Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Systematic Review
- Open access
- Published: 20 July 2022

The serotonin theory of depression: a systematic umbrella review of the evidence
- Joanna Moncrieff 1 , 2 ,
- Ruth E. Cooper 3 ,
- Tom Stockmann 4 ,
- Simone Amendola 5 ,
- Michael P. Hengartner 6 &
- Mark A. Horowitz 1 , 2
Molecular Psychiatry volume 28 , pages 3243–3256 ( 2023 ) Cite this article
1.30m Accesses
287 Citations
9467 Altmetric
Metrics details
- Diagnostic markers
A Correspondence to this article was published on 16 June 2023
A Comment to this article was published on 16 June 2023
The serotonin hypothesis of depression is still influential. We aimed to synthesise and evaluate evidence on whether depression is associated with lowered serotonin concentration or activity in a systematic umbrella review of the principal relevant areas of research. PubMed, EMBASE and PsycINFO were searched using terms appropriate to each area of research, from their inception until December 2020. Systematic reviews, meta-analyses and large data-set analyses in the following areas were identified: serotonin and serotonin metabolite, 5-HIAA, concentrations in body fluids; serotonin 5-HT 1A receptor binding; serotonin transporter (SERT) levels measured by imaging or at post-mortem; tryptophan depletion studies; SERT gene associations and SERT gene-environment interactions. Studies of depression associated with physical conditions and specific subtypes of depression (e.g. bipolar depression) were excluded. Two independent reviewers extracted the data and assessed the quality of included studies using the AMSTAR-2, an adapted AMSTAR-2, or the STREGA for a large genetic study. The certainty of study results was assessed using a modified version of the GRADE. We did not synthesise results of individual meta-analyses because they included overlapping studies. The review was registered with PROSPERO (CRD42020207203). 17 studies were included: 12 systematic reviews and meta-analyses, 1 collaborative meta-analysis, 1 meta-analysis of large cohort studies, 1 systematic review and narrative synthesis, 1 genetic association study and 1 umbrella review. Quality of reviews was variable with some genetic studies of high quality. Two meta-analyses of overlapping studies examining the serotonin metabolite, 5-HIAA, showed no association with depression (largest n = 1002). One meta-analysis of cohort studies of plasma serotonin showed no relationship with depression, and evidence that lowered serotonin concentration was associated with antidepressant use ( n = 1869). Two meta-analyses of overlapping studies examining the 5-HT 1A receptor (largest n = 561), and three meta-analyses of overlapping studies examining SERT binding (largest n = 1845) showed weak and inconsistent evidence of reduced binding in some areas, which would be consistent with increased synaptic availability of serotonin in people with depression, if this was the original, causal abnormaly. However, effects of prior antidepressant use were not reliably excluded. One meta-analysis of tryptophan depletion studies found no effect in most healthy volunteers ( n = 566), but weak evidence of an effect in those with a family history of depression ( n = 75). Another systematic review ( n = 342) and a sample of ten subsequent studies ( n = 407) found no effect in volunteers. No systematic review of tryptophan depletion studies has been performed since 2007. The two largest and highest quality studies of the SERT gene, one genetic association study ( n = 115,257) and one collaborative meta-analysis ( n = 43,165), revealed no evidence of an association with depression, or of an interaction between genotype, stress and depression. The main areas of serotonin research provide no consistent evidence of there being an association between serotonin and depression, and no support for the hypothesis that depression is caused by lowered serotonin activity or concentrations. Some evidence was consistent with the possibility that long-term antidepressant use reduces serotonin concentration.
Similar content being viewed by others

Beyond the serotonin deficit hypothesis: communicating a neuroplasticity framework of major depressive disorder

