

59529 Ultrasound Images & Clips
Browse our free ultrasound library offered to you by SonoSkills and FUJIFILM Healthcare Europe. Make sure to sign-up for our newsletter to receive the latest cases and news in your inbox!
Abdomen and retroperitoneum
Urinary tract and male reproductive system, gynaecology, head and neck, breast and axilla, musculoskeletal joints and tendons, musculoskeletal, bone, muscle, nerves and other soft tissues, peripheral vessels, case of the month, calcaneus orif with failed hardware affecting fibularis tendons.
The patient is a 30 year old male referred to physical therapy after trauma to bilateral ankles with pinning with ORIF of bilateral calcaneus. The patient's left foot and ankle have been progressing well with physical therapy and the right foot and ankle have had limitations throughout the physical therapy plan of care. Two weeks prior to the ultrasound scan the patient's right ankle was forcibly dorsiflexed and the patient had an acute onset of pain.

From the Archive
- July: Calcaneus ORIF With Failed...
- June: Scapulothoracic Bursitis

Don't have an account? Signup now

By sharing our collective experience through interesting and classic patient cases, we can make a real difference in how people are imaged and diagnosed. Each case belongs to a contributing member and all cases are reviewed by our dedicated editors to ensure they reach quality standards and abide by privacy guidelines. Cases can public or unlisted and then be viewed directly or added to articles, playlists or multiple choice questions. Find out more about cases.
Create new case

Large bowel obstruction with gallstone in rectosigmoid colon

Left tubal block and hydrosalpinx

Benign prostatic hyperplasia and bladder diverticulum

Mayer-Rokitansky-Küster-Hauser syndrome with rudimentary uterine horns

Intravesical urachal cyst

Plexiform neurofibromatosis (neck)
Sturge-Weber syndrome

Pontocerebellar hypoplasia with filum terminale lipoma
Hematocolpos in imperforate hymen

Bucket-handle meniscal tear

Placenta increta (MRI pelvis)
Osteochondroma
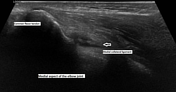
Partial tear of medial collateral ligament of the elbow
Annular pancreas

Mastectomy on chest X-ray

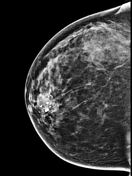
Popcorn-like calcification - breast
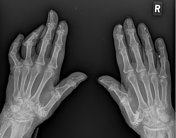
Scleroderma - musculoskeletal manifestations in the hands
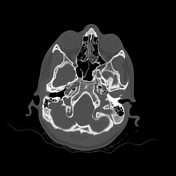
Bilateral condylar canal
Cysticercosis - anterior abdominal wall

Orbital schwannoma

- All Systems
- Central Nervous System
- Gastrointestinal
- Head & Neck
- Hepatobiliary
- Interventional
- Musculoskeletal
- Not Applicable
+ Case Diagnostic Certainty
- At Least Probable
- At Least Almost Certain
+ Study Modality
- All Modalities
- Annotated image
- DSA (angiography)
- Fluoroscopy
- Mammography
- Nuclear medicine
× Sort By
- Case Completion %
- Date of Publication
- Date of last edit
ADVERTISEMENT: Supporters see fewer/no ads
By Section:
- Artificial Intelligence
- Classifications
- Imaging Technology
- Interventional Radiology
- Radiography
- Gynaecology
- Haematology
- Paediatrics
Radiopaedia.org
- Feature Sponsor
- Expert advisers


- Search by keyword
- Search by citation
Page 1 of 13
Off-plane technique ultrasound-guided pericardiocentesis via anterior approach: short communication
The pericardiocentesis procedure is common, often performed via the subxiphoid approach, although other transthoracic approaches have been described. This short communication describes an off-plane technique u...
- View Full Text
A do it yourself (DIY) point-of-care wrist ultrasound phantom for joint access training
Joint access is essential for arthrocentesis, or joint aspiration of fluids. Joint treatments that are not performed properly can result in avoidable patient issues such as damage to the muscles, tendons, and ...
Ultrasound-guided percutaneous tracheostomy: a risk-based protocol
Online vs in-person musculoskeletal ultrasound course: a cohort comparison study.
Point-of-care musculoskeletal (MSK) ultrasound (US) courses are typically held in-person. The COVID-19 pandemic guidelines forced courses to switch to online delivery. To determine this impact, we conducted an...
Correlation between the radial artery resistance index and the systemic vascular resistance index: a cross-sectional study
Ultrasound measurement of the radial resistance index (RRI) in the anatomical snuffbox has been proposed as a useful method for assessing the systemic vascular resistance index (SVRI). This study aims to estab...
Clinical research on point-of-care lung ultrasound: misconceptions and limitations
Over the last 20 years, advances in point-of-care lung ultrasound (PoCLUS) have been consistent. The clinical application of PoCLUS has drastically changed the diagnosis of some respiratory conditions mainly i...
Veno-venous extracorporeal membrane oxygenation (VV ECMO) cannula malposition identified with point-of-care ultrasound
Point-of-care ultrasound (POCUS) has become a mainstay in the evaluation of critically ill patients in the intensive care unit (ICU). ECMO patients are susceptible to complications during prolonged ICU stay, i...
Echocardiographic assessment of right ventricular performance in COVID-19 related acute respiratory distress syndrome: the importance of systo-diastolic interaction
The cardiac manifestations of COVID-19 have been described in patients with acute respiratory distress syndrome (ARDS) admitted to intensive care unit (ICU). The presence and impact of right ventricular (RV) d...
Results of the implementation of a double-check protocol with point-of-care ultrasound for acute heart failure in the emergency department
To determine the effectiveness of a double-check protocol using Point-of-Care Ultrasound in the management of patients diagnosed with Acute Heart Failure in an Emergency Department.
Impaired cerebral autoregulation detected in early prevasospasm period is associated with unfavorable outcome after spontaneous subarachnoid hemorrhage: an observational prospective pilot study
Subarachnoid hemorrhage (SAH) patients with cerebral autoregulation (CA) impairment at an early post-SAH period are at high risk of unfavorable outcomes due to delayed cerebral ischemia (DCI) or other complica...
Utility of the Venous Excess Ultrasound (VEXUS) score to track dynamic change in volume status in patients undergoing fluid removal during haemodialysis – the ACUVEX study
The use of ultrasound assessment, including the Venous Excess Ultrasound (VEXUS) score, is increasingly being utilised as part of fluid status assessment in clinical practice. We aime...
Roberto Copetti, MD (1954–2024)
Canadian internal medicine ultrasound (cimus) consensus statement: recommendations for mandatory ultrasound competencies for ultrasound-guided thoracentesis, paracentesis, and central venous catheterization.
To develop a Canadian Internal Medicine Ultrasound (CIMUS) consensus statement on recommended mandatory point-of-care ultrasound (POCUS) competencies for ultrasound-guided thoracentesis, paracentesis, and cent...
Lung ultrasound score predicts outcomes in patients with acute respiratory failure secondary to COVID-19 treated with non-invasive respiratory support: a prospective cohort study
Lung ultrasound has demonstrated its usefulness in several respiratory diseases management. One derived score, the Lung Ultrasound (LUS) score, is considered a good outcome predictor in patients with Acute Res...
Integrating a self-directed ultrasound curriculum for the internal medicine clerkship
Incorporating ultrasound into the clinical curriculum of undergraduate medical education has been limited by a need for faculty support. Without integration into the clinical learning environment, ultrasound s...
Point-of-care ultrasound to inform antiviral treatment initiation in chronic hepatitis B virus infection in low-resource settings – the PUSH protocol
Chronic Hepatitis B (CHB) is prevalent worldwide and most related deaths occur in low-resource settings. Antiviral treatment of CHB is indicated in those with significant liver disease and markers of viral rep...
Right ventricular free wall longitudinal strain during weaning from mechanical ventilation using high-flow or conventional oxygen treatment: a pilot study
Medico-legal risks of point-of-care ultrasound: a closed-case analysis of canadian medical protective association medico-legal cases.
Point-of-care ultrasound (POCUS) has become a core diagnostic tool for many physicians due to its portability, excellent safety profile, and diagnostic utility. Despite its growing use, the potential risks of ...
Test characteristics of point-of-care ultrasonography in patients with acute kidney injury
Acute kidney injury is a common disorder that is associated with significant morbidity and mortality. Point-of-care ultrasonography (PoCUS) is an imaging modality performed at the bedside and is used to assess...
Ultrasound contrast agent assisted ultrasonography guidance percutaneous nephrostomy for non-hydronephrotic kidney
Given the limited success rate and considerable challenges associated with conventional ultrasonography (US) guidance for percutaneous nephrostomy (PCN) in non-hydronephrotic kidneys, this study proposed a sol...
The usefulness of point-of-care ultrasound in dehydrated patients in a pediatric emergency department
Dehydration is among the most common causes of Pediatric Emergency Department admission; however, no clinical signs, symptoms, or biomarkers have demonstrated sufficient sensitivity, specificity, or reliabilit...
Evaluation of point-of-care ultrasound training among healthcare providers: a pilot study
The use of Point-of-Care Ultrasound (POCUS) has become prevalent across a variety of clinical settings. Many healthcare professionals have started getting hands-on training. To evaluate the effectiveness of su...
Thoracic ultrasound use in hospitalized and ambulatory adult patients: a quantitative picture
Thoracic ultrasound (TUS) has been established as a powerful diagnostic and monitoring tool in the Intensive Care Unit (ICU). However, studies outside the critical care setting are scarce. The aim of this stud...
Can absence of cardiac activity on point-of-care echocardiography predict death in out-of-hospital cardiac arrest? A systematic review and meta-analysis
The purpose of this systematic review and meta-analysis was to evaluate the accuracy of the absence of cardiac motion on point-of-care echocardiography (PCE) in predicting termination of resuscitation (TOR), s...
Point-of-Care Ultrasound training in undergraduate education in the European Union: current situation and perspectives
Given the widespread use of Point-of-Care UltraSound (PoCUS) in clinical practice, with ultrasound machines becoming more portable and affordable, recommendations and position statements from ultrasound societ...
Assessment of quadriceps muscle mass by ultrasound in the postoperative period of cardiac surgery
Patients undergoing cardiac surgery are exposed to many factors that activate catabolic and inflammatory pathways, which affect skeletal muscle and are, therefore, related to unfavorable hospital outcomes. Giv...
Lung ultrasound and supine chest X-ray use in modern adult intensive care: mapping 30 years of advancement (1993–2023)
In critically ill patients with acute respiratory failure, thoracic images are essential for evaluating the nature, extent and progression of the disease, and for clinical management decisions. For this purpos...
Comparing contamination rates of sterile-covered and uncovered transducers for ultrasound-guided peripheral intravenous lines
Physicians frequently use point-of-care ultrasound for intravenous access and bloodwork in the ED. Recently, AIUM and ACEP released recommendations on ultrasound-guided peripheral intravenous lines (USPIVs), b...
Change in economy of ultrasound probe motion among general medicine trainees
To observe change in economy of 9 ultrasound probe movement metrics among internal medicine trainees during a 5-day training course in cardiac point of care ultrasound (POCUS).
The role of point-of-care ultrasound (POCUS) imaging in clinical outcomes during cardiac arrest: a systematic review
Cardiac arrest in hospital and out-of-hospital settings is associated with high mortality rates. Therefore, a bedside test that can predict resuscitation outcomes of cardiac arrest patients is of great value. ...
Advancement in pleura effusion diagnosis: a systematic review and meta-analysis of point-of-care ultrasound versus radiographic thoracic imaging
Pleural effusion is a fluid buildup in the pleural space that mostly result from congestive heart failure, bacterial pneumonia, malignancy, and pulmonary embolism. The diagnosis of this condition can be challe...
Correction: Utility of ultrasound in managing acute medical conditions in space: a scoping review
The original article was published in The Ultrasound Journal 2023 15 :47
Replacement of fluoroscopy by ultrasonography in the evaluation of hemidiaphragm function, an exploratory prospective study
Dysfunction of the diaphragm may ultimately lead to respiratory insufficiency and compromise patient outcome. Evaluation of diaphragm function is cumbersome. Fluoroscopy has been the gold standard to measure d...
Utility of ultrasound in managing acute medical conditions in space: a scoping review
In long-distance spaceflight, the challenges of communication delays and the impracticality of rapid evacuation necessitate the management of medical emergencies by onboard physicians. Consequently, these phys...
The Correction to this article has been published in The Ultrasound Journal 2024 16 :2
Additional predictive value of optic nerve sheath diameter for neurological prognosis after cardiac arrest: a prospective cohort study
The goal is to estimate the additional value of ultrasonographic optic nerve sheath diameter (ONSD) measurement on days 1–3, on top of electroencephalography (EEG), pupillary light reflexes (PLR), and somatose...
Optic nerve sheath diameter measurement for the paediatric patient with an acute deterioration in consciousness
Ocular Point of Care Ultrasound (PoCUS) is emerging as a valuable utility within emergency medicine. Optic nerve sheath diameter (ONSD) has been demonstrated to correlate closely with intracranial pressure (IC...
Correction: Feasibility of using a handheld ultrasound device to detect and characterize shunt and deep vein thrombosis in patients with COVID-19: an observational study
The original article was published in The Ultrasound Journal 2020 12 :49
Correction: A survey demonstrating that the procedural experience of residents in internal medicine, critical care and emergency medicine is poor: training in ultrasound is required to rectify this
The original article was published in The Ultrasound Journal 2021 13 :20
Internal jugular access using pocket ultrasound in a simulated model: comparison between biplane and monoplane visualization techniques
Ultrasound is the current standard for central venous access due to its advantages in efficiency and safety. In-plane and out-of-plane visualization techniques are commonly used, but there is no clear evidence...
Abscess pulsatility: a sonographic sign of osteomyelitis
Early diagnosis and aggressive treatment of acute osteomyelitis may improve prognosis and prevent further complications. Sonography is useful in the evaluation of osteomyelitis. It can demonstrate early signs ...
The diagnostic accuracy of lung ultrasound to determine PiCCO-derived extravascular lung water in invasively ventilated patients with COVID-19 ARDS
Lung ultrasound (LUS) can detect pulmonary edema and it is under consideration to be added to updated acute respiratory distress syndrome (ARDS) criteria. However, it remains uncertain whether different LUS sc...
Development of a novel observed structured clinical exam to assess clinical ultrasound proficiency in undergraduate medical education
A pilot study was performed to develop and test an observed structured clinical exam (OSCE) for clinical ultrasound in second-year medical students. The goal was to assess a longitudinal clinical ultrasound cu...
Echocardiographic parameters in COVID-19 patients and their association with ICU mortality: a prospective multicenter observational study
Echocardiography has become an integral part of the management of critically ill patients. It helps to diagnose and treat various conditions. COVID-19 patients can develop cardiac dysfunction. We planned to st...
The correlation between epicardial fat thickness and longitudinal left atrial reservoir strain in patients with type 2 diabetes mellitus and controls
Diabetes mellitus (DM) has been documented among the strongest risk factors for developing heart failure with preserved ejection fraction (HFpEF). The earliest imaging changes in patients with DM are the left ...
The association of attentional foci and image interpretation accuracy in novices interpreting lung ultrasound images: an eye-tracking study
It is unclear, where learners focus their attention when interpreting point-of-care ultrasound (POCUS) images. This study seeks to determine the relationship between attentional foci metrics with lung ultrasou...
Transesophageal echocardiography (TEE)-guided transvenous pacing (TVP) in emergency department
Placement of a temporary pacemaker is a vital skill in the emergency setting in patients that present with life-threatening bradycardia. Transvenous pacing is the definitive method of stabilizing the arrhythmi...
Feasibility of chest ultrasound up to 42 m underwater
After recent advancements, ultrasound has extended its applications from bedside clinical practice to wilderness medicine. Performing ultrasound scans in extreme environments can allow direct visualization of ...
Evaluation of commercially available point-of-care ultrasound for automated optic nerve sheath measurement
Measurement of the optic nerve sheath diameter (ONSD) via ultrasonography has been proposed as a non-invasive metric of intracranial pressure that may be employed during in-field patient triage. However, first...
Simultaneous venous–arterial Doppler during preload augmentation: illustrating the Doppler Starling curve
Providing intravenous (IV) fluids to a patient with signs or symptoms of hypoperfusion is common. However, evaluating the IV fluid ‘dose–response’ curve of the heart is elusive. Two patients were studied in th...
Learning curves for point-of-care ultrasound image acquisition for novice learners in a longitudinal curriculum
A learning curve is graphical representation of the relationship between effort, such as repetitive practice or time spent, and the resultant learning based on specific outcomes. Group learning curves provide ...
- Editorial Board
- Sign up for article alerts and news from this journal
- Follow us on Twitter
- Follow us on Facebook
- ISSN: 2524-8987 (electronic)

Diagnostic Medical Sonography: Echo Case Studies
- Finding Articles
- Finding Books
- Web Resources
- ECG Simulator
- Medical Tools
- Echo Case Studies
- Mobile Apps
- Writing & Citing
- Careers & Licensing
- Echo Pathology Images
American Society of Echocardiography

Valvular Regurgitation Cases
Instructions for viewing the cases: For best viewing results, use Google Chrome or Mozilla Firefox browsers.
- Aortic Regurgitation
- Mitral Regurgitation
- Mitral Valve Regurgitation in MV Prolapse
- Aortic Regurgitation: When Anatomy Matters
- Aortic Regurgitation in the setting of Bacteremia
- Degenerative Mitral Regurgitation
- Aortic Regurgitation in Bicuspid Aortic Valve
- Tricuspid Regurgitation
- Mitral Regurgitation: Doppler Volumetric Quantitation
- Eccentric MR and Atrial Fibrillation
- Aortic Regurgitation Integrative Assessment
- Pulmonary Regurgitation
- Assessing Severity of Mitral Regurgitation
- Pulmonary Regurgitation in a Repaired Tetralogy of Fallot
- Color Flow Doppler in Mitral Regurgitation
Case Journal
Practical echocardiography cases: video index, east tennessee state university.

