Writing about COVID-19 in a college admission essay
by: Venkates Swaminathan | Updated: September 14, 2020
Print article

For students applying to college using the CommonApp, there are several different places where students and counselors can address the pandemic’s impact. The different sections have differing goals. You must understand how to use each section for its appropriate use.

The CommonApp COVID-19 question
First, the CommonApp this year has an additional question specifically about COVID-19 :
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces. Please use this space to describe how these events have impacted you.
This question seeks to understand the adversity that students may have had to face due to the pandemic, the move to online education, or the shelter-in-place rules. You don’t have to answer this question if the impact on you wasn’t particularly severe. Some examples of things students should discuss include:
- The student or a family member had COVID-19 or suffered other illnesses due to confinement during the pandemic.
- The candidate had to deal with personal or family issues, such as abusive living situations or other safety concerns
- The student suffered from a lack of internet access and other online learning challenges.
- Students who dealt with problems registering for or taking standardized tests and AP exams.
Jeff Schiffman of the Tulane University admissions office has a blog about this section. He recommends students ask themselves several questions as they go about answering this section:
- Are my experiences different from others’?
- Are there noticeable changes on my transcript?
- Am I aware of my privilege?
- Am I specific? Am I explaining rather than complaining?
- Is this information being included elsewhere on my application?
If you do answer this section, be brief and to-the-point.
Counselor recommendations and school profiles
Second, counselors will, in their counselor forms and school profiles on the CommonApp, address how the school handled the pandemic and how it might have affected students, specifically as it relates to:
- Grading scales and policies
- Graduation requirements
- Instructional methods
- Schedules and course offerings
- Testing requirements
- Your academic calendar
- Other extenuating circumstances
Students don’t have to mention these matters in their application unless something unusual happened.
Writing about COVID-19 in your main essay
Write about your experiences during the pandemic in your main college essay if your experience is personal, relevant, and the most important thing to discuss in your college admission essay. That you had to stay home and study online isn’t sufficient, as millions of other students faced the same situation. But sometimes, it can be appropriate and helpful to write about something related to the pandemic in your essay. For example:
- One student developed a website for a local comic book store. The store might not have survived without the ability for people to order comic books online. The student had a long-standing relationship with the store, and it was an institution that created a community for students who otherwise felt left out.
- One student started a YouTube channel to help other students with academic subjects he was very familiar with and began tutoring others.
- Some students used their extra time that was the result of the stay-at-home orders to take online courses pursuing topics they are genuinely interested in or developing new interests, like a foreign language or music.
Experiences like this can be good topics for the CommonApp essay as long as they reflect something genuinely important about the student. For many students whose lives have been shaped by this pandemic, it can be a critical part of their college application.
Want more? Read 6 ways to improve a college essay , What the &%$! should I write about in my college essay , and Just how important is a college admissions essay? .

Homes Nearby
Homes for rent and sale near schools

How our schools are (and aren't) addressing race

The truth about homework in America

What should I write my college essay about?
What the #%@!& should I write about in my college essay?
Yes! Sign me up for updates relevant to my child's grade.
Please enter a valid email address
Thank you for signing up!
Server Issue: Please try again later. Sorry for the inconvenience
- CBSE Class 10th
- CBSE Class 12th
- UP Board 10th
- UP Board 12th
- Bihar Board 10th
- Bihar Board 12th
Top Schools
- Top Schools in India
- Top Schools in Delhi
- Top Schools in Mumbai
- Top Schools in Chennai
- Top Schools in Hyderabad
- Top Schools in Kolkata
- Top Schools in Pune
- Top Schools in Bangalore
Products & Resources
- JEE Main Knockout April
- Free Sample Papers
- Free Ebooks
- NCERT Notes
- NCERT Syllabus
- NCERT Books
- RD Sharma Solutions
- Navodaya Vidyalaya Admission 2024-25
- NCERT Solutions
- NCERT Solutions for Class 12
- NCERT Solutions for Class 11
- NCERT solutions for Class 10
- NCERT solutions for Class 9
- NCERT solutions for Class 8
- NCERT Solutions for Class 7
- JEE Main 2024
- MHT CET 2024
- JEE Advanced 2024
- BITSAT 2024
- View All Engineering Exams
- Colleges Accepting B.Tech Applications
- Top Engineering Colleges in India
- Engineering Colleges in India
- Engineering Colleges in Tamil Nadu
- Engineering Colleges Accepting JEE Main
- Top IITs in India
- Top NITs in India
- Top IIITs in India
- JEE Main College Predictor
- JEE Main Rank Predictor
- MHT CET College Predictor
- AP EAMCET College Predictor
- GATE College Predictor
- KCET College Predictor
- JEE Advanced College Predictor
- View All College Predictors
- JEE Advanced Cutoff
- JEE Main Cutoff
- MHT CET Result 2024
- JEE Advanced Result
- Download E-Books and Sample Papers
- Compare Colleges
- B.Tech College Applications
- AP EAMCET Result 2024
- MAH MBA CET Exam
- View All Management Exams
Colleges & Courses
- MBA College Admissions
- MBA Colleges in India
- Top IIMs Colleges in India
- Top Online MBA Colleges in India
- MBA Colleges Accepting XAT Score
- BBA Colleges in India
- XAT College Predictor 2024
- SNAP College Predictor
- NMAT College Predictor
- MAT College Predictor 2024
- CMAT College Predictor 2024
- CAT Percentile Predictor 2024
- CAT 2024 College Predictor
- Top MBA Entrance Exams 2024
- AP ICET Counselling 2024
- GD Topics for MBA
- CAT Exam Date 2024
- Download Helpful Ebooks
- List of Popular Branches
- QnA - Get answers to your doubts
- IIM Fees Structure
- AIIMS Nursing
- Top Medical Colleges in India
- Top Medical Colleges in India accepting NEET Score
- Medical Colleges accepting NEET
- List of Medical Colleges in India
- List of AIIMS Colleges In India
- Medical Colleges in Maharashtra
- Medical Colleges in India Accepting NEET PG
- NEET College Predictor
- NEET PG College Predictor
- NEET MDS College Predictor
- NEET Rank Predictor
- DNB PDCET College Predictor
- NEET Result 2024
- NEET Asnwer Key 2024
- NEET Cut off
- NEET Online Preparation
- Download Helpful E-books
- Colleges Accepting Admissions
- Top Law Colleges in India
- Law College Accepting CLAT Score
- List of Law Colleges in India
- Top Law Colleges in Delhi
- Top NLUs Colleges in India
- Top Law Colleges in Chandigarh
- Top Law Collages in Lucknow
Predictors & E-Books
- CLAT College Predictor
- MHCET Law ( 5 Year L.L.B) College Predictor
- AILET College Predictor
- Sample Papers
- Compare Law Collages
- Careers360 Youtube Channel
- CLAT Syllabus 2025
- CLAT Previous Year Question Paper
- NID DAT Exam
- Pearl Academy Exam
Predictors & Articles
- NIFT College Predictor
- UCEED College Predictor
- NID DAT College Predictor
- NID DAT Syllabus 2025
- NID DAT 2025
- Design Colleges in India
- Top NIFT Colleges in India
- Fashion Design Colleges in India
- Top Interior Design Colleges in India
- Top Graphic Designing Colleges in India
- Fashion Design Colleges in Delhi
- Fashion Design Colleges in Mumbai
- Top Interior Design Colleges in Bangalore
- NIFT Result 2024
- NIFT Fees Structure
- NIFT Syllabus 2025
- Free Design E-books
- List of Branches
- Careers360 Youtube channel
- IPU CET BJMC
- JMI Mass Communication Entrance Exam
- IIMC Entrance Exam
- Media & Journalism colleges in Delhi
- Media & Journalism colleges in Bangalore
- Media & Journalism colleges in Mumbai
- List of Media & Journalism Colleges in India
- CA Intermediate
- CA Foundation
- CS Executive
- CS Professional
- Difference between CA and CS
- Difference between CA and CMA
- CA Full form
- CMA Full form
- CS Full form
- CA Salary In India
Top Courses & Careers
- Bachelor of Commerce (B.Com)
- Master of Commerce (M.Com)
- Company Secretary
- Cost Accountant
- Charted Accountant
- Credit Manager
- Financial Advisor
- Top Commerce Colleges in India
- Top Government Commerce Colleges in India
- Top Private Commerce Colleges in India
- Top M.Com Colleges in Mumbai
- Top B.Com Colleges in India
- IT Colleges in Tamil Nadu
- IT Colleges in Uttar Pradesh
- MCA Colleges in India
- BCA Colleges in India
Quick Links
- Information Technology Courses
- Programming Courses
- Web Development Courses
- Data Analytics Courses
- Big Data Analytics Courses
- RUHS Pharmacy Admission Test
- Top Pharmacy Colleges in India
- Pharmacy Colleges in Pune
- Pharmacy Colleges in Mumbai
- Colleges Accepting GPAT Score
- Pharmacy Colleges in Lucknow
- List of Pharmacy Colleges in Nagpur
- GPAT Result
- GPAT 2024 Admit Card
- GPAT Question Papers
- NCHMCT JEE 2024
- Mah BHMCT CET
- Top Hotel Management Colleges in Delhi
- Top Hotel Management Colleges in Hyderabad
- Top Hotel Management Colleges in Mumbai
- Top Hotel Management Colleges in Tamil Nadu
- Top Hotel Management Colleges in Maharashtra
- B.Sc Hotel Management
- Hotel Management
- Diploma in Hotel Management and Catering Technology
Diploma Colleges
- Top Diploma Colleges in Maharashtra
- UPSC IAS 2024
- SSC CGL 2024
- IBPS RRB 2024
- Previous Year Sample Papers
- Free Competition E-books
- Sarkari Result
- QnA- Get your doubts answered
- UPSC Previous Year Sample Papers
- CTET Previous Year Sample Papers
- SBI Clerk Previous Year Sample Papers
- NDA Previous Year Sample Papers
Upcoming Events
- NDA Application Form 2024
- UPSC IAS Application Form 2024
- CDS Application Form 2024
- CTET Admit card 2024
- HP TET Result 2023
- SSC GD Constable Admit Card 2024
- UPTET Notification 2024
- SBI Clerk Result 2024
Other Exams
- SSC CHSL 2024
- UP PCS 2024
- UGC NET 2024
- RRB NTPC 2024
- IBPS PO 2024
- IBPS Clerk 2024
- IBPS SO 2024
- Top University in USA
- Top University in Canada
- Top University in Ireland
- Top Universities in UK
- Top Universities in Australia
- Best MBA Colleges in Abroad
- Business Management Studies Colleges
Top Countries
- Study in USA
- Study in UK
- Study in Canada
- Study in Australia
- Study in Ireland
- Study in Germany
- Study in China
- Study in Europe
Student Visas
- Student Visa Canada
- Student Visa UK
- Student Visa USA
- Student Visa Australia
- Student Visa Germany
- Student Visa New Zealand
- Student Visa Ireland
- CUET PG 2024
- IGNOU B.Ed Admission 2024
- DU Admission 2024
- UP B.Ed JEE 2024
- LPU NEST 2024
- IIT JAM 2024
- IGNOU Online Admission 2024
- Universities in India
- Top Universities in India 2024
- Top Colleges in India
- Top Universities in Uttar Pradesh 2024
- Top Universities in Bihar
- Top Universities in Madhya Pradesh 2024
- Top Universities in Tamil Nadu 2024
- Central Universities in India
- CUET DU Cut off 2024
- IGNOU Date Sheet 2024
- CUET DU CSAS Portal 2024
- CUET Response Sheet 2024
- CUET Result 2024
- CUET Participating Universities 2024
- CUET Previous Year Question Paper
- CUET Syllabus 2024 for Science Students
- E-Books and Sample Papers
- CUET College Predictor 2024
- CUET Exam Date 2024
- CUET Cut Off 2024
- NIRF Ranking 2024
- IGNOU Exam Form 2024
- CUET PG Counselling 2024
- CUET Answer Key 2024
Engineering Preparation
- Knockout JEE Main 2024
- Test Series JEE Main 2024
- JEE Main 2024 Rank Booster
Medical Preparation
- Knockout NEET 2024
- Test Series NEET 2024
- Rank Booster NEET 2024
Online Courses
- JEE Main One Month Course
- NEET One Month Course
- IBSAT Free Mock Tests
- IIT JEE Foundation Course
- Knockout BITSAT 2024
- Career Guidance Tool
Top Streams
- IT & Software Certification Courses
- Engineering and Architecture Certification Courses
- Programming And Development Certification Courses
- Business and Management Certification Courses
- Marketing Certification Courses
- Health and Fitness Certification Courses
- Design Certification Courses
Specializations
- Digital Marketing Certification Courses
- Cyber Security Certification Courses
- Artificial Intelligence Certification Courses
- Business Analytics Certification Courses
- Data Science Certification Courses
- Cloud Computing Certification Courses
- Machine Learning Certification Courses
- View All Certification Courses
- UG Degree Courses
- PG Degree Courses
- Short Term Courses
- Free Courses
- Online Degrees and Diplomas
- Compare Courses
Top Providers
- Coursera Courses
- Udemy Courses
- Edx Courses
- Swayam Courses
- upGrad Courses
- Simplilearn Courses
- Great Learning Courses
Covid 19 Essay in English
Essay on Covid -19: In a very short amount of time, coronavirus has spread globally. It has had an enormous impact on people's lives, economy, and societies all around the world, affecting every country. Governments have had to take severe measures to try and contain the pandemic. The virus has altered our way of life in many ways, including its effects on our health and our economy. Here are a few sample essays on ‘CoronaVirus’.
100 Words Essay on Covid 19
200 words essay on covid 19, 500 words essay on covid 19.

COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very short period of time. It has affected lives, economies and societies across the world, leaving no country untouched. The virus has caused governments to take drastic measures to try and contain it. From health implications to economic and social ramifications, COVID-19 impacted every part of our lives. It has been more than 2 years since the pandemic hit and the world is still recovering from its effects.
Since the outbreak of COVID-19, the world has been impacted in a number of ways. For one, the global economy has taken a hit as businesses have been forced to close their doors. This has led to widespread job losses and an increase in poverty levels around the world. Additionally, countries have had to impose strict travel restrictions in an attempt to contain the virus, which has resulted in a decrease in tourism and international trade. Furthermore, the pandemic has put immense pressure on healthcare systems globally, as hospitals have been overwhelmed with patients suffering from the virus. Lastly, the outbreak has led to a general feeling of anxiety and uncertainty, as people are fearful of contracting the disease.
My Experience of COVID-19
I still remember how abruptly colleges and schools shut down in March 2020. I was a college student at that time and I was under the impression that everything would go back to normal in a few weeks. I could not have been more wrong. The situation only got worse every week and the government had to impose a lockdown. There were so many restrictions in place. For example, we had to wear face masks whenever we left the house, and we could only go out for essential errands. Restaurants and shops were only allowed to operate at take-out capacity, and many businesses were shut down.
In the current scenario, coronavirus is dominating all aspects of our lives. The coronavirus pandemic has wreaked havoc upon people’s lives, altering the way we live and work in a very short amount of time. It has revolutionised how we think about health care, education, and even social interaction. This virus has had long-term implications on our society, including its impact on mental health, economic stability, and global politics. But we as individuals can help to mitigate these effects by taking personal responsibility to protect themselves and those around them from infection.
Effects of CoronaVirus on Education
The outbreak of coronavirus has had a significant impact on education systems around the world. In China, where the virus originated, all schools and universities were closed for several weeks in an effort to contain the spread of the disease. Many other countries have followed suit, either closing schools altogether or suspending classes for a period of time.
This has resulted in a major disruption to the education of millions of students. Some have been able to continue their studies online, but many have not had access to the internet or have not been able to afford the costs associated with it. This has led to a widening of the digital divide between those who can afford to continue their education online and those who cannot.
The closure of schools has also had a negative impact on the mental health of many students. With no face-to-face contact with friends and teachers, some students have felt isolated and anxious. This has been compounded by the worry and uncertainty surrounding the virus itself.
The situation with coronavirus has improved and schools have been reopened but students are still catching up with the gap of 2 years that the pandemic created. In the meantime, governments and educational institutions are working together to find ways to support students and ensure that they are able to continue their education despite these difficult circumstances.
Effects of CoronaVirus on Economy
The outbreak of the coronavirus has had a significant impact on the global economy. The virus, which originated in China, has spread to over two hundred countries, resulting in widespread panic and a decrease in global trade. As a result of the outbreak, many businesses have been forced to close their doors, leading to a rise in unemployment. In addition, the stock market has taken a severe hit.
Effects of CoronaVirus on Health
The effects that coronavirus has on one's health are still being studied and researched as the virus continues to spread throughout the world. However, some of the potential effects on health that have been observed thus far include respiratory problems, fever, and coughing. In severe cases, pneumonia, kidney failure, and death can occur. It is important for people who think they may have been exposed to the virus to seek medical attention immediately so that they can be treated properly and avoid any serious complications. There is no specific cure or treatment for coronavirus at this time, but there are ways to help ease symptoms and prevent the virus from spreading.
Applications for Admissions are open.

Aakash iACST Scholarship Test 2024
Get up to 90% scholarship on NEET, JEE & Foundation courses

JEE Main Important Physics formulas
As per latest 2024 syllabus. Physics formulas, equations, & laws of class 11 & 12th chapters

JEE Main Important Chemistry formulas
As per latest 2024 syllabus. Chemistry formulas, equations, & laws of class 11 & 12th chapters

TOEFL ® Registrations 2024
Accepted by more than 11,000 universities in over 150 countries worldwide

PTE Exam 2024 Registrations
Register now for PTE & Save 5% on English Proficiency Tests with ApplyShop Gift Cards

JEE Main high scoring chapters and topics
As per latest 2024 syllabus. Study 40% syllabus and score upto 100% marks in JEE
Download Careers360 App's
Regular exam updates, QnA, Predictors, College Applications & E-books now on your Mobile
Certifications
We Appeared in
More From Forbes
A guide to writing the covid-19 essay for the common app.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Students can use the Common App's new Covid-19 essay to expand on their experiences during the ... [+] pandemic.
Covid-19 has heavily impacted students applying to colleges in this application cycle. High schools have gone virtual, extracurricular activities have been canceled and family situations might have changed. Having recognized this, the Common App added a new optional 250-word essay that will give universities a chance to understand the atypical high school experience students have had. The prompt will be:
“Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces.”
Should I Write About The Coronavirus Pandemic?
For many high schoolers, the pandemic will have had a lasting impact on their education and everyday lives. Some students might have had a negative experience: a parent laid off or furloughed, limited access to online classes or a family member (or the student) having fallen ill from the virus.
Other students might have had the opposite experience. Even though they might have undergone a few negative events or stressful times, they might have learned something new, started a new project or gained a new perspective that changed their future major or career choice.
If you fit into either of these categories, writing the optional essay might be a good idea.
Remember, the admission officers have also been dealing with the crisis and understand the situation students are going through. They are well aware that the AP exams were administered remotely, SAT/ACT test dates were canceled and numerous schools transitioned to a virtual learning model. There is likely no need to reiterate this in an essay unless there was a direct impact on an aspect of your application.
NYT ‘Strands’ Hints, Spangram And Answers For Tuesday, July 9th
Wwe raw results, winners and grades as rhea ripley returns, the best brewery in the u.s.—according to the u.s. open beer championship, what not to write .
As with every college essay you write, it is important to think about the tone and word choice. You want to remain sensitive to the plight of other students during this global crisis. While every student has likely been affected by the pandemic, the level of impact will vary greatly. For some, classes moved online, but life remained more or less the same. For these types of students, it might not be a strategic move to write about the coronavirus if you don’t have anything meaningful, unique or personal to say. If you only have a limited time to impress the admission officer, you want to ensure that each word is strategically thought out and showcases a new aspect of your personality.
Using this space as a time to complain about how you weren’t able to go to the beach, see friends or eat out could be seen as you flaunting your privilege. Careful consideration of how you portray yourself will be key.
Nearly every student has had an activity or event canceled. It likely won’t be a good use of your word count lamenting on the missed opportunities. Instead, it would be more illuminating to talk about how you remained flexible and pivoted to other learning opportunities.
How To Write The Covid-19 Essay
The Covid-19 essay was introduced so universities could gain a better understanding of how their applicants have had their lives and education disrupted due to the pandemic. You’ll want to give the admission officers context to understand your experiences better.
Here are some examples of how to write this optional essay.
- Outline any extenuating circumstances related to Covid-19. Some students might find themselves crammed in a small apartment or home with their entire family. This disruptive environment might have made it difficult for the student to concentrate on their classes. Some students might be required to care for younger siblings during the day. In many areas of the country, lack of access to high-speed internet or smart devices meant that students couldn’t participate in online learning. Now is the time to share those details.
- Include the impact. Ultimately, this essay is about you. Things likely happened to family members, friends or your community, but you need to show how it altered your life specifically.
- Provide specific details. Give the admission officers a peek into your everyday life. Including specific details can help make your story come alive. For example, don’t just say that it was hard dealing with the emotional trauma of seeing friends and family fall ill. Instead, be specific and talk about how your friend was diagnosed with Covid-19 and had to be hospitalized. Seeing the long-term effects caused you to take the pandemic much more seriously and moved you to take action. Perhaps you were inspired to start a nonprofit that makes masks or to help your neighbors through this difficult time.
Covid-19 Essay for School Counselors
It’s not just students who will get to submit an additional statement regarding the impact of the coronavirus: Counselors will also get a chance to submit a 500-word essay. Their prompt will be:
Your school may have made adjustments due to community disruptions such as COVID–19 or natural disasters. If you have not already addressed those changes in your uploaded school profile or elsewhere, you can elaborate here. Colleges are especially interested in understanding changes to:
- Grading scales and policies
- Graduation requirements
- Instructional methods
- Schedules and course offerings
- Testing requirements
- Your academic calendar
- Other extenuating circumstances
The counselor’s response will populate to all the applications of students from the high school. They will cover any school or district policies that have impacted students. No specific student details will be included.
Students can ask to see a copy of this statement so they know what information has already been shared with colleges. For example, if the school states that classes went virtual starting in March, you don’t need to repeat that in your Covid-19 essay.
Should I Write About The Covid-19 In My Personal Statement?
The world before Covid-19 might seem like a distant memory, but you did spend more than 15 years engaging in a multitude of meaningful activities and developing your passions. It’s important to define yourself from more than just the coronavirus crisis. You likely will want to spend the personal statement distinguishing yourself from other applicants. With the Covid-19 optional essay and the additional information section, you should have plenty of space to talk about how you’ve changed—for better or for worse—due to the pandemic. Use the personal statement to talk about who you were before quarantining.
- Editorial Standards
- Reprints & Permissions
Find anything you save across the site in your account
A Pandemic College Essay That Probably Won’t Get You Into Brown

Community disruptions such as COVID -19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. — The 2020-21 college-admissions Common Application.
COVID -19 is a very destructive respiratory disease that has caused much pain and suffering for millions of people around the world. Although my heart grieves for all the lives lost, each of us has suffered in our own unique ways. For me, that suffering took the form of not getting an opportunity to play the lead in our spring drama, which was, so tragically, cancelled.
For years, I have been working toward this goal. As a freshman, I auditioned for the role of Laura in the Tennessee Williams famous American drama “The Glass Menagerie.” While I did not win the role, I find it very ironic that now, only three years later, we have all become aware that life is as precious as those fateful glass figurines due to COVID -19.
As a sophomore, my efforts to secure the role of the wrongly accused Desdemona in William Shakespeare’s important play “Othello” were, once again, thwarted. Our drama coach, Ms. Wilkie, told me during the audition process that sophomores would be considered for leading roles, but the parts of Othello, Iago, and Desdemona all went to upperclassmen, even though none of them had taken private acting classes, as I have, with Leonard Michaels (Broadway credits include “Company,” “Starlight Express,” “Pump Boys and Dinettes”), at the Willows Dramatic Academy for Young Performers.
This experience taught me that authority figures do not always have “the answers,” a lesson reinforced when Dr. Anthony Fauci, who is a very respected medical adviser to many Presidents of the United States of America, said at first that masks should not be worn but then said that they should.
When discussing masks these days, it is impossible not to conjure in one’s mind images of the famous “Comedy and Tragedy” masks, which were worn in ancient Greece during the classical period, from approximately 500 to 300 B.C.
Junior year was a turning point for my high-school theatrical career. I auditioned to portray Abigail Williams in “The Crucible,” a play that on the surface purports to be about the Salem witch trials but is in fact a parable about McCarthyism, which was a terrible episode of American history that itself had a long-lasting impact on American history. Although I did not receive the part of Abigail Williams, I did play the pivotal role of Deputy Governor Danforth, who has several lines. Our school newspaper declared my presentation “dramatic” (review attached).
This year, my senior year, Ms. Wilkie said that we would be doing the Pulitzer Prize-winning drama “Our Town.” Never could I have foreseen that “our town” would be affected by the respiratory disease only a few short months later.
Needless to say, I watched in horror in January and February of last year as news reports emerged from China about a new respiratory ailment that threatened to sicken people and shut down vast portions of the economy. In March, we received word that our very high school would be closing its mahogany doors. The curtain on my high-school theatrical career, tragically, fell forever, before I even had the chance to audition for the central role of the Stage Manager, which I planned to reinterpret as a strong, independent woman in the wake of #MeToo.
Perhaps Fate is the real Stage Manager.
The Stanislavski method of acting teaches us to incorporate our actual experiences into our Craft. Should I have the great honor of studying at the Department of Theatre Arts and Performance Studies at Brown University, I vow to incorporate the suffering of this past year into my Art as a tribute to all those, including myself, who have experienced such tremendous loss.
It is believed that the immortal bard, William Shakespeare, said, “Instead of weeping when a tragedy occurs in a songbird’s life, it sings away its grief.” My time at Brown will be my chance to “sing away grief,” except that, unlike the tragedies of Shakespeare and other playwrights, my tragedy is real and therefore more tragic.
Please find attached a video of me in a scene from Herb Gardner’s “A Thousand Clowns” (performed with J. Leonard Mitchell, member, Actors’ Equity). ♦
Daily Humor
By signing up, you agree to our User Agreement and Privacy Policy & Cookie Statement . This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.

