Home — Essay Samples — Nursing & Health — Pathophysiology — A Comprehensive Exploration of Asthma

A Comprehensive Exploration of Asthma
- Categories: Pathophysiology
About this sample

Words: 1260 |
Published: Feb 13, 2024
Words: 1260 | Pages: 3 | 7 min read
Table of contents
Acute asthma, chronic asthma, impact of gender on pathophysiology, diagnosis and treatment.
- Centers for Disease Control and Prevention (2018). Asthma. Retrieved from https://www.cdc.gov/nchs/fastats/asthma.htm
- Dodge, R., R., & Burrows, B. (2018). The prevalence and incidence of asthma-like symptoms in a general population sample. Am Rev Respir Dis 2018; 122:567–75.
- Holgate, S., T. (2017). Genetic and environmental interaction in allergy and asthma. J Allergy Clin Immunol 2017; 104: 1139–46
- Lemanske, R., F., & Busse., W., W. (2017). Asthma: Clinical expression and molecular mechanisms. J Allergy Clin Immunol. 2017, 125: S95-102. 10.1016/j.jaci.2009.10.047.
- Mandhane, P., J., Greene, J., M., Cowan, J., O., et al. (2015). Sex differences in factors associated with childhood and adolescent-onset wheeze. Am J Respir Crit Care Med 2015; 172:45–54
- Thomas, A., O., Lemanske, R.., F., & Jackson, D., J. (2014). Infections and their role in childhood asthma inception. Pediatr Allergy Immunol. 2014; 25: 122–128
- Wright, A., L., Stern, D., A., Kauffmann, F., et al. (2016). Factors influencing gender differences in the diagnosis and treatment of asthma in childhood: the Tucson Children' s Respiratory Study. Pediatr Pulmonol 2016; 41:318–25.
- Wright, A., L., Stern, D., A., Kauffmann, F., et al. (2016). Factors influencing gender differences in the diagnosis and treatment of asthma in childhood: the Tucson Children's Respiratory Study. Pediatr Pulmonol 2016; 41:318–25.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr Jacklynne
Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
10 pages / 4461 words
3 pages / 1416 words
1 pages / 620 words
3 pages / 1427 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Pathophysiology
The article called “Frontiers in the Bioarchaeology of Stress and Disease: Cross-Disciplinary Perspectives From Pathophysiology, Human Biology, and Epidemiology” by Haagen D. Klaus (2014) reviews a few different aspects of a [...]
Syncope and Vertigo are often used as interchangeable terms. This is inaccurate, despite both being forms of dizziness. The term ‘Dizziness’ is given when a patient experiences changes of consciousness, movement, sensation and [...]
The gestational diabetes mellitus ,likewise perceive as GDM is a customary intricacy of certain pregnancies, when hyperglycemia appears throughout the being pregnant . In light of the latest (from 2017) [...]
The scenario presents a 4-month pregnant female with Phenylketonuria (PKU). Due the teratogenic effects that phenylalanine has on a foetus, her GP has advised her to go on a low-protein diet. The distress that this caused to [...]
We are connected to our surroundings by five senses: Sight, smell, taste, touch and hearing. Hearing is more than sounds, it is a biopsychosocial process. There are sounds, with specific features, that can damage our hearing [...]
The ileum is the longest segment of the small intestine and it contains a circular smooth muscular layer. The smooth muscle contains muscarinic acetylcholine receptors which should respond to the presence of acetylcholine (ACh) [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Asthma: pathophysiology, causes and diagnosis
Despite asthma affecting more than 5.4 million people in the UK, there is no gold standard test and diagnosis is based on signs and symptoms.
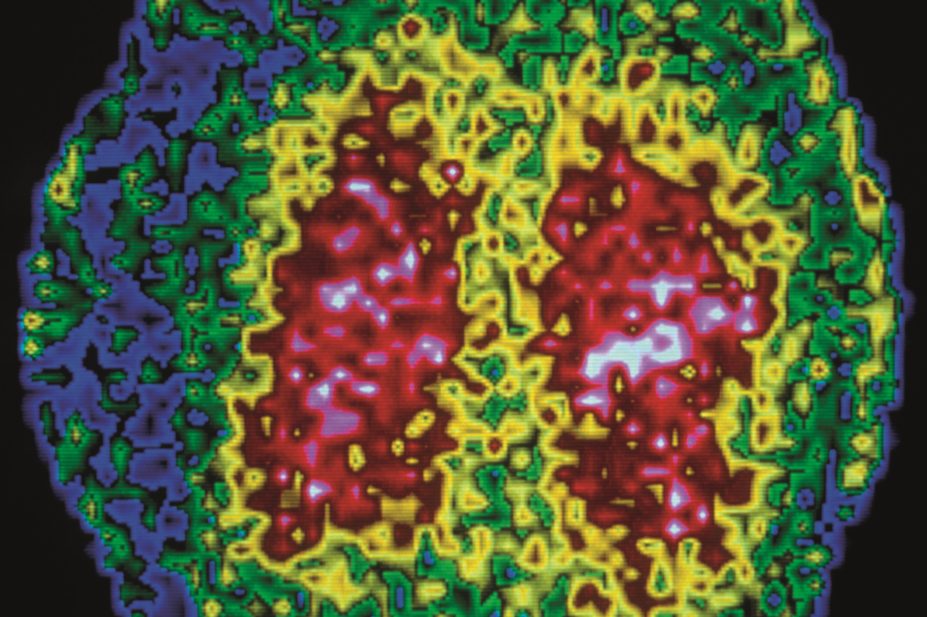
Centre Jean Perrin / Science Photo Library
There is no single cause for asthma, and a range of environmental and genetic factors are known to influence its development. These include premature birth and low birth weight and exposure to tobacco smoke (especially if the mother smokes in pregnancy). It is more common in prepubertal boys, but girls are more likely to remain asthmatic in adolescence.
A diagnosis of asthma in both children and adults is based on assessment of symptoms. The classic signs of asthma are wheezing (especially expiratory wheezing), breathlessness, coughing (typically in the early morning or at night time) and chest tightness. Children and adults with a high probability of asthma on assessment usually start a treatment trial with a corticosteroid such as beclometasone. Children and adults with an intermediate probability of asthma are assessed with lung function tests such as spirometry, peak flow and airway responsiveness to confirm the diagnosis.
Asthma is a chronic inflammatory disorder of the airways. Chronic inflammation causes an increase in airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible, either spontaneously or with treatment [1] .
It is estimated that more than 5.4 million people in the UK are currently diagnosed with asthma, of whom 1.1 million are children. In the UK, asthma causes 1,200 deaths each year, or one death from asthma every eight hours. This number has remained stable over the past few years despite raised awareness [2] , [3] .
Pathophysiology
Asthma is usually mediated by immunoglobulin E (IgE) and precipitated by an allergic response to an allergen. IgE is formed in response to exposure to allergens such as pollen or animal dander [4] . Sensitisation occurs at first exposure, which produces allergen-specific IgE antibodies that attach to the surface of mast cells. Upon subsequent exposure, the allergen binds to the allergen-specific IgE antibodies present on the surface of mast cells, causing the release of inflammatory mediators such as leukotrienes, histamine and prostaglandins. These inflammatory mediators cause bronchospasm, triggering an asthma attack.
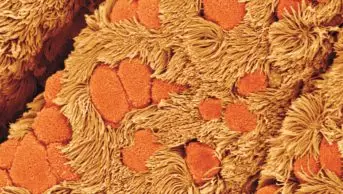
If an attack is left untreated, eosinophils, T-helper cells and mast cells migrate into the airways [1] . Excess mucus production caused by goblet cells plug the airway and, together with increased airway tone and airway hyperresponsiveness, this causes the airway to narrow and further exacerbates symptoms.
There is some evidence to suggest that airway remodelling can occur if asthma is poorly controlled over a period of years. Chronic inflammation causes bronchial smooth muscle hypertrophy, the formation of new vessels and interstitial collagen deposition, which results in persistent airflow obstruction similar to that seen in patients with chronic obstructive pulmonary disease (COPD) [5] .
Although there is no single cause of asthma, certain environmental and genetic factors are known to contribute to the development of the condition. These include:
- Family history of asthma (especially a parent or sibling) or other atopic conditions (for example, eczema or hayfever)
- Bronchiolitis in childhood — 40% of children exposed to respiratory syncytial virus or parainfluenza virus will continue to wheeze or have asthma into later childhood [1]
- Exposure to tobacco smoke, particularly if the mother smokes during pregnancy
- Premature birth
- Low birth weight
- Occupational exposure to plastics, agricultural substances and volatile chemicals, such as solvents. Asthma is more prevalent in industrialised countries
- A body mass index of 30kg/m 2 or more
- Bottle feeding — evidence shows that if an infant is breastfed there is a decreased risk of wheezing illness compared with infants who are fed formula or soya-based milk feeds [3]
Environmental and cultural factors in recent decades, such as changes in housing, air pollution levels and a more hygienic lifestyle (reducing early exposure to allergens), may also increase the risk of asthma.
Asthma is more common in prepubertal boys, but boys are more likely to grow out of their asthma during adolescence than girls [1] .
Phenotyping is becoming increasingly important for clinicians in determining why some people are predisposed to develop asthma and others are not. Furthermore, it is believed that a person’s phenotype may also contribute to the way he or she responds to treatment [6] . For example, variations in the gene that codes for beta-adrenoceptors have been linked to differences in how cells respond to beta-agonists. In the future, as more information emerges, it may be possible to tailor treatments for individual patients to enhance response — which is particularly important as more high-cost, highly specific medicines are being developed [3] , [6] .
Clinical features
There are many factors likely to trigger an asthma attack, and potential causes will vary between patients. Possible triggers include: the common cold; allergens (e.g. house dust mites, pollen); exercise; exposure to hot or cold air; medicines (e.g. NSAIDs); and emotions such as anger, anxiety or sadness.
The classic signs of asthma are wheezing (especially expiratory wheezing), breathlessness, coughing (typically in the early morning or at night time) and chest tightness. Wheezing that occurs as a result of airway bronchoconstriction and coughing are likely to be caused by stimulation of sensory nerves in the airways.
In a severe exacerbation, when there is severe obstruction of the airway, wheeze may be absent and the chest may be silent on auscultation (listening to the chest). In such cases, other signs such as cyanosis and drowsiness may be present, and the patient may be unable to complete full sentences. Severe exacerbations of asthma are medical emergencies.
Diagnosis of asthma is based on medical history, physical examination, lung function testing and response to medication (see ‘Diagnosis of asthma’). There is no gold standard test that can be used to confirm the diagnosis.
Diagnosis of asthma [1]
Clinical features that increase the probability of asthma
- More than one of the following symptoms: wheeze, cough, difficulty breathing, chest tightness, particularly if these are frequent and recurrent; are worse at night and in the early morning; occur in response to, or are worse after, exercise or other triggers; occur apart from colds; are associated with taking aspirin or beta-blockers in adults
- Personal history of atopic disorder
- Family history of atopic disorder and/or asthma
- Widespread wheeze heard on auscultation
- History of improvement in symptoms or lung function in response to adequate therapy (in children)
- Otherwise unexplained peripheral blood eosinophilia, or low forced expiratory volume in one second or peak expiratory flow (in adults)
Clinical features that lower the probability of asthma
- Symptoms with colds only
- Isolated cough with no wheeze or difficulty breathing, or history of moist cough (in children)
- Chronic productive cough with no wheeze or difficulty breathing (in adults)
- Prominent dizziness, light-headedness, peripheral tingling
- Repeatedly normal physical examination of chest when symptomatic
- Normal peak expiratory flow or spirometry when symptomatic
- Cardiac disease (in adults)
- Voice disturbance (in adults)
- History of smoking for more than 20 pack-years (in adults)
Children and adults with a high probability of asthma on assessment usually start a treatment trial, where their response is assessed using spirometry. Children and adults with an intermediate probability of asthma usually have lung function tests conducted, such as spirometry, peak flow and airway responsiveness.
Spirometry can be used to measure lung function and is a good guide to diagnosing asthma in adults. It is not always definitive; normal findings do not exclude a diagnosis of asthma if the patient is well at the time of testing. The spirometric measures used in the diagnosis of asthma are:
- Forced vital capacity (FVC) — the total volume of air expelled by a forced exhalation after a maximal inhalation
- Forced expiratory volume in one second (FEV 1 ) — the volume of air expelled in the first second of a forced exhalation after maximal inhalation
- FEV 1 /FVC ratio
An FEV 1 /FVC ratio below 0.7 is suggestive of airway obstruction, which can increase the probability of asthma, but it can also be caused by conditions such as COPD.
Peak expiratory flow using a peak flow meter measures the resistance of the airway. Although it is not as accurate as spirometry, it can be used to demonstrate variability of lung function throughout the day. Measurements should be taken in the morning and evening (as a minimum) and recorded in a diary to see if there is diurnal variability. Readings are dependent on technique and expiratory effort, therefore the best of three expiratory blows from total lung capacity should be recorded during each session. Peak flow diaries are better for monitoring patients with an established diagnosis of asthma rather than for making an initial diagnosis [1] , [3] .
Assessment of airway responsiveness using inhaled mannitol or methacholine is used for diagnosing patients with normal or near normal spirometry who have a baseline FEV 1 of less than 70% of that predicted using population data. Both drugs induce bronchospasm [1] , [3] . A fall in FEV 1 of more than 15% following a test with mannitol is a specific indicator for asthma. This assessment is useful for distinguishing asthma from other common conditions that can be confused with asthma (for example, rhinitis, gastro-oesophageal reflux, heart failure and vocal cord dysfunction).
A treatment trial in adults involves a patient being prescribed a six-to-eight week trial of inhaled beclometasone 200µg (or equivalent) twice a day, or two weeks of oral prednisolone 30mg daily. An improvement in FEV 1 of 400ml or more following the trial is strongly suggestive of an underlying diagnosis of asthma. Spirometric assessment after a treatment trial is more effective for patients with known airflow obstruction, and is less helpful for patients who had near normal lung function before the trial.
Non-invasive testing of sputum eosinophils and exhaled nitric oxide concentration can also help guide a diagnosis of asthma. A raised sputum eosinophil count (>2%) is seen in around 70–80% of patients with uncontrolled asthma. However, patients with COPD or chronic cough may also exhibit abnormal levels of eosinophils and the test should not be used for definite diagnosis [7] . Sputum eosinophils and exhaled nitric oxide concentration are not routinely measured in general practice, but are in designated difficult asthma clinics [3] . An exhaled nitric oxide level of more than 25 parts per billion supports a diagnosis of asthma.
Assessing asthma control
Many people with asthma do not have their condition well controlled. A survey of 8,000 people with asthma in Europe between July 2012 and October 2012 found that despite 91% of patients considering themselves as having well controlled asthma, only 20% of cases were controlled according to standards set out by national and international guidance [8] .
The aim of asthma management is to achieve and maintain complete control of the disease. This is defined as having:
- No daytime symptoms or night time awakening due to asthma
- No need for rescue medication
- No exacerbations
- No limitations on activity including exercise
- Normal lung function
- Minimal side effects from medication
It is important that control of asthma is measured objectively. One effective way to assess the level of control is the Asthma control test questionnaire (available from asthma.com ). This validated five-point questionnaire is a simple and easy way for patients to self assess their asthma control and guide healthcare professionals to develop a treatment plan in accordance with the results obtained [1] .
[1] British Thoracic Society and Scottish Intercollegiate Guidelines Network. British guideline on the management of asthma. Clinical Guideline 141. London: BTS. October 2014.
[2] Royal College of Physicians (London). Why asthma still kills. London: RCP. May 2014.
[3] Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Geneva: GINA. 2014.
[4] Barnes P. Similarities and differences in inflammatory mechanisms of asthma and COPD. Breathe 2011;7:229–238.
[5] Dournes G & Laurent F. Airway remodelling in asthma and COPD: findings, similarities and differences using quantitative CT. Pulmonary Medicine 2012.
[6] Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med 2012;18:716–725.
[7] Green RH, Brightling CE, McKenna S, et al. Asthma exacerbations and sputum eosinophilia counts: a randomised controlled trial. The Lancet 2002;360:1715–1721.
[8] Price D, van der Molen T, Fletcher M. Exacerbations and symptoms remain common in patients with asthma control: a survey of 8000 patients in Europe. Abstract presented at the European Respiratory Society conference 2013.
You might also be interested in…

Helping respiratory patients breathe easy
Asthma therapies get personal

Asthma: long-term management
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Diet and asthma: a narrative review.