Genetic contributions to brain serotonin transporter levels in healthy adults
The kynurenine pathway in major depressive disorder, bipolar disorder, and schizophrenia: a meta-analysis of 101 studies
Introduction.
The idea that depression is the result of abnormalities in brain chemicals, particularly serotonin (5-hydroxytryptamine or 5-HT), has been influential for decades, and provides an important justification for the use of antidepressants. A link between lowered serotonin and depression was first suggested in the 1960s [ 1 ], and widely publicised from the 1990s with the advent of the Selective Serotonin Reuptake Inhibitor (SSRI) antidepressants [ 2 , 3 , 4 ]. Although it has been questioned more recently [ 5 , 6 ], the serotonin theory of depression remains influential, with principal English language textbooks still giving it qualified support [ 7 , 8 ], leading researchers endorsing it [ 9 , 10 , 11 ], and much empirical research based on it [ 11 , 12 , 13 , 14 ]. Surveys suggest that 80% or more of the general public now believe it is established that depression is caused by a ‘chemical imbalance’ [ 15 , 16 ]. Many general practitioners also subscribe to this view [ 17 ] and popular websites commonly cite the theory [ 18 ].
It is often assumed that the effects of antidepressants demonstrate that depression must be at least partially caused by a brain-based chemical abnormality, and that the apparent efficacy of SSRIs shows that serotonin is implicated. Other explanations for the effects of antidepressants have been put forward, however, including the idea that they work via an amplified placebo effect or through their ability to restrict or blunt emotions in general [ 19 , 20 ].
Despite the fact that the serotonin theory of depression has been so influential, no comprehensive review has yet synthesised the relevant evidence. We conducted an ‘umbrella’ review of the principal areas of relevant research, following the model of a similar review examining prospective biomarkers of major depressive disorder [ 21 ]. We sought to establish whether the current evidence supports a role for serotonin in the aetiology of depression, and specifically whether depression is associated with indications of lowered serotonin concentrations or activity.
Search strategy and selection criteria
The present umbrella review was reported in accordance with the 2009 PRISMA statement [ 22 ]. The protocol was registered with PROSPERO in December 2020 (registration number CRD42020207203) ( https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=207203 ). This was subsequently updated to reflect our decision to modify the quality rating system for some studies to more appropriately appraise their quality, and to include a modified GRADE to assess the overall certainty of the findings in each category of the umbrella review.
In order to cover the different areas and to manage the large volume of research that has been conducted on the serotonin system, we conducted an ‘umbrella’ review. Umbrella reviews survey existing systematic reviews and meta-analyses relevant to a research question and represent one of the highest levels of evidence synthesis available [ 23 ]. Although they are traditionally restricted to systematic reviews and meta-analyses, we aimed to identify the best evidence available. Therefore, we also included some large studies that combined data from individual studies but did not employ conventional systematic review methods, and one large genetic study. The latter used nationwide databases to capture more individuals than entire meta-analyses, so is likely to provide even more reliable evidence than syntheses of individual studies.
We first conducted a scoping review to identify areas of research consistently held to provide support for the serotonin hypothesis of depression. Six areas were identified, addressing the following questions: (1) Serotonin and the serotonin metabolite 5-HIAA–whether there are lower levels of serotonin and 5-HIAA in body fluids in depression; (2) Receptors - whether serotonin receptor levels are altered in people with depression; (3) The serotonin transporter (SERT) - whether there are higher levels of the serotonin transporter in people with depression (which would lower synaptic levels of serotonin); (4) Depletion studies - whether tryptophan depletion (which lowers available serotonin) can induce depression; (5) SERT gene – whether there are higher levels of the serotonin transporter gene in people with depression; (6) Whether there is an interaction between the SERT gene and stress in depression.
We searched for systematic reviews, meta-analyses, and large database studies in these six areas in PubMed, EMBASE and PsycINFO using the Healthcare Databases Advanced Search tool provided by Health Education England and NICE (National Institute for Health and Care Excellence). Searches were conducted until December 2020.
We used the following terms in all searches: (depress* OR affective OR mood) AND (systematic OR meta-analysis), and limited searches to title and abstract, since not doing so produced numerous irrelevant hits. In addition, we used terms specific to each area of research (full details are provided in Table S1 , Supplement). We also searched citations and consulted with experts.
Inclusion criteria were designed to identify the best available evidence in each research area and consisted of:
Research synthesis including systematic reviews, meta-analysis, umbrella reviews, individual patient meta-analysis and large dataset analysis.
Studies that involve people with depressive disorders or, for experimental studies (tryptophan depletion), those in which mood symptoms are measured as an outcome.
Studies of experimental procedures (tryptophan depletion) involving a sham or control condition.
Studies published in full in peer reviewed literature.
Where more than five systematic reviews or large analyses exist, the most recent five are included.
Exclusion criteria consisted of:
Animal studies.
Studies exclusively concerned with depression in physical conditions (e.g. post stroke or Parkinson’s disease) or exclusively focusing on specific subtypes of depression such as postpartum depression, depression in children, or depression in bipolar disorder.
No language or date restrictions were applied. In areas in which no systematic review or meta-analysis had been done within the last 10 years, we also selected the ten most recent studies at the time of searching (December 2020) for illustration of more recent findings. We performed this search using the same search string for this domain, without restricting it to systematic reviews and meta-analyses.
Data analysis
Each member of the team was allocated one to three domains of serotonin research to search and screen for eligible studies using abstract and full text review. In case of uncertainty, the entire team discussed eligibility to reach consensus.
For included studies, data were extracted by two reviewers working independently, and disagreement was resolved by consensus. Authors of papers were contacted for clarification when data was missing or unclear.
We extracted summary effects, confidence intervals and measures of statistical significance where these were reported, and, where relevant, we extracted data on heterogeneity. For summary effects in the non-genetic studies, preference was given to the extraction and reporting of effect sizes. Mean differences were converted to effect sizes where appropriate data were available.
We did not perform a meta-analysis of the individual meta-analyses in each area because they included overlapping studies [ 24 ]. All extracted data is presented in Table 1 . Sensitivity analyses were reported where they had substantial bearing on interpretation of findings.
The quality rating of systematic reviews and meta-analyses was assessed using AMSTAR-2 (A MeaSurement Tool to Assess systematic Reviews) [ 25 ]. For two studies that did not employ conventional systematic review methods [ 26 , 27 ] we used a modified version of the AMSTAR-2 (see Table S3 ). For the genetic association study based on a large database analysis we used the STREGA assessment (STrengthening the REporting of Genetic Association Studies) (Table S4 ) [ 28 ]. Each study was rated independently by at least two authors. We report ratings of individual items on the relevant measure, and the percentage of items that were adequately addressed by each study (Table 1 , with further detail in Tables S3 and S4 ).
Alongside quality ratings, two team members (JM, MAH) rated the certainty of the results of each study using a modified version of the GRADE guidelines [ 29 ]. Following the approach of Kennis et al. [ 21 ], we devised six criteria relevant to the included studies: whether a unified analysis was conducted on original data; whether confounding by antidepressant use was adequately addressed; whether outcomes were pre-specified; whether results were consistent or heterogeneity was adequately addressed if present; whether there was a likelihood of publication bias; and sample size. The importance of confounding by effects of current or past antidepressant use has been highlighted in several studies [ 30 , 31 ]. The results of each study were scored 1 or 0 according to whether they fulfilled each criteria, and based on these ratings an overall judgement was made about the certainty of evidence across studies in each of the six areas of research examined. The certainty of each study was based on an algorithm that prioritised sample size and uniform analysis using original data (explained more fully in the supplementary material), following suggestions that these are the key aspects of reliability [ 27 , 32 ]. An assessment of the overall certainty of each domain of research examining the role of serotonin was determined by consensus of at least two authors and a direction of effect indicated.
Search results and quality rating
Searching identified 361 publications across the 6 different areas of research, among which seventeen studies fulfilled inclusion criteria (see Fig. 1 and Table S1 for details of the selection process). Included studies, their characteristics and results are shown in Table 1 . As no systematic review or meta-analysis had been performed within the last 10 years on serotonin depletion, we also identified the 10 latest studies for illustration of more recent research findings (Table 2 ).
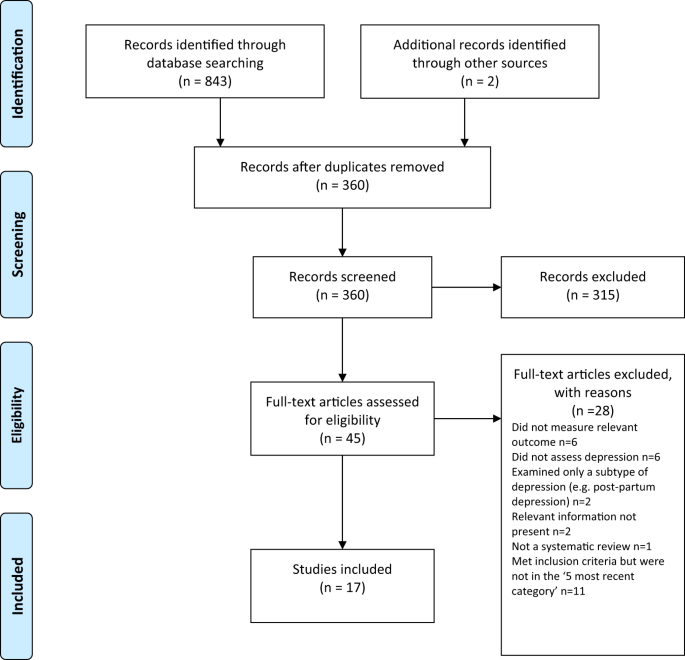
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flow diagramme.
Quality ratings are summarised in Table 1 and reported in detail in Tables S2 – S3 . The majority (11/17) of systematic reviews and meta-analyses satisfied less than 50% of criteria. Only 31% adequately assessed risk of bias in individual studies (a further 44% partially assessed this), and only 50% adequately accounted for risk of bias when interpreting the results of the review. One collaborative meta-analysis of genetic studies was considered to be of high quality due to the inclusion of several measures to ensure consistency and reliability [ 27 ]. The large genetic analysis of the effect of SERT polymorphisms on depression, satisfied 88% of the STREGA quality criteria [ 32 ].
Serotonin and 5-HIAA
Serotonin can be measured in blood, plasma, urine and CSF, but it is rapidly metabolised to 5-hydroxyindoleacetic acid (5-HIAA). CSF is thought to be the ideal resource for the study of biomarkers of putative brain diseases, since it is in contact with brain interstitial fluid [ 33 ]. However, collecting CSF samples is invasive and carries some risk, hence large-scale studies are scarce.
Three studies fulfilled inclusion criteria (Table 1 ). One meta-analysis of three large observational cohort studies of post-menopausal women, revealed lower levels of plasma 5-HT in women with depression, which did not, however, reach statistical significance of p < 0.05 after adjusting for multiple comparisons. Sensitivity analyses revealed that antidepressants were strongly associated with lower serotonin levels independently of depression.
Two meta-analyses of a total of 19 studies of 5-HIAA in CSF (seven studies were included in both) found no evidence of an association between 5-HIAA concentrations and depression.
Fourteen different serotonin receptors have been identified, with most research on depression focusing on the 5-HT 1A receptor [ 11 , 34 ]. Since the functions of other 5-HT receptors and their relationship to depression have not been well characterised, we restricted our analysis to data on 5-HT 1A receptors [ 11 , 34 ]. 5-HT 1A receptors, known as auto-receptors, inhibit the release of serotonin pre-synaptically [ 35 ], therefore, if depression is the result of reduced serotonin activity caused by abnormalities in the 5-HT 1A receptor, people with depression would be expected to show increased activity of 5-HT 1A receptors compared to those without [ 36 ].
Two meta-analyses satisfied inclusion criteria, involving five of the same studies [ 37 , 38 ] (see Table 1 ). The majority of results across the two analyses suggested either no difference in 5-HT 1A receptors between people with depression and controls, or a lower level of these inhibitory receptors, which would imply higher concentrations or activity of serotonin in people with depression. Both meta-analyses were based on studies that predominantly involved patients who were taking or had recently taken (within 1–3 weeks of scanning) antidepressants or other types of psychiatric medication, and both sets of authors commented on the possible influence of prior or current medication on findings. In addition, one analysis was of very low quality [ 37 ], including not reporting on the numbers involved in each analysis and using one-sided p-values, and one was strongly influenced by three studies and publication bias was present [ 38 ].
The serotonin transporter (SERT)
The serotonin transporter protein (SERT) transports serotonin out of the synapse, thereby lowering the availability of serotonin in the synapse [ 39 , 40 ]. Animals with an inactivated gene for SERT have higher levels of extra-cellular serotonin in the brain than normal [ 41 , 42 , 43 ] and SSRIs are thought to work by inhibiting the action of SERT, and thus increasing levels of serotonin in the synaptic cleft [ 44 ]. Although changes in SERT may be a marker for other abnormalities, if depression is caused by low serotonin availability or activity, and if SERT is the origin of that deficit, then the amount or activity of SERT would be expected to be higher in people with depression compared to those without [ 40 ]. SERT binding potential is an index of the concentration of the serotonin transporter protein and SERT concentrations can also be measured post-mortem.
Three overlapping meta-analyses based on a total of 40 individual studies fulfilled inclusion criteria (See Table 1 ) [ 37 , 39 , 45 ]. Overall, the data indicated possible reductions in SERT binding in some brain areas, although areas in which effects were detected were not consistent across the reviews. In addition, effects of antidepressants and other medication cannot be ruled out, since most included studies mainly or exclusively involved people who had a history of taking antidepressants or other psychiatric medications. Only one meta-analysis tested effects of antidepressants, and although results were not influenced by the percentage of drug-naïve patients in each study, numbers were small so it is unlikely that medication-related effects would have been reliably detected [ 45 ]. All three reviews cited evidence from animal studies that antidepressant treatment reduces SERT [ 46 , 47 , 48 ]. None of the analyses corrected for multiple testing, and one review was of very low quality [ 37 ]. If the results do represent a positive finding that is independent of medication, they would suggest that depression is associated with higher concentrations or activity of serotonin.
Depletion studies
Tryptophan depletion using dietary means or chemicals, such as parachlorophenylalanine (PCPA), is thought to reduce serotonin levels. Since PCPA is potentially toxic, reversible tryptophan depletion using an amino acid drink that lacks tryptophan is the most commonly used method and is thought to affect serotonin within 5–7 h of ingestion. Questions remain, however, about whether either method reliably reduces brain serotonin, and about other effects including changes in brain nitrous oxide, cerebrovascular changes, reduced BDNF and amino acid imbalances that may be produced by the manipulations and might explain observed effects independent of possible changes in serotonin activity [ 49 ].
One meta-analysis and one systematic review fulfilled inclusion criteria (see Table 1 ). Data from studies involving volunteers mostly showed no effect, including a meta-analysis of parallel group studies [ 50 ]. In a small meta-analysis of within-subject studies involving 75 people with a positive family history, a minor effect was found, with people given the active depletion showing a larger decrease in mood than those who had a sham procedure [ 50 ]. Across both reviews, studies involving people diagnosed with depression showed slightly greater mood reduction following tryptophan depletion than sham treatment overall, but most participants had taken or were taking antidepressants and participant numbers were small [ 50 , 51 ].
Since these research syntheses were conducted more than 10 years ago, we searched for a systematic sample of ten recently published studies (Table 2 ). Eight studies conducted with healthy volunteers showed no effects of tryptophan depletion on mood, including the only two parallel group studies. One study presented effects in people with and without a family history of depression, and no differences were apparent in either group [ 52 ]. Two cross-over studies involving people with depression and current or recent use of antidepressants showed no convincing effects of a depletion drink [ 53 , 54 ], although one study is reported as positive mainly due to finding an improvement in mood in the group given the sham drink [ 54 ].
SERT gene and gene-stress interactions
A possible link between depression and the repeat length polymorphism in the promoter region of the SERT gene (5-HTTLPR), specifically the presence of the short repeats version, which causes lower SERT mRNA expression, has been proposed [ 55 ]. Interestingly, lower levels of SERT would produce higher levels of synaptic serotonin. However, more recently, this hypothesis has been superseded by a focus on the interaction effect between this polymorphism, depression and stress, with the idea that the short version of the polymorphism may only give rise to depression in the presence of stressful life events [ 55 , 56 ]. Unlike other areas of serotonin research, numerous systematic reviews and meta-analyses of genetic studies have been conducted, and most recently a very large analysis based on a sample from two genetic databanks. Details of the five most recent studies that have addressed the association between the SERT gene and depression, and the interaction effect are detailed in Table 1 .
Although some earlier meta-analyses of case-control studies showed a statistically significant association between the 5-HTTLPR and depression in some ethnic groups [ 57 , 58 ], two recent large, high quality studies did not find an association between the SERT gene polymorphism and depression [ 27 , 32 ]. These two studies consist of by far the largest and most comprehensive study to date [ 32 ] and a high-quality meta-analysis that involved a consistent re-analysis of primary data across all conducted studies, including previously unpublished data, and other comprehensive quality checks [ 27 , 59 ] (see Table 1 ).
Similarly, early studies based on tens of thousands of participants suggested a statistically significant interaction between the SERT gene, forms of stress or maltreatment and depression [ 60 , 61 , 62 ], with a small odds ratio in the only study that reported this (1.18, 95% CI 1.09 to 1.28) [ 62 ]. However, the two recent large, high-quality studies did not find an interaction between the SERT gene and stress in depression (Border et al [ 32 ] and Culverhouse et al.) [ 27 ] (see Table 1 ).
Overall results
Table 3 presents the modified GRADE ratings for each study and the overall rating of the strength of evidence in each area. Areas of research that provided moderate or high certainty of evidence such as the studies of plasma serotonin and metabolites and the genetic and gene-stress interaction studies all showed no association between markers of serotonin activity and depression. Some other areas suggested findings consistent with increased serotonin activity, but evidence was of very low certainty, mainly due to small sample sizes and possible residual confounding by current or past antidepressant use. One area - the tryptophan depletion studies - showed very low certainty evidence of lowered serotonin activity or availability in a subgroup of volunteers with a family history of depression. This evidence was considered very low certainty as it derived from a subgroup of within-subject studies, numbers were small, and there was no information on medication use, which may have influenced results. Subsequent research has not confirmed an effect with numerous negative studies in volunteers.
Our comprehensive review of the major strands of research on serotonin shows there is no convincing evidence that depression is associated with, or caused by, lower serotonin concentrations or activity. Most studies found no evidence of reduced serotonin activity in people with depression compared to people without, and methods to reduce serotonin availability using tryptophan depletion do not consistently lower mood in volunteers. High quality, well-powered genetic studies effectively exclude an association between genotypes related to the serotonin system and depression, including a proposed interaction with stress. Weak evidence from some studies of serotonin 5-HT 1A receptors and levels of SERT points towards a possible association between increased serotonin activity and depression. However, these results are likely to be influenced by prior use of antidepressants and its effects on the serotonin system [ 30 , 31 ]. The effects of tryptophan depletion in some cross-over studies involving people with depression may also be mediated by antidepressants, although these are not consistently found [ 63 ].
The chemical imbalance theory of depression is still put forward by professionals [ 17 ], and the serotonin theory, in particular, has formed the basis of a considerable research effort over the last few decades [ 14 ]. The general public widely believes that depression has been convincingly demonstrated to be the result of serotonin or other chemical abnormalities [ 15 , 16 ], and this belief shapes how people understand their moods, leading to a pessimistic outlook on the outcome of depression and negative expectancies about the possibility of self-regulation of mood [ 64 , 65 , 66 ]. The idea that depression is the result of a chemical imbalance also influences decisions about whether to take or continue antidepressant medication and may discourage people from discontinuing treatment, potentially leading to lifelong dependence on these drugs [ 67 , 68 ].
As with all research synthesis, the findings of this umbrella review are dependent on the quality of the included studies, and susceptible to their limitations. Most of the included studies were rated as low quality on the AMSTAR-2, but the GRADE approach suggested some findings were reasonably robust. Most of the non-genetic studies did not reliably exclude the potential effects of previous antidepressant use and were based on relatively small numbers of participants. The genetic studies, in particular, illustrate the importance of methodological rigour and sample size. Whereas some earlier, lower quality, mostly smaller studies produced marginally positive findings, these were not confirmed in better-conducted, larger and more recent studies [ 27 , 32 ]. The identification of depression and assessment of confounders and interaction effects were limited by the data available in the original studies on which the included reviews and meta-analyses were based. Common methods such as the categorisation of continuous measures and application of linear models to non-linear data may have led to over-estimation or under-estimation of effects [ 69 , 70 ], including the interaction between stress and the SERT gene. The latest systematic review of tryptophan depletion studies was conducted in 2007, and there has been considerable research produced since then. Hence, we provided a snapshot of the most recent evidence at the time of writing, but this area requires an up to date, comprehensive data synthesis. However, the recent studies were consistent with the earlier meta-analysis with little evidence for an effect of tryptophan depletion on mood.
Although umbrella reviews typically restrict themselves to systematic reviews and meta-analyses, we aimed to provide the most comprehensive possible overview. Therefore, we chose to include meta-analyses that did not involve a systematic review and a large genetic association study on the premise that these studies contribute important data on the question of whether the serotonin hypothesis of depression is supported. As a result, the AMSTAR-2 quality rating scale, designed to evaluate the quality of conventional systematic reviews, was not easily applicable to all studies and had to be modified or replaced in some cases.
One study in this review found that antidepressant use was associated with a reduction of plasma serotonin [ 26 ], and it is possible that the evidence for reductions in SERT density and 5-HT 1A receptors in some of the included imaging study reviews may reflect compensatory adaptations to serotonin-lowering effects of prior antidepressant use. Authors of one meta-analysis also highlighted evidence of 5-HIAA levels being reduced after long-term antidepressant treatment [ 71 ]. These findings suggest that in the long-term antidepressants might produce compensatory changes [ 72 ] that are opposite to their acute effects [ 73 , 74 ]. Lowered serotonin availability has also been demonstrated in animal studies following prolonged antidepressant administration [ 75 ]. Further research is required to clarify the effects of different drugs on neurochemical systems, including the serotonin system, especially during and after long-term use, as well as the physical and psychological consequences of such effects.
This review suggests that the huge research effort based on the serotonin hypothesis has not produced convincing evidence of a biochemical basis to depression. This is consistent with research on many other biological markers [ 21 ]. We suggest it is time to acknowledge that the serotonin theory of depression is not empirically substantiated.
Data availability
All extracted data is available in the paper and supplementary materials. Further information about the decision-making for each rating for categories of the AMSTAR-2 and STREGA are available on request.
Coppen A. The biochemistry of affective disorders. Br J Psychiatry. 1967;113:1237–64.
Article CAS PubMed Google Scholar
American Psychiatric Association. What Is Psychiatry? 2021. https://www.psychiatry.org/patients-families/what-is-psychiatry-menu .
GlaxoSmithKline. Paxil XR. 2009. www.Paxilcr.com (site no longer available). Last accessed 27th Jan 2009.
Eli Lilly. Prozac - How it works. 2006. www.prozac.com/how_prozac/how_it_works.jsp?reqNavId=2.2 . (site no longer available). Last accessed 10th Feb 2006.
Healy D. Serotonin and depression. BMJ: Br Med J. 2015;350:h1771.
Article Google Scholar
Pies R. Psychiatry’s New Brain-Mind and the Legend of the “Chemical Imbalance.” 2011. https://www.psychiatrictimes.com/view/psychiatrys-new-brain-mind-and-legend-chemical-imbalance . Accessed March 2, 2021.
Geddes JR, Andreasen NC, Goodwin GM. New Oxford Textbook of Psychiatry. Oxford, UK: Oxford University Press; 2020.
Book Google Scholar
Sadock BJ, Sadock VA, Ruiz P. Kaplan & Sadock’s Comprehensive Textbook of Psychiatry. 10th Editi. Lippincott Williams & Wilkins (LWW); 2017.
Cowen PJ, Browning M. What has serotonin to do with depression? World Psychiatry. 2015;14:158–60.
Article PubMed PubMed Central Google Scholar
Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? New perspectives for refining future treatment approaches. Lancet Psychiatry. 2017;4:409–18.
Yohn CN, Gergues MM, Samuels BA. The role of 5-HT receptors in depression. Mol Brain. 2017;10:28.
Hahn A, Haeusler D, Kraus C, Höflich AS, Kranz GS, Baldinger P, et al. Attenuated serotonin transporter association between dorsal raphe and ventral striatum in major depression. Hum Brain Mapp. 2014;35:3857–66.
Amidfar M, Colic L, Kim MWAY-K. Biomarkers of major depression related to serotonin receptors. Curr Psychiatry Rev. 2018;14:239–44.
Article CAS Google Scholar
Albert PR, Benkelfat C, Descarries L. The neurobiology of depression—revisiting the serotonin hypothesis. I. Cellular and molecular mechanisms. Philos Trans R Soc Lond B Biol Sci. 2012;367:2378–81.
Article CAS PubMed PubMed Central Google Scholar
Pilkington PD, Reavley NJ, Jorm AF. The Australian public’s beliefs about the causes of depression: associated factors and changes over 16 years. J Affect Disord. 2013;150:356–62.
Article PubMed Google Scholar
Pescosolido BA, Martin JK, Long JS, Medina TR, Phelan JC, Link BG. A disease like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. Am J Psychiatry. 2010;167:1321–30.
Read J, Renton J, Harrop C, Geekie J, Dowrick C. A survey of UK general practitioners about depression, antidepressants and withdrawal: implementing the 2019 Public Health England report. Therapeutic Advances in. Psychopharmacology. 2020;10:204512532095012.
Google Scholar
Demasi M, Gøtzsche PC. Presentation of benefits and harms of antidepressants on websites: A cross-sectional study. Int J Risk Saf Med. 2020;31:53–65.
Jakobsen JC, Gluud C, Kirsch I. Should antidepressants be used for major depressive disorder? BMJ Evidence-Based. Medicine. 2020;25:130–130.
Moncrieff J, Cohen D. Do antidepressants cure or create abnormal brain states? PLoS Med. 2006;3:e240.
Kennis M, Gerritsen L, van Dalen M, Williams A, Cuijpers P, Bockting C. Prospective biomarkers of major depressive disorder: a systematic review and meta-analysis. Mol Psychiatry. 2020;25:321–38.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Fusar-Poli P, Radua J. Ten simple rules for conducting umbrella reviews. Evid Based Ment Health. 2018;21:95–100.
Pollock M, Fernandes RM, Becker LA, Pieper D, Hartling L. Chapter V: Overviews of Reviews. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al., editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2,. version 6.Cochrane; 2021.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Huang T, Balasubramanian R, Yao Y, Clish CB, Shadyab AH, Liu B, et al. Associations of depression status with plasma levels of candidate lipid and amino acid metabolites: a meta-analysis of individual data from three independent samples of US postmenopausal women. Mol Psychiatry. 2020;2020. https://doi.org/10.1038/s41380-020-00870-9 .
Culverhouse RC, Saccone NL, Horton AC, Ma Y, Anstey KJ, Banaschewski T, et al. Collaborative meta-analysis finds no evidence of a strong interaction between stress and 5-HTTLPR genotype contributing to the development of depression. Mol Psychiatry. 2018;23:133–42.
Little J, Higgins JPT, Ioannidis JPA, Moher D, Gagnon F, von Elm E, et al. STrengthening the REporting of Genetic Association Studies (STREGA)— An Extension of the STROBE Statement. PLoS Med. 2009;6:e1000022.
Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ. What is quality of evidence and why is it important to clinicians? BMJ. 2008;336:995–8.
Yoon HS, Hattori K, Ogawa S, Sasayama D, Ota M, Teraishi T, et al. Relationships of cerebrospinal fluid monoamine metabolite levels with clinical variables in major depressive disorder. J Clin Psychiatry. 2017;78:e947–56.
Kugaya A, Seneca NM, Snyder PJ, Williams SA, Malison RT, Baldwin RM, et al. Changes in human in vivo serotonin and dopamine transporter availabilities during chronic antidepressant administration. Neuropsychopharmacology. 2003;28:413–20.
Border R, Johnson EC, Evans LM, Smolen A, Berley N, Sullivan PF, et al. No support for historical candidate gene or candidate gene-by-interaction hypotheses for major depression across multiple large samples. Am J Psychiatry. 2019;176:376–87.
Ogawa S, Tsuchimine S, Kunugi H. Cerebrospinal fluid monoamine metabolite concentrations in depressive disorder: A meta-analysis of historic evidence. J Psychiatr Res. 2018;105:137–46.
Nautiyal KM, Hen R. Serotonin receptors in depression: from A to B. F1000Res. 2017;6:123.
Rojas PS, Neira D, Muñoz M, Lavandero S, Fiedler JL. Serotonin (5‐HT) regulates neurite outgrowth through 5‐HT1A and 5‐HT7 receptors in cultured hippocampal neurons. J Neurosci Res. 2014;92:1000–9.
Kaufman J, DeLorenzo C, Choudhury S, Parsey RV. The 5-HT1A receptor in Major Depressive Disorder. Eur Neuropsychopharmacol. 2016;26:397–410.
Nikolaus S, Müller H-W, Hautzel H. Different patterns of 5-HT receptor and transporter dysfunction in neuropsychiatric disorders – a comparative analysis of in vivo imaging findings. Rev Neurosci. 2016;27:27–59.
Wang L, Zhou C, Zhu D, Wang X, Fang L, Zhong J, et al. Serotonin-1A receptor alterations in depression: A meta-analysis of molecular imaging studies. BMC Psychiatry. 2016;16:1–9.
Kambeitz JP, Howes OD. The serotonin transporter in depression: Meta-analysis of in vivo and post mortem findings and implications for understanding and treating depression. J Affect Disord. 2015;186:358–66.
Meyer JH. Imaging the serotonin transporter during major depressive disorder and antidepressant treatment. J Psychiatry Neurosci. 2007;32:86–102.
PubMed PubMed Central Google Scholar
Mathews TA, Fedele DE, Coppelli FM, Avila AM, Murphy DL, Andrews AM. Gene dose-dependent alterations in extraneuronal serotonin but not dopamine in mice with reduced serotonin transporter expression. J Neurosci Methods. 2004;140:169–81.
Shen H-W, Hagino Y, Kobayashi H, Shinohara-Tanaka K, Ikeda K, Yamamoto H, et al. Regional differences in extracellular dopamine and serotonin assessed by in vivo microdialysis in mice lacking dopamine and/or serotonin transporters. Neuropsychopharmacology. 2004;29:1790–9.
Hagino Y, Takamatsu Y, Yamamoto H, Iwamura T, Murphy DL, Uhl GR, et al. Effects of MDMA on extracellular dopamine and serotonin levels in mice lacking dopamine and/or serotonin transporters. Curr Neuropharmacol. 2011;9:91–5.
Zhou Z, Zhen J, Karpowich NK, Law CJ, Reith MEA, Wang D-N. Antidepressant specificity of serotonin transporter suggested by three LeuT-SSRI structures. Nat Struct Mol Biol. 2009;16:652–7.
Gryglewski G, Lanzenberger R, Kranz GS, Cumming P. Meta-analysis of molecular imaging of serotonin transporters in major depression. J Cereb Blood Flow Metab. 2014;34:1096–103.
Benmansour S, Owens WA, Cecchi M, Morilak DA, Frazer A. Serotonin clearance in vivo is altered to a greater extent by antidepressant-induced downregulation of the serotonin transporter than by acute blockade of this transporter. J Neurosci. 2002;22:6766–72.
Benmansour S, Cecchi M, Morilak DA, Gerhardt GA, Javors MA, Gould GG, et al. Effects of chronic antidepressant treatments on serotonin transporter function, density, and mRNA level. J Neurosci. 1999;19:10494–501.
Horschitz S, Hummerich R, Schloss P. Down-regulation of the rat serotonin transporter upon exposure to a selective serotonin reuptake inhibitor. Neuroreport. 2001;12:2181–4.
Young SN. Acute tryptophan depletion in humans: a review of theoretical, practical and ethical aspects. J Psychiatry Neurosci. 2013;38:294–305.
Ruhe HG, Mason NS, Schene AH. Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry. 2007;12:331–59.
Fusar-Poli P, Allen P, McGuire P, Placentino A, Cortesi M, Perez J. Neuroimaging and electrophysiological studies of the effects of acute tryptophan depletion: A systematic review of the literature. Psychopharmacology. 2006;188:131–43.
Hogenelst K, Schoevers RA, Kema IP, Sweep FCGJ, aan het Rot M. Empathic accuracy and oxytocin after tryptophan depletion in adults at risk for depression. Psychopharmacology. 2016;233:111–20.
Weinstein JJ, Rogers BP, Taylor WD, Boyd BD, Cowan RL, Shelton KM, et al. Effects of acute tryptophan depletion on raphé functional connectivity in depression. Psychiatry Res. 2015;234:164–71.
Moreno FA, Erickson RP, Garriock HA, Gelernter J, Mintz J, Oas-Terpstra J, et al. Association study of genotype by depressive response during tryptophan depletion in subjects recovered from major depression. Mol. Neuropsychiatry. 2015;1:165–74.
Munafò MR. The serotonin transporter gene and depression. Depress Anxiety. 2012;29:915–7.
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 2003;301:386–9.
Kiyohara C, Yoshimasu K. Association between major depressive disorder and a functional polymorphism of the 5-hydroxytryptamine (serotonin) transporter gene: A meta-analysis. Psychiatr Genet. 2010;20:49–58.
Oo KZ, Aung YK, Jenkins MA, Win AK. Associations of 5HTTLPR polymorphism with major depressive disorder and alcohol dependence: A systematic review and meta-analysis. Aust N. Z J Psychiatry. 2016;50:842–57.
Culverhouse RC, Bowes L, Breslau N, Nurnberger JI, Burmeister M, Fergusson DM, et al. Protocol for a collaborative meta-analysis of 5-HTTLPR, stress, and depression. BMC Psychiatry. 2013;13:1–12.
Karg K, Burmeister M, Shedden K, Sen S. The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited. Arch Gen Psychiatry. 2011;68:444.
Sharpley CF, Palanisamy SKA, Glyde NS, Dillingham PW, Agnew LL. An update on the interaction between the serotonin transporter promoter variant (5-HTTLPR), stress and depression, plus an exploration of non-confirming findings. Behav Brain Res. 2014;273:89–105.
Bleys D, Luyten P, Soenens B, Claes S. Gene-environment interactions between stress and 5-HTTLPR in depression: A meta-analytic update. J Affect Disord. 2018;226:339–45.
Delgado PL. Monoamine depletion studies: implications for antidepressant discontinuation syndrome. J Clin Psychiatry. 2006;67:22–26.
CAS PubMed Google Scholar
Kemp JJ, Lickel JJ, Deacon BJ. Effects of a chemical imbalance causal explanation on individuals’ perceptions of their depressive symptoms. Behav Res Ther. 2014;56:47–52.
Lebowitz MS, Ahn W-K, Nolen-Hoeksema S. Fixable or fate? Perceptions of the biology of depression. J Consult Clin Psychol. 2013;81:518.
Zimmermann M, Papa A. Causal explanations of depression and treatment credibility in adults with untreated depression: Examining attribution theory. Psychol Psychother. 2020;93:537–54.
Maund E, Dewar-Haggart R, Williams S, Bowers H, Geraghty AWA, Leydon G, et al. Barriers and facilitators to discontinuing antidepressant use: A systematic review and thematic synthesis. J Affect Disord. 2019;245:38–62.
Eveleigh R, Speckens A, van Weel C, Oude Voshaar R, Lucassen P. Patients’ attitudes to discontinuing not-indicated long-term antidepressant use: barriers and facilitators. Therapeutic Advances in. Psychopharmacology. 2019;9:204512531987234.
Harrell FE Jr. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. Springer, Cham; 2015.
Schafer JL, Kang J. Average causal effects from nonrandomized studies: a practical guide and simulated example. Psychol Methods. 2008;13:279–313.
Pech J, Forman J, Kessing LV, Knorr U. Poor evidence for putative abnormalities in cerebrospinal fluid neurotransmitters in patients with depression versus healthy non-psychiatric individuals: A systematic review and meta-analyses of 23 studies. J Affect Disord. 2018;240:6–16.
Fava GA. May antidepressant drugs worsen the conditions they are supposed to treat? The clinical foundations of the oppositional model of tolerance. Therapeutic Adv Psychopharmacol. 2020;10:2045125320970325.
Kitaichi Y, Inoue T, Nakagawa S, Boku S, Kakuta A, Izumi T, et al. Sertraline increases extracellular levels not only of serotonin, but also of dopamine in the nucleus accumbens and striatum of rats. Eur J Pharm. 2010;647:90–6.
Gartside SE, Umbers V, Hajós M, Sharp T. Interaction between a selective 5‐HT1Areceptor antagonist and an SSRI in vivo: effects on 5‐HT cell firing and extracellular 5‐HT. Br J Pharmacol. 1995;115:1064–70.
Bosker FJ, Tanke MAC, Jongsma ME, Cremers TIFH, Jagtman E, Pietersen CY, et al. Biochemical and behavioral effects of long-term citalopram administration and discontinuation in rats: role of serotonin synthesis. Neurochem Int. 2010;57:948–57.
Download references
There was no specific funding for this review. MAH is supported by a Clinical Research Fellowship from North East London NHS Foundation Trust (NELFT). This funder had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and affiliations.
Division of Psychiatry, University College London, London, UK
Joanna Moncrieff & Mark A. Horowitz
Research and Development Department, Goodmayes Hospital, North East London NHS Foundation Trust, Essex, UK
Faculty of Education, Health and Human Sciences, University of Greenwich, London, UK
Ruth E. Cooper
Psychiatry-UK, Cornwall, UK
Tom Stockmann
Department of Dynamic and Clinical Psychology, and Health Studies, Faculty of Medicine and Psychology, Sapienza University of Rome, Rome, Italy
Simone Amendola
Department of Applied Psychology, Zurich University of Applied Sciences, Zurich, Switzerland
Michael P. Hengartner
You can also search for this author in PubMed Google Scholar
Contributions
JM conceived the idea for the study. JM, MAH, MPH, TS and SA designed the study. JM, MAH, MPH, TS, and SA screened articles and abstracted data. JM drafted the first version of the manuscript. JM, MAH, MPH, TS, SA, and REC contributed to the manuscript’s revision and interpretation of findings. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding author
Correspondence to Joanna Moncrieff .
Ethics declarations
Competing interests.
All authors have completed the Unified Competing Interest form at http://www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). SA declares no conflicts of interest. MAH reports being co-founder of a company in April 2022, aiming to help people safely stop antidepressants in Canada. MPH reports royalties from Palgrave Macmillan, London, UK for his book published in December, 2021, called “Evidence-biased Antidepressant Prescription.” JM receives royalties for books about psychiatric drugs, reports grants from the National Institute of Health Research outside the submitted work, that she is co-chairperson of the Critical Psychiatry Network (an informal group of psychiatrists) and a board member of the unfunded organisation, the Council for Evidence-based Psychiatry. Both are unpaid positions. TS is co-chairperson of the Critical Psychiatry Network. RC is an unpaid board member of the International Institute for Psychiatric Drug Withdrawal.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary tables, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Moncrieff, J., Cooper, R.E., Stockmann, T. et al. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry 28 , 3243–3256 (2023). https://doi.org/10.1038/s41380-022-01661-0
Download citation
Received : 21 June 2021
Revised : 31 May 2022
Accepted : 07 June 2022
Published : 20 July 2022
Issue Date : August 2023
DOI : https://doi.org/10.1038/s41380-022-01661-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Association between junk food consumption and mental health problems in adults: a systematic review and meta-analysis.
- Hanieh-Sadat Ejtahed
- Parham Mardi
- Mostafa Qorbani
BMC Psychiatry (2024)
The involvement of serotonin in major depression: nescience in disguise?
- Danilo Arnone
- Catherine J. Harmer
Molecular Psychiatry (2024)
- Chloe E. Page
- C. Neill Epperson
- Scott M. Thompson
Serotonin effects on human iPSC-derived neural cell functions: from mitochondria to depression
- Iseline Cardon
- Sonja Grobecker
- Christian H. Wetzel
Neither serotonin disorder is at the core of depression nor dopamine at the core of schizophrenia; still these are biologically based mental disorders
- Konstantinos N. Fountoulakis
- Eva Maria Tsapakis
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Call to +1 844 889-9952
Literature Review on Depression
| 📄 Words: | 2255 |
|---|---|
| 📝 Subject: | |
| 📑 Pages: | 8 |
| 📚 Topics: | , , |
Depression alters one’s mood, making one feel sad and lose interest in people, events, and objects, and thus may cause physical and emotional problems. It may involve treatment in the long run if it persists, which includes medication and psychotherapy. This paper will focus on a detailed summary of other researchers’ work addressing the issue of depression using several databases and carry out a curative study on depression in full text. The following literature review is based on selected articles meeting the criteria of inclusion.
According to Lim et al. (2018), depression in the general population is a common mental health condition. It is highly associated with sadness, low self-esteem, poor concentration, anxiety, interest loss, and a feeling of being a quilt. The study also shows that the World Health Organization (WHO) predicted that depression will be ranked as the second global disease burden by 2020. The research also covered the nomothetic and idiographic measures of depression, which means that the assessed item is common to every person at different degree levels. In contrast, the idiographic measure is based on the distinct features and views of the patient. The study concludes that during the patient assessment on the defined objective of treatment, idiographic measures are preferred due to being more relevant.
An investigation done by Bernaras et al. (2019) states that depression is the main cause of disability-related illness in the world. The research focused on depression among children and adolescents since these two groups are agilely associated with high incidence. It also analyses the theories that construct and explain depression and provides an overview of disorders among children and adolescents. In this study, the authors conclude that depression in terms of the mental distinction between adults and children has no difference, and thus, the theory of explanation is highly taken into account to elaborate a better understanding of depression. The research further stated that treatment and prevention should be multifactorial (Bernaras et al., 2019). Besides, it is estimated that universal programs can be more efficient considering their wide application. The research results are limited in providing a good conclusion and fail to demonstrate any solid long-term efficacy.
Bernaras et al.(2019) in their examination found that biological factors such as tryptophan have a strong influence on the appearance of a depressive disorder. The increase seen in the prevalence of depression is explained by having negative interpersonal relations and the relationship with one’s surroundings accompanied by social-cultural changes. Additionally, the authors conclude that many instruments can be applied in elevating depression, but it is more important to have a continued test to diagnose the condition at the early stages. Regarding the prevention programs, the study suggested that they should be implemented at early initial ages, and finally, most depression treatments are more rigorous and effective.
Additionally, Health Quality Ontario (2017) suggests that the most diagnosed disorders in Canada on depression are major depressive and generalized anxiety disorders that are mostly associated with high disorders and economic hardship. It is important to note that the treatment of the two conditions is known to include pharmacological and psychological preventions. The highly used psychological interventions include cognitive-behavioral therapy (CBT), supportive therapy, and interpersonal therapy.
The study supports the fact that depression is the world’s second-largest health problem based on illness-induced disability. The three most used psychotherapeutic treatments which are well explained in this research include CBT, interpersonal therapy, and supportive therapy. CBT focuses on helping patients understand how automated thoughts on beliefs, expectations, and attitudes have a major contribution to anxiety and sadness. Interpersonal therapy aims to identify and solve problems through the establishment and maintenance of a satisfying relationship. Lastly, supportive therapy is an unstructured approach that relies on the basic interpersonal skills of the therapist.
Research conducted by Lu (2019) on adolescent depression on the topic of national trends, health care disparities, and risk factors shows that in the US, depression is a major cause of suicide among adolescents in aged between 10 and 19. Suicide is marked as the third major cause of death in the US, and research reflects that depression is the major factor in these cases. According to Lu (2019), depression is mostly underdiagnosed among adolescents, although mental health treatment is available. Lu (2019) states that if depression is not treated at the early age of an adolescent, it can have substantial negative effects on health and social results in late adolescence and adulthood.
Findings from the study revealed a growing number of untreated adolescents with major depression from 2011 to 2016 from the National Survey on Drug Use and Health (NSDUH) data. The research outcomes highlighted some of the major causes of depression among young people. Such factors include some sociodemographic, school, and family parameters, and the underutilization of mental health services. The study findings also highlight the importance of family and school in the treatment of depression. Finally, it was proved that adolescents with less family attention were more vulnerable to depression and less likely to receive mental and medical treatment.
The treatment of depression among adults in the United has been covered by a study done by Olfson et al. (2016). Based on the national survey conducted from 2001 to 2003, it was approximated that 49.5 percent of adults with a history of depression had not received any treatment, and about 48.4 percent had not received mental treatment over the past year (Olfson et al., 2016). According to the study, the US Preventive Service Task Force (USPSTF) has recommended adult screening on depression and a follow-up on the treatment that should be provided through a clinical setting arrangement.
The study findings showed that although there is the increased use of antidepressants, there still exists a gap in the treatment of depression. The number of adults who received screening for depression did not receive treatment that year. The research also showed that there was a low hood on receiving treatment to racial /ethnic minority groups. Regarding the application of antidepressants, the patient who had less serious depression had a high likelihood of receiving antidepressants than seriously depressed patients.
Antipsychotics, anxiolytics and mood stabilizers were mostly used to treat patients with higher than lower degrees of distress. Olfson et al. (2016) stated that this type of medication was mostly kept to treat patients with more complicated and resistant to treatment conditions. Antipsychotic treatment is suitable for patients with resistance to the use of antidepressants. Anxiolytics largely aid in managing anxiety problems that do not respond to the use of antidepressants. Finally, mood stabilizers help in the adjustment of agitations related to depression.
Research by Stark et al. (2018) on the issue of depression perspective in older primary care patients, treatment, and depression management opportunities showed that depression in old age is very common and has health-related consequences on the elderly. Research findings showed that symptoms like sadness and withdrawal are associated with older people. The consequences of depression can lead to death through suicide, social isolation, loss of family and work, and low esteem. The causes of the condition, as stated by Stark et al. (2018), are classified based on changing life events and internal factors.
According to Stark et al. (2018), depression does not only occur at young age people but is also a threat to older people. In age-related causes, the increased incidence of deaths among relatives can cause loneliness and boredom. Treatment of depression among older adults is possible. The main obstacles to the successful recovery from depression among the elderly, according to research, include beliefs on there is no treatment for depression among older people as well as fear of stigmatization. Similarly, it is believed that people should only care about their problems.
Research on adolescent depression, in particular, the one conducted by Lu (2019), has greatly contributed to literature work. Vrijen et al. (2016) have concentrated their research on predicting depression through the slow identification of facial happiness during early adolescent stages. As seen from previous research, depression remains a major concern in mental health problems. The study proved how facial emotions in the early ages of depression could predict depressive disorders and symptoms.
Research findings suggested that facial emotion identification prejudice may be a symptom corresponding trait marker for depressive disorder and anhedonia. The associations were found only based on multi-emotional models. The study found that individuals who portray sadness in comparison to happy ones are more likely to develop depression or anhedonia symptoms. The emotion identification effects on depressive disorders are mainly seen as carried by the symptoms of anhedonia but not symptoms of sadness. There is a relationship between symptoms of anhedonia and facial emotion identification (Vrijen et al., 2016). On the elimination of adolescents, the research findings were stronger on the predictive value on the identification of facial reactions for individuals with depressive disorders related to anhedonia and despair and may inversely be connected with facial identification of emotions.
Furthermore, depression and depressive symptoms among outpatients showed that the features are very common in people with mental disorders and gave a considerable number of effects on patient quality of health. The results of previous studies vary from the consideration presented in the research by Wang et al. (2017). In this study, it was found that the number of outpatients from otolaryngology clinics was higher, marking 53.0 %. The research also highlighted that depression was a mediator among conditions in otolaryngology.
The outcomes also have shown that there is a psychoneuroimmunology link between medical illness and depression. Besides, stroke burdens were found to cause depression among patients and their caregivers. For patience with stroke, it was found that novel rehabilitation interventions might reduce depression. A medical professional often overlooks depression or depressive symptoms due to not having been offered specific mental health training. In this research, it was found that outpatients between the age of 30 and 40 had related depression prevalence as compared to outpatients between the age of 80 and 90 years old. The result contradicts research done by Benaras et al. (2019) on depression among children and adolescents, which focused on the rise of the incidence of suicide cases caused by depression. Yang’s study showed that depression levels declined with age. The author presents different results as he stresses that there was no pattern on depression centering his argument on age.
Depression has been a global problem that has raised concerns among employees and employers. According to McCart and Nesbit (2020), the number of days of absenteeism in jobs results from depression is higher than those related to diseases like heart attack and hypertension all put together. According to the study, billions of dollars are spent on medical care, mortality due to suicide, and the loss of productivity as a result of depression. McCart and Nesbit (2020) have discussed a connection between disorders caused by depression and such chronic conditions as the unemployment period and the total income.
In the employment setting, research has shown that some reasons make it difficult to diagnose depression. In the workplace, employees can avoid diagnosis because of the lack of skills by physicians, stigma, unavailability of treatment and providers, restrictions on drugs, psychotherapeutic care, and limitations due to third-party coverage. The study results from most organizations lack a way of huddling the employee’s depression. Education institutions were found to be having programs that help depressed personnel. Other organizations stated that depression is a personal issue, and unless an employee asks for help, the services are not openly offered.
Among pregnant women, depression has been found to affect both the mother and the unborn child. Looking at both depression and anxiety during the period of antenatal and post-natal, there is a notable effect of depression among these groups. According to Smith et al. (2019), there is a preference in pregnant women for non-pharmacological treatment options; instead, they prefer the use of therapies and complementary medicines to manage the symptoms.
Martínez-Paredes and Jácome-Pérez (2019) conducted a similar study on depression among pregnant women, which confirmed that depression in this group is common psychiatric mobility. Diagnosis of depression is based on guidelines by the DSM-5 to validate scales like the Edinburgh Postnatal Depression Scale. According to medical professionals, the research also shows negative effects on the treatment, diagnosis, and recognition of the fetus. The study concluded that depression is a common condition among pregnant women, though it is underlooked as its symptoms are linked to pregnancy.
Several personal and mental effects are caused by depression among patients of total knee arthroplasty. Findings of the research have indicated that patients with higher education levels have less depression and are happier before surgery. Results have also illustrated that people with depression and anxiety were found to improve at a low rate than other groups. It also stated that patients with greater health were seen to have a considerable improvement in mental health. The conclusion of the research showed that the main determinant of physical, mental, and functional outcomes was depression.
Depression remains to be among the top five illnesses in the world, and research works have reflected that age does not matter, with everyone being at risk of developing the condition. In most studies, it is indicated as the main cause of suicide and death among children and adolescents. There are ways to help individuals suffering from despair such as the use of antidepressants among people with low depression levels. Likewise, early detection and treatment of the disorder can help individuals in their late adolescent stages and adulthood. Families can offer their support instead of contributing and worsening this condition.
Bernaras, E., Jaureguizar, J., & Garaigordobil, M. (2019). Child and adolescent depression: A review of theories, evaluation instruments, prevention programs, and treatments . Frontiers in Psychology, 10 (543), 1-24. Web.
Health Quality Ontario. (2017). Psychotherapy for major depressive disorder and generalized anxiety disorder: A health technology assessment. Ontario Health Technology Assessment Series, 17 (15), 1-167.
Lim, G. Y., Tam, W. W., Lu, Y., Ho, C. S., Zhang, M. W., & Ho, R. C. (2018). Prevalence of depression in the community from 30 countries between 1994 and 2014 . Scientific reports , 8 (1), 1-10. Web.
Lu, W. (2019). Adolescent depression: National trends, risk factors, and healthcare disparities . American Journal of Health Behavior, 43 (1), 181-194. Web.
McCart A, & Nesbit, J. (2020). S trategies to support employees with depression: Applying the Centers for Disease Control health scorecard . Journal of Depression and Anxiety, 9 (5), 1-4. Web.
Martínez-Paredes, J. F., & Jácome-Pérez, N. (2019). Depression in pregnancy . Revista Colombiana de Psiquiatría (English ed.) , 48 (1), 58-65. Web.
Moghtadaei, M., Yeganeh, A., Hosseinzadeh, N., Khazanchin, A., Moaiedfar, M., Jolfaei, A. G., & Nasiri, S. (2020). The Impact of depression, personality, and mental health on outcomes of total knee arthroplasty . Clinics in Orthopedic Surgery, 12 (4), 456-463. Web.
Olfson, M., Blanco, C., & Marcus, S. C. (2016). Treatment of adult depression in the United States . JAMA Internal Medicine, 176 (10), 1482-1491. Web.
Smith, C. A., Shewamene, Z., Galbally, M., Schmied, V., & Dahlen, H. (2019). The effect of complementary medicines and therapies on maternal anxiety and depression in pregnancy: A systematic review and meta-analysis . Journal of Affective Disorders , 245 , 428-439. Web.
Stark, A., Kaduszkiewicz, H., Stein, J., Maier, W., Heser, K., Weyerer, S., Werle, J., Wiese, B., Mamone, S., König, H., & Bock, J. O. (2018). A qualitative study on older primary care patients’ perspectives on depression and its treatments-potential barriers to and opportunities for managing depression . BMC Family Practice, 19 (1), 1-10. Web.
Vrijen, C., Hartman, C. A., & Oldehinkel, A. J. (2016). Slow identification of facial happiness in early adolescence predicts the onset of depression during eight years of follow-up. European Child & Adolescent Psychiatry, 25 (11), 1255-1266. Web.
Wang, J., Wu, X., Lai, W., Long, E., Zhang, X., Li, W.,… & Wang, D. (2017). Prevalence of depression and depressive symptoms among outpatients: a systematic review and meta-analysis . BMJ Open , 7 (8). Web.
Cite this paper
Select style
- Chicago (A-D)
- Chicago (N-B)
PsychologyWriting. (2024, January 24). Literature Review on Depression. https://psychologywriting.com/literature-review-on-depression/
"Literature Review on Depression." PsychologyWriting , 24 Jan. 2024, psychologywriting.com/literature-review-on-depression/.
PsychologyWriting . (2024) 'Literature Review on Depression'. 24 January.
PsychologyWriting . 2024. "Literature Review on Depression." January 24, 2024. https://psychologywriting.com/literature-review-on-depression/.
1. PsychologyWriting . "Literature Review on Depression." January 24, 2024. https://psychologywriting.com/literature-review-on-depression/.
Bibliography
PsychologyWriting . "Literature Review on Depression." January 24, 2024. https://psychologywriting.com/literature-review-on-depression/.
#Depression: Findings from a Literature Review of 10 Years of Social Media and Depression Research
- This person is not on ResearchGate, or hasn't claimed this research yet.

