An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Biological, Psychological, and Social Determinants of Depression: A Review of Recent Literature
Olivia remes.
1 Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK
João Francisco Mendes
2 NOVA Medical School, Universidade NOVA de Lisboa, 1099-085 Lisbon, Portugal; ku.ca.mac@94cfj
Peter Templeton
3 IfM Engage Limited, Institute for Manufacturing, University of Cambridge, Cambridge CB3 0FS, UK; ku.ca.mac@32twp
4 The William Templeton Foundation for Young People’s Mental Health (YPMH), Cambridge CB2 0AH, UK
Associated Data
Depression is one of the leading causes of disability, and, if left unmanaged, it can increase the risk for suicide. The evidence base on the determinants of depression is fragmented, which makes the interpretation of the results across studies difficult. The objective of this study is to conduct a thorough synthesis of the literature assessing the biological, psychological, and social determinants of depression in order to piece together the puzzle of the key factors that are related to this condition. Titles and abstracts published between 2017 and 2020 were identified in PubMed, as well as Medline, Scopus, and PsycInfo. Key words relating to biological, social, and psychological determinants as well as depression were applied to the databases, and the screening and data charting of the documents took place. We included 470 documents in this literature review. The findings showed that there are a plethora of risk and protective factors (relating to biological, psychological, and social determinants) that are related to depression; these determinants are interlinked and influence depression outcomes through a web of causation. In this paper, we describe and present the vast, fragmented, and complex literature related to this topic. This review may be used to guide practice, public health efforts, policy, and research related to mental health and, specifically, depression.
1. Introduction
Depression is one of the most common mental health issues, with an estimated prevalence of 5% among adults [ 1 , 2 ]. Symptoms may include anhedonia, feelings of worthlessness, concentration and sleep difficulties, and suicidal ideation. According to the World Health Organization, depression is a leading cause of disability; research shows that it is a burdensome condition with a negative impact on educational trajectories, work performance, and other areas of life [ 1 , 3 ]. Depression can start early in the lifecourse and, if it remains unmanaged, may increase the risk for substance abuse, chronic conditions, such as cardiovascular disease, and premature mortality [ 4 , 5 , 6 , 7 , 8 ].
Treatment for depression exists, such as pharmacotherapy, cognitive behavioural therapy, and other modalities. A meta-analysis of randomized, placebo-controlled trials of patients shows that 56–60% of people respond well to active treatment with antidepressants (selective serotonin reuptake inhibitors, tricyclic antidepressants) [ 9 ]. However, pharmacotherapy may be associated with problems, such as side-effects, relapse issues, a potential duration of weeks until the medication starts working, and possible limited efficacy in mild cases [ 10 , 11 , 12 , 13 , 14 ]. Psychotherapy is also available, but access barriers can make it difficult for a number of people to get the necessary help.
Studies on depression have increased significantly over the past few decades. However, the literature remains fragmented and the interpretation of heterogeneous findings across studies and between fields is difficult. The cross-pollination of ideas between disciplines, such as genetics, neurology, immunology, and psychology, is limited. Reviews on the determinants of depression have been conducted, but they either focus exclusively on a particular set of determinants (ex. genetic risk factors [ 15 ]) or population sub-group (ex. children and adolescents [ 16 ]) or focus on characteristics measured predominantly at the individual level (ex. focus on social support, history of depression [ 17 ]) without taking the wider context (ex. area-level variables) into account. An integrated approach paying attention to key determinants from the biological, psychological, and social spheres, as well as key themes, such as the lifecourse perspective, enables clinicians and public health authorities to develop tailored, person-centred approaches.
The primary aim of this literature review: to address the aforementioned challenges, we have synthesized recent research on the biological, psychological, and social determinants of depression and we have reviewed research from fields including genetics, immunology, neurology, psychology, public health, and epidemiology, among others.
The subsidiary aim: we have paid special attention to important themes, including the lifecourse perspective and interactions between determinants, to guide further efforts by public health and medical professionals.
This literature review can be used as an evidence base by those in public health and the clinical setting and can be used to inform targeted interventions.
2. Materials and Methods
We conducted a review of the literature on the biological, psychological, and social determinants of depression in the last 4 years. We decided to focus on these determinants after discussions with academics (from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas), charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020. In several aspects, we attempted to conduct this review according to PRISMA guidelines [ 18 ].
The inclusion and exclusion criteria are the following:
- - We included documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries on the determinants of depression. The determinants refer to variables that appear to be linked to the development of depression, such as physiological factors (e.g., the nervous system, genetics), but also factors that are further away or more distal to the condition. Determinants may be risk or protective factors, and individual- or wider-area-level variables.
- - We focused on major depressive disorder, treatment-resistant depression, dysthymia, depressive symptoms, poststroke depression, perinatal depression, as well as depressive-like behaviour (common in animal studies), among others.
- - We included papers regardless of the measurement methods of depression.
- - We included papers that focused on human and/or rodent research.
- - This review focused on articles written in the English language.
- - Documents published between 2017–2020 were captured to provide an understanding of the latest research on this topic.
- - Studies that assessed depression as a comorbidity or secondary to another disorder.
- - Studies that did not focus on rodent and/or human research.
- - Studies that focused on the treatment of depression. We made this decision, because this is an in-depth topic that would warrant a separate stand-alone review.
- Next, we searched PubMed (2017–2020) using keywords related to depression and determinants. Appendix A contains the search strategy used. We also conducted focused searches in Medline, Scopus, and PsycInfo (2017–2020).
- Once the documents were identified through the databases, the inclusion and exclusion criteria were applied to the titles and abstracts. Screening of documents was conducted by O.R., and a subsample was screened by J.M.; any discrepancies were resolved through a communication process.
- The full texts of documents were retrieved, and the inclusion and exclusion criteria were again applied. A subsample of documents underwent double screening by two authors (O.R., J.M.); again, any discrepancies were resolved through communication.
- a. A data charting form was created to capture the data elements of interest, including the authors, titles, determinants (biological, psychological, social), and the type of depression assessed by the research (e.g., major depression, depressive symptoms, depressive behaviour).
- b. The data charting form was piloted on a subset of documents, and refinements to it were made. The data charting form was created with the data elements described above and tested in 20 studies to determine whether refinements in the wording or language were needed.
- c. Data charting was conducted on the documents.
- d. Narrative analysis was conducted on the data charting table to identify key themes. When a particular finding was noted more than once, it was logged as a potential theme, with a review of these notes yielding key themes that appeared on multiple occasions. When key themes were identified, one researcher (O.R.) reviewed each document pertaining to that theme and derived concepts (key determinants and related outcomes). This process (a subsample) was verified by a second author (J.M.), and the two authors resolved any discrepancies through communication. Key themes were also checked as to whether they were of major significance to public mental health and at the forefront of public health discourse according to consultations we held with stakeholders from the Manchester Metropolitan University, University of Cardiff, University of Colorado, Boulder, University of Cork, University of Leuven, University of Texas, charity representatives, and people with lived experience at workshops held by the University of Cambridge in 2020.
We condensed the extensive information gleaned through our review into short summaries (with key points boxes for ease of understanding and interpretation of the data).
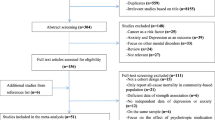
Through the searches, 6335 documents, such as primary studies, literature reviews, systematic reviews, meta-analyses, reports, and commentaries, were identified. After applying the inclusion and exclusion criteria, 470 papers were included in this review ( Supplementary Table S1 ). We focused on aspects related to biological, psychological, and social determinants of depression (examples of determinants and related outcomes are provided under each of the following sections.
3.1. Biological Factors
The following aspects will be discussed in this section: physical health conditions; then specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway. Finally, aspects related to cognition will also be discussed in the context of depression.
3.1.1. Physical Health Conditions
Studies on physical health conditions—key points:
- The presence of a physical health condition can increase the risk for depression
- Psychological evaluation in physically sick populations is needed
- There is large heterogeneity in study design and measurement; this makes the comparison of findings between and across studies difficult
A number of studies examined the links between the outcome of depression and physical health-related factors, such as bladder outlet obstruction, cerebral atrophy, cataract, stroke, epilepsy, body mass index and obesity, diabetes, urinary tract infection, forms of cancer, inflammatory bowel disorder, glaucoma, acne, urea accumulation, cerebral small vessel disease, traumatic brain injury, and disability in multiple sclerosis [ 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 ]. For example, bladder outlet obstruction has been linked to inflammation and depressive behaviour in rodent research [ 24 ]. The presence of head and neck cancer also seemed to be related to an increased risk for depressive disorder [ 45 ]. Gestational diabetes mellitus has been linked to depressive symptoms in the postpartum period (but no association has been found with depression in the third pregnancy trimester) [ 50 ], and a plethora of other such examples of relationships between depression and physical conditions exist. As such, the assessment of psychopathology and the provision of support are necessary in individuals of ill health [ 45 ]. Despite the large evidence base on physical health-related factors, differences in study methodology and design, the lack of standardization when it comes to the measurement of various physical health conditions and depression, and heterogeneity in the study populations makes it difficult to compare studies [ 50 ].
The next subsections discuss specific biological factors, including genetics; the microbiome; inflammatory factors; stress and hypothalamic–pituitary–adrenal (HPA) axis dysfunction, and the kynurenine pathway; and aspects related to cognition.
3.1.2. Genetics
Studies on genetics—key points:
There were associations between genetic factors and depression; for example:
- The brain-derived neurotrophic factor (BDNF) plays an important role in depression
- Links exist between major histocompatibility complex region genes, as well as various gene polymorphisms and depression
- Single nucleotide polymorphisms (SNPs) of genes involved in the tryptophan catabolites pathway are of interest in relation to depression
A number of genetic-related factors, genomic regions, polymorphisms, and other related aspects have been examined with respect to depression [ 61 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 ]. The influence of BDNF in relation to depression has been amply studied [ 117 , 118 , 141 , 142 , 143 ]. Research has shown associations between depression and BDNF (as well as candidate SNPs of the BDNF gene, polymorphisms of the BDNF gene, and the interaction of these polymorphisms with other determinants, such as stress) [ 129 , 144 , 145 ]. Specific findings have been reported: for example, a study reported a link between the BDNF rs6265 allele (A) and major depressive disorder [ 117 ].
Other research focused on major histocompatibility complex region genes, endocannabinoid receptor gene polymorphisms, as well as tissue-specific genes and gene co-expression networks and their links to depression [ 99 , 110 , 112 ]. The SNPs of genes involved in the tryptophan catabolites pathway have also been of interest when studying the pathogenesis of depression.
The results from genetics studies are compelling; however, the findings remain mixed. One study indicated no support for depression candidate gene findings [ 122 ]. Another study found no association between specific polymorphisms and major depressive disorder [ 132 ]. As such, further research using larger samples is needed to corroborate the statistically significant associations reported in the literature.
3.1.3. Microbiome
Studies on the microbiome—key points:
- The gut bacteria and the brain communicate via both direct and indirect pathways called the gut-microbiota-brain axis (the bidirectional communication networks between the central nervous system and the gastrointestinal tract; this axis plays an important role in maintaining homeostasis).
- A disordered microbiome can lead to inflammation, which can then lead to depression
- There are possible links between the gut microbiome, host liver metabolism, brain inflammation, and depression
The common themes of this review have focused on the microbiome/microbiota or gut metabolome [ 146 , 147 , 148 , 149 , 150 , 151 , 152 , 153 , 154 , 155 , 156 , 157 , 158 , 159 , 160 , 161 ], the microbiota-gut-brain axis, and related factors [ 152 , 162 , 163 , 164 , 165 , 166 , 167 ]. When there is an imbalance in the intestinal bacteria, this can interfere with emotional regulation and contribute to harmful inflammatory processes and mood disorders [ 148 , 151 , 153 , 155 , 157 ]. Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome [ 158 ].
Research has also attempted to disentangle the links between the gut microbiome, host liver metabolism, brain inflammation, and depression, as well as the role of the ratio of lactobacillus to clostridium [ 152 ]. The literature has also examined the links between medication, such as antibiotics, and mood and behaviour, with the findings showing that antibiotics may be related to depression [ 159 , 168 ]. The links between the microbiome and depression are complex, and further studies are needed to determine the underpinning causal mechanisms.
3.1.4. Inflammation
Studies on inflammation—key points:
- Pro-inflammatory cytokines are linked to depression
- Pro-inflammatory cytokines, such as the tumour necrosis factor (TNF)-alpha, may play an important role
- Different methods of measurement are used, making the comparison of findings across studies difficult
Inflammation has been a theme in this literature review [ 60 , 161 , 164 , 169 , 170 , 171 , 172 , 173 , 174 , 175 , 176 , 177 , 178 , 179 , 180 , 181 , 182 , 183 , 184 ]. The findings show that raised levels of inflammation (because of factors such as pro-inflammatory cytokines) have been associated with depression [ 60 , 161 , 174 , 175 , 178 ]. For example, pro-inflammatory cytokines, such as tumour necrosis factor (TNF)-alpha, have been linked to depression [ 185 ]. Various determinants, such as early life stress, have also been linked to systemic inflammation, and this can increase the risk for depression [ 186 ].
Nevertheless, not everyone with elevated inflammation develops depression; therefore, this is just one route out of many linked to pathogenesis. Despite the compelling evidence reported with respect to inflammation, it is difficult to compare the findings across studies because of different methods used to assess depression and its risk factors.
3.1.5. Stress and HPA Axis Dysfunction
Studies on stress and HPA axis dysfunction—key points:
- Stress is linked to the release of proinflammatory factors
- The dysregulation of the HPA axis is linked to depression
- Determinants are interlinked in a complex web of causation
Stress was studied in various forms in rodent populations and humans [ 144 , 145 , 155 , 174 , 176 , 180 , 185 , 186 , 187 , 188 , 189 , 190 , 191 , 192 , 193 , 194 , 195 , 196 , 197 , 198 , 199 , 200 , 201 , 202 , 203 , 204 , 205 , 206 , 207 , 208 , 209 , 210 , 211 ].
Although this section has some overlap with others (as is to be expected because all of these determinants and body systems are interlinked), a number of studies have focused on the impact of stress on mental health. Stress has been mentioned in the literature as a risk factor of poor mental health and has emerged as an important determinant of depression. The effects of this variable are wide-ranging, and a short discussion is warranted.
Stress has been linked to the release of inflammatory factors, as well as the development of depression [ 204 ]. When the stress is high or lasts for a long period of time, this may negatively impact the brain. Chronic stress can impact the dendrites and synapses of various neurons, and may be implicated in the pathway leading to major depressive disorder [ 114 ]. As a review by Uchida et al. indicates, stress may be associated with the “dysregulation of neuronal and synaptic plasticity” [ 114 ]. Even in rodent studies, stress has a negative impact: chronic and unpredictable stress (and other forms of tension or stress) have been linked to unusual behaviour and depression symptoms [ 114 ].
The depression process and related brain changes, however, have also been linked to the hyperactivity or dysregulation of the HPA axis [ 127 , 130 , 131 , 182 , 212 ]. One review indicates that a potential underpinning mechanism of depression relates to “HPA axis abnormalities involved in chronic stress” [ 213 ]. There is a complex relationship between the HPA axis, glucocorticoid receptors, epigenetic mechanisms, and psychiatric sequelae [ 130 , 212 ].
In terms of the relationship between the HPA axis and stress and their influence on depression, the diathesis–stress model offers an explanation: it could be that early stress plays a role in the hyperactivation of the HPA axis, thus creating a predisposition “towards a maladaptive reaction to stress”. When this predisposition then meets an acute stressor, depression may ensue; thus, in line with the diathesis–stress model, a pre-existing vulnerability and stressor can create fertile ground for a mood disorder [ 213 ]. An integrated review by Dean and Keshavan [ 213 ] suggests that HPA axis hyperactivity is, in turn, related to other determinants, such as early deprivation and insecure early attachment; this again shows the complex web of causation between the different determinants.
3.1.6. Kynurenine Pathway
Studies on the kynurenine pathway—key points:
- The kynurenine pathway is linked to depression
- Indolamine 2,3-dioxegenase (IDO) polymorphisms are linked to postpartum depression
The kynurenine pathway was another theme that emerged in this review [ 120 , 178 , 181 , 184 , 214 , 215 , 216 , 217 , 218 , 219 , 220 , 221 ]. The kynurenine pathway has been implicated not only in general depressed mood (inflammation-induced depression) [ 184 , 214 , 219 ] but also postpartum depression [ 120 ]. When the kynurenine metabolism pathway is activated, this results in metabolites, which are neurotoxic.
A review by Jeon et al. notes a link between the impairment of the kynurenine pathway and inflammation-induced depression (triggered by treatment for various physical diseases, such as malignancy). The authors note that this could represent an important opportunity for immunopharmacology [ 214 ]. Another review by Danzer et al. suggests links between the inflammation-induced activation of indolamine 2,3-dioxegenase (the enzyme that converts tryptophan to kynurenine), the kynurenine metabolism pathway, and depression, and also remarks about the “opportunities for treatment of inflammation-induced depression” [ 184 ].
3.1.7. Cognition
Studies on cognition and the brain—key points:
- Cognitive decline and cognitive deficits are linked to increased depression risk
- Cognitive reserve is important in the disability/depression relationship
- Family history of cognitive impairment is linked to depression
A number of studies have focused on the theme of cognition and the brain. The results show that factors, such as low cognitive ability/function, cognitive vulnerability, cognitive impairment or deficits, subjective cognitive decline, regression of dendritic branching and hippocampal atrophy/death of hippocampal cells, impaired neuroplasticity, and neurogenesis-related aspects, have been linked to depression [ 131 , 212 , 222 , 223 , 224 , 225 , 226 , 227 , 228 , 229 , 230 , 231 , 232 , 233 , 234 , 235 , 236 , 237 , 238 , 239 ]. The cognitive reserve appears to act as a moderator and can magnify the impact of certain determinants on poor mental health. For example, in a study in which participants with multiple sclerosis also had low cognitive reserve, disability was shown to increase the risk for depression [ 63 ]. Cognitive deficits can be both causal and resultant in depression. A study on individuals attending outpatient stroke clinics showed that lower scores in cognition were related to depression; thus, cognitive impairment appears to be associated with depressive symptomatology [ 226 ]. Further, Halahakoon et al. [ 222 ] note a meta-analysis [ 240 ] that shows that a family history of cognitive impairment (in first degree relatives) is also linked to depression.
In addition to cognitive deficits, low-level cognitive ability [ 231 ] and cognitive vulnerability [ 232 ] have also been linked to depression. While cognitive impairment may be implicated in the pathogenesis of depressive symptoms [ 222 ], negative information processing biases are also important; according to the ‘cognitive neuropsychological’ model of depression, negative affective biases play a central part in the development of depression [ 222 , 241 ]. Nevertheless, the evidence on this topic is mixed and further work is needed to determine the underpinning mechanisms between these states.
3.2. Psychological Factors
Studies on psychological factors—key points:
- There are many affective risk factors linked to depression
- Determinants of depression include negative self-concept, sensitivity to rejection, neuroticism, rumination, negative emotionality, and others
A number of studies have been undertaken on the psychological factors linked to depression (including mastery, self-esteem, optimism, negative self-image, current or past mental health conditions, and various other aspects, including neuroticism, brooding, conflict, negative thinking, insight, cognitive fusion, emotional clarity, rumination, dysfunctional attitudes, interpretation bias, and attachment style) [ 66 , 128 , 140 , 205 , 210 , 228 , 235 , 242 , 243 , 244 , 245 , 246 , 247 , 248 , 249 , 250 , 251 , 252 , 253 , 254 , 255 , 256 , 257 , 258 , 259 , 260 , 261 , 262 , 263 , 264 , 265 , 266 , 267 , 268 , 269 , 270 , 271 , 272 , 273 , 274 , 275 , 276 , 277 , 278 , 279 , 280 , 281 , 282 , 283 , 284 , 285 , 286 , 287 , 288 , 289 , 290 ]. Determinants related to this condition include low self-esteem and shame, among other factors [ 269 , 270 , 275 , 278 ]. Several emotional states and traits, such as neuroticism [ 235 , 260 , 271 , 278 ], negative self-concept (with self-perceptions of worthlessness and uselessness), and negative interpretation or attention biases have been linked to depression [ 261 , 271 , 282 , 283 , 286 ]. Moreover, low emotional clarity has been associated with depression [ 267 ]. When it comes to the severity of the disorder, it appears that meta-emotions (“emotions that occur in response to other emotions (e.g., guilt about anger)” [ 268 ]) have a role to play in depression [ 268 ].
A determinant that has received much attention in mental health research concerns rumination. Rumination has been presented as a mediator but also as a risk factor for depression [ 57 , 210 , 259 ]. When studied as a risk factor, it appears that the relationship of rumination with depression is mediated by variables that include limited problem-solving ability and insufficient social support [ 259 ]. However, rumination also appears to act as a mediator: for example, this variable (particularly brooding rumination) lies on the causal pathway between poor attention control and depression [ 265 ]. This shows that determinants may present in several forms: as moderators or mediators, risk factors or outcomes, and this is why disentangling the relationships between the various factors linked to depression is a complex task.
The psychological determinants are commonly researched variables in the mental health literature. A wide range of factors have been linked to depression, such as the aforementioned determinants, but also: (low) optimism levels, maladaptive coping (such as avoidance), body image issues, and maladaptive perfectionism, among others [ 269 , 270 , 272 , 273 , 275 , 276 , 279 , 285 , 286 ]. Various mechanisms have been proposed to explain the way these determinants increase the risk for depression. One of the underpinning mechanisms linking the determinants and depression concerns coping. For example, positive fantasy engagement, cognitive biases, or personality dispositions may lead to emotion-focused coping, such as brooding, and subsequently increase the risk for depression [ 272 , 284 , 287 ]. Knowing the causal mechanisms linking the determinants to outcomes provides insight for the development of targeted interventions.
3.3. Social Determinants
Studies on social determinants—key points:
- Social determinants are the conditions in the environments where people are born, live, learn, work, play, etc.; these influence (mental) health [ 291 ]
- There are many social determinants linked to depression, such as sociodemographics, social support, adverse childhood experiences
- Determinants can be at the individual, social network, community, and societal levels
Studies also focused on the social determinants of (mental) health; these are the conditions in which people are born, live, learn, work, play, and age, and have a significant influence on wellbeing [ 291 ]. Factors such as age, social or socioeconomic status, social support, financial strain and deprivation, food insecurity, education, employment status, living arrangements, marital status, race, childhood conflict and bullying, violent crime exposure, abuse, discrimination, (self)-stigma, ethnicity and migrant status, working conditions, adverse or significant life events, illiteracy or health literacy, environmental events, job strain, and the built environment have been linked to depression, among others [ 52 , 133 , 235 , 236 , 239 , 252 , 269 , 280 , 292 , 293 , 294 , 295 , 296 , 297 , 298 , 299 , 300 , 301 , 302 , 303 , 304 , 305 , 306 , 307 , 308 , 309 , 310 , 311 , 312 , 313 , 314 , 315 , 316 , 317 , 318 , 319 , 320 , 321 , 322 , 323 , 324 , 325 , 326 , 327 , 328 , 329 , 330 , 331 , 332 , 333 , 334 , 335 , 336 , 337 , 338 , 339 , 340 , 341 , 342 , 343 , 344 , 345 , 346 , 347 , 348 , 349 , 350 , 351 , 352 , 353 , 354 , 355 , 356 , 357 , 358 , 359 , 360 , 361 , 362 , 363 , 364 , 365 , 366 , 367 , 368 , 369 , 370 , 371 ]. Social support and cohesion, as well as structural social capital, have also been identified as determinants [ 140 , 228 , 239 , 269 , 293 , 372 , 373 , 374 , 375 , 376 , 377 , 378 , 379 ]. In a study, part of the findings showed that low levels of education have been shown to be linked to post-stroke depression (but not severe or clinical depression outcomes) [ 299 ]. A study within a systematic review indicated that having only primary education was associated with a higher risk of depression compared to having secondary or higher education (although another study contrasted this finding) [ 296 ]. Various studies on socioeconomic status-related factors have been undertaken [ 239 , 297 ]; the research has shown that a low level of education is linked to depression [ 297 ]. Low income is also related to depressive disorders [ 312 ]. By contrast, high levels of education and income are protective [ 335 ].
A group of determinants touched upon by several studies included adverse childhood or early life experiences: ex. conflict with parents, early exposure to traumatic life events, bullying and childhood trauma were found to increase the risk of depression (ex. through pathways, such as inflammation, interaction effects, or cognitive biases) [ 161 , 182 , 258 , 358 , 362 , 380 ].
Gender-related factors were also found to play an important role with respect to mental health [ 235 , 381 , 382 , 383 , 384 , 385 ]. Gender inequalities can start early on in the lifecourse, and women were found to be twice as likely to have depression as men. Gender-related factors were linked to cognitive biases, resilience and vulnerabilities [ 362 , 384 ].
Determinants can impact mental health outcomes through underpinning mechanisms. For example, harmful determinants can influence the uptake of risk behaviours. Risk behaviours, such as sedentary behaviour, substance abuse and smoking/nicotine exposure, have been linked to depression [ 226 , 335 , 355 , 385 , 386 , 387 , 388 , 389 , 390 , 391 , 392 , 393 , 394 , 395 , 396 , 397 , 398 , 399 , 400 , 401 ]. Harmful determinants can also have an impact on diet. Indeed, dietary aspects and diet components (ex. vitamin D, folate, selenium intake, iron, vitamin B12, vitamin K, fiber intake, zinc) as well as diet-related inflammatory potential have been linked to depression outcomes [ 161 , 208 , 236 , 312 , 396 , 402 , 403 , 404 , 405 , 406 , 407 , 408 , 409 , 410 , 411 , 412 , 413 , 414 , 415 , 416 , 417 , 418 , 419 , 420 , 421 , 422 , 423 , 424 , 425 , 426 , 427 , 428 ]. A poor diet has been linked to depression through mechanisms such as inflammation [ 428 ].
Again, it is difficult to constrict diet to the ‘social determinants of health’ category as it also relates to inflammation (biological determinants) and could even stand alone as its own category. Nevertheless, all of these factors are interlinked and influence one another in a complex web of causation, as mentioned elsewhere in the paper.
Supplementary Figure S1 contains a representation of key determinants acting at various levels: the individual, social network, community, and societal levels. The determinants have an influence on risk behaviours, and this, in turn, can affect the mood (i.e., depression), body processes (ex. can increase inflammation), and may negatively influence brain structure and function.
3.4. Others
Studies on ‘other’ determinants—key points:
- A number of factors are related to depression
- These may not be as easily categorized as the other determinants in this paper
A number of factors arose in this review that were related to depression; it was difficult to place these under a specific heading above, so this ‘other’ category was created. A number of these could be sorted under the ‘social determinants of depression’ category. For example, being exposed to deprivation, hardship, or adversity may increase the risk for air pollution exposure and nighttime shift work, among others, and the latter determinants have been found to increase the risk for depression. Air pollution could also be regarded as an ecologic-level (environmental) determinant of mental health.
Nevertheless, we have decided to leave these factors in a separate category (because their categorization may not be as immediately clear-cut as others), and these factors include: low-level light [ 429 ], weight cycling [ 430 ], water contaminants [ 431 ], trade [ 432 ], air pollution [ 433 , 434 ], program-level variables (ex. feedback and learning experience) [ 435 ], TV viewing [ 436 ], falls [ 437 ], various other biological factors [ 116 , 136 , 141 , 151 , 164 , 182 , 363 , 364 , 438 , 439 , 440 , 441 , 442 , 443 , 444 , 445 , 446 , 447 , 448 , 449 , 450 , 451 , 452 , 453 , 454 , 455 , 456 , 457 , 458 , 459 , 460 , 461 , 462 , 463 , 464 , 465 , 466 , 467 , 468 , 469 ], mobile phone use [ 470 ], ultrasound chronic exposure [ 471 ], nighttime shift work [ 472 ], work accidents [ 473 ], therapy enrollment [ 226 ], and exposure to light at night [ 474 ].
4. Cross-Cutting Themes
4.1. lifecourse perspective.
Studies on the lifecourse perspective—key points:
- Early life has an importance on mental health
- Stress has been linked to depression
- In old age, the decline in social capital is important
Trajectories and life events are important when it comes to the lifecourse perspective. Research has touched on the influence of prenatal or early life stress on an individual’s mental health trajectory [ 164 , 199 , 475 ]. Severe stress that occurs in the form of early-life trauma has also been associated with depressive symptoms [ 362 , 380 ]. It may be that some individuals exposed to trauma develop thoughts of personal failure, which then serve as a catalyst of depression [ 380 ].
