeline of clinical events. The patient received three courses of repeated KAP for extreme and enduring BN, consisting of six sessions per course scheduled twice weekly for 3 weeks. KAP, ketamine assisted psychotherapy; BN, bulimia nervosa; B/P, binge-eating and purging.
Dissociation, ego dissolution, and perceptual distortions were present during all KAP sessions, as evidenced by the patient's description of “being disconnected from reality,” “losing [her] sense of identity and self,” and “seeing abstract geometric patterns.” She further exhibited mild diplopia (double vision), nystagmus (involuntary oscillations of the eyes), and alogia (lack of speech) during treatment that resolved completely. No other side effects or adverse events were reported. The patient's eating disorder symptoms remitted over the course of treatments, as measured by change in scoring on the EDE-Q as well as entries from a daily tracking log that recorded frequency of binge-eating and purging. On the EDE-Q, her global score dropped from 31.8 at baseline to 15.0 by the end of all three courses (18 sessions), with similar patterns recorded across all four subscales: “Restraint” ( M = 5.0, SD = 2.2 to M = 1.8, SD = 1.3), “Eating Concern” ( M = 5.8, SD = 0.5 to M = 2.2, SD = 1.5), “Weight Concern” ( M = 5.8, SD = 0.5 to M = 4.0, SD = 1.9), and “Shape Concern” ( M = 5.5, SD = 0.8 to M = 2.5, SD = 1.6) ( Figure 2 ). Additionally, the patient's tracking log showed decreases in binge-eating and purging from 40 to 18 episodes per day after the first course of treatment (6 sessions), 18 to 13 episodes per day after the second course of treatment (12 sessions), and 13 to 4 episodes per day after the third course of treatment (18 sessions) ( Figure 3 ).
Figure 2 . Change in scoring on the Eating Disorder Examination Questionnaire (EDE-Q).
Figure 3 . Frequency of daily binge-eating and purging following repeated ketamine assisted psychotherapy.
Most notably, the patient stopped her binge-eating and purging behaviors 3 months post-treatment. Given her initial severity and chronic refractory state, this degree of improvement was striking. The patient's daily tracking log additionally showed no signs of relapse 1 year later, accompanied by marked improvement in psychosocial functioning. Specifically, she reported feeling “free” from intrusive BN thoughts and compulsions, “less impulsive” when faced with the urge to binge and purge, and “more confident” about her body in general. The patient has since resumed her academic studies in preparation for a doctoral program.
Severe, chronic, and refractory eating disorder symptoms are unfortunately common among patients with BN. In this case, we describe a young woman with extreme and enduring BN, who remained unresponsive to first-line treatment for nearly a decade, despite care at the outpatient, residential, and inpatient level. Her eating disorder was extreme, insofar as she engaged in recurrent binge-eating and purging by self-induced vomiting 40 episodes per day, which significantly exceeds DSM-5 criterion (14 or more episodes per week). Given the severity of her illness, complete and sustained remission with three courses of repeated KAP (18 sessions) was both remarkable and unanticipated. These findings are more robust provided the patient was not active in psychiatric treatment for 1 year prior to clinic admission, excluding her long-standing prescription of potassium chloride for hypokalemia and trazodone for sleep. If ketamine and psychotherapy act synergistically, with therapy priming and enhancing the response to treatment, then its combined effect may explain the striking improvements in symptoms. Serial treatments likely account for the durability of response necessary for sustained remission, which is consistent with literature ( 45 – 48 ).
Provided this is the first report of repeated KAP used as an exploratory and off-label intervention for BN, it is important to consider the a-priori context. Clinical recommendation to pursue repeated KAP was prompted by three factors. First, the patient's psychiatric and medical history that detailed unsuccessful treatment attempts, including pharmacotherapies, behavioral treatments, and nutritional counseling—even at higher levels of eating disorder care; and significant trauma to which accumulating evidence has shown ketamine to yield positive effects for ( 49 – 51 ). Second, her severe functional impairment in three major life domains, including academic work, social and family engagement, and personal responsibilities. The patient was binge-eating and purging nearly to the exclusion of all other activities, spending more time “alone in the bathroom than with [her] friends or family.” Finally, an open-label case series on repeated ketamine in severe and enduring anorexia nervosa, showing modest improvements in eating disorder symptoms ( 38 ).
The patient's impetus for treatment was largely driven by fear of premature mortality—that if she did not attempt something new, she was going to “eat [herself] to death,” quite literally. Serious degradation in the patient's physical and mental health status were particularly motivating. Apart from transient psychological (dissociation, ego dissolution, and perceptual distortions) and physiological (mild diplopia, nystagmus, and alogia) side effects of ketamine that resolved completely after each session, the treatment was well-tolerated. Following all three courses of treatment, the patient dramatically reduced her binge-eating and purging behaviors by 90% compared to baseline, as measured by the EDE-Q and daily tracking logs. She also demonstrated considerable improvements in disordered eating psychopathology that were captured by the subscales of the EDE-Q, most notably “Restraint” (e.g., dietary rules and avoidance of food) and “Eating Concerns” (e.g., preoccupation with calories and fear of losing control over eating). Moreover, the patient regained control of her impulsive eating as well as resolved her obsessive-compulsive neurosis, which align with previous BN-specific findings from a study on intermittent ketamine infusions in eating disorders ( 35 ). At 3 months follow-up, she achieved complete cessation of binge-eating and purging and no longer met diagnostic criteria for BN. The magnitude of response neither diminished over time, with no signs of relapse at 15 months follow-up, contrary to studies showing rapid decline of effects after treatment ( 28 , 52 , 53 ). With sustained remission, the patient has adopted a healthier relationship with food, established psychosocial stability in her life, and resumed her academic studies in preparation for graduate school.
This is a single case report with inherent limitations in generalizing the findings to other patients with BN. The lack of polypharmacy or medication washout is an additional limitation that may have unknowingly mediated improvements. Furthermore, it is unclear as to whether ketamine or psychotherapy produced greater clinical benefit, if both are coadjuvant and necessary, or if the treatment would have been as effective without psychotherapy and/or fewer sessions. Finally, a person-centered, humanistic approach to psychotherapy was employed, differing from more traditional methods, such as cognitive-behavioral, interpersonal, and psychodynamic therapy. Open pilot studies as well as fully-powered randomized controlled trials with longitudinal assessment are thus required to establish whether the outcome of this case can be replicated, to what degree ketamine and psychotherapy contribute to the overall success of the treatment, and the comparative efficacy of different psychotherapeutic interventions. Further research is also warranted to optimize KAP duration and frequency for this patient population.
Conclusions
This study provides compelling evidence that repeated KAP is an effective treatment for extreme and enduring BN, which is exceedingly resistant to first-line therapies and associated with poor prognosis. It further highlights the utility of combined strategies that may prolong ketamine's efficacy, and subsequently maximize therapeutic outcomes at the individual level.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
PH-B assessed, treated, and followed-up with the patient. AR interviewed the patient, conceptualized the case report, drafted the manuscript, and developed all figures. LKJ and SC contributed to the literature review and assisted with manuscript preparation. LG, QT, and MR provided substantial contributions to the interpretation of data as well as manuscript revisions. All authors have read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Dr. Andrew Petersen, the lead physician on this case, for his contributions to this study and continued innovation in the field.
Abbreviations
BMI, body mass index; BN, bulimia nervosa; DSM-5, diagnostics and statistical manual of mental disorders, 5th edition; EDE-Q, eating disorder examination questionnaire; KAP, ketamine assisted psychotherapy; NMDAr, N-methyl-D-aspartate receptor; PBS, pseudo-bartter's syndrome.
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5 . 5th ed. Washington DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Grilo CM, Ivezaj V, White MA. Evaluation of the DSM-5 severity indicator for bulimia nervosa. Behav Res Ther. (2015) 67:41–4. doi: 10.1016/j.brat.2015.02.002
3. van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry. (2020) 33:521–7. doi: 10.1097/YCO.0000000000000641
4. Qian J, Wu Y, Liu F, Zhu Y, Jin H, Zhang H, et al. An update on the prevalence of eating disorders in the general population: a systematic review and meta-analysis. Eat Weight Disord. (2021) 1–4. doi: 10.1007/s40519-021-01162-z
5. Himmerich H, Hotopf M, Shetty H, Schmidt U, Treasure J, Hayes RD, et al. Psychiatric comorbidity as a risk factor for the mortality of people with bulimia nervosa. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:813–21. doi: 10.1007/s00127-019-01667-0
6. Dalle Grave R, Sartirana M, Calugi S. Complex Cases and Comorbidity in Eating Disorders: Assessment and Management . Springer Nature (2021). p. 79–97. doi: 10.1007/978-3-030-69341-1
7. Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: a meta-analysis of 36 studies. Arch Gen Psychiatry. (2011) 68:724–31. doi: 10.1001/archgenpsychiatry.2011.74
8. Huas C, Godart N, Caille A, Pham-Scottez A, Foulon C, Divac SM, et al. Mortality and its predictors in severe bulimia nervosa patients. Eur Eat Disord Rev. (2013) 21:15–9. doi: 10.1002/erv.2178
9. Franko DL, Tabri N, Keshaviah A, Murray HB, Herzog DB, Thomas JJ, et al. Predictors of long-term recovery in anorexia nervosa and bulimia nervosa: data from a 22-year longitudinal study. J Psychiatr Res. (2018) 96:183–8. doi: 10.1016/j.jpsychires.2017.10.008
10. Preti A, Rocchi MB, Sisti D, Camboni MV, Miotto P. A comprehensive meta-analysis of the risk of suicide in eating disorders. Acta Psychiatr. Scand. (2011) 124:6–17. doi: 10.1111/j.1600-0447.2010.01641.x
11. Cucchi A, Ryan D, Konstantakopoulos G, Stroumpa S, Kaçar AS, Renshaw S, et al. Lifetime prevalence of non-suicidal self-injury in patients with eating disorders: a systematic review and meta-analysis. Psychol Med. (2016) 46:1345–58. doi: 10.1017/S0033291716000027
12. Mitchell JE, Agras S, Wonderlich S. Treatment of bulimia nervosa: where are we and where are we going? Int J Eat Disord. (2007) 40:95–101. doi: 10.1002/eat.20343
13. Vocks S, Tuschen-Caffier B, Pietrowsky R, Rustenbach SJ, Kersting A, Herpertz S. Meta-analysis of the effectiveness of psychological and pharmacological treatments for binge eating disorder. Int J Eat Disord. (2010) 43:205–17. doi: 10.1002/eat.20696
14. Wonderlich S, Mitchell JE, Crosby RD, Myers TC, Kadlec K, LaHaise K, et al. Minimizing and treating chronicity in the eating disorders: a clinical overview. Int J Eat Disord. (2012) 45:467–75. doi: 10.1002/eat.20978
15. Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery from anorexia nervosa and bulimia nervosa at 22-year follow-up. J Clin Psychiatry. (2017) 78:184–9. doi: 10.4088/JCP.15m10393
16. Steinhausen HC, Weber S. The outcome of bulimia nervosa: findings from one-quarter century of research. Am J Psychiatry. (2009) 166:1331–41. doi: 10.1176/appi.ajp.2009.09040582
17. Westmoreland P, Mehler PS. Caring for patients with severe and enduring eating disorders (SEED): certification, harm reduction, palliative care, and the question of futility. J Psychiatr Pract. (2016) 22:313–20. doi: 10.1097/PRA.0000000000000160
18. Strand M, Sjöstrand M, Lindblad A. A palliative care approach in psychiatry: clinical implications. BMC Med Ethics. (2020) 21:29. doi: 10.1186/s12910-020-00472-8
19. Park LT, Falodun TB, Zarate CA Jr. Ketamine for treatment-resistant mood disorders. Focus. (2019) 17:8–12. doi: 10.1176/appi.focus.20180030
20. Wilkinson ST, Sanacora G. A new generation of antidepressants: an update on the pharmaceutical pipeline for novel and rapid-acting therapeutics in mood disorders based on glutamate/GABA neurotransmitter systems. Drug Discov Today. (2019) 24:606–15. doi: 10.1016/j.drudis.2018.11.007
21. Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, et al. Antidepressant effects of ketamine in depressed patients. Biol Psychiatry. (2000) 47:351–4. doi: 10.1016/S0006-3223(99)00230-9
22. Zarate CA, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. (2006) 63:856–64. doi: 10.1001/archpsyc.63.8.856
23. Diazgranados N, Ibrahim L, Brutsche NE, Newberg A, Kronstein P, Khalife S, et al. A randomized add-on trial of an N-methyl-D-aspartate antagonist in treatment-resistant bipolar depression. Arch Gen Psychiatry. (2010) 67:793–802. doi: 10.1001/archgenpsychiatry.2010.90
24. Zarate CA Jr., Brutsche NE, Ibrahim L, Franco-Chaves J, Diazgranados N, Cravchik A, et al. Replication of ketamine's antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry. (2012) 71:939–46. doi: 10.1016/j.biopsych.2011.12.010
25. Murrough JW, Iosifescu DV, Chang LC, Al Jurdi RK, Green CE, Perez AM, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. (2013) 170:1134–42. doi: 10.1176/appi.ajp.2013.13030392
26. Lapidus KA, Levitch CF, Perez AM, Brallier JW, Parides MK, Soleimani L, et al. A randomized controlled trial of intranasal ketamine in major depressive disorder. Biol Psychiatry. (2014) 76:970–6. doi: 10.1016/j.biopsych.2014.03.026
27. Lai R, Katalinic N, Glue P, Somogyi AA, Mitchell PB, Leyden J, et al. Pilot dose–response trial of iv ketamine in treatment-resistant depression. World J Biol Psychiatry. (2014) 15:579–84. doi: 10.3109/15622975.2014.922697
28. Marcantoni WS, Akoumba BS, Wassef M, Mayrand J, Lai H, Richard-Devantoy S, et al. A systematic review and meta-analysis of the efficacy of intravenous ketamine infusion for treatment resistant depression: January 2009–January 2019. J Affect Disord. (2020) 277:831–41. doi: 10.1016/j.jad.2020.09.007
29. Krupitsky EM, Grinenko AY. Ketamine psychedelic therapy (KPT): a review of the results of ten years of research. J Psychoactive Drugs. (1997) 29:165–83. doi: 10.1080/02791072.1997.10400185
30. Kolp E, Young MS, Friedman H, Krupitsky E, Jansen K, O'Connor L. Ketamine-enhanced psychotherapy: preliminary clinical observations on its effects in treating death anxiety. Int J Transpers Stud. (2007) 26:1–7. doi: 10.24972/ijts.2007.26.1.1
CrossRef Full Text | Google Scholar
31. Calabrese L. Titrated serial ketamine infusions stop outpatient suicidality and avert ER visits and hospitalizations. Int J Psychiatr Res. (2019) 2:1–2. Available online at: http://scivisionpub.com/pdfs/titrated-serial-ketamine-infusions-stop-outpatient-suicidality-and-avert-er-visits-and-hospitalizations-918.pdf
32. Dore J, Turnipseed B, Dwyer S, Turnipseed A, Andries J, Ascani G, et al. Ketamine assisted psychotherapy (KAP): patient demographics, clinical data and outcomes in three large practices administering ketamine with psychotherapy. J Psychoactive Drugs. (2019) 51:189–98. doi: 10.1080/02791072.2019.1587556
33. Wheeler SW, Dyer NL. A systematic review of psychedelic-assisted psychotherapy for mental health: an evaluation of the current wave of research and suggestions for the future. Psychol Conscious. (2020) 7:279. doi: 10.1037/cns0000237
34. Halstead M, Reed S, Krause R, Williams MT. Ketamine-assisted psychotherapy for PTSD related to racial discrimination. J Clin Case Stud. (2021) 20:310–30. doi: 10.1177/1534650121990894
35. Mills IH, Park GR, Manara AR, Merriman RJ. Treatment of compulsive behaviour in eating disorders with intermittent ketamine infusions. QJM. (1998) 91:493–503. doi: 10.1093/qjmed/91.7.493
36. Dechant E, Boyle B, Ross RA. Ketamine in a patient with comorbid anorexia and MDD. J Women's Health Dev. (2020) 3:373–5. doi: 10.26502/fjwhd.2644-28840044
37. Scolnick B, Zupec-Kania B, Calabrese L, Aoki C, Hildebrandt T. Remission from chronic anorexia nervosa with ketogenic diet and ketamine: case report. Front Psychiatry. (2020) 11:763. doi: 10.3389/fpsyt.2020.00763
38. Schwartz T, Trunko ME, Feifel D, Lopez E, Peterson D, Frank GK, et al. A longitudinal case series of IM ketamine for patients with severe and enduring eating disorders and comorbid treatment-resistant depression. Clin Case Rep. (2021) 9:e03869. doi: 10.1002/ccr3.3869
39. Gagnier J, Kienle G, Altman DG, Moher D, Sox H, Riley DS, et al. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. (2013) 67:46–51. doi: 10.1111/head.12246
40. Fairburn CG, Cooper Z, O'Connor M. The eating disorder examination. Int J Eat Disord. (1993) 6:1–8.
Google Scholar
41. Fairburn CG, Cooper Z, O'Connor M. Eating Disorder Examination (Edition 16.0 D). In: Fairburn CG, editor. Cognitive Behavior Therapy and Eating Disorders. New York, NY: Guilford Press (2008). p. 265–308.
42. Nitsch A, Dlugosz H, Gibson D, Mehler PS. Medical complications of bulimia nervosa. Clevel Clin J Med. (2021) 88:333–43. doi: 10.3949/ccjm.88a.20168
43. Andrade C. Ketamine for depression, 4: in what dose, at what rate, by what route, for how long, and at what frequency? J Clin Psychiatry. (2017) 78:e852–7. doi: 10.4088/JCP.17f11738
44. Peyrovian B, McIntyre RS, Phan L, Lui LM, Gill H, Majeed A, et al. Registered clinical trials investigating ketamine for psychiatric disorders. J Psychiatr Res. (2020) 127:1–2. doi: 10.1016/j.jpsychires.2020.03.020
45. Murrough JW, Perez AM, Pillemer S, Stern J, Parides MK, aan het Rot M, et al. Rapid and longer-term antidepressant effects of repeated ketamine infusions in treatment-resistant major depression. Biol Psychiatry. (2013) 74:250–6. doi: 10.1016/j.biopsych.2012.06.022
46. Albott CS, Lim KO, Forbes MK, Erbes C, Tye SJ, Grabowski JG, et al. Efficacy, safety, and durability of repeated ketamine infusions for comorbid posttraumatic stress disorder and treatment-resistant depression. J Clin Psychiatry. (2018) 79:17m11634. doi: 10.4088/JCP.17m11634
47. Phillips JL, Norris S, Talbot J, Birmingham M, Hatchard T, Ortiz A, et al. Single, repeated, and maintenance ketamine infusions for treatment-resistant depression: a randomized controlled trial. Am J Psychiatry. (2019) 176:401–9. doi: 10.1176/appi.ajp.2018.18070834
48. Krystal JH, Abdallah CG, Sanacora G, Charney DS, Duman RS. Ketamine: a paradigm shift for depression research and treatment. Neuron. (2019) 101:774–8. doi: 10.1016/j.neuron.2019.02.005
49. McGhee LL, Maani CV, Garza TH, Gaylord KM, Black IH. The correlation between ketamine and posttraumatic stress disorder in burned service members. J Trauma Acute Care Surg. (2008) 64:S195–9. doi: 10.1097/TA.0b013e318160ba1d
50. Feder A, Parides MK, Murrough JW, Perez AM, Morgan JE, Saxena S, et al. Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. (2014) 71:681–8. doi: 10.1001/jamapsychiatry.2014.62
51. Feder A, Rutter SB, Schiller D, Charney DS. The emergence of ketamine as a novel treatment for posttraumatic stress disorder. Adv Pharmacol. (2020) 89:261–86. doi: 10.1016/bs.apha.2020.05.004
52. aan het Rot M, Collins KA, Murrough JW, Perez AM, Reich DL, Charney DS, et al. Safety and efficacy of repeated-dose intravenous ketamine for treatment-resistant depression. Biol Psychiatry. (2010) 67:139–45. doi: 10.1016/j.biopsych.2009.08.038
53. Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB, et al. Ketamine and other NMDA antagonists: early clinical trials and possible mechanisms in depression. Am J Psychiatry. (2015) 172:950–66. doi: 10.1176/appi.ajp.2015.15040465
Keywords: bulimia nervosa, eating disorder, binge-eating, purging, ketamine, ketamine assisted psychotherapy, psychopharmacology, case report
Citation: Ragnhildstveit A, Jackson LK, Cunningham S, Good L, Tanner Q, Roughan M and Henrie-Barrus P (2021) Case Report: Unexpected Remission From Extreme and Enduring Bulimia Nervosa With Repeated Ketamine Assisted Psychotherapy. Front. Psychiatry 12:764112. doi: 10.3389/fpsyt.2021.764112
Received: 25 August 2021; Accepted: 27 October 2021; Published: 17 November 2021.
Reviewed by:
Copyright © 2021 Ragnhildstveit, Jackson, Cunningham, Good, Tanner, Roughan and Henrie-Barrus. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anya Ragnhildstveit, anya.ragnhildstveit@utah.edu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- June 01, 2024 | VOL. 181, NO. 6 CURRENT ISSUE pp.461-564
- May 01, 2024 | VOL. 181, NO. 5 pp.347-460
- April 01, 2024 | VOL. 181, NO. 4 pp.255-346
- March 01, 2024 | VOL. 181, NO. 3 pp.171-254
- February 01, 2024 | VOL. 181, NO. 2 pp.83-170
- January 01, 2024 | VOL. 181, NO. 1 pp.1-82
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
The Outcome of Bulimia Nervosa: Findings From One-Quarter Century of Research
- Hans-Christoph Steinhausen M.D., Ph.D., D.M.Sc.
- Sandy Weber Cand.Phil.
Search for more papers by this author
Objective: The present review addresses the outcome of bulimia nervosa, effect variables, and prognostic factors. Method: A total of 79 study series covering 5,653 patients suffering from bulimia nervosa were analyzed with regard to recovery, improvement, chronicity, crossover to another eating disorder, mortality, and comorbid psychiatric disorders at outcome. Forty-nine studies dealt with prognosis only. Final analyses on prognostic factors were based on 4,639 patients. Results: Joint analyses of data were hampered by a lack of standardized outcome criteria. There were large variations in the outcome parameters across studies. Based on 27 studies with three outcome criteria (recovery, improvement, chronicity), close to 45% of the patients on average showed full recovery of bulimia nervosa, whereas 27% on average improved considerably and nearly 23% on average had a chronic protracted course. Crossover to another eating disorder at the follow-up evaluation in 23 studies amounted to a mean of 22.5%. The crude mortality rate was 0.32%, and other psychiatric disorders at outcome were very common. Among various variables of effect, duration of follow-up had the largest effect size. The data suggest a curvilinear course, with highest recovery rates between 4 and 9 years of follow-up evaluation and reverse peaks for both improvement and chronicity, including rates of crossover to another eating disorder, before 4 years and after 10 years of follow-up evaluation. For most prognostic factors, there was only conflicting evidence. Conclusions: One-quarter of a century of specific research in bulimia nervosa shows that the disorder still has an unsatisfactory outcome in many patients. More refined interventions may contribute to more favorable outcomes in the future.
The introduction and definition of bulimia nervosa were presented only 30 years ago. In his salient publication, Gerald Russell (1) emphasized the dread of overeating, various compensatory measures, and the morbid fear of gaining weight and getting fat. Within this relatively short period of time, a remarkably large number of outcome studies have been published. Early reviews included one review based on eight studies (2) and another on 24 follow-up studies (3) . The latter found a mean recovery rate of 47.5% and mean rates of 26% for both improvement and chronicity. Shortly before the turn of the century, Keel and Mitchell (4) analyzed the course of 56 patient series and found a recovery rate of 50% and chronicity in 20% of the patients. The mortality rate of 0.3% was slightly lower than that reported in the prior review of 24 studies (3) . The review by Vaz (5) concentrated on prognostic factors only, and Quadflieg and Fichter (6) reviewed various outcome measures in a total of 33 studies. Finally, a recent, more selective review based on very rigorous inclusion criteria by Berkman et al. (7) provided findings from 13 patient series. Steinhausen’s analysis (8) of the outcome of anorexia nervosa in the second half of the last century served as a model for the present review.
Selection criteria for the inclusion of studies in the present review were 1) data on at least one out of five outcome measures for bulimia nervosa after a minimum follow-up evaluation period of 6 months following the treatment episode and/or 2) data on any prognostic factor of the disorder. The aforementioned reviews consisted of a total of 141 studies. A systematic search with various databases was performed using the terms “bulimia nervosa,” “outcome,” “follow-up,” and “prognosis.” A search using PubMed led to an additional 60 studies, and a search using PsycINFO resulted in 19 studies. Thus, before applying any exclusion criteria, a total of 220 published studies were available. As a result of duplicate or review-type studies, 68 studies were excluded. Furthermore, 26 studies did not include sufficient information on the duration of follow-up evaluation or provided pre-post measures only or were based only on follow-up periods <6 months. In another 21 studies, information on the course of the disorder was insufficient (e.g., no information on sample size or no independent assessment of anorexia and bulimia nervosa patients was provided). Finally, there were 14 studies dealing with prognostic factors only, and another 12 studies presented additional data based on the same patient cohort. Thus, at the end, a total of 79 patient series were entered into the analyses for the outcome of bulimia nervosa in the present review. Findings were published between 1981 and 2007. Data based on reports from a total of 32 studies were extracted by the expert senior author. Decisions on the inclusion of the remaining studies were jointly made by both the junior and senior authors.
Study Characteristics
The 79 published reports (9 – 87) were composed of 5,653 patients (group mean size=71.6 [SD=113.4], range=4–884). There were considerable differences in design, group size, methods, duration of follow-up evaluation, and missing data. Diagnostic classification changed considerably over the period in which the studies were conducted. Since the 1990s, there has been an increasing reliance on DSM-IV and ICD-10 criteria. In 46 studies consisting of 2,508 patients, the mean age at onset was 17.2 years (SD=1.7, range=4.3–23.2), and the mean age at follow-up assessment was 28.4 years (SD=4.3, range=16.6–38.0) in 39 studies consisting of 2,478 patients. The mean duration of follow-up evaluation varied between 6 months and 12.5 years (mean=3.2 months [SD=3.3]) in 77 studies of 5,239 patients. In 66 studies of 3,830 patients, a total of 75 men (1.9%) were included.
A minority of studies used combined intervention and follow-up evaluation, whereas the majority of studies used only limited evaluation of treatment effects. The available information on treatment was classified as 1) nonbehavioral psychotherapy, 2) unspecified medical intervention, 3) cognitive-behavioral therapy (CBT), 4) family intervention, or 5) mixed or uncontrolled intervention.
In the analyses for prognostic factors, 35 studies included information on prognostic factors in addition to data on outcome (10 , 14 , 15 , 17 , 21 , 24 , 25 , 30 , 34 – 36 , 40 – 44 , 52 , 54 , 55 , 57 , 61 , 63 , 65 , 68 , 71 – 73 , 75 , 76 , 83 , 88 – 92) , and 14 studies (93 – 106) dealt exclusively with prognostic factors. The total sample of these studies on prognosis consisted of 4,639 patients (mean=94.62 [SD=133.76], range=4–884).
Outcome Measures
The five central outcome criteria for the present analyses were recovery, improvement, chronicity, mortality, and crossover to other eating disorders. In addition, information on comorbid mental disorders was collected. Information on recovery was provided in the studies as part of 1) a three-level classification in combination with improvement and chronicity, 2) a two-level classification mostly in combination with chronicity, or 3) a single criterion. There were 22 synonyms of recovery (e.g., “abstinent”). Improvement was most commonly used as a medium category of a three-level classification. In a few instances, rates of improvement were reported in combination with recovery only. Among the 27 synonyms of improvement were terms such as “intermediate course,” “some remaining symptoms,” or “partial remission.” Finally, among 21 synonyms of chronicity, the most common were “bulimia nervosa,” and “poor course.” Some studies used crossover to another eating disorder according to DSM-IV criteria as an outcome category in addition to recovery and chronicity. All mortality rates represented crude mortality rates. None of the studies reported standardized mortality rates.
Statistical Analyses
The five outcome measures were calculated in percentages that were rounded to the nearest whole value. In order to take into account the large variation in sample sizes, weighted percentages were calculated by weighting each reported rate with the size of the study group. Data for all studies were converted into individual data for performance of statistical analyses using SPSS 14 (SPSS, Chicago).
All analyses were based on adjusted sample sizes at follow-up assessments rather than actual sample sizes after patient recruitment. Differences between these two figures were considered the dropout rate. The latter was dichotomized into high (≥16% of the original sample) and low (0%–15% of the original sample) categories and served as a first independent effect variable. In accordance with previous analyses (8) , the duration of follow-up evaluations was the second independent effect variable and categorized as <4 years, 4 to 9 years, or ≥10 years. Studies with a variable length of course were not considered for analyses of effect. In case there was more than one report based on the same cohort, only the last report with the longest duration of follow-up assessment was considered for the analyses. The third independent variable was represented by the type of intervention. Because of limited data, the aforementioned classification of available information on treatment into five types was restricted to the following three types: nonbehavioral psychotherapy, unspecified medical therapy, and CBT.
Effects of these three variables for treatment type on four outcome measures were analyzed using multivariate analyses of variance. In addition, effect sizes were calculated using partial eta-squared (η 2 ) as a measure of association between independent and dependent variables. According to Cohen (107) , η 2 =0.01–0.059 represents a small effect, η 2 =0.06–0.13 represents a median effect, and there is a large effect starting with η 2 =0.14. Furthermore, the frequencies of positive, negative, and insignificant prognostic factors were calculated.
Main Outcome Findings
Detailed information on crossover diagnoses was available in 23 studies. As shown in Table 1 , more than one-fifth of the patients fulfilled this criterion, with a majority of 16% on average crossing over to eating disorder not otherwise specified, which in most cases was a subclinical manifestation of bulimia nervosa, and nearly 6% on average developed full anorexia nervosa. A few patients developed binge eating disorder.
Seventy-six studies reported on mortality, and there were 14 deaths among 4,309 patients, leading to a crude mortality rate of 0.32%. For two patients, car accidents were the cause of death, four deaths were the result of suicide, one death was the result of a drug overdose, two deaths were caused by an eating disorder, and no causes of death were given for two subjects.
There was a large list of reported comorbid mental disorders. At follow-up assessments, patients most frequently suffered from affective disorders, followed by neurotic disorders (mostly anxiety disorders). Nonspecific personality disorders and borderline personality disorder were also frequent. Substance use disorders were less frequently seen, and obsessive-compulsive and schizophrenia spectrum disorders were described only in a single study.
Findings From Repeated Follow-Up Assessments
A few studies shed some light on the differential course of bulimia nervosa across time. Fichter and Quadflieg (91) published findings after 2-, 6-, and 12-year follow-up evaluations (34) and found substantial improvement in patients who completed longer follow-up assessment periods. Similarly, in the study by Herzog et al. (42) , recovery rates increased between the first follow-up assessment after 2 years and the second follow-up assessment after 7 years, but rates of improvement and chronicity declined correspondingly. Another study on intervention (59) found that the reduction of binge eating episodes and compensatory vomiting and laxative abuse remained constant between the 6- and 12-month follow-up evaluations. A change in outcome rates was observed in two smaller studies. Nevonen and Broberg (64) found a decreased recovery rate and an increased improvement rate between 1 and 2.5 years of follow-up evaluation when comparing individual and group psychotherapy. Similarly, in a very small sample of six patients, Toro et al. (80) observed that all patients were recovered at the first follow-up evaluation, but only four patients remained recovered after 25 years.
Intervention Effects on Outcome
There are various intervention studies on bulimia nervosa that include follow-up assessments. Two studies (28 , 30) compared three types of interventions and found that both interpersonal therapy and CBT were superior to behavior therapy without cognitive components. Other studies reported that CBT was superior to interpersonal therapy (29 , 84) or found no significant differences in the effects of either CBT or the combination of behavior therapy and hypnotherapy (40) . In another study (12) , more patients became symptom-free by the use of a self-help manual rather than CBT. Physical activity, but not diet counseling, was shown to be superior to CBT in one report (78) .
In a study on the optimization of CBT (82) , one group of patients used a self-help manual and received additional CBT when necessary. The other patients received behavior therapy only. There were no significant differences between these two approaches. In a study on the effectiveness of either the antidepressant fluoxetine or interpersonal therapy after a first inefficient phase of CBT (62) , no significant differences between the two approaches were found.
When comparing the effects of the antidepressant desipramine, CBT, or a combination of both measures (11) , CBT or the combined intervention resulted in stronger reduction of symptoms after 24 weeks relative to the pure antidepressant treatment. Adding exposure and response prevention to CBT did not result in improved results (19) . Another study (59) revealed that relative to a coping with stress program, diet counseling led to a more rapid improvement of eating behavior and to reduction and abstinence of binge eating episodes.
Two studies on the effects of family therapy revealed contradictory findings. One study (74) found that family intervention was inferior to individual psychotherapy, whereas family therapy was found to be superior in another study (39) . No significant differences were found in the effectiveness of group versus individual psychotherapy (64) . Finally, a positive effect of after-treatment control visits on the course of bulimia nervosa has been documented (58) .
Effect Variables
As a result of methodological restrictions, the presentation of findings based on effect analyses was limited to the set of 27 studies that used the three-level classification with recovery, improvement, and chronicity, supplemented by the smaller number of studies that provided additional information on rates of diagnoses for crossover to other eating disorders. There were no missing data in this data set.
Dropout rate
Duration of follow-up evaluation.


