- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board

Gender Confirmation Surgery (GCS)
What is Gender Confirmation Surgery?
- Transfeminine Tr
Transmasculine Transition
- Traveling Abroad
Choosing a Surgeon
Gender confirmation surgery (GCS), known clinically as genitoplasty, are procedures that surgically confirm a person's gender by altering the genitalia and other physical features to align with their desired physical characteristics. Gender confirmation surgeries are also called gender affirmation procedures. These are both respectful terms.
Gender dysphoria , an experience of misalignment between gender and sex, is becoming more widely diagnosed. People diagnosed with gender dysphoria are often referred to as "transgender," though one does not necessarily need to experience gender dysphoria to be a member of the transgender community. It is important to note there is controversy around the gender dysphoria diagnosis. Many disapprove of it, noting that the diagnosis suggests that being transgender is an illness.
Ellen Lindner / Verywell
Transfeminine Transition
Transfeminine is a term inclusive of trans women and non-binary trans people assigned male at birth.
Gender confirmation procedures that a transfeminine person may undergo include:
- Penectomy is the surgical removal of external male genitalia.
- Orchiectomy is the surgical removal of the testes.
- Vaginoplasty is the surgical creation of a vagina.
- Feminizing genitoplasty creates internal female genitalia.
- Breast implants create breasts.
- Gluteoplasty increases buttock volume.
- Chondrolaryngoplasty is a procedure on the throat that can minimize the appearance of Adam's apple .
Feminizing hormones are commonly used for at least 12 months prior to breast augmentation to maximize breast growth and achieve a better surgical outcome. They are also often used for approximately 12 months prior to feminizing genital surgeries.
Facial feminization surgery (FFS) is often done to soften the lines of the face. FFS can include softening the brow line, rhinoplasty (nose job), smoothing the jaw and forehead, and altering the cheekbones. Each person is unique and the procedures that are done are based on the individual's need and budget,
Transmasculine is a term inclusive of trans men and non-binary trans people assigned female at birth.
Gender confirmation procedures that a transmasculine person may undergo include:
- Masculinizing genitoplasty is the surgical creation of external genitalia. This procedure uses the tissue of the labia to create a penis.
- Phalloplasty is the surgical construction of a penis using a skin graft from the forearm, thigh, or upper back.
- Metoidioplasty is the creation of a penis from the hormonally enlarged clitoris.
- Scrotoplasty is the creation of a scrotum.
Procedures that change the genitalia are performed with other procedures, which may be extensive.
The change to a masculine appearance may also include hormone therapy with testosterone, a mastectomy (surgical removal of the breasts), hysterectomy (surgical removal of the uterus), and perhaps additional cosmetic procedures intended to masculinize the appearance.
Paying For Gender Confirmation Surgery
Medicare and some health insurance providers in the United States may cover a portion of the cost of gender confirmation surgery.
It is unlawful to discriminate or withhold healthcare based on sex or gender. However, many plans do have exclusions.
For most transgender individuals, the burden of financing the procedure(s) is the main difficulty in obtaining treatment. The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed.
A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019.
Traveling Abroad for GCS
Some patients seek gender confirmation surgery overseas, as the procedures can be less expensive in some other countries. It is important to remember that traveling to a foreign country for surgery, also known as surgery tourism, can be very risky.
Regardless of where the surgery will be performed, it is essential that your surgeon is skilled in the procedure being performed and that your surgery will be performed in a reputable facility that offers high-quality care.
When choosing a surgeon , it is important to do your research, whether the surgery is performed in the U.S. or elsewhere. Talk to people who have already had the procedure and ask about their experience and their surgeon.
Before and after photos don't tell the whole story, and can easily be altered, so consider asking for a patient reference with whom you can speak.
It is important to remember that surgeons have specialties and to stick with your surgeon's specialty. For example, you may choose to have one surgeon perform a genitoplasty, but another to perform facial surgeries. This may result in more expenses, but it can result in a better outcome.
A Word From Verywell
Gender confirmation surgery is very complex, and the procedures that one person needs to achieve their desired result can be very different from what another person wants.
Each individual's goals for their appearance will be different. For example, one individual may feel strongly that breast implants are essential to having a desirable and feminine appearance, while a different person may not feel that breast size is a concern. A personalized approach is essential to satisfaction because personal appearance is so highly individualized.
Davy Z, Toze M. What is gender dysphoria? A critical systematic narrative review . Transgend Health . 2018;3(1):159-169. doi:10.1089/trgh.2018.0014
Morrison SD, Vyas KS, Motakef S, et al. Facial Feminization: Systematic Review of the Literature . Plast Reconstr Surg. 2016;137(6):1759-70. doi:10.1097/PRS.0000000000002171
Hadj-moussa M, Agarwal S, Ohl DA, Kuzon WM. Masculinizing Genital Gender Confirmation Surgery . Sex Med Rev . 2019;7(1):141-155. doi:10.1016/j.sxmr.2018.06.004
Dowshen NL, Christensen J, Gruschow SM. Health Insurance Coverage of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information . Transgend Health . 2019;4(1):131-135. doi:10.1089/trgh.2018.0055
American Society of Plastic Surgeons. Rhinoplasty nose surgery .
Rights Group: More U.S. Companies Covering Cost of Gender Reassignment Surgery. CNS News. http://cnsnews.com/news/article/rights-group-more-us-companies-covering-cost-gender-reassignment-surgery
The Sex Change Capital of the US. CBS News. http://www.cbsnews.com/2100-3445_162-4423154.html
By Jennifer Whitlock, RN, MSN, FN Jennifer Whitlock, RN, MSN, FNP-C, is a board-certified family nurse practitioner. She has experience in primary care and hospital medicine.
Jump to content
Updated visitor policies
Other michigan medicine sites.
- About Michigan Medicine
- UofMHealth.org
- Medical School
- Find a Clinical Trial

Michigan Medicine
Federated search page form block, quick links.
- Patient Portal Login
- For Health Providers
- Maps & Directions
Gender Confirmation Surgery
The University of Michigan Health System offers procedures for surgical gender transition. Working together, the surgical team of the Comprehensive Gender Services Program, which includes specialists in plastic surgery, urology and gynecology, bring expertise, experience and safety to procedures for our transgender patients.
Access to gender-related surgical procedures for patients is made through the University of Michigan Health System Comprehensive Gender Services Program .
The Comprehensive Gender Services Program adheres to the WPATH Standards of Care , including the requirement for a second-opinion prior to genital sex reassignment.
Available surgeries:
Male-to-Female: Tracheal Shave Breast Augmentation Facial Feminization Male-to-Female genital sex reassignment
Female-to-Male: Hysterectomy, oophorectomy, vaginectomy Chest Reconstruction Female-to-male genital sex reassignment
Sex Reassignment Surgeries (SRS)
At the University of Michigan Health System, we are dedicated to offering the safest proven surgical options for sex reassignment (SRS.) Because sex reassignment surgery is just one step for transitioning people, the Comprehensive Gender Services Program has access to providers for mental health services, hormone therapy, pelvic floor physiotherapy, and speech therapy. Surgical procedures are done by a team that includes, as appropriate, gynecologists, urologists, pelvic pain specialists and a reconstructive plastic surgeon. A multi-disciplinary team helps to best protect the health of the patient.
For patients receiving mental health and medical services within the University of Michigan Health System, the UMHS-CGSP will coordinate all care including surgical referrals. For patients who have prepared for surgery elsewhere, the UMHS-CGSP will help organize the needed records, meet WPATH standards, and coordinate surgical referrals. Surgical referrals are made through Sara Wiener the Comprehensive Gender Services Program Director.
Male-to-female sex reassignment surgery
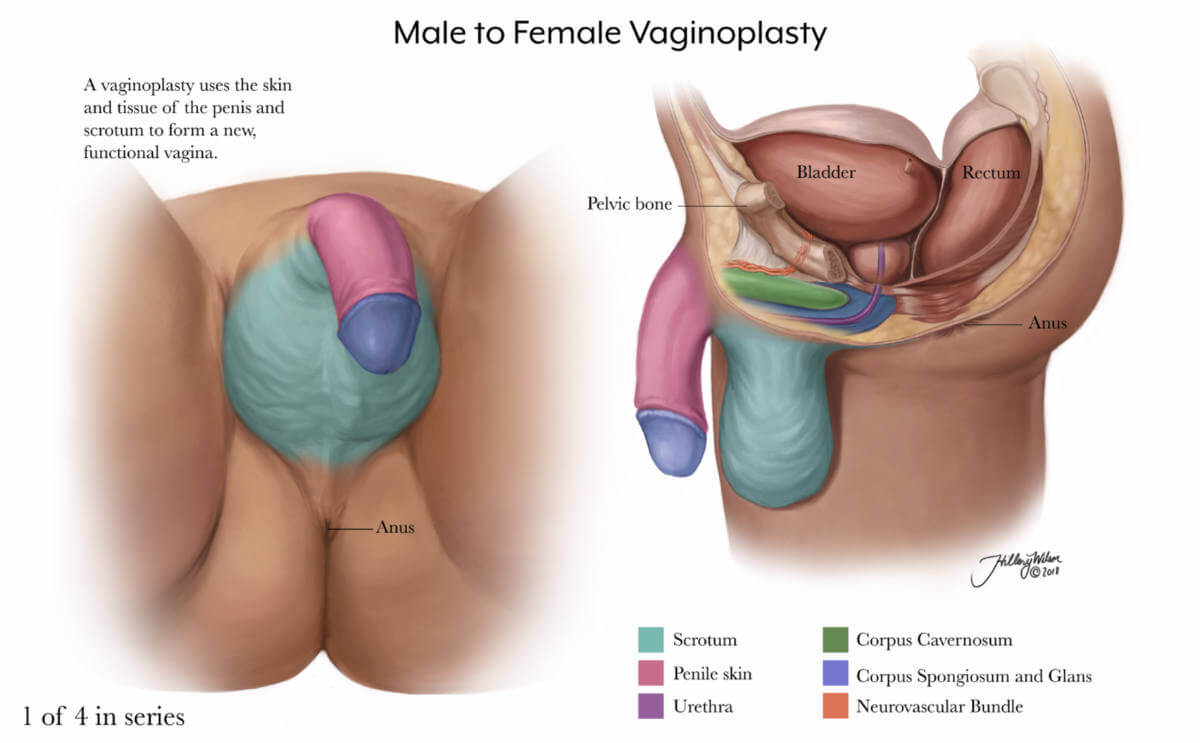
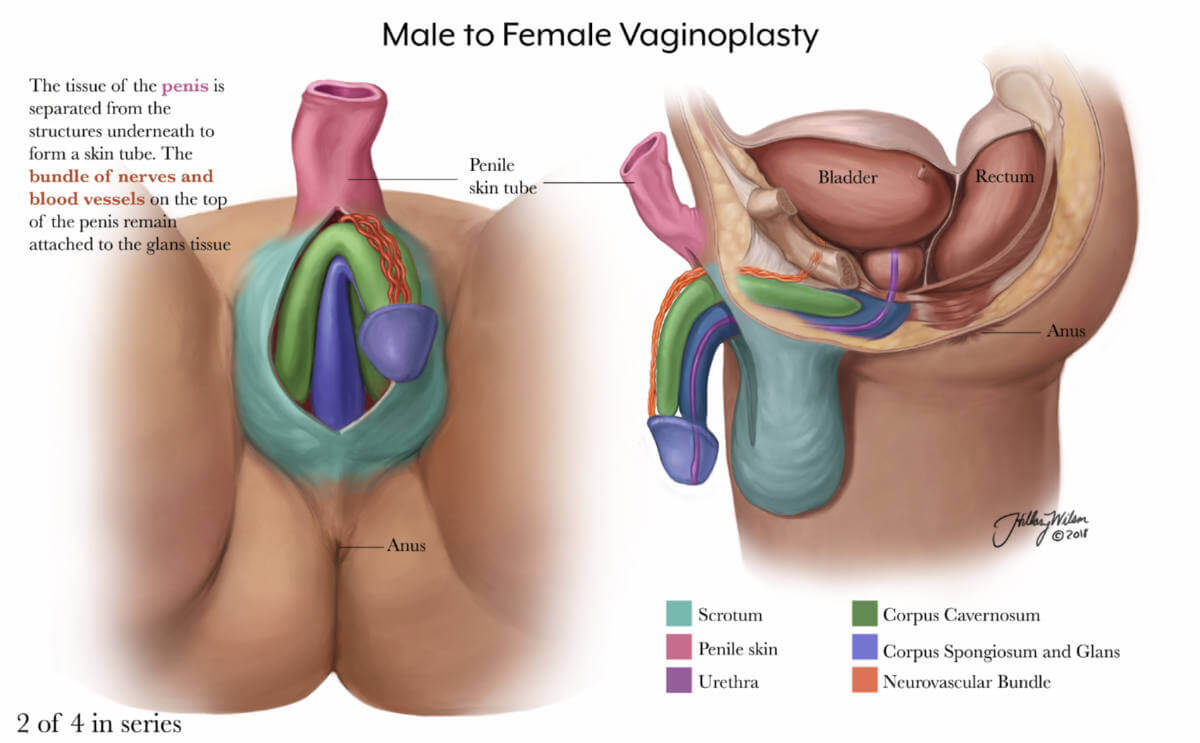
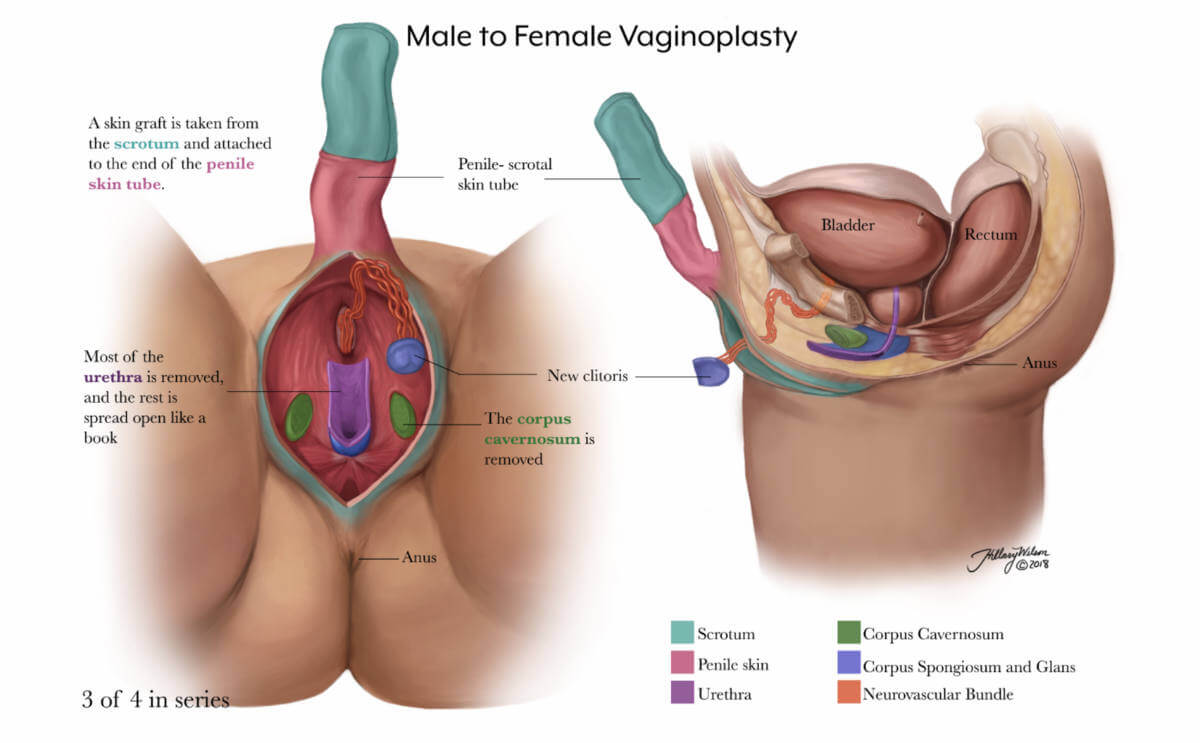
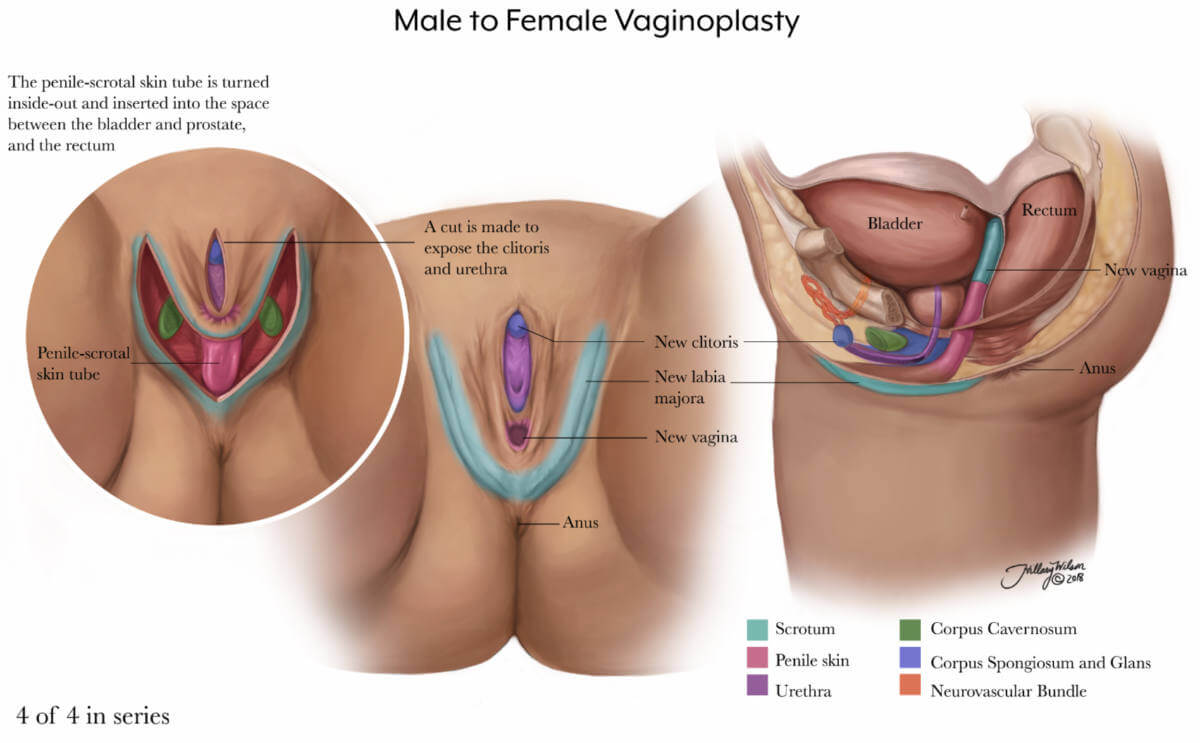
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a male-to-female sex reassignment surgery will be offered a penile inversion vaginoplasty with a neurovascular neoclitoris.
During this procedure, a surgeon makes “like become like,” using parts of the original penis to create a sensate neo-vagina. The testicles are removed, a procedure called orchiectomy. The skin from the scrotum is used to make the labia. The erectile tissue of the penis is used to make the neoclitoris. The urethra is preserved and functional.
This procedure provides for aesthetic and functional female genitalia in one 4-5 hour operation. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation. What to Expect: Vaginoplasty at Michigan Medicine .
Female-to-male sex reassignment
At the University of Michigan, participants of the Comprehensive Gender Services Program who are ready for a female-to-male sex reassignment surgery will be offered a phalloplasty, generally using the radial forearm flap method.
This procedure, which can be done at the same time as a hysterectomy/vaginectomy, creates an aesthetically appropriate phallus and creates a urethera for standing urination. Construction of a scrotum with testicular implants is done as a second stage. The details of the procedure, the course of recovery, the expected outcomes, and the possible complications will be covered in detail during your surgical consultation.
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected] . W e will assist you in obtaining what you need to qualify for surgery.
Advertisement
Stages of Gender Reassignment
- Share Content on Facebook
- Share Content on LinkedIn
- Share Content on Flipboard
- Share Content on Reddit
- Share Content via Email

