Foundations of Clinical Research
This Harvard Medical School six-month, application-based certificate program provides the essential skill sets and fundamental knowledge required to begin or expand your clinical research career.


Associated Schools

Harvard Medical School
What you'll learn.
Understand and apply the foundational concepts of biostatistics and epidemiology
Develop a research question and formulate a testable hypothesis
Design and begin to implement a clinical research study
Cultivate the skills required to present a clinical research study
Critically evaluate the research findings in medical literature
Synthesize crucial statistical analyses using Stata software
Course description
The Foundations of Clinical Research program is rooted in the belief that clinical research training is critical to professional development in health care. Clinical research training not only creates potential independent investigators, but also enables clinicians to advance their careers through a greater understanding of research evidence. Designed to provide learners with the foundational knowledge and skill sets required to produce high-quality clinical research, our program will lay the fundamental groundwork in epidemiology and biostatistics required for a multifaceted career in clinical research.
The overarching goal of the Foundations of Clinical Research program is to equip the next generation of researchers with the skill sets essential to evaluating evidence, understanding biostatistics, and beginning their clinical research careers. Our aim is to ensure that learners develop a strong foundation in the design, implementation, analysis and interpretation of clinical research studies.
During the program, our innovative active learning approach emphasizes the traditional tutorial system with weekly live video tutorials, seminars and symposia anchored by 3 live intense weekend online workshops. The Foundations of Clinical Research program’s six-month online curriculum emphasizes real-time skill-based learning.
Participants will be eligible for Associate Alumni status upon successful completion of the program. Early tuition and need-based tuition reductions may be available.
Course Outline
Live Workshops
The interactive workshop curriculum will focus on hands-on skill development through active learning. To that end, the intensive schedule is designed to accelerate the growth of high-yield clinical research skills via individual and team-based workshop exercises. Students will be immersed in a dynamic learning environment that encourages collaboration and collegial networking with faculty and peers.
Essential elements of the workshop include instruction and practical exercises in the core concepts of biostatistics, epidemiology and research question development, as well as critical assessment of the medical literature and practical training in statistical software using real-life datasets. In addition to providing training in mentorship, academic career development and leadership, we create a supportive and active learning environment where opportunities for knowledge retention and networking abound.
Live Symposia, Tutorials and Seminars
Symposia, tutorials and seminars are mandatory and will be delivered live online and organized according to eight specific clinical research topics.
Eight 3-Hour Symposia
- Instruction on a specific clinical research topic (e.g., cohort study design and interpretation)
- In-depth discussion on a related epidemiology concept (e.g., odds ratio)
- Hands-on guidance for implementing the related analysis with statistical programming in Stata
Eight 1-Hour Tutorials
- Interpret and report on papers related to the specific clinical research topic
Eight 1-Hour Special-Topic Seminars
- The biostatistical and epidemiological concepts to specific clinical research topics with concrete examples
Assignments
All students will be expected to complete all assignments by the due dates. Assignments will be graded as either “pass” or “fail.”
Individual Assignment 1
Individual Research Question and Study Design
- Generate a novel research question in the evidence-based PICO format
- Receive expert faculty review
Individual Assignment 2
Design, Implement and Present an Original Abstract
- Design and implement a clinical research study based on a publicly available dataset
- Analyze and create data visualizations via a user-friendly R Shiny web app
- Write a formal 350-word abstract suitable for submission to an international conference
- Present a digital poster to faculty at Workshop 3
Online Lectures
Research Study Introduction
- Designing a Clinical Research Study I–III
- Introduction to Evidence-Based Medicine, Systematic Review and Meta-Analysis
- Study Design 1 – Observational
- Study Design 2 – Randomized Controlled Trials
- Study Design 3 – Quasi-Experimental Studies
- Introduction to Biostatistics
- An Investigator’s Responsibility for Protection of Research Subjects
- How to Search PubMed
- Overview of Evidence-Based Medicine
Statistical Programming in Stata
- Loading Data
- Basic Programming Commands
- Data Cleansing
- Data Analytics I – Central Tendency
- Data Analytics II – Statistical Testing
- Data Analytics III – Regression Testing
Instructors

Jamie Robertson

Djøra Soeteman
You may also like.

Global Clinical Scholars Research Training
This Harvard Medical School one-year, application-based certificate program provides advanced training in health care research and methods.

Clinical Drug Development
Learning about the process of clinical drug development has important implications for anyone working in health care and related sectors.
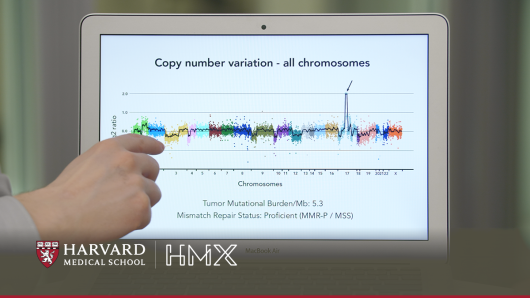
Cancer Genomics and Precision Oncology
Learn how cancer treatment is evolving due to advances in genetics., join our list to learn more.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- BMC Med Educ
- PMC10605271

Developing research skills in medical students online using an active research study
Aziz u. r. asghar.
1 Centre for Anatomical and Human Sciences, Hull York Medical School, University of Hull, Hull, HU6 7RX UK
2 Experimental Medicine and Biomedicine, Hull York Medical School, University of Hull, Hull, HU6 7RX UK
3 York Biomedical Research Institute, University of York, York, YO10 5DD UK
Murat Aksoy
Alison i. graham.
4 Health Professions Education Unit, Hull York Medical School, University of York, York, YO10 5DD UK
Heidi A. Baseler
5 Department of Psychology, University of York, York, YO10 5DD UK
Associated Data
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Developing research skills and scholarship are key components of medical education. The COVID-19 pandemic necessitated that all teaching be delivered online. We introduced an approach to small group teaching in the academic year 2020–2021 online which involved students in an active (ongoing) research study to develop their research skills.
We acquired student feedback to evaluate their perspectives quantitatively on development of research and scholarship skills, teaching content and format, and tutor performance using this teaching approach. In addition, we captured free text responses from both students and tutors on the positives and negatives of our course, and their suggested improvements. We also compared summative assessment marks for the online/active research course (2020–2021) with those obtained from previous (2017–2019) and subsequent (2021–2023) teaching sessions.
Students were largely positive about most aspects of the online course utilising an active research study ( n = 13). Students agreed that they were able to acquire research skills, particularly related to data analysis, transferable skills, and giving scientific presentations. A one-way ANOVA revealed no significant difference for assessment marks across all five teaching years (two years prior and two years following the online/active research course), indicating that the course achieved the learning outcomes. Students enjoyed the convenience of online teaching and the availability of course resources, but least liked the lack of in-person interaction and laboratory training. Tutors enjoyed the collaborative aspects of online teaching, but least liked the lack of face-to-face interactions with students.
Conclusions
Our study demonstrates that delivering online teaching which involves students in active research engages and motivates them to develop their research and scholarship skills. We recommend that educators consider incorporating a current research study in their undergraduate courses as this can enhance the student learning experience as well as the research project itself.
The General Medical Council in the United Kingdom requires that medical students achieve ‘ Professional Knowledge’ learning outcomes related to ‘Clinical research and scholarship’ [ 1 ]. The outcomes stipulate that ‘… newly qualified doctors must be able to apply scientific method and approaches to medical research and integrate these with a range of sources of information used to make decisions for care. ’ Specifically, they must be able to: ‘ Interpret and communicate research evidence in a meaningful way … ’; ‘ Describe the role and value of … quantitative methodological approaches to scientific enquiry ’; ‘ Interpret common statistical tests used in medical research … ’; ‘ Critically appraise a range of research information … as reported in the medical and scientific literature ’; and ‘ Describe basic principles and ethical implications of research governance … ’. One way the Hull York Medical School addresses this requirement is via its compulsory Scholarship and Special Interest Programme (SSIP), equivalent to the Student-Selected Component (SSC) in other medical schools in the United Kingdom.
Evidence for how best to teach research methods to undergraduate medicine students is limited, although there have been attempts to review best practice in this area [ 2 ]. Training in research skills can be integrated into the main curriculum and/or be available through extra-curricular components [ 3 ]. Transferrable research skills such as critical thinking and problem solving can be integrated into the main curriculum relatively easily. However, given the time and resource requirements needed for more authentic research experiences (for example, extended research projects), it may not be possible to offer these to all students. Laidlaw and colleagues suggest that student-selected components are a key space within the medical curriculum in which research skills can be developed [ 3 ].
The SSIP allows all undergraduate medical students to develop their academic research and scholarship skills and is led by tutors who are researchers and experts in their fields. Students select and study a specific area of interest in depth within fields including neuroscience, immunology, pharmacology, nutrition, cancer, psychiatry, palliative care, public health, and health inequalities. At the Hull York Medical School, all students undertake an SSIP module in both years of Phase I (Years 1 and 2) and once in Phase II (Years 3 and 4). The SSIP discussed in this paper was aimed at Year 1 students. SSIP teaching sits alongside prescribed parts of the curriculum which includes lectures, small-group tutorials using problem-based learning, clinical skills, and placements.
The Hull York Medical School is a five-year undergraduate medical programme with an annual intake of ~ 250 students per year. The academic year is divided into three terms. As part of the current SSIP in Term 1, Year 1 students undertake a series of whole-cohort sessions on a variety of general research-related skills which provides a grounding for the discipline-specific SSIP content in Terms 2 and 3. During Term 1, they also submit their preferences from the module choices available. Students are then allocated to one of their preferred modules which they study in Terms 2 and 3. The format of individual modules can vary but must meet the following learning outcomes: 1) introduce all students to the scientific method and different approaches to research; 2) provide the opportunity for students to develop as a scholar, scientist and practitioner; 3) promote the skills and attitudes required for in-depth study; 4) promote skills relevant to the doctor as a professional, including pedagogical skills.
For medical students in Year 1, the content of the current SSIP (from 2019 onwards) in Terms 2 and 3 is delivered to groups of students by staff based within academic research centres in the Hull York Medical School. Term 2 SSIP consists of six hours of teaching which takes place over eight consecutive weeks. Term 3 SSIP consists of six hours of teaching over nine consecutive working days. Students are expected to spend 100 h on the SSIP in total, and non-timetabled time is used for self-directed learning. Prior to the COVID-19 pandemic, the SSIP modules in neuroscience consisted of small group teaching delivered in person and included laboratory-based practical sessions. Laboratory practical sessions have been demonstrated to play a vital role in science education [ 4 – 6 ]. The purpose of our in-person laboratory sessions was to provide students with hands-on experience of neuroscience techniques with the aim of enhancing their understanding of neuroscientific concepts. Tutors acted as expert instructors, consultants to whom students could ask questions, and facilitated group interactions [ 7 , 8 ].
The COVID-19 pandemic necessitated the rapid move to an online teaching format in higher education institutions, a particular challenge for laboratory-based teaching [ 9 – 11 ]. Consequently, the pandemic prevented the delivery of our SSIP teaching in person for the 2020–2021 academic year. This posed a challenge for course tutors, as the replacement SSIP teaching had to enable students to successfully develop their research and scholarship skills entirely online. An innovative option was to involve the SSIP students in an active research study as a means of delivering their research and scholarship learning outcomes online. We define an ‘active research study’ as an ongoing research investigation in which data are collected and analysed concurrently while the course is being taught. This allows undergraduate students to observe the research process contemporaneously and gives them the opportunity to be involved in data collection and analysis.
Concurrent with SSIP teaching, the authors (AURA, MA, HAB) were researching the effects of COVID-19 on memory function using an online survey and memory quiz, the ‘COVID-19 Online Rapid Objective Neuro-Memory Assessment’ (CORONA) study [ 12 ]. We decided to utilise this investigation for our SSIP teaching. There are potential advantages of using an active research study for our SSIP teaching for both the students and to the research study. The primary advantage for the students would be in enabling them to gain research and scholarship skills in the absence of an in-person laboratory setting. By using an active research study, we hypothesise that students might find this more engaging and exciting than a standard practical exercise where the outcomes are known. Additionally, students could acquire skills and experience in the participant recruitment process. There could also be secondary advantages to the research study itself. For example, as students distributed the survey/memory quiz to their networks, there could be wider survey distribution, thereby increasing the size and demographic breadth of the study sample. Moreover, given the rapid output of COVID-19 research publications at that time, having multiple students engaged in literature searches enabled the timely identification of relevant literature.
The aim of this study was to explore student perceptions of an online SSIP course which involved them in an active research study. Within this context, we used a questionnaire to ask students whether the course developed their research and scholarship skills, and to evaluate the teaching content and format, as well as tutor performance. We captured and analysed student and tutor reflections on the positives and negatives of the online SSIP and possible improvements. To evaluate objectively whether learning outcomes were met successfully in the online/active research study SSIP course (2020–2021), we compared the student SSIP assessment marks across five years which included two years pre-pandemic and two subsequent years. We predicted that using an active research study to deliver SSIP teaching would interest, engage, and motivate the students while meeting the learning outcomes.
SSIP in-person teaching prior to COVID-19 (2017–2019)
Prior to the COVID-19 pandemic, the SSIP in neuroscience consisted of mandatory face-to-face tutorials and laboratory-based sessions delivered by three different tutors. Face-to-face tutorials (~ eight Year 1 students per tutor group) consisted of introduction to research methods, ethics, scientific oral/poster presentation and writing skills. Neuroscience-related practical sessions covered a range of topics, including clinical vision assessment and magnetic resonance imaging, recordings of neuronal oscillations and human electroencephalography. In all practical sessions, students gained live, in-person experience in experimental research design and set-up, data acquisition, analysis, visualisation, and interpretation. Additional supporting resources were provided online using the virtual learning environment (VLE), including timetables, research articles and relevant videos. Summative assessments consisted of scientific essays, posters and oral presentations based on their reading of the background literature and practical work.
SSIP online teaching during COVID-19 (2020–2021)
During the COVID-19 pandemic, the online SSIP content was designed to meet the same learning outcomes set out by the General Medical Council as in previous years (under ‘Clinical research and scholarship’) [ 1 ] . SSIP teaching sessions were redesigned and delivered completely online and synchronously using video conferencing via Microsoft Teams, and again, attendance was mandatory. In Term 2, teaching sessions started in January 2021 which coincided with the third national lockdown in England, UK [ 13 ]. During the COVID-19 pandemic, Year 1 students undertaking the SSIP had no prior experience with in-person teaching in the medical school. The students were based in two geographical locations (eight students based in Hull and seven based in York) but tutors and their respective student groups were combined, and all eight teaching sessions across Terms 2 and 3 were delivered synchronously online by all three tutors together. Online tutorial sessions covered an introduction to the CORONA research study, research ethics, questionnaire distribution, research methods, data analysis and basic statistics, scientific oral/poster presentation and writing skills. The design of the online teaching sessions drew on best practice in online learning and teaching [ 8 , 14 ]. The first teaching session in Term 2 included icebreaker exercises to engage with students and to replicate the informal environment of in-person small-group sessions. At the start of every online session, tutors encouraged all students to turn on their video cameras and ask questions to facilitate engagement and interaction. Students and tutors could interact via onscreen cameras and the ‘chat’ function in Microsoft Teams to allow students to give immediate feedback, provide reactions (e.g., ‘raised hand’), ask questions, and share their ideas. In one SSIP teaching session, we invited the clinicians involved in the CORONA research study to give their perspectives during an open discussion with the students. Following each online session, tutors had a debriefing session with each other reflecting on what went well and any areas of improvement.
Supporting resources were provided online on Microsoft Teams and the VLE, including timetables, research articles and relevant videos (for example, how to perform statistical tests in Microsoft Excel). Resources available to students in the online/active research course were therefore broadly equivalent to those provided in other years, although the scientific references provided were necessarily different due to the change in research topic. Students gave a formative scientific oral presentation online based on their reading of the background literature and were given written feedback from tutors. The students aided in the distribution of the CORONA survey and memory quiz during the period of the SSIP. Each student was given an individual research hypothesis/data associated with the CORONA study and undertook data analysis and interpretation to address the hypothesis. The summative assessment comprised a written scientific report. Tutors offered one-to-one online sessions to provide data analysis support, and separate sessions giving feedback on draft reports.
Ethics and consent
The study was carried out in conformity with the principles outlined in the Declaration of Helsinki, and local ethical approval was given by the Hull York Medical School Ethics Committee (Reference 20 62). All participants were adults aged 18 years old or older and consisted of undergraduate medical students at the Hull York Medical School and their lecturers/tutors. Only participants who gave their active digital written informed consent were allowed to complete the questionnaire. As part of consenting, we informed participants that the questionnaire was voluntary and anonymous. Moreover, it was stated on the consent page of the questionnaire that taking part or not taking part would not in any way affect the SSIP assessment marks. All data collected were non-identifiable.
Questionnaire design and dissemination
The online questionnaire was delivered using the Qualtrics platform accessed via a University of York license (Qualtrics, Provo, UT). The questionnaire was accessible via a Uniform Resource Locator (URL). The questionnaire required responses to 19 statements covering four categories: tutor performance (six statements), student skills (four statements), teaching content (four statements) and teaching format (five statements). Questionnaire statements were displayed one question at a time on the screen. Participants were instructed to indicate how much they agreed or disagreed with each statement using a slider scale. Participants were required to drag a circle (initially located at the halfway point) along a horizontal line to their selected point between two opposite labels at either end, ‘Strongly disagree’ (left) and ‘Strongly agree’ (right). There were no numerical labels on the horizontal line. This allowed respondents access to the full range of points between these two labels on the slider scale. Next, they were asked the following four open-ended free text questions to gather further details on student perceptions of the online SSIP and teaching preferences: ‘ What did you enjoy most about the SSIP being taught online?’; ‘What did you least like about the SSIP being taught online?’;‘What could be done to improve the SSIP being taught in an online format?’; ‘Which aspects of the SSIP would you prefer to be taught online and which aspects would you prefer to be taught in person? ’. Questions were created by AURA, MA and HAB based on previous literature [ 15 – 17 ] and other similar feedback questionnaires used within the Hull York Medical School and then reviewed by all of the authors including AIG who has experience in assessment and feedback research.
The web link to the SSIP feedback questionnaire was disseminated to all 15 Year 1 students on the neuroscience SSIP course. The questionnaire was issued on the last day of the SSIP course, one month prior to the release of the SSIP assessment marks. This was to ensure student response accuracy and avoid recall bias, and also bias based on assessment outcomes. All three SSIP tutors completed only the free text sections of the questionnaire.
Data analysis
The responses to the questionnaire were exported from Qualtrics to Microsoft Excel (version 2210, Microsoft Corp., Redmond, WA, USA). Although not visible to the participants, the response outputs from each of the 19 slider scale statements ranged from 0 to 100 arbitrary numerical units (resolution of 1 unit), where 0 represented ‘Strongly disagree’, and 100 represented ‘Strongly agree’. Means, standard error of the means and ranges were computed across 13 respondents using Excel.
Individual student and tutor free text responses were categorised and analysed using a six-step thematic analysis as described by Braun and Clarke [ 18 ] and Kiger and Varpio [ 19 ]. Two authors (AURA, HAB) used an inductive approach to collaborative coding [ 20 ] where codes were developed whilst working through the data set and there were no preconceptions about themes. We first highlighted free text responses for key words and phrases using Microsoft Word. Next, we looked for patterns and shared meanings in the highlighted key words and phrases, and then grouped them into themes. We counted the number of student responses within each theme and calculated the frequency as a percentage of the total number of students ( n = 13). All tutor responses were included ( n = 3). Given the relatively small number of student and staff participants, we thought it appropriate and important to report and consider all the viewpoints.
For the neuroscience SSIP for the period 2017–2019, marks were derived from summative assessments of essays in Term 1, posters in Term 2, and oral presentations in Term 3. From academic year 2019–2020 and for all subsequent years to date, the assessment format of the SSIP was changed by the Hull York Medical School, whereby the SSIP course marks were derived from a single summative assessment of a written scientific report/essay in Term 3. However, summative assessments were suspended in the 2019–2020 academic year due to the COVID-19 pandemic. For the SSIP teaching in the years 2017–2019, the marks for Terms 1, 2 and 3 were averaged to produce a single summative mark for each student. Importantly, assessments for all years (2017–2023) were evaluated considering the same elements related to scientific background, data analysis/visualisation, and interpretation of the results in the context of the published literature. The same marking scale and rubric were used for SSIP assessments across all years: 1 = Fail ( Failed to meet many of the intended learning outcomes; work was deficient in critical aspects and demonstrated significant lack of understanding; lacked a secure basis in relevant facts and analysis; lacked a good structure. ), 2 = Pass ( Achieved the intended learning outcomes; used a sufficient range of evidence and displayed a good grasp of analytical issues and concepts; produced well-structured work. ), and 3 = Excellent ( Achieved all intended learning outcomes; used a comprehensive range of relevant materials and analyses; showed in-depth understanding of all key issues and concepts and clear evidence of critical and synthetic skills. ). A one-way ANOVA was used to compare mean summative marks across the SSIP teaching years 2017–2023, except the year 2019–2020 when no student summative assessments took place.
Student quantitative perceptions to questionnaire statements
Thirteen out of 15 students completed the questionnaire (87%); all who completed did so within two days of dissemination. Figure 1 shows student responses to 19 statements covering four categories: tutor performance, student skills, teaching content and teaching format. The mean scores for all the questionnaire statements exceeded 59/100 (although some individual responses were lower) indicating that most students agreed with the statements (Fig. 1 ).

Questionnaire statements arranged in rank order from highest (strongly agree) to lowest (strongly disagree) scores. The filled black circles represent the mean ± standard error of the mean. Parentheses after each questionnaire statement give the number of students who scored that statement > 50 (range: neutral to strongly agree). Square brackets give the range of participant responses (minimum and maximum values)
Students most strongly agreed with statements associated within the tutor performance category (Fig. 1 ). The highest mean scores ( most strongly agree ) were given for statements related to the level of tutor support (96.6 ± 2.5), tutor knowledge of course material (93.9 ± 3.1), the ability of tutors to present material in an engaging manner (92.3 ± 2.9), and whether tutors gave appropriate feedback on reports (91.8 ± 4.4). Relatively lower mean agreement scores were given for tutors making course materials available in good time (85.9 ± 6.7), and provision of appropriate feedback on online oral presentations (79.5 ± 8.7).
Within the student skills category, students agreed on average that the online/active research course enabled them to improve data analysis skills (91.9 ± 4.4), gain transferable skills (90.4 ± 4.3), and oral presentation skills (87.9 ± 3.7). The average scores were lower when asked whether they enjoyed the data analysis aspects of the SSIP course online (73.2 ± 6.7).
For the teaching content category, on average students found the topics interesting (90.2 ± 3.3), understood the content (87.8 ± 3.8), engaged well with the content (87.2 ± 3.8) and were motivated to learn more about the topic (84.9 ± 3.7).
Students agreed least with statements within the online teaching format category, related to enjoyment of the online SSIP course (63.2 ± 4.8) and undertaking another SSIP online (59.4 ± 7.1). On average, students agreed that they were looking forward to a laboratory-based SSIP (88.9 ± 4.9), thinking at the point of allocation that it would have been held in-person and not in an online format. On average, students agreed that the SSIP teaching was presented in a structured way (83.5 ± 7.1) and they engaged well with the online teaching format (81.5 ± 4.0).
Student qualitative perceptions of online course teaching
Table Table1 1 lists five themes identified from free text student responses to the question, ‘ What did you enjoy most about the SSIP being taught online? ’ The most frequent theme for this question was related to convenience (54%), followed by use of online resources (23%) and use of screen sharing (15%). Other students enjoyed being able to experience research (8%) and communication/interaction online (8%). Table Table2 2 lists three themes identified for the question ‘ What did you least like about the SSIP being taught online? ’ The most frequent theme for this question was related to communication/interaction (46%), followed by laboratory skills (31%) and engagement (23%). Table Table3 3 lists four themes identified for the question ‘ What could be done to improve the SSIP being taught in an online format? ’ The most frequent theme for this question was related to resources (31%), followed by engagement (23%). A smaller number of students gave responses related to communication/interaction and laboratory skills (15% each). Table Table4 4 lists six themes identified for the question ‘ What aspects of the SSIP would you prefer to be taught online …? ’ and six themes identified for ‘ … and which aspects would you prefer to be taught in person? ’. The most frequent themes for online teaching were related to content and data analysis (23% each), and for in-person teaching, the most frequent student responses were related to presentation skills (23%) and communication/interaction (15%).
Themes identified from student responses to the question, ‘ What did you enjoy most about the SSIP being taught online? ’
| | ||
|---|---|---|
| 7 (54%) |
| |
| 3 (23%) | ||
| 2 (15%) | ||
| 1 (8%) | ||
| 1 (8%) |
Themes identified from student responses to the question, ‘ What did you least like about the SSIP being taught online? ’
| | ||
|---|---|---|
| 6 (46%) | ||
| 4 (31%) | ||
| 3 (23%) |
Themes identified from student responses to the question, ‘ What could be done to improve the SSIP being taught in an online format? ’
| | ||
|---|---|---|
| 4 (31%) | ||
| 3 (23%) |
| |
| 2 (15%) | ||
| 2 (15%) |
Themes identified from student responses to the question, ‘ Which aspects of the SSIP would you prefer to be taught online and which aspects would you prefer to be taught in person? ’
| | ||
|---|---|---|
| 3 (23%) | ||
| 3 (23%) | ||
| 2 (15%) | ||
| 2 (15%) | ||
| 1 (8%) | ||
| 1 (8%) | ||
| 3 (23%) | ||
| 2 (15%) | ||
| 1 (8%) | ||
| 1 (8%) | ||
| 1 (8%) | ||
| 1 (8%) | ||
Tutor qualitative perceptions of online course teaching
As there were only three tutors, we have included all their responses to the free text questions (Tables (Tables5, 5 , ,6, 6 , ,7 7 and and8). 8 ). The four themes identified for the question, ‘ What did you enjoy most about the SSIP being taught online? ’ were related to communication and interaction, collaborative teaching, convenience, and novelty (Table (Table5). 5 ). Communication and interaction, laboratory skills and preparation time were the three themes identified for the question, ‘ What did you least like about the SSIP being taught online? ’ (Table (Table6). 6 ). Only one theme, communication and interaction, was identified for the question, ‘What could be done to improve the SSIP being taught in an online format?’ (Table (Table7). 7 ). Therefore, communication and interaction were a common theme throughout tutor responses to these three questions. Four themes were identified for preferences for online teaching (data analysis, academic writing, presentation skills and content) and two themes for in-person teaching (laboratory skills and general preference) (Table (Table8 8 ).
Themes identified from tutor responses to the question, ‘ What did you enjoy most about the SSIP being taught online ?’
| |
| |
Themes identified from tutor responses to the question, ‘ What did you least like about the SSIP being taught online ?’
| |
| |
Themes identified from tutor responses to the question, ‘ What could be done to improve the SSIP being taught in an online format? ’
|
Themes identified from tutor responses to the question, ‘ Which aspects of the SSIP would you prefer to be taught online and which aspects would you prefer to be taught in person? ’
| |
| |
Comparison of academic assessment marks
Student attendance overall for the online/active research SSIP was 97.5%; out of eight mandatory teaching sessions for 15 students (8 sessions × 15 students = 120), a total of 117/120 attended with only three absences over the course. Assignment completion was 100%, and every student submitted their assignments within the deadline set. As an objective measure to determine whether learning outcomes were met during the year of the study (2020–2021), we compared summative assessment marks across five teaching years (2017–2023) which included two years prior to the onset of the COVID-19 pandemic and two years after the study year (Fig. 2 ). A one-way ANOVA revealed no significant difference for summative marks across all five years, F(4, 60) = 1.84, p = 0.133, eta squared = 0.109. All students achieved a Pass or Excellent mark with no Fails.