Bulimia Nervosa Clinical Presentation
- Author: Guido Klaus Wilhelm Frank, MD; Chief Editor: David Bienenfeld, MD more...
- Sections Bulimia Nervosa
- Practice Essentials
- Pathophysiology
- Epidemiology
- Mortality/Morbidity
- Patient Education
- Diagnostic Criteria
- Physical Examination
- Comorbidities
- Complications
- Laboratory Studies
- Imaging Studies
- Other Tests
- Approach Considerations
- Medical Care
- Nonpharmacologic Interventions
- Pharmacologic Treatments
- Surgical Care
- Consultations
- Long-Term Monitoring
- Media Gallery
Bulimia nervosa (BN) is often not diagnosed for many months or even years after onset because of patients' secretiveness about their symptoms, usually associated with a great deal of shame. These patients often see physicians for other problems, such as anxiety, depression, infertility, bowel irregularities, fatigue, or palpitations. Similarly, they may see mental health professionals for mood and anxiety problems, personality issues, relationship issues, histories of childhood or adolescent trauma, or substance abuse, without revealing the presence of an eating disorder.
One common presenting scenario is that of a patient who is concerned about their weight who seeks help with weight loss. Symptoms may include bloating, constipation, and menstrual irregularities. Far less often, people may present with palpitations resulting from arrhythmias, which are often associated with electrolyte abnormalities and dehydration. BN is also often, but not always, characterized by an inappropriate premium placed on slender physical appearance. It is important to note that the diagnostic criteria do not necessarily require an individual to express a desire to lose weight or change their appearance to meet criteria for BN. Some, especially younger patients, may not be able or willing to articulate why they engage in eating disorder behaviors. Others may express a motivation for control, a fear of fullness, or other reasons for their disordered eating behaviors. Failure to make an appropriate eating disorder diagnosis that an individual would otherwise meet criteria for, whether it be anorexia nervosa (AN), BN, or other specified feeding or eating disorder (OSFED), because of a lack of expressed concern or denial of concern about body weight/shape is dangerous for patients’ physical and mental health due to causing delays in diagnosis that can contribute to significant morbidity and mortality.
A dietary history may reveal attempts to control weight by dieting and abstaining entirely from high-calorie foods at all times except during binge eating episodes. Often, an all-encompassing preoccupation with food and eating is present, and recurring cycles of extreme dieting and/or fasting may alternate with gorging behavior. The clinician should inquire further about types of foods and quantities of foods consumed when a patient endorses binging behavior. A binge eating episode, by definition, must constitute consumption of more food than would typically be consumed in a single setting by an individual, so there is some subjectivity in what is a binge. Some patients with AN or with periods of very restrictive eating patterns may endorse a “binge,” but on further inquiry may be describing an episode that would be either less than or normative for typical eating for a non-eating-disordered individual but perceived subjectively as a binge eating episode. In the context of highly restrictive eating, any instance of normative eating, such as consuming a dessert, eating high-calorie snacks, or even allowing oneself to eat until feeling full, might appear to be binge eating to an individual who is used to eating very little amounts of food most of the time.
Most patients self-induce vomiting by gagging themselves with their fingers or a toothbrush. Some patients are able to regurgitate reflexively, without requiring external stimulation of the pharynx. [ 34 ] A minority of patients will chew, then regurgitate, without actually swallowing the food. One particularly dangerous form of vomiting is via induction through the use of emetics (eg, ipecac). Ipecac is a tightly binding and slowly released mycotoxin that may lead to fatal cardiomyopathy in habitual users. Up to 40% of patients misuse laxatives, thinking that their use will help them lose weight. In fact, laxative misuse results in additional dehydration and often electrolyte abnormalities as well. Screening for laxative use should be a routine topic of assessment.
For children and adolescents, the parents/guardians of the patient should be asked to check for signs of vomiting and laxative misuse in the home when the patient is denying purging behavior but there is a strong suspicion of purging behaviors occurring. Indications of surreptitious purging behaviors that parents/guardians should be instructed to look for in the home include hidden vomitus in concealed places in the home (eg, closets, floorboards), concealed laxatives in the patients’ room or belongings, clogged drains with vomit, vomit in trash cans, and so on. The parents/guardians should also be instructed to be observant for other signs of purging behavior both for diagnostic and preventative purposes such as unusual online orders (which could be for laxatives or other emetics) and unusually long periods of time spent in the bathroom or shower, which may or may not be after meals and may or may not be accompanied by retching noises. For both children and adults, collateral informants can be very useful sources of information for the clinician about surreptitious purging or other eating disorder behaviors.
Clinicians should be aware of misconceptions that eating disorders are almost exclusively present in young women to avoid missing diagnoses of BN or other eating disorders in male patients or older patients. Additionally, it is a misconception that eating disorders, including BN, mostly occur in White women and people from Western cultures. While research is still evolving on the epidemiology of BN and other eating disorders in males, older individuals, people in developing countries, and so on, in the authors’ clinical experiences, we have encountered a great many patients with BN and other eating disorders who are male, not White, and of a great many different ethnic and racial backgrounds.
Patients with BN may experience the following symptoms:
General - Dizziness, lightheadedness, palpitations (due to dehydration, orthostatic hypotension, possibly hypokalemia)
Gastrointestinal symptoms - Pharyngeal irritation, abdominal pain (more common among persons who self-induce vomiting), blood in vomitus (from esophageal irritation and more rarely actual tears, which may be fatal), difficulty swallowing, bloating, flatulence, constipation, and obstipation
Pulmonary symptoms - Uncommonly aspiration pneumonitis or, more rarely, pneumomediastinum
A high index of suspicion is required in any depressed or anxious weight-conscious young woman.
A set of screening questions, such as the SCOFF mnemonic questionnaire, [ 35 ] is useful to obtain a quick impression as to the potential need for further in-depth questioning. The SCOFF questionnaire includes the following 5 questions:
Do you make yourself S ick because you feel uncomfortably full?
Do you worry you have lost Co ntrol over how much you eat?
Have you recently lost more than O ne stone (about 14 lbs or 6.35 kg) in a 3-month period?
Do you believe yourself to be F at when others say you are too thin?
Would you say that F ood dominates your life?
The Eating Disorder Screen for Primary Care (ESP) questionnaire is an alternative screening tool. [ 36 ] It contains the following 5 questions:
Are you satisfied with your eating patterns?
Do you ever eat in secret?
Does your weight affect the way you feel about yourself?
Have family members suffered from an eating disorder?
Do you currently suffer with or have you in the past suffered with an eating disorder?
The Eating Attitudes Test (EAT) is a self-report population-based screening instrument that patients can complete in the waiting room prior to seeing the health care provider. [ 37 ] (See Psych Central for more information.)
Family history of eating disorders, anxiety, mood disorders, and alcohol and/or substance abuse/dependence may contribute to the risk of BN and should be investigated.
Generally, patients with BN are more likely than controls to view their families as conflicted, badly organized, non-cohesive, and lacking in nurturance and caring. These patients have also been shown to more often appear to be angrily submissive to hostile and neglectful parents.
Perceptions of appearance-related teasing by family members may be present. [ 38 ]
For individuals still living with their parents, careful assessment of the family’s dynamics should be undertaken.
Physiological abnormalities
Many physiological abnormalities may be seen in association with eating disorders, but virtually all appear to be consequences of the abnormal behaviors, not their causes. In most cases of BN, laboratory abnormalities are relatively minor. In cases of very frequent purging (eg, daily or multiple times per day), abnormalities in electrolyte and serum amylase levels occur, but these and most other laboratory abnormalities are reversible with weight restoration and cessation of compensatory behaviors.
Among the identified metabolic consequences sometimes seen in BN are low plasma insulin, C peptide, triiodothyronine, and glucose values, as well as increased beta-hydroxybutyrate and free fatty acid levels. Both fasting and post-binge/post-vomiting hypoglycemia are sometimes seen in some patients with BN. Some studies suggest increased secretory diurnal amplitudes in cortisol and adrenocorticotropic hormone (ACTH) in BN as well as blunted responses to corticotrophin-releasing hormone (CRH). However, these findings have been inconsistent among research studies.
Reports have also suggested abnormal responses to dexamethasone suppression like those seen in AN and major depressive disorder, more common among individuals with significant dietary restriction. Some authors have attributed these abnormalities to impaired dexamethasone absorption, which is demonstrated in some patients with BN. Similar to findings in AN, patients with BN tend to have higher growth hormone levels at night, while nocturnal prolactin levels tend to be less than those seen in controls.
About half of women with BN have anovulatory cycles, while about 20% have luteal phase defects. Patients with anovulatory cycles generally have impaired luteinizing hormone pulsatile secretion patterns and associated reduced estradiol and progesterone pulse amplitudes. [ 39 , 40 ]
Although the implications of many research findings are still unclear, and none of the following offer clinical tests of any merit, reports suggest involvement of the serotonin transporter, [ 41 , 42 ] autoantibodies against neuropeptides, [ 43 ] various chromosome regions, [ 44 ] brain-derived neurotrophic factor, [ 45 ] and peptides leptin and ghrelin. [ 46 ] In a few instances, cerebral hemispheric lesions may be involved in pathogenesis. [ 47 ] Regional cerebral blood flow abnormalities have been noted in adolescents. [ 48 ] Endogenous opioids and beta-endorphins have been implicated in the maintenance of binge eating. Therefore, diagnosis of BN and other eating disorders should be made mostly on the basis of interview with the patient and their collateral informants as well as behavioral observation at times (eg, purging witnessed by family or a staff member). Laboratory tests and physical examination can provide important information about comorbid medical sequelae of BN, but diagnosis requires a thorough diagnostic interview and clinical history.
The underlying causes for buimia nervosa (BN) remain elusive. However, a variety of biological and psychological factors have been suggested to be involved the development of BN.
Behavioral traits
BN has long been associated with inadequate mechanisms to control food intake beyond ones physiological needs, and behavioral traits could contribute. [ 183 , 184 , 185 , 186 , 187 ]
Emotion regulation has been defined as the “extrinsic and intrinsic process responsible for monitoring, evaluating, and modifying emotional reactions, to accomplish one’s goals." [ 188 ] A disturbance in emotion regulation has been found in eating disorders. [ 189 ] Individuals with BN have difficulties modulating strong emotions and controlling rash, impulsive response. [ 190 ] Most but not all studies suggest that negative affect precedes binge eating episodes, [ 191 ] followed by initial relief. [ 192 , 193 ]
Impulsivity, the “opposite to aspects of executive function,” [ 194 ] is a tendency to act with insufficient forethought, or a predisposition toward rapid, unplanned reactions to internal or external stimuli without regard for the negative consequences of these reactions. Impulsivity has relevance for binge eating behaviors, as those episodes typically occur impulsively in response to an external or internal trigger. Increased impulsivity had been found across BN. [ 195 , 196 ] Overall, the literature on executive function in BN is limited, but there is evidence that altered impulsivity and executive function distinguish binge eating individuals from normal weight or obese controls.
Negative urgency, the tendency to experience strong impulses under the influence of negative emotions, or to act rashly when distressed, is related to emotion regulation and impulsivity and has been associated with binge eating. [ 197 , 198 ] Negative urgency is a trait that is triggered by negative affect and may result in binge eating in vulnerable individuals. [ 199 , 200 , 201 , 202 , 203 , 204 ] Interestingly, negative urgency and affect seem to be more relevant than impulsivity, at least for some with binge eating. [ 205 ]
Sensitivity to reward and punishment described in the reinforcement sensitivity theory (RST) provides a framework for how differences in brain systems' responsiveness to reward and punishment are reflected in individual personality. [ 206 , 207 ] Reward sensitivity influences decision making in eating disorders. [ 208 ] Sensitivity to reward was found elevated in BN and it has been hypothesized that an imbalance between reward sensitivity, impulsivity and inhibition are mechanistically involved in binge eating. [ 209 , 210 , 211 ] In addition, individuals with binge eating behaviors showed greater risk taking, and obese binge eating disorder has been associated with altered value computation and discrimination of salient stimuli. [ 212 ]
Taken together, emotion regulation, impulsivity, negative affect, negative urgency, and sensitivity to reward have been linked to binge eating and may create a vulnerability for developing or perpetuation BN behaviors. [ 213 ] However, we do not have a transdiagnostic model for their underlying neurobiology.
Neurocircuitry of emotion regulation, impulsiveness, and cognitive control in BN
A complex interplay exists between emotion regulation and cognitive control. Emotions affect attention, drive cognitive bias, and may interrupt proper decision making; on the other hand, attention to specific goals can control emotions and override strong feelings. [ 214 , 215 , 216 ] Control of food cravings is thought to involve prefrontal cortical areas, whereas greater caloric intake has been related to higher activation in gustatory cortex and brain regions for reward computation. [ 217 , 218 , 219 ] Little is known about how emotion regulation and cognitive control circuits affect binge eating. One study found reduced prefrontal cortical activity in BN when viewing food pictures. [ 220 ] BN showed hypoactivity in brain areas involved in self-regulation and impulse control, such as the prefrontal cortex or insula. [ 221 , 222 , 223 , 224 ] Only one study directly investigated negative affect in relation to binge eating in BN, finding a positive correlation between negative affect and striatal brain response during anticipation of a milkshake. [ 225 ] Altogether, studies suggest altered brain function related to emotion regulation in individuals with binge eating, but the literature is inconsistent.
Neurotransmitters and hormones
Animal models have shown that dopamine, serotonin, acetylcholine, and norepinephrine have all been associated with cognitive control and impulse control in frontal cortical circuits. [ 226 , 227 ] For instance, dopamine D2 and serotonin 2A and 2C receptor signaling can modulate impulsivity. [ 228 , 229 ] Human studies in BN found that serotonin 1A or dopamine D2/3 receptor binding correlated with harm avoidance or behavior inhibition. [ 230 , 231 ] Endocrine factors such as ghrelin, leptin, sex hormones, and cortisol can influence food intake behaviors, [ 232 ] but how they contribute to eating disorders is still elusive. [ 233 , 234 ] Basic research on the gut–brain axis showed how leptin or ghrelin activate brain stem and ventral striatum to activate dopamine circuits and motivation to eat. [ 231 , 234 ] Stress, via cortisol and gut hormone activation, leads to dopamine-mediated decreased food intake in animals, although in humans stress often leads to increased food intake, suggesting a different pathophysiology. [ 235 ] Dopamine drives motivation and food approach, while hedonic aspects of food intake (“liking”) are processed by opioids. [ 236 , 237 ] Those systems could be altered premorbidly as a vulnerability factor but also change in response to extremes of eating, which is an important part of our overall model of eating disorder pathophysiology. [ 238 ] Dopamine has a unique position. It is the only neurotransmitter that we have a mathematical understanding of neuronal function for, which can be used for computational modeling of brain function. Dopamine mediates reward learning [ 239 ] and has been implicated in the pathophysiology of taste and reward processing in eating disorders using the so-called prediction error model, which provides a very strong framework to study reward function in eating disorders. [ 240 , 241 , 242 , 243 , 244 ]
Although patients with bulimia nervosa (BN) are often unremarkable in general appearance and frequently have no signs of illness on physical examination, several characteristic findings may occur.
Physical findings may include the following:
- Bilateral parotid enlargement, largely consequent to noninflammatory stimulation of the salivary glands, may be seen. [ 65 ] See parotid gland swelling in following image.
Parotid hypertrophy. Reprinted with permission from Mandel, L and Siamak, A. Diagnosing bulimia nervosa with parotid gland swelling. J Am Dent Assoc 2004, Vol 135, No 5, 613-616.

See the list below:
- In patients with significant self-induced vomiting, erosions of the lingual surface of the teeth, loss of enamel, periodontal disease, and extensive dental caries may be observed, as in the following image. [ 66 ]
Dental caries. Reprinted with permission from Wolcott, RB, Yager, J, Gordon, G. Dental sequelae to the binge-purge syndrome (bulimia): report of cases. JADA. 1984; 109:723-725.
- Russell sign (one of the few physical examination findings in psychiatry) manifests as callosities, scarring, and abrasions on the knuckles secondary to repeated self-induced vomiting. [ 67 ]
Russell sign. Reprinted with permission from Glorio R, et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int J Derm, 2000, 39(5), 348-353.

Other cutaneous manifestations can include telogen effluvium (sudden, diffuse hair loss), acne, xerosis (dry skin), nail dystrophy (degeneration), and scarring resulting from cutting, burning, and other self-induced trauma. [ 68 ]
Other nonspecific but suggestive findings that may reflect the severity of the disease include bradycardia or tachycardia, hypothermia, and hypotension (often associated with dehydration). Edema, particularly of the feet (and less commonly the hands), is found more often among patients with a history of diuretic abuse, laxative abuse, or both or in patients with significant protein malnourishment causing hypoalbuminemia.
Some patients may be clinically obese, but morbid obesity is rare. Patients with BN who are overweight may have excessive fat folds that favor humidity and maceration with bacterial and fungal overgrowth, striae due to skin overextension, stasis pigmentation related to peripheral vascular disease, and plantar hyperkeratosis due to increased weight. [ 68 ]
A community-based household survey involving 52,095 adults in 19 countries found, after adjustment for pertinent comorbidities, that the rate of BN among the 2580 identified cases of adult-onset diabetes mellitus was twice that of non-diabetic individuals. [ 69 ]
A typical Mental Status Examination for a patient with BN is detailed below. (The formal Folstein Mini-Mental Status Examination [MMSE] is usually unnecessary in the evaluation of patients with BN because symptoms of dementia and delirium are not common in these patients.)
Appearance: Patients are typically neat, well dressed, and show attention to detail. Grooming is often meticulous and may further demonstrate a patient's concern about personal appearance.
Behavior: Patients usually do not have kinetic abnormalities, but anxious feelings may heighten psychomotor agitation. Movements are spontaneous, and patients generally are cooperative and able to carry out requested tasks.
Cooperation: Patients generally avoid eye contact due to shame and embarrassment.
Mood and affect: Patients often demonstrate a depressed mood but may also have significant anxiety.
Speech: Content and articulation are generally normal.
Thought process: Patients likely have a linear thought process that is goal-directed.
Thought content: Thoughts tend to revolve around food and concerns regarding body image and weight.
Perceptual disturbances: Delusions and hallucinations are typically absent.
Suicidal ideation: Suicidal ideation is a significant consideration, especially in patients with depressed moo. Although suicidal ideation is often restricted to thoughts rather than concrete plans, suicidal thinking should be taken very seriously.
Homicidal ideations: Homicidal ideation is not typically associated with those diagnosed with BN.
Cognition: Patients are generally alert, and oriented to their surroundings. Attention and concentration typically measured by serial sevens and digit span are generally normal. Immediate memory is normal, as is recent and remote memory recall. Intellect is usually judged as normal, and in some cases, intellect ability may surpass average. Capacity to read and write is within normal limits. Visuospatial functions are also intact.
Judgment: Patients generally demonstrate poor judgment regarding self-care and treatment. Weight-reducing strategies such as induced vomiting, laxative, and diuretic ingestion are often perceived as legitimate and appropriate methods of weight management.
Insight: Insight regarding the presence and significance of disturbances is variable. While patients typically admit to episodes of binge eating, they often do not appreciate their inappropriate fixation on eating or their distorted ideas of body image and weight.
A national comorbidity study examined lifetime comorbidities of other psychiatric diagnoses in conjunction with bulimia nervosa (BN). [ 10 ] In general, the lifetime comorbidity of any psychiatric disorder is 94.5%.
Affective disorders
The common co-occurrence of eating disorders with affective disorders suggests a possible relationship between them. [ 49 ] Major depressive disorder (MDD) is particularly common (approximately 50%) in this regard. Whether the association is causative (primary), secondary to the BN itself, or represents a common set of risk factors for BN and MDD is still unclear. Depressive symptoms can occur during pregnancy and postpartum in women with BN. [ 50 ] Bipolar II disorder also appears to be more common in patients with BN than in patients without eating disorders. The lifetime comorbidity for bipolar I or II is 17.7%.
Anxiety disorders
Obsessive-compulsive disorder (OCD) is more common in persons with BN (17.4% lifetime comorbidity) than in controls. Panic disorder , social phobia , specific phobias , generalized anxiety disorder (GAD), and posttraumatic stress disorder (PTSD) significantly contribute to comorbidity. Lifetime comorbidities have been reported at approximately 17.4% for OCD, 16.2% for panic disorder, 41.3% for social phobia, 50.1% for specific phobias, 11.8% for GAD, and 45.4% for PTSD.
One study suggests that baseline clinical predictors such as female gender and family history of eating disorders might be specific to the later development of eating disorders in the context of childhood OCD. [ 51 ]
Substance use disorders
Some evidence suggested a relationship between disorders of substance abuse and dependence and BN, including alcohol dependence, [ 52 ] nicotine dependence, [ 53 ] and drug dependence. [ 54 ] For example, with regard to smoking in healthy controls, there were significantly more smokers among people with bulimia (lifetime OR = 2.165) and BED (lifetime OR = 1.792), but not for those with AN (lifetime OR = 0.927). Studies on caffeine intake are mixed. [ 55 ] Alcohol abuse or dependence has a lifetime comorbidity with BN of 33.7%, whereas illicit drug abuse or dependence has a lifetime comorbidity of 26%.
Impulse control disorders
In a study of lifetime prevalence of impulse control disorders in patients with BN, compulsive buying, and intermittent explosive disorder were the most frequently reported disorders, at 17.6% and 13.2%, respectively. Higher than expected rates of kleptomania, pathological gambling, and trichotillomania have also been reported in patients with BN. [ 56 ]
Attention deficit hyperactivity disorder (ADHD)
ADHD may be associated with BN. [ 57 ] In one study of more than 2000 female inpatients treated for BN, 9% were also diagnosed with ADHD. The average rate of ADHD in the general population of young women is approximately 3.4%. [ 58 ] Lifetime comorbidity with ADHD and BN has been reported to be as high as 34.9%.
Other psychopathology
The role of sexual abuse in the development of eating disorders is controversial. [ 59 ] Some reports suggest a strong association, while others detect no increased association. Borderline personality disorder is found frequently. [ 60 ] These patients usually have histories of trauma and abuse and may represent a distinct subgroup. Pathologic narcissism [ 61 ] and identity impairment [ 62 ] may be present. Features of obsessive-compulsive personality disorder (OCPD), particularly perfectionism, may be increased among patients with BN.
Suicidal behavior
BN is associated with increased risk of suicide attempts and suicidal ideations. [ 63 ] In one study, all-cause mortality rate for BN was 3.9%, higher than other studies reported in the past. [ 64 ] However, the standardized mortality ratio with respect to suicide was 6.51, a much higher than expected rate.