At the other end of the life trajectory—old age—specific determinants have been linked to an increased risk for depression. Older people are at a heightened risk of losing their social networks, and structural social capital has been identified as important in relation to depression in old age [ 293 ].
4.2. Gene–Environment Interactions
Studies on gene–environment interactions—key points:
- The environment and genetics interact to increase the risk of depression
- The etiology of depression is multifactorial
- Adolescence is a time of vulnerability
A number of studies have touched on gene–environment interactions [ 72 , 77 , 82 , 119 , 381 , 476 , 477 , 478 , 479 , 480 , 481 ]. The interactions between genetic factors and determinants, such as negative life events (ex. relationship and social difficulties, serious illness, unemployment and financial crises) and stressors (ex. death of spouse, minor violations of law, neighbourhood socioeconomic status) have been studied in relation to depression [ 82 , 135 , 298 , 449 , 481 ]. A study reported an interaction of significant life events with functional variation in the serotonin-transporter-linked polymorphic region (5-HTTLPR) allele type (in the context of multiple sclerosis) and linked this to depression [ 361 ], while another reported an interaction between stress and 5-HTTLPR in relation to depression [ 480 ]. Other research reported that the genetic variation of HPA-axis genes has moderating effects on the relationship between stressors and depression [ 198 ]. Another study showed that early-life stress interacts with gene variants to increase the risk for depression [ 77 ].
Adolescence is a time of vulnerability [ 111 , 480 ]. Perceived parental support has been found to interact with genes (GABRR1, GABRR2), and this appears to be associated with depressive symptoms in adolescence [ 480 ]. It is important to pay special attention to critical periods in the lifecourse so that adequate support is provided to those who are most vulnerable.
The etiology of depression is multifactorial, and it is worthwhile to examine the interaction between multiple factors, such as epigenetic, genetic, and environmental factors, in order to truly understand this mental health condition. Finally, taking into account critical periods of life when assessing gene–environment interactions is important for developing targeted interventions.
5. Discussion
Depression is one of the most common mental health conditions, and, if left untreated, it can increase the risk for substance abuse, anxiety disorders, and suicide. In the past 20 years, a large number of studies on the risk and protective factors of depression have been undertaken in various fields, such as genetics, neurology, immunology, and epidemiology. However, there are limitations associated with the extant evidence base. The previous syntheses on depression are limited in scope and focus exclusively on social or biological factors, population sub-groups, or examine depression as a comorbidity (rather than an independent disorder). The research on the determinants and causal pathways of depression is fragmentated and heterogeneous, and this has not helped to stimulate progress when it comes to the prevention and intervention of this condition—specifically unravelling the complexity of the determinants related to this condition and thus refining the prevention and intervention methods.
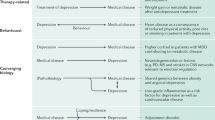
The scope of this paper was to bring together the heterogeneous, vast, and fragmented literature on depression and paint a picture of the key factors that contribute to this condition. The findings from this review show that there are important themes when it comes to the determinants of depression, such as: the microbiome, dysregulation of the HPA axis, inflammatory reactions, the kynurenine pathway, as well as psychological and social factors. It may be that physical factors are proximal determinants of depression, which, in turn, are acted on by more distal social factors, such as deprivation, environmental events, and social capital.
The Marmot Report [ 291 ], the World Health Organization [ 482 ], and Compton et al. [ 483 ] highlight that the most disadvantaged segments of society are suffering (the socioeconomic context is important), and this inequality in resources has translated to inequality in mental health outcomes [ 483 ]. To tackle the issue of egalitarianism and restore equality in the health between the groups, the social determinants need to be addressed [ 483 ]. A wide range of determinants of mental health have been identified in the literature: age, gender, ethnicity, family upbringing and early attachment patterns, social support, access to food, water and proper nutrition, and community factors. People spiral downwards because of individual- and societal-level circumstances; therefore, these circumstances along with the interactions between the determinants need to be considered.
Another important theme in the mental health literature is the lifecourse perspective. This shows that the timing of events has significance when it comes to mental health. Early life is a critical period during the lifespan at which cognitive processes develop. Exposure to harmful determinants, such as stress, during this period can place an individual on a trajectory of depression in adulthood or later life. When an individual is exposed to harmful determinants during critical periods and is also genetically predisposed to depression, the risk for the disorder can be compounded. This is why aspects such as the lifecourse perspective and gene–environment interactions need to be taken into account. Insight into this can also help to refine targeted interventions.
A number of interventions for depression have been developed or recommended, addressing, for example, the physical factors described here and lifestyle modifications. Interventions targeting various factors, such as education and socioeconomic status, are needed to help prevent and reduce the burden of depression. Further research on the efficacy of various interventions is needed. Additional studies are also needed on each of the themes described in this paper, for example: the biological factors related to postpartum depression [ 134 ], and further work is needed on depression outcomes, such as chronic, recurrent depression [ 452 ]. Previous literature has shown that chronic stress (associated with depression) is also linked to glucocorticoid receptor resistance, as well as problems with the regulation of the inflammatory response [ 484 ]. Further work is needed on this and the underpinning mechanisms between the determinants and outcomes. This review highlighted the myriad ways of measuring depression and its determinants [ 66 , 85 , 281 , 298 , 451 , 485 ]. Thus, the standardization of the measurements of the outcomes (ex. a gold standard for measuring depression) and determinants is essential; this can facilitate comparisons of findings across studies.
5.1. Strengths
This paper has important strengths. It brings together the wide literature on depression and helps to bridge disciplines in relation to one of the most common mental health problems. We identified, selected, and extracted data from studies, and provided concise summaries.
5.2. Limitations
The limitations of the review include missing potentially important studies; however, this is a weakness that cannot be avoided by literature reviews. Nevertheless, the aim of the review was not to identify each study that has been conducted on the risk and protective factors of depression (which a single review is unable to capture) but rather to gain insight into the breadth of literature on this topic, highlight key biological, psychological, and social determinants, and shed light on important themes, such as the lifecourse perspective and gene–environment interactions.
6. Conclusions
We have reviewed the determinants of depression and recognize that there are a multitude of risk and protective factors at the individual and wider ecologic levels. These determinants are interlinked and influence one another. We have attempted to describe the wide literature on this topic, and we have brought to light major factors that are of public mental health significance. This review may be used as an evidence base by those in public health, clinical practice, and research.
This paper discusses key areas in depression research; however, an exhaustive discussion of all the risk factors and determinants linked to depression and their mechanisms is not possible in one journal article—which, by its very nature, a single paper cannot do. We have brought to light overarching factors linked to depression and a workable conceptual framework that may guide clinical and public health practice; however, we encourage other researchers to continue to expand on this timely and relevant work—particularly as depression is a top priority on the policy agenda now.
Acknowledgments
Thank you to Isla Kuhn for the help with the Medline, Scopus, and PsycInfo database searches.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/brainsci11121633/s1 , Figure S1: Conceptual framework: Determinants of depression, Table S1: Data charting—A selection of determinants from the literature.
Appendix A.1. Search Strategy
Search: ((((((((((((((((“Gene-Environment Interaction”[Majr]) OR (“Genetics”[Mesh])) OR (“Genome-Wide Association Study”[Majr])) OR (“Microbiota”[Mesh] OR “Gastrointestinal Microbiome”[Mesh])) OR (“Neurogenic Inflammation”[Mesh])) OR (“genetic determinant”)) OR (“gut-brain-axis”)) OR (“Kynurenine”[Majr])) OR (“Cognition”[Mesh])) OR (“Neuronal Plasticity”[Majr])) OR (“Neurogenesis”[Mesh])) OR (“Genes”[Mesh])) OR (“Neurology”[Majr])) OR (“Social Determinants of Health”[Majr])) OR (“Glucocorticoids”[Mesh])) OR (“Tryptophan”[Mesh])) AND (“Depression”[Mesh] OR “Depressive Disorder”[Mesh]) Filters: from 2017—2020.
Ovid MEDLINE(R) and Epub Ahead of Print, In-Process, In-Data-Review & Other Non-Indexed Citations, Daily and Versions(R)
- exp *Depression/
- exp *Depressive Disorder/
- exp *”Social Determinants of Health”/
- exp *Tryptophan/
- exp *Glucocorticoids/
- exp *Neurology/
- exp *Genes/
- exp *Neurogenesis/
- exp *Neuronal Plasticity/
- exp *Kynurenine/
- exp *Genetics/
- exp *Neurogenic Inflammation/
- exp *Gastrointestinal Microbiome/
- exp *Genome-Wide Association Study/
- exp *Gene-Environment Interaction/
- exp *Depression/et [Etiology]
- exp *Depressive Disorder/et
- or/4-16 637368
- limit 22 to yr = “2017–Current”
- “cause* of depression”.mp.
- “cause* of depression”.ti.
- (cause adj3 (depression or depressive)).ti.
- (caus* adj3 (depression or depressive)).ti.
Appendix A.2. PsycInfo
(TITLE ( depression OR “ Depressive Disorder ”) AND TITLE (“ Social Determinants of Health ” OR tryptophan OR glucocorticoids OR neurology OR genes OR neurogenesis OR “ Neuronal Plasticity ” OR kynurenine OR genetics OR “ Neurogenic Inflammation ” OR “ Gastrointestinal Microbiome ” OR “ Genome-Wide Association Study ” OR “ Gene-Environment Interaction ” OR aetiology OR etiology )) OR TITLE ( cause* W/3 ( depression OR depressive )).
Author Contributions
O.R. was responsible for the design of the study and methodology undertaken. Despite P.T.’s involvement in YPMH, he had no role in the design of the study; P.T. was responsible for the conceptualization of the study. Validation was conducted by O.R. and J.F.M. Formal analysis (data charting) was undertaken by O.R. O.R. and P.T. were involved in the investigation, resource acquisition, and data presentation. The original draft preparation was undertaken by O.R. The writing was conducted by O.R., with review and editing by P.T. and J.F.M. Funding acquisition was undertaken by O.R. and P.T. All authors have read and agreed to the published version of the manuscript.
This research was funded by The William Templeton Foundation for Young People’s Mental Health, Cambridge Philosophical Society, and the Aviva Foundation.
Conflicts of Interest
The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
7 Depression Research Paper Topic Ideas
Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
In psychology classes, it's common for students to write a depression research paper. Researching depression may be beneficial if you have a personal interest in this topic and want to learn more, or if you're simply passionate about this mental health issue. However, since depression is a very complex subject, it offers many possible topics to focus on, which may leave you wondering where to begin.
If this is how you feel, here are a few research titles about depression to help inspire your topic choice. You can use these suggestions as actual research titles about depression, or you can use them to lead you to other more in-depth topics that you can look into further for your depression research paper.
What Is Depression?
Everyone experiences times when they feel a little bit blue or sad. This is a normal part of being human. Depression, however, is a medical condition that is quite different from everyday moodiness.
Your depression research paper may explore the basics, or it might delve deeper into the definition of clinical depression or the difference between clinical depression and sadness .
What Research Says About the Psychology of Depression
Studies suggest that there are biological, psychological, and social aspects to depression, giving you many different areas to consider for your research title about depression.
Types of Depression
There are several different types of depression that are dependent on how an individual's depression symptoms manifest themselves. Depression symptoms may vary in severity or in what is causing them. For instance, major depressive disorder (MDD) may have no identifiable cause, while postpartum depression is typically linked to pregnancy and childbirth.
Depressive symptoms may also be part of an illness called bipolar disorder. This includes fluctuations between depressive episodes and a state of extreme elation called mania. Bipolar disorder is a topic that offers many research opportunities, from its definition and its causes to associated risks, symptoms, and treatment.
Causes of Depression
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic.
For instance, how does an imbalance in brain chemistry or poor nutrition relate to depression? Is there a relationship between the stressful, busier lives of today's society and the rise of depression? How can grief or a major medical condition lead to overwhelming sadness and depression?
Who Is at Risk for Depression?
This is a good research question about depression as certain risk factors may make a person more prone to developing this mental health condition, such as a family history of depression, adverse childhood experiences, stress , illness, and gender . This is not a complete list of all risk factors, however, it's a good place to start.
The growing rate of depression in children, teenagers, and young adults is an interesting subtopic you can focus on as well. Whether you dive into the reasons behind the increase in rates of depression or discuss the treatment options that are safe for young people, there is a lot of research available in this area and many unanswered questions to consider.
Depression Signs and Symptoms
The signs of depression are those outward manifestations of the illness that a doctor can observe when they examine a patient. For example, a lack of emotional responsiveness is a visible sign. On the other hand, symptoms are subjective things about the illness that only the patient can observe, such as feelings of guilt or sadness.
An illness such as depression is often invisible to the outside observer. That is why it is very important for patients to make an accurate accounting of all of their symptoms so their doctor can diagnose them properly. In your depression research paper, you may explore these "invisible" symptoms of depression in adults or explore how depression symptoms can be different in children .
How Is Depression Diagnosed?
This is another good depression research topic because, in some ways, the diagnosis of depression is more of an art than a science. Doctors must generally rely upon the patient's set of symptoms and what they can observe about them during their examination to make a diagnosis.
While there are certain laboratory tests that can be performed to rule out other medical illnesses as a cause of depression, there is not yet a definitive test for depression itself.
If you'd like to pursue this topic, you may want to start with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The fifth edition, known as DSM-5, offers a very detailed explanation that guides doctors to a diagnosis. You can also compare the current model of diagnosing depression to historical methods of diagnosis—how have these updates improved the way depression is treated?
Treatment Options for Depression
The first choice for depression treatment is generally an antidepressant medication. Selective serotonin reuptake inhibitors (SSRIs) are the most popular choice because they can be quite effective and tend to have fewer side effects than other types of antidepressants.
Psychotherapy, or talk therapy, is another effective and common choice. It is especially efficacious when combined with antidepressant therapy. Certain other treatments, such as electroconvulsive therapy (ECT) or vagus nerve stimulation (VNS), are most commonly used for patients who do not respond to more common forms of treatment.
Focusing on one of these treatments is an option for your depression research paper. Comparing and contrasting several different types of treatment can also make a good research title about depression.
A Word From Verywell
The topic of depression really can take you down many different roads. When making your final decision on which to pursue in your depression research paper, it's often helpful to start by listing a few areas that pique your interest.
From there, consider doing a little preliminary research. You may come across something that grabs your attention like a new study, a controversial topic you didn't know about, or something that hits a personal note. This will help you narrow your focus, giving you your final research title about depression.
Remes O, Mendes JF, Templeton P. Biological, psychological, and social determinants of depression: A review of recent literature . Brain Sci . 2021;11(12):1633. doi:10.3390/brainsci11121633
National Institute of Mental Health. Depression .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition . American Psychiatric Association.
National Institute of Mental Health. Mental health medications .
Ferri, F. F. (2019). Ferri's Clinical Advisor 2020 E-Book: 5 Books in 1 . Netherlands: Elsevier Health Sciences.
By Nancy Schimelpfening Nancy Schimelpfening, MS is the administrator for the non-profit depression support group Depression Sanctuary. Nancy has a lifetime of experience with depression, experiencing firsthand how devastating this illness can be.
Clinical Trials
Teen depression.
Displaying 12 studies
The purpose of this study is to gather information regarding the use of rTMS as a treatment for depression in adolescents with Major Depressive Disorder. The investigators also hope to learn if measures of brain activity (cortical excitability and inhibition) collected with transcranial magnetic stimulation (TMS) can be used to identify which patients will benefit from certain types of rTMS treatment.
This research proposal aims to better understand the neurobiology of depression in adolescents and how repetitive transcranial magnetic stimulation (rTMS) may therapeutically impact brain function and mood. This investigation also proposes the first study to examine the efficacy of rTMS maintenance therapy in adolescents who have met clinical criteria following acute rTMS treatment. The magnetic resonance (MR) spectroscopy pattern of rTMS response will be analyzed according to previously established protocols.
The overall goal of this investigator-initiated trial is to evaluate the impact of platform algorithm products designed to rapidly identify pharmacokinetic (PK) and/or pharmacodynamic (PD) genomic variation on treatment outcome of depression in adolescents. This new technology may have the potential to optimize treatment selection by improving response, minimizing unfavorable adverse events / side effects and increasing treatment adherence
This research study aims to test the safety and effectiveness of repetitive transcranial magnetic stimulation (rTMS) on teens with depression. The study also seeks to understand how rTMS treatment affects the neurobiology of teens with depression.
The purpose of this study is to learn if measures of brain chemicals from a brain scan called Magnetic Resonance Imaging and Spectroscopy (MRI/MRS) and brain activity (known as cortical excitability and inhibition) collected by Transcranial Magnetic Stimulation (TMS) are different in adolescents with depression who are in different stages of treatment. Researchers are conducting this study to learn more about how the brain works in adolescents with depression and without depression (healthy controls). This is important because it may identify a biological marker (a measure of how bad an illness is) for depression that could one day be used ...
The purpose of this study is to contribute to our understanding of the relationships between social media use in adolescents and psychological development, psychiatric comorbidity, and physiological markers of stress.
The proposed study seeks to obtain preliminary signal of the tolerability and efficacy of transcranial direct current stimulation (tDCS) for depressive symptoms in a sample of adolescents with depression and epilepsy. Additionally, effects of tDCS will be assessed via electroencephalographic, cognitive, and psychosocial measures.
In an effort to understand the effects of evidence-based interventions on children and adolescents, the aims of this study are to 1) evaluate the feasibility of utilizing wearable devices to track health information (i.e., sleep, physical activity); 2) evaluate the effectiveness of evidence-based intervention components on emotional and interpersonal functioning, family engagement, and sleep and physical activity level outcomes.
The purpose of this study is to:
- Increase screening of adolescents for symptoms of depression in primary care La Crosse, WI clinics using the PHQ9M screening tool.Screening to occur at all well child visits and all subsequent visits for adolescents with Depression on their problem list.Clinics to include Pediatrics, Family Medicine, Family Health, Center for Womens Health.
- Develop a clear care pathway for adolescents identified with clinically meaningful symptoms of depression through increased screening, referral and treatment options. Pathway may include psychoeducational materials (multimedia options), intake paperwork and process for Department of Behavioral Health locally, and ...
The purpose of this study is to study brain chemistry in depressed patients compared to healthy patients who are not depressed.
The proposed study will examine sequential bilateral accelerated theta burst stimulation (aTBS). Three sessions are administered daily for 10 days (5 days per week). During each session continuous theta burst stimulation (cTBS) in which 1800 pulses are delivered continuously over 120 seconds to the right dorsolateral prefrontal cortex (RDPFC) is administered first, followed by iTBS in which 1800 pulses are delivered in 2 second bursts, repeated every 10 seconds for 570 seconds (1800 pulses) to the left dorsolateral prefrontal cortex (LDPFC). The theta burst stimulation (TBS) parameters were adopted from prior work, with 3-pulse 50 Hz bursts given ...
The purpose of this study is to see if there is a connection between bad experiences in the patient's childhood, either by the patient or the parent, and poor blood sugar control, obesity, poor blood lipid levels, and depression in patients with type 1 diabetes.
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 24 May 2024
Assessment of depression symptoms among cancer patients: a cross-sectional study from a developing country
- Maher Battat 1 ,
- Nawal Omair 2 ,
- Mohammad A. WildAli 2 ,
- Aidah Alkaissi 3 ,
- Riad Amer 2 , 4 ,
- Amer A. Koni 5 , 6 ,
- Husam T. Salameh 2 , 4 &
- Sa’ed H. Zyoud 6 , 7 , 8
Scientific Reports volume 14 , Article number: 11934 ( 2024 ) Cite this article
197 Accesses
Metrics details
- Health care
Cancer patients experience psychological symptoms such as depression during the cancer treatment period, which increases the burden of symptoms. Depression severity can be assessed using the beck depression inventory (BDI II). The purpose of the study was to use BDI-II scores to measure depression symptoms in cancer patients at a large tertiary hospital in Palestine. A convenience sample of 271 cancer patients was used for a cross-sectional survey. There are descriptions of demographic, clinical, and lifestyle aspects. In addition, the BDI-II is a tool for determining the severity of depression. Two hundred seventy-one patients participated in the survey, for a 95% response rate. Patients ranged in age from 18 to 84 years, with an average age of 47 years. The male-to-female ratio was approximately 1:1, and 59.4% of the patients were outpatients, 153 (56.5%) of whom had hematologic malignancies. Most cancer patients ( n = 104, 38.4%) had minimal depression, while 22.5%, 22.1%, and 17.0% had mild, moderate, and severe depression, respectively. Education level, economic status, smoking status, and age were significantly associated with depression. The BDI-II is a useful instrument for monitoring depressive symptoms. The findings support the practice of routinely testing cancer patients for depressive symptoms as part of standard care and referring patients who are at a higher risk of developing psychological morbidity to specialists for treatment as needed.
Similar content being viewed by others

Association of pre-existing depression with all-cause, cancer-related, and noncancer-related mortality among 5-year cancer survivors: a population-based cohort study
Depression and anxiety in relation to cancer incidence and mortality: a systematic review and meta-analysis of cohort studies
Comorbid depression in medical diseases
Introduction.
Cancer is the second leading cause of mortality both worldwide and in Palestine, accounting for 14% of all deaths, after heart disease (30%) 1 , 2 . Additionally, the anticipated rise in cancer diagnoses among Palestinians is likely to place added strain on the already stretched financial and infrastructural resources of the healthcare system, particularly given the prevailing financial and political uncertainties 2 , 3 , 4 , 5 . As advancements in cancer treatments progress, more patients are experiencing either complete cures or extended life expectancies. As a result, there is increased focus on the emotional challenges that come with being diagnosed with and treated for cancer. Research indicates that approximately 30% of patients experience mental health issues such as anxiety, depression, and adjustment disorders 6 , although the exact prevalence varies depending on the specific condition 7 . Treating depression can lead to better emotional and psychological health, even amidst the physical toll of cancer symptoms. Mood plays a significant role in how patients perceive their quality of life (QoL) and the extent of their suffering. It can begin at the time of diagnosis and continue beyond the completion of cancer treatment 8 .
Depression is associated with decreased functional status, decreased adherence to treatment, longer hospitalizations, and the desire to die sooner 9 . Almost 25% of cancer patients experience severe depressive symptoms, whereas 77% of those with advanced disease experience severe depressive symptoms 10 . Depression is common in cancer patients and is strongly associated with oropharyngeal (22–57%), pancreatic (33 to 50%), breast (1.5–46%), and lung (11 to 44%) cancer. Patients with other malignancies, such as colon (13–25%), gynecological (12–23%), and lymphoma (8–19%), had a lower frequency of depression 7 .
Depressive symptoms are often identical to those of physical illness or its treatments, making it difficult to diagnose depression in physically ill people. This is especially true when a cancer patient is diagnosed with depression. Many of the symptoms needed to diagnose depression are often caused by cancer treatments (e.g. chemotherapy, biological therapy), such as fatigue, weight loss, anhedonia (the inability to feel pleasure in typically enjoyable activities) and psychomotor retardation.
Depression, also known as clinical depression or severe depressive disorder, is a prevalent yet serious mood disorder. It manifests as severe symptoms that impact a person's emotions, thoughts, and ability to cope with daily activities such as sleeping, eating, and working. These symptoms must persist for at least two weeks to be diagnosed 7 .
Various techniques have been created to evaluate how well symptoms are managed, aiding in the recognition of linked symptoms. For instance, the beck depression inventory (BDI II)-21 is capable of evaluating prevalent psychological symptoms among cancer patients. The BDI-II remains instrumental in exploring the characteristics and evaluation of depression. Its effectiveness as a screening tool in patients with medical conditions and cancer has been examined in multiple research studies, establishing it as a reliable self-reported assessment tool 11 .
Cancer patients suffer many symptoms during cancer progression that negatively affect their QoL. Importantly, there is no comforting care assessment tool, such as the BDI, available for cancer patients in Palestine. Therefore, the purpose of this study was to evaluate cancer patients’ reported depression symptoms using the beck depression scale (BDS) at a large tertiary care hospital. However, to our knowledge, this is the first study assessing depression using the BDI-II in occupied Palestinian territories in the context of mental health.
Study design
The research objectives were pursued through a quantitative cross-sectional investigation.
Study setting
An-Najah National University Hospital (NNUH) was established in 2013 through a partnership with the Faculty of Medicine and Health Sciences. NNUH stands as Palestine's sole facility, offering sophisticated electrophysiology, intricate open-heart surgeries, autologous bone marrow transplants, and specialized care for both adult and pediatric leukemia patients. NNUH encompasses various medical units, an emergency ward, dialysis facilities, radiology services, and ultrasound and tomography departments and has a capacity of 120 beds 12 .
Study population
Cancer patients receive comprehensive care through outpatient oncology clinics and inpatient services at NNUH. These services cover various procedures, including diagnosis, chemotherapy, autologous bone marrow transplantation (autoBMT), and the management of treatment side effects or complications. In certain oncological scenarios, such as neutropenic fever, patients may require immediate attention, leading to visits to the emergency room followed by hospital admission. This integrated approach ensures that patients receive comprehensive and timely care for their cancer treatment needs at NNUH.
Sample size
During the research period spanning from April 2021 to August 2021, the NNUH received an average of 600 cancer patients each month. This number served as the basis for determining the necessary sample size for analysis. Using the Raosoft sample size calculator with a response distribution of 0.50, an error margin of 5%, and a confidence interval of 95%, a preliminary sample size of 235 was calculated. However, to accommodate potential dropout rates, this figure was adjusted, indicating a requirement of 259 patients. To bolster the study's robustness and mitigate the risk of erroneous results, an additional 10% of the sample (24 patients) was included, bringing the final targeted sample size to 285. The validity and reliability of the questionnaire were evaluated through content validity, construct validity, and reliability testing methods. Hence, we only used triangulation, involving two hemato-oncology physicians, three oncology nurses, and one statistician, to verify the validity of the data. We also assessed the consistency of 11 patients (22 questionnaires) between their two visits. Moreover, after creating the questionnaire, we piloted it on 11 patients, making adjustments as necessary based on their feedback.
Sampling procedure
The researchers utilized convenience sampling, involving 271 cancer patients.
Inclusion and exclusion criteria
Inclusion criteria.
Ensuring that patients agree to participate is vital for ethical research.
The ability to read and write at age 18 ensures that patients can understand the study information and provide feedback.
Specifying cancer and hematologic malignancies keeps the study focused on the relevant patient population. Both inpatients and outpatients are included to capture a broader range of experiences.
Exclusion criteria
Patients in the ICU may be too critically ill to participate effectively.
Patients in a coma were unable to consent or participate in the study.
Patients with preexisting cognitive issues may not be able to understand or participate in the study reliably.
Isolated patients may have difficulty communicating or require special protocols that the study may not be equipped for.
Data collection instrument
Patients completed the questionnaires themselves, and nurses explained the questions if patients requested further clarification. All surveys were performed on paper and then analyzed using an electronic database. This study involved a secondary analysis of previously published data using various approaches in another study on factors related to palliative care symptoms in cancer patients in Palestine 13 . The data included patient demographics and clinical characteristics collected at various points during cancer treatment, such as diagnosis, chemotherapy, clinic visits, AutoBMT, advanced cancer stages, outpatient and inpatient oncology visits, and related factors. The data were collected over 5 months, from April to August 2021. Patients were provided with the Arabic version of the BDI-II 14 by either the researcher or a designated nurse and were encouraged to fill it out themselves, with assistance available if needed.
The surveys were kept in a designated location within particular departments designed for adult patients with cancer. These departments included outpatient oncology clinics, medical oncology units, vascular units, surgical units, bone marrow transplant and leukemia units, and surgical cardiac care units. Furthermore, the researcher gathered additional medical data from the patients' records. Approximately 15 patients chose not to participate, and 10 surveys were unfinished. Assessment tools for psychological symptoms, such as the BDI-II, provide a baseline assessment and evaluation for depression in cancer patients.
Beck depression inventory (BDI) II
Many factors contribute to the variation in depression incidence, including patient age and sex, medical status, cancer diagnosis, and cancer stage 15 . Hence, these inquiries also aid in evaluating depression among individuals with cancer. Moreover, questions regarding the diagnostic approach (such as inclusion or substitution methods), the type of assessment utilized (including diagnostic interviews or self-reported measures), and the criteria for inclusion (whether clinical or subclinical) are crucial for assessing depression within this demographic group.
The BDI, short for Beck Depression Inventory, is a tool consisting of 21-point self-assessment ratings designed to gauge attitudes and symptoms of depression. Completing the BDI typically takes approximately 10 min, yet individuals are required to possess a reading level equivalent to fifth or sixth grade to comprehend the questionnaire adequately. Clinicians employ this inventory to ascertain the severity of depression in individuals and tailor appropriate therapeutic interventions. The BDI was developed by Aaron T. Beck, a prominent psychiatrist recognized as the pioneer of cognitive behavior therapy 16 .