Plot showing the mean assessment marks for the SSIP teaching spanning the years 2017–2023. The vertical dotted line represents the start of the COVID-19 pandemic. A one-way ANOVA revealed no significant difference across the years ( p > 0.05). *There were no SSIP assessments for the year 2019–2020. Marks: 1 = Fail, 2 = Pass, 3 = Excellent
Learning outcomes and developing student research skills
In this study we were interested in investigating student perceptions of a course delivered online which involved them in an active research study. The student responses to questionnaire statements indicate that despite major changes from in-person laboratory-based SSIP teaching to the fully online format using an active research study, students were largely positive about most aspects of the redesigned course delivered during the COVID-19 pandemic. Even though students agreed least with the statements related to enjoying the online teaching format, and whether they would undertake another SSIP online, the average agreement scores were still above 50%. While students expressed a preference for a laboratory-based course, they nonetheless reported that they developed valuable research skills from the online/active research course. Students agreed that they were able to acquire research skills, particularly related to data analysis, transferable skills, and giving an oral scientific presentation. However, they found the online data analysis component comparatively less enjoyable.
Assessments required students to demonstrate research skills gained, including researching and consolidating the relevant scientific literature, data analysis and visualisation, and interpretation of the results in the context of the field. In addition, students presented an overview of their selected topic based on their review of the literature, and generated a scientific report based on their data analysis, demonstrating their presentation and written research skills. SSIP summative assessment marks for the online/active research course in 2020–2021 were comparable to marks in earlier and later years, providing evidence that students achieved the learning outcomes and successfully acquired research skills.
Benefits of using an active research study to engage and motivate students
Our survey results show that using an active research study led to high student engagement with the online SSIP content and motivated them to learn more about the topic. There are several reasons that could explain why our students found the online/active research SSIP course engaging and motivating. Firstly, the choice of topic, the effects of COVID-19 on memory, may have been of special interest because it was timely and of current global concern. Most students agreed (a score of ~ 90%) that the topic was interesting, and that the teaching content was understandable. One student stated that the most enjoyable part of the online teaching was “Being able to see real-life research”. Secondly, students had the opportunity to contribute to an ongoing research study by distributing the survey online to recruit participants and by performing preliminary data analyses. Thirdly , the small group size (15 students to three tutors, a student-staff ratio of 5:1) may have encouraged greater student-to-tutor and student-to-student interactions (approximately half the students were located in Hull and half in York). In a previous study, some UK medical students reported that small group sizes elevated student engagement [ 16 ]. Indeed, one student based in York reported that the most enjoyable aspect of the online teaching was, “Being able to meet some Hull-based students.” Fourthly, students may have been more engaged because they were especially pleased with tutor performance. Indeed, the three statements with highest agreement from the students were that they felt well supported by tutors, that tutors were knowledgeable about the course and presented material in an engaging manner. Given that tutors were invested in the active research study, this may have been reflected in their knowledge of and enthusiasm for the topic.
In line with our results, a study of first-year undergraduate medical students demonstrated that early experiences of successful engagement with authentic research practices increases subsequent motivation for research [ 21 ]. Advice given by Ommering et al. states the importance of providing students with authentic research experiences, in particular addressing authentic research questions of clinical importance where possible [ 22 ]. The active research study used in the current investigation was timely and clinically relevant given the impact of COVID-19 on cognition, particularly memory function [ 12 ]. Engaging medical students with authentic research experiences early in their career is a potential way to reverse the decline in the clinical academic (also called ‘physician scientist’) workforce [ 23 ].
Learning context is important. Embedding an active research study in research methods training aligns with the principles of situated learning [ 24 ]. Lave and Wenger describe how learners learn through legitimate peripheral participation and benefit from exposure to a community of practice [ 25 ]. Through small-group discussions with expert tutors and exposure to real-world data, the students in this study began to integrate into the research community (five of the students from this group have actively sought to continue their involvement with research post-SSIP). Indeed, in their ‘Twelve tips’ guide to encouraging student engagement in academic medicine, Lawson McLean et al. encourage involving students in the practicalities of research [ 26 ]. Involving students in authentic ongoing research has been shown to benefit students in other practical disciplines such as language translation, with the potential to enhance the proficiency of students both as researchers and as reflective practitioners [ 27 ].
Benefits to research
Involving undergraduates had a direct benefit to our research study. For example, by distributing the research survey/memory quiz link to their networks, they aided in participant recruitment. In addition, they helped identify relevant references from the scientific literature and summarised them in their oral presentations. Another benefit of involving students was that they provided a diversity of perspectives, experiences and previously acquired skills to our research study. Based on these benefits, we recommend that educators consider involving undergraduate students in an active research study. Tutors may first need to consider the appropriateness of the research project for undergraduate teaching purposes. A second consideration is to ensure that ethical approval allows for student involvement in the research study, including aspects related to safety and confidentiality. Thirdly, the timing of the teaching sessions needs to be coordinated within the context of the research study, e.g., data collection. An alternative would be to involve students only in secondary data analysis, which would allow for greater flexibility. Overall, using an active research study not only advances student research skills, but can also bring value to the research project itself.
Benefits of the online teaching format
In a study investigating online clinical medicine teaching, faculty members reported high satisfaction with student engagement levels and the quality of student interactions for the online technology-enhanced sessions but low satisfaction with the in-person traditional clinical sessions [ 28 ]. In our current study, student and tutor free text responses indicated that they particularly enjoyed the convenience of learning/working online, the availability and use of online resources and the use of online video technology (screen sharing). Because it was online, it meant it was easier for students and tutors to attend without the need to commute, which was important because attendance for the SSIP was mandatory. Student attendance for our online SSIP teaching was high (97.5%), which is similar to the 100% attendance reported by Kay & Pasarica in a study using online teaching in medical education where the attendance was also mandatory [ 28 ]. This study reported that 100% of their students completed the online assignments ( n = 27), which aligns with the 100% assignment completion rate in our online SSIP teaching ( n = 15). This shows that for mandatory online teaching sessions, attendance and assignment completion rates are high.
Another aspect of online teaching that students liked was the availability of online resources which they could view before or after online sessions. For example, we made online resources available including the documents associated with the research study, literature references and video recordings on how to analyse the data using statistics. Our approach to the online sessions was in line with recommendations outlined by Ohnigian and colleagues [ 29 ]. For example, we made use of the chat function and encouraged students to turn their cameras on to ask questions and interact with the tutors and other students. Some students mentioned that they enjoyed most the way tutors used screen sharing function in Teams to demonstrate specific concepts, such as data analysis.
From the tutors’ perspective, they enjoyed the novelty and collaborative aspects of online teaching. For example, one tutor stated that they enjoyed the pre- and post-meeting sessions with the other course tutors. Another tutor pointed out that a benefit of working online with tutors at different locations was to gain from their diverse perspectives and teaching styles. Although these positives are both possible with in-person teaching, the online format made collaboration across geographical boundaries easier. Another advantage of conducting the course online is that clinicians were able to contribute to one of our online teaching sessions, which would have been much more difficult to arrange in person due to their demanding schedules.
Disadvantages of online teaching
There were aspects that students and tutors were less positive about the online teaching. Both students and tutors highlighted the lack of face-to-face interactions. Students were not able to meet tutors and other members of the group in person. Both students and tutors were concerned that the online format reduced student engagement. The lack of interaction with fellow students has been noted in a previous study which highlighted problems with student motivation, concentration and asking questions online [ 16 ]. Since the SSIP students often turned off their cameras and microphones, tutors also expressed concern that they were less engaged talking to a blank screen. Using a phenomenological approach, Schwenck & Pryor found that it was important for students to have cameras switched on rather than looking at a blank screen to feel engaged and connected [ 30 ]. Although there are several reasons why students do not turn their video cameras on, including it being considered the norm, and concerns about physical appearance or screen background, it may be possible to use strategies such as active learning techniques to encourage camera usage [ 31 ]. Cheung and colleagues found that students’ perceptions of online teaching were more favourable when video cameras were turned on so, although students are reluctant to do so, as educators, we should support students to turn their cameras on in sessions [ 32 ].
When students were asked which aspects of the SSIP they would prefer to be taught online and which aspects they would prefer to be taught in person, there was, in many cases, little agreement amongst students. For example, some students would prefer data analysis and statistics to be taught online whereas others would prefer these subjects to be taught in person. Similarly, some students think oral presentations should be done online, some think they should be done in person. This reflects the heterogenous nature of the student body and tutors should be mindful of this. Tutors could cater for the needs of a diverse group by offering multiple formats of engagement to increase accessibility. For instance, data analysis classes could alternate between classes being held online and in person.
Both students and tutors mentioned that they would have benefited from the experiences of learning and teaching in a physical laboratory space. One important point was that students were not able to develop laboratory skills that could best be learned using a hands-on, practical approach. One student captured this by stating, ‘ I was looking forward to the practical elements in the lab which could not be done online’. Colthorpe & Ainscough similarly found that although students believe the online teaching to be helpful, the lack of in-person laboratory classes and face-to-face interactions negatively affected their learning experience [ 11 ]. In our study, two students suggested that a compromise could be to demonstrate online some of the practical skills that would normally be done in the laboratory. One limitation of our study is that as the Year 1 students started during the COVID-19 pandemic, they did not have any prior experience with in-person laboratory teaching within the medical curriculum. Therefore, they were not able to compare the SSIP teaching we delivered online with a face-to-face taught laboratory course. Moreover, since the SSIP teaching coincided with a national lockdown, this may have impacted on how well students engaged with the online course. Because students were mandated to stay at home, they could have seen the online SSIP teaching as one of their only opportunities to gain research experience and interact with students/tutors, which may have inclined them to respond more favourably to our questionnaire.
One tutor expressed concern that more time was needed to prepare materials for the online sessions compared to in person. Given that tutors had to become familiar with new online software and features to deliver online teaching, this will have increased their preparation time. In line with this, a survey of academics found that more time is needed to prepare for online teaching compared to on-campus teaching [ 33 ].
Students and tutors both suggested future improvements to the online SSIP teaching. For example, recommendations included making the online course more interactive, keeping cameras on, using breakout rooms and the chat feature more, incorporating student-led sessions and keeping sessions shorter. When students and tutors were asked which aspects they preferred to be taught online versus in person, several students and tutors suggested that content and data analysis could be taught online, while laboratory skills could be taught in person.
Limitations
One limitation of the current study is the relatively small number of student ( n = 13) and tutor ( n = 3) participants. Ours is not the first study to consider the views of small numbers of medical students engaging with innovative teaching practices. For example, Margolin et al. considered the views of 13 medical students to make recommendations for online urologic education during the COVID-19 pandemic [ 34 ], and Blackard et al. piloted an online research training course with 27 medical students [ 35 ]. Our current study, which was undertaken in the context of small group teaching, provides data with initial indications that student perceptions were positive for teaching research skills online using an active research study during the COVID-19 pandemic. The hope is that our study encourages future studies using an active research study in larger cohorts across different medical schools and disciplines.
Both of the researchers (AURA and HAB) who coded the free text responses were involved in teaching and assessing the SSIP module and were investigators in the active research study. Whilst their familiarity with both the educational and research aspects of the project provided valuable context to the coding, we acknowledge that an independent researcher may have coded the free text comments differently.
Student engagement and motivation scores may have been affected by both the online teaching format and involvement in an active research study. We cannot disentangle the separate effects of each component in the current investigation. Each component would have to be evaluated in separate student groups, but such a study could lead to a lack of teaching parity across groups. A crossover design in which all students are exposed to each component consecutively could be another possible approach to extract the independent contributions of the online teaching versus the active research component.
Taken together, our results indicate that a course can be delivered online using an active research study that will enable medical students to acquire research and scholarship skills, thereby fulfilling the ‘Clinical research and scholarship’ learning outcomes of the General Medical Council. More generally, this approach could be utilised as a model to deliver online teaching in other disciplines requiring the development of student research skills. It would enhance course accessibility and accommodate the needs of student groups who find it challenging to attend in-person courses such as students based outside the university, or those with physical disabilities or caring responsibilities. Moreover, online teaching with an active research component could encourage greater collaboration between instructors and researchers, as there would be fewer time and space constraints, thereby enriching the student and tutor experiences.
Acknowledgements
The authors gratefully acknowledge the participants in the study and thank the students on the SSIP course.
Abbreviations
| SSIP | Scholarship and Special Interest Programme |
| SSC | Student-Selected Component |
| COVID-19 | Coronavirus Disease 2019 |
| VLE | Virtual Learning Environment |
| CORONA | COVID-19 Online Rapid Objective Neuro-Memory Assessment |
| URL | Uniform Resource Locator |
Authors’ contributions
AURA conceptualised and designed the study, collected and analysed data and was a major contributor in writing the manuscript. MA helped design the study and provided significant technical support for survey design, data collection and analysis. AIG helped design the survey, provided feedback and advice on data analysis, and contributed to writing and editing the manuscript. HAB conceptualised and designed the study, collected, and analysed data and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Not applicable.
Availability of data and materials
Declarations.
The study was carried out in conformity with the principles outlined in the Declaration of Helsinki, and local ethical approval was given by the Hull York Medical School Ethics Committee (Reference 20 62). All participants were adults aged 18 years old or older and consisted of undergraduate medical students at the Hull York Medical School and their lecturers/tutors. Only participants who gave their active digital written informed consent were allowed to complete the questionnaire. As part of consenting, we informed participants that the questionnaire was voluntary and anonymous. Moreover, it was stated on the consent page of the questionnaire that taking part or not taking part would not in any way affect students’ assessment marks. All data collected were non-identifiable.
The authors declare no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Developing research skills in medical students: AMEE Guide No. 69
Affiliation.
- 1 Medical School, University of St Andrews, UK.
- PMID: 22905661
- DOI: 10.3109/0142159X.2012.704438
This Guide has been written to provide guidance for individuals involved in curriculum design who wish to develop research skills and foster the attributes in medical undergraduates that help develop research. The Guide will provoke debate on an important subject, and although written specifically with undergraduate medical education in mind, we hope that it will be of interest to all those involved with other health professionals' education. Initially, the Guide describes why research skills and its related attributes are important to those pursuing a medical career. It also explores the reasons why research skills and an ethos of research should be instilled into professionals of the future. The Guide also tries to define what these skills and attributes should be for medical students and lays out the case for providing opportunities to develop research expertise in the undergraduate curriculum. Potential methods to encourage the development of research-related attributes are explored as are some suggestions as to how research skills could be taught and assessed within already busy curricula. This publication also discusses the real and potential barriers to developing research skills in undergraduate students, and suggests strategies to overcome or circumvent these. Whilst we anticipate that this Guide will appeal to all levels of expertise in terms of student research, we hope that, through the use of case studies, we will provide practical advice to those currently developing this area within their curriculum.
PubMed Disclaimer
Similar articles
- Integrating professionalism into the curriculum: AMEE Guide No. 61. O'Sullivan H, van Mook W, Fewtrell R, Wass V. O'Sullivan H, et al. Med Teach. 2012;34(2):e64-77. doi: 10.3109/0142159X.2012.655610. Med Teach. 2012. PMID: 22289014 Review.
- Communication skills: an essential component of medical curricula. Part I: Assessment of clinical communication: AMEE Guide No. 51. Laidlaw A, Hart J. Laidlaw A, et al. Med Teach. 2011;33(1):6-8. doi: 10.3109/0142159X.2011.531170. Med Teach. 2011. PMID: 21182378 Review.
- What do medical students understand by research and research skills? Identifying research opportunities within undergraduate projects. Murdoch-Eaton D, Drewery S, Elton S, Emmerson C, Marshall M, Smith JA, Stark P, Whittle S. Murdoch-Eaton D, et al. Med Teach. 2010;32(3):e152-60. doi: 10.3109/01421591003657493. Med Teach. 2010. PMID: 20218832
- Student Selected Components (SSCs): AMEE Guide No 46. Riley SC. Riley SC. Med Teach. 2009 Oct;31(10):885-94. doi: 10.3109/01421590903261096. Med Teach. 2009. PMID: 19877860
- Medical students' perceptions of an undergraduate research elective. Houlden RL, Raja JB, Collier CP, Clark AF, Waugh JM. Houlden RL, et al. Med Teach. 2004 Nov;26(7):659-61. doi: 10.1080/01421590400019542. Med Teach. 2004. PMID: 15763861
- vSEMERA: pilot project assessing health profession students' experiences in an international virtual research program. Bell L, Lemos E, Krimphove J, Kaiser S, Guerra-Giraldez C, Lemos M. Bell L, et al. BMC Med Educ. 2024 Jun 1;24(1):606. doi: 10.1186/s12909-024-05528-6. BMC Med Educ. 2024. PMID: 38824559 Free PMC article.
- Scientific competence during medical education - insights from a cross-sectional study at a German Medical School. Vogt M, Schuchardt N, Geissler ME, Bereuter JP, Geissler RB, Glauche I, Gerdes S, Deußen A, Günther L. Vogt M, et al. BMC Med Educ. 2024 May 28;24(1):590. doi: 10.1186/s12909-024-05470-7. BMC Med Educ. 2024. PMID: 38807084 Free PMC article.
- Effectiveness of simulation-based clinical research curriculum for undergraduate medical students - a pre-post intervention study with external control. Huang Q, Yan SY, Huang J, Guo Y, Zeng XT, Jin YH. Huang Q, et al. BMC Med Educ. 2024 May 15;24(1):542. doi: 10.1186/s12909-024-05455-6. BMC Med Educ. 2024. PMID: 38750452 Free PMC article.
- Assessing the impact of Medical Education's Innovation & Entrepreneurship Program in China. You X, Wu W. You X, et al. BMC Med Educ. 2024 May 10;24(1):519. doi: 10.1186/s12909-024-05467-2. BMC Med Educ. 2024. PMID: 38730441 Free PMC article.
- Perception, practice, and barriers toward research among pediatric undergraduates: a cross-sectional questionnaire-based survey. Zhan C, Zhang Y. Zhan C, et al. BMC Med Educ. 2024 Apr 3;24(1):364. doi: 10.1186/s12909-024-05361-x. BMC Med Educ. 2024. PMID: 38570767 Free PMC article.
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Taylor & Francis
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
COVID-19: Vaccine Program | Testing | Visitor Guidelines | Information for Employees MONKEYPOX: UConn Health is NOT currently offering the monkeypox vaccine. Please visit the CT DPH website for more information or contact your health provider directly. -->
School of Medicine Office of Faculty Affairs
Faculty Development
Research skills.
Strengthening research skills, including grant and scholarly writing, is pivotal for faculty. These abilities not only secure funding but also drive transformative advancements in research and practice.
Grant Development Resources
- UConn’s Office for the Vice President for Research (OVPR) The OVPR Research Development Program aims to enhance UConn’s research climate by promoting faculty research by helping faculty be better positioned to generate external funding for their scholarly activities. The OVPR Research Development provides a grant writing seminars and workshops, proposal development services, and technical assistance.
- The UConn Health Center Research Advisory Council (HCRAC) advises the Vice President for Research and the Research Deans on the development, management, and disposition of the Health Center’s central research resources and intramural grants programs. HCARC provides a number of grant development resources.
- UConn School of Medicine provides links to funding opportunities as well as grant development support including Mock Study Section and Scientific Writing, Editing, and Grant Support
- UConn’s Institute for Collaboration on Health, Intervention, and Policy (InCHIP) brings together individuals with diverse scientific, clinical, and methodological expertise and supports their evolution into collaborative investigators who conduct innovative interdisciplinary research that impacts public health and well-being. InCHIP provides assistance with Research Training & Development including training, mentorship, research team development, grant proposal writing and internal funding opportunities.
Scholarship
- UConn School of Medicine Seminars. The following seminars from the UConn School of Medicine Faculty offer advice and tips for publishing.
- Forming Writing Groups: One Person’s Experience. Anne Kenny, M.D. September 26, 2013. (55:52)
- A Writing Accountability Group or WAG is an active writing group that meets once a week over a 10-week block and follows a strict agenda. WAGs are focused on the process not the content of writing. For more information in starting or joining a WAG at UConn Health, please contact Jenn Cavallari, ScD, Director of Faculty Development ([email protected]) .
- Getting started with scholarship. Coming soon
Predatory Publishing
- Predatory Journals – How to Identify and Avoid Them . Peter Setlow, Ph.D., and Anne Kenny, M.D., January 2019. (16:17)
- Think, Check, Submit . Follow this checklist to make sure you choose trusted journals for your research.
External Career Development Resources for Research
- The National Institutes of Health Research Training and Career Development programs provide information and training opportunities to support a broad range of training and career goals.
- The Burroughs Wellcome Fund Career Development Guides provide guidance for scientists and researchers at all levels covering topics including communicating science, managing career transitions and intellectual property.
- The Burroughs Wellcome Fund Lab Management Guide . Making the Right Moves is a collection of practical advice and experiences from seasoned biomedical investigators and includes chapters on laboratory leadership, getting funded, project management, and teaching and course design.
- Science Careers provides articles and other careers information, tips and advice relevant to a broad range of disciplines.
- The National Center for Faculty Development and Diversity provides programs and resources to support faculty success across all-levels and disciplines. UConn Health Center faculty are eligible for a no-cost sub-account through UConn’s Center for Excellence in Teaching and Learning (CETL) Institutional Membership. Additional information on creating your account is provided by CETL.
- Explore Options
Research career paths
Sign in for full access to careers in medicine’s tools, learn if you are eligible for a free subscription.
- Academic medicine
Careers in Medicine (“CiM”) is an online resource owned and operated by the Association of American Medical Colleges (“AAMC”). After purchase, the CiM online content (“CiM Material”) is made available through https://careersinmedicine.aamc.org (the “Site”). Acceptance of Terms of Use These terms and conditions (“Terms”) govern your purchase and use of the CiM Material. In addition, the AAMC Website Terms and Conditions are incorporated herein by reference, if a conflict exists these Terms shall take precedence. If you do not accept these Terms, do not purchase the CiM Material nor use the services provided through the Site. By visiting the Site, you also agree we may revise these Terms from time to time without providing notice to you. Your continued use of the Site after such revision marks your acceptance of the Terms as revised. We recommend you review these Terms regularly as they are subject to change. Personal Information Personal information submitted in connection with the use of the CiM Material is subject to the AAMC Privacy Statement, as it may be amended from time to time, which is incorporated into these Terms by reference. Your CiM assessment and exercise results are confidential. However, designated school representatives can view individual registration, login, and assessment dates. Permitted Use and Access The AAMC grants you a personal, non-exclusive, non-transferrable, limited privilege to access the Site and CiM Material. Your permitted use of the Site and CiM Material is limited solely to career planning and decision making. No other use of the Site or CiM Material is permitted under these Terms. Your access to the Site is limited to the forward-facing portions of the Site and CIM Material webpages. Unauthorized access includes, but is not limited to, attempts to gain access to any portion or feature of the Site or CIM Material, or any other systems or networks connected to the Site, CIM Material, or associated server, or to any of the services offered on or through the Site or CIM Material, by hacking, password mining, application or scripts or other electronic means, or any other illegitimate means. The AAMC reserves the right to refuse service or provide CiM Material access to any person or entity at our sole discretion.

- 1-844-994-6376
- [email protected]

The Guide to Becoming a Medical Researcher
- February 1, 2023
Share Post:
As a medical researcher, your job is to conduct research to improve the health status and longevity of the population. The career revolves around understanding the causes, treatments, and prevention of diseases and medical conditions through rigorous clinical investigations, epidemiological studies, and laboratory experiments. As a medical researcher, simply gaining formal education won’t suffice. You also need to hone your communication, critical thinking, decision-making, data collecting, data analyzing and observational skills. These skill sets will enable you to create a competitive edge in the research industry. On a typical day, a medical researcher would be collecting, interpreting, and analyzing data from clinical trials, working alongside engineering, regulatory, and quality assurance experts to evaluate the risk of medical devices, or maybe even preparing and examining medical samples for causes or treatments of toxicity, disease, or pathogens.
How To Become a Medical Research Doctor?
The roadmap to medical research is a bit tricky to navigate, because it is a profession that demands distinctive skills and expertise along with mandatory formal education. If you harbor an interest in scientific exploration and a desire to break new ground in medical knowledge, the first step is to earn a bachelor’s degree in a related field, such as biology, chemistry, or biochemistry. After completing your undergraduate education, you will need to earn a Medical Degree ( MD ) or a Doctor of Osteopathic Medicine (DO) degree, from a quality institution such as the Windsor university school of Medicine.
After that, the newly minted doctor of medicine (MD) may choose to complete a three-year residency program in a specialty related to medical research, such as internal medicine, pediatrics, or neurology, in addition to a doctor of philosophy (PhD) degree—the part that provides the research expertise. In some medical school programs, students may pursue a dual MD-PhD at the same time, which provides training in both medicine and research. They are specifically designed for those who want to become research physicians. Last but not the least, all physician-scientists must pass the first two steps of the United States Medical Learning Examination (USMLE).
Use your fellowship years to hone the research skills necessary to carry out independent research. You may also take courses in epidemiology, biostatistics, and other related fields. In order to publish your research in peer-reviewed journals to establish yourself as a medical researcher. To apply for a faculty position at a medical school, research institute, or hospital. To maintain your position as a medical research doctor, you must publish your research and make significant contributions to the field.
How Much Do Medical Researchers Make?
Having a clear idea of what to earn when you become a medical researcher can help you decide if this is a good career choice for you. The salaries of Medical Researchers in the US range from $26,980 to $155,180, with a median salary of $82,240. There is also room for career advancement and higher earning potential as you gain experience.
The Most Popular Careers in Medical Research
- Medical Scientists – conduct research and experiments to improve our understanding of diseases and to develop new treatments. They also develop new medical technologies and techniques.
- Biomedical engineers – design medical devices, such as pacemakers, prosthetics, and imaging machines. They also develop and improve existing medical technologies.
- Clinical Trial Coordinators – oversee and manage clinical trials, which test new drugs and treatments. They are responsible for recruiting participants, collecting and analyzing data, and ensuring the trial is conducted in compliance with ethical standards.
- Medical Laboratory Technicians – analyze bodily fluids and tissues to diagnose diseases and conditions. They perform tests using specialized equipment and techniques, and report results to physicians.
- Biostatisticians – collect statistics to analyze data and test hypotheses in medical research. They design and analyze clinical trials, and use statistical models to understand the causes and effects of diseases.
- Epidemiologists – study the causes, distribution, and control of diseases in populations. They collect and analyze data, and use their findings to develop strategies for preventing and controlling diseases.
- Pathologists – diagnose diseases by examining tissues and bodily fluids. They use microscopes and other diagnostic tools to identify and study the changes in tissues caused by disease.
- Genetic Counselors – help individuals understand and manage the risks associated with inherited genetic disorders. They educate patients about genetic tests and help families make informed decisions about their health.
- Health Services Researchers – study the delivery of healthcare and identify ways to improve it.
- Medical writers – write articles, reports, and other materials related to medical research.
- Microbiologists – study microorganisms, including bacteria and viruses, to understand their behavior and impact on human health.
- Neuroscientists – study the brain and nervous system to understand the underlying causes of neurological conditions.
- Toxicologists – study the effects of toxic substances on living organisms and the environment.
Skills You Need to Become a Medical Researcher?
To be a successful medical scientist, you need a range of soft and hard skills to excel in your work. First things first, medical researchers must be able to analyze data, identify patterns, and draw conclusions from their findings. They must be able to think critically, ask relevant questions, and design experiments to answer those questions. Additionally, you should also have the knack of articulating your findings clearly and effectively, be it writing research papers, grant proposals, or technical reports that are clear, concise, and free from errors.
Medical researchers must be proficient in using various computer programs and software to collect, manage, analyze and interpret research data. They must be able to use laboratory equipment and techniques, as well as statistical analysis software and other tools for data analysis. Since medical research involves precise and meticulous work, so you must also pay close attention to detail to ensure that your findings are accurate and reliable. Not to mention, medical researchers often work in teams, so it pays off if you are good at collaborating with others effectively, sharing ideas, and working together to solve complex problems.
Lastly, medical researchers must have a thorough understanding of regulations and ethical guidelines that govern research, such as obtaining informed consent from study participants, ensuring data confidentiality, and adhering to safety protocols.
Related posts

Top Emerging Fields in Medicine you may not have heard of

A Day in the Life of an EM doctor

The Path to Becoming a Neonatologist – The Education, Career, and Job Duties
Start online application.

Latest Post
Most viewed.
As the field of medicine evolves, so do the types of specialties that are in demand. A plethora of new career paths have emerged in
Are you thinking of a career in Emergency medicine? Do you often wonder what it’s like to step in to the busy shoes of an
Neonatology involves caring for and treating newborn babies, sick babies or premature babies, from the time that they are born to when they are stable
Follow us on Twitter

St. Kitts Campus Windsor University School of Medicine 1621 Brighton’s Estate, Cayon St. Kitts, West Indies Call: 1.844.994.6376 Email: [email protected]
U.S. Information Office Royal Medical & Technical Consultants Inc. Suite # 303 20646 Abbey Wood Ct. Frankfort, IL 60423 United States Call: 1 708 235 1940 Email: [email protected]
Copyrights © Windsor University School of Medicine 2024. All rights reserved.
- Skip to main menu
- Skip to user menu
How to make a career in medical research?
- Career guides
Starting a career in medical research
If you have the intellectual and emotional resilience, also if you wish to contribute to the body of knowledge in medical sciences then you are a right candidate for a career in Medical Research. Devising and conducting experiments, investigating the epidemiological basis of a disease, working in collaboration with a team, ability to question intricate complexities of genome and proteome and effective written and oral communication skills are the chief qualities of an inborn medical researcher. If the following description sounds like you, then you are probably well suited for a career as a medical researcher.
Qualifications to become a medial researcher
The roadmap to medical researcher is complex because it’s a profession that demands distinctive skills and expertise along with mandatory formal education. The simplest formal degree requirement is minimum Masters or a Ph.D. For an outstanding career as a medical researcher, a Ph.D. will help you to go the distance in an academic career. There is right now an extraordinarily extensive overabundance of post-doctoral partnerships battling for an exceptional set number of lasting scholarly positions. Having said that, accomplishing a PhD in a science subject will stand you in great stead for various research positions. You can pursue a career in medical research by obtaining a formal education in either biological sciences or medicine however; medicine can broaden your options. Furthermore, after earning a formal education in either biology or medicine, the next milestone towards the development of a career in medical research is participating in a research-based internship. In most graduate schools, participating in a research internship and undertaking a research project is the part of the exclusively designed curriculum. This opportunity will allow you to get a chance to be mentored by a physician or research scientist where you can work in collaboration with the team on the ongoing research project.
In order to escalate to the position of the medical researcher, it is integral to complete an advanced degree program in either science or medicine. According to the US Bureau Labor Statistics (BLS), postgraduates and graduates with dual undergraduate degrees become successful candidates for the job positions.
After completing your advanced education, as a medical researcher you can start your aspiring and a challenging career with entry-level positions of medical research associate. As an associate, you are required to assist a scientist in devising, planning and conducting research trials. You can add something extraordinary to your resume by earning credentials offered to research professionals by regulatory bodies. Credential based certifications are not only going to prepare you for some verifiable skills needed in the career but will also aid you in advancing your career path to medical research.
The job role
As a medical researcher, it is your utmost responsibility to conduct research to improve the health status and longevity of the population. The career revolves around clinical investigations to understand human diseases and rigorous lab work. As a medical researcher, formal education will not suffice. As a developing medical researcher, you need to have effective communication, critical thinking, decision-making, data collecting, data analysing and observational skills. These skill sets will enable you to create a competitive edge in the research industry.
Your interest in scientific exploration and a desire to provide a breakthrough in medical knowledge will help you to explore and solve some unknown mysteries associated with complex diseases.
Share this article
Related articles

What does an Engineering Officer (NATO Air Policing) do?

What does a Deputy Director Digital & Chief Information Security Officer do?

The New Scientist 2024 Global Talent Trends and Insights Report in association with SRG: Download your complimentary copy today
Latest articles.