- University of Pittsburgh

Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- FUTURE GENER COMP SY

- Henrique S. Silva

- Laura A. Stockdale

- Lect Notes Comput Sci
- Christopher C. Frye
- Julissa Murrieta

- Lucia Lushi Chen
- Christopher H. K. Cheng
- CLIN SOC WORK J

- Gretchen Anstadt
- Bryan Casselman
- Kamala Ganesh
- NEW MEDIA SOC
- Jennifer Park
- Jada Hallman
- Jeff Hancock

- Pinar Ozturk
- Andrea Forte
- Kristen Purcell

- Clive E Adams

- MED CARE RES REV

- Marilyn F Downs
- Ezra Golberstein

- FIELD METHOD

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
- Introduction
- Conclusions
- Article Information
Contributing studies for clinically elevated depression symptoms are presented in order of largest to smallest prevalence rate. Square data markers represent prevalence rates, with lines around the marker indicating 95% CIs. The diamond data marker represents the overall effect size based on included studies.
Contributing studies for clinically elevated anxiety symptoms are presented in order of largest to smallest prevalence rate. Square data markers represent prevalence rates, with lines around the marker indicating 95% CIs. The diamond data marker represents the overall effect size based on included studies.
eTable 1. Example Search Strategy from Medline
eTable 2. Study Quality Evaluation Criteria
eTable 3. Quality Assessment of Studies Included
eTable 4. Sensitivity analysis excluding low quality studies (score=2) for moderators of the prevalence of clinically elevated depressive symptoms in children and adolescence during COVID-19
eTable 5. Sensitivity analysis excluding low quality studies (score=2) for moderators of the prevalence of clinically elevated anxiety symptoms in children and adolescence during COVID-19
eFigure 1. PRISMA diagram of review search strategy
eFigure 2. Funnel plot for studies included in the clinically elevated depressive symptoms
eFigure 3. Funnel plot for studies included in the clinically elevated anxiety symptoms
- Pediatric Depression and Anxiety Doubled During the Pandemic JAMA News From the JAMA Network October 5, 2021 Anita Slomski
- Guidelines Synopsis: Screening for Anxiety in Adolescent and Adult Women JAMA JAMA Clinical Guidelines Synopsis March 8, 2022 This JAMA Clinical Guidelines Synopsis summarizes the 2020 Women’s Preventive Services Initiative recommendation on screening for anxiety in adolescent and adult women. Tiffany I. Leung, MD, MPH; Adam S. Cifu, MD; Wei Wei Lee, MD, MPH
- Addressing the Global Crisis of Child and Adolescent Mental Health JAMA Pediatrics Editorial November 1, 2021 Tami D. Benton, MD; Rhonda C. Boyd, PhD; Wanjikũ F.M. Njoroge, MD
- Effect of the COVID-19 pandemic on Adolescents With Eating Disorders JAMA Pediatrics Comment & Response February 1, 2022 Thonmoy Dey, BSc; Zachariah John Mansell, BSc; Jasmin Ranu, BSc
See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
- CME & MOC
Racine N , McArthur BA , Cooke JE , Eirich R , Zhu J , Madigan S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19 : A Meta-analysis . JAMA Pediatr. 2021;175(11):1142–1150. doi:10.1001/jamapediatrics.2021.2482
Manage citations:
© 2024
- Permissions
Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19 : A Meta-analysis
- 1 Department of Psychology, University of Calgary, Calgary, Alberta, Canada
- 2 Alberta Children’s Hospital Research Institute, Calgary, Alberta, Canada
- Editorial Addressing the Global Crisis of Child and Adolescent Mental Health Tami D. Benton, MD; Rhonda C. Boyd, PhD; Wanjikũ F.M. Njoroge, MD JAMA Pediatrics
- News From the JAMA Network Pediatric Depression and Anxiety Doubled During the Pandemic Anita Slomski JAMA
- JAMA Clinical Guidelines Synopsis Guidelines Synopsis: Screening for Anxiety in Adolescent and Adult Women Tiffany I. Leung, MD, MPH; Adam S. Cifu, MD; Wei Wei Lee, MD, MPH JAMA
- Comment & Response Effect of the COVID-19 pandemic on Adolescents With Eating Disorders Thonmoy Dey, BSc; Zachariah John Mansell, BSc; Jasmin Ranu, BSc JAMA Pediatrics
Question What is the global prevalence of clinically elevated child and adolescent anxiety and depression symptoms during COVID-19?
Findings In this meta-analysis of 29 studies including 80 879 youth globally, the pooled prevalence estimates of clinically elevated child and adolescent depression and anxiety were 25.2% and 20.5%, respectively. The prevalence of depression and anxiety symptoms during COVID-19 have doubled, compared with prepandemic estimates, and moderator analyses revealed that prevalence rates were higher when collected later in the pandemic, in older adolescents, and in girls.
Meaning The global estimates of child and adolescent mental illness observed in the first year of the COVID-19 pandemic in this study indicate that the prevalence has significantly increased, remains high, and therefore warrants attention for mental health recovery planning.
Importance Emerging research suggests that the global prevalence of child and adolescent mental illness has increased considerably during COVID-19. However, substantial variability in prevalence rates have been reported across the literature.
Objective To ascertain more precise estimates of the global prevalence of child and adolescent clinically elevated depression and anxiety symptoms during COVID-19; to compare these rates with prepandemic estimates; and to examine whether demographic (eg, age, sex), geographical (ie, global region), or methodological (eg, pandemic data collection time point, informant of mental illness, study quality) factors explained variation in prevalence rates across studies.
Data Sources Four databases were searched (PsycInfo, Embase, MEDLINE, and Cochrane Central Register of Controlled Trials) from January 1, 2020, to February 16, 2021, and unpublished studies were searched in PsycArXiv on March 8, 2021, for studies reporting on child/adolescent depression and anxiety symptoms. The search strategy combined search terms from 3 themes: (1) mental illness (including depression and anxiety), (2) COVID-19, and (3) children and adolescents (age ≤18 years). For PsycArXiv , the key terms COVID-19 , mental health , and child/adolescent were used.
Study Selection Studies were included if they were published in English, had quantitative data, and reported prevalence of clinically elevated depression or anxiety in youth (age ≤18 years).
Data Extraction and Synthesis A total of 3094 nonduplicate titles/abstracts were retrieved, and 136 full-text articles were reviewed. Data were analyzed from March 8 to 22, 2021.
Main Outcomes and Measures Prevalence rates of clinically elevated depression and anxiety symptoms in youth.
Results Random-effect meta-analyses were conducted. Twenty-nine studies including 80 879 participants met full inclusion criteria. Pooled prevalence estimates of clinically elevated depression and anxiety symptoms were 25.2% (95% CI, 21.2%-29.7%) and 20.5% (95% CI, 17.2%-24.4%), respectively. Moderator analyses revealed that the prevalence of clinically elevated depression and anxiety symptoms were higher in studies collected later in the pandemic and in girls. Depression symptoms were higher in older children.
Conclusions and Relevance Pooled estimates obtained in the first year of the COVID-19 pandemic suggest that 1 in 4 youth globally are experiencing clinically elevated depression symptoms, while 1 in 5 youth are experiencing clinically elevated anxiety symptoms. These pooled estimates, which increased over time, are double of prepandemic estimates. An influx of mental health care utilization is expected, and allocation of resources to address child and adolescent mental health concerns are essential.
Prior to the COVID-19 pandemic, rates of clinically significant generalized anxiety and depressive symptoms in large youth cohorts were approximately 11.6% 1 and 12.9%, 2 respectively. Since COVID-19 was declared an international public health emergency, youth around the world have experienced dramatic disruptions to their everyday lives. 3 Youth are enduring pervasive social isolation and missed milestones, along with school closures, quarantine orders, increased family stress, and decreased peer interactions, all potential precipitants of psychological distress and mental health difficulties in youth. 4 - 7 Indeed, in both cross-sectional 8 , 9 and longitudinal studies 10 , 11 amassed to date, the prevalence of youth mental illness appears to have increased during the COVID-19 pandemic. 3 However, data collected vary considerably. Specifically, ranges from 2.2% 12 to 63.8% 13 and 1.8% 12 to 49.5% 13 for clinically elevated depression and anxiety symptoms, respectively. As governments and policy makers deploy and implement recovery plans, ascertaining precise estimates of the burden of mental illness for youth are urgently needed to inform service deployment and resource allocation.
Depression and generalized anxiety are 2 of the most common mental health concerns in youth. 14 Depressive symptoms, which include feelings of sadness, loss of interest and pleasure in activities, as well as disruption to regulatory functions such as sleep and appetite, 15 could be elevated during the pandemic as a result of social isolation due to school closures and physical distancing requirements. 6 Generalized anxiety symptoms in youth manifest as uncontrollable worry, fear, and hyperarousal. 15 Uncertainty, disruptions in daily routines, and concerns for the health and well-being of family and loved ones during the COVID-19 pandemic are likely associated with increases in generalized anxiety in youth. 16
When heterogeneity is observed across studies, as is the case with youth mental illness during COVID-19, it often points to the need to examine demographic, geographical, and methodological moderators. Moderator analyses can determine for whom and under what circumstances prevalence is higher vs lower. With regard to demographic factors, prevalence rates of mental illness both prior to and during the COVID-19 pandemic are differentially reported across child age and sex, with girls 17 , 18 and older children 17 , 19 being at greater risk for internalizing disorders. Studies have also shown that youth living in regions that experienced greater disease burden 2 and urban areas 20 had greater mental illness severity. Methodological characteristics of studies also have the potential to influence the estimated prevalence rates. For example, studies of poorer methodological quality may be more likely to overestimate prevalence rates. 21 The symptom reporter (ie, child vs parent) may also contribute to variability in the prevalence of mental illness across studies. Indeed, previous research prior to the pandemic has demonstrated that child and parent reports of internalizing symptoms vary, 22 with children/adolescents reporting more internalizing symptoms than parents. 23 Lastly, it is important to consider the role of data collection timing on potential prevalence rates. While feelings of stress and overwhelm may have been greater in the early months of the pandemic compared with later, 24 extended social isolation and school closures may have exerted mental health concerns.
Although a narrative systematic review of 6 studies early in the pandemic was conducted, 8 to our knowledge, no meta-analysis of prevalence rates of child and adolescent mental illness during the pandemic has been undertaken. In the current study, we conducted a meta-analysis of the global prevalence of clinically elevated symptoms of depression and anxiety (ie, exceeding a clinical cutoff score on a validated measure or falling in the moderate to severe symptom range of anxiety and depression) in youth during the first year of the COVID-19 pandemic. While research has documented a worsening of symptoms for children and youth with a wide range of anxiety disorders, 25 including social anxiety, 26 clinically elevated symptoms of generalized anxiety are the focus of the current meta-analysis. In addition to deriving pooled prevalence estimates, we examined demographic, geographical, and methodological factors that may explain between-study differences. Given that there have been several precipitants of psychological distress for youth during COVID-19, we hypothesized that pooled prevalence rates would be higher compared with prepandemic estimates. We also hypothesized that child mental illness would be higher among studies with older children, a higher percentage of female individuals, studies conducted later in the pandemic, and that higher-quality studies would have lower prevalence rates.
This systematic review was registered as a protocol with PROSPERO (CRD42020184903) and the Preferred Reporting Items for Systematic Reviews and Meta-analyses ( PRISMA ) reporting guideline was followed. 27 Ethics review was not required for the study. Electronic searches were conducted in collaboration with a health sciences librarian in PsycInfo, Cochrane Central Register of Controlled Trials (CENTRAL), Embase, and MEDLINE from inception to February 16, 2021. The search strategy (eTable 1 in the Supplement ) combined search terms from 3 themes: (1) mental illness (including depression and anxiety), (2) COVID-19, and (3) children and adolescents (age ≤18 years). Both database and subject headings were used to search keywords. As a result of the rapidly evolving nature of research during the COVID-19 pandemic, we also searched a repository of unpublished preprints, PsycArXiv . The key terms COVID-19 , mental health , and child/adolescent were used on March 8, 2021, and yielded 38 studies of which 1 met inclusion criteria.
The following inclusion criteria were applied: (1) sample was drawn from a general population; (2) proportion of individuals meeting clinical cutoff scores or falling in the moderate to severe symptom range of anxiety or depression as predetermined by validated self-report measures were provided; (3) data were collected during COVID-19; (4) participants were 18 years or younger; (5) study was empirical; and (6) studies were written in English. Samples of participants who may be affected differently from a mental health perspective during COVID-19 were excluded (eg, children with preexisting psychiatric diagnoses, children with chronic illnesses, children diagnosed or suspected of having COVID-19). We also excluded case studies and qualitative analyses.
Five (N.R., B.A.M., J.E.C., R.E. and J.Z.) authors used Covidence software (Covidence Inc) to review all abstracts and to determine if the study met criteria for inclusion. Twenty percent of abstracts reviewed for inclusion were double-coded, and the mean random agreement probability was 0.89; disagreements were resolved via consensus with the first author (N.R.). Two authors (N.R. and B.A.M.) reviewed full-text articles to determine if they met all inclusion criteria and the percent agreement was 0.80; discrepancies were resolved via consensus.
When studies met inclusion criteria, prevalence rates for anxiety and depression were extracted, as well as potential moderators. When more than 1 wave of data was provided, the wave with the largest sample size was selected. For 1 study in which both parent and youth reports were provided, 26 the youth report was selected, given research that they are the reliable informants of their own behavior. 28 The following moderators were extracted: (1) study quality (see the next subsection); (2) participant age (continuously as a mean); (3) sex (% female in a sample); (4) geographical region (eg, East Asia, Europe, North America), (5) informant (child, parent), (6) month in 2020 when data were collected (range, 1-12). Data from all studies were extracted by 1 coder and the first author (N.R.). Discrepancies were resolved via consensus.
Adapted from the National Institute of Health Quality Assessment Tool for Observation Cohort and Cross-Sectional Studies, a short 5-item questionnaire was used (eTable 2 in the Supplement ). 29 Studies were given a score of 0 (no) or 1 (yes) for each of the 5 criteria (validated measure; peer-reviewed, response rate ≥50%, objective assessment, sufficient exposure time) and summed to give a total score of 5. When information was unclear or not provided by the study authors, it was marked as 0 (no).
All included studies are from independent samples. Comprehensive Meta-Analysis version 3.0 (Biostat) software was used for data analysis. Pooled prevalence estimates with associated 95% confidence intervals around the estimate were computed. We weighted pooled prevalence estimates by the weight of the inverse of their variance, which gives greater weight to large sample sizes.
We used random-effects models to reflect the variations observed across studies and assessed between-study heterogeneity using the Q and I 2 statistics. Pooled prevalence is reported as an event rate (ie, 0.30) but interpreted as prevalence (ie, 30.0%). Significant Q statistics and I 2 values more than 75% suggest moderator analyses should be explored. 30 As recommended by Bornstein et al, 30 we examined categorical moderators when k of 10 or higher and a minimum cell size of k more than 3 were available. A P value of .05 was considered statistically significant. For continuous moderators, random-effect meta-regression analyses were conducted. Publication bias was examined using the Egger test 31 and by inspecting funnel plots for symmetry.
Our electronic search yielded 3094 nonduplicate records (eFigure 1 in the Supplement ). Based on the abstract review, a total of 136 full-text articles were retrieved to examine against inclusion criteria, and 29 nonoverlapping studies 10 , 12 , 13 , 17 , 19 , 20 , 26 , 32 - 53 met full inclusion criteria.
A total of 29 studies were included in the meta-analyses, of which 26 had youth symptom reports and 3 studies 39 , 42 , 48 had parent reports of child symptoms. As outlined in Table 1 , across all 29 studies, 80 879 participants were included, of which the mean (SD) perecentage of female individuals was 52.7% (12.3%), and the mean age was 13.0 years (range, 4.1-17.6 years). All studies provided binary reports of sex or gender. Sixteen studies (55.2%) were from East Asia, 4 were from Europe (13.8%), 6 were from North America (20.7%), 2 were from Central America and South America (6.9%), and 1 study was from the Middle East (3.4%). Eight studies (27.6%) reported having racial or ethnic minority participants with the mean across studies being 36.9%. Examining study quality, the mean score was 3.10 (range, 2-4; eTable 3 in the Supplement ).
The pooled prevalence from a random-effects meta-analysis of 26 studies revealed a pooled prevalence rate of 0.25 (95% CI, 0.21-0.30; Figure 1 ) or 25.2%. The funnel plot was symmetrical (eFigure 2 in the Supplement ); however, the Egger test was statistically significant (intercept, −9.5; 95% CI, −18.4 to −0.48; P = .02). The between-study heterogeneity statistic was significant ( Q = 4675.91; P < .001; I 2 = 99.47). Significant moderators are reported below, and all moderator analyses are presented in Table 2 .
As the number of months in the year increased, so too did the prevalence of depressive symptoms ( b = 0.26; 95% CI, 0.06-0.46). Prevalence rates were higher as child age increased ( b = 0.08; 95% CI, 0.01-0.15), and as the percentage of female individuals ( b = 0.03; 95% CI, 0.01-0.05) in samples increased. Sensitivity analyses removing low-quality studies were conducted (ie, scores of 2) 32 , 43 (eTable 4 in the Supplement ). Moderators remained significant, except for age, which became nonsignificant ( b = 0.06; 95% CI, −0.02 to 0.13; P = .14).
The overall pooled prevalence rate across 25 studies for elevated anxiety was 0.21 (95% CI, 0.17-0.24; Figure 2 ) or 20.5%. The funnel plot was symmetrical (eFigure 3 in the Supplement ) and the Egger test was nonsignificant (intercept, −6.24; 95% CI, −14.10 to 1.62; P = .06). The heterogeneity statistic was significant ( Q = 3300.17; P < .001; I 2 = 99.27). Significant moderators are reported below, and all moderator analyses are presented in Table 3 .
As the number of months in the year increased, so too did the prevalence of anxiety symptoms ( b = 0.27; 95% CI, 0.10-0.44). Prevalence rates of clinically elevated anxiety was higher as the percentage of female individuals in the sample increased ( b = 0.04; 95% CI, 0.01-0.07) and also higher in European countries ( k = 4; rate = 0.34; 95% CI, 0.23-0.46; P = .01) compared with East Asian countries ( k = 14; rate = 0.17; 95% CI, 0.13-0.21; P < .001). Lastly, the prevalence of clinically elevated anxiety was higher in studies deemed to have poorer quality ( k = 21; rate = 0.22; 95% CI, 0.18-0.27; P < .001) compared with studies with better study quality scores ( k = 4; rate = 0.12; 95% CI, 0.07-0.20; P < .001). Sensitivity analyses removing low quality studies (ie, scores of 2) 32 , 43 yielded the same pattern of results (eTable 5 in the Supplement ).
The current meta-analysis provides a timely estimate of clinically elevated depression and generalized anxiety symptoms globally among youth during the COVID-19 pandemic. Across 29 samples and 80 879 youth, the pooled prevalence of clinically elevated depression and anxiety symptoms was 25.2% and 20.5%, respectively. Thus, 1 in 4 youth globally are experiencing clinically elevated depression symptoms, while 1 in 5 youth are experiencing clinically elevated anxiety symptoms. A comparison of these findings to prepandemic estimates (12.9% for depression 2 and 11.6% for anxiety 1 ) suggests that youth mental health difficulties during the COVID-19 pandemic has likely doubled.
The COVID-19 pandemic, and its associated restrictions and consequences, appear to have taken a considerable toll on youth and their psychological well-being. Loss of peer interactions, social isolation, and reduced contact with buffering supports (eg, teachers, coaches) may have precipitated these increases. 3 In addition, schools are often a primary location for receiving psychological services, with 80% of children relying on school-based services to address their mental health needs. 54 For many children, these services were rendered unavailable owing to school closures.
As the month of data collection increased, rates of depression and anxiety increased correspondingly. One possibility is that ongoing social isolation, 6 family financial difficulties, 55 missed milestones, and school disruptions 3 are compounding over time for youth and having a cumulative association. However, longitudinal research supporting this possibility is currently scarce and urgently needed. A second possibility is that studies conducted in the earlier months of the pandemic (February to March 2020) 12 , 51 were more likely to be conducted in East Asia where self-reported prevalence of mental health symptoms tends to be lower. 56 Longitudinal trajectory research on youth well-being as the pandemic progresses and in pandemic recovery phases will be needed to confirm the long-term mental health implications of the COVID-19 pandemic on youth mental illness.
Prevalence rates for anxiety varied according to study quality, with lower-quality studies yielding higher prevalence rates. It is important to note that in sensitivity analyses removing lower-quality studies, other significant moderators (ie, child sex and data collection time point) remained significant. There has been a rapid proliferation of youth mental health research during the COVID-19 pandemic; however, the rapid execution of these studies has been criticized owing to the potential for some studies to sacrifice methodological quality for methodological rigor. 21 , 57 Additionally, several studies estimating prevalence rates of mental illness during the pandemic have used nonprobability or convenience samples, which increases the likelihood of bias in reporting. 21 Studies with representative samples and/or longitudinal follow-up studies that have the potential to demonstrate changes in mental health symptoms from before to after the pandemic should be prioritized in future research.
In line with previous research on mental illness in childhood and adolescence, 58 female sex was associated with both increased depressive and anxiety symptoms. Biological susceptibility, lower baseline self-esteem, a higher likelihood of having experienced interpersonal violence, and exposure to stress associated with gender inequity may all be contributing factors. 59 Higher rates of depression in older children were observed and may be due to puberty and hormonal changes 60 in addition to the added effects of social isolation and physical distancing on older children who particularly rely on socialization with peers. 6 , 61 However, age was not a significant moderator for prevalence rates of anxiety. Although older children may be more acutely aware of the stress of their parents and the implications of the current global pandemic, younger children may be able to recognize changes to their routine, both of which may contribute to similar rates of anxiety with different underlying mechanisms.
In terms of practice implications, a routine touch point for many youth is the family physician or pediatrician’s office. Within this context, it is critical to inquire about or screen for youth mental health difficulties. Emerging research 42 suggests that in families using more routines during COVID-19, lower child depression and conduct problems are observed. Thus, a tangible solution to help mitigate the adverse effects of COVID-19 on youth is working with children and families to implement consistent and predictable routines around schoolwork, sleep, screen use, and physical activity. Additional resources should be made available, and clinical referrals should be placed when children experience clinically elevated mental distress. At a policy level, research suggests that social isolation may contribute to and confer risk for mental health concerns. 4 , 5 As such, the closure of schools and recreational activities should be considered a last resort. 62 In addition, methods of delivering mental health resources widely to youth, such as group and individual telemental health services, need to be adapted to increase scalability, while also prioritizing equitable access across diverse populations. 63
There are some limitations to the current study. First, although the current meta-analysis includes global estimates of child and adolescent mental illness, it will be important to reexamine cross-regional differences once additional data from underrepresented countries are available. Second, most study designs were cross-sectional in nature, which precluded an examination of the long-term association of COVID-19 with child mental health over time. To determine whether clinically elevated symptoms are sustained, exacerbated, or mitigated, longitudinal studies with baseline estimates of anxiety and depression are needed. Third, few studies included racial or ethnic minority participants (27.6%), and no studies included gender-minority youth. Given that racial and ethnic minority 64 and gender-diverse youth 65 , 66 may be at increased risk for mental health difficulties during the pandemic, future work should include and focus on these groups. Finally, all studies used self- or parent-reported questionnaires to examine the prevalence of clinically elevated (ie, moderate to high) symptoms. Thus, studies using criterion standard assessments of child depression and anxiety disorders via diagnostic interviews or multimethod approaches may supplement current findings and provide further details on changes beyond generalized anxiety symptoms, such symptoms of social anxiety, separation anxiety, and panic.
Overall, this meta-analysis shows increased rates of clinically elevated anxiety and depression symptoms for youth during the COVID-19 pandemic. While this meta-analysis supports an urgent need for intervention and recovery efforts aimed at improving child and adolescent well-being, it also highlights that individual differences need to be considered when determining targets for intervention (eg, age, sex, exposure to COVID-19 stressors). Research on the long-term effect of the COVID-19 pandemic on mental health, including studies with pre– to post–COVID-19 measurement, is needed to augment understanding of the implications of this crisis on the mental health trajectories of today’s children and youth.
Corresponding Author: Sheri Madigan, PhD, RPsych, Department of Psychology University of Calgary, Calgary, AB T2N 1N4, Canada ( [email protected] ).
Accepted for Publication: May 19, 2021.
Published Online: August 9, 2021. doi:10.1001/jamapediatrics.2021.2482
Author Contributions: Drs Racine and Madigan had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Racine, Madigan.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Racine, McArthur, Eirich, Zhu, Madigan.
Critical revision of the manuscript for important intellectual content: Racine, Cooke, Eirich, Madigan.
Statistical analysis: Racine, McArthur.
Administrative, technical, or material support: Madigan.
Supervision: Racine, Madigan.
Conflict of Interest Disclosures: Dr Racine reported fellowship support from Alberta Innovates. Dr McArthur reported a postdoctoral fellowship award from the Alberta Children’s Hospital Research Institute. Ms Cooke reported graduate scholarship support from Vanier Canada and Alberta Innovates Health Solutions outside the submitted work. Ms Eirich reported graduate scholarship support from the Social Science and Humanities Research Council. No other disclosures were reported.
Additional Contributions: We acknowledge Nicole Dunnewold, MLIS (Research and Learning Librarian, Health Sciences Library, University of Calgary), for her assistance with the search strategy, for which they were not compensated outside of their salary. We also acknowledge the contribution of members of the Determinants of Child Development Laboratory at the University of Calgary, in particular, Julianna Watt, BA, and Katarina Padilla, BSc, for their contribution to data extraction, for which they were paid as research assistants.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
The website will be down for maintenance from 6:00 a.m. to noon CDT on Sunday, June 30.