Read these 12 moving essays about life during coronavirus
Artists, novelists, critics, and essayists are writing the first draft of history.
by Alissa Wilkinson

The world is grappling with an invisible, deadly enemy, trying to understand how to live with the threat posed by a virus . For some writers, the only way forward is to put pen to paper, trying to conceptualize and document what it feels like to continue living as countries are under lockdown and regular life seems to have ground to a halt.
So as the coronavirus pandemic has stretched around the world, it’s sparked a crop of diary entries and essays that describe how life has changed. Novelists, critics, artists, and journalists have put words to the feelings many are experiencing. The result is a first draft of how we’ll someday remember this time, filled with uncertainty and pain and fear as well as small moments of hope and humanity.
- The Vox guide to navigating the coronavirus crisis
At the New York Review of Books, Ali Bhutto writes that in Karachi, Pakistan, the government-imposed curfew due to the virus is “eerily reminiscent of past military clampdowns”:
Beneath the quiet calm lies a sense that society has been unhinged and that the usual rules no longer apply. Small groups of pedestrians look on from the shadows, like an audience watching a spectacle slowly unfolding. People pause on street corners and in the shade of trees, under the watchful gaze of the paramilitary forces and the police.
His essay concludes with the sobering note that “in the minds of many, Covid-19 is just another life-threatening hazard in a city that stumbles from one crisis to another.”
Writing from Chattanooga, novelist Jamie Quatro documents the mixed ways her neighbors have been responding to the threat, and the frustration of conflicting direction, or no direction at all, from local, state, and federal leaders:
Whiplash, trying to keep up with who’s ordering what. We’re already experiencing enough chaos without this back-and-forth. Why didn’t the federal government issue a nationwide shelter-in-place at the get-go, the way other countries did? What happens when one state’s shelter-in-place ends, while others continue? Do states still under quarantine close their borders? We are still one nation, not fifty individual countries. Right?
- A syllabus for the end of the world
Award-winning photojournalist Alessio Mamo, quarantined with his partner Marta in Sicily after she tested positive for the virus, accompanies his photographs in the Guardian of their confinement with a reflection on being confined :
The doctors asked me to take a second test, but again I tested negative. Perhaps I’m immune? The days dragged on in my apartment, in black and white, like my photos. Sometimes we tried to smile, imagining that I was asymptomatic, because I was the virus. Our smiles seemed to bring good news. My mother left hospital, but I won’t be able to see her for weeks. Marta started breathing well again, and so did I. I would have liked to photograph my country in the midst of this emergency, the battles that the doctors wage on the frontline, the hospitals pushed to their limits, Italy on its knees fighting an invisible enemy. That enemy, a day in March, knocked on my door instead.
In the New York Times Magazine, deputy editor Jessica Lustig writes with devastating clarity about her family’s life in Brooklyn while her husband battled the virus, weeks before most people began taking the threat seriously:
At the door of the clinic, we stand looking out at two older women chatting outside the doorway, oblivious. Do I wave them away? Call out that they should get far away, go home, wash their hands, stay inside? Instead we just stand there, awkwardly, until they move on. Only then do we step outside to begin the long three-block walk home. I point out the early magnolia, the forsythia. T says he is cold. The untrimmed hairs on his neck, under his beard, are white. The few people walking past us on the sidewalk don’t know that we are visitors from the future. A vision, a premonition, a walking visitation. This will be them: Either T, in the mask, or — if they’re lucky — me, tending to him.
Essayist Leslie Jamison writes in the New York Review of Books about being shut away alone in her New York City apartment with her 2-year-old daughter since she became sick:
The virus. Its sinewy, intimate name. What does it feel like in my body today? Shivering under blankets. A hot itch behind the eyes. Three sweatshirts in the middle of the day. My daughter trying to pull another blanket over my body with her tiny arms. An ache in the muscles that somehow makes it hard to lie still. This loss of taste has become a kind of sensory quarantine. It’s as if the quarantine keeps inching closer and closer to my insides. First I lost the touch of other bodies; then I lost the air; now I’ve lost the taste of bananas. Nothing about any of these losses is particularly unique. I’ve made a schedule so I won’t go insane with the toddler. Five days ago, I wrote Walk/Adventure! on it, next to a cut-out illustration of a tiger—as if we’d see tigers on our walks. It was good to keep possibility alive.
At Literary Hub, novelist Heidi Pitlor writes about the elastic nature of time during her family’s quarantine in Massachusetts:
During a shutdown, the things that mark our days—commuting to work, sending our kids to school, having a drink with friends—vanish and time takes on a flat, seamless quality. Without some self-imposed structure, it’s easy to feel a little untethered. A friend recently posted on Facebook: “For those who have lost track, today is Blursday the fortyteenth of Maprilay.” ... Giving shape to time is especially important now, when the future is so shapeless. We do not know whether the virus will continue to rage for weeks or months or, lord help us, on and off for years. We do not know when we will feel safe again. And so many of us, minus those who are gifted at compartmentalization or denial, remain largely captive to fear. We may stay this way if we do not create at least the illusion of movement in our lives, our long days spent with ourselves or partners or families.
- What day is it today?
Novelist Lauren Groff writes at the New York Review of Books about trying to escape the prison of her fears while sequestered at home in Gainesville, Florida:
Some people have imaginations sparked only by what they can see; I blame this blinkered empiricism for the parks overwhelmed with people, the bars, until a few nights ago, thickly thronged. My imagination is the opposite. I fear everything invisible to me. From the enclosure of my house, I am afraid of the suffering that isn’t present before me, the people running out of money and food or drowning in the fluid in their lungs, the deaths of health-care workers now growing ill while performing their duties. I fear the federal government, which the right wing has so—intentionally—weakened that not only is it insufficient to help its people, it is actively standing in help’s way. I fear we won’t sufficiently punish the right. I fear leaving the house and spreading the disease. I fear what this time of fear is doing to my children, their imaginations, and their souls.
At ArtForum , Berlin-based critic and writer Kristian Vistrup Madsen reflects on martinis, melancholia, and Finnish artist Jaakko Pallasvuo’s 2018 graphic novel Retreat , in which three young people exile themselves in the woods:
In melancholia, the shape of what is ending, and its temporality, is sprawling and incomprehensible. The ambivalence makes it hard to bear. The world of Retreat is rendered in lush pink and purple watercolors, which dissolve into wild and messy abstractions. In apocalypse, the divisions established in genesis bleed back out. My own Corona-retreat is similarly soft, color-field like, each day a blurred succession of quarantinis, YouTube–yoga, and televized press conferences. As restrictions mount, so does abstraction. For now, I’m still rooting for love to save the world.
At the Paris Review , Matt Levin writes about reading Virginia Woolf’s novel The Waves during quarantine:
A retreat, a quarantine, a sickness—they simultaneously distort and clarify, curtail and expand. It is an ideal state in which to read literature with a reputation for difficulty and inaccessibility, those hermetic books shorn of the handholds of conventional plot or characterization or description. A novel like Virginia Woolf’s The Waves is perfect for the state of interiority induced by quarantine—a story of three men and three women, meeting after the death of a mutual friend, told entirely in the overlapping internal monologues of the six, interspersed only with sections of pure, achingly beautiful descriptions of the natural world, a day’s procession and recession of light and waves. The novel is, in my mind’s eye, a perfectly spherical object. It is translucent and shimmering and infinitely fragile, prone to shatter at the slightest disturbance. It is not a book that can be read in snatches on the subway—it demands total absorption. Though it revels in a stark emotional nakedness, the book remains aloof, remote in its own deep self-absorption.
- Vox is starting a book club. Come read with us!
In an essay for the Financial Times, novelist Arundhati Roy writes with anger about Indian Prime Minister Narendra Modi’s anemic response to the threat, but also offers a glimmer of hope for the future:
Historically, pandemics have forced humans to break with the past and imagine their world anew. This one is no different. It is a portal, a gateway between one world and the next. We can choose to walk through it, dragging the carcasses of our prejudice and hatred, our avarice, our data banks and dead ideas, our dead rivers and smoky skies behind us. Or we can walk through lightly, with little luggage, ready to imagine another world. And ready to fight for it.
From Boston, Nora Caplan-Bricker writes in The Point about the strange contraction of space under quarantine, in which a friend in Beirut is as close as the one around the corner in the same city:
It’s a nice illusion—nice to feel like we’re in it together, even if my real world has shrunk to one person, my husband, who sits with his laptop in the other room. It’s nice in the same way as reading those essays that reframe social distancing as solidarity. “We must begin to see the negative space as clearly as the positive, to know what we don’t do is also brilliant and full of love,” the poet Anne Boyer wrote on March 10th, the day that Massachusetts declared a state of emergency. If you squint, you could almost make sense of this quarantine as an effort to flatten, along with the curve, the distinctions we make between our bonds with others. Right now, I care for my neighbor in the same way I demonstrate love for my mother: in all instances, I stay away. And in moments this month, I have loved strangers with an intensity that is new to me. On March 14th, the Saturday night after the end of life as we knew it, I went out with my dog and found the street silent: no lines for restaurants, no children on bicycles, no couples strolling with little cups of ice cream. It had taken the combined will of thousands of people to deliver such a sudden and complete emptiness. I felt so grateful, and so bereft.
And on his own website, musician and artist David Byrne writes about rediscovering the value of working for collective good , saying that “what is happening now is an opportunity to learn how to change our behavior”:
In emergencies, citizens can suddenly cooperate and collaborate. Change can happen. We’re going to need to work together as the effects of climate change ramp up. In order for capitalism to survive in any form, we will have to be a little more socialist. Here is an opportunity for us to see things differently — to see that we really are all connected — and adjust our behavior accordingly. Are we willing to do this? Is this moment an opportunity to see how truly interdependent we all are? To live in a world that is different and better than the one we live in now? We might be too far down the road to test every asymptomatic person, but a change in our mindsets, in how we view our neighbors, could lay the groundwork for the collective action we’ll need to deal with other global crises. The time to see how connected we all are is now.
The portrait these writers paint of a world under quarantine is multifaceted. Our worlds have contracted to the confines of our homes, and yet in some ways we’re more connected than ever to one another. We feel fear and boredom, anger and gratitude, frustration and strange peace. Uncertainty drives us to find metaphors and images that will let us wrap our minds around what is happening.
Yet there’s no single “what” that is happening. Everyone is contending with the pandemic and its effects from different places and in different ways. Reading others’ experiences — even the most frightening ones — can help alleviate the loneliness and dread, a little, and remind us that what we’re going through is both unique and shared by all.
Most Popular
The supreme incompetents, web3 is the future, or a scam, or both, stop setting your thermostat at 72, the lawsuit accusing trump of raping a 13-year-old girl, explained, the real lesson for america in the french and british elections, today, explained.
Understand the world with a daily explainer plus the most compelling stories of the day.
More in Culture

Having an Asian Bachelorette is a milestone. It’s also about power.

The existential struggle of being Black

The baffling case of Karen Read

Why is everyone talking about Kamala Harris and coconut trees?

Simone Biles is so back

Diljit Dosanjh is one of India’s biggest stars. Now he’s taking on America.

France’s elections showed a polarized country

The death of the summer job is a good thing

The case against summer

This tiny doll is making everyone so happy

- Get Press Releases

- Media Contacts
- News Releases
- Photos & B-Roll Downloads
- VUMC Facts and Figures
- Credo Award
- DAISY Award
- Elevate Team Award
- Health, Yes
- Employee Spotlight
- Five Pillar Leader Award
Patient Spotlight
- Pets of VUMC
- Tales of VUMC Past
- All Voice Stories
Explore by Highlight
- Community & Giving
- Education & Training
- Growth & Finance
- Leadership Perspectives
- VUMC People
Explore by Topic
- Emergency & Trauma
- Genetics & Genomics
- Health Equity
- Health Policy
- Tech & Health
- Women's Health
Explore by Location
- Monroe Carell Jr. Children’s Hospital at Vanderbilt
- Vanderbilt Bedford County Hospital
- Vanderbilt Health One Hundred Oaks
- Vanderbilt Health Affiliated Network
- Vanderbilt-Ingram Cancer Center
- Vanderbilt Kennedy Center
- Vanderbilt Psychiatric Hospital
- Vanderbilt Wilson County Hospital
- Vanderbilt Stallworth Rehabilitation Hospital
- Vanderbilt Tullahoma-Harton Hospital
- Vanderbilt University Hospital

- Photos & B-Roll Downloads
Featured Story

A gunshot to the head. A long recovery. Then a wedding.
December 28, 2020, first-person essay: doing my part to end the pandemic .
I want to particularly encourage the African American community, which has been disproportionately impacted by COVID-19, to step forward, receive this vaccine and spread the word to your families. Let’s put this pandemic behind us in 2021 — together.

by Kevin Johnson, MD, MS, FAAP, FACMI
Rev. Martin Luther King, Jr. once said, “Our lives begin to end the day we become silent about things that matter.” In that spirit, please allow me to be vocal, opinionated, hopeful and forgiving.
From the beginning of the pandemic, it was clear each of us had to join ranks to save our loved ones and society from the ramifications of COVID-19. We could wear masks, social distance, and dispel myths and skepticism about the vaccine. As a pediatrician, chair of the Department of Biomedical Informatics and member of the health care, LGBTQ, and African American communities, I am compelled by duty to do more. So in August 2020, I joined the Moderna COVID-19 vaccine trial. I’d like to tell you why.
Before joining the trial, my family and I were quick to find ways we could actively fight against the pandemic. We recognized many people in our country, including the African American community, were skeptical about the impact of this virus, so we used social media to magnify important messages to local and national audiences. I pivoted the focus of my podcast Informatics in the Round to issues around data sharing, mask-wearing, research on COVID-19, and finding trustworthy information about the virus. I eagerly wanted to give blood to mitigate the national blood supply shortage but as a gay man that’s not an option for me. Restrictions prevent my husband and me from contributing in that way. It was then when we heard about the Moderna trial.
Vaccine studies are generally very safe; the study participants and I understood the risks were low. I also was fully cognizant that participation in the trial could improve the validity of the study — perhaps even the outcomes for underrepresented groups. The importance of showing the African American community that one of its members was a willing participant in the trial was not lost on me. It was an easy decision to enroll in the study to help our society get back to some semblance of normal.
The vaccine trial was incredibly well run. I enrolled online, attended an hour-long group Zoom call, completed a two-hour visit with the study team, and, finally, received an injection of either the vaccine or a saltwater placebo. I was required to report symptoms into a diary using a simple app on my phone. I also had periodic phone check-ins with the research team. There were some blood draws, too.
Here, I should note that while I can tolerate needle sticks, I don’t like pain. Drawing blood from a turnip is easier than getting it from me! Despite this, I believed my “voice” in the trial mattered too much for something as small as a needle to silence me. The four or so blood draws were a small price to pay.
I had no symptoms following my first injection. Two days after my second injection, I had some symptoms. I developed a mild fever (100 degrees) and chills, some underarm gland tenderness, and skin redness and swelling at the injection site. I also felt more tired than usual, but I was in touch with the study team, who was supportive and reassuring throughout this whole process. By day three, all of my symptoms disappeared!
I am honored to be a piece of the solution to a pandemic. I would do it again for all of us: my husband, our children, my parents, my friends, our patients, and our world. I’m sharing my story in hopes that you’ll get vocal to your circle of friends, family, and neighbors about why you’re getting this vaccine. I also realize that there are some who are either unwilling or unable to feel comfortable about this vaccine, even after reading the CDC website or the state of Tennessee COVID website. This is, of course, your choice. I’ll hope that through our action, the rest of us will help keep you and your loved ones safe.
We’re all in this pandemic together and thousands of us banded together to test the safety of these vaccines. I encourage everyone to receive this vaccine if you can do so. I want to particularly encourage the African American community, which has been disproportionately impacted by COVID-19, to step forward, receive this vaccine and spread the word to your families. Let’s put this pandemic behind us in 2021 — together.
Dr. Johnson is the Cornelius Vanderbilt Professor and chair of the Department of Biomedical Informatics; professor of Pediatrics and Informatician-in-Chief, VUMC

- Games & Quizzes
- History & Society
- Science & Tech
- Biographies
- Animals & Nature
- Geography & Travel
- Arts & Culture
- On This Day
- One Good Fact
- New Articles
- Lifestyles & Social Issues
- Philosophy & Religion
- Politics, Law & Government
- World History
- Health & Medicine
- Browse Biographies
- Birds, Reptiles & Other Vertebrates
- Bugs, Mollusks & Other Invertebrates
- Environment
- Fossils & Geologic Time
- Entertainment & Pop Culture
- Sports & Recreation
- Visual Arts
- Demystified
- Image Galleries
- Infographics
- Top Questions
- Britannica Kids
- Saving Earth
- Space Next 50
- Student Center
- Introduction
Horrific history
The early days, health and medicine.

What was the impact of COVID-19?
Our editors will review what you’ve submitted and determine whether to revise the article.
- Table Of Contents

Recent News
On February 25, 2020, a top official at the Centers for Disease Control and Prevention decided it was time to level with the U.S. public about the COVID-19 outbreak. At the time, there were just 57 people in the country confirmed to have the infection, all but 14 having been repatriated from Hubei province in China and the Diamond Princess cruise ship , docked off Yokohama , Japan .
The infected were in quarantine. But Nancy Messonnier, then head of the CDC’s National Center for Immunization and Respiratory Diseases, knew what was coming. “It’s not so much a question of if this will happen anymore but rather more a question of exactly when this will happen and how many people in this country will have severe illness,” Messonnier said at a news briefing.
“I understand this whole situation may seem overwhelming and that disruption to everyday life may be severe,” she continued. “But these are things that people need to start thinking about now.”
Looking back, the COVID-19 pandemic stands as arguably the most disruptive event of the 21st century, surpassing wars, the September 11, 2001, terrorist attacks , the effects of climate change , and the Great Recession . It has killed more than seven million people to date and reshaped the world economy, public health , education, work, social interaction, family life, medicine, and mental health—leaving no corner of the globe untouched in some way. Now endemic in many societies, the consistently mutating virus remains one of the leading annual causes of death, especially among people older than 65 and the immunosuppressed.
“The coronavirus outbreak, historically, beyond a doubt, has been the most devastating pandemic of an infectious disease that global society has experienced in well over 100 years, since the 1918 influenza pandemic ,” Anthony Fauci , who helped lead the U.S. government’s health response to the pandemic under Pres. Donald Trump and became Pres. Joe Biden ’s chief medical adviser, told Encyclopædia Britannica in 2024.
“I think the impact of this outbreak on the world in general, on the United States , is really historic. Fifty years from now, 100 years from now, when they talk about the history of what we’ve been through, this is going to go down equally with the 1918 influenza pandemic , with the stock market crash of 1929 , with World War II —all the things that were profoundly disruptive of the social order.”
What few could imagine in the first days of the pandemic was the extent of the disruption the disease would bring to the everyday lives of just about everyone around the globe.
Within weeks, schools and child-care centers began shuttering, businesses sent their workforces home, public gatherings were canceled, stores and restaurants closed, and cruise ships were barred from sailing. On March 11, actor Tom Hanks announced that he had COVID-19, and the NBA suspended its season. (It was ultimately completed in a closed “bubble” at Walt Disney World .) On March 12, as college basketball players left courts mid-game during conference tournaments, the NCAA announced that it would not hold its wildly popular season-ending national competition, known as March Madness , for the first time since 1939. Three days later, the New York City public school system, the country’s largest, with 1.1 million students, closed. On March 19, all 40 million Californians were placed under a stay-at-home order.

By mid-April, with hospital beds and ventilators in critically short supply, workers were burying the coffins of COVID-19 victims in mass graves on Hart Island, off the Bronx . At first, the public embraced caregivers. New Yorkers applauded them from windows and balconies, and individuals sewed masks for them. But that spirit soon gave way to the crushing long-term reality of the pandemic and the national division that followed.
Around the world, it was worse. On the day Messonnier spoke, the virus had spread from its origin point in Wuhan , China, to at least two dozen countries, sickening thousands and killing dozens. By April 4, more than one million cases had been confirmed worldwide. Some countries, including China and Italy, imposed strict lockdowns on their citizens. Paris restricted movement, with certain exceptions, including an hour a day for exercise, within 1 km (0.62 mile) of home.
In the United States, the threat posed by the virus did not keep large crowds from gathering to protest the May 25 slaying of George Floyd , a 46-year-old Black man, by a white police officer, Derek Chauvin. The murder, taped by a bystander in Minneapolis , Minnesota , sparked raucous and sometimes violent street protests for racial justice around the world that contributed to an overall sense of societal instability.
The official World Health Organization total of more than seven million deaths as of March 2024 is widely considered a serious undercount of the actual toll. In some countries there was limited testing for the virus and difficulty attributing fatalities to it. Others suppressed total counts or were not able to devote resources to compiling their totals. In May 2021, a panel of experts consulted by The New York Times estimated that India ’s actual COVID-19 death toll was likely 1.6 million, more than five times the reported total of 307,231.
An average of 3,100 people—one every 28 seconds—died of COVID-19 every day in the United States in January 2021.
When “excess mortality”—COVID and non-COVID deaths that likely would not have occurred under normal, pre-outbreak conditions—are included in the worldwide tally, the number of pandemic victims was about 15 million by the end of 2021, WHO estimated.
Not long after the pandemic took hold, the United States, which spends more per capita on medical care than any other country, became the epicenter of COVID-19 fatalities. The country fell victim to a fractured health care system that is inequitable to poor and rural patients and people of color, as well as a deep ideological divide over its political leadership and public health policies, such as wearing protective face masks. By early 2024, the U.S. had recorded nearly 1.2 million COVID-19 deaths.
Life expectancy at birth plunged from 78.8 years in 2019 to 76.4 in 2021, a staggering decline in a barometer of a country’s health that typically changes by only a tenth or two annually. An average of 3,100 people—one every 28 seconds—died of COVID-19 every day in the United States in January 2021, before vaccines for the virus became widely available, The Washington Post reported.
The impact on those caring for the sick and dying was profound. “The second week of December [2020] was probably the worst week of my career,” said Brad Butcher, director of the medical-surgical intensive care unit at UPMC Mercy hospital in Pittsburgh , Pennsylvania. “The first day I was on service, five patients died in a shift. And then I came back the next day, and three patients died. And I came back the next day, and three more patients died. And it was completely defeating,” he told The Washington Post on January 11, 2021.
“We can’t get the graves dug fast enough,” a Maryland funeral home operator told The Washington Post that same day.
As the pandemic surged in waves around the world, country after country was plunged into economic recession , the inevitable damage caused by layoffs, business closures, lockdowns, deaths, reduced trade, debt repayment moratoriums , the cost to governments of responding to the crisis, and other factors. Overall, the virus triggered the greatest economic calamity in more than a century, according to a 2022 report by the World Bank .
“Economic activity contracted in 2020 in about 90 percent of countries, exceeding the number of countries seeing such declines during two world wars, the Great Depression of the 1930s, the emerging economy debt crises of the 1980s, and the 2007–09 global financial crisis,” the report noted. “In 2020, the first year of the COVID-19 pandemic, the global economy shrank by approximately 3 percent, and global poverty increased for the first time in a generation.”
A 2020 study that attempted to aggregate the costs of lost gross domestic product (GDP) estimated that premature deaths and health-related losses in the United States totaled more than $16 trillion, or roughly “90% of the annual GDP of the United States. For a family of 4, the estimated loss would be nearly $200,000.”
In April 2020, the U.S. unemployment rate stood at 14.7 percent, higher than at any point since the Great Depression. There were 23.1 million people out of work. The hospitality, leisure, and health care industries were especially hard hit. Consumer spending, which accounts for about two-thirds of the U.S. economy, plunged.
With workers at home, many businesses turned to telework, a development that would persist beyond the pandemic and radically change working conditions for millions. In 2023, 12.7 percent of full-time U.S. employees worked from home and 28.2 percent worked a hybrid office-home schedule, according to Forbes Advisor . Urban centers accustomed to large daily influxes of workers have suffered. Office vacancies are up, and small businesses have closed. The national office vacancy rate rose to a record 19.6 percent in the fourth quarter of 2023, according to Moody’s Analytics , which has been tracking the statistic since 1979.
Many hospitals were overwhelmed during COVID-19 surges, with too few beds for the flood of patients. But many also demonstrated their resilience and “surge capacity,” dramatically expanding bed counts in very short periods of time and finding other ways to treat patients in swamped medical centers. Triage units and COVID-19 wards were hastily erected in temporary structures on hospital grounds.
Still, U.S. hospitals suffered severe shortages of nurses and found themselves lacking basic necessities such as N95 masks and personal protective garb for the doctors, nurses, and other workers who risked their lives against the new pathogen at the start of the outbreak. Mortuaries and first responders were overwhelmed as well. The dead were kept in refrigerated trucks outside hospitals.
The country’s fragmented public health system proved inadequate to the task of coping with the outbreak, sparking calls for major reform of the CDC and other agencies. The CDC botched its initial attempt to create tests for the virus, leaving the United States almost blind to its spread during the early stages of the pandemic.
Beyond the physical dangers, mental health became a serious issue for overburdened health care personnel, other “essential” workers who continued to labor in crucial jobs, and many millions of isolated, stressed, fearful, locked-down people in the United States and elsewhere. Parents struggled to care for children kept at home by the pandemic while also attending to their jobs.
In a June 2020 survey, the CDC found that 41 percent of respondents said they were struggling with mental health and 11 percent had seriously considered suicide recently. Essential workers, unpaid caregivers , young adults, and members of racial and ethnic minority groups were found to be at a higher risk for experiencing mental health struggles, with 31 percent of unpaid caregivers reporting that they were considering suicide. WHO reported two years later that the pandemic had caused a 25 percent increase in anxiety and depression worldwide, young people and women being at the highest risk.
The rate of homicides by firearm in the United States rose by 35 percent during the pandemic to the highest rate in more than a quarter century.
A silver lining in the chaos of the pandemic’s opening year was the development in just 11 months of highly effective vaccines for the virus, a process that normally had taken 7–10 years. The U.S. government’s bet on unproven messenger RNA technology under the Trump administration’s Operation Warp Speed paid off, and the result validated the billions of dollars that the government pours into basic research every year.
On December 14, 2020, New York nurse Sandra Lindsay capped the tumultuous year by receiving the first shot of the vaccine that eventually would help end the public health crisis caused by COVID-19 pandemic.
- How to Order
Persuasive Essay Guide
Persuasive Essay About Covid19
How to Write a Persuasive Essay About Covid19 | Examples & Tips
11 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
200+ Persuasive Essay Topics to Help You Out
Learn How to Create a Persuasive Essay Outline
30+ Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
Crafting a Convincing Persuasive Essay About Abortion
Learn to Write Persuasive Essay About Business With Examples and Tips
Check Out 12 Persuasive Essay About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About Covid19
- 3. Examples of Persuasive Essay About Covid-19 Vaccine
- 4. Examples of Persuasive Essay About Covid-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
| "COVID-19 vaccination mandates are necessary for public health and safety." |
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
| The COVID-19 pandemic has presented an unprecedented global challenge, and in the face of this crisis, many countries have debated the implementation of vaccination mandates. This essay argues that such mandates are essential for safeguarding public health and preventing further devastation caused by the virus. |
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
| COVID-19, caused by the novel coronavirus SARS-CoV-2, emerged in late 2019 and quickly spread worldwide, leading to millions of infections and deaths. Vaccination has proven to be an effective tool in curbing the virus's spread and severity. |
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences, evidence, and analysis. Here's an example:
| One compelling reason for implementing COVID-19 vaccination mandates is the overwhelming evidence of vaccine effectiveness. According to a study published in the New England Journal of Medicine, the Pfizer-BioNTech and Moderna vaccines demonstrated an efficacy of over 90% in preventing symptomatic COVID-19 cases. This level of protection not only reduces the risk of infection but also minimizes the virus's impact on healthcare systems. |
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
| Some argue that vaccination mandates infringe on personal freedoms and autonomy. While individual freedom is a crucial aspect of democratic societies, public health measures have long been implemented to protect the collective well-being. Seatbelt laws, for example, are in place to save lives, even though they restrict personal choice. |
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
| In conclusion, COVID-19 vaccination mandates are a crucial step toward controlling the pandemic, protecting public health, and preventing further loss of life. The evidence overwhelmingly supports their effectiveness, and while concerns about personal freedoms are valid, they must be weighed against the greater good of society. It is our responsibility to take collective action to combat this global crisis and move toward a safer, healthier future. |
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About Covid19
When writing a persuasive essay about the Covid-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
|
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About Covid-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of Covid-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the Covid-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About Covid-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
Choose a Specific Angle
Start by narrowing down your focus. COVID-19 is a broad topic, so selecting a specific aspect or issue related to it will make your essay more persuasive and manageable. For example, you could focus on vaccination, public health measures, the economic impact, or misinformation.
Provide Credible Sources
Support your arguments with credible sources such as scientific studies, government reports, and reputable news outlets. Reliable sources enhance the credibility of your essay.
Use Persuasive Language
Employ persuasive techniques, such as ethos (establishing credibility), pathos (appealing to emotions), and logos (using logic and evidence). Use vivid examples and anecdotes to make your points relatable.
Organize Your Essay
Structure your essay involves creating a persuasive essay outline and establishing a logical flow from one point to the next. Each paragraph should focus on a single point, and transitions between paragraphs should be smooth and logical.
Emphasize Benefits
Highlight the benefits of your proposed actions or viewpoints. Explain how your suggestions can improve public health, safety, or well-being. Make it clear why your audience should support your position.
Use Visuals -H3
Incorporate graphs, charts, and statistics when applicable. Visual aids can reinforce your arguments and make complex data more accessible to your readers.
Call to Action
End your essay with a strong call to action. Encourage your readers to take a specific step or consider your viewpoint. Make it clear what you want them to do or think after reading your essay.
Revise and Edit
Proofread your essay for grammar, spelling, and clarity. Make sure your arguments are well-structured and that your writing flows smoothly.
Seek Feedback
Have someone else read your essay to get feedback. They may offer valuable insights and help you identify areas where your persuasive techniques can be improved.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You have read good sample essays and got some helpful tips. You now have the tools you needed to write a persuasive essay about Covid-19. So don't let the doubts stop you, start writing!
If you need professional writing help, don't worry! We've got that for you as well.
MyPerfectWords.com is a professional persuasive essay writing service that can help you craft an excellent persuasive essay on Covid-19. Our experienced essay writer will create a well-structured, insightful paper in no time!
So don't hesitate and place your ' write my essay online ' request today!
Frequently Asked Questions
Are there any ethical considerations when writing a persuasive essay about covid-19.
Yes, there are ethical considerations when writing a persuasive essay about COVID-19. It's essential to ensure the information is accurate, not contribute to misinformation, and be sensitive to the pandemic's impact on individuals and communities. Additionally, respecting diverse viewpoints and emphasizing public health benefits can promote ethical communication.
What impact does COVID-19 have on society?
The impact of COVID-19 on society is far-reaching. It has led to job and economic losses, an increase in stress and mental health disorders, and changes in education systems. It has also had a negative effect on social interactions, as people have been asked to limit their contact with others.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.