The idea of getting stuck in the wrong body sounds like the premise for a movie in "Freaky Friday," a mother and a daughter swap bodies, and in "Big" and "13 Going on 30," teenagers experience life in an adult's body. These movies derive their humor from the ways in which the person's attitude and thoughts don't match their appearance. A teenager trapped in her mother's body, for example, revels in breaking curfew and playing air guitar, while a teenager trapped in an adult's body is astounded by the trappings of wealth that come with a full-time job. We laugh because the dialogue and actions are so contrary to what we'd expect from someone who is a mother, or from someone who is an employed adult.
But for some people, living as an incongruous gender is anything but a joke. A transgender person is someone who has a different gender identity than their birth sex would indicate. We interchange the words sex, sexuality and gender all the time, but they don't actually refer to the same thing. Sex refers to the parts we were born with; boys, we assume, have a penis, while girls come equipped with a vagina. Sexuality generally refers to sexual orientation , or who we're attracted to in a sexual and/or romantic sense. Gender expression refers to the behavior used to communicate gender in a given culture. Little girls in the U.S., for example, would be expected express their feminine gender by playing with dolls and wearing dresses, and little boys would be assumed to express their masculinity with penchants for roughhousing and monster trucks. Another term is g ender identity, the private sense or feeling of being either a man or woman, some combination of both or neither [source: American Psychological Association ].
Sometimes, a young boy may want to wear dresses and have tea parties, yet it's nothing more than a phase that eventually subsides. Other times, however, there is a longing to identify with another gender or no gender at all that becomes so intense that the person experiencing it can't function anymore. Transgender is an umbrella term for people who identify outside of the gender they were assigned at birth and for some gender reassignment surgeries are crucial to leading a healthy, happy life.
Gender Dysphoria: Diagnosis and Psychotherapy
Real-life experience, hormone replacement therapy, surgical options: transgender women, surgical options: transgender men, gender reassignment: regrets.

Transgender people may begin identifying with a different gender, rather than the one assigned at birth, in early childhood, which means they can't remember a time they didn't feel shame or distress about their bodies. For other people, that dissatisfaction with their biological sex begins later, perhaps around puberty or early adulthood, though it can occur later in life as well.
It's estimated that about 0.3 percent of the U.S. population self-identify as transgender, but not all who are transgender will choose to undergo a gender transition [source: Gates ]. Some may choose to affirm their new gender through physically transforming their bodies from the top down, while others may prefer to make only certain cosmetic changes, such as surgeries to soften facial features or hair removal procedures, for example.
Not all who identify with a gender different than their birth sex suffer from gender dysphoria or go on to seek surgery. Transgender people who do want gender reassignment surgery, however, must follow the standards of care for gender affirmation as defined by the World Professional Association for Transgender Health (WPATH).
In 1980, when gender identity disorder (GID) was first recognized, it was considered a psychiatric disorder. In 2013, though, GID was, in part, reconsidered as biological in nature, and renamed gender dysphoria . It was reclassified as a medical condition in the American Psychological Association's Diagnostic and Statistical Manual of Mental Disorders (DSM-V), a common language and standards protocol manual for the classification of mental disorders. With this classification, transgender people must be diagnosed prior to any treatment [source: International Foundation for Gender Education ].
Gender dysphoria is diagnosed when a person has a persistent desire to become a different gender. The desire may manifest itself as disgust for one's reproductive organs, hatred for the clothing and other outward signs of one's given gender, and/or a desire to act and be recognized as another gender. This desire must be continuously present for six months in order to be recognized as a disorder [source: WPATH].
In addition to receiving the diagnosis from a mental health professional, a person seeking reassignment must also take part in psychotherapy. The point of therapy isn't to ignite a change, begin a conversion or otherwise convince a transgender person that it's wrong to want to be of a different gender (or of no specific gender at all) . Rather, counseling is required to ensure that the person is realistic about the process of gender affirmation and understands the ramifications of not only going through with social and legal changes but with permanent options such as surgery. And because feeling incongruous with your body can be traumatizing and frustrating, the mental health professional will also work to identify any underlying issues such as anxiety, depression, substance abuse or borderline personality disorder.
The mental health professional can also help to guide the person seeking gender reassignment through the next step of the process: real-life experience.

WPATH requires transgender people desiring gender reassignment surgery to live full-time as the gender that they wish to be before pursuing any permanent options as part of their gender transition. This period is a known as real-life experience (RLE) .
It's during the RLE that the transgender person often chooses a new name appropriate for the desired gender, and begins the legal name-change process. That new name often comes with a set of newly appropriate pronouns, too; for example, when Chastity Bono, biologically born as Sonny and Cher's daughter in 1969, began her transition in 2008 she renamed herself as Chaz and instructed people to use "he" rather than "she" [source: Donaldson James ].
In addition to a new name and pronouns, during this time gender-affirming men and women are expected to also adopt the clothing of their desired gender while maintaining their employment, attending school or volunteering in the community. Trans women might begin undergoing cosmetic procedures to rid themselves of body hair; trans men might take voice coaching in attempt to speak in a lower pitch. The goal of real-life experience is to expose social issues that might arise if the individual were to continue gender reassignment. How, for example, will a boss react if a male employee comes to work as a female? What about family? Or your significant other? Sometimes, during RLE people realize that living as the other gender doesn't bring the happiness they thought it would, and they may not continue to transition. Other times, a social transition is enough, and gender reassignment surgery isn't pursued. And sometimes, this test run is the confirmation people need to pursue physical changes in order to fully become another gender.
In addition to the year-long real-life experience requirement before surgical options may be pursued, WPATH recommends hormonal therapy as a critical component to transitioning before surgery. Candidates for hormone therapy may choose to complete a year-long RLE and counseling or complete six months of a RLE or three-months of a RLE/three months of psychotherapy before moving ahead with hormone therapy.
Upon successfully completing a RLE by demonstrating stable mental health and a healthy lifestyle, the transitioning individual becomes eligible for genital reconstructive surgery — but it can't begin until a mental health professional submits a letter (or letters) of recommendation indicating that the individual is ready to move forward [source: WPATH].

Hormone replacement therapy (HRT) , also called cross-sex hormones, is a way for transgender individuals to feel and look more like the gender they identify with, and so it's a major step in gender reassignment. In order to be eligible for hormone therapy, participants must be at least 18 years old (though sometimes, younger adolescents are allowed to take hormone blockers to prohibit their naturally occurring puberty) and demonstrate to a mental health professional that they have realistic expectations of what the hormones will and won't do to their bodies. A letter from that mental health professional is required, per the standards of care established by WPATH.
Hormone therapy is used to balance a person's gender identity with their body's endocrine system. Male-to-female candidates begin by taking testosterone-blocking agents (or anti-androgens ) along with female hormones such as estrogen and progesterone . This combination of hormones is designed to lead to breast growth, softer skin, less body hair and fewer erections. These hormones also change the body by redistributing body fat to areas where women tend to carry extra weight (such as around the hips) and by decreasing upper body strength. Female-to-male candidates begin taking testosterone , which will deepen the voice and may cause some hair loss or baldness. Testosterone will also cause the clitoris to enlarge and the person's sex drive to increase. Breasts may slightly shrink, while upper body strength will increase [source: WPATH].
It usually takes two continuous years of treatment to see the full results of hormone therapy. If a person were to stop taking the hormones, then some of these changes would reverse themselves. Hormone therapy is not without side effects — both men and women may experience an increased risk for cardiovascular disease, and they are also at risk for fertility problems. Some transgender people may choose to bank sperm or eggs if they wish to have children in the future.
Sometimes hormonal therapy is enough to make a person feel he or she belongs to the desired gender, so treatment stops here. Others may pursue surgical means as part of gender reassignment.

Surgical options are usually considered after at least two years of hormonal therapy, and require two letters of approval by therapists or physicians. These surgeries may or may not be covered by health insurance in the U.S. — often only those that are considered medically necessary to treat gender dysphoria are covered, and they can be expensive. Gender reassignment costs vary based on each person's needs and desires; expenses often range between $7,000 and $50,000 (in 2014), although costs may be much greater depending upon the type (gender reconstructive surgeries versus cosmetic procedures) and number of surgeries as well as where in the world they are performed [source: AP ].
Gender affirmation is done with an interdisciplinary team, which includes mental health professionals, endocrinologists, gynecologists, urologists and reconstructive cosmetic surgeons.
One of the first surgeries male-to-female candidates pursue is breast augmentation, if HRT doesn't enlarge their breasts to their satisfaction. Though breast augmentations are a common procedure for cisgender women (those who identify with the gender they were assigned at birth), care must be taken when operating on a biologically male body, as there are structural differences, like body size, that may affect the outcome.
The surgical options to change male genitalia include orchiectomy (removal of the testicles), penile inversion vaginoplasty (creation of a vagina from the penis), clitoroplasty (creation of a clitoris from the glans of the penis) and labiaplasty (creation of labia from the skin of the scrotum) [source: Nguyen ]. The new vagina, clitoris and labia are typically constructed from the existing penile tissue. Essentially, after the testicles and the inner tissue of the penis is removed and the urethra is shortened, the skin of the penis is turned inside out and fashioned into the external labia and the internal vagina. A clitoris is created from excess erectile tissue, while the glans ends up at the opposite end of the vagina; these two sensitive areas usually mean that orgasm is possible once gender reassignment is complete. Male-to-female gender reconstructive surgery typically takes about four or five hours [source: University of Michigan ]. The major complication from this surgery is collapse of the new vaginal cavity, so after surgery, patients may have to use dilating devices.
Trans women may also choose to undergo cosmetic surgeries to further enhance their femininity. Procedures commonly included with feminization are: blepharoplasty (eyelid surgery); cheek augmentation; chin augmentation; facelift; forehead and brow lift with brow bone reduction and hair line advance; liposuction; rhinoplasty; chondrolargynoplasty or tracheal shave (to reduce the appearance of the Adam's apple); and upper lip shortening [source: The Philadelphia Center for Transgender Surgery]. Trans women may pursue these surgeries with any cosmetic plastic surgeon, but as with breast augmentation, a doctor experienced with this unique situation is preferred. One last surgical option is voice modification surgery , which changes the pitch of the voice (alternatively, there is speech therapy and voice training, as well as training DVDs and audio recordings that promise the same thing).

Female-to-male surgeries are pursued less often than male-to-female surgeries, mostly because when compared to male-to-female surgeries, trans men have limited options; and, historically, successful surgical outcomes haven't been considered on par with those of trans women. Still, more than 80 percent of surgically trans men report having sexual intercourse with orgasm [source: Harrison ].
As with male-to-female transition, female-to-male candidates may begin with breast surgery, although for trans men this comes in the form of a mastectomy. This may be the only surgery that trans men undergo in their reassignment, if only because the genital surgeries available are still far from perfect. Forty percent of trans men who undergo genital reconstructive surgeries experience complications including problems with urinary function, infection and fistulas [sources: Harrison , WPATH].
Female-to-male genital reconstructive surgeries include hysterectomy (removal of the uterus) and salpingo-oophorectomy (removal of the fallopian tubes and ovaries). Patients may then elect to have a metoidioplasty , which is a surgical enlargement of the clitoris so that it can serve as a sort of penis, or, more commonly, a phalloplasty . A phalloplasty includes the creation of a neo-phallus, clitoral transposition, glansplasty and scrotoplasty with prosthetic testicles inserted to complete the appearance.
There are three types of penile implants, also called penile prostheses: The most popular is a three-piece inflatable implant, used in about 75 percent of patients. There are also two-piece inflatable penile implants, used only 15 percent of the time; and non-inflatable (including semi-rigid) implants, which are used in fewer than 10 percent of surgeries. Inflatable implants are expected to last about five to 10 years, while semi-rigid options typically have a lifespan of about 20 years (and fewer complications than inflatable types) [source: Crane ].
As with trans women, trans men may elect for cosmetic surgery that will make them appear more masculine, though the options are slightly more limited; liposuction to reduce fat in areas in which cisgender women i tend to carry it is one of the most commonly performed cosmetic procedures.