Radiopaedia

- << Previous: Medical Tools
- Next: Mobile Apps >>
- Last Updated: Jun 24, 2024 11:45 AM
- URL: https://lawsonstate.libguides.com/diagnosticmedicalsonography
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Radiol Case Rep
- v.17(11); 2022 Nov
A case report on ultrasound evaluation of pediatric post-operative abdominal pain
Alexander b. white.
a University of North Carolina, School of Medicine, 1001 Bondurant Hall, CB #9535, Chapel Hill, NC 27599, USA
Daniel R. Bacon
b Department of Surgery, The Ohio State University College of Medicine, Suite 670, 395 W. 12th Ave, Columbus, OH 43210-1267, USA
Kristen Olinger
c Department of Radiology, University of North Carolina School of Medicine, 2000 Old Clinic Building, CB #7510, Chapel Hill, NC 27599, USA
Jeffrey J. Dehmer
d Pediatric Surgery, Novant Health – New Hanover Regional Medical Center, 2131 S. 17th St, PO Box 9000, Wilmington, NC 28401-7407, USA
Pediatric post-operative abdominal pain can present a unique diagnostic challenge. The case presented here describes a 9-year-old female who presented with fever and worsening abdominal pain 4 days after laparoscopic resection of a benign ovarian teratoma. Computed tomography failed to provide adequate diagnostic imaging. Ultrasound was subsequently used to rule-out a major post-operative complication and ultimately led to a successful non-operative approach while avoiding repeat radiation exposure. Thin body habitus, increased radiosensitivity of pediatric organs, and increased lifetime risk of cancer complicate the use of computed tomography in the pediatric population. Ultrasound, when correlated to clinical findings, has unique advantages over CT such as detailed delineation of soft tissue structures and dynamic assessment of anatomy that make it advantageous in the pediatric post-operative setting.
Introduction
The role of ultrasound for post-operative pain evaluation in the pediatric population may be of particular benefit when evaluating whether further operative management or cross-sectional imaging is warranted. Ultrasound is often used in the pediatric population in acute care settings for time-sensitive imaging of the pediatric abdomen when evaluating pyloric stenosis, intussusception and appendicitis [1 , 2] . Ultrasound has also been successfully used in the evaluation of pediatric blunt trauma to identify intra-abdominal hemorrhage [ 3 ]. Focused assessment with sonography in trauma (FAST) exams enables providers to use bedside ultrasound to identify pathology that could warrant surgical intervention [ 4 ]. Ultrasound has a strong positive likelihood ratio (14.5) for identifying pediatric hemoperitoneum, and in the hemodynamically stable child, a positive ultrasound warrants imaging of the abdomen with computed tomography (CT) [ 3 ]. The use of ultrasound prior to CT is of particular value in pediatric patients in order to minimize radiation exposure. Frequency of CT use in children is increasing, however, implementation of CT regulations is delayed in the pediatric population compared to adult guidelines [ 5 , 6 ]. This delay in regulation disproportionately affects children from non-pediatric referring institutions, which have been associated with producing scans of lower technical quality while utilizing higher doses of radiation [ 7 , 8 ]. Furthermore, pediatric patients have increased radiosensitivity of certain tissues such as the thyroid, gonads, and breast tissue [ 9 ]. Postnatal CT exposure has been associated with increased lifetime risk of leukemia and brain cancer [ 10 , 11 ]. Children inherently have a longer lifespan for accumulating imaging studies with ionizing radiation and radiation-related cancer to occur and there is often a lack of physical, size-based adjustments in technique and radiation dosing [ 9 , 12 ].
Ultrasound findings in correlation with clinical findings may steer surgical intervention without the need for CT imaging in certain settings. One example is the use of US as the primary imaging modality for the pediatric female pelvis, whereby US can differentiate hemorrhage and complex free fluid from decompressed bowel loops due to lack of peristalsis [ 13 ]. While ultrasound has been predominantly used in the initial evaluation of abdominal and pelvic pain in pediatric patients, its role in the post-operative evaluation of pediatric surgical patients is incompletely described and may aid in diagnostic accuracy.
Case report
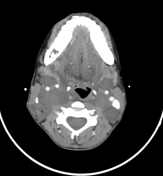
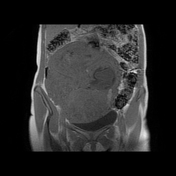
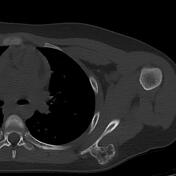
A 9-year-old female underwent a laparoscopic right ovarian cystectomy for a benign mature teratoma. On post-operative day 4 she developed intermittent fevers (max 102.8°F) and transient abdominal and shoulder pain. She was seen in pediatric surgery clinic on post-operative day 4 and was found to have small-volume pneumoperitoneum on her plain films that was deemed within normal limits following a laparoscopic procedure. Her abdominal exam was relatively benign, and the decision was made to proceed with watchful waiting at home with close follow-up. On post-operative day 5, the patient reported persistent shoulder and abdominal pain, a temperature of 100.9°F overnight, and loose green stools. She was admitted for observation and underwent a CT abdomen/pelvis with oral and intravenous contrast that showed an obscured lower pelvic mass without extravasation of either oral or intravenous contrast ( Figs. 1 and and2). 2 ). However, the study sensitivity was poor secondary to the patient's thin body habitus, making detailed delineation of pelvic structures unclear. She had a negative stool panel work-up and a normocytic anemia of 10.1 g/dL (pre-op 11.3 g/dL). On post-operative day 6 (hospital day 2), the patient experienced acute worsening of abdominal pain with rebound tenderness. Abdominal and transabdominal pelvic ultrasound were performed in lieu of repeat CT imaging or immediate laparoscopy. This showed complex free fluid in the hepatorenal space ( Figs. 3 and and4). 4 ). There was also a focal hematoma in the lower pelvis measuring 7.5×6.6×4.3 cm that demonstrated an absence of internal Doppler flow, suggesting a hematoma with low likelihood of active bleed ( Figs. 5 and and6). 6 ). She was discharged home on hospital day 2 to close follow-up without further post-operative issues.

Axial view – CT abdomen/pelvis with IV and PO contrast demonstrating small-volume pneumoperitoneum (red arrow) and complex free fluid in the hepatorenal space (yellow arrow).

Coronal view – CT abdomen/pelvis with IV and PO contrast demonstrating complex hyperdense mass external to bowel located within the pelvis (yellow arrow).

Right upper quadrant transabdominal ultrasound demonstrating complex free fluid in the hepatorenal space 1.9-cm wide suggesting hemoperitoneum.

Right upper quadrant sagittal ultrasound demonstrating hemoperitoneum along the inferior hepatic margin.

Right lower quadrant sagittal ultrasound demonstrating heterogeneous mass external to bowel measuring 7.5 × 6.6 × 4.3 cm consistent with focal hematoma.

Right lower quadrant sagittal ultrasound demonstrating an absence of internal Doppler flow suggesting hematoma without active bleed.
In this case presentation, ultrasound was successfully utilized to elucidate abdominal and pelvic findings after an initial CT scan failed to provide a definitive diagnosis. This illustrates a potential role for ultrasound in the triage of post-operative pediatric patients when determining if operative management is required while minimizing further radiation exposure. There has been a recent movement to preferentially employ contrast-enhanced ultrasound to identify intraabdominal organ injury and inform further surgical management due to its comparable diagnostic accuracy to contrast-enhanced CT in the pediatric population [ 14 , 15 ]. Ultrasound can potentially produce a more detailed image compared to CT regarding internal composition of a finding, associated vascularity, and relationship with adjacent structures. With the patient described in this case, the team attributed her post-operative symptoms to peritoneal irritation by the space-occupying hematoma that was identified on ultrasound. A non-operative management strategy was utilized and was successful.
The concept of using ultrasound in the post-operative period has already been established in the adult population. For example, ultrasound is used in the soft tissue evaluation of post-hip arthroplasty pain in the setting of normal radiography [ 16 ]. Ultrasound can detect hip effusions, bursitis, tendinitis, infections, and thromboses with adequate sensitivity in this post-operative setting [ 17 ]. Additionally, in vascular surgery, duplex ultrasound demonstrates safe and effective post-operative evaluation of endoleaks when compared to concurrent computed tomography angiography (PPV 0.88; NPV 0.94) [ 18 ]. While these post-operative applications of ultrasound are distinct from the pediatric abdomen, they nonetheless describe a clinical framework for the post-operative use of ultrasound. When considering the increased radiosensitivity of pediatric organs, anatomic interference encountered with CT, and comparable diagnostic accuracy, there exists a need for risk-mitigating diagnostic modalities such as ultrasound within the pediatric population.
An important consideration is that the clinical utility of pediatric post-operative ultrasound relies on the skill of the sonographer or physician as well as the appropriate correlation of physical exam and laboratory findings. Furthermore, ultrasound has limitations over CT, including limited assessment for bowel injury, challenges associated with small field of view, and potential for poor visualization of the anatomy in patients with prominent bowel gas or large body habitus. The financial cost of diagnostic ultrasound warrants mention, and has been reported as 4-7 times less expensive than abdominal CT amongst uninsured patients when comparing national minimum and maximum prices, respectively [ 19 ]. Despite the limitations described above, ultrasound offers a safe diagnostic modality that is more cost-effective and better suited for pediatric anatomy.
Ultrasound is non-invasive, cost-effective, and can provide superior imaging quality in a certain subset of cases of pediatric post-operative pain. There exists a framework for the incorporation of ultrasound as a diagnostic tool in the post-operative pediatric setting when the etiology of pain is unclear. Ultrasound has a unique position to aid the surgeon in determining whether additional radiation exposure is warranted, and whether further surgical intervention should be pursued.
Patient consent
Written patient consent was obtained for the use of medical imaging and case details for teaching publication purposes in a deidentified manner.
Competing Interests: None.

UltrasoundCases.info
The worlds largest ultrasound case library, select your language.
Select a region to show relevant information. This may change the language
Obstetric cases
Obstetric cases – common and uncommon cases
Be boundless
Connect with us:.
© 2024 University of Washington | Seattle, WA

Case Study Library
Prepare for the rpvi, check out our vascular interpretation preceptorship, innovations in ultrasound – image and case study library.
For more than twenty years our staff at Mint Medical Education have been providing health care services across imaging modalities. With over twenty thousand case studies on file in ultrasound alone, and with more than fifteen hundred additional scans performed each month, we have a rich base of educational case studies for our medical professionals seeking to continue their medical education.
Take a look at this sampling of Case Studies discussing various aspects of diagnosis, treatment and imaging in patient care, and stay tuned as we prepare to release our Case Study Management System as part of our Vascular Interpretation Preceptorship coming this Summer.
Women’s Health Ultrasound
Vascular Ultrasound
Point-of-Care Ultrasound
- EDUCATION & CME
- REGISTRY REVIEW
ULTRASOUND CASE STUDIES & IMAGE GALLERY
This online collection of ultrasound and echocardiography images is available for free, compliments of All About Ultrasound and iHeartEcho! Register for this free resource today!
Please note that our case study and image gallery collection is ever growing and we are adding images frequently, so check back often. You can also contribute and upload your cases & images for publication on our website.
Content Modules
- Preview Publish your Case Studies!
- Start Incidental Bicuspid AV on Adult Echo (0:54)
- Start Contrast Stress Echocardiography - Anterior Wall STEMI (0:57)
- Start Tricuspid Vegetation (0:54)
- Start TEE Bubble Study (0:19)
- Start TEE Endocarditis (0:26)
- Start TEE Mitral Regurgitation (2:50)
- Start TEE Aortic Stenosis & Mitral Vegetation (0:50)
- Start TEE Bovine Aortic Valve Replacement (1:51)
- Start TEE MVR with Endocarditis (1:43)
- Start TEE Mitral Ring with Endocarditis (with 3D) (2:49)
- Start TEE MitraClip with Amplatzer (with 3D) (1:42)
- Start Patent Ductus Arteriosus (0:26)
- Start Hypoplastic Left Heart Syndrome - Fontan (1:06)
- Start Hypoplastic Left Heart Syndrome - Neonate (1:22)
- Start Muscular Ventricular Septal Defect
- Start Pericardiocentesis (1:41)
- Start Quadricuspid Aortic Valve (0:32)
- Start Adult Congenital Echo - Double Orifice Mitral Valve (with3D) (0:50)
- Start Carotid Duplex - ICA Stenosis (2:03)
- Start Venous Insufficiency (0:28)
- Start Venous LLE DVT (1:29)
- Start Venous Insufficiency (1:35)
- Start Carotid Occlusion
- Start Internal Jugular Vein Thrombus (0:16)
- Start Anterior Tibial Artery Stent Perforation (0:38)
- Start Lower Arterial Duplex - Fem-Pop Bypass (2:28)
- Start Popliteal Artery Stenosis (2:13)
- Start Hydatid Cyst
- Start Gallbladder Sludge
- Start Liver Cirrhosis
- Start Cholecystitis
- Start Epididymal Cyst
- Start Renal Angiomyolipoma (0:12)
- Start Appendicitis
- Start US Guided Thyroid FNA (0:43)
Get started now!
Free course coupon discount.
- Case Report
- Open access
- Published: 07 August 2009
Primary abdominal ectopic pregnancy: a case report
- Recep Yildizhan 1 ,
- Ali Kolusari 1 ,
- Fulya Adali 2 ,
- Ertan Adali 1 ,
- Mertihan Kurdoglu 1 ,
- Cagdas Ozgokce 1 &
- Numan Cim 1
Cases Journal volume 2 , Article number: 8485 ( 2009 ) Cite this article
21k Accesses
Metrics details
Introduction
We present a case of a 13-week abdominal pregnancy evaluated with ultrasound and magnetic resonance imaging.
Case presentation
A 34-year-old woman, (gravida 2, para 1) suffering from lower abdominal pain and slight vaginal bleeding was transferred to our hospital. A transabdominal ultrasound and magnetic resonance imaging were performed. The diagnosis of primary abdominal pregnancy was confirmed according to Studdiford's criteria. A laparatomy was carried out. The placenta was attached to the mesentery of sigmoid colon and to the left abdominal sidewall. The placenta was dissected away completely and safely. No postoperative complications were observed.
Ultrasound examination is the usual diagnostic procedure of choice. In addition magnetic resonance imaging can be useful to show the localization of the placenta preoperatively.
Abdominal pregnancy, with a diagnosis of one per 10000 births, is an extremely rare and serious form of extrauterine gestation [ 1 ]. Abdominal pregnancies account for almost 1% of ectopic pregnancies [ 2 ]. It has reported incidence of one in 2200 to one in 10,200 of all pregnancies [ 3 ]. The gestational sac is implanted outside the uterus, ovaries, and fallopian tubes. The maternal mortality rate can be as high as 20% [ 3 ]. This is primarily because of the risk of massive hemorrhage from partial or total placental separation. The placenta can be attached to the uterine wall, bowel, mesentery, liver, spleen, bladder and ligaments. It can be detach at any time during pregnancy leading to torrential blood loss [ 4 ]. Accurate localization of the placenta pre-operatively could minimize blood loss during surgery by avoiding incision into the placenta [ 5 ]. It is thought that abdominal pregnancy is more common in developing countries, probably because of the high frequency of pelvic inflammatory disease in these areas [ 6 ]. Abdominal pregnancy is classified as primary or secondary. The diagnosis of primary abdominal pregnancy was confirmed according to Studdiford's criteria [ 7 ]. In these criteria, the diagnosis of primary abdominal pregnancy is based on the following anatomic conditions: 1) normal tubes and ovaries, 2) absence of an uteroplacental fistula, and 3) attachment exclusively to a peritoneal surface early enough in gestation to eliminate the likelihood of secondary implantation. The placenta sits on the intra-abdominal organs generally the bowel or mesentery, or the peritoneum, and has sufficient blood supply. Sonography is considered the front-line diagnostic imaging method, with magnetic resonance imaging (MRI) serving as an adjunct in cases when sonography is equivocal and in cases when the delineation of anatomic relationships may alter the surgical approach [ 8 ]. We report the management of a primary abdominal pregnancy at 13 weeks.
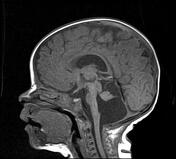
The patient was a 34-year-old Turkish woman, gravida 2 para 1 with a normal vaginal delivery 15 years previously. Although she had not used any contraceptive method afterwards, she had not become pregnant. She was transferred to our hospital from her local clinic at the gestation stage of 13 weeks because of pain in the lower abdomen and slight vaginal bleeding. She did not know when her last menstrual period had been, due to irregular periods. At admission, she presented with a history of abdominal distention together with steadily increasing abdominal and back pain, weakness, lack of appetite, and restlessness with minimal vaginal bleeding. She denied a history of pelvic inflammatory disease, sexually transmitted disease, surgical operations, or allergies. Blood pressure and pulse rate were normal. Laboratory parameters were normal, with a hemoglobin concentration of 10.0 g/dl and hematocrit of 29.1%. Transvaginal ultrasonographic scanning revealed an empty uterus with an endometrium 15 mm thick. A transabdominal ultrasound (Figure 1 ) examination demonstrated an amount of free peritoneal fluid and the nonviable fetus at 13 weeks without a sac; the placenta measured 58 × 65 × 67 mm. Abdominal-Pelvic MRI (Philips Intera 1.5T, Philips Medical Systems, Andover, MA) in coronal, axial, and sagittal planes was performed especially for localization of the placenta before she underwent surgery. A non-contrast SPAIR sagittal T2-weighted MRI strongly suggested placental invasion of the sigmoid colon (Figure 2 ).

Pelvic ultrasound scanning . Diffuse free intraperitoneal fluid was seen around the fetus and small bowel loops.

T2W SPAIR sagittal MRI of lower abdomen demonstrating the placental invasion . Placenta (a) , invasion area (b) , sigmoid colon (c) , uterine cavity (d) .
Under general anesthesia, a median laparotomy was performed and a moderate amount of intra-abdominal serohemorrhagic fluid was evident. The placenta was attached tightly to the mesentery of sigmoid colon and was loosely adhered to the left abdominal sidewall (Figure 3 ). The fetus was localized at the right of the abdomen and was related to the placenta by a chord. The placenta was dissected away completely and safely from the mesentery of sigmoid colon and the left abdominal sidewall. Left salpingectomy for unilateral hydrosalpinx was conducted. Both ovaries were conserved. After closure of the abdominal wall, dilatation and curettage were also performed but no trophoblastic tissue was found in the uterine cavity. As a management protocol in our department, we perform uterine curettage in all patients with ectopic pregnancy gently at the end of the operation, not only for the differential diagnosis of ectopic pregnancy, but also to help in reducing present or possible postoperative vaginal bleeding.