HEATHER KOVICH, MD, WILLIAM KIM, MS, MD, AND ANTHONY M. QUASTE, PharmD, USPHS
Am Fam Physician. 2023;107(2):173-181
Related editorial: Comparing Clinical Guidelines for the Management of Major Depressive Disorder
Patient information: See related handout on treating depression with medicine .
Author disclosure: No relevant financial relationships.
The prevalence of depression and the use of antidepressant medications have risen steadily in the United States over the past three decades. Antidepressants are the most commonly prescribed medications for U.S. adults 20 to 59 years of age. Second-generation antidepressants (e.g., selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, serotonin modulators, atypical antidepressants) are first-line therapy for depression. Psychotherapy, including cognitive behavior therapy and other types of individual and group therapy, is also a first-line treatment. The combination of medication and psychotherapy is preferred for severe depression. Treatment history, comorbidities, costs, and risk of adverse effects should be considered when choosing an antidepressant medication. Although many patients use antidepressants indefinitely, few studies have examined safety and effectiveness beyond two years. There is an increased risk of relapse or recurrence of depressive symptoms when an antidepressant is discontinued, compared with continued use. Gradually tapering the dosage while concurrently providing cognitive behavior therapy can decrease this risk. High-quality evidence on antidepressant use in pregnancy is lacking. Depression and use of antidepressants are both associated with preterm birth.
The use of antidepressant medications in the United States has increased fivefold since the introduction of selective serotonin reuptake inhibitors (SSRIs) in the late 1980s. 1 , 2 Between 2015 and 2018, the percentage of U.S. adults who reported taking an antidepressant medication in the past 30 days was 13.2%, compared with 2.4% between 1988 and 1994. 1 , 2
| Between 2015 and 2018, the percentage of U.S. adults who reported taking an antidepressant medication in the past 30 days was 13.2%, compared with 2.4% between 1988 and 1994. |
| Modest evidence shows that escitalopram, mirtazapine, paroxetine, venlafaxine, and amitriptyline are the most effective antidepressants for reducing acute depressive symptoms by greater than 50% at eight weeks. |
| A 2021 network meta-analysis demonstrated a low risk of ventricular arrhythmia or sudden cardiac death in those taking selective serotonin reuptake inhibitors, serotonin-norepinephrine reuptake inhibitors, or tricyclic antidepressants. |
| Typical symptoms of antidepressant discontinuation syndrome can be described using the FINISH mnemonic (flulike symptoms, insomnia, nausea, imbalance, sensory disturbances, hyperarousal). |
| – | Network meta-analysis, systematic reviews, clinical practice guidelines | |
| , , | Clinical practice guidelines, systematic reviews | |
| – | Double-blind randomized controlled trial, systematic reviews, meta-analyses | |
| Two studies included in larger meta-analysis | ||
| Systematic reviews of six clinical trials (n = 11,869) showing decrease in depressive symptoms in patients who are screened, even in the absence of follow-up measures | ||
| Clinical practice guidelines |
Antidepressants are the most commonly prescribed medications for U.S. adults 20 to 59 years of age. 3 Rates of depression and suicide have increased, primarily among those younger than 25 years. 4 , 5 The percentage of adults 18 to 25 years of age reporting a major depressive episode in the past year doubled from 8.8% in 2005 to 17% in 2020. During the same period, rates among adults 26 years and older increased only slightly from 6.2% to 7.1%. 6 , 7
The definition of a major depressive episode is based on the Diagnostic and Statistical Manual of Mental Disorders , 5th ed., criteria for major depressive disorder. 6 , 8 Five or more depressive symptoms must be present for at least two weeks, cause distress or functional impairment, and not be due to another medical or psychiatric condition. Symptoms include depressed mood, anhedonia, changes in weight or sleep patterns, fatigue, psychomotor agitation or retardation, feelings of worthlessness or guilt, impaired concentration, and recurrent thoughts of death. 6 , 8 Clinical trials of antidepressants often use major depressive episode as an inclusion criterion. Although most patients with clinician-identified depression do not meet diagnostic criteria for a major depressive episode, many are prescribed antidepressants. 9
Second-generation antidepressants are the most common medications used to treat depression in the United States. 10 These include SSRIs (e.g., escitalopram, paroxetine), serotonin-norepinephrine reuptake inhibitors (SNRIs; e.g., duloxetine [Cymbalta], venlafaxine), serotonin modulators (e.g., nefazodone, trazodone), and atypical antidepressants (e.g., bupropion, mirtazapine).
Effectiveness
Despite thousands of clinical trials, the effectiveness of antidepressants is not well established. High-quality reviews of randomized controlled studies show a statistically significant improvement in depression with use of antidepressant medications. 11 , 12 A 2016 systematic review showed that the number needed to treat for response to treatment or remission is 9 for tricyclic antidepressants, 7 for SSRIs, and 6 for venlafaxine. 11 Outcomes of other studies challenge these conclusions, with minimal difference in symptoms between placebo and antidepressants, publication bias favoring effectiveness, and pharmaceutical industry sponsorship of most clinical trials. 11 , 13 , 14 A recent national survey of adults with depression revealed that those who used antidepressants had no improvement in health-related quality of life at two years of follow-up compared with those who did not use antidepressants. 15
Psychotherapy (e.g., behavior therapy, cognitive therapy, cognitive behavior therapy, interpersonal psychotherapy, psychodynamic therapy, supportive therapy) is also a first-line treatment for depression. 16 , 17 The effectiveness of psychotherapy is similar to that of antidepressants in the primary care setting (relative risk [RR] = 1.03; 95% CI, 0.88 to 1.22). 18 Evidence for cognitive behavior therapy is more robust than for other types of therapy. 10 The combination of psychotherapy and pharmacotherapy may be more effective than either treatment alone for moderate or severe depression and may reduce risk of relapse and recurrence. 17 , 19 , 20
Selection of Initial Depression Therapy
Guidelines from the United Kingdom's National Institute for Health and Care Excellence recommend against routinely offering medication for mild to moderate depression (defined as a Patient Health Questionnaire-9 score of less than 16). If the patient prefers medication, SSRIs are recommended. Active monitoring, group exercise, and several types of individual and group therapy are recommended as management options. For more severe depression, a combination of individual cognitive behavior therapy and an antidepressant (SSRI or SNRI) is recommended. 17
Shared decision-making should be used when choosing an initial treatment. Prior treatment and response, comorbidities, costs, and risk of adverse effects should be considered. Pharmacogenetic testing, intended to tailor therapy to an individual's genetic variants, has not shown consistent benefit in outcomes or cost-effectiveness. 21
For the general adult population, treatment should start with a second-generation antidepressant or psychotherapy. 10 , 16 , 17 If an antidepressant is selected, modest evidence shows that escitalopram, mirtazapine, paroxetine, venlafaxine, and amitriptyline are most effective in reducing depressive symptoms by greater than 50% at eight weeks (odds ratio = 1.19 to 1.96). 12
Adverse Effects
Nausea and vomiting were the most commonly reported symptoms leading to antidepressant discontinuation during clinical trials. Patients taking SNRIs have a higher incidence of nausea and vomiting than those taking SSRIs. 22 Other common adverse effects across drug classes include sexual adverse effects and weight gain, although these are less likely with bupropion. 22 , 23
Despite concerns about increased risk of cardiac arrhythmia with SSRIs, a 2021 network meta-analysis demonstrated a low risk of ventricular arrhythmia or sudden cardiac death in those taking SSRIs, SNRIs, or tricyclic antidepressants. 24 QT prolongation can occur with these drug classes; therefore, caution should be used when combining them with other medications that cause QT prolongation (e.g., antiemetics, antiarrhythmics, neuroleptics). Bupropion has the lowest risk of QT prolongation in patients at high risk of ventricular arrhythmias. Because of its side effect profile and potential for beneficial antiplatelet activity, sertraline may be preferred for those with ischemic heart disease. 25
Long-term adverse effects should also be considered when prescribing antidepressants. Limited-quality evidence, including a 12-year cohort study, found a correlation between SSRI use and falls (hazard ratio [HR] = 1.48; 95% CI, 1.39 to 1.59); fractures (HR = 1.30; 95% CI, 1.21 to 1.39); and all-cause mortality (HR = 1.38; 95% CI, 1.26 to 1.51). 26
In a review of 21 antidepressants, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine (Trintellix) were most tolerated with less discontinuation of treatment (odds ratio = 0.43 to 0.77). 12 Adverse effects associated with antidepressants are summarized in Table 1 . 23 , 27 – 36
| Gastrointestinal bleeding | Odds ratio = 1.55 (95% CI, 1.35 to 1.78) | SSRIs, especially when used with nonsteroidal anti-inflammatory drugs or antiplatelet drugs; risk mitigated by acid-suppressing medications | Anytime during treatment | Meta-analysis |
| Hepatotoxicity | Incidence = 0.5% to 3% | Nefazodone, bupropion, duloxetine (Cymbalta), trazodone | Anytime during treatment | Literature review |
| Hyponatremia (sodium < 130 mEq per L [130 mmol per L]) | Incidence = 0.06% to 2.6% | SSRIs, SNRIs, mirtazapine, TCAs | Within the first month | Literature review |
| Osteoporosis and fractures | Hazard ratio = 1.88 (95% CI, 1.48 to 2.39) for fragility fracture | SSRIs, SNRIs | Over 10 years | Prospective cohort |
| QT prolongation | Dose dependent | Citalopram, escitalopram, amitriptyline U.S. Food and Drug Administration warns against exceeding recommended dose of citalopram (≤ 60 years of age, 40 mg per day; > 60 years, 20 mg per day) | At initiation Typically dependent on coexisting risk factors | Cross-sectional retrospective studies , |
| Sexual adverse effects | Weighted mean incidence = 40% (95% CI, 28.3 to 52.6) across observational studies | Trend toward increased risk with escitalopram and paroxetine; decreased risk with bupropion | Within the first week | Meta-analysis , |
| Suicidality | Age-related risk < 18 years: odds ratio = 2.39 (95% CI, 1.31 to 4.3) ≥ 18 years: odds ratio = 0.81 (95% CI, 0.51 to 1.2) | Duloxetine, fluoxetine, paroxetine, sertraline, venlafaxine | Not defined | Systematic review, meta-analysis of clinical reports |
| Weight gain (> 5%) | Rate ratio 1.21 (95% CI, 1.20 to 1.23) for SSRIs 1.17 (95% CI, 1.13 to 1.21) for SNRIs 1.16 (95% CI, 1.14 to 1.18) for TCAs | SSRIs, SNRIs, TCAs Decreased risk with bupropion | Over 10 years (highest risk in first two years) | Population-based cohort study, systematic review , |
Duration of Treatment
The treatment of depression is often described in three phases. The acute phase of six to 12 weeks is intended to induce remission of symptoms and aid in recovery of function. The continuation phase of four to nine months is aimed at reducing relapse (return of symptoms). The maintenance phase is intended to prevent recurrence (a new episode of depression) after one year of treatment. 10 , 37
Although up to 75% of patients discontinue antidepressant use within six months, others continue indefinitely. 38 The increase in antidepressant use over the past 30 years is largely due to longer treatment duration. 39 The longer patients are in the maintenance phase, the less often treatment is reviewed by their primary care physicians. 40 Few studies have evaluated safety and effectiveness beyond two years. 41
Whenever antidepressants are discontinued, there is an increased risk of relapse or recurrence, with the highest risk in the first six months. 42 – 44 Compared with antidepressants, psychotherapy may have a longer duration of benefit and lower rate of relapse after discontinuation. 15
U.S. guidelines do not specify a duration of treatment for antidepressants. 10 , 16 Canadian guidelines recommend at least six months of treatment and two years or more for those at higher risk of relapse. 45 Because each episode of depression adds to a patient's risk of future episodes, indefinite maintenance treatment is often recommended for patients with three or more episodes of depression. 37
Discontinuation
The Diagnostic and Statistical Manual of Mental Disorders , 5th ed., defines antidepressant discontinuation syndrome as “a set of symptoms that can occur after an abrupt cessation (or marked reduction in dose) of an antidepressant medication that was taken continuously for at least one month.” 8 Effects typically manifest within two to four days and can last for several months. 46 Typical symptoms can be described using the FINISH mnemonic (flulike symptoms, insomnia, nausea, imbalance, sensory disturbances, hyperarousal). 47 Patients should be counseled on symptoms that may occur with abrupt cessation of treatment. 48
Symptoms of antidepressant discontinuation syndrome can be difficult to distinguish from relapse and recurrence. The prevalence of these symptoms varies, but some reviews have found that 50% of patients are affected. 46 Regardless of pharmacologic mechanism, the risk of antidepressant discontinuation syndrome is higher for drugs with a shorter half-life ( Table 2 ) . 49 , 50
| Bupropion | + |
| Mirtazapine | + |
| Desvenlafaxine (Pristiq) | +++ |
| Venlafaxine | +++ |
| Duloxetine (Cymbalta) | ++ |
| Milnacipran | + |
| Fluvoxamine | +++ |
| Paroxetine | +++ |
| Citalopram | ++ |
| Escitalopram | ++ |
| Sertraline | ++ |
| Fluoxetine | + |
| Trazodone | ++ |
| Vortioxetine (Trintellix) | ++ |
| Vilazodone (Viibryd) | + |
| Imipramine | +++ |
| Nortriptyline | +++ |
| Amitriptyline | ++ |
| Clomipramine | ++ |
| Desipramine | ++ |
| Doxepin | ++ |
Despite a lack of head-to-head trials, research shows that a slow medication taper of at least 14 days is best practice; a taper of several months may be needed. 51 – 54 Tapering strategies are detailed in Table 3 . 51 – 53 A dose taper of approximately 25% every four weeks and a faster taper of 12.5% every two weeks are both reasonable strategies. A gradual taper has been shown to result in as few as 5% of patients experiencing discontinuation symptoms. 55 Use of cognitive behavior therapy during the medication taper may help prevent relapse or recurrence. 56
| 10% reduction per week | Reduce dose every four weeks to match 10% reduction in serotonin transporter occupancy | Citalopram: 40 mg for four weeks 20 mg for four weeks 19 mg for four weeks 9.1 mg for four weeks 5.4 mg for four weeks 3.4 mg for four weeks 2.3 mg for four weeks 1.5 mg for four weeks 0.8 mg for four weeks 0.37 mg for four weeks | Formulated using pharmacokinetic data but difficult to precisely implement | ||
| Three- to four-month taper | Reduce dose by 25% every four weeks or by 12.5% every two weeks | Citalopram: 40 mg for four weeks 30 mg for four weeks 20 mg for four weeks 15 mg for four weeks 10 mg for four weeks 7.5 mg for four weeks 5 mg for four weeks 2.5 mg for four weeks | Easier to accomplish in real-world practice, but linear dose decrease may still result in antidepressant discontinuation syndrome | ||
| Cross taper | Slowly decrease dose of the current medication while increasing dose of the new medication | Citalopram (current medication, 40-mg starting dose): 30 mg for four weeks 20 mg for four weeks 15 mg for four weeks 10 mg for four weeks 7.5 mg for four weeks 5 mg for four weeks 2.5 mg for four weeks | Sertraline (new medication): 12.5 mg for four weeks 18.75 mg for four weeks 25 mg for four weeks 37.5 mg for four weeks 50 mg for four weeks 75 mg for four weeks 100 mg for four weeks | Exposure to multiple serotonergic agents has inherent risks Potential for cytochrome P450– mediated drug reactions depending on drug choice Increased pill burden and financial strain for patients | |
| Direct switch | Start a new medication immediately after discontinuing the current one | Discontinue citalopram, 20 mg | Initiate sertraline, 50 mg | May be difficult to determine if patient-reported adverse effects are due to the new agent or antidepressant discontinuation syndrome | |
| Moderate switch | Current medication is tapered down, followed by a washout period of two or three days New medication is initiated at a conservative dose, then increased | Citalopram (current medication): 20 mg for four weeks 15 mg for four weeks 10 mg for four weeks 7.5 mg for four weeks 5 mg for four weeks 2.5 mg for four weeks Discontinue for two- to three-day washout period Start sertraline: 25 mg for four weeks 37.5 mg for four weeks 50 mg for four weeks | Potential for antidepressant discontinuation syndrome due to drug-free period More time-consuming but considered to be safer | ||
| Conservative switch | Current medication is tapered down, followed by a washout period of four or five half-lives New medication is initiated at a conservative dose, then increased | Same as moderate switch but with longer washout period (seven days for most drugs, except those with long half-lives [e.g., fluoxetine]) | Potential for antidepressant discontinuation syndrome due to drug-free period Patients must wait longer for treatment benefit from new medication | ||
Special Populations
Pregnant patients.
Approximately 12% of patients in the perinatal period meet criteria for major depressive disorder. 57 Patients with untreated depression during pregnancy have a higher incidence of preterm birth and low-birth-weight infants compared with those without depression. 58 Treatment of depression has not been shown to improve these outcomes, and SSRIs may be independently associated with preterm birth. 59 , 60
Screening pregnant and postpartum patients for depression is associated with a 2% to 9% reduction in absolute risk of depression at three to five months, with or without treatment. 61 The U.S. Preventive Services Task Force recommends that clinicians provide or refer pregnant and postpartum patients who are at increased risk of perinatal depression to counseling interventions. 62
For patients taking antidepressants before pregnancy, discontinuation is more likely to lead to relapse when depression is severe or recurrent. A meta-analysis showed that discontinuation of antidepressants in patients with mild to moderate depression is not significantly associated with relapse. 63 Patients should continue their antidepressant when, through shared decision-making, the risk of relapse is determined to be greater than the risk of rare neonatal complications.
Cohort studies have inconsistently shown a small correlation between first-trimester SSRI use and cardiac malformations (RR = 1.24; 95% CI, 1.11 to 1.37). 64 – 66 SSRI use during the third trimester may increase the risk of newborn respiratory distress, tremors, and admission to the neonatal intensive care unit. 67 – 69 Discontinuation of SSRIs in the third trimester does not improve these outcomes. 70 There are no data on long-term neurocognitive effects.
A U.S. Food and Drug Administration advisory on SSRI use during pregnancy and the risk of persistent pulmonary hypertension in newborns cites conflicting findings; a causal relationship is unclear. 71 A systematic review and meta-analysis found a slightly increased risk of persistent pulmonary hypertension in newborns with prenatal exposure to SSRIs and SNRIs (number needed to harm = 1,000). 72