Depression is a medical condition characterized by a prolonged feeling of sadness. This leads to a lack of interest in previously enjoyable activities and can greatly disrupt daily life. While experiencing sadness is normal in response to events such as the loss of a loved one, financial strain, relationship issues, or job loss, clinical depression occurs when these feelings persist for an extended period without an obvious cause 16 .
Questions on the BDI-II
The BDI-II comprises 21 inquiries aligned with the diagnostic criteria outlined in the DSM-V, which professionals use to assess mental health conditions. Each question offers multiple-choice responses with scores ranging from 0 to 3. These questions address various aspects, such as feelings of sadness, pessimism, past failures, loss of pleasure, guilt, self-criticism, suicidal thoughts, agitation, changes in sleeping and eating patterns, concentration difficulties, fatigue, and diminished interest in activities once enjoyed.
Scores on the BDI-II
The Beck Depression Inventory (BDI) utilizes a straightforward scoring method in which each of the four multiple-choice options is given a score ranging from 0 to 3. After all 21 questions are answered, the total points are tallied. Based on the total score, the severity of depression was categorized as follows: no depression (0–13 points), mild depression (14–19 points), moderate depression (20–28 points), or severe depression (29–63 points) 16 .
Statistical analysis
The data were analyzed using the Social Sciences Statistical Package (SPSS) version 21. Basic demographic data were summarized using descriptive statistics. When comparing continuous variables provided as the median and interquartile range, Mann‒Whitney U /Kruskal‒Wallis tests were used. P values less than 0.05 were considered to indicate statistical significance.
Ethics approval and consent to participate
The Institutional Review Board (IRB) of An-Najah National University and the NNUH administrator approved this study. All methods used in the study were conducted in accordance with relevant guidelines and regulations, including the Helsinki Declaration. Participants signed an informed consent form guaranteeing data privacy, and all the data were kept confidential and used exclusively for research purposes.
Demographic data
The study included 271 participants, for a response rate of 95%. Table 1 shows the distribution of cancer types among our sample. Among them, 52% were younger than 50 years, and the majority (67.9%, n = 184) were married. The average age was 47.17 years, ranging from 18 to 84 years. The gender distribution was nearly equal, with 51.3% men and 48.7% women. In terms of education, the majority (67.5%, n = 183) had completed high school, while 32.5% (n = 88) had completed university or college. Regarding socioeconomic status, 53.9% had a low income (< 2000 NIS), 38.4% had a middle income (2000–5000 NIS), and only 7.7% had a high income (> 5000 NIS).
Among all participants, 22.1% were smokers, 4.8% had deformities such as Tal Hashomer syndrome, 36.5% were employed, 47.6% lived in villages, and 41.0% resided in cities. Furthermore, 59.4% were outpatients, and 56.5% were diagnosed with hematologic malignancies. Notably, the majority of cancer patients (88.9%, n = 241) were receiving treatment, with 75.6% actively receiving chemotherapy. Family psychological support was the most common form of support (59.8%), followed by support from healthcare teams (44.3%), religious support (38.0%), and social support (34.3%) (see Table 2 ).
The severity among cancer patients according to the BDI-II
The majority of cancer patients (38.4%) had minimal depression, while 22.5%, 22.1%, and 17.0% had mild, moderate, or severe depression, respectively (see Table 3 ). However, the median BDI score [Q1-Q3] was 17.0 [10.0–24.0], and the mean ± SD was 18.2 ± 11.0.
The associations between patient characteristics and depression are shown in Table 2 . The results showed that cancer patients over 50 years of age had significantly more depression than those younger than 50 years of age did ( p = 0.024), and the median BDI score was 18.5 [11.0–25.0] for the > 50 years age group and 15.0 [9.0–24.0] for the > 50 years age group. A significant difference was also found in the categories of educational level ( p < 0.001), where cancer patients with low educational levels had higher depression scores than those with higher educational levels (university or college). Furthermore, poor socioeconomic status was significantly associated with increased depression intensity. The current study showed that smokers had moderate depression, as indicated by a BDI-II score of 20.0 [13.0–29.0], while nonsmokers had mild depression, with a BDI-II score of 16.0 [10.0–24.0]. This difference was significant (p = 0.004). Other factors, such as sex, social status, type of cancer, hospitalization status, and psychological support, were not significantly associated with the BDI-II score.
Cancer patients receiving treatment at NNUH visit outpatient oncology clinics or are admitted as inpatients for various purposes, including diagnosis, chemotherapy sessions, autologous bone marrow transplants, and managing side effects or complications of treatment. These services cater to patients with solid tumors and hematologic malignancies such as leukemia, lymphomas, and multiple myeloma. Some oncological conditions, such as neutropenic fever, require referral to the emergency room followed by admission to the hospital.
In our research group, we observed an equal distribution between males and females, approximately 1:1, mirroring the broader pattern of cancer cases in Palestine. According to data from the Palestinian Ministry of Health in 2020 17 , nearly half of all cancer patients were male (49.3%), with slightly more females (50.7%). Conversely, a study conducted in Italy demonstrated a greater proportion of female participants, accounting for 58% of the sample 18 .
In our research, the average age of the individuals involved was 47 years, whereas in previous studies, the average ages ranged from 49.12 years 19 to 61.9 years 18 . In our study, 88.9% of the individuals diagnosed with cancer received treatment, while the remainder were in the diagnostic phase. This proportion closely resembles that found in an earlier study, which also focused on patients undergoing chemotherapy, where 82% were in the treatment stage 18 .
In Palestine, depression represents approximately 15.3% of mental disorders 20 . In this study, 38.4% of cancer patients had minimal depression, 22.5% had mild depression, 22.1% had moderate depression, and 17.0% had severe depression based on the BDI-II scale. On the other hand, a study conducted in Gaza Strip, Palestine, used the same scale (BDI) and reported that 7.7% of cancer patients were minimally depressed, 15% were mildly depressed, 53.4% were moderately depressed, and 24.2% were severely depressed. Another study used a different scale (the center for epidemiological studies depression scale, CES-D) and reported that 44% of Palestinian cancer patients had severe depression 21 . In another population group in Palestine, 33.9% of hemodialysis patients were moderately depressed, and 29% had severe depression 22 .
The elevated rate of depression in Palestine could be linked to major stress factors such as the enduring siege and occupation 23 , heightened anxiety levels 24 , and challenges in obtaining healthcare services 25 .
In comparison to research conducted in other regions, various studies have examined the prevalence of depression among breast cancer patients. In Jordan, 52.7% of respondents experienced minimal depression, 26.0% displayed mild symptoms, 19.5% exhibited moderate symptoms, and 1.8% had severe symptoms 19 . Similarly, in Turkey, 52.0% of breast cancer patients scored 17 or higher on the BDI scale 26 . Another study employed the hospital anxiety depression scale (HADS) to assess depression among cancer patients, revealing prevalence rates of 23.1% for mild depression, 11.1% for moderate depression, and 2.3% for severe depression 27 . A cross-sectional investigation in Milan, Italy, utilizing the HADS reported that 4.1% of cancer patients experienced severe depression 18 . Moreover, a study in Greece using the Greek translation of the BDI-21 revealed that 69.5% of respondents scored above 10 (indicating mild depression), 39% scored above 16 (indicating moderate to severe depression), and 11.4% scored above 30 (indicating severe depression). Notably, women were more prone to depression than men, with a significant portion experiencing mild to severe depression 28 . Unfortunately, there is a lack of specialized centers in Palestine that are crucial for mitigating depression symptoms in cancer patients 29 .
In the current study, we found that depression was more prevalent in cancer patients aged > 50 years. As previously demonstrated in a study using the HADS for breast cancer patients undergoing radiation therapy in Palestine, age older than 51 years was associated with a greater risk of depression 30 . A cross-sectional study conducted in two Jordanian hospitals concluded that age was not significantly associated with BDI-II scores 19 .
Regarding educational level, we found that cancer patients with low educational levels had more depression, which is similar to the findings of other studies 31 , 32 . However, other publications did not show a significant difference between the two variables of education level and depression 19 , 33 . Depression was also associated with socioeconomic status since patients with poor socioeconomic status had more depression. However, compared to other studies, depression was not significantly associated with socioeconomic status 19 , 32 .
Our findings revealed that smoking cancer patients had greater depression scores than nonsmokers. Smoking habits may develop through stressful life events. For example, in Palestine, many people complain of psychological problems resulting from traumatic events from the Israeli occupation 20 , 24 , 34 and anxiety 24 , 25 . Smokers account for more than one-fifth of people aged 18 and over; according to the Palestinian Household Survey conducted by the Palestinian Central Bureau of Statistics (PCBS) in 2010, 22.5% of Palestinians aged 18 and over in the Palestinian territory are smokers (26.7% in the West Bank compared to 14.6% in the Gaza Strip). The Jenin Governorate had the highest percentage of smokers (32.2%), while the North Gaza Governorate had the lowest percentage (11.3%) 35 . Smoking is also common in cancer patients 36 . Additionally, other studies have corroborated reports of diminished well-being among smokers 37 , 38 . The findings of the current study revealed that psychosocial assistance was not associated with lower depression scores; however, these findings contradict previous research that suggested that cancer patients should take advantage of accessible psychological support services to reduce their depression and that cancer patients should take advantage of available psychological support services to reduce their depression 39 , 40 .
Additionally, the analysis of depression levels revealed a significant link between socioeconomic status and smoking habits, consistent with prior research 41 , 42 , 43 , 44 . Furthermore, there was a correlation between anxiety levels and educational attainment among cancer patients. Those with lower education levels reported higher anxiety scores, while those with higher education levels showed lower scores, indicating a potential protective effect of higher education on long-term anxiety and sadness 45 . Our study also revealed that anxiety levels were greater in cancer patients at the diagnosis stage than in those undergoing treatment, in line with previous research that identified chronic inflammatory conditions as risk factors for anxiety and depression in cancer patients, particularly during the diagnostic phase 46 .
The 4.8% prevalence of deformities reported in our study encompasses various types of deformities, including tal Hashomer syndrome. However, due to the rarity of Tal Hashomer syndrome, its specific prevalence within our study population is also very low. The literature has noted infrequent instances of Tel Hashomer syndrome and Guillain‒Barré syndrome among lymphoma patients 47 .
The scales utilized in our research possess several advantages. First, by assessing ten symptoms, they allow for the identification of symptom patterns and enable swift evaluation. Moreover, these scales are widely adopted by clinical and research institutions globally, underscoring their broad acceptance. Their validity has been confirmed through psychometric testing, and they are accessible in more than 20 languages, making them usable across diverse populations. Furthermore, they exhibit minimal clinically significant differences and demonstrate high sensitivity to changes over time. Finally, these scales are freely accessible, facilitating their utilization in both clinical and research contexts 48 .
The strengths of the BDI-II are that it is user-friendly, applicable across international age groups (13 years and older), has a low reading level (average Flesch‒Kincaid grade level 3.6), and provides a substantial foundation for further research 49 .
Strengths and limitations
This study involved cancer patients from across Palestine, encompassing both the West Bank and the Gaza Strip, representing diverse socioeconomic backgrounds. This is an inaugural Palestinian investigation shedding light on the occurrence of depression symptoms among cancer patients. Nonetheless, this study has several limitations. Among these limitations is its cross-sectional design, which inhibits the examination of how depression in cancer patients progresses with varying treatment modalities. Further limitations include the use of convenience sampling solely from a single tertiary hospital, a restricted sample size, and a predominantly hematologic malignancy-focused sample, potentially skewing the representation of broader cancer demographics. Consequently, the findings may lack generalizability.

Conclusions
This study highlights the high prevalence of depression symptoms among cancer patients. The beck depression inventory-II (BDI-II) score was associated with factors such as age, educational level, socioeconomic status, and smoking, underlining the complexity of addressing depression in this population. Our findings underscore the utility of the BDI-II as a tool for assessing and managing depression symptoms in cancer patients, complementing the broader spectrum of care that includes psycho-oncological and psychiatric support. This integrated approach is crucial for enhancing the quality of life of cancer patients throughout their disease trajectory.
Recommendations
Depression symptoms were reported and referred to a social worker or available psychosocial personnel.
Involve a psychiatric/mental health nurse or social worker in the session to break the bad news about the cancer diagnosis.
More research is recommended considering different hospitals in Palestine and sample randomization.
Data availability
The data from our surveillance are not publicly available due to privacy and ethical restrictions. However, individuals interested in using the data for scientific purposes can request permission from the corresponding authors. Those with granted access will receive anonymized data to maintain patient privacy and data integrity. This manuscript is part of the Master of Community Mental Health Nursing graduation project submitted to An-Najah National University. It has been published as part of self-archiving in institutional repositories, accessible through the university repository ( https://repository.najah.edu/server/api/core/bitstreams/de047bba-0136-4a7b-9e9d-a484ad5126d1/content ).
Abbreviations
Beck depression scale
Beck depression inventory
An-Najah National University Hospital
Quality of life
Autologous bone marrow transplant
Ministry of Health
United States of America
The Palestinian Central Bureau of Statistics
Center for epidemiological studies depression scale
Hospital anxiety depression scale
Ministry of Health. Health Annual Report, Palestine 2020. https://site.moh.ps/Content/Books/mv2fIO4XVF1TbERz9cwytaKoWKAsRfslLobNuOmj7OPSAJOw2FvOCI_DQYaIXdf2i8gCmPHbCsav29dIHqW26gZu9qJDiW2QsifZt6FrdS4H2.pdf (Accessed 2 January 2022) (2021).
Salem, H. S. Cancer status in the Occupied Palestinian Territories: Types; incidence; mortality; sex, age, and geography distribution; and possible causes. J. Cancer Res. Clin. Oncol. 149 , 5139–5163. https://doi.org/10.1007/s00432-022-04430-2 (2023).
Article PubMed Google Scholar
Halahleh, K. & Gale, R. P. Cancer care in the Palestinian territories. Lancet Oncol. 19 , e359–e364. https://doi.org/10.1016/S1470-2045(18)30323-1 (2018).
Halahleh, K., Abu-Rmeileh, N. M. E. & Abusrour, M. M. Cancer in the Arab World 195–213 (Springer Singapore, 2022).
Book Google Scholar
AlWaheidi, S. Promoting cancer prevention and early diagnosis in the occupied Palestinian territory. J. Cancer Policy 35 , 100373. https://doi.org/10.1016/j.jcpo.2022.100373 (2023).
Derogatis, L. R. The prevalence of psychiatric disorders among cancer patients. JAMA 249 , 751–757. https://doi.org/10.1001/jama.1983.03330300035030 (1983).
Article CAS PubMed Google Scholar
Massie, M. J. Prevalence of depression in patients with cancer. J. Natl. Cancer Inst. Monogr. 57–71 , 2004. https://doi.org/10.1093/jncimonographs/lgh014 (2004).
Article Google Scholar
Cheng, B. T. et al. Palliative care initiation in pediatric oncology patients: A systematic review. Cancer Med. 8 , 3–12. https://doi.org/10.1002/cam4.1907 (2019).
Boonyathee, S., Nagaviroj, K. & Anothaisintawee, T. The accuracy of the Edmonton symptom assessment system for the assessment of depression in patients with cancer: A systematic review and meta-analysis. Am. J. Hosp. Palliat. Care 35 , 731–739. https://doi.org/10.1177/1049909117745292 (2018).
Bukberg, J., Penman, D. & Holland, J. C. Depression in hospitalized cancer patients. Psychosom. Med. 46 , 199–212. https://doi.org/10.1097/00006842-198405000-00002 (1984).
Berard, R. M., Boermeester, F. & Viljoen, G. Depressive disorders in an out-patient oncology setting: Prevalence, assessment, and management. Psychooncology 7 , 112–120. https://doi.org/10.1002/(SICI)1099-1611(199803/04)7:2%3c112::AID-PON300%3e3.0.CO;2-W (1998).
Odeh, J. B. & Qassidu, S. A. An-Najah National University Hospital (An-Najah National University, 2015).
Google Scholar
Battat, M. et al. Factors associated with palliative care symptoms in cancer patients in Palestine. Sci. Rep. 13 , 16190. https://doi.org/10.1038/s41598-023-43469-0 (2023).
Article ADS CAS PubMed PubMed Central Google Scholar
Naja, S. et al. Psychometric properties of the Arabic version of EPDS and BDI-II as a screening tool for antenatal depression: Evidence from Qatar. BMJ Open 9 , e030365. https://doi.org/10.1136/bmjopen-2019-030365 (2019).
Article PubMed PubMed Central Google Scholar
Aapro, M. & Cull, A. Depression in breast cancer patients: The need for treatment. Ann. Oncol. 10 , 627–636. https://doi.org/10.1023/a:1008328005050 (1999).
BetterHelp. What Is The Beck Depression Inventory? https://www.betterhelp.com/advice/depression/what-is-the-beck-depression-inventory/ (Accessed 2 December 2020) (2020).
Ministry of Health. Distribution of Reported Cancer Cases by Sex & Governorate, West Bank, Palestine 2020. https://info.wafa.ps/ar_page.aspx?id=14977 (Accessed 12 July 2023) (2020).
Ripamonti, C. I. et al. The Edmonton symptom assessment system (ESAS) as a screening tool for depression and anxiety in non-advanced patients with solid or haematological malignancies on cure or follow-up. Support Care Cancer 22 , 783–793. https://doi.org/10.1007/s00520-013-2034-x (2014).
Alquraan, L. et al. Prevalence of depression and the quality-of-life of breast cancer patients in Jordan. J. Multidiscip. Healthc. 13 , 1455–1462. https://doi.org/10.2147/JMDH.S277243 (2020).
Marie, M., Hannigan, B. & Jones, A. Mental health needs and services in the West Bank, Palestine. Int. J. Ment. Health Syst. 10 , 23. https://doi.org/10.1186/s13033-016-0056-8 (2016).
Dreidi, M. M., Asmar, I. T. & Rjoub, B. A. An original research about: The associations of depression and fatigue with quality of life among palestinian patients with cancer. Health Sci. J. https://doi.org/10.21767/1791-809x.1000474 (2017).
Al-Jabi, S. W. et al. Depression among end-stage renal disease patients undergoing hemodialysis: A cross-sectional study from Palestine. Ren Replace Ther. 7 , 12. https://doi.org/10.1186/s41100-021-00331-1 (2021).
Awni Bseiso, R. & Thabet, A. M. The relationship between siege stressors, anxiety, and depression among patients with cancer in Gaza Strip. Health Sci. J. 11 , 499. https://doi.org/10.21767/1791-809x.1000499 (2017).
Marie, M., SaadAdeen, S. & Battat, M. Anxiety disorders and PTSD in Palestine: A literature review. BMC Psychiatry 20 , 509. https://doi.org/10.1186/s12888-020-02911-7 (2020).
Marie, M. & Bataat, M. Health care access difficulties of palestinian patients in the context of mental health: A literature review study. J. Psychiatry Ment. Disord. 7 , 1062 (2022).
Nazlican, E., Akbaba, M. & Okyay, R. A. Evaluation of depression in newly diagnosed breast cancer cases in Hatay province of Turkey in 2011. Asian Pac. J. Cancer Prev. 13 , 2557–2561. https://doi.org/10.7314/apjcp.2012.13.6.2557 (2012).
Vignaroli, E. et al. The Edmonton symptom assessment system as a screening tool for depression and anxiety. J. Palliat. Med. 9 , 296–303. https://doi.org/10.1089/jpm.2006.9.296 (2006).
Mystakidou, K. et al. Beck depression inventory: Exploring its psychometric properties in a palliative care population of advanced cancer patients. Eur. J. Cancer Care (Engl.) 16 , 244–250. https://doi.org/10.1111/j.1365-2354.2006.00728.x (2007).
Shawawra, M. & Khleif, A. D. Palliative care situation in Palestinian Authority. J. Pediatr. Hematol. Oncol. 33 (Suppl 1), S64-67. https://doi.org/10.1097/MPH.0b013e31821223a3 (2011).
Almasri, H. & Rimawi, O. Assessment of depression and anxiety in breast cancer patients undergoing radiotherapy in Palestine. SN Compr. Clin. Med. 2 , 2787–2791. https://doi.org/10.1007/s42399-020-00635-z (2020).
Goldzweig, G. et al. Depression, hope and social support among older people with cancer: A comparison of Muslim Palestinian and Jewish Israeli cancer patients. Support Care Cancer 30 , 1511–1519. https://doi.org/10.1007/s00520-021-06554-6 (2022).
Cvetkovic, J. & Nenadovic, M. Depression in breast cancer patients. Psychiatry Res. 240 , 343–347. https://doi.org/10.1016/j.psychres.2016.04.048 (2016).
Arslan, S., Celebioglu, A. & Tezel, A. Depression and hopelessness in Turkish patients with cancer undergoing chemotherapy. Jpn. J. Nurs. Sci. 6 , 105–110. https://doi.org/10.1111/j.1742-7924.2009.00127.x (2009).
Abdeen, Z., Qasrawi, R., Nabil, S. & Shaheen, M. Psychological reactions to Israeli occupation: Findings from the national study of school-based screening in Palestine. Int. J. Behav. Dev. 32 , 290–297. https://doi.org/10.1177/0165025408092220 (2008).
Tucktuck, M., Ghandour, R. & Abu-Rmeileh, N. M. E. Waterpipe and cigarette tobacco smoking among Palestinian university students: A cross-sectional study. BMC Public Health 18 , 1. https://doi.org/10.1186/s12889-017-4524-0 (2017).
Jalambo, M., Alfaleet, F. & Aljazzar, S. Nutritional status, psychological stress, and lifestyle habits among cancer patients in Gaza Strip, Palestine. Int. J. Clin. Case Stud. Clin. Res. 4 , 1–9 (2020).
Hirpara, D. H. et al. Severe symptoms persist for up to one year after diagnosis of stage I-III lung cancer: An analysis of province-wide patient reported outcomes. Lung Cancer 142 , 80–89. https://doi.org/10.1016/j.lungcan.2020.02.014 (2020).
Bazargan, M., Cobb, S., Castro Sandoval, J. & Assari, S. Smoking status and well-being of underserved African American Older adults. Behav. Sci. (Basel) 10 , 78. https://doi.org/10.3390/bs10040078 (2020).
Aldaz, B. E., Treharne, G. J., Knight, R. G., Conner, T. S. & Perez, D. Oncology healthcare professionals’ perspectives on the psychosocial support needs of cancer patients during oncology treatment. J. Health Psychol. 22 , 1332–1344. https://doi.org/10.1177/1359105315626999 (2017).
Biracyaza, E., Habimana, S. & Rusengamihigo, D. Psychometric properties of the beck depression inventory (BDI-II) in cancer patients: Cancer patients from Butaro Ambulatory Cancer Center, Rwanda. Psychol. Res. Behav. Manag. 14 , 665–674. https://doi.org/10.2147/PRBM.S306530 (2021).
Chaaya, M., Sibai, A. M., Fayad, R. & El-Roueiheb, Z. Religiosity and depression in older people: Evidence from underprivileged refugee and non-refugee communities in Lebanon. Aging Ment. Health 11 , 37–44. https://doi.org/10.1080/13607860600735812 (2007).
Article CAS PubMed PubMed Central Google Scholar
Alduraidi, H. & Waters, C. M. Depression, perceived health, and right-of-return hopefulness of palestinian refugees. J. Nurs. Scholarsh. 50 , 163–171. https://doi.org/10.1111/jnu.12363 (2018).
Covey, L. S., Glassman, A. H. & Stetner, F. Depression and depressive symptoms in smoking cessation. Compr. Psychiatry 31 , 350–354. https://doi.org/10.1016/0010-440x(90)90042-q (1990).
Glassman, A. H. et al. Smoking, smoking cessation, and major depression. JAMA 264 , 1546–1549 (1990).
Bjelland, I. et al. Does a higher educational level protect against anxiety and depression? The HUNT study. Soc. Sci. Med. 66 , 1334–1345. https://doi.org/10.1016/j.socscimed.2007.12.019 (2008).
Bronner, M. B., Nguyen, M. H., Smets, E. M. A., van de Ven, A. W. H. & van Weert, J. C. M. Anxiety during cancer diagnosis: Examining the influence of monitoring coping style and treatment plan. Psychooncology 27 , 661–667. https://doi.org/10.1002/pon.4560 (2018).
Kivity, S., Shalmon, B. & Sidi, Y. Guillain-Barre syndrome: An unusual presentation of intravascular lymphoma. Isr. Med. Assoc. J. 8 , 137–138 (2006).
PubMed Google Scholar
Hui, D. & Bruera, E. The Edmonton symptom assessment system 25 years later: Past, present, and future developments. J. Pain Symp. Manag. 53 , 630–643. https://doi.org/10.1016/j.jpainsymman.2016.10.370 (2017).
Halfaker, D. A., Akeson, S. T., Hathcock, D. R., Mattson, C. & Wunderlich, T. L. Pain Procedures in Clinical Practice 13–22 (Hanley & Belfus, 2011).
Download references
Acknowledgements
We would like to thank all the researchers for their collaboration organized by the research center at NNUH.
Author information
Authors and affiliations.
Bone Marrow Transplant and Leukemia Unit, An-Najah National University Hospital, Nablus, 44839, Palestine
Maher Battat
Department of Hematology and Oncology, An-Najah National University Hospital, Nablus, 44839, Palestine
Nawal Omair, Mohammad A. WildAli, Riad Amer & Husam T. Salameh
Department of Nursing, College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Aidah Alkaissi
Department of Medicine, College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Riad Amer & Husam T. Salameh
Division of Clinical Pharmacy, Department of Hematology and Oncology, An-Najah National University Hospital, Nablus, 44839, Palestine
Amer A. Koni
Department of Clinical and Community Pharmacy, College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Amer A. Koni & Sa’ed H. Zyoud
Poison Control and Drug Information Center (PCDIC), College of Medicine and Health Sciences, An-Najah National University, Nablus, 44839, Palestine
Sa’ed H. Zyoud
Clinical Research Center, An-Najah National University Hospital, Nablus, 44839, Palestine
You can also search for this author in PubMed Google Scholar
Contributions
MB proposed the project, collected the data, evaluated the findings, and authored the report. NO and MAW conducted the literature reviews and assisted with data collection. AA contributed to the study proposal and evaluated the manuscript. AAK performed the statistical analysis, interpreted the results, reviewed the work for intellectual content improvement, revised the manuscript, and addressed reviewer comments.. MB, RA, and HTS were responsible for data integrity, critically examined the paper for intellectual content improvement, and helped write the final version and addressed reviewer comments. SHZ conceived and designed the study, supervised the project, and participated in writing the original draft and reviewing and editing subsequent drafts. The final manuscript was reviewed and approved by all the authors.
Corresponding authors
Correspondence to Husam T. Salameh or Sa’ed H. Zyoud .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Battat, M., Omair, N., WildAli, M.A. et al. Assessment of depression symptoms among cancer patients: a cross-sectional study from a developing country. Sci Rep 14 , 11934 (2024). https://doi.org/10.1038/s41598-024-62935-x
Download citation
Received : 23 May 2023
Accepted : 22 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1038/s41598-024-62935-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Depression symptoms
- Cancer patients
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
- Introduction
- Conclusions
- Article Information
Flowchart shows sample sizes and corresponding rates of depression screening and management in our study population for the most recent fiscal year. Sample sizes and rates shown in the text differ and reflect observations aggregated from all 4 study years.
a Refers to the 1-year prospective time frame when numbers were obtained.
b Refers to the 6-month retrospective time frame when numbers were obtained.
eTable 1. ICD-10 Codes Used for Depression Diagnosis
eTable 2. List of Drugs Classified as Antidepressant Medication in Study
eTable 3. Current Procedural Terminology (CPT) Codes for Psychotherapy
eTable 4. VA Clinic Stop Codes for Mental Health Specialty Visits
eTable 5. ICD-10 Codes Used for Other Mental Health Diagnoses in Study
eTable 6. Associations Between Receipt of Timely Depression Follow-up and Treatment and Various Patient Characteristics (Among All Screen-Positive Patients)
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Leung LB , Chu K , Rose D, et al. Electronic Population-Based Depression Detection and Management Through Universal Screening in the Veterans Health Administration. JAMA Netw Open. 2022;5(3):e221875. doi:10.1001/jamanetworkopen.2022.1875
Manage citations:
© 2024
- Permissions
Electronic Population-Based Depression Detection and Management Through Universal Screening in the Veterans Health Administration
- 1 Center for the Study of Healthcare Innovation, Implementation, and Policy, VA Greater Los Angeles Healthcare System, Los Angeles, California
- 2 Division of General Internal Medicine and Health Services Research, UCLA David Geffen School of Medicine, Los Angeles, California
- 3 VA Ann Arbor, Center for Clinical Management Research, Ann Arbor, Michigan
- 4 Department of Medicine, University of Michigan Medical School, Ann Arbor
- 5 Department of Psychiatry and Biobehavioral Sciences, UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles, California
- 6 RAND Corporation, Santa Monica, California
Question Among health care systems that implement universal depression screening, do patients who screen positive for depression receive timely follow-up and treatment?
