- 2023 Lancet Countdown U.S. Launch Event
- 2023 Lancet Countdown U.S. Brief
- PAST BRIEFS

2020 CASE STUDY 3
Promoting food security, resilience and equity during climate-related disasters.
The U.S. is often viewed as a nation of abundance , yet paradoxically, one in ten households were “food insecure” in 2019, meaning that they struggle to get the proper nutrition to keep their family healthy. CS_77
These challenges are not borne equally. Rates of food insecurity were nearly three times higher for low-income and single mother-headed households and nearly twice as high for Black and Latino households than for White households.
Early research has found a doubling of the average food insecurity rate across the U.S. linked to the COVID-19 pandemic, with even greater increases among vulnerable populations. CS_78 , CS_79 , CS_80 , CS_81 Disruptive events, whether climate-related disasters or the COVID-19 pandemic, can exacerbate existing barriers to securing healthy food for vulnerable populations and further widen food and health disparities. CS_82
Food insecurity has clear health implications. Adults who are food-insecure may be at an increased risk of health problems, including obesity, heart disease, diabetes, depression, and increased susceptibility to COVID-19. CS_83 , CS_84 , CS_85 Food insecurity also puts children at a higher risk of asthma, anemia, and obesity, as well as behavioral, developmental, and emotional problems. CS_83 , CS_86
Climate-intensified extreme events are compounding existing food insecurity
Climate change is anticipated to worsen existing food insecurity as climate-related disasters, such as drought and flooding, become more frequent and severe and as agricultural pests become more persistent. CS_72 , CS_87 In 2019, there were fourteen climate-related disasters within the U.S. that each caused over a billion dollars in damages. CS_52
Historic floods in the Midwest destroyed millions of acres of agriculture and caused widespread infrastructure damage ( see the Case Study ). In addition, an above-normal Atlantic hurricane season inundated coastlines with unprecedented rainfall, high winds, and storm surge; and wildfires in California and Alaska caused widespread energy disruptions, compromising the health and well-being of residents. CS_52
The mechanisms of food system disruption
Disasters such as these threaten all aspects of food production, distribution, and accessibility, with subsequent impacts for affordability that can further exacerbate food insecurity for vulnerable populations. When food is not consumed where it is produced, it must be processed, stored, transported, and then sold or donated. These processes involve complex interdependent, and at times, international systems. Roads, bridges, warehouses, airports, energy grids, and other transportation or telecommunication infrastructure are at risk of direct damage from climate change, severely disrupting the food system as a whole. CS_88 , CS_89
For example, following the 2019 floods in the Central states, the flood waters caused more than forty state and federal highways to close, hydroelectric dams to be breached, and threatened nuclear power stations (see Case Study). CS_90 , CS_91 These disturbances limited the movement and storage of goods throughout the region and prevented consumers from accessing food sources. CS_91 , CS_92 In the midst of an extreme fire season in California that same year, utility providers turned off power to millions of homes and businesses, plunging low-income households into hunger and financial crisis as their food spoiled. CS_93
Recent climate disasters decreased food security
Climate disasters can lead to acute food insecurity in the short-term and exacerbate chronic food insecurity in the long-term (see Table 1). Populations already struggling from chronic insecurity, or those who are only marginally food secure, are particularly vulnerable to the socioeconomic impacts of disasters, such as loss of livelihood, rising food prices, forced migration, loss of social support, and health-related impacts. Data from the aftermath of 2019 disasters is still scarce, but the impacts from previous disasters that are similar in nature are well documented.
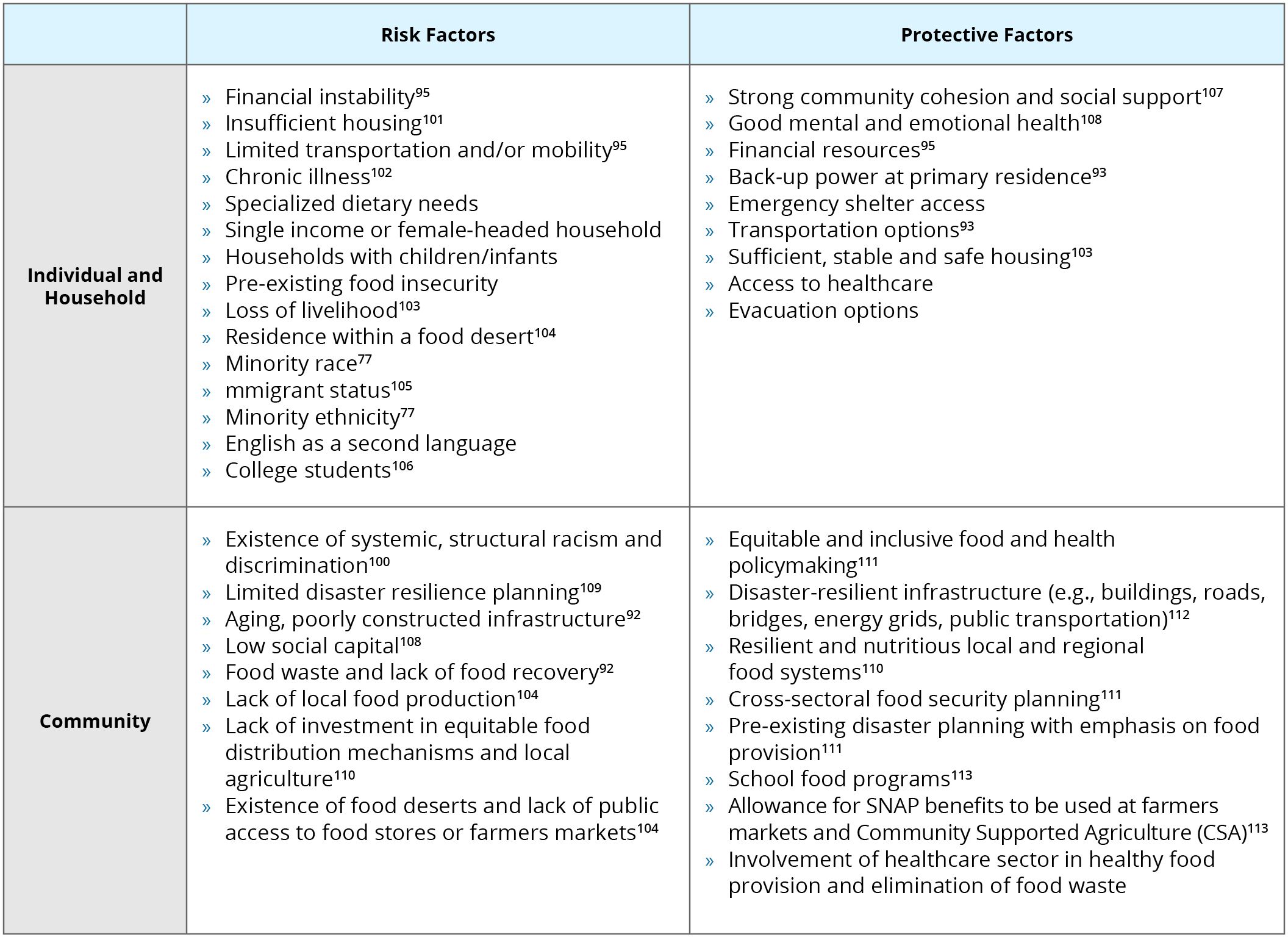
Individual, household and community level risk factors to food insecurity following climate-related disasters.
For example, nearly five years after Hurricane Katrina, many of the households heavily impacted by the hurricane in Louisiana and Mississippi remained food insecure. This was especially true for women, Black households, and those living with chronic illness, mental health issues, or low social support. CS_94 Similar impacts were demonstrated in New York City following Hurricane Sandy, where one-third of surveyed households in the heavily impacted Rockaway Peninsula reported difficulty obtaining food due to economic hardship, disruption of public transportation, and long-term closure of grocery stores months after the storm. CS_95
A path towards equitable food security
Learning from baltimore.
In the era of complex disasters, community-level resilience is essential, as federal relief is often too slow and under-equipped to meet the immediate needs of individuals and households. A growing number of U.S. cities are working to protect and improve food security in the aftermath of climate-related disasters and help build climate-resilient local and regional food systems.
For example, officials from Baltimore, Maryland worked with researchers at the Johns Hopkins University in 2017 to assess the resilience of the city’s food supply to climate-related disruptions and to identify ways to support communities at risk of experiencing food insecurity both before and after disasters. CS_96 This is a wonderful example of the power of academic and public partnerships.
Baltimore also designated a food liaison to sit within the Office of Emergency Management during crises. This city received funding from FEMA to coordinate a collaborative regional food and water resilience plan with surrounding jurisdictions. When COVID-19 spread to Baltimore in early 2020 — closing schools and many businesses — the city quickly put its food resilience planning into action and convened a group of food assistance stakeholders to better coordinate responses supporting food access for residents.
Adaptive actions for health and equity
Local and state governments across the country can take similar steps to incorporate food insecurity risk analysis and adaptive planning into emergency management and climate adaptation planning ( see Table 2 ). Local governments and community partners can ensure food assistance programs provide well-balanced meals and are targeted to reach vulnerable individuals and communities.
It is critical to support federal and state assistance programs during non-disaster times, such as the Supplemental Nutritional Assistance Program (SNAP), Women, Infants and Children (WIC), and school lunches. As an example, SNAP and WIC services have been pathways to try to meet the rise in food insecurity during the pandemic, and many schools have attempted to continue to provide meals to children most in need. CS_97 , CS_98 Thus, ongoing support can ensure that these programs are even more adaptable, optimally funded, and able to be rapidly mobilized during a disaster of any kind, thus reducing vulnerability and supporting food security in the short- and long-term.
Simultaneously, addressing food insecurity in the wake of disasters goes hand in hand with combating the root causes of food insecurity and health disparities, such as poverty and food deserts. CS_99 Structural racism is also deeply interconnected through complex pathways, including through the creation of disadvantaged social and economic factors that contribute to food insecurity. CS_100 Yet, even when these factors are removed, some evidence suggests food insecurity remains for people of color, highlighting the need for further research. CS_100 Finally, applying a food systems approach to food security after disasters, such as production of and access to healthy foods, and supporting diverse, local, and regional agriculture, is an important long-term strategy with clear benefits for both health and climate change.
Suggested adaptive actions for communities and organizations.
Adaptive actions for communities and organizations.
- Identify and address the impact of systematic racism and discrimination in food insecurity and food distribution systems CS_100 , CS_114
- Assess and consider public access to food for people with limited capacity to travel CS_94
- Promote policies and practices to enhance access to affordability of nutritious foods, including food diversion programs that reduce food waste CS_115
- Increase flexibility and access to emergency food for vulnerable populations (D-SNAP, WIC, food banks, and school meals)
- Screen for food insecurity in the healthcare setting
- Address food sovereignty for tribal and Indigenous people116
- Identify and address food deserts within communities CS_99
- Foster partnerships with local food producers through community cooperatives in order to promote food access and local economic resilience
- Create community collaborations for resource sharing CS_117
- Strengthen social support networks among vulnerable populations CS_117
- Undertake risk assessments to understand climate change threats and the current state of preparedness, specifically with regard to food supply CS_118
- Undertake food vulnerability mapping to understand risk profiles among neighborhoods CS_119
- Promote resilient local and regional agricultural practices, including urban agriculture and community gardens CS_120
- Urban food chain supply resilience CS_121
- Local food system resilience and food insecurity CS_122
- A food systems approach to climate change preparedness CS_103
Introduction Compounding Food Insecurity Mechanisms of Food System Disruption Decreased Food Security A Path Towards Equitable Food Security – Table 1: Food Insecurity Risk Factors Adaptive Actions for Health and Equity – Table 2: Adaptive Actions