Paper Due? Why Suffer? That’s our Job!
Keep reading


45,000+ students realised their study abroad dream with us. Take the first step today
Meet top uk universities from the comfort of your home, here’s your new year gift, one app for all your, study abroad needs, start your journey, track your progress, grow with the community and so much more.

Verification Code
An OTP has been sent to your registered mobile no. Please verify

Thanks for your comment !
Our team will review it before it's shown to our readers.

- School Education /
Essay On Covid-19: 100, 200 and 300 Words
- Updated on
- Apr 30, 2024

COVID-19, also known as the Coronavirus, is a global pandemic that has affected people all around the world. It first emerged in a lab in Wuhan, China, in late 2019 and quickly spread to countries around the world. This virus was reportedly caused by SARS-CoV-2. Since then, it has spread rapidly to many countries, causing widespread illness and impacting our lives in numerous ways. This blog talks about the details of this virus and also drafts an essay on COVID-19 in 100, 200 and 300 words for students and professionals.

Table of Contents
- 1 Essay On COVID-19 in English 100 Words
- 2 Essay On COVID-19 in 200 Words
- 3 Essay On COVID-19 in 300 Words
- 4 Short Essay on Covid-19
Essay On COVID-19 in English 100 Words
COVID-19, also known as the coronavirus, is a global pandemic. It started in late 2019 and has affected people all around the world. The virus spreads very quickly through someone’s sneeze and respiratory issues.
COVID-19 has had a significant impact on our lives, with lockdowns, travel restrictions, and changes in daily routines. To prevent the spread of COVID-19, we should wear masks, practice social distancing, and wash our hands frequently.
People should follow social distancing and other safety guidelines and also learn the tricks to be safe stay healthy and work the whole challenging time.
Also Read: National Safe Motherhood Day 2023
Essay On COVID-19 in 200 Words
COVID-19 also known as coronavirus, became a global health crisis in early 2020 and impacted mankind around the world. This virus is said to have originated in Wuhan, China in late 2019. It belongs to the coronavirus family and causes flu-like symptoms. It impacted the healthcare systems, economies and the daily lives of people all over the world.
The most crucial aspect of COVID-19 is its highly spreadable nature. It is a communicable disease that spreads through various means such as coughs from infected persons, sneezes and communication. Due to its easy transmission leading to its outbreaks, there were many measures taken by the government from all over the world such as Lockdowns, Social Distancing, and wearing masks.
There are many changes throughout the economic systems, and also in daily routines. Other measures such as schools opting for Online schooling, Remote work options available and restrictions on travel throughout the country and internationally. Subsequently, to cure and top its outbreak, the government started its vaccine campaigns, and other preventive measures.
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness.
Also Read : Essay on My Best Friend

Essay On COVID-19 in 300 Words
COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide. It was first discovered in late 2019 in Cina and then got spread in the whole world. It had a major impact on people’s life, their school, work and daily lives.
COVID-19 is primarily transmitted from person to person through respiratory droplets produced and through sneezes, and coughs of an infected person. It can spread to thousands of people because of its highly contagious nature. To cure the widespread of this virus, there are thousands of steps taken by the people and the government.
Wearing masks is one of the essential precautions to prevent the virus from spreading. Social distancing is another vital practice, which involves maintaining a safe distance from others to minimize close contact.
Very frequent handwashing is also very important to stop the spread of this virus. Proper hand hygiene can help remove any potential virus particles from our hands, reducing the risk of infection.
In conclusion, the Coronavirus has changed people’s perspective on living. It has also changed people’s way of interacting and how to live. To deal with this virus, it is very important to follow the important guidelines such as masks, social distancing and techniques to wash your hands. Getting vaccinated is also very important to go back to normal life and cure this virus completely.
Also Read: Essay on Abortion in English in 650 Words
Short Essay on Covid-19
Please find below a sample of a short essay on Covid-19 for school students:
Also Read: Essay on Women’s Day in 200 and 500 words
to write an essay on COVID-19, understand your word limit and make sure to cover all the stages and symptoms of this disease. You need to highlight all the challenges and impacts of COVID-19. Do not forget to conclude your essay with positive precautionary measures.
Writing an essay on COVID-19 in 200 words requires you to cover all the challenges, impacts and precautions of this disease. You don’t need to describe all of these factors in brief, but make sure to add as many options as your word limit allows.
The full form for COVID-19 is Corona Virus Disease of 2019.
Related Reads
Hence, we hope that this blog has assisted you in comprehending with an essay on COVID-19. For more information on such interesting topics, visit our essay writing page and follow Leverage Edu.
Simran Popli
An avid writer and a creative person. With an experience of 1.5 years content writing, Simran has worked with different areas. From medical to working in a marketing agency with different clients to Ed-tech company, the journey has been diverse. Creative, vivacious and patient are the words that describe her personality.
Leave a Reply Cancel reply
Save my name, email, and website in this browser for the next time I comment.
Contact no. *

Connect With Us
45,000+ students realised their study abroad dream with us. take the first step today..

Resend OTP in

Need help with?
Study abroad.
UK, Canada, US & More
IELTS, GRE, GMAT & More
Scholarship, Loans & Forex
Country Preference
New Zealand
Which English test are you planning to take?
Which academic test are you planning to take.
Not Sure yet
When are you planning to take the exam?
Already booked my exam slot
Within 2 Months
Want to learn about the test
Which Degree do you wish to pursue?
When do you want to start studying abroad.
January 2024
September 2024
What is your budget to study abroad?
How would you describe this article ?
Please rate this article
We would like to hear more.
Have something on your mind?

Make your study abroad dream a reality in January 2022 with
India's Biggest Virtual University Fair

Essex Direct Admission Day
Why attend .

Don't Miss Out
/media/video/upload/Opener_rt.mp4)
How Science Beat the Virus
And what it lost in the process

Listen to this article
Listen to more stories on audm
This article was published online on December 14, 2020.
In fall of 2019, exactly zero scientists were studying COVID‑19, because no one knew the disease existed. The coronavirus that causes it, SARS‑CoV‑2, had only recently jumped into humans and had been neither identified nor named. But by the end of March 2020, it had spread to more than 170 countries, sickened more than 750,000 people, and triggered the biggest pivot in the history of modern science. Thousands of researchers dropped whatever intellectual puzzles had previously consumed their curiosity and began working on the pandemic instead. In mere months, science became thoroughly COVID-ized.
As of this writing, the biomedical library PubMed lists more than 74,000 COVID-related scientific papers—more than twice as many as there are about polio, measles, cholera, dengue, or other diseases that have plagued humanity for centuries. Only 9,700 Ebola-related papers have been published since its discovery in 1976; last year, at least one journal received more COVID‑19 papers than that for consideration. By September, the prestigious New England Journal of Medicine had received 30,000 submissions—16,000 more than in all of 2019. “All that difference is COVID‑19,” Eric Rubin, NEJM ’s editor in chief, says. Francis Collins, the director of the National Institutes of Health, told me, “The way this has resulted in a shift in scientific priorities has been unprecedented.”
Much like famous initiatives such as the Manhattan Project and the Apollo program, epidemics focus the energies of large groups of scientists. In the U.S., the influenza pandemic of 1918, the threat of malaria in the tropical battlegrounds of World War II, and the rise of polio in the postwar years all triggered large pivots. Recent epidemics of Ebola and Zika each prompted a temporary burst of funding and publications . But “nothing in history was even close to the level of pivoting that’s happening right now,” Madhukar Pai of McGill University told me.
That’s partly because there are just more scientists: From 1960 to 2010, the number of biological or medical researchers in the U.S. increased sevenfold , from just 30,000 to more than 220,000. But SARS-CoV-2 has also spread farther and faster than any new virus in a century. For Western scientists, it wasn’t a faraway threat like Ebola. It threatened to inflame their lungs. It shut down their labs. “It hit us at home,” Pai said.
In a survey of 2,500 researchers in the U.S., Canada, and Europe, Kyle Myers from Harvard and his team found that 32 percent had shifted their focus toward the pandemic. Neuroscientists who study the sense of smell started investigating why COVID‑19 patients tend to lose theirs. Physicists who had previously experienced infectious diseases only by contracting them found themselves creating models to inform policy makers. Michael D. L. Johnson at the University of Arizona normally studies copper’s toxic effects on bacteria. But when he learned that SARS‑CoV‑2 persists for less time on copper surfaces than on other materials, he partially pivoted to see how the virus might be vulnerable to the metal. No other disease has been scrutinized so intensely, by so much combined intellect, in so brief a time.
These efforts have already paid off. New diagnostic tests can detect the virus within minutes. Massive open data sets of viral genomes and COVID‑19 cases have produced the most detailed picture yet of a new disease’s evolution. Vaccines are being developed with record-breaking speed. SARS‑CoV‑2 will be one of the most thoroughly characterized of all pathogens, and the secrets it yields will deepen our understanding of other viruses, leaving the world better prepared to face the next pandemic.
But the COVID‑19 pivot has also revealed the all-too-human frailties of the scientific enterprise . Flawed research made the pandemic more confusing, influencing misguided policies. Clinicians wasted millions of dollars on trials that were so sloppy as to be pointless. Overconfident poseurs published misleading work on topics in which they had no expertise. Racial and gender inequalities in the scientific field widened.
Amid a long winter of sickness , it’s hard not to focus on the political failures that led us to a third surge. But when people look back on this period, decades from now, they will also tell stories, both good and bad, about this extraordinary moment for science. At its best, science is a self-correcting march toward greater knowledge for the betterment of humanity. At its worst, it is a self-interested pursuit of greater prestige at the cost of truth and rigor. The pandemic brought both aspects to the fore. Humanity will benefit from the products of the COVID‑19 pivot. Science itself will too, if it learns from the experience.
In February, Jennifer Doudna, one of America’s most prominent scientists, was still focused on CRISPR—the gene-editing tool that she’d co-discovered and that won her a Nobel Prize in October. But when her son’s high school shut down and UC Berkeley, her university, closed its campus, the severity of the impending pandemic became clear. “In three weeks, I went from thinking we’re still okay to thinking that my whole life is going to change,” she told me. On March 13, she and dozens of colleagues at the Innovative Genomics Institute, which she leads, agreed to pause most of their ongoing projects and redirect their skills to addressing COVID‑19. They worked on CRISPR-based diagnostic tests. Because existing tests were in short supply, they converted lab space into a pop-up testing facility to serve the local community. “We need to make our expertise relevant to whatever is happening right now,” she said.
Scientists who’d already been studying other emerging diseases were even quicker off the mark. Lauren Gardner, an engineering professor at Johns Hopkins University who has studied dengue and Zika, knew that new epidemics are accompanied by a dearth of real-time data. So she and one of her students created an online global dashboard to map and tally all publicly reported COVID‑19 cases and deaths. After one night of work, they released it, on January 22. The dashboard has since been accessed daily by governments, public-health agencies, news organizations, and anxious citizens.
Studying deadly viruses is challenging at the best of times, and was especially so this past year. To handle SARS‑CoV‑2, scientists must work in “biosafety level 3” labs, fitted with special airflow systems and other extreme measures; although the actual number is not known, an estimated 200 such facilities exist in the U.S. Researchers often test new drugs and vaccines on monkeys before proceeding to human trials, but the U.S. is facing a monkey shortage after China stopped exporting the animals, possibly because it needed them for research. And other biomedical research is now more difficult because of physical-distancing requirements. “Usually we had people packed in, but with COVID, we do shift work,” Akiko Iwasaki, a Yale immunologist, told me. “People are coming in at ridiculous hours” to protect themselves from the very virus they are trying to study.
Recommended Reading

What the Chaos in Hospitals Is Doing to Doctors

How the Pandemic Defeated America

Why Are American Homes So Big?
Experts on emerging diseases are scarce: These threats go neglected by the public in the lulls between epidemics. “Just a year ago I had to explain to people why I was studying coronaviruses,” says Lisa Gralinski of the University of North Carolina at Chapel Hill. “That’s never going to be a concern again.” Stressed and stretched, she and other emerging-disease researchers were also conscripted into unfamiliar roles. They’re acting as makeshift advisers to businesses, schools, and local governments. They’re barraged by interview requests from journalists. They’re explaining the nuances of the pandemic on Twitter, to huge new follower counts. “It’s often the same person who’s helping the Namibian government to manage malaria outbreaks and is now being pulled into helping Maryland manage COVID‑19,” Gardner told me.
But the newfound global interest in viruses also means “you have a lot more people you can talk through problems with,” Pardis Sabeti, a computational geneticist at the Broad Institute of MIT and Harvard, told me. Indeed, COVID‑19 papers are more likely than typical biomedical studies to have authors who had never published together before, according to a team led by Ying Ding, who works at the University of Texas at Austin.
Fast-forming alliances could work at breakneck speed because many researchers had spent the past few decades transforming science from a plodding, cloistered endeavor into something nimbler and more transparent. Traditionally, a scientist submits her paper to a journal, which sends it to a (surprisingly small) group of peers for (several rounds of usually anonymous) comments; if the paper passes this (typically months-long) peer-review gantlet, it is published (often behind an expensive paywall). Languid and opaque, this system is ill-suited to a fast-moving outbreak. But biomedical scientists can now upload preliminary versions of their papers, or “preprints,” to freely accessible websites, allowing others to immediately dissect and build upon their results. This practice had been slowly gaining popularity before 2020, but proved so vital for sharing information about COVID‑19 that it will likely become a mainstay of modern biomedical research. Preprints accelerate science, and the pandemic accelerated the use of preprints. At the start of the year, one repository, medRxiv (pronounced “med archive”), held about 1,000 preprints. By the end of October, it had more than 12,000.
Open data sets and sophisticated new tools to manipulate them have likewise made today’s researchers more flexible. SARS‑CoV‑2’s genome was decoded and shared by Chinese scientists just 10 days after the first cases were reported. By November, more than 197,000 SARS‑CoV‑2 genomes had been sequenced. About 90 years ago, no one had even seen an individual virus; today, scientists have reconstructed the shape of SARS‑CoV‑2 down to the position of individual atoms. Researchers have begun to uncover how SARS‑CoV‑2 compares with other coronaviruses in wild bats, the likely reservoir; how it infiltrates and co-opts our cells; how the immune system overreacts to it, creating the symptoms of COVID‑19. “We’re learning about this virus faster than we’ve ever learned about any virus in history,” Sabeti said.
By March, the odds of quickly eradicating the new coronavirus looked slim. A vaccine became the likeliest endgame, and the race to create one was a resounding success. The process normally takes years, but as I write this, 54 different vaccines are being tested for safety and efficacy, and 12 have entered Phase 3 clinical trials—the final checkpoint. As of this writing, Pfizer/BioNTech and Moderna have announced that, based on preliminary results from these trials, their respective vaccines are roughly 95 percent effective at preventing COVID‑19. * “We went from a virus whose sequence was only known in January, and now in the fall, we’re finishing— finishing —a Phase 3 trial,” Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases and a member of the White House’s coronavirus task force, told me. “Holy mackerel.”
Most vaccines comprise dead, weakened, or fragmented pathogens, and must be made from scratch whenever a new threat emerges. But over the past decade, the U.S. and other countries have moved away from this slow “one bug, one drug” approach. Instead, they’ve invested in so-called platform technologies, in which a standard chassis can be easily customized with different payloads that target new viruses. For example, the Pfizer/BioNTech and Moderna vaccines both consist of nanoparticles that contain pieces of SARS‑CoV‑2’s genetic material—its mRNA. When volunteers are injected with these particles, their cells use the mRNA to reconstruct a noninfectious fragment of the virus, allowing their immune system to prepare antibodies that neutralize it. No company has ever brought an mRNA vaccine to market before, but because the basic platform had already been refined, researchers could quickly repurpose it with SARS‑CoV‑2’s mRNA. Moderna got its vaccine into Phase 1 clinical trials on March 16, just 66 days after the new virus’s genome was first uploaded—far faster than any pre-COVID vaccine.
Meanwhile, companies compressed the process of vaccine development by running what would normally be sequential steps in parallel, while still checking for safety and efficacy. The federal government’s Operation Warp Speed, an effort to accelerate vaccine distribution, funded several companies at once—an unusual move. It preordered doses and invested in manufacturing facilities before trials were complete, reducing the risk for pharmaceutical companies looking to participate. Ironically, federal ineptitude at containing SARS‑CoV‑2 helped too. In the U.S., “the fact that the virus is everywhere makes it easier to gauge the performance of a vaccine,” says Natalie Dean of the University of Florida, who studies vaccine trials. “You can’t do a [Phase 3] vaccine trial in South Korea,” because the outbreak there is under control.
Read: How the pandemic will end
Vaccines will not immediately end the pandemic . Millions of doses will have to be manufactured, allocated, and distributed ; large numbers of Americans could refuse the vaccine ; and how long vaccine-induced immunity will last is still unclear. In the rosiest scenario, the Pfizer/BioNTech and Moderna vaccines are approved and smoothly rolled out over the next 12 months. By the end of the year, the U.S. achieves herd immunity, after which the virus struggles to find susceptible hosts. It still circulates, but outbreaks are sporadic and short-lived. Schools and businesses reopen. Families hug tightly and celebrate joyously over Thanksgiving and Christmas.
And the next time a mystery pathogen emerges, scientists hope to quickly slot its genetic material into proven platforms, and move the resulting vaccines through the same speedy pipelines that were developed during this pandemic. “I don’t think the world of vaccine development will ever be the same again,” says Nicole Lurie of the Coalition for Epidemic Preparedness Innovations.
As fast as the vaccine-development process was, it could have been faster. Despite the stakes, some pharmaceutical companies with relevant expertise chose not to enter the race, perhaps dissuaded by intense competition. Instead, from February to May, the sector roughly tripled its efforts to develop drugs to treat COVID‑19, according to Kevin Bryan, an economist at the University of Toronto. The decades-old steroid dexamethasone turned out to reduce death rates among severely ill patients on ventilators by more than 12 percent. Early hints suggest that newer treatments such as the monoclonal-antibody therapy bamlanivimab, which was just approved for emergency use by the FDA, could help newly infected patients who have not yet been hospitalized. But although these wins are significant, they are scarce. Most drugs haven’t been effective. Health-care workers became better at saving hospitalized patients more through improvements in basic medical care than through pharmaceutical panaceas—a predictable outcome, because antiviral drugs tend to offer only modest benefits.
The quest for COVID‑19 treatments was slowed by a torrent of shoddy studies whose results were meaningless at best and misleading at worst. Many of the thousands of clinical trials that were launched were too small to produce statistically solid results. Some lacked a control group—a set of comparable patients who received a placebo, and who provided a baseline against which the effects of a drug could be judged. Other trials needlessly overlapped. At least 227 involved hydroxychloroquine—the antimalarial drug that Donald Trump hyped for months. A few large trials eventually confirmed that hydroxychloroquine does nothing for COVID‑19 patients, but not before hundreds of thousands of people were recruited into pointlessly small studies . More than 100,000 Americans have also received convalescent plasma—another treatment that Trump touted. But because most were not enrolled in rigorous trials, “we still don’t know if it works—and it likely doesn’t,” says Luciana Borio, the former director for medical and biodefense preparedness at the National Security Council. “What a waste of time and resources.”
Read: How we survive the winter
In the heat of a disaster, when emergency rooms are filling and patients are dying, it is hard to set up one careful study, let alone coordinate several across a country. But coordination is not impossible. During World War II , federal agencies unified private companies, universities, the military, and other entities in a carefully orchestrated effort to speed pharmaceutical development from benchtop to battlefield. The results—revolutionary malaria treatments, new ways of mass-producing antibiotics, and at least 10 new or improved vaccines for influenza and other diseases—represented “not a triumph of scientific genius but rather of organizational purpose and efficiency,” Kendall Hoyt of Dartmouth College has written.
Similar triumphs occurred last year—in other countries. In March, taking advantage of the United Kingdom’s nationalized health system, British researchers launched a nationwide study called Recovery, which has since enrolled more than 17,600 COVID‑19 patients across 176 institutions. Recovery offered conclusive answers about dexamethasone and hydroxychloroquine and is set to weigh in on several other treatments. No other study has done more to shape the treatment of COVID‑19. The U.S. is now catching up. In April, the NIH launched a partnership called ACTIV , in which academic and industry scientists prioritized the most promising drugs and coordinated trial plans across the country. Since August, several such trials have started. This model was late, but is likely to outlast the pandemic itself, allowing future researchers to rapidly sort medical wheat from pharmaceutical chaff. “I can’t imagine we’ll go back to doing clinical research in the future the way we did in the past,” the NIH’s Francis Collins said.
Even after the COVID‑19 pandemic, the fruits of the pivot will leave us better equipped for our long and intensifying war against harmful viruses. The last time a virus caused this much devastation—the flu pandemic of 1918—scientists were only just learning about viruses, and spent time looking for a bacterial culprit. This one is different. With so many scientists observing intently as a virus wreaks its horrible work upon millions of bodies, the world is learning lessons that could change the way we think about these pathogens forevermore.
Consider the long-term consequences of viral infections. Years after the original SARS virus hit Hong Kong in 2003, about a quarter of survivors still had myalgic encephalomyelitis—a chronic illness whose symptoms, such as extreme fatigue and brain fogs, can worsen dramatically after mild exertion. ME cases are thought to be linked to viral infections, and clusters sometimes follow big outbreaks. So when SARS‑CoV‑2 started spreading, people with ME were unsurprised to hear that tens of thousands of COVID‑19 “long-haulers” were experiencing incapacitating symptoms that rolled on for months . “Everyone in my community has been thinking about this since the start of the pandemic,” says Jennifer Brea, the executive director of the advocacy group #MEAction.
ME and sister illnesses such as dysautonomia, fibromyalgia, and mast cell activation syndrome have long been neglected, their symptoms dismissed as imaginary or psychiatric. Research is poorly funded, so few scientists study them. Little is known about how to prevent and treat them. This negligence has left COVID‑19 long-haulers with few answers or options, and they initially endured the same dismissal as the larger ME community. But their sheer numbers have forced a degree of recognition. They started researching, cataloging their own symptoms. They gained audiences with the NIH and the World Health Organization. Patients who are themselves experts in infectious disease or public health published their stories in top journals. “Long COVID” is being taken seriously, and Brea hopes it might drag all post-infection illnesses into the spotlight. ME never experienced a pivot. COVID‑19 might inadvertently create one.
Anthony Fauci hopes so. His career was defined by HIV, and in 2019 he said in a paper he co-wrote that “the collateral advantages of” studying HIV “have been profound.” Research into HIV/AIDS revolutionized our understanding of the immune system and how diseases subvert it. It produced techniques for developing antiviral drugs that led to treatments for hepatitis C. Inactivated versions of HIV have been used to treat cancers and genetic disorders. From one disease came a cascade of benefits. COVID‑19 will be no different. Fauci had personally seen cases of prolonged symptoms after other viral infections, but “I didn’t really have a good scientific handle on it,” he told me. Such cases are hard to study, because it’s usually impossible to identify the instigating pathogen. But COVID‑19 has created “the most unusual situation imaginable,” Fauci said—a massive cohort of people with long-haul symptoms that are almost certainly caused by one known virus. “It’s an opportunity we cannot lose,” he said.
Read: The core lesson of the COVID-19 heart debate
COVID‑19 has developed a terrifying mystique because it seems to behave in unusual ways. It causes mild symptoms in some but critical illness in others. It is a respiratory virus and yet seems to attack the heart, brain, kidneys, and other organs. It has reinfected a small number of people who had recently recovered. But many other viruses share similar abilities; they just don’t infect millions of people in a matter of months or grab the attention of the entire scientific community. Thanks to COVID‑19, more researchers are looking for these rarer sides of viral infections, and spotting them.
At least 20 known viruses, including influenza and measles, can trigger myocarditis—inflammation of the heart. Some of these cases resolve on their own, but others cause persistent scarring, and still others rapidly progress into lethal problems. No one knows what proportion of people with viral myocarditis experience the most mild fate, because doctors typically notice only those who seek medical attention. But now researchers are also intently scrutinizing the hearts of people with mild or asymptomatic COVID‑19 infections, including college athletes, given concerns about sudden cardiac arrest during strenuous workouts. The lessons from these efforts could ultimately avert deaths from other infections.
Respiratory viruses, though extremely common, are often neglected. Respiratory syncytial virus, parainfluenza viruses, rhinoviruses, adenoviruses, bocaviruses, a quartet of other human coronaviruses—they mostly cause mild coldlike illnesses, but those can be severe. How often? Why? It’s hard to say, because, influenza aside, such viruses attract little funding or interest. “There’s a perception that they’re just colds and there’s nothing much to learn,” says Emily Martin of the University of Michigan, who has long struggled to get funding to study them. Such reasoning is shortsighted folly. Respiratory viruses are the pathogens most likely to cause pandemics, and those outbreaks could potentially be far worse than COVID‑19’s.
Read: We need to talk about ventilation
Their movements through the air have been poorly studied, too. “There’s this very entrenched idea,” says Linsey Marr at Virginia Tech, that viruses mostly spread through droplets (short-range globs of snot and spit) rather than aerosols (smaller, dustlike flecks that travel farther). That idea dates back to the 1930s, when scientists were upending outdated notions that disease was caused by “bad air,” or miasma. But the evidence that SARS‑CoV‑2 can spread through aerosols “is now overwhelming,” says Marr, one of the few scientists who, before the pandemic, studied how viruses spread through air. “I’ve seen more acceptance in the last six months than over the 12 years I’ve been working on this.”
Another pandemic is inevitable, but it will find a very different community of scientists than COVID‑19 did. They will immediately work to determine whether the pathogen—most likely another respiratory virus—moves through aerosols, and whether it spreads from infected people before causing symptoms. They might call for masks and better ventilation from the earliest moments, not after months of debate. They will anticipate the possibility of an imminent wave of long-haul symptoms, and hopefully discover ways of preventing them. They might set up research groups to prioritize the most promising drugs and coordinate large clinical trials. They might take vaccine platforms that worked best against COVID‑19, slot in the genetic material of the new pathogen, and have a vaccine ready within months.
For all its benefits, the single-minded focus on COVID‑19 will also leave a slew of negative legacies. Science is mostly a zero-sum game, and when one topic monopolizes attention and money, others lose out. Last year, between physical-distancing restrictions, redirected funds, and distracted scientists, many lines of research slowed to a crawl. Long-term studies that monitored bird migrations or the changing climate will forever have holes in their data because field research had to be canceled. Conservationists who worked to protect monkeys and apes kept their distance for fear of passing COVID‑19 to already endangered species. Roughly 80 percent of non-COVID‑19 clinical trials in the U.S.—likely worth billions of dollars—were interrupted or stopped because hospitals were overwhelmed and volunteers were stuck at home. Even research on other infectious diseases was back-burnered. “All the non-COVID work that I was working on before the pandemic started is now piling up and gathering dust,” says Angela Rasmussen of Georgetown University, who normally studies Ebola and MERS. “Those are still problems.”
The COVID‑19 pandemic is a singular disaster, and it is reasonable for society—and scientists—to prioritize it. But the pivot was driven by opportunism as much as altruism. Governments, philanthropies, and universities channeled huge sums toward COVID‑19 research. The NIH alone received nearly $3.6 billion from Congress. The Bill & Melinda Gates Foundation apportioned $350 million for COVID‑19 work. “Whenever there’s a big pot of money, there’s a feeding frenzy,” Madhukar Pai told me. He works on tuberculosis, which causes 1.5 million deaths a year—comparable to COVID‑19’s toll in 2020. Yet tuberculosis research has been mostly paused. None of Pai’s colleagues pivoted when Ebola or Zika struck, but “half of us have now swung to working on COVID‑19,” he said. “It’s a black hole, sucking us all in.”
While the most qualified experts became quickly immersed in the pandemic response, others were stuck at home looking for ways to contribute. Using the same systems that made science faster, they could download data from free databases, run quick analyses with intuitive tools, publish their work on preprint servers, and publicize it on Twitter. Often, they made things worse by swerving out of their scholarly lanes and plowing into unfamiliar territory. Nathan Ballantyne, a philosopher at Fordham University, calls this “ epistemic trespassing .” It can be a good thing: Continental drift was championed by Alfred Wegener, a meteorologist; microbes were first documented by Antonie van Leeuwenhoek, a draper. But more often than not, epistemic trespassing just creates a mess, especially when inexperience couples with overconfidence.
On March 28, a preprint noted that countries that universally use a tuberculosis vaccine called BCG had lower COVID‑19 mortality rates. But such cross-country comparisons are infamously treacherous. For example, countries with higher cigarette-usage rates have longer life expectancies, not because smoking prolongs life but because it is more popular in wealthier nations. This tendency to draw faulty conclusions about individual health using data about large geographical regions is called the ecological fallacy. Epidemiologists know to avoid it. The BCG-preprint authors, who were from an osteopathic college in New York, didn’t seem to . But their paper was covered by more than 70 news outlets, and dozens of inexperienced teams offered similarly specious analyses. “People who don’t know how to spell tuberculosis have told me they can solve the link between BCG and COVID‑19,” Pai said. “Someone told me they can do it in 48 hours with a hackathon.”