As surgical techniques improve, complication rates have fallen too. For instance, long-term complication risks for male-to-female reconstructive surgeries have fallen below 1 percent. Despite any complications, though, the overwhelming majority of people who've undergone surgical reconstruction report they're satisfied with the results [source: Jarolím ]. Other researchers have noted that people who complete their transition process show a marked improvement in mental health and a substantial decrease in substance abuse and depression. Compare these results to 2010 survey findings that revealed that 41 percent of transgender people in the U.S. attempted suicide, and you'll see that finally feeling comfortable in one's own skin can be an immensely positive experience [source: Moskowitz ].
It's difficult, though, to paint a complete picture of what life is like after people transition to a new gender, as many people move to a new place for a fresh start after their transition is complete. For that reason, many researchers, doctors and therapists have lost track of former patients. For some people, that fresh start is essential to living their new lives to the fullest, while others have found that staying in the same job, the same marriage or the same city is just as rewarding and fulfilling and vital to their sense of acceptance.
In many ways, the process of gender affirmation is ongoing. Even after the surgeries and therapies are complete, people will still have to deal with these discrimination issues. Transgender people are often at high risk for hate crimes. Regular follow-ups will be necessary to maintain both physical and mental health, and many people continue to struggle with self-acceptance and self-esteem after struggling with themselves for so long. Still, as more people learn about gender reassignment, it seems possible that that these issues of stigma and discrimination won't be so prevalent.
As many as 91 percent Americans are familiar with the term "transgender" and 76 percent can correctly define it; 89 percent agree that transgender people deserve the same rights, privileges and protections as those who are cisgender [source: Public Religion Research Institute ]. But that's not to say that everything becomes completely easy once a person transitions to his or her desired gender.
Depending upon where you live, non-discrimination laws may or may not cover transgender individuals, so it's completely possible to be fired from one's job or lose one's home due to gender expression. Some people have lost custody of their children after divorces and have been unable to get courts to recognize their parental rights. Historically, some marriages were challenged — consider, for example, what happens when a man who is married to a woman decides to become a woman; after the surgery, if the two people decide to remain married, it now appears to be a same-sex marriage, which is now legalized in the U.S. Some organizations and governments refuse to recognize a person's new gender unless genital reconstructive surgery has been performed, despite the fact that some people only pursue hormone therapy or breast surgery [sources: U.S. Office of Personnel Management , Glicksman ].
Lots More Information
Author's note: stages of gender reassignment.
It's interesting how our terminology changes throughout the years, isn't it? (And in some cases for the better.) What we used to call a sex change operation is now gender realignment surgery. Transsexual is now largely replaced with transgender. And with good reason, I think. Knowing that sex, sexuality and gender aren't interchangeable terms, updating "sex change" to "gender reassignment" or "gender affirmation" and "transsexual" to "transgender" moves the focus away from what sounds like something to do with sexual orientation to one that is a more accurate designation.
Related Articles
- How Gender Identity Disorder Works
- Is gender just a matter of choice?
- What is transgender voice therapy?
- How fluid is gender?
- Why do girls wear pink and boys wear blue?
More Great Links
- DSM-5: Gender Dysphoria
- National Center for Transgender Equality
- The Williams Institute
- American Medical Student Association (AMSA). "Transgender Health Resources." 2014. (April 20, 2015) http://www.amsa.org/AMSA/Homepage/About/Committees/GenderandSexuality/TransgenderHealthCare.aspx
- American Psychological Association (APA). "Definition of Terms: Sex, Gender, Gender Identity, Sexual Orientation." 2011. (July 1, 2015) http://www.apa.org/pi/lgbt/resources/sexuality-definitions.pdf
- AP. "Medicare ban on sex reassignment surgery lifted." May 30, 2014. (April 20, 2015) http://www.usatoday.com/story/news/nation/2014/05/30/medicare-sex-reassignment/9789675/
- Belkin, Lisa. "Smoother Transitions." The New York Times. Sept. 4, 2008. (Aug. 1, 2011) http://www.nytimes.com/2008/09/04/fashion/04WORK.html
- Crane, Curtis. "The Total Guide to Penile Implants For Transsexual Men." Transhealth. May 2, 2014. (April 20, 2015) http://www.trans-health.com/2013/penile-implants-guide/
- Donaldson James, Susan. "Trans Chaz Bono Eyes Risky Surgery to Construct Penis." ABC News. Jan. 6, 2012. (April 20, 2015) http://abcnews.go.com/Health/transgender-chaz-bono-seeks-penis-genital-surgery-risky/story?id=15299871Gates, Gary J. "How many people are lesbian, gay, bisexual, and transgender?" April 2011. (July 29, 2015) http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf
- Glicksman, Eve. "Transgender today." Monitor on Psychology. Vol. 44, no. 4. Page 36. April 2013. (April 20, 2015) http://www.apa.org/monitor/2013/04/transgender.aspx
- Harrison, Laird. "Sex-Change Operations Mostly Successful." Medscape Medical News. May 20, 2013. (April 20, 2015) http://www.medscape.com/viewarticle/804432
- HealthResearchFunding.org (HRF). "14 Unique Gender Identity Disorder Statistics." July 28, 2014. (April 20, 2015) http://healthresearchfunding.org/gender-identity-disorder-statistics/
- International Foundation for Gender Education. "APA DSM-5 Sexual and Gender Identity Disorders: 302.85 Gender Identity Disorder in Adolescents or Adults." (April 20, 2015) http://www.ifge.org/302.85_Gender_Identity_Disorder_in_Adolescents_or_Adults
- Moskowitz, Clara. "High Suicide Risk, Prejudice Plague Transgender People." LiveScience. Nov. 18, 2010. (April 20, 2015) http://www.livescience.com/11208-high-suicide-risk-prejudice-plague-transgender-people.html
- Nguyen, Tuan A. "Male-To-Female Procedures." Lake Oswego Plastic Surgery. 2013. (April 20, 2015) http://www.lakeoswegoplasticsurgery.com/grs/grs_procedures_mtf.html
- Public Religion Research Institute. "Survey: Strong Majorities of Americans Favor Rights and Legal Protections for Transgender People." Nov. 3, 2011. (April 20, 2015) http://publicreligion.org/research/2011/11/american-attitudes-towards-transgender-people/#.VSmlgfnF9bw
- Steinmetz, Katy. "Board Rules That Medicare Can Cover Gender Reassignment Surgery." Time. (April 20, 2015) http://time.com/2800307/medicare-gender-reassignment/
- The Philadelphia Center for Transgender Surgery. "Phalloplasty: Frequently Asked Questions." (April 20, 2015) http://www.thetransgendercenter.com/index.php/surgical-procedures/phalloplasty-faqs.html
- U.S. Office of Personnel Management. "Guidance Regarding the Employment of Transgender Individuals in the Federal Workplace." 2015. (April 20, 2015) http://www.opm.gov/diversity/Transgender/Guidance.asp
- University of California, San Francisco - Department of Family and Community Medicine, Center of Excellence for Transgender Health. "Primary Care Protocol for Transgender Patient Care." April 2011. (April 20, 2015) http://transhealth.ucsf.edu/trans?page=protocol-hormones
- University of Miami - Miller School of Medicine, Department of Surgery, Plastic, Aesthetic and Reconstructive Surgery. "Transgender Reassignment." 2015. (April 20, 2015) http://surgery.med.miami.edu/plastic-and-reconstructive/transgender-reassignment-surgery
- University of Michigan Health System. "Gender Affirming Surgery." (April 20, 2015) http://www.uofmhealth.org/medical-services/gender-affirming-surgery
- World Professional Association for Transgender Health (WPATH). "Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People." Version 7. 2012. (April 20, 2015) http://www.wpath.org/uploaded_files/140/files/Standards%20of%20Care,%20V7%20Full%20Book.pdf
- World Professional Association for Transgender Health (WPATH). "WPATH Clarification on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage for Transgender and Transsexual People Worldwide." 2015. (April 20, 2015) http://www.wpath.org/site_page.cfm?pk_association_webpage_menu=1352&pk_association_webpage=3947
Please copy/paste the following text to properly cite this HowStuffWorks.com article:

- FIND A PROVIDER
I'm a Candidate
I'm a Provider
Log In / Sign Up
I'm a candidate
Provider login
I'm a provider
List your practice
MTF Gender Confirmation: Genital Construction
The specifics, the takeaway.
Download the app
As part of a transgender individual’s transition, genital reassignment surgery alters male genitalia into female genitalia.
Written By: Erin Storm, PA-C
Published: October 07, 2021
Last updated: February 18, 2022
- Procedure Overview
- Ideal Candidate
- Side Effects
- Average Cost
thumbs-up Pros
- Can Help Complete A Gender Affirmation Journey
thumbs-down Cons
- Potentially Cost Prohibitive
Invasiveness Score
Invasiveness is graded based on factors such as anesthesia practices, incisions, and recovery notes common to this procedure.
Average Recovery
Application.
Surgical Procedure
$ 7000 - $ 24000
What is a male to female (MTF) gender reassignment surgery?
Male to female (MTF) gender reassignment surgery is also known as sex reassignment surgery (SRS), genital construction, and generally as Gender Confirmation Surgery. These procedures are used to remove and alter male genitalia into traditional female genitalia. Plastic surgeons will remove the scrotum, perform a penile inversion to create the neovagina, remove and alter penile erectile tissue to form the clitoral tissue of the clitoris, and construct labia usually from scrotal tissue. The prostate gland is left intact. These procedures create fully functional female genitalia in transgender patients.
Typically gender reassignment surgery is performed as a last step in a transgender individuals transition journey. Guidelines from The World Professional Association for Transgender Health (WPATH) state candidates must have letters of recommendation from their mental health provider and physician, have been living full time as a woman for one year, and have completed one year of hormonal therapy to be eligible.
Information on facial feminization surgeries, top surgeries (like a breast construction), and other male to female gender affirming surgeries as part of a gender transition for transwomen can be found in our comprehensive guide to MTF gender affirmation solutions .
What concerns does a MTF gender reassignment surgery treat?
- Transfeminine Bottom Surgery & Genital Construction : Male to female gender reassignment surgery creates female genitalia that are aesthetically authentic and functional. A vaginoplasty, penectomy, orchiectomy (testicle removal), clitoroplasty, and labiaplasty are typically performed.
Who is the ideal candidate for a MTF gender reassignment surgery?
The ideal candidate for MTF gender reassignment surgery is a transgender women seeking to complete her physical embodiment of her gender identity. This reconstructive genital surgery creates functioning female genitalia.
MTF gender reassignment surgery is not recommended for those who have not been on hormone therapy for one year, have not been living full time as a woman for one year, do not have letters of recommendation from their mental health provider and physician, children under the age of 18, and those with certain chronic medical conditions.
What is the average recovery associated with a MTF gender reassignment surgery?
Most patients experience four to six weeks of recovery time following a MTF gender reassignment surgery. Patients can expect bruising, swelling, and tenderness following the procedure. A urinary catheter is placed for one week and vaginal packing as well which may cause a sensation of fullness. Vaginal dilation is a component of the procedure and the patient will be advised on how to complete this progressive dilation at home over the course of a few weeks.
What are the potential side effects of a MTF gender reassignment surgery?
Possible side effects following a MTF gender reassignment surgery include bleeding, swelling, bruising, site infection, altered sensation, difficulty urinating, difficulty with sexual function, prolonged edema, and complications from anesthesia or the procedure.
What can someone expect from the results of a MTF gender reassignment surgery?
The results of MTF gender reassignment surgery are permanent. This procedure creates functional female genitalia and removes all male genitalia. The prostate gland is left intact which is important for transgender individuals ongoing healthcare and preventative screenings.
What is the average cost of a MTF gender reassignment surgery?
What to expect.
A MTF Gender Reassignment Surgery creates female genitalia. Here is a quick guide for what to expect before, during, and after a MTF Gender Reassignment Surgery:
Before Surgery
- Prophylactic antibiotics or antivirals may be prescribed
- Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol, Aspirin, and prescription anticoagulants
- Stop smoking four weeks prior to the procedure and continue cessation for four weeks post op
- No alcohol two days prior to the procedure
- Do not eat or drink six hours before
During Surgery
- General anesthesia
- A penile inversion is performed to create the vaginal canal
- The scrotum is removed
- Skin grafts are used to create the labia and vulva
- Erectile tissue is removed from the new vaginal walls, and erectile tissue from the head of the penis is used to create the clitoris
- The urethra is shortened
Immediately After Treatment
- Swelling, bruising, and tenderness
1 - 30 After Treatment & Beyond
- Resume most activities after a few days
- Swelling typically resolves within a few weeks
- Avoid strenuous activity for two to four weeks
- Remove urinary catheter and vaginal packing after one week
- Continue progressive vaginal dilation
Result Notes
- Results are permanent
- Proper aftercare will ensure optimal results
Gender confirmation surgeries for transgender individuals are an important component of transgender health and in creating an embodied gender identity. Gender reassignment surgery allows transgender women who feel it is a part of their transition to more fully embrace their gender identity.
To learn more about our content creation practices, visit our Editorial Process page .
Source List
AEDIT uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- American Society of Plastic Surgeons Gender Confirmation Surgeries plasticsurgery.org
- Karel E Y Claes Chest Surgery for Transgender and Gender Nonconforming Individuals PubMed.gov ; 2018-07-02
Related Procedures

MTF Gender Confirmation Solutions

MTF Gender Confirmation: Facial Feminization

Adam’s Apple Reduction

MTF Gender Confirmation: Transfeminine Top & Bottom Surgeries
View all procedures
Learn More About MTF Gender Confirmation: Genital Construction in The AEDITION

Gender Transitioning And Skincare: Taking Care Of Your Changing Face
Side effects of hormone therapy often show up on the skin in the form of acne, pigmentation, and uneven skin texture. Here’s what you need to know about the most common skin concerns and treatment options.

A Guide To Non-Surgical Facial Feminization
Facial feminization procedures have been gaining popularity among men hoping to look more approachable or transition to female as well as among women hoping to have a more feminine appearance.

Finding The Right Plastic Surgeon, Dermatologist, Or Cosmetic Dentist
When considering a cosmetic procedure, it is so important to find the right doctor for you.
Discover more articles

‘Try on’ aesthetic procedures and instantly visualize possible results with AEDIT and our patented 3D aesthetic simulator.
Find Top Aesthetic Providers Near You
Providers by locations.
- Alpharetta, GA Providers
- Bay Harbor Islands, FL Providers
- Chevy Chase, MD Providers
- Fall River, MA Providers
- Glenview, IL Providers
- Lone Tree, CO Providers
- Metairie, LA Providers
- More Locations
- New Haven, CT Providers
- Newport Beach, CA Providers
- Prairie Village, KS Providers
- Scottsdale, AZ Providers
- Southfield, MI Providers
- Springdale, AR Providers
- Washington, DC Providers
Providers by Specialties
- Cosmetic Dentistry Providers
- Cosmetic Dermatology Providers
- Cosmetic Surgery Providers
- Dermatologic Surgery Providers
- Dermatology Providers
- Facial Plastic and Reconstructive Surgery Providers
- General Surgery Providers
- Hair Restoration Surgery Providers
- Head and Neck Surgery Providers
- Medspa Providers
- More Procedures
- Oculoplastic Surgery Providers
- Other Providers
- Plastic and Reconstructive Surgery Providers
- Vaginal Rejuvenation Providers
Providers by Procedures
- Acne Scar Treatment Providers
- Acne Treatment Providers
- Birthmark Removal Providers
- Blepharoplasty Providers
- Botox Providers
- Brow Lift Providers
- Buccal Fat Removal (Cheek Reduction) Providers
- Cheek Augmentation (Cheek Implants) Providers
- Cheek Surgery Providers
- Chemical Peels Providers
- Chin Surgery (Mentoplasty) Providers
- Dental Treatments Providers
- Dermabrasion Treatment Providers
- Dermal Fillers & Injectables Providers
- More Specialties
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Vaginoplasty for Gender Affirmation
Featured Experts:

Fan Liang, M.D.