- High contrast
- Press Centre
Search UNICEF
Building food and nutrition resilience in quezon city: a case study on integrated food systems.
Quezon City is at a paradox where some communities suffer from hunger while others are eating too much of the wrong foods. Increasing evidence of the triple burden of malnutrition—undernutrition, micronutrient deficiencies and overweight/obesity—points to the urgent need for innovative approaches to re-shape urban food environments.
Files available for download
Related topics, more to explore, children eating well in cities: a roadmap for action to support nutritious diets and healthy environments for all children in urban settings, the amsterdam healthy weight approach: investing in healthy urban childhoods: a case study on healthy diets for children, transforming lives with flexible funding.
Timely and flexible funding can save children’s lives today, while helping UNICEF and partners prepare for tomorrow’s threats
Air pollution accounted for 8.1 million deaths globally in 2021, becoming the second leading risk factor for death, including for children under five years
Other content with the tag "Case Study".
The study investigates four Public-Private Partnerships (PPPs) in Mexico, revealing a lack of public information on their implementation and effect

To articulate what it means to take a food systems approach and support policymakers around the world to do so, R4D and City, University of London

Access to Nutrition Initiative (ATNI) has been commissioned to benchmark the world’s 25 largest food and beverage (F&B) companies’ lobbying-rel

Many impact-oriented initiatives are increasingly recognizing the opportunity to support the private sector to empower women in the workplace and g

This study is the result of a landscape analysis undertaken by Action Against Hunger UK for the Global Al

This study was in rural Bangladesh tested the cost effectiveness of a home micronutrient powder food fortification programme for children under the
The Consumer Good Forum (CGF)'s Collaboration for Healthier Lives (CHL) Coalition works to drive collaborative actions through local initiatives to

Almost half of the world’s population – 3 billion people – are directly affected by land degradation.

Nutrition programmes within commodity value chains provide a unique opportunity to improve health outcomes for workers, farmers,

This study looks at research around the implementation of a nutrition programme in a garment factory in Bangladesh.

In 2018, GAIN and HarvestPlus created a partnership with the shared ambition to expand coverage of biofortified nutrient dense foods to at least 20

This study summarises the findings of research undertaken by GAIN and NewForesight to explore the business case for investing in and implementing n

In this research paper, the authors build on nutrition sensitive value chain frameworks and then present an implementation case study that seeks to

As part of the principles of engagement, the global members of the SUN Business Network (SBN) support workforce nutrition commitments (including br
The Partnerships Resource Centre (PrC) conducts research projects to facilitate further knowledge accumulation and learning in the area of sustaina
People’s perception of their ability to meet their needs and the level of autonomy they feel they can exert over their own lives directly correlate

This is an uplifting evidence-based assessment of what it takes to successfully campaign against corporate power.
In this supplement issue of Maternal & Child Nutrition, Helen Keller International ( HKI ) authors have writte
The Global Alliance for Improved Nutrition’s Marketplace for Nutritious Foods program sparks private sector production and marketing of nutritious
This report provides an approach for collaborative policymaking and governance improvement for sustainable food systems.
Ever wondered what it’s like for the people growing your chocolate? Ever thought that they may be children?
The Center for Strategic and International studies have looked at the impact of Feed the Future Investments in Guatemala.
The Center for Strategic and International studies have looked at the impact of Feed the Future Investments in Bangladesh.
The Center for Strategic and International studies have looked at the impact of Feed the Future Investments in Tanzania.
Sight and Life, DSM, and John Hopkin’s Bloomberg School of Public Health have come together to publish lessons from a four decade partnership.
Partnerships for Forests provides financial and technical assistant to help partners do business differently when it comes to land use and preventi
Two page briefing by IBM looking at the causes of supply chain inefficiencies.
Irresponsible resource management does not make business sense – a truism that Kavita Prakash-Mani and Joao Campari at WWF call out in this blog.
Cocoa may not be the most nutritious of agricultural products, but it has huge environmental and economic importance.
This public private partnership in Nigeria demonstrates what can be done to improve crop safety and reduce the non beneficial impacts of toxic crop
Restricted access paper looking at the role for public private partnerships in making agriculture value chains work for smallholder farmers, based