Other epistemic trespassers spent their time reinventing the wheel. One new study, published in NEJM , used lasers to show that when people speak, they release aerosols. But as the authors themselves note, the same result—sans lasers—was published in 1946, Marr says. I asked her whether any papers from the 2020 batch had taught her something new. After an uncomfortably long pause, she mentioned just one.
In some cases, bad papers helped shape the public narrative of the pandemic. On March 16, two biogeographers published a preprint arguing that COVID‑19 will “marginally affect the tropics” because it fares poorly in warm, humid conditions. Disease experts quickly noted that techniques like the ones the duo used are meant for modeling the geographic ranges of animal and plant species or vector-borne pathogens, and are ill-suited to simulating the spread of viruses like SARS-CoV-2. But their claim was picked up by more than 50 news outlets and echoed by the United Nations World Food Program. COVID‑19 has since run rampant in many tropical countries, including Brazil, Indonesia, and Colombia—and the preprint’s authors have qualified their conclusions in later versions of the paper. “It takes a certain type of person to think that weeks of reading papers gives them more perspective than someone with a Ph.D. on that subject, and that type of person has gotten a lot of airtime in this pandemic,” says Colin Carlson of Georgetown.
The incentives to trespass are substantial. Academia is a pyramid scheme: Each biomedical professor trains an average of six doctoral students across her career, but only 16 percent of the students get tenure-track positions . Competition is ferocious, and success hinges on getting published—a feat made easier by dramatic results. These factors pull researchers toward speed, short-termism, and hype at the expense of rigor—and the pandemic intensified that pull. With an anxious world crying out for information, any new paper could immediately draw international press coverage—and hundreds of citations.
The tsunami of rushed but dubious work made life harder for actual experts, who struggled to sift the signal from the noise. They also felt obliged to debunk spurious research in long Twitter threads and relentless media interviews—acts of public service that are rarely rewarded in academia. And they were overwhelmed by requests to peer-review new papers. Kristian Andersen, an infectious-disease researcher at Scripps Research, told me that journals used to send him two or three such requests a month. Now “I’m getting three or five a day,” he said in September.
The pandemic’s opportunities also fell inequitably upon the scientific community. In March, Congress awarded $75 million to the National Science Foundation to fast-track studies that could quickly contribute to the pandemic response. “That money just went ,” says Cassidy Sugimoto of Indiana University, who was on rotation at the agency at the time. “It was a first-come, first-served environment. It advantaged people who were aware of the system and could act upon it quickly.” But not all scientists could pivot to COVID‑19, or pivot with equal speed.
Among scientists, as in other fields, women do more child care, domestic work, and teaching than men, and are more often asked for emotional support by their students. These burdens increased as the pandemic took hold, leaving women scientists “less able to commit their time to learning about a new area of study, and less able to start a whole new research project,” says Molly M. King, a sociologist at Santa Clara University. Women’s research hours fell by nine percentage points more than did men’s because of the pressures of COVID‑19. And when COVID‑19 created new opportunities, men grabbed them more quickly. In the spring, the proportion of papers with women as first authors fell almost 44 percent in the preprint repository medRxiv, relative to 2019. And published COVID‑19 papers had 19 percent fewer women as first authors compared with papers from the same journals in the previous year. Men led more than 80 percent of national COVID‑19 task forces in 87 countries . Male scientists were quoted four times as frequently as female scientists in American news stories about the pandemic.
American scientists of color also found it harder to pivot than their white peers, because of unique challenges that sapped their time and energy. Black, Latino, and Indigenous scientists were most likely to have lost loved ones, adding mourning to their list of duties. Many grieved, too, after the killings of Breonna Taylor, George Floyd, Ahmaud Arbery, and others. They often faced questions from relatives who were mistrustful of the medical system, or were experiencing discriminatory care. They were suddenly tasked with helping their predominantly white institutions fight racism. Neil Lewis Jr. at Cornell, who studies racial health disparities, told me that many psychologists had long deemed his work irrelevant. “All of a sudden my inbox is drowning,” he said, while some of his own relatives have become ill and one has died.
Science suffers from the so-called Matthew effect, whereby small successes snowball into ever greater advantages, irrespective of merit. Similarly, early hindrances linger. Young researchers who could not pivot because they were too busy caring or grieving for others might suffer lasting consequences from an unproductive year. COVID‑19 “has really put the clock back in terms of closing the gap for women and underrepresented minorities,” Yale’s Akiko Iwasaki says. “Once we’re over the pandemic, we’ll need to fix it all again.”
COVID-19 has already changed science immensely, but if scientists are savvy, the most profound pivot is still to come—a grand reimagining of what medicine should be. In 1848, the Prussian government sent a young physician named Rudolf Virchow to investigate a typhus epidemic in Upper Silesia. Virchow didn’t know what caused the devastating disease, but he realized its spread was possible because of malnutrition, hazardous working conditions, crowded housing, poor sanitation, and the inattention of civil servants and aristocrats—problems that require social and political reforms. “Medicine is a social science,” Virchow said, “and politics is nothing but medicine in larger scale.”
This viewpoint fell by the wayside after germ theory became mainstream in the late 19th century. When scientists discovered the microbes responsible for tuberculosis, plague, cholera, dysentery, and syphilis, most fixated on these newly identified nemeses. Societal factors were seen as overly political distractions for researchers who sought to “be as ‘objective’ as possible,” says Elaine Hernandez, a medical sociologist at Indiana University. In the U.S., medicine fractured. New departments of sociology and cultural anthropology kept their eye on the societal side of health, while the nation’s first schools of public health focused instead on fights between germs and individuals. This rift widened as improvements in hygiene, living standards, nutrition, and sanitation lengthened life spans: The more social conditions improved, the more readily they could be ignored.
The ideological pivot away from social medicine began to reverse in the second half of the 20th century. The women’s-rights and civil-rights movements, the rise of environmentalism, and anti-war protests created a generation of scholars who questioned “the legitimacy, ideology, and practice of any science … that disregards social and economic inequality,” wrote Nancy Krieger of Harvard . Beginning in the 1980s, this new wave of social epidemiologists once again studied how poverty, privilege, and living conditions affect a person’s health—to a degree even Virchow hadn’t imagined. But as COVID‑19 has shown, the reintegration is not yet complete.
Politicians initially described COVID‑19 as a “great equalizer,” but when states began releasing demographic data, it was immediately clear that the disease was disproportionately infecting and killing people of color . These disparities aren’t biological. They stem from decades of discrimination and segregation that left minority communities in poorer neighborhoods with low-paying jobs, more health problems, and less access to health care—the same kind of problems that Virchow identified more than 170 years ago.
From the September 2020 issue: How the pandemic defeated America
Simple acts like wearing a mask and staying at home, which rely on people tolerating discomfort for the collective good, became society’s main defenses against the virus in the many months without effective drugs or vaccines. These are known as nonpharmaceutical interventions—a name that betrays medicine’s biological bias. For most of 2020, these were the only interventions on offer, but they were nonetheless defined in opposition to the more highly prized drugs and vaccines.
In March, when the U.S. started shutting down, one of the biggest questions on the mind of Whitney Robinson of UNC at Chapel Hill was: Are our kids going to be out of school for two years? While biomedical scientists tend to focus on sickness and recovery, social epidemiologists like her “think about critical periods that can affect the trajectory of your life,” she told me. Disrupting a child’s schooling at the wrong time can affect their entire career, so scientists should have prioritized research to figure out whether and how schools could reopen safely. But most studies on the spread of COVID‑19 in schools were neither large in scope nor well-designed enough to be conclusive. No federal agency funded a large, nationwide study, even though the federal government had months to do so. The NIH received billions for COVID‑19 research , but the National Institute of Child Health and Human Development—one of its 27 constituent institutes and centers—got nothing.
The horrors that Rudolf Virchow saw in Upper Silesia radicalized him, pushing the future “father of modern pathology” to advocate for social reforms. The current pandemic has affected scientists in the same way. Calm researchers became incensed as potentially game-changing innovations like cheap diagnostic tests were squandered by a negligent administration and a muzzled Centers for Disease Control and Prevention. Austere publications like NEJM and Nature published explicitly political editorials castigating the Trump administration for its failures and encouraging voters to hold the president accountable. COVID‑19 could be the catalyst that fully reunifies the social and biological sides of medicine, bridging disciplines that have been separated for too long.
“To study COVID‑19 is not only to study the disease itself as a biological entity,” says Alondra Nelson, the president of the Social Science Research Council. “What looks like a single problem is actually all things, all at once. So what we’re actually studying is literally everything in society, at every scale, from supply chains to individual relationships.”
The scientific community spent the pre-pandemic years designing faster ways of doing experiments, sharing data, and developing vaccines, allowing it to mobilize quickly when COVID‑19 emerged. Its goal now should be to address its many lingering weaknesses. Warped incentives, wasteful practices, overconfidence, inequality, a biomedical bias—COVID‑19 has exposed them all. And in doing so, it offers the world of science a chance to practice one of its most important qualities: self-correction.
* The print version of this article stated that the Moderna and Pfizer/BioNTech vaccines were reported to be 95 percent effective at preventing COVID-19 infections. In fact, the vaccines prevent disease, not infection.
This article appears in the January/February 2021 print edition with the headline “The COVID-19 Manhattan Project.”

Morning Edition
Listen live.

BBC Newshour
In-depth analysis and commentary on today's biggest news stories as only the BBC can deliver. BBC "Newshour" covers everything from the growth of democracy to the threat of terrorism with a fresh, clear perspective from across the globe.
Coronavirus: The world has come together to flatten the curve. Can we stay united to tackle other crises?
Watching the world come together gives me hope for the future, writes mira patel, a high school junior..

Mira Patel and her sister Veda. (Courtesy of Dee Patel)
Related Content

This 24-year-old entrepreneur is helping Black-owned restaurants survive coronavirus
Black and Mobile is an online delivery service that caters to Black-owned restaurants. The coronavirus shutdown has increased demand for its service.
4 years ago

Home desks won’t replace Philly’s high-rise office towers anytime soon, analysts say
Philadelphia’s office market might fare better post-coronavirus than those of other U.S. cities, CBRE analysts said in a new report.
Before the pandemic, I had often heard adults say that young people would lose the ability to connect in-person with others due to our growing dependence on technology and social media. However, this stay-at-home experience has proven to me that our elders’ worry is unnecessary. Because isolation isn’t in human nature, and no advancement in technology could replace our need to meet in person, especially when it comes to learning.
As the weather gets warmer and we approach summertime, it’s going to be more and more tempting for us teenagers to go out and do what we have always done: hang out and have fun. Even though the decision-makers are adults, everyone has a role to play and we teens can help the world move forward by continuing to self-isolate. It’s incredibly important that in the coming weeks, we respect the government’s effort to contain the spread of the coronavirus.
In the meantime, we can find creative ways to stay connected and continue to do what we love. Personally, I see many 6-feet-apart bike rides and Zoom calls in my future.
If there is anything that this pandemic has made me realize, it’s how connected we all are. At first, the infamous coronavirus seemed to be a problem in China, which is worlds away. But slowly, it steadily made its way through various countries in Europe, and inevitably reached us in America. What was once framed as a foreign virus has now hit home.
Watching the global community come together, gives me hope, as a teenager, that in the future we can use this cooperation to combat climate change and other catastrophes.
As COVID-19 continues to creep its way into each of our communities and impact the way we live and communicate, I find solace in the fact that we face what comes next together, as humanity.
When the day comes that my generation is responsible for dealing with another crisis, I hope we can use this experience to remind us that moving forward requires a joint effort.
Mira Patel is a junior at Strath Haven High School and is an education intern at the Foreign Policy Research Institute in Philadelphia. Follow her on Instagram here.
Becoming a storyteller at WHYY, your local public media station, is easier than you might think. Text STORYTELLER to 267-494-9949 to learn more.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
Part of the series

Coronavirus Pandemic
You may also like.
Threats and violence suspend high school football games Friday night
Fight breaks out at a game between Pennsauken and Camden High Schools, threats suspend games in Chester and Northampton Counties.
3 years ago

Philly students get vaxxed at the zoo before heading back to school
The event is the first of its kind for the school district, but arrives after months of partnering with CHOP to organize other vaccination clinics around the city.

Montco high school senior reflects on missing experiences because of coronavirus
Grace Honeyman, a senior at Harriton High School, talks with her father about how she’s dealing with missing milestones due to coronavirus.
Want a digest of WHYY’s programs, events & stories? Sign up for our weekly newsletter.
Together we can reach 100% of WHYY’s fiscal year goal
- Fact sheets
- Facts in pictures
- Publications
- Questions and answers
- Tools and toolkits
- Endometriosis
- Excessive heat
- Mental disorders
- Polycystic ovary syndrome
- All countries
- Eastern Mediterranean
- South-East Asia
- Western Pacific
- Data by country
- Country presence
- Country strengthening
- Country cooperation strategies
- News releases
- Feature stories
- Press conferences
- Commentaries
- Photo library
- Afghanistan
- Cholera
- Coronavirus disease (COVID-19)
- Greater Horn of Africa
- Israel and occupied Palestinian territory
- Disease Outbreak News
- Situation reports
- Weekly Epidemiological Record
- Surveillance
- Health emergency appeal
- International Health Regulations
- Independent Oversight and Advisory Committee
- Classifications
- Data collections
- Global Health Estimates
- Mortality Database
- Sustainable Development Goals
- Health Inequality Monitor
- Global Progress
- Data collection tools
- Global Health Observatory
- Insights and visualizations
- COVID excess deaths
- World Health Statistics
- Partnerships
- Committees and advisory groups
- Collaborating centres
- Technical teams
- Organizational structure
- Initiatives
- General Programme of Work
- WHO Academy
- Investment in WHO
- WHO Foundation
- External audit
- Financial statements
- Internal audit and investigations
- Programme Budget
- Results reports
- Governing bodies
- World Health Assembly
- Executive Board
- Member States Portal
- Questions and answers /
Coronavirus disease (COVID-19): Post COVID-19 condition
Most people who develop COVID-19 fully recover, but current evidence suggests approximately 10–20% of people experience a variety of mid and long-term effects after they recover from their initial illness. Although our current understanding of causes of post COVID-19 condition and why some people are more affected is limited, this questions and answers page will help you understand more about post COVID-19 condition so you can make informed decisions that help protect yourself and those around you.
Post COVID-19 condition, also known as long COVID, refers to long-term symptoms that some people experience after they have had COVID-19. People who experience post COVID-19 condition sometimes refer to themselves as “long-haulers”.
These symptoms might persist from their initial illness or develop after their recovery. They can come and go or relapse over time.
The most common symptoms associated with post COVID-19 condition include fatigue, breathlessness and cognitive dysfunction (for example, confusion, forgetfulness, or a lack of mental focus or clarity). Post COVID-19 condition can affect a person’s ability to perform daily activities such as work or household chores.
Post COVID-19 condition is usually diagnosed by a healthcare provider at least 3 months after a patient falls ill with COVID-19. This 3-month period allows healthcare providers to rule out the usual recovery period from an acute illness. Sometimes this recovery period can be long, especially if someone is very sick.
Symptoms should last for at least 2 months from when someone first falls ill for it to be considered as post COVID-19 condition.
Symptoms of post COVID-19 condition can persist from the initial illness or begin after recovery. The symptoms and effects of post COVID-19 condition can only be explained when other conditions with similar symptoms as post COVID-19 condition have been ruled out through a medical diagnosis. Symptoms may also change over time.
Symptoms differ between people, and between adults and children. Overall, the most common symptoms of post COVID-19 condition include:
- shortness of breath or difficulty breathing
- memory, concentration or sleep problems
- persistent cough
- trouble speaking
- muscle aches
- loss of smell or taste
- depression or anxiety
People with post COVID-19 condition, also known as long COVID, may have difficulty functioning in everyday life. Their condition may affect their ability to perform daily activities such as work or household chores.
If you have ongoing symptoms after COVID-19, seek help from your healthcare provider. They will help you to determine the cause and provide you with the care you need to manage your symptoms.
At present, there are no proven drug treatments for post COVID-19 condition. This is an area of active research. However, some commonly available medications can alleviate symptoms. There are data suggesting that holistic care can help patients regain their physical, cognitive and emotional function and help to improve their quality of life.
Anyone can develop post COVID-19 condition. Research suggests that approximately 10–20% of COVID-19 patients go on to develop prolonged symptoms that are associated with post COVID-19 condition. Current evidence doesn’t allow us to confidently know who is more likely to be affected, although certain problems (for example breathlessness) seem to be more common amongst those with more severe initial COVID-19, and more common in women.
According to the WHO definition, symptoms should last two months or more before a diagnosis of post COVID-19 condition can be made, as we know that normal recovery can take this long. It is important that other causes for ongoing symptoms are considered. For more information, see the clinical case definition of post COVID-19 condition.
We cannot predict how long post COVID-19 condition will last for any given person. Most people experience improvement in their symptoms, but we know that lingering symptoms can last from weeks to months. Currently, it remains impossible to predict how long post COVID-19 condition may last for any given person.
Taking measures to avoid COVID-19 infection is the most effective way to protect yourself against post COVID-19 condition. This includes public health and social measures that reduce your chances of getting infected. To keep you and your family safe remember to:
- continue to wash your hands regularly
- keep a distance from others
- wear a mask when in a crowded, enclosed or poorly ventilated area
- get vaccinated and stay up to date with booster doses
- practice respiratory etiquette; cough or sneeze into your bent elbow.
Research is ongoing. A vaccine’s ability to prevent post COVID-19 condition depends on its ability to prevent COVID-19 in the first place. The vaccines we use today are aimed at preventing severe disease and death from COVID-19. However, some people may still get infected with COVID-19 even after they are vaccinated.
No, post COVID-19 condition cannot be passed to others.
WHO expert group which includes patients, healthcare workers and researchers has been considering the impact of post-COVID-19 condition on children and adolescents. Findings of this report can be found here . A free webinar is available for more information: Post COVID-19 Condition: Children and Young Persons (who.int)
Young children with COVID-19 mainly present with respiratory symptoms and are more likely to seek long-term medical care for a persistent cough. Children with post COVID-19 condition are also more likely to have fatigue, altered smell and anxiety than healthy children.
Essay on COVID-19 Pandemic
As a result of the COVID-19 (Coronavirus) outbreak, daily life has been negatively affected, impacting the worldwide economy. Thousands of individuals have been sickened or died as a result of the outbreak of this disease. When you have the flu or a viral infection, the most common symptoms include fever, cold, coughing up bone fragments, and difficulty breathing, which may progress to pneumonia. It’s important to take major steps like keeping a strict cleaning routine, keeping social distance, and wearing masks, among other things. This virus’s geographic spread is accelerating (Daniel Pg 93). Governments restricted public meetings during the start of the pandemic to prevent the disease from spreading and breaking the exponential distribution curve. In order to avoid the damage caused by this extremely contagious disease, several countries quarantined their citizens. However, this scenario had drastically altered with the discovery of the vaccinations. The research aims to investigate the effect of the Covid-19 epidemic and its impact on the population’s well-being.
There is growing interest in the relationship between social determinants of health and health outcomes. Still, many health care providers and academics have been hesitant to recognize racism as a contributing factor to racial health disparities. Only a few research have examined the health effects of institutional racism, with the majority focusing on interpersonal racial and ethnic prejudice Ciotti et al., Pg 370. The latter comprises historically and culturally connected institutions that are interconnected. Prejudice is being practiced in a variety of contexts as a result of the COVID-19 outbreak. In some ways, the outbreak has exposed pre-existing bias and inequity.
Thousands of businesses are in danger of failure. Around 2.3 billion of the world’s 3.3 billion employees are out of work. These workers are especially susceptible since they lack access to social security and adequate health care, and they’ve also given up ownership of productive assets, which makes them highly vulnerable. Many individuals lose their employment as a result of lockdowns, leaving them unable to support their families. People strapped for cash are often forced to reduce their caloric intake while also eating less nutritiously (Fraser et al, Pg 3). The epidemic has had an impact on the whole food chain, revealing vulnerabilities that were previously hidden. Border closures, trade restrictions, and confinement measures have limited farmer access to markets, while agricultural workers have not gathered crops. As a result, the local and global food supply chain has been disrupted, and people now have less access to healthy foods. As a consequence of the epidemic, many individuals have lost their employment, and millions more are now in danger. When breadwinners lose their jobs, become sick, or die, the food and nutrition of millions of people are endangered. Particularly severely hit are the world’s poorest small farmers and indigenous peoples.
Infectious illness outbreaks and epidemics have become worldwide threats due to globalization, urbanization, and environmental change. In developed countries like Europe and North America, surveillance and health systems monitor and manage the spread of infectious illnesses in real-time. Both low- and high-income countries need to improve their public health capacities (Omer et al., Pg 1767). These improvements should be financed using a mix of national and foreign donor money. In order to speed up research and reaction for new illnesses with pandemic potential, a global collaborative effort including governments and commercial companies has been proposed. When working on a vaccine-like COVID-19, cooperation is critical.
The epidemic has had an impact on the whole food chain, revealing vulnerabilities that were previously hidden. Border closures, trade restrictions, and confinement measures have limited farmer access to markets, while agricultural workers have been unable to gather crops. As a result, the local and global food supply chain has been disrupted, and people now have less access to healthy foods (Daniel et al.,Pg 95) . As a consequence of the epidemic, many individuals have lost their employment, and millions more are now in danger. When breadwinners lose their jobs, the food and nutrition of millions of people are endangered. Particularly severely hit are the world’s poorest small farmers and indigenous peoples.
While helping to feed the world’s population, millions of paid and unpaid agricultural laborers suffer from high levels of poverty, hunger, and bad health, as well as a lack of safety and labor safeguards, as well as other kinds of abuse at work. Poor people, who have no recourse to social assistance, must work longer and harder, sometimes in hazardous occupations, endangering their families in the process (Daniel Pg 96). When faced with a lack of income, people may turn to hazardous financial activities, including asset liquidation, predatory lending, or child labor, to make ends meet. Because of the dangers they encounter while traveling, working, and living abroad; migrant agricultural laborers are especially vulnerable. They also have a difficult time taking advantage of government assistance programs.
The pandemic also has a significant impact on education. Although many educational institutions across the globe have already made the switch to online learning, the extent to which technology is utilized to improve the quality of distance or online learning varies. This level is dependent on several variables, including the different parties engaged in the execution of this learning format and the incorporation of technology into educational institutions before the time of school closure caused by the COVID-19 pandemic. For many years, researchers from all around the globe have worked to determine what variables contribute to effective technology integration in the classroom Ciotti et al., Pg 371. The amount of technology usage and the quality of learning when moving from a classroom to a distant or online format are presumed to be influenced by the same set of variables. Findings from previous research, which sought to determine what affects educational systems ability to integrate technology into teaching, suggest understanding how teachers, students, and technology interact positively in order to achieve positive results in the integration of teaching technology (Honey et al., 2000). Teachers’ views on teaching may affect the chances of successfully incorporating technology into the classroom and making it a part of the learning process.
In conclusion, indeed, Covid 19 pandemic have affected the well being of the people in a significant manner. The economy operation across the globe have been destabilized as most of the people have been rendered jobless while the job operation has been stopped. As most of the people have been rendered jobless the living conditions of the people have also been significantly affected. Besides, the education sector has also been affected as most of the learning institutions prefer the use of online learning which is not effective as compared to the traditional method. With the invention of the vaccines, most of the developed countries have been noted to stabilize slowly, while the developing countries have not been able to vaccinate most of its citizens. However, despite the challenge caused by the pandemic, organizations have been able to adapt the new mode of online trading to be promoted.
Ciotti, Marco, et al. “The COVID-19 pandemic.” Critical reviews in clinical laboratory sciences 57.6 (2020): 365-388.
Daniel, John. “Education and the COVID-19 pandemic.” Prospects 49.1 (2020): 91-96.
Fraser, Nicholas, et al. “Preprinting the COVID-19 pandemic.” BioRxiv (2021): 2020-05.
Omer, Saad B., Preeti Malani, and Carlos Del Rio. “The COVID-19 pandemic in the US: a clinical update.” Jama 323.18 (2020): 1767-1768.
Cite this page
Similar essay samples.
- Project management and quality plan for designing and implementing an ...
- Brexit Case Study
- Essay on the Basic Parts for a Successful Training Program
- Essay on Implications of Sigmund Freud’s Psychoanalysis on the Afric...
- Essay on Artificial Intelligence as a Threat in the Society
- Women’s History Newspaper: Women in the Military
Why the Pandemic Probably Started in a Lab, in 5 Key Points

By Alina Chan
Dr. Chan is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “Viral: The Search for the Origin of Covid-19.”
This article has been updated to reflect news developments.
On Monday, Dr. Anthony Fauci returned to the halls of Congress and testified before the House subcommittee investigating the Covid-19 pandemic. He was questioned about several topics related to the government’s handling of Covid-19, including how the National Institute of Allergy and Infectious Diseases, which he directed until retiring in 2022, supported risky virus work at a Chinese institute whose research may have caused the pandemic.
For more than four years, reflexive partisan politics have derailed the search for the truth about a catastrophe that has touched us all. It has been estimated that at least 25 million people around the world have died because of Covid-19, with over a million of those deaths in the United States.
Although how the pandemic started has been hotly debated, a growing volume of evidence — gleaned from public records released under the Freedom of Information Act, digital sleuthing through online databases, scientific papers analyzing the virus and its spread, and leaks from within the U.S. government — suggests that the pandemic most likely occurred because a virus escaped from a research lab in Wuhan, China. If so, it would be the most costly accident in the history of science.
Here’s what we now know:
1 The SARS-like virus that caused the pandemic emerged in Wuhan, the city where the world’s foremost research lab for SARS-like viruses is located.
- At the Wuhan Institute of Virology, a team of scientists had been hunting for SARS-like viruses for over a decade, led by Shi Zhengli.
- Their research showed that the viruses most similar to SARS‑CoV‑2, the virus that caused the pandemic, circulate in bats that live r oughly 1,000 miles away from Wuhan. Scientists from Dr. Shi’s team traveled repeatedly to Yunnan province to collect these viruses and had expanded their search to Southeast Asia. Bats in other parts of China have not been found to carry viruses that are as closely related to SARS-CoV-2.