Psychiatric complications
Studies suggest that patients with bulimia nervosa (BN) have increased rates of major depressive disorder, substance abuse, anxiety disorders, bipolar II disorder, and sexual abuse; these conditions should be considered and managed as necessary. Mortality and morbidity associated with depression (suicidal thoughts or self-injury) and poor impulse control (eg, substance abuse, sexually transmitted diseases, unintended pregnancy, accidental injuries) should always be anticipated and assessed. Patients with BN who are depressed and who have concurrent alcohol dependence are at exceptionally high risk of suicide, particularly those who overexercise. Studies have shown that in people with eating disorders, excessive exercise appears to be linked to an increased prevalence of acquired capability for suicide (ACS) and suicide attempts. [ 75 , 76 ]
Medical complications
The all-cause mortality rate for BN per se is slightly lower than for anorexia nervosa (AN) (3.9% vs 4.0%, respectively). [ 64 ] Medical complications do arise and should be assessed carefully.
While the results of formal gastric emptying studies in patients with BN have yielded variable results (some suggesting delayed emptying time and others suggesting normal emptying time), acute gastric dilatation is a rare but concerning risk. This complication may result in gastric rupture, which may be fatal.
Among other rare potential complications are Mallory-Weiss tears of the esophagus, esophageal rupture, reflux esophagitis, and cardiomyopathies secondary to ipecac use.
Ipecac toxicity may be associated with skeletal myopathy, while chronic hypokalemia may also be associated with intestinal ileus, abdominal distension, exertional rhabdomyolysis, or both.
Hypokalemia-related distal renal tubulopathy is very rarely associated with BN.
Xerosis (dry skin) is a common finding in bulimia nervosa, which appears to be related to the chronic dehydration to which persons with BN are often prone.
Skin health usually requires an overall healthy nutritional status. Dermatological treatment is ordinarily topical.
Patients who chronically overuse and abuse laxatives risk chronic constipation, cathartic colon with pseudo-Hirschsprung syndrome, melanosis coli with increased risk for colon cancer, steatorrhea, and/or protein-losing enteropathy and metabolic consequences of hypophosphatemia and hypomagnesemia.
Other potential complications include osteopenia or osteoporosis, menstrual irregularity and infertility, and, less commonly, cognitive changes associated with dehydration and electrolyte and metabolic abnormalities.
A 21-year-old woman is brought into an outpatient clinic by her mother, who complains that her daughter has been demonstrating unusual eating patterns since she moved back home 6 months ago. Her mother observes her to eat large amounts of food, such as desserts, when she is alone, often finding food wrappers hidden in her daughter’s room. She is worried that her daughter may be engaging in vomiting after these episodes of heavy eating. She often isolates herself in the bathroom for 10–20 minutes after a large meal.
When the patient was asked about her eating habits, she admitted to a “loss of control.” She described feeling deep remorse when she eats more than she would like. Furthermore, she described feeling so laden with guilt about her eating binges that she purposefully induces vomiting at least once every other day. This act gives her tremendous relief. She admits that she is unhappy with her overall appearance and feels that she is “fat” and “out of shape.” She is preoccupied with her appearance and says that she compares herself to other women “all day long.” She also admits to feeling sad most days. She endorses experiencing occasional missed menstrual periods, low libido, low energy, and intermittent sore throat.
Historically, the patient has memories of a chaotic childhood. She is an only child whose parents fought often and finally divorced when she was 9 years old. The patient remembers the first time she induced vomiting at 10 years old, after she felt “too full after a large meal.” The mother describes her daughter as having few friends and as tending to isolate herself. However, the mother describes her as very bright; in fact, she was valedictorian of her high school.
On physical examination, the patient’s blood pressure is 90/60, heart rate is 100, and BMI is 19. Her oropharynx appears injected without areas of erosion, and multiple dental caries are seen. Bilateral parotid enlargement with minor tenderness is present. The patient is tachycardic and bowel sounds are hyperactive. The abdomen is soft, nontender, and nondistended. Skin turgor is poor.
On mental status examination, the patient presents as a young White woman with average body habitus and pale skin. She is meticulously dressed and groomed. She answers questions curtly, makes poor eye contact, and demonstrates mild foot tapping throughout the interview. Her mood is anxious, and her affect is mood congruent but restricted to negative emotionality. She is highly articulate. Thought process is linear and goal directed. Methodical about her statements, she often takes time to clarify what she “really means.”
Thought content displays themes of shame and self-reproach, [ 33 ] though it is unclear whether shame is a risk factor for the development of the eating problems or a consequence of these difficulties; while guilt may be present, its role is unclear. No active delusions or hallucinations are present. Her cognition is grossly intact. She denies suicidal thoughts, but sometimes wishes she was “invisible.” She has no violent or homicidal thoughts. Insight is limited regarding her ability to acknowledge her psychiatric illness. Her judgment is impaired considering her inability to recognize the potential negative health consequences of her eating behaviors.
Prior to entering the clinic, laboratory assessment obtained at the suggestion of the patient's primary care doctor reveals a serum potassium level of 3.8 Meq/L and serum amylase level of 140 Units/L.
Take-home points
- The differential diagnosis of BN includes depression, anxiety and age-appropriate developmental problems (eg, lack of esteem). These issues are common comorbidities.
- A biopsychosocial treatment plan will be necessary to provide the patient with the care she needs.
- Developing a treatment team and collaboration with primary care providers and psychotherapist is often necessary for the short term and sometimes for the long term.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders . 5th ed, Text Revision. Washington DC: American Psychiatric Association; 2013.
Mehler PS, Birmingham LC, Crow SJ, Jahraus JP. Medical Complications of Eating Disorders. Grilo CM, Mitchell JE. The Treatment of Eating Disorders: A Clinical Handbook . New York: The Guilford Press; 2010. 66.
Brown CA, Mehler PS. Medical complications of self-induced vomiting. Eat Disord . 2013. 21 (4):287-94. [QxMD MEDLINE Link] .
Brown CA, Mehler PS. Successful "detoxing" from commonly utilized modes of purging in bulimia nervosa. Eat Disord . 2012. 20 (4):312-20. [QxMD MEDLINE Link] .
Denholm M, Jankowski J. Gastroesophageal reflux disease and bulimia nervosa: a review of the literature. Dis Esophagus . 2011 Feb. 24 (2):79-85. [QxMD MEDLINE Link] .
Treasure J, Claudino AM, Zucker N. Eating disorders. Lancet . 2010 Feb 13. 375(9714):583-93. [QxMD MEDLINE Link] .
Academy for Eating Disorders' (AED) Medical Care Standards Committee. Eating Disorders: A Guide to Medical Care — Academy for Eating Disorders Report 2021 . 4th ed. [Full Text] .
Crone C, Fochtmann LJ, Attia E, Boland R, Escobar J, Fornari V, et al. The American Psychiatric Association Practice Guideline for the Treatment of Patients With Eating Disorders. Am J Psychiatry . 2023 Feb 1. 180 (2):167-171. [QxMD MEDLINE Link] .
Hudson, JI, Hirpi, E, Pope, HG, et al. The prevalence and correlates of eating disorders in National Comorbidity Survey Replication. Biol Psychiatry . 2—7;61:348-358.
Ghaderi A, Odeberg J, Gustafsson S, Råstam M, Brolund A, Pettersson A, et al. Psychological, pharmacological, and combined treatments for binge eating disorder: a systematic review and meta-analysis. Peer Journal . 2018 Jun. 21;6:e5113. doi: 10.7717/peerj.5113. eCollection 2018. [QxMD MEDLINE Link] .
Goldfield GS, Blouin AG, Woodside DB. Body image, binge eating, and bulimia nervosa in male bodybuilders. Can J Psychiatry . 2006 Mar. 51(3):160-8. [QxMD MEDLINE Link] .
Arthur-Cameselle JN, Burgos J, Burke J, Cairo J, Colón M, Piña ME. Factors that assist and hinder efforts towards recovery from eating disorders: a comparison of collegiate female athletes and non-athletes. Eat Disord . 2018 Nov-Dec. 26(6):538-55. [QxMD MEDLINE Link] .
Ravaldi C, Vannacci A, Bolognesi E, Mancini S, Faravelli C, Ricca V. Gender role, eating disorder symptoms, and body image concern in ballet dancers. J Psychosom Res . 2006 Oct. 61(4):529-35. [QxMD MEDLINE Link] .
Arcelus J, Mitchell AJ, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Arch Gen Psychiatry . 2011 Jul. 68(7):724-31. [QxMD MEDLINE Link] .
Cassidy O, Sbrocco T, Tanofsky-Kraff M. Utilizing non-traditional research designs to explore culture-specific risk factors for eating disorders in African American adolescents. Adv Eat Disord . 2015 Jan. 3(1):91-102. [QxMD MEDLINE Link] .
Franko DL, Becker AE, Thomas JJ, Herzog DB. Cross-ethnic differences in eating disorder symptoms and related distress. Int J Eat Disord . 2007 Mar. 40(2):156-64. [QxMD MEDLINE Link] . [Full Text] .
Morgan CD, Marsh C. Bulimia nervosa in an elderly male: a case report. Int J Eat Disord . 2006 Mar. 39(2):170-1. [QxMD MEDLINE Link] . [Full Text] .
Ágh T, Kovács G, Supina D, Pawaskar M, Herman BK, Vokó Z, et al. A systematic review of the health-related quality of life and economic burdens of anorexia nervosa, bulimia nervosa, and binge eating disorder. Eat Weight Disord . 2016 Sep. 21(3):353-64. [QxMD MEDLINE Link] .
Fichter MM, Quadflieg N. Long-term stability of eating disorder diagnoses. Int J Eat Disord . 2007 Nov. 40 Suppl:S61-6. [QxMD MEDLINE Link] . [Full Text] .
Fichter, MM, Quadflieg, N, Hedlund, S. Long term course of binge eating disorder and bulimia nervosa: relevance for nosology and diagnostic criteria. Int J Eat Disorders . 2008. 41:577-586.
Arikian, A, Keel, PK, Miler, KG. Parental psychopathology as a predictor of long-term outcome in bulimia nervosa patients. Eating Disorders . 2008. 16:30-39.
Grilo CM, Pagano ME, Skodol AE, et al. Natural course of bulimia nervosa and of eating disorder not otherwise specified: 5-year prospective study of remissions, relapses, and the effects of personality disorder psychopathology. J Clin Psychiatry . 2007 May. 68(5):738-46. [QxMD MEDLINE Link] . [Full Text] .
Björck C, Clinton D, Sohlberg S, Norring C. Negative self-image and outcome in eating disorders: results at 3-year follow-up. Eat Behav . 2007 Aug. 8(3):398-406. [QxMD MEDLINE Link] .
Fosse GK, Holen A. Childhood maltreatment in adult female psychiatric outpatients with eating disorders. Eat Behav . 2006 Nov. 7(4):404-9. [QxMD MEDLINE Link] .
Micali N, Holliday J, Karwautz A, et al. Childhood eating and weight in eating disorders: a multi-centre European study of affected women and their unaffected sisters. Psychother Psychosom . 2007. 76(4):234-41. [QxMD MEDLINE Link] .
Fernandez-Aranda F, Krug I, Granero R, et al. Individual and family eating patterns during childhood and early adolescence: an analysis of associated eating disorder factors. Appetite . 2007 Sep. 49(2):476-85. [QxMD MEDLINE Link] .
Mikami AY, Hinshaw SP, Patterson KA, Lee JC. Eating pathology among adolescent girls with attention-deficit/hyperactivity disorder. J Abnorm Psychol . 2008 Feb. 117(1):225-35. [QxMD MEDLINE Link] .
Eddy KT, Dorer DJ, Franko DL, Tahilani K, Thompson-Brenner H, Herzog DB. Should bulimia nervosa be subtyped by history of anorexia nervosa? A longitudinal validation. Int J Eat Disord . 2007 Nov. 40 Suppl:S67-71. [QxMD MEDLINE Link] . [Full Text] .
Svaldi J, Schmitz F, Baur J, Hartmann AS, Legenbauer T, Thaler C, et al. Experiences of shame and guilt in anorexia and bulimia nervosa: a systematic review. Psychol Psychother . 2018 Sep 4. doi: 10.1111/papt.12198. [Epub ahead of print]: [QxMD MEDLINE Link] .
Ruiz MC, Soler-Gonzalez J. Images in clinical medicine. Unfortunate ingestion. N Engl J Med . 2005 Nov 24. 353(21):2270. [QxMD MEDLINE Link] . [Full Text] .
Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ . 1999 Dec 4. 319(7223):1467-8. [QxMD MEDLINE Link] . [Full Text] .
Cotton MA, Ball C, Robinson P. Four simple questions can help screen for eating disorders. J Gen Intern Med . 2003 Jan. 18(1):53-6. [QxMD MEDLINE Link] . [Full Text] .
Mintz LB, O'Halloran MS. The Eating Attitudes Test: validation with DSM-IV eating disorder criteria. J Pers Assess . 2000 Jun. 74(3):489-503. [QxMD MEDLINE Link] .
Keery H, Boutelle K, van den Berg P, Thompson JK. The impact of appearance-related teasing by family members. J Adolesc Health . 2005 Aug. 37(2):120-7. [QxMD MEDLINE Link] .
Poyastro Pinheiro A, Thornton LM, Plotonicov KH, et al. Patterns of menstrual disturbance in eating disorders. Int J Eat Disord . 2007 Jul. 40(5):424-34. [QxMD MEDLINE Link] . [Full Text] .
Pinheiro, AP, Thornton, LH, Plotonicov, KH, et al. Patterns of menstrual disturbance in eating disorders. Intl J Eat Disord . 2007. 40:424-434.
Ribases M, Fernandez-Aranda F, Gratacos M, et al. Contribution of the serotoninergic system to anxious and depressive traits that may be partially responsible for the phenotypical variability of bulimia nervosa. J Psychiatr Res . 2008 Jan. 42(1):50-7. [QxMD MEDLINE Link] .
Monteleone P, Santonastaso P, Mauri M, et al. Investigation of the serotonin transporter regulatory region polymorphism in bulimia nervosa: relationships to harm avoidance, nutritional parameters, and psychiatric comorbidity. Psychosom Med . 2006 Jan-Feb. 68(1):99-103. [QxMD MEDLINE Link] . [Full Text] .
Fetissov SO, Harro J, Jaanisk M, et al. Autoantibodies against neuropeptides are associated with psychological traits in eating disorders. Proc Natl Acad Sci U S A . 2005 Oct 11. 102(41):14865-70. [QxMD MEDLINE Link] . [Full Text] .
Bacanu SA, Bulik CM, Klump KL, et al. Linkage analysis of anorexia and bulimia nervosa cohorts using selected behavioral phenotypes as quantitative traits or covariates. Am J Med Genet B Neuropsychiatr Genet . 2005 Nov 5. 139B(1):61-8. [QxMD MEDLINE Link] . [Full Text] .
Mercader JM, Ribases M, Gratacos M, et al. Altered brain-derived neurotrophic factor blood levels and gene variability are associated with anorexia and bulimia. Genes Brain Behav . 2007 Nov. 6(8):706-16. [QxMD MEDLINE Link] . [Full Text] .
Ando T, Komaki G, Naruo T, et al. Possible role of preproghrelin gene polymorphisms in susceptibility to bulimia nervosa. Am J Med Genet B Neuropsychiatr Genet . 2006 Dec 5. 141B(8):929-34. [QxMD MEDLINE Link] . [Full Text] .
Uher R, Treasure J. Brain lesions and eating disorders. J Neurol Neurosurg Psychiatry . 2005 Jun. 76(6):852-7. [QxMD MEDLINE Link] . [Full Text] .
Frank GK, Bailer UF, Meltzer CC, et al. Regional cerebral blood flow after recovery from anorexia or bulimia nervosa. Int J Eat Disord . 2007 Sep. 40(6):488-92. [QxMD MEDLINE Link] . [Full Text] .
Godart NT, Perdereau F, Rein Z, et al. Comorbidity studies of eating disorders and mood disorders. Critical review of the literature. J Affect Disord . 2007 Jan. 97(1-3):37-49. [QxMD MEDLINE Link] .
Mazzeo SE, Slof-Op't Landt MC, Jones I, et al. Associations among postpartum depression, eating disorders, and perfectionism in a population-based sample of adult women. Int J Eat Disord . 2006 Apr. 39(3):202-11. [QxMD MEDLINE Link] . [Full Text] .
Micali N, Hilton K, Natatani E, et al. Is childhood OCD a risk factor for eating disorders later in life? A longitudinal study. Psychol Med . 2011 Jun 7. 1-7. [QxMD MEDLINE Link] .
Duncan AE, Neuman RJ, Kramer JR, Kuperman S, Hesselbrock VM, Bucholz KK. Lifetime psychiatric comorbidity of alcohol dependence and bulimia nervosa in women. Drug Alcohol Depend . 2006 Sep 1. 84(1):122-32. [QxMD MEDLINE Link] .
Solmi M, Veronese N, Sergi G, Luchini C, Favaro A, Santonastaso P, et al. The association between smoking prevalence and eating disorders: a systematic review and meta-analysis. Addiction . 2016 Nov. 111(11):1914-22. [QxMD MEDLINE Link] .
Baker JH, Mazzeo SE, Kendler KS. Association between broadly defined bulimia nervosa and drug use disorders: common genetic and environmental influences. Int J Eat Disord . 2007 Dec. 40(8):673-8. [QxMD MEDLINE Link] . [Full Text] .
Striegel-Moore RH, Franko DL, Thompson D, Barton B, Schreiber GB, Daniels SR. Caffeine intake in eating disorders. Int J Eat Disord . 2006 Mar. 39(2):162-5. [QxMD MEDLINE Link] . [Full Text] .
Fernandez-Aranda F, Jimenez-Murcia S, Alvarez-Moya EM, Granero R, Vallejo J, Bulik CM. Impulse control disorders in eating disorders: clinical and therapeutic implications. Compr Psychiatry . 2006 Nov-Dec. 47(6):482-8. [QxMD MEDLINE Link] .
Surman CB, Randall ET, Biederman J. Association between attention-deficit/hyperactivity disorder and bulimia nervosa: analysis of 4 case-control studies. J Clin Psychiatry . 2006 Mar. 67(3):351-4. [QxMD MEDLINE Link] . [Full Text] .
Yates, WR, Lund, BC, Johnson, C, et al. Attention deficit hyperactivity symptoms and disorder in eating disorder inpatients. Int J Eat Disord . 2009. 42:375-378.
Wonderlich SA, Rosenfeldt S, Crosby RD, et al. The effects of childhood trauma on daily mood lability and comorbid psychopathology in bulimia nervosa. J Trauma Stress . 2007 Feb. 20(1):77-87. [QxMD MEDLINE Link] . [Full Text] .
Zeeck A, Birindelli E, Sandholz A, Joos A, Herzog T, Hartmann A. Symptom severity and treatment course of bulimic patients with and without a borderline personality disorder. Eur Eat Disord Rev . 2007 Nov. 15(6):430-8. [QxMD MEDLINE Link] . [Full Text] .
Waller G, Sines J, Meyer C, Foster E, Skelton A. Narcissism and narcissistic defences in the eating disorders. Int J Eat Disord . 2007 Mar. 40(2):143-8. [QxMD MEDLINE Link] . [Full Text] .
Stein KF, Corte C. Identity impairment and the eating disorders: content and organization of the self-concept in women with anorexia nervosa and bulimia nervosa. Eur Eat Disord Rev . 2007 Jan. 15(1):58-69. [QxMD MEDLINE Link] . [Full Text] .
Pisetsky EM, Wonderlich SA, Crosby RD, Peterson CB, Mitchell JE, Engel SG, et al. Depression and personality traits associated with emotion dysregulation: correlates of suicide attempts in women with bulimia nervosa. Eur Eat Disord Rev . 2015 Nov. 23(6):537-44. [QxMD MEDLINE Link] .
Crow, SJ, Peterson CB, Swanson, SA. Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry . 2009. 166:1343-1346.
Mandel L, Abai S. Diagnosing bulimia nervosa with parotid gland swelling. J Am Dent Assoc . 2004 May. 135(5):613-6; quiz 655. [QxMD MEDLINE Link] . [Full Text] .
Kisely S, Baghaie H, Lalloo R, Johnson NW. Association between poor oral health and eating disorders: systematic review and meta-analysis. Br J Psychiatry . 2015 Oct. 207(4):299-305. [QxMD MEDLINE Link] .
Glorio R, Allevato M, De Pablo A, et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int J Dermatol . 2000 May. 39(5):348-53. [QxMD MEDLINE Link] . [Full Text] .
Strumia R. Dermatologic signs in patients with eating disorders. Am J Clin Dermatol . 2005. 6(3):165-73. [QxMD MEDLINE Link] .
de Jonge P, Alonso J, Stein DJ, Kiejna A, Aguilar-Gaxiola S, Viana MC, et al. Associations between DSM-IV mental disorders and diabetes mellitus: a role for impulse control disorders and depression. Diabetologia . 2014 Apr. 57(4):699-709. [QxMD MEDLINE Link] .
Scherag,S, Hebebrand, J, Hinney, A. Eating disorders: the current status of molecular genetic research. Eur Child Adolesc Psychiatry . 2010. 19:211-226.
Kaye,W. Neurobiology of anorexia and bulimia nervosa. Physiology & Behavior 94 . (2008). 121-135.
Bailer, UF, Kaye, WH. A review of neuropeptides and neuroendocrine dysregulation in anorexia nervosa and bulimia nervosa. CNS and Neurological Disorders . 2003. 2:53-59.
Monteleone P, Maj M. Dysfunctions of leptin, ghrelin, BDNF and endocannabinoids in eating disorders: beyond the homeostatic control of food intake. Psychoneuroendocrinology . 2013 Mar. 38 (3):312-30. [QxMD MEDLINE Link] .
Sadock BJ, and Sadock VA. Eating Disorders. Grebb, J.A., Pataki, C.S., and Sussman, N. Synopsis of Psychiatry . 10th Edition. Lippincott, Williams, & Wilkins; 2007. Chapter 23.
Brauser D. Excessive Exercise Predicts Suicidal Behavior in Eating Disorders. Medscape Medical News. Apr 18 2013. Available at http://www.medscape.com/viewarticle/782742 . Accessed: Apr 22 2013.
Smith AR, Fink EL, Anestis MD, Ribeiro JD, Gordon KH, Davis H, et al. Exercise caution: Over-exercise is associated with suicidality among individuals with disordered eating. Psychiatry Res . 2013 Apr 30. 206(2-3):246-55. [QxMD MEDLINE Link] .
Kruger D. Bulimia nervosa: easy to hide but essential to recognize. JAAPA . 2008 Jan. 21(1):48-52. [QxMD MEDLINE Link] .
Donnelly B, Touyz S, Hay P, Burton A, Russell J, Caterson I. Neuroimaging in bulimia nervosa and binge eating disorder: a systematic review. J Eat Disord . 2018 Feb. 20(6)3:1-24. [QxMD MEDLINE Link] . [Full Text] .
Bosanac P, Kurlender S, Stojanovska L, et al. Neuropsychological study of underweight and "weight-recovered" anorexia nervosa compared with bulimia nervosa and normal controls. Int J Eat Disord . 2007 Nov. 40(7):613-21. [QxMD MEDLINE Link] . [Full Text] .
Brand M, Franke-Sievert C, Jacoby GE, Markowitsch HJ, Tuschen-Caffier B. Neuropsychological correlates of decision making in patients with bulimia nervosa. Neuropsychology . 2007 Nov. 21(6):742-50. [QxMD MEDLINE Link] .
Griffiths S, Rossell SL, Mitchison D, Murray SB, Mond JM. Pathways into treatment for eating disorders: a quantitative examination of treatment barriers and treatment attitudes. Eat Disord . 2018 Nov-Dec. 26(6):556-74. [QxMD MEDLINE Link] .
Ali K, Farrer L, Fassnacht DB, Gulliver A, Bauer S, Griffiths KM. Perceived barriers and facilitators towards help-seeking for eating disorders: a systematic review. Int J Eat Disord . 2017 Jan. 50(1):9-21. [QxMD MEDLINE Link] .
Stockford C, Stenfert Kroese B, Beesley A, Leung N. Women's recovery from anorexia nervosa: a systematic review and meta-synthesis of qualitative research. Eat Disord . 2018 Sep. 24:1-26. [QxMD MEDLINE Link] .
Shapiro JR, Berkman ND, Brownley KA, Sedway JA, Lohr KN, Bulik CM. Bulimia nervosa treatment: a systematic review of randomized controlled trials. Int J Eat Disord . 2007 May. 40(4):321-36. [QxMD MEDLINE Link] . [Full Text] .
Mitchell JE, Agras WS, Wilson GT, Halmi K, Kraemer H, Crow S. A trial of a relapse prevention strategy in women with bulimia nervosa who respond to cognitive-behavior therapy. Int J Eat Disord . 2004 May. 35(4):549-55. [QxMD MEDLINE Link] .
Slade E, Keeney E, Mavranezouli I, Dias S, Fou L, Stockton S, et al. Treatments for bulimia nervosa: a network meta-analysis. Psychol Med . 2018 Dec. 48(16):2629-2636. [QxMD MEDLINE Link] .
Cooper Z, Fairburn CG. The evolution of "enhanced" cognitive behavior therapy for eating disorders: learning from treatment nonresponse. Cogn Behav Pract . 2011 Aug. 18 (3):394-402. [QxMD MEDLINE Link] .
Bulik CM, Marcus MD, Zerwas S, Levine MD, La Via M. The changing "weightscape" of bulimia nervosa. Am J Psychiatry . 2012 Oct. 169 (10):1031-6. [QxMD MEDLINE Link] .
de Jong M, Schoorl M, Hoek HW. Enhanced cognitive behavioural therapy for patients with eating disorders: a systematic review. Curr Opin Psychiatry . 2018 Nov. 31(6):436-444. [QxMD MEDLINE Link] .
Miniati M, Callari A, Maglio A, Calugi S. Interpersonal psychotherapy for eating disorders: current perspectives. Psychol Res Behav Manag . 2018 Sep 5. 11:353-369. [QxMD MEDLINE Link] .
Le Grange D, Lock J, Agras WS, Bryson SW, Jo B. Randomized clinical trial of family-based treatment and cognitive-behavioral therapy for adolescent bulimia nervosa. J Am Acad Child Adolesc Psychiatry . 2015 Nov. 54 (11):886-94.e2. [QxMD MEDLINE Link] .
Schembri C, Evans L. Adverse relationship processes: the attempts of women with bulimia nervosa symptoms to fit the perceived ideal of intimate partners. Eur Eat Disord Rev . 2008 Jan. 16(1):59-66. [QxMD MEDLINE Link] . [Full Text] .
Mitchell JE, Agras S, Wonderlich S. Treatment of bulimia nervosa: where are we and where are we going?. Int J Eat Disord . 2007 Mar. 40(2):95-101. [QxMD MEDLINE Link] . [Full Text] .
de Carvalho MR, Dias TRS, Duchesne M, Nardi AE, Appolinario JC. Virtual reality as a promising strategy in the assessment and treatment of bulimia nervosa and binge eating disorder: a systematic review. Behav Sci (Basel) . 2017 Jul 9. 7(3): [QxMD MEDLINE Link] . [Full Text] .
Self-help and guided self-help for eating disorders, Volume 4 [database online]. The Cochrane Database of Systematic Reviews: The Cochrane Library, The Cochrane Collaboration; 2002. Updated 2007.
Treatment of patients with eating disorders,third edition. American Psychiatric Association. Am J Psychiatry . 2006 Jul. 163(7 Suppl):4-54. [QxMD MEDLINE Link] . [Full Text] .
Mitchell JE, Crow S. Medical complications of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry . 2006 Jul. 19(4):438-43. [QxMD MEDLINE Link] .
Schlegl S, Bürger C, Schmidt L, Herbst N, Voderholzer U. The potential of technology-based psychological interventions for anorexia and bulimia nervosa: a systematic review and recommendations for future research. J Med Internet Res . 2015 Mar 31. 17 (3):e85. [QxMD MEDLINE Link] .
ter Huurne ED, de Haan HA, Postel MG, van der Palen J, VanDerNagel JE, DeJong CA. Web-based cognitive behavioral therapy for female patients with eating disorders: randomized controlled trial. J Med Internet Res . 2015 Jun 18. 17 (6):e152. [QxMD MEDLINE Link] .
Mayer LE, Walsh BT. The use of selective serotonin reuptake inhibitors in eating disorders. J Clin Psychiatry . 1998. 59 Suppl 15:28-34. [QxMD MEDLINE Link] .
Milano W, Siano C, Putrella C, Capasso A. Treatment of bulimia nervosa with fluvoxamine: a randomized controlled trial. Adv Ther . 2005 May-Jun. 22(3):278-83. [QxMD MEDLINE Link] .
Leombruni P, Amianto F, Delsedime N, Gramaglia C, Abbate-Daga G, Fassino S. Citalopram versus fluoxetine for the treatment of patients with bulimia nervosa: a single-blind randomized controlled trial. Adv Ther . 2006 May-Jun. 23(3):481-94. [QxMD MEDLINE Link] .
Walsh BT, Sysko R, Parides MK. Early response to desipramine among women with bulimia nervosa. Int J Eat Disord . 2006 Jan. 39(1):72-5. [QxMD MEDLINE Link] . [Full Text] .
Bacaltchuk J, Hay P. Antidepressants versus placebo for people with bulimia nervosa. Cochrane Database Syst Rev . 2003. CD003391. [QxMD MEDLINE Link] .
McElroy SL, Arnold LM, Shapira NA, et al. Topiramate in the treatment of binge eating disorder associated with obesity: a randomized, placebo-controlled trial. Am J Psychiatry . 2003 Feb. 160(2):255-61. [QxMD MEDLINE Link] .
Arbaizar, B, Gomez-Acebo, I, Llorca, J. Efficacy of Topiramate in bulimia nervosa an binge-eating disorder: a systematic review. General Hospital Psychiatry . 2008. 30:471-475.
Hsu LK, Clement L, Santhouse R, Ju ES. Treatment of bulimia nervosa with lithium carbonate. A controlled study. J Nerv Ment Dis . 1991 Jun. 179(6):351-5. [QxMD MEDLINE Link] .
Faris PL, Kim SW, Meller WH, et al. Effect of decreasing afferent vagal activity with ondansetron on symptoms of bulimia nervosa: a randomised, double-blind trial. Lancet . 2000 Mar 4. 355(9206):792-7. [QxMD MEDLINE Link] .
Broft AI, Spanos A, Corwin RL, et al. Baclofen for binge eating: an open-label trial. Int J Eat Disord . 2007 Dec. 40(8):687-91. [QxMD MEDLINE Link] . [Full Text] .
Naessen S, Carlstrom K, Bystrom B, Pierre Y, Hirschberg AL. Effects of an antiandrogenic oral contraceptive on appetite and eating behavior in bulimic women. Psychoneuroendocrinology . 2007 Jun. 32(5):548-54. [QxMD MEDLINE Link] .
Broft A, Berner LA, Walsh BT. Pharmacotherapy for Bulimia Nervosa. Grilo CM, Mitchell JE. The Treatment of Eating Disorders: A Clinical Handbook . New York: The Guilford Press; 2010. 388.
Psychotherapy for bulimia nervosa and binging, Volume 1 [database online]. The Cochrane Database of Systematic Reviews: The Cochrane Library, The Cochrane Collaboration; 1998. Updated 2005.
Antidepressants versus psychological treatments and their combination for bulimia nervosa [database online]. The Cochrane Database of Systematic Reviews: The Cochrane Library, The Cochrane Collaboration; 1997. Updated 2005.
Jacobi C, Morris L, Beckers C, et al. Maintenance of internet-based prevention: a randomized controlled trial. Int J Eat Disord . 2007 Mar. 40(2):114-9. [QxMD MEDLINE Link] .
Ljotsson B, Lundin C, Mitsell K, Carlbring P, Ramklint M, Ghaderi A. Remote treatment of bulimia nervosa and binge eating disorder: a randomized trial of Internet-assisted cognitive behavioural therapy. Behav Res Ther . 2007 Apr. 45(4):649-61. [QxMD MEDLINE Link] . [Full Text] .
Robinson S, Perkins S, Bauer S, Hammond N, Treasure J, Schmidt U. Aftercare intervention through text messaging in the treatment of bulimia nervosa--feasibility pilot. Int J Eat Disord . 2006 Dec. 39(8):633-8. [QxMD MEDLINE Link] . [Full Text] .
Adson DE, Mitchell JE, Trenkner SW. The superior mesenteric artery syndrome and acute gastric dilatation in eating disorders: a report of two cases and a review of the literature. Int J Eat Disord . 1997 Mar. 21(2):103-14. [QxMD MEDLINE Link] .
DeBate RD, Shuman D, Tedesco LA. Eating disorders in the oral health curriculum. J Dent Educ . 2007 May. 71(5):655-63. [QxMD MEDLINE Link] . [Full Text] .
Haines, J, Neumark=Sztainer, D, Perry, CL, et al. V.I.K. (Very Important Kids): a school based program designed to reduce teasing and unhealthy weight-control behaviors. Health Education Research-Theory and Practic . 2006. 21(6):884-895.
Burton KW. APA Releases Updated Eating Disorder Guidelines. Medscape Medical News. Available at https://www.medscape.com/viewarticle/989058 . March 3, 2023; Accessed: March 31, 2023.
Couturier J, Isserlin L, Norris M, et al. Canadian practice guidelines for the treatment of children and adolescents with eating disorders. J Eat Disord . 2020. 8:4. [QxMD MEDLINE Link] .
Brauser D. Autoimmune diseases implicated in eating disorders. Medscape Medical News . September 8, 2014. [Full Text] .
Raevuori A, Haukka J, Vaarala O, Suvisaari JM, Gissler M, Grainger M, et al. The increased risk for autoimmune diseases in patients with eating disorders. PLoS One . 2014. 9(8):e104845. [QxMD MEDLINE Link] . [Full Text] .
Woodside BD, Staab R. Management of psychiatric comorbidity in anorexia nervosa and bulimia nervosa. CNS Drugs . 2006. 20(8):655-63. [QxMD MEDLINE Link] .
Goebel-Fabbri, AE, Fikkan, J, Franko, DL, et al. Insulin restriction and associated morbidity and mortality in women with type 1 diabetes. Diabetes Care . 2008. 31:415-419.
Micali N, Treasure J, Simonoff E. Eating disorders symptoms in pregnancy: a longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res . 2007 Sep. 63(3):297-303. [QxMD MEDLINE Link] .
Micali N, Simonoff E, Treasure J. Risk of major adverse perinatal outcomes in women with eating disorders. Br J Psychiatry . 2007 Mar. 190:255-9. [QxMD MEDLINE Link] . [Full Text] .
Marsden P, Karagianni E, Morgan JF. Spirituality and clinical care in eating disorders: a qualitative study. Int J Eat Disord . 2007 Jan. 40(1):7-12. [QxMD MEDLINE Link] . [Full Text] .
Graap H, Bleich S, Herbst F, Trostmann Y, Wancata J, de Zwaan M. The needs of carers of patients with anorexia and bulimia nervosa. Eur Eat Disord Rev . 2008 Jan. 16(1):21-9. [QxMD MEDLINE Link] . [Full Text] .
Brooks M. Enhanced CBT Bests Psychoanalysis for Bulimia. Medscape Medical News. Available at http://www.medscape.com/viewarticle/815300 . Accessed: December 8, 2013.
Button E, Aldridge S. Season of birth and eating disorders: patterns across diagnoses in a specialized eating disorders service. Int J Eat Disord . 2007 Jul. 40(5):468-71. [QxMD MEDLINE Link] .
Lehoux PM, Howe N. Perceived non-shared environment, personality traits, family factors and developmental experiences in bulimia nervosa. Br J Clin Psychol . 2007 Mar. 46:47-66. [QxMD MEDLINE Link] .
Morgan JF, Lacey JH. Season of birth and bulimia nervosa. Int J Eat Disord . 2000 May. 27(4):452-8. [QxMD MEDLINE Link] . [Full Text] .
Poulsen S, Lunn S, Daniel SI, Folke S, Mathiesen BB, Katznelson H, et al. A randomized controlled trial of psychoanalytic psychotherapy or cognitive-behavioral therapy for bulimia nervosa. Am J Psychiatry . 2013 Nov 26. [QxMD MEDLINE Link] .
Wolcott, RB, Yager, J, Gordon, G. Dental sequelae to the binge-purge syndrome (bulimia): report of cases. JADA . 1984. 109:723-725.
Monteleone AM, Pellegrino F, Croatto G, et al. Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neurosci Biobehav Rev . 2022 Nov. 142:104857. [QxMD MEDLINE Link] .
Tozzi F, Thornton LM, Klump KL, Fichter MM, Halmi KA, Kaplan AS, et al. Symptom fluctuation in eating disorders: correlates of diagnostic crossover. Am J Psychiatry . 2005 Apr. 162 (4):732-40. [QxMD MEDLINE Link] .
Hudson JI, Hiripi E, Pope HG Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry . 2007 Feb 1. 61 (3):348-58. [QxMD MEDLINE Link] .
Silén Y, Keski-Rahkonen A. Worldwide prevalence of DSM-5 eating disorders among young people. Curr Opin Psychiatry . 2022 Nov 1. 35 (6):362-371. [QxMD MEDLINE Link] .
Chua SN, Fitzsimmons-Craft EE, Austin SB, Wilfley DE, Taylor CB. Estimated prevalence of eating disorders in Malaysia based on a diagnostic screen. Int J Eat Disord . 2022 Jun. 55 (6):763-775. [QxMD MEDLINE Link] .
Koposov RA, Stickley A, Ruchkin V. Bulimia Symptoms in Russian Youth: Prevalence and Association With Internalizing Problems. Front Psychiatry . 2021. 12:797388. [QxMD MEDLINE Link] .
Crow SJ, Peterson CB, Swanson SA, Raymond NC, Specker S, Eckert ED, et al. Increased mortality in bulimia nervosa and other eating disorders. Am J Psychiatry . 2009 Dec. 166 (12):1342-6. [QxMD MEDLINE Link] .
van Hoeken D, Hoek HW. Review of the burden of eating disorders: mortality, disability, costs, quality of life, and family burden. Curr Opin Psychiatry . 2020 Nov. 33 (6):521-527. [QxMD MEDLINE Link] .
Tith RM, Paradis G, Potter BJ, Low N, Healy-Profitós J, He S, et al. Association of Bulimia Nervosa With Long-term Risk of Cardiovascular Disease and Mortality Among Women. JAMA Psychiatry . 2020 Jan 1. 77 (1):44-51. [QxMD MEDLINE Link] .
Carrino EA, Flatt RE, Pawar PS, Sanzari CM, Tregarthen JP, Argue S, et al. Sociodemographic and clinical characteristics of treated and untreated adults with bulimia nervosa or binge-eating disorder recruited for a large-scale research study. J Eat Disord . 2023 Jul 31. 11 (1):126. [QxMD MEDLINE Link] .
Traut P, Halbeisen G, Braks K, Huber TJ, Paslakis G. Sociodemographic and clinical features of men and women with eating disorders: a diagnosis-matched, retrospective comparison among inpatients. Front Psychiatry . 2023. 14:1192693. [QxMD MEDLINE Link] .
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry . 2022 Jan. 27 (1):281-295. [QxMD MEDLINE Link] .
Avena NM, Bocarsly ME, Hoebel BG. Animal models of sugar and fat bingeing: relationship to food addiction and increased body weight. Methods Mol Biol . 2012. 829:351-65. [QxMD MEDLINE Link] .
Avena NM, Bocarsly ME, Rada P, Kim A, Hoebel BG. After daily bingeing on a sucrose solution, food deprivation induces anxiety and accumbens dopamine/acetylcholine imbalance. Physiol Behav . 2008 Jun 9. 94 (3):309-15. [QxMD MEDLINE Link] .
Johnson PM, Kenny PJ. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat Neurosci . 2010 May. 13 (5):635-41. [QxMD MEDLINE Link] .
Cai X, Liu H, Feng B, Yu M, He Y, Liu H, et al. A D2 to D1 shift in dopaminergic inputs to midbrain 5-HT neurons causes anorexia in mice. Nat Neurosci . 2022 May. 25 (5):646-658. [QxMD MEDLINE Link] .
Berner LA, Brown TA, Lavender JM, Lopez E, Wierenga CE, Kaye WH. Neuroendocrinology of reward in anorexia nervosa and bulimia nervosa: Beyond leptin and ghrelin. Mol Cell Endocrinol . 2019 Nov 1. 497:110320. [QxMD MEDLINE Link] .
Monteleone AM, Castellini G, Volpe U, Ricca V, Lelli L, Monteleone P, et al. Neuroendocrinology and brain imaging of reward in eating disorders: A possible key to the treatment of anorexia nervosa and bulimia nervosa. Prog Neuropsychopharmacol Biol Psychiatry . 2018 Jan 3. 80 (Pt B):132-142. [QxMD MEDLINE Link] .
Broft A, Shingleton R, Kaufman J, Liu F, Kumar D, Slifstein M, et al. Striatal dopamine in bulimia nervosa: a PET imaging study. Int J Eat Disord . 2012 Jul. 45 (5):648-56. [QxMD MEDLINE Link] .
Mihov Y, Treyer V, Akkus F, Toman E, Milos G, Ametamey SM, et al. Metabotropic glutamate receptor 5 in bulimia nervosa. Sci Rep . 2020 Apr 14. 10 (1):6374. [QxMD MEDLINE Link] .
Mitchell JS, Anijärv TE, Levenstein JL, Hermens DF, Lagopoulos J. Excitatory and inhibitory neurometabolites in anorexia nervosa: A systematic review of proton magnetic resonance spectroscopy studies. Neurosci Biobehav Rev . 2023 Sep. 152:105279. [QxMD MEDLINE Link] .
Kelley AE, Berridge KC. The neuroscience of natural rewards: relevance to addictive drugs. J Neurosci . 2002 May 1. 22 (9):3306-11. [QxMD MEDLINE Link] .
Plassmann H, O'Doherty JP, Rangel A. Appetitive and aversive goal values are encoded in the medial orbitofrontal cortex at the time of decision making. J Neurosci . 2010 Aug 11. 30 (32):10799-808. [QxMD MEDLINE Link] .
Puglisi-Allegra S, Ventura R. Prefrontal/accumbal catecholamine system processes emotionally driven attribution of motivational salience. Rev Neurosci . 2012. 23 (5-6):509-26. [QxMD MEDLINE Link] .
Kelley AE, Baldo BA, Pratt WE, Will MJ. Corticostriatal-hypothalamic circuitry and food motivation: integration of energy, action and reward. Physiol Behav . 2005 Dec 15. 86 (5):773-95. [QxMD MEDLINE Link] .
O'Doherty JP, Dayan P, Friston K, Critchley H, Dolan RJ. Temporal difference models and reward-related learning in the human brain. Neuron . 2003 Apr 24. 38 (2):329-37. [QxMD MEDLINE Link] .
Frank GKW, Shott ME, Stoddard J, Swindle S, Pryor TL. Association of Brain Reward Response With Body Mass Index and Ventral Striatal-Hypothalamic Circuitry Among Young Women With Eating Disorders. JAMA Psychiatry . 2021 Oct 1. 78 (10):1123-1133. [QxMD MEDLINE Link] .
Mueller SV, Morishima Y, Schwab S, Wiest R, Federspiel A, Hasler G. Neural Correlates of Impaired Reward-Effort Integration in Remitted Bulimia Nervosa. Neuropsychopharmacology . 2018 Mar. 43 (4):868-876. [QxMD MEDLINE Link] .
Bohon C, Stice E. Negative affect and neural response to palatable food intake in bulimia nervosa. Appetite . 2012 Jun. 58 (3):964-70. [QxMD MEDLINE Link] .
Cyr M, Wang Z, Tau GZ, Zhao G, Friedl E, Stefan M, et al. Reward-Based Spatial Learning in Teens With Bulimia Nervosa. J Am Acad Child Adolesc Psychiatry . 2016 Nov. 55 (11):962-971.e3. [QxMD MEDLINE Link] .
Frank GK. Altered brain reward circuits in eating disorders: chicken or egg?. Curr Psychiatry Rep . 2013 Oct. 15 (10):396. [QxMD MEDLINE Link] .
Lee JE, Namkoong K, Jung YC. Impaired prefrontal cognitive control over interference by food images in binge-eating disorder and bulimia nervosa. Neurosci Lett . 2017 Jun 9. 651:95-101. [QxMD MEDLINE Link] .
Dreyfuss MFW, Riegel ML, Pedersen GA, Cohen AO, Silverman MR, Dyke JP, et al. Patients with bulimia nervosa do not show typical neurodevelopment of cognitive control under emotional influences. Psychiatry Res Neuroimaging . 2017 Aug 30. 266:59-65. [QxMD MEDLINE Link] .
Jacobs MJ, Roesch S, Wonderlich SA, Crosby R, Thornton L, Wilfley DE, et al. Anorexia nervosa trios: behavioral profiles of individuals with anorexia nervosa and their parents. Psychol Med . 2009 Mar. 39 (3):451-61. [QxMD MEDLINE Link] .
Lilenfeld LR. Personality and temperament. Curr Top Behav Neurosci . 2011. 6:3-16. [QxMD MEDLINE Link] .
Kaye W. Neurobiology of anorexia and bulimia nervosa. Physiol Behav . 2008 Apr 22. 94 (1):121-35. [QxMD MEDLINE Link] .
Boureau YL, Dayan P. Opponency revisited: competition and cooperation between dopamine and serotonin. Neuropsychopharmacology . 2011 Jan. 36 (1):74-97. [QxMD MEDLINE Link] .
Frank GKW. From Desire to Dread-A Neurocircuitry Based Model for Food Avoidance in Anorexia Nervosa. J Clin Med . 2021 May 21. 10 (11): [QxMD MEDLINE Link] .
Castro DC, Cole SL, Berridge KC. Lateral hypothalamus, nucleus accumbens, and ventral pallidum roles in eating and hunger: interactions between homeostatic and reward circuitry. Front Syst Neurosci . 2015. 9:90. [QxMD MEDLINE Link] .
Li BU, Lefevre F, Chelimsky GG, Boles RG, Nelson SP, Lewis DW, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition consensus statement on the diagnosis and management of cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr . 2008 Sep. 47 (3):379-93. [QxMD MEDLINE Link] .
Bahji A, Brothers TD, Danilewitz M. Considering Cannabis Use in Differential Diagnosis: A Teachable Moment. JAMA Intern Med . 2022 Jan 1. 182 (1):66-67. [QxMD MEDLINE Link] .
Eddy KT, Tabri N, Thomas JJ, Murray HB, Keshaviah A, Hastings E, et al. Recovery From Anorexia Nervosa and Bulimia Nervosa at 22-Year Follow-Up. J Clin Psychiatry . 2017 Feb. 78 (2):184-189. [QxMD MEDLINE Link] .
Blundell JE, Gillett A. Control of food intake in the obese. Obes Res . 2001 Nov. 9 Suppl 4:263S-270S. [QxMD MEDLINE Link] .
Craighead LW, Agras WS. Mechanisms of action in cognitive-behavioral and pharmacological interventions for obesity and bulimia nervosa. J Consult Clin Psychol . 1991 Feb. 59 (1):115-25. [QxMD MEDLINE Link] .
de Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metab Disord . 2001 May. 25 Suppl 1:S51-5. [QxMD MEDLINE Link] .
Devlin MJ. Binge-eating disorder and obesity. A combined treatment approach. Psychiatr Clin North Am . 2001 Jun. 24 (2):325-35. [QxMD MEDLINE Link] .
de Zwaan M, Mitchell JE, Raymond NC, Spitzer RL. Binge eating disorder: clinical features and treatment of a new diagnosis. Harv Rev Psychiatry . 1994 Mar-Apr. 1 (6):310-25. [QxMD MEDLINE Link] .
Thompson RA. Emotion regulation: a theme in search of definition. Monogr Soc Res Child Dev . 1994. 59 (2-3):25-52. [QxMD MEDLINE Link] .
Berking, M. Affect Regulation Training: A Practitioners' Manual . New York, NY: Springer Science+Business Media, LLC; 2014.
Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clin Psychol Rev . 2015 Aug. 40:111-22. [QxMD MEDLINE Link] .
Engel SG, Crosby RD, Thomas G, Bond D, Lavender JM, Mason T, et al. Ecological Momentary Assessment in Eating Disorder and Obesity Research: a Review of the Recent Literature. Curr Psychiatry Rep . 2016 Apr. 18 (4):37. [QxMD MEDLINE Link] .
Berg KC, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA, et al. Negative affect prior to and following overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Int J Eat Disord . 2015 Sep. 48 (6):641-53. [QxMD MEDLINE Link] .
Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychol Bull . 2011 Jul. 137 (4):660-681. [QxMD MEDLINE Link] .
Bickel WK, Jarmolowicz DP, Mueller ET, Gatchalian KM, McClure SM. Are executive function and impulsivity antipodes? A conceptual reconstruction with special reference to addiction. Psychopharmacology (Berl) . 2012 Jun. 221 (3):361-87. [QxMD MEDLINE Link] .
Gerlach G, Herpertz S, Loeber S. Personality traits and obesity: a systematic review. Obes Rev . 2015 Jan. 16 (1):32-63. [QxMD MEDLINE Link] .
Waxman SE. A systematic review of impulsivity in eating disorders. Eur Eat Disord Rev . 2009 Nov. 17 (6):408-25. [QxMD MEDLINE Link] .
Lavender JM, Green D, Anestis MD, Tull MT, Gratz KL. Negative affect, negative urgency, thought suppression, and bulimic symptoms: a moderated mediation analysis in a sample at-risk for bulimic symptoms. Eur Eat Disord Rev . 2015 May. 23 (3):246-50. [QxMD MEDLINE Link] .
Wenzel KR, Weinstock J, Vander Wal JS, Weaver TL. Examining the role of negative urgency in a predictive model of bulimic symptoms. Eat Behav . 2014 Aug. 15 (3):343-9. [QxMD MEDLINE Link] .
Racine SE, Burt SA, Keel PK, Sisk CL, Neale MC, Boker S, et al. Examining associations between negative urgency and key components of objective binge episodes. Int J Eat Disord . 2015 Jul. 48 (5):527-31. [QxMD MEDLINE Link] .
Pearson CM, Wonderlich SA, Smith GT. A risk and maintenance model for bulimia nervosa: From impulsive action to compulsive behavior. Psychol Rev . 2015 Jul. 122 (3):516-35. [QxMD MEDLINE Link] .
Culbert KM, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, Peterson CB, et al. Associations between negative affect and binge/purge behaviors in women with anorexia nervosa: Considering the role of negative urgency. Compr Psychiatry . 2016 Apr. 66:104-12. [QxMD MEDLINE Link] .
Lavender JM, Utzinger LM, Cao L, Wonderlich SA, Engel SG, Mitchell JE, et al. Reciprocal associations between negative affect, binge eating, and purging in the natural environment in women with bulimia nervosa. J Abnorm Psychol . 2016 Apr. 125 (3):381-6. [QxMD MEDLINE Link] .
Racine SE, Martin SJ. Exploring divergent trajectories: Disorder-specific moderators of the association between negative urgency and dysregulated eating. Appetite . 2016 Aug 1. 103:45-53. [QxMD MEDLINE Link] .
De Young KP, Zander M, Anderson DA. Beliefs about the emotional consequences of eating and binge eating frequency. Eat Behav . 2014 Jan. 15 (1):31-6. [QxMD MEDLINE Link] .
Fischer S, Smith GT, Anderson KG. Clarifying the role of impulsivity in bulimia nervosa. Int J Eat Disord . 2003 May. 33 (4):406-11. [QxMD MEDLINE Link] .
Bijttebier P, Beck I, Claes L, Vandereycken W. Gray's Reinforcement Sensitivity Theory as a framework for research on personality-psychopathology associations. Clin Psychol Rev . 2009 Jul. 29 (5):421-30. [QxMD MEDLINE Link] .
Gray JA. The psychophysiological basis of introversion-extraversion. Behav Res Ther . 1970 Aug. 8 (3):249-66. [QxMD MEDLINE Link] .
Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich HC. Reward-related decision making in eating and weight disorders: A systematic review and meta-analysis of the evidence from neuropsychological studies. Neurosci Biobehav Rev . 2016 Feb. 61:177-96. [QxMD MEDLINE Link] .
Kessler RM, Hutson PH, Herman BK, Potenza MN. The neurobiological basis of binge-eating disorder. Neurosci Biobehav Rev . 2016 Apr. 63:223-38. [QxMD MEDLINE Link] .
Wierenga CE, Ely A, Bischoff-Grethe A, Bailer UF, Simmons AN, Kaye WH. Are Extremes of Consumption in Eating Disorders Related to an Altered Balance between Reward and Inhibition?. Front Behav Neurosci . 2014. 8:410. [QxMD MEDLINE Link] .
Frank GKW, Reynolds JR, Shott ME, O'Reilly RC. Altered temporal difference learning in bulimia nervosa. Biol Psychiatry . 2011 Oct 15. 70 (8):728-735. [QxMD MEDLINE Link] .
Voon V, Morris LS, Irvine MA, Ruck C, Worbe Y, Derbyshire K, et al. Risk-taking in disorders of natural and drug rewards: neural correlates and effects of probability, valence, and magnitude. Neuropsychopharmacology . 2015 Mar. 40 (4):804-12. [QxMD MEDLINE Link] .
Cyders MA, Smith GT. Emotion-based dispositions to rash action: positive and negative urgency. Psychol Bull . 2008 Nov. 134 (6):807-28. [QxMD MEDLINE Link] .
Okon-Singer H, Hendler T, Pessoa L, Shackman AJ. The neurobiology of emotion-cognition interactions: fundamental questions and strategies for future research. Front Hum Neurosci . 2015. 9:58. [QxMD MEDLINE Link] .
Gilmartin MR, Balderston NL, Helmstetter FJ. Prefrontal cortical regulation of fear learning. Trends Neurosci . 2014 Aug. 37 (8):455-64. [QxMD MEDLINE Link] .
Rolls ET. A biased activation theory of the cognitive and attentional modulation of emotion. Front Hum Neurosci . 2013. 7:74. [QxMD MEDLINE Link] .
Yokum S, Stice E. Cognitive regulation of food craving: effects of three cognitive reappraisal strategies on neural response to palatable foods. Int J Obes (Lond) . 2013 Dec. 37 (12):1565-70. [QxMD MEDLINE Link] .
Stice E, Yokum S, Burger KS, Epstein LH, Small DM. Youth at risk for obesity show greater activation of striatal and somatosensory regions to food. J Neurosci . 2011 Mar 23. 31 (12):4360-6. [QxMD MEDLINE Link] .
Joos AA, Saum B, Zeeck A, Perlov E, Glauche V, Hartmann A, et al. Frontocingular dysfunction in bulimia nervosa when confronted with disease-specific stimuli. Eur Eat Disord Rev . 2011 Sep-Oct. 19 (5):447-53. [QxMD MEDLINE Link] .
Balodis IM, Molina ND, Kober H, Worhunsky PD, White MA, Rajita Sinha, et al. Divergent neural substrates of inhibitory control in binge eating disorder relative to other manifestations of obesity. Obesity (Silver Spring) . 2013 Feb. 21 (2):367-77. [QxMD MEDLINE Link] .
Marsh R, Steinglass JE, Gerber AJ, Graziano O'Leary K, Wang Z, Murphy D, et al. Deficient activity in the neural systems that mediate self-regulatory control in bulimia nervosa. Arch Gen Psychiatry . 2009 Jan. 66 (1):51-63. [QxMD MEDLINE Link] .
Marsh R, Horga G, Wang Z, Wang P, Klahr KW, Berner LA, et al. An FMRI study of self-regulatory control and conflict resolution in adolescents with bulimia nervosa. Am J Psychiatry . 2011 Nov. 168 (11):1210-20. [QxMD MEDLINE Link] .
Haukoos JS, Lewis RJ. The Propensity Score. JAMA . 2015 Oct 20. 314 (15):1637-8. [QxMD MEDLINE Link] .
Corwin RL, Avena NM, Boggiano MM. Feeding and reward: perspectives from three rat models of binge eating. Physiol Behav . 2011 Jul 25. 104 (1):87-97. [QxMD MEDLINE Link] .
Logue SF, Gould TJ. The neural and genetic basis of executive function: attention, cognitive flexibility, and response inhibition. Pharmacol Biochem Behav . 2014 Aug. 123:45-54. [QxMD MEDLINE Link] .
Fineberg NA, Potenza MN, Chamberlain SR, Berlin HA, Menzies L, Bechara A, et al. Probing compulsive and impulsive behaviors, from animal models to endophenotypes: a narrative review. Neuropsychopharmacology . 2010 Feb. 35 (3):591-604. [QxMD MEDLINE Link] .
London ED. Impulsivity, Stimulant Abuse, and Dopamine Receptor Signaling. Adv Pharmacol . 2016. 76:67-84. [QxMD MEDLINE Link] .
Bailer UF, Bloss CS, Frank GK, Price JC, Meltzer CC, Mathis CA, et al. 5-HT₁A receptor binding is increased after recovery from bulimia nervosa compared to control women and is associated with behavioral inhibition in both groups. Int J Eat Disord . 2011 Sep. 44 (6):477-87. [QxMD MEDLINE Link] .
Bailer UF, Frank GK, Price JC, Meltzer CC, Becker C, Mathis CA, et al. Interaction between serotonin transporter and dopamine D2/D3 receptor radioligand measures is associated with harm avoidant symptoms in anorexia and bulimia nervosa. Psychiatry Res . 2013 Feb 28. 211 (2):160-8. [QxMD MEDLINE Link] .
Murray S, Tulloch A, Gold MS, Avena NM. Hormonal and neural mechanisms of food reward, eating behaviour and obesity. Nat Rev Endocrinol . 2014 Sep. 10 (9):540-52. [QxMD MEDLINE Link] .
Scott MM, Xu Y, Elias CF, Williams KW. Central regulation of food intake, body weight, energy expenditure, and glucose homeostasis. Front Neurosci . 2014. 8:384. [QxMD MEDLINE Link] .
Culbert KM, Racine SE, Klump KL. Hormonal Factors and Disturbances in Eating Disorders. Curr Psychiatry Rep . 2016 Jul. 18 (7):65. [QxMD MEDLINE Link] .
Sam AH, Troke RC, Tan TM, Bewick GA. The role of the gut/brain axis in modulating food intake. Neuropharmacology . 2012 Jul. 63 (1):46-56. [QxMD MEDLINE Link] .
Maniam J, Morris MJ. The link between stress and feeding behaviour. Neuropharmacology . 2012 Jul. 63 (1):97-110. [QxMD MEDLINE Link] .
Barbano MF, Cador M. Opioids for hedonic experience and dopamine to get ready for it. Psychopharmacology (Berl) . 2007 Apr. 191 (3):497-506. [QxMD MEDLINE Link] .
Kelley AE, Bakshi VP, Fleming S, Holahan MR. A pharmacological analysis of the substrates underlying conditioned feeding induced by repeated opioid stimulation of the nucleus accumbens. Neuropsychopharmacology . 2000 Oct. 23 (4):455-67. [QxMD MEDLINE Link] .
Avena NM, Bocarsly ME. Dysregulation of brain reward systems in eating disorders: neurochemical information from animal models of binge eating, bulimia nervosa, and anorexia nervosa. Neuropharmacology . 2012 Jul. 63 (1):87-96. [QxMD MEDLINE Link] .
Schultz W, Dayan P, Montague PR. A neural substrate of prediction and reward. Science . 1997 Mar 14. 275 (5306):1593-9. [QxMD MEDLINE Link] .
Frank GK. Recent advances in neuroimaging to model eating disorder neurobiology. Curr Psychiatry Rep . 2015 Apr. 17 (4):559. [QxMD MEDLINE Link] .
Frank GK. What causes eating disorders, and what do they cause?. Biol Psychiatry . 2015 Apr 1. 77 (7):602-3. [QxMD MEDLINE Link] .
O'Hara CB, Campbell IC, Schmidt U. A reward-centred model of anorexia nervosa: a focussed narrative review of the neurological and psychophysiological literature. Neurosci Biobehav Rev . 2015 May. 52:131-52. [QxMD MEDLINE Link] .
Frank GK. Advances in the diagnosis of anorexia nervosa and bulimia nervosa using brain imaging. Expert Opin Med Diagn . 2012 May 1. 6 (3):235-244. [QxMD MEDLINE Link] .
Agras, W. S., Dorian, B., Kirkley, B. G., et al. Imipramine in the treatment of bulimia: A double-blind controlled study. Int J Eat Disord . 1987. 6(1):29–38.
Pope HG Jr, Hudson JI, Jonas JM, Yurgelun-Todd D. Bulimia treated with imipramine: a placebo-controlled, double-blind study. Am J Psychiatry . 1983 May. 140 (5):554-8. [QxMD MEDLINE Link] .
Mitchell JE, Groat R. A placebo-controlled, double-blind trial of amitriptyline in bulimia. J Clin Psychopharmacol . 1984 Aug. 4 (4):186-93. [QxMD MEDLINE Link] .
Mitchell JE, Pyle RL, Eckert ED, Hatsukami D, Pomeroy C, Zimmerman R. A comparison study of antidepressants and structured intensive group psychotherapy in the treatment of bulimia nervosa. Arch Gen Psychiatry . 1990 Feb. 47 (2):149-57. [QxMD MEDLINE Link] .
Agras WS, Rossiter EM, Arnow B, Schneider JA, Telch CF, Raeburn SD, et al. Pharmacologic and cognitive-behavioral treatment for bulimia nervosa: a controlled comparison. Am J Psychiatry . 1992 Jan. 149 (1):82-7. [QxMD MEDLINE Link] .
Barlow J, Blouin J, Blouin A, Perez E. Treatment of bulimia with desipramine: a double-blind crossover study. Can J Psychiatry . 1988 Mar. 33 (2):129-33. [QxMD MEDLINE Link] .
Blouin AG, Blouin JH, Perez EL, Bushnik T, Zuro C, Mulder E. Treatment of bulimia with fenfluramine and desipramine. J Clin Psychopharmacol . 1988 Aug. 8 (4):261-9. [QxMD MEDLINE Link] .
McCann UD, Agras WS. Successful treatment of nonpurging bulimia nervosa with desipramine: a double-blind, placebo-controlled study. Am J Psychiatry . 1990 Nov. 147 (11):1509-13. [QxMD MEDLINE Link] .
Walsh BT, Hadigan CM, Devlin MJ, Gladis M, Roose SP. Long-term outcome of antidepressant treatment for bulimia nervosa. Am J Psychiatry . 1991 Sep. 148 (9):1206-12. [QxMD MEDLINE Link] .
Sabine EJ, Yonace A, Farrington AJ, Barratt KH, Wakeling A. Bulimia nervosa: a placebo controlled double-blind therapeutic trial of mianserin. Br J Clin Pharmacol . 1983. 15 Suppl 2 (Suppl 2):195S-202S. [QxMD MEDLINE Link] .
Carruba MO, Cuzzolaro M, Riva L, Bosello O, Liberti S, Castra R, et al. Efficacy and tolerability of moclobemide in bulimia nervosa: a placebo-controlled trial. Int Clin Psychopharmacol . 2001 Jan. 16 (1):27-32. [QxMD MEDLINE Link] .
Walsh BT, Gladis M, Roose SP, Stewart JW, Stetner F, Glassman AH. Phenelzine vs placebo in 50 patients with bulimia. Arch Gen Psychiatry . 1988 May. 45 (5):471-5. [QxMD MEDLINE Link] .
Walsh BT, Stewart JW, Roose SP, Gladis M, Glassman AH. Treatment of bulimia with phenelzine. A double-blind, placebo-controlled study. Arch Gen Psychiatry . 1984 Nov. 41 (11):1105-9. [QxMD MEDLINE Link] .
Kennedy SH, Piran N, Warsh JJ, Prendergast P, Mainprize E, Whynot C, et al. A trial of isocarboxazid in the treatment of bulimia nervosa. J Clin Psychopharmacol . 1988 Dec. 8 (6):391-6. [QxMD MEDLINE Link] .
Kennedy SH, Goldbloom DS, Ralevski E, Davis C, D'Souza JD, Lofchy J. Is there a role for selective monoamine oxidase inhibitor therapy in bulimia nervosa? A placebo-controlled trial of brofaromine. J Clin Psychopharmacol . 1993 Dec. 13 (6):415-22. [QxMD MEDLINE Link] .
Rothschild R, Quitkin HM, Quitkin FM, Stewart JW, Ocepek-Welikson K, McGrath PJ, et al. A double-blind placebo-controlled comparison of phenelzine and imipramine in the treatment of bulimia in atypical depressives. Int J Eat Disord . 1994 Jan. 15 (1):1-9. [QxMD MEDLINE Link] .
Horne RL, Ferguson JM, Pope HG Jr, Hudson JI, Lineberry CG, Ascher J, et al. Treatment of bulimia with bupropion: a multicenter controlled trial. J Clin Psychiatry . 1988 Jul. 49 (7):262-6. [QxMD MEDLINE Link] .
Pope HG Jr, Keck PE Jr, McElroy SL, Hudson JI. A placebo-controlled study of trazodone in bulimia nervosa. J Clin Psychopharmacol . 1989 Aug. 9 (4):254-9. [QxMD MEDLINE Link] .
Brambilla F, Draisci A, Peirone A, Brunetta M. Combined cognitive-behavioral, psychopharmacological and nutritional therapy in bulimia nervosa. Neuropsychobiology . 1995. 32 (2):68-71. [QxMD MEDLINE Link] .
Milano W, Siano C, Putrella C, Capasso A. Treatment of bulimia nervosa with fluvoxamine: a randomized controlled trial. Adv Ther . 2005 May-Jun. 22 (3):278-83. [QxMD MEDLINE Link] .
Fichter MM, Krüger R, Rief W, Holland R, Döhne J. Fluvoxamine in prevention of relapse in bulimia nervosa: effects on eating-specific psychopathology. J Clin Psychopharmacol . 1996 Feb. 16 (1):9-18. [QxMD MEDLINE Link] .
Fichter MM, Leibl C, Krüger R, Rief W. Effects of fluvoxamine on depression, anxiety, and other areas of general psychopathology in bulimia nervosa. Pharmacopsychiatry . 1997 May. 30 (3):85-92. [QxMD MEDLINE Link] .
Schmidt U, Cooper PJ, Essers H, Freeman CP, Holland RL, Palmer RL, et al. Fluvoxamine and graded psychotherapy in the treatment of bulimia nervosa: a randomized, double-blind, placebo-controlled, multicenter study of short-term and long-term pharmacotherapy combined with a stepped care approach to psychotherapy. J Clin Psychopharmacol . 2004 Oct. 24 (5):549-52. [QxMD MEDLINE Link] .
Fluoxetine in the treatment of bulimia nervosa. A multicenter, placebo-controlled, double-blind trial. Fluoxetine Bulimia Nervosa Collaborative Study Group. Arch Gen Psychiatry . 1992 Feb. 49 (2):139-47. [QxMD MEDLINE Link] .
Goldstein DJ, Wilson MG, Thompson VL, Potvin JH, Rampey AH Jr. Long-term fluoxetine treatment of bulimia nervosa. Fluoxetine Bulimia Nervosa Research Group. Br J Psychiatry . 1995 May. 166 (5):660-6. [QxMD MEDLINE Link] .
Goldbloom DS, Olmsted M, Davis R, Clewes J, Heinmaa M, Rockert W, et al. A randomized controlled trial of fluoxetine and cognitive behavioral therapy for bulimia nervosa: short-term outcome. Behav Res Ther . 1997 Sep. 35 (9):803-11. [QxMD MEDLINE Link] .
Walsh BT, Wilson GT, Loeb KL, Devlin MJ, Pike KM, Roose SP, et al. Medication and psychotherapy in the treatment of bulimia nervosa. Am J Psychiatry . 1997 Apr. 154 (4):523-31. [QxMD MEDLINE Link] .
Romano SJ, Halmi KA, Sarkar NP, Koke SC, Lee JS. A placebo-controlled study of fluoxetine in continued treatment of bulimia nervosa after successful acute fluoxetine treatment. Am J Psychiatry . 2002 Jan. 159 (1):96-102. [QxMD MEDLINE Link] .
Hsu LK, Clement L, Santhouse R, Ju ES. Treatment of bulimia nervosa with lithium carbonate. A controlled study. J Nerv Ment Dis . 1991 Jun. 179 (6):351-5. [QxMD MEDLINE Link] .
Hoopes SP, Reimherr FW, Hedges DW, Rosenthal NR, Kamin M, Karim R, et al. Treatment of bulimia nervosa with topiramate in a randomized, double-blind, placebo-controlled trial, part 1: improvement in binge and purge measures. J Clin Psychiatry . 2003 Nov. 64 (11):1335-41. [QxMD MEDLINE Link] .
Nickel C, Tritt K, Muehlbacher M, Pedrosa Gil F, Mitterlehner FO, Kaplan P, et al. Topiramate treatment in bulimia nervosa patients: a randomized, double-blind, placebo-controlled trial. Int J Eat Disord . 2005 Dec. 38 (4):295-300. [QxMD MEDLINE Link] .
Faris PL, Kim SW, Meller WH, Goodale RL, Oakman SA, Hofbauer RD, et al. Effect of decreasing afferent vagal activity with ondansetron on symptoms of bulimia nervosa: a randomised, double-blind trial. Lancet . 2000 Mar 4. 355 (9206):792-7. [QxMD MEDLINE Link] .
Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. J Consult Clin Psychol . 2008 Apr. 76 (2):329-40. [QxMD MEDLINE Link] .
Franko DL, Tabri N, Keshaviah A, Murray HB, Herzog DB, Thomas JJ, et al. Predictors of long-term recovery in anorexia nervosa and bulimia nervosa: Data from a 22-year longitudinal study. J Psychiatr Res . 2018 Jan. 96:183-188. [QxMD MEDLINE Link] .
- Parotid hypertrophy. Reprinted with permission [Mandel L, Siamak A. Diagnosing bulimia nervosa with parotid gland swelling. J Am Dent Assoc. 2004 May;135 (5):613-16.]
- Dental caries. Reprinted with permission [Wolcott RB, Yager J, Gordon G. Dental sequelae to the binge-purge syndrome (bulimia): report of cases. J Am Dent Assoc. 1984 Nov;109(5):723-25.].
- Russell sign. Reprinted with permission [Glorio R, Allevato M, De Pablo A, et al. Prevalence of cutaneous manifestations in 200 patients with eating disorders. Int J Derm. 2001 Dec;39(5):348-53.].
- This chest radiograph demonstrates pneumomediastinum, which can occur in association with esophageal rupture from forceful vomiting.
- Water-soluble contrast esophagram from a patient with esophageal perforation after esophageal dilation shows contrast leak (arrowheads) and normal esophageal lumen (arrows).
- Mallory-Weiss tear. Typical longitudinal mucosal tear with overlying fibrinous exudate extending from the distal esophagus to the gastric cardia. Courtesy of Christopher J Gostout, MD.
Anorexia Nervosa | AN and BN | Bulimia Nervosa |
|---|---|---|
Restriction of energy intake relative to requirement, leading to significantly low body weight in the context of age, sex, developmental trajectory, and physical health | Recurrent episodes of binge eating: a) eating in a discrete period of time, within a 2-hour period, an amount that is definitely larger than what most would eat in that time period; b) a sense of lack of control over eating | |
Intense fear of gaining weight or of becoming fat, or persistent behavior that interferes with weight gain, even though at a significantly low weight | Recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise | |
Disturbance in which one's body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or persistent lack of recognition of the seriousness of the current low body weight | The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months | |
Two types: Restrictive and Purge/Binge-Eating type | The disturbance does not occur exclusively during episodes of AN | |
Body Dysmorphic Disorder | BDD and BN | BN |
Preoccupation with one or more perceived defects or flaws in physical appearance that are not observable or appear slight to others | Disturbance in which one's body weight or shape is experienced, undue influence of body weight or shape on self-evaluation | Recurrent episodes of binge eating: a) eating in a discrete period of time, within a 2-hour period, an amount that is definitely larger than what most would eat in that time period; b) a sense of lack of control over eating |
At some point during the course of the disorder, the individual has performed repetitive behaviors or mental acts in response to the appearance concerns | The preoccupation causes significant distress or impairment in social, occupational, or other important areas of functioning | Recurrent inappropriate compensatory behaviors in order to prevent weight gain, such as self-induced vomiting; misuse of laxatives, diuretics, or other medications; fasting; or excessive exercise |
The appearance preoccupation is not better explained by concerns with body fat or weight in an individual whose symptoms meet diagnostic criteria for an eating disorder | The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for 3 months | |
Differential Diagnosis of Bulimia Nervosa ] | ||
Contributor Information and Disclosures
Guido Klaus Wilhelm Frank, MD Professor, Department of Psychiatry, University of California, San Diego, School of Medicine; Director of Psychiatry, Medical Behavioral Unit, Rady Children’s Hospital-San Diego Guido Klaus Wilhelm Frank, MD is a member of the following medical societies: Academy for Eating Disorders, American Academy of Child and Adolescent Psychiatry , American College of Neuropsychopharmacology , Eating Disorders Research Society, German Medical Association , Society of Biological Psychiatry Disclosure: Nothing to disclose.
Lisa D Adler, MD Assistant Professor of Clinical Health Sciences, Department of Psychiatry, University of California San Diego Health Sciences, UCSD Eating Disorder Center for Treatment and Research, Medical Behavioral Unit, Rady Children’s Hospital Lisa D Adler, MD is a member of the following medical societies: American Academy of Child and Adolescent Psychiatry Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Received salary from Medscape for employment. for: Medscape.
David Bienenfeld, MD Professor, Departments of Psychiatry and Geriatric Medicine, Wright State University, Boonshoft School of Medicine David Bienenfeld, MD is a member of the following medical societies: American Medical Association , American Psychiatric Association , Association for Academic Psychiatry Disclosure: Nothing to disclose.
Donald M Hilty, MD, MBA Associate Chief of Staff, Mental Health, Northern California VA Healthcare System; Professor of Psychiatry, Department of Psychiatry and Behavioral Sciences, University of California, Davis, School of Medicine Donald M Hilty, MD, MBA is a member of the following medical societies: American Association for Technology in Psychiatry , American Psychiatric Association , American Telemedicine Association , Association for Academic Psychiatry Disclosure: Nothing to disclose.
Christine I Osterhout, MD Resident Physician, Department of Psychiatry and Behavioral Sciences, University of California, Davis Health System Christine I Osterhout, MD is a member of the following medical societies: Alpha Omega Alpha , American Academy of Child and Adolescent Psychiatry , American Academy of Psychiatry and the Law , American Medical Association , American Psychiatric Association Disclosure: Nothing to disclose.
Lorin M Scher, MD, FACLP Clinical Professor of Psychiatry and Behavioral Sciences, Vice-Chair for Education, Roy T Brophy Endowed Chair, Director, Integrated Behavioral Health Services, Medical Director, Government and Community Relations, UC Davis Health Lorin M Scher, MD, FACLP is a member of the following medical societies: Academy of Consultation-Liaison Psychiatry, Alpha Omega Alpha , American Medical Association , American Psychiatric Association , Association of Directors of Medical Student Education in Psychiatry, California Medical Association , Central California Psychiatric Society, Sierra Sacramento Valley Medical Society Disclosure: Nothing to disclose.
Joel Yager, MD Professor of Psychiatry, University of Colorado Health Sciences Center; Professor of Psychiatry Emeritus, University of California, Los Angeles, David Geffen School of Medicine; Professor of Psychiatry Emeritus, University of New Mexico School of Medicine Joel Yager, MD is a member of the following medical societies: Alpha Omega Alpha , American Association for the Advancement of Science , American Medical Association , American Psychiatric Association , Association for Academic Psychiatry Disclosure: Nothing to disclose.
Gagandeep Randhawa, MBBS Resident Physician, Department of Psychiatry, Kaweah Delta Medical Center, University of California, Irvine, School of Medicine Gagandeep Randhawa, MBBS is a member of the following medical societies: American Psychiatric Association , Indian Doctors for Peace and Development Disclosure: Nothing to disclose.
Robert C Daly, MB, ChB, MPH Senior Fellow, Department of Behavioral Endocrinology, National Institute of Mental Health, National Institutes of Health
Disclosure: Nothing to disclose.
Raj K Kalapatapu, MD Fellow, Addiction Psychiatry, Columbia University College of Physicians and Surgeons
Raj K Kalapatapu is a member of the following medical societies: American Academy of Addiction Psychiatry, American Academy of Child and Adolescent Psychiatry, American Association for Geriatric Psychiatry, American Medical Association, and American Psychiatric Association.
Gabriel I Uwaifo, MD Associate Professor, Section of Endocrinology, Diabetes and Metabolism, Louisiana State University School of Medicine in New Orleans; Adjunct Professor, Joint Program on Diabetes, Endocrinology and Metabolism, Pennington Biomedical Research Center in Baton Rouge
Gabriel I Uwaifo, MD is a member of the following medical societies: American Association of Clinical Endocrinologists, American College of Physicians-American Society of Internal Medicine, American Diabetes Association, American Medical Association, American Society of Hypertension, and The Endocrine Society
Kelda Harris Walsh, MD Assistant Professor of Clinical Psychiatry, Section of Child and Adolescent Psychiatry, Department of Psychiatry, Indiana University School of Medicine; Chief, Obsessive-Compulsive/Tourette/Anxiety Disorders Clinic, Riley Hospital for Children
Acknowledgments
The authors would also like to acknowledge the contributions of Rebecca Davis, Librarian at the University of California (UC), Davis and Dr. Eric Rickin, Director for the Center for Overcoming Problem Eating (COPE) at the Western Psychiatric Institute and Clinic, University of Pittsburgh Medical Center. Finally, the authors thank the Department of Psychiatry and Behavioral Sciences at UC Davis.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- Binge Eating Disorder (BED)
- Nutrition for the Female Athlete
- Grief Support in the ED
- Fast Five Quiz: Test Your Knowledge of Binge-Eating Disorder
- Ocular Burns and Chemical Injuries
- Acute Conjunctivitis (Pink Eye)
- Fast Five Quiz: Bulimia Nervosa
- Psychiatric Comorbidity Prevalent in Eating Disorders
- Why Do MDs Have Such a High Rate of Eating Disorders?
- How to Cure Hedonic Eating?