The Demand Engine: Growth Hacking

Partnership between Ipsos – a social market and research company, and The Bill and Melinda Gates Foundation.
FoodSwitch is an example of innovation that is empowering consumers to make smarter nutrition decisions.
Public information on Pepsico's agricultural commodities. For more information on Pepsico’s core business and reporting standards go to our Advanci
Multinationals have the power to change people’s relationship with food – as this short opinion piece demonstrates.
Partnership between Unilever, DSM, Gain, Mondelez, U.N.

The South Asia Food and Nutrition Security Initiative (SAFANSI) is an example of a multi

The cost of a nutritious meal is not fixed and it can be heavily dependent upon the season.
One-page correspondence in the Lancet looking at the benefit of investing in workplace wellness programmes in India.

This report produced by the UK Health Forum provides case studies from around the world to help provide a framework for governing public private in
Realising the potential of workplaces to prevent and control NCDs: How public policy can encourage businesses and governments to work toget
A worksite intervention in South Africa demonstrates the importance of identifying employees with increased risk of cardiovascular disease.
China has undergone rapid change in recent years which has impacted on the health of its workforce.
Two-page briefing on a research study by the United Nations International Labour Organisation assessing Chile’s national workforce nutrition progra
An academic paper by the International Food Policy Research Institute looking at expectations that drive formal public private partnerships in agri

This study of agricultural PPPs in Ghana, Malawi, and Kenya calls for governments, donors, and companies to ensure greater participation from small
For anyone interested in the cost-benefit of food fortification as a public health intervention.
This short video shows the successes of public private collaboration in South Africa.
This article has a useful summary of challenges along the food value chain that prevent compliance with national standards.
Nearly half of India’s population suffer from micronutrient deficiency.

Case studies embedded in local political economy, covering: dairy value chains in Afghanistan, milk value chains in Bangladesh, flour fortification
Lindiwe’s personal story leads into an in-depth analysis of supply chain bottlenecks for subsistence farmers.
Companion document to the United States National Center for Chronic Disease Prevention and Health Promotion Food Service Guidelines in Public Servi

This is the full report from the 2015 Future Fortified Global Summit on Food Fortification - the first ever Global Summit dedicated to large scale

A highly recommended resource on consumer demand from the perspective of public private engagement.

Base of the pyramid typically refers to the largest and poorest socio-economic grouping, and it is estimated that people in this ‘category’ spend u

Improving diets in an era of food market transformation: Challenges and opportunities for engagement between the public and private sectors
Looking outside of the nutrition sector towards the climate change agenda brings a fresh perspective to the issue of incentivising responsible priv

This report, compiled for the European Competitiveness and Sustainable Industrial Policy Consortium, gives a detailed look into the impact of food
Briefing by ActionAid revealing that one in every two dollars of large corporate investment in developing countries is being routed from or a via a

Policy brief by the Global Panel on Agriculture and Food Systems for Nutrition looking at the evidence for gov
Working paper by Consultative Group for International Agricultural Research (CGIAR) looking at how corporate social responsibility and supply agree
Dietary Guidelines for Americans set the country’s nutrition policy and help direct over $80 billion federal spending.
This report from FAO and the Food Climate Research Network looks at national dietary guidelines as a practical intervention to improve nutrition an
In this policy brief, the Global Panel makes the case that healthy diets are a foundation underpinning positive progress towards the Sustainable De
Mars have produced a position statement on their contribution to greenhouse gas emissions.
Unilever’s Paul Polman is a Champion 12.3 – part of a global coalition to accelerate action to achieve UN Sustainable Development Goal 12.3 to half
Report from a workshop on collaborative learning at the Institute of Development Studies in 2017, Brighton, U.K.
This report by the European Union addresses challenges of implementing country cooperation frameworks that fall under the auspices of the New Allia
This report summarizes the findings of a workshop for representatives of the Tanzanian government, development partners, civil society, and private

This 21-page briefing by Society Works summarizes information on 152 social entrepreneurs working on food production, manufacturing, distribution,
Written evidence submitted by Farm Africa and Self Help Africa on December 2012 to the U.K International Development Committee.

Public-Private Partnership Lab: Food and Water is a four-year action research and joint learning initiative to explore the effectiveness of PPPs.
Blog, originally published on Food Security Portal, discussing how global and regional seed companies are working to support smallholder farmers to

This briefing addresses the distinct roles that each partner can play in promoting nutrition under the Comprehensive African Agricultural Developme

Covers a checklist for formal public private partnerships spanning: rationale, design, implementation, sustainability, and the roles for brokers at

A detailed review by the FAO on public private partnerships in agribusiness.
Health gossip is rife in Indonesia.
Presentation for the Wellcome Trust looking at the role of policy on public food choices.
As a systematic and rigorous analysis, this Lancet paper provides perspective on the issue of consumer demand creation by systematically reviewing
The Access to Nutrition Index has produced a 2018 scorecard for Campbell Soup company.
Principles guiding Unilever’s food and beverage marketing communications, including a promise not to direct any marketing communications to childre
A look into how business models can be reshaped to respond to changing consumer preferences.
This is a detailed overview of why people did not take up fortified complementary foods in Ghana, Cote d'Ivoire, India, Bangladesh, and Vietnam.

Alive & Thrive is an initiative that aims to improve infant and young child feeding practices by increasing rates of exclusiv

This paper reviews 41 workforce nutrition interventions published between 1995 and 2006 in the South African Journal of Clinical

Blueprint for Business Action on Health Literacy supports the Europe 2020 strategy and the renewed EU strategy for Corporate Soci
This short report gives an overview of rice fortification literature indexed in PubMed, including examples of successful public private engagement
This lively blog series by Future Fortified - an online platform to explore micronutrient deficiency, covers a range of topics relating to public p
This book examines food fortification in all its forms.
In this synopsis - aimed at business leaders, governments and implementing agencies - IFPRI and Nourishing Millions provide recommendations on how
In 2015 the Nourishing Millions project reviewed literature and case studies to show the evolution of nutrition during the past 50 years.