Fetus, placenta and bowels .
The patient was awakened, extubated, and sent to the room. The patient was discharged on post-operative day five with the standard of care at our hospital.
In the present case, we were able to demonstrate primary abdominal pregnancy according to Studdiford's criteria with the use of transvaginal and transabdominal ultrasound examination and MRI. In our case, both fallopian tubes and ovaries were intact. With regard to the second criterion, we did not observe any uteroplacental fistulae in our case. Since abdominal pregnancy at less than 20 weeks of gestation is considered early [ 9 ], our case can be regarded as early, and so we dismissed the possibility of secondary implantation.
The recent use of progesterone-only pills and intrauterine devices with a history of surgery, pelvic inflammatory disease, sexually transmitted disease, and allergy increases the risk of ectopic pregnancy. Our patient had not been using any contraception, and did not report a history of the other risk factors.
The clinical presentation of an abdominal pregnancy can differ from that of a tubal pregnancy. Although there may be great variability in symptoms, severe lower abdominal pain is one of the most consistent findings [ 10 ]. In a study of 12 patients reported by Hallatt and Grove [ 11 ], vaginal bleeding occurred in six patients.
Ultrasound examination is the usual diagnostic procedure of choice, but the findings are sometimes questionable. They are dependent on the examiner's experience and the quality of the ultrasound. Transvaginal ultrasound is superior to transabdominal ultrasound in the evaluation of ectopic pregnancy since it allows a better view of the adnexa and uterine cavity. MRI provided additional information for patients who needed precise diagnosing. After the diagnosis of abdominal pregnancy became definitive, it was essential to determine the localization of the placenta. Meanwhile, MRI may help in surgical planning by evaluating the extent of mesenteric and uterine involvement [ 12 ]. Non-contrast MRI using T 2 -weighted imaging is a sensitive, specific, and accurate method for evaluating ectopic pregnancy [ 13 ], and we used it in our case.
Removal of the placental tissue is less difficult in early pregnancy as it is likely to be smaller and less vascular. Laparoscopic removal of more advanced abdominal ectopic pregnancies, where the placenta is larger and more invasive, is different [ 14 ]. Laparoscopic treatment must be considered for early abdominal pregnancy [ 15 ].
Complete removal of the placenta should be done only when the blood supply can be identified and careful ligation performed [ 11 ]. If the placenta is not removed completely, it has been estimated that the remnant can remain functional for approximately 50 days after the operation, and total regression of placental function is usually complete within 4 months [ 16 ].
In conclusion, ultrasound scanning plus MRI can be useful to demonstrate the anatomic relationship between the placenta and invasion area in order to be prepared preoperatively for the possible massive blood loss.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-chief of this journal.
Abbreviations
Magnetic Resonance Imaging
Spectral Presaturation Attenuated by Inversion Recovery.
Yildizhan R, Kurdoglu M, Kolusari A, Erten R: Primary omental pregnancy. Saudi Med J. 2008, 29: 606-609.
PubMed Google Scholar
Ludwig M, Kaisi M, Bauer O, Diedrich K: The forgotten child-a case of heterotopic, intra-abdominal and intrauterine pregnancy carried to term. Hum Reprod. 1999, 14: 1372-1374. 10.1093/humrep/14.5.1372.
Article CAS PubMed Google Scholar
Alto WA: Abdominal pregnancy. Am Fam Physician. 1990, 41: 209-214.
CAS PubMed Google Scholar
Ang LP, Tan AC, Yeo SH: Abdominal pregnancy: a case report and literature review. Singapore Med J. 2000, 41: 454-457.
Martin JN, Sessums JK, Martin RW, Pryor JA, Morrison JC: Abdominal pregnancy: current concepts of management. Obstet Gynecol. 1988, 71: 549-557.
Maas DA, Slabber CF: Diagnosis and treatment of advanced extra-uterine pregnancy. S Afr Med J. 1975, 49: 2007-2010.
Studdiford WE: Primary peritoneal pregnancy. Am J Obstet Gynecol. 1942, 44: 487-491.
Google Scholar
Wagner A, Burchardt A: MR imaging in advanced abdominal pregnancy. Acta Radiol. 1995, 36: 193-195. 10.3109/02841859509173377.
Gaither K: Abdominal pregnancy-an obstetrical enigma. South Med J. 2007, 100: 347-348.
Article PubMed Google Scholar
Onan MA, Turp AB, Saltik A, Akyurek N, Taskiran C, Himmetoglu O: Primary omental pregnancy: case report. Hum Reprod. 2005, 20: 807-809. 10.1093/humrep/deh683.
Hallatt JG, Grove JA: Abdominal pregnancy: a study of twenty-one consecutive cases. Am J Obstet Gynecol. 1985, 152: 444-449.
Malian V, Lee JH: MR imaging and MR angiography of an abdominal pregnancy with placental infarction. AJR Am J Roentgenol. 2001, 177: 1305-1306.
Yoshigi J, Yashiro N, Kinoshito T, O'uchi T, Kitagaki H: Diagnosis of ectopic pregnancy with MRI: efficacy of T2-weighted imaging. Magn Reson Med Sci. 2006, 5: 25-32. 10.2463/mrms.5.25.
Kwok A, Chia KKM, Ford R, Lam A: Laparoscopic management of a case of abdominal ectopic pregnancy. Aust N Z J Obstet Gynaecol. 2002, 42: 300-302. 10.1111/j.0004-8666.2002.300_1.x.
Pisarska MD, Casson PR, Moise KJ, Di Maio DJ, Buster JE, Carson SA: Heterotopic abdominal pregnancy treated at laparoscopy. Fertil Steril. 1998, 70: 159-160. 10.1016/S0015-0282(98)00104-6.
France JT, Jackson P: Maternal plasma and urinary hormone levels during and after a successful abdominal pregnancy. Br J Obstet Gynaecol. 1980, 87: 356-362.
Download references
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, School of Medicine, Yuzuncu Yil University, Van, Turkey
Recep Yildizhan, Ali Kolusari, Ertan Adali, Mertihan Kurdoglu, Cagdas Ozgokce & Numan Cim
Department of Radiology, Women and Child Hospital, Van, Turkey
Fulya Adali
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Recep Yildizhan .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
All authors were involved in patient's care. RY, AK and FA analyzed and interpreted the patient data regarding the clinical and radiological findings of the patient and prepared the manuscript. EA, MK and CO edit and coordinated the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Yildizhan, R., Kolusari, A., Adali, F. et al. Primary abdominal ectopic pregnancy: a case report. Cases Journal 2 , 8485 (2009). https://doi.org/10.4076/1757-1626-2-8485
Download citation
Received : 12 January 2009
Accepted : 19 June 2009
Published : 07 August 2009
DOI : https://doi.org/10.4076/1757-1626-2-8485
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sigmoid Colon
- Ectopic Pregnancy
- Pelvic Inflammatory Disease
- Lower Abdominal Pain
- Transabdominal Ultrasound
Cases Journal
ISSN: 1757-1626

Renal ultrasound cases
Mike cadogan.
- Nov 3, 2020
Worked examples of clinical cases for specific pathological conditions and signs from the Renal Ultrasound Modules
Distal VUJ Stone:
- Case 1 – Case 2 – Case 3 – Case 4 – Case 5
Bladder Stone:
- Case 1 – Case 2
Distal Ureteric Stone:
- Case 1 –
ULTRASOUND LIBRARY
BA MA (Oxon) MBChB (Edin) FACEM FFSEM. Emergency physician, Sir Charles Gairdner Hospital. Passion for rugby; medical history; medical education; and asynchronous learning #FOAMed evangelist. Co-founder and CTO of Life in the Fast lane | Eponyms | Books | Twitter |
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

UCSD Ultrasound

Case # 22: Abdominal Aortic Aneurysm
A 72 year old male with known abdominal aortic aneurysm (5.7 cm s/p fem-tib bypass, L AKA) presents for 3 weeks with diarrhea and mild LLQ pain. No nausea, vomiting, fever, back pain, urinary symptoms, or blood in stool. He has no localizing abdominal exam & no peritoneal signs, strong even radial pulses, and normal cardiopulmonary exam. On further chart review, patient is noted to have a 5+ cm aorta for the past 2 years, with the most recent CT scan a few weeks ago showing growth from 5.5 cm to 5.7 cm. An abdominal ultrasound is performed with the following findings.
Vitals:
T 98.7 HR 64 BP 167/80 RR 18 O2 100%
What are we concerned about for this patient and why? What is the interpretation of the abdominal ultrasound? What are the next steps for management in the ED?
Answer and Learning Points
The patient’s presenting complaints (diarrhea, mild abdominal pain) do not coincide with the classic triad of ruptured AAA (hypotension, back pain, pulsatile abdominal mass). In addition, this patient is hemodynamically stable and comfortable, which is reassuring. However, ruptured AAA can have a wide variety of presentations and should always be considered in patients with known large AAA. In addition, this patient had a known AAA >5 cm for the past two years with poor vascular surgery follow-up, and the risk for rupture for AAA’s 5.0-5.9cm increases by 5-10% each year. (1)
As this patient recently had a CT scan a few weeks ago revealing large, stable AAA, the decision was made to investigate via ultrasound rather than undergo more radiation from CT. Ultrasound is also highly sensitive and specific for detecting AAA. (2) The above images show the AAA has a large intramural thrombus with no evidence of leaking fluid nor dissection flap. The AAA is stable, measuring a similar width of 5.7 cm. The clinician can investigate further by doing a RUSH exam to reassure against intraperitoneal bleeding and other types of shock. Elective aortic surgery is recommended for patients with AAA >5.5 cm, because at this threshold the risk of rupture is greater than risk of surgery, therefore it is reasonable to consult vascular surgery for this patient in the ED. (1)
Learning Points
- Elective aortic surgery is the most effective management, however, is not recommended until the aneurysm exceeds 5.5 cm diameter. In the ED setting, it is reasonable to consult vascular surgery for an asymptomatic patient with an incidental finding of aneurysm >5.5 cm. (1)
- A systematic review of seven studies (n=655) evaluated operating characteristics of emergency department ultrasonography for AAA. With AAA defined as >3cm dilation of aorta, the review showed that ultrasound yielded excellent diagnostic performance. (2)
- An effective abdominal aortic ultrasound requires:
(1) Evaluation of the entire aorta from the subxiphoid area to the iliac branch bifurcation. Most abdominal aortic aneurysms lie in the infrarenal aorta.
(2) Moving bowel gas out of the way with the probe with either graded compression or curvilinear probe with larger footprint
(3) Careful differentiation aorta from IVC. The aorta will be anterior to the vertebrae and the left of the IVC.
(4) Measuring outer to outer wall. Clot can create can second inner wall and falsely decrease aortic width measurement.
(1) Abdominal Aortic Aneurysms (AAA) - Cardiovascular Disorders. Merck Manuals Professional Edition. Accessed July 9, 2020. https://www.merckmanuals.com/professional/cardiovascular-disorders/diseases-of-the-aorta-and-its-branches/abdominal-aortic-aneurysms-aaa
(2) Rubano E, Mehta N, Caputo W, Paladino L, Sinert R. Systematic review: emergency department bedside ultrasonography for diagnosing suspected abdominal aortic aneurysm. Acad Emerg Med . 2013;20(2):128-138. doi: 10.1111/acem.12080
(3) Michelle H-B. Tips and Tricks: Big Red - The Aorta and How to Improve Your Image. ACEP Emergency Ultrasound. Accessed July 9, 2020. https://www.acep.org/how-we-serve/sections/emergency-ultrasound/news/february-2016/tips-and-tricks-big-red---the-aorta-and-how-to-improve-your-image/
This post was written by Caresse Vuong, MS4, Charles Murchison, MD and Amir Aminlari MD
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

- Tests and Treatments
- Pediatric Care
- Diseases and Conditions
General Ultrasound
Ultrasound imaging uses sound waves to produce pictures of the inside of the body. It helps diagnose the causes of pain, swelling and infection in the body's internal organs and to examine an unborn child (fetus) in pregnant women. In infants, doctors commonly use ultrasound to evaluate the brain, hips, and spine. It also helps guide biopsies, diagnose heart conditions, and assess damage after a heart attack. Ultrasound is safe, noninvasive, and does not use radiation.
This procedure requires little to no special preparation. Your doctor will tell you how to prepare, including whether you should not eat or drink beforehand. Leave jewelry at home and wear loose, comfortable clothing. You may need to change into a gown .
What is General Ultrasound Imaging?
What are some common uses of the procedure, how should i prepare, what does the equipment look like, how does the procedure work, how is the procedure performed, what will i experience during and after the procedure, who interprets the results and how do i get them, what are the benefits vs. risks, what are the limitations of general ultrasound imaging.
Conventional ultrasound displays the images in thin, flat sections of the body. Advancements in ultrasound technology include three-dimensional (3-D) ultrasound that formats the sound wave data into 3-D images.
A Doppler ultrasound study may be part of an ultrasound examination.
Doppler ultrasound is a special ultrasound technique that evaluates movement of materials in the body. It allows the doctor to see and evaluate blood flow through arteries and veins in the body.
There are three types of Doppler ultrasound:
- Color Doppler uses a computer to convert Doppler measurements into an array of colors to show the speed and direction of blood flow through a blood vessel.
- Power Doppler is a newer technique that is more sensitive than color Doppler and capable of providing greater detail of blood flow, especially when blood flow is little or minimal. Power Doppler, however, does not help the radiologist determine the direction of blood flow, which may be important in some situations.
- Spectral Doppler displays blood flow measurements graphically, in terms of the distance traveled per unit of time, rather than as a color picture. It can also convert blood flow information into a distinctive sound that can be heard with every heartbeat.
top of page
Ultrasound exams can help diagnose a variety of conditions and assess organ damage following illness.
Doctors use ultrasound to evaluate :
Ultrasound is a useful way of examining many of the body's internal organs, including but not limited to the:
- heart and blood vessels, including the abdominal aorta and its major branches
- gallbladder
- uterus , ovaries , and unborn child ( fetus ) in pregnant patients
- thyroid and parathyroid glands
- scrotum (testicles)
- brain in infants
- hips in infants
- spine in infants
Ultrasound is also used to:
- guide procedures such as needle biopsies , in which needles remove cells from an abnormal area for laboratory testing.
- image the breasts and guide biopsy of breast cancer ( see the Ultrasound-Guided Breast Biopsy page .
- diagnose a variety of heart conditions, including valve problems and congestive heart failure, and to assess damage after a heart attack. Ultrasound of the heart is commonly called an "echocardiogram" or "echo" for short.
Doppler ultrasound helps the doctor to see and evaluate:
- blockages to blood flow (such as clots)
- narrowing of vessels
- tumors and congenital vascular malformations
- reduced or absent blood flow to various organs, such as the testes or ovary
- increased blood flow, which may be a sign of infection
With knowledge about the speed and volume of blood flow gained from a Doppler ultrasound image, the doctor can often determine whether a patient is a good candidate for a procedure like angioplasty .
Wear comfortable, loose-fitting clothing. You may need to remove all clothing and jewelry in the area to be examined.
You may need to change into a gown for the procedure.
Preparation for the procedure will depend on the type of exam you will have. For some scans, your doctor may tell you not to eat or drink for up to 12 hours before your exam. This timeframe is lower for babies and young children. For others, the doctor may ask you to drink up to six glasses of water two hours prior to your exam and avoid urinating. This will ensure your bladder is full when the scan begins.
Ultrasound machines consist of a computer console, video monitor and an attached transducer . The transducer is a small hand-held device that resembles a microphone. Some exams may use different transducers (with different capabilities) during a single exam. The transducer sends out inaudible, high-frequency sound waves into the body and listens for the returning echoes. The same principles apply to sonar used by boats and submarines.
The technologist applies a small amount of gel to the area under examination and places the transducer there. The gel allows sound waves to travel back and forth between the transducer and the area under examination. The ultrasound image is immediately visible on a video monitor. The computer creates the image based on the loudness (amplitude), pitch (frequency), and time it takes for the ultrasound signal to return to the transducer. It also considers what type of body structure and/or tissue the sound is traveling through.
Ultrasound imaging uses the same principles as the sonar that bats, ships, and fishermen use. When a sound wave strikes an object, it bounces back or echoes. By measuring these echo waves, it is possible to determine how far away the object is as well as its size, shape, and consistency. This includes whether the object is solid or filled with fluid.
Doctors use ultrasound to detect changes in the appearance of organs, tissues, and vessels and to detect abnormal masses, such as tumors.
In an ultrasound exam, a transducer both sends the sound waves and records the echoing (returning) waves. When the transducer is pressed against the skin, it sends small pulses of inaudible, high-frequency sound waves into the body. As the sound waves bounce off internal organs, fluids and tissues, the sensitive receiver in the transducer records tiny changes in the sound's pitch and direction. A computer instantly measures these signature waves and displays them as real-time pictures on a monitor. The technologist typically captures one or more frames of the moving pictures as still images. They may also save short video loops of the images.
Doppler ultrasound, a special ultrasound technique, measures the direction and speed of blood cells as they move through vessels. The movement of blood cells causes a change in pitch of the reflected sound waves (called the Doppler effect). A computer collects and processes the sounds and creates graphs or color pictures that represent the flow of blood through the blood vessels.
For most ultrasound exams, you will lie face-up on an exam table that can be tilted or moved. Patients may turn to either side to improve the quality of the images.
The radiologist (a doctor specifically trained to supervise and interpret radiology exams) or sonographer will position you on the exam table. They will apply a water-based gel to the area of the body under examination. The gel will help the transducer make secure contact with the body. It also eliminates air pockets between the transducer and the skin that can block the sound waves from passing into your body. The sonographer places the transducer on the body and moves it back and forth over the area of interest until it captures the desired images.
There is usually no discomfort from pressure as they press the transducer against the area being examined. However, if the area is tender, you may feel pressure or minor pain from the transducer.
Doctors perform Doppler sonography with the same transducer.
Very rarely, young children may need sedation to hold still for the procedure. Parents should ask about this beforehand and be made aware of prior food and drink restrictions that sedation requires.
Once the imaging is complete, the technologist will wipe off the clear ultrasound gel from your skin. Any portions that remain will dry quickly. The ultrasound gel does not usually stain or discolor clothing.
In some ultrasound exams, the doctor attaches a probe to the transducer and inserts into a body cavity. These exams include:
- Transesophageal echocardiogram. The doctor inserts the probe into the esophagus to obtain images of the heart.
- Transrectal ultrasound. The doctor inserts the probe into a man's rectum to view the prostate.
- Transvaginal ultrasound. The doctor inserts the probe into a woman's vagina to view the uterus and ovaries .
Most ultrasound exams are painless, fast, and easily tolerated.
Ultrasound exams that insert the transducer into a body cavity may produce minimal discomfort.
If the doctor performs a Doppler ultrasound exam, you may hear pulse-like sounds that change in pitch as they monitor and measure the blood flow.
Most ultrasound exams take about 30 minutes. More extensive exams may take up to an hour.
When the exam is complete, the technologist may ask you to dress and wait while the doctor reviews the ultrasound images .
After an ultrasound exam, you should be able to resume your normal activities immediately.
A radiologist, a doctor trained to supervise and interpret radiology exams, will analyze the images. The radiologist will send a signed report to the doctor who requested the exam. Your doctor will then share the results with you. In some cases, the radiologist may discuss results with you after the exam.
You may need a follow-up exam. If so, your doctor will explain why. Sometimes a follow-up exam further evaluates a potential issue with more views or a special imaging technique. It may also see if there has been any change in an issue over time. Follow-up exams are often the best way to see if treatment is working or if a problem needs attention.
- Most ultrasound scanning is noninvasive (no needles or injections).
- Occasionally, an ultrasound exam may be temporarily uncomfortable, but it should not be painful.
- Ultrasound is widely available, easy to use, and less expensive than most other imaging methods.
- Ultrasound imaging is extremely safe and does not use radiation.
- Ultrasound scanning gives a clear picture of soft tissues that do not show up well on x-ray images.
- Ultrasound is the preferred imaging modality for the diagnosis and monitoring of pregnant women and their unborn babies.
- Ultrasound provides real-time imaging. This makes it a good tool for guiding minimally invasive procedures such as needle biopsies and fluid aspiration.
- Standard diagnostic ultrasound has no known harmful effects on humans.
Ultrasound waves are disrupted by air or gas. Therefore, ultrasound is not an ideal imaging technique for the air-filled bowel or organs obscured by the bowel. Ultrasound is not as useful for imaging air-filled lungs, but it may be used to detect fluid around or within the lungs. Similarly, ultrasound cannot penetrate bone, but may be used for imaging bone fractures or for infection surrounding a bone.
Large patients are more difficult to image by ultrasound because greater amounts of tissue weaken the sound waves as they pass deeper into the body and need to return to the transducer for analysis.
Ultrasound has difficulty penetrating bone and, therefore, can only see the outer surface of bony structures and not what lies within (except in infants who have more cartilage in their skeletons than older children or adults). Doctors typically use other imaging modalities such as MRI to visualize the internal structure of bones or certain joints.
This page was reviewed on November 01, 2022
Send us your feedback
Please type your comment or suggestion into the text box below. Note: we are unable to answer specific questions or offer individual medical advice or opinions.
Image Gallery