25 Soft Skills for Clinical Research Associates (CRA) and Coordinators (CRC)
- by Kunal Sampat
- June 16, 2019
- in Clinical Operations
As clinical research professionals, we often hear about GCP, HIPAA, compliance, monitoring, Code of Federal Regulations (CFR), so on and so forth.
When trying to secure that next promotion, we often focus on our clinical research skills: the ability to enroll a trial fast, locking that trial database on schedule or passing the FDA audit.
Rarely we take a step back and think about soft skills. Today soft skills are more important than ever. It would be too dangerous to ignore them.
In this post, I’ll share my top 25 favorite soft skills in a clinical research context. You can leverage these soft skills in all areas of your life as well.
So let’s get started:
1. Adaptability to changing requirements
Globalization and harmonization continue to change the clinical research landscape. For example, in the medical device world, the most talked-about changes are the European Medical Device Directive (MDD). There is a lot of buzz on this topic (and complaining too).
Last year I attended a one day roadshow hosted by BSI Group. The presenter asked people to raise their hands if they had read the draft MDD. Less than 5 people in a room of 100+ attendees raised their hands. This goes to show how underprepared the audience was. Very few people had invested the time to understand the proposed changes to the MDD. Yet most of us we anxious about how the change was going to impact our work.
The question you must ask yourself “how will I adapt to these changes?” Change is not limited to government regulations. You’ll experience unanticipated changes in your department, your role, or your project. Take some quiet time to understand change and then adapt.
Change is always hard because it forces us to break our old habits and form new habits.
2. Authenticity and consistent behavior
Being authentic and consistent is hard work.
For example, if you are CRA responsible for on-site monitoring, you probably expect the research coordinator to respond to your emails, answer open queries and complete data entry in a timely manner. When you visit the site, you want the research coordinator to welcome you with a smile.
However, as a CRA, you are equally responsible for authentic and consistent behavior. As CRA you need to show up on time for the monitoring visit, send out monitoring follow-up letters within a few days of your visit (not weeks or months), and answer research coordinator questions with great accuracy and a smile.
Many of us fail to see the other side of the equation, especially when we feel we are in charge of the situation. Being authentic and consistent is hardest when no one is watching us.
3. Coach-ability and the desire to coach others
When I was a CRA, I remember my project manager required our team to cross-train each other. At that time, I thought cross-training was a waste of time. Obviously the project manager wanted team members to be cross-trained, should someone decide to quit their job.
But aside from this obvious reason for coaching others, there are many other benefits. If you take the time to teach someone how to use the excel spreadsheet you’ve created or explained the clinical jargon in the protocol, they’ll always remember you for helping them succeed. This, in turn, creates a lot of goodwill and karma.
4. Collaborative mindset
You may have heard a coworker say, “He is very territorial.” Rather than being afraid of others eating our share of the pie, we must develop an abundance mindset. The more willing you are to collaborate with our fellow colleagues, the more respect you’ll earn. This, in turn, will create opportunities for you and others.
Clinical trials require cross-functional expertise to succeed. Every person involved in the clinical trial has a role to play. Learn to collaborate with an open and curious mind.
5. Conscientiousness in keeping promises
When was the last time you or someone you know, made a promise and couldn’t keep it? I bet you can think of at least one situation in the recent past.
As clinical research professionals, we’re constantly bombarded with requests from sites, sponsors or our management. We generally agree to everything that gets sent our way. It’s hard to say “No”, especially to someone who we wish to please.
But what’s worse is that you get overwhelmed and can’t keep your promises. This leaves a bad impression with the other person.
Before you make your next promise, think about everything you have going on personally and professionally. You can always ask for time to think about the request before making a commitment.
6. Customer service passion
Whether you work at a clinical site, sponsor, clinical research organization (CRO) or the government, providing exceptional customer service to internal and external stakeholders can go a long way in building strong and positive working relationships.
Let’s use CRO-sponsor relationship as an example. The CRO works for the sponsor. It’s expected that the CRO provides excellent customer service to the sponsor. How about the sponsor providing excellent customer service to the CRO as well?
Sponsors can help CROs be successful at their job by documenting clear expectations, addressing areas of ambiguity and being transparent.
When I’m frustrated with customer service, I say to myself, “They are trying to do their very best.” This immediately puts me in a mindset of acceptance and empathy.
7. Eagerness to learn from criticism
Whether you work at an organization or run your own clinical research business, you can’t escape from criticism. There will always be someone who is going to be unhappy with you. Rather than reacting to the criticism, you must welcome it with both hands and learn from it.
Sites criticize sponsors for creating a complex clinical protocols, sponsors criticize regulatory agencies for not accepting their clinical strategy, and a CRO criticizes sponsors for being too demanding at all times.
Spend the time to understand the root cause for such criticism. It might be worth having discussions in a team environment to dissect the cause and how you can learn and improve in the future.
8. Enthusiasm for the work
Yawning is contagious. So is enthusiasm. If you’re enthusiastic for the work, you’ll get others excited too. Your output at work will be much better too.
Bored to read that Standard Operating Procedure? Or don’t want to write that clinical study report? Well, the good news is that everyone experiences dull moments. Enthusiasm is what keeps us going.
9. Ethics even when not under scrutiny
Clinical research and ethics are two sides of the same coin. For example, you don’t want to to take shortcuts by not following procedures. The impact of your decision to take shortcuts can result in a serious audit finding years later.
10. Managing difficult conversations
Difficult conversations can be emotionally exhausting. I remember several difficult conversations I’ve had over the years, particularly with employees who were a misfit for the organization.
If you’re a people manager, you need to learn the art of having difficult conversations with your team. If there are performance concerns, don’t wait till that next annual review. Be proactive and provide ongoing feedback – good and bad. People appreciate knowing where they stand.
11. Motivated to take on new challenges
Sooner or later you’ll be asked to take on new challenges, asked to do things that make you uncomfortable. Some challenges are more direct and others are subtle. For example, if you are a clinical research assistant, you maybe notice that the team needs help with some higher-level work to meet a timeline. Put yourself out there and make it known that you are willing to take on new challenges.
Remember that there may not be any immediate financial benefits to you. However, it is certain that you’ll grow personally and professionally as a result of taking on the new challenge.
12. Self-awareness
If there is one soft skill you must master on this list, it’s self-awareness. As clinical research professionals, we’re constantly interacting with various stakeholders. Before reacting to any situation, you want to be in full control of yourself by being self-aware.
For example, if you are choosing to take a tough stance on an issue, be sure to understand the “why” behind your decision. Don’t be tough for the sake of being tough. Put yourself in the other person’s shoes before you call the shots.
13. Sense of humor
A few years ago, I recollect a conversation between a Clinical Vice President (VP) and a well-respected clinician. The clinician wanted to design a large sample size study. But there was no scientific or statistical reasoning behind the clinician’s proposal. The VP was quick to comment, “I’ve never heard you be so unscientific in all the years we’ve worked together” The VP’s comment broke everyone into laughter, making it easier to have the much harder conversation of reducing the sample size.
Clinical research is a regulated industry. We’re always talking about compliance, patient safety, and good clinical practice. A sense of humor can put you and your colleagues at ease and not take everything so seriously.
14. Diligence and attention to detail
Paying attention to details is exceptionally important. Some people, intentionally or unintentionally, just don’t pay attention to details.
For example, if you are planning an investigator meeting, you need to understand pay attention to meeting logistics and content. Why? Because you’re inviting physicians and research coordinators to spend anywhere between 2-16 hours on your project. If you expect them to the attentive during your presentations, the meeting flow needs to be top-notch with every single detail mapped out.
Another area where attention to detail is necessary is medical writing. Writing clinical reports is not an easy task. Combined that with paying attention to document formatting and grammar can be daunting. If you are not good with formatting documents, learn to master the skill or outsource the work.
15. Facilitation of discussion
We’ve all been through painful meetings. People give boring “updates” on a project or simply digress on the least important topic on the agenda.
Facilitating an effective discussion by asking the right questions will help you a long way. When holding meetings, you need to think about the purpose of your meeting and focus on achieving that purpose. If the purpose is to provide updates, more often than not, it can be achieved through a well-crafted update summary. People can read the summary at a time that works best for them.
16. Listening skills
A few years back, my manager at the time gave four bullet feedback. One of the bullets read, “Talk Less, Listen More.” As humans, we love to talk. But if you can master the art of listening, you’ll start to understand what really matters to the person you are communicating with. Once you know what matters, you can tailor your response to address that person’s question or concern.
We’ve all been on a few teleconference calls where people are talking over each other. Let’s not do that.
17. Managing up
When you land with your first job, no one tells us that you need to learn how to “manage up.” You may be putting in a ton of hours at work. Yet your manager may be disappointed with your performance.
Seldom do managers want to give their employees a hard time. In fact, it’s in the best interest of the manager to keep an employee happy at work. Learning to manage up, gives you the ability to get in sync with your manager.
For example, a site investigator may expect the research coordinator to lead a dozen clinical studies. The coordinator single-handedly can’t possibly manage such a heavy workload without burning out. But the coordinator can track how long it is taking her to perform her tasks. She can share this data with the investigator to discuss potential options to make her workload more manageable.
When you are managing up, don’t be defensive. Instead explain the issue you are facing in a calm and objective manner, backed by real data.
18. Planning for projects
Planning for projects shouldn’t be left to the project manager. Although it’s nice if the project manager did all the project planning for us. As a clinical researcher, you likely have your own projects or deliverables.
For example, a clinical quality manager may be responsible for developing or updating standard operating procedures. She would need to allocate focused time to update procedures, schedule time with other team members to get their input t on the procedure changes, read FDA guidance documents to understand the regulatory landscape and more.
Planning for projects can be boring because you’re tempted to spend that extra time on doing the work itself and planning seems like a huge waste of time. However, when you actually sit down and write your plan on paper, it helps bring clarity to your mind and work.
19. Technology savvy
I love technology. It helps us do our work faster and better. I won’t argue with you if you told me technology also leads to issues that can take a long time to fix. But overall, we are net positive with technology.
As a clinical research industry, we should leverage technology to make research more interesting and engaging. Being tech-savvy doesn’t end once you learn how to use Microsoft Word, Excel, PowerPoint or Electronic Data Capture (EDC) systems.
For example, sponsors can use email software such as Marketo to send out well-designed clinical trial newsletters to research sites rather than sending an email with a PDF attachment that very few people bother to open.
Other ideas include the use of electronic informed consent solutions (eICF), transfer imaging data online rather than via courier services or using social media to recruit patients.
20. Conflict resolution instincts
We’re prone to conflicts because each one of us has a unique worldview. This leads to disagreements. Developing conflict resolution instincts can take years of practice. One strategy I’ve found particularly useful is putting myself in the other person’s shoes.
For example, let’s assume you and your colleague are disagreeing with the clinical protocol design. It would be wise for you to take the time to understand your colleagues’ concerns. Discuss or think through the concerns one-by-one and be creative about mutually resolving disagreements.
Ultimately a few concerns will need to be elevated to senior leadership. But at least you and your colleague would have vetted out most issues before escalating to the next level.
21. Creativity in the face of challenges
It is quite common to face challenges when conducting research.
It’s taking months to negotiate a clinical trial contract, the CRO is not meeting sponsor expectations, patient recruitment is significantly slow and an audit led to major findings are some common challenges.
Rather than reacting to these challenges, it’s important to take a step back and brainstorm all potential solutions to the challenge at hand. In order to come up with creative solutions, you need to have an open and curious mind.
22. Dealing with difficult people
There are many ways to deal with difficult people. You approach will vary depending on whether the difficult person you are dealing with is your subordinate, supervisor or colleague.
My only suggestion when it comes to dealing with difficult individuals is that you conserve your finite amount of energy. If you drain your energy in trying to correct other people, you’ll distract yourself from fulfilling your own dreams and doing work that actually matters.
23. Diplomacy in difficult situations
The author Maya Angelou once said, “I’ve learned that people will forget what you said, people will forget what you did, but people will never forget how you made them feel”.
When you find yourself in difficult situations, don’t say things that will hurt the other person or make them feel bad about themselves.
I also find myself using silence as a way to gather my thoughts before speaking my mind in difficult situations.
24. Storytelling
You may feel that storytelling does not apply to clinical research. But actually, take a minute now to think about any talk or presentation you thoroughly enjoyed. I bet the speaker was harnessing the power of storytelling.
Humans love stories. Therefore the next time you are invited to present at an investigator meeting or a site initiation visit, practice storytelling. Don’t read the slides verbatim because no one will remember you or what you said.
25. Empathy for customers, co-workers, and vendors
Being able to understand the feelings of our customers, coworkers and vendors make us more approachable. People will want to connect with you if you care about them. Showing empathy is not a sign of weakness but rather of strength and maturity.
For example, assume you are a CRA out at a site for a monitoring visit. If the research coordinator is stressed about missing patient records, you can express empathy by acknowledging the coordinator’s efforts in trying to find the missing records. The missing records won’t magically appear. However, the coordinator will recognize the fact that you are able to understand her plight.
We’ve covered 25 foundational soft skills that will serve well in your clinical research career. In order to put these skills to practice, pick just one soft skill and practice it for 30 days. Then see what magic is done for you. At the end of 30-days, spend 30 minutes reflecting what worked well and what didn’t. Then move onto the next skill of your choice. Within a year, you would have mastered 12 soft skills. That’s a lot!
Let me know if which soft skill you’re planning to put into practice next and why? I’d love to hear your thoughts, ideas, and suggestions in the comments sections below.
Clinical Project Management with Antoinette (Torres) Frankum
Ctp 021: getting into research and cro partnerships with jessie coe, 14 thoughts on "25 soft skills for clinical research associates (cra) and coordinators (crc)".
Dr chitrangda
I am about to start my career as a clinical researcher, these points sounds helpful to me. Thank you.
Kunal Sampat
Great, I’m glad to hear.
I am a PhD in oncology. There’s a job opening which asks what relevant skills do you bring with you for CRA role. What should be my response? It should be something exceptional which I cant think of! Please help.
I would suggest that you make a list of ALL the skills you have acquired as part of your education, work or hobbies. Then identify 3-5 top skills that are relevant to the CRA role. Then use examples to demonstrate what makes you exceptional. At the end of the day, soft skills trump technical skills. Both are important but if you’re not able to work with other people, it can be challenging to work in teams. So your response should be a combination of soft skills from this blog post and a few other technical skills you possess. Goodluck!
I have found his quite helpful. I am currently interviewing for a position as a CRA with a background in lab based science (RA). I find myself with at least some ability in all of these soft skills. I hope to find a fit as a CRA and it may help me with my insatiable quest for all things ambitious.
Ridhima Patel
This information is so gonna help who are fresher and want to enter in this field and thanks for that because i am one of them
Hi Kunal, All soft skill you have given in this blog regarding CRC and CRA are very helpful for me, I am M.Pharmacy fresher and I am seeking for CRA profile so your content is like study material for me. Thanks for sharing – Divya Shetty
you are welcome, Divya
Yvonne Gautam
Thanks, a really good and thoughtful overview. I am just moving jobs from one CRC role to another, so have been reviewing how I can improve my performance going forward. I think you pick out 25 very important skills. Your suggestion to practice one soft skill per months is a great idea.
Thank you for this! I just came across this post on a Google search, and even though my career is in a completely different domain, these points are very relevant to any career and are the keys to success. They are the skills that are often lacking in the workplace and are difficult, if not impossible to teach. It’s certainly easier to teach someone how to use Excel than trying to teach enthusiasm or listening skills!
Rutuja Ware
Hey, I’m a final year grad student. Looking forward to exciting opportunities in the clinical research field. I came across your podcast, which seemed very promising. This can help a lot in preparing for interviews in a multifaceted manner. Thank you so much for sharing! Best wishes.
Hello, This is good content to read. Am a clinician aspiring to be a CRA and I will be learning adaptability to new requirements
These soft skills can really make someone a very organised, competent and lovely CRA. I have to start practicing now
I’m glad to hear you’ve started practicing now. According to US Department of Labor, 3 out of 5 skills for Natural Science Managers are soft/ people skills i.e. interpersonal skills, leadership skills, and time management skills.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
- Get new issue alerts Get alerts
- Submit a Manuscript
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Justifying the Need of Developing Research Skills among Medical Students to Strengthen the Practice of Evidence-Based Medicine
Shrivastava, Saurabh RamBihariLal; Shrivastava, Prateek Saurabh 1
Medical Education Unit Coordinator and Member of the Institute Research Council, Department of Community Medicine, Shri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth – Deemed to be University, Ammapettai, Chengalpet District, Tamilnadu, India
1 Department of Community Medicine, Shri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth – Deemed to be University, Ammapettai, Nellikuppam, Chengalpet District, Tamilnadu, India
Address for correspondence: Dr. Saurabh RamBihariLal Shrivastava, MD, FAIMER, PGDHHM, DHRM, FCS, ACME, Professor, Department of Community Medicine, Shri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth (SBV) – Deemed to be University, Thiruporur - Guduvancherry Main Road, Ammapettai, Nellikuppam, Chengalpet District - 603108, Tamil Nadu, India. E-mail: [email protected]
Received April 18, 2021
Received in revised form May 19, 2021
Accepted May 22, 2021
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
Encouragement of research has been recognized as one of the most important reasons for the advancement in the field of medicine and the same stands true for the adoption of curricular innovations in the delivery of medical education. However, there have been significant concerns about the fact that many of the medical doctors are not participating in clinical research or basic research. An extensive search of all materials related to the topic was carried out in the PubMed search engine and a total of eight articles were selected based upon the suitability with the current review objectives. These are ominous signs for the field of medical education and research in medicine and call for an urgent need to expose medical students to the basic skills of performing research at an early stage in their training period. The idea is that students should be informed about the set of research skills which they should develop during their graduation period and the ways in which these research skills will help them in their academic career and professional practice. In conclusion, a medical student has to master multiple research skills during their undergraduation period to ensure effective patient care as well as enhance their contribution in the field of medical research. However, considering the already packed curriculum, it is a must that the research should be integrated within the curriculum in a longitudinal manner throughout the duration of medical training.
Introduction
Encouragement of research has been recognized as one of the most important reasons for the advancement in the field of medicine and the same stands true for the adoption of curricular innovations in the delivery of medical education.[ 1 ] However, there have been significant concerns about the fact that many of the medical doctors are not participating in clinical research or basic research. In fact, regardless of the expansion in basic scientific research, the number of medical doctors participating in research-related activities continue to decline.[ 1 ]
An extensive search of all materials related to the topic was carried out in the PubMed search engine. Relevant research articles focusing on research skills among medical students published in the period 2010-2020 were included in the review. A total of ten studies similar to the current study objectives were identified initially, of which two were excluded due to the unavailability of the complete version of the articles. Overall, eight articles were selected based upon the suitability with the current review objectives and analyzed. Keywords used in the search include research skills, medical students, and undergraduate. The collected information is presented under the following sub-headings, namely Limited focus on research, Research skills and practicing evidence-based medicine, Lessons from the field, and Implications for practice.
Limited Focus on Research
The limited focus on research could be either due to the lack of exposure of medical students to research skills or they are finding it difficult to maintain a balance between conducting research and practicing clinical medicine.[ 1 2 ] Moreover, we cannot also ignore that most of the passed out undergraduate medical students have opted for the postgraduation courses in their selected specialty, while the knowledge and skills required to perform research has been negatively impacted.[ 2 3 ]
These are ominous signs for the field of medical education and research in medicine and call for an urgent need to expose the medical students to basic skills of performing research at an early stage in their training period. The idea is that students should be informed about the set of research skills which they should develop during their graduation period and the ways in which these research skills will help them in their academic career and professional practice.[ 1 2 3 ]
Research Skills and Practicing Evidence-Based Medicine
In general, good medical doctors should acquire research skills and thus there is an immense need to train the medical students with regard to that as an integral part of the curriculum itself.[ 4 ] The first and foremost skill to perform research is to have inquisitiveness and a desire to stay abreast with the recent developments in the field of medicine. A student who has a curiosity to know things will not only be able to prosper in a research career, but will also be able to deliver effective patient care.[ 3 ] It is quite obvious that being inquisitive alone won't be of much use, unless the medical doctor has a strong base of knowledge about their specialty and the research area.[ 4 5 ]
Medical students should also develop critical appraisal skills, which essentially include analysis, critical thinking, and development of new information. These sets of research skills will help the medical students to understand the results of the patient better and give an in-depth understanding about the results of the study findings.[ 3 4 ] The students should also learn the skill to practice evidence-based medicine, which will depend on their ability to acknowledge the role of clinical research and aid them to decide the correct line of management.[ 1 2 ]
As the practice of medicine as well as research is governed by ethics, it is quite essential that the medical students learn about ethics in research and always respect the fundamental principles of ethics.[ 2 3 4 ] Moreover, medical students also need to develop the research skill of ability to work in a team and effectively communicate with the patients, colleagues, and research participants.[ 3 4 5 ] A medical student should develop all these research skills during the course of their training and it is the responsibility of the faculty members to give them adequate number of learning experiences to strengthen their grip on research.[ 3 5 6 ]
Lessons from the Field
At Shri Sathya Sai Medical College and Research Institute, a constituent unit of Sri Balaji Vidyapeeth, Puducherry, a dedicated unit in the name of Institute Research Council has been established. The ultimate aim of the Institute Research Council is to foster, encourage, and support research activities among all the stakeholders (viz., undergraduate medical students, postgraduate medical students, M.Phil scholars, PhD scholars, and faculty members). With regard to developing research skills among medical undergraduate students, a series of initiatives have been taken, namely organizing a 1-day workshop for the students to expose them to research methodology (the workshop deals with right from the selection of topic, review of literature, development of the data collection tool, ethics in research, writing a research protocol, importance of plagiarism, publishing the study, etc.). In addition, during the difficult times of coronavirus disease-19, the Council organized a series of webinar sessions for the 1 st professional year students with an aim to inculcate research skills among students. Further, the undergraduate students are being guided in each and every step of their research proposals by the medical teachers and all efforts are being taken to improve their familiarity with different aspects of research.
In the University of Edinburgh, an integrated model for developing research skills in the undergraduate medical curriculum was implemented. In fact, as a part of the evaluation of the program, feedback from target students was obtained, and it was reported that the integrated model played a significant role in the attainment of the research competencies, which will help them to effectively practice evidence-based medicine in their clinical practice.[ 7 ] In a medical college in Karnataka, mentored student projects were initiated for the undergraduate medical students of 2 nd professional year and the students were extremely benefitted in terms of acquiring research skills.[ 8 ]
Implications for Practice
Training of medical students with regard to research skills is an essential integral component of the undergraduation period. This calls for the need to explore different opportunities for the benefit of students, without compromising the regular teaching–learning activities. As we cannot further stretch the period of undergraduate training, it becomes important to look for avenues within the available timeframe for accomplishing our aim. The exposure of students to research skills can start right from the 1 st professional year during the period of foundation course, especially about the basics of research, types of research, and the importance of research in successful clinical practice.
The period of vacation can be utilized and the students can be motivated to carry out brief research projects. In addition, there is always an option to start an elective course on research methodology and help students to understand the intricacies in research. The Department of Community Medicine of Shri Sathya Sai Medical College and Research Institute has taken an initiative to expose all the medical interns to be a part of brief research projects and drafting of the research findings in the form of a scientific presentation during their posting with the department. Moreover, the students can be encouraged or guided to apply for funded research projects. In fact, the Sri Balaji Vidyapeeth, Puducherry, has taken the lead by rewarding student projects with financial assistance to both the student and the guiding teacher.
A medical student has to master multiple research skills during their undergraduation period to ensure effective patient care as well as enhance their contribution in the field of medical research. However, considering the already-packed curriculum, it is a must that the research should be integrated within the curriculum in a longitudinal manner throughout the duration of medical training.
Financial support and sponsorship
Conflicts of interest.
There are no conflicts of interest.
Evidence-based medicine; medical students; research
- + Favorites
- View in Gallery
Cookies on this website
We use cookies to ensure that we give you the best experience on our website. If you click 'Accept all cookies', we'll assume that you are happy to receive all cookies and you won't see this message again. If you click 'Reject all non-essential cookies', only necessary cookies providing core functionality such as security, network management, and accessibility will be enabled. Click 'Find out more' for information on how to change your cookie settings.

- Accessibility
Introduction to Medical Research: Essential Skills
Our ‘Introduction to Medical Research: Essential Skills’ course provides an overview of key steps and common methods in medical research and its publication.
The course is provided by OUCAGS in collaboration with the EQUATOR Centre , an expert provider in health research education and the Centre for Statistics in Medicine . It is available to Oxford Foundation School doctors free of charge. Other m edical doctors and healthcare professionals working within NHSE - Thames Valley may also apply.
The course is divided into four modules which run over four Saturday mornings during Autumn online via MS Teams:
- Research planning: before you start your research project - this module lays the foundation for getting involved in medical research, from basic research conduct principles through to building the evidence base underpinning a research project
- Research design and protocols - this module introduces the main types of study design and the skills required to critically appraise a research study, and explores the practicalities of writing a protocol
- Statistical thinking - this module introduces the basics of medical statistics, such as understanding sampling, and making inferences from samples to populations
- Research publication and dissemination - this module covers the process of getting your research published in peer-reviewed journals or presented at conferences
To find out when the next courses will be run and be put on the course's mailing list, email [email protected]
© Image copyright Oxford University Images / PS:unlimited -- All rights reserved

Related pages
Our Academic Specialised Foundation Programme (ASFP)
Our Clinical Academic Programmes
The Clinical Academic Pathway
What are the top skills you need to work in clinical research?

Clinical research is the backbone of the life sciences industry . In fact, the established processes used to accurately trial and research medical, surgical and behavioural intervention are essential to its existence. They allow life science businesses to safely push the boundaries of our understanding and formulate better treatments for everything from the common cold to life-changing illnesses and diseases.
The role of clinical researchers has come into the spotlight in recent years. The Covid-19 pandemic required extensive, comprehensive medical research to be executed faster than ever before . As we continue to face threats of this nature, it is clear that the clinical research space will need more ambitious, highly skilled and innovative professionals to help overcome major challenges.
In this article, we explore six of the most sought-after skills in clinical research.
People skills
We start this list with an often-overlooked skill when it comes to conducting clinical trials. Although you may imagine that clinical research trial professionals spend considerable time working in isolation, in fact, they often find themselves interacting with others.
It is crucial that professionals in this space are able to build strong and long-lasting relationships with trial centre staff and colleagues. Clinical trials always require a range of skills and therefore tend to depend on multiple professionals working together to ensure their smooth running.
A clinical trial manager will also often deal directly with the client, making people skills essential to successful communication and securing ongoing funding for essential research.
Critical thinking
The majority of clinical trials require critical thinking. Most challenges and options tend not to be binary – either yes or no - and instead require clinical research professionals to analyse facts, evidence, observations and arguments to form a judgment on the best options to take.
Professionals that gather information and assess situations as a whole will be assets to clinical research teams. Critical thinking is often a skill that employers look for when filling junior roles such as clinical research-associated jobs, as it is something that will pay dividends right from day one. In fact, critical thinking is often cited as a topmost employable skill in almost every industry.
Change management
Life science has always been fast-moving and unpredictable. Yet the advent of Covid-19 made the industry even more aware that the unknown future may require rapid and wide-reaching changes with very little notice. This is why change management is such an essential skill for those in clinical research careers .
Process improvement
Although clinical trials are often comprehensive in nature, there is always room for improvement. In fact, clinical research professionals typically spend considerable time looking to make improvements in everything from reducing the cost and timespan of trials to improving the quality and reliability of results.
Those with a keen eye for identifying areas where improvement can be made will be seen as highly valuable to customers and employers.
Detail orientation
There are few industries where details are as important as in clinical trials. The difference between picking up on potential inaccuracies or not can literally mean life or death. So, there are also few other careers where those who are detail-orientated can have such a positive impact.
Data analysis
Although as a clinical trial professional you will certainly be relying on a wide range of skills such as people management and process improvement , ultimately the majority share of most roles will involve deep data analysis.
Professionals that can correctly gather, work with and analyse data will thrive in the clinical trial space. Other skills that are valuable in this area include knowledge of data models and an understanding of how to use data analytic tools.
Are you looking for your next opportunity within clinical research?
Clinical trials are an exciting space to start or progress your career. Although you will likely need qualifications in order to apply for roles in this space , the skills you need go far beyond simply holding a degree. Those who possess skills such as people skills, a keen eye for data analysis and change management will thrive in clinical research teams.
If you see yourself developing a career in the clinical research space, you can browse our project management jobs , clinical trial jobs , clinical research associate roles and pharmacovigilance and patient safety roles .
Sign up for post alerts
Icon & you the potential of together..
Careers that improve the lives of patients, our clients and each other. Are you ready to make a difference?
Related jobs at ICON
Ireland, Dublin
Full Service - Development & Commercialisation Solutions
Cambridgeshire
Northhamptonshire
Warwickshire
Remote Working
Hybrid: Office/Remote
Business Area
ICON Full Service & Corporate Support
Job Categories
Technical Project Management
Non-Clinical Project Management
Description
ICON plc is a world-leading healthcare intelligence and clinical research organisation. From molecule to medicine, we advance clinical research providing outsourced services to pharmaceutical, biotech
Expiry date

US, Raleigh, NC
Full Service - Medical Affairs & Pharmacovigilance
Clinical Project Management
Title: Project Manager, IDEALocation: Remote (US-Based)At ICON, it’s our people that set us apart. Our diverse teams enable us to become a better partner to our customers and help us to fulfil our mis

UK, Swansea (PRA)
Office Based
Project/ Program Management

Mexico, Mexico City
Full Service - Early Clinical and Bioanalytical Solutions
Mexico City

Related stories
.png)
Teaser label
Content type
Publish date
In today's rapidly evolving job market, especially within the STEM fields, staying competitive requires continuous skill development. As we look forward to 2024, certain skills have become indispensa
Discover the top 5 essential skills to boost your career in 2024, especially for STEM professionals in clinical research.
.png)
Introduction to Clinical Research Management Clinical research management is a complex and multifaceted field that encompasses the planning, execution, and oversight of clinical trials and studies
In this guide we explore the intricacies of clinical research management.
.png)
International Day of Families 2024 ICON plc recently celebrated the International Day of Families on May 15th, creating an event that truly captured the spirit of this day. Working with the SPACE
On May 15th, we recently celebrated the International Day of Families at ICON plc.
Recently viewed jobs