A concise account of lessons learned on salt and iron iodization by world renowned economists, as part of the costs benefit analysis on leading dev
Written by world renowned economists, this paper highlights the cost efficiency of select nutrition interventions and ranks fortification among the

This report analyses fourteen projects in low and middle income countries working on reducing food loss and waste in food systems.
SNV is a team of advisers that work with business, governments, and implementing agencies.
This presentation is the outcome of a high level policy dialogue in 2015 by the Asia-Pacific Economic Cooperation.
This article by a non-profit called Concordia makes the simple argument that food insecurity and loss can only be addressed by increased collaborat

Recommendations from the Global Panel on Agriculture and Food Systems are targeted at policy makers in low- and middle-income countries
This report looks at supply chain waste based on Feedback's research on export supply chains in Peru, Senegal, South Africa, the UK and a major Eur
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Case studies and evidence based nutrition
Affiliation.
- 1 Fuli Institute of Food Science and Nutrition, Room D437 Agricultural, Biological and Environmental Building, Zijingang Campus, Zhejiang University. [email protected].
- PMID: 24231006
- DOI: 10.6133/apjcn.2013.22.4.22
Abstract in English, Chinese
The clinical nutrition case study is a neglected area of activity and publication. This may be in part because it is not regarded as a serious contributor to evidence-based nutrition (EBN). Yet it can play a valuable part in hypothesis formulation and in the cross-checking of evidence. Most of all, it is usually a point at which the operationalisation of nutrition evidence is granted best current practice status.
臨床營養之個案研究在施行與出版中是一個被忽視的領域。部分原因可能在 於,它不被視為實證營養學(EBN)之重要貢獻者。然而,它卻在假說成形與交 叉驗證中扮演重要角色。最重要的,在認為營養證據操作化乃是目前最好實 行方式下,個案研究確實有其意義。
PubMed Disclaimer
Similar articles
- How evidence-based medicine biases physicians against nutrition. Thomas LE. Thomas LE. Med Hypotheses. 2013 Dec;81(6):1116-9. doi: 10.1016/j.mehy.2013.10.016. Epub 2013 Oct 30. Med Hypotheses. 2013. PMID: 24238959
- The opportunities and challenges of evidence-based nutrition (EBN) in the Asia Pacific region: clinical practice and policy-setting. Wahlqvist ML, Lee MS, Lau J, Kuo KN, Huang CJ, Pan WH, Chang HY, Chen R, Huang YC. Wahlqvist ML, et al. Asia Pac J Clin Nutr. 2008;17(1):2-7. Asia Pac J Clin Nutr. 2008. PMID: 18364319 Review.
- Evidence-based nutrition practice guidelines: A valuable resource in the evidence analysis library. Blumberg-Kason S, Lipscomb R. Blumberg-Kason S, et al. J Am Diet Assoc. 2006 Dec;106(12):1935-6. doi: 10.1016/j.jada.2006.10.025. J Am Diet Assoc. 2006. PMID: 17126620 No abstract available.
- Seeking the balance between individual and community-based nutritional interventions. Rosser WW. Rosser WW. Eur J Clin Nutr. 2005 Aug;59 Suppl 1:S102-5; discussion S106-7. doi: 10.1038/sj.ejcn.1602181. Eur J Clin Nutr. 2005. PMID: 16052176 Review. No abstract available.
- Systems for evaluating nutrition research for nutrition care guidelines: do they apply to population dietary guidelines? Myers E. Myers E. J Am Diet Assoc. 2003 Dec;103(12 Suppl 2):S34-41. doi: 10.1016/j.jada.2003.09.035. J Am Diet Assoc. 2003. PMID: 14666498
Publication types
- Search in MeSH
LinkOut - more resources
Full text sources.
- HEC Press, Healthy Eating Club PTY LTD
- MedlinePlus Health Information

- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
- AI Content Shield
- AI KW Research
- AI Assistant
- SEO Optimizer
- AI KW Clustering
- Customer reviews
- The NLO Revolution
- Press Center
- Help Center
- Content Resources
- Facebook Group
Creative Steps to Write a Nutrition Case Study
Table of Contents
Nutrition plays a vital role in improving a patient’s health. However, each patient has unique nutritional needs requiring a personalized healthcare approach. That’s where nutrition case studies come in. These case studies comprehensively assess a patient’s nutritional status and help develop an individualized nutrition plan. They also help to monitor and evaluate the patient’s progress toward their health goals over time. In this article, we will provide a step-by-step guide on how to write a nutrition case study . This post will help you understand the importance of nutrition case studies, whether you are a healthcare professional or a student.
What Is a Nutrition Case Study?
A nutrition case study comprehensively reports an individual’s nutritional status, dietary habits, and health outcomes . Healthcare professionals typically use these case studies to evaluate and treat patients. This is with various nutritional concerns, such as obesity, malnutrition, or chronic diseases. If you are a nutrition student or practitioner, learning how to write a nutrition case study is an essential skill to have.
Importance of Nutrition Case Study
Nutrition case studies are a crucial tool for healthcare professionals in nutrition and dietetics. Here are some of the reasons why nutrition case studies are essential:
Provides a Comprehensive Assessment of a Patient’s Nutritional Status
Nutrition case studies involve a detailed analysis of a patient’s dietary intake, medical history, and lifestyle factors that may impact their nutritional status. This information is used to develop a personalized nutrition plan tailored to the patient’s needs.
Develops an Individualized Nutrition Plan
A nutrition case study’s personalized approach to healthcare leads to an individualized nutrition plan. This approach can lead to better patient outcomes, improved health outcomes, and a higher quality of life for the patient.
Monitors and Evaluates Progress Over Time
Nutrition case studies track a patient’s food intake, weight, body composition, and other health outcomes over time. This enables healthcare professionals to monitor and evaluate the patient’s progress toward their health goals and adjust the nutrition plan as needed.
Provides Education About Healthy Eating Habits and Lifestyle Changes
Nutrition case studies can help educate patients about healthy eating habits and lifestyle changes. By providing a detailed assessment of a patient’s nutritional status, healthcare professionals can help patients make sustainable changes to their diet and lifestyle.
Supports Evidence-Based Practice
Nutrition case studies are based on evidence-based practice, meaning the nutrition plan is grounded in scientific research and clinical expertise. This approach ensures that the patient receives the best care based on the latest research and clinical knowledge.
Steps on How to Write a Nutrition Case Study
Selecting the patient.
The first step in writing a nutrition case study is selecting the patient. Typically, the patient has sought out nutritional counseling or treatment for a specific reason. These reasons include weight management, a chronic disease, or a food allergy. The patient should be willing to participate in the case study and provide detailed information about their diet, health history, and lifestyle habits. When selecting a patient, obtaining their written consent to participate in the case study is essential. This should include an explanation of the purpose of the case study and how their information will be used. It should also add any potential risks or benefits of participating. The patient should know that they can stop participating in the research at any moment if they don’t want to.
Gathering Information
The next step in writing a nutrition case study is gathering information about the patient. This includes a comprehensive assessment of their dietary habits, health status, medical history, and lifestyle factors that may impact their nutrition. To gather this information, you may need to conduct a nutrition assessment, which typically includes the following components:
Anthropometric Measurements
This involves measuring the patient’s height, weight, body mass index (BMI), and other body composition measures.
Dietary Intake Assessment
This involves collecting information about the patient’s dietary habits, including food preferences, allergies, and cultural or religious dietary restrictions.
Biochemical Assessment
This involves analyzing the patient’s blood, urine, or other biological samples to assess their nutritional status.
Medical History
This involves collecting information about the patient’s past and current medical conditions, medications, and surgeries.
Lifestyle Assessment
This involves collecting information about the patient’s physical activity, stress, and other lifestyle factors that may impact their nutrition status. Gathering as much information as possible is essential to create a comprehensive nutrition case study. This information will help you develop an individualized nutrition plan addressing the patient’s needs and concerns.
Developing a Nutrition Plan
Once you have gathered all the necessary information, the next step is to develop a nutrition plan for the patient. The nutrition plan should be based on the patient’s dietary needs, health goals, and lifestyle factors. It should also consider any medical conditions or medications that may impact the patient’s nutritional status. The nutrition plan should include the following components:
Macronutrient and Micronutrient Recommendations
This involves recommending specific amounts of carbohydrates, protein, fat, and other essential nutrients the patient should consume daily.
Food Group Recommendations
This involves recommending specific food groups for the patient, such as fruits, vegetables, whole grains, and lean proteins.
Meal and Snack Recommendations
This involves recommending specific meals and snacks for the patient to meet their nutritional needs throughout the day.
Nutritional Supplements
This involves recommending specific nutritional supplements, such as vitamins, minerals, or protein powders, that may help patients meet their nutritional needs.
Behavioral Recommendations
This involves recommending specific behavioral changes that may impact the patient’s nutrition status, such as increasing physical activity or reducing stress. The nutrition plan should be individualized to the patient’s needs and preferences. It should also be realistic and achievable, considering any barriers the patient may face in following the plan.
Implementing the Nutrition Plan
Once the nutrition plan has been developed, the next step is implementing it with the patient. This may involve educating the patient about healthy eating habits and strategies for making dietary changes. The patient should also be encouraged to track their food intake and monitor their progress toward their health goals. Working collaboratively with the patient throughout the implementation process is essential, as ongoing support and guidance are needed. This may involve regular follow-up appointments or communication via phone or email. The patient should be encouraged to ask questions and share any concerns or challenges they may be experiencing.
Monitoring and Evaluating Progress
The final step in writing a nutrition case study is monitoring and evaluating the patient’s progress. This involves tracking the patient’s food intake, weight, body composition, and other health outcomes. The patient’s progress should be regularly assessed, and adjustments made to the nutrition plan as needed. Objective measures such as laboratory values or body composition assessments are essential to evaluate the patient’s progress. This can help ensure that the nutrition plan is effective and that the patient is progressing toward their health goals.