BREASTFEEDING PATIENTS
Antidepressants transfer into breast milk in low concentrations. This transfer is thought to be lower for paroxetine and sertraline than other antidepressants, producing undetectable concentrations in infant plasma. Fluoxetine and venlafaxine produce the highest infant plasma concentrations. Potential adverse effects in infants exposed to SSRIs via breast milk have been documented only in case reports, most commonly with fluoxetine and citalopram. The effects are nonspecific and include irritability and decreased feeding. Overall, there is little evidence to support a causal link between antidepressant use in breastfeeding patients and adverse effects in their infants. 73
OLDER ADULTS
Approximately 50% of patients older than 65 years who have depression report at least a 50% improvement in symptoms with antidepressant use. 74 Although prior studies showed no difference in the effectiveness of antidepressants in older patients, a 2019 network meta-analysis found that response rates are significantly higher with quetiapine (RR = 2.09) and duloxetine (RR = 1.83) in this population compared with placebo. 75 Quetiapine includes a U.S. Food and Drug Administration boxed warning due to increased mortality risk in older patients with dementia-related psychosis. Some drugs are associated with higher rates of remission compared with placebo: quetiapine (RR = 2.38), mirtazapine (RR = 1.90), and duloxetine (RR = 1.52). In older patients, fall risk should be evaluated and steps taken to mitigate the risk because untreated depression and antidepressant use can both contribute to falls. 76
Because older adults are at greater risk of adverse drug reactions, initiating treatment at approximately one-half of the usual adult starting dose is often recommended. Guidelines recommend sertraline, duloxetine, or escitalopram as good first-line options for older patients. 77 Bupropion, mirtazapine, and venlafaxine are also considered appropriate because of their favorable side effect profiles. Paroxetine is associated with more anticholinergic effects, and fluoxetine has a greater risk of agitation and overstimulation; neither should be used in older adults. 77 Before initiating SSRIs and SNRIs in older adults, clinicians should screen for a history of hyponatremia and measure serum sodium level two to four weeks after initiating therapy. 77
This article updates previous articles on this topic by Kovich and DeJong 78 ; Adams, et al. 79 ; and Warner, et al. 80
Data Sources: PubMed searches were completed using key terms such as depression, antidepressant, and antidepressant discontinuation and specific classes of antidepressant medications (e.g., selective serotonin reuptake inhibitor). Additional terms were added to further refine results. For example, after an initial search generated a list of common antidepressant adverse effects, each effect was searched separately. The search included meta-analyses, randomized controlled trials, systematic reviews, and clinical trials. The U.S. Preventive Services Task Force recommendations were referenced, and citations from relevant recommendations were examined. Essential Evidence Plus and the Cochrane database were also searched. Search dates: February through December 2022.
U.S. Department of Health and Human Services. National Centers for Health Statistics. Health, United States, 2013: with special feature on prescription drugs. Accessed April 21, 2022. http://www.cdc.gov/nchs/data/hus/hus13.pdf
Brody DJ, Gu Q. Antidepressant use among adults: United States, 2015–2018. NCHS Data Brief. 2020(377):1-8.
Martin CB, Hales CM, Gu Q, et al. Prescription drug use in the United States, 2015–2016. NCHS Data Brief. 2019(334):1-8.
Twenge JM, Cooper AB, Joiner TE, et al. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Abnorm Psychol. 2019;128(3):185-199.
Hedegaard H, Curtin SC, Warner M. Suicide mortality in the United States, 1999–2019. NCHS Data Brief. 2021(398):1-8.
U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. National Survey on Drug Use and Health. 2020 NSDUH detailed tables. January 11, 2022. Accessed April 21, 2022. https://www.samhsa.gov/data/report/2020-nsduh-detailed-tables
Weinberger AH, Gbedemah M, Martinez AM, et al. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol Med. 2018;48(8):1308-1315.
Diagnostic and Statistical Manual of Mental Disorders . 5th ed. American Psychiatric Association; 2014.
Mojtabai R. Clinician-identified depression in community settings: concordance with structured-interview diagnoses. Psychother Psychosom. 2013;82(3):161-169.
Qaseem A, Barry MJ, Kansagara D. Nonpharmacologic versus pharmacologic treatment of adult patients with major depressive disorder: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;164(5):350-359.
Arroll B, Chin WY, Martis W, et al. Antidepressants for treatment of depression in primary care: a systematic review and meta-analysis. J Prim Health Care. 2016;8(4):325-334.
Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357-1366.
Stone M, Kalaria S, Richardville K, et al. Components and trends in treatment effects in randomized placebo-controlled trials in major depressive disorder from 1979–2016. Poster presented at: American Society of Clinical Psychopharmacology Annual Conference; May 2018; Miami, FL.
Turner EH, Cipriani A, Furukawa TA, et al. Selective publication of anti-depressant trials and its influence on apparent efficacy: updated comparisons and meta-analyses of newer versus older trials. PLoS Med. 2022;19(1):e1003886.
Almohammed OA, Alsalem AA, Almangour AA, et al. Antidepressants and health-related quality of life (HRQoL) for patients with depression: analysis of the medical expenditure panel survey from the United States. PLoS One. 2022;17(4):e0265928.
American Psychological Association. Clinical practice guideline for the treatment of depression across three age cohorts. February 2019. Accessed April 21, 2022. https://www.apa.org/depression-guideline
National Institute for Health and Care Excellence. Depression in adults: treatment and management. June 29, 2022. Accessed August 12, 2022. https://www.nice.org.uk/guidance/ng222
Cuijpers P, Oud M, Karyotaki E, et al. Psychologic treatment of depression compared with pharmacotherapy and combined treatment in primary care: a network meta-analysis. Ann Fam Med. 2021;19(3):262-270.
Cuijpers P, Noma H, Karyotaki E, et al. A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry. 2020;19(1):92-107.
Guidi J, Fava GA. Sequential combination of pharmacotherapy and psychotherapy in major depressive disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2021;78(3):261-269.
Li KX, Loshak H. Pharmacogenomic testing in depression: a review of clinical effectiveness, cost-effectiveness, and guidelines. Canadian Agency for Drugs and Technologies in Health. January 31, 2020. Updated February 18, 2020. Accessed December 5, 2022. https://www.cadth.ca/pharmacogenomic-testing-depression-review-clinical-effectiveness-cost-effectiveness-and-guidelines
Gartlehner G, Gaynes BN, Hansen RA, et al. Comparative benefits and harms of second-generation antidepressants: background paper for the American College of Physicians. Ann Intern Med. 2008;149(10):734-750.
Alonso-Pedrero L, Bes-Rastrollo M, Marti A. Effects of antidepressant and antipsychotic use on weight gain: a systematic review. Obes Rev. 2019;20(12):1680-1690.
Prasitlumkum N, Cheungpasitporn W, Tokavanich N, et al. Antidepressants and risk of sudden cardiac death: a network meta-analysis and systematic review. Med Sci (Basel). 2021;9(2):26.
Teply RM, Packard KA, White ND, et al. Treatment of depression in patients with concomitant cardiac disease. Prog Cardiovasc Dis. 2016;58(5):514-528.
Coupland C, Hill T, Morriss R, et al. Antidepressant use and risk of adverse outcomes in people aged 20–64 years: cohort study using a primary care database. BMC Med. 2018;16(1):36.
Jiang HY, Chen HZ, Hu XJ, et al. Use of selective serotonin reuptake inhibitors and risk of upper gastrointestinal bleeding: a systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2015;13(1):42-50.e3.
Voican CS, Corruble E, Naveau S, et al. Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry. 2014;171(4):404-415.
De Picker L, Van Den Eede F, Dumont G, et al. Antidepressants and the risk of hyponatremia: a class-by-class review of literature. Psychosomatics. 2014;55(6):536-547.
Moura C, Bernatsky S, Abrahamowicz M, et al. Antidepressant use and 10-year incident fracture risk: the population-based Canadian Multicentre Osteoporosis Study (CaMoS). Osteoporos Int. 2014;25(5):1473-1481.
U.S. Food and Drug Administration drug safety communication: revised recommendations for Celexa (citalopram hydrobromide) related to a potential risk of abnormal heart rhythms with high doses. March 28, 2012. Accessed April 21, 2022. https://www.fda.gov/Drugs/DrugSafety/ucm297391.htm
Castro VM, Clements CC, Murphy SN, et al. QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ. 2013;346:f288.
Reichenpfader U, Gartlehner G, Morgan LC, et al. Sexual dysfunction associated with second-generation antidepressants in patients with major depressive disorder: results from a systematic review with network meta-analysis. Drug Saf. 2014;37(1):19-31.
Worthington JJ III, Peters PM. Treatment of antidepressant-induced sexual dysfunction. Drugs Today (Barc). 2003;39(11):887-896.
Sharma T, Guski LS, Freund N, et al. Suicidality and aggression during antidepressant treatment: systematic review and meta-analyses based on clinical study reports. BMJ. 2016;352:i65.
Gafoor R, Booth HP, Gulliford MC. Antidepressant utilisation and incidence of weight gain during 10 years' follow-up: population based cohort study. BMJ. 2018;361:k1951.
Gelenberg AJ, Freeman MP, Markowitz JC, et al. Practice guideline for the treatment of patients with major depressive disorder. Third edition. American Psychiatric Association. October 2010. Accessed August 10, 2022. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf
Jung WY, Jang SH, Kim SG, et al. Times to discontinue antidepressants over 6 months in patients with major depressive disorder. Psychiatry Investig. 2016;13(4):440-446.
McCrea RL, Sammon CJ, Nazareth I, et al. Initiation and duration of selective serotonin reuptake inhibitor prescribing over time: UK cohort study. Br J Psychiatry. 2016;209(5):421-426.
Sinclair JE, Aucott LS, Lawton K, et al. The monitoring of longer term prescriptions of antidepressants: observational study in a primary care setting. Fam Pract. 2014;31(4):419-426.
- Sim K, Lau WK, Sim J, et al. Prevention of relapse and recurrence in adults with major depressive disorder: systematic review and meta-analyses of controlled trials [published correction appears in Int J Neuropsychopharmacol . 2016;19(10);pyw031]. Int J Neuropsychopharmacol. 2015;19(2):pyv076.
Lewis G, Marston L, Duffy L, et al. Maintenance or discontinuation of antidepressants in primary care. N Engl J Med. 2021;385(14):1257-1267.
Machmutow K, Meister R, Jansen A, et al. Comparative effectiveness of continuation and maintenance treatments for persistent depressive disorder in adults. Cochrane Database Syst Rev. 2019(5):CD012855.
Baldessarini RJ, Lau WK, Sim J, et al. Duration of initial antidepressant treatment and subsequent relapse of major depression. J Clin Psychopharmacol. 2015;35(1):75-76.
- Kennedy SH, Lam RW, McIntyre RS, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: section 3. Pharmacological treatments [published correction appears in Can J Psychiatry . 2017;62(5):356]. Can J Psychiatry. 2016;61(9):540-560.
- Davies J, Read J. A systematic review into the incidence, severity and duration of antidepressant withdrawal effects: are guidelines evidence-based? Addict Behav. 2019;97:111-121.
Bhat V, Kennedy SH. Recognition and management of antidepressant discontinuation syndrome. J Psychiatry Neurosci. 2017;42(4):E7-E8.
Horowitz MA, Taylor D. Tapering of SSRI treatment to mitigate withdrawal symptoms. Lancet Psychiatry. 2019;6(6):538-546.
Henssler J, Heinz A, Brandt L, et al. Antidepressant withdrawal and rebound phenomena. Dtsch Arztebl Int. 2019;116(20):355-361.
Zwiebel SJ, Viguera AC. Discontinuing antidepressants: pearls and pitfalls. Cleve Clin J Med. 2022;89(1):18-26.
Fava GA, Benasi G, Lucente M, et al. Withdrawal symptoms after serotonin-noradrenaline reuptake inhibitor discontinuation: systematic review. Psychother Psychosom. 2018;87(4):195-203.
- Tint A, Haddad PM, Anderson IM. The effect of rate of antidepressant tapering on the incidence of discontinuation symptoms: a randomised study [published correction appears in J Psychopharmacol . 2009;23(8):1006]. J Psychopharmacol. 2008;22(3):330-332.
Phelps J. Tapering antidepressants: is 3 months slow enough?. Med Hypotheses. 2011;77(6):1006-1008.
Jefferson JW. Strategies for switching antidepressants to achieve maximum efficacy. J Clin Psychiatry. 2008;69(suppl E1):14-18.
Himei A, Okamura T. Discontinuation syndrome associated with paroxetine in depressed patients: a retrospective analysis of factors involved in the occurrence of the syndrome. CNS Drugs. 2006;20(8):665-672.
Maund E, Stuart B, Moore M, et al. Managing antidepressant discontinuation: a systematic review. Ann Fam Med. 2019;17(1):52-60.
Woody CA, Ferrari AJ, Siskind DJ, et al. A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord. 2017;219:86-92.
Jarde A, Morais M, Kingston D, et al. Neonatal outcomes in women with untreated antenatal depression compared with women without depression: a systematic review and meta-analysis. JAMA Psychiatry. 2016;73(8):826-837.
Eke AC, Saccone G, Berghella V. Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis. BJOG. 2016;123(12):1900-1907.
Vlenterie R, van Gelder MMHJ, Anderson HR, et al. Associations between maternal depression, antidepressant use during pregnancy, and adverse pregnancy outcomes: an individual participant data meta-analysis. Obstet Gynecol. 2021;138(4):633-646.
O'Connor E, Rossom RC, Henninger M, et al. Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2016;315(4):388-406.
Curry SJ, Krist AH, Owens DK, et al. Interventions to prevent perinatal depression: US Preventive Services Task Force recommendation statement. JAMA. 2019;321(6):580-587.
- Bayrampour H, Kapoor A, Bunka M, et al. The risk of relapse of depression during pregnancy after discontinuation of antidepressants: a systematic review and meta-analysis. J Clin Psychiatry. 2020;81(4):19r13134.
Huybrechts KF, Palmsten K, Avorn J, et al. Antidepressant use in pregnancy and the risk of cardiac defects. N Engl J Med. 2014;370(25):2397-2407.
Bérard A, Zhao JP, Sheehy O. Antidepressant use during pregnancy and the risk of major congenital malformations in a cohort of depressed pregnant women: an updated analysis of the Quebec Pregnancy Cohort. BMJ Open. 2017;7(1):e013372.
Gao SY, Wu QJ, Sun C, et al. Selective serotonin reuptake inhibitor use during early pregnancy and congenital malformations: a systematic review and meta-analysis of cohort studies of more than 9 million births. BMC Med. 2018;16(1):205.
McDonagh MS, Matthews A, Phillipi C, et al. Depression drug treatment outcomes in pregnancy and the postpartum period: a systematic review and meta-analysis. Obstet Gynecol. 2014;124(3):526-534.
Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. The effect of prenatal antidepressant exposure on neonatal adaptation: a systematic review and meta-analysis. J Clin Psychiatry. 2013;74(4):e309-e320.
Nörby U, Forsberg L, Wide K, et al. Neonatal morbidity after maternal use of antidepressant drugs during pregnancy. Pediatrics. 2016;138(5):e20160181.
Warburton W, Hertzman C, Oberlander TF. A register study of the impact of stopping third trimester selective serotonin reuptake inhibitor exposure on neonatal health. Acta Psychiatr Scand. 2010;121(6):471-479.
U.S. Food and Drug Administration. FDA Drug Safety Communication: selective serotonin reuptake inhibitor (SSRI) antidepressant use during pregnancy and reports of a rare heart and lung condition in newborn babies. December 14, 2011. Accessed April 27, 2022. https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-selective-serotonin-reuptake-inhibitor-ssri-antidepressant-use-during
Masarwa R, Bar-Oz B, Gorelik E, et al. Prenatal exposure to selective serotonin reuptake inhibitors and serotonin norepinephrine reuptake inhibitors and risk for persistent pulmonary hypertension of the newborn: a systematic review, meta-analysis, and network meta-analysis. Am J Obstet Gynecol. 2019;220(1):57.e1-57.e13.
Schoretsanitis G, Augustin M, Saßmannshausen H, et al. Antidepressants in breast milk; comparative analysis of excretion ratios. Arch Womens Ment Health. 2019;22(3):383-390.
Gutsmiedl K, Krause M, Bighelli I, et al. How well do elderly patients with major depressive disorder respond to antidepressants: a systematic review and single-group meta-analysis. BMC Psychiatry. 2020;20(1):102.
Krause M, Gutsmiedl K, Bighelli I, et al. Efficacy and tolerability of pharmacological and non-pharmacological interventions in older patients with major depressive disorder: a systematic review, pairwise and network meta-analysis. Eur Neuropsychopharmacol. 2019;29(9):1003-1022.
van Poelgeest EP, Pronk AC, Rhebergen D, et al. Depression, antidepressants and fall risk: therapeutic dilemmas—a clinical review. Eur Geriatr Med. 2021;12(3):585-596.
Canadian Coalition for Seniors' Mental Health. Canadian guidelines on prevention, assessment and treatment of depression among older adults. Updated June 2021. Accessed August 13, 2022. https://ccsmh.ca/wp-content/uploads/2021/06/CCSMH_Depression_Guidelines_FINAL_EN.pdf
Kovich H, DeJong A. Common questions about the pharmacologic management of depression in adults. Am Fam Physician. 2015;92(2):94-100.
Adams SM, Miller KE, Zylstra R. Pharmacologic management of adult depression. Am Fam Physician. 2008;77(6):785-792.
Warner CH, Bobo W, Warner C, et al. Antidepressant discontinuation syndrome. Am Fam Physician. 2006;74(3):449-456.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2023 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

Anxiety, Depression and Quality of Life—A Systematic Review of Evidence from Longitudinal Observational Studies
Associated data.
Not applicable.
This review aimed to systematically review observational studies investigating the longitudinal association between anxiety, depression and quality of life (QoL). A systematic search of five electronic databases (PubMed, PsycINFO, PSYNDEX, NHS EED and EconLit) as well as forward/backward reference searches were conducted to identify observational studies on the longitudinal association between anxiety, depression and QoL. Studies were synthesized narratively. Additionally, a random-effects meta-analysis was performed using studies applying the mental and physical summary scores (MCS, PCS) of the Short Form Health Survey. The review was prospectively registered with PROSPERO and a study protocol was published. n = 47 studies on heterogeneous research questions were included, with sample sizes ranging from n = 28 to 43,093. Narrative synthesis indicated that QoL was reduced before disorder onset, dropped further during the disorder and improved with remission. Before onset and after remission, QoL was lower in comparison to healthy comparisons. n = 8 studies were included in random-effects meta-analyses. The pooled estimates of QoL at follow-up (FU) were of small to large effect sizes and showed that QoL at FU differed by disorder status at baseline as well as by disorder course over time. Disorder course groups differed in their MCS scores at baseline. Effect sizes were generally larger for MCS relative to PCS. The results highlight the relevance of preventive measures and treatment. Future research should consider individual QoL domains, individual anxiety/depressive disorders as well as the course of both over time to allow more differentiated statements in a meta-analysis.
1. Introduction
The World Health Organization [ 1 ] estimates that 264 million people worldwide were suffering from an anxiety disorder and 322 million from a depressive disorder in 2015, corresponding to prevalence rates of 3.6% and 4.4%. While their prevalence varies slightly by age and gender [ 1 ], they are among the most common mental disorders in the general population [ 2 , 3 , 4 , 5 , 6 ]. During the COVID-19 pandemic, multiple challenges have arisen for many, such as loneliness [ 7 ] or financial hardship. A meta-analysis showed a prevalence of anxiety of about 32% (95% CI: 28–37) and a prevalence of depression ( n = 14 studies) of about 34% (95% CI: 28–41) in general populations during the COVID-19 pandemic [ 8 ].
Anxiety and depression have been associated with adverse societal and individual correlates, including higher health care costs [ 9 , 10 , 11 ] and an increased risk for physical comorbidities, such as cardiovascular illnesses [ 12 , 13 ]. Moreover, they have been linked to a reduced quality of life (QoL) in numerous cross-sectional as well as longitudinal studies in which they significantly predicted QoL outcomes [ 14 , 15 , 16 , 17 , 18 ]. Other studies have reported a reverse association, whereby QoL was predictive of mental health outcomes [ 19 ] or a bi-directional association [ 20 , 21 ]. Some very recent studies also examined these associations among quite different samples (e.g., [ 22 , 23 , 24 , 25 ]).
Looking at longitudinal rather than cross-sectional data from observational studies has several advantages. It allows for the identification of trajectories over time within the same individuals rather than focusing on group differences at one point in time only [ 26 ]. Moreover, when appropriate methods are applied to longitudinal data, intraindividual heterogeneity can be taken into account, resulting in more consistent estimates [ 27 ]. This has previously been demonstrated in QoL research [ 28 ]. A need to analyze longitudinal changes in QoL domains in QoL research in people with mental disorders has also been previously identified [ 29 ]. Beyond individual longitudinal studies suggesting a link between anxiety or depression and QoL, several systematic reviews have synthesized longitudinal evidence on these associations and mostly reported negative associations between the variables. These reviews have tended to focus on specific age groups, such as older adults [ 30 ], samples with specific diseases [ 31 , 32 ], or have investigated the effect of specific treatments on QoL in patients with anxiety [ 33 ]. Investigating these associations in samples without these limitations could reduce the effect of specific conditions and treatments on the association and strengthen the conclusions that can be drawn.
In light of the previous findings, this study aims to add to the present literature by systematically synthesizing evidence from observational studies on the longitudinal association between anxiety, depression and QoL across all age groups in samples who do not have other specific illnesses and do not receive specific treatments.
2. Materials and Methods
This review was registered with PROSPERO (CRD42018108008) and a study protocol was published [ 34 ].
2.1. Search Strategy
Five electronic databases from several fields of research (PubMed, PsycINFO, PSYNDEX, NHS EED and EconLit) were examined until December 2020. Where possible, search terms were entered as Medical Subject Headings (MeSH) or as keywords in the title/abstract. The PubMed search strategy was: (anxi*[Title/Abstract] or depress*[Title/Abstract] or anxiety disorder[MeSH] or depressive disorder[MeSH]) and quality of life[MeSH] and longitudinal study[MeSH]. Please note that “*” is a truncation symbol. Time or location were not restricted. In addition, we applied backward and forward reference searches of included studies to identify additional references. The forward reference search was conducted until January 2021 using Web of Science to identify cited papers.
2.2. Study Selection Process
The study selection process is displayed in Figure 1 . Most identified studies were screened in a two-step process (title/abstract; full-text screening) independently by two reviewers (J.K.H., E.Q.) against defined criteria (see Table 1 ). The last updated literature screening before submission was conducted by one reviewer (J.K.H.) and encompassed 9% of the studies included for title/abstract screening. Before the final criteria were applied, they were pretested and refined. Disagreements during the selection process were resolved through discussion or by the inclusion of a third party (A.H.) if a consensus could not be reached.