Graphical Abstract
1. Introduction
2. asthma phenotypes and endotypes, 3. airway inflammation, 4. diet and asthma, 4.1. fruits and vegetables, 4.4. fats and fish, 4.6. dairy products, 4.7. dietary patterns, 5. discussion, 6. limitations and strengths, 7. conclusions, 8. future directions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Dharmage, S.C.; Perret, J.L.; Custovic, A. Epidemiology of Asthma in Children and Adults. Front. Pediatr. 2019 , 7 , 246. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2022. Available online: www.ginasthma.org (accessed on 14 March 2023).
- Guilleminault, L.; Williams, E.J.; Scott, H.A.; Berthon, B.S.; Jensen, M.; Wood, L.G. Diet and Asthma: Is It Time to Adapt Our Message? Nutrients 2017 , 9 , 1227. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Andrianasolo, R.M.; Kesse-Guyot, E.; Adjibade, M.; Hercberg, S.; Galan, P.; Varraso, R. Associations between dietary scores with asthma symptoms and asthma control in adults. Eur. Respir. J. 2018 , 52 , 1702572. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Peters, U.; Dixon, A.E.; Forno, E. Obesity and asthma. J. Allergy Clin. Immunol. 2018 , 141 , 1169–1179. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Baena-Cagnani, C.E.; Badellino, H.A. Diagnosis of allergy and asthma in childhood. Curr. Allergy Asthma Rep. 2011 , 11 , 71–77. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Agache, I.; Akdis, C.A. Global Atlas of Asthma ; European Academy of Allergy and Clinical Immunology (EAACI): Zurich, Switzerland, 2021. [ Google Scholar ]
- Ntontsi, P.; Photiades, A.; Zervas, E.; Xanthou, G.; Samitas, K. Genetics and Epigenetics in Asthma. Int. J. Mol. Sci. 2021 , 22 , 2412. [ Google Scholar ] [ CrossRef ]
- Kuruvilla, M.E.; Lee, F.E.; Lee, G.B. Understanding Asthma Phenotypes, Endotypes, and Mechanisms of Disease. Clin. Rev. Allergy Immunol. 2019 , 56 , 219–233. [ Google Scholar ] [ CrossRef ]
- Skloot, G.S. Asthma phenotypes and endotypes: A personalized approach to treatment. Curr. Opin. Pulm. Med. 2016 , 22 , 3–9. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Agache, I.; Eguiluz-Gracia, I.; Cojanu, C.; Laculiceanu, A.; del Giacco, S.; Zemelka-Wiacek, M.; Kosowska, A.; Akdis, C.A.; Jutel, M. Advances and highlights in asthma in 2021. Allergy 2021 , 76 , 3390–3407. [ Google Scholar ] [ CrossRef ]
- Fahy, J.V. Type 2 inflammation in asthma—Present in most, absent in many. Nat. Rev. Immunol. 2015 , 15 , 57–65. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Papi, A.; Brightling, C.; Pedersen, S.E.; Reddel, H.K. Asthma. Lancet 2018 , 391 , 783–800. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Sansone, F.; Attanasi, M.; Di Pillo, S.; Chiarelli, F. Asthma and Obesity in Children. Biomedicines 2020 , 8 , 231. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mims, J.W. Asthma: Definitions and pathophysiology. Int. Forum Allergy Rhinol. 2015 , 5 (Suppl. 1), S2–S6. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Liu, P.C.; Kieckhefer, G.M.; Gau, B.S. A systematic review of the association between obesity and asthma in children. J. Adv. Nurs. 2013 , 69 , 1446–1465. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Rastogi, D.; Holguin, F. Metabolic Dysregulation, Systemic Inflammation, and Pediatric Obesity-related Asthma. Ann. Am. Thorac. Soc. 2017 , 14 (Suppl. 5), S363–S367. [ Google Scholar ] [ CrossRef ]
- Chen, Z.; Salam, M.T.; Alderete, T.L.; Habre, R.; Bastain, T.M.; Berhane, K.; Gilliland, F.D. Effects of Childhood Asthma on the Development of Obesity among School-aged Children. Am. J. Respir. Crit. Care Med. 2017 , 195 , 1181–1188. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Papoutsakis, C.; Priftis, K.N.; Drakouli, M.; Prifti, S.; Konstantaki, E.; Chondronikola, M.; Antonogeorgos, G.; Matziou, V. Childhood overweight/obesity and asthma: Is there a link? A systematic review of recent epidemiologic evidence. J. Acad. Nutr. Diet 2013 , 113 , 77–105. [ Google Scholar ] [ CrossRef ]
- Shan, L.S.; Zhou, Q.L.; Shang, Y.X. Bidirectional Association Between Asthma and Obesity during Childhood and Adolescence: A Systematic Review and Meta-Analysis. Front. Pediatr. 2020 , 8 , 576858. [ Google Scholar ] [ CrossRef ]
- Bhatt, N.A.; Lazarus, A. Obesity-related asthma in adults. Postgrad. Med. 2016 , 128 , 563–566. [ Google Scholar ] [ CrossRef ]
- Eder, W.; Ege, M.J.; von Mutius, E. The asthma epidemic. N. Engl. J. Med. 2006 , 355 , 2226–2235. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Li, X.; Cao, X.; Guo, M.; Xie, M.; Liu, X. Trends and risk factors of mortality and disability adjusted life years for chronic respiratory diseases from 1990 to 2017: Systematic analysis for the Global Burden of Disease Study 2017. BMJ 2020 , 368 , m234. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Zhang, D.; Zheng, J. The Burden of Childhood Asthma by Age Group, 1990–2019: A Systematic Analysis of Global Burden of Disease 2019 Data. Front. Pediatr. 2022 , 10 , 823399. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Barros, R.; Moreira, P.; Padrão, P.; Teixeira, V.H.; Carvalho, P.; Delgado, L.; Moreira, A. Obesity increases the prevalence and the incidence of asthma and worsens asthma severity. Clin. Nutr. 2017 , 36 , 1068–1074. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Miethe, S.; Karsonova, A.; Karaulov, A.; Renz, H. Obesity and asthma. J. Allergy Clin. Immunol. 2020 , 146 , 685–693. [ Google Scholar ] [ CrossRef ]
- Vezir, E.; Civelek, E.; Dibek Misirlioglu, E.; Toyran, M.; Capanoglu, M.; Karakus, E.; Kahraman, T.; Ozguner, M.; Demirel, F.; Gursel, I.; et al. Effects of Obesity on Airway and Systemic Inflammation in Asthmatic Children. Int. Arch. Allergy Immunol. 2021 , 182 , 679–689. [ Google Scholar ] [ CrossRef ]
- Shore, S.A. Obesity and asthma: Lessons from animal models. J. Appl. Physiol. 2007 , 102 , 516–528. [ Google Scholar ] [ CrossRef ]
- Fainardi, V.; Passadore, L.; Labate, M.; Pisi, G.; Esposito, S. An Overview of the Obese-Asthma Phenotype in Children. Int. J. Environ. Res. Public Health 2022 , 19 , 636. [ Google Scholar ] [ CrossRef ]
- Cunha, P.; Paciência, I.; Cavaleiro Rufo, J.; Castro Mendes, F.; Farraia, M.; Barros, R.; Silva, D.; Delgado, L.; Padrão, P.; Moreira, A.; et al. Dietary Acid Load: A Novel Nutritional Target in Overweight/Obese Children with Asthma? Nutrients 2019 , 11 , 2255. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Barros, R.; Delgado, L. Visceral adipose tissue: A clue to the obesity-asthma endotype(s)? Rev. Port. Pneumol. 2016 , 22 , 253–254. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Sood, A.; Shore, S.A. Adiponectin, Leptin, and Resistin in Asthma: Basic Mechanisms through Population Studies. J. Allergy 2013 , 2013 , 785835. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Patel, S.; Custovic, A.; Smith, J.A.; Simpson, A.; Kerry, G.; Murray, C.S. Cross-sectional association of dietary patterns with asthma and atopic sensitization in childhood—In a cohort study. Pediatr. Allergy Immunol. 2014 , 25 , 565–571. [ Google Scholar ]
- Le Chatelier, E.; Nielsen, T.; Qin, J.; Prifti, E.; Hildebrand, F.; Falony, G.; Almeida, M.; Arumugam, M.; Batto, J.M.; Kennedy, S.; et al. Richness of human gut microbiome correlates with metabolic markers. Nature 2013 , 500 , 541–546. [ Google Scholar ] [ CrossRef ]
- Turnbaugh, P.J.; Hamady, M.; Yatsunenko, T.; Cantarel, B.L.; Duncan, A.; Ley, R.E.; Sogin, M.L.; Jones, W.J.; Roe, B.A.; Affourtit, J.P.; et al. A core gut microbiome in obese and lean twins. Nature 2009 , 457 , 480–484. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ley, R.E.; Turnbaugh, P.J.; Klein, S.; Gordon, J.I. Microbial ecology: Human gut microbes associated with obesity. Nature 2006 , 444 , 1022–1023. [ Google Scholar ] [ CrossRef ]
- Halnes, I.; Baines, K.J.; Berthon, B.S.; MacDonald-Wicks, L.K.; Gibson, P.G.; Wood, L.G. Soluble Fibre Meal Challenge Reduces Airway Inflammation and Expression of GPR43 and GPR41 in Asthma. Nutrients 2017 , 9 , 57. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Shore, S.A.; Cho, Y. Obesity and Asthma: Microbiome-Metabolome Interactions. Am. J. Respir. Cell Mol. Biol. 2016 , 54 , 609–617. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jönsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br. J. Nutr. 2011 , 106 (Suppl. 3), S5–S78. [ Google Scholar ] [ CrossRef ]
- Forte, G.C.; da Silva, D.T.R.; Hennemann, M.L.; Sarmento, R.A.; Almeida, J.C.; de Tarso Roth Dalcin, P. Diet effects in the asthma treatment: A systematic review. Crit. Rev. Food Sci. Nutr. 2018 , 58 , 1878–1887. [ Google Scholar ] [ CrossRef ]
- Mishra, V.; Banga, J.; Silveyra, P. Oxidative stress and cellular pathways of asthma and inflammation: Therapeutic strategies and pharmacological targets. Pharmacol. Ther. 2018 , 181 , 169–182. [ Google Scholar ] [ CrossRef ]
- Kudo, M.; Ishigatsubo, Y.; Aoki, I. Pathology of asthma. Front. Microbiol. 2013 , 4 , 263. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Aghasafari, P.; George, U.; Pidaparti, R. A review of inflammatory mechanism in airway diseases. Inflamm. Res. 2019 , 68 , 59–74. [ Google Scholar ] [ CrossRef ]
- Pijnenburg, M.W.; De Jongste, J.C. Exhaled nitric oxide in childhood asthma: A review. Clin. Exp. Allergy 2008 , 38 , 246–259. [ Google Scholar ] [ CrossRef ]
- Tenero, L.; Zaffanello, M.; Piazza, M.; Piacentini, G. Measuring Airway Inflammation in Asthmatic Children. Front. Pediatr. 2018 , 6 , 196. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Bowler, R.P. Oxidative stress in the pathogenesis of asthma. Curr. Allergy Asthma Rep. 2004 , 4 , 116–122. [ Google Scholar ] [ CrossRef ]
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020 , 60 , 2174–2211. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Berthon, B.S.; Macdonald-Wicks, L.K.; Gibson, P.G.; Wood, L.G. Investigation of the association between dietary intake, disease severity and airway inflammation in asthma. Respirology 2013 , 18 , 447–454. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- DeVries, A.; Vercelli, D. Epigenetic Mechanisms in Asthma. Ann. Am. Thorac. Soc. 2016 , 13 (Suppl. 1), S48–S50. [ Google Scholar ] [ CrossRef ]
- Kabesch, M.; Michel, S.; Tost, J. Epigenetic mechanisms and the relationship to childhood asthma. Eur. Respir. J. 2010 , 36 , 950–961. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Norman, R.E.; Carpenter, D.O.; Scott, J.; Brune, M.N.; Sly, P.D. Environmental exposures: An underrecognized contribution to noncommunicable diseases. Rev. Environ. Health 2013 , 28 , 59–65. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Mendes, F.C.; Paciência, I.; Cavaleiro Rufo, J.; Silva, D.; Delgado, L.; Moreira, A.; Moreira, P. Dietary Acid Load Modulation of Asthma-Related miRNAs in the Exhaled Breath Condensate of Children. Nutrients 2022 , 14 , 1147. [ Google Scholar ] [ CrossRef ]
- Cunha, P.; Moreira, A.; Moreira, P.; Delgado, L. Dietary diversity and childhood asthma—Dietary acid load, an additional nutritional variable to consider. Allergy 2020 , 75 , 2418–2420. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Romieu, I.; Barraza-Villarreal, A.; Escamilla-Núñez, C.; Texcalac-Sangrador, J.L.; Hernandez-Cadena, L.; Díaz-Sánchez, D.; De Batlle, J.; Del Rio-Navarro, B.E. Dietary intake, lung function and airway inflammation in Mexico City school children exposed to air pollutants. Respir. Res. 2009 , 10 , 122. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Cardinale, F.; Tesse, R.; Fucilli, C.; Loffredo, M.S.; Iacoviello, G.; Chinellato, I.; Armenio, L. Correlation between exhaled nitric oxide and dietary consumption of fats and antioxidants in children with asthma. J. Allergy Clin. Immunol. 2007 , 119 , 1268–1270. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Mendes, F.C.; Paciência, I.; Cavaleiro Rufo, J.; Farraia, M.; Silva, D.; Padrão, P.; Delgado, L.; Garcia-Larsen, V.; Moreira, A.; Moreira, P. Higher diversity of vegetable consumption is associated with less airway inflammation and prevalence of asthma in school-aged children. Pediatr. Allergy Immunol. 2021 , 32 , 925–936. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Metsälä, J.; Vuorinen, A.L.; Takkinen, H.M.; Peltonen, E.J.; Ahonen, S.; Åkerlund, M.; Tapanainen, H.; Mattila, M.; Toppari, J.; Ilonen, J.; et al. Longitudinal consumption of fruits and vegetables and risk of asthma by 5 years of age. Pediatr. Allergy Immunol. 2023 , 34 , e13932. [ Google Scholar ] [ CrossRef ]
- Sdona, E.; Ekström, S.; Andersson, N.; Hallberg, J.; Rautiainen, S.; Håkansson, N.; Wolk, A.; Kull, I.; Melén, E.; Bergström, A. Fruit, vegetable and dietary antioxidant intake in school age, respiratory health up to young adulthood. Clin. Exp. Allergy 2022 , 52 , 104–114. [ Google Scholar ] [ CrossRef ]
- Wood, L.G.; Garg, M.L.; Powell, H.; Gibson, P.G. Lycopene-rich treatments modify noneosinophilic airway inflammation in asthma: Proof of concept. Free Radic. Res. 2008 , 42 , 94–102. [ Google Scholar ] [ CrossRef ]
- Wood, L.G.; Garg, M.L.; Smart, J.M.; Scott, H.A.; Barker, D.; Gibson, P.G. Manipulating antioxidant intake in asthma: A randomized controlled trial. Am. J. Clin. Nutr. 2012 , 96 , 534–543. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Seyedrezazadeh, E.; Moghaddam, M.P.; Ansarin, K.; Vafa, M.R.; Sharma, S.; Kolahdooz, F. Fruit and vegetable intake and risk of wheezing and asthma: A systematic review and meta-analysis. Nutr. Rev. 2014 , 72 , 411–428. [ Google Scholar ] [ CrossRef ]
- Hosseini, B.; Berthon, B.S.; Wark, P.; Wood, L.G. Effects of Fruit and Vegetable Consumption on Risk of Asthma, Wheezing and Immune Responses: A Systematic Review and Meta-Analysis. Nutrients 2017 , 9 , 341. [ Google Scholar ] [ CrossRef ]
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 Dietary Guidelines for Americans. Available online: https://www.ars.usda.gov/nea/bhnrc/fsrg (accessed on 20 February 2023).
- Vinolo, M.A.; Rodrigues, H.G.; Nachbar, R.T.; Curi, R. Regulation of inflammation by short chain fatty acids. Nutrients 2011 , 3 , 858–876. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Thorburn, A.N.; Macia, L.; Mackay, C.R. Diet, metabolites, and “western-lifestyle” inflammatory diseases. Immunity 2014 , 40 , 833–842. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Zapolska-Downar, D.; Siennicka, A.; Kaczmarczyk, M.; Kołodziej, B.; Naruszewicz, M. Butyrate inhibits cytokine-induced VCAM-1 and ICAM-1 expression in cultured endothelial cells: The role of NF-kappaB and PPARalpha. J. Nutr. Biochem. 2004 , 15 , 220–228. [ Google Scholar ] [ CrossRef ]
- Roduit, C.; Frei, R.; Ferstl, R.; Loeliger, S.; Westermann, P.; Rhyner, C.; Schiavi, E.; Barcik, W.; Rodriguez-Perez, N.; Wawrzyniak, M.; et al. High levels of butyrate and propionate in early life are associated with protection against atopy. Allergy 2019 , 74 , 799–809. [ Google Scholar ] [ CrossRef ]
- Tabak, C.; Wijga, A.H.; de Meer, G.; Janssen, N.A.; Brunekreef, B.; Smit, H.A. Diet and asthma in Dutch school children (ISAAC-2). Thorax 2006 , 61 , 1048–1053. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Han, Y.Y.; Forno, E.; Brehm, J.M.; Acosta-Pérez, E.; Alvarez, M.; Colón-Semidey, A.; Rivera-Soto, W.; Campos, H.; Litonjua, A.A.; Alcorn, J.F.; et al. Diet, interleukin-17, and childhood asthma in Puerto Ricans. Ann. Allergy Asthma Immunol. 2015 , 115 , 288–293.e1. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- de Souza, R.G.M.; Schincaglia, R.M.; Pimentel, G.D.; Mota, J.F. Nuts and Human Health Outcomes: A Systematic Review. Nutrients 2017 , 9 , 1311. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Krogulska, A.; Dynowski, J.; Jędrzejczyk, M.; Sardecka, I.; Małachowska, B.; Wąsowska-Królikowska, K. The impact of food allergens on airway responsiveness in schoolchildren with asthma: A DBPCFC study. Pediatr. Pulmonol. 2016 , 51 , 787–795. [ Google Scholar ] [ CrossRef ]
- Chatzi, L.; Apostolaki, G.; Bibakis, I.; Skypala, I.; Bibaki-Liakou, V.; Tzanakis, N.; Kogevinas, M.; Cullinan, P. Protective effect of fruits, vegetables and the Mediterranean diet on asthma and allergies among children in Crete. Thorax 2007 , 62 , 677–683. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Du Toit, G.; Roberts, G.; Sayre, P.H.; Bahnson, H.T.; Radulovic, S.; Santos, A.F.; Brough, H.A.; Phippard, D.; Basting, M.; Feeney, M.; et al. Randomized trial of peanut consumption in infants at risk for peanut allergy. N. Engl. J. Med. 2015 , 372 , 803–813. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Roduit, C.; Frei, R.; Depner, M.; Schaub, B.; Loss, G.; Genuneit, J.; Pfefferle, P.; Hyvärinen, A.; Karvonen, A.M.; Riedler, J.; et al. Increased food diversity in the first year of life is inversely associated with allergic diseases. J. Allergy Clin. Immunol. 2014 , 133 , 1056–1064. [ Google Scholar ] [ CrossRef ]
- Mazzocchi, A.; Leone, L.; Agostoni, C.; Pali-Schöll, I. The Secrets of the Mediterranean Diet. Does [Only] Olive Oil Matter? Nutrients 2019 , 11 , 2941. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Calder, P.C. Marine omega-3 fatty acids and inflammatory processes: Effects, mechanisms and clinical relevance. Biochim. Biophys. Acta 2015 , 1851 , 469–484. [ Google Scholar ] [ CrossRef ]
- Wood, L.G.; Garg, M.L.; Gibson, P.G. A high-fat challenge increases airway inflammation and impairs bronchodilator recovery in asthma. J. Allergy Clin. Immunol. 2011 , 127 , 1133–1140. [ Google Scholar ] [ CrossRef ]
- Venter, C.; Meyer, R.; Nwaru, B.; Roduit, C.; Untersmayr, E.; Adel-Patient, K.; Agache, I.; Agostoni, C.; Akdis, C.; Bischoff, S.; et al. EAACI Position Paper: Influence of Dietary Fatty Acids on Asthma, Food Allergy and Atopic Dermatitis. Allergy 2019 , 74 , 1429–1444. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Barros, R.; Moreira, A.; Fonseca, J.; Delgado, L.; Castel-Branco, M.G.; Haahtela, T.; Lopes, C.; Moreira, P. Dietary intake of α-linolenic acid and low ratio of n -6: n -3 PUFA are associated with decreased exhaled NO and improved asthma control. Br. J. Nutr. 2011 , 106 , 441–450. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Cazzoletti, L.; Zanolin, M.E.; Spelta, F.; Bono, R.; Chamitava, L.; Cerveri, I.; Garcia-Larsen, V.; Grosso, A.; Mattioli, V.; Pirina, P.; et al. Dietary fats, olive oil and respiratory diseases in Italian adults: A population-based study. Clin. Exp. Allergy 2019 , 49 , 799–807. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Kim, J.L.; Elfman, L.; Mi, Y.; Johansson, M.; Smedje, G.; Norbäck, D. Current asthma and respiratory symptoms among pupils in relation to dietary factors and allergens in the school environment. Indoor Air 2005 , 15 , 170–182. [ Google Scholar ] [ CrossRef ]
- Yang, H.; Xun, P.; He, K. Fish and fish oil intake in relation to risk of asthma: A systematic review and meta-analysis. PLoS ONE 2013 , 8 , e80048. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Papamichael, M.M.; Shrestha, S.K.; Itsiopoulos, C.; Erbas, B. The role of fish intake on asthma in children: A meta-analysis of observational studies. Pediatr. Allergy Immunol. 2018 , 29 , 350–360. [ Google Scholar ] [ CrossRef ]
- Zhang, G.Q.; Liu, B.; Li, J.; Luo, C.Q.; Zhang, Q.; Chen, J.L.; Sinha, A.; Li, Z.Y. Fish intake during pregnancy or infancy and allergic outcomes in children: A systematic review and meta-analysis. Pediatr. Allergy Immunol. 2017 , 28 , 152–161. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Woods, R.K.; Thien, F.C.; Abramson, M.J. Dietary marine fatty acids (fish oil) for asthma in adults and children. Cochrane Database Syst. Rev. 2002 , 2 , Cd001283. [ Google Scholar ]
- Anandan, C.; Nurmatov, U.; Sheikh, A. Omega 3 and 6 oils for primary prevention of allergic disease: Systematic review and meta-analysis. Allergy 2009 , 64 , 840–848. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Burney, P. A diet rich in sodium may potentiate asthma. Epidemiologic evidence for a new hypothesis. Chest 1987 , 91 (Suppl. 6), 143s–148s. [ Google Scholar ] [ CrossRef ]
- Mickleborough, T.D.; Fogarty, A. Dietary sodium intake and asthma: An epidemiological and clinical review. Int. J. Clin. Pract. 2006 , 60 , 1616–1624. [ Google Scholar ] [ CrossRef ]
- Burney, P.G. The causes of asthma—Does salt potentiate bronchial activity? Discussion paper. J. R. Soc. Med. 1987 , 80 , 364–367. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Britton, J.; Pavord, I.; Richards, K.; Knox, A.; Wisniewski, A.; Weiss, S.; Tattersfield, A. Dietary sodium intake and the risk of airway hyperreactivity in a random adult population. Thorax 1994 , 49 , 875–880. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ardern, K.D. Dietary salt reduction or exclusion for allergic asthma. Cochrane Database Syst. Rev. 2004 , 3 , Cd000436. [ Google Scholar ]
- Pogson, Z.; McKeever, T. Dietary sodium manipulation and asthma. Cochrane Database Syst. Rev. 2011 , 2011 , Cd000436. [ Google Scholar ] [ CrossRef ]
- Sozańska, B.; Pearce, N.; Dudek, K.; Cullinan, P. Consumption of unpasteurized milk and its effects on atopy and asthma in children and adult inhabitants in rural Poland. Allergy 2013 , 68 , 644–650. [ Google Scholar ] [ CrossRef ]
- Loss, G.; Apprich, S.; Waser, M.; Kneifel, W.; Genuneit, J.; Büchele, G.; Weber, J.; Sozanska, B.; Danielewicz, H.; Horak, E.; et al. The protective effect of farm milk consumption on childhood asthma and atopy: The GABRIELA study. J. Allergy Clin. Immunol. 2011 , 128 , 766–773.e4. [ Google Scholar ] [ CrossRef ]
- Woods, R.K.; Walters, E.H.; Raven, J.M.; Wolfe, R.; Ireland, P.D.; Thien, F.C.K.; Abramson, M.J. Food and nutrient intakes and asthma risk in young adults. Am. J. Clin. Nutr. 2003 , 78 , 414–421. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Berthon, B.S.; Wood, L.G. Nutrition and Respiratory Health—Feature Review. Nutrients 2015 , 7 , 1618–1643. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Garcia-Larsen, V.; Del Giacco, S.R.; Moreira, A.; Bonini, M.; Charles, D.; Reeves, T.; Carlsen, K.H.; Haahtela, T.; Bonini, S.; Fonseca, J.; et al. Asthma and dietary intake: An overview of systematic reviews. Allergy 2016 , 71 , 433–442. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Reyes-Angel, J.; Han, Y.Y.; Litonjua, A.A.; Celedón, J.C. Diet and asthma: Is the sum more important than the parts? J. Allergy Clin. Immunol. 2021 , 148 , 706–707. [ Google Scholar ] [ CrossRef ]
- Morrissey, E.; Giltinan, M.; Kehoe, L.; Nugent, A.P.; McNulty, B.A.; Flynn, A.; Walton, J. Sodium and Potassium Intakes and Their Ratio in Adults (18–90 y): Findings from the Irish National Adult Nutrition Survey. Nutrients 2020 , 12 , 938. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Medina-Remón, A.; Kirwan, R.; Lamuela-Raventós, R.M.; Estruch, R. Dietary patterns and the risk of obesity, type 2 diabetes mellitus, cardiovascular diseases, asthma, and neurodegenerative diseases. Crit. Rev. Food Sci. Nutr. 2018 , 58 , 262–296. [ Google Scholar ] [ CrossRef ]
- Blonstein, A.C.; Lv, N.; Camargo, C.A.; Wilson, S.R.; Buist, A.S.; Rosas, L.G.; Strub, P.; Ma, J. Acceptability and feasibility of the ‘DASH for Asthma’ intervention in a randomized controlled trial pilot study. Public Health Nutr. 2016 , 19 , 2049–2059. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Li, Z.; Kesse-Guyot, E.; Dumas, O.; Garcia-Aymerich, J.; Leynaert, B.; Pison, C.; Le Moual, N.; Romieu, I.; Siroux, V.; Camargo, C.A.; et al. Longitudinal study of diet quality and change in asthma symptoms in adults, according to smoking status. Br. J. Nutr. 2017 , 117 , 562–571. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Zhang, P.; Lopez, R.; Arrigain, S.; Rath, M.; Khatri, S.B.; Zein, J.G. Dietary patterns in patients with asthma and their relationship with asthma-related emergency room visits: NHANES 2005–2016. J. Asthma 2021 , 59 , 2051–2059. [ Google Scholar ] [ CrossRef ]
- Ma, J.; Strub, P.; Lv, N.; Xiao, L.; Camargo, C.A., Jr.; Buist, A.S.; Lavori, P.W.; Wilson, S.R.; Nadeau, K.C.; Rosas, L.G. Pilot randomised trial of a healthy eating behavioural intervention in uncontrolled asthma. Eur. Respir. J. 2016 , 47 , 122–132. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Garcia-Marcos, L.; Castro-Rodriguez, J.A.; Weinmayr, G.; Panagiotakos, D.B.; Priftis, K.N.; Nagel, G. Influence of Mediterranean diet on asthma in children: A systematic review and meta-analysis. Pediatr. Allergy Immunol. 2013 , 24 , 330–338. [ Google Scholar ] [ CrossRef ]
- Papamichael, M.M.; Itsiopoulos, C.; Susanto, N.H.; Erbas, B. Does adherence to the Mediterranean dietary pattern reduce asthma symptoms in children? A systematic review of observational studies. Public Health Nutr. 2017 , 20 , 2722–2734. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Koumpagioti, D.; Boutopoulou, B.; Moriki, D.; Priftis, K.N.; Douros, K. Does Adherence to the Mediterranean Diet Have a Protective Effect against Asthma and Allergies in Children? A Systematic Review. Nutrients 2022 , 14 , 1618. [ Google Scholar ] [ CrossRef ]
- Tarazona-Meza, C.E.; Hanson, C.; Pollard, S.L.; Romero Rivero, K.M.; Galvez Davila, R.M.; Talegawkar, S.; Rojas, C.; Rice, J.L.; Checkley, W.; Hansel, N.N. Dietary patterns and asthma among Peruvian children and adolescents. BMC Pulm. Med. 2020 , 20 , 63. [ Google Scholar ] [ CrossRef ]
- Menezes, A.M.B.; Schneider, B.C.; Oliveira, V.P.; Prieto, F.B.; Silva, D.L.R.; Lerm, B.R.; da Costa, T.B.; Bouilly, R.; Wehrmeister, F.C.; Gonçalves, H.; et al. Longitudinal Association Between Diet Quality and Asthma Symptoms in Early Adult Life in a Brazilian Birth Cohort. J. Asthma Allergy 2020 , 13 , 493–503. [ Google Scholar ] [ CrossRef ]
- Amazouz, H.; Roda, C.; Beydon, N.; Lezmi, G.; Bourgoin-Heck, M.; Just, J.; Momas, I.; Rancière, F. Mediterranean diet and lung function, sensitization, and asthma at school age: The PARIS cohort. Pediatr. Allergy Immunol. 2021 , 32 , 1437–1444. [ Google Scholar ] [ CrossRef ]
- Douros, K.; Thanopoulou, M.I.; Boutopoulou, B.; Papadopoulou, A.; Papadimitriou, A.; Fretzayas, A.; Priftis, K.N. Adherence to the Mediterranean diet and inflammatory markers in children with asthma. Allergol. Immunopathol. 2019 , 47 , 209–213. [ Google Scholar ] [ CrossRef ]
- Papamichael, M.M.; Katsardis, C.; Lambert, K.; Tsoukalas, D.; Koutsilieris, M.; Erbas, B.; Itsiopoulos, C. Efficacy of a Mediterranean diet supplemented with fatty fish in ameliorating inflammation in paediatric asthma: A randomised controlled trial. J. Hum. Nutr. Diet. 2019 , 32 , 185–197. [ Google Scholar ] [ CrossRef ]
- Zhang, Y.; Lin, J.; Fu, W.; Liu, S.; Gong, C.; Dai, J. Mediterranean diet during pregnancy and childhood for asthma in children: A systematic review and meta-analysis of observational studies. Pediatr. Pulmonol. 2019 , 54 , 949–961. [ Google Scholar ] [ CrossRef ]
- Varraso, R.; Chiuve, S.E.; Fung, T.T.; Barr, R.G.; Hu, F.B.; Willett, W.C.; Camargo, C.A. Alternate Healthy Eating Index 2010 and risk of chronic obstructive pulmonary disease among US women and men: Prospective study. BMJ 2015 , 350 , h286. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Visser, E.; de Jong, K.; Pepels, J.J.S.; Kerstjens, H.A.M.; Ten Brinke, A.; van Zutphen, T. Diet quality, food intake and incident adult-onset asthma: A Lifelines Cohort Study. Eur. J. Nutr. 2023 , 62 , 1635–1645. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Han, Y.Y.; Jerschow, E.; Forno, E.; Hua, S.; Mossavar-Rahmani, Y.; Perreira, K.M.; Sotres-Alvarez, D.; Afshar, M.; Punjabi, N.M.; Thyagarajan, B.; et al. Dietary Patterns, Asthma, and Lung Function in the Hispanic Community Health Study/Study of Latinos. Ann. Am. Thorac. Soc. 2020 , 17 , 293–301. [ Google Scholar ] [ CrossRef ]
- de Castro Mendes, F.; Paciência, I.; Rufo, J.C.; Farraia, M.; Silva, D.; Padrão, P.; Delgado, L.; Garcia-Larsen, V.; Moreira, A.; Moreira, P. Increasing Vegetable Diversity Consumption Impacts the Sympathetic Nervous System Activity in School-Aged Children. Nutrients 2021 , 13 , 1456. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moreira, A.; Moreira, P.; Delgado, L.; Fonseca, J.; Teixeira, V.; Padrão, P.; Castel-Branco, G. Pilot study of the effects of n -3 polyunsaturated fatty acids on exhaled nitric oxide in patients with stable asthma. J. Investig. Allergol. Clin. Immunol. 2007 , 17 , 309–313. [ Google Scholar ] [ PubMed ]
- Li, J.; Pora, B.L.R.; Dong, K.; Hasjim, J. Health benefits of docosahexaenoic acid and its bioavailability: A review. Food Sci. Nutr. 2021 , 9 , 5229–5243. [ Google Scholar ] [ CrossRef ]
- Krebs-Smith, S.M.; Pannucci, T.E.; Subar, A.F.; Kirkpatrick, S.I.; Lerman, J.L.; Tooze, J.A.; Wilson, M.M.; Reedy, J. Update of the Healthy Eating Index: HEI-2015. J. Acad. Nutr. Diet 2018 , 118 , 1591–1602. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Wood, L.G.; Gibson, P.G. Dietary factors lead to innate immune activation in asthma. Pharmacol. Ther. 2009 , 123 , 37–53. [ Google Scholar ] [ CrossRef ]
- Barrea, L.; Muscogiuri, G.; Frias-Toral, E.; Laudisio, D.; Pugliese, G.; Castellucci, B.; Garcia-Velasquez, E.; Savastano, S.; Colao, A. Nutrition and immune system: From the Mediterranean diet to dietary supplementary through the microbiota. Crit. Rev. Food Sci. Nutr. 2021 , 61 , 3066–3090. [ Google Scholar ] [ CrossRef ]
Click here to enlarge figure
| Fruits and Vegetables | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Romieu et al., 2009, Cross-sectional [ ] | A total of 208 children (median age (years)) (quartiles (Q)25, Q75)), comprising 158 asthmatic children, 9.6 (7.9, 11.0 y), and fifty non-asthmatic children, 9.3 (7.9, 11.5 y). | Dietary intake assessed through a 108-item food frequency questionnaire (FFQ): fruit and vegetable index (FVI); Mediterranean diet index (MDI) were constructed. | Higher FVI: (+) inflammation. Higher MDI: (+) lung function. |
| Cardinale et al., 2007, Cross-sectional [ ] | A total of 130 children with mild-to-moderate asthma were included (mean age: N/R). | Dietary intake assessed by 4-point FFQ: 8 food items (margarine, butter, milk, fresh fruit, tomatoes, salad, cooked vegetables and nuts). | Higher consumption of salad: (+) FENO levels. |
| Mendes et al., 2021, Cross-sectional [ ] | In total, 647 children, with 44 asthmatics, were included. mean age = 8.81 ± 0.80 y. | Vegetable intake and fruit intake were assessed by a single self-reported 24-h recall questionnaire. A diversity score for fruits and vegetables was built. | Higher daily vegetable diversity intake: (+) asthma prevalence; (+) airway inflammation; (+) breathing difficulties. |
| Metsälä et al., 2023, Cohort study [ ] | In total, 3053 children, with 184 incidents with asthma. Children were evaluated up to 5 years of age. | Child’s food consumption were assessed by 3-day food records at the age of 3 and 6 months, and at 1, 2, 3, 4, and 5 years of age. Consumption of processed and unprocessed fruits and vegetables was calculated. | All fruits and vegetables intake: (=) asthma prevalence. Leafy vegetables and unprocessed vegetables intake: (+) asthma prevalence. |
| Wood et al., 2008, Randomized controlled trial [ ] | Thirty-two asthmatic adults, mean age ± SEM = 52.1 ± 2.4 y. | Follow-up of a low-antioxidant diet during 10 days, then commence of a randomized, cross-over trial involving 3 × 7-day treatment arms (placebo, tomato extract (45 mg lycopene/day) and tomato juice (45 mg lycopene/day). | Lower intake of antioxidant-rich foods: (−) asthma control; (−) lung function. Lycopene-rich treatments (tomato juice): (+) airway inflammation. |
| Wood et al., 2012, Randomized controlled trial [ ] | In total, 137 asthmatics adults were included, mean age: high-antioxidant diet: 54 ± 14 y; and low-antioxidant diet: 58 ± 15 y. | Individuals were assigned to a high-antioxidant diet (n = 46) or a low-antioxidant diet (n = 91) for 14days and then subjects on the high-antioxidant diet received placebo and subjects on the low-antioxidant diet received placebo or tomato extract (45 mg lycopene/d). | High-antioxidant diet: (+) FEV1, and (+) FVC. Antioxidant supplementation: (=) asthma exacerbations (improvements were only observed after increasing fruit and vegetable consumption). |
| Seyedrezazadeh et al., 2014, Meta-analysis [ ] | Adult and children, papers included in the meta-analysis (n = 42): cohort studies (n = 12); case-control studies (n = 4); cross-sectional studies (n = 26). | Fruit and vegetable intake. | High intake of fruit and vegetables: (+) asthma prevalence; (+) wheezing prevalence. |
| Hosseini et al., 2017, Meta-analysis [ ] | Adult and children, papers included in the meta-analysis (n = 58): cross-sectional (n = 30); cohort studies (n = 13); case-control studies (n = 8); experimental designs (n = 7). | Fruit and vegetable intake. | Vegetable intake: (+) asthma prevalence. Fruit intake: (+) wheeze prevalence; (+) asthma severity prevalence. Fruit and vegetable intake: (+) airway/systemic inflammation. |
| Fiber | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Halnes et al., 2017, Randomized controlled trial [ ] | Twenty-nine subjects with stable asthma, mean age: soluble fiber group: 42.1 ± 3.4 y, control group: 40.4 ± 4.6 y. | Effect of a single meal rich in soluble fiber (175 g yogurt with 3.5 g inulin and probiotics) compared with a simple carbohydrate meal (200 g of mashed potato) on asthmatic airway inflammation. | Soluble fiber intake: (+) inflammation; (+) lung function. |
| Tabak et al., 2006, Cross-sectional [ ] | A total of 598 children, with 39 asthmatics, mean age: 10.4 ± 1.2 y. | Dietary intake was estimated using a semi-quantitative FFQ. | Whole grain products intake: (+) asthma prevalence. |
| Berthon BS et al., 2013, Cross-sectional [ ] | In total, 202 participants, with 137 stable asthmatics. Mean age: healthy controls: 46.7 ± 17.4 y; intermittent, mild, and moderate persistent asthma: 54.5 ± 15.5 y; severe persistent asthma: 57.8 ± 14.4 y. | Dietary intake was estimated through a 186-item semi-quantitative FFQ. | Less fiber intake: (−) forced volume in 1 s (FEV1); (−) airway eosinophilia. |
| Han YY, et al., 2015, Case-control [ ] | A total of 678 children, with 351 asthmatics. Mean age: controls: 10.5 ± 2.7 y, asthma: 10.0 ± 2.6 y. | Dietary intake was assessed through a 75-item questionnaire regarding the child’s food consumption, including wholegrains in the prior week. | High consumption of wholegrains: (+) asthma prevalence. |
| Nuts | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Chatzi, L. et al., 2007, Cross-sectional [ ] | A total of 690 children aged 7 to 18 years, mean age: N/R. | Dietary intake was assessed through a 58-item FFQ, including nuts consumption. | High consumption of nuts: (+) wheezing prevalence. |
| Du Toit, G. et al., 2015, Randomized trial [ ] | In total, 640 infants with severe eczema, egg allergy, or both. Mean age: 7.8 ± 1.7 months. | Participants were stratified into two study cohorts based on the results of a skin-prick test for peanut allergy and were then randomly assigned to a group in which dietary peanuts would be consumed, or to a group in which its consumption would be avoided. | Peanut consumption: (=) asthma at 5 y. |
| Roduit et al., 2014, Cohort study [ ] | A total of 856 children (from 3–12 months to 6 years old) Mean age: N/R. | Assessment of introduction of nuts in the first year of life. | Introduction of nuts in the first year of life: (=) asthma at 6 y. |
| Fats and Fish | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Berthon BS et al., 2013, Cross-sectional [ ] | In total, there were 202 participants, with 137 stable asthmatics, and 65 healthy controls. Mean age: healthy controls: 46.7 ± 17.4 y; intermittent, mild, and moderate persistent asthma: 54.5 ± 15.5 y; severe persistent asthma: 57.8 ± 14.4 y. | Dietary intake was estimated using a 186-item semi-quantitative FFQ. | Higher fat intake: (−) FEV1; (−) airway eosinophilia. Saturated fat: (−) airway inflammation. |
| Cardinale et al., 2007, Cross-sectional [ ] | A total of 130 children with mild to moderate asthma (mean age: N/R). | Dietary intake was estimated using a 4-point food-consumption frequency questionnaire: 8 food items (butter, margarine, milk, tomatoes, fresh fruit, cooked vegetables, salad, and nuts). | Higher butter intake: (−) FENO levels; (−) clinical score severity of asthma. |
| Tabak et al., 2006, Cross-sectional [ ] | In total, there were 598 children, with 39 asthmatics. Mean age: 10.4 ± 1.2 y. | Dietary intake was estimated using a semi-quantitative FFQ. | Fish Intake: (+) asthma prevalence. |
| Wood LG et al., 2011, Randomized controlled trial [ ] | Seventy-two adults, with fifty-one asthmatics. Mean age ± SEMs: Healthy controls high-fat: 49.6 ± 4.6 y. Asthma low-fat/low-energy: 41.7 ± 3.2 y. Asthma-high-fat/high-energy, nonobese: 50.9 ± 4.3 y. Asthma high-fat/high-energy, obese: 56.5 ± 4.3 y. | High-fat/high meal challenge; high-trans (n = 5) or non-trans (n = 5) fatty acid meal challenge. | High-fat/high-energy meal: (−) airway inflammation; (−) bronchodilator responsiveness. High-trans fatty acid meal: (−) airway inflammation. |
| Cazzoletti L et al., 2019, Cross-sectional [ ] | A total of 871 subjects, with 145 asthmatics. Mean age: controls: 51.5 ± 11.5 y. asthmatics: 49.5 ± 11.7 y. | Food intake was collected using an FFQ. | Oleic acid and of olive oil intake: (+) asthma prevalence. |
| Barros R et al., 2011, Cross-sectional [ ] | A total of 174 adult asthmatics. Mean age ± SD: 40 ± 15 years. | Dietary intake was obtained by an FFQ. | High n-6:n-3 PUFA ratio: (−) airway inflammation; (−) asthma control. |
| Kim JL et al., 2005, Cross-sectional [ ] | In total, there were 1014 children, with 78 asthmatics. Median age: 9 (range 5–14 years). | Current consumption and frequency of fish. | Fish consumption: (+) asthma prevalence. |
| Yang H et al., 2013, Meta-analysis [ ] | Adults and children, papers included in the meta-analysis (n = 8), consisting of prospective cohort studies (n = 8). | Fish and fish oil intake. | Fish consumption: (+) asthma prevalence in children; (=) asthma prevalence in adults. |
| Papamichael MM et al., 2018, Meta-analysis [ ] | Children, papers included in the meta-analysis (n = 23): cross-sectional studies (n = 12); case-control studies (n = 2); cohort studies (n = 9). | Fish intake. | All fish (lean and fatty) consumption: (+) asthma prevalence; (+) wheeze prevalence in children up to 4.5 y. Fatty fish consumption: (+) asthma prevalence in children 8 to 14 y. |
| Zhang GQ et al., 2017, Meta-analysis [ ] | Papers included in the meta-analysis (n = 19): cohort studies (n = 8) for fish intake in infancy. | Fish intake during pregnancy or infancy. | Fish consumption: (=) asthma prevalence. |
| Salt | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Ardern KD et al., 2004, Systematic Review [ ] | Studies included in the systematic review (n = 6). Six RCTs were included in the review. | Salt intake. | Dietary salt reduction: (=) symptoms of allergic asthma. |
| Pogson Z et al., 2011, Systematic Review [ ] | Studies included in the systematic review (n = 9): nine RCTs in relation to sodium manipulation and asthma, of which five were in people with asthma (318 participants), and four in people with exercise-induced asthma (63 participants). | Salt intake. | Dietary salt reduction: (+) lung function; (+) symptoms of asthma. |
| Dairy | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Han YY, et al., 2015, Case-control [ ] | A total of 678 children, with 351 asthmatics. Mean age: controls: 10.5 ± 2.7 y. asthma: 10.0 ± 2.6 y. | Dietary intake was estimated using a 75-item questionnaire on the child’s food consumption, including dairy, in the prior week. | Frequent consumption of dairy products: (−) asthma prevalence. |
| Sozańska B, et al., 2013, Cross-sectional [ ] | In total, there were 1700 children, with 78 asthmatics. Mean age: N/R. | Assessment of consumption of unpasteurized milk in the first year of life. | Consumption of unpasteurized milk: (+) asthma prevalence. |
| Loss G, et al., 2011, Cross-sectional [ ] | In total, there were 8334 school-aged children, with 2033 asthmatics. Mean age: N/R. | A comprehensive questionnaire about farm milk consumption was completed by the parents. | Consumption of farm milk: (+) asthma prevalence. |
| Woods RK, et al., 2003, Cross-sectional [ ] | In total, 1601 young adults were included, with 180 asthmatics. mean age: 34.6 ± 7.1 y. | Semiquantitative FFQ, which assessed their habitual food intake over the preceding 12 months. | Whole milk consumption: (+) asthma prevalence. Consumption of low-fat cheese: (−) asthma prevalence. Ricotta cheese intake: (−) asthma prevalence. |
| Dietary Patterns | |||
|---|---|---|---|
| Author, Year, Study Design | Sample, Age | Dietary Assessment/Intervention | Results |
| Andrianasolo RM, et al., 2018, Cross-sectional [ ] | A total of 34,766 adults were included, mean age by tertiles of the Alternate Healthy Eating Index 2010 (AHEI-2010): Women: 1st: 46.7 ± 13.4; 2nd: 53.5 ± 13.1; and 3rd: 57.3 ± 12.4. Men: 1st: 55.8 ± 14.2; 2nd: 60.2 ± 13.0; and 3rd: 62.5 ± 12.0). | Quality of diet was evaluated by three dietary scores: the AHEI-2010, the literature-based adherence score to Mediterranean diet (MEDI-LITE), and the modified Programme National Nutrition Santé Guideline Score (mPNNS-GS) through FFQ. | Higher dietary scores assessed by AHEI-2010, MEDI-LITE, and mPNNS-GS: (+) asthma symptom score. |
| Patel S, et al., 2014, Cohort study [ ] | 1252 children. Follow-up age 8, mean age: 7.98 ± 0.17. Follow-up age 11, mean age: 11.5 ± 0.54. | Dietary Patterns were obtained through FFQ: ‘Traditional’—mostly fruit and vegetables with meat and oily fish ‘Western’—mostly processed foods, which are associated with a modern Western diet (chips, crisps, and pizza) ‘Other’—mostly items that are eaten by people following a vegetarian diet (lentils, soya, rice, and nuts) but also contained fried foods, offal, and pastry dishes. | Following a strict western diet: (−) asthma prevalence. |
| Zhang Y et al., 2021, Cross Sectional [ ] | A total of 1681 individuals, mean age: N/R. | 2015 Healthy Eating Index (HEI-2015). | Low fruit and vegetable intake and low mean ± SE HEI-2015 score: (−) asthma prevalence. |
| Ma J et al., 2016, Pilot randomized trial [ ] | Ninety adults, mean age: 51.8 ± 12.4 y. | 6-month behavioral intervention promoting the DASH diet in patients with uncontrolled persistent asthma. | Adherence to DASH diet: (+) asthma control; (+) asthma-related quality of life. |
| Garcia-Marcos L et al., 2013, Systematic review and meta-analysis [ ] | Children, papers included in the meta-analysis (n = 8), comprising cross-sectional studies (n = 8). | Mediterranean diet. | Higher adherence to the Mediterranean diet during childhood: (+) wheeze prevalence; (+) asthma prevalence; (=) severe current wheeze prevalence. |
| Papamichael MM et al., 2017, Systematic review [ ] | Children Papers included in the systematic review (n = 15): cross-sectional studies (n = 11); intervention trial (n = 1); case-control studies (n = 1); cohort studies (n = 2). | Mediterranean diet. | Following a Mediterranean dietary pattern: (+) asthma prevalence. |
| Tarazona-Meza CE et al., 2020, Cross-sectional study (nested in a case-control study) [ ] | A total of 767 children and adolescents were included (573 with asthma and 194 controls), mean age: 13.8 ± 2.6 y | Diet was assessed using an FFQ, with food groups classified as “healthy” or “unhealthy”. | Better diet quality: (+) asthma prevalence. |
| Menezes AMB et al., 2020, Cohort study [ ] | In total, there were 2986 young individuals. 1st evaluation: 18 years. 2nd evaluation: 22 years. | Longitudinal study with follow-up information from 18- and 22-year-olds. Diet quality was measured with a revised version of the Healthy Eating Index (IQD-R) for the Brazilian population at 18 y and 22 y with FFQ referring to the last 12 months. | Higher values in the Revised Brazilian Healthy Eating Index score, both at 18 and 22 y: (+) wheezing prevalence. Remaining on a poor diet from age 18 to 22 y: (−) wheezing prevalence. |
| Amazouz H et al., 2021, Cross sectional study [ ] | In total, 975 school-aged children were included, age of evaluation: 8 y. | Adherence to the MD was assessed with FFQ and based on two scores: the KIDMED index and the Mediterranean Diet Score (MDS). | Higher tertile group of adherences to the Mediterranean diet: (+) asthma prevalence. |
| Koumpagioti D et al., 2022, Systematic review [ ] | Children, papers included in the systematic review (n = 12): cross-sectional studies (n = 7); randomized controlled trial (n = 1); case-control studies (n = 1); cohort studies (n = 1). | Adherence to MD was measured by diet quality indices as KIDMED and MDS. | Adherence to MD: (+) asthma prevalence. |
| Douros K et al., 2019, Cross-sectional study [ ] | Seventy children, mean age: asthmatic: 8.9 ± 2.4 y. Non-asthmatic: 8.6 ± 2.1 y. | Adherence to MD was estimated with the Mediterranean Diet Quality Index for children and adolescents (KIDMED) score | Higher adherence to MD: (+) IL-4 and IL-17 values. |
| Papamichael et al., 2019, Randomized controlled trial [ ] | Seventy-two asthmatic children, mean age: 7.98 ± 2.24 y. | A single-centered, 6-month, parallel randomized controlled trial comparing the consumption of a Mediterranean diet supplemented with two meals of 150 g of cooked fatty fish weekly (intervention) with the usual diet (control). | Mediterranean diet supplemented with two meals of 150 g of cooked fatty fish: (+) airway inflammation. |
| Zhang Y et al., 2019, A systematic review and meta-analysis [ ] | Papers included in the meta-analysis (n = 16): cross-sectional studies (n = 12); case-control studies (n = 1); cohort studies (n = 5). | Adherence to the Mediterranean diet | Adherence to MD: (=) asthma prevalence; (=) severe asthma prevalence. |
| Visser et al., 2023 Cohort study (105) | A total of 34,698 controls, with 477 incidents of asthma. Mean age: BMI < 25 kg/m : cases: 40.4 ± 13.3 y, Controls: 44.3 ± 12.6 y BMI ≥ 25 kg/m : cases: 46.8 ± 12.5 y, Controls: 49.1 ± 12.0 y | Diet quality-assessed by the Lifelines Diet Score and Mediterranean Diet Score | Higher diet quality: (=) adult-onset asthma prevalence. |
| Varraso et al. (2015), Cohort study [ ] | A total of 73,228 adults. Mean age according to fifths of AHEI-2010: 1st: 48.6 ± 7.2; 2nd: 49.5 ± 7.2; 3rd: 50.3 ± 7.1; 4th: 51.0 ± 7.0; 5th: 52.1 ± 6.8. | Scores of AHEI-2010, assessed by FFQ. | High AHEI-2010 scores: (=) adult-onset asthma prevalence. |
| Han et al. (2020), Cross-sectional study [ ] | A total of 12,687 adults, with 962 asthmatics included. Mean age: no current asthma: 41.4 ± 0.3 y. current asthma: 43.6 ± 0.8 y. | The energy-adjusted Dietary Inflammatory Index [E-DII]) and AHEI-2010 were calculated based on two 24 h dietary recalls. | Higher E-DII score: (+) asthma prevalence; (+) asthma symptoms. AHEI-2010 score: (=) asthma prevalence; (=) asthma symptoms. |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Rodrigues, M.; de Castro Mendes, F.; Delgado, L.; Padrão, P.; Paciência, I.; Barros, R.; Rufo, J.C.; Silva, D.; Moreira, A.; Moreira, P. Diet and Asthma: A Narrative Review. Appl. Sci. 2023 , 13 , 6398. https://doi.org/10.3390/app13116398
Rodrigues M, de Castro Mendes F, Delgado L, Padrão P, Paciência I, Barros R, Rufo JC, Silva D, Moreira A, Moreira P. Diet and Asthma: A Narrative Review. Applied Sciences . 2023; 13(11):6398. https://doi.org/10.3390/app13116398
Rodrigues, Mónica, Francisca de Castro Mendes, Luís Delgado, Patrícia Padrão, Inês Paciência, Renata Barros, João Cavaleiro Rufo, Diana Silva, André Moreira, and Pedro Moreira. 2023. "Diet and Asthma: A Narrative Review" Applied Sciences 13, no. 11: 6398. https://doi.org/10.3390/app13116398
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Asthma Res Pract