How to Write a Nutrition Case Study
Once the nutrition plan has been implemented and the patient’s progress has been evaluated, it is time to write the case study. The case study should be organized in a logical and easy-to-read format, and should include the following sections:
Introduction
This should provide an overview of the patient’s case and outline the purpose of the case study.
Patient History
You should provide a comprehensive overview of the patient’s medical history, dietary habits, and lifestyle factors that may impact their nutritional status.
Nutrition Assessment
This should provide a detailed assessment of the patient’s nutritional status, including anthropometric measurements, dietary intake, biochemical markers, and medical history.
Nutrition Plan
This should provide a comprehensive overview of the patient’s individualized nutrition plan. They include macronutrient and micronutrient recommendations, food group recommendations, meal and snack recommendations, nutritional supplement recommendations, and behavioral recommendations.
Implementation and Follow-Up
This should provide an overview of the patient’s progress in implementing the nutrition plan, including any challenges or barriers encountered. It should also outline the follow-up appointments or communication that took place between the patient and healthcare provider.
This should provide an overview of the patient’s progress towards their health goals, including any changes in weight, body composition, or laboratory values.
This should provide an interpretation of the patient’s results, including any limitations or strengths of the case study. It should also provide a summary of the key takeaways and implications for future practice.
Writing a nutrition case study may not be the most exciting task in the world, but it is a crucial one. By following these steps and using a bit of wit and creativity, healthcare professionals can effectively communicate their patient’s nutritional needs . This shows progress toward their health goals. Who knows, maybe writing a nutrition case study will be more fun than you thought!

Abir Ghenaiet
Abir is a data analyst and researcher. Among her interests are artificial intelligence, machine learning, and natural language processing. As a humanitarian and educator, she actively supports women in tech and promotes diversity.
Explore All Write A Case Study Articles
How to write a leadership case study (sample) .
Writing a case study isn’t as straightforward as writing essays. But it has proven to be an effective way of…
- Write A Case Study
Top 5 Online Expert Case Study Writing Services
It’s a few hours to your deadline — and your case study college assignment is still a mystery to you.…
Examples Of Business Case Study In Research
A business case study can prevent an imminent mistake in business. How? It’s an effective teaching technique that teaches students…
How to Write a Multiple Case Study Effectively
Have you ever been assigned to write a multiple case study but don’t know where to begin? Are you intimidated…
How to Write a Case Study Presentation: 6 Key Steps
Case studies are an essential element of the business world. Understanding how to write a case study presentation will give…
How to Write a Case Study for Your Portfolio
Are you ready to showcase your design skills and move your career to the next level? Crafting a compelling case…
- Interactivity
- AI Assistant
- Digital Sales
- Online Sharing
- Offline Reading
- Custom Domain
- Branding & Self-hosting
- SEO Friendly
- Create Video & Photo with AI
- PDF/Image/Audio/Video Tools
- Art & Culture
- Food & Beverage
- Home & Garden
- Weddings & Bridal
- Religion & Spirituality
- Animals & Pets
- Celebrity & Entertainment
- Family & Parenting
- Science & Technology
- Health & Wellness
- Real Estate
- Business & Finance
- Cars & Automobiles
- Fashion & Style
- News & Politics
- Hobbies & Leisure
- Recipes & Cookbooks
- Photo Albums
- Invitations
- Presentations
- Newsletters
- Sell Content
- Fashion & Beauty
- Retail & Wholesale
- Presentation
- Help Center Check out our knowledge base with detailed tutorials and FAQs.
- Learning Center Read latest article about digital publishing solutions.
- Webinars Check out the upcoming free live Webinars, and book the sessions you are interested.
- Contact Us Please feel free to leave us a message.