A better career. A better world. A better you.
Browse popular job categories below or search all jobs above
Resume Worded | Resume Skills
Skill profile, medical researcher, improve your resume's success rate by using these medical researcher skills and keywords ..
- Hard Skills and Keywords for your Medical Researcher Resume
- ATS Scan : Compare Your Resume To These Skills
- Sample Resume Templates
- How To Add Skills
- Medical Researcher More Resume Templates
Browse Skills from Similar Jobs
Frequently asked questions.
- 3. Effective Action Verbs for your Resume
Get a Free Resume Review
Looking for keywords for a specific job search for your job title here., © 2024 resume worded. all rights reserved., medical researcher resume keywords and skills (hard skills).
Here are the keywords and skills that appear most frequently on recent Medical Researcher job postings. In other words, these are the most sought after skills by recruiters and hiring managers. Go to Sample Templates ↓ below to see how to include them on your resume. Remember that every job is different. Instead of including all keywords on your resume, identify those that are most relevant to the job you're applying to. Use the free Targeted Resume tool to help with this.
- Clinical Research
- Clinical Trials
- Medical Affairs
- Medical Writing
- Medical Research
- Find out what your resume's missing
- Medical Education
- Molecular Biology
- Life Sciences
- Cell Culture
- Biotechnology
- Polymerase Chain Reaction (PCR)
- Clinical Development
- Pharmacology
- Pharmacovigilance
- Infectious Diseases
- Public Health
Resume Skills: Data Analysis
- GraphPad Prism
- Match your resume to these skills
Resume Skills: Lab Techniques
- Flow Cytometry
- Western Blot
- Western Blotting
- Immunohistochemistry
- Fluorescent Microscopy
Resume Skills: Research Software
Resume skills: clinical trial management.
- Trial Design
- Clinical Monitoring
- Data Monitoring
- Study Protocols
- Safety Reporting
Resume Skills: Regulatory Affairs
- FDA Guidelines
- EMA Submissions
- Drug Safety
Resume Skills: Clinical Research
- Data Collection
- Epidemiology
- Patient Recruitment
- Literature Reviews
- Designing Clinical Trials
Resume Skills: Research Tools
- Medidata Solutions
- Oracle Clinical
- Clinical Conductor
Resume Skills: Programming
- Python (BioPython, Pandas)
- R (Bioconductor)
Resume Skills: Software & Technical Knowledge
- Proficiency in Oracle Clinical
Resume Skills: Regulations & Guidelines
- Knowledgeable in ICH-GCP
- EMA regulations
- and NIH policies
Resume Skills: Biostatistics
- Survival Analysis
- Longitudinal Data Analysis
- Structural Equation Modeling
- Logistic Regression
- Cluster Analysis
Resume Skills: Softwares & Tools
- Electronic Data Capture (EDC)
Resume Skills: Regulatory & Guidelines
- ICH Guidelines
- FDA regulations
- Clinical Trial Protocols
Where on my resume do I add these buzzwords? Add keywords directly into your resume's work experiences , education or projects. Alternatively, you can also include a Skills section where you can list your technical skills in order of your proficiency. Only include these technical skills or keywords into your resume if you actually have experience with them.
Does your resume contain all the right skills? Paste in your resume in the AI Resume Scan ↓ section below and get an instant score.
Compare Your Resume To These Medical Researcher Skills (ATS Scan)
Paste your resume below and our AI will identify which keywords are missing from your resume from the list above (and what you need to include). Including the right keywords will help you get past Applicant Tracking Systems (i.e. resume screeners) which may scan your resume for keywords to see if you're a match for the job.
Sample Medical Researcher Resume Examples: How To Include These Skills
Add keywords directly into your resume's work experiences , education or skills section , like we've shown in the examples below. use the examples below as inspiration..
Where on my resume do I add these buzzwords? Add keywords directly into your resume's work experiences , education or projects. Only include these technical skills or keywords into your resume if you actually have experience with them.
How do I add skills to a Medical Researcher resume?
Go through the Medical Researcher posting you're applying to, and identify hard skills the company is looking for. For example, skills like Clinical Trials, Clinical Research and Medical Research are possible skills. These are skills you should try to include on your resume.
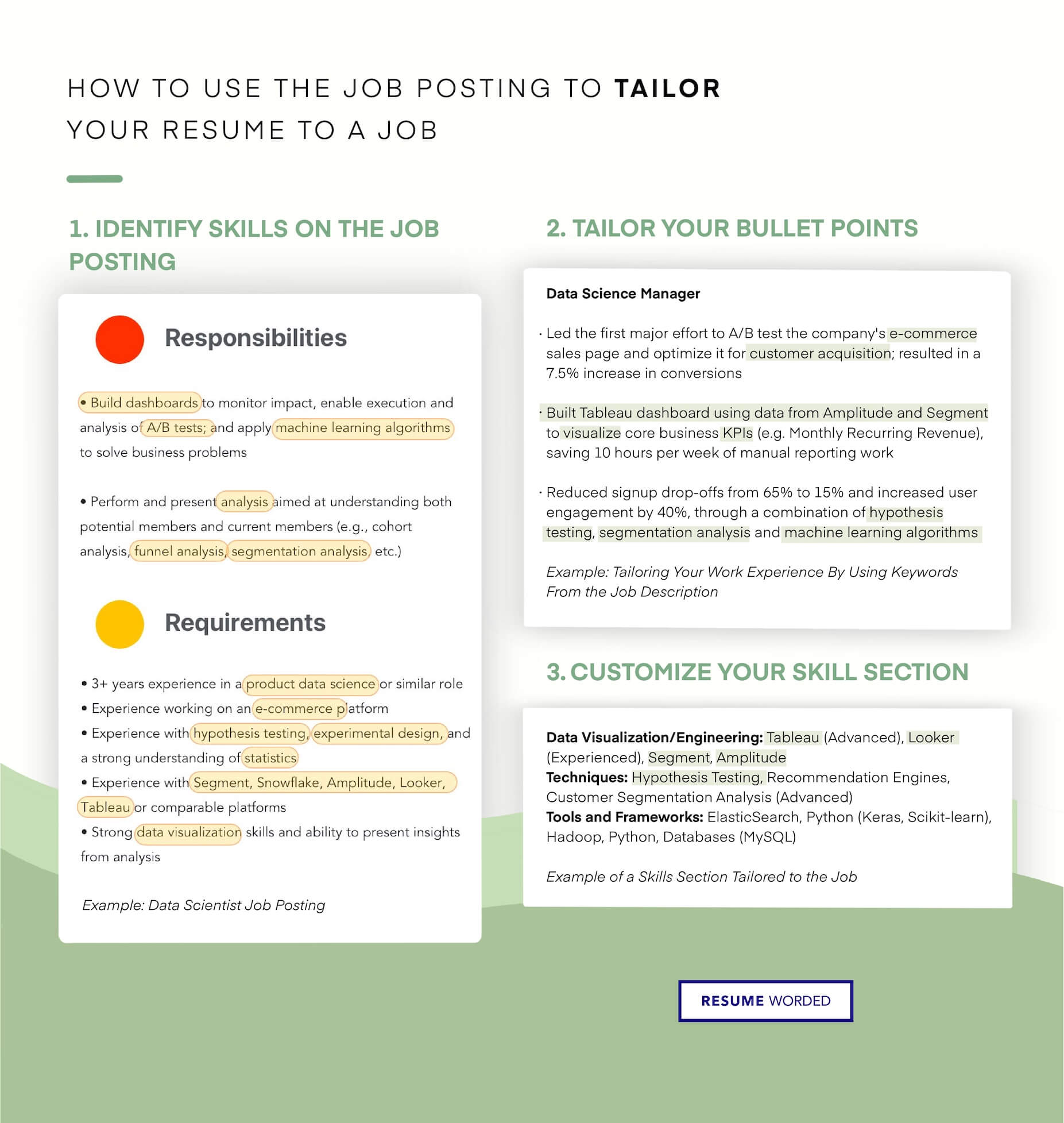
Add other common skills from your industry - such as Oncology, Medical Affairs and Medical Education - into your resume if they're relevant.

Incorporate skills - like Molecular Biology, Healthcare and Infectious Diseases - into your work experience too. This shows hiring managers that you have practical experience with these tools, techniques and skills.
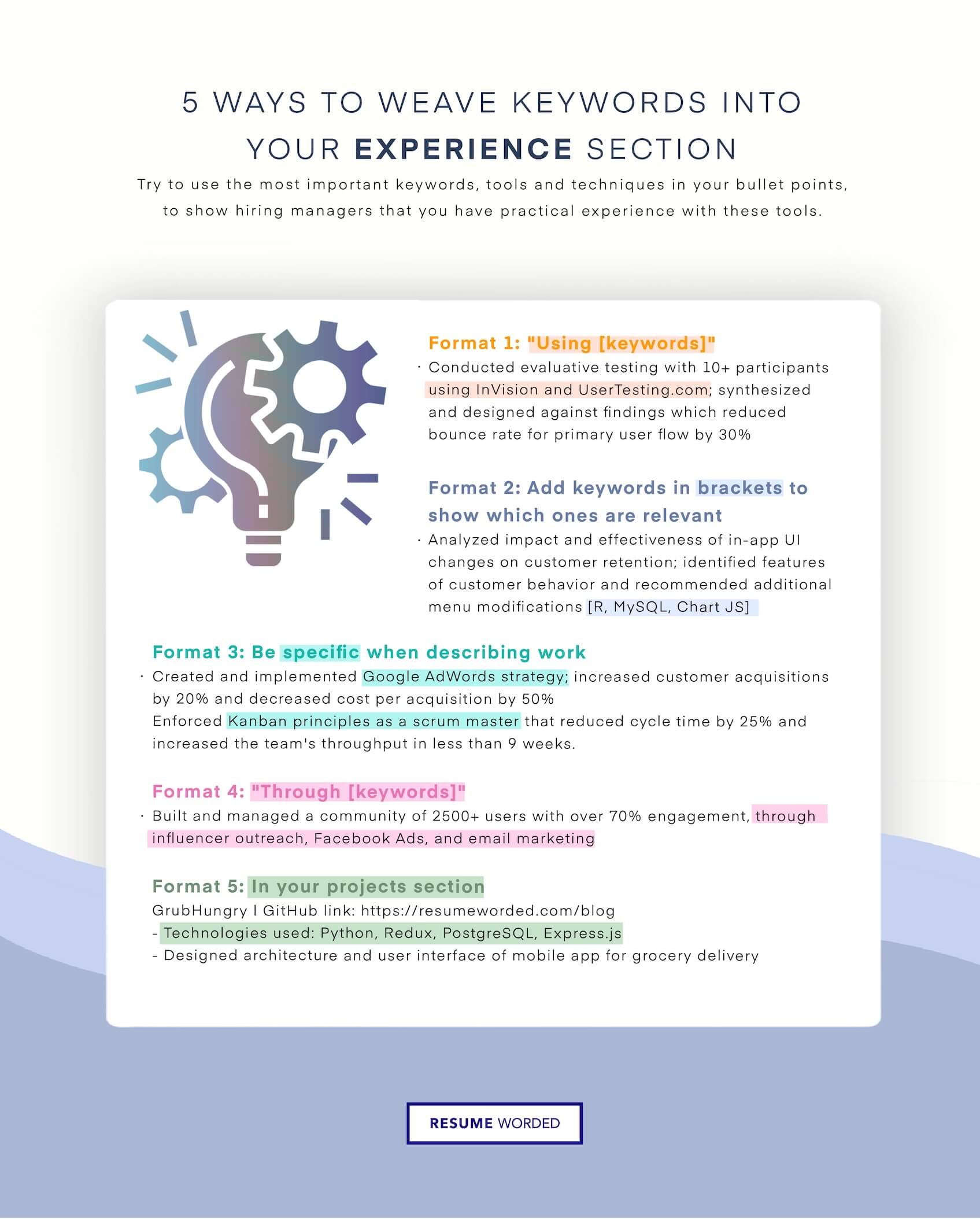
Consider including a section in your resume dedicated to your research experience. On Medical Researcher resumes, hiring managers want to see research projects which you led or where involved with, and their outcomes.
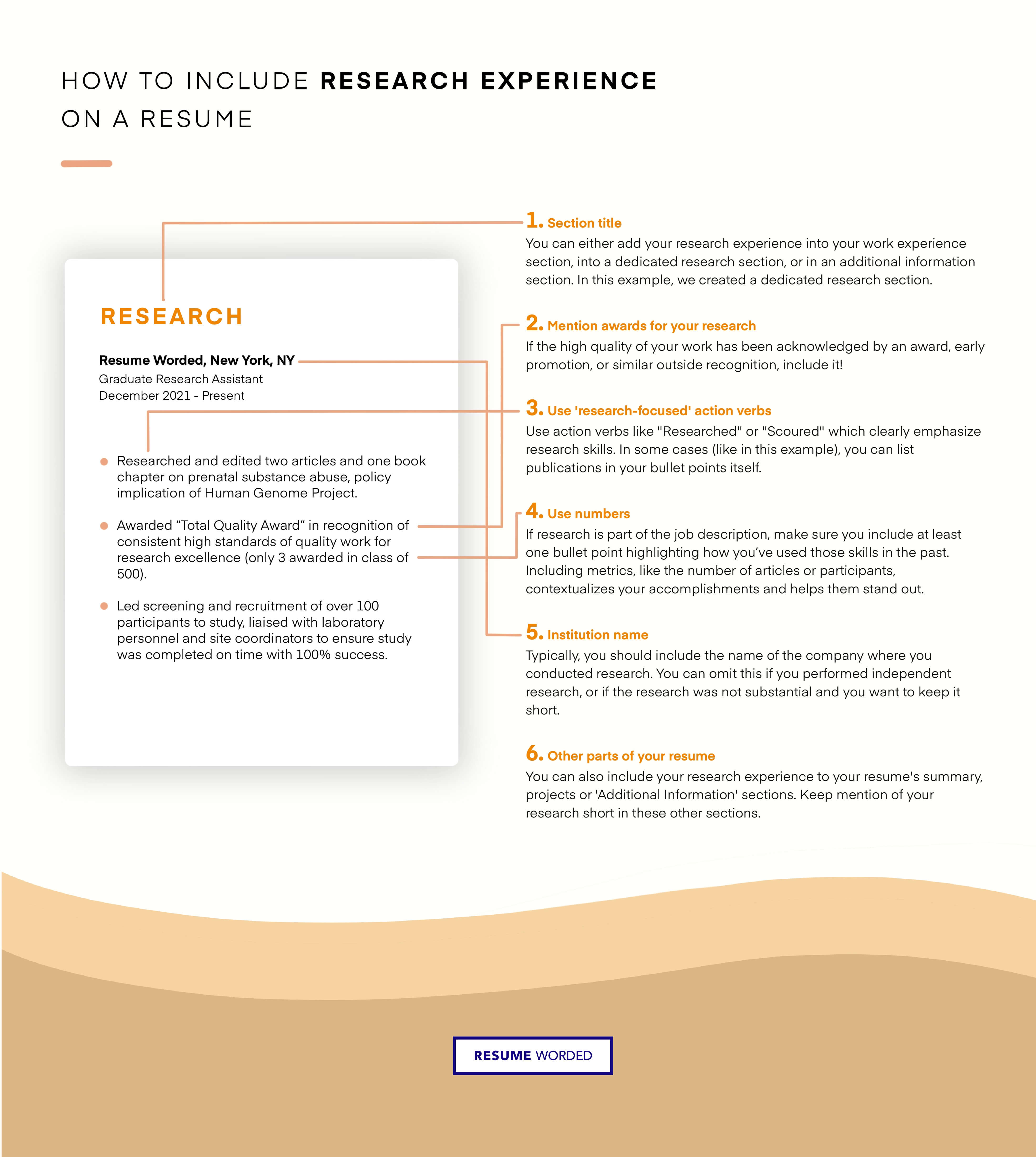
Try to add the exact job title, Medical Researcher, somewhere into your resume to get past resume screeners. See the infographic for how to do this.
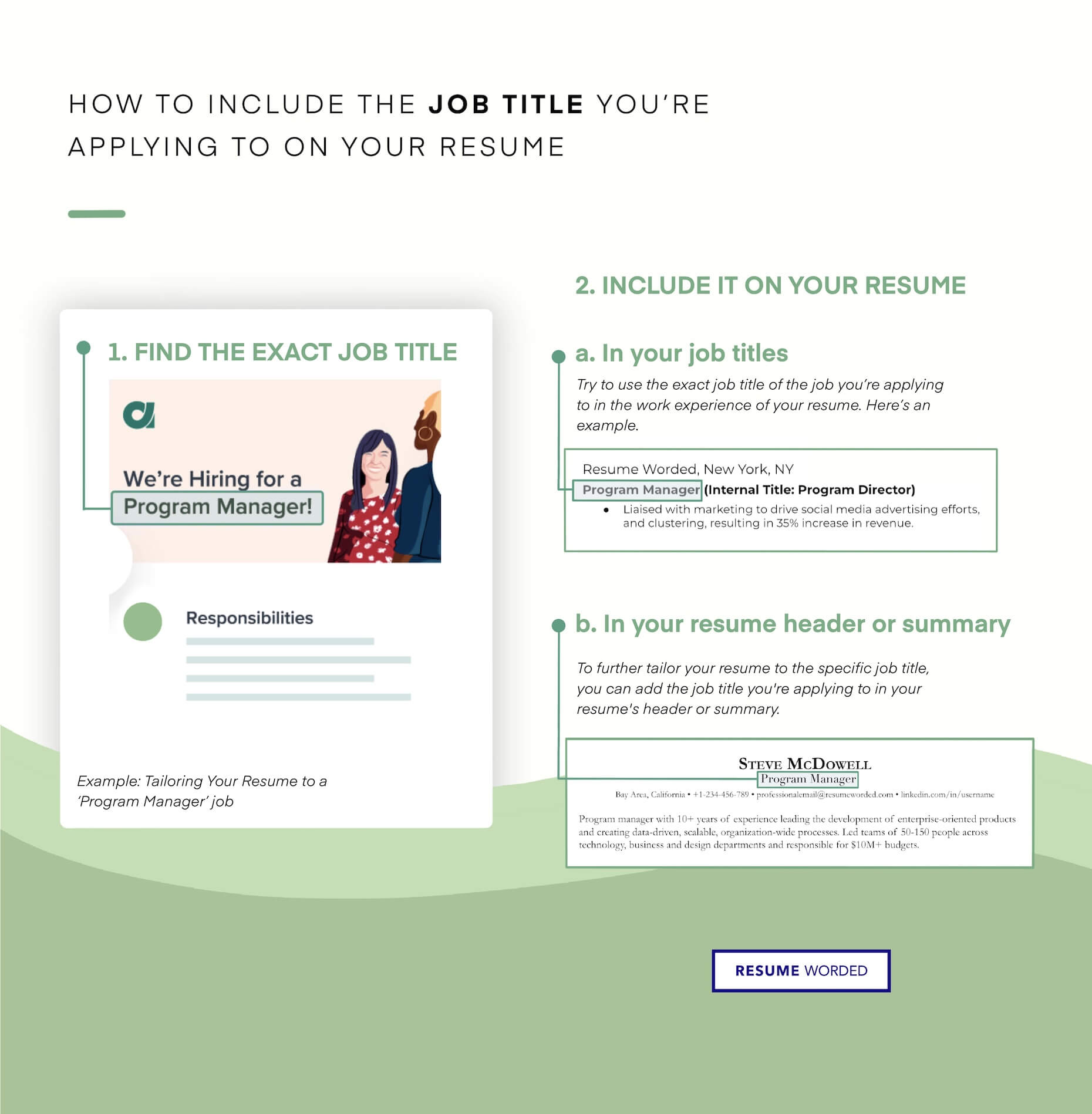
Word Cloud for Medical Researcher Skills & Keywords
The following word cloud highlights the most popular keywords that appear on Medical Researcher job descriptions. The bigger the word, the more frequently it shows up on employer's job postings. If you have experience with these keywords, include them on your resume.

Get your Resume Instantly Checked, For Free
Upload your resume and we'll spot the issues in it before an actual medical researcher recruiter sees it. for free., medical researcher resume templates.
Here are examples of proven resumes in related jobs and industries, approved by experienced hiring managers. Use them as inspiration when you're writing your own resume. You can even download and edit the resume template in Google Docs.
Resume Example Entry Level Medical Coder
An effective Description of the templates...
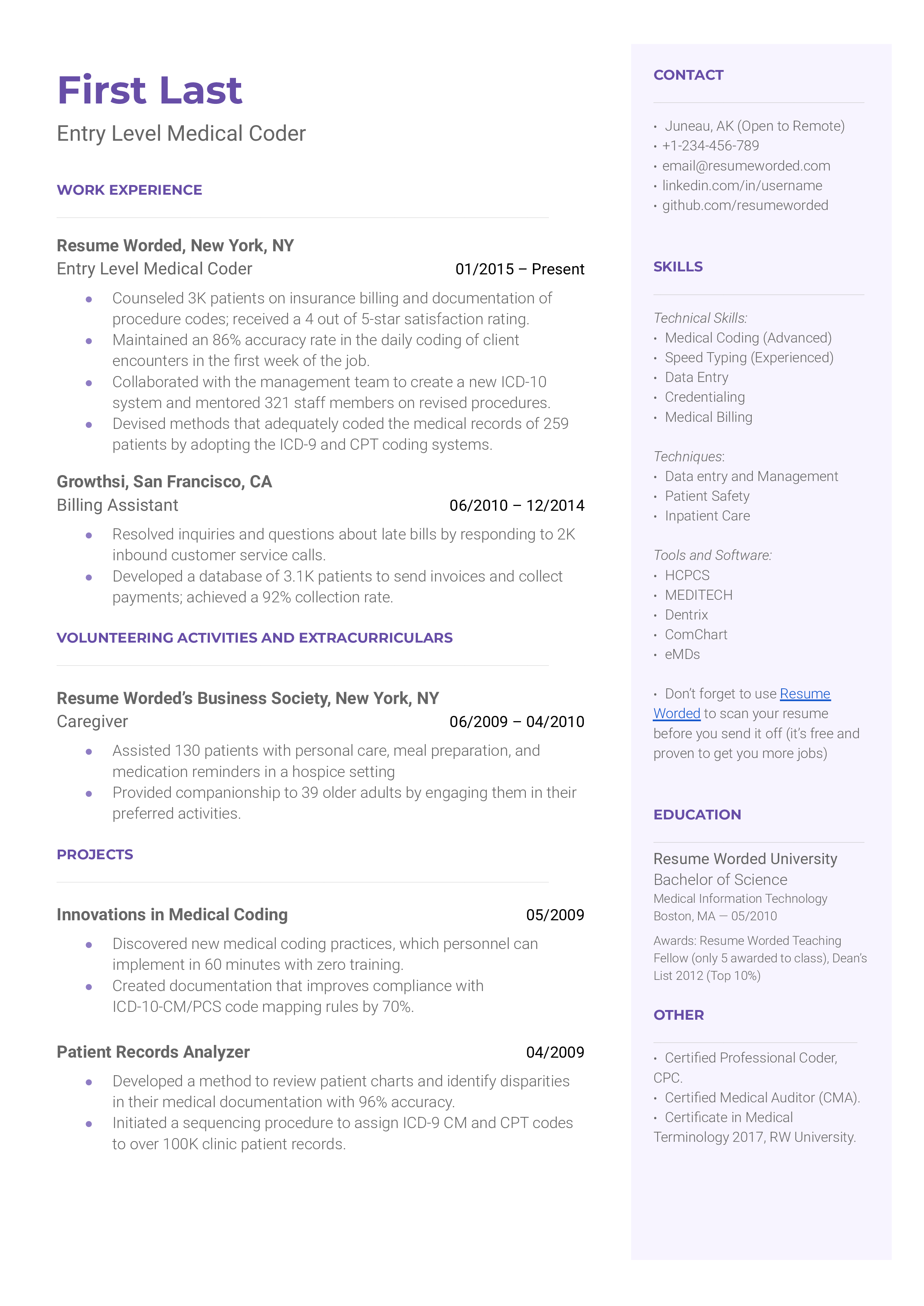
Download this resume template
A medical coder is a healthcare information management professional. An entry level medical coder will work alongside tenured medical coders to ensure patient data is encrypted, secured, and organized. The job of the medical coder revolves around translating sensitive patient data into ambiguous codes for easy storage and simple retrieval. To get a job as an entry level medical coder, a Bachelor’s degree in medical informational technology, computer science, or healthcare administration is ideal. Hiring managers will like to see any relevant research projects, internships, or externships you have completed alongside your education. A part-time job in a healthcare setting, such as a role as a medical billing assistant, can also help you land an entry level medical coder role.
Tips on why this template works
highlight relevant projects that relate to the role of a medical coder.
Being that this is an entry level job, hiring managers will be looking to see if you were engaging in concepts relevant to the position throughout your undergraduate career. A great way to showcase your knowledge in the field is to detail research papers or projects you’ve completed in college. Any project you’ve completed in information technology is valuable, but particularly if the subject matter was specific to medical coding.
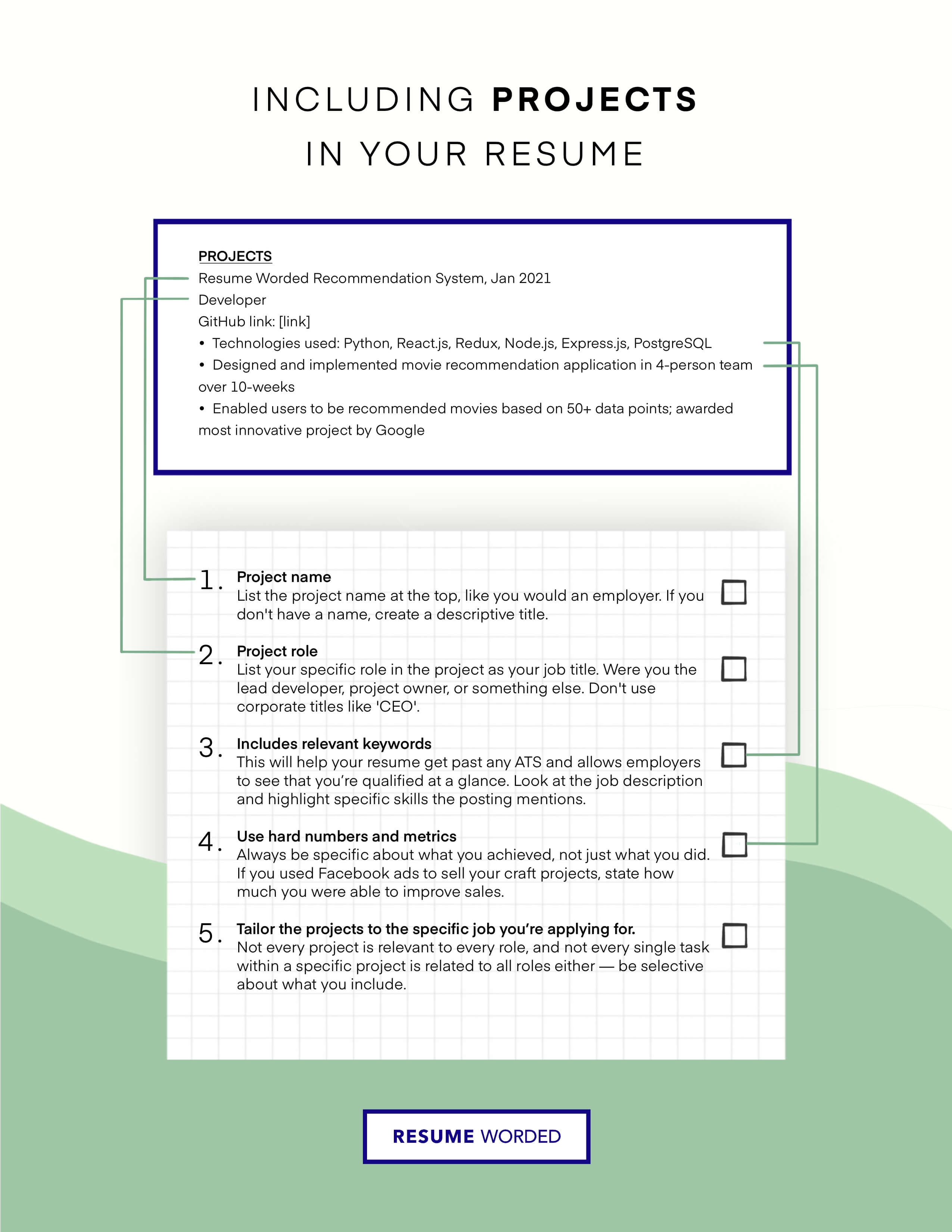
Showcase your knowledge with certificates
Certificates are a great way to enhance an entry level resume. Certifications like the CPC (Certified Professional Coder) and CMA (Certified Medical Auditor) show hiring managers you have specialized knowledge in the field of medical coding and are proficient in the subjects that will make you a great medical coder.
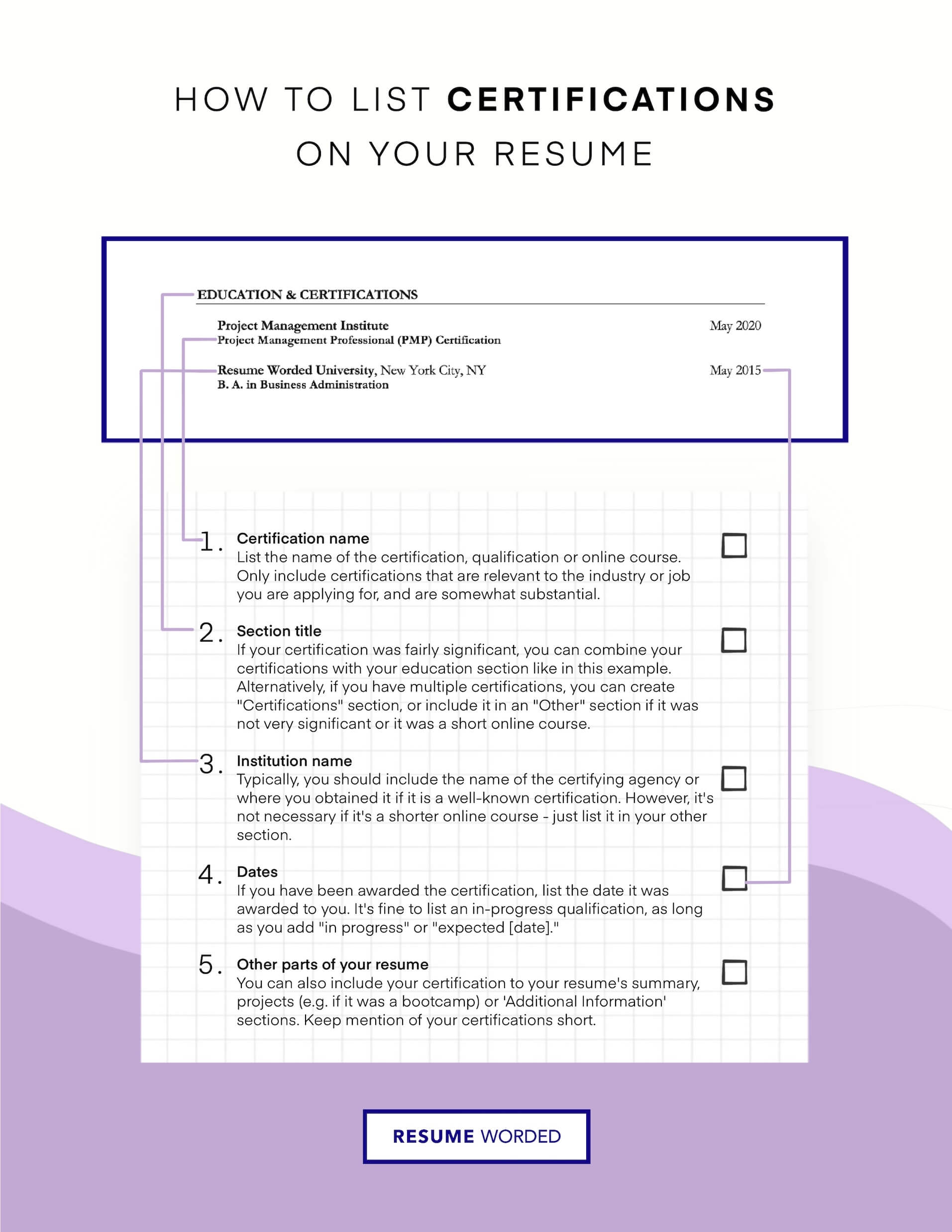
Resume Example Professional