Andrew Jason Cohen, M.D.
Vaginoplasty is a surgical procedure for feminizing gender affirmation. Fan Liang, M.D. , medical director of the Johns Hopkins Center for Transgender and Gender Expansive Health , and Andrew Cohen, M.D. , director of benign urology at Johns Hopkins' Brady Urological Institute , review the options for surgery.
What is vaginoplasty?
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum.
During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a feminine-appearing outer genital area with a shallow vaginal canal.
What are the different types of vaginoplasty?
There are two main surgical approaches for this gender affirming surgery.
Vaginoplasty with Canal
This surgery is also known as full depth vaginoplasty. Vaginoplasty with canal creates not only the outer vulva but also a complete vaginal canal that makes it possible for the person to have receptive vaginal intercourse.
Vaginoplasty with canal requires dilation as part of the recovery process in order to ensure a functioning vagina suitable for penetrative sex. There are two approaches to full depth vaginoplasty.
For penile inversion vaginoplasty , surgeons create the vaginal canal using a combination of the skin surrounding the existing penis along with the scrotal skin. Depending on how much skin is available in the genital area, the surgeon may need to use a skin graft from the abdomen or thigh to construct a full vaginal canal.
Robotic-assisted peritoneal flap vaginoplasty , also called a robotic Davydov peritoneal vaginoplasty or a robotic peritoneal gender affirming vaginoplasty, is a newer approach that creates the vaginal canal with the help of a single port robotic surgical system.
The robotic system enables surgeons to reach deep into the body through a small incision by the belly button. It helps surgeons visualize the inside of the person’s pelvis more clearly and, for this procedure, creates a vaginal canal.
There are several advantages to this surgical technique. Because using the robotic system makes the surgery shorter and more precise, with a smaller incision, it can lower risk of complications. Also, the robotic vaginoplasty approach can create a full-depth vaginal canal regardless of how much preexisting (natal) tissue the person has for the surgeon to use in making the canal.
Not every surgical center has access to a single port robotic system, and getting this procedure may involve travel.
Vulvoplasty
This procedure may be called shallow depth vaginoplasty, zero depth vaginoplasty or vaginoplasty without canal. The surgeons create feminine external genitalia (vulva) with a very shallow canal. The procedure includes the creation of the labia (outer and inner lips), clitoris and vaginal opening (introitus).
The main drawback to this approach is the person cannot have receptive vaginal intercourse because no canal is created.
There are advantages, however. Because this is a much less complicated approach than vaginoplasty with canal, vulvoplasty can mean a much shorter operation, with less time in the hospital and a faster recovery. Vulvoplasty also involves less risk of complications, and does not require hair removal or postoperative dilation.
Do I need to have hair removal before vaginoplasty? When should I start?
Permanent hair removal (to remove the hair follicles to prevent regrowth) before surgery is recommended for optimal results. Patients are advised to start hair removal as soon as possible in advance of vaginoplasty, since it can take three to six months to complete the process. The hair removal process readies the tissue that will be used to create the internal vaginal canal. For people who are not able to complete the hair removal in advance, there may be residual hair in the canal after surgery.
How long is vaginoplasty surgery?
Most vaginoplasty surgeries last between four and six hours. Recovery in the hospital takes three to five days.
Illustrated Vaginoplasty Surgery
Vaginoplasty.
1 of 4 in series. Enlarged image .
2 of 4 in series. Enlarged image .
3 of 4 in series. Enlarged image .
4 of 4 in series. Enlarged image .
Recovery After Vaginoplasty
After surgery, you will be admitted to the hospital for one to five days. You will spend most of this time in bed recovering. Your care team will monitor your pain, and make sure you are healing appropriately and are able to go to the bathroom and walk.
On average, it can take six to eight weeks to recover from a vaginoplasty. Every person’s recovery is different, but proper home hygiene and postoperative care will give you the best chance for a faster recovery. Patients who have had vaginoplasties need to stay within a 90-minute drive of the hospital for four weeks after surgery so doctors can follow up and address any issues.
Consistent daily dilation for the first three months is essential for best outcome. Before you go home, you will be taught how to dilate if you have a vaginoplasty with canal. You will be given dilators before discharge to use at home.
What is dilation after vaginoplasty?
Part of the healing process after vaginoplasty involves dilation — inserting a medical grade dilator into the vagina to keep your vaginal canal open as it heals. The hospital may provide you with a set of different sized dilators to use.
A doctor or therapist from your care team will show you how to dilate. This can be difficult at first, but professionals will work with you and your comfort level to help you get accustomed to this aspect of your healing process. You will begin dilating with the smallest dilator in the dilator pack. You continue to use this dilator until cleared to advance to the next size by your care team.
During the first few weeks after surgery, you must dilate three times a day for at least 20 minutes. It is very important that you continue dilating, especially during your immediate postoperative period, to prevent losing vaginal depth and width. Patients continue to use a dilator for as long as the care team recommends. Some patients may need to dilate their whole lives.
Is dilation after vaginoplasty painful?
Dilation should not be a painful process. At first, you may feel discomfort as you learn the easiest angles and techniques for your body. If you feel severe pain at any time during dilation, it is important to stop, adjust the dilator, and reposition your body so you are more comfortable. It is also important to use lubricant when you dilate. A pelvic floor therapist can work with you to help you get used to this aspect of recovery.
Will I have a catheter?
Yes. While you are in the hospital, you will have a Foley catheter in the urethra that will be taken out before you go home.
Will I have surgical drains?
Yes, your surgeon will place a drain while you are in the operating room, which will be removed before you leave.
Can I shower after vaginoplasty surgery?
Yes. It is very important to clean the area to prevent infections. You can gently wash the area with soap and water. Never scrub or allow water to be sprayed directly at the surgical site.
Is going to the bathroom different?
It is important to remember for the rest of your life that when wiping with toilet paper or washing the genital area, always wipe front to back. This helps keep your vagina clean and prevents infection from the anal region.
You may notice some spraying when you urinate. This is common, and can be addressed with physical therapy to help strengthen the pelvic floor. A physical therapist can help you with exercises, which may help improve urination over time.
Is the vagina created by vaginoplasty sexually functional?
Yes. After vaginoplasty that includes creation of a vaginal canal, a person can have receptive, penetrative sex.
You must avoid any form of sexual activity for 12 weeks after surgery to allow your body to recover and avoid complications. After 12 weeks, the vagina is healed enough for receptive intercourse.
What will my vagina look like?
Vulvas and vaginas are as unique as a fingerprint, and there are many anatomic variations from person to person. Surgical results vary, also. You can expect that the surgery will recreate the labia minora and majora, a clitoral hood and the clitoris will be under the hood. Make sure you discuss your concerns with your surgeon, who can help you understand what to expect from your individual surgical results.
What is the average depth of a vagina after vaginoplasty?
The depth of a fully constructed vaginal canal depends on patient preferences and anatomy. On average, the constructed vaginal canal is between 5 and 7 inches deep. Vaginal depth may depend on the amount of skin available in the genital area before your vaginoplasty. This varies among individuals, and some patients may need skin grafts.
Newer robotic techniques may be able to increase the vaginal depth for those people with less existing tissue for the surgeon to work with.
Will I need any additional surgery after vaginoplasty?
You may need additional surgical procedures to revise the appearance of the new vagina and vulva. Later revisions can improve aesthetic appearance, but these are not typically covered by insurance.
Vaginoplasty Complications
Vaginoplasty is safe, overall, and newer techniques are reducing the risks of problems even further. But sometimes, patients experience complications related to the procedure. These can include:
- Slow wound healing
- Narrowing of the vaginal canal (regular dilating as prescribed can lower this risk)
Some rare complications may require further surgery to repair:
- A fistula (an abnormal connection between the new vagina and the rectum or bladder)
- Injury to the urethra, which may require surgery or a suprapubic catheter
- Rectal injury (very rare) may require a low-fiber diet, a colostomy or additional surgery.
Be sure to discuss your concerns with your surgeon, who will work with you for optimal results.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
- Plastic and Reconstructive Surgery
Find Additional Treatment Centers at:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital

Request an Appointment

Phalloplasty for Gender Affirmation

Top Surgery

Facial Feminization Surgery (FFS)
Related Topics
- LGBTQ Health
- Gender Affirmation
Road closure on Marquam Hill: Part of S.W. Campus Drive is closed until March 2025.
Transgender Health Program
Gender-affirming surgery.
OHSU surgeons are leaders in gender-diverse care. We provide specialized services tailored to the needs and goals of each patient. We offer:
- Specialists who do hundreds of surgeries a year.
- Plastic surgeons, urologists and other specialists who are leading experts in bottom surgery, top surgery and other gender-affirming options.
- Vocal surgery with a highly trained ear, nose and throat doctor.
- Peer volunteers who can provide support during visits.
- Welcoming care for every patient, every gender and every journey.
Our surgical services
We offer many gender-affirming surgery options for transgender and nonbinary patients, including options within the following types. We also welcome you to request a procedure that isn’t listed on our pages.
Top surgery:
- Gender-affirming mastectomy
- Gender-affirming breast augmentation
Bottom surgery:
- Phalloplasty and metoidioplasty , including vagina-preserving options
- Vaginoplasty and vulvoplasty , including penile-preserving options
Hysterectomy
Nullification surgery, oophorectomy, orchiectomy.
Bottom surgery options also include:
- Scrotectomy
- Scrotoplasty
- Urethroplasty
- Vaginectomy
Additional gender-affirming options:
- Adam’s apple surgery
Vocal surgery
Face and body surgery, preparing for surgery.
Please see our patient guide page to learn about:
- Steps to surgery
- WPATH standards of care
- The letter of support needed for some surgeries
For patients
Request services.
Please fill out an online form:
- I am seeking services for myself.
- I am seeking services for someone else.
Other questions and concerns
Contact us at:
- 503-494-7970
- [email protected]
Refer a patient
- Please complete our Request for Transgender Health Services referral form and fax with relevant medical records to 503-346-6854 .
- Learn more on our For Health Care Professionals page.
At OHSU, our gynecologic surgeon, Dr. Lishiana Shaffer, specializes in hysterectomies (uterus and cervix removal; often combined with oophorectomy, or ovary removal) for gender-diverse patients. She does more than 150 a year.
We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Some patients choose hysterectomy to:
- More closely align their bodies with their gender identity.
- With ovary removal, to remove a main source of the hormone estrogen.
- To end pain caused by testosterone therapy that shrinks the uterus.
- To end the need for some gynecologic exams, such Pap smears.
Preparation: We usually recommend a year of hormone therapy first, to shrink the uterus. We don’t require a year of social transition.
How hysterectomy is done
Most often, we use a minimally invasive laparoscope and small incisions in the belly. We usually recommend removing fallopian tubes as well, to greatly reduce the risk of ovarian cancer.
Most patients spend one night in the hospital. Recovery typically takes about two weeks. You’re encouraged to walk during that time but to avoid heavy lifting or strenuous exercise.
Considerations and risks
Hysterectomy is usually safe, and we have a low rate of complications. Risks can include blood clots, infection and scar tissue. Because of a possible link between hysterectomy and higher risk of cardiovascular disease, your doctors may recommend regular tests.
Removing the uterus also ends the ability to carry a child. OHSU fertility experts offer options such as egg freezing before treatment, and connecting patients with a surrogacy service.
OHSU offers nullification surgery to create a gender-neutral look in the groin area.
Nullification surgery may include:
- Removing the penis (penectomy)
- Removing the testicles (orchiectomy)
- Reducing or removing the scrotum (scrotectomy)
- Shortening the urethra
- Removing the uterus (hysterectomy)
- Removing the vagina (vaginectomy)
The procedure takes several hours. Patients can expect to spend one to two nights in the hospital. Recovery typically takes six to eight weeks. Patients are asked to limit walking and to stick to light to moderate activity for four weeks. They should wait three months before bicycling or strenuous activity.
Nullification surgery cannot be reversed. Risks can include:
- Changes in sensation
- Dissatisfaction with the final look
- Healing problems
Removing the penis and testicles or the uterus also affects the ability to conceive a child. OHSU fertility experts offer options such as freezing eggs and connecting patients with a surrogacy service.
Having a gynecologic surgeon remove one or both ovaries is often done at the same time as a hysterectomy. We do nearly all these surgeries with a minimally invasive laparoscope and small incisions in the belly.
Most patients spend one night in the hospital and return to their regular routine in about two weeks.
The ovaries produce estrogen, which helps prevent bone loss and the thickening of arteries. After removal, a patient should be monitored long-term for the risk of osteoporosis and cardiovascular disease.
We encourage patients to keep at least one ovary to preserve fertility without egg freezing. This also preserves some hormone production, which can avoid early menopause.
At OHSU, expert urologists do orchiectomies (testicle removal). Patients may choose this option:
- To remove the body’s source of testosterone
- As part of a vaginoplasty or vulvoplasty (surgeries that create a vagina and/or vulva)
- To relieve dysphoria (some patients choose only this surgery)
Removing the testicles usually means a patient can stop taking a testosterone blocker. Patients may also be able to lower estrogen therapy.
How orchiectomy is done
The surgeon makes an incision in the scrotum. The testicles and the spermatic cord, which supplies blood, are removed. Scrotal skin is removed only if the patient specifically requests it. The skin is used if the patient plans a vaginoplasty or vulvoplasty.
You will probably go home the same day. Patients can typically resume normal activities in a week or two.
Reducing testosterone production may increase the risk of bone loss and cardiovascular disease, so we recommend regular tests. Without prior fertility treatment, orchiectomy also ends the ability to produce children. Serious risks are uncommon but include bleeding, infection, nerve damage and scarring.
Adam’s apple reduction (laryngochrondoplasty)
Dr. Joshua Schindler, an ear, nose and throat doctor who does Adam’s apple and vocal surgeries, completed his training at Johns Hopkins University.
Laryngochrondoplasty is also known as Adam’s apple reduction or a tracheal shave (though the trachea, or windpipe, is not affected).
A surgeon removes thyroid cartilage at the front of the throat to give your neck a smoother appearance. This procedure can often be combined with facial surgery.
Thin incision: At OHSU, this procedure can be done by an ear, nose and throat doctor (otolaryngologist) with detailed knowledge of the neck’s anatomy. The surgeon uses a thin incision, tucked into a neck line or fold. It can also be done by one of our plastic surgeons, typically with other facial surgery.
In an office or an operating room: Our team can do a laryngochrondoplasty in either setting, which may limit a patient’s out-of-pocket expenses.
OHSU also offers Adams’ apple enhancement surgery.
Many patients find that hormone therapy and speech therapy help them achieve a voice that reflects their identity. For others, vocal surgery can be added to raise the voice’s pitch.
Voice therapy: Patients have voice and communication therapy before we consider vocal surgery. Your surgeon and your speech therapist will assess your voice with tests such as videostroboscopy (allowing us to see how your vocal cords work) and acoustic voice analysis.
Effective surgery: We use a surgery called a Wendler glottoplasty. It’s done through the mouth under general anesthesia. The surgeon creates a small controlled scar between the two vocal cords, shortening them to increase tension and raise pitch. Unlike techniques that can lose effectiveness over time, this surgery offers permanent results.
Hormone therapy can bring out desired traits, but it can’t change the underlying structure or remove hair follicles. Our highly trained surgeons and other specialists offer options. Patients usually go home the same day or spend one night in a private room.
Face options:
- Browlift (done with the forehead)
- Cheek augmentation
- Chin surgery (genioplasty), including reductive, implants or bone-cut options
- Eyelid surgery
- Face-lift, neck lift
- Forehead lengthening
- Forehead reduction, including Type 3 sinus setback and orbital remodeling
- Hairline advancement (done with the forehead)
- Jawline contouring
- Lip lift and/or augmentation
- Lipofilling (transferring fat using liposuction and filling)
- Nose job (rhinoplasty)
Body options:
Hormone treatment may not result in fat distribution consistent with your gender. We offer liposuction and fat grafting to reshape areas of the body.
Ontario.ca needs JavaScript to function properly and provide you with a fast, stable experience.
To have a better experience, you need to:
- Go to your browser's settings
- Enable JavaScript
Gender confirming surgery
How to apply for gender confirming surgery (also known as sex reassignment surgery) in Ontario. If you are eligible, this service is covered under OHIP .
As of March 1, you can seek an assessment for surgery from qualified health care providers across the province.
On this page Skip this page navigation
Affirming gender identity.
Gender confirming surgery (also known as sex reassignment or gender affirming surgery) does more than change a person’s body. It affirms how they think and feel about their own gender and what it means to who they are.
Ontario is funding surgery as an option for people who experience discomfort or distress with their sex or gender at birth.
How to qualify
Ontario funds two types of gender-confirming surgery: genital and chest.
To qualify for funding, you must:
- be assessed and recommended for surgery by either one or two healthcare providers (e.g. a qualified doctor, nurse practitioner, registered nurse, psychologist or registered social worker)
- have a referral for surgery completed and submitted to the Ministry of Health and Long-Term Care by a physician or nurse practitioner; and
- have the surgery approved by the Ministry of Health and Long-Term Care before the surgery takes place
Approval for genital surgery
To be approved for genital surgery, you’ll need:
- one of the assessments must be from a doctor or nurse practitioner
- you have a diagnosis of persistent gender dysphoria
- have completed 12 continuous months of hormone therapy (unless hormones are not recommended)
- you have lived 12 continuous months in the gender role you identify with (for genital surgery only)
If you have surgery before getting approval from the ministry, the cost of the surgery will not be covered.
Approval for chest surgery
To be approved for chest surgery you’ll need:
- have a diagnosis of persistent gender dysphoria
- have completed 12 months of continuous hormone therapy with no breast enlargement (unless hormones are not recommended) if you’re seeking breast augmentation
After being approved for chest surgery, your family doctor or nurse practitioner can refer you to a specialist who can perform the surgery.
Apply for surgery
To apply for gender confirming surgery, your doctor or nurse practitioner needs to fill out and submit the application along with the assessments and recommendations for surgery, to the Ministry of Health and Long-Term Care. The application is for patients seeking services in Ontario, out of province but within Canada or outside of the country.
Your doctor or nurse practitioner will let you know if your application is approved.
Once you receive approval from the ministry, talk with your health care provider to get ready for the surgery
Additional resources
You can find useful information from organizations, such as:
- find out about their ongoing project, Trans Health Connection
- consult their service directory
- find out about the Gender Identity Clinic (Adult)
Information for healthcare providers
Find out more about your role in providing gender-confirming surgery funded by Ontario.
- Search Close Search submit
Procedure: Male to Female Gender Reassignment Surgery (MTF GRS)
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of labia major/minor, clitoris and neovagina simultaneously.
The patient who is fit for this surgery must strictly follow the standard of care set by the World Professional Association of Transgender Healthcare (WPATH) or equivalent criteria; Express desire or live in another gender role (Male gender) long enough, under hormonal replacement therapy, evaluated and approved by a psychiatrist or other qualified professional gender therapist.
Apart from genital surgery, the patient would seek other procedures to allow them to live as female smoothly such as breast aesthetic surgery, facial feminization surgery, body contouring, hair removal, voice change surgery, etc.
Interested in having this procedure?
Useful Information
Ensure you consider all aspects of a procedure. You can speak to your surgeon about these areas of the surgery in more detail during a consultation.
The surgery is quite complicated and only a handful of surgeons are able to perform this procedure. It can be completed in one stage or more stages depending on techniques and surgeons. The average surgical time ranges between 5-8 hours. There are several options of neovaginal construction depending on the type of tissue, single or in combination, such as penile skin, scrotal skin, large intestine, small intestine, or peritoneum.
The procedure is done under general anesthesia and might be combined with spinal anesthesia for faster recovery by reducing the usage of anesthetic gas.
Inpatient/Outpatient
The patient will be hospitalized as an in-patient for between 5-14 days depending on the technique and surgeon. The patient will have a urinary catheter at all times in the hospital.
Additional Information
What is the recovery process.
During hospitalization, the patient must be restricted in bed continuously or intermittently for several days between 3-5 days. After release from the hospital, the patient can return to their normal lives but not have to do physical exercise during the first 2 months after surgery. The patient has to do vaginal dilation continuously for 6 months to maintain the neovagina canal until completely healed and is ready for sexual intimacy.
What are the results?
With the good surgical technique, the result is very satisfying with an improved quality of life. The patient is able to live in a female role completely and happily either on their own or with their male or female partners.
What are the risks?
The most frequent complication of MTF GRS is bleeding, wound infection, skin flap or graft necrosis, urinary stenosis, neovaginal contracture, unsightly scar or deformed genitalia, vaginal fistula, etc. The revision procedures to improve external appearance are composed of secondary labiaplasty/ urethroplasty/ perineoplasty/ and vulvaplasty. The other revision procedure is secondary vaginoplasty to help the patient able to have sexual intimacy with the partner.
- Patient Information
- Global Statistics
- Media Centre
- Global Sponsors
- Privacy Policy
19 Mantua Road, Mount Royal, NJ 08061 United States
Registration number: 0330131
US Office: +1-603-643-2325
UK Office: +44 20 7038 7812
© 2022 International Society of Aesthetic Plastic Surgery. All Rights Reserved.
- Create an account
Log into My ISAPS
Forgot your password? Reset it here
Join the ISAPS Community
All members will continue to receive information relevant to their membership and ISAPS events.
I confirm by clicking below I would like to receive information about:

Welcome to the ISAPS community
By creating an account, you can:.
- Register for events
- Update your personal details
- Gain access to ISAPS publications and video library
- Become a member (explore our memberships here)
ISAPS Members can also:
- Access your member benefits
- Secure discounted member rates for events
- Read the Aesthetic Plastic Surgery Journal
- Gain full access to the video library
- View the Members Directory
- Update your 'Find a Surgeon' profile details
- Renew/Upgrade your Membership
The first step to becoming a part of the community is creating an account, so join us!
How Gender Reassignment Surgery Works (Infographic)
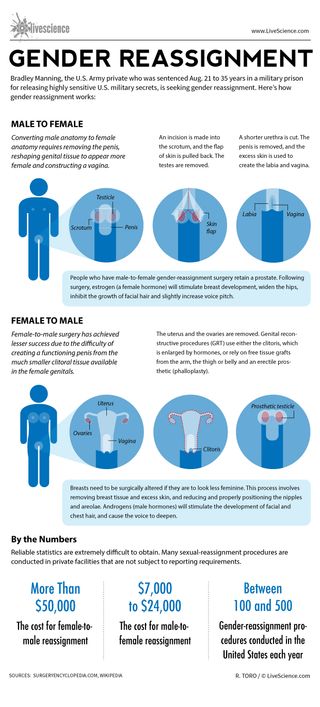
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Scientists made mice with Y chromosomes female by deleting just 6 tiny molecules
Man's years of premature ejaculation had a rare cause
'Lovely freak of nature': Mutant blue frog hops into wildlife sanctuary workshop
Most Popular
- 2 2,000 years ago, a bridge in Switzerland collapsed on top of Celtic sacrifice victims, new study suggests
- 3 What causes you to get a 'stitch in your side'?
- 4 What defines a species? Inside the fierce debate that's rocking biology to its core
- 5 Self-healing 'living skin' can make robots more humanlike — and it looks just as creepy as you'd expect
- 2 What causes you to get a 'stitch in your side'?
- 3 Tasselled wobbegong: The master of disguise that can eat a shark almost as big as itself
- 4 Self-healing 'living skin' can make robots more humanlike — and it looks just as creepy as you'd expect
- 5 This robot could leap higher than the Statue of Liberty — if we ever build it properly
Give your feedback to help us improve our website This is the new Equality and Human Rights Commission website
- Gender reassignment discrimination
Published: 22 December 2021
Last updated: 23 February 2023
On this page
What the equality act says about gender reassignment discrimination, different types of gender reassignment discrimination, circumstances when being treated differently due to gender reassignment is lawful, pages in this guide.
- Your rights under the Equality Act 2010
- Age discrimination
- Disability discrimination
- Marriage and civil partnership discrimination
- Pregnancy and maternity discrimination
- Race discrimination
- Religion or belief discrimination
- Sex discrimination
- Sexual orientation discrimination
- Terms used in the Equality Act
- Harassment and victimisation
- Direct and indirect discrimination
What countries does this apply to?
On this page we have used plain English to help explain legal terms. This does not change the meaning of the law.
The Equality Act 2010 uses the term ‘transsexual’ for individuals who have the protected characteristic of gender reassignment. We recognise that some people consider this term outdated, so we have used the term ‘trans’ to refer to a person who has the protected characteristic of gender reassignment. However, we note that some people who identify as trans may not fall within the legal definition.
This page is subject to updates due to the evolving nature of some of the issues highlighted.
This is when you are treated differently because you are trans in one of the situations covered by the Equality Act . The treatment could be a one-off action or as a result of a rule or policy. It doesn’t have to be intentional to be unlawful.
There are some circumstances when being treated differently due to being trans is lawful. These are explained below.
The Equality Act 2010 says that you must not be discriminated against because of gender reassignment.
In the Equality Act, gender reassignment means proposing to undergo, undergoing or having undergone a process to reassign your sex.
To be protected from gender reassignment discrimination, you do not need to have undergone any medical treatment or surgery to change from your birth sex to your preferred gender.
You can be at any stage in the transition process, from proposing to reassign your sex, undergoing a process of reassignment, or having completed it. It does not matter whether or not you have applied for or obtained a Gender Recognition Certificate, which is the document that confirms the change of a person's legal sex.
For example, a person who was born female and decides to spend the rest of their life as a man, and a person who was born male and has been living as a woman for some time and obtained a Gender Recognition Certificate, both have the protected characteristic of gender reassignment.
There are four types of gender reassignment discrimination.
Direct discrimination
Direct discrimination happens when someone treats you worse than another person in a similar situation because you are trans.
You inform your employer that you intend to spend the rest of your life living as the opposite sex. If your employer alters your role against your wishes to avoid you having contact with clients, this would be direct gender reassignment discrimination.
The Equality Act says that you must not be directly discriminated against because:
- you have the protected characteristic of gender reassignment. A wide range of people identify as trans. However, you are not protected under the Equality Act unless you have proposed, started or completed a process to change your sex.
- someone thinks you have the protected characteristic of gender reassignment. For example, because you occasionally cross-dress or do not conform to gender stereotypes (this is known as discrimination by perception).
- you are connected to a person who has the protected characteristic of gender reassignment, or someone wrongly thought to have this protected characteristic (this is known as discrimination by association).
Absences from work
If you are absent from work because of your gender reassignment, your employer cannot treat you worse than you would be treated if you were absent:
- due to an illness or injury.
Example –
Your employer cannot pay you less than you would have received if you were off sick.
- due to some other reason - however, in this case it is only discrimination if your employer is acting unreasonably.
If your employer would agree to a request for time off for someone to attend their child’s graduation ceremony, then it may be unreasonable to refuse you time off for part of a gender reassignment process. This would include, for example, time off for counselling.
Indirect discrimination
Indirect discrimination happens when an organisation has a particular policy or way of working that puts people with the protected characteristic of gender reassignment at a disadvantage. Sometimes indirect gender reassignment discrimination can be permitted if the organisation or employer is able to show that there is a good reason for the discrimination. This is known as objective justification .
An employer has a practice of starting induction sessions for new staff with an ice-breaker designed to introduce everyone in the room to each other. Each worker is required to provide a picture of themselves as a toddler. One worker is a trans woman who does not wish her colleagues to know that she was brought up as a boy, so she does not bring her photo and is criticised by the employer in front of the group for not joining in. The same approach is taken for all new staff, but it puts people with the protected characteristic of gender reassignment at a particular disadvantage. This would be unlawful indirect discrimination unless the employer could show that the practice was justified.
Harassment is when someone makes you feel humiliated, offended or degraded for reasons related to gender reassignment.
A person who has undergone male-to-female gender reassignment is having a drink in a pub with friends and the landlord keeps calling her ‘sir’ or ‘he’ when serving drinks, despite her complaining about it.
Harassment can never be justified. However, if an organisation or employer can show it did everything it could to prevent people who work for it from harassing you, you will not be able to make a claim for harassment against the organisation, only against the harasser.
Victimisation
Victimisation is when you are treated badly because you have made a complaint of gender reassignment discrimination under the Equality Act. It can also occur if you are supporting someone who has made a complaint of gender reassignment discrimination.
A person proposing to undergo gender reassignment is being harassed by a colleague at work. He makes a complaint about the way his colleague is treating him and is sacked.
A difference in treatment may sometimes be lawful. This will be the case where the circumstances fall under one of the exceptions in the Equality Act that allow organisations to provide different treatment or services on the basis of gender reassignment.
Examples –
The organisers of a women’s triathlon event decide to exclude a trans woman with a Gender Recognition Certificate as they think her strength or stamina gives her an unfair advantage. However, the organisers would need to be able to show that this was necessary to make the event fair or safe for everyone.
A service provider provides single-sex services. The Equality Act allows a lawfully established separate or single-sex service provider to prevent, limit or modify people’s access on the basis of gender reassignment in some circumstances. However, limiting or modifying access to, or excluding a trans person from, the separate or single-sex service of the gender in which they present will be unlawful if you cannot show such action is a proportionate means of achieving a legitimate aim. This applies whether or not the person has a Gender Recognition Certificate.
Updated: 23 Feb 2023
- Removed paragraph on language recommendations made by Women and Equalities Committee (WEC) in 2016
- Removed the term ‘transsexual’ as per WEC 2016 recommendations
- Added paragraph explaining use of plain English in the guidance
- Removed a paragraph on intersex people not being explicitly protected from discrimination by the Equality Act
Page updates
22 December 2021
Last updated:
23 February 2023
Advice and support
If you think you might have been treated unfairly and want further advice, you can contact the Equality Advisory and Support Service (EASS) .
The EASS is an independent advice service, not operated by the Equality and Human Rights Commission.
Phone: 0808 800 0082
Call the EASS on:
0808 800 0082
Was this page useful? Yes No
Thank you for your feedback
Help us to improve this website
Why isn't this page helpful.
Please tell us more about why this page is not helpful. We can't reply, so, if you need help with a problem, find out where to go for advice.
Do not include personal information such as e-mail, telephone number or address.
What kind of problem are you experiencing on this page?
Stay informed.
Sign up to receive our email newsletter for the latest news, legal action and guidance.