Asthma and stroke: a narrative review
A. corlateanu.
1 Department of Internal Medicine, Division of Pneumology and Allergology, Nicolae Testemitanu State University of Medicine and Pharmacy, Stefan cel Mare street 165, 2004 Chisinau, Republic of Moldova
S. Covantev
O. corlateanu.
2 Department of Internal Medicine, Nicolae Testemitanu State University of Medicine and Pharmacy, Stefan cel Mare street 165, 2004 Chisinau, Republic of Moldova
N. Siafakas
3 Department of Thoracic Medicine, University General Hospital, Stavrakia, 71110 Heraklion, Crete, Greece
Associated Data
Not applicable.
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation, bronchial reversible obstruction and hyperresponsiveness to direct or indirect stimuli. It is a severe disease causing approximately half a million deaths every year and thus possessing a significant public health burden. Stroke is the second leading cause of death and a major cause of disability worldwide. Asthma and asthma medications may be a risk factors for developing stroke. Nevertheless, since asthma is associated with a variety of comorbidities, such as cardiovascular, metabolic and respiratory, the increased incidence of stroke in asthma patients may be due to a confounding effect. The purpose of this review is to analyze the complex relationship between asthma and stroke.
Introduction
Asthma is a heterogeneous disease, usually characterized by chronic airway inflammation, bronchial reversible obstruction and hyperresponsiveness to direct or indirect stimuli. It is a problem worldwide with estimated 495,000 deaths every year, thus possessing a significant public health burden [ 1 ]. Asthma complications are often the reason for admission to emergency healthcare service and therefore require special attention [ 2 ]. Asthma is not curable, but it should be controlled by continuous patient assessment in two domains: symptoms control and future risk of adverse outcomes [ 1 ]. Poorly controlled asthma and patients with frequent exacerbations show a greater risk for cardiovascular diseases and ischemic stroke [ 3 , 4 ]. It is also revealed that the pharmacotherapy of asthma, including β2-agonists and systemic corticosteroids, has implications in the development of asthma comorbidities such as stroke [ 5 , 6 ]. In addition, as a chronic inflammation, asthma has also a systemic impact by having a correlation with increased atherosclerotic vessel disorders [ 7 ]. However, smokers with asthma compared to non-smokers with asthma have frequent asthma symptoms, more medication use, poorer lung function and higher prevalence of comorbidities [ 3 ]. This raises the question that stroke in asthmatics may be due to confounding effect (smoking).
Stroke is the second leading cause of death and a major cause of disability worldwide, and there is a further increase in its incidence due to expanding population numbers and aging as well as the increased prevalence of modifiable stroke risk factors [ 8 ]. It was demonstrated that stroke may be more frequent in patients with respiratory conditions [ 9 ]. Therefore, there may be a significant interplay between asthma and stroke, as it may be an independent risk factor for stroke, and its severity exhibits a linear response of stroke development [ 10 ]. These facts represent the base for development of neuropulmonology, which emphasizes the importance of the interconnection between the central nervous and respiratory systems for optimizing the management of patients wherein these pathologies co-exist, especially in the neurocritical care environment [ 11 ].
The purpose of this review is to summarize available data on the association between asthma and stroke and to describe their possible pathophysiological links.
AC, SIu, SC performed the literature review using the terms “asthma”, “stroke”, “subarachnoid hemorrhage”, “smoking”, “SABA”, “LABA”, “SAMA”, “LAMA”, “corticosteroids”, “TPA”, “antiepileptic”, “seizure”, “hypoxia”, “aspirin”, “beta blockers”, “angiotensin converting enzyme”, “comorbidities” along with the MESH terms. The reference list of the articles was carefully reviewed as a potential source of information. The search was based on Medline, Scopus and Google Scholar engines. Selected publications were analyzed and their synthesis was used to write the review and support the hypothesis of the relationship between asthma and stroke.
Risk factors
Shared risk factors between asthma and stroke.
Asthma may be categorized by itself as a risk factor for stroke that is independent of basal lung functioning. It can trigger directly cerebral hypoxemic episodes during asthma attacks or can indirectly increase stroke risk by inducing prothrombotic factors and endothelial dysfunction, thus initiating the development of atherothrombosis [ 12 ]. The major risk factors for stroke are history of hypertension, diabetes mellitus, cerebrovascular disease; tobacco exposure, older age, stress, depression, sleep disorders, obesity [ 13 ]. Some of these risk factors can also be seen in asthma patients and thus the link between asthma and stroke can be to some degree due to confounding effect (Fig. 1 ).