Findings In a cohort study of 607 730 patients at 82 Veterans Health Administration primary care clinics from 2015 to 2019, 15 155 patients newly screened positive on the 2-item Patient Health Questionnaire and also were detected by clinicians as having depression; 77% met guidelines for completing at least minimal treatment in 1 year, but only 32% received clinical follow-up within 3 months of screening.
Meaning These findings suggest that screening paired with integrated services offers a reasonable opportunity to engage primary care patients in depression treatment, supporting collaborative care’s extensive evidence base; yet, access to timely services remains limited.
Importance In 2016, the US Preventive Services Task Force newly recommended universal screening for depression, with the expectation that screening would be associated with appropriate treatment. Few studies have been able to assess the population-based trajectory from screening to receipt of follow-up and treatment for individuals with depression.
Objective To examine adherence to guidelines for follow-up and treatment among primary care patients who newly screened positive for depression in the Veterans Health Administration (VA).
Design, Setting, and Participants This retrospective cohort study used VA electronic data to identify patients who newly screened positive for depression on the 2-item Patient Health Questionnaire at 82 primary care VA clinics in California, Arizona, and New Mexico between October 1, 2015, and September 30, 2019. Data analysis was performed from December 2020 to August 2021.
Main Outcomes and Measures Receipt of guideline-concordant care for screen-positive patients who were determined by clinicians as having depression was assessed. Timely follow-up (within 84 days of screening) was defined as receiving 3 or more mental health specialty visits, 3 or more psychotherapy visits, or 3 or more primary care visits with a depression diagnosis according to the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision . Completing at least minimal treatment (within 12 months) was defined as having 60 days or more of antidepressant prescriptions filled, 4 or more mental health specialty visits, or 3 or more psychotherapy visits.
Results The final cohort included 607 730 veterans (mean [SD] age, 59.4 [18.2] years; 546 516 men [89.9%]; 339 811 non-Hispanic White [55.9%]); 8%, or 82 998 of 997 185 person-years, newly screened positive for depression. Clinicians identified fewer than half with depression (15 155 patients), of whom 32% (5034 of 15 650 person-years) met treatment guidelines for timely follow-up and 77% (12 026 of 15 650 person-years) completed at least minimal treatment. Younger age (odds ratio, 0.990; 95% CI, 0.986-0.993; P < .001), Black race (odds ratio, 1.19; 95% CI, CI 1.05-1.34; P = .01), and having comorbid psychiatric diagnoses were significantly associated with timely follow-up. Individual quality metric components (eg, medication or psychotherapy) were associated differently with overall quality results among patient groups, except for age.
Conclusions and Relevance In this cohort study, most patients met the guidelines for completing at least minimal treatment, but only a minority received timely follow-up after screening positive and being identified as having depression. More research is needed to understand whether the discrepancy between patients who screened positive and patients identified as having depression reflects a gap in recognition of needed care.
Major depressive disorder is the leading cause of disability worldwide. 1 In 2016, the US Preventive Services Task Force (USPSTF) newly recommended universal depression screening in the general adult population, with the expectation that screening would be linked to appropriate treatment. 2 USPSTF recognized that staff-assisted depression care directed at ensuring accurate diagnosis, appropriate follow-up, and effective treatment conferred substantial improvement in clinical outcomes and was increasingly available in primary care settings. Yet, others have disagreed 3 and cited that evidence supporting the benefits of universal depression screening is too limited. For example, 4 2013 guidelines from the Canadian Task Force on Preventive Health Care recommended against routine depression screening to avoid depression overdiagnosis. Knowledge gaps in depression screening remain because few health care systems have been able to pragmatically study the population-based trajectory from screening to follow-up and treatment for those who have depression.
For more than 2 decades, the Veterans Health Administration (VA) has mandated annual depression screening in primary care 5 and currently achieves nearly universal screening rates among clinics nationally. 6 Primary care nurses conduct initial screening; then, primary care clinicians follow up with patients who screen positive for confirmation and treatment of depression. Primary care mental health integration teams also provide diagnostic support and collaboratively treat mental and behavioral health conditions, with a focus on mild-to-moderate severity depression and anxiety. 7 Primary care mental health integration teams (eg, psychologists, psychiatrists, and nurse care managers) are readily available in person or virtually throughout primary care clinics nationally, in addition to more intensive services provided through traditional mental health specialty referrals. The VA system is thereby equipped to address patients who are identified as having mental health needs, especially those with clinical depression.
In the US, there is an increasing call for depression to be addressed at the population level and for its detection and management to be done through public health approaches. 8 Other health care systems similarly embarking on guideline-concordant depression care (via screening, follow-up, and treatment) may benefit from anticipatory guidance on the volume of positive screens and treatment seekers within a primary care population. We use a new method to generate electronic population-based depression care quality measures to add to the limited evidence base on patient outcomes from universal depression screening. This cohort study aims to examine adherence to guidelines for follow-up and treatment among primary care patients who newly screened positive for depression in the VA.
The VA Greater Los Angeles institutional review board approved this study. Because the evaluation efforts were part of an ongoing quality improvement effort at the VA, the institutional review board deemed this study to be nonhuman participants research and, therefore, exempt from informed consent requirements. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
In a retrospective cohort study, we identified primary care patients among 82 clinics in 1 VA region between October 1, 2015, and September 30, 2019, using VA electronic data. Patient data were drawn from 11 hospital-based and 71 community-based VA clinics in Southern California, Arizona, and New Mexico that administered depression screening via the 2-item Patient Health Questionnaire.
This study expanded on recognized depression care quality metrics 9 by newly incorporating depression screening data using administrative and pharmacy databases from VA’s Corporate Data Warehouse. First, we identified 71 421 patients who screened positive for depression in primary care clinics by scoring 3 or higher on the 2-item Patient Health Questionnaire. Second, we restricted the cohort to patients who visited the same primary care site at least 1 additional time, allowing opportunity for clinical intervention. Third, to isolate patients with a new episode of depression, we further restricted the cohort to those who had not already received a diagnosis of depression (ie, International Statistical Classification of Diseases and Related Health Problems, Tenth Revision [ICD-10] depression diagnosis) or engaged in mental health care (ie, ≥60 days of antidepressant prescriptions, ≥4 mental health specialty visits, or ≥3 psychotherapy visits) (eTable 1, eTable 2, eTable 3, and eTable 4 in the Supplement ) within the past 6 months. Among our cohort who screened positive and met the aforementioned criteria, we further identified patients who were also detected by a clinician as having depression via diagnostic coding or antidepressant prescription within 12 months of screening positive ( Figure 1 shows data for fiscal year 2019).
Our 3 study outcomes were population-based depression care quality metrics established and detailed in prior research. 9 Measures were constructed on the basis of VA and National Committee for Quality Assurance guidelines and then were agreed on by a modified Delphi panel of VA and non-VA experts. We used 2 measures of timely follow-up, defined as 3 or more mental health specialty visits, 3 or more psychotherapy visits, or 3 or more primary care visits with a depression ICD-10 diagnosis within (1) 84 days and (2) 180 days. Also, we measured completion of at least minimally appropriate treatment (ie, having ≥60 days of antidepressant prescriptions, ≥4 mental health specialty visits, or ≥3 psychotherapy visits within 12 months of screening positive). Prescriptions with subtherapeutic doses and with nondepression indications (or keywords written on the dosing instructions) were excluded as antidepressant medications. We dichotomized outcomes as patients either having received or not received guideline-concordant depression care in each study year.
This study comprehensively examined available patient and clinic characteristics known or hypothesized to be associated with depression care quality. Data sources included VA’s Corporate Data Warehouse, National Patient Care Database, Vital Status File, and Site Tracking System. Patient covariates consisted of age, sex, self-reported race and ethnicity (ie, non-Hispanic White, non-Hispanic Black, Hispanic, other [American Indian or Alaska Native, Asian, and Native Hawaiian or other Pacific Islander], or unknown or missing), marital status, and income proxies (because patients may be eligible for VA care on the basis of a service-connected disability or exempt from copayment on the basis of having low financial means). Race and ethnicity were assessed in this study because disparities in mental health treatment by racial and ethnic group have been reported. 10 We used ICD-10 codes in outpatient and inpatient visits to identify mental health diagnoses (ie, depression, anxiety, posttraumatic stress disorder [PTSD], alcohol and substance use disorders, and serious mental illness [specifically, schizophrenia and bipolar disorder]) (eTable 5 in the Supplement ) and to calculate Charlson Comorbidity Index scores to risk-adjust physical health for each patient during each study year. Finally, we adjusted for whether patients’ assigned clinics were community-based vs hospital-based, rural vs urban location, and 5000 or more vs fewer assigned primary care patients (as a proxy for clinic size).
For descriptive purposes, we calculated unadjusted, aggregate rates of achieving depression care quality measures across our cohort and then examined patient and clinic characteristics for (1) screen-positive patients and (2) screen-positive patients who were also detected by clinicians as having depression, using t and χ 2 tests. We analyzed patient and clinic characteristics among those who met and did not meet depression care quality outcome measures, using χ 2 tests.
This study used multilevel regression models to examine for associations between depression care quality and the aforementioned patient and clinic characteristics among all study patients. We included year and health care system fixed effects to account for secular trends and invariant organizational characteristics. Patient random effects were included to account for the possibility of patients having multiple nonindependent observations during the 4 study years. SEs were also adjusted to account for clustering of patients within clinics. Given the dichotomous distributions of our quality outcomes, we reported odds ratios (ORs) and 95% CIs from multilevel logistic regressions in adjusted models. Estimates were also presented as probabilities (and SEs were calculated via the delta method), with all covariates held constant at their means. In additional analyses, we examined the contribution of each quality metric component (eg, counts of antidepressant prescriptions and psychotherapy visits) and reported incidence rate ratios (IRRs) and 95% CIs from multilevel negative binomial regression models. Finally, sensitivity analyses were conducted to examine for interactions between patient demographic characteristics (eg, age, sex, race, and ethnicity) and between demographic and clinic variables (eg, rurality, hospital-based vs community-based), to account for known demographic differences among veterans across age groups and clinic locations. For all models, we determined significance by using a 2-tailed α = .05. Data were analyzed in Stata statistical software version 15.1 (StataCorp). Data analysis was performed from December 2020 to August 2021.
Our study included 607 730 veterans (mean [SD] age, 59.4 [18.2] years; 546 516 men [89.9%]; 339 811 non-Hispanic White [55.9%]). Approximately 8% (82 998 of 997 185 person-years, or 71 421 patients) screened positive for new depressive symptoms in VA primary care. Among those who screened positive, 80% (66 305 of 82 998 person-years, or 57 779 patients) continued to receive primary care services that year in the same site, allowing opportunities for clinical intervention. Among those, 56% (37 063 of 66 305 person-years) had not already engaged in mental health care (within the past 6 months). We then examined the remaining 33 694 patients who newly screened positive for depression in our study cohort and noted several patient (ie, age, race, ethnicity, and comorbid conditions) and clinic characteristics to be significantly associated with depression care quality ( Table 1 and eTable 6 in the Supplement ).
However, fewer than one-half of screen-positive patients were detected by clinicians as having depression via diagnosis and/or antidepressant prescription (15 155 patients). When clinicians detected depression among patients who screened positive, 32% (5034 of 15 650 person-years) met treatment guidelines for appropriate timely follow-up by receiving 3 or more mental health specialty visits, 3 or more psychotherapy visits, or 3 or more primary care visits with a depression ICD-10 diagnosis within 84 days of screening; 77% (12 026 of 15 650 person-years) completed at least minimally appropriate treatment by having 60 days or more of antidepressant prescriptions filled, 4 or more mental health specialty visits, or 3 or more psychotherapy visits within 12 months of screening. Figure 1 shows data for fiscal year 2019. Percentages were stable across all 4 study years at the VA ( Figure 2 ).
Certain patient characteristics remained significantly associated with depression care quality among screen-positive patients who were also detected by clinicians as having depression ( Table 2 ). Younger age (OR for receiving treatment, 0.990; 95% CI, 0.986-0.993; P < .001) and comorbid mental illness were factors significantly associated with higher depression care quality. Probabilities for timely follow-up were 33% among patients younger than 45 years and 21% among patients older than 75 years; probabilities for receiving treatment were 81% among the younger patients and 71% among the older patients. Mental health comorbidities were important factors associated with high-quality depression care; as an example, probabilities for timely follow-up were 38% among patients with PTSD and 24% for patients without PTSD, probabilities for receiving treatment were 85% among those with PTSD and 72% among those without PTSD. Although having physical health comorbidities was not associated with receipt of treatment, it was an important factor associated with not receiving timely follow-up (OR, 0.80; 95% CI, 0.70-0.90; P < .001), with probabilities of 12% for Charlson Comorbidity Index scores of 2 or higher vs 14% for Charlson Comorbidity Index scores of 0. Black race was significantly associated with higher odds of timely follow-up vs White race (OR, 1.19; 95% CI, 1.05-1.34; P = .01), but race was not otherwise associated with treatment completion. When controlling for all covariates at their means, probabilities for follow-up among Black and White patients were 32% and 29%, respectively.
Each quality metric component (eg, antidepressant treatment, psychotherapy visits), appeared to contribute differently among patient groups, apart from age. Among patients with and without mental health comorbidities, results were similar across quality metric components, except PTSD. Among patients with and without PTSD, we found that mental health specialty (IRR, 1.18; 95% CI, 1.10-1.27; P < .001) and psychotherapy visits (IRR, 1.63; 95% CI, 1.52-1.75; P < .001) were associated with higher rates of timely follow-up; there was no difference in primary care visits. Similarly, among patients with Charlson Comorbidity Index score of 2 or higher vs those with a score of 0, we observed lower rates of timely follow-up through mental health specialty (IRR, 0.89; 95% CI, 0.81-0.99; P = .04) and psychotherapy visits (IRR, 0.86; 95% CI, 0.77-0.97; P = .01); there was no difference in primary care visits. For Black veterans compared with White veterans, greater use of mental health specialty care (IRR, 1.12; 95% CI, 1.02-1.23; P = .01) was associated with differences in timely follow-up. Although we did not see racial or ethnic differences in overall rates of treatment completion, we saw differences in use of different treatment types between White veterans and those from minority groups. Black veterans (IRR, 0.8; 95% CI, 0.76-0.86; P < .001) and Hispanic veterans (IRR, 0.88; 95% CI, 0.76-0.93; P < .001) had lower rates of treatment with antidepressant medication but had higher rates of mental health specialty visits (Black veterans, IRR, 1.18; 95% CI, 1.1-1.27; P < .001) and psychotherapy visits (Hispanic veterans, IRR, 1.11; 95% CI, 1.02-1.20; P = .01), compared with White veterans. Although no sex differences were observed among quality metrics, we noted that of individual metric components, primary care visits with a depression ICD-10 diagnosis were significantly more likely for women (IRR, 1.82; 95% CI, 1.44-2.31; P < .001) than men. Finally, no significant interactions were identified among tested patient demographic and clinic variables in sensitivity analyses.
The VA has invested heavily in screening as an important part of the pathway for patients to initiate and access mental health treatment, 11 allowing us to assess results of a primary care population receiving USPSTF guideline-concordant depression care. 2 For some researchers, without more data, routine use of depression screening in medical settings remains controversial. 3 , 4 In the absence of randomized clinical trials, our large observational cohort study attempts to fill knowledge gaps surrounding systemwide implementation of depression screening. We found that 8% of patients screened positive among primary care populations in our integrated VA health care system, but clinicians identified fewer than one-half of screen-positive patients as having depression. Those who were not detected as having depression are likely an unknown mix of patients who were appropriately assessed and were found to not meet the criteria for a depression diagnosis (desired care process) and patients who were never appropriately assessed or assessed with no diagnosis recorded (undesired care process). More research is needed to understand whether this indicates a gap in recognition of needed care or overdetection from universal screening in the VA.
Although most patients with depression met guidelines for completing treatment within a year of screening positive, only a minority received timely clinical follow-up within 3 to 6 months. Trends did not improve over time for the approximately two-thirds and one-half of screen-positive patients who were detected by clinicians as having depression and did not receive follow-up visits within 3 to 6 months. Across all years, approximately one-quarter of these patients did not receive at least minimal treatment within 1 year. As a system that aims to lead in care of PTSD (a common comorbidity to depression) 12 and to prioritize suicide prevention (for which depression is a major risk factor), 13 improving timeliness of follow-up and treatment after a positive depression screen remains necessary in the VA. Similarly, other health care systems have struggled and cited that only 36% of patients with newly diagnosed depression even start medication and/or complete 1 psychotherapy visit during the first 3 months. 14 Nonetheless, screening paired with accessible mental health services generally offered reasonable opportunity to engage VA primary care patients in treatment, supporting the extensive evidence base for collaborative care of depression. 15
This study also highlights notable differences in depression care quality between patient groups. We found that timely follow-up and treatment continued to lag for geriatric patients 16 and those with chronic physical health comorbidities, 17 likely related to competing demands such as specialty care. Patients who had comorbid mental health conditions, however, fared well in the receipt of high-quality depression care, as noted before, 18 likely a testament to VA-specific services for those with PTSD or serious mental illness (eg, Mental Health Intensive Case Management). 19 In a male-dominated health system, we again noted sex differences in mental health care access, seemingly occurring preferentially for women through primary care services. 20 Although some disparities between patient groups have been remedied by an integrated health system that prioritizes mental health care accessibility, efforts to improve the timeliness of care after a positive depression screen and treatment of geriatric patients and patients with physical health comorbidities remain necessary.
A new and noteworthy observation pertains to the absence of and possible reversal of oft-seen racial disparities in overall mental health care access across health care systems. Although it was again noted that Black veterans were treated with antidepressant medication at lower rates than White veterans, 10 we did not see racial disparities in overall rates of treatment completion when we fully accounted for veterans who chose to seek nonmedication treatment through mental health specialty care. The VA has striven for increasing accessibility of psychotherapy as part of integrated primary care teams, 7 which is the treatment modality that is preferred by patients, especially those in racial and ethnic minority groups. 21 Such systemwide changes may have resulted in previously documented racial and ethnic disparities in guideline-concordant depression treatment 10 to seemingly be eliminated in the VA. Depression is often underdetected and undertreated among minoritized groups in the US. 22 This study continues to support that systematic quality improvement of screening and treatment are potential tools to mitigate racial and ethnic disparities in mental health care. 23
To our knowledge, this study is one of the first to examine timely follow-up and treatment for primary care patients who screen positive for depression in an integrated health care system, but several limitations are worth noting. First, because we leveraged existing electronic databases, we were unable to investigate patient-reported quality outcomes, such as depression symptoms or quality of life. Second, our study excluded fewer than 20% of patients who did not return for primary care after screening. Our study cohort was designed to assess care quality for patients who had the opportunity to receive continuity primary care. Focusing on patients who drop out of VA care, often because they have had an acute problem when traveling, are switching VA clinics, or are seeking non-VA care, requires a different study approach and lead to different implications than were the case for this study. Third, similar to other studies based on administrative data, coding inaccuracies (eg, inactive depression diagnoses being incorrectly recoded, possible discrepancies related to antidepressant prescriptions without listed indications) may be limitations. Fourth, although the results may not be generalizable beyond our study population of mostly male veterans in 1 VA region, prior studies show that the large majority of mental health services are delivered to veterans by the VA. 24
With increasing recognition of population-level impacts of mental health disorders, an epidemiological framework for mapping access to care for patients who screen positive for depression in VA primary care is methodologically crucial. In the VA, we observed that universal screening yields a stable proportion of patients who screen positive for depression, of whom the minority receive timely follow-up but the majority receive guideline-concordant treatment. Although the VA’s investments in depression screening and subsequent follow-up care and treatment have seemingly closed some disparity gaps (in mental health comorbidities and race), several others remain (in age and in physical health comorbidities). Continued research in mapping access to care pathways for patients who screen positive for depression is needed to ultimately improve upon patient health outcomes for VA and other health care systems.
Accepted for Publication: January 23, 2022.
Published: March 10, 2022. doi:10.1001/jamanetworkopen.2022.1875
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2022 Leung LB et al. JAMA Network Open .
Corresponding Author: Lucinda B. Leung, MD, PhD, Center for the Study of Healthcare Innovation, Implementation, and Policy, VA Greater Los Angeles Healthcare System, 11301 Wilshire Blvd (111G), Los Angeles, CA 90073 ( [email protected] ).
Author Contributions: Dr Leung and Ms Chu had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Leung, Wells, Rubenstein.
Acquisition, analysis, or interpretation of data: Leung, Chu, Rose, Stockdale, Post.
Drafting of the manuscript: Leung, Rubenstein.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Leung, Chu, Rose.
Obtained funding: Leung, Stockdale.
Administrative, technical, or material support: Leung, Chu, Post, Wells.
Supervision: Leung, Stockdale, Wells, Rubenstein.
Conflict of Interest Disclosures: Dr Rubenstein reported receiving nonfinancial support from the Department of Veterans Affairs (VA) during the conduct of the study. No other disclosures were reported.
Funding/Support: Dr Leung is supported by Career Development Award IK2 HX002867 from the VA Health Services Research and Development Service.
Role of Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the US government. This work was undertaken as part of the Veterans Health Administration’s Primary Care Analytics Team (Seattle, Washington), supporting and evaluating the VA’s transition to a patient-centered medical home. Funding for the Primary Care Analytics Team is provided by the VA Office of Primary Care (Washington, DC).
Additional Contributions: Michael McClean, BA (VA Greater Los Angeles Healthcare System), assisted with data management, and Jessica Severin, BA (VA Greater Los Angeles Healthcare System), assisted with manuscript preparation. Neither of them was compensated for this work beyond their normal salaries.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 30 May 2024
The relationship between childhood psychological abuse and depression in college students: a moderated mediation model
- Yang Liu 1 na1 ,
- Qingxin Shen 1 na1 ,
- Liangfan Duan 1 na1 ,
- Lei Xu 1 , 2 ,
- Yongxiang Xiao 1 &
- Tiancheng Zhang 1
BMC Psychiatry volume 24 , Article number: 410 ( 2024 ) Cite this article
87 Accesses
Metrics details
Childhood psychological abuse (CPA) are highly correlated with depression among college students, but the underlying mechanisms between variables need further exploration. This study aims to investigate internet addiction as a mediating factor and alexithymia as a moderating factor, in order to further elucidate the potential risk factors between CPA and depression among college students.
A self-report survey was conducted among 1196 college students from four universities in three provinces in China. The survey included measures of CPA, internet addiction, alexithymia, and depression. Descriptive and correlational analyses were performed on these variables, and a moderated mediation model was constructed.
CPA was positively correlated with depression among college students, as well as internet addiction with alexithymia. Internet addiction partially mediated the relationship between CPA and depression among college students, while alexithymia strengthened the relationships among the paths in the moderated mediation model.
This study provides further insights into the psychological mechanisms underlying the relationship between CPA and depression among college students. Internet addiction serves as a mediating factor in this relationship, while alexithymia may enhance the strength of the relationships among the three variables.
Peer Review reports
Introduction
Depression is a highly prevalent psychological disorder among young people, characterized by symptoms such as sadness, lack of energy, and despair [ 1 ]. Over the past decade, the incidence of depression has been continuously increasing [ 2 , 3 ]. Studies show that the prevalence of depression among Chinese university students exceeds 25% [ 4 , 5 ], and the global incidence rate is close to 30% [ 6 ]. Individuals with depression exhibit a variety of complex negative physical and mental manifestations [ 7 ]. Feelings of worthlessness, hopelessness, and self-blame are strong emotional experiences among depressed individuals [ 8 ]. Major cognitive impairments displayed by these individuals include emotional dysregulation, cognitive biases, difficulties in attention and memory, and inhibitory dysfunction [ 9 , 10 ]. Similarly, outward behaviors manifest a range of negative patterns, such as social withdrawal [ 11 ], sleep disturbances [ 12 ], and abnormal changes in appetite [ 13 ]. These physical and mental manifestations further deepen the severity of depression [ 14 ]. Additionally, the etiology of depression is complex, with early-life stress being a significant risk factor [ 15 ], and that is often associated with adverse childhood experiences [ 16 ], such as childhood abuse. Childhood abuse has a close relationship with depression [ 17 , 18 , 19 , 20 ], and studies have found that among the subtypes of childhood abuse that childhood psychological abuse (CPA) is most closely related to depression [ 18 , 21 ]. Given the significant harm of depression, social attention, and its strong association with CPA, this study strongly needs to explore the underlying mechanisms between the two, in order to intervene and prevent timely and predict the impact of CPA on individual depression.
CPA refers to inappropriate psychological parenting behavior that guardians continuously and repeatedly adopt during childhood, which has an adverse effect on individuals' growth [ 22 ]. Due to its particular nature, the detection rate of CPA is quite high in different countries [ 23 , 24 ]. Abuse and neglect are two subtypes of CPA that are increasingly accepted by scholars in related studies. Longitudinal studies have found that parents' psychological neglect predicts future depression in adolescents [ 25 ]. In addition, research has found that among the classifications of childhood abuse, the correlation between psychological abuse and depression is the highest [ 18 ]. Based on the above review, this study hypothesized that CPA can significantly predict the occurrence of depression in college students.
Individuals who have experienced CPA often encounter emotional distress. Faced with such distress, they may be at an increased risk of engaging in hazardous behaviors, such as internet addiction, as these online activities may serve as a coping mechanism to alleviate negative emotions [ 26 ]. Without intervention, this reliance on the internet can form a cyclical pattern, potentially leading to internet addiction. Internet addiction is characterized by an excessive, problematic, and compulsive engagement in behaviors related to internet use [ 27 , 28 ]. Research indicates that among the various subtypes of childhood maltreatment, CPA has the strongest association with internet addiction [ 29 ]. CPA can significantly predict individuals internet addiction, and internet addiction has been found to mediate the relationship between CPA and suicidal internet addiction behaviors [ 30 ]. In discussions that integrate the relationship between childhood maltreatment and internet addiction, CPA is highlighted as a particularly salient predictor [ 31 ]. Consistent with the social compensation theory [ 32 ], CPA may lead individuals to seek emotional fulfillment through online interactions. Furthermore, there is a recognized association between internet addiction and depression. Research has found a strong correlation between internet addiction and depression [ 33 ], with internet addiction being a significant predictor of depression [ 34 ]. Longitudinal studies have shown a significant bidirectional relationship between internet addiction and depression among college students [ 35 ]. The displacement hypothesis [ 36 ] suggests that excessive internet use may impede real-life social interactions, reduce well-being, and deepen depression. Depression can also intensify the level of internet addiction, creating a vicious cycle and leading to a "rich get richer" scenario [ 37 ]. Based on this evidence, this study posits that CPA can significantly predict internet addiction among college students, which in turn can significantly predict depression.
However, when individuals possess certain traits, the relationships among the variables mentioned above may be strengthened, exacerbating negative behaviors or psychological outcomes. Among these variables, the level of alexithymia is one of the more important ones. Alexithymia is a stable personality trait [ 38 ], characterized by limited ability to understand one's own feelings and others' emotions, inadequate emotion regulation in interpersonal interactions [ 39 ], difficulty in recognizing emotions, describing emotions, and an externally oriented thinking style [ 40 ]. Alexithymia, due to emotional dysregulation, can lead to the intensification of negative emotions such as anxiety and depression [ 41 ], and inaccurate attention and expression of emotions may result in poor interpersonal relationships [ 42 ], thereby increasing individuals' psychological burden. To escape or alleviate such negative psychological states, the internet on mobile phones provides an easily accessible avenue [ 42 , 43 , 44 , 45 ]. According to the alexithymia stress hypothesis, individuals with high levels of alexithymia often find themselves in a state of stress due to their inadequate understanding and recognition of their own and others' emotions [ 46 ], which further predicts severe negative psychological states [ 47 ]. Therefore, based on the aforementioned review, it is evident that alexithymia may enhance the relationship between CPA, internet addiction, and depression discussed in this study, further exacerbating the degree of negative psychological and behavioral outcomes. Additionally, individuals with alexithymic characteristics not only neglect emotions [ 48 ], but they may also have a generalized impairment in perceiving internal bodily sensations (interoception) compared to individuals with lower levels of alexithymia [ 49 ], as demonstrated by various studies on the accuracy of perceiving heart rate [ 50 , 51 ], delayed healthcare seeking for illnesses [ 52 ], and unstable substance intake [ 53 ], among others. Based on these features, individuals with high levels of alexithymia tend to overlook their own discomfort symptoms even when they excessively use the internet [ 54 , 55 ] due to their lower sensory perception. Therefore, we hypothesize that alexithymia moderates the relationships among CPA, internet addiction, and depression mediated by various paths.