Gender Affirming Surgery
- Clinical Policy Bulletins
- Medical Clinical Policy Bulletins
Number: 0615
Table Of Contents
| --> This Clinical Policy Bulletin addresses gender affirming surgery. : Some plans may cover gender affirming procedures in addition to the following policy. Please check the specific benefit plan documents. Aetna considers gender affirming surgery medically necessary when criteria for each of the following procedures is met: ) assessing the transgender/gender diverse individual’s readiness for physical treatment; ); ) assessing the transgender/gender diverse individual’s readiness for physical treatments; ); ) assessing the transgender/gender diverse individual’s readiness for physical treatments; ); ) assessing the transgender/gender diverse individual’s readiness for physical treatments; );Gender-specific services may be medically necessary for transgender persons appropriate to their anatomy. Examples include: Aetna considers reversal of gender affirming surgery (performing surgical procedures to return anatomy to that of the sex assigned at birth) medically necessary for persons who regret their gender-related surgical intervention, where applicable requirements for gender affirming surgery listed above are met. Aetna considers gonadotropin-releasing hormone medically necessary to suppress puberty in trans identified adolescents if they meet World Professional Association for Transgender Health (WPATH) criteria (see ). Aetna considers more than one breast augmentation not medically necessary. This does not include the medically necessary replacement of breast implants (see ). Aetna considers the following procedures that may be performed as a component of a gender transition as not medically necessary and cosmetic (not an all-inclusive list) (see also ): -->
The International Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) and the Diagnostic and Statistical Manual of Mental Disorders, (DSM-5-TR) are the diagnostic classifications and criteria manuals used in the United States. Notwithstanding, the World Professional Association of Transgender Health Standard of Care 8th edition (WPATH SOC8) states: “While Gender Dysphoria (GD) is still considered a mental health condition in the Diagnostic and Statistical Manual of Mental Disorders, (DSM-5-TR) of the American Psychiatric Association. Gender incongruence is no longer seen as pathological or a mental disorder in the world health community. Gender Incongruence is recognized as a condition in the International Classification of Diseases and Related Health Problems, 11th Version of the World Health Organization (ICD-11). Because of historical and current stigma, TGD people can experience distress or dysphoria that may be addressed with various gender-affirming treatment options. While nomenclature is subject to change and new terminology and classifications may be adopted by various health organizations or administrative bodies, the medical necessity of treatment and care is clearly recognized for the many people who experience dissonance between their sex assigned at birth and their gender identity.” Gender dysphoria refers to discomfort or distress that is caused by a discrepancy between an individual’s gender identity and the gender assigned at birth (and the associated gender role and/or primary and secondary sex characteristics). A diagnosis of gender dysphoria requires a marked difference between the individual’s expressed/experienced gender and the gender others would assign him or her, and it must continue for at least six months. This condition may cause clinically significant distress or impairment in social, occupational or other important areas of functioning. Gender affirming surgery is performed to change primary and/or secondary sex characteristics. For transfeminine (assigned male at birth) gender transition, surgical procedures may include genital reconstruction (vaginoplasty, penectomy, orchidectomy, clitoroplasty), breast augmentation (implants, lipofilling), and cosmetic surgery (facial reshaping, rhinoplasty, abdominoplasty, thyroid chondroplasty (laryngeal shaving), voice modification surgery (vocal cord shortening), hair transplants) (Day, 2002). For transmasculine (assigned female at birth) gender transition, surgical procedures may include mastectomy, genital reconstruction (phalloplasty, genitoplasty, hysterectomy, bilateral oophorectomy), mastectomy, and cosmetic procedures to enhance male features such as pectoral implants and chest wall recontouring (Day, 2002). The criterion noted above for some types of genital surgeries is based on expert clinical consensus that this experience provides ample opportunity for patients to experience and socially adjust in their desired gender role, before undergoing irreversible surgery (Coleman, et al., 2022). It is recommended that transfeminine persons undergo feminizing hormone therapy (minimum 6 months) prior to breast augmentation surgery. The purpose is to maximize breast growth in order to obtain better surgical (aesthetic) results. In addition to hormone therapy and gender affirming surgery, psychological adjustments are necessary in affirming sex. Treatment should focus on psychological adjustment, with hormone therapy and gender affirming surgery being viewed as confirmatory procedures dependent on adequate psychological adjustment. Mental health care may need to be continued after gender affirming surgery. The overall success of treatment depends partly on the technical success of the surgery, but more crucially on the psychological adjustment of the trans identified person and the support from family, friends, employers and the medical profession. Nakatsuka (2012) noted that the third versions of the guideline for treatment of people with gender dysphoria (GD) of the Japanese Society of Psychiatry and Neurology recommends that feminizing/masculinizing hormone therapy and genital surgery should not be carried out until 18 years old and 20 years old, respectively. On the other hand, the sixth (2001) and the seventh (2011) versions of the standards of care for the health of transsexual, transgender, and gender non-conforming people of World Professional Association for Transgender Health (WPATH) recommend that transgender adolescents (Tanner stage 2, [mainly 12 to 13 years of age]) are treated by the endocrinologists to suppress puberty with gonadotropin-releasing hormone (GnRH) agonists until age 16 years old, after which gender-affirming hormones may be given. A questionnaire on 181 people with GID diagnosed in the Okayama University Hospital (Japan) showed that female to male (FTM) trans identified individuals hoped to begin masculinizing hormone therapy at age of 15.6 +/- 4.0 (mean +/- S.D.) whereas male to female (MTF) trans identified individuals hoped to begin feminizing hormone therapy as early as age 12.5 +/- 4.0, before presenting secondary sex characters. After confirmation of strong and persistent trans gender identification, adolescents with GD should be treated with gender-affirming hormone or puberty-delaying hormone to prevent developing undesired sex characters. These treatments may prevent transgender adolescents from attempting suicide, suffering from depression, and refusing to attend school. Spack (2013) stated that GD is poorly understood from both mechanistic and clinical standpoints. Awareness of the condition appears to be increasing, probably because of greater societal acceptance and available hormonal treatment. Therapeutic options include hormone and surgical treatments but may be limited by insurance coverage because costs are high. For patients seeking MTF affirmation, hormone treatment includes estrogens, finasteride, spironolactone, and GnRH analogs. Surgical options include feminizing genital and facial surgery, breast augmentation, and various fat transplantations. For patients seeking a FTM gender affirmation, medical therapy includes testosterone and GnRH analogs and surgical therapy includes mammoplasty and phalloplasty. Medical therapy for both FTM and MTF can be started in early puberty, although long-term effects are not known. All patients considering treatment need counseling and medical monitoring. Leinung and colleagues (2013) noted that the Endocrine Society's recently published clinical practice guidelines for the treatment of transgender persons acknowledged the need for further information on transgender health. These investigators reported the experience of one provider with the endocrine treatment of transgender persons over the past 2 decades. Data on demographics, clinical response to treatment, and psychosocial status were collected on all transgender persons receiving gender-affirming hormone therapy since 1991 at the endocrinology clinic at Albany Medical Center, a tertiary care referral center serving upstate New York. Through 2009, a total 192 MTF and 50 FTM transgender persons were seen. These patients had a high prevalence of mental health and psychiatric problems (over 50 %), with low rates of employment and high levels of disability. Mental health and psychiatric problems were inversely correlated with age at presentation. The prevalence of gender affirming surgery was low (31 % for MTF). The number of persons seeking treatment has increased substantially in recent years. Gender-affirming hormone therapy achieves very good results in FTM persons and is most successful in MTF persons when initiated at younger ages. The authors concluded that transgender persons seeking hormonal therapy are being seen with increasing frequency. The dysphoria present in many transgender persons is associated with significant mood disorders that interfere with successful careers. They stated that starting therapy at an earlier age may lessen the negative impact on mental health and lead to improved social outcomes. Meyer-Bahlburg (2013) summarized for the practicing endocrinologist the current literature on the psychobiology of the development of gender identity and its variants in individuals with disorders of sex development or with transgenderism. Gender reassignment remains the treatment of choice for strong and persistent gender dysphoria in both categories, but more research is needed on the short-term and long-term effects of puberty-suppressing medications and cross-sex hormones on brain and behavior. Note on Breast Reduction/Mastectomy and Nipple ReconstructionThe CPT codes for mastectomy (CPT codes 19303) are for breast cancer, and are not appropriate to bill for reduction mammaplasty for female to male (transmasculine) gender affirmation surgery. CPT 2020 states that “Mastectomy procedures (with the exception of gynecomastia [19300]) are performed either for treatment or prevention of breast cancer.” CPT 2020 also states that "Code 19303 describes total removal of ipsilateral breast tissue with or without removal of skin and/or nipples (eg, nipple-sparing), for treatment or prevention of breast cancer.” There are important differences between a mastectomy for breast cancer and a mastectomy for gender reassignment. The former requires careful attention to removal of all breast tissue to reduce the risk of cancer. By contrast, careful removal of all breast tissue is not essential in mastectomy for gender reassignment. In mastectomy for gender reassignment, the nipple areola complex typically can be preserved. Some have tried to justify routinely billing CPT code 19350 for nipple reconstruction at the time of mastectomy for gender reassignment based upon the frequent need to reduce the size of the areola to give it a male appearance. However, the nipple reconstruction as defined by CPT code 19350 describes a much more involved procedure than areola reduction. The typical patient vignette for CPT code 19350, according to the AMA, is as follows: “The patient is measured in the standing position to ensure even balanced position for a location of the nipple and areola graft on the right breast. Under local anesthesia, a Skate flap is elevated at the site selected for the nipple reconstruction and constructed. A full-thickness skin graft is taken from the right groin to reconstruct the areola. The right groin donor site is closed primarily in layers.” The AMA vignette for CPT code 19318 (reduction mammaplasty) clarifies that this CPT code includes the work that is necessary to reposition and reshape the nipple to create an aesthetically pleasing result, as is necessary in female to male breast reduction. "The physician reduces the size of the breast, removing wedges of skin and breast tissue from a female patient. The physician makes a circular skin incision above the nipple, in the position to which the nipple will be elevated. Another skin incision is made around the circumference of the nipple. Two incisions are made from the circular cut above the nipple to the fold beneath the breast, one on either side of the nipple, creating a keyhole shaped skin and breast incision. Wedges of skin and breast tissue are removed until the desired size is achieved. Bleeding vessels may be ligated or cauterized. The physician elevates the nipple and its pedicle of subcutaneous tissue to its new position and sutures the nipple pedicle with layered closure. The remaining incision is repaired with layered closure" (EncoderPro, 2019). CPT code 19350 does not describe the work that that is being done, because that code describes the actual construction of a new nipple. Code 19350 is a CCI “incidental to” edit to code 19318, and, accordingly, the services of code 19350 are included in code 19318. Similarly, graft codes, such as code 15200 (full thickness skin graft) and 15877 (liposuction), are CCI “incidental to” edits to code 19318, and, accordingly, the services of graft codes, such as 15200, and liposuction codes, such as 15877, are included in code 19318. Vulvoplasty Versus Vaginoplasty as Gender-Affirming Genital Surgery for Transgender WomenJiang and colleagues (2018) noted that gender-affirming vaginoplasty aims to create the external female genitalia (vulva) as well as the internal vaginal canal; however, not all patients desire nor can safely undergo vaginal canal creation. These investigators described the factors influencing patient choice or surgeon recommendation of vulvoplasty (creation of the external appearance of female genitalia without creation of a neovaginal canal) and evaluated the patient's satisfaction with this choice. Gender-affirming genital surgery consults were reviewed from March 2015 until December 2017, and patients scheduled for or who had completed vulvoplasty were interviewed by telephone. These investigators reported demographic data and the reasons for choosing vulvoplasty as gender-affirming surgery for patients who either completed or were scheduled for surgery, in addition to patient reports of satisfaction with choice of surgery, satisfaction with the surgery itself, and sexual activity after surgery. A total of 486 patients were seen in consultation for trans-feminine gender-affirming genital surgery: 396 requested vaginoplasty and 39 patients requested vulvoplasty; 30 Patients either completed or are scheduled for vulvoplasty. Vulvoplasty patients were older and had higher body mass index (BMI) than those seeking vaginoplasty. The majority (63 %) of the patients seeking vulvoplasty chose this surgery despite no contraindications to vaginoplasty. The remaining patients had risk factors leading the surgeon to recommend vulvoplasty. Of those who completed surgery, 93 % were satisfied with the surgery and their decision for vulvoplasty. The authors concluded that this was the first study of factors impacting a patient's choice of or a surgeon's recommendation for vulvoplasty over vaginoplasty as gender-affirming genital surgery; it also was the first reported series of patients undergoing vulvoplasty only. Drawbacks of this study included its retrospective nature, non-validated questions, short-term follow-up, and selection bias in how vulvoplasty was offered. Vulvoplasty is a form of gender-affirming feminizing surgery that does not involve creation of a neovagina, and it is associated with high satisfaction and low decision regret. Autologous Fibroblast-Seeded Amnion for Reconstruction of Neo-vagina in Transfeminine Reassignment SurgerySeyed-Forootan and colleagues (2018) stated that plastic surgeons have used several methods for the construction of neo-vaginas, including the utilization of penile skin, free skin grafts, small bowel or recto-sigmoid grafts, an amnion graft, and cultured cells. These researchers compared the results of amnion grafts with amnion seeded with autograft fibroblasts. Over 8 years, these investigators compared the results of 24 male-to-female transsexual patients retrospectively based on their complications and levels of satisfaction; 16 patients in group A received amnion grafts with fibroblasts, and the patients in group B received only amnion grafts without any additional cellular lining. The depths, sizes, secretions, and sensations of the vaginas were evaluated. The patients were monitored for any complications, including over-secretion, stenosis, stricture, fistula formation, infection, and bleeding. The mean age of group A was 28 ± 4 years and group B was 32 ± 3 years. Patients were followed-up from 30 months to 8 years (mean of 36 ± 4) after surgery. The depth of the vaginas for group A was 14 to 16 and 13 to 16 cm for group B. There was no stenosis in neither group. The diameter of the vaginal opening was 34 to 38 mm in group A and 33 to 38 cm in group B. These researchers only had 2 cases of stricture in the neo-vagina in group B, but no stricture was recorded for group A. All of the patients had good and acceptable sensation in the neo-vagina; 75 % of patients had sexual experience and of those, 93.7 % in group A and 87.5% in group B expressed satisfaction. The authors concluded that the creation of a neo-vaginal canal and its lining with allograft amnion and seeded autologous fibroblasts is an effective method for imitating a normal vagina. The size of neo-vagina, secretion, sensation, and orgasm was good and proper. More than 93.7 % of patients had satisfaction with sexual intercourse. They stated that amnion seeded with fibroblasts extracted from the patient's own cells will result in a vagina with the proper size and moisture that can eliminate the need for long-term dilatation. The constructed vagina has a 2-layer structure and is much more resistant to trauma and laceration. No cases of stenosis or stricture were recorded. Level of Evidence = IV. These preliminary findings need to be validated by well-designed studies. Pitch-Raising Surgery in Transfeminine PersonsVan Damme and colleagues (2017) reviewed the evidence of the effectiveness of pitch-raising surgery performed in male-to-female transsexuals. These investigators carried out a search for studies in PubMed, Web of Science, Science Direct, EBSCOhost, Google Scholar, and the references in retrieved manuscripts, using as keywords "transsexual" or "transgender" combined with terms related to voice surgery. They included 8 studies using cricothyroid approximation, 6 studies using anterior glottal web formation, and 6 studies using other surgery types or a combination of surgical techniques, leading to 20 studies in total. Objectively, a substantial rise in post-operative fundamental frequency was identified. Perceptually, mainly laryngeal web formation appeared risky for decreasing voice quality. The majority of patients appeared satisfied with the outcome. However, none of the studies used a control group and randomization process. The authors concluded that future research needs to investigate long-term effects of pitch-raising surgery using a stronger study design. Azul and associates (2017) evaluated the currently available discursive and empirical data relating to those aspects of trans-masculine people's vocal situations that are not primarily gender-related, and identified restrictions to voice function that have been observed in this population, and made suggestions for future voice research and clinical practice. These researchers conducted a comprehensive review of the voice literature. Publications were identified by searching 6 electronic databases and bibliographies of relevant articles. A total of 22 publications met inclusion criteria. Discourses and empirical data were analyzed for factors and practices that impact on voice function and for indications of voice function-related problems in trans-masculine people. The quality of the evidence was appraised. The extent and quality of studies investigating trans-masculine people's voice function was found to be limited. There was mixed evidence to suggest that trans-masculine people might experience restrictions to a range of domains of voice function, including vocal power, vocal control/stability, glottal function, pitch range/variability, vocal endurance, and voice quality. The authors concluded that more research into the different factors and practices affecting trans-masculine people's voice function that took account of a range of parameters of voice function and considered participants' self-evaluations is needed to establish how functional voice production can be best supported in this population. Facial Feminization SurgeryRaffaini and colleagues (2016) stated that gender dysphoria refers to the discomfort and distress that arise from a discrepancy between a person's gender identity and sex assigned at birth. The treatment plan for gender dysphoria varies and can include psychotherapy, hormone treatment, and gender affirmation surgery, which is, in part, an irreversible change of sexual identity. Procedures for transformation to the female sex include facial feminization surgery, vaginoplasty, clitoroplasty, and breast augmentation. Facial feminization surgery can include forehead re-modeling, rhinoplasty, mentoplasty, thyroid chondroplasty, and voice alteration procedures. These investigators reported patient satisfaction following facial feminization surgery, including outcome measurements after forehead slippage and chin re-modeling. A total of 33 patients between 19 and 40 years of age were referred