Dietetic and Nutrition Case Studies
Description: dietetic and nutrition case studies, keywords: diet,nutrition, read the text version.
No Text Content!
Dietetic and Nutrition Case Studies This book is dedicated to Pat Judd (1947–2015), inspirational dietitian and educator. Dietetic and Nutrition Case Studies EDITED BY Judy Lawrence Registered Dietitian, the Research Officer for the BDA, and Visiting Researcher, Nutrition and Dietetics, King’s College London, England Pauline Douglas Registered Dietitian, a Senior Lecturer and Clinical Dietetic Facilitator, Northern Ireland Centre for Food and Health (NICHE), Ulster University, Northern Ireland Joan Gandy Registered Dietitian, a Freelance Dietitian and Visiting Researcher in Nutrition and Dietetics, University of Hertfordshire, England This edition first published 2016 © 2016 by John Wiley & Sons, Ltd Registered office: John Wiley & Sons, Ltd, The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK Editorial offices: 9600 Garsington Road, Oxford, OX4 2DQ, UK The Atrium, Southern Gate, Chichester, West Sussex, PO19 8SQ, UK 111 River Street, Hoboken, NJ 07030-5774, USA For details of our global editorial offices, for customer services and for information about how to apply for permission to reuse the copyright material in this book please see our website at www.wiley.com/wiley-blackwell The right of the author to be identified as the author of this work has been asserted in accordance with the UK Copyright, Designs and Patents Act 1988. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, except as permitted by the UK Copyright, Designs and Patents Act 1988, without the prior permission of the publisher. Designations used by companies to distinguish their products are often claimed as trademarks. All brand names and product names used in this book are trade names, service marks, trademarks or registered trademarks of their respective owners. The publisher is not associated with any product or vendor mentioned in this book. It is sold on the understanding that the publisher is not engaged in rendering professional services. If professional advice or other expert assistance is required, the services of a competent professional should be sought. The contents of this work are intended to further general scientific research, understanding, and discussion only and are not intended and should not be relied upon as recommending or promoting a specific method, diagnosis, or treatment by health science practitioners for any particular patient. The publisher and the author make no representations or warranties with respect to the accuracy or completeness of the contents of this work and specifically disclaim all warranties, including without limitation any implied warranties of fitness for a particular purpose. In view of ongoing research, equipment modifications, changes in governmental regulations, and the constant flow of information relating to the use of medicines, equipment, and devices, the reader is urged to review and evaluate the information provided in the package insert or instructions for each medicine, equipment, or device for, among other things, any changes in the instructions or indication of usage and for added warnings and precautions. Readers should consult with a specialist where appropriate. The fact that an organization or Website is referred to in this work as a citation and/or a potential source of further information does not mean that the author or the publisher endorses the information the organization or Website may provide or recommendations it may make. Further, readers should be aware that Internet Websites listed in this work may have changed or disappeared between when this work was written and when it is read. No warranty may be created or extended by any promotional statements for this work. Neither the publisher nor the author shall be liable for any damages arising herefrom. Library of Congress Cataloging-in-Publication Data Names: Lawrence, Judy, 1960- , editor. | Gandy, Joan, editor. | Douglas, Pauline, 1961- , editor. Title: Dietetic and nutrition case studies / edited by Judy Lawrence, Joan Gandy, Pauline Douglas. Description: Chichester, West Sussex ; Hoboken, NJ : John Wiley & Sons, 2016. | Complemented by: Manual of dietetic practice / edited by Joan Gandy in conjunction with the British Dietetic Association. Fifth edition. 2014. | Includes bibliographical references and index. Identifiers: LCCN 2015040817 (print) | LCCN 2015042999 (ebook) | ISBN 9781118897102 (pbk.) | ISBN 9781118898239 (pdf) | ISBN 9781118898246 (epub) Subjects: | MESH: Dietetics. | Nutritional Physiological Phenomena. | Diet Therapy. | Problem-Based Learning. Classification: LCC RM216 (print) | LCC RM216 (ebook) | NLM WB 400 | DDC 615.8/54 – dc23 LC record available at http://lccn.loc.gov/2015040817 A catalogue record for this book is available from the British Library. Wiley also publishes its books in a variety of electronic formats. Some content that appears in print may not be available in electronic books. Set in 9/12pt, MeridienLTStd by SPi Global, Chennai, India. 1 2016 Contents List of contributors, ix Preface, xvii Online resources, xix PART I 1 Model and process for nutrition and dietetic practice, 3 2 Nutrition care process terminology (NCPT), 8 3 Record keeping, 12 4 Assessment, 16 PART II Case studies 1 Veganism, 25 2 Older person – ethical dilemma, 28 3 Older person, 31 4 Learning disabilities: Prader–Willi syndrome, 34 5 Freelance practice, 39 6 Public health – weight management, 41 7 Public health – learning disabilities, 48 8 Public health – calorie labelling on menus, 52 9 Genetics and hyperlipidaemia, 55 10 Intestinal failure, 59 11 Irritable bowel syndrome, 62 12 Liver disease, 66 13 Renal disease, 69 14 Renal – black and ethnic minority, 72 15 Motor neurone disease/amyotrophic lateral sclerosis, 75 16 Chronic fatigue syndrome/myalgic encephalopathy, 78 v vi Contents 17 Refsum’s disease, 81 18 Adult phenylketonuria, 83 19 Osteoporosis, 86 20 Eating disorder associated with obesity, 90 21 Forensic mental health, 92 22 Food allergy, 97 23 HIV/AIDS, 102 24 Type 1 diabetes mellitus, 106 25 Type 2 diabetes mellitus – Kosher diet, 111 26 Type 2 diabetes mellitus – private patient, 114 27 Gestational diabetes mellitus, 117 28 Polycystic ovary syndrome, 121 29 Obesity – specialist management, 125 30 Obesity – Prader–Willi syndrome, 131 31 Bariatric surgery, 136 32 Stroke and dysphagia, 140 33 Hypertension, 143 34 Coronary heart disease, 146 35 Haematological cancer, 150 36 Head and neck cancer, 153 37 Critical care, 157 38 Traumatic brain injury, 160 39 Spinal cord injury, 164 40 Burns, 167 41 Telehealth and cystic fibrosis, 170 Case studies’ answers 1 Veganism, 173 2 Older person-ethical dilemma, 177 3 Older person, 180 4 Learning disabilities: Prader–Willi syndrome, 183 5 Freelance practice, 186 6 Public health – weight management, 189 7 Public health – learning disabilities, 193 Contents vii 8 Public health – calorie labelling on menus, 197 9 Genetics and hyperlipidaemia, 199 10 Intestinal failure, 205 11 Irritable bowel syndrome, 207 12 Liver disease, 210 13 Renal disease, 216 14 Renal – black and ethnic minority, 221 15 Motor neurone disease/amyotrophic lateral sclerosis, 224 16 Chronic fatigue syndrome/myalgic encephalopathy, 227 17 Refsum’s disease, 230 18 Adult phenylketonuria, 233 19 Osteoporosis, 236 20 Eating disorder associated with obesity, 238 21 Forensic mental health, 242 22 Food allergy, 245 23 HIV/AIDS, 248 24 Type 1 diabetes mellitus, 251 25 Type 2 diabetes mellitus – Kosher diet, 254 26 Type 2 diabetes mellitus – private patient, 257 27 Gestational diabetes mellitus, 261 28 Polycystic ovary syndrome, 266 29 Obesity – specialist management, 269 30 Obesity – Prader–Willi syndrome, 272 31 Bariatric surgery, 276 32 Stroke and dysphagia, 283 33 Hypertension, 285 34 Coronary heart disease, 287 35 Haematological cancer, 290 36 Head and neck cancer, 296 37 Critical care, 302 38 Traumatic brain injury, 307 39 Spinal cord injury, 312 40 Burns, 315 41 Telehealth and cystic fibrosis, 317 viii Contents Appendices A1 Dietary reference values, 323 A2 Weights and measures, 328 A3 Dietary data, 335 A4 Body mass index, 342 A5 Anthropometric and functional data, 346 A6 Predicting energy requirements, 352 A7 Clinical chemistry, 353 Index, 361 List of contributors Ellie Allen Clinical Lead Dietitian, University College London Hospitals NHS Foundation Trust, London, United Kingdom Barbara Martini Arora Freelance Registered Dietitian, Bromley, United Kingdom Eleanor Baldwin Advanced Dietitian – Adult Refsums Disease and Bariatrics, Chelsea and Westminster NHS Foundation Trust, London, United Kingdom Julie Beckerson Haemato-Oncology Specialist, Imperial College Healthcare NHS Trust, London, United Kingdom Kathleen Beggs Clinical Tutor, The University of British Columbia, Vancouver, BC, Canada Helen Bennewith Professional Lead for Addiction and Mental Health Dietetics, NHS Greater Glasgow and Clyde, Glasgow, Scotland, United