This resume template is suitable for experienced hires or mid-level hires. The education contains two examples of an education experiences, but only include one (your most recent one) if you're a senior level employee.
Makes great use of space
It strikes the right balance between white space and content, and doesn't waste space on unnecessary images and icons. Remember, recruiters aren't looking at how creative you are when it comes to your template. Your content is core and should be the focus.
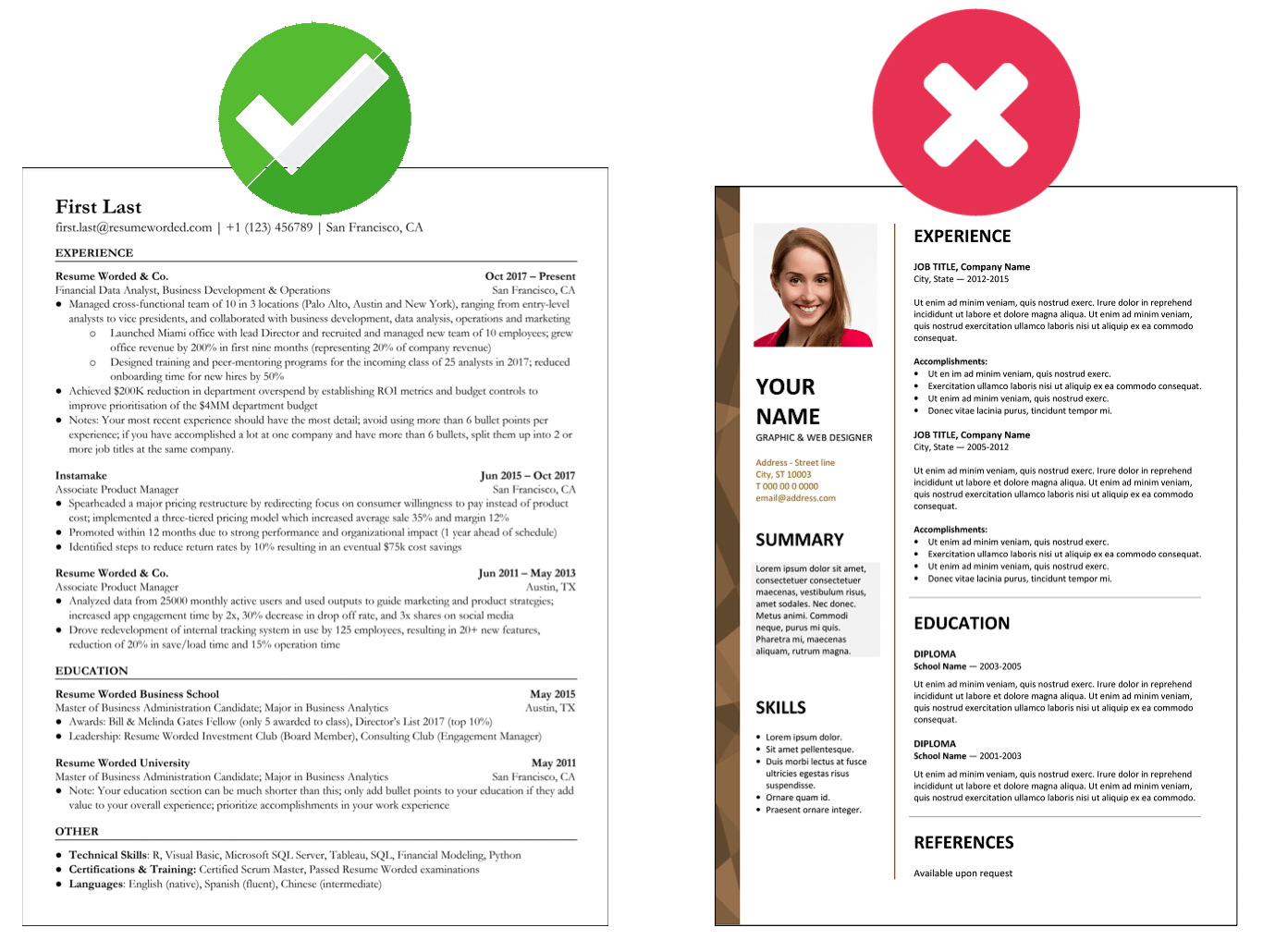
Strong resume bullet points
This job seeker uses resume bullet points that uses strong action verbs, and most importantly, contain numbers that demonstrate the significance of their accomplishments.
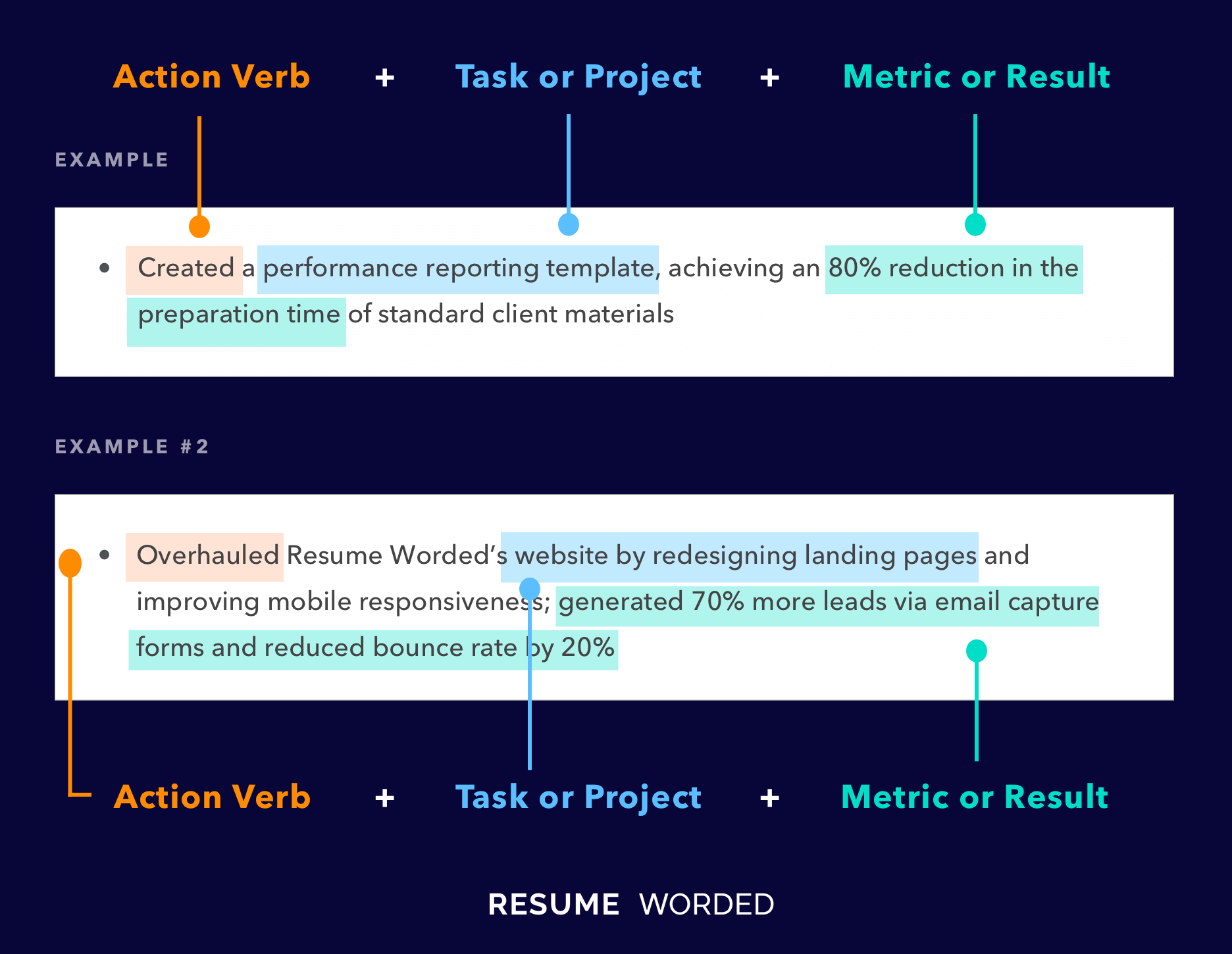
Resume Example Highlights (Free)
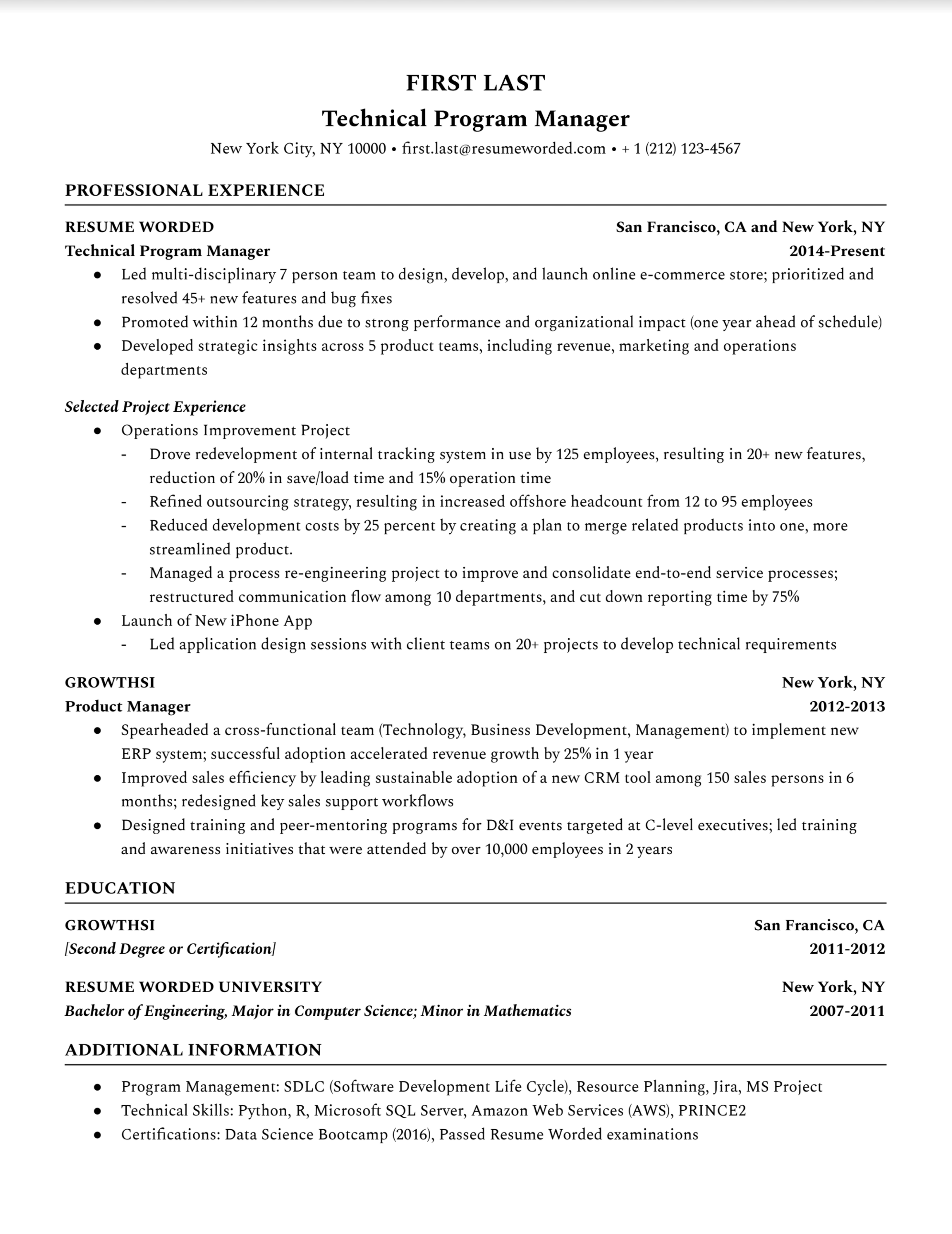
This template is clean, readable by resume screeners, and is effective at calling out key accomplishments and projects from specific work experiences. This would be useful if you have been at a company for a while, or been in a consulting-type of role, and want to point hiring managers to your most impressive accomplishments.
Strong action verbs
Action verbs are important on your resume are vital. They evoke strong imagery to your reader, and this resume does an excellent job by using words such as “spearheaded,” “managed,” and “drove.” These words will help you to put your achievements in perspective, in conjunction with measurable results. Use action verbs relating to the skills you want to highlight.
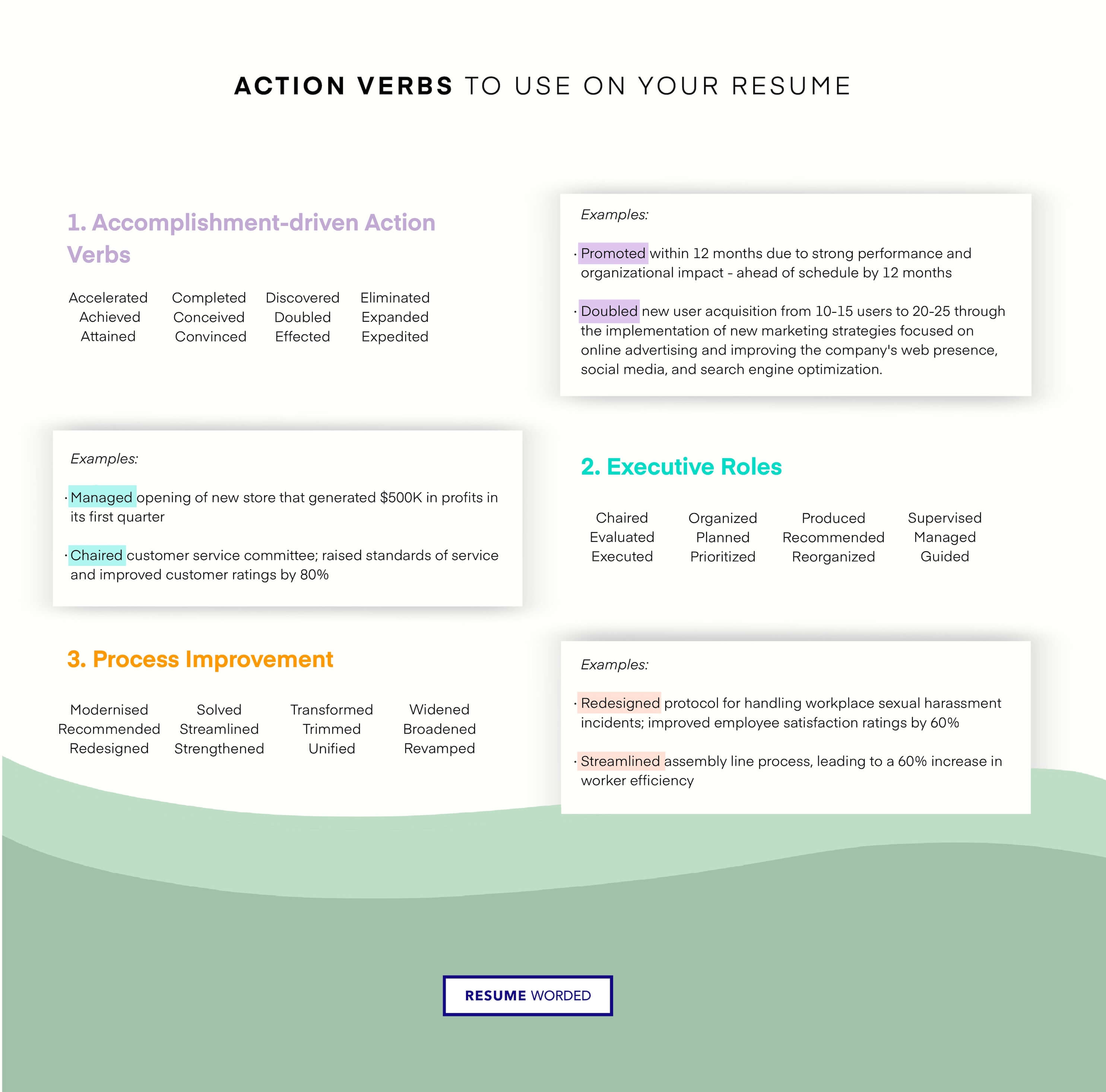
Specific examples of finished projects
Many of your accomplishments will involve your responsibilities in your employer's high-level projects. Recruiters want to see what you’ve completed in previous roles -- such as the Operations Improvement Project and new iPhone app launch highlighted in this resume. The numbers make your experience real, rather than a vague “oversaw several teams for a project.” What did you do specifically? Be specific.
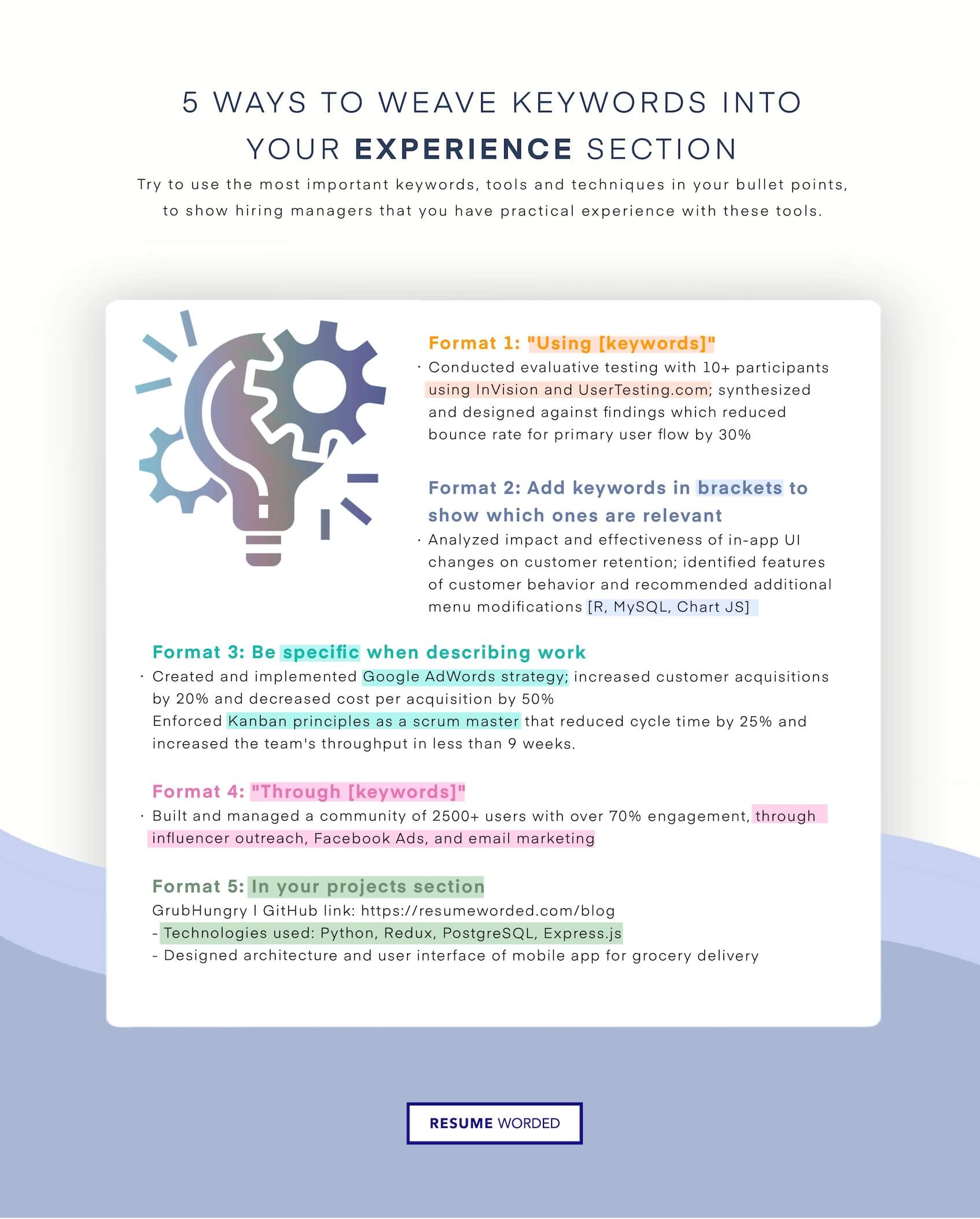
Resume Example Modern Two-Column
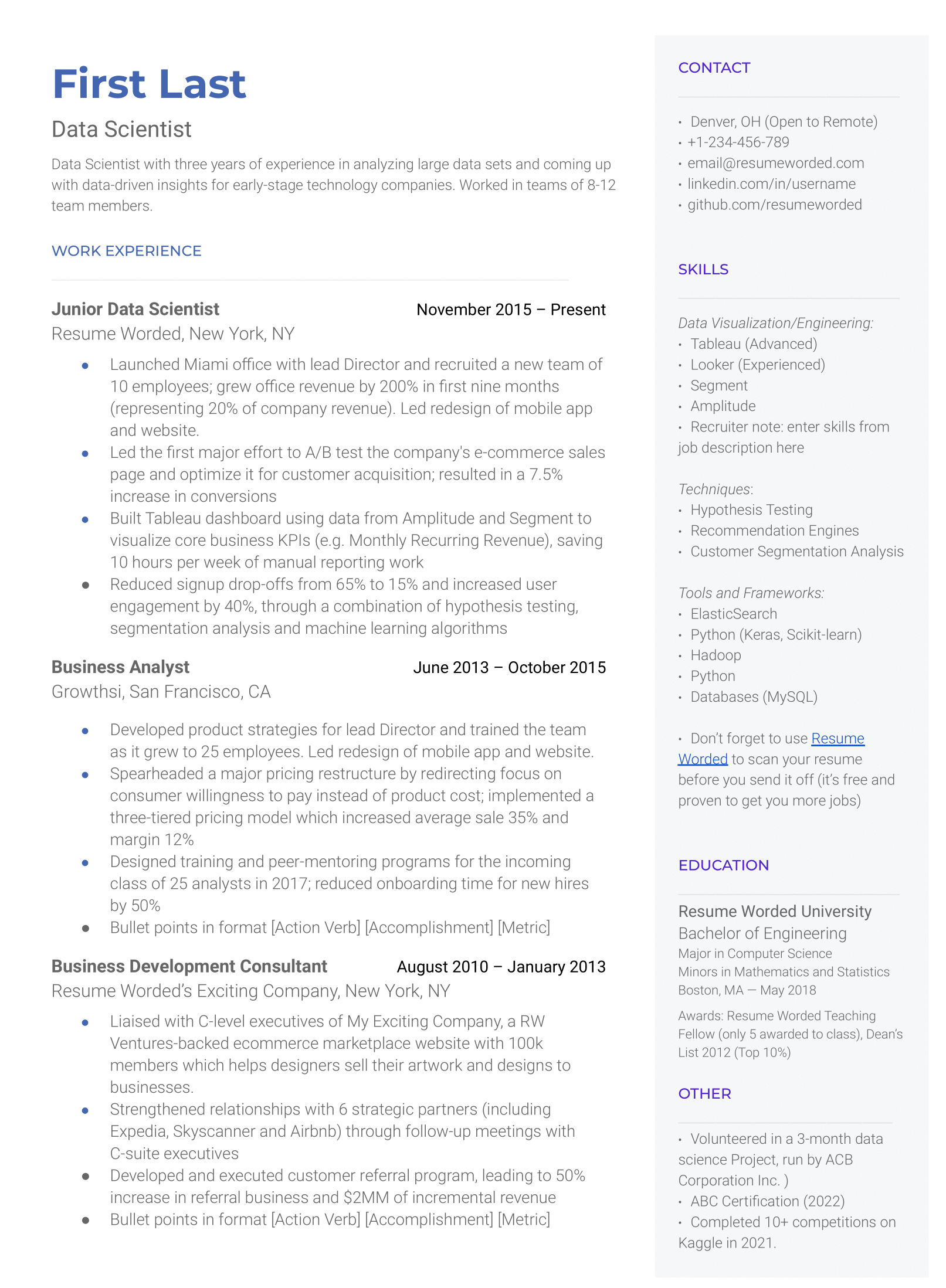
This two column resume template has been designed and created in Google Docs, and puts an emphasis on a skills section. You can download it in Word, or edit it directly in Google Docs.
Prioritize work experience, while including other key sections
The two-column in this Google Docs resume template prioritizes the work experience sections, while maximizing the content into the resume. Not all two column templates are ATS-compatible, but this one is when it is saved as PDF and passed through a resume screener.
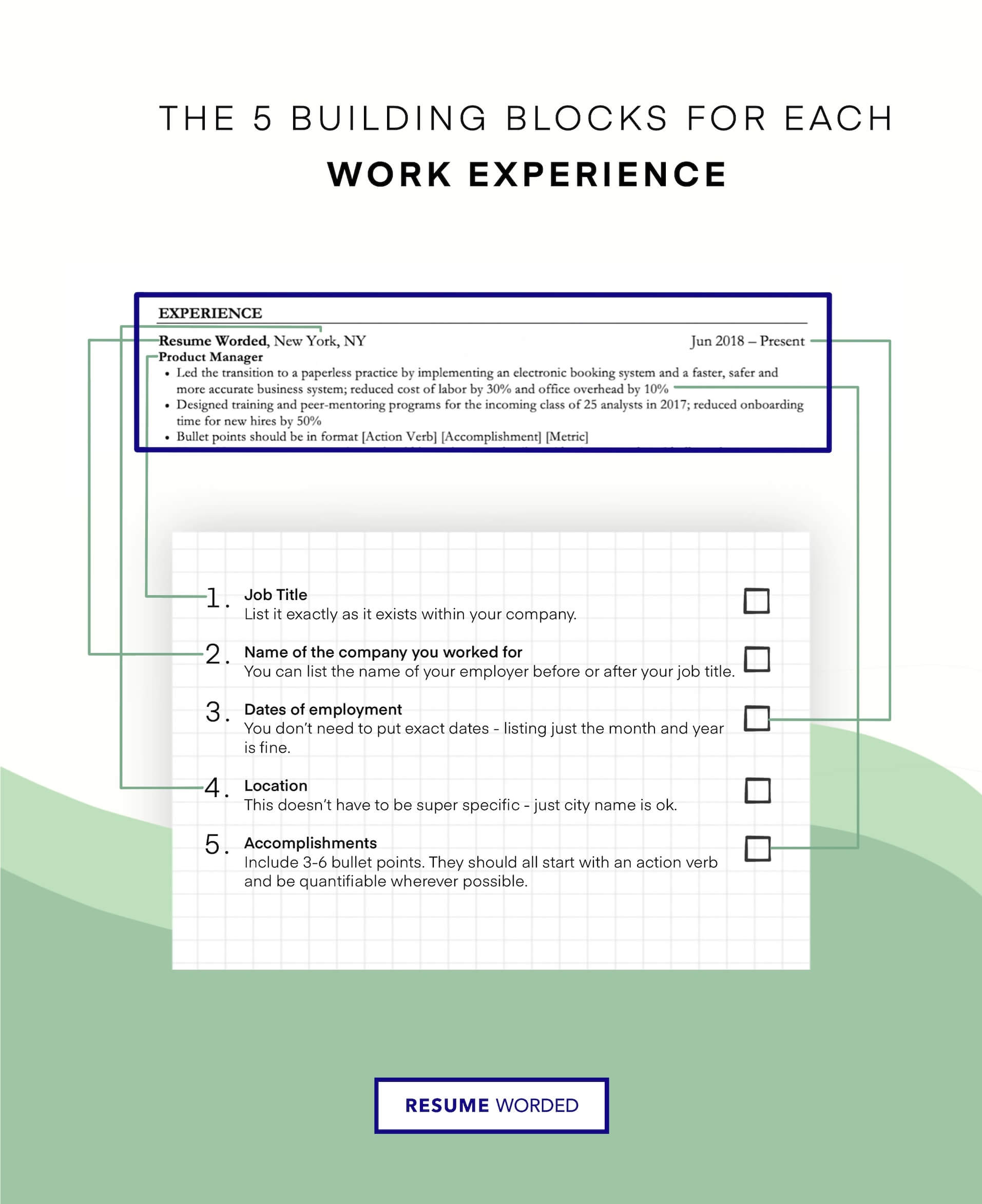
Includes a strong Skills section
Skills sections are a great way to include specific keywords and skills that you have, that haven't been included in other parts of your resume. This helps you get past resume screeners that scan your resume for specific keywords.
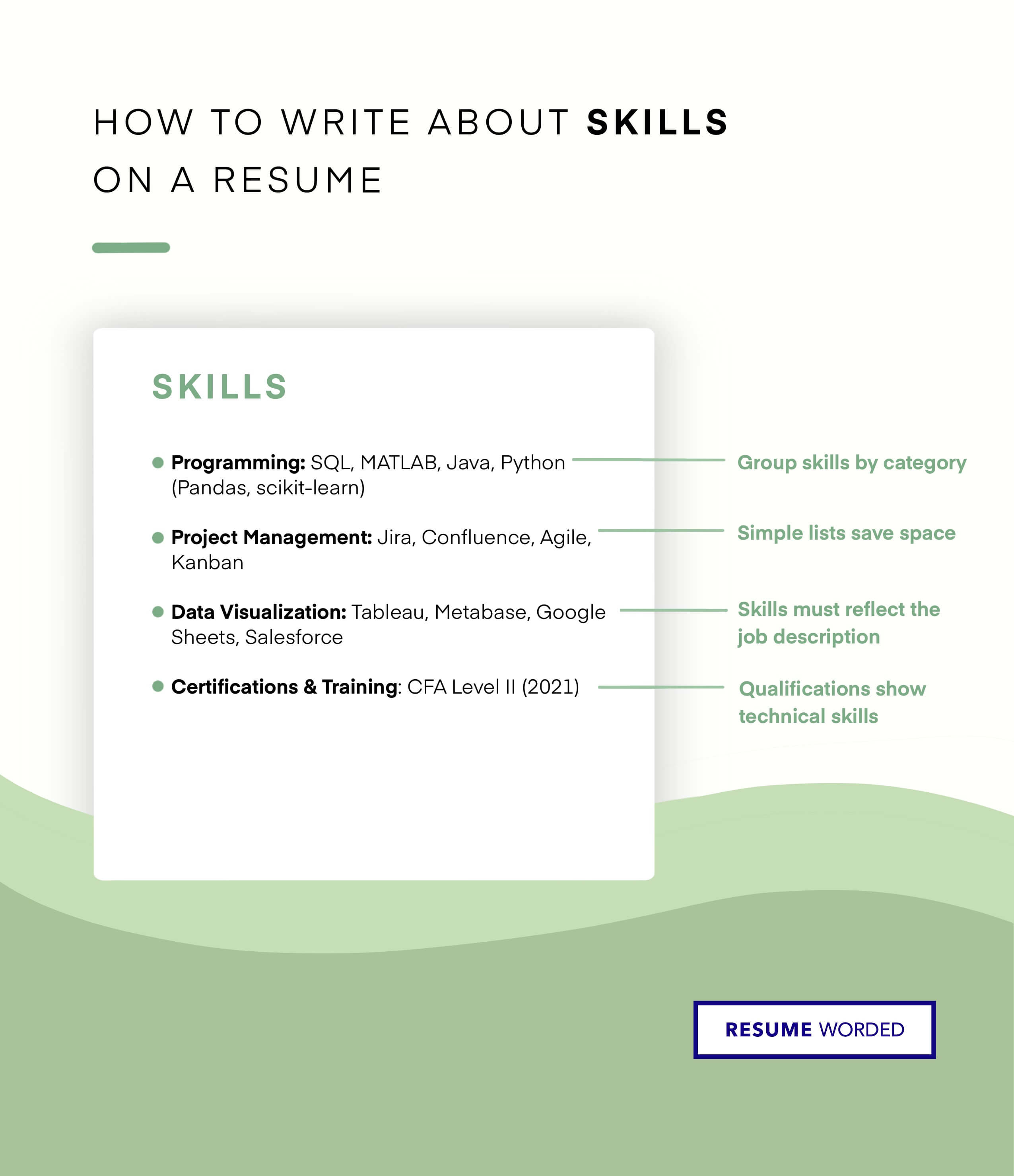
Resume Example Clean Modern
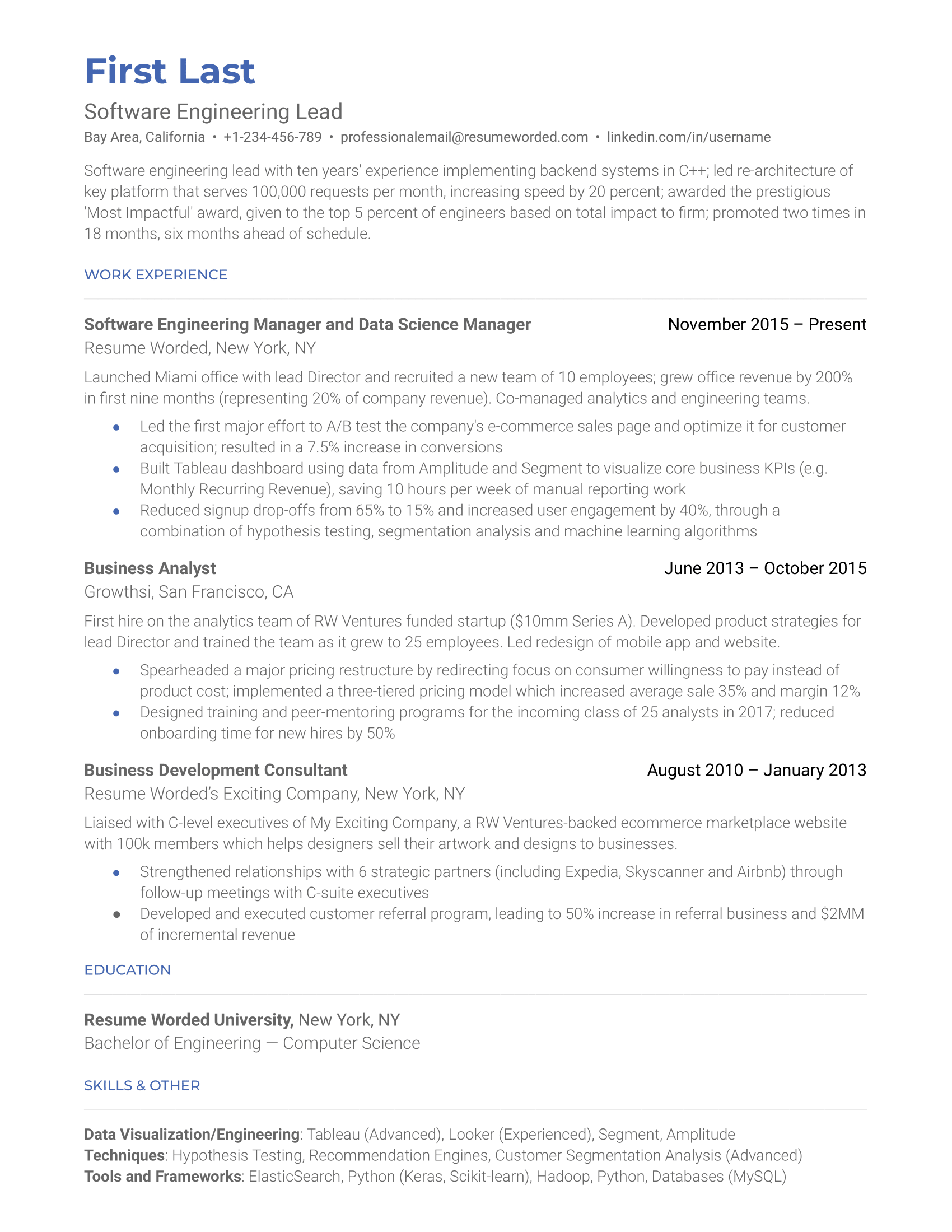
If you're a job seeker with a few years of experience under your belt, use a template like this one. It's simple, effective at highlighting our work experience, and minimizes the emphasis on the education section (the dates are omitted which is good to prevent ageism, especially if you graduated more than 10 years ago).
Professionally-designed template
Minimal templates like this one are exactly what mid-to-senior level recruiters want to see - it shows professionalism, focuses on accomplishments, and makes full use of each page.
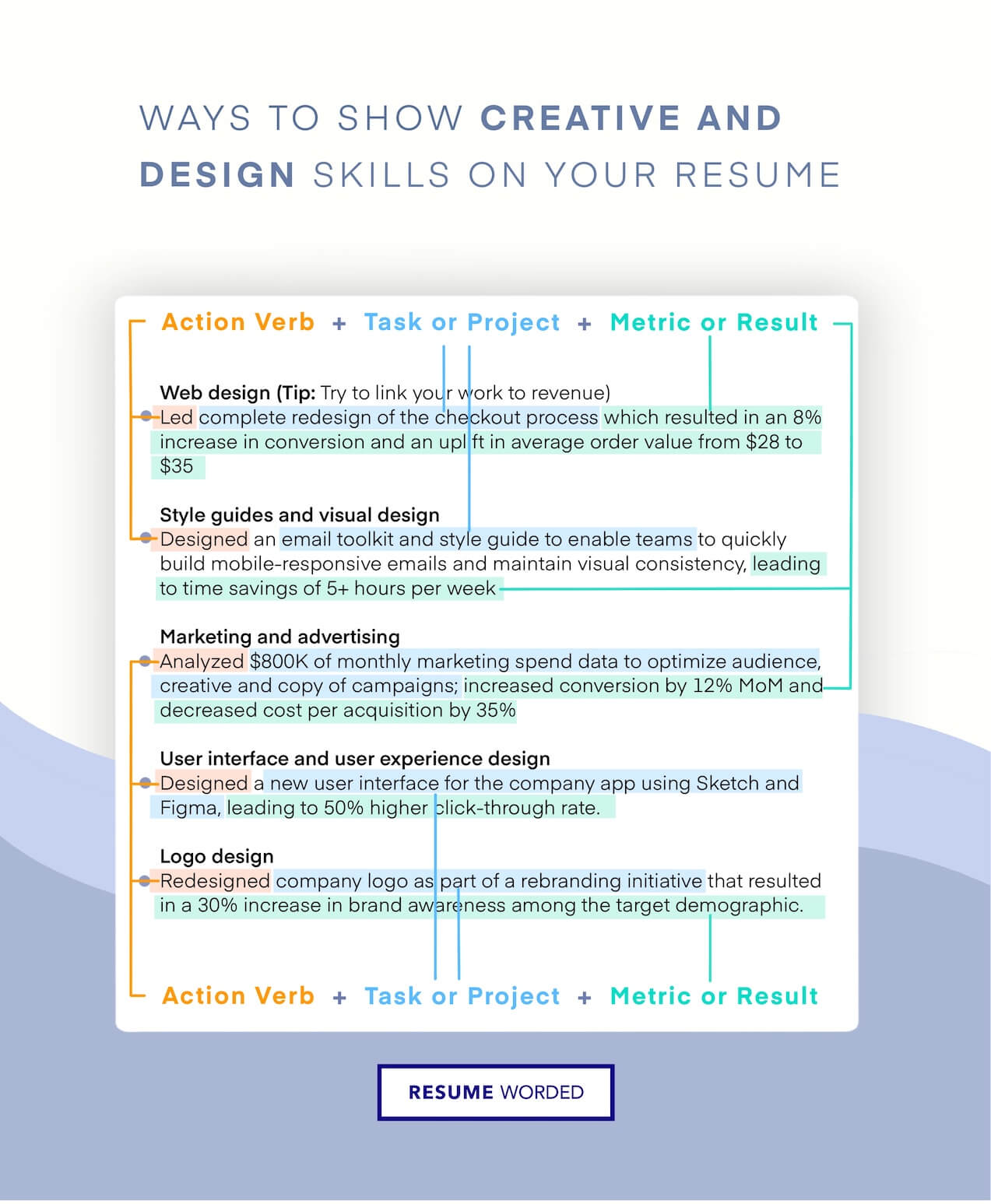
Resume summary highlights key accomplishments
The first rule about including a resume summary is that it does not repeat accomplishments mentioned elsewhere on the resume. This resume stresses new software engineering and leadership skills right at the top of the resume, and includes an award too. If you include a summary, try to include a mix of both technical accomplishments (e.g. projects you developed or led), as well as career-related accomplishments (e.g. being promoted).
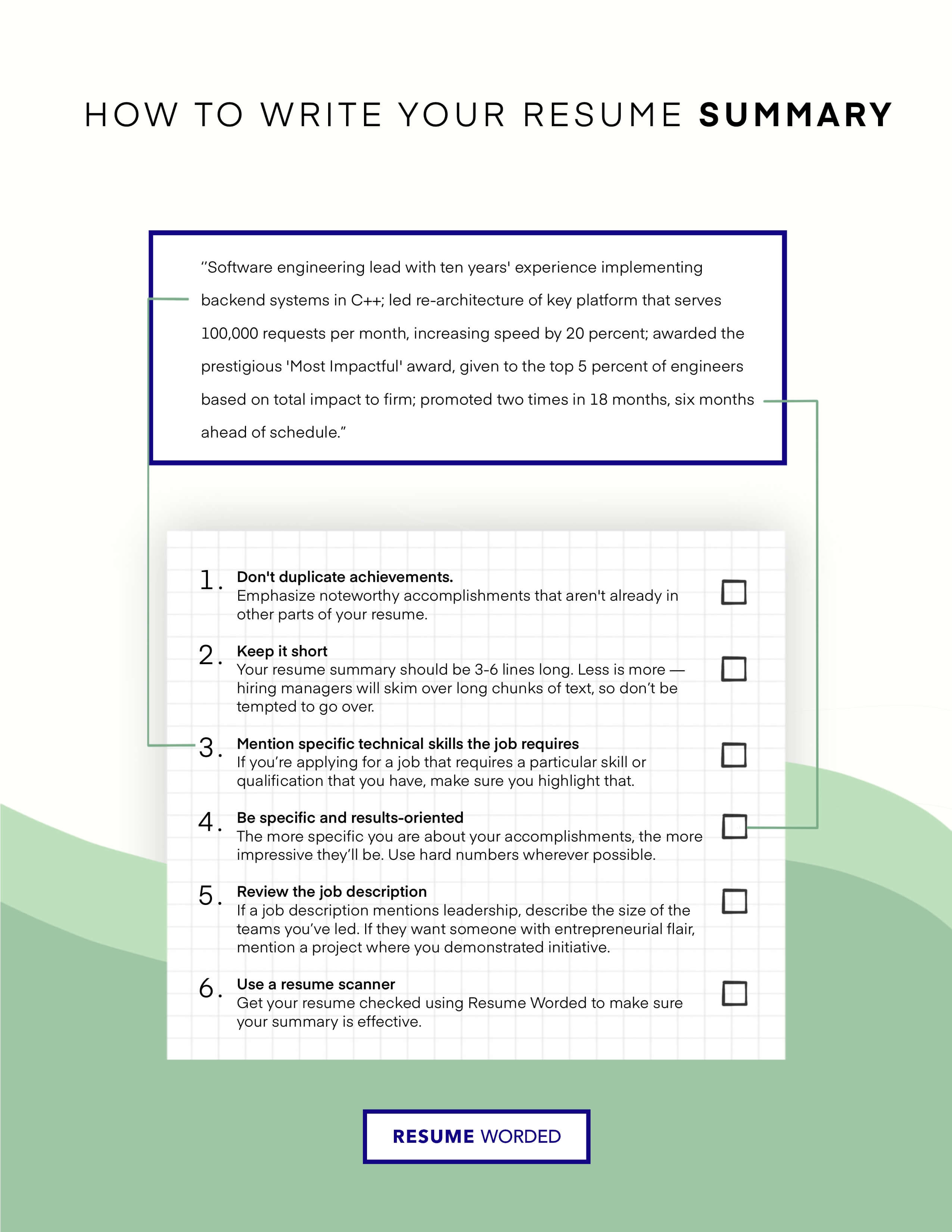
Resume Example Entry-Level (Free)
Use this Google Docs template if you're a student, recent graduate, or a career changer. Right out of college, you may not have much experience in the field. To supplement that, use your experience in clubs and activities, volunteering, projects, and useful coursework to help highlight your knowledge on the subject.
Emphasis on education
If you're an entry-level job seeker that has recently completed education (or in the process of completing a degree), you should prioritize your education and include it first. This Google Docs template does this.
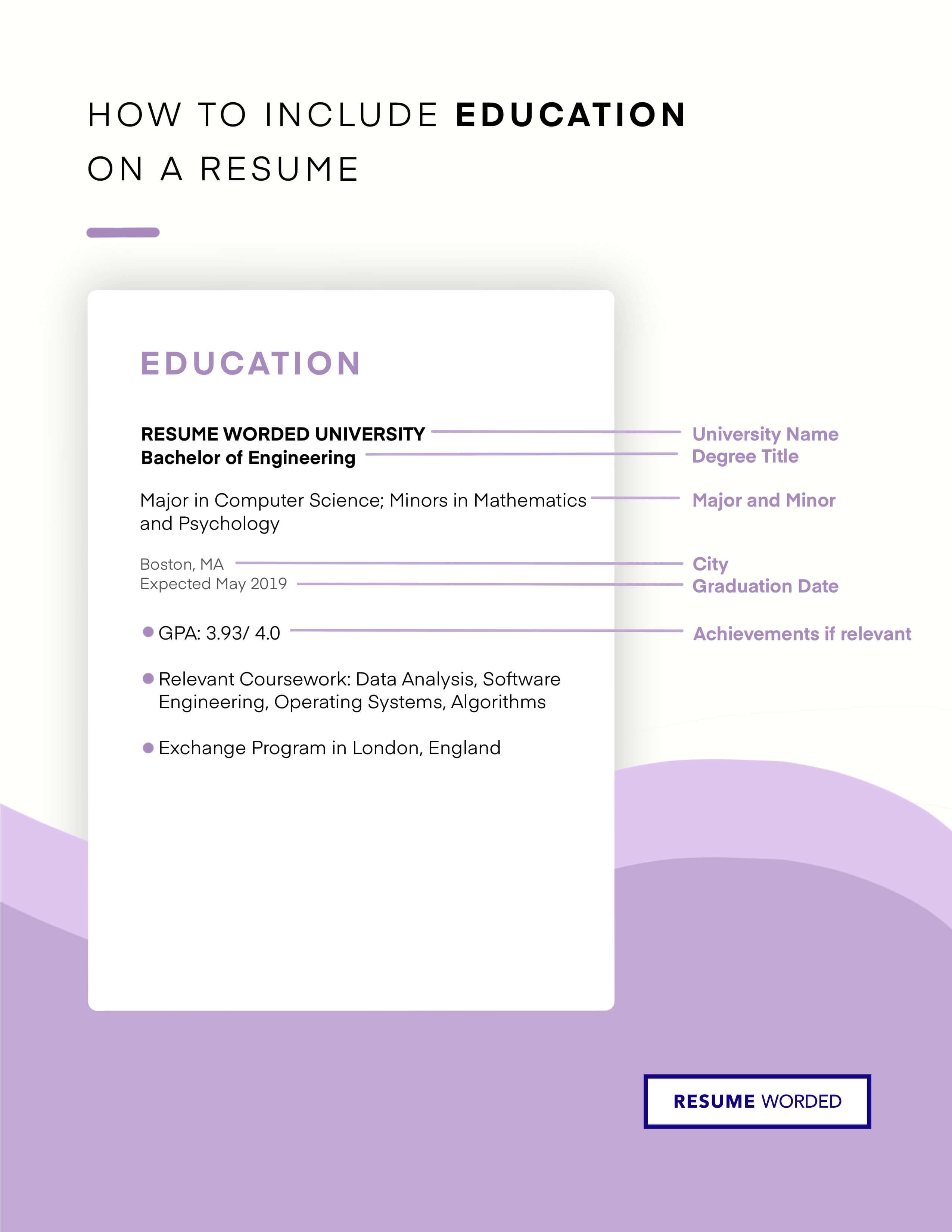
University projects relevant to the job
If you're an entry level job seeker (or a career-changer), you may not have enough work experience to fill up your resume. This is where class projects and university projects come in. This template has a section dedicated to projects, which you can use to talk about volunteering, class projects, or personal projects relevant to the job.
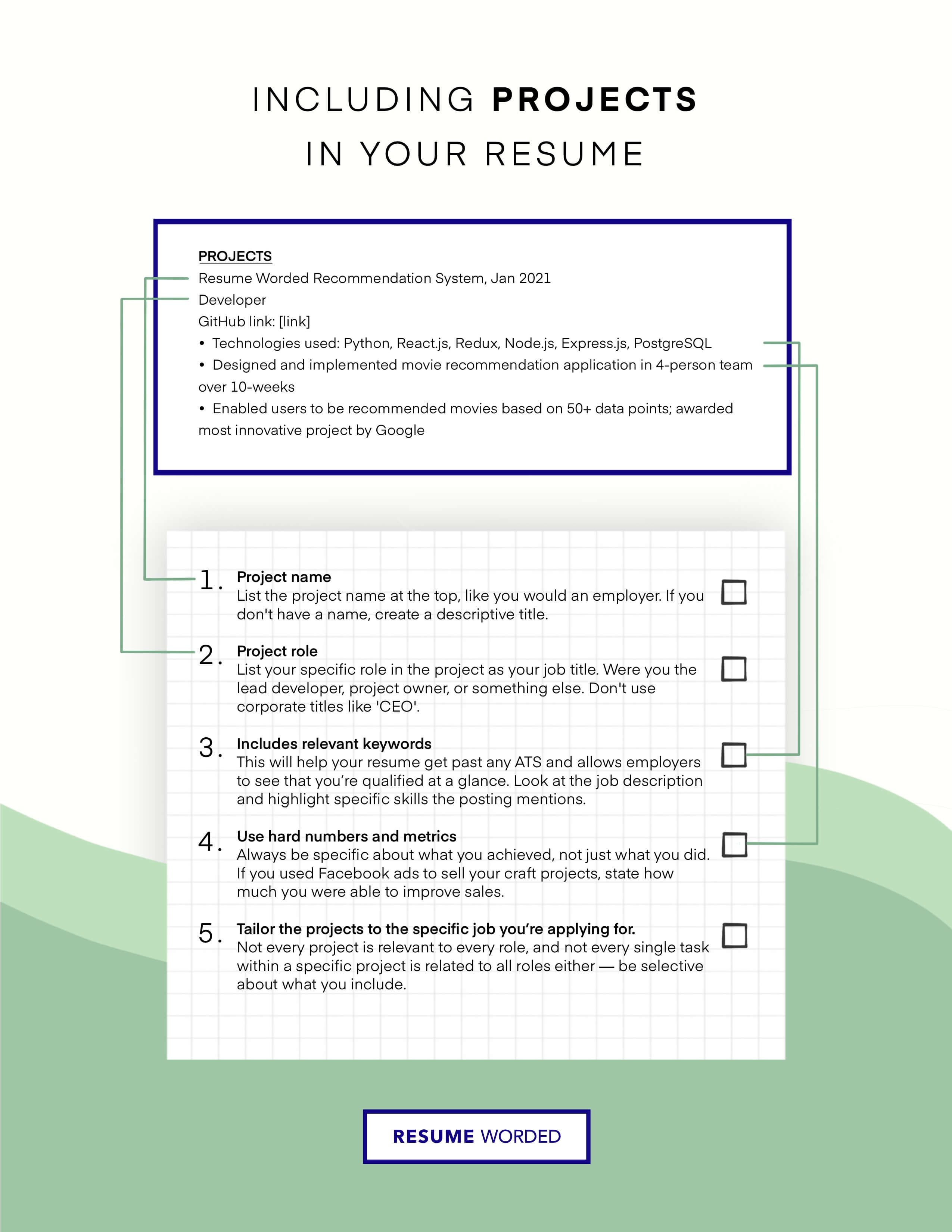
What skills do hiring managers want to see on a Medical Researcher resume?
On top Medical Researcher resumes, skills like Clinical Research, Medicine, Clinical Trials, Oncology, Medical Affairs, Medical Writing, Medical Research and Medical Education appear most often. Depending on the exact role you're applying to, skills like Healthcare, Pharmacovigilance, Infectious Diseases, Pharmacology and Molecular Biology can also be effective keywords to include on your resume.
Target your Resume to a Job Description
While the keywords above are a good indication of what skills you need on your resume, you should try to find additional keywords that are specific to the job. To do this, use the free Targeted Resume tool. It analyzes the job you are applying to and finds the most important keywords you need on your resume. It is personalized to your resume, and is the best way to ensure your resume will pass the automated resume filters. Start targeting your resume
Most resumes get auto-rejected because of small, simple errors. These errors are easy to miss but can be costly in your job search. If you want to make sure your resume is error-free, upload it to Score My Resume for a free resume review. You'll get a score so you know where your resume stands, as well as actionable feedback to improve it. Get a free resume review
Scan your skills and keywords.
Creating an account is free and takes five seconds. you'll get instant access to all skills and keywords, plus be able to score your resume against them - no strings attached., choose an option..
- Have an account? Sign in
E-mail Please enter a valid email address This email address hasn't been signed up yet, or it has already been signed up with Facebook or Google login.
Password Show Your password needs to be between 6 and 50 characters long, and must contain at least 1 letter and 1 number. It looks like your password is incorrect.
Remember me
Forgot your password?
Sign up to get access to Resume Worded's Career Coaching platform in less than 2 minutes
Name Please enter your name correctly
E-mail Remember to use a real email address that you have access to. You will need to confirm your email address before you get access to our features, so please enter it correctly. Please enter a valid email address, or another email address to sign up. We unfortunately can't accept that email domain right now. This email address has already been taken, or you've already signed up via Google or Facebook login. We currently are experiencing a very high server load so Email signup is currently disabled for the next 24 hours. Please sign up with Google or Facebook to continue! We apologize for the inconvenience!
Password Show Your password needs to be between 6 and 50 characters long, and must contain at least 1 letter and 1 number.
Receive resume templates, real resume samples, and updates monthly via email
By continuing, you agree to our Terms and Conditions and Privacy Policy .
Lost your password? Please enter the email address you used when you signed up. We'll send you a link to create a new password.
E-mail This email address either hasn't been signed up yet, or you signed up with Facebook or Google. This email address doesn't look valid.
Back to log-in
Find out what keywords recruiters search for. These keywords will help you beat resume screeners (i.e. the Applicant Tracking System).
get a resume score., find out how effective your resume really is. you'll get access to our confidential resume review tool which will tell you how recruiters see your resume..