The closest known relatives to SARS-CoV-2 were found in southwestern China and in Laos.
Large cities
Mine in Yunnan province
Cave in Laos
South China Sea

The closest known relatives to SARS-CoV-2
were found in southwestern China and in Laos.
philippines

The closest known relatives to SARS-CoV-2 were found
in southwestern China and Laos.
Sources: Sarah Temmam et al., Nature; SimpleMaps
Note: Cities shown have a population of at least 200,000.

There are hundreds of large cities in China and Southeast Asia.

There are hundreds of large cities in China
and Southeast Asia.

The pandemic started roughly 1,000 miles away, in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away,
in Wuhan, home to the world’s foremost SARS-like virus research lab.

The pandemic started roughly 1,000 miles away, in Wuhan,
home to the world’s foremost SARS-like virus research lab.
- Even at hot spots where these viruses exist naturally near the cave bats of southwestern China and Southeast Asia, the scientists argued, as recently as 2019 , that bat coronavirus spillover into humans is rare .
- When the Covid-19 outbreak was detected, Dr. Shi initially wondered if the novel coronavirus had come from her laboratory , saying she had never expected such an outbreak to occur in Wuhan.
- The SARS‑CoV‑2 virus is exceptionally contagious and can jump from species to species like wildfire . Yet it left no known trace of infection at its source or anywhere along what would have been a thousand-mile journey before emerging in Wuhan.
2 The year before the outbreak, the Wuhan institute, working with U.S. partners, had proposed creating viruses with SARS‑CoV‑2’s defining feature.
- Dr. Shi’s group was fascinated by how coronaviruses jump from species to species. To find viruses, they took samples from bats and other animals , as well as from sick people living near animals carrying these viruses or associated with the wildlife trade. Much of this work was conducted in partnership with the EcoHealth Alliance, a U.S.-based scientific organization that, since 2002, has been awarded over $80 million in federal funding to research the risks of emerging infectious diseases.
- The laboratory pursued risky research that resulted in viruses becoming more infectious : Coronaviruses were grown from samples from infected animals and genetically reconstructed and recombined to create new viruses unknown in nature. These new viruses were passed through cells from bats, pigs, primates and humans and were used to infect civets and humanized mice (mice modified with human genes). In essence, this process forced these viruses to adapt to new host species, and the viruses with mutations that allowed them to thrive emerged as victors.
- By 2019, Dr. Shi’s group had published a database describing more than 22,000 collected wildlife samples. But external access was shut off in the fall of 2019, and the database was not shared with American collaborators even after the pandemic started , when such a rich virus collection would have been most useful in tracking the origin of SARS‑CoV‑2. It remains unclear whether the Wuhan institute possessed a precursor of the pandemic virus.
- In 2021, The Intercept published a leaked 2018 grant proposal for a research project named Defuse , which had been written as a collaboration between EcoHealth, the Wuhan institute and Ralph Baric at the University of North Carolina, who had been on the cutting edge of coronavirus research for years. The proposal described plans to create viruses strikingly similar to SARS‑CoV‑2.
- Coronaviruses bear their name because their surface is studded with protein spikes, like a spiky crown, which they use to enter animal cells. T he Defuse project proposed to search for and create SARS-like viruses carrying spikes with a unique feature: a furin cleavage site — the same feature that enhances SARS‑CoV‑2’s infectiousness in humans, making it capable of causing a pandemic. Defuse was never funded by the United States . However, in his testimony on Monday, Dr. Fauci explained that the Wuhan institute would not need to rely on U.S. funding to pursue research independently.

The Wuhan lab ran risky experiments to learn about how SARS-like viruses might infect humans.
1. Collect SARS-like viruses from bats and other wild animals, as well as from people exposed to them.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of human cells.

2. Identify high-risk viruses by screening for spike proteins that facilitate infection of
human cells.

In Defuse, the scientists proposed to add a furin cleavage site to the spike protein.
3. Create new coronaviruses by inserting spike proteins or other features that could make the viruses more infectious in humans.

4. Infect human cells, civets and humanized mice with the new coronaviruses, to determine how dangerous they might be.

- While it’s possible that the furin cleavage site could have evolved naturally (as seen in some distantly related coronaviruses), out of the hundreds of SARS-like viruses cataloged by scientists, SARS‑CoV‑2 is the only one known to possess a furin cleavage site in its spike. And the genetic data suggest that the virus had only recently gained the furin cleavage site before it started the pandemic.
- Ultimately, a never-before-seen SARS-like virus with a newly introduced furin cleavage site, matching the description in the Wuhan institute’s Defuse proposal, caused an outbreak in Wuhan less than two years after the proposal was drafted.
- When the Wuhan scientists published their seminal paper about Covid-19 as the pandemic roared to life in 2020, they did not mention the virus’s furin cleavage site — a feature they should have been on the lookout for, according to their own grant proposal, and a feature quickly recognized by other scientists.
- Worse still, as the pandemic raged, their American collaborators failed to publicly reveal the existence of the Defuse proposal. The president of EcoHealth, Peter Daszak, recently admitted to Congress that he doesn’t know about virus samples collected by the Wuhan institute after 2015 and never asked the lab’s scientists if they had started the work described in Defuse. In May, citing failures in EcoHealth’s monitoring of risky experiments conducted at the Wuhan lab, the Biden administration suspended all federal funding for the organization and Dr. Daszak, and initiated proceedings to bar them from receiving future grants. In his testimony on Monday, Dr. Fauci said that he supported the decision to suspend and bar EcoHealth.
- Separately, Dr. Baric described the competitive dynamic between his research group and the institute when he told Congress that the Wuhan scientists would probably not have shared their most interesting newly discovered viruses with him . Documents and email correspondence between the institute and Dr. Baric are still being withheld from the public while their release is fiercely contested in litigation.
- In the end, American partners very likely knew of only a fraction of the research done in Wuhan. According to U.S. intelligence sources, some of the institute’s virus research was classified or conducted with or on behalf of the Chinese military . In the congressional hearing on Monday, Dr. Fauci repeatedly acknowledged the lack of visibility into experiments conducted at the Wuhan institute, saying, “None of us can know everything that’s going on in China, or in Wuhan, or what have you. And that’s the reason why — I say today, and I’ve said at the T.I.,” referring to his transcribed interview with the subcommittee, “I keep an open mind as to what the origin is.”
3 The Wuhan lab pursued this type of work under low biosafety conditions that could not have contained an airborne virus as infectious as SARS‑CoV‑2.
- Labs working with live viruses generally operate at one of four biosafety levels (known in ascending order of stringency as BSL-1, 2, 3 and 4) that describe the work practices that are considered sufficiently safe depending on the characteristics of each pathogen. The Wuhan institute’s scientists worked with SARS-like viruses under inappropriately low biosafety conditions .

In the United States, virologists generally use stricter Biosafety Level 3 protocols when working with SARS-like viruses.
Biosafety cabinets prevent
viral particles from escaping.
Viral particles
Personal respirators provide
a second layer of defense against breathing in the virus.
DIRECT CONTACT
Gloves prevent skin contact.
Disposable wraparound
gowns cover much of the rest of the body.

Personal respirators provide a second layer of defense against breathing in the virus.
Disposable wraparound gowns
cover much of the rest of the body.
Note: Biosafety levels are not internationally standardized, and some countries use more permissive protocols than others.

The Wuhan lab had been regularly working with SARS-like viruses under Biosafety Level 2 conditions, which could not prevent a highly infectious virus like SARS-CoV-2 from escaping.
Some work is done in the open air, and masks are not required.
Less protective equipment provides more opportunities
for contamination.

Some work is done in the open air,
and masks are not required.
Less protective equipment provides more opportunities for contamination.
- In one experiment, Dr. Shi’s group genetically engineered an unexpectedly deadly SARS-like virus (not closely related to SARS‑CoV‑2) that exhibited a 10,000-fold increase in the quantity of virus in the lungs and brains of humanized mice . Wuhan institute scientists handled these live viruses at low biosafet y levels , including BSL-2.
- Even the much more stringent containment at BSL-3 cannot fully prevent SARS‑CoV‑2 from escaping . Two years into the pandemic, the virus infected a scientist in a BSL-3 laboratory in Taiwan, which was, at the time, a zero-Covid country. The scientist had been vaccinated and was tested only after losing the sense of smell. By then, more than 100 close contacts had been exposed. Human error is a source of exposure even at the highest biosafety levels , and the risks are much greater for scientists working with infectious pathogens at low biosafety.
- An early draft of the Defuse proposal stated that the Wuhan lab would do their virus work at BSL-2 to make it “highly cost-effective.” Dr. Baric added a note to the draft highlighting the importance of using BSL-3 to contain SARS-like viruses that could infect human cells, writing that “U.S. researchers will likely freak out.” Years later, after SARS‑CoV‑2 had killed millions, Dr. Baric wrote to Dr. Daszak : “I have no doubt that they followed state determined rules and did the work under BSL-2. Yes China has the right to set their own policy. You believe this was appropriate containment if you want but don’t expect me to believe it. Moreover, don’t insult my intelligence by trying to feed me this load of BS.”
- SARS‑CoV‑2 is a stealthy virus that transmits effectively through the air, causes a range of symptoms similar to those of other common respiratory diseases and can be spread by infected people before symptoms even appear. If the virus had escaped from a BSL-2 laboratory in 2019, the leak most likely would have gone undetected until too late.
- One alarming detail — leaked to The Wall Street Journal and confirmed by current and former U.S. government officials — is that scientists on Dr. Shi’s team fell ill with Covid-like symptoms in the fall of 2019 . One of the scientists had been named in the Defuse proposal as the person in charge of virus discovery work. The scientists denied having been sick .
4 The hypothesis that Covid-19 came from an animal at the Huanan Seafood Market in Wuhan is not supported by strong evidence.
- In December 2019, Chinese investigators assumed the outbreak had started at a centrally located market frequented by thousands of visitors daily. This bias in their search for early cases meant that cases unlinked to or located far away from the market would very likely have been missed. To make things worse, the Chinese authorities blocked the reporting of early cases not linked to the market and, claiming biosafety precautions, ordered the destruction of patient samples on January 3, 2020, making it nearly impossible to see the complete picture of the earliest Covid-19 cases. Information about dozens of early cases from November and December 2019 remains inaccessible.
- A pair of papers published in Science in 2022 made the best case for SARS‑CoV‑2 having emerged naturally from human-animal contact at the Wuhan market by focusing on a map of the early cases and asserting that the virus had jumped from animals into humans twice at the market in 2019. More recently, the two papers have been countered by other virologists and scientists who convincingly demonstrate that the available market evidence does not distinguish between a human superspreader event and a natural spillover at the market.
- Furthermore, the existing genetic and early case data show that all known Covid-19 cases probably stem from a single introduction of SARS‑CoV‑2 into people, and the outbreak at the Wuhan market probably happened after the virus had already been circulating in humans.

An analysis of SARS-CoV-2’s evolutionary tree shows how the virus evolved as it started to spread through humans.
SARS-COV-2 Viruses closest
to bat coronaviruses
more mutations

Source: Lv et al., Virus Evolution (2024) , as reproduced by Jesse Bloom

The viruses that infected people linked to the market were most likely not the earliest form of the virus that started the pandemic.

- Not a single infected animal has ever been confirmed at the market or in its supply chain. Without good evidence that the pandemic started at the Huanan Seafood Market, the fact that the virus emerged in Wuhan points squarely at its unique SARS-like virus laboratory.
5 Key evidence that would be expected if the virus had emerged from the wildlife trade is still missing.

In previous outbreaks of coronaviruses, scientists were able to demonstrate natural origin by collecting multiple pieces of evidence linking infected humans to infected animals.
Infected animals
Earliest known
cases exposed to
live animals
Antibody evidence
of animals and
animal traders having
been infected
Ancestral variants
of the virus found in
Documented trade
of host animals
between the area
where bats carry
closely related viruses
and the outbreak site

Infected animals found
Earliest known cases exposed to live animals
Antibody evidence of animals and animal
traders having been infected
Ancestral variants of the virus found in animals
Documented trade of host animals
between the area where bats carry closely
related viruses and the outbreak site

For SARS-CoV-2, these same key pieces of evidence are still missing , more than four years after the virus emerged.

For SARS-CoV-2, these same key pieces of evidence are still missing ,
more than four years after the virus emerged.
- Despite the intense search trained on the animal trade and people linked to the market, investigators have not reported finding any animals infected with SARS‑CoV‑2 that had not been infected by humans. Yet, infected animal sources and other connective pieces of evidence were found for the earlier SARS and MERS outbreaks as quickly as within a few days, despite the less advanced viral forensic technologies of two decades ago.
- Even though Wuhan is the home base of virus hunters with world-leading expertise in tracking novel SARS-like viruses, investigators have either failed to collect or report key evidence that would be expected if Covid-19 emerged from the wildlife trade . For example, investigators have not determined that the earliest known cases had exposure to intermediate host animals before falling ill. No antibody evidence shows that animal traders in Wuhan are regularly exposed to SARS-like viruses, as would be expected in such situations.
- With today’s technology, scientists can detect how respiratory viruses — including SARS, MERS and the flu — circulate in animals while making repeated attempts to jump across species . Thankfully, these variants usually fail to transmit well after crossing over to a new species and tend to die off after a small number of infections. In contrast, virologists and other scientists agree that SARS‑CoV‑2 required little to no adaptation to spread rapidly in humans and other animals . The virus appears to have succeeded in causing a pandemic upon its only detected jump into humans.
The pandemic could have been caused by any of hundreds of virus species, at any of tens of thousands of wildlife markets, in any of thousands of cities, and in any year. But it was a SARS-like coronavirus with a unique furin cleavage site that emerged in Wuhan, less than two years after scientists, sometimes working under inadequate biosafety conditions, proposed collecting and creating viruses of that same design.
While several natural spillover scenarios remain plausible, and we still don’t know enough about the full extent of virus research conducted at the Wuhan institute by Dr. Shi’s team and other researchers, a laboratory accident is the most parsimonious explanation of how the pandemic began.
Given what we now know, investigators should follow their strongest leads and subpoena all exchanges between the Wuhan scientists and their international partners, including unpublished research proposals, manuscripts, data and commercial orders. In particular, exchanges from 2018 and 2019 — the critical two years before the emergence of Covid-19 — are very likely to be illuminating (and require no cooperation from the Chinese government to acquire), yet they remain beyond the public’s view more than four years after the pandemic began.
Whether the pandemic started on a lab bench or in a market stall, it is undeniable that U.S. federal funding helped to build an unprecedented collection of SARS-like viruses at the Wuhan institute, as well as contributing to research that enhanced them . Advocates and funders of the institute’s research, including Dr. Fauci, should cooperate with the investigation to help identify and close the loopholes that allowed such dangerous work to occur. The world must not continue to bear the intolerable risks of research with the potential to cause pandemics .
A successful investigation of the pandemic’s root cause would have the power to break a decades-long scientific impasse on pathogen research safety, determining how governments will spend billions of dollars to prevent future pandemics. A credible investigation would also deter future acts of negligence and deceit by demonstrating that it is indeed possible to be held accountable for causing a viral pandemic. Last but not least, people of all nations need to see their leaders — and especially, their scientists — heading the charge to find out what caused this world-shaking event. Restoring public trust in science and government leadership requires it.
A thorough investigation by the U.S. government could unearth more evidence while spurring whistleblowers to find their courage and seek their moment of opportunity. It would also show the world that U.S. leaders and scientists are not afraid of what the truth behind the pandemic may be.
More on how the pandemic may have started

Where Did the Coronavirus Come From? What We Already Know Is Troubling.
Even if the coronavirus did not emerge from a lab, the groundwork for a potential disaster had been laid for years, and learning its lessons is essential to preventing others.
By Zeynep Tufekci

Why Does Bad Science on Covid’s Origin Get Hyped?
If the raccoon dog was a smoking gun, it fired blanks.
By David Wallace-Wells

A Plea for Making Virus Research Safer
A way forward for lab safety.
By Jesse Bloom
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here’s our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
Alina Chan ( @ayjchan ) is a molecular biologist at the Broad Institute of M.I.T. and Harvard, and a co-author of “ Viral : The Search for the Origin of Covid-19.” She was a member of the Pathogens Project , which the Bulletin of the Atomic Scientists organized to generate new thinking on responsible, high-risk pathogen research.
- Share full article
Advertisement
- Paragraph Writing
- Paragraph Writing On Covid 19
Paragraph Writing on Covid 19 - Check Samples for Various Word Limits
The Covid-19 pandemic has been a deadly pandemic that has affected the whole world. It was a viral infection that affected almost everyone in some way or the other. However, the effects have been felt differently depending on various factors. As it is a virus, it will change with time, and different variants might keep coming. The virus has affected the lifestyle of human beings. The pandemic has affected the education system and the economy of the world as well. Many people have lost their lives, jobs, near and dear, etc.
Table of Contents
Paragraph writing on covid-19 in 100 words, paragraph writing on covid-19 in 150 words, paragraph writing on covid-19 in 200 words, paragraph writing on covid-19 in 250 words, frequently asked questions on covid-19.
Check the samples provided below before you write a paragraph on Covid-19.
Coronavirus is an infectious disease and is commonly called Covid-19. It affects the human respiratory system causing difficulty in breathing. It is a contagious disease and has been spreading across the world like wildfire. The virus was first identified in 2019 in Wuhan, China. In March, WHO declared Covid-19 as a pandemic that has been affecting the world. The virus was spreading from an infected person through coughing, sneezing, etc. Therefore, the affected people were isolated from everyone. The affected people were even isolated from their own family members and their dear ones. Other symptoms noticed in Covid – 19 patients include weariness, sore throat, muscle soreness, and loss of taste and smell.
Coronavirus, often known as Covid-19, is an infectious disease. It affects the human respiratory system, making breathing difficult. It’s a contagious disease that has been spreading like wildfire over the world. The virus was initially discovered in Wuhan, China, in 2019. Covid-19 was declared a global pandemic by the World Health Organization in March. The virus was transferred by coughing, sneezing, and other means from an infected person. As a result, the people who were affected were isolated from the rest of society. The folks who were afflicted were even separated from their own family members and loved ones. Weariness, sore throat, muscle stiffness, and loss of taste and smell are among the other complaints reported by Covid-19 individuals. Almost every individual has been affected by the virus. A lot of people have lost their lives due to the severity of the infections. The dropping of oxygen levels and the unavailability of oxygen cylinders were the primary concerns during the pandemic.
The Covid-19 pandemic was caused due to a man-made virus called coronavirus. It is an infectious disease that has affected millions of people’s lives. The pandemic has affected the entire world differently. It was initially diagnosed in 2019 in Wuhan, China but later, in March 2020, WHO declared that it was a pandemic that was affecting the whole world like wildfire. Covid-19 is a contagious disease. Since it is a viral disease, the virus spreads rapidly in various forms. The main symptoms of this disease were loss of smell and taste, loss of energy, pale skin, sneezing, coughing, reduction of oxygen level, etc. Therefore, all the affected people were asked to isolate themselves from the unaffected ones. The affected people were isolated from their family members in a separate room. The government has taken significant steps to ensure the safety of the people. The frontline workers were like superheroes who worked selflessly for the safety of the people. A lot of doctors had to stay away from their families and their babies for the safety of their patients and their close ones. The government has taken significant steps, and various protocols were imposed for the safety of the people. The government imposed a lockdown and shut down throughout the country.
The coronavirus was responsible for the Covid-19 pandemic. It is an infectious disease that has affected millions of people’s lives. The pandemic has impacted people all across the world in diverse ways. It was first discovered in Wuhan, China, in 2019. However, the World Health Organization (WHO) proclaimed it a pandemic in March 2020, claiming that it has spread throughout the globe like wildfire. The pandemic has claimed the lives of millions of people. The virus had negative consequences for those who were infected, including the development of a variety of chronic disorders. The main symptoms of this disease were loss of smell and taste, fatigue, pale skin, sneezing, coughing, oxygen deficiency, etc. Because Covid-19 was an infectious disease, all those who were infected were instructed to segregate themselves from those who were not. The folks who were affected were separated from their families and locked in a room. The government has prioritised people’s safety. The frontline personnel were like superheroes, working tirelessly to ensure the public’s safety. For the sake of their patients’ and close relatives’ safety, many doctors had to stay away from their families and babies. The government had also taken significant steps and implemented different protocols for the protection of people.
What is meant by the Covid-19 pandemic?
The Covid-19 pandemic was a deadly pandemic that affected the lives of millions of people. A lot of people lost their lives, and some people lost their jobs and lost their entire families due to the pandemic. Many covid warriors, like doctors, nurses, frontline workers, etc., lost their lives due to the pandemic.
From where did the Covid-19 pandemic start?
The Covid-19 pandemic was initially found in Wuhan, China and later in the whole world.
What are the symptoms of Covid-19?
The symptoms of Covid-19 have been identified as sore throat, loss of smell and taste, cough, sneezing, reduction of oxygen level, etc.
| ENGLISH Related Links | |
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Request OTP on Voice Call
Post My Comment
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.
COVID's Hidden Toll: Full-Body Scans Reveal Long-Term Immune Effects
Long COVID is a brutal illness without a known mechanism or cure. Far from being psychosomatic in nature , a new study adds weight to the idea that this misunderstood disease is very much biological.
The lingering toll the SARS-CoV-2 virus exacts on the immune system is widespread and hiding in plain sight, argue researchers at the University of California, San Francisco, CellSight Technologies, and Kaiser Permanente South San Francisco Medical Center.
When 24 patients who had recovered from COVID-19 had their whole bodies scanned by a PET ( positron emission tomography ) imaging test, their insides lit up like Christmas trees.
A radioactive drug called a tracer revealed abnormal T cell activity in the brain stem, spinal cord, bone marrow, nose, throat, some lymph nodes, heart and lung tissue, and the wall of the gut, compared to whole-body scans from before the pandemic.
This widespread effect was apparent in the 18 participants with long COVID symptoms and the six participants who had fully recovered from the acute phase of COVID-19.
The activation of immune T cells in some tissues, like the spinal cord and the gut wall, was higher in patients who reported long COVID symptoms compared to those who made a complete recovery. Participants with ongoing respiratory issues also showed increased uptake of the PET tracer in their lungs and pulmonary artery walls.
That said, even those who recovered fully from COVID-19 still showed persistent changes to their T cell activity in numerous organs compared to pre- pandemic controls, in some cases two and a half years after they first contracted the virus .
"In some individuals, this activity may persist for years following initial COVID-19 onset and be associated with systemic changes in immune activation as well as the presence of [long COVID] symptoms," researchers at UCSF conclude .
"Together, these observations suggest that even clinically mild infection could have long-term consequences on tissue-based immune homeostasis and potentially result in an active viral reservoir in deeper tissues."
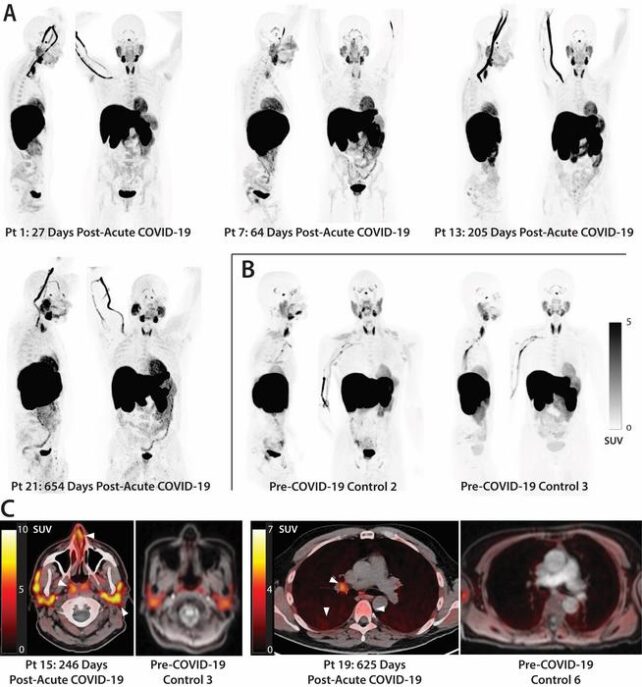
The findings are only correlative, but they provide compelling evidence that long COVID is tied to the persistence of the SARS-CoV-2 virus in the body and abnormal immune activity. It's worth noting that all but one participant in the study had received at least one COVID-19 vaccination prior to the PET imaging.
Long COVID is currently defined by a host of unexplained symptoms that appear after a SARS-Cov-2 infection, lasting months, or even years, with no other known cause.
Diagnosis is extremely tricky, as there can be more than 200 symptoms , which often overlap with other illnesses, such as 'brain fog', post-exertional malaise, fatigue, memory loss, or diarrhea.
Studies show that 'long haulers' can suffer from lingering issues in their heart , brain , lungs , skin , kidneys , liver , spleen , gut , thyroid , and ovaries .
One explanation for this widespread effect involves activity of the immune system. S cientists have found biomarkers of inflammation and immune activation are often present in a patient's blood after the acute phase of a viral infection.
COVID autopsies also show evidence of the SARS-CoV-2 virus persisting throughout the body, including in the colon, the thorax, muscles, nerves, the reproductive tract, and the eye. In some cases, remnants of the virus showed up in the brain of a deceased patient 230 days after their first initial symptoms.
Some studies even suggest an infection of the SARS-CoV-2 virus can 'reawaken' other dormant viruses in the body, like the Epstein barr virus, which has been linked to chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME).
CFS/ME shares many of the same symptoms as long COVID, and some scientists suspect they may be one and the same. Brain scans have found that long COVID changes to the brain parallel the effects of CFS/ME, and re cently, a landmark study confirmed that CFS/ME is " unambiguously biological " with multiple organ systems affected.
Today, long COVID is increasingly recognized as having neurological underpinnings, and the recent discovery of T cell abnormalities in the spinal cord and brain stem suggest that these overactive immune cells are being 'trafficked' to tissues of the central nervous system.
"Overall, these observations challenge the paradigm that COVID-19 is a transient acute infection, building on recent observations in blood," the team from UCSF concludes .
The findings need to be confirmed among larger cohorts, now that this new technique for mapping the immune effects of long COVID in the body shows such great promise.
The study was published in Science Translational Medicine .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 08 July 2024
Complex patterns of multimorbidity associated with severe COVID-19 and long COVID
- Maik Pietzner ORCID: orcid.org/0000-0003-3437-9963 1 , 2 , 3 ,
- Spiros Denaxas 4 , 5 , 6 , 7 ,
- Summaira Yasmeen 1 ,
- Maria A. Ulmer ORCID: orcid.org/0000-0002-9326-7227 8 ,
- Tomoko Nakanishi ORCID: orcid.org/0000-0001-9510-5646 2 ,
- Matthias Arnold ORCID: orcid.org/0000-0002-4666-0923 8 , 9 ,
- Gabi Kastenmüller ORCID: orcid.org/0000-0002-2368-7322 8 ,
- Harry Hemingway ORCID: orcid.org/0000-0003-2279-0624 4 , 5 , 7 na1 &
- Claudia Langenberg ORCID: orcid.org/0000-0002-5017-7344 1 , 2 , 3 na1
Communications Medicine volume 4 , Article number: 94 ( 2024 ) Cite this article
7 Altmetric
Metrics details
- Epidemiology
- Infectious diseases
Early evidence that patients with (multiple) pre-existing diseases are at highest risk for severe COVID-19 has been instrumental in the pandemic to allocate critical care resources and later vaccination schemes. However, systematic studies exploring the breadth of medical diagnoses are scarce but may help to understand severe COVID-19 among patients at supposedly low risk.
We systematically harmonized >12 million primary care and hospitalisation health records from ~500,000 UK Biobank participants into 1448 collated disease terms to systematically identify diseases predisposing to severe COVID-19 (requiring hospitalisation or death) and its post-acute sequalae, Long COVID.
Here we identify 679 diseases associated with an increased risk for severe COVID-19 ( n = 672) and/or Long COVID ( n = 72) that span almost all clinical specialties and are strongly enriched in clusters of cardio-respiratory and endocrine-renal diseases. For 57 diseases, we establish consistent evidence to predispose to severe COVID-19 based on survival and genetic susceptibility analyses. This includes a possible role of symptoms of malaise and fatigue as a so far largely overlooked risk factor for severe COVID-19. We finally observe partially opposing risk estimates at known risk loci for severe COVID-19 for etiologically related diseases, such as post-inflammatory pulmonary fibrosis or rheumatoid arthritis, possibly indicating a segregation of disease mechanisms.
Conclusions
Our results provide a unique reference that demonstrates how 1) complex co-occurrence of multiple – including non-fatal – conditions predispose to increased COVID-19 severity and 2) how incorporating the whole breadth of medical diagnosis can guide the interpretation of genetic risk loci.
Plain Language Summary
Early in the COVID-19 pandemic it was clear that people with multiple chronic diseases were vulnerable and needed special protection, such as shielding. However, many people without such diseases required hospital care or died from COVID-19. Here, we investigated the importance of underlying diseases, including mild diseases not requiring hospitalization, for COVID-19 outcomes. Using information from electronic health records we find that many severe, but also less severe diseases increase the risk for severe COVID-19 and its impact on health even months after acute infection (Long COVID). This included an almost two-fold higher risk among people that reported poor well-being and fatigue. Our findings show the value of using primary care health records and the need to consider all the medical history of patients to identify those in need of special protection.
Similar content being viewed by others