for facial feminization surgery between January of 2003 and December of 2013, for a total of 180 procedures. Surgical outcome was analyzed both subjectively through questionnaires administered to patients and objectively by serial photographs. Most facial feminization surgery procedures could be safely completed in 6 months, barring complications. All patients showed excellent cosmetic results and were satisfied with their procedures. Both frontal and profile views achieved a loss of masculine features. The authors concluded that patient satisfaction following facial feminization surgery was high; they stated that the reduction of gender dysphoria had psychological and social benefits and significantly affected patient outcome. The level of evidence of this study was IV. Morrison and associates (2018) noted that facial feminization surgery encompasses a broad range of cranio-maxillofacial surgical procedures designed to change masculine facial features into feminine features. The surgical principles of facial feminization surgery could be applied to male-to-female transsexuals and anyone desiring feminization of the face. Although the prevalence of these procedures is difficult to quantify, because of the rising prevalence of transgenderism (approximately 1 in 14,000 men) along with improved insurance coverage for gender-confirming surgery, surgeons versed in techniques, outcomes, and challenges of facial feminization surgery are needed. These researchers appraised the current facial feminization surgery literature. They carried out a comprehensive literature search of the Medline, PubMed, and Embase databases was conducted for studies published through October 2014 with multiple search terms related to facial feminization. Data on techniques, outcomes, complications, and patient satisfaction were collected. A total of 15 articles were selected and reviewed from the 24 identified, all of which were either retrospective or case series/reports. Articles covered a variety of facial feminization procedures. A total of 1,121 patients underwent facial feminization surgery, with 7 complications reported, although many articles did not explicitly comment on complications. Satisfaction was high, although most studies did not use validated or quantified approaches to address satisfaction. The authors concluded that facial feminization surgery appeared to be safe and satisfactory for patients. These researchers stated that further studies are needed to better compare different techniques to more robustly establish best practices; prospective studies and patient-reported outcomes are needed to establish quality-of-life (QOL) outcomes for patients. In a systematic review, Gorbea et al (2021) provided a portrait of gender affirmation surgery (GAS) insurance coverage across the U.S., with attention to procedures of the head and neck. State policies on transgender care for Medicaid insurance providers were collected for all 50 states. Each state's policy on GAS and facial gender affirmation surgery (FGAS) was examined. The largest medical insurance companies in the U.S. were identified using the National Association of Insurance Commissioners Market Share report. Policies of the top 49 primary commercial medical insurance companies were examined. Medicaid policy reviews found that 18 states offer some level of gender-affirming coverage for their patients, but only 3 include FGAS (17 %); 13 states prohibit Medicaid coverage of all transgender surgery, and 19 states have no published gender-affirming medical care coverage policy; 92 % of commercial medical insurance providers had a published policy on GAS coverage. Genital reconstruction was described as a medically necessary aspect of transgender care in 100 % of the commercial policies reviewed; 93 % discussed coverage of FGAS, but 51 % considered these procedures cosmetic. Thyroid chondroplasty (20 %) was the most commonly covered FGAS procedure. Mandibular and frontal bone contouring, rhinoplasty, blepharoplasty, and facial rhytidectomy were each covered by 13 % of the medical policies reviewed. The authors concluded that while certain surgical aspects of gender-affirming medical care are nearly ubiquitously covered by commercial insurance providers, FGAS is considered cosmetic by most Medicaid and commercial insurance providers. Level of Evidence = V. Hohman and Teixeira (2022) stated that with respect to gender affirmation procedures for the face, the majority of interventions will occur in patients transitioning from male to female, i.e., transgender women. While there are slightly more transgender women than transgender men in the population (33 % transgender women, 29 % transgender men, 35 % non-binary, 3 % cross-dressers, according to the USTS), the reason that more females require surgery than males is that testosterone therapy typically produces enough changes in secondary sex characteristics of the face (growth of facial hair, thickening of the skin, increase in frontal bossing, lowering of the voice, etc.) that surgery is not necessary . In some cases, placement of implants or fat transfer can increase volume in the lower 1/3 of the face and contribute to masculinization. Still, the primary area of focus for facial feminization is generally the upper 1/3. Feminization of the upper 1/3 of the face often requires several techniques to be applied in combination: The advancement of the hairline, hair transplantation, brow-lifting, and reduction of frontal bossing or "frontal cranioplasty". While the advancement of a scalp flap, hair transplant, and pretrichial brow-lifting are commonly employed cosmetic surgery interventions, frontal cranioplasty bears special consideration. Several methods of reducing the brow's prominence are often described as type 1, 2, and 3 frontal cranioplasties. Type 1 cranioplasty reduces the supra-orbital ridge's protrusion, usually using a drill, including decreasing the thickness of the anterior table of the frontal sinus. This technique is the simplest, but it is only effective in patients with either a very thick anterior frontal sinus table or an absent pneumatized frontal sinus. Type 2 cranioplasty involves augmentation of the forehead's convexity using bone cement or methyl methacrylate in addition to a reduction of the supra-orbital ridge with a drill. Type 3 cranioplasty is advocated by many prominent facial feminization surgeons and consists of removal of the anterior table of the frontal sinus, thinning of the bone flap, and replacement of that bone onto the frontal sinus but in a more recessed position, in addition to a reduction of the remainder of the supra-orbital ridge. An alternative to removal and recession of the frontal sinus's anterior table is to thin the bone with a drill and then fracture it in a controlled fashion to produce the desired contour, which is also performed routinely by some authors. Forehead Feminization CranioplastyEggerstedt and colleagues (2020) stated that forehead feminization cranioplasty (FFC) is an important component of gender-affirming surgery and has become increasingly popular in recent years. However, there is little objective evidence for the procedure's safety and clinical impact via patient-reported outcome measures (PROMs). In a systematic review, these researchers determined what complications are observed following FFC, the relative frequency of complications by surgical technique, and what impact the procedure has on patient's QOL. They carried out database searches in PubMed/Medline, Scopus, CINAHL, Cochrane CENTRAL, Cochrane Database of Systematic Reviews, and PsycINFO. The search terms included variations of forehead setback/FFC. Both controlled vocabularies (i.e., MeSH and CINAHL's Suggested Subject Terms) and keywords in the title or abstract fields were searched. Two independent reviewers screened the titles and abstracts of all articles; and 2 independent surgeon reviewers examined the full text of all included articles, and relevant data points were extracted. Main outcomes and measures included complications and complication rate observed following FFC. Additional outcome measures were the approach used, concurrent procedures carried out, and the use and findings of a PROM. A total of 10 articles describing FFC were included, entailing 673 patients. The overall pooled complication rate was 1.3 %; PROMs were used in 50 % of studies, with no standardization among studies. The authors concluded that complications following FFC were rare and infrequently required reoperation. Moreover, these researchers stated that further studies into standardized and validated PROMs in facial feminization patients are needed. Level of Evidence = III. Hand Feminization and MasculinizationLee and colleagues (2021) noted that anatomical characteristics that are incongruent with an individual's gender identity can cause significant gender dysphoria. Hands exhibit prominent dimorphic sexual features, but despite their visibility, there are limited studies examining gender affirming procedures for the hands. These researchers examined the anatomical features that define feminine and masculine hands, the surgical and non-surgical approaches for feminization and masculinization of the hand; and adapted established aesthetic hand techniques for gender affirming care. They carried out a comprehensive database search of PubMed, Embase OVID and SCOPUS to identify articles on the characterization of feminine or masculine hands, hand treatments related to gender affirmation, and articles related to techniques for hand feminization and masculinization in the non-transgender population. From 656 possibly relevant articles, 42 met the inclusion criteria for the current literature search. There is currently no medical literature specifically examining the surgical or non-surgical options for hand gender affirmation. The available techniques for gender affirming procedures discussed in this paper were appropriated from those more commonly used for hand rejuvenation. The authors concluded that there is very little evidence addressing the options for transgender individuals seeking gender affirming procedures of the hand. These researchers stated that although established procedures used for hand rejuvenation may be employed in gender affirming care, further study is needed to determine relative salience of various hand features to gender dysphoria in transgender patients of various identities, as well as development of novel techniques to meet these needs. Level of Evidence = III. Peritoneal Pull-Through Technique Vaginoplasty in Neovagina Construction in Gender-Affirming SurgeryTay and Lo (2022) reviewed the application, effectiveness and outcomes of a novel surgical technique, peritoneal pull-through technique vaginoplasty, in gender-affirming surgery. Specific outcome parameters included healing time, depth of cavity achieved,) alleviation of dysphoria, and morbidity of the surgery. These researchers carried out a systematic review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement and PROSPERO registration obtained before commencement. A search was performed in OVID Medline, Embase, Willey Online Library and PubMed. Specialty-related journals, grey literature and reference lists of relevant articles were manually searched. From 476 potentially relevant articles, 12 articles were analyzed; and the publications were all level 4 or level 5 evidence. Healing times were poorly reported or often not mentioned. A total of 8 authors reported neovagina cavity depth of at least 13 cm and good patient satisfaction. Alleviation of dysphoria was not discussed by any of the publications and only 6reported complications. Average follow-up ranged from 6 weeks to 14.8 months. The authors concluded that the use of peritoneal pull-through vaginoplasty in gender-affirming surgery is promising and novel; however, there is a paucity of data. These investigators stated that further research and longer-term data are needed to examine the safety and effectiveness of this technique including stabilization of vaginal depth, later morbidity and complications. Patients seeking this surgery overseas should be informed of the potential difficulties they may face. Urethral Complications and Outcomes in Transgender MenHu et al (2022) noted that urologic problems, such as urethral fistulas and strictures, are among the most frequent complications following phalloplasty. Although many studies have reported successful phalloplasty and urethral reconstruction with reliable outcomes in transgender men; so far, no method has become standardized. These researchers examined the reports on urological complications and outcomes in transgender men with respect to various types of urethral reconstruction. They carried out a comprehensive literature search of PubMed, Scopus, and Google Scholar databases for studies related to phalloplasty in transsexuals. Data on various phallic urethral techniques, urethral complications, and outcomes were collected and analyzed using the random-effects model. A total of 21 studies (1,566 patients) were included: 8 studies (1,061 patients) on "tube-in-tube", 9 studies (273 patients) on "prelaminated flap, and 6 studies (221 patients) on "second flap". Compared with the tube-in-tube technique, the pre-laminated flap was associated with a significantly higher urethral stricture/stenosis rate; however, there was no difference between the pre-laminated flap and the 2nd flap techniques. For all phalloplasty patients, the pooled rate of urethral fistula or stenosis was 48.9 %, the rate of the ability to void while standing was 91.5 %, occurrence rate of tactile or erogenous sensation was 88 %, the prosthesis complication rate was 27.9 %, and patient-reported satisfactory outcome rate was 90.5 %. The authors concluded that urethral reconstruction with a pre-laminated flap was associated with a significantly higher urethral stricture rate and increased need of revision surgery compared with that observed using a skin flap. Overall, most patients were able to void while standing and were satisfied with the outcomes. DSM 5 Criteria for Gender Dysphoria in Adults and AdolescentsA marked incongruence between one’s experienced/expressed gender and assigned gender, of at least 6 months duration, as manifested by two or more of the following:
The condition is associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning. There is no minimum duration of relationship required with mental health professional. It is the professional’s judgment as to the appropriate length of time before a referral letter can appropriately be written. A common period of time is three months, but there is significant variation in both directions. Evaluation of candidacy for gender affirmation surgery by a mental health professional is covered under the member’s medical benefit, unless the services of a mental health professional are necessary to evaluate and treat a mental health problem, in which case the mental health professional’s services are covered under the member’s behavioral health benefit. Please check benefit plan descriptions. Characteristics of a Qualified Health Professionals (From SOC-8)Qualifications of Mental Health Professional for assessing transgender and gender diverse adults for physical treatments (from WPATH SOC-8):
Credentials of surgeons who perform gender-affirming surgical procedures (fromWPATH SOC-8):
Characteristics of health care professionals working with gender diverse adolescents:
The above policy is based on the following references:
Policy History Effective: 05/14/2002 Next Review: 07/11/2024 Review History Definitions Additional InformationClinical Policy Bulletin Notes State InformationCA, CO, IL, MD, NY, OR, WA You are now leaving the Aetna website .Links to various non-Aetna sites are provided for your convenience only. Aetna Inc. and its subsidiary companies are not responsible or liable for the content, accuracy, or privacy practices of linked sites, or for products or services described on these sites. 
 Search formBy continuing to use our site, you agree to our Private Policy and Terms of Use . Japanese court allows trans woman to legally change gender without surgery The woman successfully argued that Japan's surgery requirement for receiving a legal gender change presented her with huge financial and physical burdens.A transgender woman is the first person in Japan to be granted a legal gender change without having to undergo compulsory gender-affirming surgery. In order to legally change one's gender on official documents, a 20-year-old law in Japan requires that transgender people receive a “gender identity disorder" diagnosis and undergo surgery reconfiguring their reproductive organs. The woman, in her late 40s, was first denied a gender change by lower courts in the country because she had not undergone surgery, despite her being unable to receive the procedure. The woman appealed her case to a higher court, arguing that the requirements presented her with huge financial and physical burdens, and was therefore in violation of her rights. The Hiroshima High Court ruled in her favor Wednesday, determining that the current requirements may be unconstitutional. The law previously required that those seeking a legal change have "no reproductive capacity," forcing transgender people to undergo sterilization procedures. The nation's Supreme Court ruled that the provision is unconstitutional in October, though it did not rule on the gender-affirming surgery requirement, and sent the woman's case back to the High Court. The woman said at the time that while “it is very regrettable that [my] gender change was not approved by the Grand Chamber of Justice and that the case has been postponed, I am glad that the outcome of this case will lead to a positive direction.” Now, Kazuyuki Minami, one of the woman's lawyers, said via The Associated Press that when he informed his client of the recent ruling over the phone, she cried in relief. The High Court's ruling did not encompass transgender people who are not on hormone replacement therapy, but it does pave the way for others seeking legal changes. The Japan Alliance for LGBT Legislation said in a statement Thursday that the ruling can still be considered progress because “it can open the door for transgender females to be able to legally change their gender without undergoing surgery.”
Want more breaking equality news & trending entertainment stories? Check out our NEW 24/7 streaming service: the Advocate Channel! Download the Advocate Channel App for your mobile phone and your favorite streaming device! APPLE STORE - GOOGLE PLAY ROKU - APPLE TV - FIRE TV - GOOGLE TV From our SponsorsMost popular, meet all 37 of the queer women in this season's wnba, lauren boebert mercilessly mocked for calling white house press secretary karine jean-pierre a 'dei hire'. 13 LGBTQ+ British Royals in HistoryA local nbc anchor came out as gay on live tv. now, he shares how the moment has changed his life, here are the 15 gayest travel destinations in the world: report, black transgender woman starr brown shot to death in memphis. her coworker has confessed to the killing, 13 of the most batsh*t things n.c. republican governor candidate mark robinson has said, 21+ steamy photos of scotland’s finest gay men in elska glasgow, more than 50 of our favorite lgbtq+ moms, conjoined twins lori schappell and trans man george schappell dead at 62, latest stories, 18% of lgbtq+ adults are parents — and they're raising over 5 million children, bethel park, butler and milwaukee, and how maga hate persists, climate change is increasingly worrying lgbtq+ youth: report, alpha phi alpha, a prominent black fraternity, moves to bar transgender members, pete buttigieg calls out donald trump’s disrespect for military at minnesota biden campaign event, gay democrat ritchie torres joins republican lawmaker to call for secret service reform, elon musk moves spacex and x to texas because california is too supporting of trans youth, kamala harris challenges trump’s vp pick jd vance to televised debate, jd vance embraced project 2025 before maga republicans tried distancing themselves from it, ohioans explain abandoning republican party for love of their transgender grandchild, california bans forced outing of lgbtq+ students as gov. gavin newsom signs landmark law, a history of political violence in the u.s., from hamilton to harvey milk to gabby giffords, a trans woman was denied entry into usa powerlifting events. now, her lawsuit heads to the mn supreme court, tucker carlson accuses pete buttigieg of being ’not gay at all’, rachel maddow roasts trump vp pick jd vance with his own words, marjorie taylor greene and other republicans attack transgender rights on rnc opening night, judge aileen cannon is a redo of annie wilkes in 'misery', the haunting true story of a gay man's murder that inspired stephen king's 'it', paris olympics will give out 300,000 condoms to athletes, continuing long-held tradition, it's official: donald trump is the republican nominee for president again, trending stories.  20 sexy pics of 'All Stars 8's trade of the season Naysha Lopez Jersey City is the ‘Cream’ of the crop thanks to these two cannabis-loving husbands 'Summer House' star Preston Mitchum dishes on wedding plans & queering up reality TV The best of 2024 (so far) 'RuPaul's Drag Race Global All Stars' cast has been Ru-vealed! 35 of the best lesbian films & TV shows you can watch on Netflix now Omar Apollo shuts down rumors that he's feuding with Troye Sivan Meet the queens competing on 'RuPaul's Drag Race Global All Stars' Activist and philanthropist Bruce Bastian dies at 76 Michaela Jaé Rodriguez finally found a spot for her Golden Globe Biden officials urged syphilis, hepatitis & HIV tests on National HIV Testing Day Exclusive: We kiki with Q from 'RuPaul's Drag Race' Here's everything you missed at Toronto's unbelievable Pride festival This private island is the perfect romantic escape France becomes world’s first country to enshrine abortion rights in constitution Joe Biden has tied the record for most LGBTQ+ judges confirmed in federal courts Elon Musk uses burner accounts on X, doesn’t fact-check: report Court rules to keep PrEP coverage under Obamacare Nudists in the Castro save tourist from 'crazy pirate' with blowtorch using mean right hook 45+ queer-affirming pics of Toronto's Pride Parade and Trans and Dyke Marches How climate disasters hurt mental health in young people Just John Duff bares all in Ptown this summer Is fandom gatekeeping a good or bad thing? Anime Expo 2024 goers weigh in Yes, HIV-positive people can safely breastfeed All 6 rogue Mississippi cops got long prison sentences in 'Goon Squad' torture of 2 Black menMost recent.  How Shannen Doherty's on-screen legacy changed our gay lives Election season got you down? This crisis line is soothing LGBTQ+ mental health The internet has turned Kamala Harris into the ultimate pop girlie and we are L-I-V-I-N-G Joe Biden launches ‘Out for Biden-Harris’ campaign initiative to engage & woo LGBTQ+ voters (exclusive) Celebrities stand up for brain health at the Power of Love gala in Las Vegas GAYLE talks 'Internet Baby,' touring with Pink & Taylor Swift Wait, is Kit Connor about to become our new favorite gay Marvel superhero? Armie Hammer's gay friends told him his cannibalism texts were mild compared to Grindr messages WNBA legend Sue Bird is getting her own Barbie The Talk: What HIV isn’t Are horny girls saving pop music this summer? The menthol diaries: Taking back pride from tobacco The Talk: Thriving with HIV Pride, passport stamps, and PrEP’d with options: One man’s journey with HIV prevention Meet the chaotic, queer-inclusive cast of MTV's 'Surreal Life: Villa of Secrets' Here's everything you must see as an LGBTQ+ traveler in Saugatuck, Michigan Two series from The Advocate Channel launch on Hulu Kandy Muse reacts to Elliott With 2 Ts' 'Drag Race' tea—Elliott responds back Pensacola, Florida is the secret Pride destination where you can truly be yourself Insomniac is making history with the EDC Orlando 2024 lineup Federal judge grants Casa Ruby founder Ruby Corado pre-trial release from D.C. jail Before AIDS, gay artist Rex drew hot men on the prowl — then he disappeared The July/Aug 'Treatment Guide' issue of Plus is here! The Talk: Finding balance with HIV 15 hot pics of Joel Kim Booster in honor of 'Loot' being renewed for season 3Recommended stories for you, ryan adamczeski.