Overlapping risk factors for asthma and stroke
A nationwide population-based cohort study was conducted in an Asian population to investigate the effects of asthma on the risk of stroke. The people enrolled in the National Health Insurance program represented the data source, divided into 2 cohorts: patients with newly diagnosed asthma that received treatment (without stroke baseline), were matched for age, sex and index year with 4 reference subjects without asthma. The risk of stroke was analyzed using Cox proportional hazard regression models. The overall incidence of stroke was greater in the asthmatic cohort than in the non-asthmatic cohort (HR = 1.53, 95% CI = 1.47–1.60) with an adjusted HR of 1.37 (95% CI = 1.27–1.48) when adjusting for age, sex and comorbidities [ 10 ]. Similar results were registered in 2020 in the HUNT study wherein participants with active asthma showed evidence for a modest increased risk for stroke (adjusted HR 1.17, 95% CI = 0.97–1.41) [ 3 ].
Conversely, a recent Korean study did not find increased ischemic stroke risk among asthma subjects (HR = 0.91, 95% CI = 0.86–0.95) [ 14 ]. However, there was a significantly higher risk of stroke among asthma patients who encounter more than 3 exacerbations per year (HR = 3.05, 95% CI = 2.75–3.38) [ 10 ].
Stroke subtypes and asthma
A recent meta-analysis on stroke risk in asthma patients that included five articles comprising 524,637 participants and 6031 stroke cases demonstrated that asthma was associated with a significantly increased risk for (see all similar) developing stroke [ 15 ]. However, it is not clear whether the increased risk persists for all stroke subtypes. The nationwide study on Asian population revealed that patients with asthma were 1.38 fold more likely to develop ischemic stroke (95% CI = 1.27–1.49) and were 1.31 fold more likely to develop hemorrhagic stroke (95% CI = 1.09–1.65) than were the non-asthmatic controls after adjusting for age, sex, and comorbidities. Thus, incidence of both subtypes of stroke are increased in asthma, especially in those with more than three annual exacerbations [ 10 ]. However, the data on subarachnoid hemorrhage (SAH) and asthma is limited mostly presented as case reports [ 16 , 17 ]. In a prospective cohort study of 20,534 men and 7237 women that lasted 26 years baseline lung function, expressed as low FEV1 or FEV1/FVC, was a risk factor for SAH, independently of smoking [ 18 ]. These results suggest that asthma patients may also be at risk for SAH and this depends on degree of obstruction. Therefore, it seems that the current evidence demonstrates an increased risk of all major stroke subtypes in patients with asthma.
Impact of smoking on stroke risk among asthma patients
One of the main risk factor for death after stroke is smoking [ 19 ]. However, the impact of tobacco smoking on health is not limited to those who smoke, but they also affect those in the vicinity who are exposed to secondhand smoke (SHS) [ 20 ]. One of the largest number of deaths attributable to SHS in adults is caused by CAD and stroke [ 21 ]. Current smoking is linked to poorer outcomes of asthma treatment and thus for more frequent exacerbations and medication use, that represents a major additional risk factor for stroke as will be discussed below. In addition, a cohort study on Copenhagen general population emphasizes the substantial role of tobacco smoking in development of asthma’s cardiovascular comorbidities, through comparison of never smokers asthma patients with former or current smokers asthma patients. Adjusted hazard ratios for ischemic heart disease were 1.2 (0.9–1.6) in never smokers, 1.5 (1.2–2.0) in former smokers, and 2.0 (1.4–2.9) in current smokers. Similar results were found for ischemic stroke 1.4 (0.9–2.1) in never smokers, 1.2 (0.8–1.9) in former smokers, and 3.0 (1.7–5.3) in current smokers [ 22 ]. Also, we should mention that smoking is highly associated with COPD, that represent by itself an independent risk factor for stroke [ 23 ]. Asthma and COPD can occur concurrently and is termed as asthma-COPD overlap (ACO). Acute exacerbation of ACO may aggravate hypoxemia and inflammation of blood vessels, which are the key risk factors for CHD and stroke [ 24 ]. Thus, excess of stroke risk in individuals with asthma and smoking could be partly due to ACO or misclassification of COPD as asthma in smokers [ 3 ]. These results bring into light the importance of smoking cessation as a first line action in asthma treatment, since the prevalence of tobacco smoking is similar in individuals with asthma, as it is in the general population [ 25 ].
Pathogenesis and pathophysiology
Atherosclerosis is the main pathophysiological mechanism of stroke development in asthma.
Asthma has a systemic impact that is associated with the development of atherosclerosis and several studies revealed measurable modifications in the structure and function of blood vessels. In details, central pulse wave velocity has the highest values in severe asthma cohort ( p = 0.005); vascular strains presented a relevant decrease of circumferential and radial strains in severe asthma (3.18 ± 0.23%, 3.47 ± 0.20%, respectively) in comparison to controls (4.29 ± 0.35%; p = 0.013) [ 7 ]. Brachial-ankle pulse wave velocity measurement is a marker of early atherosclerotic changes that was assessed in a cohort study, demonstrating an increase in baPWV in patients with asthma compared with control subjects [ 26 ]. Also, asthma was not only associated with preatherosclerotic vessel alterations, such as higher arterial stiffness, but much more with increased prevalence of manifested atherosclerosis compared to non-asthma individuals. Specifically, atherosclerotic plaques were seen in 43.1% of patients with severe asthma, 25% of mild-to-moderate asthma and 14.3% of control study participants ( p = 0.035) [ 7 ]. Subclinical atherosclerosis in asthmatic patients was described in a cross-sectional study, through measurement of carotid and femoral intima thickness, which both were significantly higher in patients with asthma compared to control groups (5.52 ± 0.4 mm vs 5.36 ± 0.4 mm; p = 0.038 and 5.64 ± 0.4 mm vs 5.46 ± 0.5 mm; p = 0.036, respectively) [ 27 ].
Underlying mechanisms in initiating atherosclerosis seems to be related to the hypercoagulable state of asthma. Bazan-Socha and coworkers demonstrated the increase in both thrombin generation and platelet activation and the decrease in fibrinolysis. Asthma patients had 20.0% increased endogenous thrombin potential and 14.4% longer clot lysis time ( p = 0.001) associated with 21.3% higher plasminogen activator inhibitor-1 [ 28 ]. Furthermore, they investigated whether this prothrombotic state is due to chronic inflammation, and showed that asthma was characterized by 62% higher plasma Il-6 and 35% higher TNFα, along with higher CRP, fibrinogen, as well as α2-macroglobulin and PF-4 [ 29 ]. Similar results were obtained also by Sneeboer and coworkers, who revealed high levels of PAI-1, D-dimer, von Willebrand factor and plasmin-α2-antiplasmin complexes in asthma [ 30 ]. While pro-inflammatory cytokine Il-6 is an inducer of acute phase proteins, such as CRP, hepcidin, fibrinogen, which are the cause of increased thrombin generation, PAI-1 and TNFα are the main regulators of fibrinolysis. PF-4 has implications in platelet activation cascade and α2-macroglobulin seems to counteract the enhanced thrombin dynamics, but can also promote coagulation by binding to protein C and accelerate the cascade [ 28 ]. In addition, it was associated an increase in both baPWV and CRP in asthma patients compared with control subjects [ 26 ]. There are evidences that CRP is associated mostly with plaque instability [ 31 ]. It was found a link between the activity of lipoprotein-associated phospholipase A2 and increased risk of atherosclerosis in asthma patients [ 32 ]. The elevated risk of thromboembolic and cardiovascular events in asthma could be also linked to fibronectin, a marker of vascular injury, which is suggested to be a newly determined modulator of prothrombotic plasma properties, and also a sign of the degree of severity of asthma [ 33 ].
All the above findings highlights the importance of evaluating the hypercoagulable state of asthmatic patient in order to monitor as predictors of atherosclerotic and thromboembolic events, events that per se can lead to stroke.
Relationship between FEV1 and stroke risk
The relationship between pulmonary function expressed by forced expiratory volume in 1 s (FEV1) and asthma comorbidities such as CVD or stroke was established by several cohort studies. FEV1 at rest and after response to bronchodilation are the generally accepted surrogate marker of asthma severity. Gulsvik and coworkers conducted an extensive study on 5617 participants, and observed an association between baseline FEV1 and risk of fatal stroke HR = 1.38 (95% CI = 1.11–1.71) and HR = 1.62 (95% CI = 1.22–2.15) for men and women, respectively (adjusted for age and height). The findings could not be explained by smoking, hypertension, diabetes, atherosclerosis, socioeconomic status, obstructive lung disease, physical inactivity, cholesterol or body mass index and persisted in s never-smokers, subgroups without respiratory symptoms and survivors of the first 20 years of follow-up [ 34 ]. Similarly, the Atherosclerosis Risk in Communities study which followed 13,842 middle-aged adults initially free of stroke and CHD for 13 years it was demonstrated that white subjects with impaired lung function have a modestly higher risk of ischemic stroke even if they have never smoked nor had respiratory symptoms [ 35 ].
However, another cohort study suggested a correlation between FEV1 and arterial stiffness in asthmatic patients. In detail, FEV1 in asthmatics was positively correlated with small arteries elasticity index and negatively correlated with the systemic vascular resistance in these patients. These correlations were not observed in non-asthmatic controls [ 36 ]. Moreover, there was a negative correlation between baPWV and FEV1, after adjusting age, gender, BMI and smoking status [ 26 ] and both CIMT and FIMT were negatively correlated with FEV1 (r = − 0.417, p < 0.001 and r = − 0.294, p = 0.007, respectively) [ 27 ]. These findings suggest once more the importance of prospective monitoring and treatment of asthma patients.
Impaired lung function and CVD risk and stroke
The chronic inflammation present in asthma mediates the initiation and progression of atherosclerosis and is intricately involved in plaque rupture and acute CVD events. A large contemporary, multiethnic, long-term, prospective cohort study was conducted by Tattersall and coworkers to analyze the association of asthma and CVD. They found that persistent asthmatics had greater risk of CVD events than non-asthmatics (HR = 1.6, 95% CI = 1.01–2.5), even after adjustment for age, sex, race, CVD risk factors, and antihypertensive and lipid medication use [ 37 ]. Furthermore, a cohort study comprising 446,346 Taiwanese adults, showed similar results: an increase of 27% risk of dying from CVD in individuals with active asthma (adjusted HR = 1.32, 95% CI = 1.08–1.62). Additionally, they established that the risk of death from CHD or stroke was increased in a similar manner (HR = 1.16, 95% CI = 0.77–1.73 and HR = 1.23, 95% CI = 0.86–1.74, respectively). Moreover, deaths from CVD and stroke, were stronger associated with active asthma in men than in women [ 38 ]. Unlikely, a recent study in Korean adults confirmed a significantly higher prevalence of ischemic heart disease (OR = 1.46, 95% CI = 1.25–1.71) in those with asthma, especially, in older patients and// or untreated asthma patients, but stroke was not significantly associated with asthma (OR = 1.17, 95% CI = 0.92–1.48) in adjusted model [ 39 ]. A previous HUNT study concluded that asthma and lack of asthma control were associated with moderately increased risks of atrial fibrillation [ 40 ].
Heart diseases, such as acute myocardial infarction, atrial fibrillation and other can induce stroke. These abnormalities are frequent comorbidities in asthma patients. The prothrombotic state encountered in asthma p that we covered above, along with cardiotoxic effects of beta-2 agonists, that we will cover later, are some of the plausible mechanism of CVD due to asthma. Furthermore, we should mention that long-term effects of airway remodeling due to inflammatory response and the subsequent repair mechanism in asthma can induce irreversible airway obstruction and contribute to decreased lung function over time, leading to chronic hypoxia and oxidative stress that may lead to ischemic heart disease [ 39 ]. Dysfunction of the airway autonomic nervous system in asthma patients could be an inducer of dysfunctional atrial electrophysiology, causing atrial arrhythmias [ 41 ]. Also asthma may be associated with CVD due to other factors such as obesity, smoking, or physical inactivity [ 39 ].
Therefore, CVD through multiple factors are a direct risk factor for stroke. Increased tendency for thrombosis may contribute to thrombus formations inside or outside the ventricular cavity, with subsequent cerebral embolization or rupture of a vulnerable plaque in the remote cerebral circulation. Also, high plasma levels of brain natriuretic peptide and D-dimer are independent risk factors for cardioembolic stroke [ 12 ]. We, therefore, once again underline the importance of monitoring these parameters in asthma patients.
Asthma phenotypes, severity and comorbidities
Asthma phenotypes and stroke.
Early-onset asthma and late-onset asthma are 2 substantially different disease phenotypes and differ in risk factors, pathophysiology, answer to treatment, and incidence of comorbidities, such as CVD, stroke. It has been shown by certain cohort studies that late-onset asthmatics had a higher adjusted risk of CVD than non-asthmatics (HR = 1.57, 95% CI = 1.01–2.45) [ 37 ]. Furthermore, adult asthma was associated with a 1.40-fold (95% CI = 1.35–1.45) increased hazard of CHD, a 1.20-fold (95% CI = 1.15–1.25) hazard of cerebrovascular disease [ 42 ].
In addition, Onufrak et al. conducted a study in which was assessed the correlation between intima-media thickness and adult-onset asthma. They ascertained that the mean CIMT difference between women with adult onset asthma and no history of asthma was attenuated but remained significant (0.713 mm vs. 0.687 mm, p = 0.008), thus demonstrating that adult-onset asthma but not child-onset asthma is associated with increased carotid atherosclerosis among women but not among men. Important to mention that, both men and women with history of adult-onset asthma were older, had less education, lower FEV1, more pack/years of smoking, and were more likely to have diabetes and hypertension than their non-asthmatic counterparts. The mechanism of predisposition of women to atherosclerosis is thought to be linked with hormonal effect on leukotriene production. Women with adult onset asthma also had elevated BMI and reported lower leisure physical activity [ 43 ], again emphasizing the importance of smoking, obesity, sedentariness as the main risk factors for both asthma and atherosclerosis associated with CVD events and stroke.
It was demonstrated that there is a differential enrichment of genes between adult-onset asthma and childhood-onset asthma. In details, patients with the adult-onset form have more gene signatures associated with eosinophilic airway inflammation, mast cells, and group 3 innate lymphoid cells [ 44 ]. It seems that eosinophil cationic protein is a biomarker of coronary atherosclerosis [ 31 ]. It could be implemented especially in adult-onset non-atopic, inflammation-predominant asthma phenotype to quantify ECP in order to improve the monitoring of cardiovascular risk.
Adult-onset asthma is characterized by worse prognosis and poorer response to standard asthma treatment, that the cause of elevated use of beta-adrenergic and glucocorticoid drugs [ 45 ], that could be a secondary risk for CVD events or worsening of comorbidities in asthma patients, as we will point out below.
Asthma control, severity and stroke risk
According to GINA report, asthma symptom control represents an important predictor of asthma outcomes. Thus, uncontrolled asthma is the ultimate step to severe asthma and an important risk factor for exacerbations [ 1 ]. As it was stated in the HUNT study, patients with not controlled asthma had an increased risk of stroke (HR = 1.34, 95% CI = 1.03–1.73) compared to controlled asthma (HR = 1.34, 95% CI = 1.03–1.73) [ 3 ]. Moreover, severe asthma was related to a statistically significant difference in CIMT and FIMT ( p = 0.002 and p < 0.001, respectively) [ 27 ] and the highest risk for AF (adjusted HR = 1.74, 95% CI = 1.26–2.42) [ 40 ]. Likewise, patients with severe asthma had increased baPWV and CRP compared to patients with stable asthma and control subjects [ 26 ].
As we mentioned, there is an obvious risk of atherosclerosis, CVD events in those with severe and uncontrolled asthma. The underlying causes could correlate to the high frequency of comorbid conditions associated with asthma control and severity, [ 46 ] more flare-ups, additional medication use with increasing side-effects, and the remodeling process linked to decreased lung function.
Therefore, it is imperative to have a good control on asthma symptoms by a comprehensive therapy.
Asthma exacerbations and stroke risk
Asthma exacerbations are highly related to further complications, especially myocardial infarction and stroke. Raita and coworkers identified 4607 adults hospitalized for asthma exacerbation who had a first episode of acute myocardial infarction or ischemic stroke. During the reference period, the incidence rate of CVD events was 25.0/100 person-years. In the subsequent risk period of one to 7 days after asthma exacerbations, the incidence rate significantly increased to 129.1/100 person-years with a corresponding adjusted incidence rate ratio of 5.04 (95% CI = 4.29–5.88) [ 4 ]. As well, compared with the non-asthmatic cohort, the patients in the asthmatic cohort that visited the emergency room more than 3 times per year were associated with a significantly higher risk of stroke (adjusted HR = 3.05, 95% CI = 2.75–3.38) [ 10 ]. Moreover patients who have wheeze attacks with shortness of breath have a greater risk for stroke [ 47 ].
There are several potential mechanisms linking asthma exacerbation to the increased incidence of CVD events, including stroke. Specifically, in acute inflammation, thin-cap atheroma could rupture and release inflammatory cells, causing acute accumulation of platelets, neutrophils, and fibrin as well as trapping of red blood cells. Moreover, patients with asthma exacerbation experience hypoxemia, resulting in oxidative stress and insufficient oxygen supply to the myocardium or brain tissue. Also, dysfunction of autonomic nervous system – common mechanism in asthma and coronary vasospasm – could be the cause of myocardial infarction. Furthermore, management of asthma exacerbation, especially excessive use of β2-agonists, necessity of oral or systemic corticosteroids, may have attributed to the subsequent cardiovascular event risks [ 4 ].
Among laboratory parameters describing prothrombotic plasma properties, asthmatics with at least one exacerbation were characterized by longer clot lysis time and lower levels of α2-macroglobulin. Both these laboratory variables were also shown as independent predictors of asthma exacerbation in a multiple logistic regression model [ 48 ]. As we mentioned previously the counteractive function of α2-macroglobulin, lower levels of these universal protease inhibitor in patients with asthma exacerbations, loose the contributing effect to the attenuation of the prothrombotic state, thus the patients become prone to thromboembolic events.
These findings provide opportunities for clinicians to apply cardiovascular prevention measures (antithrombotics) for patients with severe asthma exacerbation during hospitalization and transition to outpatient care [ 4 ].
ACO and stroke
Chronic obstructive pulmonary disease and asthma are the most frequent chronic respiratory diseases that affect the general population and may sometimes coexist [ 49 ]. It is presumed that patients with ACO experience more frequent exacerbations, poorer quality o life, more progressive lung function deterioration, and elevated health care utilization in comparison to asthma or COPD alone. These characteristics, as we explored earlier, dramatically augment the risk of CVD events and stroke. In a cohort study, asthma, COPD and ACO patients were analyzed and differentiated under certain criteria: comorbid conditions, including diabetes, CHD, stroke, were significantly more common in ACO group compared to asthma and COPD groups; the ACO, vs age-matched asthma subgroup had lower prebronchodilator FEV1 (82.1% vs 88%. P = 0.017); also ACO group had significantly more asthma attacks in the past year that the age-matched asthma subgroup (49.8% vs 38.4%) and more participants with blood eosinophil counts ≥400 cells/μL (16.9%) vs COPD (9.5%) and asthma subgroup (6.7%) [ 50 ].
Yeh et al. evaluated the relation between ACO, neurodegenerative diseases and stroke. They showed that for ACO cohort the incidence rate of stroke (18.5 vs 15.1 per 1000 person-years) were higher than did with the non ACO cohort, with a crude HR of 1.23 (95% CI = 1.15–1.32) The main mechanisms of increased stroke risk are: the high frequency of exacerbations that aggravate systemic inflammation, hypoxemia that trigger oxidative stress - which is presumed to be the main mechanism of neurodegeneration, and which in turn aggravate the existing atherosclerosis [ 51 ].
Asthma comorbidities and stroke
Chronic respiratory diseases are associated with a number of comorbidities due to their proinflammatory state [ 52 ]. Asthma is not an exception and there list of commonly encountered comorbidities includes chronic rhinitis, chronic sinusitis/rhinosinusitis, gastroesophageal reflux disease, obstructive sleep apnea/sleep-disordered breathing, psychological disturbances (particularly depression and anxiety disorders), chronic/recurrent respiratory infections, hyperventilation syndrome, hormonal disturbances and other [ 53 ]. There are also possible emerging comorbid conditions such as cardiovascular, obesity, metabolic syndrome, diabetes mellitus, degenerative joint disease/arthritis and psychiatric diseases [ 53 , 54 ]. Some of these comorbidities lead to an increased risk of stroke and are highly prevalent in asthma patient (Table 1 ). This raises the question that the increased risk of stroke in asthma patients may be due to confounding effect. Nevertheless, the important point is that proper screening and diagnosis of comorbidities in asthmatics is essential for preventing serious complications including stroke.
Prevalence of comorbidities in asthmatics and risk of developing stroke
| Comorbidity | Prevalence in asthma patients | Risk of stroke in non-asthmatics |
|---|---|---|
| Hypertension | 12–40% [ ] | in treated controlled group aHR was 2.21 (95% CI, 1.01–4.82), in untreated hypertension group 2.55 (95% CI, 1.93–3.37), in treated uncontrolled group 4.30 (95% CI, 3.16–5.85) [ ] |
| CAD | 7.2–12.9% [ , ] | HR of 1.8 (95% CI, 1.03–3.43) [ ] |
| Atrial fibrillation | 3.8–8.95% [ , ] | aHR 3.13 (95% CI, 1.50–6.56) [ ] |
| Obesity | 21–48% [ – ] | OR 1.57, (95% CI,1.28–1.94) [ ] |
| Diabetes mellitus | 8.4%-31.1 [ , ] | aHR 1.75, 95% CI, 1.64–1.86) [ ] |
| OSAS | 40–50% [ , ] | HR 2.52, (95% CI, 1.04–6.01) [ ] |
| GERD | 25.4–82% [ , ] | 1.68-times more likely (95% CI, 1.03–2.76) [ ] |
Impact of asthma treatment on stroke
Asthma treatment, including bronchodilators and oral or systemic corticosteroids, has been identified as risk factor for CVD events and stroke, whereas, inhaled corticosteroids showed a protective effect. Compared with asthmatic patients who received inhaled corticosteroids the patients who received inhaled SABA or LABA had a significantly increased risk of stroke (aHR-193, 95% CI = 163–227), followed by those who had received both inhaled corticosteroids and inhaled SABA or LABA treatment (aHR = 133, CI = 113–156) [ 10 ]. Also, carotid atherosclerosis is reduced in asthmatic patients treated with ICS compared with matched controls, this study suggests that ICS may have protective effects against atherosclerosis [ 76 ].
Bronchodilators are important in the management of asthma because they play an essential role in reversing airway obstruction and provide “bronchoprotection” against bronchospasm due to exercise and other spasmogenic stimuli, although the current view is that asthma treatment with a bronchodilator should never be started in the absence of an ICS [ 1 ]. Contrary ICS, use of oral corticosteroids, alone or in combination, was associated with greatly enhanced risk of CHD (HR = 2.59, 95% CI = 2.49–2.69), cerebrovascular disease (HR = 1.91, 95% CI = 1.81–2.01) and heart failure (HR = 3.48, 95% CI = 3.34–3.63) [ 42 ]. Oral and systemic corticosteroid therapy comes with known risks for acute and chronic complications, including hypertension, metabolic syndrome, osteoporosis, weight gain, cataracts, gastrointestinal bleeds, impaired wound healing and psychological disorders. Adults receiving SCS treatment had greater odds of complications and greater associated costs over 3 years than matched non-SCS asthma patients [ 5 ]. The adjusted OR for myocardial infarction in current users of oral corticosteroids compared to non-users was 1.42 (95% CI = 1.17–1.72) [ 77 ]. Asthmatic patients have a prothrombotic state that increases with asthma severity. This prothrombotic state is most likely caused by chronic airway inflammation as we pointed above, and combined with the effect of high-dose corticosteroids and might explain the increased risk of patients with severe asthma to have venous thromboembolism [ 30 ]. Most patients with severe asthma are exposed to SCS, which increase SCS-related adverse effects risk. This suggests that SCS exposure should be minimized as recommended by asthma treatment guidelines [ 78 ].
Recent increases in understandings of the mechanisms of asthma and new biomarkers have led to development of potentially more targeted therapy for the management of severe asthma, supplanting the use of long-term steroids and thereby bypassing steroid-related adverse events [ 79 ]. Benralizumab administration for 28 weeks significantly reduced oral glucocorticoid dose by 75% compared with placebo, with about half of subjects receiving baseline prednisone doses of less than or equal to 12.5 mg/d stopping steroids completely [ 80 ]. Dupilumab reduced the rate of severe exacerbations, improved lung function, and improved quality of life in patients with uncontrolled persistent asthma receiving medium- to high-dose ICSs and LABAs [ 81 ]. Furthermore, FEV1 increased after 52 weeks in the low-, medium-, and high-dose tezepelumab groups compared with the placebo group [ 82 ]. Nowadays, pharmacological research has promised safe and effective therapeutic options for patients with severe, uncontrolled asthma, a very complex and heterogeneous entity [ 83 ].
However, a follow-up analysis evaluated the risk of serious cardiovascular and cerebrovascular adverse events and showed a higher crude incidence of these events in omalizumab-treated patients (13.4 per 1000 person-years) compared with non-omalizumab-treated patients (8.1 per 1000 person-years) [ 84 ].
Specific potential adverse cardiovascular effects are more frequent with β2-agonists, including circulatory disturbances via hypokalemia, prolongation of depolarization-repolarization (QT) interval and sinus tachycardia and interference with cardiovascular autonomic control [ 85 ]. There is an apparent association between altered autonomic cardiovascular control and asthma. This relationship is twofold: a consequence of both the pathophysiology of asthma per se and the effects of asthma pharmacotherapy. Consequently, it is possible that these drugs might be implicated in the pathogenesis of a number of CVD risk factors, including insulin-resistance, hypertension and cardiovascular hypertrophy and in the evolution of CHD, cerebrovascular disease and sudden death [ 41 ]. In detail, a nationwide population-based nested case-control study in Taiwan documented that inhaled bronchodilators were independently associated with an increased risk of atrial fibrillation. New users of bronchodilator had the highest risk of atrial fibrillation during first 6 m [ 86 ]. Actually, β2-agonists have been described as a direct or indirect potential mechanism of death in asthmatics; they can induce increased risk of myocardial infarction, congestive heart failure, cardiac arrhythmia/arrest and sudden cardiac death with particularly high-risk of cardiac event in patients with long-QT syndrome [ 87 ]. However, an Australian population based cohort study reported significant associations of incident cardiovascular disease and stroke events in both male and female subjects with traditional risk factors, including use of a SABA. These events were positively associated with as-needed SABA use (OR, 2.66) but not at least once-daily use (OR, 0.81), and there was an inverse and non-significant association of LABA use alone or in combination with ICSs (OR, 0.58), although incident events were correlated with asthma and LABA use with or without an ICS in female subjects [ 88 ]. Furthermore, a nested case-control study showed that the use of inhaled ipratropium was associated with an increased risk of arrhythmia in adolescents and young adults with asthma compared to non-users, although the absolute risk was low [ 89 ]. Theophylline can cause tachycardia and serious arrhythmias even at serum theophylline concentrations considered to be therapeutic. Multifocal atrial tachycardia, an arrhythmia associated with use of this drug, may herald sudden cardiac death. However, there is evidence that doxofylline could offer a promising alternative to theophylline with a superior efficacy and safety profile in the management of patients with asthma [ 90 ]. In young, otherwise healthy asthmatic subjects, combined therapy with theophylline and an oral β-adrenergic agonist (terbutaline) does not lead to an increase in the total number of ectopic beats but may increase the degree of complexity of ventricular premature beats [ 91 ]. This effect could be partly due to hypokalemia and hypomagnesemia were more prevalent among asthmatics that received β2-agonist in either monotherapy or combined with steroid and or theophylline [ 92 ].
Nonetheless, both β-agonists and xanthines have direct effects on the human lower esophagus. These actions most probably are due to an inhibitory effect on active resting tension in the circular muscle layer of the human esophago-gastric junction. Actually, inhaled salbutamol reduces lower esophageal sphincter basal tone and contractile amplitudes in the smooth muscle esophageal body in a dose-dependent manner and may increase the likelihood of acid reflux at least in patients who receive cumulative dosing, and theophylline treatment causes a significant increase in total reflux time and reflux symptoms but does not worsen asthma [ 93 ]. Anticholinergic agents not only influence lower esophageal sphincter performance, but also affect other activities in the gastrointestinal tract that are involved in the etiology of reflux. They decrease saliva secretion, esophageal peristalsis, TLOSRs, gastric emptying, and gastric acid production [ 94 ].
Alternatively, Lee and coworkers showed that inhaled respiratory treatments including LAMA have no effects on the development of stroke. LAMA use was not significantly associated with any increase in the risk of stroke in total study group (in total LAMA; aOR, 0.97; 95% CI, 0.90–1.05) or any subgroup. After adjusting for covariates, there were no statistically significant effects of inhaled drugs on the stroke incidence. All of the aOR ranges were between 0.97 and 1.08. The inhaled bronchodilators did not affect either hemorrhagic or ischemic strokes. However, ICS without LABA was statistically significantly associated with hemorrhagic stroke (aOR, 1.51; 95% CI, 1.01–2.25) [ 95 ].
Impact of stroke treatment on asthma
Several medications are used in treatment and prophylaxis of stroke. Although, it is not commonly underlined but some of them can have positive and negative effects in asthma patients.
Tissue plasminogen activator (TPA) is the main drug that revolutionized the management of ischemic stroke. As with any other drug there have been cases of anaphylactic reaction which require emergency treatment. Allergic reactions included angioedema, facial swelling, urticaria, skin rash, cutaneous hypesthesia, hypotension, anaphylactic shock, and death [ 96 ]. The true incidence of these events is hard to assess. Out of 924 adverse events only 12 cases were directly attributed to IV thrombolytic medication. Eleven cases were due to IV alteplase and one due to IV reteplase [ 96 ]. Asthma patients are generally more likely to have allergic events due to the atopic nature of their disease [ 97 , 98 ]. TPA is an essential lifesaving medication for ischemic stroke that is associated with an improvement of quality of life and general prognosis of the disease [ 99 , 100 ]. However, as asthma patients are prone to allergic events general awareness of the possible side effects are important to consider in selective cases. Mild allergic reaction that involve skin and subcutaneous tissue generally responds well to steroids and antihistamine drugs, however they should not be confused with acute anaphylaxis which requires epinephrine [ 101 , 102 ]. In cases of orolingual angioedema the general steps in the management are stopping the TPA infusion, diphenhydramine, ranitidine/famotidine, methylprednisolone, epinephrine, and otolaryngology or anesthesia consult with the assessment of airways every 15–20 min [ 103 – 105 ].
Aspirin and non-steroidal anti-inflammatory medication are well known drugs that can trigger allergies particularly in asthma patients (Samter’s triade) [ 106 ]. This limits the use of aspirin as an antithrombotic drug in clinical practice as a method to achieve optimum medical management prior to and after neurointerventional treatment [ 107 ]. In this group of patients aspirin desensitization therapy can be used to overcome this problem and have proven their effectiveness in cardiovascular and cerebrovascular disease [ 107 , 108 ]. Clopidrogel and ticlopidine allergies can be managed in a similar fashion [ 109 ].
β-blockers are frequently used to manage arrhythmias, hypertension and other cardiovascular disease. Traditionally, they are contraindicated in patients with asthma as they may lead to bronchoconstriction and exacerbate the condition. However, there is more data on the use of β-blockers in fundamental and clinical practice [ 110 ]. There is a debate between the use of selective versus non-selective β-blockers as some studies indicate that selective β-blockers possess less risk for asthma patients [ 111 , 112 ]. Therefore, it seems that β-blockers can be used more widely when they are indicated but when the cardiovascular risks overweight the risk for pulmonary complications [ 113 ]. Another group of drugs frequently used to manage hypertension are angiotensin converting enzyme inhibitors. Although, that they do not cause changes of pulmonary function they can cause cough and wheezing which can be interpreted as asthma manifestation [ 114 ]. Therefore angiotensin-receptor blockers are a better alternative for asthma patients [ 115 ]. Hypertension can also be managed with calcium channel blockers. They are not contraindicated in asthma and in some types of asthma can event be beneficial for lung function improvement [ 116 ].
Seizures are a frequent complication in stroke patients. Interestingly, asthma patients have a higher risk of epilepsy [ 117 ]. This makes them particularly at risk of stroke-associated seizures. Some antiepileptic drugs might play roles in preventing or reducing the frequency of asthma attacks particularly phenytoin, valproic acid and carbamazepin [ 118 – 120 ]. Interestingly, lidocaine that works primarily by blocking sodium channels and decreasing membrane excitability is effective in a form of nebulizer for treating asthma patients [ 121 ]. Although, this group of medications is not the standard of care in asthma, reports of antiepileptic drug efficiency raises several important questions that some patients have a neurogenic component to their disease, particularly in a form of channelopathies.
Disease progression, relationship and prevention
Overall pathophysiological mechanisms from asthma to stroke.
Based on the evidences presented above we may argue that atherosclerosis could be the main pathophysiological mechanism in development of stroke in asthma patients, including the facts analyzed previously (Fig. (Fig.2). 2 ). This concept is also sustained by other studies which try to explain in detail the pathways that potentially explain how lung inflammation can trigger acute vascular events such as heart attacks and stroke. Lung inflammation due to COPD, asthma, infection, or exposure to air pollution results in a systemic inflammatory response (split over) with increase in the levels of circulating leukocytes, platelets, cytokines, and acute-phase proteins. These mediators activate the vascular endothelium, causing endothelial dysfunction that is characterized by reduced vasodilatation with decreases in nitric oxide (NO), increases in endothelin (ET) expression, and increases in vascular permeability and the uptake of oxidized low-density lipoproteins (LDLs) into atherosclerotic plaques. Collectively, these events destabilize plaque by the up-regulation of adhesion molecules with accelerated leukocyte recruitment, increase foam cell formation and the recruitment of smooth muscle cells, release and activate proteases that degrade the extracellular matrix and destabilize plaques, making them vulnerable for rupture [ 122 ]. Indeed, a cohort study demonstrated the close interplay between systemic endothelial dysfunction and lung dysfunction could begin already prior to the development of overt respiratory or cardiovascular disease and suggest that even individuals with mild impairment of lung function may have vascular damage that increase the risk for cardiovascular disease [ 123 ]. Therefore, patients with asthma may induce an inflammatory environment that favor atherosclerosis progression [ 124 ].