Thank you for the checklist! I realized I was making so many mistakes on my resume that I've now fixed. I'm much more confident in my resume now.

Can’t keep your job search organized?
Track all your applications in one place with the Zippia extension for Chrome.
Medical Researcher skills for your resume and career
Medical researchers need a range of technical skills to excel in their field. These include proficiency in statistical analysis, laboratory practices, and conducting clinical research studies. They must also be knowledgeable about medical devices, DNA and RNA analysis, and gene expression techniques like PCR. According to Mario Jimenez Chacon, Assistant Professor at the University of Wisconsin - Green Bay, "a qualified researcher needs to have the hard skills associated with their field, for example, the appropriate certification/degrees or the ability to use technology effectively."
On the other hand, soft skills are equally important for medical researchers. They need to be able to work effectively with patients, maintain accurate records, and collaborate with other professionals in their field. Effective communication is also crucial, as they must present their research findings in a clear and concise manner. As Dr. Jeffrey Hughes, Deputy Director at the University of St Andrews, points out, "cultivating these skills would result in increased earning potential."
15 medical researcher skills for your resume and career
1. patients.
Patients are individuals receiving medical care or treatment. Medical researchers use patients in various ways. They conduct studies on patients to determine factors influencing their conditions, review medical records to select suitable patients for clinical trials, and even recruit patients in clinics. They also communicate with patients to explain policies and procedures, manage their payment details, and ensure they have the correct follow-up appointment dates.
- Conducted a preoperative anxiety study on Hispanic patients to determine what different factors could influence anxiety levels.
- Chart reviewer assessed over 1000 patients' medical records with Parkinson's Disease to select appropriate patients for clinical trial.
2. Statistical Analysis
Statistical analysis is the process of collecting and analyzing data to understand patterns and trends. Medical researchers use statistical analysis to design experiments, identify areas for improvement, and understand the effectiveness of different techniques. They collect and analyze data, and then present their findings to management or stakeholders. For example, a researcher might use statistical analysis to identify key parameters that maximize the optical absorption of airborne particles.
- Designed experiments and conducted statistical analysis
- Collected and performed statistical analysis on data and presented to management in order to identify opportunities to improve finished goods quality.
3. Vital Signs
Vital signs are measurements of the body's basic functions, such as heart rate, blood pressure, and breathing rate. Medical researchers use vital signs to monitor and record patients' conditions. They take these measurements, confirm orders with physicians, and record the data into systems. This information helps them in their research and patient care.
- Call physicians to confirm hand written orders measured patient's vital signs and recorded into appropriate systems.
- Assisted with sterile biopsy's, EKG's, Phlebotomy, Vital signs, Performed Pulmonary Function testing.
4. Laboratory Practices
Laboratory practices involve maintaining records, inventory, and equipment. Medical researchers use these practices to keep track of their laboratory activities. They ensure that their equipment is in good condition and that they have the necessary materials for their research.
- Maintained laboratory equipment records and inventory in keeping with Good Laboratory Practices.
5. Clinical Research Studies
Clinical research studies are investigations that aim to improve human health and quality of life. Medical researchers use these studies to gain insights into various medical conditions and develop new treatments. They conduct these studies, analyze the data, and present their findings. For instance, they might coordinate studies involving older adults with Alzheimer's disease or investigate pain, anxiety, and appearance concerns.
- Assist clinical research studies and programs.
- Worked directly with industry sponsors in initiating and conducting clinical research studies as coordinator and sub-investigator.
6. Research Projects
Research projects involve designing and conducting studies to gather information and answer specific questions. Medical researchers use these projects to advance our understanding of health and disease. They work in teams to design and conduct clinical research projects, manage projects to completion on time and within budget, and initiate and lead research projects on specific topics.
- Worked in a team to design and conduct the clinical research projects in the department.
- Managed research projects to completion on time and within budget.
Choose from 10+ customizable medical researcher resume templates
7. medical research.
Medical research is the study of the prevention, diagnosis, and treatment of diseases. Medical researchers use medical research to provide personalized services to customers, support medical expert witness testimonies, present papers at conferences, and act as consultants. They also participate in clinical trials and assist in creating websites for medical research.
- MetaMed is an innovative start-up that provides personalized medical research to its customers.
- Conducted medical research at Hershey Medical Library to support medical expert witness testimonies.
RNA, or ribonucleic acid, is a molecule that carries genetic information from DNA to the ribosome, which is the site of protein synthesis. Medical researchers use RNA in various ways, such as quantifying and synthesizing complementary DNA from RNA. They also extract RNA using TRIzol reagent and analyze specific interactions between proteins and RNA using biophysical and biochemical methods.
- Experienced in quantifying RNA and protein (BCA method) as well as synthesizing complementary DNA from RNA.
- Extracted RNA and protein using TRIzol reagent.
9. Clinical Trials
Clinical trials are research studies that test new treatments or medications on human subjects. Medical researchers use clinical trials to test the safety and effectiveness of these new treatments. They ensure that ethical procedures are followed, analyze the trial data, and collaborate with other departments to prepare the results for global product launch. They also develop materials for medical professionals and clinical trial participants.
- Ensured that ethical procedures were strictly followed in the course of executing clinical trials.
- Analyzed and translated clinical trial data and collaborated with marketing and regulatory departments to prepare scientific data for global product launch.
10. Stem Cells
Stem cells are cells that can become different cell types in the body. Medical researchers use stem cells in their work by investigating their interactions with other cells and their potential to suppress or affect certain diseases. For example, they might study how human adipose derived stem cells interact with monocytes, or how neural stem cells affect glioblastoma cells.
- Investigated specific interactions between monocytes and human adipose derived stem cells.
- Investigated the tumor suppressive abilities of neural stem cells with glioblastoma cells.
DNA, or deoxyribonucleic acid, is a molecule that carries genetic information. Medical researchers use DNA in various ways, such as extracting and purifying it for analysis, applying molecular techniques like amplification and sequencing, and studying the effects of certain substances on DNA repair pathways. They also use DNA to detect heavy metals and identify anti-cancer properties.
- Gas and liquid Chroma-tography, Western Blot and DNA gels.
- Perform laboratory rtPCR, 454 sequencing, DNA extraction and purification on all of the samples.
12. Chemistry
Chemistry is the study of the properties, composition, and reactions of substances. Medical researchers use chemistry in various ways, such as predicting efficient pathways for organic reactions, analyzing molecular spectra, designing experiments, and optimizing protein production and purification. They also use chemistry to assist in diverse areas of research, like pharmaceutical chemistry.
- Employed computational chemistry tools to predict feasible and efficient pathways for organic reactions and transformations for our collaborators within the department.
- Analyzed spectra of numerous three-component molecules and ions while gaining a deeper understanding of physical chemistry and spectroscopic techniques.
13. Medical Data
Medical data is information that is collected from patient records, medical literature, and clinical trials. Medical researchers use this data to research clients' medical history. They search through computer databases to gather this information, which helps them understand the patient's condition and develop potential treatments.
- Researched clients' medical data on computer database.
14. Medical Devices
Medical devices refer to apparatus for use in medical procedures.
- Conducted market research on products for niche medical manufacturing company that produces medical devices.
- Compiled, analyzed, and graphed clinical results on various medical devices from hospitals, clinics, and centers.
An institutional review board (IRB), is a form of committee that applies research ethics by vetting research procedures to ensure they are ethical. In order to decide whether or not research can be undertaken, they often perform a kind of risk-benefit analysis. The IRB's function is to ensure that adequate safeguards are in place to protect the interests and health of humans who are participants of a research sample.
- Supported IRB applications and analyzed collected data.
- Manage site master file contents and work with sites to ensure communication requirements between site and IRB are adhered to.
5 Medical Researcher Resume Examples
Build a professional medical researcher resume in minutes. Browse through our resume examples to identify the best way to word your resume. Then choose from 5 + resume templates to create your medical researcher resume.
What skills help Medical Researchers find jobs?
Tell us what job you are looking for, we’ll show you what skills employers want. Get Started
List of medical researcher skills to add to your resume