Study flow (PRISMA flow chart).
Study selection criteria.
| Studies were eligible for inclusion if they: (i) Were observational studies analyzing the longitudinal association between anxiety or depression (disorders as well as symptom severity) and QoL, (ii) Analyzed samples without a specific disease or disorder other than anxiety and depression, (iii) Applied appropriate, validated measures for the main variables (e.g., for anxiety/depression: psychiatric diagnosis according to criteria of the International Classification of Diseases (ICD), the Diagnostic and Statistical Manual of Mental Disorders (DSM), or using a valid self-report screening tool), and (iv) Were published in English or German in a peer-reviewed journal. | |
| Studies were excluded if they: (i) Analyzed samples where participants were suffering or recovering from conditions other than anxiety/depression, (ii) Analyzed samples receiving or recovering from a specific intervention or treatment, (iii) Had no observational study design, (iv) Used a measure for the main variables other than those defined, or (v) Had publication characteristics that were different than those defined (e.g., were published in a language other than German or English, as well as not published in a scientific, peer-reviewed journal). | |
| After pre-testing, the following refinements were made to the screening criteria (ii) and (iii): (ii) Regarding the samples of interest, we decided to exclude studies analyzing dyads such as caregivers or partners to ill family members, due to possible spillover-effects on the individual’s QoL, which has been demonstrated in previous studies [ , ]. Additionally, samples consisting exclusively of people with anxiety or depressive disorders may receive some unspecific type of care for their mental health problems. We eliminated studies evaluating the effects of treatments using pre–post-treatment comparisons. Only studies where some naturalistic treatment that is usual for mental health problems that began prior to study baseline (BL) were included. Studies indicating that treatment was initiated at or after study BL (e.g., before or at admission to a psychiatric clinic) were excluded. (iii) Lastly, we specified the QoL assessments. In health and medicine research, numerous QoL instruments are used [ ]. Guided by previous literature reviews [ , , ]), we compiled a list of ten validated QoL assessments that have been used in children, adolescents or adults from the general population and/or samples with mental health problems, and that are frequently used in QoL research. Versions of the following instruments were included: Short Form Health Survey (e.g., SF-36, SF-12), EuroQol (e.g., EQ-5D, EQ-5D-Y), WHOQOL (e.g., WHOQOL-100, WHOQOL-BREF), Quality of Well-Being Scale, Quality of Life Scale, Pediatric Quality of Life Inventory, KIDSCREEN, KINDL, Quality of Life in Depression Scale, and the Quality of Life Enjoyment and Satisfaction Questionnaire. |
Abbreviations: QoL = quality of life; ICD = International Classification of Diseases; DSM = Diagnostic and Statistical Manual of Mental Disorders; BL = study baseline; KIDSCREEN = Health Related Quality of Life Questionnaire for Children and Young People and their Parents; KINDL = German generic quality of life instrument for children
2.3. Data Extraction and Synthesis
We extracted information regarding the study design, operationalization of the variables, sample characteristics, statistical methods and results regarding the research question of interest. If several analyses were presented for the same research question, we extracted the final covariate-adjusted model for narrative synthesis. Data were extracted by one reviewer (J.K.H.) and cross-checked by a second reviewer (E.Q.). If needed, extracted data were standardized (e.g., by calculating the weighted average means when combining groups) to present comparable information. If clarification was needed, the corresponding authors were contacted.
For the narrative synthesis, all studies were first grouped by research question, e.g., whether disorders or the degree of symptoms were analyzed, which comparison groups were used, which QoL domains were considered, and at which waves the variables of interest were considered in the analyses. Because research questions and analyses were heterogeneous, a concise narrative synthesis of the main results of all studies was not feasible. Therefore, we provide an overview of all identified studies in the tables and a detailed narrative synthesis of those studies, analyzing trajectories of disorders or changes in symptoms in association with changes in QoL over time.
Additionally, we examined whether data were appropriate for meta-analysis. The specific research questions, the operationalization of main variables and statistical methods were heterogeneous across studies and not all the statistical estimates needed could be obtained from covariate-adjusted analyses. Therefore, to enhance the comparability of the underlying data and the interpretation of the pooled estimates, we used descriptive information. Because most papers applied variations of the Short Form Health Survey and analyzed mental and physical component scores (MCS, PCS), we considered these studies as eligible for meta-analysis. The necessary information could be obtained for 8 publications. Random-effects meta-analysis was used for pooling. Heterogeneity was assessed by means of I 2 , with higher values representing a larger degree of heterogeneity in terms of variability in effect size estimates between studies [ 41 ]. Pooled estimates are reported as Hedge’s g standardized mean difference (SMD), representing the difference in mean outcomes between groups relative to outcome measure variability [ 42 ]. According to Cohen (as cited in [ 43 ]), SMDs can be grouped into small ≤0.20, medium = 0.50 and large effects ≥0.80. Stata 16 was used for meta-analyses.
2.4. Quality/Risk of Bias Assessment
Two reviewers (J.K.H., E.Q.) independently assessed the quality and risk of bias of the included studies using the Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies, which was developed by the National Heart, Lung, and Blood Institute [ 44 ].
3.1. Selection Process
The literature search yielded 4027 unique references. After title/abstract screening, 215 studies were included for full-text screening. Finally, 47 publications were included in the final synthesis. During full-text screening, most studies were excluded because they exclusively analyzed data on a cross-sectional level (56.5%). For further details, see the PRISMA flow chart ( Figure 1 ).
3.2. Overview of Included Studies
Descriptive characteristics and quality/risk of bias assessment of the included studies are provided in Table S1 (Supplementary Material) . In short, sample size ranged from 28 to 43,093. Most studies focused on adults; only four analyzed children/adolescents. Regarding the settings, 17 of the analyzed samples were exclusively recruited in a health care setting, 12 of the studies analyzed general population samples, 14 recruited in another or in several settings, and all studies on children/adolescents recruited in schools ( n = 4). Twenty studies (42.6%) applied data from the same seven underlying datasets. Most studies reported on depression ( n = 36), less reported on anxiety ( n = 20) and some reported on the comorbidity between depression and anxiety ( n = 7). To assess mental disorders, half (48.9%) used structured interviews. Regarding QoL, most studies applied variations of the Short Form Health Survey (SF, n = 27) or the WHOQOL ( n = 12). A total of 38.3% of the studies were rated as “good”, 55.3% as “fair” and 6.4% as “poor” in the quality assessment.
3.3. Overview of Studies on the Association between Anxiety/Depression as Independent Variables and QoL Outcomes
Detailed results on all studies investigating the association between anxiety/depression as independent variables and QoL outcomes are reported in Table 2 . As described in the methods section, the following paragraphs give an overview of those studies focusing on disorder trajectories/changes in symptoms over time and changes in QoL outcomes over time, because they allow for more differentiated interpretations.
Studies on depression/anxiety as independent variables and QoL outcomes.
| First Author (Year) | Disorder or Symptoms Analyzed; QoL Domains Analyzed | Research Question Regarding QoL | Methods | Results |
|---|---|---|---|---|
| Årdal (2013) [ ] | Controls and patients in the acute phase of recurrent MD and FU (DSM-IV, HDRS); SF-36 (physical functioning, role physical, vitality, bodily pain, mental health, role emotional, social functioning, general health, as well as summary scores PCS, MCS and total score) | (a) Whether QoL scores differ between MD patients and healthy comparisons across domains over time. (b) Whether QoL in patients with recurrent MDD differed between acute phase and recovery. | (a) ANOVA (b) Paired-sample -tests | (a) There was a significant interaction effect between time, QoL domain and group, indicating that QoL scores differed between MD patients and controls over time. Compared to the healthy control group, the MDD group had reduced QoL in all domains at BL and reduced QoL in several domains at FU (significant for general health, social, emotional role, mental health, PCS, MCS and total score). (b) In the MD group, QoL scores significantly improved during recovery from recurrent MDD in most domains (significant for physical functioning, physical role, vitality, social functioning, role emotional, mental health, PCS, MCS and total score). |
| Buist-Bouwman (2004) [ ] | Onset, acute phase and subsequent remission from MDE (CIDI); comorbid anxiety disorder (CIDI); SF-36 (physical functioning, physical role, vitality, pain, psychological health, psychological role, social functioning and general health) | (a) Whether incident MDE and recovery from MDE are associated with changes in QoL and whether pre- and post-morbid QoL scores in the MD group differ from the comparison group without MD. (b) In the subgroup with worse QoL after MDE: whether the severity of depression and number of depressive episodes were associated with worse QoL. (c) Whether comorbid anxiety during MDE is associated with reduced QoL (i.e., lower QoL after MDE compared to before MDE). | (a)–(c) Multivariate logistic regression | (a) Incident MDE was associated with a drop in QoL (significant for vitality, psychological, psychological role and social functioning). Subsequent recovery from MDE was associated with an improvement in QoL (significant for physical role, vitality, psychological health, psychological role, social functioning and general health). Comparing pre- and post-morbid levels, QoL did not differ or was higher after MDE in some domains (significantly higher for psychological health and psychological role). Moreover, before MD onset, QoL was significantly lower compared to healthy controls in all domains. After remission from MDE, QoL scores in nearly all domains (not significant for psychological role) were significantly lower compared to healthy controls. (b) About 40% of the MDE group had worse QoL after recovery from MDE compared to pre-morbid levels. The severity of depression was associated with worse QoL only for the psychological health domain, but no other domains. The number of depressive episodes was not significantly associated with worsening QoL in any domain. (c) In the MDE cohort, comorbid anxiety was associated with a significant reduction in QoL (significant for physical role and psychological health). |
| Cabello (2014) [ ] | Chronic MD (AUDADIS interview; summary score of the number of symptoms to identify severity); SF-12, “disability” (i.e., domain-specific reduced QoL, defined as score ≤ 25th percentile in the subscale; physical functioning, physical role, bodily pain, general health, vitality, social functioning, emotional role and mental health) | (a) Whether chronic MD is associated with the incidence/persistence of “disability” (i.e., reduced QoL) in a general population sample. (b) Whether the severity of depressive symptoms is associated with the incidence/persistence of “disability” (i.e., reduced QoL) in the MD subgroup of the sample. | Both (a) and (b) Generalized Estimating Equations and logistic regressions | (a) In the general population, chronic MD was a significant risk factor for the persistence of disability (i.e., reduced QoL) in all domains and of the incidence of disability (i.e., reduced QoL) in all domains except for the physical role. (b) In the chronic MD subgroup, the severity of depressive symptoms was associated with the persistence of disability (i.e., reduced QoL) (significant for general health, social functioning, emotional role and mental health) and not significantly associated with the incidence of reduced QoL in any domain. |
| Cerne (2013) [ ] | Number of depressive episodes over time according to CIDI; number of episodes of panic and other anxiety syndromes over time (PHQ); SF-12 (PCS, MCS) | Whether the pooled number of (a) depressive episodes over time, (b) panic and anxiety episodes over time are are associated with the pooled QoL over time. | (a) and (b) Multivariate linear regression | (a) A higher number of depressive episodes over time was associated with lower pooled PCS and MCS. (b) a higher number of pooled panic episodes over time was associated with a lower mean MCS but not PCS. A higher number of pooled other anxiety syndrome episodes over time was not associated with the mean MCS or PCS. |
| Chin (2015) [ ] | Depression according to PHQ-9 (>9), clinician’s diagnosis; SF-12v2 (PCS, MCS) | (a) Whether depressive symptoms and a clinician’s detection of depression at BL are associated with QoL at FU. (b) Whether a clinician’s detection of depression at BL is associated with a change in QoL. | (a) Multivariable non-linear mixed-effects regression (b) Independent -tests | (a) Depressive symptoms and a clinician’s detection of depression at BL were not predictive of QoL at FU. (b) A clinician’s detection of depression at BL was related to change (improvement) in MCS, but not PCS over time in a primary care sample screened as positive for depression. |
| Chung (2012) [ ] | Depression diagnosis and symptoms (DSM-IV, HRSD depression scale, HADS depression scale); anxiety symptoms (HRSD anxiety scale, HADS anxiety scale; SF-36 (physical functioning, role physical, bodily pain, general health, vitality, social functioning, role emotional, mental health, PCS and MCS) | (a) Whether BL depressive symptoms are associated with QoL at FU. (b) Whether BL depressive symptoms or changes in depressive symptoms are associated with changes in QoL over time. (c) Whether BL anxiety symptoms are associated with QoL at FU. (d) Whether BL anxiety symptoms or changes in anxiety symptoms are associated with changes in QoL over time. | (a)–(d) Hierarchical regression | (a) BL depressive symptoms were not associated with any QoL domain at FU. (b) BL depressive symptoms were not associated with changes in any QoL domain over time. Changes in depressive symptoms were significantly associated with changes in some QoL domains over time (significant for: general health, vitality, mental health and MCS). (c) BL anxiety symptoms were not associated with any QoL domain at FU. (d) BL anxiety symptoms were not associated with changes in any QoL domain over time. Changes in anxiety symptoms were significantly associated with changes in some QoL domains over time (significant for: bodily pain, general health and mental health). |
| Diehr (2006) [ ] | Depression according to CIDI, CES-D (>16); QLDS, WHOQOL-Bref (environmental, physical, psychological and social), SF-12 (PCS, MCS) | (a) Whether the quartile of change in depressive symptoms is associated with changes in QoL. (b) Whether the remission of depression at FU is associated with changes in QoL. | Regression | (a) No/little change in CES-D associated with changes in QoL over time (significant for SF-12 MCS). Every other quartile of change in depressive symptoms was significantly associated with changes in QoL in most scales/domains (significant for: QLDS, all domains of WHOQOL-Bref and SF-12 MCS), meaning a higher reduction in depressive symptoms was associated with a higher increase in QoL, and more severe depressive symptoms were associated with a reduction in QoL. (b) Remission of depression at FU was associated with improvement in all QoL measures and domains (SF-12, QLDS and WHOQOL-Bref). There was no significant change in QoL in those with persistent clinical depression at FU. |
| Hajek (2015) [ ] | Depressive symptoms (GDS); EQ-VAS | Whether an initial change in depressive symptoms is associated with a subsequent change in QoL in the whole sample and by sex. | Vector autoregressive models | No significant association between an initial change in depression score and a subsequent change in QoL was found for the whole sample or stratified by sex. |
| Hasche (2010) [ ] | Depression status at BL (according to DIS diagnosis and CES-D ≥ 9); SF-8 (PCS, MCS) | (a) Whether depression status groups at BL differed according to QoL at FU. (b) Whether depression status groups at BL differed according to QoL changes in score over time. | (a) -tests (b) Linear mixed effects regression models | (a) At 6- and 12-month FU, those with and without depression at BL differed significantly in QoL scores, with the depression group reporting lower QoL at FUs (significant for MCS and PCS). (b) While depression at BL was significantly related to improvements in MCS (but not PCS) scores over time, those with depression still reported lower QoL compared to those without. |
| Heo (2008) [ ] | Depression (BDI ≥ 10); SF-36 (decrease in total score over time) | Whether FU depression is associated with a reduction in QoL over time. | Binary logistic regression | Depression at FU was associated with a significant reduction in QoL total score over time. |
| Ho (2014) [ ] | Depression (according to GDS ≥ 5); SF-12 (PCS, MCS) | Whether depression at BL is associated with QoL at FU. | Linear regression | BL depression was associated with lower QoL at FU (significant for MCS and PCS). |
| Hussain (2016) [ ] | Depressive disorders (SCID, MINI); current PTSD, specific phobias, other anxiety disorders (SCID, MINI); WHOQOL-Bref (general QoL and hrqol) | (a) Whether current depressive disorders at BL predict QoL at FU. (b) Whether current PTSD, specific phobias and other anxiety disorders at BL predict QoL at FU. | (a) and (b) Multiple linear regression | (a) Depressive disorders at BL predicted reduced QoL at FU (significant for general QoL and hrqol). (b) PTSD, but not specific phobias or other anxiety disorders, predicted reduced general QoL at FU. None of the anxiety disorders predicted hrqol at FU. |
| Joffe (2012) [ ] | Lifetime history of depression (according to SCID); anxiety disorder (according to SCID); SF-36 (impaired QoL according to 25th percentile of SF-36; social functioning, role emotional, role physical, pain and vitality) | (a) Whether a lifetime history of depression is associated with impaired QoL during FU. (b) Whether a prior lifetime history of anxiety disorder (compared to no depression or anxiety) is associated with reduced QoL during FU. (c) Whether a lifetime history of comorbid depression and anxiety is associated with impaired QoL during FU. | (a)–(c) Repeated measure multilevel regression | (a) A history of depression only was associated with reduced QoL during FU (significant for social functioning and pain). (b) Prior lifetime history of anxiety disorder was associated with reduced QoL (significant for physical role). (c) A history of comorbid anxiety and depression was associated with reduced QoL during FU (significant for social functioning, emotional role, physical role and pain). |
| Johansen (2007) [ ] | Level of PTSD symptoms according to IES-15; WHOQOL-Bref (physical health, psychological health, social relationships and environment) | Whether PTSD symptoms predict QoL at FU. | Structural equation model | More severe PTSD symptoms predicted QoL at FU (significant positive association between FU1 and FU2). |
| Kramer (2003) [ ] | Current or lifetime depression/PTSD (according to Q-DIS); SF-36 (energy/fatigue, emotional role, general health, mental health, pain, physical functioning, physical role and social) | Whether QoL outcomes over time differed among the disorder groups. | Random/fixed effects model | There was no significant interaction between time and diagnostic group (no depression/PTSD, PTSD, depression and comorbid depression/PTSD) on QoL. Comparing the adjusted means for all three times among the disorder groups showed significant differences between the groups in most domains. In comparison, those with depression at BL reported reduced QoL over time in several domains compared to the PTSD group and the group without PTSD/depression. In comparison, those with PTSD only showed higher QoL compared to those with depression or comorbid depression/PTSD in several domains. |
| Kuehner (2009) [ ] | Depressive symptoms (MADRS); WHOQOL (overall, physical, psychological, social and environmental) | Whether the lag in levels of depressive symptoms predicts future levels of QoL and whether the association differs by group (formerly depressed inpatients vs. community controls). | Time-lagged linear models | Higher depressive symptoms predict future lower QoL (significant for social). The association was not moderated by group status. |
| Kuehner (2012) [ ] | Depression score (according to MADRS, FDD-DSM-IV); WHOQOL-Bref (physical, psychological, social and environment) | Whether the lag in depressive symptoms predicted QoL at FU. | Hierarchical, time-lagged linear models | Higher depressive symptoms significantly predicted lower QoL at FU (significant for physical and psychological). |
| Lenert (2000) [ ] | Remission or persistent depression (according to DSM-III criteria, DIS); SF-12 (PCS, MCS) | Whether the remission of depression (compared to no remission) is associated with changes in QoL over time. | OLS regression | Remission of depression was associated with improved QoL (significant for MCS) at FU1 and FU2. |
| Mars (2015) [ ] | Asymptomatic, mild and high symptoms of depression (according to SCAN); EQ-5D (without anxiety/depression item) | Whether depression symptom trajectories over time (asymptomatic, mild symptoms and chronic–high symptoms) are associated with QoL at FU. | Latent class growth analysis with distal outcome models | QoL at FU differed significantly among different depression symptom trajectories, with persons from the the chronic–high depressive symptom class showing lower QoL scores relative to the asymptomatic class. |
| Moutinho (2019) [ ] | Depression at BL (according to DASS cut-off: 9); anxiety at BL (according to DASS anxiety scale cutoff: 7); WHOQOL-Bref at FU (physical, psychological, social and environment) | (a) Whether BL depression predicted QoL at FU. (b) Whether BL anxiety predicted QoL at FU. | (a) and (b) Stepwise linear regression | (a) Depression at BL was significantly associated with reduced QoL at FU (significant for psychological functioning, social functioning and environmental). (b) Anxiety at BL was associated with reduced QoL at FU (significant for physical). |
| Ormel (1999) [ ] | Depression at BL (according to CIDI); “disability” (i.e., reduced QoL according MOS SF 6-item physical functioning scale ≥ 2) | Whether depression at BL is associated with the onset of disability (i.e., reduced QoL) during FU. | Logistic regression models | Compared to the non-depressed group, people with depression at BL showed higher odds for the onset of disability (i.e., reduced QoL) during FU (significant for 12-month FU, but not 3-month FU). |
| Pan (2012) [ ] | Depressive symptoms (CES-D); WHOQOL-Bref-TW (overall score, physical, psychological, social and environmental) | Whether depressive symptoms were associated with QoL over time. | Linear mixed-effects models | Higher depressive symptoms were associated with lower QoL in MDD patients (significant for overall score, physical, psychological, social and environmental). |
| Panagioti (2018) [ ] | Depressive symptoms (MHI-5); WHOQOL-Bref (physical, psychological, environmental and social) | Whether depressive symptoms at BL are associated with changes in QoL over time. | Multivariate regression models | Higher depressive symptoms at BL were associated with a decline in QoL over time (significant for physical and psychological). |
| Pakpour (2018) [ ] | Dental anxiety at BL (MDAS); PedsQL 4.0 general hrqol and oral hrqol scale at FU | Whether dental anxiety at BL predicted oral- and general-health-related QoL at FU. | Structural equation modeling | Dental anxiety at BL was no significant direct predictor of generic QoL at FU and was significantly associated with worse oral-health-related QoL at FU. |
| Pyne (1997) [ ] | MD-diagnosis (SCID/SADS) and depressive symptoms (HAM-D); QWB | Whether group status over time (community controls, continuously non-depressed patients, incident depression patients and continuously depressed patients) is associated with changes in QoL. | Repeated measure analysis (ANOVA) | There was no significant interaction term between group status and time, indicating that changes in QoL did not differ between the groups. At both points in time, QoL differed significantly among all groups, except between the incident depression and continuous depression group. |
| Remmerswaal (2020) [ ] | OCD course (SCID), Y-BOCS, BDI, BAI over time; EQ-5D over time | (a) Whether OCD symptom severity and QoL over time were associated. (b) Whether QoL over time differs between OCD course groups (chronic, intermittent and remitting) and general population norms. (c) Whether OCD symptom severity, anxiety and depressive symptoms over time are associated with changes in QoL over time in patients with OCD. | (a) Pearson’s correlation (b)–(c) Linear mixed models | (a) QoL over time and OCD symptom severity were significantly correlated. (b) The QoL of OCD patients was significantly lower compared to general population norms, except the QoL of the intermittent OCD group at FU1, where there was no significant difference compared to the general population. When comparing the OCD course groups, the chronic OCD group had a significantly lower QoL over time compared to the other groups. The remitting group had moderately improved until FU1 and a small QoL improvement between FU1 and FU2 relative to the chronic group. (c) In those with a remitting OCD, only more severe symptoms of comorbid anxiety and depressive symptoms, but not OCD symptom severity over time, were significantly associated with a lower QoL over time. |
| Rhebergen (2010) [ ] | MD-/dysthymia-/DD diagnosis at BL and subsequent recovery at FU (according to CIDI); comorbid anxiety at BL (CIDI); SF-36 (physical health summary score) | Whether QoL trajectories over time differ between: (a) different depression status groups who achieved remission (MDD, dysthymia and double depression) and a comparison group without mental health disorders. (b) The different depression status groups. (c) Whether comorbid anxiety at BL in a sample recovering from depression is associated with changes in QoL. | (a)–(c) Linear mixed models | (a) There was a significant interaction between group status and time. More specifically, compared to changes in QoL over time in people without a mental health diagnosis, QoL improved over time in those with MDD and DD, but not dysthymia. All depression diagnosis groups showed a significantly lower QoL compared to the no diagnosis group at all waves. (b) Considering the depression groups, only the interaction term between dysthymia and time until FU1 was significant. Those with dysthymia had a significantly lower QoL compared to those with MDD at FU1. This difference was not significant at FU2. (c) Comorbid anxiety disorder at BL in people who recovered from depression over time was not associated with a significant change in QoL over time. |
| Rubio (2014) [ ] | First episode of incident MDD (AUDADIS-IV) at FU; incident GAD, social anxiety disorder, PD, specific phobia (AUDADIS-IV); SF-12 (MCS) | Whether incident MDD is associated with changes in QoL over time compared to: (a) people without history of MDD, (b) without history of any mental health disorder, (c) and whether the association differed by gender. Whether incident anxiety disorders are associated with changes in QoL over time: (d) compared to no history of the specific anxiety disorder, (e) compared to no history of any psychiatric disorder, (f) and whether the association differed by gender. | Linear regression model | (a) Incidence of MDD (compared to no MDD) was associated with a significant decrease in QoL until FU. (b) Incidence of MDD (compared to no mental health disorder) was associated with a significant decrease in QoL until FU. (c) The association did not vary by gender. (d) Incidence of all anxiety disorders (with comorbid disorders; ref: no history of anxiety disorder) was associated with a significant decrease in QoL over time. (e) Incident anxiety disorders were not significantly associated with QoL when only considering “pure” anxiety without any comorbidities (ref: no history of any psychiatric disorder). (f) The association did not vary by gender. |
| Rubio (2013) [ ] | Remission from MDD, dysthymia (AUDADIS-IV); Remission from GAD, PD, SAD, specific phobia (AUDADIS-IV); SF-12 (MCS) | Whether remission from depression (MDD, dysthymia) is associated with: (a) changes in QoL over time (compared to non-remitted cases), (b) QoL at FU (compared to people with no history of a specific depressive disorder), (c) QoL at FU, when only considering depressive disorders without any psychiatric comorbidity (compared to people without any lifetime psychiatric diagnosis). Whether remission from anxiety disorders are associated with: (d) changes in QoL over time (compared to non-remitted cases), (e) QoL at FU (compared to people with no history of a specific anxiety disorder), (f) QoL at FU, when only considering anxiety disorders without any psychiatric comorbidity (compared to people without any lifetime psychiatric diagnosis). | (a)–(f) Linear regression models | (a) Remission from MD and dysthymia was associated with a significant positive change in QoL compared to non-remitted cases. (b) Remission of MD and dysthymia was associated with significantly lower QoL at FU compared to people without history of a specific diagnosis. (c) Remission of MD and dysthymia was associated with significantly lower QoL at FU compared to people without any lifetime psychiatric diagnosis. (d) Remission from SAD and GAD was associated with significant positive changes in QoL compared to non-remitted cases. (e) Remission of PD, SAD, specific phobia and GAD was associated with significantly lower QoL at FU compared to people without history of a specific diagnosis. (f) Remission of “pure” PD, SAD, specific phobias and GAD was associated with significantly lower QoL at FU compared to people without any lifetime psychiatric diagnosis. |
| Rozario (2006) [ ] | Depressive symptoms (GDS); SF-12 (MCS and PCS) | Whether depressive symptom severity was associated with QoL change profiles over time (no change, declined and improved groups). | Multinomial logistic regression | There was no significant association between depressive symptom severity and QoL change score profiles at FU. |
| Sareen (2013) [ ] | Depression trajectory groups over time (according to AUDADIS-IV); anxiety disorder trajectory groups over time (according to AUDADIS-IV); SF-12 (MCS and PCS) | (a) Whether depression trajectory groups (no past year disorder/no suicide attempt at FU, remission without treatment, persistent disorder/comorbidity/suicide attempt/treatment) differed according to QoL at FU. (b) Whether anxiety disorder trajectory groups (no past year disorder/no suicide attempt at FU, remission without treatment, persistent disorder/comorbidity/suicide attempt/treatment) differed according to QoL at FU. | (a) and (b) Multiple linear regression models | (a) QoL at FU differed among the different depression trajectory groups (MCS was significant for all groups: no disorder > remitted disorder > persistent disorder; PCS: no disorder > remitted disorder; remitted disorder < persistent disorder). (b) QoL at FU differed among the different anxiety trajectory groups (MCS was significant for all groups: no disorder > remitted disorder > persistent disorder; PCS: no disorder > persistent disorder, remitted disorder > persistent disorder). |
| Shigemoto (2020) [ ] | PTSD symptoms (PCL-C); Q-LES-Q (psychosocial and physical) | Whether previous PTSD symptoms are associated with QoL at FU. | Longitudinal structural equation model | Previous PTSD symptoms were associated with physical QoL at FU1, but not FU2 or psychosocial QoL at both FUs. |
| Siqveland (2015) [ ] | Depressive symptoms (according to the depression scale from the GHQ-28); PTSD symptoms (PCL-S); WHOQOL-Bref (global and hrqol) | (a) Whether depressive symptoms at BL are associated with QoL at FU. (b) Whether PTSD symptoms at BL are associated with QoL at FU. | (a) and (b) Multiple mixed effects regression analyses | (a) Higher depressive symptoms at BL were associated with reduced QoL at FU. (b) PTSD levels at BL were not significantly associated with reduced QoL at FU. |
| Spijker (2004) [ ] | Depression status (CIDI); Comorbid anxiety (CIDI); SF-36 (social, role emotional) | (a) Whether depression status over time (non-depressed, recovered or depressed (including persistent, relapsing course)) is associated with QoL at FU. Whether comorbid anxiety is associated with QoL at FU (b) in a group with persistent depression and (c) in a group recovered from depression. | ANOVA | (a) QoL at FU was significantly reduced in depressed samples compared to the non-depressed group, and lower in the persistently depressed compared to the recovered group (significant for: role emotional and social). Among the depressed subgroups, there was no significant difference between a persistent or a relapsing course regarding QoL at FU. (b) In the persistently depressed group, comorbid anxiety was significantly associated with reduced QoL at FU (significant for role emotional and social). (c) In those who recovered from depression, comorbid anxiety was significantly associated with reduced QoL (significant for role emotional). |
| Stegenga (2012) [ ] | MDD status according to CIDI (remitted, intermittent and chronic); SF-12 (PCS and MCS) | Whether MDD course (remitted, intermittent and chronic) is associated with QoL over time. | Random coefficient analysis | While change in QoL over time did not differ between course groups, QoL at BL (MCS) was lower in those with a chronic course compared to those who remitted from BL. |
| Stegenga (2012) [ ] | MDD (CIDI); anxiety syndromes (panic disorder and others, PHQ); SF-12 (PCS) | (a) Whether MDD at BL predicts change in QoL over time. (b) Whether anxiety syndrome at BL (compared to no psychiatric diagnosis) predict changes in QoL over time. (c) Whether comorbid anxiety and MDD at BL (compared to no psychiatric diagnosis) predict changes in QoL over time. | (a)–(c) Random coefficient model | (a) While changes in QoL over time did not differ significantly between those with MDD at BL and those without any psychiatric diagnosis, QoL at BL was lower in those with depression. (b) While changes in QoL over time did not differ significantly between those with anxiety syndrome at BL and those without any psychiatric diagnosis, QoL at BL was lower in those with anxiety compared to those without any psychiatric diagnosis. (c) While changes in QoL over time did not differ significantly between those with comorbid anxiety and MDD at BL and those without any psychiatric diagnosis, QoL at BL was lower in those with comorbid anxiety and MDD compared to those without any psychiatric diagnosis. |
| Stevens (2020) [ ] | Posttraumatic stress symptoms (VETR-PTSD); SF-36 (MCS, PCS, physical functioning, bodily pain, general health, role physical, role emotional, mental health, vitality and social functioning) | Whether PTSS at BL is associated with QoL at FU. | Generalized estimating equations | Higher BL PTSS was significantly associated with lower QoL (PCS and MCS) at FU. Using a Bonferroni-corrected alpha value, only the domains of mental health, vitality and social functioning at FU were significantly associated with BL PTSS symptoms. The interaction between time and PTSS at BL was not significant, indicating that PTSS had the same effect on QoL outcomes at both FUs. |
| Tsai (2007) [ ] | Increased post-traumatic stress symptoms (DRPST); MOS SF-36 (physical functioning, role physical, pain, general health, vitality, social functioning, role emotional, mental health, PCS and MCS) | (a) Whether different PTSS trajectory groups over time (persistent PTSS, recovered, delayed and persistently healthy) differed in QoL at FU. (b) Whether increased post-traumatic stress symptoms at BL predicted QoL at FU. | (a) ANOVA (b) Multiple regression models | (a) At FU, those who were persistently healthy had the highest QoL scores (significantly higher compared to the persistent group in all domains; significantly higher than the recovered group for: pain, general health, vitality, mental health and MCS; significantly higher compared to delayed PTSS in all domains). In addition, those with delayed PTSS (significantly lower than the recovered group in all domains except physical functioning) and those with persistent PTSS (significantly lower than recovered group in all domains) had the lowest QoL overall. (b) Increased PTSS at BL was not significantly associated with QoL at FU. |
| Vulser (2018) [ ] | Depressive symptom levels (CES-D score), depression status (CES-D ≥ 19); SF-12v2 (role emotional and social) | Whether depressive symptoms or depression status at BL are associated with QoL at FU. | Generalized linear models | Both the level of depressive symptoms at BL as well as depression status at BL were associated with QoL at FU (significant for: role emotional and social). |
| Wang (2000) [ ] | Depressive symptoms (SCL-90 subscale); anxiety symptoms (SCL-90 subscale); WHOQOL-Bref (total) | (a) Whether depressive symptoms at BL were associated with QoL at FU. (b) Whether anxiety symptoms at BL were associated with QoL at FU. | (a) and (b) Stepwise regression | (a) Higher depressive symptoms at BL were associated with reduced QoL at FU. (b) Anxiety symptoms BL were not included in the final stepwise regression model. |
| Wang (2017) [ ] | Depressive disorder course groups (CIDI); anxiety disorder course (CIDI); SF-36 (MCS, PCS) | (a) Whether QoL at FU differs between three different course groups of depressive disorders (1. no disorder at BL and no suicide attempt until FU; 2. remitted without treatment; 3. persistent disorder/treatment/developed psychiatric co-morbidity/suicide attempt until FU). (b) Whether QoL at FU differs between three different course groups of anxiety disorders (1. no disorder at BL and no suicide attempt until FU; 2. remitted without treatment; 3. persistent disorder/treatment/developed psychiatric co-morbidity/suicide attempt until FU). | (a) and (b) Multiple linear regression | (a) Those with depression at BL that remitted without treatment had lower QoL at FU (significant for MCS and PCS) than those without the disorder and higher QoL at FU (significant for MCS) than those with a persistent disorder. (b) Those with anxiety at BL that remitted without treatment over time had lower QoL at FU than those without the disorder and higher QoL (MCS, but not PCS) than those with a persistent disorder. |
| Wu (2015) [ ] | Depressive symptoms according to CDI; social anxiety symptoms (SASC); QOLS | (a) Whether depressive symptoms at BL are associated with QoL at FU. (b) Whether social anxiety symptoms at BL are associated with QoL at FU. | (a) and (b) Multivariate stepwise forward regression | (a) Higher depressive symptoms at BL were significantly associated with reduced QoL at FU. (b) Higher social anxiety symptoms at BL were not significantly associated with QoL at FU. |
Abbreviations: QoL = quality of life; MD = major depression; FU = follow-up; DSM = Diagnostic and Statistical Manual of Mental Disorders; HDRS = Hamilton Depression Rating Scale; PCS = Physical Component Score; MDS = Mental Component Score; MDD = major depressive disorder; ANOVA = analysis of variance; BL = baseline; MDE = major depressive episode; CIDI = Composite International Diagnostic Interview; SF-36 = Short Form 36; AUDADIS = Alcohol Use Disorders and Associated Disabilities Interview Schedule; SF-12 = Short Form 12; PHQ = Patient Health Questionnaire; SF-12v2: Short Form 12, Version 2; HRSD = Hamilton Rating Scale for Depression; HADS = Hospital Anxiety and Depression Scale; QLDS = Quality of Life in Depression Scale; EQ-VAS = EQ Visual Analogue Scale; DIS = Diagnostic Interview Schedule; BDI = Beck Depression Inventory; SCID = Short Children’s Depression Inventory; MINI = Mini-International Neuropsychiatric Interview; PTSD = post-traumatic stress disorder; hrqol = health-related quality of life, IES-15 = Impact of Event Scale 15; Q-DIS = Quick Version of the Mental Health’s Diagnostic Interview Schedule; MADRS = Montgomery–Åsberg Depression Rating Scale; FDD-DSM-IV = Fragebogen zur Depressionsdiagnostik nach Diagnostic and Statistical Manual of Mental Disorders IV; SCAN = Schedule for Clinical Assessment in Neuropsychiatry; DASS = Depression Anxiety Stress Scales; MOS SF = Medical Outcomes Study Short Form; CES-D = Center for Epidemiological Studies Depression Scale; WHOQOL-Bref-TW = WHOQOL-Bref Taiwan Version; MHI-5 = Mental Health Inventory 5; OCD = obsessive compulsive disorder; Y-BOCS = Yale–Brown Obsessive Compulsive Scale; BAI = Beck Angst Inventar; DD = depressive disorder; PD = psychiatric disorder; SAD = social anxiety disorder; Q-LES-Q = Quality of Life Enjoyment and Satisfaction Questionnaire; GHQ-28 = General Health Questionnaire 28; PCL-S = Post-traumatic Stress Disorder Checklist Scale; VETR-PTSD = Vietnam Era Twin Registry Posttraumatic Stress Disorder; DRPST = Disaster-Related Psychological Screening Test; SCL-90 = Symptomcheckliste bei psychischen Störungen 90; SASC = SpLD Assessment Standards Committee; QOLS = Quality of Life Scale; CDI = Children’s Depression Inventory.
Depression as independent variable and QoL as outcome. One study investigated QoL at several time points during the entire course of an episode of MD .
Buist-Bouwman, Ormel, de Graaf and Vollebergh [ 46 ] analyzed an MD group from a general population setting (NEMESIS) with data on SF-36 domains in the onset, acute and recovery phase of the depressive episode. The onset of MD was associated with a significant drop in several QoL domains and recovery with a significant increase. Pre- and post-morbid QoL levels were not significantly different for most domains, and post-morbid QoL was even higher for the psychological role functioning and psychological health domains. In comparison to a group without MD, pre- and post-morbid QoL levels in the MD group were significantly lower, except for the psychological role functioning domain, where no significant differences were found. Additionally, it should be noted that 40% of the sample had lower post-morbid QoL compared to pre-morbid levels.
Two studies investigated changes in QoL for people experiencing an onset of depression relative to different comparison groups over two points in time.
One study investigated incident MD in a general population sample (NESARC; Rubio, Olfson, Perez-Fuentes, Garcia-Toro, Wang and Blanco [ 14 ]). Here, incident MD (compared to those without a history of MD as well as to a group without any mental disorder) was associated with a significant drop in QoL (SF-12 MCS). Additionally, analyzing two waves, Pyne, Patterson, Kaplan, Ho, Gillin, Golshan and Grant [ 67 ] compared the QoL (Quality of Well-Being scale) between MD patients and community controls. The patient group was further divided into those continuously not receiving an MD diagnosis, those who continuously received the diagnosis and those who only received the diagnosis at FU (onset). The authors found that changes in QoL did not differ between the groups. At both points in time, QoL scores differed significantly between the groups, except for the incident and the continuous depression group [ 67 ].
Six studies investigated different courses of depression over time in people with depression at BL with or without a healthy comparison group as reference.
Two primary care studies analyzed groups with clinical depression at BL with different FU depression statuses (remission, no remission). One study [ 51 ] analyzed changes in generic QoL measures (SF-12, WHOQOL-Bref) and the disease-specific Quality of Life in Depression Scale. In this study, remission was associated with an improvement in all QoL domains, whereas QoL did not change significantly over time for the non-remitted group. Another study [ 60 ] investigated SF-12 MCS and PCS scores and reported a significant increase in MCS over time in the remitting group. MCS scores in the continuously depressed group and PCS scores in both groups improved, albeit not significantly.
Another study [ 47 ] investigated whether chronic MD in a general population sample (NESARC) was associated with domain-specific reduced QoL (SF-12). They found that chronic MD was a significant risk factor for persistently reduced QoL in all domains and for the onset of reduced QoL at FU in all domains except for physical role.
Two population-based studies further differentiated between the depressive disorders. Analyzing MCS scores (NESARC), Rubio, Olfson, Villegas, Perez-Fuentes, Wang and Blanco [ 15 ] reported a significant increase in QoL for those who remitted from MD and from dysthymia relative to those who had a persistent disorder. Rhebergen, Beekman, de Graaf, Nolen, Spijker, Hoogendijk and Penninx [ 69 ] differentiated between people with MD, double depression or dysthymia at BL who remitted until FU relative to a group without a mental health diagnosis (NEMESIS). Physical health (SF-36) was lowest at BL for double depression, dysthymia and then the MD group. Over time, the MD and double depression groups improved significantly in their physical health, while the dysthymia group did not improve significantly. QoL was significantly lower relative to healthy comparisons for all depression groups at all waves. There were no significant differences regarding physical health trajectories over time among the depressive disorder groups.
Stegenga, Kamphuis, King, Nazareth and Geerlings [ 75 ] investigated more than two MD course groups over time (remitted, intermittent and chronic MD) in association with SF-12 MCS and PCS over time in a primary care-recruited sample with BL MD (Predict study). MCS increased over time in all groups, while changes in PCS were small. Compared to those who remitted, MCS at BL was significantly lower for the chronic course group. While the intermittent group also displayed a lower mean MCS at BL, the coefficient was not significant.
Three studies investigated changes in depressive symptom levels as the independent variable and changes in QoL as outcomes in adults.
One study found no significant association between an initial change in depressive symptoms and subsequent change in QoL (EQ-VAS) in older adults recruited in primary care [ 21 ]. The two other studies analyzed changes in depressive symptoms in samples with MD at BL [ 50 , 51 ]. Chung, Tso, Yeung and Li [ 50 ] found that changes in depressive symptom levels was associated with changes in several QoL domains (SF-36: general health, vitality, social functioning, mental health and MCS). Diehr, Derleth, McKenna, Martin, Bushnell, Simon and Patrick [ 51 ] investigated whether quartiles of change in depressive symptoms were associated with changes in QoL (SF-12, QLDS and WHOQOL-Bref). Those without any change in depressive symptoms generally showed no change in QoL. For all QoL domains and scores except for SF-12 PCS, improvement in depressive symptoms over time was associated with a significant increase in QoL, while a reduction in depressive symptoms was associated with a significant reduction in QoL. Those who had the largest reduction in depressive symptoms also had the largest improvement in QoL measures.
Anxiety as an independent variable and QoL as an outcome. Two publications used a general population sample (NESARC) to investigate incident anxiety disorders [ 14 ] and the remission of anxiety disorders [ 15 ] in association with SF-12 MCS. Both studies separated generalized anxiety disorder (GAD), social anxiety disorder (SAD), panic disorder (PD) and social phobia (SP). All incident disorders were associated with a significant reduction in QoL compared to people without a history of the specific disorders. When the analysis was restricted to incident cases without comorbidities, QoL levels were not significantly different compared to people without a history of any psychiatric disorder [ 14 ]. Those who remitted from SAD showed a significant increase in QoL compared to persistent cases. While QoL improved for all remitting anxiety disorders, change scores for PD and SP were not significant [ 15 ].
Another study investigated different courses (intermittent, chronic or remitting) of obsessive compulsive disorder (OCD) and course in QoL (EQ-5D) as well as a comparison group from the general population [ 68 ]. They found that the OCD groups mostly reported a lower QoL compared to the general population. Moreover, the course groups differed regarding their QoL over time, with remitters reporting small to moderate improvements compared to the chronic group.
One study investigated changes in anxiety symptoms in association with changes in all SF-36 domains and both summary scores over time in a sample with MD at BL [ 50 ]. Changes in anxiety symptoms were significantly associated with changes in bodily pain, general health and the mental health domain.
3.4. Overview of Studies on the Association between QoL as Independent Variable and Anxiety/Depression as Outcomes
Additionally, we identified publications operationalizing QoL as the independent variable and anxiety/depression as outcomes with details on all studies reported in Table 3 . Only one study reported on change in QoL over time and change/trajectories in mental health outcomes over time. This study operationalized change in QoL as a predictor of future change in depressive symptoms over time and reported that an initial improvement in EQ-VAS was associated with a future reduction in depressive symptoms in older adults [ 21 ].
Studies on QoL as the independent variable and depression/anxiety as outcome.
| First Author (Year) | Disorder or Symptoms Analyzed; QoL Domains Analyzed | Research Question | Methods | Results |
|---|---|---|---|---|
| Chou (2011) [ ] | Depressive sympt oms (CES-D-20 score); WHOQOL-Bref (total) | Whether QoL at BL is associated with depressive symptoms at FU. | Multiple regression | Lower QoL at BL was associated with higher depressive symptoms at FU. |
| De Almeida Fleck (2005) [ ] | Depression status (remission vs. no complete remission, CIDI and CES-D-20 cutoff >16); QLDS, WHOQOL-Bref (physical, psychological, social and environment), SF-12 (PCS, MCS) | Whether QoL at BL is associated with course of depression (complete remission vs. non-complete remission) in a depressed sample. | Stepwise multiple logistic regression | Disease-specific QoL measure at BL significantly predicted the remission of depression at FU (significant for QLDS). |
| Hajek (2015) [ ] | Depressive symptoms (GDS); EQ-VAS | Whether an initial change in QoL is associated with subsequent changes in depressive symptoms. | Vector autoregressive model | Initial changes in QoL were associated with a subsequent reduction in depression score (significant for total sample and women). |
| Hoertel (2017) [ ] | MD (according to AUDADIS-IV): SF-12v2 (PCS and MCS) | Whether QoL at BL predicted recurrence (vs. remission) or persistence (vs. remission) of MD over time. | Structural equation model | Lower QoL at BL was a predictor of risk of persistence (PCS and MCS) and recurrence of MDE over time. |
| Johansen (2007) [ ] | PTSD symptoms according to IES-15; WHOQOL-Bref (total) | Whether QoL predicted PTSD symptoms at FU. | Structural equation model | QoL did not significantly predict PTSD symptoms at FU. |
| Kuehner (2009) [ ] | Depressive symptoms (MADRS); WHOQOL (overall, physical, psychological, social and environmental) | Whether the lag of levels of QoL predicts future levels of depressive symptoms and whether the association differs by group (formerly depressed inpatients vs. community controls) | Time-lagged linear models | Lower levels of QoL were associated with higher future depressive symptoms (significant for physical, psychological, environmental and overall). The association was not moderated by group status. |
| Stegenga (2012) [ ] | MDD (CIDI); anxiety syndromes (panic disorder and others, PHQ); SF-12 (PCS) | (a) Whether “dysfunction” (i.e., reduced QoL) at BL (mildly reduced, moderately reduced or severely reduced; compared to no reduced QoL) predicts MDD onset over time. (b) Whether “dysfunction” (i.e., reduced QoL) at BL (mildly reduced, moderately reduced or severely reduced; compared to no reduced QoL) predicts anxiety syndrome onset over time. (c) Whether “dysfunction” (i.e., reduced QoL) at BL (mildly reduced, moderately reduced or severely reduced; compared to no reduced QoL) predicts onset of comorbid anxiety and MDD over time. | (a)–(c) Multinomial logistic regressions | (a) Dysfunction (i.e., reduced QoL) at BL was associated with higher odds of onset of MDD over time in the sample of people without a diagnosis at BL (significant for severely reduced QoL). (b) Dysfunction (i.e., reduced QoL) at BL was associated with higher odds of onset of anxiety syndrome over time in the sample of people without a diagnosis at BL (significant for moderately and severely reduced QoL). (c) Dysfunction (i.e., reduced QoL) at BL was associated with higher odds of onset of comorbid anxiety and depression over time in the sample of people without a diagnosis at BL (significant for mild, moderately and severely reduced QoL). |
| Wu (2016) [ ] | Elevated social anxiety symptoms (SASC cutoff 9); QOLS | Whether QoL is associated with changes in elevated social anxiety symptoms over time. | Generalized Estimating Equation | Higher QoL was associated with a decreased risk for developing elevated social anxiety symptoms over time. |
| Wu (2017) [ ] | Elevated depressive symptoms (according to CDI ≥19); QOLS | Whether QoL at BL is associated with elevated depressive symptoms at FU. | Multiple stepwise logistic regression | QoL at BL was not significantly related to depressive symptoms at FU. |
Abbreviations: CES-D-20 = Center for Epidemiological Studies Depression Scale 20; BL = baseline; FU = follow-up; QoL = quality of life; CIDI = Composite International Diagnostic Interview; QLDS = Quality of Life in Depression Scale; SF-12 = Short Form 12; PCS = Physical Component Score; MCS = Mental Component Score; GDS = Geriatric Depression Scale; EQ-VAS = EQ Visual Analogue Scale; MD = mental disorder; AUDADIS-IV = Alcohol Use Disorders and Associated Disabilities Interview Schedule; SF-12v2 = Short Form 12 Version 2; PTSD = post-traumatic stress disorder; IES-15 = Impact of Event Scale 15; MADRS = Montgomery–Åsberg Depression Rating Scale; MDD = major depressive disorder; PHQ = Patient Health Questionnaire; SASC = SpLD Assessment Standards Committee; QOLS = Quality of Life Scale; CDI = Children’s Depression Inventory.
3.5. Meta-Analyses on Anxiety, Depression and SF Summary Scores
In total, eight studies on adults were included in a supplementary meta-analyses of several research questions on SF PCS and MCS in association with anxiety and depressive disorders. Forest plots for the analyses are provided in the supplementary materials (Figures S1–S10) .
Differences in SF summary scores at FU among adults with and without depressive disorders at BL. Based on a pooling of four studies [ 45 , 49 , 52 , 54 ], those with depression at BL showed lower MCS scores at FU compared to a group without depression at BL with a large effect size (SMD = −0.96, 95% CI: −1.04 to −0.88, p < 0.001, I 2 = 0.0%). PCS scores at FU were lower for the depression group compared to the non-depression group with a medium effect size (SMD = −0.68, 95% CI: −1.06 to −0.30, p < 0.001, I 2 = 94.6%). Excluding the study rated “poor” in the quality/risk of bias assessment from the pooling did not substantially affect the results (MCS: SMD = −0.96, 95% CI: −1.03 to −0.88, p < 0.001, I 2 = 0.01%; PCS: SMD = −0.63, 95% CI: −1.08 to −0.19, p < 0.01, I 2 = 96.8%).
BL differences in SF summary scores among adults with MD at BL with and without remitting courses over time. Based on a pooling of two studies [ 19 , 84 ] of samples with MD at BL, those with persistent MD at FU had significantly lower MCS at BL (SMD = −0.25, 95% CI: −0.41 to −0.10, p = 0.001, I 2 = 74.95) and PCS scores at BL (SMD = −0.24, 95% CI: −0.39 to −0.09, p = 0.002, I 2 = 73.14) compared to those who achieved remission until FU. Effect sizes were small for both summary scores.
FU differences in SF summary scores among adults with depressive and anxiety disorders at BL with and without remitting courses . Based on the pooling of two studies [ 71 , 81 ] of samples with MD and/or dysthymia, the group where the disorder had persisted/a co-morbid condition was present/had a suicide attempt until FU had significantly lower MCS scores at FU compared to the group where the disorder had remitted without treatment until FU, with a medium effect size for depressive disorders (SMD = −0.59, 95% CI: −0.75 to −0.42, p < 0.001, I 2 = 37.72) and a small effect size for anxiety disorders (SMD = −0.44, 95% CI: −0.58 to −0.30, p < 0.001, I 2 = 58.87). The SMD for PCS scores at FU was negligible in terms of effect size for both disorder groups (depressive disorders: SMD = 0.02, 95% CI: −0.24 to 0.27, p = 0.90, I 2 = 73.65; anxiety disorders: SMD = −0.09, 95% CI: −0.17 to −0.01, p = 0.03, I 2 = 0.01).
4. Discussion
4.1. main results.
This review adds to the present literature by providing an overview of longitudinal observational studies investigating the association between depression, anxiety and QoL in samples without other specific illnesses or specific treatments. Additional meta-analyses investigated group differences according to SF MCS and PCS.
While a concise synthesis of all the identified studies is challenging due to heterogeneity, the following picture emerges from studies investigating change–change associations: before the onset of disorders, QoL is already lower in disorder groups in comparison to healthy comparisons. The onset of the disorders further reduces the QoL. Remission is associated with an increase in QoL, mostly to pre-morbid levels. Additionally, some studies show that remission patterns are relevant for QoL outcomes as well. Moreover, a bi-directional effect was reported, whereby QoL is also predictive of mental health outcomes.
Evidence for a bi-directional association as well as studies showing lower QoL across the entire course of the disorders (before onset, during disorder, after disorder) relative to a healthy comparison group seem to suggest that impairments in QoL may result from a certain pre-disorder vulnerability in these groups. Longitudinal studies using general population data have investigated different hypotheses on (QoL) impairments after remission of anxiety disorders and MD [ 87 , 88 ]. One hypothesis suggests that impairments after the illness episode reflect a pre-disorder vulnerability (vulnerability or trait hypothesis), while the another states that impairments develop during the mental health episode and remain as a residual after recovery (scar hypothesis). Generally, both studies favored the vulnerability hypothesis [ 87 , 88 ]. For subgroups with recurrent anxiety disorders, scarring effects were also found for mental functioning [ 88 ]. Yet, it has to be noted that it was not the aim of our review to gather evidence for these hypotheses using QoL as an indicator, which represents an opportunity for future research.
To be able to investigate possible domain-specific differences across studies, we aimed to conduct a meta-analysis on all studies on the same research question which reported on QoL subdomains (e.g., using WHOQOL and SF). However, as described in the Methods section above, only eight studies reported comparable information on different research questions and could be included in meta-analyses. Due to the limited number of studies included in each meta-analysis, the focus on SF MCS and PCS scores, and most studies reporting on depression, the results of the meta-analyses should be viewed with caution. Keeping this in mind, our results indicate that both mental and physical QoL are significantly impacted by anxiety and depressive disorders and that the course of the disorder is also relevant for QoL outcomes. Not surprisingly, effect sizes for MCS were larger compared to PCS for most research questions. A pooling of two studies on different courses of anxiety and depressive disorders found that effect sizes for MCS at FU were of moderate size for depressive (SMD = −0.59) and of small size for anxiety disorders (SMD = −0.44), while SMDs for PCS at FU were negligible in size.
Overall, effect sizes from meta-analyses ranged from negligible to large, and heterogeneity varied considerably (I 2 between 0% and 95%). Because of the small number of studies, possible influential study-level factors (e.g., setting, operationalization of the variables, length of FU) could not be investigated in further detail by means of a meta-regression, which remains a question for future research.
4.2. Implications for Future Research
Based on the results described and study heterogeneity discussed above, we provide recommendations for future research.
First recommendation: future research should differentiate between individual disorders and focus on anxiety disorders. The majority of the studies investigated depressive disorders or symptoms. On the level of individual disorders, most focused on MD, while two studies additionally reported on dysthymia [ 15 , 69 ]. One of these investigated double depression [ 69 ]. On the level of anxiety disorders, three publications differentiated between individual anxiety disorders within the same study [ 14 , 15 , 63 ]. While it was not possible to conduct a meta-analysis comparing different anxiety disorders in our case, individual studies suggest possible disorder-specific differences when analyzing changes in QoL over time: Rubio, Olfson, Villegas, Perez-Fuentes, Wang and Blanco [ 15 ] suggest that QoL significantly improved for those remitting from GAD and SAD (compared to non-remission). QoL improved for PD and SP as well, but differences in change scores were smaller and did not reach statistical significance. The incidences of all of these disorders were associated with a significant drop in QoL [ 14 ]. In summary, future longitudinal studies should focus on anxiety disorders and generally differentiate between individual disorders to investigate possible disorder-specific differences.
Second recommendation: future research should consider trajectories of disorders/change in symptoms and changes in QoL over time. We would have liked to include a meta-analysis of disorder trajectories and change scores in QoL over time. Because of the small, diverse number of studies on this association in general and the number of assumptions that would have had to have been made for a meta-analysis, we refrained from pooling effects for this research question. In total, 17 studies investigated changes in independent variables associated with changes in outcomes. This approach has several advantages. On the one hand, different disorder or symptom trajectories can be identified. Several studies reported that QoL outcomes differ according to disorder course and the degree of change in symptoms. The focus on the change in characteristics over time in future research could additionally reduce the problem of unobserved time-constant heterogeneity in observational studies when appropriate methods are applied [ 26 ].
Third recommendation: future research should investigate individual QoL domains. Several systematic reviews on cross-sectional studies found that effect sizes differed by QoL domains [ 32 , 89 ]. For example, Olatunji, Cisler and Tolin [ 89 ] reported that health and social functioning were most impaired for anxiety disorders (compared to non-clinical controls). Comparing individuals with diabetes and depressive symptoms to those with diabetes only, Schram, Baan and Pouwer [ 32 ] reported that while SF pain scores were mild to moderately impaired, role and social functioning displayed moderate to severe impairments in those with comorbid depressive symptoms. The other scores were moderately impaired. As described above in detail, a meta-analysis using all subdomains was not feasible in this review. Further research differentiating between QoL domains would thus allow future meta-analyses to investigate whether the observed domain-specific differences reported in previous reviews of cross-sectional data can be observed in longitudinal studies as well.
Fourth recommendation: future research should consider bi-directional effects. While investigating QoL as the outcome measure and anxiety/depression as independent variables seems relatively straightforward, ten studies investigated QoL as the independent variable and anxiety/depression as outcomes. In light of possible bi-directional effects and pre-existing vulnerability suggested by individual studies, future research considering QoL as an independent variable could inform a deeper understanding of this complex association.
4.3. Strengths and Limitations
A strength of this work is the transparent methodological process: the review was prospectively registered with PROSPERO and a study protocol was published [ 34 ]. Two reviewers were included in screening, data extraction and quality assessment processes. There were no limitations regarding the time or location of the publications. Moreover, all versions of the ICD/DSM and validated questionnaires were considered eligible to identify anxiety or depression. Another strength is the thorough literature search that enabled us to identify all relevant studies. Additionally, we did not limit the age range and were therefore able to shed light on studies investigating children/adolescents. Moreover, some studies could be pooled using random-effects meta-analyses, which allows for stronger conclusions regarding effect sizes compared to individual studies. Besides the content analysis, this review emphasizes difficulties in meta-analysis from observational, longitudinal studies. We hope that our work can facilitate discussion on this topic.
The study has some limitations. We did not limit our search to specific research questions, which led to the inclusion of heterogeneous studies. Heterogeneity particularly stemmed from the operationalization of the variables of interest. Due to this, a concise narrative synthesis of all results was not feasible. The positive aspect of this broad focus is that it allowed us to provide an overview of studies and research questions analyzed and to formulate more nuanced recommendations for future research. We have to acknowledge that there is an abundance of QoL assessments used in medicine and health sciences [ 37 ]. The list applied in this work was derived with respect to previous relevant reviews on QoL research. It was not designed to be fully comprehensive or exhaustive. Rather, it provided us with a working definition for this review and helped to enhance the transparency of our selection processes. Additionally, because we included validated QoL measures frequently used in research, we assume that exclusion would particularly have been the case for novel or study-specific measures. Finally, the focus on peer-reviewed literature means that studies in other languages and gray literature were not considered. Nonetheless, this focus on literature published in peer-reviewed journals should ensure a certain scientific quality.
5. Conclusions and Relevance for Clinical Practice
Overall, the results indicate that QoL is lower before the onset of anxiety and depressive disorders, further reduces upon onset of the disorders and generally improves with remission to pre-morbid levels. Moreover, disorder course (e.g., remitted, intermittent, chronic) seems to play an important role; however, only a few studies analyzed this. Changes in anxiety and depressive symptoms were also associated with changes in QoL over time. Meta-analyses found that effect sizes were larger for MCS relative to PCS, highlighting the relevance of differentiation between QoL domains. While our review identified some gaps in the current literature and made recommendations for future research, the following should be noted for clinical practice. On the one hand, an improvement in mental health is associated with better QoL, which emphasizes the relevance of support during the disorders. This is also shown by meta-analyses, which show that cognitive behavioral therapy additionally improves QoL [ 90 , 91 ]. Moreover, the results indicate reduced QoL even before disorder onset, highlighting the relevance of early preventive measures in vulnerable groups. In line with this, studies on school-based prevention programs show a significant reduction in anxiety and depressive symptoms [ 92 , 93 ], and psychosocial prevention programs may additionally improve QoL [ 94 ].
During the COVID-19 pandemic, it is of high relevance to tackle the arising challenges associated with this pandemic. For example, it is important to face the high prevalence rates of both depression and anxiety with appropriate measures.
Acknowledgments
The authors would like to thank Elzbieta Kuzma for her consultation (Albertinen-Haus Centre for Geriatrics and Gerontology, University of Hamburg, Hamburg, Germany; University of Exeter Medical School, Exeter, UK).
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph182212022/s1 , Table S1: detailed descriptive information for included studies ( n = 47); Figure S1: forest plot for differences in SF MCS at FU among adults with and without depressive disorders at BL; Figure S2: forest plot for differences in SF PCS at FU among adults with and without depressive disorders at BL; Figure S3: forest plot for differences in SF MCS at FU among adults with and without depressive disorders at BL (sensitivity analysis); Figure S4: forest plot for differences in SF PCS at FU among adults with and without depressive disorders at BL (sensitivity analysis); Figure S5: forest plot for BL differences in SF MCS among adults with MD at BL with and without remitting courses over time; Figure S6: forest plot for BL differences in SF PCS among adults with MD at BL with and without remitting courses over time; Figure S7: forest plot for FU differences in SF MCS among adults with depressive disorders at BL with and without remitting courses; Figure S8: forest plot for FU differences in SF PCS among adults with depressive disorders at BL with and without remitting courses; Figure S9: forest plot for FU differences in SF MCS among adults with anxiety disorders at BL with and without remitting courses; Figure S10: forest plot for FU differences in SF PCS among adults with anxiety disorders at BL with and without remitting courses.
Author Contributions
J.K.H.: conceptualization of research question; development of search strategy; study screening and selection; risk of bias/quality assessment; study synthesis; writing—original draft, review and editing; H.-H.K.: conceptualization of research question; writing—review and editing; E.Q.: study screening and selection; risk of bias/quality assessment; writing—review and editing; A.H.: conceptualization of research question; development of search strategy; study screening and selection (third party); study synthesis; writing—review and editing. All authors have read and agreed to the published version of the manuscript.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
A narrative literature review of depression following traumatic brain injury: prevalence, impact, and management challenges
Affiliations.
- 1 Department of Physical Medicine and Rehabilitation.
- 2 Department of Rehabilitation Counseling, University of Texas Southwestern Medical Center, Dallas, TX.
- 3 Department of Neuroscience.
- 4 Safar Center for Resuscitation Research, University of Pittsburgh, Pittsburgh, PA, USA.
- PMID: 28652833
- PMCID: PMC5476717
- DOI: 10.2147/PRBM.S113264
Depression is one of the most common conditions to emerge after traumatic brain injury (TBI), and despite its potentially serious consequences it remains undertreated. Treatment for post-traumatic depression (PTD) is complicated due to the multifactorial etiology of PTD, ranging from biological pathways to psychosocial adjustment. Identifying the unique, personalized factors contributing to the development of PTD could improve long-term treatment and management for individuals with TBI. The purpose of this narrative literature review was to summarize the prevalence and impact of PTD among those with moderate to severe TBI and to discuss current challenges in its management. Overall, PTD has an estimated point prevalence of 30%, with 50% of individuals with moderate to severe TBI experiencing an episode of PTD in the first year after injury alone. PTD has significant implications for health, leading to more hospitalizations and greater caregiver burden, for participation, reducing rates of return to work and affecting social relationships, and for quality of life. PTD may develop directly or indirectly as a result of biological changes after injury, most notably post-injury inflammation, or through psychological and psychosocial factors, including pre injury personal characteristics and post-injury adjustment to disability. Current evidence for effective treatments is limited, although the strongest evidence supports antidepressants and cognitive behavioral interventions. More personalized approaches to treatment and further research into unique therapy combinations may improve the management of PTD and improve the health, functioning, and quality of life for individuals with TBI.
Keywords: antidepressants; depression; inflammation; rehabilitation; traumatic brain injury.
PubMed Disclaimer
Conflict of interest statement
Disclosure The authors report no conflicts of interest in this work.
Conceptual diagram of inflammatory-induced PTD.…
Conceptual diagram of inflammatory-induced PTD. Notes: A conceptual diagram of potential pathways by…
Similar articles
- The effects of post-traumatic depression on cognition, pain, fatigue, and headache after moderate-to-severe traumatic brain injury: a thematic review. Kumar RG, Gao S, Juengst SB, Wagner AK, Fabio A. Kumar RG, et al. Brain Inj. 2018;32(4):383-394. doi: 10.1080/02699052.2018.1427888. Epub 2018 Jan 22. Brain Inj. 2018. PMID: 29355429 Review.
- The impact of pre-injury anticoagulation therapy in the older adult patient experiencing a traumatic brain injury: A systematic review. Smith K, Weeks S. Smith K, et al. JBI Libr Syst Rev. 2012;10(58):4610-4621. doi: 10.11124/jbisrir-2012-429. JBI Libr Syst Rev. 2012. PMID: 27820526
- Genetic Influences in Traumatic Brain Injury. Bennett ER, Reuter-Rice K, Laskowitz DT. Bennett ER, et al. In: Laskowitz D, Grant G, editors. Translational Research in Traumatic Brain Injury. Boca Raton (FL): CRC Press/Taylor and Francis Group; 2016. Chapter 9. In: Laskowitz D, Grant G, editors. Translational Research in Traumatic Brain Injury. Boca Raton (FL): CRC Press/Taylor and Francis Group; 2016. Chapter 9. PMID: 26583176 Free Books & Documents. Review.
- Models of Posttraumatic Brain Injury Neurorehabilitation. Failla MD, Wagner AK. Failla MD, et al. In: Kobeissy FH, editor. Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Boca Raton (FL): CRC Press/Taylor & Francis; 2015. Chapter 35. In: Kobeissy FH, editor. Brain Neurotrauma: Molecular, Neuropsychological, and Rehabilitation Aspects. Boca Raton (FL): CRC Press/Taylor & Francis; 2015. Chapter 35. PMID: 26269917 Free Books & Documents. Review.
- Variants of SLC6A4 in depression risk following severe TBI. Failla MD, Burkhardt JN, Miller MA, Scanlon JM, Conley YP, Ferrell RE, Wagner AK. Failla MD, et al. Brain Inj. 2013 Jun;27(6):696-706. doi: 10.3109/02699052.2013.775481. Epub 2013 Apr 5. Brain Inj. 2013. PMID: 23672445
- Good Health-Related Quality of Life in Older Patients One Year after mTBI despite Incomplete Recovery: An Indication of the Disability Paradox? Coffeng SM, Abdulle AE, van der Horn HJ, de Koning ME, Ter Maaten JC, Spikman JM, van der Naalt J. Coffeng SM, et al. J Clin Med. 2024 May 1;13(9):2655. doi: 10.3390/jcm13092655. J Clin Med. 2024. PMID: 38731184 Free PMC article.
- Branching out: Feasibility of examining the effects of greenspace on mental health after traumatic brain injury. Holland AB, Cohen A, Faerman A, Nelson TA, Wright B, Kumar RG, Ngan E, Herrera S, Juengst SB. Holland AB, et al. Dialogues Health. 2023 Mar 25;2:100129. doi: 10.1016/j.dialog.2023.100129. eCollection 2023 Dec. Dialogues Health. 2023. PMID: 38515481 Free PMC article.
- Self-directed versus peer-supported digital self-management programmes for mental and sexual wellbeing after acquired brain injury (HOPE4ABI): protocol for a feasibility randomised controlled trial. Wright H, Walker-Clarke A, Drummond A, Kidd L, Yeates G, Williams D, McWilliams D, Clyne W, Clark CCT, Kimani P, Turner A. Wright H, et al. Pilot Feasibility Stud. 2023 Nov 29;9(1):194. doi: 10.1186/s40814-023-01421-z. Pilot Feasibility Stud. 2023. PMID: 38031132 Free PMC article.
- Body Image and Emotional Status in Patients with Acquired Brain Injury. Lo Buono V, Corallo F, Bonanno L, Quartarone A, De Cola MC. Lo Buono V, et al. J Clin Med. 2023 Jun 15;12(12):4070. doi: 10.3390/jcm12124070. J Clin Med. 2023. PMID: 37373763 Free PMC article.
- Measuring Intolerance of Uncertainty After Acquired Brain Injury: Factor Structure, Reliability, and Validity of the Intolerance of Uncertainty Scale-12. Kusec A, Murphy FC, Peers PV, Manly T. Kusec A, et al. Assessment. 2024 Jun;31(4):794-811. doi: 10.1177/10731911231182693. Epub 2023 Jun 26. Assessment. 2024. PMID: 37357954 Free PMC article.
- Hibbard MR, Uysal S, Kepler K, Bogdany J, Silver J. Axis I psychopathology in individuals with traumatic brain injury. J Head Trauma Rehabil. 1998;13(4):24–39. - PubMed
- Jorge RE, Robinson RG, Moser D, Tateno A, Crespo-Facorro B, Arndt S. Major depression following traumatic brain injury. Arch Gen Psychiatry. 2004;61(1):42–50. - PubMed
- Bombardier CH, Fann JR, Temkin NR, Esselman PC, Barber J, Dikmen SS. Rates of major depressive disorder and clinical outcomes following traumatic brain injury. JAMA. 2010;303(19):1938–1945. - PMC - PubMed
- Strakowski SM, Adler CM, Delbello MP. Is depression simply a nonspecific response to brain injury? Curr Psychiatry Rep. 2013;15(9):386. - PMC - PubMed
- Green BN, Johnson CD, Adams A. Writing narrative literature reviews for peer-reviewed journals: secrets of the trade. J Chiropr Med. 2006;5(3):101–117. - PMC - PubMed
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Dove Medical Press
- Europe PubMed Central
- PubMed Central
Other Literature Sources
- scite Smart Citations