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 20022221362-overviewDiseases & Conditions Diseases & Conditions Binge Eating Disorder (BED)
- 2003/viewarticle/993379Clinical Review Is Disordered Eating in Young People Now a Public Health Emergency? 0.25 CME / CE / ABIM MOC Credits Clinical Review You are being redirected to Medscape Education Yes, take me there 0.25 CME / CE / ABIM MOC Is Disordered Eating in Young People Now a Public Health Emergency?
- 2001/s/viewarticle/996166 Screen Patients With Bipolar Disorders for Eating Disorders
- 2001/viewarticle/975126 Youth With Bipolar Disorder at High Risk of Eating Disorders
Dublin 01 677 1021 [email protected]
Galway 091 725 750 [email protected]
Mon-Fri 8am-9pm Sat 9am-6pm
Case Study of Bulimia Nervosa (BN)
- By : Maggie Molloy
Bulimia Nervosa is an eating disorder characterized by binge eating followed by purging. Binge eating refers to eating a large amount of food in a short amount of time. Purging refers to the attempts to get rid of the food consumed. Bulimia means to ‘eat like an ox’, although people have been known to ‘eat like an ox‘ from antiquity, it was not until 1979 that a London psychiatrist, Gerald Russell, identified 40% of his Anorexia Nervosa patients with an ‘ominous variation’ of the disorder – the variation being that they from time to time went on binges.
In this case study I sought to give an insight into Cognitive Behavioural Therapy (CBT) treatment for Bulimia Nervosa (BN). It was important to back up my assessment in the first session with a G.P report which contained Complete blood count;
Chem-20 panel which measures electrolytes, vitamins, liver and pancreatic function, adrenal glands, (levels of cortisol and adrenaline produced in times of stress);
Thyroid and parathyroid pane l which indicates level of metabolic functions.
**Ask permission from your client to get the report.
Suitability for treatment was formally measured using the Safron and Segal (1990) Suitability for Short–term Cognitive Therapy Rating Scale. (aspects of the cognitive therapy process are rated on a scale of 0-5). High Rating indicate a good prognosis and low ratings indicate a poor one.
Client History
Jessica (pseudonym) aged 22 presented to the centre with a four-year history of binge eating, vomiting and laxative use. Jessica stated that at the age of 18, following the break-up of a one-year relationship with her boyfriend (she did not want to become intimate with him). She had begun to eat excessively at times (comfort eating) as a way of coping with the heartache it caused.
Jessica put on some extra weight, approximately 4 kg over the course of a few months and was very upset when she discovered that some of her outfits were not fitting her, especially in the run up to a summer holiday.
Jessica had known about people vomiting as a means of weight control and recalled some of her school friends telling her it was a handy way not to put on weight. However, she had never really considered doing this herself, as she thought it was a ‘disgusting thing to do’.
She stated that one evening after a particularly large bout of over eating, she felt very uncomfortable and thought that if she could only vomit it would at least relieve the discomfort. Using her forefinger, she stuck it down the back of her throat and began vomiting.
Afterwards she felt unwell, her throat was raw and her stomach sore, but she admitted feeling some relief from the feeling of guilt and regret of having eaten too much. She vowed at the time never to do it again. A few evenings later after a night out with friends and having consumed ‘a few too many‘ alcoholic beverages she engaged in what she described as a ‘feeding frenzy ‘, eating almost anything she could get her hands on in the fridge and cupboard.
It seemed easier to vomit this time and the next day she bought a packet of laxatives, to clear out the system, taking 3 times the recommended dose.
Jessica tried starving herself over the next few days, feeling determined to try and get her weight under control and start a ‘new chapter in her life’. This lasted until day 3 when weak with hunger and coming home from a late night at work, she could not resist the temptation to stop off at a local Chinese restaurant as she passed by it. They had a buffet–style service that meant she could keep going back up to eat whatever she wanted. Having left feeling stuffed and very guilty, vomiting seemed the obvious option and laxatives were used the following day.
Over the course of the next few months a pattern developed whereby she would attempt any and every new diet, she lasted 2 to 4 days and this would end up in bingeing and purging behaviour.
Jessica Weight was 9st-8lbs and her Height was 5ft-3ins
None of Jessica’s family or friends were aware of her difficulties, although they know she was constantly dieting. Jessica felt very unhappy with life, the thought of suicide had occasionally crossed her mind but it always occurred after a night out drinking followed by a binge and purging episode. Jessica was taking 40 mg of Fluoxetine (Prozac) when she attended therapy.
Personal background
Jessica was raised the eldest the eldest of 5 children. She had 1 sister and 3 brothers, her parents divorced when she was aged 16 yrs, mainly due to her father’s drinking.
Jessica felt close to her Mum who had a history of been treated for depression by her G.P.
Jessica disclosed that from the age of 12 to 14 she was sexually abused by a neighbour, she never told her parents until she reached the age of sixteen after they moved back to Ireland. Leaving school at sixteen she managed to secure employment in a marketing company and had worked her way up the firm, taking several professional examinations along the way.
The main DSM-V criteria for Bulimia Nervosa that Jessica was displaying were as follows;
- Eating a large amount of food with a short space of time
- Bingeing three to four times per week
- She also experiences a sense of lack of control over eating, a feeling that she cannot stop.
- She was taking laxatives at least twice a week
- Over-evaluation or concern about shape, weight and appearance
- Secretive behaviour
- Vomiting three to four times per week
- Co-morbidity features – depression, alcohol misuse
CBT Treatment
Phase 1: Sessions 1 to 4
Establishing a sound therapeutic relationship. Setting treatment goals, setting homework. Explaining the CBT model of Bulimia Nervosa, including discussing predisposing, precipitating and perpetuating factors which resulted in an initial formulation been established. Motivation for Change (Pros and Cons of changing)
Psychoeducation, educating Jessica on the adverse consequences of bingeing and purging behaviour and explained the blood sugar imbalance, glycemic index (GI), foods that have high and low GI and how neurotransmitters influence hunger and mood.
Explaining the importance of introducing a regular eating pattern of 3 meals and 2 snacks/day (gave her a detailed specific food dairy). Disrupting the vicious cycle of bingeing and purging behaviour, noting particular triggers. Identifying the connection between thoughts, feelings and behaviour within the context of the Eating Disorder.
Phase 2: Sessions 5 to 15
This phase is at the heart of therapy for Jessica. It involved addressing the maintaining factors listed below:
- Negative Body Image
- Cognitive Distortions
- Feelings, (regret, guilt, low mood, shame etc.)
- Lifestyle activities, Self –Esteem
- Physiology (blood sugar, stimulants)
- Relationships
- Food Scripts
- Addictive Process (bingeing/purging alcohol misuse)
Interventions and homework worksheets in treating the above was carried out in the sessions.
Phase 3 (Final): Sessions 16 -19
Relapse Management Skills discussed.
- What made her vulnerable to developing the problem in the first place?
- What has she learned in Treatment?
- What areas leave her vulnerable?
- What strategies can undermine these vulnerabilities?
- Dealing with a setback
- What are her personal strengths?
Contact the Author of This Article
If you would like to get in touch with the author please click below and send a quick email.
- Bereavement & Grief
- Life Existential Issues
- Self-Improvement
Advertisement
Psychological Intervention in a Case of Bulimia Nervosa: A Case Report
- Published: 20 February 2014
- Volume 59 , pages 68–75, ( 2014 )
Cite this article