General ultrasound procedure
Pediatric Content
Some imaging tests and treatments have special pediatric considerations. The teddy bear denotes child-specific content.
Related Articles and Media
- Angioplasty and Vascular Stenting
- General Biopsy
- Ultrasound-Guided Breast Biopsy
- Obstetric Ultrasound
- Ultrasound - Prostate
- Images related to General Ultrasound
- Videos related to General Ultrasound
- RadInfo 4 Kids
Sponsored By
Please note
RadiologyInfo.org is not a medical facility. Please contact your physician with specific medical questions or for a referral to a radiologist or other physician. To locate a medical imaging or radiation oncology provider in your community, you can search the ACR-accredited facilities database .
This website does not provide cost information. The costs for specific medical imaging tests, treatments and procedures may vary by geographic region. Discuss the fees associated with your prescribed procedure with your doctor, the medical facility staff and/or your insurance provider to get a better understanding of the possible charges you will incur.
Web page review process: This Web page is reviewed regularly by a physician with expertise in the medical area presented and is further reviewed by committees from the Radiological Society of North America (RSNA) and the American College of Radiology (ACR), comprising physicians with expertise in several radiologic areas.
Outside links: For the convenience of our users, RadiologyInfo .org provides links to relevant websites. RadiologyInfo.org , RSNA and ACR are not responsible for the content contained on the web pages found at these links.

- Mechanical Condition Monitoring
- Bearing Lubrication Monitoring
- Air & Gas Leak Detection
- Electrical Fault Detection
- Steam Trap Testing
- Hydraulics Systems inspection
- Valve Condition Monitoring
- Tightness Testing
- LUBExpert ON-GUARD
- LEAKChecker
- LUBEChecker
- TRAPChecker
- TIGHTChecker
- ULTRAChecker
- CRYSOUND 8120 Series
- CRYSOUND 2600 Series
- Sensors & Transmitters
- LEAKReporter
- SHERLOGReporter
- Level 1/2 Ultrasound Certification
- ISO CAT I Ultrasound Certification
- ISO CAT I/II/III Vibration Certification
- SDT Ultrasound Power User
- SDT-IMCS Ultrasound Marine Power User
- Hatch Cover Tightness Testingd Certification
- Partnered Ultrasound
- LUBExpert Training
- LUBExpert Implementation Master Class
- Training Schedule and Registration
- Lifetime Warranty
- Software Support
- Hardware Support
- The SDT Family
Case Study: Electrical Inspection on High-Voltage Transformer Leads to Corona Discovery
Our client, a utility company operating in europe was looking for a reliable method for the inspection of their high-voltage electrical assets under management. they recognize that total electrical systems failures are often 10 times more expensive than planned maintenance. not to mention all the potential safety risks associated with a run-to-failure strategy with electrical assets., ultrasound is an effective way to pinpoint common electrical system defects such as arcing, tracking, partial discharge, and corona..
Arcing: Arcing occurs when electricity jumps between two conductors, creating a visible or invisible arc. Ultrasound can detect the high-frequency noise generated by arcing, helping technicians locate the source of the problem.
Tracking: Tracking is the formation of a conductive path on the surface of an insulating material, typically due to electrical breakdown. Ultrasound can detect the corona discharge and tracking sounds, allowing technicians to identify and repair damaged components.
Partial Discharge: Partial discharge is a localized breakdown of insulation that can lead to equipment failure. Ultrasound can detect the high-frequency noise produced by partial discharge, helping technicians identify areas of concern before a major failure occurs.
Corona: Corona discharge is a type of partial discharge that occurs in high-voltage systems, often leading to equipment degradation. Ultrasound can detect the ultrasonic signals produced by corona discharge, aiding in the early detection of potential issues.
The SDT340, UAS3, & Flexible Wand
By implementing an ultrasound-based inspection program using the SDT340 ultrasound data collector with a Flexible Sensor attachment, maintenance technicians can perform a wide range of inspections and checks on electrical systems, and equipment components utilizing airborne ultrasound.
Typically, inspections of electrical assets such as this transformer consist of scanning around air gaps in the paneling or vents. Circled in Figure 1 is where the inspectors found the defect. We’re listening for distinct buzzing noises. Pristine electrical equipment is silent. Further analysis can be performed in UAS3.

In the Ultrasound Spectrum seen in Figure 2 we can see peaks with a Delta F= 50Hz (electrical frequency in Europe where the readings were taken).
Periodic shocks such as this are linked to a destructive corona effect. Which will degrade insulation further.
It was recommended that the transformer be thoroughly cleaned. The successful implementation of ultrasound technology helped our client better monitor the health of their high-voltage electrical systems. They were able to proactively address a potential issue right away. Reducing future downtime.
The insights gained from these inspections, coupled with the advanced analysis capabilities of UAS3, provided ultrasound inspectors with a comprehensive solution for ensuring the reliability and longevity of their electrical assets.

SDT MISSION
SDT provides ultrasound solutions that help our customers gain a better understanding about the health of their factory. We help them predict failures, control energy costs, and improve product quality while contributing to the overall reliability of their assets.
Mechanical Condition Monitoring Bearing Lubrication Monitoring Air and Gas Leak Detection Electrical Fault Detection Steam Trap Testing Valve Condition Monitoring Hydraulics Systems Monitoring Tightness Testing Marine Applications
SDT340 SDT270 SDT200 LUBExpert The Checker Range Online4US Vigilant SonaVu Sensors-transmitters Software
Why SDT ? Highlights Contact Training Information Training Schedule Hardware Support Software Support Privacy Policy Experience Feedback
SDT Dealers Corner
SDT340 SDT270 SDT200 LUBExpert LUBExpert ON-GUARD The Checker Range Online4US Vigilant CRYSOUND Sensors-transmitters Software
- Search Menu
- Sign in through your institution
- Advance articles
- Supplement Archive
- Virtual Issues
- Editor's Choice
- Author Guidelines
- Open Access
- How to get published (video)
- Reasons to Publish
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- About Pain Medicine
- About the American Academy of Pain Medicine
- About the Faculty of Pain Medicine
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction.
- < Previous
A Systematic Review and Meta-Analysis of Efficacy of Ultrasound-Guided Single-Shot Quadratus Lumborum Block for Postoperative Analgesia in Adults Following Total Hip Arthroplasty
- Article contents
- Figures & tables
- Supplementary Data
Bikram Kishore Behera, Satyajeet Misra, Satyaki Sarkar, Nitasha Mishra, A Systematic Review and Meta-Analysis of Efficacy of Ultrasound-Guided Single-Shot Quadratus Lumborum Block for Postoperative Analgesia in Adults Following Total Hip Arthroplasty, Pain Medicine , Volume 23, Issue 6, June 2022, Pages 1047–1058, https://doi.org/10.1093/pm/pnab353
- Permissions Icon Permissions
To evaluate the efficacy of ultrasound-guided single-shot quadratus lumborum block (QLB) for postoperative analgesia in adults following total hip arthroplasty (THA).
Systematic review and meta-analysis.
Perioperative period.
Adult patients undergoing THA.
Studies were identified by performing searches in the following electronic databases, PubMed (Medline), Cochrane Central Registry of Trials (CENTRAL), and Google Scholar. We sought studies in adult patients undergoing THA, comparing QLB with a control group (no block, sham block or any other ultrasound guided regional nerve blocks). A total of 774 patients from 10 studies (7 randomized controlled, one controlled clinical and two retrospective study) were included in this meta-analysis.
The 24 hour opioid consumption was similar in both the groups (WMD −4.09; 95% CI [−9.00, 0.83]; P = 0.10; I 2 = 95%). The pain scores at rest at 24 hours was significantly less in QLB group (WMD −0.62; 95% CI [−1.15, −0.10]; P = 0.02; I 2 = 75%). The difference in pain scores was however not clinically significant. The pain scores on movement at 24 hours, time to first analgesic request, and time to discharge from hospital were similar in both the groups.
QLB as part of multimodal analgesia did not result in any significant analgesic benefits in patients undergoing hip arthroplasty in terms of either postoperative opioid consumption or pain scores at rest and on movement. Overall, the level of certainty is low. Further, well-designed trials are required to verify the results.
After total hip arthroplasty (THA), acute postoperative pain is a common problem affecting recovery, rehabilitation, and ambulation [ 1 ]. Appropriate pain management with minimal opioid use is necessary to reduce short and long-term opioid-related complications [ 2 ] .Multimodal pain management interventions, including regional nerve blocks, are used in THA to reduce pain and opioid usage [ 3 , 4 ]. Various techniques like femoral nerve block, epidural analgesia, and lumbar plexus block (LPB) used for pain management in hip arthroplasty have fallen out of favor due to their side effects along with the associated motor blockade [ 5 , 6 ]. Single-shot fascia iliaca block (FIB) or local infiltration anesthesia (LIA) are now being considered for postoperative analgesia for THA as they cause less of motor weakness thereby allow for early ambulation and participation in physical therapy following surgery [ 7 ]. Ultrasound-guided quadratus lumborum block (QLB) is a promising truncal block technique, which has been shown to provide postoperative analgesia in abdominal surgery and hip surgery [ 8–10 ]. QLB has been used for pain management following THA by many investigators but with conflicting results [ 11–20 ].
The procedure-specific postoperative pain management (PROSPECT) working group for hip arthroplasty does not currently recommend QLB for postoperative analgesia due to the availability of limited procedure-specific evidence [ 7 ]. And to date, no systematic review has assessed the efficacy of QLB specifically for THA. We, therefore, conducted this systematic review and meta-analysis of the available studies to evaluate the effectiveness of single-shot ultrasound-guided QLB compared to placebo or other nerve blocks for postoperative analgesia in adults undergoing THA.
The review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 6 June 2021, with registration number CRD42021253425 ( https://www.crd.york.ac.uk/PROSPERO ). The authors followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement guidelines for conducting this review [ 21 ].
Literature Search
Studies were identified by performing electronic searches in the following electronic databases, PubMed (Medline), Cochrane Central Registry of Trials (CENTRAL), and Google Scholar. Both Mesh terms, non-Mesh terms, and free keywords were used for database search. The following Mesh terms with Boolean operators were used to build the search strategy: ((“quadratus lumborum block” OR “QL block” OR “nerve block” OR “regional block” OR “regional anesthesia” OR “pain management” OR “postoperative pain management” OR “postoperative pain control”) AND (“hip replacement,” OR “hip surgery” OR “hip arthroplasty” OR “total hip replacement” OR “total hip arthroplasty” OR “hip joint replacement”)). Along with this, the “related articles” function of PubMed was utilized, and a manual search of the bibliography of selected articles was done to retrieve related articles. Database search was conducted from inception through April 2021, and studies reported in the English language were retrieved.
Population, Intervention, and Comparator
We sought clinical studies in adult patients undergoing THA, comparing QLB with a control group. We defined the control group as no block, sham block (QLB with saline), or other nerve blocks. For this review, three types of QLB were included and defined depending on the needle tip position and deposition of local anesthetic (LA). QLB1 (Lateral) was defined as needle tip placed, and LA deposited at the anterolateral border of the quadratus lumborum (QL) at the junction of the QL muscle with the transversalis fascia. QLB2 (Posterior) was defined as needle tip placed, and LA deposited posterior to the QL muscle. QLB3 (Anterior) was defined as needle tip placed, and LA deposited between the psoas major muscle and the QL muscle.
Pain-related outcomes included were opioid consumption in 24 hours post-operatively, pain at rest and on movement at 24-hour post-operatively, and time to first request of analgesia. Other block-related outcomes were time to ambulate, motor weakness, and block-related complications (as reported by patient/patient records or health care professionals). Postoperative nausea and vomiting (PONV), patient satisfaction, and the time to discharge from hospital were other quality of recovery and resource-related outcomes.
Data Extraction
The following information were extracted from each study: author, year of publication, study design, the sample size of the study, type of QLB, type of comparator group (sham block, no block, or any other nerve block), type of anesthesia, perioperative pain management, intraoperative and 24-hr postoperative opioid consumption, pain scores at rest and on movement at 24 hours, time to first demand of analgesia, time to discharge from hospital, PONV, block related complications, and patient satisfaction scores.
Methodological Quality Assessment
The methodological quality of each randomized controlled trials (RCT) was evaluated using the Cochrane Risk of Bias Tool [ 22 ] and the nonrandomized studies of intervention (NRSI) were evaluated using Downs and Black quality assessment system [ 23 ]. All the studies were assessed for the method of randomization, allocation concealment, blinding of participants and outcome assessors, and attrition bias. Furthermore, the study protocol was retrieved from the respective trial registries to assess the reporting bias. Conflict of interest declaration was referred to determine any other bias.
The methodological quality for each outcome pooled across trials was assessed using the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) guidelines [ 24 ]. Statistically significant results were then compared with the minimal clinically important difference (MCID) values. MCID reflects whether or not the difference can be considered clinically relevant. Outcomes were considered clinically significant only when they reached the MCID for pain score, that is, a 1.5 cm difference in pain at rest and 1.8 cm difference in pain on movement, on a 0–10 cm visual analog scale (VAS); and 10 mg reduction in intravenous morphine equivalents for opioid consumption [ 25 ].
Statistical Analysis
Mean and standard deviation (SD) for continuous variables were extracted from the studies. For studies where data were reported as the median and interquartile range (IQR), mean was derived from the median using the formula by Luo et al. [ 26 ], and SD was derived from IQR using the formula by Wan et al. [ 27 ] For studies reporting a mean and standard error (SE), the SD was derived using the formula S E = S D N where N is sample size. Studies presenting mean and 95% confidence interval (CI) data, the SD was calculated from the 95% CI using the formula, SD= √N × (Upper limit of CI—Lower limit of CI)/3.92, where N is sample size.
All pain score data were converted to a VAS score of 0–10 cm. The total opioid consumption data were converted to IV morphine equivalents in milligrams [ 28 ]. Weighted mean difference (WMD) was used for all continuous outcome variables. Risk ratio (RR) was used for summary statistics of dichotomous outcome variables. Results were considered statistically significant when P was < .05, and the 95% CI did not include the line of no treatment effect.
The meta-analysis was conducted using Review Manager Software (RevMan version 5.2; Nordic Cochrane Center, Cochrane Collaboration). Data were pooled for analysis only for this review when more than two studies reported the outcome measure. A random-effect model was used to calculate all the pooled results for significant heterogeneity; else, a fixed-effect model was used.
Assessment of Heterogeneity
The Cochrane I 2 statistic test was used to assess heterogeneity. I 2 values > 50% were considered as considerable heterogeneity [ 29 ]. The types of QLB, type, and volume of LA used, the type of anesthesia, and non-opioid usage was considered as possible factors introducing heterogeneity for assessing pain scores and opioid consumption. Leave-one-out sensitivity analyses were conducted for all outcomes based on Cochrane's recommendation.
Assessment of Publication Bias
Potential publication bias was assessed graphically with funnel plots [ 30 ]. Funnel plots were used to evaluate publication bias for each outcome measure. In the absence of reporting bias, a funnel plot is symmetrical in shape, that is, the points are scattered in the form of a funnel centrally around the total overall estimated effect. In the presence of a publication bias, the plot is asymmetrical.
Of the 634 records identified from the literature search, 65 potential studies were assessed for eligibility, of which 10 studies (seven randomized controlled [ 11–17 ], one controlled clinical [ 20 ], and two retrospective studies [ 18 , 19 ] were included in this review ( Figure 1 ). A total of 774 patients underwent THA, of whom 346 patients received ultrasound-guided single-shot QLB, and 428 patients were in a control group (no block, sham block, or other nerve block).

PRISMA flow diagram.
Figure 2 summarizes the risk of bias of the RCTs included in this meta-analysis as assessed with Cochrane’s RoB Tool [ 22 ]. There was one study with an unclear risk of bias in all assessed categories [ 14 ]. Unclear risk of bias related to blinding of outcome assessors was present in one additional study [ 15 ] and related to selective reporting (protocol not found) was present in two other studies [ 11 , 15 ]. High risk of bias for selective reporting was found in one study [ 16 ]. Among the NRSI included in this review, one was good quality study [ 18 ], and two were of fair quality [ 19 , 20 ] as assessed with Downs and Black quality assessment [ 23 ].