Short- and long-term neuropsychiatric outcomes in long COVID in South Korea and Japan

Long COVID: major findings, mechanisms and recommendations
Principal component-based clinical aging clocks identify signatures of healthy aging and targets for clinical intervention
Introduction.
From the outset of the COVID-19 pandemic it was evident that underlying conditions were associated with both the risk of infection with SARS-CoV-2, the cause of COVID-19, and the risk of it being severe, based on the risk of hospitalisation, to ventilation and death 1 . Initial focus was on the small number of diseases known to put people at higher risk of other respiratory viral infections, such as influenza. The Center for Disease Control in the US and other national bodies published lists of diseases associated with COVID-19 and in the UK more than 1 million people were identified as clinically extremely vulnerable and required ‘shielding’ based on having one or more specified diseases 2 . This included older individuals, men, and those with the presence of multiple, pre-exiting long-term conditions, such as impaired immunity, type 2 diabetes, hypertension, or chronic kidney disease (CKD) 1 .
However, the vast body of COVID-19 risk factor studies were based on a candidate approach (e.g., diseases known to be associated with immune compromise), studying common diseases in limited numbers (usually fewer than 100 diseases) 3 , 4 , 5 , 6 . Studies that systematically investigated diseases across clinical specialties, including those primarily managed and treated in primary care, are largely lacking, but are needed to understand why some patients with COVID-19 suffer from a severe outcome or dead, albeit at supposedly low-risk. Such a systematic, ‘diseasome’-wide study can further improve our understanding of how variation in the host genome 7 , 8 confers risk for severe COVID-19 and guide drug target prioritisation strategies.
Here, we collate millions of health records from primary care, hospitalisations and cancer registrations, and death records among ~500,000 participants of the UK Biobank (UKB) into medical diagnosis concept terms 9 , so-called ‘phecodes’ 10 , to systematically assess the risk for severe COVID-19 and its post-acute sequalae, Long COVID, across the breadth of medical diagnosis. Apart from well-recognized high-risk patient groups, such as those with chronic kidney disease or those with compromised immune function, we demonstrate consistent evidence for the possible role of less recognized diseases and symptoms, including malaise and fatigue, based on survival and genetic susceptibility analyses. We finally observe that some genomic regions conferring a higher risk for severe COVID-19 might be protective for diseases that partially share pathomechanisms with COVID-19, or vice versa, with possible implications for drug development programs, such as TYK2-inhibitors that may increase the risk for severe COVID-19.
Study population
UKB is a prospective cohort study from the UK, which contains more than 500,000 volunteers between 40 and 69 years of age at inclusion. The study design, sample characteristics and genome-wide genotype data have been described in Sudlow et al. 9 and Bycroft et al. 11 . The UKB was approved by the National Research Ethics Service Committee Northwest Multi-Centre Haydock and all study procedures were performed in accordance with the World Medical Association Declaration of Helsinki ethical principles for medical research. All participants gave broad consent to use of their anonymised data and samples for any health-related research and for UKB to access their health-related records. UKB is registered as a Research Tissue Bank ( https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/research-tissue-banks-and-research-databases/ ) and hence all approved data applications (here ID: 44448) can use this ethical clearance to conduct their research. We included 502,460 individuals who had not withdrawn their consent. For survival analysis we considered a set of 438,917 individuals who were still alive at the beginning of the COVID-19 pandemic (01/01/2020) and had genetically inferred ancestry also beyond white Europeans. We chose the entire set of white Europeans ( n = 441,671) that passed standard quality control for genetic analysis to maximise statistical power.
COVID-19 and Long COVID outcome definitions
We defined a total of four different COVID-19 related outcomes closely aligned with previous studies 8 , 12 , 13 . We used hospital episode statistics to identify participants who had been ‘hospitalised’ with COVID-19 based on ICD-10 codes U07.1 and U07.2, and the same ICD-10 codes to identify participants who have died from/with COVID-19 based on death registries. We did not require a positive PCR COVID-19 test due to differences in local reporting of test results. We adopted a slightly more sophisticated definition for ‘severe respiratory failure’, demanding a positive COVID-19 test (based on test results released for England, Scotland, and Wales provided by UKB through the COVID-19 Second Generation Surveillance System) within a month of acute respiratory failure, defined by ICD-10 codes J80, J96.00, J96.09, Z99.1 from hospital episode statistics or E85.1 and E85.2 when admitted to the intensive care unit. To define ‘Long COVID’ we used primary care data released by UKB (covid19_emis_gp_clinical.txt, covid19_tpp_gp_clinical.txt) searching for codes indicating suspected diagnosis [CTV3: Y2b89 – “Referral to post-COVID assessment clinic”, Y2b8a – “Referral to Your COVID Recovery rehabilitation platform”, Y2b87 – “Post-COVID-19 syndrome”, and Y2b88 – “Signposting to Your COVID Recovery”; SNOMED-CT: 1325161000000102 – “Post-COVID-19 syndrome”, 1325031000000108 – “Referral to post-COVID assessment clinic”, 1325041000000104 – “Newcastle post-COVID syndrome Follow-up Screening Questionnaire”, 1325181000000106 – “Referral to Your COVID Recovery rehabilitation platform”, 1325021000000106 – “Ongoing symptomatic disease caused by severe acute respiratory syndrome coronavirus 2”, 1325141000000103 – “Signposting to Your COVID Recovery”, 1325081000000107 – “Assessment using Post-COVID-19 Functional Status Scale structured interview”, 1325061000000103 – “Assessment using COVID-19 Yorkshire Rehabilitation Screening tool”, 1325071000000105 – “Assessment using Newcastle post-COVID syndrome Follow-up Screening Questionnaire”, 1325051000000101 – “COVID-19 Yorkshire Rehabilitation Screening tool”]. For each event, we took the earliest record to define disease onset.
We identified a total of 7507 (hospitalisation), 662 (respiratory failure), and 1546 cases (death), with first cases occurring end of January 2020. Due to restricted availability of primary care data, we only included records up until 30/09/2021 to identify 470 cases of Long COVID.
Disease ascertainment
We collated electronic health records (EHRs) from primary and secondary care, cancer registries, and death certificates based on tables provided by UKB (gp_clinical.txt, covid19_emis_gp_clinical.txt, covid19_tpp_gp_clinical.txt, hesin_diag.txt, death.txt) downloaded in June 2022. We parsed all records to exclude codes with a recorded date before or within the year of birth of the participant to minimize coding errors from EHRs. We used mappings provided by UK Biobank to include self-reported conditions based on ICD-10 codes. For each data set separately, we generated mapping tables that link ICD-10, ICD-9, Read version 2, Clinical Terms Version 3 (CTV3) terms, or SNOMED-CT codes to a set of 1560 summarized clinical entities called phecodes 14 , 15 (Supplementary Data 1 ). For example, more than 90 ICD-10 codes can indicate participants with type 1 diabetes that are here collectively summarized under the phecode ‘type 1 diabetes’ 16 . We subsequently fused all data sources based on a common set of phecodes and retained for each participant and each phecode only the earliest entry across all EHR resources. We identified a total of 1448 phecodes with at least 100 cases in the overall UKB sample. For each participant and phecode, we kept only the earliest date as an indicator for disease onset and defined all events occurring before 01/01/2020 as prevalent, while we considered any event for genetic analysis. To increase the accessibility of our results, we use the term ‘disease’ instead of ‘phecode’ throughout the paper.
Survival analysis
We used Cox-proportional hazard models to estimate the risk associated with each disease and any of the four COVID-19 related outcomes with age as the underlying scale, adjusting for sex (omitted for sex-specific diseases) and genetically inferred ancestry. For each COVID-19 outcome, we defined controls separately as all those participants without a corresponding record during the time course of the study. We repeated Cox-proportional hazard models considering all-cause death as a competing event rather than censoring as a sensitivity analysis. We selected 01/03/2020 as the starting point of our study and used 31/12/2022 (COVID-19 endpoints) or 30/09/2021 (Long COVID) as endpoints of the observation period depending on the availability of health record linkage. We computed Schoenfeld residuals to test for the proportional hazard assumption, and further computed time varying effects of diseases by introducing 6 months breaks. For each disease – COVID-19 model, we considered all participants that passed inclusion criteria. We applied stringent multiple testing correction ( p < 0.05/4*1448 = 4.8 × 10 −8 ) and further filtered results for those possibly violating the proportional hazard assumption ( p < 10 −3 ). To establish endpoint-specific associations, we performed meta-analysis across disease associations for all three COVID-19 endpoints derived using the R package metafor (v.3.8.1) . We performed additional sensitivity analysis using an extended set of confounders similar to previous work 17 , including self-reported smoking status and alcohol consumption, body mass index, and Townsend deprivation index (all based on baseline values), healthcare utilization in the five years before the pandemic (number of stays and total days in hospital), as well as a variable indicating participants with two or more long-term conditions.
We tested for a potential modifying effect of sex, non-European ancestry, age ( ≤ 65 years vs > 65 years), and social deprivation (Townsend index above median vs below median; median = −2.22) on the results by systematically performing interaction testing, i.e., introducing a disease – sex/non-European ancestry interaction term into Cox-models. For the latter, we requested to have at least 50 observations in each group to ensure model convergence. We subsequently corrected for a total of 13,728 tests ( p < 3.6 × 10 −6 ). All statistical analysis were implemented using R v4.1.2.
Disease network
We computed a sex-aware disease network using partial correlations as implemented in the R package ppcor (v.2.1.1) following previous work 18 . Briefly, partial correlations (r P ) account for the fact, that a correlation, or co-occurrence, between two diseases might be driven by a third or any other disease considered. We retained only partial correlations passing stringent multiple testing ( p < 4.9 × 10 −8 ) and r P > 0.02 as we reasoned that a disease-disease network likely exhibits scale-free properties 19 with node degrees following a power law. The latter step omitted many significant, but very weak and potentially artificial edges. The final network contained 5212 edges connecting 1381 diseases. We then performed community detection based on the Girvan-Newman algorithm to identify groups of diseases that were more closely connected with each other compared to all other diseases in the network. We finally computed different node characteristics to identify diseases with important roles in the network. We implemented and visualized this analysis with the R package igraph (v.1.3.1).
Genotyping, quality control, and participant selection
Details on genotyping for UKB have been reported in detail by Bycroft et al. 11 . Briefly, we used data from the ‘v3’ release of UKB containing the full set of Haplotype Reference Consortium (HRC) and 1000 Genomes imputed variants. We applied recommended sample exclusions by UKB including low quality control values, sex mismatch, and heterozygosity outliers. We defined a subset of ‘white European’ ancestry by clustering participants based on the first four genetic principal components derived from the genotyped data using a k-means clustering approach with k = 5. We classified all participants who belonged to the largest cluster and self-identified as of being ‘white,’ ‘British’, ‘Any other white background’, or ‘Irish’ as ‘white European’. After application of quality control criteria and dropping participants who have withdrawn their consent, a total of 441,671 UKB participants were available for analysis with genotype and phenotype data.
We used only called or imputed genotypes and short insertions/deletions (here commonly referred to as single nucleotide polymorphisms (SNPs) for simplicity) with a minor allele frequency (MAF) > 0.001%, imputation score > 0.4 for common (MAF ≥ 0.5%) and > 0.9 for rare (MAF < 0.5%), within Hardy-Weinberg equilibrium (p HWE > 10 −15 ), and minor allele count (MAC) > 10. This left us with 15,519,342 autosomal and X-chromosomal variants for statistical analysis. GRCh37 was used as reference genome assembly.
Genome-wide association studies
We performed genome-wide association studies (GWAS) for a total of 1445 diseases with at least 80 cases ( n > 100 prior genetic exclusions; 3 diseases dropped out) using REGENIE v2.2.4 via a two-step procedure to account for population structure as described in detail elsewhere 20 . We used a set of high-quality genotyped variants (MAF > 1%, MAC > 100, missingness < 10%, p HWE > 10 −15 ) in the first step for individual trait predictions using the leave one chromosome out (LOCO) scheme. These predictions were used in the second step as offset to run logistic regression models with saddle point approximation to account for case/control imbalance and rare variant associations. Each model was adjusted for age, sex, genotyping batch, assessment centre, and the first ten genetic principal components. For diseases reported in only one sex ( n = 113 in women, n = 26 in men), we excluded the respective sex from GWAS to avoid inflation by inappropriate controls. In general, we included all participant with a disease in their records as case and treated all other participants as controls to make best use of the computational efficacy of REGENIE. Testing for reported SNPs showed highly consistent results whether related diseases were included as controls rather than omitted. We used LD-score regression to test for genomic inflation (LDSC v1.0.1) 21 .
COVID-19 genetic correlation and Mendelian randomization
We downloaded GWAS summary statistics for two different endpoints related to COVID-19 (A2 – critical illness; B2 – hospitalisation) and Long COVID (stringent case definition vs broad control set) provided by the COVID-19 Host Genetics Initiative (release 7) 8 , 13 . We used summary statistics excluding UKB to avoid sample overlap. We computed genetic correlations as implemented by LD-score regression (LDSC v1.0.1) 21 with precomputed LD-scores, excluding the extended MHC region. To test for potentially causal associations of diseases onto COVID-19, we used genetic instruments identified in the present study for a total of 41 diseases with at least five genetic variants and evidence for significant genetic correlations in a two-sample MR setting. We used MR-PRESSO 22 as a first line tool as previously suggested 23 to account for possible pleiotropy and subsequently report effect estimates from inverse-variance weighted analysis as the primary results. We flagged MR results that showed signs of heterogeneity across instruments using Cochran Q statistic. We excluded any variants mapping to the MHC regions for all analysis and implemented MR using the R packages MendelianRandomization (v0.6.0) 24 and TwoSampleMR (v0.5.6) 25 .
Colocalisation at COVID-19 risk loci
We collected association statistics for a total of 49 independent risk loci for COVID-19 (selected based on regional clumping ( ± 500 kb) of COVID-19 HGI GWAS statistics excluding UKB participants, but SNPs available among imputed genetic data in UKB) across all 1445 diseases included in the genetic analysis. For variant – disease pairings passing a moderate significance threshold ( p < 10 −6 ), we implemented statistical colocalization 26 accounting for multiple causal genetic variants via fine-mapping 27 using the R packages coloc (v.5.3.2) and susieR (v.0.11.92). We allowed for a maximum of five causal variants during fine-mapping of the disease and linked COVID-19 outcome (via a potentially shared genetic variant) and subsequently tested each credible set for colocalization. We applied a stringent prior to consider a shared signal (p 12 = 5 × 10 −6 ) and further filtered signals with evidence that the lead signal (r 2 with best remaining signal > 0.8) for COVID-19 was dropped from the set of overlapping genetic variants between our UKB GWAS and the COVID-19 GWAS.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Here, we systematically investigate the risk conferred by the presence and potential causal relevance of 1448 diseases for COVID-19 severity (hospitalisation, severe respiratory failure, and death) and Long COVID (Fig. 1 ), based on medical disorder concepts 14 , 16 defined and collated from > 12 million medical records from primary (general practice), secondary care (hospital admissions), and disease registry (cancer registry), death certificates, and patient-reported conditions among 502,460 UKB participants (Fig. 1 and Supplementary Data 1 ). Incorporating primary care data more than doubled case numbers for more than half ( n = 817; 56.4%) of the diseases we considered (Supplementary Data 1 ).

Scheme of the study design and analysis done, illustrating our workflow to define disease mechanisms that may causally contribute to severe COVID-19 or Long COVID. SNPs Single nucleotide polymorphisms; SPA = saddle point approximation; MAF = minor allele frequency; *COVID-19 HGI = COVID-19 Host Genetic Initiative, but excluding contributions from UK Biobank
Disease risk profiles for COVID-19 and Long COVID
We identified 1128 significant ( p < 1.1 × 10 − 5 ) disease – COVID-19 outcome associations, including almost half ( n = 679) of the diseases considered with at least one of the four COVID-19 outcomes derived (Fig. 2 and Supplementary Data 2 ). Pre-existing diseases were almost exclusively associated with a higher risk for COVID-19 endpoints (median hazard ratio (HR): 2.39, range: 0.59–17.3), only two diseases (benign neoplasm of skin and varicella infection) were associated with a decreased risk. Associated diseases spanned almost all chapters of the ICD-10 (17 out of 18) but were consistently enriched in the chapters ‘respiratory’ (odds ratio [OR]: 5.96; p -value: 2.7 x 10 − 8 ), ‘circulatory’ (OR: 2.95; p -value: 3.5 x 10 − 7 ), and ‘endocrine/metabolic’ diseases (OR: 2.76; p -value: 9.1 × 10 − 4 ) when associated with severe COVID-19. In contrast, pre-existing disease-codes classified as ‘symptoms’ were more than 13-fold enriched among diseases associated with an increased risk for Long COVID (OR: 13.2; p -value: 3.6 x 10 −8 ) but also hospitalisation (OR: 5.53; p -value: 9.9 x 10 −5 ) and death (OR: 3.06; p -value: 7.3 x 10 −3 ).