- Paakhi Srivastava 1 ,
- Piyali Mandal 1 ,
- Manju Mehta 1 &
- Rajesh Sagar 1
624 Accesses
Explore all metrics
This paper presents a case report detailing the use of an enhanced form of enhanced cognitive behavior therapy (CBT) and other techniques that were employed when faced with impediments in adhering to manualized CBT-E. Ms. S, 22 years old unmarried female pursuing MBBS final year, belonging to upper middle socioeconomic status and urban domicile was provided with 28 weekly sessions of psychotherapy to simultaneously address the patient’s symptoms and try to effect change across multiple domains. A single case design was adopted. Therapy was conducted over 9 months. A total of 28 sessions were taken, with the frequency of two sessions/week initially, and then moving onto one session/week. Pre and Post assessments using Binge Eating Scale, BDI-II, height and weight measurements and frequency of binging episodes using visual analogue scale were done. On measures of pre and post assessment there was 87 % improvement in Binging Episodes, 82 % improvement on Binge Eating Scale and client had 3 kg weight gain with reduction in depression as assessed on BDI-II. The gains were maintained at 1 month follow up. The use and deviations from CBT E, therapy process, role of family and challenges to intervention will be discussed in this case report.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Psychotherapy for Binge Eating
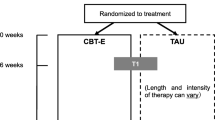
Effectiveness of enhanced cognitive behavior therapy for bulimia nervosa in Japan: a randomized controlled trial protocol