Risk of bias summary according to Cochrane’s risk of bias tool.
Characteristics of Studies
Table 1 presents the study characteristics. Two studies compared QLB2 [ 12 , 19 ], and the rest eight studies compared QLB3 [ 11 , 13–18 , 20 ] .Blocks were performed before surgery in all studies except in two studies [ 11 , 14 ], where it was performed at the end of surgery. THA was carried out under spinal anesthesia (SA) in five studies [ 11 , 13 , 15–17 ], under combined spinal-epidural in one study [ 14 ], and under general anesthesia (GA) in three studies [ 12 , 18 , 20 ], and under GA or SA in one study [ 19 ]. The LA agents used for QLB were bupivacaine in three studies [ 11 , 16 , 17 ] and ropivacaine in seven studies [ 12–15 , 18–20 ]. The volume of LA used varied from 20 to 40 mL. LA additives dexamethasone + dexmedetomidine were used in one study [ 15 ], and epinephrine was used in another study [ 16 ].
Summary of included studies
| . | Study . | Type of Surgery . | Type of QLB . | Comparator Group . | Type of Anesthesia . | Primary Outcome Studied . | Conclusion of the Study . | LA Agent and Volume of Drug Used for QLB . | Intraop Analgesia . | Postop Analgesia . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ] 2020 | THA | Sham block (n = 30) | SA | 24 hr opioid consumption | Intrathecal fentanyl | ||||
| 2 | ] | THA | GA | 24 hr opioid consumption | ||||||
| 3 | ] 2020 | THA | SA | NRS pain score 24 hours after surgery | QLB3 yields non-inferior analgesia compared with LPB for hip replacement surgery | Nil | ||||
| 4 | ] | THA | CSE | Dexmedetomidine infusion | ||||||
| 5 | ] | THA | SA | Pain scores at different time points | Nil | |||||
| 6 | ] 2019 | THA | SA | Pain scores and 24 hr opioid consumption | Significant opioid sparing up to 48 hr of surgery in QLB group | Nil | Opioids as required | |||
| 7 | ] | THA | SA | Time to first rescue analgesia | 30 ml 0.25% BupivacaineBlock performed before spinal anesthesia | Intrathecal fentanyl | ||||
| 8 | ] 2018 | THA | GA | 24 hr opioid consumption | IV fentanyl | |||||
| 9 | ] 2019 [ ] | THA | GA or SA | 24 hr opioid consumption | QLB decreased opioid requirements up to 48 hr of surgery | Opioids as required | Opioids as required | |||
| 10 | ] | THA | GA | Length of hospital stay | IV fentanyl | IV fentanyl bolus as required |
| . | Study . | Type of Surgery . | Type of QLB . | Comparator Group . | Type of Anesthesia . | Primary Outcome Studied . | Conclusion of the Study . | LA Agent and Volume of Drug Used for QLB . | Intraop Analgesia . | Postop Analgesia . |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ] 2020 | THA | Sham block (n = 30) | SA | 24 hr opioid consumption | Intrathecal fentanyl | ||||
| 2 | ] | THA | GA | 24 hr opioid consumption | ||||||
| 3 | ] 2020 | THA | SA | NRS pain score 24 hours after surgery | QLB3 yields non-inferior analgesia compared with LPB for hip replacement surgery | Nil | ||||
| 4 | ] | THA | CSE | Dexmedetomidine infusion | ||||||
| 5 | ] | THA | SA | Pain scores at different time points | Nil | |||||
| 6 | ] 2019 | THA | SA | Pain scores and 24 hr opioid consumption | Significant opioid sparing up to 48 hr of surgery in QLB group | Nil | Opioids as required | |||
| 7 | ] | THA | SA | Time to first rescue analgesia | 30 ml 0.25% BupivacaineBlock performed before spinal anesthesia | Intrathecal fentanyl | ||||
| 8 | ] 2018 | THA | GA | 24 hr opioid consumption | IV fentanyl | |||||
| 9 | ] 2019 [ ] | THA | GA or SA | 24 hr opioid consumption | QLB decreased opioid requirements up to 48 hr of surgery | Opioids as required | Opioids as required | |||
| 10 | ] | THA | GA | Length of hospital stay | IV fentanyl | IV fentanyl bolus as required |
RCT = randomized controlled trial; THA = total hip arthroplasty; QLB = quadratus lumborum block; LPB = lumbar plexus block; FIB = fascia iliaca block; GA = general anesthesia; SA = spinal anesthesia; CSE = combined spinal epidural; IVPCA = intravenous patient controlled analgesia; NSAIDs = non-steroidal anti-inflammatory drugs;LA= local anesthetics.
Perioperative pain management was similar in both the groups studied. None of the studies used intrathecal morphine. Out of the five studies that used SA, only two studies used intrathecal fentanyl [ 11 , 17 ]. Paracetamol was prescribed as standard postoperative order as part of multimodal analgesia in six studies [ 11–13 , 15 , 17 , 18 ]. Various non-steroidal anti-inflammatory agents (NSAID)s and COX-2 inhibitors were used in six studies either alone or with injection paracetamol [ 12–15 , 17 , 18 ]. Intravenous patient-controlled analgesia (IVPCA) with opioids was used for postoperative analgesia in three studies. Two studies used IVPCA morphine [ 12 , 15 ], and one used IVPCA sufentanil [ 14 ].
Pain-related outcomes (Opioid consumption, Pain at rest and on movement, Time to request for first analgesia)
Overall opioid consumption was not different in patients receiving QLB compared to control group (WMD -4.09; 95% CI [-9.00, 0.83]; P = 0.10; I 2 = 95%) ( Figure 3 ). The reduction in opioid consumption by approximately 4 mg was also not clinically significant as it failed to reach MCID.

Opioid consumption (24 hr).
When compared to control group, QLB resulted in significantly less pain at rest (WMD −0.62; 95% CI [−1.15, −0.10]; P = 0.02; I 2 = 75%) ( Figure 4 ). The reduction in VAS score at rest was not clinically significant as it failed to reach MCID.