In summary, previous research strongly indicates the relationship and predictive role of CPA and depression, but these areas are relatively understudied among Chinese university students. To further supplement research in this field and explore underlying psychological mechanisms, this study introduces the mediating variable of internet addiction and the moderating variable of alexithymia. Therefore, this study constructs a hypothetical path model (see Fig. 1 ).
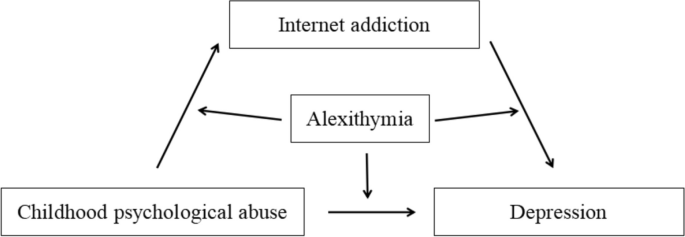
Hypothesized a moderated and mediation model
Participants
This cross-sectional survey was conducted in October 2023 among Chinese university students from four universities in Hunan Province, Hubei Province, and Guangxi Province. Prior to distribution, the researchers delivered a presentation to all participants, informing them of the main content and confidentiality of the survey data, as well as its ultimate purpose. The electronic questionnaires were distributed on a class basis, with an informed consent statement attached to the questionnaire's cover page. Participants could proceed with the survey only after choosing to agree, while those who declined would be directed to an exit page. Informed consent was obtained from all the participants. The survey was anonymous and voluntary, and it could be completed within 20 min. Prior to commencement, this study obtained approval from the Biomedicine Ethics Committee of Jishou University. We confirm that all the procedure is in accordance with the relevant guidelines and regulations such as the declaration of Helsinki. A total of 1352 students completed the survey, and after excluding respondents with excessively short response times or patterns in their answers, valid data from 1196 participants (496 males, 700 females) were ultimately obtained, with an average age of 18.69 years (SD = 1.07).
Childhood psychological abuse (CPA)
The measurement of CPA utilized the psychological abuse and neglect subscales from the Short Childhood Trauma Questionnaire (SCTQ) [ 56 ]. Each subscale included 5 items, scored on a Likert scale of 1 (never) to 5 (always), assessing the experiences of participants before the age of 17. An example item from the scale is: “Someone in my family said insulting or sad things to me”. Higher scores indicated higher levels of CPA. In this study, the Cronbach's α for the sample was 0.878.
Depression among college students was measured using the depression subscale from the Chinese version of the Depression Anxiety Stress Scale (DASS-21) [ 57 ]. The subscale comprised 7 items, scored on a Likert scale of 1 (strongly disagree) to 4 (strongly agree), assessing the level of depression experienced by participants. An example item from the scale is: “I can't be enthusiastic about anything”. Higher scores indicated more severe depression. In this study, the Cronbach's α for the sample was 0.906.
- Internet addiction
Internet addiction among college students was measured using the Problematic Social Media Use (PSMU) Scale [ 58 ]. The scale comprised 8 items, scored on a Likert scale of 1 (not at all) to 5 (completely), assessing the level of internet addiction experienced by participants. An example item from the scale is: “Using social networking sites distracts me from my studies”. Higher scores indicated more severe internet addiction. In this study, the Cronbach's α for the sample was 0.857.
- Alexithymia
The Toronto Alexithymia Scale (TAS-20) was used to assess the level of alexithymia among college students [ 59 ]. The scale comprised 20 items, scored on a Likert scale of 1 (totally disagree) to 5 (totally agree), assessing the level of alexithymia experienced by participants. An example item from the scale is: “I am often confused about what emotion I am feeling”. Higher scores indicated more severe alexithymia. In this study, the Cronbach's α for the sample was 0.804.
Considering the potential influence of demographic variables, such as gender and age [ 31 , 60 ], on the analysis results, we controlled for these variables in our analysis.
Statistical analyses
All statistical analyses were conducted using SPSS 26.0 software. Firstly, we checked for methodological biases to evaluate the potential bias resulting from self-report questionnaires. Before initiating the data analysis, we assessed the normality of our data using the Shapiro–Wilk test. According to Kim's proposal, data exhibiting an absolute skewness value below 2 and an absolute kurtosis value below 7 may be deemed to approximate a normal distribution [ 61 ]. In our study, we found that the variables CPA, depression, internet addiction, and alexithymia were normally distributed. For variables conforming to a normal distribution, descriptive analysis was conducted using the mean and standard deviation (Sd), while Pearson's correlation analysis was employed to assess the relationships among them. Then, we standardized the data of the main variables before conducting the analyses. Finally, to test our hypotheses, we used the PROCESS macro (Mode 4 and Model 59) in SPSS to analyze the relationships between variables [ 62 ]. The PROCESS macro was based on a bootstrapping method with 5000 resamples to estimate the model testing and 95% confidence intervals (95% CI), and a relationship was considered significant when the 95% CI did not include 0. Gender and age were considered as covariates in the analyses, and the significance level was set at α = 0.05.
Harman’s single factor test and normality test
Harman's single-factor test was used to examine the impact of common method bias. The analysis results showed that there were 2 factors with eigenvalues greater than 1. Without rotating the principal component factors, the explanatory rate of the first factor was 35.55%, which is lower than the recommended threshold of 40% [ 63 ]. Therefore, this study did not encounter severe common method bias. Upon assessing normality for our principal variables, all variables exhibited absolute skewness values below 2 and absolute kurtosis values below 7. Consequently, parametric tests were employed for all subsequent analyses.
Descriptive analyses
The results of Table 1 show that CPA (t = 2.62, p < 0.001), depression (t = 2.32, p < 0.05) and Internet addiction (t = -2.17, p < 0.05) are different between genders and reach statistical significance.
Correlational analyses
Table 2 presents the Pearson correlation data between the variables of interest. CPA was significantly positively correlated with college students' internet addiction ( r = 0.240, p < 0.001), depression ( r = 0.481, p < 0.001), and alexithymia ( r = 0.322, p < 0.001). College students' internet addiction was significantly positively correlated with depression ( r = 0.384, p < 0.001) and alexithymia ( r = 0.262, p < 0.001). Depression was significantly negatively correlated with college students' alexithymia ( r = 0.461, p < 0.001).
Mediation analysis
Table 3 presents the results showing that, after controlling for gender and age, CPA can significantly predict depression in college students (β = 0.473, SE = 0.026, p < 0.001). When internet addiction was included as a mediator variable, CPA continued to significantly predict depression in college students (β = 0.402, SE = 0.025, p < 0.001). Additionally, upon testing the mediation model, it was found that CPA significantly predicts internet addiction in college students (β = 0.245, SE = 0.029, p < 0.001), and internet addiction also significantly predicts depression (β = 0.290, SE = 0.025, p < 0.001).
Moderated and mediation analysis
After controlling for covariates, the moderated mediation model analysis revealed that the predictive effects of all paths in the mediation model remained significantly present (CPA predicting depression:β = 0.322, SE = 0.025, p < 0.001; CPA predicting internet addiction:β = 0.180, SE = 0.030, p < 0.001; Internet addiction predicting depression:β = 0.223, SE = 0.024, p < 0.001). Additionally, alexithymia significantly predicted college students' internet addiction (β = 0.201, SE = 0.029, p < 0.001) and depression (β = 0.281, SE = 0.025, p < 0.001). Lastly, the interaction term between alexithymia and CPA significantly predicted college students' internet addiction (β = 0.072, SE = 0.027, p < 0.01) and depression (β = 0.071, SE = 0.023, p < 0.01), and the interaction term between internet addiction and alexithymia significantly predicted college students' depression (β = 0.060, SE = 0.022, p < 0.01). Refer to Table 4 , Figs. 2 and 3 for details.
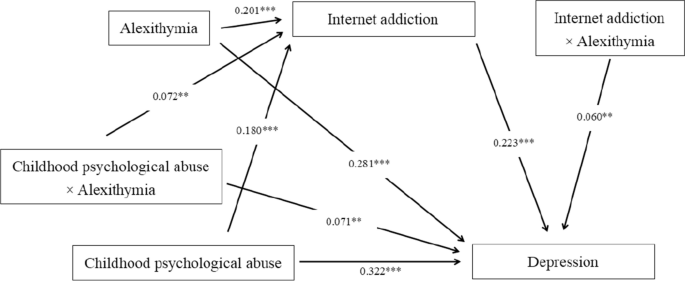
Moderated and mediation model
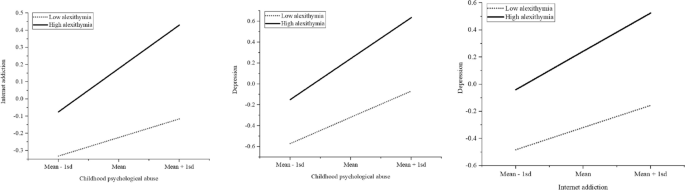
Simple slope plot
This study examines the relationships between CPA, internet addiction, depression, and alexithymia among college students. The findings reveal positive correlations between CPA, internet addiction, depression, and alexithymia, all of which are statistically significant. After controlling for demographic variables, internet addiction is found to mediate the relationship between CPA and depression in college students, while alexithymia moderates this relationship, confirming our initial hypothesis.
Our study confirms the positive correlation between CPA and depression in college students, which is consistent with previous research [ 18 , 31 ]. Studies conducted in China have shown that childhood abuse is relatively common [ 64 ], with emotional abuse being the most prevalent type [ 65 , 66 ]. Almost all types of childhood abuse are associated with mental health problems [ 20 , 23 , 67 , 68 ], increasing the risk of various adversities in individuals' later lives [ 23 , 69 , 70 ], with psychological abuse being particularly prominent [ 31 , 68 ], even predicting somatic symptoms in patients with severe depression [ 71 ]. Furthermore, research has found that CPA becomes the sole predictor of adolescent depression when controlling for other types of abuse, and early psychological abuse has a greater impact on depression [ 72 ]. Children who receive warm, rule-following, and well-bounded care from parents perform better in various aspects, including mental health [ 73 ]. On the other hand, children who experience psychological abuse from caregivers, in a state of invisible stress similar to social isolation, are more likely to develop depression, anxiety, and even aggressive behaviors [ 74 ].
Our study supports the hypothesis that internet addiction mediates the relationship between CPA and depression in college students, which is consistent with other similar studies [ 29 ]. Previous research has found a strong association between CPA and internet addiction among young people [ 30 , 31 , 75 , 76 ]. The relationship between internet addiction and depression has also been strongly supported [ 77 ], including in studies conducted in China [ 35 ]. According to the explanations of social control theory [ 78 ] and compensatory internet use theory [ 32 ], CPA seems to indicate unfavorable family support environments for adolescents, leading them to seek support from the virtual online world and developing internet addiction. It was found that adolescents who were addicted to the internet at baseline were more likely to develop depression in the future [ 77 ], which is also true in other studies [ 79 ]. Adolescents addicted to the internet often face greater stress, making them more prone to depression [ 80 ].
As previously hypothesized, alexithymia strengthens the relationships between all pathways. Individuals with alexithymia have difficulty understanding their own and others' emotions and are unable to regulate their emotions appropriately in daily interpersonal interactions [ 39 ], leading to an exacerbation of negative emotions [ 41 ]. Additionally, based on the explanations of general strain theory [ 81 ] and compensatory internet use theory [ 82 ], individuals with alexithymia feel stressed in dealing with interpersonal relationships [ 83 ]. Under this negative emotional state, in order to meet the needs of interpersonal communication and escape from the pressure of reality, they naturally choose the online world, which further leads to the development and intensification of internet addiction. However, alexithymia's "dullness" towards one's own feelings is not limited to emotions but can also extend to the perception of internal sensations [ 49 ]. Brain regions associated with these internal sensations include the anterior insula and anterior cingulate cortex [ 84 , 85 ], which not only play a role in non-emotional interoception but also have significant implications for individuals' emotional processing [ 86 , 87 ]. Studies have found structural abnormalities in these brain regions in individuals with alexithymia [ 88 , 89 , 90 ]. It is possible that individuals with severe pain and fatigue continue to use the internet despite their condition, further exacerbating their involvement in negative psychological and behavioral patterns. Therefore, high levels of alexithymia strengthen the relationships between CPA, internet addiction, and depression, which aligns with the expectations of this study.
In conclusion, our study further contributes to understanding the relationship between CPA and depression in college students, as well as the mediating role of internet addiction and the moderating role of alexithymia. These findings are not commonly seen in previous research. However, the study has several limitations. Firstly, the accuracy of self-reported CPA data may be insufficient as it involves retrospective self-reporting. Secondly, the representativeness of the sample may be inadequate as we only selected local colleges from a few provinces in China, with most of the students being locals. Future studies could increase the diversity of the sample. Lastly, due to the cross-sectional nature of the study, the causal relationships between variables are challenged. Therefore, future research could explore causal relationships based on longitudinal tracking.
This study discusses the relationships between CPA, internet addiction, depression, and alexithymia among college students, confirming the mediating role of internet addiction and the moderating role of alexithymia between CPA and depression. Individuals, families, schools, and society should pay attention to the negative impacts caused by CPA, especially for individuals with high levels of alexithymia.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due [our experimental team's policy] but are available from the corresponding author on reasonable request.
Clark MS, Jansen KL, Cloy JA. Treatment of childhood and adolescent depression. Am Fam Physician. 2012;86(5):442–8.
PubMed Google Scholar
Moreno-Agostino D, Wu Y, Daskalopoulou C, Hasan MT, Huisman M, Prina M. Global trends in the prevalence and incidence of depression:a systematic review and meta-analysis. J Affect Disord. 2021;281:235–43. https://doi.org/10.1016/j.jad.2020.12.035 .
Article PubMed Google Scholar
Twenge JM, Cooper AB, Joiner TE, Duffy ME, Binau SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005–2017. J Psychopathol Clin Sci. 2019;128(3):185–99. https://doi.org/10.1037/abn0000410 .
Article Google Scholar
Gao L, Xie Y, Jia C, Wang W. Prevalence of depression among Chinese university students: a systematic review and meta-analysis. Sci Rep. 2020;10(1):15897. https://doi.org/10.1038/s41598-020-72998-1 . Published 2020 Sep 28.
Article CAS PubMed PubMed Central Google Scholar
Zeng W, Chen R, Wang X, Zhang Q, Deng W. Prevalence of mental health problems among medical students in China. Medicine. 2019;98(18):e15337. https://doi.org/10.1097/MD.0000000000015337 .
Article PubMed PubMed Central Google Scholar
Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. J Psychiatr Res. 2013;47(3):391–400. https://doi.org/10.1016/j.jpsychires.2012.11.015 .
Guerrera CS, Platania GA, Boccaccio FM, Sarti P, Varrasi S, Colliva C, et al. The dynamic interaction between symptoms and pharmacological treatment in patients with major depressive disorder: the role of network intervention analysis. BMC Psychiatry. 2023;23(1):885. https://doi.org/10.1186/s12888-023-05300-y . Published 2023 Nov 28.
Harrison P, Lawrence AJ, Wang S, Liu S, Xie G, Yang X, et al. The psychopathology of worthlessness in depression. Front Psychiatr. 2022;13:818542. https://doi.org/10.3389/fpsyt.2022.818542 . Published 2022 May 19.
Kircanski K, Joormann J, Gotlib IH. Cognitive aspects of depression Wiley interdisciplinary reviews. Cognitive Sci. 2012;3(3):301–13. https://doi.org/10.1002/wcs.1177 .
Gotlib IH, Joormann J. Cognition and depression: current status and future directions. Annu Rev Clin Psychol. 2010;6:285–312. https://doi.org/10.1146/annurev.clinpsy.121208.131305 .
Teo AR, Nelson S, Strange W, Kubo H, Katsuki R, Kurahara K, et al. Social withdrawal in major depressive disorder: a case-control study of hikikomori in japan. J Affect Disord. 2020;274:1142–6. https://doi.org/10.1016/j.jad.2020.06.011 .
Sun X, Zheng B, Lv J, Guo Y, Bian Z, Yang L, et al. Sleep behavior and depression: Findings from the China Kadoorie Biobank of 0.5 million Chinese adults. J Affect Dis. 2018;229:120–4. https://doi.org/10.1016/j.jad.2017.12.058 .
Simmons WK, Burrows K, Avery JA, Kerr KL, Bodurka J, Savage CR, et al. Depression-related increases and decreases in appetite: dissociable patterns of aberrant activity in reward and interoceptive neurocircuitry. Am J Psychiatry. 2016;173(4):418–28. https://doi.org/10.1176/appi.ajp.2015.15020162 .
Kupferberg A, Hasler G. The social cost of depression: Investigating the impact of impaired social emotion regulation, social cognition, and interpersonal behavior on social functioning. Journal of Affective Disorders Reports. 2023;14:100631. https://doi.org/10.1016/j.jadr.2023.100631 .
Hammen C. Risk factors for depression: an autobiographical review. Annu Rev Clin Psychol. 2018;14:1–28. https://doi.org/10.1146/annurev-clinpsy-050817-084811 .
McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psycholog Med. 2010;40(10):1647–58. https://doi.org/10.1017/S0033291709992121 .
Article CAS Google Scholar
Chang JJ, Ji Y, Li YH, Yuan MY, Su PY. Childhood trauma and depression in college students: Mediating and moderating effects of psychological resilience. Asian J Psychiatr. 2021;65:102824. https://doi.org/10.1016/j.ajp.2021.102824 .
Pirdehghan A, Vakili M, Rajabzadeh Y, Puyandehpour M, Aghakoochak A. Child abuse and mental disorders in Iranian adolescents. Iranian J Pediatr. 2016;26(2):e3839. https://doi.org/10.5812/ijp.3839 . Published 2016 Jan 30.
Wang ZC. Childhood abuse and adolescent depression: moderating roles of social support and friendship quality. Soc Behav Personality. 2023;51(1):1. https://doi.org/10.2224/sbp.12136 .
VanMeter F, Nivison MD, Englund MM, Carlson EA, Roisman GI. Childhood abuse and neglect and self-reported symptoms of psychopathology through midlife. Dev Psychol. 2021;57(5):824–36. https://doi.org/10.1037/dev0001169 .
Zhou X, Zhen R. How do physical and emotional abuse affect depression and problematic behaviors in adolescents? The roles of emotional regulation and anger. Child Abuse Negl. 2022;129:105641. https://doi.org/10.1016/j.chiabu.2022.105641 .
McCrory EJ, Gerin MI, Viding E. Annual research review: childhood maltreatment, latent vulnerability and the shift to preventative psychiatry - the contribution of functional brain imaging. J Child Psychol Psychiatry. 2017;58(4):338–57. https://doi.org/10.1111/jcpp.12713 .
Diaz A, Shankar V, Nucci-Sack A, Linares LO, Salandy A, Strickler HD, et al. Effect of child abuse and neglect on risk behaviors in inner-city minority female adolescents and young adults. Child Abuse Negl. 2020;101:104347. https://doi.org/10.1016/j.chiabu.2019.104347 .
Liang JY, Zhuo YS, Li XR, Qin F. Structural equation model of childhood psychological abuse and neglect,psychologica resilience, life satisfaction and mobile phone addiction in medical students. Occupation and Health. 2020;19:36–19.
Google Scholar
Christ SL, Kwak YY, Lu T. The joint impact of parental psychological neglect and peer isolation on adolescents’ depression. Child Abuse Negl. 2017;69:151–62. https://doi.org/10.1016/j.chiabu.2017.04.015 .
Suh JJ, Ruffins S, Robins CE, Albanese MJ, Khantzian EJ. Self-medication hypothesis: connecting affective experience and drug choice. Psychoanal Psychol. 2008;25(3):518–32. https://doi.org/10.1037/0736-9735.25.3.518 .
Holden C. “Behavioral” Addictions: Do They Exist? Science (New York, NY). 2001;294(5544):980–2. https://doi.org/10.1126/science.294.5544.980 .
Article CAS PubMed Google Scholar
Young KS, Rogers RC. The relationship between depression and Internet addiction. Cyberpsychol Behav. 1998;1(1):25–8. https://doi.org/10.1089/cpb.1998.1.25 .
Yang M, Sheng XL, Ge ML, Zhang L, Huang C, Cui S, et al. Childhood trauma and psychological sub-health among Chinese adolescents: the mediating effect of Internet addiction. BMC Psychiatry. 2022;22(1):762. https://doi.org/10.1186/s12888-022-04384-2 . Published 2022 Dec 5.
Peng C, Wang MN, Cheng JH, Tan YF, Huang YX, Rong FJ, et al. Mediation of Internet addiction on association between childhood maltreatment and suicidal behaviours among Chinese adolescents. Epidemiol Psychiatric Sci. 2021;30:e64.
Dong X, Zhang RX, Zhornitsky S, Le TM, Wang WY, et al. Depression mediates the relationship between childhood trauma and internet addiction in female but not male chinese adolescents and young adults. J Clin Med. 2021;10(21):5015. https://doi.org/10.3390/jcm10215015 . Published 2021 Oct 28.
Valkenburg PM, Peter J. Social consequences of the internet for adolescents: a decade of research. Curr Dir Psychol Sci. 2009;18(1):1–5. https://doi.org/10.1111/j.1467-8721.2009.01595.x .
Saikia AM, Das J, Barman P, Bharali MD. Internet Addiction and its relationships with depression, anxiety, and stress in urban adolescents of Kamrup District, Assam. J Family Commun Med. 2019;26(2):108–12. https://doi.org/10.4103/jfcm.JFCM_93_18 .
Zhao M, Huang YL, Wang JY, Feng J, Zhou B. Internet addiction and depression among Chinese adolescents: anxiety as a mediator and social support as a moderator. Psychol Health Med. 2023;28(8):2315–28. https://doi.org/10.1080/13548506.2023.2224041 .
Yang X, Guo WJ, Tao YJ, Meng YJ, Wang HY, Li XJ, et al. A bidirectional association between internet addiction and depression: a large-sample longitudinal study among Chinese university students. J Affect Disord. 2022;299:416–24. https://doi.org/10.1016/j.jad.2021.12.013 .
Hall JA, Liu D. Social media use, social displacement, and well-being. Curr Opin Psychol. 2022;46:101339. https://doi.org/10.1016/j.copsyc.2022.101339 .
Kraut R, Kiesler S, Boneva B, Cummings JN, Helgeson V, Crawford AM. Internet paradox revisited. J Soc Issues. 2002;58(1):49–74. https://doi.org/10.1111/1540-4560.00248 .
de Timary P, Luts A, Hers D, Luminet O. Absolute and relative stability of alexithymia in alcoholic inpatients undergoing alcohol withdrawal: relationship to depression and anxiety. Psychiatry Res. 2008;157(1–3):105–13. https://doi.org/10.1016/j.psychres.2006.12.008 .
Hesse C, Floyd K. Affectionate experience mediates the effects of alexithymia on mental health and interpersonal relationships. J Soc Pers Relat. 2008;25(5):793–810. https://doi.org/10.1177/0265407508096696 .
Preece DA, Becerra R, Robinson K, Allan A, Boyes M, Chen W, et al. What is alexithymia? Using factor analysis to establish its latent structure and relationship with fantasizing and emotional reactivity. J Pers. 2020;88(6):1162–76. https://doi.org/10.1111/jopy.12563 .
De Berardis D, Campanella D, Gambi F, La Rovere R, Sepede G, Core L, et al. Alexithymia, fear of bodily sensations, and somatosensory amplification in young outpatients with panic disorder. Psychosomatics. 2007;48(3):239–46. https://doi.org/10.1176/appi.psy.48.3.239 .
Lee BW, Stapinski LA. Seeking safety on the internet: relationship between social anxiety and problematic internet use. J Anxiety Disord. 2012;26(1):197–205. https://doi.org/10.1016/j.janxdis.2011.11.001 .
Babadi-Akashe Z, Zamani BE, Abedini Y, Akbari H, Hedayati N. The relationship between mental health and addiction to mobile phones among university students of shahrekord. Iran Addict Health. 2014;6(3–4):93–9.
De Berardis D, D’Albenzio A, Gambi F, Sepede G, Valchera A, Conti CM, et al. Alexithymia and its relationships with dissociative experiences and Internet addiction in a nonclinical sample. Cycberpsychol Behav. 2009;12(1):67–9. https://doi.org/10.1089/cpb.2008.0108 .
Taylor GJ, Bagby RM, Parker JD. The alexithymia construct. A potential paradigm for psychosomatic medicine. Psychosomatics. 1991;32(2):153–64. https://doi.org/10.1016/s0033-3182(91)72086-0 .
de Timary P, Roy E, Luminet O, Fillée C, Mikolajczak M. Relationship between alexithymia, alexithymia factors and salivary cortisol in men exposed to a social stress test. Psychoneuroendocrino. 2008;33(8):1160–4.
Nekouei ZK, Doost HT, Yousefy A, Manshaee G, Sadeghei M. The relationship of Alexithymia with anxiety-depression-stress, quality of life, and social support in coronary heart disease (A psychological model). J Educ Health Promot. 2014;3:68. https://doi.org/10.4103/2277-9531.134816 . Published 2014 Jun 23.
Preece DA, Mehta A, Petrova K, Sikka P, Bjureberg J, Becerra R, et al. Alexithymia and emotion regulation. J Affect Disord. 2023;324:232–8. https://doi.org/10.1016/j.jad.2022.12.065 .
Brewer R, Cook R, Bird G. Alexithymia: a general deficit of interoception. Royal Soc Open Sci. 2016;3(10):150664. https://doi.org/10.1098/rsos.150664 . Published 2016 Oct 12.
Herbert BM, Herbert C, Pollatos O. On the relationship between interoceptive awareness and alexithymia: is interoceptive awareness related to emotional awareness? J Person. 2011;79(5):1149–75. https://doi.org/10.1111/j.1467-6494.2011.00717.x .
Shah P, Hall R, Catmur C, Bird G. Alexithymia, not autism, is associated with impaired interoception. Cortex. 2016;81:215–20. https://doi.org/10.1016/j.cortex.2016.03.021 .
Carta MG, Sancassiani F, Pippia V, Bhat KM, Sardu C, Meloni L. Alexithymia is associated with delayed treatment seeking in acute myocardial infarction. Psychother Psychosom. 2013;82(3):190–2. https://doi.org/10.1159/000341181 .
Lyvers M, Duric N, Thorberg FA. Caffeine use and alexithymia in university students. J Psychoact Drugs. 2014;46(4):340–6. https://doi.org/10.1080/02791072.2014.942043 .
Thomée S. Mobile phone use and mental health. A review of the research that takes a psychological perspective on exposure. Int J Environ Res Public Health. 2018;15(12):2692. https://doi.org/10.3390/ijerph15122692 . Published 2018 Nov 29.
Thomée S, Härenstam A, Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults–a prospective cohort study. BMC Public Health. 2011;11:66. https://doi.org/10.1186/1471-2458-11-66 . Published 2011 Jan 31.
Zhao XF, Zhang YL, Li LF, Zhou YF, Li HZ. Reliability and validity of the Chinese version of childhoodtrauma questionnaire. Chin J Clin Rehab. 2005;20:105–7.
Gong X, Xie XY, Xu R, Luo YJ. Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chin J Clin Psychol. 2010;18(04):443–6. https://doi.org/10.16128/j.cnki.1005-3611.2010.04.020 .
Wei Q. Negative Emotions and Problematic Social NetworkSites Usage: The Mediating Role of Fear of Missing Outand the Moderating Role of Gender [Master’s thesis]: Central China Normal University. 2018.
Cerutti R, Calabrese M, Valastro C. Alexithymia and personality disorders in the adolescent non-suicidal self injury: preliminary results. Procedia Soc Behav Sci. 2014;114:372–6. https://doi.org/10.1016/j.sbspro.2013.12.714 .
Chung MC, Chen ZS. Gender differences in child abuse, emotional processing difficulties, alexithymia, psychological symptoms and behavioural problems among chinese adolescents. Psychiatry Q. 2020;91(2):321–32. https://doi.org/10.1007/s11126-019-09700-w .