Atherosclerosis as a major pathophysiological mechanism in development of stroke in asthma patients
The burden of cardiovascular comorbidity in obstructive airway disease is increasingly acknowledged, and there is a need of identifying which patients are at an increased risk and thus to facilitate optimal treatment and prevention [ 125 ].
Impact of stroke in lung function
Pulmonary complications, such as respiratory failure, pneumonia, pleural effusion, acute respiratory distress syndrome, pulmonary edema, and pulmonary embolism from venous thromboembolism, are common in stroke and are among the major causes of death in stroke patients [ 126 ]. For instance, a cohort study assessed the lung function of stroke survivors and the main finding was that lung function was significantly lower in stroke patients compared with healthy participants: lower values for FEV1 (81% of predicted value vs. 95% predicted), FVC (82% vs 92% of predicted values), and PEF (52% vs 70%). Also, chest excursion was markedly lower for stroke survivors when compared to control group (3.0 ± 0.71 vs 3.5 ± 0.91 cm), which may result from weakened respiratory muscles [ 127 ].
Besides, Jung and coworkers demonstrated through ultrasonographic diaphragmatic motion analysis that diaphragmatic excursion in right-hemiplegic patients was reduced on both sides compared to that in control subjects. However, in left-hemiplegic patients diaphragmatic excursion is reduced on the left side and increased on the right side compared to that in control subjects and left diaphragmatic motion during deep breathing correlates positively with FVC (r = 0.86, p = 0.007) and FEV1 (r = 0.79, p = 0.021) [ 128 ].
The mechanism of lung damage after brain injury is described through a “double hit model”: the catecholamine storm and the systemic production of inflammatory mediators (first hit) create a systemic inflammatory environment which increases pulmonary vascular hydrostatic pressure and activates biological mechanisms that make the lung more susceptible to mechanical and non-mechanical insults (second hit), including mechanical ventilation. Indeed, a study on mice showed that ischemic stroke caused a significant increase in bronchoalveolar lavage fluid macrophages and neutrophils and whole lung tissue pro-inflammatory IL-1βmRNA expression [ 129 ]. Furthermore, the phagocytic ability of macrophages from BALF is markedly reduced in post-stroke rats [ 130 ]. Thus, damage to the alveolar capillary barrier leads to pulmonary ventilation disorder, blood perfusion disorder and oxygenation disorder, such as acute, life-threatening neurogenic pulmonary edema that occurs in about 23% of SAH patients [ 131 ].
After stroke, damage to the blood-brain barrier leads to recruitment of resident and peripheral immune cells to the affected area, resulting in a reduction in circulating immune cells and a depression of peripheral immunity that increases the susceptibility to infection [ 126 ]. Indeed, a study on mice revealed that immunosuppression after stroke is related to an increased expression of inflammatory mediators and hypothalamic-pituitary-adrenal axis activation which induces elevated glucocorticoid secretion [ 132 ].
Stroke-associated pneumonia incidence is high and can be due to: stroke-induced immunodepression syndrome, dysphagia, decreased level of consciousness, all risk factors for aspiration pneumonia [ 126 ]. In fact, a cohort study demonstrated that in ischemic stroke patients requiring invasive ventilation, pneumonia occurred in 40% of cases and was associated with a 49% increase in 1-year mortality [ 133 ].
Thus, brain-lung crosstalk is relevant to prevent further pulmonary complications after stroke. In detail, protective ventilation has to be considered in this population to obtain the target of normoxia and normocapnia avoiding high tidal volume. Respiratory muscle training showed to improve the strength and decrease the risk of respiratory complications in stroke survivors [ 134 ]. Also, interventions targeting plasma fibronectin may reduce brain damage following reperfusion – a promising reperfusion therapy for patients with acute ischemic stroke [ 135 ].
Impact of stroke on asthma outcomes
Stroke is associated with major complications, such as, dysphagia, GERD, aspiration, immunodepression and pneumonia [ 136 , 137 ]. Obstructive airway disease, such as asthma, is the most common extraesophageal manifestation of GERD, with a prevalence of 52.67% in a cohort study and a statistically significant correlation of severity of GERD and severity of bronchial asthma [ 138 ]. In addition, GERD is responsible for a high number of annual exacerbations, consultations, hospitalizations and very frequent use of short-acting bronchodilators in asthma patients [ 139 ].
Besides, GERD and the use of acid suppressing agents (histamine-2 receptor antagonists and proton pump inhibitors) which are commonly used in GERD [ 140 ]; dysphagia, the compromised immune state and the use of corticosteroids are all risk factors for SAP [ 141 ]. SAP is not associated with increased long-term mortality, but it is linked with increased mortality up to 1 y, prolonged length of stay, and poor functional outcome on discharge [ 142 ].
Impact of asthma on stroke outcomes
Stroke outcomes could be influenced in long-term by chronic inflammatory airway disease. In a cohort study, history of CIAD was independently associated with mortality during long-term follow-up (HR = 1.42, 95% CI = 1.02–2.00). However, CIAD was not significantly associated with short-term mortality after stroke. Furthermore, CIAD is an independent risk factor for pneumonia after stroke – pneumonia being a major cause of death in stroke patients [ 143 ]. Also, there is a consistent, independent and long-lasting association between lung function and fatal stroke [ 34 ]. A statistical interplay between mortality due to stroke in asthma patients was demonstrated by Strand and coworkers. Moreover, individuals with active asthma showed an increased risk of dying from CVD [ 38 ]. Stroke outcomes might be exacerbated by fibronectin, which promotes inflammation of the thrombus [ 135 ].
As we underlined previously, that asthma patients are at risk in developing atherosclerosis, atrial fibrillation, myocardial infarction, stroke and maybe even recurrent stroke. Asthma exacerbations, ACO and uncontrolled asthma could have an additional risk for poorer prognosis after stroke. Further studies should investigate whether the incidence of worse outcomes after stroke and recurrent stroke in asthma patients is increased. Similarly, in the current guidelines, asthma is not considered a relevant comorbidity to be addressed for primary or secondary stroke prevention. However, current data reveals a relevant interaction between asthma and stroke and thus this statement should be reviewed.
Prevention of stroke in asthma patients
Since stroke is an acute, burdensome, and preventable condition several preventive options may be useful in asthma patients.
Firstly, we should focus on modifiable risk factors for stroke, such as obesity and tobacco use, that could certainly have a great impact on asthma outcomes, stroke prevention, as well as, stroke outcomes. Obesity can trigger asthma development through several mechanism, but also it is associated with worsening of asthma symptoms, increased exacerbations, unresponsiveness to standard therapy [ 144 ]. Scott and coworkers found that weight loss in an obese asthma population significant improves health status among participants [ 145 ]. In addition, there is evidence that obesity is associated with bronchodilator unresponsiveness among black and Latino children and adolescents with asthma [ 146 ]. Obesity-related asthma which usually develops in adulthood might be a particular importance to the development of CVD events [ 38 ]. The importance of smoking cessation we have elucidated so far.
As we emphasized the importance of monitoring asthma patients via standard clinical and laboratory tests, in order to identify subclinical atherosclerosis prior to progression to full CVD complicated by acute events. We mentioned the acute phase reactants, like CRP, hepcidin, fibrinogen; fibronectin, α2-macroglobulin, PAI-1, von Willebrand factor, D-dimer, brain natriuretic peptide; measurement of clot lysis time, arterial stiffness through PWV. All of these are either detecting and thus preventing CVD events or are predictors of the outcomes from those events. A study suggested that routine administration of the CVHI in a primary prevention population would yield the benefits of identifying patients with existing subclinical CVD [ 147 ].
Asthmatics have a prothrombotic state that could be counteracted by heparin or enoxaparin therapy. Early studies described subjective improvement of asthma symptoms using intravenous or inhaled heparin [ 148 ]. Especially for asthma patients with estimated CVD and stroke risk it should be taken into account the adjuvant anticoagulant therapy. Furthermore, clinical studies of patients with asthma reveal heightened platelet activation and accumulation into lung tissue, thus suggesting the need for further research to exploit the potentially powerful anti-inflammatory applications possessed by anti-platelet drugs [ 149 ].
In addition, the therapy of each asthma patient should be customized according to its severity, phenotype and endotype, its congruency and response to it, as well as current comorbidities. Target therapy is the future strategy, that could minimize the risk for complications, such as stroke [ 83 ].
Statins have been shown to have multiple pleiotropic effects other than its lipid lowering activity by modulating multiple signaling pathways that govern inflammatory, mucus-inhibitory, oxidant stress and proliferation. Thus, the repurposing of statins from conventional anti-cholesterol oral therapy to inhaled anti-inflammatory formulation is promising, as it provides direct delivery to the airways, reduced risk of side effects, increased bioavailability and tailored physical-chemical properties for enhanced efficacy. Inhaled statins act by reducing airway inflammation and oxidation; regulating NOS, as well as, attenuating airway remodeling by regulation of MMP expressions and decrease MUC gene expression [ 150 ]. Indeed, a cohort study demonstrated that CHD risk was lower in all statin users, regardless of the duration of use, whereas ischemic stroke risk was lower only in the long-term statin users [ 24 ]. Consistent with these results, Chou et al. reported that in adults with a high risk of CVD but no prior CVD events, statin use is associated with a low risk of CVD events, and patients at a high baseline risk have relatively greater absolute benefits (e.g., those with hypercholesterolemia) [ 151 ]. Moreover, the use of ICS or OS with statins has an additive effect [ 152 ]. A group showed that treatment of OVA-exposed mice with i.t. pravastatin (30 mg/kg) improved asthma pathology [ 153 ]. Oxidative stress is a constantly discussed component of both of the disease and there is ongoing research for adequate antioxidant therapy [ 154 ].
Vitamin D is a recognized modulator of the immune response, which is required for an adequate physiologic response to inflammatory diseases and immune-system mediated diseases; thus, vitamin D status play a role in the association between asthma and stroke. Indeed, calcitriol acts as a direct transcriptional regulator of endothelial nitric oxide (NO) synthase (eNOS), and can promote normalization of eNOS mRNA expression and enzymatic activity in experimental atherosclerosis. Overall, it is plausible that the impaired endothelial function that may accompany low circulating vitamin D levels contributes to an increased risk of cerebrovascular diseases and mortality [ 155 ]. In asthma, reduced vitamin D levels are associated with impaired lung function, increased AHR, and reduced GC response, suggesting that supplementation of vitamin D levels in patients with asthma may improve a number 0f parameters of asthma severity and treatment response [ 156 ]. Actually, a cohort study revealed that FEV1 percent predicted and FEV1/forced vital capacity ratio showed a significant positive correlation with vitamin D levels. Also, the use of inhaled steroids, use of oral steroids, and the total steroid dose all showed significant inverse correlations with vitamin D levels. This findings support that vitamin D enhances the anti-inflammatory effects of glucocorticoids, and could be as a potential steroid-sparing agent in patients with moderate-to-severe persistent asthma, as well as a modifier of asthma disease severity [ 157 ]. Furthermore, low serum levels of vitamin D at admission have been proposed as an independent prognostic biomarker for greater stroke severity, a poorer functional outcome at discharge, a higher risk of death at one or 2 y, and a greater risk of early recurrent stroke [ 158 , 159 ].
Vagal nerve stimulation appears to be a safe and feasible modality for use in the treatment of moderate to severe, acute asthma exacerbations in patients unresponsive to initial standard of care and as a rescue intervention for mild-to-moderate asthmatic attacks. Maybe neurostimulation could be an option for management of asthma exacerbations, thus preventing complications [ 160 ].
Summary and future perspective
It is important to clarify whether asthma increase the risk of all stroke types and to elaborate safe and effective methods for stroke prevention. More studies are required to evaluate whether, adjusting the therapy with anticoagulants is a correct strategy, as well as, which predictors are the best to be implemented in routine monitoring of asthma patients. In general, the interaction between lungs and the brain is complex (Fig. 3 ). The pro-inflammatory state generated at the level of the lungs leads to atherosclerosis, comorbid conditions, procoagulatory state. SCS therapy decreases the inflammatory process but in turn, also leads to cardiovascular and metabolic diseases. Although, ICS are safer, they are also linked to comorbidities. SABA and LABA are directly linked to arythmogenic effect, which in turn can lead to thromboembolism. It seems that all of the abovementioned main drug groups that are used for asthma treatment are to some degree linked to stroke. Antimuscarinic agents on the other did not demonstrate this effect. Similarly, there are other emerging drug groups which may demonstrate a better safety profile regarding cardiovascular and metabolic comorbidities as well as stroke risk. We also need agents that can effectively combat and limit the inflammatory state at the level of the lungs. Asthma-related comorbidities should be at special attention in lights of the fact that the majority are linked to cerebrovascular disease.