The most important skills for a medical researcher resume and required skills for a medical researcher to have include:
- Statistical Analysis
- Vital Signs
- Laboratory Practices
- Clinical Research Studies
- Research Projects
- Medical Research
- Clinical Trials
- Medical Data
- Medical Devices
- Poster Presentation
- Data Analysis
- Patient Data
- Data Collection
- Research Findings
- Patient Charts
- Test Results
- Market Research
- Complete Research
- Electrophoresis
Updated June 25, 2024
Editorial Staff
The Zippia Research Team has spent countless hours reviewing resumes, job postings, and government data to determine what goes into getting a job in each phase of life. Professional writers and data scientists comprise the Zippia Research Team.
Medical Researcher Related Skills
- Associate Research Scientist Skills
- Associate Scientist Skills
- Doctoral Fellow Skills
- Fellow Skills
- Laboratory Researcher Skills
- Medical Science Liaison Skills
- PHD Researcher Skills
- Postdoctoral Associate Skills
- Postdoctoral Research Associate Skills
- Postdoctoral Scholar Skills
- Principal Scientist Skills
- Research And Development Scientist Skills
- Research Fellow Skills
- Research Laboratory Manager Skills
- Research Scientist Skills
Medical Researcher Related Careers
- Associate Research Scientist
- Associate Scientist
- Doctoral Fellow
- Laboratory Researcher
- Medical Science Liaison
- PHD Researcher
- Postdoctoral Associate
- Postdoctoral Research Associate
- Postdoctoral Scholar
- Principal Scientist
- Research And Development Scientist
- Research Fellow
- Research Laboratory Manager
- Research Scientist
Medical Researcher Related Jobs
- Associate Research Scientist Jobs
- Associate Scientist Jobs
- Doctoral Fellow Jobs
- Fellow Jobs
- Laboratory Researcher Jobs
- Medical Science Liaison Jobs
- PHD Researcher Jobs
- Postdoctoral Associate Jobs
- Postdoctoral Research Associate Jobs
- Postdoctoral Scholar Jobs
- Principal Scientist Jobs
- Research And Development Scientist Jobs
- Research Fellow Jobs
- Research Laboratory Manager Jobs
- Research Scientist Jobs
What Similar Roles Do
- What Does an Associate Research Scientist Do
- What Does an Associate Scientist Do
- What Does a Doctoral Fellow Do
- What Does a Fellow Do
- What Does a Laboratory Researcher Do
- What Does a Medical Science Liaison Do
- What Does an PHD Researcher Do
- What Does a Postdoctoral Associate Do
- What Does a Postdoctoral Research Associate Do
- What Does a Postdoctoral Scholar Do
- What Does a Principal Scientist Do
- What Does a Research And Development Scientist Do
- What Does a Research Fellow Do
- What Does a Research Laboratory Manager Do
- What Does a Research Scientist Do
- Zippia Careers
- Life, Physical, and Social Science Industry
- Medical Researcher
- Medical Researcher Skills
Browse life, physical, and social science jobs
- Open access
- Published: 04 July 2024
The application of blended teaching in medical practical course of clinical skills training
- Zhicheng He 1 ,
- Qiang Wang 1 ,
- Qingming Wu 1 &
- Lili Lu 1
BMC Medical Education volume 24 , Article number: 724 ( 2024 ) Cite this article
148 Accesses
Metrics details
Blended teaching is an effective approach that combines online and offline teaching methods, leading to improved outcomes in medical education compared to traditional offline teaching. In this study, we examined the impact of blended teaching in clinical skills training, a medical practice course.
This study involved forty-eight undergraduate students studying clinical medicine in the fifth semester at Wuhan University of Science and Technology. The students were divided into two groups: the control group, which received traditional offline teaching, and the experimental group, which received hybrid teaching. Following the completion of the 4-month course, both groups underwent the Objective Structured Clinical Examination (OSCE) to evaluate their proficiency in clinical skills. Furthermore, the experimental group was given a separate questionnaire to gauge their feedback on the Blended Teaching approach.
Based on the OSCE scores, the experimental group outperformed the control group significantly ( P <0.05). The questionnaire results indicated that a majority of students (54.2%, 3.71 ± 1.06) believed that blended teaching is superior to traditional offline teaching, and a significant number of students (58.3%, 3.79 ± 1.15) expressed their willingness to adopt blended teaching in other courses. Furthermore, students in the experimental group displayed varying levels of interest in different teaching contents, with emergency medicine (79.2%), internal medicine (70.8%), and surgery (66.7%) being the most popular among them.
Conclusions
This research demonstrates for the first time that blended teaching can achieve a good pedagogical effectiveness in the medical practice course, clinical skills training and practice. Moreover, in different teaching contents, the teaching effects are different. In the content of Emergency Medicine and Surgery, which is more attractive to students, the application of blended teaching could result in a better pedagogical outcome than other contents.
Peer Review reports
Introduction
The education system for clinical medicine students in China primarily follows the “5 + 3” model, with some variations such as the 8-year program. In the “5 + 3” model, students undergo a five-year undergraduate program to get a bachelor degree and then followed by three-year standardized residency training [ 1 ]. Undergraduate education can be divided into three parts: theoretical learning, apprenticeships, and internships. At Wuhan University of Science and Technology (WUST), the undergraduate clinical medical education program follows a unique 2.5 + 2.5 model. In this model, the first 2.5 years are dedicated to studying general courses and basic medical courses at the university. The subsequent 2.5 years are then devoted to completing clinical courses and clinical internships in affiliated hospitals.
In the career of clinical medical students, the acquisition of clinical skills is crucial for demonstrating competence in clinical practice. Before the internship stage, medical students are typically expected to master fundamental clinical skills such as physical examination, cardiopulmonary resuscitation (CPR), major puncture operations, and basic surgical operations. These skills will play an essential role in their future careers. For instance, proficient physical examinations can expedite the treatment process for patients with acute and serious illnesses, as well as guide doctors in conducting other necessary examinations promptly. This not only reduces the financial burden on patients but also improves the allocation of medical resources [ 2 ]. Additionally, regardless of the department they work in, it is imperative for medical students to master CPR and be able to apply it in emergencies [ 3 ]. According to this requirement, WUST has introduced the course “Clinical Skills Training and Practice” in the fifth semester to cultivate students’ basic clinical skills before they enter the affiliated hospitals.
With the rapid development of information technology, the traditional offline medical teaching mode alone is no longer sufficient to meet the evolving needs of medical education in this era. Initially, online medical education was primarily limited to recording and broadcasting courses, often spread through tapes and CDs. This traditional model, however, only catered to basic teaching needs with limited interactivity and feedback. The emergence of internet technologies has paved the way for innovative teaching methods such as online instruction and virtual simulations to gain popularity. These advancements have made teachers more engaging to students and facilitated increased feedback [ 4 , 5 ]. Moreover, the research on the utilization of ChatGPT in medical education reminds us that the evolution of medical education will progress alongside advancements in science and technology [ 6 ]. Changes in educational methods are influenced not only by technological advancements but also by shifts in students’ intrinsic needs. In today’s information-rich environment, traditional teaching methods centered around knowledge transfer alone fall short in meeting students’ requirements. The progress in technology has expanded the possibilities for educational approaches, including the flipped classroom model, project-based learning, and differentiated instruction. These innovations enable educators to focus on enhancing students’ learning experiences, increasing their interest and engagement, catering to their diverse and personalized learning preferences, and ensuring fair and inclusive access to education for a broader audience.
Traditional clinical skills training typically involves a structured presentation by the teacher, followed by the student’s practice under supervision [ 7 ]. However, the COVID-19 pandemic has boosted the development of online courses, such as ‘Clinical Skills Training and Practice’ in WUST. Multiple studies demonstrate that online medical education during this period has yielded unexpected advancements and potential [ 8 , 9 , 10 ]. In the past three years, WUST’s online “Clinical Skills Training and Practice” course has demonstrated promising results in improving pedagogical effectiveness. This prompts us to consider whether blending online education with traditional offline teaching (TOT) could be a better option. Blended teaching (BT), which combines online and offline methods, has been used in medical education since 1990 [ 11 , 12 ]. A meta-analysis comparing BT and TOT in medical education indicates that BT has superior pedagogical effectiveness [ 13 ].
During the transition from being a medical student to becoming a doctor, students need to take medical practice courses to enhance their understanding and application of theoretical knowledge [ 14 ]. Among these courses, clinical skills training is particularly challenging and crucial due to its practical nature. While there has been limited research on the use of BT in clinical skills training.
This study, conducted at the Clinical Skills Training Center of Wuhan University of Science and Technology, aims to investigate the effectiveness of BT in clinical skills training. The participants of this study were undergraduate students majoring in clinical medicine in their fifth semester. The researchers implemented either BT or TOT in their ‘Clinical Skills Training and Practice’ course. The teaching effectiveness was evaluated using Objective Structured Clinical Examination (OSCE) scores and questionnaires. It is hypothesized that students who receive BT will achieve higher OSCE scores and report a more positive teaching experience and effectiveness in the questionnaire.
The study utilized a prospective randomized controlled design and received approval from the Ethics Committee of Wuhan University of Science and Technology (Dossier number 2022151). Sample size was computed with the aim of 0.85 power value, predicated on an effect size of 0.9 and a margin of error set at 0.05. A minimum of 19 participants per group was calculated using PASS 15, resulting in the recruitment of a total of 38 undergraduate students. To address the potential issue of sample dropout during project implementation, the sample size was increased to 48 students. 48 students were recruited based on predefined inclusion criteria from the total 248 third-year undergraduate students from the Department of Clinical Medicine at WUST. The inclusion criteria included: (1) proficient communication and comprehension skills, (2) consistent attendance without absenteeism or truancy, and (3) a positive attitude toward learning. Exclusion criteria comprised: (1) refusal to participate, (2) class absence, (3) failure to complete the final test, and (4) incomplete questionnaire responses. The study emphasized voluntary participation, allowing participants to withdraw at any time without providing a reason. We employed a random digital method to create a set of identification numbers, which were subsequently placed in a box and shuffled. Participants then selected codes from the box to determine their assignment to either the experimental Group A ( n = 24) or the control Group B ( n = 24). The random allocation sequence was generated using IBM SPSS Statistics 27. The study was conducted from September 2022 to December 2022. Prior to the commencement of the study, none of the participants had undergone any clinical skills training.
Study design
According to the WUST clinical medicine cultivation program, the course “Clinical Skills Training and Practice” is conducted in the fifth semester. Both groups of students followed the same syllabus and were taught and assessed by the same teaching team. The objectives of this course include gaining theoretical knowledge of various clinical operations and achieving proficiency in performing CPR, the four major puncture operations (thoracentesis, lumbar, myelopuncture, and peritoneal puncture), physical examination, and basic surgical operations (Disinfect & Draping, Donning & Taking off Surgical Gowns, and Incision & Suturing). All faculty members involved in this course are part of the Department of Clinical Medicine, holding both medical practitioner and teaching certificates, and possessing extensive teaching skills and clinical experience. Offline lessons took place at WUST’s Clinical Skills Training Center. The designated textbook for this course is ‘Clinical Skills Training and Practice’ [ 15 ]. The course consists of 144 periods and lasts approximately 4 months.
Interventions
Group A utilized the online course called “Clinical Skills Training and Practice” available on the University Open Online Courses (UOOC) [ 16 ]. The course is divided into five clinical modules: internal medicine, surgery, gynecology, pediatrics, and emergency medicine. Each module consists of theoretical lecture videos, standardized operation demonstration videos, PPT resources, as well as supporting exercises and tests. The course platform also provides a discussion and exchange board for teachers and students to interact and discuss topics online. The online teaching component constitutes 25% of the total class hours (Fig. 1 ).
Before each offline class, the teacher publishes the teaching content on the platform. Students access the platform using electronic devices and independently learn the relevant material. Through platform data, teachers can monitor and adjust the offline teaching content based on students’ progress. For skills that students have mastered well, teachers will primarily guide students to practice independently during offline teaching. For skills with weak mastery data, teachers will initially emphasize the key points of skill operation and provide demonstrations during offline teaching. The approach of targeting weak areas will be more focused, avoiding redundant explanations of basic content, and offering students more chances for self-practice. Instead of traditional lectures and demonstrations, teachers guide students in practical exercises during offline classes and enhance learning through formative evaluations such as group evaluations and teacher feedback (Fig. 2 ). After the offline classes, students return to the online platform to complete tests and assignments for each chapter, reinforcing their understanding of the acquired skills. If students encounter any difficulties, they can communicate with the teacher through the online course platform’s discussion area, ensuring timely teacher-student communication. Additionally, the course team teachers utilize the discussion area of the online platform to provide high-level clinical thinking training content, such as case analysis, to cater to the individualized learning needs of students at higher levels. The specific teaching process is depicted in Fig. 1 .
Group B students adopt the TOT model, which includes theoretical teaching and demonstration conducted by the teacher (25% of class time) followed by practical exercises by the students (75% of class time) (Fig. 1 ). Additionally, student mutual evaluation and teacher comments are used to conduct formative evaluation of students’ learning effects (Fig. 2 ).
Data collection
After the course, both groups of students underwent offline OSCE assessments at the WUST Clinical Skills Training Center. These assessments were conducted by the same group of examiners. The OSCE assessment consisted of 6 examination stations, namely: physical examination, cardiopulmonary resuscitation, four major puncture operations, donning & taking off surgical gowns, disinfection & draping, and incision & suturing (Fig. 1 ).
We designed a questionnaire for students in Group A who adopted BT. We used Alpha to calculate intra-group consistency and reliability. The alpha value of the BT questionnaire in Group A is 0.941, indicating that the questionnaire meets the required reliability. After the OSCE, the teacher distributed an anonymous questionnaire to the students in Group A (Fig. 1 ). The questionnaire included two basic pieces of information about the subjects’ age and gender, 11 scale questions, 1 multiple-choice question, and 1 open-ended question. The question design is based on a Likert scale (the scale ranges from 1 to 5, indicating the degree from strongly disagree to strongly agree). We considered a score ≥ 4 as an agreement.
The primary outcome of this study was to evaluate the scores of OSCE at the end of the course for both groups of students. Additionally, the results of the questionnaire were considered as a secondary outcome.

An overview of the course design: From 248 fifth-semester clinical medicine students, 48 students were randomly selected and divided into Group A and Group B. Group A adopted BT, and Group B adopted TOT. After 4 months of teaching, both of the two groups took OSCE but only Group A took the questionnaire
BT: Blended Teaching; TOT: Traditional Offline Teaching

The formative assessment of Group A and Group B
Statistical analyses
We used the Mac 2019 version of Microsoft Excel to collect all the OSCE score data and the BT questionnaire data. IBM SPSS Statistics 27 was used to test the normality and homogeneity of variance between groups A and B. Continuous variables with normal distribution were presented as mean ± standard deviation (SD); non-normal variables were reported as median (interquartile range). Suppose the data matched the normal distribution the independent samples t-test was used, if not the Mann-Whitney U-test was used. Frequency analysis was conducted to analyze the rate of students’ agreement with each question in the BT questionnaire as reflected in the count data and expressed as a percentage (%). P < 0.050 determined that it was statistically significant.
Participants’ demographic data
The demographic data of Groups A and B are presented in Table 1 . This study comprised a total of 48 students, with 24 students in Group A and 24 students in Group B. The average age of the students in Group A was 20.08 ± 0.65, while in Group B it was 21.33 ± 0.92. The male/female ratio in Group A was 9/15 and in Group B was 12/12.
Results of OSCE
As demonstrated in Table 2 , the normality of the data was assessed using the Shapiro-Wilk Test. It is important to highlight that the P value for group A in the total score item is less than 0.05, indicating a lack of normal distribution characteristics. Notably, in studies with small sample sizes ( n < 50), meeting the criteria for data normality might be challenging. However, if the absolute value of Skewness is below 10 and the absolute value of Kurtosis is below 3, it is acceptable to proceed with corresponding statistical analyses as if the data is normality. Subsequently, based on the outcomes of the data analysis, appropriate statistical methods are applied to different types of data. The OSCE scores are shown in Table 3 . Significant differences were observed in various skills between Group A and Group B. These skills include cardiopulmonary resuscitation (92.50(4.00) vs. 86.00(3.50), P < 0.050), physical examination (90.04 ± 3.09 vs. 63.83 ± 7.03, P < 0.050), four major puncture operations (77.21 ± 8.99 vs. 71.17 ± 6.42, P < 0.050), disinfection & draping (82.79 ± 4.03 vs. 61.42 ± 12.48, P < 0.050), donning & taking off surgical gowns (84.00(5.75) vs. 78.00(9.00), P < 0.050), incision & suturing (68.42 ± 5.26 vs. 62.79 ± 8.30, P < 0.050) and total score (82.13 ± 3.36 vs. 70.00 ± 5.77, P < 0.050). These results indicate that Group A achieved higher average scores than Group B in all evaluated items at the significance level of 0.05.
Perspectives survey about online and offline blended teaching mode
Table 4 presents the experiences and opinions of students in Group A regarding BT. The questionnaire was designed with questions categorized into four dimensions: course experience, learning effect, teaching evaluation, and overall evaluation. By analyzing the responses to questions 1–4, we can assess the impact of students’ course experience. Among the students who adopted BT, a higher number of students reported an improved course experience. Specifically, the model aided in understanding the theoretical knowledge of clinical skill operations (70.8%, 4.04 ± 1.10) and facilitated faster independent learning of these operations (70.8%, 4.04 ± 1.17). Additionally, it promoted the speed of mastering skills (66.6%, 3.92 ± 1.22) without significantly increasing the learning burden, as observed under good teaching effects (70.8%, 2.79 ± 1.15). Questions 5–7 aimed to assess student learning effectiveness. The majority of students expressed that BT helped prepare for OSCE exams (66.7%, 3.83 ± 1.18), promoting self-directed learning that is not bound by time and space (62.5%, 3.83 ± 1.14), and increasing their interest in the learning process (58.3%, 3.79 ± 1.08). Students’ evaluation of teaching under BT can be assessed using questions 8–9. The majority of students expressed that both online instruction (62.5%, 3.75 ± 1.13) and offline instruction (70.9%, 3.96 ± 1.14) in BT were effective in achieving the desired outcomes and objectives. The students’ overall assessment of BT is reflected in questions 10–11. More than half of the students (54.2%, 3.71 ± 1.06) felt that BT was better than TOT, and a higher proportion of the students (58.3%, 3.79 ± 1.15) expressed their willingness to implement BT into other medical skills training. Furthermore, question 12 revealed the students’ interest in each part of the teaching content, indicating that emergency medicine (79.2%), internal medicine (70.8%), and surgery (66.7%) were the most popular choices.
Clinical skills training in clinical practice courses is characterized by a high degree of practicality and the requirement for more practice time. The TOT model is commonly used, where instructors teach the theory and demonstrate the skills, followed by students practicing on their own. However, this model often limits the duration of students’ practical exercises, which is not beneficial to the training of clinical skills. The present study aims to assess the potential of BT in practice course by integrating online courses with offline practice, developing a BT course that meets pedagogical requirements, and evaluating its teaching effectiveness in different clinical skills. The research findings indicate that students in Group A, who adopted BT, performed better overall in OSCE compared to Group B, who followed the TOT model. Moreover, the results of the questionnaire revealed that Group A students had a positive learning experience and perceived the course to be more effective in terms of pedagogy.
The OSCE is widely recognized as an effective way to judge students’ mastery of clinical skills for formative and summative purposes [ 17 ]. In terms of OSCE scores, students in Group A outperformed those in Group B in both the overall score and each individual item. The differences between all items were statistically significant. When comparing the average scores of each item between the two groups, it can be observed that Group A showed varying levels of improvement in different assessment items. The performance difference between groups A and B was more obvious in the two items of physical examination and Disinfection & Draping compared to the other items. This suggests that although BT demonstrated better teaching effectiveness overall, its strengths vary across different types of items. These two items stand out due to their extensive content but relatively simple operation. With the use of the online platform in BT, students have the opportunity to repeatedly learn and become more proficient in these operations. However, when faced with tasks that require more offline practice, such as CPR and the four major puncture operations, the performance improvement is not as significant as observed in the two aforementioned items. That means online teaching cannot fully substitute offline teaching, especially when it comes to highly practical teaching content. However, online course platforms can be utilized to enhance teaching content, broaden teaching activities, and compensate for the limitations of traditional offline teaching. The results of the questionnaire in Group A revealed that students demonstrated a great interest interest in first aid, internal medicine, and surgery skills. Additionally, Group A achieved higher scores in the OSCE at the CPR site (Emergency Medicine) and the Basic Surgical Skills-related site (Surgery). These findings indicate that when students are presented with more engaging study materials, their motivation to learn is enhanced, leading to improved learning outcomes driven by higher levels of initiative [ 18 ]. Therefore, in the next stage of course construction, it is crucial to explore the development of more course content that can effectively enhance students’ interest in learning.
In contrast to this study, much of the current research on the use of BT in clinical skills education tends to concentrate on specific skills or skill types. Amy L Halverson’s research, for example, delves into surgical skills. The findings of Halverson’s study indicate that BT has a beneficial impact on surgical skills training for rural physicians, aligning with the outcomes of our study. Nevertheless, unlike the present research, Halverson’s study relied solely on questionnaires for drawing conclusions and lacked objective evaluation metrics [ 19 ]. More studies are focusing on evaluating the effectiveness of the BT model in CPR training due to the broad audience it caters to, which includes both medical and non-medical professionals. A study conducted on 832 non-medical professional persons in Taiwan revealed that the BT model was superior to TOT [ 20 ]. Additionally, research on the application of the BT model in CPR training for underage students demonstrated a significant increase in students’ willingness to intervene during a cardiac arrest, from 56.9 to 93.1% post-course [ 21 ]. These findings highlight the positive impact of the BT model on students’ self-confidence and overall teaching outcomes. Our study further supports these results, as the group A trained with the BT model performed notably better in the OSCE at the CPR site. This study innovatively applied the BT model to various types of clinical skills training, comparing its effects with the TOT model across different skill items. Moreover, this research not only examined the differences in application effects between the two teaching models on the same skill items but also compared the differences in teaching effectiveness improvement after applying the BT model among different skill items. The findings offer a more comprehensive theoretical foundation for application of the BT teaching model in clinical skills practice courses.
In the design of the course, we offer a wealth of clinical case materials on the online course platform. These materials are available for students who are eager to learn. Our goal is to foster students’ advanced abilities through the use of relevant cases or scenarios, which can enhance their coping skills and their ability to handle emergencies [ 22 ]. Our study has shown that students in Group A demonstrate higher performance in practical projects like CPR, which require hands-on experience, through online situational clinical case training. This training method allows students to go beyond simply acquiring visual information and instead encourages them to analyze, process, and integrate the visual information. As a result, students can achieve a deeper understanding of the knowledge points, progressing from the lower levels of Bloom’s taxonomy (memorization and comprehension) to higher levels such as analysis, application, and judgment. This approach greatly enhances the effectiveness of learning [ 23 ]. According to several studies, virtual simulation has been found to be more effective in promoting the learning of skills compared to teaching theoretical knowledge alone [ 24 ]. Therefore, in future designs of BT, we propose incorporating virtual simulation teaching into the online platform. This addition aims to address the limitations of the online platform in practical training and enhance the overall learning experience [ 25 ].
The blend of online courses with the traditional TOT model can offer teachers a more personalized teaching environment and timely feedback. The online education platform enables real-time observation and regulation of students’ learning progress, allowing for dynamic adjustments in offline teaching content and methods to better achieve pedagogical goals. Furthermore, we designed a chapter test in the online course. According to Kromann, the inclusion of testing in clinical skills training can be effective in improving the effectiveness of learning [ 26 ]. In this study, we observed that teachers can effectively assess students’ understanding of this particular aspect of the theory through chapter tests. This allows them to provide targeted guidance and reinforcement for students’ weaker areas in the offline course. Such feedback evaluation, developed during the teaching process, plays a crucial role in improving teaching effectiveness due to its timeliness and relevance. In future course designs, we plan to incorporate various forms of accompanying tests in both online and offline sessions to further enhance formative evaluation and teaching effectiveness.
For students, blending the online course with the offline course can provide the advantages of being more accessible and flexible in terms of time and location. It has been claimed that students can arrange their learning according to their own schedule and rhythm through the online platform in the BT model [ 13 ]. A similar phenomenon was observed in our study. For instance, before each offline teaching session or OSCE, there was a noticeable increase in students accessing online platforms. This trend indicates that students are using online platforms to align with their learning or revision strategies. In the online course, we have also introduced a discussion board where the instructor posts clinical case information and related questions. This board serves as a platform for students to actively participate in discussions and answer the questions posed by the instructor. The instructor then provides feedback on the student’s answers. This interactive communication method helps to reinforce the students’ clinical knowledge and skills, while also training them to develop their initial clinical thinking skills. Meanwhile, it also can effectively promote student participation in this course. It has been reported that greater student engagement in courses can increase their positive experience of the course and ultimately improve the effectiveness of the instruction [ 27 ]. However, in the BT model, students are required to possess advanced self-management skills and be familiar with online teaching platforms. Therefore, it is essential to integrate suitable learning monitoring tools and provide adequate training as part of the teaching process [ 28 , 29 ].
In the analysis of the questionnaire, we also noticed that students were slightly more satisfied with offline education (70.9%) than with online education (62.5%). This reminds us that offline teaching still holds its irreplaceability compared to online teaching. For example, face-to-face communication in offline teaching fosters a closer emotional connection between teachers and students. It allows for more intuitive guidance in developing students’ skills and provides faster feedback [ 30 ]. Given the practical nature of clinical skills courses, it is reasonable to conclude that online teaching cannot fully replace offline teaching. However, our research indicates that a combination of online and offline instruction can produce a synergistic effect. The online component of the course expands teaching resources and diversifies teaching methods, while also overcoming time and space constraints and promoting independent learning. On the other hand, the offline component allows teachers to provide personalized face-to-face guidance promptly. By combining these two approaches, we can achieve improved pedagogical effectiveness by leveraging their complementary advantages.
Like all educational research articles, this study has some limitations. Firstly, the sample size in this study is relatively small, which may result in a larger margin of error. Therefore, in our future studies, we plan to increase the sample size to reduce the potential bias caused by the small sample. Additionally, the limited number of clinical skills items included in this research may not provide a comprehensive evaluation of the effectiveness of BT in various clinical skills teaching. In future research, we will incorporate more measures to assess the learning outcomes of students’ clinical skills. This will involve collecting scores from graduation operation examinations and licensing examinations to objectively evaluate students’ mastery of clinical skills. Additionally, we will enhance curriculum development by integrating more clinical skills teaching programs into the BT model. This will allow for a more comprehensive evaluation of the BT model’s effectiveness in training various clinical skills programs. The questionnaire used in this study may have limitations in evaluating the teaching effect of BT due to its subjective nature. It is more suitable for assessing students’ subjective perceptions of the BT teaching model. Future research will aim to enhance the questionnaire design to better capture the subjective experiences of both teachers and students.
The development of the times has resulted in significant changes in medical education. As educators, it is important for us to actively explore new teaching modes and methods to enhance students’ learning experiences and outcomes. This will enable us to better cultivate medical students to meet the demands of the modern era. In conclusion, the results of this research indicate that students adopting BT are better in clinical skills training than those adopting TOT. And then, BT was better at teaching content-rich but easy-to-do items (physical examination and disinfection & draping) than practice-demanding items. Finally, students adopting BT will have better pedagogical outcomes in the more interesting items (emergency medicine and surgery). The application of BT in clinical skills training has demonstrated its potential in this study, leading us to believe that applying BT to other medical skills training and courses could yield unexpected benefits. In the future, we plan to develop more courses using blended teaching to cater to the needs of the new generation of clinical medical students.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Wang W. Medical education in China: progress in the past 70 years and a vision for the future. BMC Med Educ. 2021;21(1):453.
Article Google Scholar
Zaman J. The enduring value of the physical examination. Med Clin North Am. 2018;102(3):417–23.
Dalton HJ, Berg RA, Nadkarni VM, Kochanek PM, Tisherman SA, Thiagarajan R, Alexander P, Bartlett RH. Cardiopulmonary resuscitation and rescue therapies. Crit Care Med. 2021;49(9):1375–88.
Chen V, Polley C, Dunne B, Martin K. Online delivery of surgical skills teaching. Med Educ. 2022;56(11):1130–1.
Bouchoucha S, Wikander L, Wilkin C. Assessment of simulated clinical skills and distance students: can we do it better. Nurse Educ Today. 2013;33(9):944–8.
Wu C, Chen L, Han M, Li Z, Yang N, Yu C. Application of ChatGPT-based blended medical teaching in clinical education of hepatobiliary surgery. Med Teach. 2024:1–5.
Byrne AJ, Pugsley L, Hashem MA. Review of comparative studies of clinical skills training. Med Teach. 2008;30(8):764–7.
Alsoufi A, Alsuyihili A, Msherghi A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS ONE. 2020;15(11):e0242905.
Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378.
Mortagy M, Abdelhameed A, Sexton P, et al. Online medical education in Egypt during the COVID-19 pandemic: a nationwide assessment of medical students’ usage and perceptions. BMC Med Educ. 2022;22(1):218.
Mangione S, Nieman LZ, Greenspon LW, Margulies H. A comparison of computer-assisted instruction and small-group teaching of cardiac auscultation to medical students. Med Educ. 1991;25(5):389–95.
Mars M, McLean M. Students’ perceptions of a multimedia computer-aided instruction resource in histology. S Afr Med J. 1996;86(9):1098–102.
Google Scholar
Vallée A, Blacher J, Cariou A, Sorbets E. Blended learning compared to traditional learning in medical education: systematic review and meta-analysis. J Med Internet Res. 2020;22(8):e16504.
Teagle AR, George M, Gainsborough N, Haq I, Okorie M. Preparing medical students for clinical practice: easing the transition. Perspect Med Educ. 2017;6(4):277–80.
Liu Y. Xuejun Zeng. Clinical skills training and practice. People’s Medical Publishing House; 2015.
University Open Online Courses learning platform. Shenzhen University Open Online Courses Education limited company. https://www.uooc.net.cn/league/union
Patrício MF, Julião M, Fareleira F, Carneiro AV. Is the OSCE a feasible tool to assess competencies in undergraduate medical education. Med Teach. 2013;35(6):503–14.
Song L, Singleton ES, Hill JR, Koh MH. Improving online learning: student perceptions of useful and challenging characteristics. Internet High Educ. 2004;7(1):59–70.
Halverson AL, DaRosa DA, Borgstrom DC, et al. Evaluation of a blended learning surgical skills course for rural surgeons. Am J Surg. 2014;208(1):136–42.
Chien C-Y et al. Traditional versus blended CPR training program: a randomized controlled non-inferiority study. Sci Rep. 2020;10(1):10032.
Semeraro F, Imbriaco G, Del Giudice D, et al. Empowering the next generation: an innovative kids save lives blended learning programme for schoolchildren training. Resuscitation. 2024;194:110088.
Cook DA, Triola MM. Virtual patients: a critical literature review and proposed next steps. Med Educ. 2009;43(4):303–11.
Arneson JB, Offerdahl EG. Visual literacy in bloom: using Bloom’s taxonomy to support visual learning skills. CBE Life Sci Educ. 2018;17(1):ar7.
Kononowicz AA, Woodham LA, Edelbring S, et al. Virtual patient simulations in health professions education: systematic review and meta-analysis by the digital health education collaboration. J Med Internet Res. 2019;21(7):e14676.
Wu Q, Wang Y, Lu L, Chen Y, Long H, Wang J. Virtual simulation in undergraduate medical education: a scoping review of recent practice. Front Med (Lausanne). 2022;9:855403.
Kromann CB, Jensen ML, Ringsted C. The effect of testing on skills learning. Med Educ. 2009;43(1):21–7.
Hensley A, Hampton D, Wilson JL, Culp-Roche A, Wiggins AT. A multicenter study of student engagement and satisfaction in online programs. J Nurs Educ. 2021;60(5):259–64.
Lim DH, Kim H. Motivation and learner characteristics affecting online learning and learning application. J Educational Technol Syst. 2003;31(4):423–39.
Pelaccia T, Viau R. Motivation in medical education(). Med Teach. 2017;39(2):136–40.
Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24(1):1666538.
Download references
Acknowledgements
We would like to thank our colleagues in the Department of Clinical Medicine, and the Affiliated Hospital of Wuhan University of Science and Technology, for participating in the construction of the “Clinical Skills Training and Practice” online course, teaching and scoring the enrolled students.
This work was supported by the Higher Educational Teaching Reform Project of the Hubei Province Education Department (2021236); the College Students’ Innovation Project of Hubei Province of China (Hubei Province Education Department, S202110488072); Graduate Education Quality Engineering Project of Wuhan University of Science and Technology (Yjg202327).
Author information
Authors and affiliations.
Department of Clinical Medicine, College of Medicine, Wuhan University of Science and Technology, Wuhan, Hubei, P.R. China
Zhicheng He, Hua Li, Lan Lu, Qiang Wang, Qingming Wu & Lili Lu
You can also search for this author in PubMed Google Scholar
Contributions
ZC He wrote the draft, prepared figures and interpreted the data; H Li, L Lu, and Q Wang participated in the organization and implementation of this study; LL Lu and QM Wu conceived and designed this study; LL Lu did the critically revising work; approved the final version submitted; got the funding supporting. All authors reviewed the manuscript.
Corresponding authors
Correspondence to Qingming Wu or Lili Lu .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethics Committee of Wuhan University of Science and Technology (Dossier number 2022151). Participating students completed an informed consent form. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
He, Z., Li, H., Lu, L. et al. The application of blended teaching in medical practical course of clinical skills training. BMC Med Educ 24 , 724 (2024). https://doi.org/10.1186/s12909-024-05730-6
Download citation
Received : 20 January 2024
Accepted : 01 July 2024
Published : 04 July 2024
DOI : https://doi.org/10.1186/s12909-024-05730-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Clinical skill training
- Blended teaching
- Practice course
- Teaching model
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Accessibility Options:
- Skip to Content
- Skip to Search
- Skip to footer
- Office of Disability Services
- Request Assistance
- 305-284-2374
- High Contrast
- School of Architecture
- College of Arts and Sciences
- Miami Herbert Business School
- School of Communication
- School of Education and Human Development
- College of Engineering
- School of Law
- Rosenstiel School of Marine, Atmospheric, and Earth Science
- Miller School of Medicine
- Frost School of Music
- School of Nursing and Health Studies
- The Graduate School
- Division of Continuing and International Education
- People Search
- Class Search
- IT Help and Support
- Privacy Statement
- Student Life