Kim HY. Statistical notes for clinical researchers: assessing normal distribution (2) using skewness and kurtosis. Restor Dentist Endodont. 2013;38(1):52–4. https://doi.org/10.5395/rde.2013.38.1.52 .
Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach: Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. 2013.
Podsakoff PM, Mackenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl psychol. 2003;88(5):879–903. https://doi.org/10.1037/0021-9010.88.5.879 .
Wan GW, Wang M, Chen ST. Child abuse in ethnic regions: evidence from 2899 girls in Southwest China. Child Youth Serv Rev. 2019;105:104457. https://doi.org/10.1016/j.childyouth.2019.104457 .
Shen LJ, Zhang YL, Liang W, Zhang YL. Investigation of child maltreatment: Survey among junior school pupils in Henan province of China. Asia-Pacific Psychiatry. 2015;7(1):85–90. https://doi.org/10.1111/appy.12105 .
Gao YJ, Atkinson-Sheppard S, Liu X. Prevalence and risk factors of child maltreatment among migrant families in China. Child Abuse Negl. 2017;65:171–81. https://doi.org/10.1016/j.chiabu.2017.01.023 .
Qi D, Wang YJ, Wan GW. The severity, consequences and risk factors of child abuse in China - an empirical Study of 5836 children in China’s mid-western regions. Child Youth Serv Rev. 2018;95:290–9. https://doi.org/10.1016/j.childyouth.2018.10.039 .
Witt A, Brähler E, Fegert JM. Words don’t hurt? Consequences of psychological abuse. Monatsschr Kinderh. 2021;169(7):613–21.
Sheikh MA. Psychological abuse, substance abuse distress, dissatisfaction with friendships, and incident psychiatric problems. J Psychosom Res. 2018;108:78–84. https://doi.org/10.1016/j.jpsychores.2018.03.001 .
Spann MN, Mayes LC, Kalmar JH, Guiney J, Womer FY, Pittman B, et al. Childhood abuse and neglect and cognitive flexibility in adolescents. Child neuropsychology. 2012;18(2):182–9. https://doi.org/10.1080/09297049.2011.595400 .
Güleç MY, Altintas M, Inanç L, Bezgin ÇH, Koca EK, Guleç H. Effects of childhood trauma on somatization in major depressive disorder: the role of alexithymia. J Affect Dis. 2013;146(1):137–41. https://doi.org/10.1016/j.jad.2012.06.033 .
Paul E, Eckenrode J. Childhood psychological maltreatment subtypes and adolescent depressive symptoms. Child Abuse Negl. 2015;47:38–47. https://doi.org/10.1016/j.chiabu.2015.05.018 .
Steinberg L. We know some things: parent-adolescent relationships in retrospect and prospect. J Res Adolesc. 2001;11(1):1–19. https://doi.org/10.1111/1532-7795.00001 .
Karelina K, DeVries AC. Modeling social influences on human health. Psychosom Med. 2011;73(1):67–74. https://doi.org/10.1097/PSY.0b013e3182002116 .
Chegeni M, Nakhaee N, Shahrbabaki PM, Shahrbabaki ME, Haghdoost A. Does childhood trauma associate with social media addiction? A cross-sectional study from Iran. Int J Ment Heal Addict. 2023;21(4):2225–37. https://doi.org/10.1007/s11469-021-00718-5 .
Sheng XL, Yang M, Ge ML, Zhang L, Huang C, Cui S, et al. The relationship between internet addiction and childhood trauma in adolescents: the mediating role of social support. Front Psychol. 2022;13:996086. https://doi.org/10.3389/fpsyg.2022.996086 . Published 2022 Oct 5.
Lau J, Walden DL, Wu A, Cheng KM, Lau M, Mo P. Bidirectional predictions between Internet addiction and probable depression among Chinese adolescents. J Behav Addict. 2018;7(3):633–43. https://doi.org/10.1556/2006.7.2018.87 .
Hirschi T. Theory Without Ideas: reply to Akers. Criminology. 2010;34(2):249–56. https://doi.org/10.1111/j.1745-9125.1996.tb01205.x .
Lam LT, Peng ZW. Effect of pathological use of the internet on adolescent mental health: a prospective study. Arch Pediatr Adolesc Med. 2010;164(10):901–6. https://doi.org/10.1001/archpediatrics.2010.159 .
Li W, Garland EL, Howard MO. Family factors in internet addiction among Chinese youth: a review of English- and Chinese-language studies. Comput Human Behav. 2014;31(feb.):393–411. https://doi.org/10.1016/j.chb.2013.11.004 .
Agnew R. Foundation for a general strain theory of crime and delinquency. Criminology. 1992;30(1):47–87. https://doi.org/10.1111/j.1745-9125.1992.tb01093.x .
Kardefelt-Winther DA. conceptual and methodological critique of internet addiction research: towards a model of compensatory internet use. Comput Hum Behav. 2014;31:351–4. https://doi.org/10.1016/j.chb.2013.10.059 .
Xiao W, Zhou H, Li X, Lin X. Why are individuals with alexithymia symptoms more likely to have mobile phone addiction? the multiple mediating roles of social interaction anxiousness and boredom proneness. Psychol res Behav Manag. 2021;14:1631–41. https://doi.org/10.2147/PRBM.S328768 . Published 2021 Oct 8.
Craig AD. How do you feel–now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10(1):59–70. https://doi.org/10.1038/nrn2555 .
Craig AD. Interoception: the sense of the physiological condition of the body. Curr Opin Neurobiol. 2003;13(4):500–5. https://doi.org/10.1016/s0959-4388(03)00090-4 .
Bush G, Luu P, Posner MI. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4(6):215–22. https://doi.org/10.1016/s1364-6613(00)01483-2 .
Lindquist KA, Wager TD, Kober H, Bliss-Moreau E, Barrett LF. The brain basis of emotion: a meta-analytic review. Behav Brain Sci. 2012;35(3):121–43. https://doi.org/10.1017/S0140525X11000446 .
Ihme K, Dannlowski U, Lichev V, Stuhrmann A, Grotegerd D, Rosenberg N, et al. Alexithymia is related to differences in gray matter volume: a voxel-based morphometry study. Brain Res. 2013;1491:60–7. https://doi.org/10.1016/j.brainres.2012.10.044 .
Goerlich-Dobre KS, Bruce L, Martens S, Aleman A, Hooker CI. Distinct associations of insula and cingulate volume with the cognitive and affective dimensions of alexithymia. Neuropsychologia. 2014;53:284–92. https://doi.org/10.1016/j.neuropsychologia.2013.12.006 .
Moriguchi Y, Decety J, Ohnishi T, Maeda M, Mori T, Nemoto K, et al. Empathy and judging other’s pain: an fMRI study of alexithymia. Cerebral cortex (New York, NY 1991). 2007;17(9):2223–34. https://doi.org/10.1093/cercor/bhl130 .
Download references
Acknowledgements
Zirui Zhou, Shiju Zhu.
Not applicable.
Author information
Yang Liu, Qingxin Shen and Liangfan Duan these authors have contributed equally to this work and share first authorship.
Authors and Affiliations
School of Sports Science, Jishou University, Jishou, China
Yang Liu, Qingxin Shen, Liangfan Duan, Lei Xu, Yongxiang Xiao & Tiancheng Zhang
Institute of Physical Education, Shanxi University of Finance and Economics, Taiyuan, China
You can also search for this author in PubMed Google Scholar
Contributions
Author statement: Yang Liu12345, Qingxin Sheng12345, Liangfan Duan12345, Lei Xu156, Yongxiang Xiao15, Tiancheng Zhang156. 1 Conceptualization; 2 Methodology; 3 Data curation; 4 Writing—Original Draft; 5 Writing—Review &; Editing; 6 Funding acquisition.
Corresponding author
Correspondence to Tiancheng Zhang .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Biomedicine Ethics Committee of Jishou University before the initiation of the project (Grant number: JSDX-2023–0034). And informed consent was obtained from the participants before starting the program.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Liu, Y., Shen, Q., Duan, L. et al. The relationship between childhood psychological abuse and depression in college students: a moderated mediation model. BMC Psychiatry 24 , 410 (2024). https://doi.org/10.1186/s12888-024-05809-w
Download citation
Received : 15 March 2024
Accepted : 02 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12888-024-05809-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Childhood psychological abuse
- College students
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 30 May 2024
Treating depression in patients with borderline personality disorder: clinical clues on the use of antidepressants
- Carmine Tomasetti 1 ,
- G. Autullo 2 ,
- A. Ballerini 3 ,
- A. de Bartolomeis 4 ,
- B. Dell’Osso 5 ,
- A. Fiorentini 6 ,
- F. Tonioni 7 ,
- V. Villari 2 &
- D. De Berardis 8
Annals of General Psychiatry volume 23 , Article number: 21 ( 2024 ) Cite this article
114 Accesses
Metrics details
Personality disorders (PD) are described as enduring patterns of markedly deviant and pervasive inner experiences and behaviors, with onset in adolescence, which lead to severe distress or impairment. Patients suffering from major depressive disorder (MDD) display higher rates of comorbidity with personality disorders, often complicating the treatment, and worsening the outcomes. Borderline personality disorder (BPD) is the most common of PD and is frequently associated with MDD, with which shares several features. The most part of research agrees on the fact that comorbid BPD in MDD patients quite doubles the poor response to treatments. Moreover, no treatment strategy stands out currently to emerge as more effective in these cases, thus urging the call for the need of new approaches. Herein, we revise the current literature on BPD, its neurobiology and comorbidity with MDD, as well as the more recent treatment strategies used. Then, based on its pharmacology, we propose a possible role of trazodone as a valuable tool to approach comorbid BPD-MDD.
Introduction
Major Depressive Disorder (MDD) is a leading contributor to global burden of disease, being considered as a major cause of disability worldwide, with approximately 3.8% of population affected and over 700.000 people dying of suicide every year [ 1 ]. Despite multiple treatment strategies have been developed, MDD remains a serious challenge for psychiatrists, since approximate 30% of patients do not adequately respond to therapies. The largest MDD trial, the so-called STAR*D (Sequenced Treatment Alternatives to Relieve Depression), demonstrated that, even after 4 consequential steps of treatment, the cumulative remission rate reached 67% after 14 months [ 2 ].
Since MDD is a heterogeneous disorder, multiple reasons have been put forward to support these high rates of treatment resistance: misdiagnosis (e.g., bipolar depression, or mixed states); comorbid substance use; untreated medical conditions (e.g., dysthyroidism); undiagnosed underlying traumata (i.e., post-traumatic stress disorder); cognitive impairment (i.e., neurocognitive disorders) [ 3 ].
In addition to the above-mentioned contributors, a large body of evidence points out the essential role of underpinning and/or understated personality disorders (PD) in the scarce responsivity of MDD to treatments. PDs comorbidity has been recognized in almost half of MDD patients in different meta-analyses [ 4 , 5 ]. Indeed, the pervasive symptoms of PDs, such as low self-esteem, self-criticism, mood instability, feeling of emptiness or hopelessness, suicidal thoughts or behaviors, may all represent substantial contributors to worsen or complicate depression, or even to make depressive symptoms persistent and resistant [ 6 ]. Several studies have examined the relationships amongst personality disorders traits and the quality, the severity, and the outcomes of MDD [ 7 , 8 ]. Personality disorders have been correlated to earlier onset of MDD, to specific subtypes of depression (melancholic vs. non melancholic depression) [ 5 ], as well as to severer symptoms (i.e., suicidal behaviors, self-harming, impaired cognition), and poorer outcomes (e.g., greater resistance to pharmacological and non-pharmacological treatments) [ 9 ]. Thus, the frequent association between PDs and MDD poses the classical question whether came first the chicken or the egg, since from a psychological point of view some predisposing risk factors may be associated to both the conditions [ 10 ]. Moreover, given this entangled relationship, a diagnostic issue should be considered, when assessing a patient with MDD; but, more important, a complete revision of therapeutic approaches to the treatment of depression should be contemplated, based on the possible influence of underlying preponderant personality traits in depressed patients.
In the next sections, we will consider the impact of the most devastating PD, the Borderline Personality Disorder, on MDD, and we will discuss the possible revision of classical antidepressant treatments in the light of an integrated neurobiological-psychological approach to MDD therapy.
The influence of comorbid Borderline Personality Disorder on Major Depressive Disorder
Borderline Personality Disorder (BPD) is described in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition, text revision 2022, (DSM-5-TR) [ 11 ] as a “pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, beginning by early adulthood and present in a variety of contexts”. Sensation of abandonment, unstable relationships, identity disturbances, impulsivity, recurrent suicidal behaviors, affective instability, feelings of emptiness, anger and, occasionally, transient dissociative or psychotic symptoms during periods of distress may be all features of BPD. All these features can be grouped in three main categories (“factors”, according to DSM-5-TR): disturbed relatedness, behavioral dysregulation, and affective dysregulation; all of these being strongly correlated with each others, thus representing a unique construct, although with broad and pleiotropic manifestations [ 12 ]. BPD is the most common PD, with a reported prevalence of 10% in all psychiatric outpatients [ 13 ], and 5.9% in non-clinical population [ 14 ]. Moreover, the most part of BPD patients seem not to access psychiatric care, but they represent a significant part of primary care patients, since BPD has been described as four-times more prevalent amongst general practitioners’ costumers as compared to general population [ 15 ].
Several studies have reported a high frequency of co-occurrence between BPD and MDD, since 83–85% of BPD patients have been described to suffer from MDD episodes, with high recurrences [ 16 , 17 , 18 ]. Moreover, amongst PDs, BPD seems to have the highest correlation with both genetic and environmental risk factors of MDD [ 19 ].
Manifold studies have tried to dig up the intrinsic connections between BPD and MDD, and just as many theories and models have been developed, with the precise aim to improve diagnosis and therapy of these disorders, above all when comorbid. Personality has been characteristically described as a dynamic construct of two main components: temperament, the biologically-based structure of emotion regulation, and character, which instead is modulated by social relations [ 20 ]. According to the Five Factors Model (FFM), personality traits may be taxonomically subdivided in five principal characteristics, the so-called Big Fives: neuroticism, extraversion, conscientiousness, agreeableness, and openness to experience. Given the hierarchical relationships amongst these factors, they may be further grouped in two big clusters: positive emotionality and negative emotionality [ 21 ]. There is increasing evidence that, although personality traits have solid genetical and biological bases, they are not rigid constructs, but may be dynamically modulated by development and life experiences [ 22 ]. Psychologically, MDD is characterized by a substantial deficiency in positive emotionality, with a prevalence of negative emotions, such as sadness, guilt, shame, anhedonia, depressed mood, and numbness (i.e., the inability of feeling feelings) [ 23 ]. However, it is not rare that MDD patients may manifest irritability, anger, hostility, which are all factors often correlated to self-harming or suicide [ 24 , 25 ]. By contrast, the whole symptomatologic cortege of BPD is mainly hinged on impulsivity traits, with emotional dysregulation, anger, dyscontrol, dysphoria, self-harming, and hostility [ 26 ]. Nevertheless, some typical features of BPD may resemble those seen in MDD patients, such as the feeling of emptiness, sadness, loneliness of hopelessness [ 27 ].
Therefore, BPD may add an “impulsivity color” to MDD symptoms framework, when the two disturbs manifest comorbidly. Different studies, indeed, reported that BPD patients experiencing MDD show increased levels of anger, fear, and hostility [ 28 ], as well as they manifest considerably higher impulsivity than MDD-only patients [ 29 ]. Moreover, BPD patients diagnosed with MDD tend to describe their depressive symptoms as more serious as compared to MDD-only patients, even severer than those objectively assessed by physicians [ 30 , 31 ].
Notably, BPD has been demonstrated to show significant comorbidity also with Bipolar Disorder (BD). Indeed, by analyzing data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), McDermid et al. found that the lifetime prevalence of BPD was about 29% in BD type I and 24% in BD type II, and that comorbid BPD-BD had severer presentation as compared to BD alone [ 32 ]. Successive studies confirmed that BPD may represent a risk factor for BD, and remarked the negative impact of BPD in BD, such as the higher prevalence of suicidality and the treatment-resistance [ 33 ]. Moreover, about 40% of MDD-diagnosed patients have been reported to have a history of subthreshold hypomania symptoms, this subgroup showing earlier onset and more episodes of depression, as well as more comorbidities as compared to non-hypomanic patients [ 34 ]. Last, MDD episodes where psychomotor agitation and racing thoughts are found (the so-called “agitated depression”) have been robustly associated to mixed states, unfavorably predicting the emergence of suicidal ideation and contraindicating antidepressant therapy [ 35 ]. This tight intermingling between hypomanic symptoms, MDD, and BPD may challenge the dichotomic vision of unipolar-bipolar depression, suggesting a more comprehensive “mood spectrum” diagnostic approach [ 36 ].
Thus, it is possible that the inherent “bipolarity” of BPD may colorize MDD with unstable emotional traits, lending this disorder an increased resistance to treatments, as compared to MDD alone. The Collaborative Longitudinal Personality Disorders Study (CLPS) analyzed the longitudinal course of BPD patients, as compared to other PDs and MDD-only patients [ 37 ]. Amongst the other interesting results, CLPS reported that 80% of BPD patients assessed had MDD, and that MDD-only patients showed a remission rate dramatically faster (80% by 1 year) as compared to BPD patients (30% by one year), thus indicating how much BPD comorbidity may influence MDD outcome. These results have been confirmed by the National Epidemiological Study of Alcoholism and Related Disorders, which reported that BPD was the major predictor of persistent MDD [ 38 ]. The McLean Study of Adult Development (MSAD) further demonstrated that, when BPD and MDD coexist, the remission of MDD strictly depends upon the remission of BPD symptoms [ 39 ], thus confirming a previous landmark study, in which an improvement in MDD symptoms was found when treating BPD symptoms, but not vice versa [ 40 ]. However, the mainstay treatment for MDD, antidepressant drugs, have been demonstrated to promote only partial responses in MDD-BPD patients [ 39 ]. Thus, there is a peculiar tendence to poly-treat BPD patients, which have been described to averagely take three-to-five medications, an over-prescription that could be only reduced by a BPD-specific psychotherapy regimens [ 41 ]. Also, non-pharmacological treatments, such as electroconvulsive therapy (ECT) and transcranial magnetic stimulation (TMS) have demonstrated partial efficacy in treating comorbid MDD and BPD [ 42 , 43 ]. Therefore, it appears rather obvious that the treatment of MDD in course of BPD relies on an efficacious BPD treatment. Hence, some specific psychotherapy regimens, such as Dialectical behavioral therapy (DBT) have demonstrated a good efficacy in improve MDD symptoms by improving BPD [ 44 ].
So, is there a biological basis on which the BPD-induced MDD treatment-resistance relies? And, in the light of this possible underlying basis, should it be possible to reconsider a targeted pharmacological approach to help reducing the impact of BPD on MDD?
Digging in the deep: the neurobiological bases of BPD and the underpinnings of comorbid MDD
Although BPD has been classically envisioned as a complex multifactorial disorder, in which environmental risk factors (e.g., traumata, abuses, neglect) seems to be preponderantly responsible for its development [ 45 ], increasing evidence has been pointing out the essential role of the genetic factors underlying the specific personality traits at the basis of the disorder. Indeed, twin studies have demonstrated that BPD has a heritability ranging from 46 to 69% [ 46 , 47 ]. Recently, different genome-wide association studies (GWAS) have been performed, in order to study genetic association of the “Big Five” factors of FFM with PDs in general population. BPD was found closely associated with personality traits of neuroticism and openness [ 48 ], and, more interestingly, it was reported to share positive genetic correlations with MDD, Bipolar Disorder and Schizophrenia [ 49 ]. As above-mentioned, BPD represents a unique construct intermingling specific personality traits, such as disturbed relatedness, behavioral and emotional dysregulation. However, despite the manifold researches stating the large heritability of BPD, only a few genetic studies exist, which tried to correlate these personality traits to specific gene dysfunctions. As previously mentioned, Witt and collaborators found a significant overlap of BPD-associated genes with those associated to MDD, Bipolar Disorder and Schizophrenia [ 49 ]. Two genes reached genome-wide significance: dihydropyrimidine dehydrogenase (DPYD) and Plakophilin-4 (PKP4). DPYD is implicated in pyrimidine metabolism and contains a binding site for the micro-RNA miR-137, which has been found associated to Schizophrenia [ 50 ]. PKP4 is involved in the regulation of cell adhesion and cytoskeletal modifications, which have been substantially implicated in cell junction deficits associated to MDD [ 51 ]. Previously, Lubke et al. have described a specifical association of BPD with the serine incorporator 5 gene (SERINC5), which seems to have a peculiar role in myelination, and has been involved in the development of psychiatric disorders characterized by lack of social interactions [ 52 , 53 ]. Finally, a genome-wide linkage study found a significant association of BPD features with chromosome 9 loci, which have been significantly associated also to Bipolar Disorder and Schizophrenia [ 54 ].
Given the essential role of environment in BPD development, it is not surprising that a large number of studies have reported abnormalities in BPD in epigenetic modifications, which are considered the “portal” through which environment may impact gene expression changes, via DNA methylation, histone deacetylation and non-coding RNA silencing [ 55 ]. Altered methylation of specific genes, such as dopamine D2 receptors, serotonin 3A receptors, glucocorticoid receptors and brain-derived neurotrophic factor (BDNF) receptors have been all associated to BPD [ 56 , 57 , 58 , 59 ]. It is interesting to note that these alterations may be directly correlated to the severity of childhood abuse in BPD patients [ 60 ], as well as to the intensity of depressive symptoms, and may be reinstated by specific psychotherapy regimens [ 61 ].
As already discussed, the core symptoms of BPD rely on a substantial emotional dysregulation. Different studies reported altered emotional interoception in BPD patients, the so-called alexithymia (i.e., “no words for emotions”): while their amygdaloid system highly responds to negative emotions, they have a blunted self-report of the experienced emotions [ 62 ]. This may be due to an altered regulatory control of amygdala-based emotion system: indeed, BPD patients have been described to have altered connections between prefrontal cortex and amygdala, thus probably having an impaired top-down emotional modulation [ 63 ]. Moreover, both substance use, and dissociative episodes have been reported to dampen the hyperactive emotional responses in BPD patients, thereby explaining the frequent comorbidity of BPD with substance use disorder (SUD), as well as the higher frequency of dissociative experiences in BPD patients [ 64 , 65 ]. Interestingly, altered amygdaloid responses and neuroplasticity have been demonstrated in MDD patients [ 66 ]. Moreover, a particular kind of treatment-resistant depression, called “dissociative depression”, has been characterized as frequent in younger patients with childhood traumata, and is defined by the higher frequency in dissociative episodes, as well as by its chronicity, mood instability, and often by comorbid BPD [ 67 ]. Finally, SUD is frequently diagnosed also in MDD patients, and some etiopathogenetic models propose that substances may help depressed patients to cope with their altered affective states [ 68 ].
Besides emotional dysregulation, as previously mentioned, BPD patients experience an essential disrupted relatedness, with interpersonal sensitivity leading to social difficulties.
Several studies have associated BPD social dysfunctionality to altered opioidergic and neuropeptidergic neurotransmission. Primarily, opioidergic neurotransmission is correlated in humans with pain responses. Increasing evidence suggests that µ-opioid receptors may mediate both sensory and affective dimension of pain, in different cerebral regions [ 69 ]; moreover, pain may be literally perceived in social exclusion and rejection by means of µ-opioid mediation in brain [ 70 , 71 ]. BPD patients have been demonstrated to possess a lower sensitivity to acute pain, but a heightened sensitivity to chronic pain [ 72 , 73 ]. This altered sensitivity to pain may be essentially due to an abnormal µ-opioid transmission: indeed, BPD patients have been demonstrated to possess a greater number of cortical µ-opioid receptors, probably due to a scarce baseline opioidergic transmission, with altered and enhanced compensatory opioid responses to acute stimuli [ 74 ]. Besides its primary role in pain responses modulation, µ-opioid neurotransmission has been associated to the right development of attachment behaviors in mammals [ 75 , 76 ]. Interestingly, altered µ-opioid gene expression has been found in adolescents prone to develop MDD reactions to social rejection life events [ 77 ].
Oxytocinergic neurotransmission has been also found abnormal in BPD patients, which were reported to have lower levels of oxytocin as compared to healthy individuals, these levels being correlated with childhood traumata and disrupted attachment [ 78 , 79 ]. Moreover, while in healthy subjects oxytocin administration usually enhances social behaviors, in BPD patients it may provoke counterintuitive aversive behaviors, especially correlated to history of childhood traumata [ 80 ]. Last, genetic alterations in oxytocin receptors have been directly correlated to the development of BPD in abused children [ 81 , 82 ]. The increasing evidence of a substantial role of oxytocin in the etiopathogenesis of MDD, as well as in its possible treatments, represents a further bridge between BPD and MDD [ 83 , 84 ].
Monoaminergic neurotransmission has been implicated in personality since long ago. Particularly, personality dimensions as described by Cloninger, and later by the FFM, may be directly linked to dopaminergic, serotonergic, and noradrenergic neurotransmissions [ 85 , 86 , 87 ].
Dopamine dysfunctions, for example, have been associated to three specific dimensions of BPD: impulsivity, emotional dysregulation, and cognitive impairment [ 88 ]. Specific genetic polymorphisms of the dopamine transporter gene (DAT1) have been peculiarly associated with increased risk of BPD in MDD patients [ 89 ]. Moreover, the same polymorphism has been associated to angry-impulsive traits in comorbid BPD-MDD patients [ 90 ]. On the other hand, both serotonin transporter (5HTT) and serotonin A1 receptor (5HT1A) genes have been associated with BPD [ 91 , 92 ]. Specifically, 5HT1A gene alterations have ben correlated to abnormal amygdala structure and emotional responses in BPD-MDD comorbid patients [ 91 ]. Serotonin alterations seem to be tightly correlated to the “impulsivity color” of MDD, when comorbid with BPD, as well as with an increased risk of suicide [ 93 , 94 ]. Recent studies demonstrated that serotonin and dopamine neurotransmissions closely interact in defining the personality traits underlying BPD, and the simultaneous presence of both dysfunctions may interplay in favoring the risk of BPD development [ 95 ]. Norepinephrine, along with cortisol, has been associated to dissociative responses in BPD [ 96 ].
Targeting depression in BPD: clinical clues on the use of antidepressants. Focus on trazodone
BPD patients, with their pleiotropic symptomatologic manifestations, represent a huge burden for health systems. In fact, as above mentioned, BPD is frequently associated to coexisting psychiatric disorders, above all MDD, anxiety, substance use, and it is as much as frequently misdiagnosed [ 97 ]. Due to their comorbidities, as well as to their over-endorsement of symptoms, BPD patients often tend to self-medicate (even with substances) or to access primary cares, where they are not often understood and well-treated [ 98 ]. Although BPD patients have been described to have good chances to remit over the long period [ 99 ], during the trajectory of the disorder, they have frequent relapses and serious outbursts, which lead to multiple accesses to mental health services for specialized cares or hospitalizations [ 100 ].
All the most recent guidelines for the treatment of BPD seems to agree on the fact that a specific regimen of psychotherapy should be the first line treatment, whereas medications should be used with caution for intense and disruptive symptoms during decompensation acuity, and only for the shortest possible time [ 101 , 102 , 103 , 104 ]. However, while European guidelines—which include NICE (National Institute for Health Care and Excellence) ones—suggest to pharmacologically treat only comorbid disorders in BPD [ 103 , 104 ], APA (American Psychiatric Association) and WFSBP (World Federation of Societies of Biological Psychiatry) suggest using specific classes of medications to treat specific symptom domains [ 101 , 102 ]: thus, antidepressants should be be used to treat emotional dysregulation and impulsivity, similarly to mood stabilizers, while antipsychotics should be used for dissociative and cognitive-perceptual symptoms.
Although scarce evidence exists on the efficacy of antidepressant treatments in BPD, SSRIs (Selective Serotonin Reuptake Inhibitors) are currently the most prescribed medications [ 105 ]. The most part of RCTs examining the efficacy of antidepressants in BPD are outdated, and they have not been replicated since 2010. The main antidepressants for which data are available in the treatment of BPD are: fluoxetine, fluvoxamine, sertraline, amitriptyline, phenelzine, venlafaxine, mianserin. A Cochrane review [ 106 ] reported that antidepressants had no significant effects on the overall BPD severity; no beneficial effects were noticed on impulsivity, as well as on suicidal behaviors, whereas a worsening of suicidal ideation was noticed with fluoxetine; affective instability was slightly ameliorated by fluvoxamine, while no significant effects were noticed for self-harming, feeling of emptiness, anger; the only significant effects on depression were found with amitriptyline.