The complex interaction between lungs and the brain
No clinical studies were found on the use of inhaled statins. Furthermore, studies on reformulating statins as an inhaled therapy are still in their infancy and further investigations are required to better understand the efficacy, toxicity and mechanism of action of these statin molecules in the airways and in the prevention of stroke.
The findings of vitamin D implications in asthma evolution and stroke outcomes should be confirmed in a prospective fashion that involves the generation of an efficient multivariate model, in order to include vitamin D supplementation as an adjuvant therapy for asthma patients, especially those with increased risk for stroke.
Furthermore, current treatment options are limited and may not be effective for all patient populations. Hence, new treatment options with superior efficacies to treat these diseases are urgently required as potential substitution, alternative or adjunct therapy to currently available therapies.
Conclusions
Asthma is a heterogeneous disease with several key pathophysiological mechanisms that impact the whole body. There is enough data that suggests the association between asthma and atherosclerosis, which in turn leads to CVD and stroke. It seems that asthma may increase the risk of both ischemic and hemorrhagic stroke. The proper management of asthma, prevention of exacerbations, as well as, prospective monitoring and the use of adjuvant therapy are essential to decrease the risk for stroke and improve its outcomes. Asthma comorbidities should be at special attention and there is need for a better understanding of limitations of the current treatment strategies.
Acknowledgements
Abbreviations.
| ACO | Asthma-COPD overlap |
| AHR | Airway hyperresponsiveness |
| TPA | Tissue plasminogen activator |
| baPWV | Brachial-ankle pulse wave velocity |
| BALF | Bronchoalveolar lavage fluid |
| BMI | Body mass index |
| CIMT | Carotid intima media thickness |
| CVD | Cardiovascular disease |
| CHD | Coronary heart disease |
| CVHI | Cardiovascular health index |
| CIAD | Chronic inflammatory airway disease |
| COPD | Chronic obstructive pulmonary disease |
| CRP | Reactive C protein |
| ECP | Eosinophilic cation protein |
| HR | Hazard ratio |
| GC | Glucocorticoids |
| GERD | Gastroesophageal reflux disease |
| ICS | Inhaled corticosteroids |
| IL | Interleukin |
| PAI-1 | Plasminogen activator inhibitor 1 |
| PF-4 | Platelet factor 4 |
| TNFα | Tumor necrosis factor alfa |
| FEV1 | Forced expiratory volume in 1 s |
| FIMT | Femoral intima media thickness |
| SABA | Short acting beta agonists |
| SAH | Subarachnoid hemorrhage |
| SAP | Stroke induced pneumonia |
| SCS | Systemic corticosteroids |
| LABA | Long acting beta agonists |
| LAMA | Long acting muscarinic antagonists |
| NOS | Nitric oxide synthase |
| MUC | Mucin gene |
| MMP | Matrix metalloproteinase |
Authors’ contributions
AC, IuS, SC, VB, OC, NS searched analyzed and interpreted the data. All authors were major contributors in writing the manuscript. All authors read and approved the final manuscript.
Availability of data and materials
Ethics approval and consent to participate, consent for publication, competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
A. Corlateanu, Email: moc.oohay@unaetalroc_urdnaxela .
Iu Stratan, Email: moc.liamg@0102anailui .
S. Covantev, Email: [email protected] .
V. Botnaru, Email: moc.oohay@urantob_rotciv .
O. Corlateanu, Email: [email protected] .
N. Siafakas, Email: rg.cou.dem@kafais .
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, generate accurate citations for free.
- Knowledge Base
- How to write a narrative essay | Example & tips
How to Write a Narrative Essay | Example & Tips
Published on July 24, 2020 by Jack Caulfield . Revised on July 23, 2023.
A narrative essay tells a story. In most cases, this is a story about a personal experience you had. This type of essay , along with the descriptive essay , allows you to get personal and creative, unlike most academic writing .
Instantly correct all language mistakes in your text
Upload your document to correct all your mistakes in minutes