Each panel contains association statistics, p -values (triangles), from Cox-proportional hazard models (two-sided) testing for an association between the disease on the x-axis and three different COVID-19 outcomes, as well as Long COVID. Disease associations passing the multiple testing correction (dotted line, p < 1.1 × 10 −5 ) are depicted by larger triangles of which facing up ones indicate positive, e.g., increased disease risk, associations and downward facing vice versa . The diseases are ordered by ICD-10 chapters (colours) and the top ten for each endpoint annotated. Underlying sample numbers and statistics can be found in Supplementary Data 1 and 2 .
For COVID-19 requiring hospitalisation, we replicated and refined known associations with serious pre-existing diseases that have been previously used to identify clinically extremely vulnerable people. This included respiratory diseases like pseudomonal pneumonia (HR: 7.53, 95%-CI: 4.74–11.97; p -value < 1.2 x 10 −17 ), acute renal failure (HR: 4.02, 95%-CI: 3.74–4.32, p -value: <10 −300 ) or type 2 diabetes with renal complications (HR: 7.44; 95%-CI: 5.67–9.76; p -value: 1.5 x 10 −47 ), as well as immune deficiencies (e.g., deficiency of humoral immunity HR: 6.02; 95%-CI: 4.36–8.31; p -value: 1.3 x 10 −27 ) or patients under immune suppression (e.g., liver transplants HR: 7.25 95%-CI: 4.51–11.68, p -value: 3.4 x 10 −16 ). However, we further observed strong associations with so far less recognized pre-existing mental health and psychiatric diseases and conditions with effect sizes comparable to those previously considered to identify extremely vulnerable people. This included symptoms of malaise and fatigue (HR: 2.17, 95%-CI: 2.07–2.27, p -value: 4.4 x 10 −222 ) or suicide attempts (HR 5.33, 95%-CI: 4.45–6.39, p -value: 3.6 x 10 −73 ). Most diseases ( n = 641, 95.5%, p hetero > 10 −3 ) associated with similar magnitude across all three different definitions of COVID-19 severity, with different forms of dementias (p hetero < 2.1 x 10 −24 ) being among the few exceptions, associating with hospitalisation (HR: 3.83; 95%-CI: 3.38–4.34; p -value: 2.3 x 10 −97 ) and death (HR: 10.82; 95%-CI: 9.15–12.80; p -value: 1.4 x 10 −170 ), but not severe respiratory failure (HR: 1.15; 95%-CI: 0.51–2.57; p -value: 0.74) due to COVID-19.
In contrast, pre-existing diseases associated with an increased risk for Long COVID only partially overlapped with those increasing the risk for severe COVID-19. Most notably, we replicated associations with anxiety disorders 28 (HR: 2.59; 95%-CI: 2.09–3.20; p -value:1.8 x 10 −18 ) and other mental health symptoms, but most prominently with symptoms of malaise and fatigue (HR: 2.78; 95%-CI: 2.29–3.37; p -value:1.5 x 10 −25 ) that are hallmarks of Long COVID and were also strongly associated with severe COVID-19.
Almost all significant associations (99.8%, n = 1126) were consistent when considering all-cause death as a competing event (Supplementary Data 3 ), and more than half (63.6%; n = 718) remained statistically significant ( p < 4.4 x 10 −5 ) when accounting for a large set of potential confounders in multivariable Cox-models (Supplementary Data 3 ). This suggests that potentially unreported associations, such as the increased risk for severe COVID-19 among patients reporting symptoms of malaise and fatigue (adjusted HR: 1.66, 95%-CI: 1.58 - 1.74, p -value = 7.3 x 10 −92 ), are not just a reflection of a general disease burden or other chronic diseases associated with a greater risk for severe COVID-19.
We observed limited evidence for effect modifications by sex ( n = 7), non-European ancestry ( n = 1), or age ( n = 8), but not social deprivation, with 16 disease – COVID 19 pairings showing evidence of significant differences (Supplementary Data 4 ; p < 3.6x10 −6 ). All included stronger effects in women compared to men, e.g., gout for hospitalised COVID-19 (women: HR: 2.56, 95%-CI 2.21–2.96, p -value: 1.3x10 −36 ; men: HR: 1.46, 95%-CI: 1.34–1.58, p -value: 2.1 x 10 −19 ), among Europeans reporting vitamin D deficiencies (Europeans: HR: 2.31, 95%-CI: 2.13–2.51, p -value: 2.1 x 10 −87 ; non-Europeans: HR: 1.31, 95%-CI: 1.08–1.60, p -value = 5.5 x 10 −3 ), or among younger participants, e.g., disorders of magnesium metabolism and death with COVID-19 as a likely result of renal failure (age ≤ 65 years: HR: 42.98, 95%-CI: 20.10–91.90, p -value: 3.0 x 10 −22 ; age > 65 years: HR: 5.35, 95%-CI: 3.51–8.16, p -value: 5.9 x 10 −15 ).
Complex patterns of multimorbidity are associated with increased risk
We next derived a disease-disease network 18 (Fig. 3a ) to understand, whether the large set of diseases associated with an increased risk for severe COVID-19 act independently or rather reflect an increased risk among participants suffering from multiple pre-existing conditions, i.e., multimorbidity. The network contained a total of 1381 diseases connected through 5212 edges based on non-random co-occurrence (Supplementary Data 5 a, b ). Diseases segregated into 31 ‘communities’ being more strongly connected to each other compared to the rest of the network (Fig. 3b, c ).

a Disease – disease network based on significant ( p < 4.8 x 10 −8 ) positive partial correlations (two-sided). Nodes (diseases) are coloured by ICD-10 chapters and strength of partial correlation depicted by width of the edges. The underlying data can be found in Supplementary Data 5 a –c Same network, but only highlighting two disease communities strongly enriched for associations with severe COVID-19. d Hub score for the 30 diseases with highest values and associated association statistics, hazard ratios (rectangle) with 95%-confidence intervals (lines), from Cox-proportional hazard models (two-sided). Significant associations are indicated by filled boxes. Colours according to ICD-10 chapters. All underlying data can be found in Supplementary Data 2 and 5 b .
Two disease communities were consistently and strongly enriched for diseases associated with severe COVID-19. The first (e.g., OR: 5.20; p -value = 2.2 x 10 −10 ; for severe respiratory failure) community was strongly enriched for circulatory (OR: 17.6; p -value: 4.4 x 10 −39 ) and respiratory (OR: 10.3; p -value: 7.8 x 10 −16 ) diseases, closely resembling the cardio-respiratory risk profile already described above (Fig. 3b ). The second community consisted of diverse endocrine (OR: 6.19; p -value: 1.9 x 10 −13 ) and circulatory disease (OR: 3.75; p -value: 5.4 x 10 −8 ), and largely reflected the renal-diabetic risk profile (Fig. 3c ). Accordingly, for each disease acquired during lifetime within the latter disease community, participants’ risk increased by 18% and 20% to be hospitalised (HR: 1.18; 95%-CI: 1.17–1.18; p -value: p < 10 −300 ) or die with COVID-19 (HR: 1.20; 1.19–1.20; p -value < 10 −300 ), respectively.
Diseases increasing the risk for severe COVID-19, but not Long COVID further significantly correlated with hub status (e.g., hospitalisation: r = 0.59; p -value: 2.8 x 10 −124 ) in the disease-disease network (Fig. 3d ), that is, diseases that connect a large cluster of diseases to the rest of the network and might hence be considered as multimorbidity hotspots. For example, acute renal failure, strongly associated with severe COVID-19 (Fig. 3d ), showed strong partial correlations with 30 other diseases and patients are hence prone to complex multimorbidity. However, the imperfect correlation between hub status and disease-association profiles indicates that certain forms of multimorbidity, such those related to secondary malignancies of lymph nodes, are possibly less related to severe COVID-19.
Convergence of associated disease risk and genetic liability
We next systematically characterised whether diseases identified to be associated with COVID-19 severity or Long COVID shared genetic similarity with host genetic susceptibility to severe COVID-19 to understand potential underlying causal mechanisms. We computed genetic correlation estimates for all 1128 disease – COVID-19 outcome pairs and observed 75 pairs (6.6%) that showed evidence for significant ( p < 4.4 x 10 −5 ) and directionally consistent genetic correlations (Fig. 4 and Supplementary Data 6 ), indicating a putatively causal link of any of 57 unique diseases on severe COVID-19. We did not observe evidence of convergence for Long COVID, which might likely be explained by the still low statistical power for the respective genome-wide association study 13 .

The first three panels show association statistics, hazard ratios (rectangle) and 95%-confidence interval (lines), for 57 diseases with evidence of convergence with genetic correlation analysis, that are shown in the last two panels (rectangle – genetic correlation; lines – 95%-confidence intervals). Disease have been grouped by ICD-10 chapters and coloured accordingly (see Figs. 2 or 3 for legend). NOS = not elsewhere specified; All underlying data can be found in Supplementary Data 1 (sample numbers), 2 and 6.
The diseases with consistent evidence from survival and genetic analysis included well-described risk-increasing effects of pre-existing endocrine (e.g., type 2 diabetes), respiratory (e.g., respiratory failure), or renal (e.g., chronic kidney disease) diseases, but also digestive (e.g., gastritis and duodenitis), or musculoskeletal (e.g., rheumatoid arthritis) diseases, and further symptoms of malaise and fatigue (r G = 0.26; p -value = 4.7 × 10 −6 ) and abdominal pain (r G = 0.33; p = 2.5 × 10 −11 ), as well as adverse reactions to drugs (e.g., poisoning by antibiotics: r G = 0.38; p -value = 2.2 x 10 −6 ). Findings that collectively demonstrated the need for a comprehensive assessment of disease-risk beyond few, selected common chronic conditions.
Among the 41 diseases for which we had sufficient genetic instruments to perform more stringent Mendelian randomization (MR) analyses to assess causality, we observed only nominally significant ( p < 0.05) evidence for gout and hospitalisation (OR: 1.03; 95%-CI: 1.01–1.05, p -value: 0.03), as well as arthropathy not elsewhere specified (OR: 1.28; 95%-CI: 1.06–1.55; p -value: 0.02) and unspecified monoarthrtitis (OR: 1.21; 95%-CI: 1.04–1.41; p -value: 0.02) for severe COVID-19 (Supplementary Data 7 ). While we might have been still underpowered for many diseases, this leaves the possibility that convergence of survival and genetic correlation analysis might, in part, be explained by shared risk factors.
Evidence for partially opposing roles of shared molecular mechanisms between severe COVID-19 and related disorders
To finally understand possible molecular mechanisms linking the ‘diseasome’ to COVID-19, we systematically profiled disease associations across 49 independent genomic regions linked to COVID-19 or Long COVID. We observed strong and robust evidence of a genetic signal shared between severe COVID-19 and a total of 33 diseases at nine loci (posterior probability (PP) > 80%) (Fig. 5a and Supplementary Data 8 ). Apart from known pleiotropic loci, such as ABO and FUT2 coding for blood group types, this included respiratory risk loci, albeit with contradicting effect estimates for three loci (Fig. 5b ). While COVID-19 risk increasing alleles at LZTFL1 and TRIM4 were consistently associated with a higher risk for viral pneumonia and post-inflammatory pulmonary fibrosis, respectively, risk-increasing alleles at MUC5B , NPNT , and PSMD3 were inversely associated with post-inflammatory pulmonary fibrosis and asthma. An observation that extended even beyond shared loci (Fig. 5c ) illustrating a general trend of phenotypic divergence of genetic effects on diseases that share pathological features with severe COVID-19.

a Network representation of significant (PP > 80%) colocalization results. Loci are depicted as white rectangles and diseases as coloured nodes according to ICD-10 chapters. Edges represent strong evidence for colocalization, and solid lines indicate a risk-increasing effect of the COVID-19 risk increasing allele, whereas dashed lines indicate protective effects. Underlying data can be found in Supplementary Data 8 . b Forest plot displaying hazard ratios (rectangle) with 95%-confidence intervals (lines) for each variant and different COVID-19 and colocalising disease outcomes. Effect estimates for COVID-19 have been obtained from the COVID-19 Host Genetic Initiative and effect estimates for diseases in the present study. All estimates are derived from logistic regression models. c Heatmap of effect estimates across 49 independent genetic loci associated with increased risk for sever COVID-19 and corresponding effects on six selected traits that showed evidence of colocalization at least one other locus. Black rectangles indicate genome-wide significant effects ( p < 5 × 10 −8 ). NOS not elsewhere specified; All underlying data can be found in Supplementary Data 1 and 8 or is given in the data availability statement.
A notable observation was the TYK2 locus that has previously been suggested to indicate the efficacy of successfully repurposed drugs for severe COVID-19 29 . Briefly, TYK2 encodes for tyrosine kinase 2 (TYK2) a protein partially targeted by Janus kinase (JAK) inhibitors like baricitinib, that have been approved for rheumatoid arthritis and successfully repurposed for severe COVID-19, although predating possible evidence from genetic studies 30 , 31 , 32 . Accordingly, we observed that the same genetic variant, rs34536443 (PP = 99.8%), associated with the risk for severe COVID-19 was also associated with, amongst others, the risk of rheumatoid arthritis, but in opposing effect directions (Fig. 5b ). Rs34536443 is a loss-of-function missense variant (p.Pro1104Ala) for TYK2 and the functionally impairing minor C allele was associated with a 50% increased risk for severe COVID-19 (odds ratio: 1.50; 95%-CI: 1.40– 1.62, p -value = 4.3 x 10 −29 ) but a 23% reduced risk for rheumatoid arthritis (odds ratio: 0.77; 95%-CI: 0.72–0.83; p -value = 2.4 x 10 −12 ) as well as other autoimmune diseases, in particular psoriasis (Supplementary Data 8 ). While the discrepancy between the success of the drug and genetic inference might be explained by the rather weak affinity of baricitinib for TYK2 33 , patients undergoing trials with TYK2-inhibitors for psoriasis 34 might be at an elevated risk for severe COVID-19. This observation seemingly aligns with studies on Tyk2 -/- mouse models reporting an impaired immune response to viral infections 35 .
An immediate understanding which patients are at greatest risk for severe COVID-19 and possibly death has proven to be instrumental to triage patients early in the pandemic to allocate critical care resources, such as ventilation or extracorporeal membrane oxygenation and, later, vaccination as well. The vast majority of studies 3 , 4 , 5 , 6 , however, focussed on a rather narrow set of common, usually chronic, conditions in the risk assessment leaving a considerable number of severe COVID-19 cases unexplained. We demonstrate here how capitalizing on the whole breadth of medical diagnoses through electronic health record linkage revealed 1) so far largely neglected patient populations at considerable risk, including those reporting symptoms of malaise and fatigue, and 2) that patients with multiple pre-existing conditions, in particular cardio-respiratory and endocrine-renal diseases, are probably at highest risk. Via integration of host genetics, we further provide evidence that a considerable set of diverse diseases may causally drive, or at least share causal drivers with, the risk for severe COVID-19, and exemplify how disease-wide characterisation of specific risk loci can inform disease mechanism and derivation of potentially druggable targets or adverse effects.
Among the diseases for which we observed consistent evidence from survival and genetic analysis to be linked to severe COVID-19 were multiple examples that have been rarely if at all reported. For example, we observed consistent evidence that symptoms of malaise and fatigue, as well as chronic fatigue, predispose to severe COVID-19. While the vast amount of literature currently discusses or reported these symptoms and disease as characteristics for COVID-19 and its post-acute sequelae 28 , 36 , little to nothing is known why patients reporting fatigue might be at higher risk. While our definition of ‘malaise and fatigue’ covered a broad range of partially unspecific medical codes with most cases (n = 83,316 out of 87,908, 92.4%) originating from primary care, we observed consistent evidence for the refined diagnosis of chronic fatigue classified as post-viral fatigue symptom (Supplementary Data 2 ). A hypothesis might be, that patients that are already suffering from post-viral symptoms are at a greater risk in general to suffer from more severe courses of viral infections through yet to be identified mechanisms, that may well comprise an altered immune response. However, the evidence we provide does not preclude the existence of general, currently inaccessible, risk factors that predispose to more severe long-term consequences of viral infections.
Our extensive genetic analysis revealed some partially contradicting findings that may point to a segregation of overall genetic susceptibility and risk conferred by specific loci and mechanisms, replicating and augmenting findings from a previous study in the Million Veterans Study 37 . For example, we observed consistent evidence that pre-existing post-inflammatory pulmonary fibrosis, likely representing cases of idiopathic pulmonary fibrosis, is a strong risk factor for severe COVID-19 and death, and genome-wide effects were highly correlated between both (r G =0.45, p = 2.3 x 10 −5 ), but effects at one of the strongest risk loci for post-inflammatory pulmonary fibrosis were protective for severe COVID-19. Our results thereby extend previous observations of misaligning effects at the MUC5B locus and idiopathic pulmonary fibrosis 38 , 39 . Results that might be explained by a latent, genome-wide risk component (as genome-wide significant loci do not contribute to genetic correlation analysis) that predisposes to severe lung fibrosis irrespective of the exact trigger, and specific molecular pathways characteristic for each disease that differ based on the required immune response to combat the infection. Cell-type and state-specific effects of shared genetic variants or possible design artefacts of GWAS studies of infectious disease, by which certain patient groups are ‘underrepresented’ due to tailored shielding efforts to minimize viral exposure, are other possible explanations. A similar paradoxical effect at the TYK2 locus highlights the unique potential of integrating electronic health care records with genetic data to guide drug target identification and risk estimation, including emerging diseases and targets in clinical trials.
There are a number of limitations that need to be taken in consideration when interpretating our results. Firstly, the COVID-19 pandemic was characterised by strong disruptions of social life and health care, with different waves of new SARS-CoV-2 variants of different pathogenicity, lockdowns, and implementation of vaccines programs, all of which will have influenced the general risk to develop severe COVID-19 for which we could not control for in survival analysis. However, we observed generally little evidence of violation of the proportional hazard assumptions and filtered associations with evidence for strong violations. Secondly, we cannot exclude the possibility that the multitude of diseases associated with severe COVID-19 might also be explained by shared, generic risk factors, such as obesity or smoking, and we implemented sensitivity analysis and comprehensive genetic analysis to mitigate possible confounding, although even larger genetic studies are needed to identify robust genetic signals for diseases like chronic fatigue and other rare diseases that we linked to COVID-19. Thirdly, while we obtained little evidence that disease-risk patterns differ across ancestries, the UK Biobank cohort is not a representative sample of the general population and does not sufficiently cover underrepresented populations, e.g., ethnic minorities, and additional work is needed to verify our observations in other populations. Lastly, while our effort to collate and harmonize electronic health records across various sources into medical concept terms covered almost 1500 diseases, it is still only an approximation of the complexity of medical diagnosis and more work, using electronic health records at a national scale, is needed to refine and augment the space of diseases to investigate.
Our results demonstrate the unique potential of integrating health records from primary and secondary care with host genetic data to 1) rapidly identify patients at highest risk beyond commonly assessed risk groups, 2) understand pathological pathways, and 3) inform druggable strategies for emerging health threats, such as COVID-19.
Data availability
Genome-wide summary statistics for diseases (‘phecodes’) in UK Biobank were generated, in part, from primary care data released to UK Biobank specifically for the use of COVID-19 research only, according to COPI regulations, and can therefore not be made publicly available. Access to individual level data can be requested by bona fide researchers from the UK Biobank ( https://www.ukbiobank.ac.uk/ ). This research has been conducted under the application 44448. Mapping of Read codes to phecodes can be downloaded from https://github.com/spiros/ukbiobank-read-to-phecode . We downloaded GWAS summary statistics for two different endpoints related to COVID-19 (A2 – critical illness; B2 – hospitalisation) and Long COVID (stringent case definition vs broad control set) provided by the COVID-19 Host Genetics Initiative (release 7) from https://www.covid19hg.org/ . Source data for the figures are available in Supplementary Data 1 - 8 .
Code availability
Associated code and scripts for the analysis can be found here https://github.com/comp-med/phecode-covid19-ukb 40 .
Merad, M., Blish, C. A., Sallusto, F. & Iwasaki, A. The immunology and immunopathology of COVID-19. Science 375 , 1122–1127 (2022).
Article CAS PubMed Google Scholar
Clinically extremely vulnerable receive updated guidance in line with new national restrictions. GOV.UK https://www.gov.uk/government/news/clinically-extremely-vulnerable-receive-updated-guidance-in-line-with-new-national-restrictions (2024).
Kompaniyets, L. et al. Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020-March 2021. Prev. Chronic Dis. 18 , E66 (2021).
Article PubMed PubMed Central Google Scholar
Booth, A. et al. Population risk factors for severe disease and mortality in COVID-19: A global systematic review and meta-analysis. PloS One 16 , e0247461 (2021).
Article CAS PubMed PubMed Central Google Scholar
Williamson, E. J. et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 584 , 430–436 (2020).
McKeigue, P. M. et al. Rapid Epidemiological Analysis of Comorbidities and Treatments as risk factors for COVID-19 in Scotland (REACT-SCOT): A population-based case-control study. PLoS Med. 17 , 1–17 (2020).
Article Google Scholar
Pairo-Castineira, E. et al. GWAS and meta-analysis identifies 49 genetic variants underlying critical COVID-19. Nature 617 , 764–768 (2023).
COVID-19 Host Genetics Initiative. A second update on mapping the human genetic architecture of COVID-19. Nature 621 , E7–E26 (2023).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12 , e1001779 (2015).
Wei, W.-Q. et al. Evaluating phecodes, clinical classification software, and ICD-9-CM codes for phenome-wide association studies in the electronic health record. PLoS One 12 , e0175508 (2017).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562 , 203–209 (2018).
Thygesen, J. H. et al. COVID-19 trajectories among 57 million adults in England: a cohort study using electronic health records. Lancet Digit. Health 4 , e542–e557 (2022).
Lammi, V. et al. Genome-wide Association Study of Long COVID Authors. 1–25 (2023).
Wu, P. et al. Mapping ICD-10 and ICD-10-CM Codes to Phecodes: Workflow Development and Initial Evaluation. JMIR Med. Inform. 7 , e14325 (2019).
Denaxas, S. Mapping the Read2/CTV3 controlled clinical terminologies to Phecodes in UK Biobank primary care electronic health records: implementation and evaluation. Proc Am. Med. Inform. Assoc. Annu. Symp. 2021 , 362–371 (2021).
Google Scholar
Bastarache, L. Using Phecodes for Research with the Electronic Health Record: From PheWAS to PheRS. Annu. Rev. Biomed. Data Sci. 4 , 1–19 (2021).
Zang, C. et al. Data-driven analysis to understand long COVID using electronic health records from the RECOVER initiative. Nat. Commun. 14 , 1948 (2023).
Kuan, V. et al. Identifying and visualising multimorbidity and comorbidity patterns in patients in the English National Health Service: a population-based study. Lancet Digit. Health 5 , e16–e27 (2023).
Barabasi, A. & Albert, R. Emergence of scaling in random networks. Science 286 , 509–512 (1999).
Mbatchou, J. et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 53 , 1097–1103 (2021).
Bulik-Sullivan, B. K. et al. LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47 , 291–295 (2015).
Verbanck, M., Chen, C.-Y., Neale, B. & Do, R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 50 , 693–698 (2018).
COVID-19 Host Genetics Initiative. Mapping the human genetic architecture of COVID-19. Nature 600 , 472–477 (2021).
Yavorska, O. O. & Burgess, S. MendelianRandomization: an R package for performing Mendelian randomization analyses using summarized data. Int. J. Epidemiol. 46 , 1734–1739 (2017).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 7 , e34408 (2018).
Giambartolomei, C. et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet 10 , e1004383 (2014).
Wallace, C. A more accurate method for colocalisation analysis allowing for multiple causal variants. PLoS Genet. 17 , e1009440 (2021).
Su, S. et al. Epidemiology, clinical presentation, pathophysiology, and management of long COVID: an update. Mol. Psychiatry 28 , 4056–4069 (2023).
Article PubMed Google Scholar
Pairo-Castineira, E. et al. Genetic mechanisms of critical illness in COVID-19. Nature 591 , 92–98 (2021).
Letter, T. M. An EUA for baricitinib (Olumiant) for COVID-19. Med. Lett. Drugs Ther. 62 , 202–203 (2020).
Kalil, A. C. et al. Baricitinib plus Remdesivir for Hospitalized Adults with Covid-19. N. Engl. J. Med. 384 , 795–807 (2021).
Hoang, T. N. et al. Baricitinib treatment resolves lower-airway macrophage inflammation and neutrophil recruitment in SARS-CoV-2-infected rhesus macaques. Cell 184 , 460–475.e21 (2021).
Chimalakonda, A. et al. Selectivity Profile of the Tyrosine Kinase 2 Inhibitor Deucravacitinib Compared with Janus Kinase 1/2/3 Inhibitors. Dermatol. Ther. 11 , 1763–1776 (2021).
Elyoussfi, S., Rane, S. S., Eyre, S. & Warren, R. B. TYK2 as a novel therapeutic target in psoriasis. Expert Rev. Clin. Pharmacol. 16 , 549–558 (2023).
Strobl, B. et al. Novel functions of tyrosine kinase 2 in the antiviral defense against murine cytomegalovirus. J. Immunol. Baltim. Md. 175 , 4000–4008 (2005).
CAS Google Scholar
Davis, H. E., McCorkell, L., Vogel, J. M. & Topol, E. J. Long COVID: major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 21 , 133–146 (2023).
Verma, A. et al. A Phenome-Wide Association Study of genes associated with COVID-19 severity reveals shared genetics with complex diseases in the Million Veteran Program. PLoS Genet 18 , e1010113 (2022).
Fadista, J. et al. Shared genetic etiology between idiopathic pulmonary fibrosis and COVID-19 severity. EBioMedicine 65 , 103277 (2021).
Verma, A. et al. A MUC5B Gene Polymorphism, rs35705950-T, Confers Protective Effects Against COVID-19 Hospitalization but Not Severe Disease or Mortality. Am. J. Respir. Crit. Care Med. 206 , 1220–1229 (2022).
pietznerm. comp-med/phecode-covid19-ukb: v1.0. [object Object] https://doi.org/10.5281/ZENODO.10984028 (2024).
Download references
Acknowledgements
The authors acknowledge the Scientific Computing of the IT Division at the Charité - Universitätsmedizin Berlin for providing computational resources that have contributed to the research results reported in this paper ( https://www.charite.de/en/research/research_support_services/research_infrastructure/science_it/#c30646061 ). This work was supported by funding of the German Centre for Cardiovascular Research (DZHK) and the German Ministry of Education and Research (BMBF), and the UKRI/NIHR Strategic Priorities Award in Multimorbidity Research for the Multimorbidity Mechanism and Therapeutics Research Collaborative (MR/V033867/1) to C.L.. H.H. and S.D. are supported by Health Data Research UK and the National Institute for Health Research (NIHR) Biomedical Research Centre at University College London NHS Hospitals Trust. M.A. and G.K. are supported by National Institutes of Health/National Institute on Aging grants RF1AG059093, U01AG061359, U19AG063744, R01AG069901, U19AG074879, and R01AG081322. G.K. also received funding from the German Federal Ministry of Education and Research (BMBF) (BiomarKid, 01EA2203B) under the umbrella of the European Joint Programming Initiative “A Healthy Diet for a Healthy Life” (JPI HDHL) and of the ERA-NET Cofund ERA-HDHL (GA N° 696295 of the EU Horizon 2020 Research and Innovation Programme) and of the German Network for Mitochondrial Disorders (mitoNET, 01GM1906C). This work was supported by the de.NBI Cloud within the German Network for Bioinformatics Infrastructure (de.NBI) funded by the German Federal Ministry of Education and Research (BMBF) (031A532B, 031A533A, 031A533B, 031A534A, 031A535A, 031A537A, 031A537B, 031A537C, 031A537D, 031A538A).
Author information
These authors contributed equally: Harry Hemingway, Claudia Langenberg.
Authors and Affiliations
Computational Medicine, Berlin Institute of Health at Charité – Universitätsmedizin Berlin, Berlin, Germany
Maik Pietzner, Summaira Yasmeen & Claudia Langenberg
Precision Healthcare University Research Institute, Queen Mary University of London, London, UK
Maik Pietzner, Tomoko Nakanishi & Claudia Langenberg
MRC Epidemiology Unit, University of Cambridge, Cambridge, UK
Maik Pietzner & Claudia Langenberg
Institute of Health Informatics, University College London, London, UK
Spiros Denaxas & Harry Hemingway
Health Data Research UK, London, UK
British Heart Foundation Data Science Centre, London, UK
Spiros Denaxas
National Institute of Health Research University College London Hospitals Biomedical Research Centre, London, UK
Institute of Computational Biology, Helmholtz Zentrum München - German Research Center for Environmental Health, Neuherberg, Germany
Maria A. Ulmer, Matthias Arnold & Gabi Kastenmüller
Department of Psychiatry and Behavioral Sciences, Duke University, Durham, NC, USA
Matthias Arnold
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: M.P., H.H., C.L. Data curation/Software: M.P., S.D., S.Y., M.U., M.A. Formal Analysis: M.P., S.Y. Methodology: M.P., S.D., T.N. Visualization: M.P. Funding acquisition: C.L., H.H. Project administration: C.L., H.H. Supervision: M.P., C.L., H.H. Writing – original draft: M.P., C.L., H.H. Writing – review & editing: S.D., S.Y., M.A., G.K., T.N.
Corresponding authors
Correspondence to Maik Pietzner , Harry Hemingway or Claudia Langenberg .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Communications Medicine thanks Marie Pigeyre and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Peer review file, description of additional supplementary files, supplementary data 1-9, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Pietzner, M., Denaxas, S., Yasmeen, S. et al. Complex patterns of multimorbidity associated with severe COVID-19 and long COVID. Commun Med 4 , 94 (2024). https://doi.org/10.1038/s43856-024-00506-x
Download citation
Received : 09 November 2023
Accepted : 19 April 2024
Published : 08 July 2024
DOI : https://doi.org/10.1038/s43856-024-00506-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Paxlovid is beneficial for high-risk acute COVID-19 patients, study suggests
BY FABRIZIO DARBY July 8, 2024
A study published in The New England Journal of Medicine offers evidence supporting the benefits of Paxlovid in COVID-19 patients who are at high risk for severe or prolonged disease, particularly older adults and those who are immunocompromised. Paxlovid, the brand name for a combination of nirmatrelvir (a drug that inhibits viral replication) and ritonavir (a similar drug that is also used to treat HIV), has been one of the primary weapons in the battle against COVID-19. The drug works by inhibiting a key COVID replication protein known as a protease, which in turn disrupts the ability of SARS-CoV-2 to replicate.
However, there has been limited data highlighting the efficacy of Paxlovid in treating COVID-19 and, as one would expect, this lack of utility holds true in studies conducted on Paxlovid’s effect on Long COVID (discussed later in this post). While there may be some benefit to taking Paxlovid for patients who are at high risk of hospitalization and death from COVID-19 (including those who are immunocompromised and older adults), that may not be true for patients who are not considered high risk, a new study suggests.
“We believe COVID-19 will be with us for some time, if not indefinitely,” says Jennifer Hammond, PhD, head of infectious disease development at Pfizer and one of the study’s lead authors. “We intend to provide significant medical contributions across the COVID-19 disease spectrum, from prevention with vaccines to therapeutics that help patients avoid or address severe outcomes of disease.”
Does Paxlovid affect COVID-19 recovery time?
The latest study, conducted by researchers at Pfizer (the pharmaceutical company that developed Paxlovid), involved 1,288 participants. One group received the drug and another took a placebo.
The experimental group took about 12 days, on average, to recover from COVID-19 symptoms. The placebo group recovered in approximately 13 days. However, there was no statistical difference between the groups. In other words, the study found that Paxlovid does not definitively reduce recovery time in people with acute cases of COVID-19.
“This was a well-done study, but results were somewhat surprising in that Paxlovid did not show great benefit for low-risk patients,” says Scott Roberts, MD, assistant professor of infectious diseases at Yale School of Medicine, who was not involved in the research.
Does Paxlovid reduce hospitalizations?
The research also compared hospitalizations and death across both groups. Only 0.8% of those who took Paxlovid (regardless of vaccination status) were hospitalized or died compared to 1.6% of patients who received the placebo.
Among the small number who were hospitalized, [SL2] [SL3] none of the patients who received Paxlovid were admitted to the ICU. Meanwhile 30% of hospitalized patients who took a placebo ended up in the ICU.
Furthermore, when researchers looked only at high-risk individuals, 0.9% of the group taking Paxlovid were hospitalized, while 2.2% of the patients in the placebo group were hospitalized. Finally, patients taking Paxlovid recorded a lower number of medical visits compared to the placebo group.
These findings seem to indicate that Paxlovid, while not necessarily effective at reducing the duration of COVID-19 symptoms, may lessen the number of hospitalizations related to COVID-19 in high-risk patients. [SL4] Furthermore, the reduced number of visits for medical attention in the treatment groups suggests that the illness itself may have been less severe.
Meanwhile, the researchers did not observe any difference in the number of adverse events, such as diarrhea, in patients taking the drug versus patients who were in the placebo group. However, of the minority of participants (12.7%) who had adverse events linked to Paxlovid treatment, a metallic taste was most frequently cited.
Future studies will explore Paxlovid as a treatment for Long COVID
When it comes to Long COVID there remains questions about whether Paxlovid is effective. One study, the STOP-PASC Trial , showed that Paxlovid did not improve symptoms. Another study of Paxlovid for Long COVID, led by Yale School of Medicine’s Harlan Krumholz, MD , Harold H. Hines, Jr. Professor of Medicine (Cardiology), and Akiko Iwasaki, PhD , Sterling Professor of Immunobiology, will report results soon.
Long COVID likely has multiple drivers, and there may be a subset of patients whose symptoms are indeed caused by SARS-CoV-2 persistence. The Yale study, which employed a groundbreaking decentralized design, will test the effect of Paxlovid overall and study in more detail who is most likely to benefit from antiviral treatment. To do so, the team collected biospecimens from the participants before, during, and after receiving a 15-day course of Paxlovid or placebo. They will measure many biological markers to assess predictors of response and identify possible targets for future diagnostic and therapeutic strategies.
“This study is exceptionally novel – from its decentralized design to the application of deep immune phenotyping, a method to discover how immune function relates to disease and recovery,” said Krumholz.
“While at this time PAXLOVID has not been licensed or approved for use as a treatment or prophylactic for Long COVID, we are collaborating on multiple investigator-sponsored studies, including with Yale, to evaluate Paxlovid for potential use in patients with Long COVID,” says Hammond. “By investing in this collaborative approach, we aim to help accelerate and streamline research efforts that can advance our collective knowledge about Long COVID.”
The last word by Lisa Sanders, MD
This is an important study on the use of Paxlovid to reduce symptoms in adults at risk for some of the complications of acute COVID-19. Turns out that for these patients, whose INCREASED risk primarily DUE TO smoking, obesity or hypertention, Paxlovid may reduce the severity of the illness but not the duration. However, a thoughtful editorial, published in the same issue of the New England Journal of Medicine ( Treating Acute Covid-19 — Final Chapters Still Unwritten | New England Journal of Medicine (nejm.org) ) suggests that the study “enrolled only a small percentage of persons at the highest risk for progression — older persons, those who are immunocompromised, and those with serious coexisting conditions (e.g., heart or lung disease) — who constitute most of the patients hospitalized with Covid-19.”
This segment of patients deserve a closer look at how Paxlovid may alter their COVID19 infection. However, before those outside these highest risk groups give up on Paxlovid, one issue not touched on by this study was whether Paxlovid changes an individual’s risk of developing Long COVID – for infection survivors the greatest COMPLICATION OF acute COVID19. There are studies that suggest that it can reduce that risk. One study published last year reviewed the charts of nearly 300,000 veterans with at least one risk factor for progression to severe disease and found that treatment with Paxlovid reduced the likelihood of their developing Long COVID. ( Association of Treatment With Nirmatrelvir and the Risk of Post–COVID-19 Condition | Clinical Pharmacy and Pharmacology | JAMA Internal Medicine | JAMA Network )
I would encourage those concerned about Long COVID TO continue to consider USING PAXLOVID WHEN infected with SARS CoV2, until we have good evidence that it doesn’t change outcomes beyond death and hospitalizations - important but THANKFULLY LESS COMMON outcomes these days – and that include THE INCIDENCE OF Long COVID.
Read other installments of Long COVID Dispatches here .
If you’d like to share your experience with Long COVID for possible use in a future post (under a pseudonym), write to us at: [email protected]
Information provided in Yale Medicine content is for general informational purposes only. It should never be used as a substitute for medical advice from your doctor or other qualified clinician. Always seek the individual advice of your health care provider for any questions you have regarding a medical condition.
More news from Yale Medicine