A 12-month study of dialectical behavioral therapy for bοrderline patients suffering from eating disorders
Agras, W. S., & Telch, C. F. (1998). The effects of caloric deprivation and negative affect on binge eating in obese binge-eating disordered women. Behavior Therapy, 29 , 491–503.
Article Google Scholar
Agras, W. S., Walsh, B. T., Fairburn, C. G., Wilson, G. T., & Kraemer, H. C. (2000). A multicenter comparison of cognitive-behavioural therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry, 57 , 459–466.
Article PubMed Google Scholar
Ajzen, I. (1985). From intention to actions: A theory of planned behavior. In J. Kuhl & J. Beckman (Eds.), Action-control: From cognition to behavior (pp. 11–39). Heidelberg: Springer.
Chapter Google Scholar
Beck, A. T., Rush, A. J., Shaw, B. F., & Emery, G. (1979). Cognitive therapy of depression . New York: Guilford.
Google Scholar
Bhugra, D., Bhui, K., & Gupta, K. R. (2000). Bulimic disorders and sociocentric values in north India. Social Psychiatry and Psychiatric Epidemiology, 35 , 86–93.
Chadda, R. K., & Sinha, K. D. (2013). Indian family systems, collectivistic society and psychotherapy. Indian Journal of Psychiatry, 55 (Suppl 2), S299–S309.
Article PubMed Central PubMed Google Scholar
Chandra, P. S., Shah, A., Shenoy, J., Kumar, U., Varghese, M., Bhatti, R. S., et al. (1995). Family pathology and anorexia in the Indian context. International Journal of Social Psychiatry, 41 , 292–298.
Cooper, Z., & Stewart, A. (2008). CBT-E and the younger patient. In C. G. Fairburn (Ed.), Cognitive behavior therapy and eating disorders (pp. 221–230). New York: Guilford Press.
Deitz, E. D., & Repp, A. C. (1983). Reducing behavior through reinforcement. Exceptional Education Quarterly, 3 , 34–46.
Edwards, D. J. A., Dattilio, F. M., & Bromley, D. B. (2004). Developing evidence-based practice: the role of case-based research. Professional Psychology: Research and Practice, 35 (6), 589–597.
Fairburn, C. G., Cooper, Z., & Cooper, P. J. (1986). The clinical features and maintenance of bulimia nervosa. In K. D. Brownwell & J. P. Foreyt (Eds.), Physiology, psychology and treatment of the eating disorders (pp. 389–404). New York: Basic Books.
Fairburn, C. G., Marcus, M. D., & Wilson, G. T. (1993). Cognitive behaviour therapy for binge eating and bulimia nervosa: A comprehensive treatment manual. In C. G. Fairburn, & G. T. Wilson (Eds.), Binge eating: Nature, assessment and treatment (pp. 361–404.). New York: Guilford Press.
Fairburn, C. G., Cooper, Z., & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41 , 509–528.
Fairburn, C.G., Cooper, Z., & Shafran, R.(2008). Enhanced cognitive behavior therapy for eating disorders: the core protocol. In C.G. Fairburn (Ed.), Cognitive behavior therapy and eating disorders (pp. 47–193). New York: Guilford Press.
Fairburn, C. G., Cooper, Z., Doll, H. A., O’Connor, M. E., Bohn, K., Hawker, D. M., et al. (2009). Transdiagnostic cognitive-behavioral therapy for patients with eating disorders: a two-site trial with 60-week follow-up. American Journal of Psychiatry, 166 , 311–319.
Hooley, J. M. (2007). Expressed emotion and relapse of psychopathology. Annual Review of Clinical Psychology, 3 , 329–352.
Khandelwal, S. K., Sharan, P., & Saxena, S. (1995). Eating disorders: an Indian perspective. International Journal of Social Psychiatry, 41 (2), 132–146.
Salkovskis, P. M. (2010). Cognitive behavioural therapy. In: M. Barker, A. Vossler, & D. Langdridge (Eds.), Understanding counselling and psychotherapy . SAGE Publications/Open University.
Shah, A., Varghese, M., Udaya Kumar, G. S., Bhatti, R. S., Raguram, A., Sobhana, H., et al. (2000). Brief family therapy training in India. Journal of Family Psychotherapy, 11 , 41–53.
Sudhir, P. M., Kumariah, V., & Munichoodappa, C. (2003). Role of family in the management of type-I diabetes: an Indian experience. Journal of Clinical Psychology, 59 (6), 715–722.
Wolberg, L. R. (1988). The technique of psychotherapy (4th ed.). Philadelphia: Grune & Stratton.
Download references
Acknowledgments
It has been an invaluable learning experience for the therapist to understand phenomenology of eating disorders, role of family and the process of therapy including preparation of this manuscript.
Author information
Authors and affiliations.
Department of Psychiatry, All India Institute of Medical Sciences, Room No 4089, Fourth Floor, Teaching Block, New Delhi, 110029, India
Paakhi Srivastava, Piyali Mandal, Manju Mehta & Rajesh Sagar
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Paakhi Srivastava .
Rights and permissions
Reprints and permissions
About this article
Srivastava, P., Mandal, P., Mehta, M. et al. Psychological Intervention in a Case of Bulimia Nervosa: A Case Report. Psychol Stud 59 , 68–75 (2014). https://doi.org/10.1007/s12646-014-0242-1
Download citation
Received : 22 June 2013
Accepted : 15 January 2014
Published : 20 February 2014
Issue Date : March 2014
DOI : https://doi.org/10.1007/s12646-014-0242-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Enhanced cognitive behavior therapy
- Bulimia Nervosa
- Find a journal
- Publish with us
- Track your research

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

6.34: Bulimia Nervosa
- Last updated
- Save as PDF
- Page ID 64902

- University of Central Oklahoma
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Name : Shelly Hunter Source : Hunger Point (movie, 2003)
Background Information
Shelly Hunter is a Caucasian female currently in high school. Although her age is unknown, she is presumed to be a teenager. A first look at Hunter gives evidential proof that she is seriously underweight. This raises serious concerns about her health. Hunter lives at home with her domineering mother, Marsha, and David, her passive father. She is the younger sister of Frannie, who is away at college and also struggles with eating. Shelly has a very strenuous relationship with her mother. As a child Hunter was always very slender, but she grew up listening to her mother lecture Frannie, who was not as slender, on the importance’s of being slim. Mrs. Hunter’s obsessive belief that being slender is the most important thing has severely distorted Hunter’s views on eating. Hunter clearly seeks approval from her mother and puts great strains on her body to reach that approval. Hunter’s life is devoted to her weight. Her time is spent obsessing about being slender. She does not know how to cope with her eating disorder and her irrational views on being skinny. The eating disorder is also causing severe mental problems with Hunter. She is exhibiting signs of depression and distrust from her family.
Description of the Problem
Hunter displays the symptoms of an eating disorder. She is abnormally underweight for her age and is very unhealthy. She exhibits the characteristics of Bulimia Nervosa. She eats very little when she is in the presence of other people. Most undoubtedly when she is eating in front of her mother, she becomes very self conscious about what and how much she eats. After restraining from food intake for a period of time she then will over eat. She stuffs herself with large portions of food. After doing so she begins to feel shame and guilt for over eating. The way she deals with her guilt is to self- induce vomiting. This purging is a defense mechanism Hunter uses to cope with “disappointing” herself as well as her mother. Although it only lasts for a short while, she feels satisfied with her body after vomiting.
The diagnosis for Hunter appropriately fits Bulimia Nervosa (307.51).
To be diagnosed with Bulimia Nervosa one or more or a combination of the following characteristics must be present:
1. Eating in a discrete period of time (e.g., within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances; it is common for more than 10,000 calories to be consumed per binge. 2. An abnormal constant craving for food; a sense of a lack of control of eating during an episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating). 3. Eating is usually done in secret.
Hunter displays the characteristics of 1 and 3. As described in the “Description of the Problem” she eats large portions of food alone. B. Recurrent inappropriate, compensatory behavior in order to prevent weight gain. Such as self-induced vomiting, misuse of laxatives, diuretics, enemas, or other medications, fasting, or excessive exercise.
Hunter exhibits these compensatory behaviors in order to prevent weight gain. She fasts for a long period of time. She then will binge eat and self-induce vomiting. C. The binge eating and inappropriate compensatory behaviors both occur on average at least twice a week for three months.
Hunter began binge eating at a very young age and continues to binge eat into her high school years. D. Self-evaluation is unduly influenced by body shape and weight. Hunter has a very unhealthy view about her body. She is constantly concerned with gaining weight. Even though she looks too slender and unhealthy to others, she views herself as overweight. E. The disturbance does not occur exclusively during episodes of Anorexia Nervosa.
Hunter will eat very little for a short period of time, and then she will binge eat to self-induce vomiting.
Accuracy of Portrayal
The average person watching this movie would see an accurate portrayal of the behavioral characteristics of Bulimia Nervosa. Hunter displays the onset characteristics of someone suffering from this disorder. Someone watching this movie would learn that having an eating disorder can cause many other problems. Hunter became very untrusting and displayed signs of depression. Bulimia Nervosa took control over Hunter’s life and began to affect her mentally. Therefore, the movie Hunger Point portrays an accurate depiction of Bulimia Nervosa.
After fully examining Hunter it might be best to start her on some medications. To help with depression Tricyclic antidepressants or Selective Serotonin Re-Uptake Inhibitors (SSRI’s) could be prescribed to elevate her mood. Vitamin and mineral supplements would be prescribed until signs of deficiency disappeared and normal eating patterns were reestablished. The vitamins would also help to treat acid reflux caused by bulimia. After Hunter’s weight becomes stabilized it would be a good idea to start a behavioral therapy program. This will help to change the mindset of Hunter and her negative views about her body. This will also help to control her binge eating habits. Not only does Hunter need individual therapy, but she and her mother need family therapy. Mrs. Hunter needs therapy in order to understand that her obsessive beliefs, about being slender, caused her daughter to become diagnosed with bulimia nervosa. Communication exercises will be exhibited to help resolve conflict and re-establishing boundaries. The treatments will better help Hunter to have control over Bulimia Nervosa and to gradually overcome the disorder.

A YouTube element has been excluded from this version of the text. You can view it online here: http://pb.libretexts.org/apsy/?p=174
Name : Blair Waldorf
Source : Gossip Girl (television series, 2007-present)
Blair Waldorf is a 16 year old female who lives in Manhattan, New York. She is a full time student, and attends a private high school. She is in good health, and her family is in good mental health. Her parents are divorced, mother in Manhattan and father in Paris. She has a great relationship with her father, but he left his family for a male model, so Blair suffers slightly with separation anxiety and depression. Her mother has very high status in Manhattan, and would do anything to keep it that way. Blair and her mother get into arguments every now and then, but no more than a normal teen and her mother. Blair is an only child. Serena is Blair’s best friend and has been since they were little. Blair is snobbier of the two, and Serena keeps her grounded without going overboard. They often get into tiffs, but always end up making up. Blair’s ex-boyfriend is Nate. They dated from age 5 until 16. Dealing with the breakup of her longtime lover, Blair goes a little crazy and her separation anxiety and depression shows up again. Blair drinks often, and for some reason in the world that she lives in, adults do not seem to care. She could walk into a bar and drink martinis all night, and it would be completely normal. She does not do drugs, however. Her biggest life difficulty is staying queen bee at her high school. She goes through a lot throughout the show, but staying the most popular girl in school is always her top priority. Her number one goal is to attend Yale after she graduates, and later become a trophy wife just like her mother was. Blair copes with her problems by putting other people down. She loves the fact that she is at the top of the totem pole, and she is not afraid to let anyone and everyone know it. She also often uses alcohol to cope with her problems.
During the first season of Gossip Girl, the fact that Blair had been to treatment in her past comes up a few times. Blair’s eating habits are normal for the first few episodes, but after she experiences different stressors, her eating habits become abnormal again. She starts to pick at food most of the time, but binges at other times. Also, her best friend Serena and her mother started to bring up the fact that her symptoms were returning. She completely closed them off and ignored the fact that they were. Every time that she would get into a fight with Serena, her ex boyfriend, or her mother, her lack of control for eating would return. One incident that was shown on the show was that Blair had gotten into a huge fight with Serena on Thanksgiving, which caused Blair to be extremely snappy with her mother. She found out that her mother lied to her about her father coming into town for the holiday, which caused a fight with her mother as well. She was picking at her Thanksgiving meal during dinner, and when her mother told her to go pick out a dessert, she stormed off to the kitchen. She found an apple pie that she wanted to eat, but instead of just taking one piece, she stared at it for a few minutes, and binged and ate the entire pie. Immediately, she went into her bathroom and started to purposely vomit. She has always had an issue with her self-image, and the binging and purging was her solution to make herself feel better. After vomiting in her bathroom, she called Serena, and she quickly came over and let Blair cry on her shoulder. This is not the only incident that Blair had with binging and purging, but it was a very critical event to Blair’s illness.
The diagnosis for Blair Waldorf fits most appropriately with Bulimia Nervosa (307.51). To be diagnosed with Bulimia Nervosa, you must have the following characteristics:
- Eating in a discrete period of time (e.g., within any 2-hour period), an amount of food that is larger than most people would eat during a similar period of time and under similar circumstances.
- A sense of lack of control of eating during an episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating).
Blair Waldorf displays both of these characteristics. When she has an episode, it is as if she cannot control what food she is putting into her body, or how much food she is putting into her body.
- Recurrent inappropriate compensatory behavior in order to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise.
Blair Waldorf will do whatever she thinks is necessary to prevent weight gain, and her methods of choice are self-induced vomiting and fasting.
- The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for three months.
The television show does not state what age Blair Waldorf started binge eating, but while she was only 16 years old, her mother discussed Blair already having gone to treatment for her Bulimia. So this must have been a problem in her life for quite a few years.
- Self-evaluation is unduly influenced by body shape and weight.
Blair Waldorf is very self conscious of her body image and her weight. Her mother mentions a few times that she needs to watch her weight, so this may have helped lead to Blair’s body image issues.
- The disturbance does not occur exclusively during episodes of anorexia nervosa.
Blair Waldorf will eat a very small amount and continue to pick at food at every meal, until another episode of binging and purging occurs.
The average person watching Gossip Girl and watching Blair with her eating disorder would learn the behavioral characteristics of Bulimia Nervosa. Someone watching this television show would understand that it is a disorder that a person cannot necessarily always control. There can be triggers that can lead to an episode, just like any other illness. This portrayal is accurate of Bulimia Nervosa. However, the show does not show the seriousness as much as it should of this disorder. It was mislabeled in this way because it has affected Blair’s mental health, so any issue in her life that leads to her showing any signs of depression will most likely lead to an episode. This is her way of dealing with problems in her life, and Gossip Girl does not show the severity of this.
After evaluating Blair Waldorf’s condition, it would be best to start her with a behavioral therapy program. She was not taught the proper way to handle her emotions and deal with problems that arise in her life, and therapy would help approach these issues. Therapy could also approach her body image issues, and help her to devise an exercise program that would make her feel more in shape and healthy. Her mother and her friends would have to help monitor her eating habits, but after understanding her condition fully and seeing that there are other ways of dealing with issues, Blair would take on a better eating schedule. Also, putting Blair on a very low dosage antidepressant or Selective Serotonin Re-Uptake Inhibitors (SSRI’s) and monitoring her progress very closely while on this medication would help a great deal. Communication exercises will also be necessary between Blair and her mother to teach them how to discuss this illness in a healthier manner. These different treatments will, in time, help Blair overcome this disorder. She will be able to talk about her feelings and problems, rather than regressing to binging and purging.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Retrospective Correlates for Bulimia Nervosa: A Matched Case-Control Study
Affiliations.
- 1 Psychotherapy and Psychopathology Research Unit - CIPsi, School of Psychology, University of Minho, Braga, Portugal.
- 2 Centre for Studies in Human Development, Faculty of Education and Psychology, Catholic University of Portugal, Porto, Portugal.
- 3 Parnassia Psychiatric Institute, The Hague, the Netherlands.
- 4 Department of Epidemiology, Columbia University, New York, NY, USA.
- 5 Department of Psychiatry, University of Groningen, Groningen, the Netherlands.
- PMID: 26841218
- DOI: 10.1002/erv.2434
Objective: There have been few studies investigating the risk factors for bulimia nervosa (BN), and most have been in Anglo-Saxon countries. This study aimed to (i) replicate the uncontested retrospective correlates for BN and clarify the role of factors with inconsistent findings and (ii) evaluate the strength of these factors in a different culture.
Method: A case-control design was used to compare 60 women who met the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for BN to 60 healthy controls and 60 participants with other psychiatric disorders. Retrospective correlates were assessed by interviewing each person with the Oxford Risk Factor Interview.
Results: The primary retrospective correlates identified from the comparison of BN participants to healthy controls were general high maternal expectations, negative attitudes about parental weight and obesity in childhood and adolescence. Compared with participants with other psychiatric disorders, those with BN also reported higher rates of childhood obesity, deliberate self-harm, family conflicts, general high maternal expectations and feeling fat in childhood.
Conclusions: The common findings across cultures suggest that, at least, individuals subjectively experience a number of similar factors that increase risk for developing BN. In addition, the difference regarding self-harm is notable.
Keywords: bulimia nervosa; risk factors.
Copyright © 2016 John Wiley & Sons, Ltd and Eating Disorders Association.
PubMed Disclaimer
Similar articles
- Anorexia nervosa versus bulimia nervosa: differences based on retrospective correlates in a case-control study. Machado BC, Gonçalves SF, Martins C, Brandão I, Roma-Torres A, Hoek HW, Machado PP. Machado BC, et al. Eat Weight Disord. 2016 Jun;21(2):185-97. doi: 10.1007/s40519-015-0236-6. Epub 2015 Oct 27. Eat Weight Disord. 2016. PMID: 26506924
- Self-harm and suicidal behavior in borderline personality disorder with and without bulimia nervosa. Reas DL, Pedersen G, Karterud S, Rø Ø. Reas DL, et al. J Consult Clin Psychol. 2015 Jun;83(3):643-8. doi: 10.1037/ccp0000014. Epub 2014 Dec 15. J Consult Clin Psychol. 2015. PMID: 25495360
- Adolescent bulimia nervosa. Hoste RR, Labuschagne Z, Le Grange D. Hoste RR, et al. Curr Psychiatry Rep. 2012 Aug;14(4):391-7. doi: 10.1007/s11920-012-0280-0. Curr Psychiatry Rep. 2012. PMID: 22614677 Review.
- [Self-harm and eating disorders]. Skårderud F, Sommerfeldt B. Skårderud F, et al. Tidsskr Nor Laegeforen. 2009 Apr 30;129(9):877-81. doi: 10.4045/tidsskr.08.0509. Tidsskr Nor Laegeforen. 2009. PMID: 19415089 Review. Norwegian.
- Self-injurious behavior and attempted suicide in purging bulimia nervosa: associations with psychiatric comorbidity. Favaro A, Santonastaso P, Monteleone P, Bellodi L, Mauri M, Rotondo A, Erzegovesi S, Maj M. Favaro A, et al. J Affect Disord. 2008 Jan;105(1-3):285-9. doi: 10.1016/j.jad.2007.05.010. Epub 2007 Jun 12. J Affect Disord. 2008. PMID: 17568684
- Bulimia symptoms and anger and aggression among adolescents. Koposov R, Stickley A, Sukhodolsky D, Ruchkin V. Koposov R, et al. BMC Public Health. 2023 May 5;23(1):833. doi: 10.1186/s12889-023-15664-1. BMC Public Health. 2023. PMID: 37147644 Free PMC article.
- Body Image Perception in High School Students: The Relationship with Gender, Weight Status, and Physical Activity. Toselli S, Zaccagni L, Rinaldo N, Mauro M, Grigoletto A, Maietta Latessa P, Marini S. Toselli S, et al. Children (Basel). 2023 Jan 10;10(1):137. doi: 10.3390/children10010137. Children (Basel). 2023. PMID: 36670687 Free PMC article.
- Risk factors for eating disorders: findings from a rapid review. Barakat S, McLean SA, Bryant E, Le A, Marks P; National Eating Disorder Research Consortium; Touyz S, Maguire S. Barakat S, et al. J Eat Disord. 2023 Jan 17;11(1):8. doi: 10.1186/s40337-022-00717-4. J Eat Disord. 2023. PMID: 36650572 Free PMC article. Review.
- Biological, psychological and familial specific correlates in eating disorders at onset: a control-case study protocol (ANOBAS). Sepúlveda AR, Moreno-Encinas A, Nova E, Gómez-Martínez S, Marcos A, Carrobles JA, Graell M. Sepúlveda AR, et al. Actas Esp Psiquiatr. 2022 Mar;50(2):92-105. Epub 2022 Mar 1. Actas Esp Psiquiatr. 2022. PMID: 35312995 Free PMC article.
- Toward a Biological, Psychological and Familial Approach of Eating Disorders at Onset: Case-Control ANOBAS Study. Sepúlveda AR, Moreno-Encinas A, Martínez-Huertas JA, Anastasiadou D, Nova E, Marcos A, Gómez-Martínez S, Villa-Asensi JR, Mollejo E, Graell M. Sepúlveda AR, et al. Front Psychol. 2021 Sep 9;12:714414. doi: 10.3389/fpsyg.2021.714414. eCollection 2021. Front Psychol. 2021. PMID: 34566794 Free PMC article.
- Search in MeSH
Related information
Linkout - more resources, full text sources.
- Ovid Technologies, Inc.
Other Literature Sources
- scite Smart Citations
Miscellaneous
- NCI CPTAC Assay Portal