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- Log in/Log out (Opens in new window)
- All content
- Rural Alaska
- Crime & Courts
- Alaska Legislature
- ADN Politics Podcast
- National Opinions
- Letters to the Editor
- Nation/World
- Film and TV
- Outdoors/Adventure
- High School Sports
- UAA Athletics
- National Sports
- Food and Drink
- Visual Stories
- Alaska Journal of Commerce (Opens in new window)
- The Arctic Sounder
- The Bristol Bay Times
- Today's Paper (Opens in new window)
- Legal Notices (Opens in new window)
- Peak 2 Peak Events (Opens in new window)
- Educator of the Year (Opens in new window)
- Celebrating Nurses (Opens in new window)
- Top 40 Under 40 (Opens in new window)
- Alaska Spelling Bee (Opens in new window)
- Alaska Craft Brew Festival
- Best of Alaska
- Spring Career Fair (Opens in new window)
- Achievement in Business
- Youth Summit Awards
- Highland Games VIP Experience Giveaway
- Teacher of the Month
- 2024 Alaska Summer Camps Guide (Opens in new window)
- 2024 Graduation (Opens in new window)
- Alaska Visitors Guide 2024 (Opens in new window)
- Bear Paw Festival 2024 (Opens in new window)
- 2023 Best of Alaska (Opens in new window)
- Alaska Health Care (Opens in new window)
- On the Move AK (Opens in new window)
- Senior Living in Alaska (Opens in new window)
- Youth Summit Awards (Opens in new window)
- Alaska Visitors Guide
- ADN Store (Opens in new window)
- Classifieds (Opens in new window)
- Jobs (Opens in new window)
- Place an Ad (Opens in new window)
- Customer Service
- Sponsored Content
Book review: Pulling traditional legends into the modern world, ‘Chickaloonies 2′ is a giant leap forward
A page from from "Chickaloonies 2: Watering Ways" from Dimi Macheras and Casey Silver
“Chickaloonies 2: Watering Ways”
Dimi Macheras and Casey Silver; 80% Studios, 2024; 268 pages; $39.99
“You locked away your stories,” Drasco, a bear warrior who is a central character in “Chickaloonies 2: Watering Ways,” tells the mayor and citizens of a post-apocalyptic Palmer, Alaska. “You locked away your language, you locked away your culture. You’ve severed the source of your strength.”
Pointing at the exhibits in a shuttered Ahtna cultural center, Drasco continues, “These items are not meant to be locked away. They are alive!”
It’s the pivotal scene in a story that hinges on the recovery of culture as a means of overcoming challenges. In this action-packed fantasy story set in a Palmer that has been laid to waste by giant flying creatures called “moose-quitoes,” the challenge is getting to the source where the plague of monstrous insects is hatching from, and finding a way of stopping them. This will require looking finding guidance in the accumulated lore of the Ahtna.
“Chickaloonies,” an Alaska Native-rooted graphic novel series, is the brainchild of Dimi Macheras and Casey Silver. Macheras grew up in Chickaloon, enthralled by the traditional stories his late grandmother, revered elder Katherine Wade, and his late mother Patricia Wade — both Ahtna culture bearers — told him in his childhood. Growing up, he aided his mother in her work by illustrating the legends she preserved. Silver, originally from Rhode Island, is a talented artist and storyteller himself. Macheras and Silver share a comics partnership called 80% Studios, and “Chickaloonies” is their flagship work.
A page from from "Chickaloonies 2: Watering Ways" from Dimi Macheras and Casey Silver.
The first volume in the series, “First Frost,” was published in 2021 and introduced the primary characters. Sasquatch E. Moji is a 13-year-old behemoth of a child who speaks solely in emojis. Mister Yelly, a year younger and considerably smaller, is a bit of a scamp who depends on his older pal in a pinch but isn’t lacking in bravery himself.
The opening tale, which was fairly brief, took place in Chickaloon Village at a time when light had gone from the sky. It ended with Moji and Yelly, counseled by their grandmother, embarking on a quest atop a berry-powered snowmachine named Boba to find their missing cousin Vally. It was a brief and fun little fantasy, well-conceived with expressive and colorful manga-inspired art, but it merely set the stage.
“Watering Ways” is a giant leap forward for Macheras and Silver. It’s significantly longer and far more ambitious than its predecessor. The story opens with Moji and Yelly crossing a snow-covered landscape under a darkened sky as they come across ice creatures standing rigidly in a valley with human forms contained within them. Frightened by the sight, they hurriedly make for Palmer, where they find the city all but shut down. Quickly they learn of the moose-quitoes — giant, flying moose-mosquito hybrids spreading an unknown sickness among the residents — and are drawn into the mystery of where the creatures come from and how to combat them.
After encountering a storyteller named Baca, they visit Drasco for help finding their cousin. Initially reluctant, though not for long, Drasco instead sends them on their way and they return to the besieged Palmer. There these four and other key players assemble, and the story takes form as Moji and Yelly join in the quest to defeat the moose-quitoes.
“Watering Ways” is a standalone episode within the broader story arc of the series. It’s a fast-paced adventure that weaves Ahtna legends into an action-packed quest to save Palmer from the insect infestation that has overrun the town. It’s a tale filled with excitement, humor, entertaining characters, conflicts, camaraderie and a welcoming spirit that will appeal not just to the young readers who will make up its primary audience, but also to adults looking for a good yarn to escape into.
Macheras and Silver share both writing and artistic duties, which leads to a strong fusion of imagery and words. Often, and especially toward the end, the artwork alone tells the story. As artists, the duo use manga as their launching point, but their style reaches well beyond the form. Their use of deep colors creates a mood perfectly suited for the events occurring on the page. Echoes of the seminal 1960s and 1970s work of famed Marvel and DC artist Jack Kirby also surface subtly in a few panels, tastefully so and not as mimicry, connecting the duo’s work to the long, storied history of American comics.
“Chickaloonies” is a lot of fun, and it’s instructive along the way. Macheras and Silver draw from Ahtna lore to create an Alaska Native epic of their own. Stories passed through generations surface throughout the two books, offering key insight at critical points as the plot line unfolds. This knowledge is central to the narrative, and by including it, Macheras carries forward the work of his mother and grandmother, updating and adding to a tradition of oral literature and making it vibrant for modern readers.
The duo are working as part of a collective of Alaska comics producers operating under the name Luk’ae Tse’ Taas Comics (Fish Head Soup Comics) that is focused on bringing both Alaska themes and Native cultures to the world of graphic fiction. As a work geared toward younger readers, the “Chickaloonies” series is the most accessible of those being produced and provides an easy entry point for readers just getting acquainted with the shared universe that the creators are contributing to. It’s a new direction for Alaska arts and literature, and as this book makes clear, its potential is only beginning to be explored.
[ With the Luk’ae Tse’ Taas Comics collective, Alaska visual artists help build a broader universe ]
“When you embark on the journey of rediscovering the knowledge of your culture, listen for the voices of the ancestors,” Macheras and Silver write in a brief afterword to the book. “And remember the watering ways, as a beacon to help you find your way back home.” It’s the perfect coda for “Chickaloonies 2,” which pulls traditional legends into the modern world and crafts something at once both deeply rooted and intriguingly new.
David James
David A. James is a Fairbanks-based freelance writer, and editor of the Alaska literary collection “Writing on the Edge.” He can be reached at [email protected].
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Author Biographies
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Factors, prediction, and explainability of vehicle accident risk due to driving behavior through machine learning: a systematic literature review, 2013–2023.