Similar results were obtained in a comparative meta-analysis by Vita et al. [ 107 ], with a documented, although slight, effect of antidepressants only on affective dysregulation.
Significant results have been achieved on MDD comorbid to BPD when antidepressants were combined to mentalizing psychotherapies (DBT, IPT [Interpersonal Psychotherapy]) [ 108 , 109 ].
It is worth noting that all the antidepressant drugs chosen to be tested in BPD patients, as above described, were selected based on their well-documented efficacy on MDD, which is primarily due to serotonergic effects (i.e., serotonin re-uptake inhibition), with generally scarce impact on other neurotransmitters, such as dopamine or norepinephrine [ 110 ]. On the other hand, the most significant effects in reported RCTs were obtained by means of antidepressant drugs that involved more than the sole serotonin neurotransmission, such as phenelzine, amitriptyline and fluoxetine, or even by combined treatments (e.g. fluoxetine plus olanzapine), which were able to control—although slightly—the core affective/emotional instability, which is the typical signature of BPD [ 106 ].
As above described, BPD core depressive symptoms have been hypothesized to involve multiple neurobiological substrates, such as opioidergic and oxytocinergic neurotransmission, and specific monoamine receptors, such as dopamine D2 and serotonin 2A receptors, which interplay with each others to generate the symptoms of comorbid MDD-BPD. Thus, a more targeted pharmacological approach might help to relieve, if only partially, depressive symptoms in BPD.
In this light, a revision of “old” antidepressant treatments, relying on the enhancement of their possible efficacy, based on their peculiar pharmacodynamic properties, might represent a valuable approach. According to this view, trazodone may be a useful tool to address the unmet needs of MDD in BPD.
The history itself of trazodone appears intriguing, if envisioned in the light of the abovementioned neurobiological underpinnings of BPD. Indeed, it is a triazolopyridine derivative, which was developed in 1960s in Italy based on the “mental pain” hypothesis of MDD, correlating depressive states to altered pain interoception [ 111 ]. Along with nefazodone, trazodone represents the prototype of the so-called serotonin antagonist/reuptake inhibitor antidepressants (SARIs). It is a powerful antagonist at 5HT2A serotonin receptors, which are bound already at low doses, together with alpha1- and alpha2- adrenergic receptors and H1 histamine receptors, thus exerting potent anxiolytic and sedative/hypnotic effects at these doses [ 112 ]. Trazodone also weakly binds the serotonin transporter (SERT), 5HT2B and 5HT2C serotonin receptors, even if it is not clear if it acts as a full agonist, a partial agonist or an antagonist at these last receptors [ 112 ]. Another peculiar characteristic is the strong binding to 5HT1A serotonin receptors, where it acts as a partial agonist with high intrinsic activity [ 113 ]. Moreover, trazodone has an active metabolite, the meta-chlorophenylpiperazine (mCPP), which is known to exert pro-serotonergic psychoactive functions similar to fenfluramine and MDMA (“ecstasy”), in addition to being a well-recognized agonist to multiple serotonin receptors (e.g., 5HT1A, 5HT1B, 5HT1D, 5HT2A, 5HT2B, 5HT2C, 5HT3, and 5HT7 receptors) [ 114 , 115 ]. Thus, trazodone shapes up to be a peculiar multimodal antidepressant, which may exert differential functions at different doses. In fact, the progressive recruitment of serotonin receptors—in particular 5HT2A and 5HT1A—at incremental dosages has been described to exert incremental antidepressant effects by means of multiple—and not completely understood-- mechanisms: (1) 5HT1A receptors activation may mediate some neurotrophic factors’ genes expression, which has been associated to antidepressant actions; (2) 5HT1A receptors may progressively inhibit glutamate release from cortical pyramidal neurons, whose hyperactivity has been implicated in cognitive symptoms of MDD; (3) 5HT2A and 5HT2C serotonin receptors blockade has been associated to the increase in dopamine and noradrenaline cortical release, which are complementary to serotonin in relieving depressive symptoms [ 112 ].
Currently, trazodone is marketed in three different formulations: immediate release (IR), prolonged release (PR), and once-a-day extended release (OAD). Trazodone IR has a rapid plasma peak (1 h) and a short half-life (6.6 h); trazodone PR has a slower plasma peak (4 h) and a longer half-life (12 h), and trazodone OAD shows a plateau plasma level for the entire day, with longer antidepressant concentration as compared to the other formulations [ 113 ]. A large amount of data supports the fact that trazodone has similar efficacy to all the other antidepressants when compared to placebo [ 116 ]. Moreover, the OAD formulation has been described to grant a higher antidepressant efficacy than a placebo with a once-a-day administration, with side effects comparable to other antidepressants [ 117 ]. Finally, trazodone displays high tolerability, even when administered in patients with comorbid clinical conditions, thus granting a safety profile in poly-pharmaco-treated patients [ 118 ].
Several characteristics of trazodone may let lean forward its valuable use in comorbid BPD-MDD patients.
As previously described, the concurrent blockade of 5HT2A/2C receptors and of SERT, the partial agonist activity at 5HT1A receptors, and the antagonism at 5HT7 receptors may boost the antidepressant action of trazodone by increasing serotonin postsynaptic action and the subsequent disinhibition of dopamine and noradrenaline cortical release, together with glutamate-modulated neurotrophic factors’ gene expression [ 112 , 119 ]. Indeed, some studies have described the rapid onset of trazodone antidepressant effects. Sheehan et al. [ 117 ] demonstrated that trazodone OAD (150-225 mg/day) may induce a substantial reduction in depressive symptoms within a week of treatment, and that these effects may persist until 56 weeks. Fagiolini et al. [ 120 ] reported a faster antidepressant response (within 7 days) in patients treated with trazodone OAD (150 mg/die) as compared to venlafaxine XR (75 mg/die). This faster antidepressant effects of trazodone were not only exerted, as mainly expected, on the sleep component of depressive symptoms, but also on the cognitive aspects of depression [ 121 ].
The rapid antidepressant action of trazodone could be really useful during the fast emotional outbursts of BPD patients, which often lead to hospitalization. Peculiarly, this fast action seems not to be accompanied by a heightened risk of suicidal behaviors, even in high-risk patients treated with trazodone [ 122 ].
Trazodone has been demonstrated to exert antinociceptive effects even at low dosages, possibility via a µ-opioid receptors-mediated mechanism [ 123 , 124 ]. These properties may be helpful in manage the altered pain interoception of BPD patients—their “mental pain”—, as well as in treating their susceptibility to auto-medication with analgesics or substances. Indeed, diverse studies provided evidence of a good efficacy of trazodone in the treatment of alcohol, benzodiazepines, and opioid abuse [ 125 , 126 ].
The off-label clinical use of trazodone as hypnotic is well-established [ 126 ]. Some BPD patients have been described to have particularly disrupted sleep, with frequent nightmares, which in turn have been correlated to an increased risk of dissociative experiences and suicidal behaviors [ 127 ], above all if related to childhood traumatic events [ 128 ]. Trazodone has been demonstrated to be particularly effective in improving the quality of sleeping and reducing nightmares in post-traumatic stress disorders-affected war veterans [ 129 ].
Conclusions
BPD is a devastating personality disorder, with multiple symptomatologic presentations, and often comorbid with mood disorders, particularly with MDD, thereby making it substantially treatment resistant. SSRIs have been demonstrated to be scarcely efficacious on BPD-MDD patients. However, the neurobiological underpinnings of BPD may suggest that a more targeted antidepressant approach may helpful in relieving BPD-MDD coexisting symptoms. Since its multimodal action on serotonin, dopamine, noradrenalin, opioid and glutamate neurotransmissions, as well as its incremental effectiveness, trazodone seems to embody all the characteristics which may make it a clinical valuable tool to be used in BPD-MDD patients. More specifically designed studies are warranted to corroborate these clinical clues.
Data availability
No datasets were generated or analysed during the current study.
Institute of Health Metrics and Evaluation. Global Health Data Exchange (GHDx) [Internet]. [cited 2023 Feb 26]. https://vizhub.healthdata.org/gbd-results/ .
Pigott HE. The STAR*D Trial: It Is Time to Reexamine the Clinical Beliefs That Guide the Treatment of Major Depression. Can J Psychiatry [Internet]. 2015 [cited 2023 Mar 11];60:9. https:/pmc/articles/PMC4314062/.
Voineskos D, Daskalakis ZJ, Blumberger DM. Management of Treatment-Resistant Depression: Challenges and Strategies. Neuropsychiatr Dis Treat [Internet]. 2020 [cited 2023 Mar 14];16:221. /pmc/articles/PMC6982454/.
Zimmerman M, Rothschild L, Chelminski I. The prevalence of DSM-IV personality disorders in psychiatric outpatients. Am J Psychiatry. 2005;162:1911–8.
Article PubMed Google Scholar
Friborg O, Martinsen EW, Martinussen M, Kaiser S, Overgård KT, Rosenvinge JH. Comorbidity of personality disorders in mood disorders: a meta-analytic review of 122 studies from 1988 to 2010. J Affect Disord. 2014;152–154:1–11.
Young M, Treatment-Resistant, Depression. The importance of identifying and treating co-occurring personality disorders. Psychiatric clinics of North America. W.B. Saunders; 2018. pp. 249–61.
Pfohl B, Stangl D, Zimmerman M. The implications of DSM-III personality disorders for patients with major depression. J Affect Disord. 1984;7:309–18.
Article CAS PubMed Google Scholar
Jayakody K, Gallagher P, Lloyd AJ, Cousins DA. A quantitative analysis of the relationship between affective state and personality ratings in inpatient depression (RAPID). Psychol Med [Internet]. 2022 [cited 2023 Apr 8];1–10. https://www.cambridge.org/core/journals/psychological-medicine/article/quantitative-analysis-of-the-relationship-between-affective-state-and-personality-ratings-in-inpatient-depression-rapid/83BF8CE9A12C06ECEDA4E 2018EAADAD7.
Newton-Howes G, Tyrer P, Johnson T. Personality disorder and the outcome of depression: Meta-analysis of published studies. Br J Psychiatry. 2006;188:13–20.
Liu J, Gong J, Nie G, He Y, Xiao B, Shen Y et al. The mediating effects of childhood neglect on the association between schizotypal and autistic personality traits and depression in a non-clinical sample. BMC Psychiatry [Internet]. 2017 [cited 2023 Apr 8];17:352. https://bmcpsychiatry.biomedcentral.com/articles/ https://doi.org/10.1186/s12888-017-1510-0 .
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Diagnostic and Statistical Manual of Mental Disorders. 2022.
Sanislow CA, Grilo CM, McGlashan TH. Factor analysis of the DSM-III-R borderline personality disorder criteria in psychiatric inpatients. Am J Psychiatry. 2000;157:1629–33.
Gunderson JG. Borderline personality disorder: Ontogeny of a diagnosis. Am J Psychiatry. 2009;166:530–9.
Article PubMed PubMed Central Google Scholar
Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD et al. Prevalence, Correlates, Disability, and Comorbidity of DSM-IV Borderline Personality Disorder: Results From the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry [Internet]. 2008 [cited 2023 Apr 8];69:15398. https://www.psychiatrist.com/jcp/medical/comorbidity/prevalence-correlates-disability-comorbidity-dsm-iv-borderline-personality-disorder-wave-2-nesarc .
Gross R, Olfson M, Gameroff M, Shea S, Feder A, Fuentes M, et al. Borderline personality disorder in primary care. Arch Intern Med. 2002;162:53–60.
Gunderson JG, Stout RL, Sanislow CA, Shea MT, McGlashan TH, Zanarini MC et al. New episodes and new onsets of major depression in borderline and other personality disorders. J Affect Disord [Internet]. 2008 [cited 2023 Apr 8];111:40. /pmc/articles/PMC2829969/.
Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. Am J Psychiatry. 1998;155:1733–9.
Lieb K, Zanarini MC, Schmahl C, Linehan PMM, Bohus PM. Borderline personality disorder. Lancet. 2004;364:453–61.
Reichborn-Kjennerud T, Czajkowski N, Rysamb E, Ørstavik RE, Neale MC, Torgersen S et al. Major depression and dimensional representations of DSM-IV personality disorders: a population-based twin study. Psychol Med [Internet]. 2010 [cited 2023 Apr 8];40:1475. /pmc/articles/PMC2909484/.
Krueger RF, Johnson W. Behavioral genetics and personality: A new look at the integration of nature and nurture. [Internet]. The Guildford Press; 2008 [cited 2023 Apr 9]. pp. 287–310. https://www.research.ed.ac.uk/en/publications/behavioral-genetics-and-personality-a-new-look-at-the-integration .
Markon KE, Krueger RF, Watson D. Delineating the structure of normal and abnormal personality: an integrative hierarchical approach. J Pers Soc Psychol [Internet]. 2005 [cited 2023 Apr 9];88:139–57. https://pubmed.ncbi.nlm.nih.gov/15631580/ .
Rothbart MK, Bates JE, Temperament. Handbook of Child Psychology [Internet]. 2007 [cited 2023 Apr 9]; https://onlinelibrary.wiley.com/doi/full/10.1002/9780470147658.chpsy0303 .
Bylsma LM, Morris BH, Rottenberg J. A meta-analysis of emotional reactivity in major depressive disorder. Clin Psychol Rev [Internet]. 2008 [cited 2023 Apr 9];28:676–91. https://pubmed.ncbi.nlm.nih.gov/18006196/ .
Miller MC. When depression doesn’t lead with depression. JAMA Psychiatry [Internet]. 2013 [cited 2023 Apr 9];70:1131–2. http://www.ncbi.nlm.nih.gov/pubmed/24173599 .
Judd LL, Schettler PJ, Coryell W, Akiskal HS, Fiedorowicz JG. Overt irritability/anger in unipolar major depressive episodes: past and current characteristics and implications for long-term course. JAMA Psychiatry [Internet]. 2013 [cited 2023 Apr 9];70:1171–80. https://pubmed.ncbi.nlm.nih.gov/24026579/ .
Zanarini MC, Frankenburg FR. The essential nature of borderline psychopathology. J Pers Disord. 2007;21:518–35.
Silk KR. The quality of depression in borderline personality disorder and the diagnostic process. J Pers Disord [Internet]. 2010 [cited 2023 Apr 9];24:25–37. https://pubmed.ncbi.nlm.nih.gov/20205497/ .
Köhling J, Moessner M, Ehrenthal JC, Bauer S, Cierpka M, Kämmerer A et al. Affective Instability and Reactivity in Depressed Patients With and Without Borderline Pathology. J Pers Disord [Internet]. 2016 [cited 2023 Apr 9];30:776–95. https://pubmed.ncbi.nlm.nih.gov/26623534/ .
Fertuck EA, Marsano-Jozefowicz S, Stanley B, Tryon WW, Oquendo M, Mann JJ, et al. The impact of borderline personality disorder and anxiety on neuropsychological performance in major depression. J Pers Disord. 2006;20:55–70.
Stanley B, Wilson ST. Heightened subjective experience of depression in borderline personality disorder. J Pers Disord [Internet]. 2006 [cited 2023 Apr 9];20:307–18. https://pubmed.ncbi.nlm.nih.gov/16901256/ .
Levy KN, Edell WS, McGlashan TH. Depressive experiences in inpatients with borderline personality disorder. Psychiatr Q. 2007;78:129–43.
McDermid J, Sareen J, El-Gabalawy R, Pagura J, Spiwak R, Enns MW. Co-morbidity of bipolar disorder and borderline personality disorder: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Compr Psychiatry [Internet]. 2015 [cited 2024 Mar 21];58:18–28. https://pubmed.ncbi.nlm.nih.gov/25666748/ .
Frías Á, Baltasar I, Birmaher B. Comorbidity between bipolar disorder and borderline personality disorder: Prevalence, explanatory theories, and clinical impact. J Affect Disord [Internet]. 2016 [cited 2024 Mar 21];202:210–9. https://pubmed.ncbi.nlm.nih.gov/27267293/ .
Angst J, Cui L, Swendsen J, Rothen S, Cravchik A, Kessler RC et al. Major depressive disorder with subthreshold bipolarity in the National Comorbidity Survey Replication. Am J Psychiatry [Internet]. 2010 [cited 2024 Mar 21];167:1194–201. https://pubmed.ncbi.nlm.nih.gov/20713498/ .
Akiskal HS, Benazzi F, Perugi G, Rihmer Z. Agitated unipolar depression re-conceptualized as a depressive mixed state: implications for the antidepressant-suicide controversy. J Affect Disord [Internet]. 2005 [cited 2024 Mar 21];85:245–58. https://pubmed.ncbi.nlm.nih.gov/15780694/ .
Cassano GB, Rucci P, Frank E, Fagiolini A, Dell’Osso L, Shear MK et al. The mood spectrum in unipolar and bipolar disorder: arguments for a unitary approach. Am J Psychiatry [Internet]. 2004 [cited 2024 Mar 21];161:1264–9. https://pubmed.ncbi.nlm.nih.gov/15229060/ .
Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM et al. Ten-Year Course of Borderline Personality Disorder: Psychopathology and Function From the Collaborative Longitudinal Personality Disorders Study. Arch Gen Psychiatry [Internet]. 2011 [cited 2023 Apr 9];68:827. /pmc/articles/PMC3158489/.
Skodol AE, Grilo CM, Keyes KM, Geier T, Grant BF, Hasin DS. Relationship of personality disorders to the course of major depressive disorder in a nationally representative sample. Am J Psychiatry [Internet]. 2011 [cited 2023 Apr 9];168:257–64. https://pubmed.ncbi.nlm.nih.gov/21245088/ .
Zanarini MC, Frankenbourg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. Am J Psychiatry [Internet]. 2004 [cited 2023 Apr 9];161:2108–14. https://pubmed.ncbi.nlm.nih.gov/15514413/ .
Gunderson JG, Morey LC, Stout RL, Skodol AE, Shea MT, McGlashan TH et al. Major depressive disorder and borderline personality disorder revisited: longitudinal interactions. J Clin Psychiatry [Internet]. 2004 [cited 2023 Apr 9];65:1049–56. https://pubmed.ncbi.nlm.nih.gov/15323588/ .
Broadbear J, Rao S. Psychotherapy for Borderline Personality Disorder reduces the need for prescription medication. Eur Psychiatry. 2015;30:1528.
Article Google Scholar
Feffer K, Peters SK, Bhui K, Downar J, Giacobbe P. Successful dorsomedial prefrontal rTMS for major depression in borderline personality disorder: three cases. Brain Stimul. 2017;10:716–7.
Feske U, Mulsant BH, Pilkonis PA, Soloff P, Dolata D, Sackeim HA et al. Clinical outcome of ECT in patients with major depression and comorbid borderline personality disorder. Am J Psychiatry [Internet]. 2004 [cited 2023 Apr 9];161:2073–80. https://pubmed.ncbi.nlm.nih.gov/15514409/ .
Stoffers-Winterling JM, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev [Internet]. 2012 [cited 2023 Apr 9];2012. https://pubmed.ncbi.nlm.nih.gov/22895952/ .
Bohus M, Stoffers-Winterling J, Sharp C, Krause-Utz A, Schmahl C, Lieb K. Borderline personality disorder. Lancet [Internet]. 2021 [cited 2023 Apr 10];398:1528–40. https://pubmed.ncbi.nlm.nih.gov/34688371/ .
Torgersen S, Lygren S, Øien PA, Skre I, Onstad S, Edvardsen J et al. A twin study of personality disorders. Compr Psychiatry [Internet]. 2000 [cited 2023 Apr 10];41:416–25. https://pubmed.ncbi.nlm.nih.gov/11086146/ .
Skoglund C, Tiger A, Rück C, Petrovic P, Asherson P, Hellner C et al. Familial risk and heritability of diagnosed borderline personality disorder: a register study of the Swedish population. Mol Psychiatry [Internet]. 2021 [cited 2023 Apr 10];26:999–1008. https://pubmed.ncbi.nlm.nih.gov/31160693/ .
Streit F, Witt SH, Awasthi S, Foo JC, Jungkunz M, Frank J et al. Borderline personality disorder and the big five: molecular genetic analyses indicate shared genetic architecture with neuroticism and openness. Transl Psychiatry [Internet]. 2022 [cited 2023 Apr 10];12. Available from: /pmc/articles/PMC9001677/.
Witt SH, Streit F, Jungkunz M, Frank J, Awasthi S, Reinbold CS et al. Genome-wide association study of borderline personality disorder reveals genetic overlap with bipolar disorder, major depression and schizophrenia. Transl Psychiatry [Internet]. 2017 [cited 2023 Apr 10];7:e1155. https://pubmed.ncbi.nlm.nih.gov/28632202/ .
Ripke S, Sanders AR, Kendler KS, Levinson DF, Sklar P, Holmans PA et al. Genome-wide association study identifies five new schizophrenia loci. Nat Genet [Internet]. 2011 [cited 2023 Apr 10];43:969–78. https://pubmed.ncbi.nlm.nih.gov/21926974/ .
O’dushlaine C, Rossin L, Lee PH, Duncan L, Parikshak NN, Newhouse S et al. Psychiatric genome-wide association study analyses implicate neuronal, immune and histone pathways. Nat Neurosci [Internet]. 2015 [cited 2023 Apr 10];18:199–209. https://pubmed.ncbi.nlm.nih.gov/25599223/ .
Lubke GH, Laurin C, Amin N, Hottenga JJ, Willemsen G, Van Grootheest G et al. Genome-wide analyses of borderline personality features. Molecular Psychiatry. 2013 19:8 [Internet]. 2013 [cited 2023 Apr 10];19:923–9. https://www.nature.com/articles/mp2013109 .
Liu J, Dietz K, Deloyht JM, Pedre X, Kelkar D, Kaur J et al. Impaired adult myelination in the prefrontal cortex of socially isolated mice. Nat Neurosci [Internet]. 2012 [cited 2023 Apr 10];15:1621–3. https://pubmed.ncbi.nlm.nih.gov/23143512/ .
Distel MA, Hottenga JJ, Trull TJ, Boomsma DI. Chromosome 9: linkage for borderline personality disorder features. Psychiatr Genet. 2008;18:302–7.
Mahgoub M, Monteggia LM. Epigenetics and Psychiatry. Neurotherapeutics [Internet]. 2013 [cited 2023 Apr 10];10:734. /pmc/articles/PMC3805856/.
Perroud N, Zewdie S, Stenz L, Adouan W, Bavamian S, Prada P, BORDERLINE PERSONALITY, AND BIPOLAR DISORDERS: LINK WITH SEVERITY OF THE DISORDERS AND CHILDHOOD MALTREATMENT. METHYLATION OF SEROTONIN RECEPTOR 3A IN ADHD,. Depress Anxiety [Internet]. 2016 [cited 2023 Apr 10];33:45–55. https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1002/da.22406 .
Thaler L, Gauvin L, Joober R, Groleau P, de Guzman R, Ambalavanan A, et al. Methylation of BDNF in women with bulimic eating syndromes: associations with childhood abuse and borderline personality disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2014;54:43–9.
Martín-Blanco A, Ferrer M, Soler J, Salazar J, Vega D, Andión O, et al. Association between methylation of the glucocorticoid receptor gene, childhood maltreatment, and clinical severity in borderline personality disorder. J Psychiatr Res. 2014;57:34–40.
Groleau P, Joober R, Israel M, Zeramdini N, DeGuzman R, Steiger H. Methylation of the dopamine D2 receptor (DRD2) gene promoter in women with a bulimia-spectrum disorder: associations with borderline personality disorder and exposure to childhood abuse. J Psychiatr Res. 2014;48:121–7.
Prados J, Stenz L, Courtet P, Prada P, Nicastro R, Adouan W et al. Borderline personality disorder and childhood maltreatment: a genome-wide methylation analysis. Genes Brain Behav [Internet]. 2015 [cited 2023 Apr 10];14:177–88. https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1111/gbb.12197 .
Perroud N, Salzmann A, Prada P, Nicastro R, Hoeppli ME, Furrer S et al. Response to psychotherapy in borderline personality disorder and methylation status of the BDNF gene. Translational Psychiatry. 2013 3:1 [Internet]. 2013 [cited 2023 Apr 10];3:e207–e207. https://www.nature.com/articles/tp2012140 .
Hazlett EA, Zhang J, New AS, Zelmanova Y, Goldstein KE, Haznedar MM, et al. Potentiated Amygdala response to repeated emotional pictures in Borderline personality disorder. Biol Psychiatry. 2012;72:448–56.
New AS, Hazlett EA, Buchsbaum MS, Goodman M, Mitelman SA, Newmark R et al. Amygdala–Prefrontal Disconnection in Borderline Personality Disorder. Neuropsychopharmacology 2007 32:7 [Internet]. 2007 [cited 2023 Apr 10];32:1629–40. https://www.nature.com/articles/1301283 .
Barnow S, Limberg A, Stopsack M, Spitzer C, Grabe HJ, Freyberger HJ, et al. Dissociation and emotion regulation in borderline personality disorder. Psychol Med. 2012;42:783–94.
Baschnagel JS, Coffey SF, Hawk LW, Schumacher JA, Holloman G. Psychophysiological assessment of emotional processing in patients with borderline personality disorder with and without comorbid substance use. Personality Disorders: Theory Res Treat. 2013;4:203–13.
Asim M, Wang H, Waris A. Altered neurotransmission in stress-induced depressive disorders: the underlying role of the amygdala in depression. Neuropeptides. 2023;98:102322.
Şar V. Dissociative Depression is Resistant to Treatment-As-Usual. Journal of Psychology & Clinical Psychiatry [Internet]. 2015 [cited 2023 Apr 10];Volume 3. https://medcraveonline.com/JPCPY/JPCPY-03-00128.php .
Quello SB, Brady KT, Sonne SC. Mood Disorders and Substance Use Disorder: A Complex Comorbidity. Sci Pract Perspect [Internet]. 2005 [cited 2023 Apr 10];3:13. /pmc/articles/PMC2851027/.
Zubieta JK, Smith YR, Bueller JA, Xu Y, Kilbourn MR, Jewett DM et al. Regional Mu opioid receptor regulation of sensory and affective dimensions of pain. Science (1979). 2001;293:311–5.
Eisenberger NI, Jarcho JM, Lieberman MD, Naliboff BD. An experimental study of shared sensitivity to physical pain and social rejection. Pain. 2006;126:132–8.
Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An fMRI study of social exclusion. Science (1979) [Internet]. 2003 [cited 2023 Apr 10];302:290–2. https://www.science.org/doi/ https://doi.org/10.1126/science.1089134 .
Biskin RS, Frankenburg FR, Fitzmaurice GM, Zanarini MC. Pain in patients with borderline personality disorder. Personal Ment Health [Internet]. 2014 [cited 2023 Apr 10];8:218–27. https://onlinelibrary.wiley.com/doi/full/10.1002/pmh.1265 .
Schmahl C, Meinzer M, Zeuch A, Fichter M, Cebulla M, Kleindienst N et al. Pain sensitivity is reduced in borderline personality disorder, but not in posttraumatic stress disorder and bulimia nervosa. http://dx.doi.org/103109/15622970701849952 [Internet]. 2010 [cited 2023 Apr 10];11:364–71. https://www.tandfonline.com/doi/abs/ https://doi.org/10.3109/15622970701849952 .
Prossin AR, Love TM, Koeppe RA, Zubieta JK, Silk KR. Dysregulation of regional endogenous opioid function in borderline personality disorder. American Journal of Psychiatry [Internet]. 2010 [cited 2023 Apr 10];167:925–33. https://doi.org/10.1176/appi.ajp.2010.09091348 .
Barr CS, Schwandt ML, Lindell SG, Higley JD, Maestripieri D, Goldman D et al. Variation at the mu-opioid receptor gene (OPRM1) influences attachment behavior in infant primates. Proc Natl Acad Sci U S A [Internet]. 2008 [cited 2023 Apr 10];105:5277–81. https://www.pnas.org/doi/abs/ https://doi.org/10.1073/pnas.0710225105 .
Moles A, Kieffer BL, D’Amato FR. Deficit in attachment behavior in mice lacking the µ-opioid receptor gene. Science (1979). 2004;304:1983–6.
Slavich GM, Tartter MA, Brennan PA, Hammen C. Endogenous opioid system influences depressive reactions to socially painful targeted rejection life events. Psychoneuroendocrinology. 2014;49:141–9.