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Prim Care Companion J Clin Psychiatry
- v.5(5); 2003
Bulimia Nervosa: A Primary Care Review
Bulimia nervosa is a psychiatric condition that affects many adolescent and young adult women. The disorder is characterized by bingeing and purging behavior and can lead to medical complications. Thus, patients with bulimia nervosa commonly present in the primary care setting. Physical and laboratory examinations reveal markers of bulimia nervosa that are useful in making the diagnosis. Treatment is beneficial, and outcomes of early intervention are good. This article discusses the history, presentation, and tools needed for recognizing and treating bulimia nervosa in primary care.
In the United States, eating disorders affect 5 to 10 million people, primarily young women between the ages of 14 and 40 years. 1 Much attention has been paid to the identification and treatment of anorexia nervosa in this age group. 2, 3 However, bulimia nervosa is a more prevalent disorder that is more difficult to identify in the primary care setting. It is imperative that primary care physicians are aware of the presentation and subsequent interventions available to treat patients with bulimia nervosa, considering the relatively silent presentation of the disease. In this article, we provide an overview of bulimia nervosa, associated physical and laboratory examination findings, and diagnostic strategies pertinent to primary care practice.
Bulimia nervosa was described as an ominous variant of anorexia nervosa by Russell in 1979. 4 However, as more research has been conducted and more patients suffering from bulimia nervosa have been identified, bulimia nervosa and anorexia nervosa are now recognized as 2 distinct syndromes. According to the Diagnostic and Statistical Manual for Mental Disorders , Fourth Edition (DSM-IV), bulimia nervosa is characterized by recurrent episodes of binge eating followed by 1 or more compensatory behaviors to eliminate the calories (vomiting, laxatives, fasting, etc.) that take place on average a minimum of twice weekly for 3 or more months. 5 Patients who do not meet the frequency or length criteria may be diagnosed with DSM-IV eating disorder not otherwise specified. 5
Bulimia nervosa is also delineated into 2 distinct subtypes: purging and nonpurging. With the purging subtype, patients engage in some method to remove the binged food from their bodies. This is most often accomplished by self-induced vomiting but can include the misuse of laxatives, enemas, or diuretics. Nonpurging bulimics use fasting or excessive exercise as the primary compensation for binges but do not regularly purge. Regardless of subtype, bulimic patients have negative self-evaluations, placing inappropriate importance on weight and body image.
EPIDEMIOLOGY
Whereas the prevalence of anorexia nervosa for women in the United States is 0.5% to 1%, the prevalence of bulimia nervosa is 2% to 3% and can be as high as 10% in vulnerable populations, such as college-aged women. 6 Males are affected by eating disorders at a rate one tenth of that of females. Demographically, most patients with bulimia nervosa are single, college educated, and in their mid-20s. However, most patients begin experiencing bulimic symptoms during adolescence. 7 Bulimia nervosa occurs in 2.3% of white women but in only 0.40% of black women. 8
Risk factors for bulimia nervosa include, but are not limited to, childhood sexual abuse, male homosexuality, eating alone, living in a sorority house, diabetic poor glycemic control, low self-esteem, dieting, involvement in athletics, and occupations that focus on weight. 9–14 Patients with these risk factors or in high-risk populations and those who the practitioner suspects may have an eating disorder should undergo screening.
SCREENING FOR BULIMIA NERVOSA
Many tools are available for screening in the primary care setting, yet few tools focus on the diagnosis of bulimia nervosa. In the spirit of the CAGE assessment for alcohol abuse, 15 the SCOFF questionnaire screens for eating disorders using 5 simple, easy-to-remember questions. 16 An eating disorder can be suspected with 84.6% sensitivity and 89.6% specificity if a patient responds positively to 2 or more questions. 17 The negative predictive value is 99.3% for the SCOFF questionnaire, which makes this tool useful for screening in clinical practice.
The SCOFF was recently tested against a new instrument, the Eating Disorder Screen for Primary Care. 18 The latter instrument performed slightly better than the SCOFF, with 1 or no abnormal responses ruling out an eating disorder (likelihood ratio [LR] = 0.0) compared with the SCOFF (LR = 0.25). Both were similarly effective in ruling positive for an eating disorder (LR = 11). 18
A 2-item assessment specific to bulimia nervosa may also be an effective screening tool. For responders who answered positively to 1 of the 2 screening questions (Do you ever eat in secret? and Are you satisfied with your eating patterns?), the positive and negative predictive values were 22% and 91% when based upon the gold-standard of a clinical assessment that found a 16% prevalence of bulimia nervosa in the studied population. 19 These 2 screening items had been previously shown to have a sensitivity of 1.00 and specificity of 0.90 for bulimia nervosa. 20
The Bulimic Investigatory Test, Edinburgh (BITE) questionnaire is a brief test for the detection and description of bulimia nervosa. 21 The BITE consists of a set of 33 questions (30 yes/no type and 3 graded-response) that simultaneously assess the presence and relative severity of a binge-eating disorder. The BITE is divided into 2 sections: the symptom scale and the severity scale. The symptom scale consists of the 30 yes/no questions; 1 point is assigned for every “yes” answer, and a score of 20 or greater indicates a binge-eating disorder. The 3 graded-response questions make up the severity scale and ask the patient to score the frequency of their actions. A score of 5 or more on this section is considered clinically significant, and a score of 10 or more is considered severe. The BITE takes an average of 10 minutes to complete and can be immediately scored by the practitioner. Although not intended for screening in primary care, this instrument could be used to track disease severity in patients with known disease.
The Eating Attitudes Test has been widely used in epidemiologic studies, particularly to assess for symptoms of anorexia nervosa. 22–25 The instrument has been validated for bulimia nervosa and modified for use in patients with diabetes mellitus. 26–28 We recommend starting with the Eating Disorder Screen for Primary Care or the SCOFF for screening purposes in primary care.
CLINICAL PRESENTATION
The diagnosis and long-term treatment of bulimia nervosa require the practitioner to have insight into the patient's thoughts regarding weight, food, and eating rituals. The cardinal symptoms of bulimia nervosa include only inappropriate bingeing and compensatory behavior, not low body weight. It is possible for a patient to suffer from bulimia nervosa and be at or above normal weight. For this reason, normal and overweight patients should not be overlooked if other symptoms or signs of bulimia nervosa are present.
It is necessary to understand the patient's eating behaviors, especially those involving binge eating. The bulimic's idea of a binge may not be, and most likely is not, the same as the physician's idea of a binge. Although a binge is loosely defined as a large consumption of calories in a brief period of time, bulimics tend to define binges by the type of food consumed and their mood state while consuming, not necessarily by the actual caloric intake. 29, 30 For instance, snack foods and desserts are viewed as binge foods more often than are other foods. Some bulimics may have an internal list of forbidden foods that, when consumed, will constitute a binge to that patient, regardless of caloric content. A bulimic could consume a large quantity of fruits and vegetables of the same caloric amount as a candy bar but not view it as a binge because fruits and vegetables are “good” or “safe” foods.
In any case, a sense of loss of control over eating is an important feature of bulimia nervosa. Subjective binges are defined not by the amount of food consumed, but by an appraisal that more food was eaten than should have been consumed and a concomitant sense of lack of control. 31, 32 Further, a typical behavioral pattern may be noted around the time of the binge episode. The bulimic may experience pre-episode boredom, cravings, and depression followed by post-episode depression and lack of self-control. 33 Bulimics commonly binge in private, and some may plan binges and purges according to time of day and privacy issues. They may eat normally around friends and family but then binge at other times when alone. In more severe cases, bulimics may alter daily schedules to be assured of time for bingeing and purging. They may also deprive themselves of food for hours before the binge, and it is thought that this deprivation plays into the ritualistic pattern of bulimic eating. 34 Because regular binges may be costly, food may be stolen from grocery and convenience stores. 35 The severity of weight and eating attitudes may fuel the frequency of binge and purge behaviors. It is these behaviors that may lead to serious medical and psychiatric complications.
MEDICAL COMPLICATIONS
Whereas amenorrhea is required for a DSM-IV classification of anorexia nervosa in women, only one half of patients with bulimia nervosa experience menstrual disturbances, including amenorrhea or oligomenorrhea. 36 Menstrual disturbances occurring in women with eating disorders may be secondary to a decrease in the pulsatility of gonadotropin-releasing hormone and possibly to the hormonal mechanisms of leptin, which decreases with decreasing weight. 37, 38 Since a threshold level of weight or body fat is believed to be necessary for normal reproductive functioning, normal or overweight bulimics are less likely to experience amenorrhea. 39
Gastrointestinal (GI) tract abnormalities may occur in bulimics and typically are secondary to purging behaviors. The most commonly reported GI symptoms are bloating, flatulence, and constipation. 40 Gastric emptying and motility may be delayed. 41 The patient also may develop gastroesophageal reflux disease and Mallory-Weiss tears from excessive vomiting. Rectal prolapse has been described, and when it occurs in a young woman, the clinician should include bulimia nervosa in the differential diagnosis. 42
Ipecac, an over-the-counter emetic agent, is often used by bulimics to induce vomiting. Nearly 8% of women with eating disorders may experiment with ipecac, while 1% to 2% regularly abuse the medication. 43 Ipecac has been associated with serious cardiac toxicity, including cardiomyopathy with left ventricular dysfunction. Whether or not this dysfunction is reversible remains controversial. 44 Patients with a history of ipecac abuse may be candidates for echocardiography, especially if symptoms of heart failure are present.
Due to excessive vomiting, patients may exhibit enamel erosion, especially on the lingual surface of the teeth; calluses on middle phalanges from using fingers to induce vomiting (Russell's sign); and sialadenosis, a noninflammatory enlargement of the salivary glands. 45, 46 Parotid gland swelling is commonly found. Sialadenosis is almost always associated with an underlying systemic disorder, including diabetes, alcoholism, malnutrition, anorexia nervosa, and bulimia nervosa. In bulimics, the incidence of sialadenosis ranges from 10% to 66%. The clinician should suspect bulimia nervosa in a young woman with sialadenosis who has no underlying medical conditions. 47, 48 It is thought that the various causes of sialadenosis all result in a common pathogenic effect in that they produce a peripheral autonomic neuropathy responsible for disordered metabolism and secretion, resulting in acinar enlargement. 46, 49 Although the condition may reverse once vomiting ceases, in cases of refractory swelling, parotidectomy may be considered as a last resort to improve facial aesthetics. 46
Unlike patients with anorexia nervosa, bulimic patients generally do not have disturbances in bone mineral density, especially when weight-bearing exercise is used as a compensatory mechanism. 50 Risk factors for decreased bone mineral density include total duration of amenorrhea, age at first menarche, time since last menstrual period, and low body weight. 51 Therefore, early-onset osteopenia is not a major concern for normal or overweight bulimic patients, unless a history of anorexia nervosa with a period of greater than 5 months spent below normal weight is also present.
PSYCHIATRIC COMORBIDITY
The psychiatric comorbidity associated with bulimia nervosa is striking. Bulimic patients are characterized as extroverted perfectionists who are self-critical, impulsive, and emotionally undercontrolled. 52 High prevalence rates of any affective disorder (75%), major depressive disorder (63%), and anxiety disorders (36%) have been reported. 53 The majority of patients report that the initial presentation of the depression or anxiety disorder occurred prior to the presentation of bulimic symptoms. 53 Thus, positive early identification of an affective or anxiety disorder may provide an opportunity to prevent development of eating symptoms and disorders, especially in high-risk populations. Studies describing the incidence of comorbidities in bulimia nervosa may suffer from sampling bias, referral bias, and lack of appropriate control groups.
Substance abuse is an additional common comorbidity. The National Center on Addiction and Substance Abuse at Columbia University reported that 30% to 70% of bulimics have a substance abuse problem. 54 Substances of abuse include tobacco, alcohol, and prescription and over-the-counter medications, such as diet pills and stimulants. Alcoholism has been reported to affect 31% of bulimics and is often found with major depressive disorder and posttraumatic stress disorder. 55 Strong familial relationships have also been observed between bulimia nervosa and alcoholism. 56
A controlled community sample study compared women with bulimia nervosa with normal controls and controls with other psychiatric disorders. Although current alcoholism was similar among the groups, bulimics had higher rates of deliberate self-harm than both control groups and more illicit drug use than the normal controls. 57
Self-injury is a concern for patients with bulimia nervosa. In one study, 34% of bulimic patients reported having injured themselves at sometime in their lives, and 21.3% reported having injured themselves in the last 5 months. 58 Patients most often injure themselves by cutting or scratching their arms, hands, legs, or face, and many of these injuries result in bleeding and scarring. Patients with borderline personality disorder who injure themselves are more likely to also suffer from bulimia nervosa than are those who do not injure themselves. Comorbid diagnoses of bulimia nervosa and borderline personality disorder have been shown to increase risk of frequent self-mutilation, which may influence rates of attempted and completed suicide in these patients. 59
Bulimic patients are more likely to have experienced parental alcoholism, low parental contact, and high parental expectations. 60 Although the core symptoms of this disorder are disturbed eating habits and self-perception, the significant comorbidities complicate the identification and treatment of bulimia nervosa.
LABORATORY ABNORMALITIES
The normal-weight or overweight bulimic may or may not have significant laboratory abnormalities. Laboratory abnormalities become more common with decreasing weight and increasing severity of purging behaviors. The electrolyte levels are most likely to be affected.
Hypokalemia, hypochloremia, hyperphosphatemia, and metabolic alkalosis are common, especially in lower-weight bulimics. The severity of hypokalemia and hypochloremia is directly related to the number of purging episodes the patient experiences, especially those involving diuretics, laxatives, and repetitive vomiting. 61 A recent case-control study 62 suggested that the ratio of urine sodium to urine chloride is the best predictor of bulimic behavior. A ratio of > 1.16 identified nearly 52% of cases, and the false-positive rate was 5%. 62 Additionally, the presence of metabolic alkalosis and elevated phosphorus levels should also raise clinical suspicion for surreptitious vomiting. 63–65 Although serum potassium levels have been considered a good marker for bulimic behavior, the relative infrequency (4.1% to 13.7%) of clinically significant hypokalemia among bulimics lowers its sensitivity as a screening test. 61, 62, 64, 66
Importantly, the patient's overall laboratory picture is dependent on the compensatory mechanisms. Patients who purge by vomiting may present with metabolic alkalosis (elevated serum bicarbonate levels) due to volume contraction. However, patients who primarily abuse laxatives may present with metabolic acidosis (decreased serum bicarbonate levels) due to loss of alkaline fluid from the bowel. 63 Patients using more than one purging mechanism may display mixed acid-base findings. These electrolyte imbalances contribute to weakness, fatigue, and, in severe cases, may predispose the patient to cardiac arrhythmias and sudden death.
Serum amylase determination may help to diagnose and monitor bulimia nervosa. An elevated amylase level may suggest that a patient has been vomiting. In some cases, it will be necessary to rule out an organic cause of elevated amylase levels or vomiting, such as pancreatitis. When fractionated into serum and salivary components, elevations are usually disproportionate, with elevated salivary amylase exceeding pancreatic amylase in patients who have been vomiting. The fractionated test, therefore, may be helpful to use as a diagnostic aid in cases where vomiting is denied and to monitor continued vomiting in patients undergoing treatment. 67
PHYSICAL AND LABORATORY ASSESSMENT
Unlike anorexia nervosa, which is easily discernible given low body weight, the variance in weight presentation among bulimics makes this condition more difficult to diagnose. A baseline assessment for patients suspected of eating disorders includes several elements. Historical information, including prior episodes of electrolyte abnormalities, menstrual irregularities, or GI symptoms such as constipation, provide important clues if these are otherwise unexplained.
Given time constraints in the primary care clinic, the clinician may choose to use either the 2-question assessment discussed previously or the Eating Disorder Screen for Primary Care. 18 Negative scores on these instruments do not rule out the possibility of an eating disorder, as patients who wish to keep the condition secret may not answer the questions in a positive fashion. The physical examination may provide important clues suggesting the presence of bulimia nervosa, particularly the purging subtype of the disorder. On examination, the clinician may look for signs of the medical complications mentioned previously, including dental erosion, scarring or abrasion on the knuckles, and swollen parotid glands.
Primary care providers should consider the use of laboratory tests in both the diagnostic and follow-up evaluation. For underweight patients, patients in whom bulimia nervosa is suspected but denied, and patients in whom physical symptoms and signs are present, laboratory tests may be useful to rule out other disorders or to positively diagnose bulimia nervosa. Although no standard panel of tests is described, serum and urine electrolyte counts, acid-base assessments, and phosphorus levels should be obtained from the underweight patient at both diagnosis and follow-up. Fractionated amylase testing may be beneficial in evaluating for vomiting in patients suspected of having bulimia nervosa and in patients undergoing treatment for the disorder. Electrocardiogram monitoring should be performed in bulimic patients with electrolyte abnormalities, palpitations, chest pain, or low body weight. The bulimic patient with at least a 5-month history of low body weight or anorexia should have a bone density assessment. Other testing, such as upper or lower GI endoscopy, should be considered, depending on the constellation of symptoms and signs. For instance, other conditions that can manifest with GI symptoms include inflammatory bowel diseases, celiac sprue, and irritable bowel syndrome.
Most patients with bulimia nervosa do not require hospitalization, and the preferred method of treatment is outpatient-based. 68 Cognitive-behavioral therapy (CBT) is the standard and preferred psychological method of treatment for these patients. In multiple studies, CBT has been demonstrated superior to other forms of psychological treatment, such as interpersonal psychotherapy. 59, 69 This method of treatment for bulimia nervosa was first described by Fairburn in 1981 and has 2 goals: (1) to stop the vicious circle of overeating and vomiting and (2) to modify the abnormal attitudes toward food. 70 The CBT method has 3 phases that overlap in a 20-week course of therapy. 71 During the first phase, patients are taught about bulimia nervosa and actions that perpetuate the disease. The patient keeps detailed food records, including the frequency of bingeing or purging, which are used in therapy sessions. The second phase consists of teaching the patient to broaden food choices, and additional time is spent on correcting dysfunctional food and body thoughts. The final 3 therapy sessions comprise the third stage and focus on maintenance and relapse prevention. Upon completion of CBT, 45% of patients stopped bingeing and purging and 35% no longer met diagnostic criteria for bulimia nervosa. 71
Relapse primarily occurs during the first 4 months after CBT and affects 31% to 44% of patients. 72 Relapse has been attributed to low motivation during treatment and overly ritualized eating and high frequency of vomiting before treatment. 72, 73 Rapid and sustained response to CBT has been found to be dependent upon frequency of bingeing before treatment and a self-directed personality. 74
Pharmacologic treatment may be a primary or adjunct therapy for bulimia nervosa. Fluoxetine has been shown to be effective in the treatment of bulimia nervosa. One 16-week and 2 double-blind 8-week clinical trials conducted in the early to mid-1990s all found fluoxetine, 60 mg/day, to significantly decrease overall binge eating and vomiting. 41–43, 75–77 Fluoxetine also has been reported to significantly decrease vomiting and binge eating in as little as 4 weeks of therapy. 78 Bulimic patients followed for up to 1 year on fluoxetine therapy were found to have a significantly decreased likelihood of relapse and improved overall outcome when compared with placebo. 79 A case series of 5 underweight patients with binge-eating and purging reported sertraline to be effective in weight restoration and reduction of core eating disorder behaviors. 80 Although citalopram 81 was effective in treating binge-eating disorder, no differences were noted between cases and controls for fluvoxamine. 82 Milnacipran, an antidepressant with both serotonergic and noradrenergic function, was effective for the reduction of bulimic symptoms in an uncontrolled case series. 83 To date, fluoxetine remains the only medication approved by the U.S. Food and Drug Administration for the treatment of bulimia nervosa.
The combination of CBT with fluoxetine therapy has been shown to be superior to medication or CBT alone. 84 Frequency and severity of vomiting and binge eating were decreased in patients on both therapies. Also, in a recent study, patients reported better social adjustment up to 10 years after receiving CBT, fluoxetine, or both therapies for treatment of bulimia nervosa compared with that of women who had been randomized to placebo. 85 For bulimic patients who do not respond to CBT, fluoxetine has been shown to be effective in decreasing bulimic features. 86 In light of this research, the current treatment for bulimia nervosa consists of outpatient-based CBT and fluoxetine therapy.
Generally, treatment of physical symptoms is dependent upon severity of the problem (e.g., hypokalemia) and whether or not reversal is expected at cessation of purging behaviors (e.g., dysphagia).
Primary care physicians should consider referring patients for specialty care in situations where eating disorder symptoms are persistent, comorbid psychopathology is present, or self-injurious behaviors or suicidal ideation is encountered. Specialty clinics directed at the care of patients with eating disorders may be most beneficial. 87, 88
Primary care physicians, patients, and families may benefit from reading about eating disorders or researching community or college campus resources. The American Psychiatric Association issued practice guidelines for the assessment and treatment of anorexia nervosa and bulimia nervosa. These guidelines include an overview of the clinical characteristics and evidence-based treatments. 1 Online resources are plentiful, but among the most comprehensive Web sites are http://www.mentalhealth.com and http://www.besttreatments.org/bulimianervosa . 89, 90 The former provides links to the American Psychiatric Association and National Institute of Mental Health guidelines, as well as recent articles and research advances. The latter source was produced in affiliation with the Clinical Evidence Program of the British Medical Journal . This site is designed for the lay public and provides descriptions of the clinical features of and treatment options for bulimia nervosa.
Although bulimia nervosa is more common than anorexia nervosa, the mortality rate is lower and the recovery rate higher than that of anorexia nervosa. 91 Mortality from bulimia nervosa is approximated at 0% to 3% but may be underestimated due to few long-term follow-up studies involving bulimic patients. Approximately 50% of patients are free from all bulimic symptoms 5 years after treatment. 91 Although outcomes research on bulimia nervosa is sparse, with limited statistical estimates, it has been shown that mortality and recovery are directly related to early intervention and treatment. 88
Patients who suffer from anorexia nervosa and exhibit bulimic features have more difficulty reaching normal body weight and tend to be at lower body weights, even after treatment. 92 Anorexics are also prone to developing binge eating after treatment for anorexia nervosa. A 1997 study reported that 30% of treated anorexics developed binge-eating behavior up to 5 years posthospitalization. 87 When assessing a normal or overweight patient with bulimia nervosa, it is important to gather historical information about the presence and duration of past anorexia nervosa. Anorexia nervosa complicated by bulimic symptoms is associated with higher mortality rates than those from bulimia nervosa alone. 93 However, mortality rates and comorbidity rates for all eating disorders may be overestimated due to the fact that most studies take place in academic or specialty research settings. These patients are often more severely ill than patients in outpatient, community-based settings. The actual recovery rates for eating disorders are probably greater, and the overall outcome picture not so bleak. 94 Yet, it is important for primary care physicians to be familiar with the presenting symptoms of bulimia nervosa or anorexia nervosa complicated by bulimia and to intervene early in the disease course. Unfortunately, in a study conducted nearly 10 years ago, approximately 1 in 10 patients with bulimia nervosa were in treatment. 95
CONCLUSIONS
Bulimia nervosa is a common and treatable condition that often presents in the primary care setting. The hallmark sign for bulimia nervosa is a distorted view of food and eating. Patients with this condition often maintain a normal or above-normal weight. Purging can present outwardly via sialadenosis, dental enamel erosion, and calloused middle phalanges. Patients with bulimia nervosa may have electrolyte and acid-base abnormalities. Bulimia nervosa is also often associated with depression, borderline personality disorder, substance abuse, self-injury, and a troubled family life.
Bulimia nervosa is a treatable disease, especially when diagnosed early. The majority of patients are successfully treated with fluoxetine and CBT. However, better outcomes are associated with prevention and early detection of abnormal eating patterns. It is important that primary care physicians consider this disease in patients with eating or weight symptoms, especially in the most at-risk population: single, white, educated, college-aged women. Early treatment and specialty referral for these patients is indicated.
Drug names: citalopram (Celexa), fluoxetine (Prozac and others), sertraline (Zoloft).
Pretest and Objectives