Making visible the invisible: Supporting long COVID patients and the people caring for them
Assistant Professor, Faculty of Health Sciences; Senior Scientist, Pacific Institute on Pathogens, Pandemics and Society, Simon Fraser University
Assistant Professor, Faculty of Health Sciences, Simon Fraser University
Master's Student in Communication, Research Assistant for Pacific Institute on Pathogens, Pandemics and Society, Simon Fraser University
Academic Researcher, Director of Knowledge Mobilization, Pacific Institute on Pathogens, Pandemics and Society, Simon Fraser University
Disclosure statement
Kaylee Byers collaborates with and receives funding from the Post-COVID Interdisciplinary Care Network (PC-ICCN). "The MyGuide: Long COVID" is a resource created by the PC-ICCN. The work mentioned in this study is also funded in part by Michael Smith Health Research BC.
Kayli Jamieson collaborates with and receives funding from the B.C. Post-COVID Interdisciplinary Care Network (PC-ICCN). "The MyGuide: Long COVID" is a resource created by the PC-ICCN. The work mentioned in this study is also funded in part by Michael Smith Health Research BC. She also is a patient advisor for Long COVID The Answers.
Rackeb Tesfaye collaborates and receives funding from the PC-ICCN.
Julia Smith does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Simon Fraser University provides funding as a member of The Conversation CA.
Simon Fraser University provides funding as a member of The Conversation CA-FR.
View all partners
We are living through a mass-disabling event : Over 200 million people worldwide have long COVID . In Canada, one in nine people have experienced long COVID symptoms, and this is likely an underestimate.
Occurring weeks to months after a COVID-19 infection, this multi-system chronic illness has led to what some have called “ the shadow pandemic .” Although millions are navigating this new illness, four years into the pandemic both patients and their caregivers continue to face challenges accessing the information and care they need.
Most Canadians have had COVID, and at least one in five have been infected more than once . These trends are troubling because evidence suggests that the risk of acquiring long COVID increases with reinfection .
Long COVID is a complex illness that can present with a range of neurological and cardiovascular symptoms, such as post-exertional malaise , heart palpitations, cognitive impairment, fatigue and around 200 other symptoms . Some people with long COVID, often referred to as “longhaulers,” experience other under-researched syndromes, such as myalgic encephalomyelitis (ME) — also known as chronic fatigue syndrome.

With a suite of life-altering impacts, it is unsurprising that longhaulers may also experience impacts to their mental health, financial stability and relationships with others. These experiences are further exacerbated by the fact that there remains no cure for long COVID.
Over the past year, our team at Simon Fraser University has been speaking with long COVID patients, unpaid caregivers — such as family and friends who take on caregiving roles — clinicians and long COVID researchers to better understand patient experiences. In a new report , we documented a number of challenges patients and their caregivers face as well as recommendations to reduce these barriers.
Holistic approaches to care
Because symptoms and experiences vary, there is no single approach to care that will support all longhaulers. In British Columbia, post-COVID recovery clinics have been instrumental in creating specialized regional spaces for long COVID care.
These clinics have blended physician care, allied health care — such as physiotherapy and occupational therapy — and patient support groups. The closure of in-person clinics in transition to an online care system , in combination with long wait times, has meant that some patients have difficulty accessing these clinics.

Longhaulers have emphasized the value of specialized clinics and the need for holistic approaches that encompass allied health care to address the multifaceted impacts of long COVID on patients’ lives. Caregivers in particular expressed a need for mental health supports due to additional strains on their ability to work, their relationships and other responsibilities.
Holistic approaches are being embraced by some groups such as the Clinical Post COVID Society in the United Kingdom which brings together a “ diverse multidisciplinary clinical leadership team to reflect the varied expertise needed to care for patients with long COVID .” This example may serve as a helpful model for mobilizing these approaches in Canada.
Information
Access to information about long COVID remains a significant challenge. While longhaulers obtain information from health-care providers ( which can vary and be contradictory ), many are unable to meet with a doctor.
In B.C., approximately one in five people don’t have a family doctor . As a result, many are left to search for information themselves, wading through websites and articles while trying to discern what to trust. This can be especially challenging for people experiencing brain fog and fatigue, or those limited in time and resources due to caregiving, work or other demands on their time.
Patients, caregivers, clinicians and researchers suggest that the federal government create a national long COVID information platform providing details about symptoms, symptom management, a database of health-care practitioners providing long COVID care, and updates on recent research.
This could be modelled off the Post-COVID MyGuide, produced by the Post-COVID Interdisciplinary Clinical Care Network in B.C. . And while such resources are critical to supporting longhaulers, they are only useful if people access them. Therefore, more investment is needed to raise awareness of these platforms, evaluate their usefulness and explore ways to scale them for national use.
Another key outcome for improving care is refocusing preventive efforts to reduce reinfection risk for longhaulers, and future long COVID cases. Prevention measures might include campaigns promoting wearing respirators, regular vaccinations, increasing paid sick days or improving air filtration and ventilation indoors.
Preventing long COVID also involves taking these precautions in the absence of visible illness , as some early estimates suggested that 59 per cent of transmission occurs without symptoms .
Our team put these prevention measures into practice in April when we hosted a hybrid long COVID event with Pulitzer-prize winning journalist Ed Yong and a panel of patients, caregivers, clinicians and researchers. The event included safety measures such as mandatory masking in KN95/N95 respirators, rapid testing of participants and MERV-13 air filters .
Both during and since this event we have received numerous messages from longhaulers speaking to how the event and the safety measures in place were meaningful to them and made them feel seen. In order to do this, collectively (researchers, clinicians, policymakers and the public) can take many steps to create safe spaces as a baseline to reduce transmission risks.
As we continue to grapple with the enduring legacies of the COVID-19 pandemic, we must recognize that many communities have been disproportionately affected by SARS-CoV-2. To address these differential impacts, patients and caregivers advocate for continued investments in patient-centred research and care to create initiatives that resonate and are relevant for those most affected.
To further amplify these stories and raise awareness, our team is developing a long COVID “Day in the Life” photo exhibit in partnership with the Museum of Vancouver, where long COVID patients can share their stories and photos. Activities like this are one more step to making visible the experiences of people with an invisible illness.

Audience Insight Officer

Director, Student Administration

Senior Integration Developer

Sydney Horizon Educators – Faculty of Engineering (Targeted)

Lecturer in Indigenous Health (Identified)
With long COVID, I’ve learned to take the lead on treatments and be kind to myself
First Person is a daily personal piece submitted by readers. Have a story to tell? See our guidelines at tgam.ca/essayguide .

cmyk for print Illustration by Alex Deadman-Wylie
I used to revere any GP that treated me for a medical condition, even when they overshot with prescriptions or had no answers for a particular issue. I was taught at a young age that respecting people with “authority” was the order of the day.
But that was before COVID-19.
The formula for my wellness has now become more complicated.
Like millions of others, I have Long COVID.
When it comes to this elusive condition, the doctor has become as helpless as the patient.
No, it’s not the doctors’ fault. But even though I lack the qualifications, now I am the doctor.
While waiting on science and Western medicine for cures or relief, life goes on, and many of us who struggle with this condition are forced to use what little energy we have to hold onto hope, while hope is busy taking a beating.
I, like many others, have been forced to figure it out and treat myself as best I can with whatever tools I deem helpful and while that is alarmingly inconvenient, it’s also an indicator of a developing trend moving toward more and more explorative self-care.
Don’t worry. I don’t practice witchcraft. But if I knew that might work, I would dust off my broom right away and type in a search for “cauldrons” on Amazon.
I’m always up for a good challenge, but this one has been as daunting and difficult as they come.
Desperation has taken me down many paths toward treatments I wouldn’t possibly have considered in the past. No need to list them all here. It’s not my intention to be self-righteous or prescriptive.
From what I can understand, the symptoms for Long COVID are many (over 200 listed from various sources) and can differ greatly from person to person, so currently, a blanket treatment is not in the cards. A recent study ruled out the antiviral drug Paxlovid as a potential saviour. No shock there.
So, I do the best I can with the tools I accumulate. Some have even helped a bit, but no single form of treatment has proven to be my panacea.
Silver linings have become my golden ticket to tolerance and the one that shines through is self-compassion. As I connect with what often feels like a broken body, it somehow feels instinctive to talk to myself with kindness; and while not medically substantive, it’s proving to be a useful tool. Like magic, symptoms sometimes soften under this light.
It’s no cure, but I do see it as progress. I certainly know my body better and can find some solace from that internal connection.
I recently read that a marathon winner won the race without her watch, a common tool for runners. Instead, she connected with her body. What a concept.
My marathon is a little different. It’s metaphorical at best but I’m running with it.
I used to have so much difficulty connecting with my body, even after hundreds of yoga classes. But not now.
Long COVID is like a solid Ethernet connection; you’re connected all the time. Even when you don’t want to be. So, I’ve made friends with it, even when it barks back like an angry dog.
A lot can come up when I tune in, but through the haze of symptoms such as severe fatigue and brain fog, there is an emotional lucidity that feels like a bit of a gift, albeit one that’s delivered during a thunderstorm.
This adversity has enabled me to know myself better and one of my biggest lessons has been that self-pity is both unhelpful and potentially damaging. It’s just more fuel on an already formidable fire.
In social situations, I put on a brave face – most people are unaware of my current condition. I hide it well because I’m more terrified of becoming a victim than I am of the continuing symptoms. I even feel guilty showing my wife, but to her great credit, she’s been a champ through all of it. She’s in for the long haul, so to speak, and I adore her for it.
If she can show me that kind of love, I can show it to myself as well.
She has helped me understand that self-compassion begets kindness which begets gratitude which begets acceptance. That said, I hope to “be getting” fully better soon.
When that happens, and it will, I know a better human being will emerge.
It occurs to me that the template for a person’s overall well-being can be compared to the game of chess. Western medicine may be the king, but its abilities are limited. Yes, its authority may be prominent and well-documented, but it can still only do so much.
The king needs the agility and varying talents of his queen, bishops, knights and rooks to be successful.
If we rely solely on our king, we all become pawns.
So, for now, I turn inward to self-compassion, and it gently speaks back:
“It’s not your fault, Paul. It’s not your fault.”
Paul McQuillan lives in Toronto
Report an editorial error
Report a technical issue
Editorial code of conduct
Follow related authors and topics
- Amazon Follow You must be logged in to follow. Log In Create free account
- First Person Follow You must be logged in to follow. Log In Create free account
Authors and topics you follow will be added to your personal news feed in Following .
Interact with The Globe
COVID-19 variant KP.3 remains dominant in US, rises to 36.9% of cases: See latest CDC data
The cdc predicts that the kp.3 covid-19 variant will 'continue increasing.'.

The KP.3 COVID-19 variant is continuing to lead as the dominant variant, the newest Centers for Disease Control and Prevention (CDC) data shows.
For a two-week period starting on June 23 and ending on July 6, the CDC’s Nowcast data tracker showed the projections of the COVID-19 variants. The KP.3 variant accounted for 36.9% of positive infections followed by KP.2 at 24.4%.
"Estimates predict that KP.3 is the dominant SARS-CoV-2 variant making up 31.2 to 43% of viruses nationally. KP.3 is projected to continue increasing as proportions of the variants that cause COVID-19," CDC Spokesperson, Rosa Norman, told USA TODAY in a statement. "KP.3 evolved from JN.1, which was the major viral lineage circulating since December 2023."
The data also shows that the new variant LB.1 has fallen back 3% by accounting for 14.5% of cases but was previously at 17.5% of infections. JN.1, the previous ring leader since 2023, only had 1.0% of positive cases which is a 0.6% decrease from the previous two-week period.
On July 2, the CDC said that the COVID-19 infections are growing in 39 states , stable or uncertain in 10 states and declining in zero.
Here’s what you need to know about the KP.3 variant.
More COVID-19 News: Should you get the updated COVID-19 vaccine? See current guidelines from CDC.
What is the KP.3 variant?
Like JN.1 and "FLiRT" variants KP.1.1 and KP.2, KP.3 is a similar strain. Norman said that the KP.3 variant is, “a sublineage of the JN.1 lineage” which comes from the Omicron variant.
Symptoms of COVID-19
The CDC has not said if KP.3 has its own specific symptoms. Norman said the symptoms associated with KP.3 are similar to those from JN.1. However, the government agency outlines the basic symptoms of COVID-19 on its website. These symptoms can appear between two to 14 days after exposure to the virus and can range from mild to severe.
These are some of the symptoms of COVID-19:
- Fever or chills
- Shortness of breath or difficulty breathing
- Muscle or body aches
- Loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
The CDC said you should seek medical attention if you have the following symptoms:
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray or blue-colored skin, lips, or nail beds
How can we protect ourselves from KP.3 and other variants?
The CDC recommends for everyone ages 6 months and older, with some exceptions, receive an updated 2024-2025 COVID-19 vaccine to protect against the disease, regardless whether or not you have previously been vaccinated against the virus.
CDC data shows the COVID-19 test positivity by state
CDC data shows which states has the lowest and highest COVID-19 positivity rates from June 29 to July 5, 2024.
Can't see the map? Click here to view it.
Within the past week COVID-19 test positivity has risen 9%, the CDC data shows.
Changes in COVID-19 test positivity within a week
Based on data collected by the CDC it showed that five states had the biggest increase of 4.7% in positive COVID-19 cases from June 29 to July 5, 2024.
Here's the list of states and their changes in COVID-19 positivity for the past week.
| Alabama | +2.6 |
| Alaska | +3.4 |
| Arizona | +2.1 |
| Arkansas | +4.7 |
| California | +2.1 |
| Colorado | +2.6 |
| Connecticut | +0.7 |
| Delaware | +2.3 |
| District of Columbia | +2.3 |
| Florida | +2.6 |
| Georgia | +2.6 |
| Hawaii | +2.1 |
| Idaho | +3.4 |
| Illinois | +2.9 |
| Indiana | +2.9 |
| Iowa | +2.3 |
| Kansas | +2.3 |
| Kentucky | +2.6 |
| Louisiana | +4.7 |
| Maine | +0.7 |
| Maryland | +2.3 |
| Massachusetts | +0.7 |
| Michigan | +2.9 |
| Minnesota | +2.9 |
| Mississippi | +2.6 |
| Missouri | +2.3 |
| Montana | +2.6 |
| Nebraska | +2.3 |
| Nevada | +2.1 |
| New Hampshire | +0.7 |
| New Jersey | +2.2 |
| New Mexico | +4.7 |
| New York | +2.2 |
| North Carolina | +2.6 |
| North Dakota | +2.6 |
| Ohio | +2.9 |
| Oklahoma | +4.7 |
| Oregon | +3.4 |
| Pennsylvania | +2.3 |
| Puerto Rico | +2.2 |
| Rhode Island | +0.7 |
| South Carolina | +2.6 |
| South Dakota | +1.5 |
| Tennessee | +2.6 |
| Texas | +4.7 |
| Utah | +2.6 |
| Vermont | +0.7 |
| Virginia | +2.3 |
| Washington | +3.4 |
| West Virginia | +2.3 |
| Wisconsin | +2.9 |
| Wyoming | +2.6 |
Ahjané Forbes is a reporter on the National Trending Team at USA TODAY. Ahjané covers breaking news, car recalls, crime, health, lottery and public policy stories. Email her at [email protected] . Follow her on Instagram , Threads and X (Twitter) @forbesfineest.
Contributing: Emily DeLetter

COMMENTS
This essay is an opportunity to share your pandemic experience and the lessons learned. The college admissions process has experienced significant changes as a result of COVID-19, creating new challenges for high school students. Since the onset of the pandemic, admissions officers have strongly emphasized a more holistic review process.
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it, this space is yours to describe those impacts. Colleges care about the effects on your health and well-being, safety, family circumstances, future plans, and education, including access to reliable technology and quiet study spaces.
Writing About COVID-19 in College Essays. Experts say students should be honest and not limit themselves to merely their experiences with the pandemic. The global impact of COVID-19, the disease ...
Writing about COVID-19 in your main essay. Write about your experiences during the pandemic in your main college essay if your experience is personal, relevant, and the most important thing to discuss in your college admission essay. ... Experiences like this can be good topics for the CommonApp essay as long as they reflect something genuinely ...
100 Words Essay on Covid 19. COVID-19 or Corona Virus is a novel coronavirus that was first identified in 2019. It is similar to other coronaviruses, such as SARS-CoV and MERS-CoV, but it is more contagious and has caused more severe respiratory illness in people who have been infected. The novel coronavirus became a global pandemic in a very ...
Students can use the Common App's new Covid-19 essay to expand on their ... "Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts. If you need it ...
Community disruptions such as COVID-19 and natural disasters can have deep and long-lasting impacts.If you need it, this space is yours to describe those impacts. —The 2020-21 college-admissions ...
Love came up in 286 essays; science in 128; art in 110; music in 109; and honor in 32. ... For a long time, things felt as if they weren't going to get better. ... Covid-19 has taken a lot from ...
Read these 12 moving essays about life during coronavirus. Artists, novelists, critics, and essayists are writing the first draft of history. A woman wearing a face mask in Miami. Alissa Wilkinson ...
First-person essay: Doing my part to end the pandemic. I want to particularly encourage the African American community, which has been disproportionately impacted by COVID-19, to step forward, receive this vaccine and spread the word to your families. Let's put this pandemic behind us in 2021 — together.
Horrific history. Looking back, the COVID-19 pandemic stands as arguably the most disruptive event of the 21st century, surpassing wars, the September 11, 2001, terrorist attacks, the effects of climate change, and the Great Recession. It has killed more than seven million people to date and reshaped the world economy, public health, education ...
Step 1: Choose a Specific Thesis Statement. Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example: Thesis Statement: "COVID-19 vaccination mandates are necessary for public health and safety."
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
View our collection of covid 19 essays. Find inspiration for topics, titles, outlines, & craft impactful covid 19 papers. Read our covid 19 papers today! Homework Help; Essay Examples; ... long-term financial survival, staff availability for being active even on low salaries, and delivery concerns to meet the clients needs (Tsega et al., 2020 ...
In conclusion, COVID-19 tested the patience and resilience of the mankind. This pandemic has taught people the importance of patience, effort and humbleness. Also Read: Essay on My Best Friend. Essay On COVID-19 in 300 Words. COVID-19, also known as the coronavirus, is a serious and contagious disease that has affected people worldwide.
1. In fall of 2019, exactly zero scientists were studying COVID‑19, because no one knew the disease existed. The coronavirus that causes it, SARS‑CoV‑2, had only recently jumped into humans ...
Guest Essay. The Truth About Long Covid Is Complicated. ... Covid-19 pandemic and long Covid itself requires not just containing the outbreak but also providing adequate social supports and ...
Essay Coronavirus Pandemic. Coronavirus: The world has come together to flatten the curve. ... We had taken advantage of our day off, while our teachers spent the day planning for an extended school closure due to COVID-19. ... even if it didn't last long. As days passed, it became clear to everyone, myself included, that the situation was ...
Most people who develop COVID-19 fully recover, but current evidence suggests approximately 10-20% of people experience a variety of mid and long-term effects after they recover from their initial illness. Although our current understanding of causes of post COVID-19 condition and why some people are more affected is limited, this questions and answers page will help you understand more ...
Essay on COVID-19 Pandemic. Published: 2021/11/08. Number of words: 1220. As a result of the COVID-19 (Coronavirus) outbreak, daily life has been negatively affected, impacting the worldwide economy. Thousands of individuals have been sickened or died as a result of the outbreak of this disease. When you have the flu or a viral infection, the ...
When the Covid-19 outbreak was detected, Dr. Shi initially wondered if the novel coronavirus had come from her laboratory, saying she had never expected such an outbreak to occur in Wuhan.
Paragraph Writing on Covid-19 in 100 Words. Coronavirus is an infectious disease and is commonly called Covid-19. It affects the human respiratory system causing difficulty in breathing. It is a contagious disease and has been spreading across the world like wildfire. The virus was first identified in 2019 in Wuhan, China.
PET tracer shows increased T cell activation across the body in those who contracted COVID-19 27 days before to as many as 654 days before. ( UCSF ) The findings are only correlative, but they provide compelling evidence that long COVID is tied to the persistence of the SARS-CoV-2 virus in the body and abnormal immune activity.
Here we identify 679 diseases associated with an increased risk for severe COVID-19 (n = 672) and/or Long COVID (n = 72) that span almost all clinical specialties and are strongly enriched in ...
A study published in The New England Journal of Medicine offers evidence supporting the benefits of Paxlovid in COVID-19 patients who are at high risk for severe or prolonged disease, particularly older adults and those who are immunocompromised. Paxlovid, the brand name for a combination of nirmatrelvir (a drug that inhibits viral replication) and ritonavir (a similar drug that is also used ...
The prevalence of long COVID — a multi-system chronic illness occurring weeks to months after a COVID-19 infection — has led to what some have called 'the hidden pandemic.' (Shutterstock)
Dr. Anthony Fauci was the government's top infectious disease official during the COVID-19 pandemic. Lessons he learned from that experience, and reflections on his long career in public health.
Earlier this month, the FDA endorsed a plan to update the Covid-19 shots to be more effective against the JN.1 lineage of the coronavirus. But the agency later updated its own recommendation.
But that was before COVID-19. ... From what I can understand, the symptoms for Long COVID are many (over 200 listed from various sources) and can differ greatly from person to person, so currently ...
Changes in COVID-19 test positivity within a week. Based on data collected by the CDC it showed that five states had the biggest increase of 4.7% in positive COVID-19 cases from June 29 to July 5 ...