Pain scores at rest at 24 hr.
Four studies [ 13–15 , 17 ] reported pain on movement at 24-hr after surgery. Pain on movement was similar in both the groups (WMD −1.52; 95% CI [−3.34, 0.30); P = 0.10; I 2 = 96%). The reduction in VAS score of 1.52 cm on movement was not clinically significant as it failed to reach MCID.
Three studies [ 11 , 16 , 17 ] reported the time to first request of analgesia. There was no difference in the groups in the time to first request of analgesia [WMD −0.24; 95% CI [−3.39, 2.90]; P = 0.88; I 2 = 52%).
Block related outcomes (Ambulation, Muscle power, and Block related complications)
Time to ambulation was reported by Brixel et al. [ 12 ] There was no significant difference in the time to ambulation between patients receiving QLB vs. sham block ( P = .173). Another rehabilitation outcome reported by the same authors was the time to first standing, which was not different in both groups [ 12 ]. Gutierrez et al. [ 13 ] reported time to 100 feet walking and found no difference in the QLB or LPB groups ( P = 1.00). He et al. [ 14 ] reported a range of hip joint movements and found better results with QLB than the sham block. In a different study [ 15 ], the same author also reported a 10-meter walk test but didn't have enough data for statistical analysis. Kukreja et al. [ 16 ] reported ambulation distance and found no difference between the QLB and no block groups. The ambulatory outcomes reported by various authors were different, and therefore, the data from these studies couldn't be used for meta-analysis.
Gutierrez et al. [ 13 ] and Nassar et al. [ 17 ] reported quadriceps muscle power following surgery. They reported a significantly lower incidence of quadriceps weakness and better muscle power in patients receiving QLB than patients receiving LPB or FIB. Brixel et al. [ 12 ] reported significant motor weakness only in one patient in the sham block.
Abduallah et al. [ 11 ] reported similar incidences of bradycardia, hypotension, and pruritus in both the QLB and sham block groups. He et al. [ 14 ] reported an equal incidence of urinary retention and respiratory depression in both QLB and sham block groups ( P > .05). The same author in another study reported a lower incidence of urinary retention in the QLB group ( P = .03) [ 15 ].
Quality of recovery and resource-related outcomes (PONV, Patient satisfaction, Time to discharge from hospital)
Four studies [ 11 , 12 , 14 , 15 ] reported PONV. The incidence of PONV was significantly less in the QLB group as compared to control group, 9% vs 26% respectively (RR 0.33; 95% CI [0.20, 0.56]; P < .0001; I 2 = 0%).
Four studies reported patient satisfaction [ 11 , 14–16 ]. Patient satisfaction was assessed by different non-standardized scores and recorded at different time points, making it impractical to pool the data for meta-analysis. Overall satisfaction scores were better in the QLB group and reached statistical significance in three studies [ 14–16 ].
Four studies [ 12 , 16 , 19 , 20 ] reported the time to discharge from hospital (in days). The time to discharge from hospital was not different in both the groups (WMD −0.30; 95% CI [−0.73, 0.13]; P = 0.17; I 2 = 56%).
Leave-one-out sensitivity analyses were conducted for all outcomes by leaving out one study each at a time for each analysis. None of the studies substantially influenced the heterogeneity for all the outcome measures.
Summary of the outcome data and the level of evidence (GRADE) are presented in Table 2 . The quality of evidence was downgraded by one level for the following reasons: limitation in the design and implementation of available studies (suggesting bias); inconsistency of results (considerable heterogeneity or small sample size); and imprecision of results (wide confidence intervals).
Summary of the outcomes and GRADE
| Outcomes | Studies Included | Number of Participants | WMD or RR (95%CI) | P-value for Statistical Significance | I2 -test for Heterogeneity | P-value or Heterogeneity | Quality of Evidence (GRADE) | Importance | ||
| [ ] | 754 | .1 | 95% | <.00001 | ⊕⊕⊝⊝ | Post-op opioid consumption was similar in both the groups | ||||
| [ ] | 714 | .02 | 75% | <.00001 | ⊕⊕⊝⊝ | Pains scores at rest was significantly better in QLB group | ||||
| [ ] | 225 | .1 | 96% | <.00001 | ⊕⊕⊝⊝ | Pain scores on movement were similar in both groups | ||||
| Intra-op opioid consumption | [ ] | 418 | .22 | 67% | .03 | ⊕⊕⊝⊝ | Intra-op opioid consumption was similar in both the groups | |||
| Time to first analgesia request (in hours) | [ ] | 167 | .88 | 52% | .12 | ⊕⊕⊝⊝ | Time to demand of first rescue analgesia was similar in both the groups | |||
| [ ] | 251 | .17 | 56% | .8 | ⊕⊕⊝⊝ | Time to discharge from hospital was similar in both the groups | ||||
| PONV | [ ] | 303 | <.0001 | 0% | .40 | ⊕⊕⊕⊝ | Risk of PONV was less by 67% in QLB group | |||
| Patient satisfaction | N/A | N/A | ||||||||
| Block related complications | N/A | N/A | ||||||||
| Outcomes | Studies Included | Number of Participants | WMD or RR (95%CI) | P-value for Statistical Significance | I2 -test for Heterogeneity | P-value or Heterogeneity | Quality of Evidence (GRADE) | Importance | ||
| [ ] | 754 | .1 | 95% | <.00001 | ⊕⊕⊝⊝ | Post-op opioid consumption was similar in both the groups | ||||
| [ ] | 714 | .02 | 75% | <.00001 | ⊕⊕⊝⊝ | Pains scores at rest was significantly better in QLB group | ||||
| [ ] | 225 | .1 | 96% | <.00001 | ⊕⊕⊝⊝ | Pain scores on movement were similar in both groups | ||||
| Intra-op opioid consumption | [ ] | 418 | .22 | 67% | .03 | ⊕⊕⊝⊝ | Intra-op opioid consumption was similar in both the groups | |||
| Time to first analgesia request (in hours) | [ ] | 167 | .88 | 52% | .12 | ⊕⊕⊝⊝ | Time to demand of first rescue analgesia was similar in both the groups | |||
| [ ] | 251 | .17 | 56% | .8 | ⊕⊕⊝⊝ | Time to discharge from hospital was similar in both the groups | ||||
| PONV | [ ] | 303 | <.0001 | 0% | .40 | ⊕⊕⊕⊝ | Risk of PONV was less by 67% in QLB group | |||
| Patient satisfaction | N/A | N/A | ||||||||
| Block related complications | N/A | N/A | ||||||||
GRADE Working Group grades of evidence GRADE: Grades of Recommendation, Assessment, Development, and Evaluation.
⊕⊕⊕⊕, high-quality evidence: The true effect lies close to that of the estimate of the effect.
⊕⊕⊕⊝, moderate-quality evidence: The true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different.
⊕⊕⊝⊝, low-quality evidence: The true effect may be substantially different from the estimate of the effect
⊕⊝⊝⊝, very low-quality evidence: The true effect is likely to be substantially different from the estimate of effect.
Explanations:
Level of evidence were downgraded to low-quality evidence for the following reasons.
WMD = weighted mean difference; RR = risk ratio; VAS = visual analog scale; QLB = quadratus lumborum block.
Limitation in the design and implementation of available studies, suggesting of bias.
Inconsistency of results (considerable heterogeneity or small sample size).
Imprecision of results (wide confidence intervals).
This review is the first to objectively assess and summarize the available evidence regarding the analgesic efficacy of QLB specifically for THA. The main findings of this systematic review and meta-analysis were as follows: QLB added to multimodal analgesia did not result in any significant analgesic benefit in patients undergoing THA in terms of either postoperative opioid consumption or pain scores at rest and on movement.
The 24-hour postoperative opioid consumption was not statistically significant, and morphine consumption was approximately 4 mg less in the QLB group than placebo. This failed to reach clinical significance (MCID for opioid consumption < 10 mg of IV morphine equivalents). However, to detect meaningful differences in opioid consumption, a total of 2,029 patients in each group would be required [ 12 ], and opioid consumption was the primary outcome in only five studies [ 11 , 12 , 16 , 18 , 19 ] in this review and thus, seriously underpowered to detect any differences.
Studies have shown that while regional nerve block techniques can lead to postoperative pain relief, there is no “single best technique” available for THA [ 31–33 ]. QLB is a relatively recent technique that has been adopted for abdominal, pelvic, and hip surgery. The previous meta-analyses on the efficacy of QLB for postoperative analgesia have included various types of abdominal surgeries along with pelvic and hip surgery [ 8–10 ]. Therefore, any effect of QLB on postoperative analgesia and other outcomes following THA cannot be extrapolated from these reviews.
Assessment of pain related clinical outcomes and treatment efficacy is difficult to measure due to its multifaceted and subjective nature. Most clinical studies on assessment of analgesic efficacy use two tools: reduction in opioid consumption and reduction of pain scores [ 34 ]. The opioid consumption and pain scores together may be considered as surrogate measure of the pain burden. Most of the studies in our review used either of these two criteria as the primary outcome measure except the two studies, where the length of hospital stay [ 20 ] and time to first analgesia request [ 17 ] were the primary outcome of the studies.
The pain scores at rest were significantly less in patients receiving QLB, but it failed to reach MCID and cannot be considered clinically significant. For interpretation of the analgesic efficacy the QLB should result in both statistical significant effect and clinically significant effect (MCID). Mean pain scores at rest measured at 24-hour were relatively low in all the patients studied. Pain after THA peaks at two hours and reduces to moderate pain (VAS <4) after four hours [ 35 ]. This reduction of pain intensity after four hours of surgery may be the reason for the lack of clinically significant difference in pain intensity scores (MCID for pain at rest > 1.5 cm) when measured at 24 hours after surgery. Furthermore, studies differed in the manner they assessed pain, and pain scores should not be considered as functional measure of pain reduction [ 36 ].
The postoperative analgesic use was not uniform across the studies. IVPCA, rescue opioid boluses, non-opioid medications (paracetamol, NSAIDs, COX-2 inhibitors), other drugs like clonidine, dexamethasone, and so forth, were used in various combinations, which could have affected opioid consumption and pain scores, and thus might have introduced bias in the interpretation of these results.
Only three studies [ 11 , 16 , 17 ] reported the time to first rescue analgesia. We found no difference in the time to first rescue analgesia in both groups. QLB has a possibly longer duration of action when compared to other nerve blocks since it is a fascial plane truncal block. However, the volumes of LA used, the type of agent, use of additives, different IVPCA regimens, and use of different types of non-opioid analgesics could have led to the variability in the time to first rescue analgesia in the included studies. Furthermore, QLB 2 and QLB 3 have different spread and blocks different nerves and may have differing effects on the duration of postoperative analgesia [ 37 , 38 ].
Only a few studies reported the rehabilitation outcomes in this meta-analysis which were not uniform to be pooled. Only two studies reported quadriceps muscle weakness as a rehabilitation outcome measure [ 13 , 17 ] and reported less muscle weakness in the QLB group than LPB or FIB. At the moment, QLB appears to result in less motor and quadriceps weakness compared to other active comparators for THA. Other regional nerve block techniques like pericapsular nerve group (PENG) block is becoming popular for their motor sparing effects in THA. Unlike LPB and FIB, PENG block targets the pain carrying articular branches and thus minimizes the risk of motor weakness. However, more data is required to make any conclusion.
Patient satisfaction is an important patient-reported outcome and is a measure of perioperative care. It was reported by four studies [ 11 , 14–16 ], and it was significantly better in three studies in patients receiving QLB [ 14–16 ]. However, most of the studies used different non-validated questionnaires and instruments to measure this outcome. Hence the data could not be imputed for a meta-analysis. This also calls for developing standardized methods for measuring patient satisfaction after surgery in future studies.
Our meta-analysis has many significant limitations. A notable limitation is the small number of RCTs available in the literature. Another limitation was the methodological heterogeneity of the included studies. Variable control groups (no block, sham block, other regional nerve blocks); different types of anesthesia (SA, combined spinal-epidural, and GA); different approaches of QLB (anterior and posterior); different drugs and volumes of LA; use of LA additives; and various types of postoperative non-opioid analgesic regimens may have contributed to the heterogeneity. This led us to the downgrading of evidence for all the measured outcome variables. There is also very limited number studies available for comparison of QLB with an active comparator (other analgesic techniques/nerve blocks). Hence, a subgroup analysis was not conducted for any of the outcome measures. Another limitation of this meta-analysis was that most of the studies included were not powered according to predefined MCID values for either pain or opioid consumption. Though there is no gold standard MCID values for interpretation of clinical relevance of statistically significant values in pain research and reporting [ 24 ], interpretation of statistically different results needs further questioning by the clinicians, if they are clinically meaningful or not.
To the best of our knowledge, this review and meta-analysis is the first of its kind in addressing the effectiveness of QLB in patients undergoing THA. Our results showed that QLB did not result in any clinically significant reduction in postoperative opioid consumption and pain scores in adult patients following THA. However, the level of certainty of these findings are low and results of this meta-analysis needs to be construed with caution due to small sample size, availability of limited number of studies and significant heterogeneity with clinical variations of the included studies.
As the number of THA performed worldwide increases, it becomes important to identify the perioperative strategies that result in effective postoperative analgesia and other clinically meaningful outcomes. The future RCTs should be designed with consensus on uniform drug volumes, doses. and LA additives. Furthermore, the future studies should also be powered to predefined MCID values and compare active controls like FIB, LPB, and PENG block to identify the best possible procedure-specific nerve block for THA. As opioid consumption and pain scores cannot be the only criteria for defining the effectiveness of a regional nerve block technique; other criteria like patient satisfaction, postoperative rehabilitation outcomes, measures of quadriceps muscle power and ambulation following surgery and so forth need to be uniformly defined and compared in future trials.
At present, with the limited number of available studies with significant clinical variations, our meta-analysis does not allow us to make any firm conclusion on the effectiveness of QLB for patients undergoing THA.
Disclosure statement: Author agreement: All authors have seen and approved the final version of the manuscript being submitted. The article is the authors' original work, has not received prior publication, and is not under consideration for publication elsewhere.
Conflict of interest: There are no conflicts of interest to report.
Funding source: No funding or financial support from any agency or organization has been received for this work.
Permission note: None.
Trial registration: This review was prospectively registered with PROSPERO on 6 June 2021 with registration number CRD42021253425.
CRediT author statement
1. Bikram Kishore Behera: This author helped in Conceptualization, Methodology, Data curation, Formal analysis, Visualisation, Original draft preparation, Reviewing and Editing, Final approval of the manuscript.
2. Satyajeet Misra: This author helped in Methodology, Data curation, Formal analysis, Visualisation, Reviewing and Editing, Final approval of the manuscript.
3. Satyaki Sarkar: This author helped in Methodology, Data curation, Formal analysis, Visualisation, Reviewing and Editing, Final approval of the manuscript.
4. Nitasha Mishra: This author helped in Methodology, Data curation, Formal analysis, Reviewing and Editing, Final approval of the manuscript.
Ong Sio LC , Vo C , Bautista A. Quadratus lumborum block as a rescue block following total hip arthroplasty . Pain Med 2021 ; 22 ( 3 ): 746 – 9 .
Google Scholar
Nelson ER , Gan TJ , Urman RD. Predicting postoperative pain: A complex interplay of multiple factors . Anesth Analg 2021 ; 132 ( 3 ): 652 – 5 .
Min BW , Kim Y , Cho HM , Park KS , et al. Perioperative pain management in total hip arthroplasty: Korean Hip Society guidelines . Hip Pelvis 2016 ; 28 ( 1 ): 15 – 23 .
Pagnano MW , Hebl J , Horlocker T. Assuring a painless total hip arthroplasty: A multimodal approach emphasizing peripheral nerve blocks . J Arthroplasty 2006 ; 21 (4 Suppl 1): 80 – 4 .
Guay J , Johnson RL , Kopp S. Nerve blocks or no nerve blocks for pain control after elective hip replacement (arthroplasty) surgery in adults . Cochrane Database Syst Rev 2017 ; 10 : CD011608 .
J Joshi G , Gandhi K , Shah N , Gadsden J , Corman SL. Peripheral nerve blocks in the management of postoperative pain: Challenges and opportunities . J Clin Anesth 2016 ; 35 : 524 – 9 .
Anger M , Valovska T , Beloeil H , et al. ; PROSPECT Working Group and the European Society of Regional Anaesthesia and Pain Therapy. PROSPECT guideline for total hip arthroplasty: A systematic review and procedure-specific postoperative pain management recommendations . Anaesthesia 2021 ; 76 ( 8 ): 1082 – 97 .
Korgvee A , Junttila E , Koskinen H , Huhtala H , Kalliomaki ML. Ultrasound-guided quadratus lumborum block for postoperative analgesia: A systematic review and meta-analysis . Eur J Anaesthesiol 2021 ; 38 ( 2 ): 115 – 29 .
Uppal V , Retter S , Kehoe E , McKeen DM. Quadratus lumborum block for postoperative analgesia: A systematic review and meta-analysis . Can J Anaesth 2020 ; 67 ( 11 ): 1557 – 75 .
Jin Z , Liu J , Li R , Gan TJ , He Y , Lin J. Single injection Quadratus Lumborum block for postoperative analgesia in adult surgical population: A systematic review and meta-analysis . J Clin Anesth 2020 ; 62 : 109715 .
Abduallah MA , Ahmed SA , Abdelghany MS. The effect of postoperative ultrasound-guided transmuscular quadratus lumborum block on postoperative analgesia after hip arthroplasty in elderly patients: A randomised controlled double-blind study . Indian J Anaesth 2020 ; 64 ( 10 ): 887 – 93 .
Brixel SM , Biboulet P , Swisser F , et al. Posterior quadratus lumborum block in total hip arthroplasty: A randomized controlled trial . Anesthesiology 2021 ; 134 ( 5 ): 722 – 33 .
Gutierrez JJ , Ben-David B , Rest C , Grajales MT , Khetarpal SK. Quadratus lumborum block type 3 versus lumbar plexus block in hip replacement surgery: A randomized, prospective, non-inferiority study . Reg Anesth Pain Med 2021 ; 46 ( 2 ): 111 – 7 .
He J , Zheng X , Luo C , et al. Evaluation of the effect of ultrasound-guided quadratus lumborum block for hip replacement surgery . Nat Med J China 2018 ; 98 : 565 – 9 .
He J , Zhang L , He WY , et al. Ultrasound-guided transmuscular quadratus lumborum block reduces postoperative pain intensity in patients undergoing total hip arthroplasty: A randomized, double-blind, placebo-controlled trial . Pain Res Manag 2020 ; 2020 : 1 – 8 .
Kukreja P , MacBeth L , Sturdivant A , et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty: A randomized, controlled study . Reg Anesth Pain Med 2019 ; 44 : 1075 – 9 .
Nassar H , Hasanin A , Sewilam M , et al. Transmuscular quadratus lumborum block versus suprainguinal fascia iliaca block for hip arthroplasty: A randomized, controlled pilot study . Local Reg Anesth 2021 ; 14 : 67 – 74 .
Adhikary SD , Short AJ , El-Boghdadly K , Abdelmalak MJ , Chin KJ. Transmuscular quadratus lumborum versus lumbar plexus block for total hip arthroplasty: A retrospective propensity score matched cohort study . J Anaesthesiol Clin Pharmacol 2018 ; 34 ( 3 ): 372 – 8 .
Kukreja P , MacBeth L , Potter W , et al. Posterior quadratus lumborum block for primary total hip arthroplasty analgesia: A comparative study . Einstein (Sao Paulo) 2019 ; 17 : eAO4905 .
Green MS , Hoffman CR , Iqbal U , Ives OO , Hurd B. Transmuscular quadratus lumborum block reduces length of stay in patients receiving total hip arthroplasty . Anesth Pain 2018 ; 8 ( 6 ): e80233 .
Page MJ , McKenzie JE , Bossuyt PM , et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews . Syst Rev 2021 ; 10 ( 1 ): 89 .
Higgins JP , Thomas J , Chandler J , et al. Cochrane Handbook for Systematic Reviews of Interventions . Chichester, UK : John Wiley & Sons; 2019 .
Google Preview
Downs SH , Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions . J Epidemiol Community Health 1998 ; 52 ( 6 ): 377 – 84 .
Guyatt G , Oxman AD , Akl EA , et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables . J Clin Epidemiol 2011 ; 64 ( 4 ): 383 – 94 .
Laigaard J , Pedersen C , Rønsbo TN , Mathiesen O , Karlsen APH. Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: A systematic review . Br J Anaesth 2021 ; 126 ( 5 ): 1029e1037 .
Luo D , Wan X , Liu J , Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range . Stat Methods Med Res 2018 ; 27 ( 6 ): 1785 – 805 .
Wan X , Wang W , Liu J , Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range . BMC Med Res Methodol 2014 ; 14 : 135 .
Treillet E , Laurent S , Hadjiat Y. Practical management of opioid rotation and equianalgesia . J Pain Res 2018 ; 11 : 2587 – 601 .
Cumpston M , Li T , Page MJ , Chandler J , et al. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions . Cochrane Database Syst Rev 2019 ; 10 : ED000142 .
Lin L , Chu H. Quantifying publication bias in meta-analysis . Biometrics 2018 ; 74 ( 3 ): 785 – 94 .
Hu J , Wang Q , Zeng Y , Xu M , Gong J , Yang J. The impact of ultrasound-guided transmuscular quadratus lumborum block combined with local infiltration analgesia for arthroplasty on postoperative pain relief . J Clin Anesth 2021 ; 73 : 110372 .
Lennon MJ , Isaac S , Currigan D , O'Leary S , Khan RJK , Fick DP. Erector spinae plane block combined with local infiltration analgesia for total hip arthroplasty: A randomized, placebo controlled, clinical trial . J Clin Anesth 2021 ; 69 : 110153 .
Cappelleri G , Ghisi D. Postoperative analgesia after total hip arthroplasty: Still a long way to go . Minerva Anestesiol 2021 ; 87 ( 6 ): 627 – 29 .
Younger J , McCue R , Mackey S. Pain outcomes: A brief review of instruments and techniques . Curr Pain Headache Rep 2009 ; 13 ( 1 ): 39 – 43 .
Panzenbeck P , von Keudell A , Joshi GP , et al. Procedure-specific acute pain trajectory after elective total hip arthroplasty: Systematic review and data synthesis . Br J Anaesth 2021 ; 127 ( 1 ): 110 – 32 .
Jouguelet-Lacoste J , La Colla L , Schilling D , Chelly JE. The use of intravenous infusion or single dose of low-dose ketamine for postoperative analgesia: A review of the current literature . Pain Med 2015 ; 16 ( 2 ): 383 – 403 .
Ueshima H , Otake H , Lin JA. Ultrasound-guided quadratus lumborum block: An updated review of anatomy and techniques . Biomed Res Int 2017 ; 2017 : 2752876 .
Elsharkawy H , El-Boghdadly K , Kolli S , et al. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block: A comparative cadaveric study . Eur J Anaesthesiol 2017 ; 34 ( 9 ): 587 – 95 .
- ultrasonography
- anesthesia, conduction
- patient discharge
- pain management
- hip replacement arthroplasty
- weapons of mass destruction
- quadratus lumborum muscle
- postoperative analgesia
- multimodal analgesia
| Month: | Total Views: |
|---|---|
| January 2022 | 27 |
| February 2022 | 14 |
| March 2022 | 17 |
| April 2022 | 30 |
| May 2022 | 18 |
| June 2022 | 68 |
| July 2022 | 16 |
| August 2022 | 15 |
| September 2022 | 13 |
| October 2022 | 36 |
| November 2022 | 4 |
| December 2022 | 6 |
| January 2023 | 12 |
| February 2023 | 14 |
| March 2023 | 13 |
| April 2023 | 7 |
| May 2023 | 8 |
| June 2023 | 34 |
| July 2023 | 47 |
| August 2023 | 40 |
| September 2023 | 48 |
| October 2023 | 38 |
| November 2023 | 28 |
| December 2023 | 27 |
| January 2024 | 23 |
| February 2024 | 26 |
| March 2024 | 30 |
| April 2024 | 39 |
| May 2024 | 43 |
| June 2024 | 33 |
| July 2024 | 19 |
Email alerts
Citing articles via.
- Recent Supplements
- Recommend to your Library
Affiliations
- Online ISSN 1526-4637
- Copyright © 2024 American Academy of Pain Medicine
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Evaluation of the diagnostic value of YiDiXie™-SS in thyroid ultrasound-positive patients
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- For correspondence: [email protected]
- Info/History
- Preview PDF
Background: Thyroid tumor, as an endocrine tumor with increasing incidence, causes a heavy economic burden. Ultrasound scanning is widely used for screening or preliminary diagnosis of thyroid tumors, but its large number of false-positive results brings unnecessary mental pain, expensive examination costs, physical injury and other adverse consequences. There is an urgent need to find a convenient, cost-effective and noninvasive method to reduce the false-positive rate of thyroid ultrasound. The aim of this study was to evaluate the diagnostic value of YiDiXie™-SS in thyroid ultrasound-positive patients. Patients and methods: 360 subjects ( malignant group, n=342; benign group, n=18) were finally included in this study. The remaining serum samples were collected and tested by YiDiXie™ all-cancer detection kit. The sensitivity and specificity of YiDiXie™-SS were evaluated respectively. Results: The sensitivity of YiDiXie™-SS in the malignant group was 98.5%(95% CI: 96.6% - 99.4%; 337/342) with a false negative rate of 1.5%(95% CI: 0.6% - 3.4%; 5/342). The specificity of YiDiXie™-SS for the benign group was 66.7%(95% CI: 43.7% - 83.7%; 12/18), and the false positive rate was 33.3%(95% CI: 16.3% - 56.3%; 12/18). This means that YiDiXie™-SS reduces the false positive rate by 66.7%(95% CI: 43.7% - 83.7%; 12/18) with essentially no increase in malignancy leakage. Conclusion: YiDiXie™-SS significantly reduces the false-positive rate of thyroid ultrasound-positive patients without increasing the number of under-diagnosed malignant tumors. YiDiXie™-SS has vital diagnostic value in thyroid ultrasound-positive patients, and is expected to solve the problem of "high false-positive rate of thyroid ultrasound". Clinical trial number: ChiCTR2200066840. Key words: Thyroid cancer, Ultrasound Scan, False-positive, YiDiXie™-SS
Competing Interest Statement
The authors have declared no competing interest.
Clinical Trial
ChiCTR2200066840
Funding Statement
This work was supported by Shenzhen High-level Hospital Construction Fund, Clinical Research Project of Peking University Shenzhen Hospital (LCYJ2020002, LCYJ2020015, LCYJ2020020, LCYJ2017001).
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
Ethics committee of Peking University Shenzhen Hospital gave ethical approval for this work.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
All data produced in the present study are contained in the manuscript.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Addiction Medicine (329)
- Allergy and Immunology (650)
- Anesthesia (174)
- Cardiovascular Medicine (2502)
- Dentistry and Oral Medicine (305)
- Dermatology (210)
- Emergency Medicine (385)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (882)
- Epidemiology (11977)
- Forensic Medicine (10)
- Gastroenterology (718)
- Genetic and Genomic Medicine (3900)
- Geriatric Medicine (362)
- Health Economics (653)
- Health Informatics (2515)
- Health Policy (973)
- Health Systems and Quality Improvement (934)
- Hematology (350)
- HIV/AIDS (813)
- Infectious Diseases (except HIV/AIDS) (13482)
- Intensive Care and Critical Care Medicine (778)
- Medical Education (386)
- Medical Ethics (106)
- Nephrology (416)
- Neurology (3656)
- Nursing (205)
- Nutrition (544)
- Obstetrics and Gynecology (708)
- Occupational and Environmental Health (681)
- Oncology (1901)
- Ophthalmology (554)
- Orthopedics (230)
- Otolaryngology (299)
- Pain Medicine (243)
- Palliative Medicine (71)
- Pathology (461)
- Pediatrics (1071)
- Pharmacology and Therapeutics (443)
- Primary Care Research (434)
- Psychiatry and Clinical Psychology (3290)
- Public and Global Health (6327)
- Radiology and Imaging (1340)
- Rehabilitation Medicine and Physical Therapy (779)
- Respiratory Medicine (845)
- Rheumatology (389)
- Sexual and Reproductive Health (384)
- Sports Medicine (334)
- Surgery (426)
- Toxicology (51)
- Transplantation (179)
- Urology (155)

Genetic testing cannot reveal the gender of your baby − two genetic counselors explain the complexities of sex and gender
Assistant Professor of Medicine, Boston University
Assistant Professor, Boston University
Disclosure statement
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Boston University provides funding as a founding partner of The Conversation US.
View all partners
Gender reveal parties are best known as celebrations involving pink and blue, cake and confetti, and the occasional wildfire . Along with being social media hits, gender reveals are a testament to how society is squeezing children into one of two predetermined gender boxes before they are even born.
These parties are often based on the 18- to 20-week ultrasound, otherwise known as the anatomy scan . This is the point during fetal development when the genitals are typically observed and the word “boy” or “girl” can be secretly written on a piece of paper and placed into an envelope for the planned reveal.
Now there is a new player in the gender reveal game: genetic screening.
Advancements in genetic research have led to the development of a simple blood test called cell-free DNA prenatal screening that screens for whether a baby has extra or missing pieces of genetic information – chromosomes – as early as 10 weeks into pregnancy. Included in this test are the sex chromosomes, otherwise known as X and Y, that play a role in the development and function of the body.
This blood test is more informally called noninvasive prenatal testing, or NIPT. Many people refer to it as “the gender test.” But this blood test cannot determine gender.
As genetic counselors and clinical researchers working to improve genetic services for gender-diverse and intersex people, we emphasize the significance of using precise and accurate language when discussing genetic testing. This is critical for providing affirming counseling to any patient seeking pregnancy-related genetic testing and resisting the erasure of transgender and intersex people in health care.
Distinguishing sex and sex chromosomes
Sex and gender are often used interchangeably, but they represent entirely different concepts.
Typically when people think of sex, they think of the categories female or male. Most commonly, sex is assigned by health care providers at birth based on the genitals they observe on the newborn. Sex may also be assigned based on the X and Y chromosomes found on a genetic test. Commonly, people with XX chromosomes are assigned female at birth, and people with XY chromosomes are assigned male. Since cell-free DNA, or cfDNA, prenatal screening can report on sex chromosomes months before birth, babies are receiving sex assignments much sooner than previously possible.
While cfDNA prenatal screening can offer insights into what sex chromosomes an infant may have, sex determination is much more complicated than just X’s and Y’s.
For one, sex chromosomes don’t exactly determine someone’s sex . Other chromosomes, hormone receptors, neural pathways, reproductive organs and environmental factors contribute to sex determination as well, not unlike an orchestra with its ensemble of instruments. Each cello, flute, tympani and violin plays a crucial role in the performance of the final musical score. There is no single instrument that defines the entirety of the symphony.
Intersex people , or those with variations in sex characteristics that deviate from societal norms of binary sex, exemplify the complexities of sex. These variations can manifest in various ways beyond X and Y chromosomes, such as differences in hormone levels, genitalia or secondary sexual characteristics.
The oversimplification of sex based on societal norms has led many to believe that there are only two discrete sexes. The binary framework of sex excludes intersex people and perpetuates their erasure and mistreatment within both health care and society at large.
For instance, many intersex individuals face unnecessary surgeries , such as nonconsensual genital procedures, to conform to binary norms, violating their bodily autonomy .
Where gender comes in
While sex typically describes someone’s anatomical characteristics, gender is an umbrella term that encompasses the way someone views and presents themselves to the world. Countless aspects influence how someone defines their own gender and how the world views their gender, including clothing, haircuts and voice tone. Similar to how Western cultures have historically confined sex to two buckets, it has also created two gender categories: man and woman.
Gender is not dependent on anatomical parts or chromosomes . People are not math equations, and having certain combinations of biological parts does not equal someone’s gender. For example, some people may be transgender, meaning their assigned sex is not congruent with their socially or self-defined gender. Nonbinary people do not identify exclusively with either of the two genders in the binary, regardless of their assigned sex.
Just like sex diversity, gender diversity is not rare. A 2022 Pew Research Center analysis found that approximately 5% of adults in the U.S. under the age of 30 are transgender or nonbinary.
These estimates will likely increase as societal awareness and acceptance of gender-diverse individuals increases. Anti-transgender legislation often oversimplifies gender as strictly binary, conflating it solely with sex assigned at birth.
Intersex and gender-diverse people show that sex and gender are both multidimensional . Gender is not solely determined by biology, and it is erroneous to define someone’s gender by their sex, much less by their sex chromosomes.
Challenging sex and gender norms
The idea that biology plays the largest role in determining who an individual is, or bioessentialism , has governed misconceptions about sex and gender for many years. This concept is used to confine people to buckets and limit their self-determination .
For instance, societal norms dictate that women should be nurturing and gentle, while men are expected to be protective and assertive. Such rigid gender roles, often enforced through the lens of biology, serve to uphold notions of evolutionary destiny and a purported natural order.