Instructions and Posttest

Registration and Evaluation

This work was supported by the University of Iowa Roy J. and Lucille A. Carver College of Medicine Summer Research Fellowship (Ms. Rushing) and grant K08 MH01932-01A1 from the National Institute of Mental Health, Bethesda, Md. (Dr. Carney).
In the spirit of full disclosure and in compliance with all ACCME Essential Areas and Policies, the faculty for this CME activity were asked to complete a full disclosure statement. The information received is as follows: Mss. Jones and Rushing and Dr. Carney have no significant commercial relationships to disclose relative to this article.
- American Psychiatric Association. Practice Guideline for the Treatment of Patients With Eating Disorders [Revision] . Am J Psychiatry . 2000 157 suppl 1. 1–39. [ PubMed ] [ Google Scholar ]
- Mehler PS. Diagnosis and care of patients with anorexia nervosa in primary care settings. Ann Intern Med. 2001; 134 :1048–1059. [ PubMed ] [ Google Scholar ]
- Becker AE, Grinspoon SK, and Klibanski A. et al. Eating disorders . N Engl J Med . 1999 340 :1092–1098. [ PubMed ] [ Google Scholar ]
- Russell G. Bulimia nervosa: an ominous variant of anorexia nervosa. Psychol Med. 1979; 9 :429–448. [ PubMed ] [ Google Scholar ]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition . Washington, DC: American Psychiatric Association. 1994 [ Google Scholar ]
- Hsu LK. Epidemiology of the eating disorders. Psychiatr Clin North Am. 1996; 19 :681–700. [ PubMed ] [ Google Scholar ]
- Lee NF, Rush AJ, Mitchell JE. Bulimia and depression. J Affect Disord. 1985; 9 :231–238. [ PubMed ] [ Google Scholar ]
- Striegel-Moore RH, Dohm FA, and Kraemer HC. et al. Eating disorders in white and black women . Am J Psychiatry . 2003 160 :1326–1331. [ PubMed ] [ Google Scholar ]
- Carlat DJ, Camargo CA Jr, Herzog DB. Eating disorders in males: a report on 135 patients. Am J Psychiatry. 1997; 154 :1127–1132. [ PubMed ] [ Google Scholar ]
- Russell CJ, Keel PK. Homosexuality as a specific risk factor for eating disorders in men. Int J Eat Disord. 2002; 31 :300–306. [ PubMed ] [ Google Scholar ]
- Schulken ED, Pinciaro PJ, and Sawyer RG. et al. Sorority women's body size perceptions and their weight-related attitudes and behaviors . J Am Coll Health . 1997 46 :69–74. [ PubMed ] [ Google Scholar ]
- Steiner H, Kwan W, and Shaffer TG. et al. Risk and protective factors for juvenile eating disorders . Eur Child Adolesc Psychiatry . 2003 12 suppl 1. 38–46. [ PubMed ] [ Google Scholar ]
- Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: a 2-year prospective investigation. Health Psychol. 2002; 21 :131–138. [ PubMed ] [ Google Scholar ]
- Rodin GM, Johnson LE, and Garfinkel PE. et al. Eating disorders in female adolescents with insulin dependent diabetes mellitus . Int Psychiatry Med . 1986 16 :49–57. [ PubMed ] [ Google Scholar ]
- Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984; 252 :1905–1907. [ PubMed ] [ Google Scholar ]
- Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999; 319 :1467–1468. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Luck AJ, Morgan JF, and Reid F. et al. The SCOFF questionnaire and clinical interview for eating disorders in general practice: comparative study . BMJ . 2002 325 :755–756. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cotton MA, Ball C, Robinson P. Four simple questions can help screen for eating disorders. J Gen Intern Med. 2003; 18 :53–56. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Freund KM, Boss RD, and Handleman EK. et al. Secret patterns: validation of a screening tool to detect bulimia . J Womens Health Gend Based Med . 1999 8 :1281–1284. [ PubMed ] [ Google Scholar ]
- Freund KM, Graham SM, and Lesky LG. et al. Detection of bulimia in a primary care setting . J Gen Intern Med . 1993 8 :236–242. [ PubMed ] [ Google Scholar ]
- Henderson M, Freeman CP. A self-rating scale for bulimia: the “BITE.” Br J Psychiatry. 1987; 150 :18–24. [ PubMed ] [ Google Scholar ]
- Mann AH, Wakeling A, and Wood K. et al. Screening for abnormal eating attitudes and psychiatric morbidity in an unselected population of 15-year-old schoolgirls . Psychol Med . 1983 13 :573–580. [ PubMed ] [ Google Scholar ]
- Garner DM, Olmsted MP, and Bohr Y. et al. The eating attitudes test: psychometric features and clinical correlates . Psychol Med . 1982 12 :871–878. [ PubMed ] [ Google Scholar ]
- Garner DM, Garfinkel PE. Socio-cultural factors in the development of anorexia nervosa. Psychol Med. 1980; 10 :647–656. [ PubMed ] [ Google Scholar ]
- Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979; 9 :273–279. [ PubMed ] [ Google Scholar ]
- Gross J, Rosen JC, and Leitenberg H. et al. Validity of the eating attitudes test and the eating disorders inventory in bulimia nervosa . J Consult Clin Psychol . 1986 54 :875–876. [ PubMed ] [ Google Scholar ]
- Cantwell R, Steel JM. Screening for eating disorders in diabetes mellitus. J Psychosom Res. 1996; 40 :15–20. [ PubMed ] [ Google Scholar ]
- Robertson P, Rosenvinge JH. Insulin-dependent diabetes mellitus: a risk factor in anorexia nervosa or bulimia nervosa? an empirical study of 116 women. J Psychosom Res. 1990; 34 :535–541. [ PubMed ] [ Google Scholar ]
- Rosen JC, Leitenberg H, and Fisher C. et al. Binge-eating episodes in bulimia nervosa: the amount and type of food consumed . Int J Eat Disord . 1986 5 :255–267. [ Google Scholar ]
- Gleaves DH, Williamson DA, Barker SE. Additive effects of mood and eating forbidden foods upon the perceptions of overeating and binging in bulimia nervosa. Addict Behav. 1993; 18 :299–309. [ PubMed ] [ Google Scholar ]
- Fairburn CG, Cooper Z, and Cooper PJ. The clinical features and maintenance of bulimia nervosa . In: Brownell KD, Foreyt JP, eds. Handbook of Eating Disorders: Physiology, Psychology and Treatment of Obesity, Anorexia and Bulimia. New York, NY: Basic Books. 1986 389–404. [ Google Scholar ]
- Kerzhnerman I, Lowe MR. Correlates of subjective and objective binge eating in binge-purge syndromes. Int J Eat Disord. 2002; 31 :220–228. [ PubMed ] [ Google Scholar ]
- Jansen A, van den Hout M, Griez E. Clinical and non-clinical binges. Behav Res Ther. 1990; 28 :439–444. [ PubMed ] [ Google Scholar ]
- Hetherington MM, Altemus M, and Nelson ML. et al. Eating behavior in bulimia nervosa: multiple meal analyses . Am J Clin Nutr . 1994 60 :864–873. [ PubMed ] [ Google Scholar ]
- Mitchell JE, Gibeau L, and Pyle RL. et al. Shoplifting in bulimia nervosa . Compr Psychiatry . 1992 33 :342–345. [ PubMed ] [ Google Scholar ]
- Seidenfeld ME, Rickert VI. Impact of anorexia, bulimia and obesity on the gynecologic health of adolescents. Am Fam Physician. 2001; 64 :445–450. [ PubMed ] [ Google Scholar ]
- Pirke KM, Dogs M, and Fichter MM. et al. Gonadotrophins, oestradiol and progesterone during the menstrual cycle in bulimia nervosa . Clin Endocrinol . 1988 29 :265–270. [ PubMed ] [ Google Scholar ]
- Grinspoon S, Gulick T, and Askari H. et al. Serum leptin levels in women with anorexia nervosa . J Clin Endocrinol Metab . 1996 81 :3861–3863. [ PubMed ] [ Google Scholar ]
- Frisch RE, Revelle R, Cook S. Components of weight at menarche and the initiation of the adolescent growth spurt in girls: estimated total water, lean body weight and fat. Hum Biol. 1973; 45 :469–483. [ PubMed ] [ Google Scholar ]
- Chami TN, Andersen AE, and Crowell MD. et al. Gastrointestinal symptoms in bulimia nervosa: effects of treatment . Am J Gastroenterol . 1995 90 :88–92. [ PubMed ] [ Google Scholar ]
- Kamal N, Chami T, and Andersen A. et al. Delayed gastrointestinal transit times in anorexia nervosa and bulimia nervosa . Gastroenterology . 1991 101 :1320–1324. [ PubMed ] [ Google Scholar ]
- Malik M, Stratton J, Sweeney WB. Rectal prolapse associated with bulimia nervosa: report of seven cases. Dis Colon Rectum. 1997; 40 :1382–1385. [ PubMed ] [ Google Scholar ]
- Greenfeld D, Mickley D, and Quinlan DM. et al. Ipecac abuse in a sample of eating disordered outpatients . Int J Eat Disord . 1993 13 :411–414. [ PubMed ] [ Google Scholar ]
- Ho PC, Dweik R, Cohen MC. Rapidly reversible cardiomyopathy associated with chronic ipecac ingestion. Clin Cardiol. 1998; 21 :780–783. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simmons MS, Grayden SK, Mitchell JE. The need for psychiatric-dental liaison in the treatment of bulimia. Am J Psychiatry. 1986; 143 :783–784. [ PubMed ] [ Google Scholar ]
- Coleman H, Altini M, and Nayler S. et al. Sialadenosis: a presenting sign in bulimia . Head Neck . 1998 20 :758–762. [ PubMed ] [ Google Scholar ]
- Vavrina J, Muller W, Gebbers JO. Enlargement of salivary glands in bulimia. J Laryngol Otol. 1994; 108 :516–518. [ PubMed ] [ Google Scholar ]
- Kinzl J, Biebl W, Herold M. Significance of vomiting for hyperamylasemia and sialadenosis in patients with eating disorders. Int J Eat Disord. 1993; 13 :117–124. [ PubMed ] [ Google Scholar ]
- Riad M, Barton JR, and Wilson JA. et al. Parotid salivary secretory pattern in bulimia nervosa . Acta Otolaryngol . 1991 111 :392–395. [ PubMed ] [ Google Scholar ]
- Sundgot-Borgen J, Bahr R, and Falch JA. et al. Normal bone mass in bulimic women . J Clin Endocrinol Metab . 1998 83 :3144–3149. [ PubMed ] [ Google Scholar ]
- Grinspoon S, Thomas E, and Pitts S. et al. Prevalence and predictive factors for regional osteopenia in women with anorexia nervosa . Ann Intern Med . 2000 133 :790–794. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Westen D, Harnden-Fischer J. Personality profiles in eating disorders: rethinking the distinction between axis I and axis II. Am J Psychiatry. 2001; 158 :547–562. [ PubMed ] [ Google Scholar ]
- Brewerton TD, Lydiard RB, and Herzog DB. et al. Comorbidity of axis I psychiatric disorders in bulimia nervosa . J Clin Psychiatry . 1995 56 :77–80. [ PubMed ] [ Google Scholar ]
- Vastag B. What's the connection? no easy answers for people with eating disorders and drug abuse. JAMA. 2001; 285 :1006–1007. [ PubMed ] [ Google Scholar ]
- Dansky BS, Brewerton TD, Kilpatrick DG. Comorbidity of bulimia nervosa and alcohol use disorders: results from the National Women's Study. Int J Eat Disord. 2000; 27 :180–190. [ PubMed ] [ Google Scholar ]
- Kaye WH, Lilenfeld LR, and Plotnicov K. et al. Bulimia nervosa and substance dependence: association and family transmission . Alcohol Clin Exp Res . 1996 20 :878–881. [ PubMed ] [ Google Scholar ]
- Welch SL, Fairburn CG. Impulsivity or comorbidity in bulimia nervosa: a controlled study of deliberate self-harm and alcohol and drug misuse in a community sample. Br J Psychiatry. 1996; 169 :451–458. [ PubMed ] [ Google Scholar ]
- Paul T, Schroeter K, and Dahme B. et al. Self-injurious behavior in women with eating disorders . Am J Psychiatry . 2002 159 :408–411. [ PubMed ] [ Google Scholar ]
- Dulit RA, Fyer MR, and Leon AC. et al. Clinical correlates of self-mutilation in borderline personality disorder . Am J Psychiatry . 1994 151 :1305–1311. [ PubMed ] [ Google Scholar ]
- Fairburn CG, Welch SL, and Doll HA. et al. Risk factors for bulimia nervosa: a community-based case-control study . Arch Gen Psychiatry . 1997 54 :509–517. [ PubMed ] [ Google Scholar ]
- Wolfe BE, Metzger ED, and Levine JM. et al. Laboratory screening for electrolyte abnormalities and anemia in bulimia nervosa: a controlled study . Int J Eat Disord . 2001 30 :288–293. [ PubMed ] [ Google Scholar ]
- Crow SJ, Rosenberg ME, and Mitchell JE. et al. Urine electrolytes as markers of bulimia nervosa . Int J Eat Disord . 2001 30 :279–287. [ PubMed ] [ Google Scholar ]
- Mitchell JE, Hatsukami D, Pyle RL. Metabolic acidosis as a marker for laxative abuse in patients with bulimia. Int J Eat Disord. 1987; 6 :557–560. [ Google Scholar ]
- Mitchell JE, Pyle RL, and Eckert ED. et al. Electrolyte and other physiological abnormalities in patients with bulimia . Psychol Med . 1983 13 :273–278. [ PubMed ] [ Google Scholar ]
- Bonne OB, Gur E, Berry EM. Hyperphosphatemia: an objective marker for bulimia nervosa? Compr Psychiatry. 1995; 36 :236–240. [ PubMed ] [ Google Scholar ]
- Greenfeld D, Mickley D, and Quinlan DM. et al. Hypokalemia in outpatients with eating disorders . Am J Psychiatry . 1995 152 :60–63. [ PubMed ] [ Google Scholar ]
- Robertson C, Millar H. Hyperamylasemia in bulimia nervosa and hyperemesis gravidarum. Int J Eat Disord. 1999; 26 :223–227. [ PubMed ] [ Google Scholar ]
- Powers PS. Initial assessment and early treatment options for anorexia nervosa and bulimia nervosa. Psychiatr Clin North Am. 1996; 19 :639–655. [ PubMed ] [ Google Scholar ]
- Fairburn CG, Jones R, and Peveler RC. et al. Three psychological treatments for bulimia nervosa: a comparative trial . Arch Gen Psychiatry . 1991 48 :463–469. [ PubMed ] [ Google Scholar ]
- Fairburn C. A cognitive behavioural approach to the treatment of bulimia. Psychol Med. 1981; 11 :707–711. [ PubMed ] [ Google Scholar ]
- Agras WS, Walsh T, and Fairburn CT. et al. A multicenter comparison of cognitive-behavioral therapy and interpersonal psychotherapy for bulimia nervosa . Arch Gen Psychiatry . 2000 57 :459–466. [ PubMed ] [ Google Scholar ]
- Halmi KA, Agras WS, and Mitchell J. et al. Relapse predictors of patients with bulimia nervosa who achieved abstinence through cognitive behavioral therapy . Arch Gen Psychiatry . 2002 59 :1105–1109. [ PubMed ] [ Google Scholar ]
- Olmsted MP, Kaplan AS, Rockert W. Rate and prediction of relapse in bulimia nervosa. Am J Psychiatry. 1994; 151 :738–743. [ PubMed ] [ Google Scholar ]
- Bulik CM, Sullivan PF, and Carter FA. et al. Predictors of rapid and sustained response to cognitive-behavioral therapy for bulimia nervosa . Int J Eat Disord . 1999 26 :137–144. [ PubMed ] [ Google Scholar ]
- Fichter MM, Leibl K, and Rief W. et al. Fluoxetine versus placebo: a double-blind study with bulimic inpatients undergoing intensive psychotherapy . Pharmacopsychiatry . 1991 24 :1–7. [ PubMed ] [ Google Scholar ]
- Goldstein DJ, Wilson MG, and Thompson VI. et al. Fluoxetine Bulimia Nervosa Research Group. Long-term fluoxetine treatment of bulimia nervosa . Br J Psychiatry . 1995 166 :660–666. [ PubMed ] [ Google Scholar ]
- Fluoxetine Bulimia Nervosa Collaborative Study Group. Fluoxetine in the treatment of bulimia nervosa: a multicenter, placebo-controlled, double-blind trial. Arch Gen Psychiatry. 1992; 49 :139–147. [ PubMed ] [ Google Scholar ]
- Mitchell JE, Fletcher I, and Hanson K. et al. The relative efficacy of fluoxetine and manual-based self-help in the treatment of outpatients with bulimia nervosa . J Clin Psychopharmacol . 2001 21 :298–304. [ PubMed ] [ Google Scholar ]
- Romano SJ, Halmi KA, and Sarkar NP. et al. A placebo-controlled study of fluoxetine in continued treatment of bulimia nervosa after successful acute fluoxetine treatment . Am J Psychiatry . 2002 159 :96–102. [ PubMed ] [ Google Scholar ]
- Frank GK, Kaye WH, Marcus MD. Sertraline in underweight binge eating/purging-type eating disorders: five case reports. Int J Eat Disord. 2001; 29 :495–498. [ PubMed ] [ Google Scholar ]
- McElroy SL, Hudson JI, and Malhotra S. et al. Citalopram in the treatment of binge-eating disorder: a placebo-controlled trial . J Clin Psychiatry . 2003 64 :807–813. [ PubMed ] [ Google Scholar ]
- Pearlstein T, Spurell E, and Holstein LA. et al. A double-blind, placebo-controlled trial of fluvoxamine in binge eating disorder: a high placebo response . Arch Women Ment Health . 2003 6 :147–151. [ PubMed ] [ Google Scholar ]
- El-Giamal N, de Zwaan M, and Bailer U. et al. Milnacipran in the treatment of bulimia nervosa: a report of 16 cases . Eur Neuropsychopharmacol . 2003 13 :73–79. [ PubMed ] [ Google Scholar ]
- Walsh BT, Wilson GT, and Loeb KI. et al. Medication and psychotherapy in the treatment of bulimia nervosa . Am J Psychiatry . 1997 154 :523–531. [ PubMed ] [ Google Scholar ]
- Keel PK, Mitchell JE, and Davis TL. et al. Long-term impact of treatment in women diagnosed with bulimia nervosa . Int J Eat Disord . 2002 31 :151–158. [ PubMed ] [ Google Scholar ]
- Walsh BT, Agras WS, and Devlin MJ. et al. Fluoxetine for bulimia nervosa following poor response to psychotherapy . Am J Psychiatry . 2000 157 :1332–1334. [ PubMed ] [ Google Scholar ]
- Strober MR, Freeman R, Morrell W. The long-term course of severe anorexia nervosa in adolescents: survival analysis of recovery, relapse, and outcome predictors over 10–15 years in a prospective study. Int J Eat Disord. 1997; 22 :339–360. [ PubMed ] [ Google Scholar ]
- Herzog DB, Nussbaum KM, Marmor AK. Comorbidity and outcome in eating disorders. Psychiatr Clin North Am. 1996; 19 :843–859. [ PubMed ] [ Google Scholar ]
- Best Treatments Clinical Advance for Patients and Doctors. Available at: http://www.besttreatments.org/bulimianervosa Accessed Nov 3, 2003. [ Google Scholar ]
- Internet Mental Health. Available at: http://www.mentalhealth.com . Accessed Nov 3, 2003. [ Google Scholar ]
- Keel PK, Mitchell JE. Outcome in bulimia nervosa. Am J Psychiatry. 1997; 154 :313–321. [ PubMed ] [ Google Scholar ]
- Vaz FJ, Guisado JA, Penas-Lledo EM. History of anorexia nervosa in bulimic patients: its influence on body composition. Int J Eat Disord. 2003; 34 :148–155. [ PubMed ] [ Google Scholar ]
- Herzog DB, Greenwood DN, and Dorer DJ. et al. Mortality in eating disorders: a descriptive study . Int J Eat Disord . 2000 28 :20–26. [ PubMed ] [ Google Scholar ]
- Johnson CL, Lund BC, and Yates WR. Recovery rates for anorexia nervosa [letter] . Am J Psychiatry . 2003 160 :798. author reply 798. [ PubMed ] [ Google Scholar ]
- Welch SL, Fairburn CG. Sexual abuse and bulimia nervosa: three integrated case control comparisons. Am J Psychiatry. 1994; 151 :402–407. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Sage is a 26-year-old doctoral candidate who binges and purges to cope with stress and body image issues. Learn about her symptoms, diagnosis, and treatment options from this case study by the Society of Clinical Psychology.
Case Presentation: A 21-year-old woman presented with extreme and enduring bulimia nervosa. She reported recurrent binge-eating and purging by self-induced vomiting 40 episodes per day, which proved refractory to both pharmacological and behavioral treatment at the outpatient, residential, and inpatient level.
Bulimia nervosa is a condition that occurs most commonly in adolescent females, characterized by indulgence in binge-eating, and inappropriate compensatory behaviors to prevent weight gain.[1] The Diagnostic and Statistical Manual of Mental Disorders- 5th edition (DSM-V) defines the following diagnostic criteria for bulimia nervosa:
Bulimia nervosa was unlikely, given that the patient did not have a history of binge eating or purging. ... On the basis of previous case studies that suggested a benefit from gradual exposure to ...
Bulimia nervosa (BN) is a serious psychiatric illness that typically develops during adolescence or young adulthood, rendering adolescents a target for early intervention. Despite the increasing research devoted to the treatment of youth with anorexia nervosa (AN) and adults with BN, there remains a dearth of evidence for treating younger ...
Objective: The present review addresses the outcome of bulimia nervosa, effect variables, and prognostic factors. Method: A total of 79 study series covering 5,653 patients suffering from bulimia nervosa were analyzed with regard to recovery, improvement, chronicity, crossover to another eating disorder, mortality, and comorbid psychiatric disorders at outcome. Forty-nine studies dealt with ...
A classic case of the bulimia nervosa in a young Indian female is reported. This is in the context of the impression that due to increasing western influence, and change in cultural concepts of beauty and thinness among women, illnesses previously considered rare in Indian subcontinent might be becoming more prevalent. ... Study on Indian ...
Six Years Struggling with Bulimia Nervosa: A Case Study. January 2022. DOI: 10.2991/assehr.k.220404.258. Conference: 3rd Tarumanagara International Conference on the Applications of Social ...
Enhanced Cognitive Behavioral Therapy (CBT-E) is an evidence-based treatment for bulimia nervosa (BN), which can be delivered individually or in a group format. ... Using Cognitive-Behavioral Therapy to Treat Adolescent-Onset Bulimia Nervosa: A Case Study. Show details Hide details. Ann M. Schapman-Williams and more ... Clinical Case Studies ...
To further investigate the effectiveness of integrative dynamic therapy (IDT) for bulimia nervosa (BN), our research group undertook a randomized, controlled pilot study comparing IDT with CBT for BN. The case described here was selected from a sample of N = 38 female patients with the symptoms of BN who enrolled in the study.
Susan's progress throughout treatment is detailed in this case study report. Results lend support to a scant body of case series studies attesting to the efficacy of CBT for use with adolescents with BN. Large-scale, randomized studies are needed to corroborate preliminary conclusions that have been promulgated in this case study.
Morgan CD, Marsh C. Bulimia nervosa in an elderly male: a case report. Int J Eat Disord. 2006 Mar. 39(2):170-1. ... Fluoxetine in the treatment of bulimia nervosa. A multicenter, placebo-controlled, double-blind trial. Fluoxetine Bulimia Nervosa Collaborative Study Group. Arch Gen Psychiatry. 1992 Feb. 49 (2):139-47.
The case of eating disorders is a case that is not easy to solve. This case study once explored the experience of a young woman in Indonesia who experienced the eating disorder bulimia nervosa. Through this study, the researcher wants to show the dynamics of the patient's efforts to recover from the bulimia nervosa
Case Study of Bulimia Nervosa (BN) Bulimia Nervosa is an eating disorder characterized by binge eating followed by purging. Binge eating refers to eating a large amount of food in a short amount of time. Purging refers to the attempts to get rid of the food consumed. Bulimia means to 'eat like an ox', although people have been known to ...
This approaches bulimia nervosa as a specific case of the pathology of the self. The treated person cannot rely on people to fulfil their needs such as self‐esteem. ... No statistical heterogeneity was indicated. When bulimia nervosa studies only were considered the difference was significant (n=7 trials, 484 participants, RR 0.83 95% CI 0.71 ...
This case study illustrates this gap in integrated eating disorder and obesity treatment research and describes the successful treatment of a woman with a longstanding history of bulimia nervosa (BN) and excess weight who was required to lose weight to qualify for a knee surgery. ... Phase 2 (Sessions 3-15): Bulimia Nervosa Treatment Using ...
Transition in beauty ideals indicts prevalence of eating disorders in India (Khandelwal et al 1995).There is an apparent paucity of case studies in Indian literature; the available descriptive studies on Eating disorders propose that Bulimia Nervosa is rare with most cases having an atypical presentation of the disorder (Khandelwal et al 1995; Bhugra et al. 2000).
Bulimia nervosa is a crippling and chronic disorder, with individuals experiencing repeated binge-purge episodes. ... Management of Bulimia Nervosa: A Case Study with the Roy Adaptation Model. ... Case Conceptualization and Effective Interventions. 2016. View more. View full text | Download PDF. Open in viewer. Go to. Go to. Show all references.
Abstract. Bulimia nervosa is a crippling and chronic disorder, with individuals experiencing repeated binge-purge episodes. It is not widely understood by society. The use of the Roy adaptation model for the management of bulimia nervosa is examined in this article. Nursing models are utilized to provide a structure for planning and ...
2. An abnormal constant craving for food; a sense of a lack of control of eating during an episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating). 3. Eating is usually done in secret. Hunter displays the characteristics of 1 and 3.
An Indian study described a similar case of bulimia without weight concern, and where vomiting was intended to control and reduce heaviness in the chest or discomfort in the abdomen. The cultural variability of body preoccupations in clinical practice has been well established for anorexia.
Objective: There have been few studies investigating the risk factors for bulimia nervosa (BN), and most have been in Anglo-Saxon countries. This study aimed to (i) replicate the uncontested retrospective correlates for BN and clarify the role of factors with inconsistent findings and (ii) evaluate the strength of these factors in a different culture.
EPIDEMIOLOGY. Whereas the prevalence of anorexia nervosa for women in the United States is 0.5% to 1%, the prevalence of bulimia nervosa is 2% to 3% and can be as high as 10% in vulnerable populations, such as college-aged women. 6 Males are affected by eating disorders at a rate one tenth of that of females. Demographically, most patients with bulimia nervosa are single, college educated, and ...