Table of contents
What is a narrative essay for, choosing a topic, interactive example of a narrative essay, other interesting articles, frequently asked questions about narrative essays.
When assigned a narrative essay, you might find yourself wondering: Why does my teacher want to hear this story? Topics for narrative essays can range from the important to the trivial. Usually the point is not so much the story itself, but the way you tell it.
A narrative essay is a way of testing your ability to tell a story in a clear and interesting way. You’re expected to think about where your story begins and ends, and how to convey it with eye-catching language and a satisfying pace.
These skills are quite different from those needed for formal academic writing. For instance, in a narrative essay the use of the first person (“I”) is encouraged, as is the use of figurative language, dialogue, and suspense.
Receive feedback on language, structure, and formatting
Professional editors proofread and edit your paper by focusing on:
- Academic style
- Vague sentences
- Style consistency
See an example

Narrative essay assignments vary widely in the amount of direction you’re given about your topic. You may be assigned quite a specific topic or choice of topics to work with.
- Write a story about your first day of school.
- Write a story about your favorite holiday destination.
You may also be given prompts that leave you a much wider choice of topic.
- Write about an experience where you learned something about yourself.
- Write about an achievement you are proud of. What did you accomplish, and how?
In these cases, you might have to think harder to decide what story you want to tell. The best kind of story for a narrative essay is one you can use to talk about a particular theme or lesson, or that takes a surprising turn somewhere along the way.
For example, a trip where everything went according to plan makes for a less interesting story than one where something unexpected happened that you then had to respond to. Choose an experience that might surprise the reader or teach them something.
Narrative essays in college applications
When applying for college , you might be asked to write a narrative essay that expresses something about your personal qualities.
For example, this application prompt from Common App requires you to respond with a narrative essay.
In this context, choose a story that is not only interesting but also expresses the qualities the prompt is looking for—here, resilience and the ability to learn from failure—and frame the story in a way that emphasizes these qualities.
An example of a short narrative essay, responding to the prompt “Write about an experience where you learned something about yourself,” is shown below.
Hover over different parts of the text to see how the structure works.
Since elementary school, I have always favored subjects like science and math over the humanities. My instinct was always to think of these subjects as more solid and serious than classes like English. If there was no right answer, I thought, why bother? But recently I had an experience that taught me my academic interests are more flexible than I had thought: I took my first philosophy class.
Before I entered the classroom, I was skeptical. I waited outside with the other students and wondered what exactly philosophy would involve—I really had no idea. I imagined something pretty abstract: long, stilted conversations pondering the meaning of life. But what I got was something quite different.
A young man in jeans, Mr. Jones—“but you can call me Rob”—was far from the white-haired, buttoned-up old man I had half-expected. And rather than pulling us into pedantic arguments about obscure philosophical points, Rob engaged us on our level. To talk free will, we looked at our own choices. To talk ethics, we looked at dilemmas we had faced ourselves. By the end of class, I’d discovered that questions with no right answer can turn out to be the most interesting ones.
The experience has taught me to look at things a little more “philosophically”—and not just because it was a philosophy class! I learned that if I let go of my preconceptions, I can actually get a lot out of subjects I was previously dismissive of. The class taught me—in more ways than one—to look at things with an open mind.
If you want to know more about AI tools , college essays , or fallacies make sure to check out some of our other articles with explanations and examples or go directly to our tools!
- Ad hominem fallacy
- Post hoc fallacy
- Appeal to authority fallacy
- False cause fallacy
- Sunk cost fallacy
College essays
- Choosing Essay Topic
- Write a College Essay
- Write a Diversity Essay
- College Essay Format & Structure
- Comparing and Contrasting in an Essay
(AI) Tools
- Grammar Checker
- Paraphrasing Tool
- Text Summarizer
- AI Detector
- Plagiarism Checker
- Citation Generator
If you’re not given much guidance on what your narrative essay should be about, consider the context and scope of the assignment. What kind of story is relevant, interesting, and possible to tell within the word count?
The best kind of story for a narrative essay is one you can use to reflect on a particular theme or lesson, or that takes a surprising turn somewhere along the way.
Don’t worry too much if your topic seems unoriginal. The point of a narrative essay is how you tell the story and the point you make with it, not the subject of the story itself.
Narrative essays are usually assigned as writing exercises at high school or in university composition classes. They may also form part of a university application.
When you are prompted to tell a story about your own life or experiences, a narrative essay is usually the right response.
The key difference is that a narrative essay is designed to tell a complete story, while a descriptive essay is meant to convey an intense description of a particular place, object, or concept.
Narrative and descriptive essays both allow you to write more personally and creatively than other kinds of essays , and similar writing skills can apply to both.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the “Cite this Scribbr article” button to automatically add the citation to our free Citation Generator.
Caulfield, J. (2023, July 23). How to Write a Narrative Essay | Example & Tips. Scribbr. Retrieved July 4, 2024, from https://www.scribbr.com/academic-essay/narrative-essay/

Is this article helpful?

Jack Caulfield
Other students also liked, how to write an expository essay, how to write a descriptive essay | example & tips, how to write your personal statement | strategies & examples, what is your plagiarism score.
The Ultimate Narrative Essay Guide for Beginners
A narrative essay tells a story in chronological order, with an introduction that introduces the characters and sets the scene. Then a series of events leads to a climax or turning point, and finally a resolution or reflection on the experience.
Speaking of which, are you in sixes and sevens about narrative essays? Don’t worry this ultimate expert guide will wipe out all your doubts. So let’s get started.
Table of Contents
Everything You Need to Know About Narrative Essay
What is a narrative essay.
When you go through a narrative essay definition, you would know that a narrative essay purpose is to tell a story. It’s all about sharing an experience or event and is different from other types of essays because it’s more focused on how the event made you feel or what you learned from it, rather than just presenting facts or an argument. Let’s explore more details on this interesting write-up and get to know how to write a narrative essay.
Elements of a Narrative Essay
Here’s a breakdown of the key elements of a narrative essay:
A narrative essay has a beginning, middle, and end. It builds up tension and excitement and then wraps things up in a neat package.
Real people, including the writer, often feature in personal narratives. Details of the characters and their thoughts, feelings, and actions can help readers to relate to the tale.
It’s really important to know when and where something happened so we can get a good idea of the context. Going into detail about what it looks like helps the reader to really feel like they’re part of the story.
Conflict or Challenge
A story in a narrative essay usually involves some kind of conflict or challenge that moves the plot along. It could be something inside the character, like a personal battle, or something from outside, like an issue they have to face in the world.
Theme or Message
A narrative essay isn’t just about recounting an event – it’s about showing the impact it had on you and what you took away from it. It’s an opportunity to share your thoughts and feelings about the experience, and how it changed your outlook.
Emotional Impact
The author is trying to make the story they’re telling relatable, engaging, and memorable by using language and storytelling to evoke feelings in whoever’s reading it.
Narrative essays let writers have a blast telling stories about their own lives. It’s an opportunity to share insights and impart wisdom, or just have some fun with the reader. Descriptive language, sensory details, dialogue, and a great narrative voice are all essentials for making the story come alive.
The Purpose of a Narrative Essay
A narrative essay is more than just a story – it’s a way to share a meaningful, engaging, and relatable experience with the reader. Includes:
Sharing Personal Experience
Narrative essays are a great way for writers to share their personal experiences, feelings, thoughts, and reflections. It’s an opportunity to connect with readers and make them feel something.
Entertainment and Engagement
The essay attempts to keep the reader interested by using descriptive language, storytelling elements, and a powerful voice. It attempts to pull them in and make them feel involved by creating suspense, mystery, or an emotional connection.
Conveying a Message or Insight
Narrative essays are more than just a story – they aim to teach you something. They usually have a moral lesson, a new understanding, or a realization about life that the author gained from the experience.
Building Empathy and Understanding
By telling their stories, people can give others insight into different perspectives, feelings, and situations. Sharing these tales can create compassion in the reader and help broaden their knowledge of different life experiences.
Inspiration and Motivation
Stories about personal struggles, successes, and transformations can be really encouraging to people who are going through similar situations. It can provide them with hope and guidance, and let them know that they’re not alone.
Reflecting on Life’s Significance
These essays usually make you think about the importance of certain moments in life or the impact of certain experiences. They make you look deep within yourself and ponder on the things you learned or how you changed because of those events.
Demonstrating Writing Skills
Coming up with a gripping narrative essay takes serious writing chops, like vivid descriptions, powerful language, timing, and organization. It’s an opportunity for writers to show off their story-telling abilities.
Preserving Personal History
Sometimes narrative essays are used to record experiences and special moments that have an emotional resonance. They can be used to preserve individual memories or for future generations to look back on.
Cultural and Societal Exploration
Personal stories can look at cultural or social aspects, giving us an insight into customs, opinions, or social interactions seen through someone’s own experience.
Format of a Narrative Essay
Narrative essays are quite flexible in terms of format, which allows the writer to tell a story in a creative and compelling way. Here’s a quick breakdown of the narrative essay format, along with some examples:
Introduction
Set the scene and introduce the story.
Engage the reader and establish the tone of the narrative.
Hook: Start with a captivating opening line to grab the reader’s attention. For instance:
Example: “The scorching sun beat down on us as we trekked through the desert, our water supply dwindling.”
Background Information: Provide necessary context or background without giving away the entire story.
Example: “It was the summer of 2015 when I embarked on a life-changing journey to…”
Thesis Statement or Narrative Purpose
Present the main idea or the central message of the essay.
Offer a glimpse of what the reader can expect from the narrative.
Thesis Statement: This isn’t as rigid as in other essays but can be a sentence summarizing the essence of the story.
Example: “Little did I know, that seemingly ordinary hike would teach me invaluable lessons about resilience and friendship.”
Body Paragraphs
Present the sequence of events in chronological order.
Develop characters, setting, conflict, and resolution.
Story Progression : Describe events in the order they occurred, focusing on details that evoke emotions and create vivid imagery.
Example : Detail the trek through the desert, the challenges faced, interactions with fellow hikers, and the pivotal moments.
Character Development : Introduce characters and their roles in the story. Show their emotions, thoughts, and actions.
Example : Describe how each character reacted to the dwindling water supply and supported each other through adversity.
Dialogue and Interactions : Use dialogue to bring the story to life and reveal character personalities.
Example : “Sarah handed me her last bottle of water, saying, ‘We’re in this together.'”
Reach the peak of the story, the moment of highest tension or significance.
Turning Point: Highlight the most crucial moment or realization in the narrative.
Example: “As the sun dipped below the horizon and hope seemed lost, a distant sound caught our attention—the rescue team’s helicopters.”
Provide closure to the story.
Reflect on the significance of the experience and its impact.
Reflection : Summarize the key lessons learned or insights gained from the experience.
Example : “That hike taught me the true meaning of resilience and the invaluable support of friendship in challenging times.”
Closing Thought : End with a memorable line that reinforces the narrative’s message or leaves a lasting impression.
Example : “As we boarded the helicopters, I knew this adventure would forever be etched in my heart.”
Example Summary:
Imagine a narrative about surviving a challenging hike through the desert, emphasizing the bonds formed and lessons learned. The narrative essay structure might look like starting with an engaging scene, narrating the hardships faced, showcasing the characters’ resilience, and culminating in a powerful realization about friendship and endurance.
Different Types of Narrative Essays
There are a bunch of different types of narrative essays – each one focuses on different elements of storytelling and has its own purpose. Here’s a breakdown of the narrative essay types and what they mean.
Personal Narrative
Description : Tells a personal story or experience from the writer’s life.
Purpose: Reflects on personal growth, lessons learned, or significant moments.
Example of Narrative Essay Types:
Topic : “The Day I Conquered My Fear of Public Speaking”
Focus: Details the experience, emotions, and eventual triumph over a fear of public speaking during a pivotal event.
Descriptive Narrative
Description : Emphasizes vivid details and sensory imagery.
Purpose : Creates a sensory experience, painting a vivid picture for the reader.
Topic : “A Walk Through the Enchanted Forest”
Focus : Paints a detailed picture of the sights, sounds, smells, and feelings experienced during a walk through a mystical forest.
Autobiographical Narrative
Description: Chronicles significant events or moments from the writer’s life.
Purpose: Provides insights into the writer’s life, experiences, and growth.
Topic: “Lessons from My Childhood: How My Grandmother Shaped Who I Am”
Focus: Explores pivotal moments and lessons learned from interactions with a significant family member.
Experiential Narrative
Description: Relays experiences beyond the writer’s personal life.
Purpose: Shares experiences, travels, or events from a broader perspective.
Topic: “Volunteering in a Remote Village: A Journey of Empathy”
Focus: Chronicles the writer’s volunteering experience, highlighting interactions with a community and personal growth.
Literary Narrative
Description: Incorporates literary elements like symbolism, allegory, or thematic explorations.
Purpose: Uses storytelling for deeper explorations of themes or concepts.
Topic: “The Symbolism of the Red Door: A Journey Through Change”
Focus: Uses a red door as a symbol, exploring its significance in the narrator’s life and the theme of transition.
Historical Narrative
Description: Recounts historical events or periods through a personal lens.
Purpose: Presents history through personal experiences or perspectives.
Topic: “A Grandfather’s Tales: Living Through the Great Depression”
Focus: Shares personal stories from a family member who lived through a historical era, offering insights into that period.
Digital or Multimedia Narrative
Description: Incorporates multimedia elements like images, videos, or audio to tell a story.
Purpose: Explores storytelling through various digital platforms or formats.
Topic: “A Travel Diary: Exploring Europe Through Vlogs”
Focus: Combines video clips, photos, and personal narration to document a travel experience.
How to Choose a Topic for Your Narrative Essay?
Selecting a compelling topic for your narrative essay is crucial as it sets the stage for your storytelling. Choosing a boring topic is one of the narrative essay mistakes to avoid . Here’s a detailed guide on how to choose the right topic:
Reflect on Personal Experiences
- Significant Moments:
Moments that had a profound impact on your life or shaped your perspective.
Example: A moment of triumph, overcoming a fear, a life-changing decision, or an unforgettable experience.
- Emotional Resonance:
Events that evoke strong emotions or feelings.
Example: Joy, fear, sadness, excitement, or moments of realization.
- Lessons Learned:
Experiences that taught you valuable lessons or brought about personal growth.
Example: Challenges that led to personal development, shifts in mindset, or newfound insights.
Explore Unique Perspectives
- Uncommon Experiences:
Unique or unconventional experiences that might captivate the reader’s interest.
Example: Unusual travels, interactions with different cultures, or uncommon hobbies.
- Different Points of View:
Stories from others’ perspectives that impacted you deeply.
Example: A family member’s story, a friend’s experience, or a historical event from a personal lens.
Focus on Specific Themes or Concepts
- Themes or Concepts of Interest:
Themes or ideas you want to explore through storytelling.
Example: Friendship, resilience, identity, cultural diversity, or personal transformation.
- Symbolism or Metaphor:
Using symbols or metaphors as the core of your narrative.
Example: Exploring the symbolism of an object or a place in relation to a broader theme.
Consider Your Audience and Purpose
- Relevance to Your Audience:
Topics that resonate with your audience’s interests or experiences.
Example: Choose a relatable theme or experience that your readers might connect with emotionally.
- Impact or Message:
What message or insight do you want to convey through your story?
Example: Choose a topic that aligns with the message or lesson you aim to impart to your readers.
Brainstorm and Evaluate Ideas
- Free Writing or Mind Mapping:
Process: Write down all potential ideas without filtering. Mind maps or free-writing exercises can help generate diverse ideas.
- Evaluate Feasibility:
The depth of the story, the availability of vivid details, and your personal connection to the topic.
Imagine you’re considering topics for a narrative essay. You reflect on your experiences and decide to explore the topic of “Overcoming Stage Fright: How a School Play Changed My Perspective.” This topic resonates because it involves a significant challenge you faced and the personal growth it brought about.
Narrative Essay Topics
50 easy narrative essay topics.
- Learning to Ride a Bike
- My First Day of School
- A Surprise Birthday Party
- The Day I Got Lost
- Visiting a Haunted House
- An Encounter with a Wild Animal
- My Favorite Childhood Toy
- The Best Vacation I Ever Had
- An Unforgettable Family Gathering
- Conquering a Fear of Heights
- A Special Gift I Received
- Moving to a New City
- The Most Memorable Meal
- Getting Caught in a Rainstorm
- An Act of Kindness I Witnessed
- The First Time I Cooked a Meal
- My Experience with a New Hobby
- The Day I Met My Best Friend
- A Hike in the Mountains
- Learning a New Language
- An Embarrassing Moment
- Dealing with a Bully
- My First Job Interview
- A Sporting Event I Attended
- The Scariest Dream I Had
- Helping a Stranger
- The Joy of Achieving a Goal
- A Road Trip Adventure
- Overcoming a Personal Challenge
- The Significance of a Family Tradition
- An Unusual Pet I Owned
- A Misunderstanding with a Friend
- Exploring an Abandoned Building
- My Favorite Book and Why
- The Impact of a Role Model
- A Cultural Celebration I Participated In
- A Valuable Lesson from a Teacher
- A Trip to the Zoo
- An Unplanned Adventure
- Volunteering Experience
- A Moment of Forgiveness
- A Decision I Regretted
- A Special Talent I Have
- The Importance of Family Traditions
- The Thrill of Performing on Stage
- A Moment of Sudden Inspiration
- The Meaning of Home
- Learning to Play a Musical Instrument
- A Childhood Memory at the Park
- Witnessing a Beautiful Sunset
Narrative Essay Topics for College Students
- Discovering a New Passion
- Overcoming Academic Challenges
- Navigating Cultural Differences
- Embracing Independence: Moving Away from Home
- Exploring Career Aspirations
- Coping with Stress in College
- The Impact of a Mentor in My Life
- Balancing Work and Studies
- Facing a Fear of Public Speaking
- Exploring a Semester Abroad
- The Evolution of My Study Habits
- Volunteering Experience That Changed My Perspective
- The Role of Technology in Education
- Finding Balance: Social Life vs. Academics
- Learning a New Skill Outside the Classroom
- Reflecting on Freshman Year Challenges
- The Joys and Struggles of Group Projects
- My Experience with Internship or Work Placement
- Challenges of Time Management in College
- Redefining Success Beyond Grades
- The Influence of Literature on My Thinking
- The Impact of Social Media on College Life
- Overcoming Procrastination
- Lessons from a Leadership Role
- Exploring Diversity on Campus
- Exploring Passion for Environmental Conservation
- An Eye-Opening Course That Changed My Perspective
- Living with Roommates: Challenges and Lessons
- The Significance of Extracurricular Activities
- The Influence of a Professor on My Academic Journey
- Discussing Mental Health in College
- The Evolution of My Career Goals
- Confronting Personal Biases Through Education
- The Experience of Attending a Conference or Symposium
- Challenges Faced by Non-Native English Speakers in College
- The Impact of Traveling During Breaks
- Exploring Identity: Cultural or Personal
- The Impact of Music or Art on My Life
- Addressing Diversity in the Classroom
- Exploring Entrepreneurial Ambitions
- My Experience with Research Projects
- Overcoming Impostor Syndrome in College
- The Importance of Networking in College
- Finding Resilience During Tough Times
- The Impact of Global Issues on Local Perspectives
- The Influence of Family Expectations on Education
- Lessons from a Part-Time Job
- Exploring the College Sports Culture
- The Role of Technology in Modern Education
- The Journey of Self-Discovery Through Education
Narrative Essay Comparison
Narrative essay vs. descriptive essay.
Here’s our first narrative essay comparison! While both narrative and descriptive essays focus on vividly portraying a subject or an event, they differ in their primary objectives and approaches. Now, let’s delve into the nuances of comparison on narrative essays.
Narrative Essay:
Storytelling: Focuses on narrating a personal experience or event.
Chronological Order: Follows a structured timeline of events to tell a story.
Message or Lesson: Often includes a central message, moral, or lesson learned from the experience.
Engagement: Aims to captivate the reader through a compelling storyline and character development.
First-Person Perspective: Typically narrated from the writer’s point of view, using “I” and expressing personal emotions and thoughts.
Plot Development: Emphasizes a plot with a beginning, middle, climax, and resolution.
Character Development: Focuses on describing characters, their interactions, emotions, and growth.
Conflict or Challenge: Usually involves a central conflict or challenge that drives the narrative forward.
Dialogue: Incorporates conversations to bring characters and their interactions to life.
Reflection: Concludes with reflection or insight gained from the experience.
Descriptive Essay:
Vivid Description: Aims to vividly depict a person, place, object, or event.
Imagery and Details: Focuses on sensory details to create a vivid image in the reader’s mind.
Emotion through Description: Uses descriptive language to evoke emotions and engage the reader’s senses.
Painting a Picture: Creates a sensory-rich description allowing the reader to visualize the subject.
Imagery and Sensory Details: Focuses on providing rich sensory descriptions, using vivid language and adjectives.
Point of Focus: Concentrates on describing a specific subject or scene in detail.
Spatial Organization: Often employs spatial organization to describe from one area or aspect to another.
Objective Observations: Typically avoids the use of personal opinions or emotions; instead, the focus remains on providing a detailed and objective description.
Comparison:
Focus: Narrative essays emphasize storytelling, while descriptive essays focus on vividly describing a subject or scene.
Perspective: Narrative essays are often written from a first-person perspective, while descriptive essays may use a more objective viewpoint.
Purpose: Narrative essays aim to convey a message or lesson through a story, while descriptive essays aim to paint a detailed picture for the reader without necessarily conveying a specific message.
Narrative Essay vs. Argumentative Essay
The narrative essay and the argumentative essay serve distinct purposes and employ different approaches:
Engagement and Emotion: Aims to captivate the reader through a compelling story.
Reflective: Often includes reflection on the significance of the experience or lessons learned.
First-Person Perspective: Typically narrated from the writer’s point of view, sharing personal emotions and thoughts.
Plot Development: Emphasizes a storyline with a beginning, middle, climax, and resolution.
Message or Lesson: Conveys a central message, moral, or insight derived from the experience.
Argumentative Essay:
Persuasion and Argumentation: Aims to persuade the reader to adopt the writer’s viewpoint on a specific topic.
Logical Reasoning: Presents evidence, facts, and reasoning to support a particular argument or stance.
Debate and Counterarguments: Acknowledge opposing views and counter them with evidence and reasoning.
Thesis Statement: Includes a clear thesis statement that outlines the writer’s position on the topic.
Thesis and Evidence: Starts with a strong thesis statement and supports it with factual evidence, statistics, expert opinions, or logical reasoning.
Counterarguments: Addresses opposing viewpoints and provides rebuttals with evidence.
Logical Structure: Follows a logical structure with an introduction, body paragraphs presenting arguments and evidence, and a conclusion reaffirming the thesis.
Formal Language: Uses formal language and avoids personal anecdotes or emotional appeals.
Objective: Argumentative essays focus on presenting a logical argument supported by evidence, while narrative essays prioritize storytelling and personal reflection.
Purpose: Argumentative essays aim to persuade and convince the reader of a particular viewpoint, while narrative essays aim to engage, entertain, and share personal experiences.
Structure: Narrative essays follow a storytelling structure with character development and plot, while argumentative essays follow a more formal, structured approach with logical arguments and evidence.
In essence, while both essays involve writing and presenting information, the narrative essay focuses on sharing a personal experience, whereas the argumentative essay aims to persuade the audience by presenting a well-supported argument.
Narrative Essay vs. Personal Essay
While there can be an overlap between narrative and personal essays, they have distinctive characteristics:
Storytelling: Emphasizes recounting a specific experience or event in a structured narrative form.
Engagement through Story: Aims to engage the reader through a compelling story with characters, plot, and a central theme or message.
Reflective: Often includes reflection on the significance of the experience and the lessons learned.
First-Person Perspective: Typically narrated from the writer’s viewpoint, expressing personal emotions and thoughts.
Plot Development: Focuses on developing a storyline with a clear beginning, middle, climax, and resolution.
Character Development: Includes descriptions of characters, their interactions, emotions, and growth.
Central Message: Conveys a central message, moral, or insight derived from the experience.
Personal Essay:
Exploration of Ideas or Themes: Explores personal ideas, opinions, or reflections on a particular topic or subject.
Expression of Thoughts and Opinions: Expresses the writer’s thoughts, feelings, and perspectives on a specific subject matter.
Reflection and Introspection: Often involves self-reflection and introspection on personal experiences, beliefs, or values.
Varied Structure and Content: Can encompass various forms, including memoirs, personal anecdotes, or reflections on life experiences.
Flexibility in Structure: Allows for diverse structures and forms based on the writer’s intent, which could be narrative-like or more reflective.
Theme-Centric Writing: Focuses on exploring a central theme or idea, with personal anecdotes or experiences supporting and illustrating the theme.
Expressive Language: Utilizes descriptive and expressive language to convey personal perspectives, emotions, and opinions.
Focus: Narrative essays primarily focus on storytelling through a structured narrative, while personal essays encompass a broader range of personal expression, which can include storytelling but isn’t limited to it.
Structure: Narrative essays have a more structured plot development with characters and a clear sequence of events, while personal essays might adopt various structures, focusing more on personal reflection, ideas, or themes.
Intent: While both involve personal experiences, narrative essays emphasize telling a story with a message or lesson learned, while personal essays aim to explore personal thoughts, feelings, or opinions on a broader range of topics or themes.
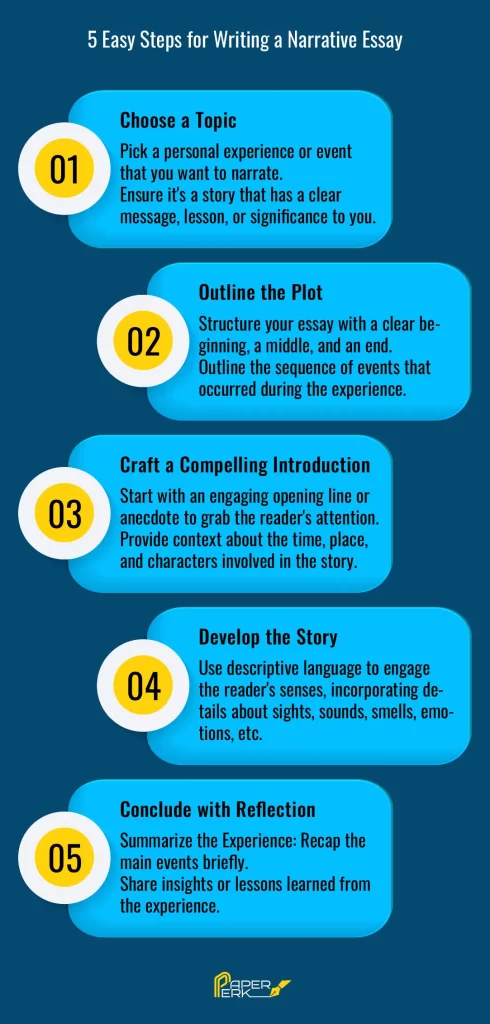
A narrative essay is more than just telling a story. It’s also meant to engage the reader, get them thinking, and leave a lasting impact. Whether it’s to amuse, motivate, teach, or reflect, these essays are a great way to communicate with your audience. This interesting narrative essay guide was all about letting you understand the narrative essay, its importance, and how can you write one.
Order Original Papers & Essays
Your First Custom Paper Sample is on Us!
Timely Deliveries
No Plagiarism & AI
100% Refund
Try Our Free Paper Writing Service
Related blogs.