Marketing strategies for children’s toys often adhere strictly to gender roles, steering girls toward dolls and domestic play sets while steering boys toward action figures and construction sets.
Educational systems often reinforce gender norms by directing girls toward subjects such as literature and arts while steering boys toward science and mathematics. This perpetuates the notion that certain traits and interests are inherently linked to one’s sex and gender, thereby reinforcing societal norms and sustaining inequality.
Upholding binary constructs of sex and gender does not allow for individuality and gender fluidity. Categorizing people from the time their chromosomes are analyzed or the moment their genitals are observed at birth restricts their autonomy and authenticity. These simple assumptions set expectations that can be harmful.
Letting children define themselves
If you’re a parent offered cfDNA prenatal screening during pregnancy, remember that it is commenting only on one instrument in the orchestra of sex. It cannot examine all of the other factors that determine sex as a whole. And it most certainly cannot determine gender, which is an entirely different concert.
In recent years, Jenna Karvunidis , the mother considered the inventor of gender reveal parties, shared her regrets for starting the trend and noted that her views on sex and gender have shifted. In a 2019 Facebook post, Karvunidis wrote, “PLOT TWIST. The world’s first gender reveal party baby is a girl who wears suits!” She had also gone on to say , “Celebrate the baby … Let’s just have a cake.”
When the envelope is opened, the balloons are popped and the crafty cake is cut, consider how these practices perpetuate social confinements and a gendered destiny for your little bundle of joy. Perhaps opt simply for a celebration that leaves space for your child to one day define who they are.
- Transgender
- Genetic testing
- Gender diversity
- Gender identity
- Gender roles
- Gender norms
- Sex chromosomes
- Biological sex

Sydney Horizon Educators – Faculty of Engineering (Targeted)

Dean, Faculty of Education

Lecturer in Indigenous Health (Identified)

Social Media Producer

PhD Scholarship
- Open access
- Published: 03 July 2024
Application of the radial artery after angiography in patients undergoing total arterial coronary revascularization
- Zanxin Wang 1 ,
- Haibing Liu 1 ,
- Zhifu Huan 1 ,
- Chao Su 1 ,
- Yao Chen 1 &
- Minxin Wei 1
Journal of Cardiothoracic Surgery volume 19 , Article number: 417 ( 2024 ) Cite this article
37 Accesses
Metrics details
There is growing evidence supporting the utilization of the radial artery as a secondary arterial graft in coronary artery bypass grafting (CABG) surgery. However, debates continue over the recovery period of the radial artery following angiography. This study aims to evaluate the clinical outcomes and experiences related to the use of the radial artery post-angiography in total arterial coronary revascularization.
A retrospective analysis was performed on data from patients who underwent total arterial CABG surgery at the University of Hong Kong Shenzhen Hospital from July 1, 2020, to September 30, 2022. Preoperative assessments included ultrasound evaluations of radial artery blood flow, diameter, intimal integrity, and the Allen test. Additionally, pathological examinations of the distal radial artery and coronary artery CT angiography were conducted, along with postoperative follow-up to assess the safety and efficacy of using the radial artery in patients undergoing total arterial CABG.
A total of 117 patients, compromising 102 males and 15 females with an average age of 60.0 ± 10.0 years, underwent total arterial CABG. The internal mammary artery was used in situ in 108 cases, while in 4 cases, it was grafted to the ascending aorta due to length limitations. Bilateral radial arteries were utilized in 88 patients, and bilateral internal mammary arteries in 4 patients. Anastomoses of the proximal radial arteries to the proximal ascending aorta included 42 cases using distal T-anastomosis and 4 using sequential grafts. The interval between bypass surgery and coronary angiography ranged from 7 to 14 days. Pathological examination revealed intact intima and continuous elastic membranes with no significant inflammatory infiltration or hyperplastic lumen stenosis in the radial arteries. There were no hospital deaths, 3 cases of perioperative cerebral infarction, 1 secondary thoracotomy for hemorrhage control, 21 instances of intra-aortic balloon pump (IABP) assistance, and 2 cases of poor wound healing that improved following debridement. CT angiography performed 2 weeks post-surgery showed no internal mammary artery occlusions, but 4 radial artery occlusions were noted.
Ultrasound may be used within 2 weeks post-angiography to assess the recovery of the radial artery in some patients. Radial arteries with intact intima may be considered in conjunction with the internal mammary artery for total arterial coronary CABG. However, long-term outcomes of these grafts require further validation through larger prospective studies.
Peer Review reports
After CABG surgery, numerous studies have confirmed the long-term patency advantage of arterial grafts [ 1 , 2 , 3 ]. The radial artery, initially proposed by Carpentier as a graft candidate for CABG surgery, offers advantages such as easy clinical evaluation and harvest, a larger diameter, and quicker wound recovery compared to veins from the lower limbs [ 4 ]. However, it was temporarily abandoned due to the risk of spasm [ 5 ]. With the introduction of antispasmodic drugs and advancements in surgical techniques, an increasing number of studies have shown that total arterial coronary artery bypass grafting surgery leads to a better long-term survival rate and a lower incidence of cardiovascular events [ 6 , 7 ]. Thus, the radial artery remains a preferred choice as the second graft in arterial bypass grafting.
Currently, the left radial artery approach for coronary angiography has become a standard procedure, with most studies reporting a four-week recovery period for the distal intima of the artery following puncture [ 8 , 9 ]. However, at our center, complete recovery of the radial artery’s intima, as assessed by ultrasound, has been observed within 7–14 days after angiography. Consequently, this study aims to analyze the timing, safety, and reliability of utilizing the radial artery in total artery bypass grafting surgery.
Materials and methods
General information.
A retrospective analysis was conducted on data from patients who underwent total arterial coronary artery bypass grafting surgery at the University of Hong Kong Shenzhen Hospital between July 1, 2020, and September 30, 2022. The inclusion criteria were patients who utilized the radial and internal mammary arteries for the surgery. The exclusion criteria were: (1) patients with venous grafts and (2) those who underwent secondary surgery. Patient demographics, graft vessels, target vessels, and follow-up results were recorded.
Radial artery evaluation
For patients who underwent coronary angiography via the right radial artery, detailed evaluations of intimal smoothness and thromboembolism at the distal end was performed. There is a specialized ultrasound physician who evaluates all radial artery intima and completes the Allen’s test to ensure consistency in the study.
The ultrasound Doppler was enhanced by introducing additional measurement indices to provide a more accurate evaluation of the radial artery, especially after use of the right radial artery for angiography. (1) Evaluation of radial artery diameter: measurements were taken at the radial styloid process, 2 cm below the elbow fossa, and the midsection of the radial artery to accurately assess vessel thickness and determine suitability for use as a bypass graft. (2) Ultrasonic ALLEN test: Traditional ALLEN tests can be influenced by some factors including the completeness of radial artery compression, skin color, and lighting conditions, potentially leading to inaccuracies. Ultrasound can eliminate these variables. A 30% increase in ulnar artery blood flow was considered indicative of adequate collateral circulation in the palm. (3) Evaluation of intima: In addition to diameter, evaluating the intima of the artery is crucial.
If a thrombus was detected, ultrasound determined the suitable length for bypass and marked it on the body surface.
The radial artery was harvested using the “NO-TOUCH” technique via an open incision to minimize damage [ 10 ] and stored in a solution of papaverine and heparin saline. After thoracotomy, the artery was placed in the pericardium for heat preservation.
The scar or thrombus at the distal end of the radial artery was removed, and a smooth and intact part of the intima was taken as a graft vessel. The sample was taken from the normal vascular part to confirm the integrity of the intima at the anastomotic site.
All samples were fixed in 4% paraformaldehyde overnight, then embedded in paraffin, and sliced into 3 μm sections. After routine dewaxing and dehydration, standard hematoxylin and eosin (HE) staining was performed, including 10 min of hematoxylin staining, decolorization with 1% dilute hydrochloric acid for 5 s, treatment with 0.01 mmol/L PBS (pH 7.2–7.4) for 5 min, and flushing with tap water for 2 min after each step. The eosin solution was applied for 30 s to 1 min, followed by dehydration with 70-100% gradient alcohol for 1–2 min, xylene clarification, and sealing with neutral gum. The vascular structure and intimal integrity of the radial artery were assessed under an optical microscope using a double-blind method.
Surgical strategy
Based on preoperative cardiac function, 99 patients underwent off-pump CABG (OPCAB), 9 patients received bypass surgery on a beating heart assisted by cardiopulmonary bypass, and 15 patients underwent on-pump surgery for mitral valve or ventricular aneurysm or other intracardiac operations. The anastomosis sequence began with the radial artery anastomosed to the ascending aorta using 7 − 0 prolene. After confirming unobstructed blood flow, the distal end of the radial artery was clamped to pre-adapt it to aortic pressure. Then, the anastomosis from the internal mammary artery to the left anterior descending branch, and the anastomosis of the distal radial artery were completed, allowing the radial artery sufficient time to regain natural tension. The typical size of an anastomosis was approximately 6 mm.
Statistical analysis
Data were analyzed using SPSS 26.0 software. Measurement data following a normal distribution were expressed as mean x ± s , while data with a non-normal distribution were presented as median (interquartile range) [M (Q1, Q3)]. Comparisons between groups were conducted using the Mann-Whitney U test. Categorical data are reported as counts and percentages. All tests were two-tailed, and P < 0.05 was considered statistically significant.
This study was approved by the Medical Ethics Committee of the University of Hong Kong Shenzhen Hospital, under project number HKUSZH2022021.
Patient characteristics
A total of 117 patients underwent total arterial coronary artery bypass grafting surgery, comprising 102 males and 15 females, with an average age of (60.0 ± 10.0) years. Patients received an average of (3.1 ± 0.6) bypass grafts each. The average operation time and postoperative ventilator time were (6.5 ± 1.2) hours and (7.7 ± 3.6) hours, respectively. During the perioperative period, 21 patients required IABP assistance. The clinical data are presented in Table 1 .
Grafts and target vessel selection
The left internal mammary artery was used in situ in 108 cases, while in 4 cases, it was redirected to the ascending aorta due to length limitations. Bilateral radial arteries were utilized in 88 patients, and bilateral internal mammary arteries in 4 patients. The target vessels for the left internal mammary artery were primarily the left anterior descending branch, while the radial artery targeted the obtuse marginal, diagonal, intermediate, posterior descending, left ventricular posterior branches, or right coronal trunk. All proximal radial arteries were anastomosed to the aorta. A distal T-graft was created in 42 cases, and a sequential graft in 4 cases. Details of the bypass grafting and target vessels are shown in Table 2 .
The radial artery had an average length of approximately 15 cm and was anastomosed to the appropriate target vessel based on its length (Fig. 1 A). In this cohort, 2 patients had a thrombus at the distal end of the right radial artery. After removal of the thrombus, the remaining vessel intima was intact and suitable for use in the bypass graft (Fig. 1 B). Before surgery, these patients underwent ultrasound examinations to assess the radial artery lumen diameter and intima smoothness, and the results were marked on the body surface. The vessels were harvested only when the required length was available. If the length of the graft vessel was insufficient during surgery, the accompanying veins of the radial artery could be excised and appropriately extended.
The mean flow rates of the main bypass grafting vessels measured during surgery were (36.0 ± 24.8) ml/min in the left anterior descending branch, (30.0 ± 21.0) ml/min in the obtuse marginal branch, (25.8 ± 16.3) ml/min in the posterior descending branch, and (29.3 ± 17.80 ml/min in the diagonal branch (Fig. 2 ).
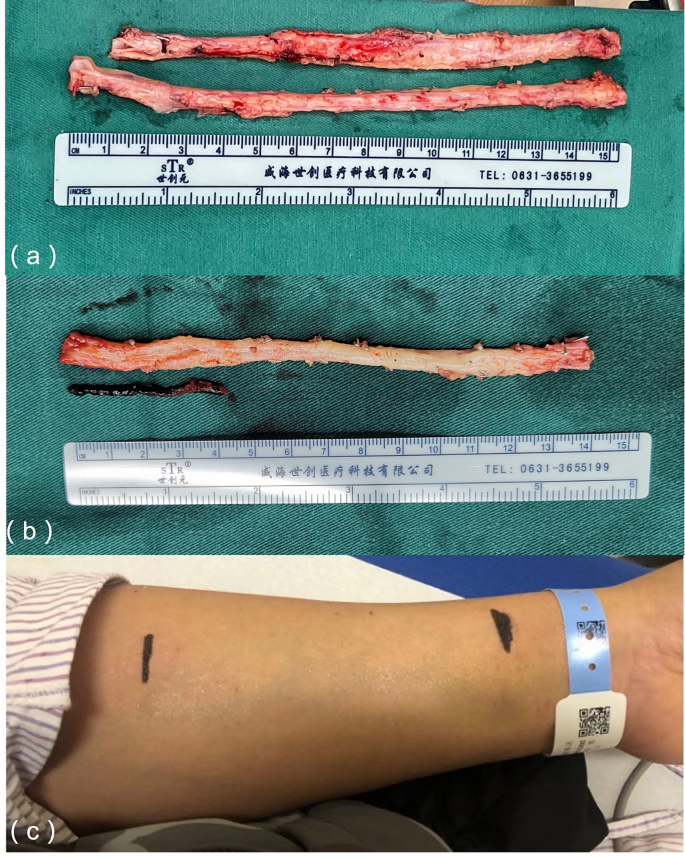
( a ) The radial artery was harvested using the “NO-TOUCH” technique, and the target blood vessel was selected based on the measured length; ( B ) The intima of the remaining bypass grafting vessel remained intact after the distal thrombus was removed and flushed from the distal end of the radial artery; ( C ) Preoperative evaluation of the radial artery intima and lumen diameter was conducted via ultrasound and marked on the body surface

Measurement of flow in the main target vessels post-operation, with systolic blood pressure between 120-130mmHg and diastolic blood pressure 60-70mmHg during measurement
Pathological examination
For patients who used the radial artery as a bypass graft, the bio-bank in our hospital preserves all distal tissue samples of the radial artery, which can be used for pathological examination. Radial artery samples were selected at 1 week and 2 weeks after angiography for pathological examination. The purpose is to confirm that the radial artery intima evaluated by ultrasound is smooth and can be used as a bridging vessel.
The HE is staining showed that the radial arteries exhibited intact intima, a continuous elastic membrane, no significant infiltration of inflammatory cells or matrix-like components, and no lumen stenosis due to hyperplasia (Fig. 3 ). These findings were consistent with those from ultrasound evaluations.