Federal appeals court upholds Tennessee's transgender birth certificate policyA federal appeals court on Friday upheld a Tennessee policy prohibiting transgender individuals from changing the sex marker on their birth certificate. In a 2-1 decision, the 6th Circuit U.S. Court of Appeals ruled the Tennessee policy is constitutional, writing that "there is no fundamental right to a birth certificate recording gender identity instead of biological sex." The majority called the policy, which is an outlier in the U.S., "a nondiscriminatory form of government speech embraced by some States about an undeniable historical fact." An attorney from Lambda Legal, a civil rights organization focusing on the LGBTQ+ community representing the plaintiffs, said the group was disappointed in the decision and is considering next steps. "The discrimination that is being suffered by transgender people in present-day America is something that, frankly, is reprehensible and shameful," said Omar Gonzalez-Pagan, senior counsel and health care strategist at Lambda Legal. "I hope that this decision doesn't give fodder to that, but rather allows us to galvanize to ensure that we can have a more inclusive and protective set of laws and policies." Chief 6th Circuit Judge Jeffrey Sutton wrote the majority opinion and was joined by Judge Amul Thapar. The opinion sides with Tennessee's argument that maintaining birth certificates that match a person's sex at their birth protects the integrity and accuracy of vital records, and the judges claim that allowing changes to the sex marker on birth certificates would mean that some birth certificates show biological sex and others show gender identity. Sutton wrote that "policymaking in this area" was better left to to legislatures than the courts. The dissenting opinion, written by Senior Judge Helene White notes that at least 43 U.S. states or territories allow changes to the sex marker on birth certificates under varying circumstances. White wrote that Tennessee's policy is inconsistent because individuals born with ambiguous genitalia are allowed to amend the sex marker on their certificates after their birth based on other characteristics. "In so doing, the State denigrates those who do not conform to societal assumptions about what it means to be male or female, like transgender individuals, conveying that they are somehow less male or female because of the accidents of their birth — that no matter what, in the eyes of the State, their genitalia at birth alone determine their identities forevermore," White wrote. Gonzalez-Pagan said that policies similar to Tennessee's have been found unconstitutional in every court where they had been challenged except for Tennessee's and a district court in Oklahoma. “Whether someone can change the sex on their birth certificate is a matter for each state to decide,” Tennessee Attorney General Jonathan Skrmetti said in a statement. “While other states have taken different approaches, for decades Tennessee has consistently recognized that a birth certificate records a biological fact of a child being male or female and has never addressed gender identity. We are grateful that the Court of Appeals agreed with the district court that any change in Tennessee's policy can only come from the people of Tennessee.” Four transgender women born in Tennessee sued the state in 2019 seeking an order to compel the state to change their birth certificates. They sought to change a 1977 Tennessee law that expressly forbade amendments to birth certificates after an individual completed sex-reassignment surgery, in response to a federal law passed the same year recommending allowing such changes. The plaintiffs said that having a birth certificate inconsistent with how they identify and present forces them to divulge their transgender status when applying for jobs or applying for a passport, which puts them at risk of harassment or violence, the majority opinion states. They argued that the policy violates the Equal Protection and Due Process Clauses of the Fourteenth Amendment. In her dissenting opinion, White agreed, writing, "Unlike the majority, I conclude that the Policy effectively discloses transgender status and thus implicates fundamental interests in bodily integrity and private sexual matters." The decision comes just more than a year after the U.S. District Court for the Middle District of Tennessee ruled against the plaintiffs. The appellate case was argued on May 2 in Nashville, a change from the 6th Circuit's home in Cincinnati. Evan Mealins is the justice reporter for The Tennessean. Contact him at [email protected] or follow him on X, formerly known as Twitter, @EvanMe a lins . Republish This Story* Please read before republishing * We’re happy to make this story available to republish for free under an Attribution-NonCommercial-NoDerivatives Creative Commons license as long as you follow our republishing guidelines, which require that you credit The 19th and retain our pixel. See our full guidelines for more information . To republish, simply copy the HTML at right, which includes our tracking pixel, all paragraph styles and hyperlinks, the author byline and credit to The 19th. Have questions? Please email [email protected] . — The Editors Modal GalleryThe 19th thanks our sponsors. Become one . Florida is quietly denying transgender residents updated birth certificatesThe rejection comes without public notice or new law — even when all other government-issued identification reflects their current gender identity. Orion Rummler LGBTQ+ Reporter Republish this story In the past year, Florida’s health department has declined to amend gender markers on birth certificates for both transgender adults and minors. Although the agency says it is basing denials on pre-existing state statutes, transgender Floridians had previously been able to update their birth certificates for at least a decade. Now, they face an opaque process that seems designed to reject all applicants. Transgender Floridians have been denied updated birth certificates even when all of their other government-issued identification reflects their current gender identity. When applicants provided paperwork detailing clinical treatment for their gender transition and their legal name change, they were still denied. This is at odds with how the agency has handled this approval process for years — and is the latest example of Florida’s state agencies enacting anti-LGBTQ+ policies even when anti-LGBTQ+ laws fail to pass. In 2023 and 2024, trans minors and adults who applied for amended birth certificates received denial letters from the state health agency’s Bureau of Vital Statistics. In those letters, reviewed by The 19th, the bureau says the paperwork that has long been accepted to update gender on birth certificates — like proof of clinical treatment and a legal name change — no longer works. “Specifically, the documentary evidence does not establish that the sex identifier on the birth record contains a misstatement, error, or omission,” one denial letter from March 2024 reads. The denial letters also offer conflicting requirements. One, from August 2023, states that for trans minors, “documentary evidence established prior to the child’s seventh birthday is required.” In another letter, the bureau says that trans adults trying to update their birth certificates must provide documentation “established prior to the registrant’s 18th birthday.” Many transgender adults did not know they were trans as children, or did not pursue gender-affirming care as children even if they did realize their identities — rendering either requirement difficult, if not impossible, to navigate.  Trans people in Florida can no longer update their driver’s licensesFlorida’s rule against updating gender on driver’s licenses may violate federal law.
Simone Chriss, an attorney with the Southern Legal Counsel in Florida and the director of the organization’s transgender rights initiative, has worked with around 80 clients who she says have all been denied updated birth certificates since last August. None of their appeals, including an administrative hearing overseen by Florida’s health agency, have worked. As a result, none of them have been able to update their birth certificates. “Most are just being ignored,” Chriss said. “I’ve filed many. There’s at least five that I have pending at this moment that the department hasn’t responded to.” The Florida Department of Health and its Bureau of Vital Statistics did not respond to requests for comment. Republican lawmakers in Florida have repeatedly failed to pass legislation that aims to prevent transgender people from being able to obtain accurate birth certificates. This year, a proposed bill to require that state identification and licenses reflect Floridian’s sex assigned at birth failed to pass. Last year, a bill that would explicitly prohibit gender markers being changed on birth certificates also failed to pass. Despite the lack of legislation, Florida agencies have moved to enforce such restrictions on their own. In January, the Florida Department of Highway Safety and Motor Vehicles told local officials that the state would no longer allow transgender people to update their driver’s license with their correct gender. That move was not prompted by any new law, and was simply based on a new agency policy. LGBTQ+ and legal experts believe the rule likely takes Florida out of compliance with federal law , which the state disputes. Now, Florida’s Bureau of Vital Statistics within its health agency has reversed course on birth certificate updates, arguing that discrepancies between sex at birth and gender identity do not constitute a paperwork error in need of fixing. Updating all of the necessary identity documents is costly. The name change fee in Florida is $400 and fingerprinting for the background check as part of that name change is $50. The requirement of a doctor’s letter for updating the gender marker on a birth certificate means paying out of pocket for a doctor’s visit or at least a copay. Then, there’s the $20 application fee to amend the birth certificate; applicants may also pay more if they opt for rush service. For many transgender Floridians, the entire process appears to have ended on a brick wall, with no public notice that a policy change has taken place and no clear path to access accurate documentation. And the new policy appears to be based on a definition of sex that excludes transgender people — a change from what was put on the books less than a decade ago. In 2018, Florida relaxed its conditions for updating gender markers on birth certificates following pressure from LGBTQ+ and legal advocacy groups . Until then, the state had required proof of sex reassignment surgery in order to change the gender marker — which at least twelve other states still do, according to the Movement Advancement Project . After 2018, Florida’s health agency began accepting letters from medical providers documenting clinical treatment for gender transition. This broadened the scope of who could apply for new documentation since some transgender people never pursue surgery. Across the country, only five other states do not update gender markers on birth certificates. Many transgender people pursue this documentation as they legally change their name or update their gender on their driver’s license or Social Security card. You have been subscribed! Please complete the following CAPTCHA to be confirmed. If you have any difficulty, contact [email protected] for help. Submitting… Uh-oh! Something went wrong. Please email [email protected] to subscribe. This email address might not be capable of receiving emails (according to Bouncer ). You should try again with a different email address. If you have any questions, contact us at [email protected] .  Without accurate personal documents that align with their gender expression and other forms of identification, trans people face harassment or discrimination when going about their daily lives, like when applying for a job or enrolling in a new school. The risk of being “outed” by an incorrect piece of paperwork can have dangerous consequences for trans people, especially in a state considered dangerous for LGBTQ+ people . “Despite making, I think, very compelling arguments as to why the department is violating the rights of transgender people born in the state of Florida, they have come back with the same rationale over and over for denying it,” Chriss said. “Which is … ‘sex doesn’t change.’” Right now, the best option for trans Floridians seeking an updated birth certificate is to update all of their other government-issued documents to reflect their gender identity, Chriss said. Passports, a primary identification document, can be used in most cases instead of state identification. “It’s clear the only avenue or the only route to reversing or striking down this policy is using federal impact litigation, like we have in all the other areas where trans folks’ rights have been eroded in Florida. We are planning to challenge this in federal court as well,” she said. Recommended for youMore states are pushing to stop legally recognizing trans people in public life, ‘they’re erased’: when trans people are misgendered after death, the consequences extend beyond paper. The 19th The 19th is a 501(c)(3) tax-exempt organization. Our stories are free to republish in accordance with these guidelines .
 | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
IMAGES
VIDEO
COMMENTS
Gender Change Effective January 1, 2018, new procedures for Gender Reassignment have been established with the implementation of Public Act 100-0360 An individual born in Illinois, with an existing Illinois birth certificate, may submit an Affidavit and Certificate of Correction Request form along with a Declaration of Gender Transition/Intersex Condition form (see FORMS in
The in place form is form must be completed by the applicant and signed in the. with the completed Declaration of Gender Transition or Intersex Condition of used form. all corrections The original to of birth, the death, and form must fetal death records. We cannot. has an intersex seeking a new certificate condition of as birth required has ...
An affidavit indicating your sex and name (if applicable) A parent or guardian must complete this form if the record change is for a minor; A notarized physician's statement that you have completed medical intervention for the purpose of permanent sex reassignment; If you also want to change the legal name on your birth certificate:
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
The cost of transitioning can often exceed $100,000 in the United States, depending upon the procedures needed. A typical genitoplasty alone averages about $18,000. Rhinoplasty, or a nose job, averaged $5,409 in 2019. Insurance Coverage for Sex Reassignment Surgery.
Trans-masculine (Female to Male) Surgeries. Please note, there might be additional steps needed as you prepare for surgery. Make a Gift. Phone: 212-604-1730. Email: [email protected]. Learn more about the full range of transgender surgeries performed by the expert surgeons at the Center for Transgender Medicine and Surgery.
Gender affirming surgery, also known as sex reassignment surgery (SRS) or confirmation surgery, is the surgical procedure(s) by which a transgender or non-binary person's physical appearance and functional abilities are changed to align with the gender they know themselves to be. ... Complete Our Surgical Interest Form. If you are interested ...
Individuals who desire surgical procedures who have not been part of the Comprehensive Gender Services Program should contact the program office at (734) 998-2150 or email [email protected]. We will assist you in obtaining what you need to qualify for surgery. University of Michigan Comprehensive Gender Services Program brings ...
Gender reassignment costs vary based on each person's needs and desires; expenses often range between $7,000 and $50,000 (in 2014), although costs may be much greater depending upon the type ... although for trans men this comes in the form of a mastectomy. This may be the only surgery that trans men undergo in their reassignment, if only ...
Male to female (MTF) gender reassignment surgery is also known as sex reassignment surgery (SRS), genital construction, and generally as Gender Confirmation Surgery. These procedures are used to remove and alter male genitalia into traditional female genitalia. Plastic surgeons will remove the scrotum, perform a penile inversion to create the ...
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
She does more than 150 a year. We also offer a Transgender Gynecology Clinic with a gender-neutral space. Services include surgery. Referrals and appointments are made through the OHSU Center for Women's Health, though the space is not in the center. Call 503-418-4500 to request an appointment.
Gender confirming surgery (also known as sex reassignment or gender affirming surgery) does more than change a person's body. It affirms how they think and feel about their own gender and what it means to who they are. Ontario is funding surgery as an option for people who experience discomfort or distress with their sex or gender at birth.
Male-to-female gender reassignment surgery (MTF GRS) is a complex and irreversible genital surgery for male transsexual who is diagnosed with gender identity disorder and has a strong desire to live as female. The procedure is to remove all male genital organs including the penis and testes with the construction of female genitalia composed of ...
Supporting evidence for providing gender-affirming treatments and procedures Transgender people may seek any one of a number of gender-affirming interventions, including hormone therapy, surgery, facial hair removal, interventions for the modification of speech and communication, and behavioral adaptations such as genital tucking or packing, or chest binding.
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
Here's how gender reassignment works: Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina. An incision ...
What the Equality Act says about gender reassignment discrimination. The Equality Act 2010 says that you must not be discriminated against because of gender reassignment. In the Equality Act, gender reassignment means proposing to undergo, undergoing or having undergone a process to reassign your sex. To be protected from gender reassignment ...
Gender reassignment remains the treatment of choice for strong and persistent gender dysphoria in both categories, but more research is needed on the short-term and long-term effects of puberty-suppressing medications and cross-sex hormones on brain and behavior. ... Vulvoplasty is a form of gender-affirming feminizing surgery that does not ...
A transgender woman is the first person in Japan to be granted a legal gender change without having to undergo compulsory gender-affirming surgery.. In order to legally change one's gender on ...
nonbinary, gender expansive, gender nonconforming, and others who do not identify as cisgender. Original Medicare . Currently, local Medicare Administrative Contractors determine coverage of gender reassignment surgery on a case-by-case basis. MACs will make the determination of whether or not to cover gender reassignment surgery based on
A federal appeals court on Friday upheld a Tennessee policy prohibiting transgender individuals from changing the sex marker on their birth certificate. In a 2-1 decision, the 6th Circuit U.S ...
In 2018, Florida relaxed its conditions for updating gender markers on birth certificates following pressure from LGBTQ+ and legal advocacy groups. Until then, the state had required proof of sex reassignment surgery in order to change the gender marker — which at least twelve other states still do, according to the Movement Advancement ...