Kingdom Sarah Bowyer PhD Research Student in Rural Health, University of the Highlands and Islands, Inver- ness, Scotland, United Kingdom Rachael Brandreth Children’s Weight Management Dietitian, Royal Cornwall Hospital Trust, Cornwall, United Kingdom Elaine Cawadias Clinical Instructor, Faculty of Land and Food Systems, The University of British Columbia, Vancouver, BC, Canada ix x List of contributors Alison Culkin Research Dietitian, London North West Healthcare NHS Trust, London, United Kingdom Rachael Donnelly Acting Clinical Lead Dietitian, Guy’s and St Thomas’ NHS Foundation Trust, London, United Kingdom Pauline Douglas Senior Lecturer and Clinical Dietetic Facilitator, Northern Ireland Centre for Food and Health (NICHE), University of Ulster, Londonderry, Northern Ireland, United Kingdom Hilary Du Cane Freelance Dietitian and Marketeer, United Kingdom Alastair Duncan Lead Dietitian, NIHR Clinical Doctoral Research Fellow, Guy’s and St. Thomas’ NHS Foundation Trust, London, United Kingdom Mary Flynn Chief Specialist Public Health Nutrition, Food Safety Authority of Ireland, Dublin, Ireland; Visiting Professor, University of Ulster, Coleraine, Northern Ireland, United Kingdom Caroline Foster Specialist Dietitian, Leeds and York Partnership NHS Foundation Trust, Leeds, United Kingdom Lisa Gaff Specialist Dietitian, Addenbrookes Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom Joan Gandy Freelance Dietitian and Visiting Researcher, Nutrition and Dietetics, University of Hertfordshire, Hatfield, United Kingdom Elaine Gardner Freelance Dietitian, London, United Kingdom Susie Hamlin Senior Specialist Dietitian Liver Transplantation, Hepatology and Critical Care, St James’s University Hospital, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom List of contributors xi Nicola Henderson AHP Team Lead, NHS Forth Valley, Larbert, United Kingdom Sandra Hood Diabetes Dietitian, The Diabetes Centre, Dorset County Hospital NHS Foundation Trust, Dorchester, Dorset, United Kingdom Nicola Howle Mental Health Dietitian, South Staffordshire and Shropshire Healthcare NHS Foun- dation Trust, Lichfield, United Kingdom Bushra Jafri Human Nutrition and Dietetics, London Metropolitan University, London, United Kingdom Yvonne Jeanes Senior Lecturer in Clinical Nutrition, University of Roehampton, London, United Kingdom Sema Jethwa Senior Diabetes Specialist Dietitian, University College London Hospital NHS Trust, London, United Kingdom; Freelance Dietitian, Hertfordshire, United Kingdom Susanna Johnson Community Paediatric Dietitian, Wembley Centre for Health and Care, Central London Community Healthcare NHS Trust, London, United Kingdom Natasha Jones Advanced Specialist Haematology/TYA dietitian, Addenbrookes Hospital, Cambridge University Hospitals NHS Foundation Trust, Cambridge, United Kingdom Ruth Kander Senior Dietitian and Consultant Dietitian, Imperial College Healthcare NHS Trust, London, United Kingdom and Consultant East Kent Dietitian. Joanna Lamming Specialist Weight Management Dietitian, East, Kent, United Kingdom Anne Laverty Specialist Dietitian, Learning Disabilities, Northern Health and Social Care Trust, Coleraine, Northern Ireland, United Kingdom xii List of contributors Judy Lawrence Research Officer BDA and Visiting Researcher, King’s College London, London, United Kingdom Julie Leaper Senior Specialist Dietitian (Liver/ICU) St James’s Hospital, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom Sian Lewis Macmillan Clinical Lead Dietitian, Chair of BDA Specialist Oncology Group, Velindre Cancer Centre, Wales, United Kingdom Sherly X. Li PhD Candidate, MRC Epidemiology Unit, University of Cambridge, Cambridge, United Kingdom Seema Lodhia HCA Healthcare, London, United Kingdom Julie Lovegrove Head of the Hugh Sinclair Unit of Human Nutrition, University of Reading, Reading, United Kingdom Marjorie Macleod Specialist Dietitian, Learning Disabilities Service, NHS Lothian, Edinburgh, Scotland, United Kingdom Paul McArdle Lead Clinical Dietitian and Deputy Head of Dietetics, NIHR Clinical Doctoral Research Fellow and Freelance Dietitian, Birmingham Community Healthcare NHS Trust, Birmingham, United Kingdom Angela McComb Health and Social Wellbeing Improvement Manager, Northern Health and Social Care Trust, Londonderry, Northern Ireland, United Kingdom Caoimhe McDonald Research Dietitian, Mercers Institute for Research on Ageing, St. James Hospital, Dublin, Ireland Jennifer McIntosh Clinical Lead Dietitian, Leeds and York Partnership NHS Foundation Trust, Leeds, United Kingdom List of contributors xiii Yvonne McKenzie Specialist in Gastrointestinal Nutrition, Clinical Lead in IBS for the Gastroenterology Specialist Group of the British Dietetic Association, Birmingham, United Kingdom Kirsty-Anna McLaughlin Community Nutrition Support Dietitian, Wiltshire Primary Care Trust, Wiltshire, United Kingdom Kassandra Montanheiro Macmillan Senior Specialist Dietitian, University College London Hospitals NHS Foundation Trust, London, United Kingdom Eileen Murray Specialist Mental Health Dietitian, NHS Greater Glasgow and Clyde Directorate of Forensic Mental Health and Learning Disabilities, Glasgow, Scotland, United Kingdom Mary O’Kane Consultant Dietitian (Adult Obesity), Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom Sian O’Shea Head of Nutrition and Dietetics for Learning Disabilities, Aberkenfig Health Board, Bridgend, United Kingdom Sue Perry Deputy Head of Dietetics, Hull Royal Infirmary, Hull and East Yorkshire Hospitals NHS Trust, Hull, United Kingdom Gail Pinnock Specialist Bariatric Surgery Dietitian, Homerton University Hospital NHS Foundation Trust, London, United Kingdom Vicki Pout Deputy Acute Dietetic Manager, Queen Elizabeth the Queen Mother Hospital, Kent Community Health NHS Foundation Trust, Margate, Kent, United Kingdom Louise Robertson Specialist Dietian, Inherited Metabolic Diseases, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom Juneeshree S. Sangani Freelance Dietitian, United Kingdom xiv List of contributors Nicola Scott Senior Specialist Haematology Dietitian, St James’s University Hospital, Leeds Teach- ing Hospital NHS Trust, Leeds, United Kingdom Ella Segaran Specialist Dietitian for Critical Care, Chair of Dietitians in Critical Care Specialist Group of the BDA, St Mary’s Hospital, Imperial College Healthcare NHS Trust, London, United Kingdom Reena Shaunak Diabetes Specialist Dietitian, West Middlesex University Hospital NHS Trust, Isleworth, United Kingdom Bushra Siddiqui Renal Dietitian, Queen Elizabeth Hospital Birmingham, University Hospitals Birm- ingham NHS Foundation Trust, Birmingham, United Kingdom Isabel Skypala Consultant Allergy Dietitian and Clinical Lead for Food Allergy, Royal Brompton and Harefield NHS Foundation Trust, London, United Kingdom Alison Smith Prescribing Support Dietitian, Aylesbury Vale Clinical Commissioning Group and Chiltern Clinical Commissioning Group, Aylesbury, United Kingdom Chris Smith Specialist Paediatric Dietitian, Royal Alexandra Hospital, Brighton, United Kingdom Clare Stradling NIHR Doctoral Research Fellow, Birmingham Heartlands Hospital, University of Birmingham, Birmingham, United Kingdom Carolyn Taylor Specialist Dietitian, Northern General Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom Lucy Turnbull Clinical Lead for Chronic Disease and Weight Management Services, Central London Community Healthcare, London, United Kingdom Evelyn Volders Senior Lecturer Nutrition and Dietetics, Monash University, Melbourne, Victoria, Australia List of contributors xv Kirsten Whitehead Assistant Professor, Division of Nutritional Sciences, University of Nottingham, Nottingham, United Kingdom Kate Williams Head of Nutrition and Dietetics, South London and Maudsley NHS Foundation Trust, London, United Kingdom E. Mark Windle Specialist Dietitian, Burns and Intensive Care, Mid Yorkshire Hospitals NHS Trust, Wakefield, United Kingdom Preface Problem-based learning (PBL) is increasingly becoming the preferred method of teaching in health care. There is currently a dearth of appropriately written case studies. This book takes a PBL approach to dietetics and nutrition and aims to address this gap. It has been written to complement the Manual of Dietetic Practice (MDP) (5th edition), and the case studies are cross-referenced accordingly. Uniquely, the case studies are written and peer reviewed by registered dietitians, drawing on their own experiences and specialist knowledge. This book has been written and edited with many readers in mind. Lecturers and staff in universities with courses in dietetics and nutrition will undoubtedly find it relevant although it will be useful to many other health care students and professionals. The case studies are also aimed at qualified dietitians and nutritionists as a tool to enhance their continuing professional development. Readers will be able to work through the case studies individually and in groups in different settings including dietetic departments. It