HE indicated that the radial arteries maintained intact intima, continuous elastic membranes, no significant infiltration of inflammatory cells and matrix-like components, and no lumen stenosis caused by hyperplasia one and two weeks after angiography
There were no in-hospital deaths after the surgery. During the perioperative period, 3 patients experienced cerebral infarctions but were discharged after receiving rehabilitation treatment. Two patients required a second thoracotomy to address bleeding, and 1 patient experienced delayed wound healing, which improved significantly after debridement. Two weeks post-operation, coronary CTA was performed to reexamine blood flow. No occlusions were observed in the internal mammary arteries, but 4 cases exhibited radial artery occlusion. Among these, 3 target vessels were the posterior descending branches (2 with 70% stenosis and 1 with 100% stenosis), and the remaining target vessel was the obtuse marginal branch (with 60% stenosis), forming a T-shaped graft with the diagonal branch at 90% stenosis. The patients exhibited no symptoms of angina pectoris and received no specific treatment. Follow-up ranged from 2 to 25 months post-discharge, with no deaths or new cardiovascular or cerebrovascular events reported. Throughout the follow-up period, the survival rate without major cardiovascular and cerebrovascular events (cardiovascular death, myocardial infarction, and stroke) remained at 100%.
Recent studies have shown that the radial artery has higher patency rates than the great saphenous vein during early and middle follow-up periods [ 11 , 12 ]. Many patients with coronary heart disease complicated with diabetes. It has been confirmed that the use of bilateral internal mammary arteries will increase the risk of poor sternal healing and infection. At the same time, the radial artery, as a graft, has a higher long-term patency rate than the great saphenous vein, faster wound healing in both upper limbs, and fewer complications.
However, it has been reported that endothelial damage at the puncture site of the radial artery after coronary angiography can take over 4 weeks to recover [ 13 ]. With the improvement of puncture techneque and gentle operation, the postoperative recovery of the radial artery intima is faster. Moreover, new techneques icluding the use of thinner sheaths, sheaths less likely to cause vascular damage, or innovative techniques in guidewire insertion, are helpful to accelerate its recover. Furthermore, it was reported that distal artery puncture was safe. And distal radial access prevents radial artery occlusion [ 14 ].
In this study, a certain part of patients displayed a smooth and fully recovered intima within 7–14 days post-angiography, as confirmed by pathology and ultrasound evaluations. The preoperative assessment of the radial artery was also refined. In addition to the clinical ALLEN test, the ultrasound Doppler examination was enhanced by introducing additional measurement indices to provide a more accurate evaluation of the radial artery, especially after use of the right radial artery for angiography. (1) Evaluation of radial artery diameter: measurements were taken at the radial styloid process, 2 cm below the elbow fossa, and the midsection of the radial artery to accurately assess vessel thickness and determine suitability for use as a bypass graft. (2) Ultrasonic ALLEN test: Traditional clinical ALLEN tests can be influenced by factors such as the completeness of radial artery compression, skin color, and lighting conditions, potentially leading to inaccuracies [ 14 ]. In this study, ultrasound was employed to perform the ALLEN test on all patients, eliminating these variables. A 30% increase in ulnar artery blood flow was considered indicative of adequate collateral circulation in the palm. (3) Evaluation of blood vessel intima: In addition to diameter, evaluating the intima of the artery is crucial. As age increases, plaques or stenosis may develop in limb blood vessels. Ultrasound is useful for identifying calcified plaques and severe stenosis in the radial artery, thus helping to avoid potential impacts on long-term patency rates. (4) Evaluation of the radial artery after angiography: Most patients scheduled for coronary artery bypass grafting underwent the procedure within 1–2 weeks after angiography. The intima appeared intact in Doppler ultrasound examinations of patients with successful puncture. Due to puncture and other factors, some patients showed thromboembolism or irregular intima at the distal end on ultrasound, while a few exhibited recanalization of the radial artery with an intact intima when awaiting surgery. For patients with distal embolism, ultrasound was able to determine the length of unobstructed radial artery and confirm its suitability as a graft if the length was sufficient. Pathological sections and HE staining corroborated these findings, showing intact intima, continuous elastic membranes, and the absence of significant inflammatory cell infiltration, matrix-like components, or hyperplasia-induced lumen stenosis in both left and right radial arteries. These results confirm that ultrasound is an effective method for preoperative evaluation of the radial artery intima, providing substantial evidence for its clinical use.
Spasm remains a primary concern regarding the use of the radial artery as a graft [ 15 , 16 ]. Various strategies, including the “NO-TOUCH” technique, have been employed to prevent perioperative spasm. This technique involves gentle handling, avoiding excessive traction, and selecting highly narrow target blood vessels to increase patency rates [ 17 , 18 ]. In this study, the application of the radial artery in bypass grafting procedures achieved satisfactory short-term results by optimizing preoperative evaluations and the grafting process. These findings provide initial evidence supporting the safety, reliability, and potential future use of radial artery bypass grafting in clinical practice. The surgical procedure was refined to optimize the bypass sequence: Firstly, the radial artery was anastomosed to the ascending aorta, ensuring unobstructed blood flow. The residual thrombus in the radial artery could be expelled by the blood flow of the ascending aorta. Subsequently, the distal radial artery was clamped to prevent bleeding and to allow the artery to adapt to the ascending aortic pressure. Previous studies have shown that the radial artery has a thick wall and abundant vascular smooth muscle cells, which may contribute to its susceptibility to spasm [ 19 , 20 ]. We hypothesize that after anastomosis to the ascending aorta, the radial artery can withstand pressure for a certain period, effectively reducing or avoiding spasm.
Maintaining effective perfusion pressure is another crucial factor in avoiding vessel spasm. In our study, patients with perioperative systolic blood pressure maintained above 120mmHg and average pressure above 70mmHg experienced no perioperative vasospasm or major cardiovascular events. Furthermore, our facility regularly provided norepinephrine and epinephrine for post-operative blood pressure management, although calcium antagonists like diltiazem were not specifically utilized. These findings demonstrate that adapting to ascending aortic pressure after completing proximal radial artery anastomosis, pre-expanding the vessel, and maintaining effective perfusion pressure are important measures for preventing or reducing perioperative spasm. It is worth noting that a relatively high proportion of patients in our study required intra-aortic balloon pump (IABP) assistance. Since the off-pump technique was employed for CABG to facilitate the procedure, patients with a left ventricular ejection fraction (EF) value of ≤ 40% before the operation received IABP assistance to maintain perioperative hemodynamic stability, ensure coronary perfusion pressure, and prevent radial artery spasm.
It is important to recognize that this study has many constraints. Firstly, the sample size was relatively small, which may limit the generalizability of the findings. Secondly, there was an absence of extended follow-up data, and no postoperative coronary angiography was conducted. Although a coronary computed tomography angiography (CTA) was conducted two weeks after the operation, revealing four undeveloped radial arteries, it is important to consider that the contrast agent may not have passed through the radial artery due to potential competitive blood flow. Subsequent examination is necessary in future studies to tackle these constraints.
Based on the initial findings of this study, it has been observed that radial artery can regain its structural integrity within a period of 7–14 days following coronary angiography in certain patients. An optimal ultrasonic examination technique can be used to adequately evaluate this restoration process. However, the survival rates and the patency rates of the grafts in the postoperative phase need to be verified through more extensive prospective investigations.
Data availability
No datasets were generated or analysed during the current study.
Gaudino M, Benedetto U, Fremes SE et al. Angiographic outcome of coronary artery bypass grafts: the Radial Artery Database International Alliance[J]. Ann Thorac Surg 2020;109(3):688–94.
Qiao E, Wang Y, Yu J, et al. Short-term assessment of radial artery grafts with multidetector computed tomography[J]. J Cardiothorac Surg. 2021;16(1):93.
Article PubMed PubMed Central Google Scholar
Tatoulis J, Buxton BF, Fuller JA. The right internal thoracic artery: is it underutilized?[J]. Curr Opin Cardiol. 2011;26(6):528–35.
Article PubMed Google Scholar
Carpentier A, Guermonprez JL, Deloche A et al. The aorta-to-coronary radial artery bypass graft. A technique avoiding pathological changes in grafts[J]. Ann Thorac Surg 1973;16(2):111–21.
Khan MZ, Patel K, Franklin S, Faruqi A, Ahmad W, Saeed J. Radial artery spasm: reviews and updates. Ir J Med Sci. 2020;189(4):1253–8.
Urso S, Sadaba R, Gonzalez JM et al. Total arterial revascularization strategies: a meta-analysis of propensity score-matched observational studies[J]. J Card Surg 2019;34(9):837–45.
Rayol SC, Van den Eynde J, Cavalcanti L, et al. Total arterial coronary bypass graft surgery is Associated with Better Long-Term Survival in patients with Multivessel Coronary Artery Disease: a systematic review with Meta-Analysis[J]. Braz J Cardiovasc Surg. 2021;36(1):78–85.
Gaudino M, Tondi P, Benedetto U et al. Radial artery as a coronary artery bypass conduit: 20-Year Results[J]. J Am Coll Cardiol 2016;68(6):603–10.
Ognerubov DV, Sedaghat A, Provatorov SI, Tereshchenko AS, Bertrand OF, Bernat I, Arutyunyan GK, Pogorelova OA, Tripoten MI, Balakhonova TV, Samko AN, Merkulov EV. A randomized trial comparing short versus prolonged hemostasis with rescue recanalization by Ipsilateral Ulnar Artery Compression: impact on radial artery occlusion-the RESCUE-RAO trial. J Interv Cardiol. 2020;2020:7928961.
Zhao Y, Zhang X, Song Y, Xia Y, Huang D, Zhang J, Liu D, Zhang D. A retrospective study of the No-Contact technique to obtain radial arteries for coronary artery bypass grafting. Heart Surg Forum. 2023;26(4):E358–62.
Gaudino M, Benedetto U, Fremes S et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass Surgery[J]. N Engl J Med 2018;378(22):2069–77.
Royse A, Pamment W, Pawanis Z, Clarke-Errey S, Eccleston D, Ajani A, Wilson W, Canty D, Royse C. Patency of conduits in patients who received internal mammary artery, radial artery and saphenous vein grafts. BMC Cardiovasc Disord. 2020;20(1):148.
Gaudino M, Benedetto U, Fremes S, Ballman K, Biondi-Zoccai G, Sedrakyan A, Nasso G, Raman J, Buxton B, Hayward PA, Moat N, Collins P, Webb C, Peric M, Petrovic I, Yoo KJ, Hameed I, Di Franco A, Moscarelli M, Speziale G, Puskas JD, Girardi LN, Hare DL, Taggart DP. RADIAL investigators. Association of Radial Artery Graft vs Saphenous Vein Graft with Long-Term Cardiovascular outcomes among patients undergoing coronary artery bypass grafting: a systematic review and Meta-analysis. JAMA. 2020;324(2):179–87.
Eid-Lidt G, Rivera RodríguezA, Jimenez Castellanos J, Farjat Pasos JI, Estrada López KE, Gaspar J. Distal Radial Artery Approach to prevent radial artery occlusion trial. JACC Cardiovasc Interv. 2021;14(4):378–85.
Chardigny C, Jebara VA, Acar C, Descombes JJ, Verbeuren TJ, Carpentier A, Fabiani JN. Vasoreactivity of the radial artery. Comparison with the internal mammary and gastroepiploic arteries with implications for coronary artery surgery. Circulation. 1993;88(5 Pt 2):II115–27.
CAS PubMed Google Scholar
Tu L, Jin Y, Li S, Yu Q, Lu Y. Distal transradial access decreases radial artery occlusion rate in percutaneous coronary interventions. Am J Transl Res. 2023;15(4):2802–10.
PubMed PubMed Central Google Scholar
He GW, Taggart DP. Antispastic Management in arterial grafts in coronary artery bypass grafting Surgery[J]. Ann Thorac Surg 2016;102(2):659–68.
Gaudino M, Crea F, Cammertoni F et al. Technical issues in the use of the radial artery as a coronary artery bypass conduit[J]. Ann Thorac Surg 2014;98(6):2247–54.
Sousa-Uva M, Gaudino M, Schwann T, et al. Radial artery as a conduit for coronary artery bypass grafting: a state-of-the-art primer[J]. Eur J Cardiothorac Surg. 2018;54(6):971–6.
Loh SH, Chang CY, Huang SF, Chao SC, Lin WK, Huang EY, Tsai CS, Tsai YT. Functional effects of urotensin-II on intracellular pH regulators in human radial artery smooth muscle cells. Peptides. 2020;126:170236.
Article CAS PubMed Google Scholar
Download references
This work was supported by the grants from the National Natural Science Foundation of China (82270280 to Z.W.); the Science and Technology project of Shenzhen of China (JCYJ20220530142200001, JCYJ20230807113016034 to Z.W.); the Sanming Project of Medicine in Shenzhen “Cardiovascular Surgery team of Professor Wang Chunsheng from Zhongshan Hospital Fudan University (SZSM202211005).
Author information
Authors and affiliations.
Department of Cardiac Surgery, The University of Hong Kong-Shenzhen Hospital, Guangdong, P.R. China
Zanxin Wang, Haibing Liu, Zhifu Huan, Chao Su, Yao Chen & Minxin Wei
You can also search for this author in PubMed Google Scholar
Contributions
Zanxin Wang was involved in conceptualization, data analysis, investigation, methodology and wrote the first draft of the manuscript. Haibing Liu and Zhifu Huan collated data and were responsible for investigating the data. Chao Su and Yao Chen were involved in data analysis and visualization. Minxin Wei validated the data and supervised the study.
Corresponding author
Correspondence to Minxin Wei .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval and consent to participate
This study complied with the principles of the Declaration of Helsinki and was approved by the ethics committee of The University of Hong Kong-Shenzhen Hospital (hkuszh2022021).
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wang, Z., Liu, H., Huan, Z. et al. Application of the radial artery after angiography in patients undergoing total arterial coronary revascularization. J Cardiothorac Surg 19 , 417 (2024). https://doi.org/10.1186/s13019-024-02893-7
Download citation
Received : 09 March 2024
Accepted : 15 June 2024
Published : 03 July 2024
DOI : https://doi.org/10.1186/s13019-024-02893-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Coronary artery bypass grafting surgery
- Radial artery
- Ultrasound test
Journal of Cardiothoracic Surgery
ISSN: 1749-8090
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
7715 Cases 59529 Ultrasound Images & Clips. Browse our free ultrasound library offered to you by SonoSkills and FUJIFILM Healthcare Europe. Make sure to sign-up for our newsletter to receive the latest cases and news in your inbox!
LITFL 100+ Ultrasound quiz. Clinical cases and self assessment problems from the Ultrasound library to enhance interpretation skills through Ultrasound problems. Preparation for examinations. Each case presents a clinical scenario; a series of questions; clinical images and finally some pearls to highlight the key learning points.
Cadaveric studies suggest that most genicular nerves are easily identifiable landmarks that may be used for therapeutic purposes. 5 Genicular nerve blocks (GNB) are traditionally used in this setting of chronic osteoarthritis knee pain via radiofrequency ablation or perioperative knee pain via ultrasound ( 1-4, 9).
Cases. By sharing our collective experience through interesting and classic patient cases, we can make a real difference in how people are imaged and diagnosed. Each case belongs to a contributing member and all cases are reviewed by our dedicated editors to ensure they reach quality standards and abide by privacy guidelines. Cases can public ...
Diagnostic ultrasound was requested to evaluate the median nerve. Case 117: 60-year-old female with pain beneath the 2nd and 3rd toes. Case 116: 18-year-old male with hand pain and weakness in the distribution of the median nerve. Case 115: 22-year-old male with snapping sensation over the medial side of the elbow.
The patient underwent imaging studies in accordance with the American College of Radiology guidelines. 1 Both breasts were imaged, ... An ultrasound image (Panel D) shows a solid, irregular mass ...
5. An unexpected association between diseases or symptoms. 6. An unexpected event in the course of observing or treating a patient. 7. Findings that shed new light on the possible pathogenesis of a disease or an adverse effect. Case reports should include an up-to-date review of all previous cases in the field.
Correction: Feasibility of using a handheld ultrasound device to detect and characterize shunt and deep vein thrombosis in patients with COVID-19: an observational study. Rajkumar Rajendram, Arif Hussain, Naveed Mahmood and Mubashar Kharal. The Ultrasound Journal 2023 15 :44. Correction Published on: 23 November 2023.
CASE, a global, open access online journal, welcomes case reports where cardiovascular ultrasound is used to diagnose or help solve a clinical problem in humans or animals. Examples include cases where cardiovascular ultrasound was used as a critical component of a multimodality approach to disease diagnosis or evaluation or where it was used ...
Lung ultrasound cases. James Rippey. Aug 18, 2023. Home Ultrasound Library. Worked examples of clinical cases for specific pathological conditions and signs from the Ultrasound Lung Modules. Chronic Obstructive Pulmonary Disease (COPD) Empyema and Abscess. Hydropneumothorax. Lung Collapse.
Case report. A 9-year-old female underwent a laparoscopic right ovarian cystectomy for a benign mature teratoma. On post-operative day 4 she developed intermittent fevers (max 102.8°F) and transient abdominal and shoulder pain. She was seen in pediatric surgery clinic on post-operative day 4 and was found to have small-volume pneumoperitoneum ...
Join us in this interactive lecture as we present a total of 5 unknown cases followed by a diagnosis reveal and key teaching points after each case, all in a...
This is the largest ultrasound case library in the world with over 7.000 cases, over 100.000 ultrasound images and 2.500 clips. It was started in 2004 by Dr. Taco Geertsma and was supported in his effort by Fujifilm Healthcare Europe. VISIT: ULTRASOUNDCASES.INFO. The site is developed as a teaching file.
The Ultrasound Physics teaching is excellent. The content is appropriate and covers the core physics syllabus for all but the most advanced student groups. The majority of the presentations are just over 10 minutes in duration and are delivered by a recognised expert in ultrasound physics, Professor Neil Pugh.
Obstetric cases - common and uncommon cases. Case 1. Case 2. Case 3. Case 4. Case 5. Case 6. Case 7. University of Washington Department of Radiology.
Innovations in Ultrasound - Image and Case Study Library. For more than twenty years our staff at Mint Medical Education have been providing health care services across imaging modalities. With over twenty thousand case studies on file in ultrasound alone, and with more than fifteen hundred additional scans performed each month, we have a ...
5 Case 1 Biliary tract (B) History: a 34-year-old male patient, asymptomatic, with no significant pathology (no prior hospitalization and surgery), presented for a routine clinical and ultrasound evaluation. The clinical examination did not reveal any abnormalities. Laboratory tests - normal complete blood cound, normal levels of AST and ALT, normal
This online collection of ultrasound and echocardiography images is available for free, compliments of All About Ultrasound and iHeartEcho! Register for this free resource today! Please note that our case study and image gallery collection is ever growing and we are adding images frequently, so check back often.
Introduction We present a case of a 13-week abdominal pregnancy evaluated with ultrasound and magnetic resonance imaging. Case presentation A 34-year-old woman, (gravida 2, para 1) suffering from lower abdominal pain and slight vaginal bleeding was transferred to our hospital. A transabdominal ultrasound and magnetic resonance imaging were performed. The diagnosis of primary abdominal ...
Nov 3, 2020. Home Ultrasound Library. Worked examples of clinical cases for specific pathological conditions and signs from the Renal Ultrasound Modules. Distal VUJ Stone: Case 1 - Case 2 - Case 3 - Case 4 - Case 5. Bladder Stone: Case 1 - Case 2. Distal Ureteric Stone: Case 1 -.
820 Jorie Blvd., Suite 200 Oak Brook, IL 60523-2251 U.S. & Canada: 1-877-776-2636 Outside U.S. & Canada: 1-630-571-7873
Medical ultrasound: Case Study 278.5 KB. pdf. 0.27 MB. Download. pdf / 0.27 MB Download. Co-developed with the Australasian Society for Ultrasound in Medicine (ASUM), this case study focuses on the work of the Ultrasonics Institute (UI) and of pioneering Australian doctors and sonographers who revolutionised the use of medical imaging.
A 72 year old male with known abdominal aortic aneurysm (5.7 cm s/p fem-tib bypass, L AKA) presents for 3 weeks with diarrhea and mild LLQ pain. No nausea, vomiting, fever, back pain, urinary symptoms, or blood in stool. He has no localizing abdominal exam & no peritoneal signs, strong even radial pulses, and normal cardiopulmonary exam. On ...
Ultrasound imaging is extremely safe and does not use radiation. Ultrasound scanning gives a clear picture of soft tissues that do not show up well on x-ray images. Ultrasound is the preferred imaging modality for the diagnosis and monitoring of pregnant women and their unborn babies. Ultrasound provides real-time imaging.
By implementing an ultrasound-based inspection program using the SDT340 ultrasound data collector with a Flexible Sensor attachment, maintenance technicians can perform a wide range of inspections and checks on electrical systems, and equipment components utilizing airborne ultrasound.
We sought studies in adult patients undergoing THA, comparing QLB with a control group (no block, sham block or any other ultrasound guided regional nerve blocks). A total of 774 patients from 10 studies (7 randomized controlled, one controlled clinical and two retrospective study) were included in this meta-analysis.
Background: Thyroid tumor, as an endocrine tumor with increasing incidence, causes a heavy economic burden. Ultrasound scanning is widely used for screening or preliminary diagnosis of thyroid tumors, but its large number of false-positive results brings unnecessary mental pain, expensive examination costs, physical injury and other adverse consequences. There is an urgent need to find a ...
These parties are often based on the 18- to 20-week ultrasound, otherwise known as the anatomy scan. This is the point during fetal development when the genitals are typically observed and the ...
After CABG surgery, numerous studies have confirmed the long-term patency advantage of arterial grafts [1,2,3].The radial artery, initially proposed by Carpentier as a graft candidate for CABG surgery, offers advantages such as easy clinical evaluation and harvest, a larger diameter, and quicker wound recovery compared to veins from the lower limbs [].