Connections with Writers and support
Privacy and Confidentiality Guarantee
Average Quality Score

Narrative Essay
Ai generator.
A narrative essay is a form of storytelling where the writer shares a personal experience in a detailed and engaging manner. Crafting a Short Narrative Essay allows the author to focus on a specific event or moment, making it concise and impactful. Writing a Beneficial Narrative Essay helps readers connect with the author’s journey, providing insight and reflection. The Thesis Statement for Narrative Essay serves as the guiding idea, encapsulating the main point or lesson learned. A well-crafted Narrative Summary ensures the story is coherent and compelling, leaving a lasting impression on the audience.
What is Narrative Essay?
A narrative essay is a form of writing that tells a story from the writer’s personal experience, using vivid details and a clear sequence of events. It aims to engage readers by making them feel a part of the journey, often imparting a meaningful lesson or insight.
Examples of Narrative Essay
- A Memorable Family Vacation – Recount a family trip that left a lasting impression.
- My First Day at School – Describe the emotions and experiences of your first school day.
- An Unexpected Adventure – Share a surprising and exciting experience you had.
- Overcoming a Fear – Narrate the story of how you faced and conquered a fear.
- A Life-Changing Event – Detail an event that significantly impacted your life.
- A Lesson Learned the Hard Way – Explain a situation where you learned an important lesson through a challenging experience.
- My Favorite Childhood Memory – Describe a cherished memory from your childhood.
- A Time I Helped Someone – Share a story where you helped someone in need and what you learned from it.
- A Day I Will Never Forget – Narrate a day that stands out vividly in your memory.
- My First Job Experience – Recount your experiences and lessons learned from your first job.
- The Best Decision I Ever Made – Explain a decision that positively changed your life.
- A Time I Stood Up for Myself – Describe an instance where you confidently defended your beliefs or actions.
- A Significant Challenge I Faced – Narrate how you dealt with a major challenge in your life.
- My Favorite Holiday Celebration – Share your experiences and traditions during a special holiday.
- A Friendship That Changed Me – Describe a friendship that had a profound impact on you.
- A Moment of Personal Growth – Explain a situation where you experienced significant personal development.
- A Funny Incident from My Life – Recount a humorous event that still makes you laugh.
- A Time I Felt Truly Happy – Describe an experience that brought you immense joy and fulfillment.
- My Experience Moving to a New Place – Share your feelings and experiences about relocating to a new environment.
- A Mistake That Taught Me a Valuable Lesson – Narrate a mistake you made and the lessons you learned from it.
Narrative Essay Examples for Students
- My First Day at High School : My first day at high school was a mix of excitement and nervousness. Walking through the crowded halls, I felt lost but eager to start a new chapter.
- Overcoming Stage Fright : In eighth grade, I was chosen to lead the school play. Though terrified, I practiced tirelessly and eventually overcame my stage fright.
- A Memorable Family Vacation : Last summer, my family and I went on a trip to the Grand Canyon. The breathtaking views and the bonding moments we shared made it an unforgettable experience.
- The Day I Got My First Pet : Getting my first pet, a golden retriever named Max, was a day filled with joy. I vividly remember the feeling of holding him for the first time and the instant bond we formed.
- Learning to Ride a Bike : Learning to ride a bike was a significant milestone in my childhood. My dad spent countless hours running beside me, encouraging me not to give up.
Narrative Essay Topics
- A Life-Changing Experience
- My First Day at a New School
- An Unforgettable Family Reunion
- The Day I Overcame a Fear
- A Time I Got Lost
- The Best Birthday Party Ever
- A Lesson Learned from a Mistake
- The Moment I Realized I Was Growing Up
- A Memorable Road Trip
- An Unexpected Act of Kindness
- A Funny Incident in My Life
- A Time I Stood Up for Myself
- A Significant Challenge I Faced
- My First Job Experience
- A Time When I Felt Truly Happy
- A Difficult Decision I Had to Make
- The Day I Met My Best Friend
- An Adventure in Nature
- A Family Tradition That Means a Lot to Me
- The First Time I Tried Something New
Narrative Essay Format
Introduction.
From a young age, I was terrified of public speaking. The very thought of standing in front of an audience made my palms sweat and my heart race. However, my journey to overcome this fear taught me valuable lessons about courage and perseverance.
In eighth grade, I was unexpectedly chosen to play the lead role in our school play. At first, I wanted to decline the offer, but my teacher encouraged me to step out of my comfort zone. With her support and my parents’ encouragement, I reluctantly agreed.
As the day of the performance approached, my nerves intensified. However, I remembered my teacher’s advice: “Focus on the story you’re telling, not on the audience.” On the night of the play, I took a deep breath and stepped onto the stage, my heart pounding in my chest.
To my surprise, as I delivered my first lines, the fear began to fade. I became immersed in my character, and the audience’s presence seemed to disappear. By the end of the play, I felt a sense of accomplishment and pride that I had never experienced before.
Overcoming my stage fright was a pivotal moment in my life. It taught me that facing my fears head-on and persevering through challenges can lead to personal growth and unexpected rewards.
How to write Narrative Essay
Choose a Topic : Pick a story or experience from your life that you can describe in detail and that has a clear point or lesson.
Create an Outline : Outline the main events of your story in the order they happened. This will help you organize your thoughts and ensure your essay flows smoothly.
Write the Introduction:
- Hook : Start with an interesting opening sentence to grab the reader’s attention.
- Setting the Scene : Provide background information about where and when the story takes place.
- Thesis Statement : Briefly explain the main point or lesson of your story.
Write the Body Paragraphs :
- Paragraph 1: Beginning of the Story
- Paragraph 2: Rising Action
- Paragraph 3: Climax
- Paragraph 4: Falling Action
- Write the Conclusion : Summarize the lesson or main point of your story.
Tips for Narrative Essay Writing
- Start with a Strong Hook
- Use Vivid Descriptions and Sensory Details
- Show, Don’t Just Tell
- Reflect on the Significance
How does a narrative essay differ from a biography?
Unlike a Biography Narrative Essay , a narrative essay focuses on a specific event or experience.
Can a narrative essay include fictional elements?
Yes, a narrative essay can blend fact and fiction for creative storytelling.
What is a narrative history essay?
A narrative history essay recounts historical events in a story-like format.
How do you start a narrative essay?
Begin with an engaging hook, setting the scene or introducing key characters.
What are the key components of a narrative essay?
Introduction, plot, characters, climax, and conclusion are essential.
How should a narrative essay be structured?
Follow a chronological order or a logical progression of events.
What tone should a narrative essay have?
The tone can vary but should suit the story’s context and audience.
How do you end a narrative essay?
Conclude by reflecting on the story’s significance or lessons learned.
How important is the setting in a narrative essay?
A well-described setting enhances the story’s mood and context.
What is the purpose of a narrative essay?
To entertain, inform, or convey personal experiences and insights.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting

IMAGES
VIDEO
COMMENTS
Narrative Essay On Asthma. Decent Essays. 721 Words. 3 Pages. Open Document. I have always generally known, who I am, however one day I began questioning it all. For as long as I can recall, I have been very active as well as healthy. As a child, I was involved in every sport there was. Then once I reached high school this all was ripped away ...
3 pages / 1303 words. Introduction Asthma is among the life-threatening medical complications that require emergency acute nursing care. Cockcroft (2018, pp. 12-18) categorizes causes of asthma as allergic and non-allergic. Irritants such as dust, smoke, airborne substances, and pollen are allergic causes while non-allergic causes include the ...
A Comprehensive Exploration of Asthma. Asthma is a chronic lung disease marked by chest tightness, wheezing, breathlessness, and coughing (Dodge & Burrows, 2018). In the United States alone, there are 19 million adults and 6.2 million children living with asthma (Centers for Disease Control and Prevention, 2018).
Asthma is the leading cause of chronic illness in children and is responsible for nearly 10% of the Emergency Room visits for children <15 year of age. It occurs in as many as 10%-12% of children in the United States and is gradually growing. Asthma can begin at any age , but most children have their first symptoms by age five.
Narrative Essay On Asthma; Narrative Essay On Asthma. Decent Essays. 455 Words; 2 Pages; Open Document. Instead of being confined with asthma I would usually spend my days outside and fight. I told myself that asthmatics are stronger because we know what it feels like to not have air, to stare at the sky and wait for our air ducts to open, to ...
Personal Narrative: How Asthma Changed My Life. In life there's always that one moment which changes your perspective on everything. Some may not notice at first, however, in my case it was handed to me on a silver platter. It all started when I was in the sixth grade.
Narrative Essay On Compare And Contrast Basketball And Simeon 2306 Words | 10 Pages. I had asthma when I was a baby but it had went away. He told me I should go to the doctor and take a test to see if I have asthma . I went to the doctor and they told me that my asthma had came back and gave prescription to get my asthma pumps.
A diagnosis of asthma in both children and adults is based on assessment of symptoms. The classic signs of asthma are wheezing (especially expiratory wheezing), breathlessness, coughing (typically in the early morning or at night time) and chest tightness. Children and adults with a high probability of asthma on assessment usually start a ...
Methods. Narrative review of papers available until February 2021 in PubMed and Google Scholar, relating severe asthma and COVID-19. Four main research topics were reviewed: SARS-CoV-2 infection: immunology and respiratory pathology; interrelationship of severe asthma endotypes and COVID-19 disease mechanisms; severe asthma epidemiology and COVID-19; and biologics for severe asthma in the ...
Pathophysiology of Asthma - Essay. Asthma is a chronic lung disease characterized by episodes in which the bronchioles constrict due to oversensitivity. In asthma, the airways (bronchioles) constrict making it difficult to get air in or out of the lungs. Breathlessness is the main symptom.
Asthma is a chronic respiratory disease that impacts millions of people worldwide. Recent studies suggest that diet may play a role in asthma pathophysiology. Several dietary factors have been recognized as potential contributors to the development and severity of asthma for its inflammatory and oxidative effects. Some food groups such as fruits and vegetables, whole grains, and healthy fats ...
Narrative Essay On Asthma. 455 Words; 2 Pages; Narrative Essay On Asthma. Instead of being confined with asthma I would usually spend my days outside and fight. I told myself that asthmatics are stronger because we know what it feels like to not have air, to stare at the sky and wait for our air ducts to open, to be aware that we are still ...
narrative.essay.docx - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. The student had their first asthma attack while sprinting against a friend on their birthday. During the race at a local stadium, the student started experiencing difficulty breathing, coughing, and wheezing after winning.
Asthma is a prevalent chronic inflammatory respiratory condition affecting millions of people worldwide and presents substantial challenges in both diagnosis and management. This respiratory condition is characterized by inflammation of the airways, causing intermittent airflow obstruction and bronchial hyperresponsiveness. The hallmark asthma symptoms include coughing, wheezing, and shortness ...
The nationwide study on Asian population revealed that patients with asthma were 1.38 fold more likely to develop ischemic stroke (95% CI = 1.27-1.49) and were 1.31 fold more likely to develop hemorrhagic stroke (95% CI = 1.09-1.65) than were the non-asthmatic controls after adjusting for age, sex, and comorbidities.
Personal Narrative: Asthma Attacks. 477 Words2 Pages. All of a sudden my lungs began to tighten and my legs started to shake. I stop to catch my breath but couldn't; at that moment I knew I was having an asthma attack. This event happened on a warm sunny day in 6th grade, at Pronghorn elementary school. On that day I learned many lessons, but ...
associated with asthma. 2. Asthma Phenotypes and Endotypes Asthma is defined as "( . . . ) a heterogeneous disease, usually characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness and cough that vary over time and in intensity, to-
Asthma Narrative Essay Be of good courage, and he shall strengthen your heart, all ye that hope in the Lord. Psalm 31:24 On the evening of July 6, 2016, I began to have what I thought was an asthma attack. My breathing was shallow and labored, so I knew I needed to use my inhaler, which usually alleviated any symptoms I was having.
Asthma Narrative Essay; Asthma Narrative Essay. Decent Essays. 468 Words; 2 Pages; Open Document. Be of good courage, and he shall strengthen your heart, all ye that hope in the Lord. Psalm 31:24 On the evening of July 6, 2016, I began to have what I thought was an asthma attack. My breathing was shallow and labored, so I knew I needed to use ...
Interactive example of a narrative essay. An example of a short narrative essay, responding to the prompt "Write about an experience where you learned something about yourself," is shown below. Hover over different parts of the text to see how the structure works. Narrative essay example.
Purpose: Reach the peak of the story, the moment of highest tension or significance. Elements: Turning Point: Highlight the most crucial moment or realization in the narrative. Example: "As the sun dipped below the horizon and hope seemed lost, a distant sound caught our attention—the rescue team's helicopters.".
Essay on The Impact of Asthma on the Patient Throughout the years knowledge about asthma has grown, as well as treating it effectively. Over 300 million people are said to be victims of this disease with another 100 million being estimated by 2025 globally (Currie and Baker, 2012).
A narrative essay is a form of storytelling where the writer shares a personal experience in a detailed and engaging manner. Crafting a Short Narrative Essay allows the author to focus on a specific event or moment, making it concise and impactful. Writing a Beneficial Narrative Essay helps readers connect with the author's journey, providing insight and reflection.