Share and Cite
Lacherre, J.; Castillo-Sequera, J.L.; Mauricio, D. Factors, Prediction, and Explainability of Vehicle Accident Risk Due to Driving Behavior through Machine Learning: A Systematic Literature Review, 2013–2023. Computation 2024 , 12 , 131. https://doi.org/10.3390/computation12070131
Lacherre J, Castillo-Sequera JL, Mauricio D. Factors, Prediction, and Explainability of Vehicle Accident Risk Due to Driving Behavior through Machine Learning: A Systematic Literature Review, 2013–2023. Computation . 2024; 12(7):131. https://doi.org/10.3390/computation12070131
Lacherre, Javier, José Luis Castillo-Sequera, and David Mauricio. 2024. "Factors, Prediction, and Explainability of Vehicle Accident Risk Due to Driving Behavior through Machine Learning: A Systematic Literature Review, 2013–2023" Computation 12, no. 7: 131. https://doi.org/10.3390/computation12070131
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

COMMENTS
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social determinants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
According to the fall 2007 American College Health Association-National College Health Assessment ( 1), a national survey of approximately 20,500 college students on 39 campuses, 43.2% of the students reported "feeling so depressed it was difficult to function" at least once in the past 12 months.More than 3,200 university students reported being diagnosed as having depression, with 39.2% of ...
This review sought to: (1) provide a synopsis of key factors associated with outcomes in MDD, and (2) synthesize the existing literature on novel treatment strategies for depression. A literature ...
Depression is a common and debilitating mental health condition whose underlying aetiology and pathophysiology is still relatively poorly understood. ... Herrmann LL, Le Masurier M, Ebmeier KP (2008) White matter hyperintensities in late life depression: A systematic review. Journal of Neurology, Neurosurgery, and Psychiatry 79(6): 619-624 ...
A review of the literature on the selegiline transdermal system: an effective and well-tolerated monoamine oxidase inhibitor for the treatment of depression. Prim Care Companion J Clin Psychiatry. 2008; 10 :25-30.
The review was registered with PROSPERO (CRD42020207203). 17 studies were included: 12 systematic reviews and meta-analyses, 1 collaborative meta-analysis, 1 meta-analysis of large cohort studies ...
A systematic literature review of the PubMed and MEDLINE databases was performed to identify articles on the prevalence of MDD and its correlates. The search was restricted to manuscripts published between January 2001 and December 2018. ... According to the Global Burden of Disease study, depression is the fourth leading cause of disability ...
We included 470 documents in this literature review. The findings showed that there are a plethora of risk and protective factors (relating to biological, psychological, and social determinants) that are related to depression; these determinants are interlinked and influence depression outcomes through a web of causation.
Depression: A Literature Review on Diagnosis, Subtypes, Patterns of Recovery, and. Psychotherapeutic Models. Mark Widdowson. Abstract. This art icle summarizes dat a on the preva-
Objective: The mental health of U.S. college students is a growing public health concern. Particularly alarming is the prevalence of depression and risk of suicide in this cohort. Methods: A literature review of PsycINFO, MEDLINE, and CINAHL databases was conducted in order to identify and evaluate depression and treatment outcomes among U.S. college students since 1990.
Depression is a common and serious mental disorder that affects millions of people worldwide. How to treat it effectively and achieve full recovery is a crucial question for both patients and clinicians. This systematic review summarizes the evidence on various treatment options for depression, including pharmacological, psychological, and combined therapies. It also provides recommendations ...
depression and risk of suicide in this cohort. Methods: A literature review of PsycINFO, MEDLINE, and CINAHL databases was con-ducted in order to identify and evaluate depression and treat-ment outcomes among U.S. col-lege students since 1990. Results: Four studies documenting de-pression and treatment outcomes among U.S. college students were
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions. 2. Materials and Methods. We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years.
Abstract. Major depression is a mood disorder characterized by a sense of inadequacy, despondency, decreased activity, pessimism, anhedonia and sadness where these symptoms severely disrupt and ...
Depression is a leading cause of disability worldwide (World Health Organization [WHO], 2020), with a 12-month prevalence in the United States of approximately 7% and a lifetime prevalence of approximately 16% (Kessler et al., 2003).While 40%-60% of the affected individuals will experience single-episode, non-recurrent depression followed by high-end-state functioning (Eaton et al., 2008 ...
Literature Review on Depression. Depression alters one's mood, making one feel sad and lose interest in people, events, and objects, and thus may cause physical and emotional problems. It may involve treatment in the long run if it persists, which includes medication and psychotherapy. This paper will focus on a detailed summary of other ...
Introduction. Globally, mental illness affects approximately 22% of the population [].Depression is the most prevalent psychiatric disorder, which affects more than 300 million individuals [].It is an incapacitating disorder, responsible for most of the 800,000 annual suicides [].Along with population growth and aging, the number of individuals with depression has also increased considerably ...
Some studies 35,116 and a literature review by Linton 128 have suggested that depression has a greater impact than other clinical factors on outcomes, especially functional impairment, in patients with pain, and that neglecting to treat the depression accounts for some of the pain treatment failures. 38,52 Patients with depression and chronic ...
The purpose of our literature review was to understand the state of research related to social media and depression within the past 10 years. We were particularly interested in understanding what ...
Given the inconsistencies in the provision of psychological interventions identified in the literature and through reports, this report aimed to (1) review existing recommendations on psychosocial interventions to address UASC mental health needs, (2) examine the current mental health provision within health and social care in England from service providers' perspectives, and (3) synthesise ...
Background: Despite the great burden of depression on sufferers and society, there is a lack of reliable information regarding the full range of psychosocial difficulties associated with depression and their related variables. This systematic review aimed to demonstrate the utility of the International Classification of Functioning, Disability and Health (ICF) in describing the psychosocial ...
Depression and generalized anxiety are 2 of the most common mental health concerns in youth. 14 Depressive symptoms, which include feelings of sadness, loss of interest and pleasure in activities, as well as disruption to regulatory functions such as sleep and appetite, 15 could be elevated during the pandemic as a result of social isolation ...
Qualitative literature related to depression was examined through a search of peer-reviewed academic journals and solicitation of non-peer-reviewed programmatic reports related to mental health programs. The literature review followed PRISMA guidelines (Moher et al., 2009) (See Supplemental Material for PRISMA checklist). The first search was ...
Literature review 29: Osteoporosis and fractures: Hazard ratio = 1.88 (95% CI, 1.48 to 2.39) for fragility fracture ... Li KX, Loshak H. Pharmacogenomic testing in depression: a review of clinical ...
Perimenopausal depression (PMD) is a psychological disorder that occurs in women during perimenopause. In addition to the common clinical symptoms of depression, it often manifests as a perimenopausal complication, and its notable cause is the decline in estrogen levels. Despite numerous studies and trials confirming the benefits of estrogen replacement therapy (ERT) for PMD, ERT remains ...
Tropical depression 2 is set to strengthen into a tropical storm later Friday night and a Category 1 hurricane by the time it reaches the Windward Islands late Sunday. National Hurricane Center A ...
This review adds to the present literature by providing an overview of longitudinal observational studies investigating the association between depression, anxiety and QoL in samples without other specific illnesses or specific treatments. ... Pouwer F. Depression and quality of life in patients with diabetes: A systematic review from the ...
Depression is one of the most common conditions to emerge after traumatic brain injury (TBI), and despite its potentially serious consequences it remains undertreated. ... The purpose of this narrative literature review was to summarize the prevalence and impact of PTD among those with moderate to severe TBI and to discuss current challenges in ...
The follow-up book in the series from Dimi Macheras and Casey Silver continues a new direction for Alaska arts and literature under the Luk'ae Tse' Taas Comics banner.
A systematic review of the literature produced between 2013 and July 2023 on factors, prediction algorithms, and explainability methods to predict the risk of traffic accidents was carried out. Factors were categorized into five domains, and the most commonly used predictive algorithms and explainability methods were determined.