- Main College
- College News
Biomedical Engineering
- Chemical, Environmental and Materials Engineering
- Civil and Architectural Engineering
- Electrical and Computing Engineering
- Industrial Engineering
- Mechanical and Aerospace Engineering
- Letter from the Chair
- Department Clusters
- Undergraduate
- Imaging, Optics, & Lasers
- Biomechanics, Microfluidics, Biomaterials and Tissue
- Neural Engineering, Signals, & Instrumentation
- News and Events
- Advisory Board
- PhD Students
- graduate programs
MS in Medical Physics

Coming Soon
FOR MORE INFORMATION ABOUT OUR PROGRAM, PLEASE FILL OUT OUR CONTACT FORM BY CLICKING HERE.
Mission statement.
- Coming soon
Program Goals
- To train students to develop the necessary academic framework as well as a thorough practical understanding in medical physics, including areas of diagnostic radiologic physics, health physics, nuclear medicine, and a designated focus on radiation therapy.
Learning Outcomes
- Students will be able to apply knowledge of mathematics, science and engineering to formulate and solve relevant medical physics problems.
- Students will be able to communicate scientific and technical research effectively in writing and oral presentations.
- Students will be able to work with physicians and technicians in conducting diagnostic radiology or radiation therapy
Course List

- 1251 Memorial Drive McArthur Engineering Building Coral Gables , FL 33146
- 305-284-2445 305-284-2445
- Academic Calendar
- Alumni & Friends
- Medical Center
- Hurricane Sports
- Parking & Transportation
- social-facebook
- social-twitter
- social-youtube
- social-instagram
Copyright: 2024 University of Miami. All Rights Reserved. Emergency Information Privacy Statement & Legal Notices
Individuals with disabilities who experience any technology-based barriers accessing the University’s websites or services can visit the Office of Workplace Equity and Inclusion .
- School of Medicine Columbia
- Location Location
- Contact Contact
- Colleges and Schools
- Research News
Who is your prenatal care provider? An algorithm to identify the predominant prenatal care provider with claims data
Dr. Songyuan Deng, an Associate Scientist at the South Carolina Center for Rural and Primary Healthcare at the USC School of Medicine-Columbia, has conducted a study proposing an algorithm to identify the predominant prenatal care provider and estimate the percentage of identified predominant providers.
Previous studies applied plurality (providing the most visits) and majority (providing majority of visits) to identify the predominant provider in primary care setting, with only visit frequency information. This study proposed an algorithm that included both visit frequency and sequence information in prenatal care (PNC) to identify the predominant provider and estimated the percentage of identified predominant providers.
By applying PNC frequency information, a predominant provider can be identified for 81% of pregnancies. After adding sequential information, a predominant provider can be identified for 92% of pregnancies. In addition, applying this algorithm revealed a longer distance for pregnant individuals travelling to their predominant provider (an average of 5 miles) than to the nearest provider.
Integrating visit frequency and sequence information, rather than relying solely on frequency, and incorporating dispersion information as a supplement allows for a better understanding of how patients seek PNC, particularly for the continuity of prenatal care. This insight is crucial for understanding which provider renders a big impact on prenatal care and birth outcomes for a pregnant woman.
Deng S, Renaud S, Bennett KJ. Who is your prenatal care provider? An algorithm to identify the predominant prenatal care provider with claims data. BMC Health Serv Res. 2024 May 27;24(1):665. doi: 10.1186/s12913-024-11080-2. PMID: 38802871; PMCID: PMC11131320.
Challenge the conventional. Create the exceptional. No Limits.
- Research into trans medicine has been manipulated
Court documents offer a window into how this happens

Your browser does not support the <audio> element.
I N APRIL HILARY CASS , a British paediatrician, published her review of gender-identity services for children and young people, commissioned by NHS England. It cast doubt on the evidence base for youth gender medicine. This prompted the World Professional Association for Transgender Health ( WPATH ), the leading professional organisation for the doctors and practitioners who provide services to trans people, to release a blistering rejoinder. WPATH said that its own guidelines were sturdier, in part because they were “based on far more systematic reviews”.
Systematic reviews should evaluate the evidence for a given medical question in a careful, rigorous manner. Such efforts are particularly important at the moment, given the feverish state of the American debate on youth gender medicine, which is soon to culminate in a Supreme Court case challenging a ban in Tennessee. The case turns, in part, on questions of evidence and expert authority.
Court documents recently released as part of the discovery process in a case involving youth gender medicine in Alabama reveal that WPATH ’s claim was built on shaky foundations. The documents show that the organisation’s leaders interfered with the production of systematic reviews that it had commissioned from the Johns Hopkins University Evidence-Based Practice Centre ( EPC ) in 2018.
From early on in the contract negotiations, WPATH expressed a desire to control the results of the Hopkins team’s work. In December 2017, for example, Donna Kelly, an executive director at WPATH , told Karen Robinson, the EPC ’s director, that the WPATH board felt the EPC researchers “cannot publish their findings independently”. A couple of weeks later, Ms Kelly emphasised that, “the [ WPATH ] board wants it to be clear that the data cannot be used without WPATH approval”.
Ms Robinson saw this as an attempt to exert undue influence over what was supposed to be an independent process. John Ioannidis of Stanford University, who co-authored guidelines for systematic reviews, says that if sponsors interfere or are allowed to veto results, this can lead to either biased summaries or suppression of unfavourable evidence. Ms Robinson sought to avoid such an outcome. “In general, my understanding is that the university will not sign off on a contract that allows a sponsor to stop an academic publication,” she wrote to Ms Kelly.
Months later, with the issue still apparently unresolved, Ms Robinson adopted a sterner tone. She noted in an email in March 2018 that, “Hopkins as an academic institution, and I as a faculty member therein, will not sign something that limits academic freedom in this manner,” nor “language that goes against current standards in systematic reviews and in guideline development”.
Not to reason XY
Eventually WPATH relented, and in May 2018 Ms Robinson signed a contract granting WPATH power to review and offer feedback on her team’s work, but not to meddle in any substantive way. After wpath leaders saw two manuscripts submitted for review in July 2020, however, the parties’ disagreements flared up again. In August the WPATH executive committee wrote to Ms Robinson that WPATH had “many concerns” about these papers, and that it was implementing a new policy in which WPATH would have authority to influence the EPC team’s output—including the power to nip papers in the bud on the basis of their conclusions.
Ms Robinson protested that the new policy did not reflect the contract she had signed and violated basic principles of unfettered scientific inquiry she had emphasised repeatedly in her dealings with WPATH . The Hopkins team published only one paper after WPATH implemented its new policy: a 2021 meta-analysis on the effects of hormone therapy on transgender people. Among the recently released court documents is a WPATH checklist confirming that an individual from WPATH was involved “in the design, drafting of the article and final approval of [that] article”. (The article itself explicitly claims the opposite.) Now, more than six years after signing the agreement, the EPC team does not appear to have published anything else, despite having provided WPATH with the material for six systematic reviews, according to the documents.
No one at WPATH or Johns Hopkins has responded to multiple inquiries, so there are still gaps in this timeline. But an email in October 2020 from WPATH figures, including its incoming president at the time, Walter Bouman, to the working group on guidelines, made clear what sort of science WPATH did (and did not) want published. Research must be “thoroughly scrutinised and reviewed to ensure that publication does not negatively affect the provision of transgender health care in the broadest sense,” it stated. Mr Bouman and one other coauthor of that email have been named to a World Health Organisation advisory board tasked with developing best practices for transgender medicine.
Another document recently unsealed shows that Rachel Levine, a trans woman who is assistant secretary for health, succeeded in pressing wpath to remove minimum ages for the treatment of children from its 2022 standards of care. Dr Levine’s office has not commented. Questions remain unanswered, but none of this helps WPATH ’s claim to be an organisation that bases its recommendations on science. ■
Stay on top of American politics with The US in brief , our daily newsletter with fast analysis of the most important electoral stories, and Checks and Balance , a weekly note from our Lexington columnist that examines the state of American democracy and the issues that matter to voters.
Explore more
This article appeared in the United States section of the print edition under the headline “Marking their own homework”
United States June 29th 2024
- Young voters strongly favour Joe Biden, but will they turn out?
- True-crime fans are banding together online to try to solve cases
- Przekrój, an iconic Polish magazine, relaunches in America
- Non-white American parents are embracing AI faster than white ones
- What to make of the US Supreme Court’s latest abortion ruling
- In New York, the Democratic establishment strikes back

From the June 29th 2024 edition
Discover stories from this section and more in the list of contents
More from United States

Anguish about Joe Biden’s candidacy is rational, polls suggest
Would Kamala Harris fare better?

Las Vegas’s power couple says goodbye to power
The Goodmans were mayors for 25 years. Their evolution mirrors that of Sin City

Meet a leading Trump vice-presidential contender
How Doug Burgum went from dark horse to favourite
Joe Biden’s ABC interview will not quell doubts about his future
Nor will it resolve the Democratic Party’s dilemma
Jill Biden; Defender-in-chief
What happens next in the Democratic leadership saga may depend on the First Lady
Will IVF really be the next frontier in America’s culture wars?
Banning it would be political suicide. But it could get harder to find in conservative states
July 8, 2024

Researchers from Emory AI.Health and Cleveland Clinic have developed an AI-powered method to detect eye inflammation caused by anti-VEGF drugs before it becomes severe.
— Getty Images
Age-related macular degeneration (AMD) is a leading cause of vision loss in the U.S., affecting 11 million people, particularly older adults. The more severe form, neovascular age-related macular degeneration (nAMD), is characterized by abnormal blood vessel growth under the retina. These vessels leak fluid or blood, leading to vision loss. Besides age, smoking, poor diet, and lack of physical activity also contribute to the risk.
The primary treatment for nAMD is anti-VEGF drugs. This treatment involves injecting a drug into the eye that blocks a protein called vascular endothelial growth factor (VEGF), which is responsible for the growth of abnormal blood vessels in the retina; however, it can cause eye inflammation as a serious side effect.
A team of researchers from Emory AI.Health and Cleveland Clinic aimed to predict which patients might develop this inflammatory response. By combining routine optical coherence tomography (OCT) scans with machine learning and precision medicine, they sought to identify patterns in eye scan images that could appear before or during inflammation caused by anti-VEGF drugs. Identifying these patterns early could help doctors detect inflammation sooner and adjust treatment to prevent vision loss.
Detecting trouble early: the study
Published in the Cell Press journal Heliyon , the study analyzed images of 67 eyes from a retrospective clinical trial involving patients with nAMD. Researchers extracted specific texture-based features from OCT scans, focusing on the vitreous compartment — the clear gel in the eye. Using a machine learning model developed by Emory AI.Health, they identified patterns signaling inflammation before it was clinically visible.
Promising results
The machine learning model accurately distinguished which patients would develop inflammation, achieving a 76% accuracy rate before anti-VEGF treatment and 81% accuracy at the time of injection. This data suggests its potential as a valuable tool for early detection.
Why it matters
“Macular degeneration is personal to me because my father suffers from it. As our population ages, more people will experience nAMD. Anti-VEGF agents can slow down macular degeneration but come with risks,” said Anant Madabhushi, PhD , executive director of Emory AI.Health and principal investigator of the study. “Our study provides valuable data for clinicians to make better treatment decisions, potentially reducing the dosage or combining these agents with anti-inflammatory drugs to prevent severe complications.”
Looking ahead
“This study validates our AI algorithms in a retrospective clinical trial and underscores the potential of precision medicine in ophthalmology,” said Sudeshna Sil Kar, PhD , first author of the study and associate scientist at Emory AI.Health. “Next, we hope to embed our algorithms in prospective clinical trials to identify patients likely to develop these adverse events in real-time.”
- Artificial Intelligence
- School of Medicine
- Woodruff Health Sciences Center
- News Releases
Recent News
Download emory news photo.
By downloading Emory news media, you agree to the following terms of use:
Creative Commons Attribution-NoDerivatives 4.0 International Public License
By exercising the Licensed Rights (defined below), You accept and agree to be bound by the terms and conditions of this Creative Commons Attribution-NoDerivatives 4.0 International Public License ("Public License"). To the extent this Public License may be interpreted as a contract, You are granted the Licensed Rights in consideration of Your acceptance of these terms and conditions, and the Licensor grants You such rights in consideration of benefits the Licensor receives from making the Licensed Material available under these terms and conditions.
Section 1 – Definitions.
- Adapted Material means material subject to Copyright and Similar Rights that is derived from or based upon the Licensed Material and in which the Licensed Material is translated, altered, arranged, transformed, or otherwise modified in a manner requiring permission under the Copyright and Similar Rights held by the Licensor. For purposes of this Public License, where the Licensed Material is a musical work, performance, or sound recording, Adapted Material is always produced where the Licensed Material is synched in timed relation with a moving image.
- Copyright and Similar Rights means copyright and/or similar rights closely related to copyright including, without limitation, performance, broadcast, sound recording, and Sui Generis Database Rights, without regard to how the rights are labeled or categorized. For purposes of this Public License, the rights specified in Section 2(b)(1)-(2) are not Copyright and Similar Rights.
- Effective Technological Measures means those measures that, in the absence of proper authority, may not be circumvented under laws fulfilling obligations under Article 11 of the WIPO Copyright Treaty adopted on December 20, 1996, and/or similar international agreements.
- Exceptions and Limitations means fair use, fair dealing, and/or any other exception or limitation to Copyright and Similar Rights that applies to Your use of the Licensed Material.
- Licensed Material means the artistic or literary work, database, or other material to which the Licensor applied this Public License.
- Licensed Rights means the rights granted to You subject to the terms and conditions of this Public License, which are limited to all Copyright and Similar Rights that apply to Your use of the Licensed Material and that the Licensor has authority to license.
- Licensor means the individual(s) or entity(ies) granting rights under this Public License.
- Share means to provide material to the public by any means or process that requires permission under the Licensed Rights, such as reproduction, public display, public performance, distribution, dissemination, communication, or importation, and to make material available to the public including in ways that members of the public may access the material from a place and at a time individually chosen by them.
- Sui Generis Database Rights means rights other than copyright resulting from Directive 96/9/EC of the European Parliament and of the Council of 11 March 1996 on the legal protection of databases, as amended and/or succeeded, as well as other essentially equivalent rights anywhere in the world.
- You means the individual or entity exercising the Licensed Rights under this Public License. Your has a corresponding meaning.
Section 2 – Scope.
- reproduce and Share the Licensed Material, in whole or in part; and
- produce and reproduce, but not Share, Adapted Material.
- Exceptions and Limitations . For the avoidance of doubt, where Exceptions and Limitations apply to Your use, this Public License does not apply, and You do not need to comply with its terms and conditions.
- Term . The term of this Public License is specified in Section 6(a) .
- Media and formats; technical modifications allowed . The Licensor authorizes You to exercise the Licensed Rights in all media and formats whether now known or hereafter created, and to make technical modifications necessary to do so. The Licensor waives and/or agrees not to assert any right or authority to forbid You from making technical modifications necessary to exercise the Licensed Rights, including technical modifications necessary to circumvent Effective Technological Measures. For purposes of this Public License, simply making modifications authorized by this Section 2(a)(4) never produces Adapted Material.
- Offer from the Licensor – Licensed Material . Every recipient of the Licensed Material automatically receives an offer from the Licensor to exercise the Licensed Rights under the terms and conditions of this Public License.
- No downstream restrictions . You may not offer or impose any additional or different terms or conditions on, or apply any Effective Technological Measures to, the Licensed Material if doing so restricts exercise of the Licensed Rights by any recipient of the Licensed Material.
- No endorsement . Nothing in this Public License constitutes or may be construed as permission to assert or imply that You are, or that Your use of the Licensed Material is, connected with, or sponsored, endorsed, or granted official status by, the Licensor or others designated to receive attribution as provided in Section 3(a)(1)(A)(i) .
Other rights .
- Moral rights, such as the right of integrity, are not licensed under this Public License, nor are publicity, privacy, and/or other similar personality rights; however, to the extent possible, the Licensor waives and/or agrees not to assert any such rights held by the Licensor to the limited extent necessary to allow You to exercise the Licensed Rights, but not otherwise.
- Patent and trademark rights are not licensed under this Public License.
- To the extent possible, the Licensor waives any right to collect royalties from You for the exercise of the Licensed Rights, whether directly or through a collecting society under any voluntary or waivable statutory or compulsory licensing scheme. In all other cases the Licensor expressly reserves any right to collect such royalties.
Section 3 – License Conditions.
Your exercise of the Licensed Rights is expressly made subject to the following conditions.
Attribution .
If You Share the Licensed Material, You must:
- identification of the creator(s) of the Licensed Material and any others designated to receive attribution, in any reasonable manner requested by the Licensor (including by pseudonym if designated);
- a copyright notice;
- a notice that refers to this Public License;
- a notice that refers to the disclaimer of warranties;
- a URI or hyperlink to the Licensed Material to the extent reasonably practicable;
- indicate if You modified the Licensed Material and retain an indication of any previous modifications; and
- indicate the Licensed Material is licensed under this Public License, and include the text of, or the URI or hyperlink to, this Public License.
- You may satisfy the conditions in Section 3(a)(1) in any reasonable manner based on the medium, means, and context in which You Share the Licensed Material. For example, it may be reasonable to satisfy the conditions by providing a URI or hyperlink to a resource that includes the required information.
- If requested by the Licensor, You must remove any of the information required by Section 3(a)(1)(A) to the extent reasonably practicable.
Section 4 – Sui Generis Database Rights.
Where the Licensed Rights include Sui Generis Database Rights that apply to Your use of the Licensed Material:
- for the avoidance of doubt, Section 2(a)(1) grants You the right to extract, reuse, reproduce, and Share all or a substantial portion of the contents of the database, provided You do not Share Adapted Material;
- if You include all or a substantial portion of the database contents in a database in which You have Sui Generis Database Rights, then the database in which You have Sui Generis Database Rights (but not its individual contents) is Adapted Material; and
- You must comply with the conditions in Section 3(a) if You Share all or a substantial portion of the contents of the database.
Section 5 – Disclaimer of Warranties and Limitation of Liability.
- Unless otherwise separately undertaken by the Licensor, to the extent possible, the Licensor offers the Licensed Material as-is and as-available, and makes no representations or warranties of any kind concerning the Licensed Material, whether express, implied, statutory, or other. This includes, without limitation, warranties of title, merchantability, fitness for a particular purpose, non-infringement, absence of latent or other defects, accuracy, or the presence or absence of errors, whether or not known or discoverable. Where disclaimers of warranties are not allowed in full or in part, this disclaimer may not apply to You.
- To the extent possible, in no event will the Licensor be liable to You on any legal theory (including, without limitation, negligence) or otherwise for any direct, special, indirect, incidental, consequential, punitive, exemplary, or other losses, costs, expenses, or damages arising out of this Public License or use of the Licensed Material, even if the Licensor has been advised of the possibility of such losses, costs, expenses, or damages. Where a limitation of liability is not allowed in full or in part, this limitation may not apply to You.
- The disclaimer of warranties and limitation of liability provided above shall be interpreted in a manner that, to the extent possible, most closely approximates an absolute disclaimer and waiver of all liability.
Section 6 – Term and Termination.
- This Public License applies for the term of the Copyright and Similar Rights licensed here. However, if You fail to comply with this Public License, then Your rights under this Public License terminate automatically.
Where Your right to use the Licensed Material has terminated under Section 6(a) , it reinstates:
- automatically as of the date the violation is cured, provided it is cured within 30 days of Your discovery of the violation; or
- upon express reinstatement by the Licensor.
- For the avoidance of doubt, the Licensor may also offer the Licensed Material under separate terms or conditions or stop distributing the Licensed Material at any time; however, doing so will not terminate this Public License.
- Sections 1 , 5 , 6 , 7 , and 8 survive termination of this Public License.
Section 7 – Other Terms and Conditions.
- The Licensor shall not be bound by any additional or different terms or conditions communicated by You unless expressly agreed.
- Any arrangements, understandings, or agreements regarding the Licensed Material not stated herein are separate from and independent of the terms and conditions of this Public License.
Section 8 – Interpretation.
- For the avoidance of doubt, this Public License does not, and shall not be interpreted to, reduce, limit, restrict, or impose conditions on any use of the Licensed Material that could lawfully be made without permission under this Public License.
- To the extent possible, if any provision of this Public License is deemed unenforceable, it shall be automatically reformed to the minimum extent necessary to make it enforceable. If the provision cannot be reformed, it shall be severed from this Public License without affecting the enforceability of the remaining terms and conditions.
- No term or condition of this Public License will be waived and no failure to comply consented to unless expressly agreed to by the Licensor.
- Nothing in this Public License constitutes or may be interpreted as a limitation upon, or waiver of, any privileges and immunities that apply to the Licensor or You, including from the legal processes of any jurisdiction or authority.
Creative Commons is not a party to its public licenses. Notwithstanding, Creative Commons may elect to apply one of its public licenses to material it publishes and in those instances will be considered the “Licensor.” The text of the Creative Commons public licenses is dedicated to the public domain under the CC0 Public Domain Dedication . Except for the limited purpose of indicating that material is shared under a Creative Commons public license or as otherwise permitted by the Creative Commons policies published at creativecommons.org/policies , Creative Commons does not authorize the use of the trademark “Creative Commons” or any other trademark or logo of Creative Commons without its prior written consent including, without limitation, in connection with any unauthorized modifications to any of its public licenses or any other arrangements, understandings, or agreements concerning use of licensed material. For the avoidance of doubt, this paragraph does not form part of the public licenses.

IMAGES
VIDEO
COMMENTS
This requires looking beyond the research setting to determine how best to apply a variety of discoveries in real-world scenarios. Such critical thinking skills are essential to bring real benefit, such as through the creation of new treatments that lead to improved outcomes for patients. Apply Clinical Research Skills Broadly
The Need for Clinicians to Strengthen Health Care Research Skills. January 28, 2020. If you're a medical professional interested in health care research, it's important to strengthen your understanding of good study design, epidemiology, and biostatistics so you can interpret and design projects that will have a meaningful impact on the field.
The event is the largest national, multispecialty medical research conference for medical students and residents and offers a $10,000 grand prize for the winning poster. Dive deeper: AMA Research Challenge: How to prepare a research poster. What you need to know to ace a poster abstract. 5 reasons to showcase your work in the AMA Research ...
Foundations of Clinical Research. This Harvard Medical School six-month, application-based certificate program provides the essential skill sets and fundamental knowledge required to begin or expand your clinical research career. Learn More. September 28, 2024 - April 6, 2025. $6,900 - $7,900.
Developing research skills and scholarship are key components of medical education. The COVID-19 pandemic necessitated that all teaching be delivered online. We introduced an approach to small group teaching in the academic year 2020-2021 online which involved students in an active (ongoing) research study to develop their research skills.
Deadline: July 16, 2024. One method to sharpen your critical analysis skills and prepare for medical school is to participate in research opportunities for premed students as either an undergraduate or during the time between college and medical school. "Any and all research—including non-medical research—is beneficial," said Haidn ...
Abstract. This Guide has been written to provide guidance for individuals involved in curriculum design who wish to develop research skills and foster the attributes in medical undergraduates that help develop research. The Guide will provoke debate on an important subject, and although written specifically with undergraduate medical education ...
There is a decreasing number of physician scientists at a time when there is an increased demand for evidence based medicine and research [1,2,3].Medical schools have a key role to play in this regard, as studies have shown that involving medical students in active research in their undergraduate careers may increase the likelihood that they will be research active after graduation [4,5,6].
Step 1 - Get as much research training as you can. The more skills that you have, the more likely that you are going to be competitive in our current research environment. There are a lot of people going after a little bit of money. The better qualified you are, the more likely you are to succeed.
Here are four steps you can take to become a researcher: 1. Take relevant classes. Clinical researchers typically pursue an undergraduate degree in biology, chemistry, medicine, psychology or a related field. Many also earn a master's, especially if they hope to work at a university or pharmaceutical company.
Strengthening research skills, including grant and scholarly writing, is pivotal for faculty. ... The following seminars from the UConn School of Medicine Faculty offer advice and tips for publishing. Forming Writing Groups: One Person's Experience. Anne Kenny, M.D. September 26, 2013. (55:52)
Physicians and physician-scientists in academic research careers usually spend greater than 50 percent of their time conducting research. ... Skills (PSI) Personality (MBTI®, KTS®) Explore Options ... Careers in Medicine ("CiM") is an online resource owned and operated by the Association of American Medical Colleges ("AAMC"). ...
The roadmap to medical research is a bit tricky to navigate, because it is a profession that demands distinctive skills and expertise along with mandatory formal education. If you harbor an interest in scientific exploration and a desire to break new ground in medical knowledge, the first step is to earn a bachelor's degree in a related field ...
As a developing medical researcher, you need to have effective communication, critical thinking, decision-making, data collecting, data analysing and observational skills. These skill sets will ...
1. Earn a bachelor's degree. To become a medical scientist, you first need to get a bachelor's degree in chemistry, biology, or related fields. A bachelor's degree is the minimum requirement and takes three to four years, and you can proceed to earn a master's degree, which takes another two years.
25 Soft Skills for Clinical Research Associates (CRA) and Coordinators (CRC) As clinical research professionals, we often hear about GCP, HIPAA, compliance, monitoring, Code of Federal Regulations (CFR), so on and so forth.. When trying to secure that next promotion, we often focus on our clinical research skills: the ability to enroll a trial fast, locking that trial database on schedule or ...
With regard to developing research skills among medical undergraduate students, a series of initiatives have been taken, namely organizing a 1-day workshop for the students to expose them to research methodology (the workshop deals with right from the selection of topic, review of literature, development of the data collection tool, ethics in ...
Research skills are required in all branches of medicine ( Laidlaw et al., 2012 ). Clinicians need to be lifelong learners, able to evaluate evidence and understand the process of scientific enquiry. Whether or not a doctor pursues a research career, they still need to be able to make sense, and be critical, of the huge amount of information ...
Our 'Introduction to Medical Research: Essential Skills' course provides an overview of key steps and common methods in medical research and its publication. The course is provided by OUCAGS in collaboration with the EQUATOR Centre, an expert provider in health research education and the Centre for Statistics in Medicine. It is available to ...
Professionals that gather information and assess situations as a whole will be assets to clinical research teams. Critical thinking is often a skill that employers look for when filling junior roles such as clinical research-associated jobs, as it is something that will pay dividends right from day one. In fact, critical thinking is often cited ...
Developing research skills and scholarship are key components of medical education. The COVID-19 pandemic necessitated that all teaching be delivered online. We introduced an approach to small group teaching in the academic year 2020-2021 online which involved students in an active (ongoing) research study to develop their research skills. We acquired student feedback to evaluate their ...
Go through the Medical Researcher posting you're applying to, and identify hard skills the company is looking for. For example, skills like Clinical Trials, Clinical Research and Medical Research are possible skills. These are skills you should try to include on your resume. Expand. 2.
Continue reading to find out what skills a medical researcher needs to be successful in the workplace. The eight most common skills for medical researchers in 2024 based on resume usage. Patients, 13.6%. Statistical Analysis, 10.5%. Vital Signs, 9.6%. Laboratory Practices, 8.2%. Clinical Research Studies, 7.5%. Research Projects, 6.6%.
Health care professionals working in a range of roles and settings can benefit from strengthening their clinical research skills and learning to examine data from different perspectives. That's one of the lessons recently learned by scholars in Harvard Medical School's Postgraduate Foundations of Clinical Research program.
Blended teaching is an effective approach that combines online and offline teaching methods, leading to improved outcomes in medical education compared to traditional offline teaching. In this study, we examined the impact of blended teaching in clinical skills training, a medical practice course. This study involved forty-eight undergraduate students studying clinical medicine in the fifth ...
Qualities which make a good medical researcher include critical thinking skills to determine effective research methodology. It is important you are comfortable working both independently and in a team, while effectively communicating your conclusions and processes, and that you can translate your work into compelling grant proposals.
The medical physics graduate program is accredited by the Commission on Accreditation of Medical Physics Education Programs, Inc. (CAMPEP). The program, serving both MS and PhD degrees, ensures that the students receive adequate didactic and clinical training to continue in education and research, enter clinical physics residencies or begin working as medical physicists in radiation therapy ...
Dr. Songyuan Deng, an Associate Scientist at the South Carolina Center for Rural and Primary Healthcare at the USC School of Medicine-Columbia, has conducted a study proposing an algorithm to identify the predominant prenatal care provider and estimate the percentage of identified predominant providers.
Research into trans medicine has been manipulated; In New York, the Democratic establishment strikes back; From the June 29th 2024 edition. Discover stories from this section and more in the list ...
AI technology advances early detection of severe eye inflammation, new research shows. July 8, 2024. ... (OCT) scans with machine learning and precision medicine, they sought to identify patterns in eye scan images that could appear before or during inflammation caused by anti-VEGF drugs. Identifying these patterns early could help doctors ...