Article CAS PubMed PubMed Central Google Scholar
Jobst A, Padberg F, Mauer MC, Daltrozzo T, Bauriedl-Schmidt C, Sabass L et al. Lower Oxytocin Plasma Levels in Borderline Patients with Unresolved Attachment Representations. Front Hum Neurosci [Internet]. 2016 [cited 2023 Apr 10];10:1–11. Available from: /pmc/articles/PMC4811864/.
Bertsch K, Schmidinger I, Neumann ID, Herpertz SC. Reduced plasma oxytocin levels in female patients with borderline personality disorder. Horm Behav. 2013;63:424–9.
Ebert A, Kolb M, Heller J, Edel MA, Roser P, Brüne M. Modulation of interpersonal trust in borderline personality disorder by intranasal oxytocin and childhood trauma. https://doi.org/101080/174709192013807301 [Internet]. 2013 [cited 2023 Apr 10];8:305–13. https://www.tandfonline.com/doi/abs/ https://doi.org/10.1080/17470919.2013.807301 .
Hammen C, Bower JE, Cole SW. Oxytocin Receptor Gene Variation and Differential Susceptibility to Family Environment in Predicting Youth Borderline Symptoms. https://doi.org/101521/pedi_2014_28_152 [Internet]. 2015 [cited 2023 Apr 10];29:177–92. https://doi.org/10.1521/pedi_2014_28_152 .
Cicchetti D, Rogosch FA, Hecht KF, Crick NR, Hetzel S. Moderation of maltreatment effects on childhood borderline personality symptoms by gender and oxytocin receptor and FK506 binding protein 5 genes. Dev Psychopathol. 2014;26:831–49.
Xie S, Hu Y, Fang L, Chen S, Botchway BOA, Tan X et al. The association of oxytocin with major depressive disorder: Role of confounding effects of antidepressants. Rev Neurosci [Internet]. 2022 [cited 2023 Apr 10];33:59–77. https://www.degruyter.com/document/doi/ https://doi.org/10.1515/revneuro-2020-0128/html .
De Cagna F, Fusar-Poli L, Damiani S, Rocchetti M, Giovanna G, Mori A et al. The Role of Intranasal Oxytocin in Anxiety and Depressive Disorders: A Systematic Review of Randomized Controlled Trials. Clinical Psychopharmacology and Neuroscience [Internet]. 2019 [cited 2023 Apr 10];17:1. /pmc/articles/PMC6361048/.
Aston-Jones G, Cohen JD. An integrative theory of locus coeruleus-norepinephrine function: adaptive gain and optimal performance. Annu Rev Neurosci. 2005;28:403–50.
DeYoung CG. The neuromodulator of exploration: A unifying theory of the role of dopamine in personality. Front Hum Neurosci [Internet]. 2013 [cited 2023 Apr 10];7. /pmc/articles/PMC3827581/.
Hansenne M, Pitchot W, Ansseau M. Serotonin, personality and borderline personality disorder. Acta Neuropsychiatr [Internet]. 2002 [cited 2023 Apr 10];14:66–70. https://www.cambridge.org/core/journals/acta-neuropsychiatrica/article/abs/serotonin-personality-and-borderline-personality-disorder/A3138A543C9B5B39C5182B039EAB7183 .
Friedel RO. Dopamine Dysfunction in Borderline Personality Disorder: A Hypothesis. Neuropsychopharmacology 2004 29:6 [Internet]. 2004 [cited 2023 Apr 10];29:1029–39. https://www.nature.com/articles/1300424 .
Joyce PR, McHugh PC, McKenzie JM, Sullivan PF, Mulder RT, Luty SE et al. A dopamine transporter polymorphism is a risk factor for borderline personality disorder in depressed patients. Psychol Med [Internet]. 2006 [cited 2023 Apr 10];36:807–13. https://www.cambridge.org/core/journals/psychological-medicine/article/dopamine-transporter-polymorphism-is-a-risk-factor-for-borderline-personality-disorder-in-depressed-patients/1E0E65F97161555F868C13A659C451A3 .
Joyce PR, McHugh PC, Light KJ, Rowe S, Miller AL, Kennedy MA. Relationships between angry-impulsive personality traits and genetic polymorphisms of the dopamine transporter. Biol Psychiatry. 2009;66:717–21.
Zetzsche T, Preuss UW, Bondy B, Frodl T, Zill P, Schmitt G et al. 5-HT1A receptor gene C – 1019 G polymorphism and amygdala volume in borderline personality disorder. Genes Brain Behav [Internet]. 2008 [cited 2023 Apr 10];7:306–13. https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1111/j.1601-183X.2007.00353.x .
Ni X, Chan K, Bulgin N, Sicard T, Bismil R, McMain S, et al. Association between serotonin transporter gene and borderline personality disorder. J Psychiatr Res. 2006;40:448–53.
Soloff PH, Lynch KG, Kelly TM, Malone KM, John Mann J. Characteristics of suicide attempts of patients with major depressive episode and borderline personality disorder: a comparative study. Am J Psychiatry. 2000;157:601–8.
Serretti A, Mandelli L, Giegling I, Schneider B, Hartmann AM, Schnabel A et al. HTR2C and HTR1A gene variants in German and Italian suicide attempters and completers. American Journal of Medical Genetics Part B: Neuropsychiatric Genetics [Internet]. 2007 [cited 2023 Apr 10];144B:291–9. https://onlinelibrary.wiley.com/doi/full/ https://doi.org/10.1002/ajmg.b.30432 .
Joyce PR, Stephenson J, Kennedy M, Mulder RT, McHugh PC. The presence of both serotonin 1A receptor (HTR1A) and dopamine transporter (DAT1) gene variants increase the risk of borderline personality disorder. Front Genet. 2013;4:313.
Google Scholar
Simeon D, Knutelska M, Smith L, Baker BR, Hollander E. A preliminary study of cortisol and norepinephrine reactivity to psychosocial stress in borderline personality disorder with high and low dissociation. Psychiatry Res [Internet]. 2007 [cited 2023 Apr 10];149:177–84. https://pubmed.ncbi.nlm.nih.gov/17169436/ .
Leichsenring F, Heim N, Leweke F, Spitzer C, Steinert C, Kernberg OF. Borderline Personality Disorder: A Review. JAMA [Internet]. 2023 [cited 2023 Apr 11];329:670–9. https://pubmed.ncbi.nlm.nih.gov/36853245/ .
Wu T, Hu J, Davydow D, Huang H, Spottswood M, Huang H. Demystifying borderline personality disorder in primary care. Front Med (Lausanne) [Internet]. 2022 [cited 2023 Apr 11];9. https://pubmed.ncbi.nlm.nih.gov/36405597/ .
Temes CM, Zanarini MC, The Longitudinal Course of Borderline Personality Disorder. Psychiatr Clin North Am [Internet]. 2018 [cited 2023 Apr 11];41:685–94. https://pubmed.ncbi.nlm.nih.gov/30447732/ .
MC Z, FR F. J H, KR S. Mental health service utilization by borderline personality disorder patients and Axis II comparison subjects followed prospectively for 6 years. J Clin Psychiatry [Internet]. 2004 [cited 2023 Apr 11];65:28–35. https://pubmed.ncbi.nlm.nih.gov/14744165/ .
Herpertz S, Zanarini M, Schulz C, Siever L, Lieb K, Möller HJ. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of personality disorders. World J Biol Psychiatry [Internet]. 2007 [cited 2023 Apr 11];8:212–44. https://pubmed.ncbi.nlm.nih.gov/17963189/ .
Oldham JM, Glen Gabbard CO, Goin MK, Gunderson J, Soloff P, Spiegel D, GROUP ON BORDERLINE PERSONALITY DISORDER AMERICAN PSYCHIATRIC ASSOCIATION STEERING COMMITTEE ON PRACTICE GUIDELINES AREA AND COMPONENT LIAISONS STAFF Treatment of Patients. Practice Guidelines for the Treatment of Patients With Borderline Personality Disorder WORK With Borderline Personality Disorder [Internet]. 2010. http://www.appi.org/CustomerService/Pages/Permissions.aspx .
Simonsen S, Bateman A, Bohus M, Dalewijk HJ, Doering S, Kaera A et al. European guidelines for personality disorders: Past, present and future. Borderline Personal Disord Emot Dysregul [Internet]. 2019 [cited 2023 Apr 11];6:1–10. https://bpded.biomedcentral.com/articles/ https://doi.org/10.1186/s40479-019-0106-3 .
Borderline personality disorder: recognition and management Clinical guideline [Internet]. 2009. www.nice.org.uk/guidance/cg78 .
Bozzatello P, Rocca P, De Rosa ML, Bellino S. Current and emerging medications for borderline personality disorder: is pharmacotherapy alone enough? Expert Opin Pharmacother. Taylor and Francis Ltd; 2020. pp. 47–61.
Stoffers J, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Reviews. 2010.
Vita A, De Peri L, Sacchetti E. Antipsychotics, antidepressants, anticonvulsants, and placebo on the symptom dimensions of borderline personality disorder: A meta-analysis of randomized controlled and open-label trials. J Clin Psychopharmacol [Internet]. 2011 [cited 2023 Apr 11];31:613–24. https://journals.lww.com/psychopharmacology/Fulltext/2011/10000/Antipsychotics,_Antidepressants,_Anticonvulsants,.12.aspx .
Bellino S, Zizza M, Rinaldi C, Bogetto F. Combined treatment of Major Depression in patients with Borderline personality disorder: a comparison with pharmacotherapy. Can J Psychiatry. 2006.
Simpson EB, Yen S, Costello E, Rosen K, Begin A, Pistorello J et al. Combined Dialectical Behavior Therapy and Fluoxetine in the Treatment of Borderline Personality Disorder. J Clin Psychiatry [Internet]. 2004 [cited 2023 Apr 11];65:3235. https://www.psychiatrist.com/jcp/personality/combined-dialectical-behavior-therapy-fluoxetine-treatment .
Edinoff AN, Akuly HA, Hanna TA, Ochoa CO, Patti SJ, Ghaffar YA et al. Selective Serotonin Reuptake Inhibitors and Adverse Effects: A Narrative Review. Neurol Int [Internet]. 2021 [cited 2023 Apr 11];13:387–401. https://pubmed.ncbi.nlm.nih.gov/34449705/ .
Silvestrini B, Trazodone. From the Mental Pain to the Dys-Stress Hypothesis of Depression. Clin Neuropharmacol [Internet]. 1989;12:S4. https://journals.lww.com/clinicalneuropharm/Abstract/1989/01001/Trazodone__From_the_Mental_Pain_to_the.2.aspx .
Stahl SM. Mechanism of action of trazodone: a multifunctional drug. CNS Spectr [Internet]. 2009;14:536–46. http://www.ncbi.nlm.nih.gov/pubmed/20095366 .
Fagiolini A, Comandini A, Catena Dell’Osso M, Kasper S. Rediscovering trazodone for the treatment of major depressive disorder. CNS Drugs [Internet]. 2012;26:1033–49. http://www.ncbi.nlm.nih.gov/pubmed/23192413 .
Rotzinger S, Bourin M, Akimoto Y, Coutts RT, Baker GB. Metabolism of some ’second’- and ’fourth’-generation antidepressants: Iprindole, viloxazine, bupropion, mianserin, maprotiline, trazodone, nefazodone, and venlafaxine. Cell Mol Neurobiol [Internet]. 1999 [cited 2023 Apr 11];19:427–42. https://link.springer.com/article/ https://doi.org/10.1023/A:1006953923305 .
Kahn RS, Wetzler S. m-Chlorophenylpiperazine as a probe of serotonin function. Biol Psychiatry. 1991;30:1139–66.
Cipriani A, Furukawa TA, Salanti G, Chaimani A, Atkinson LZ, Ogawa Y et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet [Internet]. 2018 [cited 2022 Dec 27];391:1357–66. https://pubmed.ncbi.nlm.nih.gov/29477251/ .
Sheehan DV, Croft HA, Gossen ER, Levitt RJ, Brullé C, Bouchard S et al. Extended-release Trazodone in Major Depressive Disorder: A Randomized, Double-blind, Placebo-controlled Study. Psychiatry (Edgmont) [Internet]. 2009 [cited 2022 Dec 28];6:20. /pmc/articles/PMC2719441/.
Cuomo A, Ballerini A, Bruni AC, Decina P, Di Sciascio G, Fiorentini A et al. Clinical guidance for the use of trazodone in major depressive disorder and concomitant conditions: pharmacology and clinical practice. Riv Psichiatr [Internet]. 2019 [cited 2022 Dec 27];54:137–49. https://pubmed.ncbi.nlm.nih.gov/31379379/ .
Stahl SM. Mechanism of action of the SPARI vilazodone: serotonin 1A partial agonist and reuptake inhibitor. CNS Spectr [Internet]. 2014;19:105–9. https://www.cambridge.org/core/journals/cns-spectrums/article/mechanism-of-action-of-the-spari-vilazodone-serotonin-1a-partial-agonist-and-reuptake-inhibitor/9D75F76A67C4E33898E1C5E655EB4DAB #.
Fagiolini A, Albert U, Ferrando L, Herman E, Muntean C, Pálová E et al. A randomized, double-blind study comparing the efficacy and safety of trazodone once-a-day and venlafaxine extended-release for the treatment of patients with major depressive disorder. Int Clin Psychopharmacol [Internet]. 2020;35:137–46. https://journals.lww.com/intclinpsychopharm/Fulltext/2020/05000/A_randomized,_double_blind_study_comparing_the.3.aspx .
Albert U, Lamba P, Stahl SM. Early response to trazodone once-a-day in major depressive disorder: review of the clinical data and putative mechanism for faster onset of action. CNS Spectr [Internet]. 2021 [cited 2022 Dec 27];26:232–42. https://pubmed.ncbi.nlm.nih.gov/33731232/ .
Lavigne JE, Hur K, Kane C, Au A, Bishop TM, Pigeon WR. Prescription Medications for the Treatment of Insomnia and Risk of Suicide Attempt: a Comparative Safety Study. J Gen Intern Med [Internet]. 2019 [cited 2023 Apr 11];34:1554–63. https://pubmed.ncbi.nlm.nih.gov/31161572/ .
Schreiber S, Backer MM, Herman I, Shamir D, Boniel T, Pick CG. The antinociceptive effect of trazodone in mice is mediated through both µ-opioid and serotonergic mechanisms. Behavioural Brain Research [Internet]. 2000 [cited 2023 Apr 11];114:51–6. https://pubmed.ncbi.nlm.nih.gov/10996046/ .
Schreiber S, Pick CG. Trazodone and mirtazapine: A possible opioid involvement in their use (at low dose) for sleep? Med Hypotheses [Internet]. 2020 [cited 2023 Apr 11];136. https://pubmed.ncbi.nlm.nih.gov/31759303/ .
Ockert DM, Volpicelli JR, Baier AR, Coons EE, Fingesten A. A nonopioid procedure for outpatient opioid detoxification. J Addict Med [Internet]. 2011 [cited 2023 Apr 11];5:110–4. https://pubmed.ncbi.nlm.nih.gov/21769056/ .
Bossini L, Coluccia A, Casolaro I, Benbow J, Amodeo G, De Giorgi R et al. Off-Label Trazodone Prescription: Evidence, Benefits and Risks. Curr Pharm Des [Internet]. 2015 [cited 2023 Apr 11];21:3343–51. https://pubmed.ncbi.nlm.nih.gov/26088119/ .
Semiz UB, Basoglu C, Ebrinc S, Cetin M. Nightmare disorder, dream anxiety, and subjective sleep quality in patients with borderline personality disorder. Psychiatry Clin Neurosci. 2008;62:48–55.
Agargun MY, Kara H, Özer ÖA, Selvi Y, Kiran Ü, Kiran S. Nightmares and dissociative experiences: the key role of childhood traumatic events. Psychiatry Clin Neurosci [Internet]. 2003 [cited 2023 Apr 11];57:139–45. https://pubmed.ncbi.nlm.nih.gov/12667159/ .
Geldenhuys C, van den Heuvel LL, Steyn P, Seedat S. Pharmacological Management of Nightmares Associated with Posttraumatic Stress Disorder. CNS Drugs [Internet]. 2022 [cited 2023 Apr 11];36:721–37. https://link.springer.com/article/10.1007/s40263-022-00929-x .
Download references
This publication was supported by an unrestricted grant from Angelini Pharma.
Author information
Authors and affiliations.
Department of Mental Health, Alzheimer Center of Giulianova, Hospital “Maria SS dello Splendore”, ASL Teramo, Giulianova (TE), Italy
Carmine Tomasetti
Psychiatry and Psychology Institute, Catholic University of Sacred Heart of Rome, Rome, Italy
G. Autullo & V. Villari
Psychiatry Unit, Department of Health Science, University of Florence, Largo Brambilla 3, Florence, 50134, Italy
A. Ballerini
Laboratory of Molecular and Translational Psychiatry and Unit of Treatment Resistant Psychosis, Section of Psychiatry, Department of Neuroscience, Reproductive Science and Dentistry, University of Naples “Federico II”, Naples, Italy
A. de Bartolomeis
Department of Mental Health, Department of Biomedical and Clinical Sciences Luigi Sacco, University of Milan, Milan, Italy
B. Dell’Osso
Department of Neurosciences and Mental Health, Ca’ Granda Ospedale Maggiore Policlinico, Fondazione Istituto di Ricerca e Cura a Carattere Scientifico (IRCCS), University of Milan, Milan, Italy
A. Fiorentini
Psychiatric Emergency Service, Department of Neuroscience and Mental Health, A.O.U. “Città della Salute e della Scienza”, Turin, Italy
Department of Mental Health, Mental Health Center of Giulianova, ASL Teramo, Teramo, Italy
D. De Berardis
You can also search for this author in PubMed Google Scholar
Contributions
DDB developed the original idea; CT wrote the first and the last draft of the manuscript; all the authors equally contributed to the conception, put into writing, and revisions of the paper.
Corresponding author
Correspondence to Carmine Tomasetti .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tomasetti, C., Autullo, G., Ballerini, A. et al. Treating depression in patients with borderline personality disorder: clinical clues on the use of antidepressants. Ann Gen Psychiatry 23 , 21 (2024). https://doi.org/10.1186/s12991-024-00507-z
Download citation
Received : 28 January 2024
Accepted : 23 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12991-024-00507-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Serotonin antagonist/Reuptake inhibitors
- Comorbidity
- Psychiatric disorders
- Neurobiology
Annals of General Psychiatry
ISSN: 1744-859X
- Submission enquiries: [email protected]

Depression, schizophrenia and bipolar disorder linked with ancient viral DNA in our genome – new research
Research Fellow, King's College London
Professor of Immunology in Medicine, Cornell University
Senior lecturer, King's College London
Disclosure statement
Rodrigo Duarte received funding from the National Institutes of Health, USA.
Douglas Nixon receives funding from the National Institutes of Health, USA.
Timothy Powell receives funding from the National Institute for Health and Care Research, the National Institutes of Health, and the Medical Research Council.
King's College London provides funding as a member of The Conversation UK.
View all partners
Around 8% of human DNA is made up of genetic sequences acquired from ancient viruses . These sequences, known as human endogenous retroviruses (or Hervs), date back hundreds of thousands to millions of years – with some even predating the emergence of Homo sapiens .
Our latest research suggests that some ancient viral DNA sequences in the human genome play a role in susceptibility to psychiatric disorders such as schizophrenia, bipolar disorder and major depressive disorder.
Hervs represent the remnants of these infections with ancient retroviruses. Retroviruses are viruses that insert a copy of their genetic material into the DNA of the cells they infect. Retroviruses probably infected us on multiple occasions during our evolutionary past. When these infections occurred in sperm or egg cells that generated offspring, the genetic material from these retroviruses was passed on to subsequent generations , becoming a permanent part of our lineage.
Initially, scientists considered Hervs to be “junk DNA” – parts of our genome with no discernible function. But as our understanding of the human genome has advanced, it’s become evident that this so-called junk DNA is responsible for more functions than originally hypothesised.
First, researchers found that Hervs can regulate the expression of other human genes. A genetic feature is said to be “expressed” if its DNA segment is used to produce RNA (ribonucleic acid) molecules. These RNA molecules can then serve as intermediaries leading to the production of specific proteins , or help to regulate other parts of the genome .
Initial research suggested that Hervs regulate the expression of neighbouring genes with important biological functions. One example of this is a Herv that regulates the expression of a gene involved in modifying connections between brain cells.
Hervs have also been found to produce RNAs and even proteins in blood and brain samples . These molecules have the potential to exert a wide range of functions, as they can travel across cellular compartments to execute different roles.
Scientists have also found evidence suggesting certain human genes are derived from Hervs. This indicates there were instances during evolution where Hervs were co-opted for specialised biological functions. For example, the human genes syncytins 1 and 2, which are derived from Hervs, play pivotal roles in placental development .
HERVs in psychiatric disorders
Considering the abundance of Hervs in the genome and their potentially numerous functions, we wanted to better understand whether genetic susceptibility to certain psychiatric disorders was associated with differences in Herv expression.

In our study , we profiled Herv expression in nearly 800 autopsy brain samples. This helped us identify DNA variations that influenced Herv expression in the brain.
We then cross-referenced this information with findings from large genetic studies which had compared genetic differences between tens of thousands of people – both with and without mental health conditions. These studies identified variations in DNA associated with different psychiatric conditions.
We found that that the expression of four Hervs was linked with genetic susceptibility to major psychiatric disorders. The expression of two of these Hervs was associated with schizophrenia, one Herv with both schizophrenia and bipolar disorder, and one with depression. These results suggest that Hervs may be playing a more important role in the brain than initially thought.
Read more: Discovering how genetic 'dark matter' plays a role in mental illness is just the tip of the iceberg for human health
There are many genes involved in psychiatric disorders – and Hervs are only a part of this puzzle. Although the precise impact of these Hervs on brain cells and on a person’s susceptibility to certain psychiatric disorders requires further research, our study is the first to show that genetic susceptibility for a psychiatric disorder also acts through these ancient viral DNA sequences.
It’s still too early to determine the practical applications of our findings – and whether they might be used to develop new treatments. But we’re optimistic about this line of research. By linking Herv expression in the brain with psychiatric disorders, our research recognises the importance of these mysterious sequences in the human genome, which have been ignored for years.
- Schizophrenia
- Bipolar disorder
- Retroviruses
- Psychiatric disorders

Head of School, School of Arts & Social Sciences, Monash University Malaysia

Chief Operating Officer (COO)

Clinical Teaching Fellow

Data Manager

Director, Social Policy
Write Winning NIH Grant Proposals
Dr. John Robertson
Business, Energy, Engineering, Human Rights, Humanities, Law, Natural Sciences, Panel/Seminar/Colloquium, Research, Social Sciences, Sustainability, Workshop/Short Course

IMAGES
VIDEO
COMMENTS
Rodent research has shown that there may be a bidirectional association between the gut microbiota and depression: a disordered gut microbiota can play a role in the onset of this mental health problem, but, at the same time, the existence of stress and depression may also lead to a lower level of richness and diversity in the microbiome .
Our lack of knowledge cannot be put down to a scarcity of research in existing treatments. In the past decades, more than 500 randomised trials have examined the effects of antidepressant medications, and more than 600 trials have examined the effects of psychotherapies for depression (although comparatively few are conducted for early-onset depression).
This research proposal aims to better understand the neurobiology of depression in adolescents and how repetitive transcranial magnetic stimulation (rTMS) may therapeutically impact brain function and mood. This investigation also proposes the first study to examine the efficacy of rTMS maintenance therapy in adolescents who have met clinical ...
To improve our understanding, some research has been undertaken in which YP themselves are asked about their experience of depression. In a questionnaire study involving adolescents with depression in New Zealand, the researchers identified the aforementioned irritability as the most common characteristic alongside interpersonal problems and ...
The possible causes of depression are many and not yet well understood. However, it most likely results from an interplay of genetic vulnerability and environmental factors. Your depression research paper could explore one or more of these causes and reference the latest research on the topic. For instance, how does an imbalance in brain ...
The current paper critically evaluates Beck and Bredemeier's (2016) Unified Model of Depression (UMD) and explores some of the wider issues it raises about explanations of depression. Our ...
Background: Depression is a common mental health disease, especially in mid to late adolescence that, due to its. particularities, is a challenge and requires an effective diagnosis. Primary care ...
In depression research, these people can be the participants filling out self-rated instruments or being interviewed, observers scoring observer-rated scales or clinicians administering an interview.
The research is done on both gender, male and female. 29 students are female and. male students are 112. This portion of research is to check whether female students can have more chances. of ...
According to the fall 2007 American College Health Association-National College Health Assessment ( 1), a national survey of approximately 20,500 college students on 39 campuses, 43.2% of the students reported "feeling so depressed it was difficult to function" at least once in the past 12 months.More than 3,200 university students reported being diagnosed as having depression, with 39.2% of ...
Social media. The term 'social media' refers to the various internet-based networks that enable users to interact with others, verbally and visually (Carr & Hayes, Citation 2015).According to the Pew Research Centre (Citation 2015), at least 92% of teenagers are active on social media.Lenhart, Smith, Anderson, Duggan, and Perrin (Citation 2015) identified the 13-17 age group as ...
rTMS for Depressed Teens: A Sham-Controlled Trial, Part 2 Rochester, MN. This research proposal aims to better understand the neurobiology of depression in adolescents and how repetitive transcranial magnetic stimulation (rTMS) may therapeutically impact brain function and mood. This investigation also proposes the first study to examine the ...
Final Research Proposal: Depression and Anxiety. Grand Canyon University PSY- 495 Capstone Dr. Helmholdt February 27, 2022. Introduction. There have been many studies addressing correlations between the use of social media and mental health issues like depression. Social media platforms are common in modern society, insinuating their ...
Depression severity can be assessed using the beck depression inventory (BDI II). ... In our research, ... AA contributed to the study proposal and evaluated the manuscript. AAK performed the ...
name of assessment: research proposal; factors of depression lecturer's name: madam adibah binti zainualdin date of submission: 5 th june 2020 prepared by: no. name student id 1. aadli hakim bin yusof 62213220144 2. anis atira binti abdul rahman 62213220212 3. nur sabrina binti mahdzir 62213220002 4. nik aimi sufiah binti nik hamidi ...
Research Proposal on Depression among Teenagers - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. The document discusses depression among teenagers, including causes, symptoms, effects, and treatments. It provides background on depression, stating that it is a common mental health problem worldwide and in the Philippines that can negatively ...
More research is needed to understand whether this indicates a gap in recognition of needed care or overdetection from universal screening in the VA. Although most patients with depression met guidelines for completing treatment within a year of screening positive, only a minority received timely clinical follow-up within 3 to 6 months.
RESEARCH PROPOSAL- DEPRESSION IN TEENS. Introduction Depression is identified as a mood disorder that can affect the daily life of an individual, whereby basically at the moment teenagers are the most affected with depression due to the various predisposing factors that expose them to depression. Teen are relatively young, and range from the ages of 11 to 19 years.
A recent study has shown psilocybin to be more effective than anti-depressant medication for major depression with side effects considered minor and transient. The National Institute for Health ...
Research proposal examples. Writing a research proposal can be quite challenging, but a good starting point could be to look at some examples. We've included a few for you below. Example research proposal #1: "A Conceptual Framework for Scheduling Constraint Management".
Depression is a highly prevalent psychological disorder among young people, characterized by symptoms such as sadness, lack of energy, and despair [].Over the past decade, the incidence of depression has been continuously increasing [2, 3].Studies show that the prevalence of depression among Chinese university students exceeds 25% [4, 5], and the global incidence rate is close to 30% [].
Postpartum depression: Proposal for prevention through an integrated care and support network. September 1997. Applied and Preventive Psychology 6 (4):169-178. DOI: 10.1016/S0962-1849 (97)80006-6 ...
Personality disorders (PD) are described as enduring patterns of markedly deviant and pervasive inner experiences and behaviors, with onset in adolescence, which lead to severe distress or impairment. Patients suffering from major depressive disorder (MDD) display higher rates of comorbidity with personality disorders, often complicating the treatment, and worsening the outcomes. Borderline ...
Depression, schizophrenia and bipolar disorder linked with ancient viral DNA in our genome - new research Published: May 24, 2024 12:24pm EDT. Rodrigo Duarte, King's ...
If yes, you are required to include a PDF or Word document of your NASA Research License as part of your proposal package submission. As described in section 3 of this solicitation, the offeror meets the following requirements completely: 7. All 10 parts of the proposal narrative are included in part order and the page limitation is met.
A virtual two-day seminar from Grant Writers' Seminars and Workshops focusing on writing successful NIH grant proposals. All Duke research personnel involved in writing proposals for funding are invited to attend, though the sessions are geared towards faculty who are writing or planning to write NIH grant applications.