will also help dietetic students and dietitians to identify further areas of practice that may be of interest to them. Each case study follows the Process for Nutrition and Dietetic Practice (PNDP) that was published by the British Dietetic Association (BDA) in 2012. While throughout the world there are slight variations in nutrition and dietetic models and processes, the case studies can be successfully used alongside these. In addition, the Nutrition Care Process Terminology (NCPT), formally known as International Dietetics and Nutrition Terminology (IDNT), is used throughout the case studies – a feature prac- titioners worldwide will find useful. Each case study starts with a scenario, which will enable the reader to identify the need for a nutritional intervention. This is followed by the assessment step of the PNDP and is standardised by the use the ABCDE format in most cases. Questions are posed about the assessment, the intervention and evaluation and monitoring steps. Some case studies also include further questions to stretch more newly qualified and more experienced practitioners. The PNDP is central to all areas of practice although it may be easier to identify each step in clinical areas than in other areas such as public health. This book includes real life case studies in public health, an increasingly impor- tant area of practice, and although they may be more detailed by carefully working through the case study and answers, it is possible to identify each and every step of PNDP. Questions on ethical issues are included in some case studies; however, ethics should always be of prime importance to any health care professional and is central to practice. xvii xviii Preface The book is split into two parts; firstly to reinforce keys areas of practice pertinent to this book it starts with the following introductory chapters: • Model and process for dietetic practice • Nutrition care process terminology • Documentation and record keeping • Assessment – including the ABCDE assessment process This is followed by the case studies and separate answers. To avoid duplication the references for both the case studies and the answers are given at the end of each case study regardless of where they are cited. For completeness and to aid readers, many appendices from the Manual of Dietetic Practice are reproduced in the book. They include dietary reference values, weight and measures, dietary data, anthropometric data, energy prediction equations and so on and clinical chemistry. Many of the case studies also have a link to a relevant PEN, Practice Based Evidence in Nutrition (PEN), practice question or resource. Dietitians in Australia, Canada, the United Kingdom and Ireland will be familiar with this global resource for nutrition practice. We hope that readers enjoy using this book as much as we have enjoyed compiling it. Finally, we would like to thank the contributors and reviewers who have been invaluable when compiling this book. Judy Lawrence Pauline Douglas Joan Gandy Online resources Additional resources, which may be of interest to readers of this book, can be found on the companion website for the Manual of Dietetic Practice, 5th Edition, edited by Joan Gandy. http://www.manualofdieteticpractice.com/ The website includes • Case study summaries (PDF) • An alphabetical list of web resources • Appendices from the book (PDF) • Reference lists with CrossRef links • Tables from the Manual of Dietetic Practice (PDF) • Figures from the Manual of Dietetic Practice (PPT) • Updates xix PART I CHAPTER 1 Model and process for nutrition and dietetic practice Judy Lawrence The nutrition care process and model was first conceived by the Academy of Nutrition and Dietetics (Lacey & Pritchett, 2003). Since then it has evolved and been adapted and is now used by dietitians and nutritionists worldwide. The case studies in this book are written with the nutrition and dietetic care process in mind. The process can be used in any setting including clinical dietetics and public health. Although case studies in this book are based around the British Dietetic Association’s (BDA) (2012) model and process (Figure 1.1) used by dietitians in the United Kingdom, they can be used alongside other versions of the process and model as well. The model starts with the identification of nutritional need, followed by six stages, namely, assess- ment, identification of the nutrition and dietetic diagnosis, planning the nutrition and dietetic intervention, implementing the intervention, monitoring and reviewing the intervention and finally evaluating the intervention. The case studies use the ABCDE approach (Gandy, 2014), were A is for anthropome- try, B stands for biochemical and haematological markers, C for clinical, D for dietary and E is used to include economic, environmental and social issues that may be rele- vant. Information collected during the assessment is used to make the nutrition and dietetic diagnosis. More details of the assessment can be found in Chapter 4. Identifying the nutrition and dietetic diagnosis The nutrition and dietetic diagnosis is the nutritional problem that is assessed using the dietitian’s clinical reasoning skills and resolved or improved by dietetic interven- tion. The nutrition and dietetic diagnosis is a key part of the care process, and once the correct diagnosis has been made the intervention and the most appropriate outcomes to monitor will fall into place. The nutrition and dietetic diagnosis is written as a struc- tured sentence known as the PASS statement, where P is the problem, A the aetiology and SS the signs and symptoms. The PASS statement should describe the ‘Problem’ related to ‘Aetiology’ as characterised by ‘Signs/Symptoms’, for example; inadequate energy intake (problem) related to an overly restrictive gluten free diet (aetiology) as characterised by weight loss of 4 kg and anxiety regarding appropriate food choices Dietetic and Nutrition Case Studies, First Edition. Edited by Judy Lawrence, Pauline Douglas, and Joan Gandy. © 2016 John Wiley & Sons, Ltd. Published 2016 by John Wiley & Sons, Ltd. Companion Website: http://www.manualofdieteticpractice.com/ 3 4 Dietetic and Nutrition Case Studies Identification of nutritional need Evaluation 6 1 Assessment Monitor Service user’s values and Identification and review 5 service user/dietitian 2 of nutrition relationship and dietetic diagnosis 43 Implement Plan nutrition and nutrition and dietetic dietetic intervention intervention Figure 1.1 Nutrition and dietetic process (BDA (2012), p. 7. Reproduced with permission of British Dietetis Association). (signs and symptoms). A well-written PASS statement is one where the dietitian or nutritionist can improve or resolve the problem, the intervention addresses the aeti- ology and the signs and symptoms can be monitored and improved. The nutrition and dietetic diagnosis can be broken down into the three steps; problem, aetiology and signs and symptoms. Problem This is the nutritional (dietetic) problem not the medical problem; it is the problem that can be addressed by dietetic intervention. In these case studies, the problems are expressed using the diagnosis terms as approved by the BDA. More details about the terminology can be found in Chapter 2 on international language and terminology. The problem is the change in the nutrition state that is described by adjectives such as decreased/increased, excessive/inadequate, restricted and imbalanced. In the United Kingdom, nutrition and dietetic diagnosis terms fall into one of the following seven categories: • Energy balance; • Oral or nutritional support; • Nutrient intake; Model and process for nutrition and dietetic practice 5 • Function, for example, swallowing; • Biochemical; • Weight; and • Behavioural/environmental. There may be more than one problem, so a number of nutritional and dietetic diagnoses may be possible but these can often be consolidated into one diagnosis or one diagnosis may be prioritised, using clinical judgement and the client’s wishes. Some nutrition and dietetic diagnosis may be more appropriate than others; practice and experience will hone this skill. Aetiology The aetiology is the cause of the nutritional problem. Causes may be related to behavioural issues such as food choices, environmental issues such as food avail- ability, knowledge such as not knowing which foods are gluten free, physical such as inability to chew food, or cultural such as beliefs about foods. There may be more than one cause for the problem that a client has but the dietitian should be able to identify the basis of the problem using the information gained during the assessment process. For example, a client may have an incomplete knowledge of their gluten-free diet and this may be caused by: • Missing a dietetic appointment; • Not appreciating that all gluten-containing foods need to avoided; • A misconception that the diet was not important; and • A lack of awareness of the gluten content of many manufactured foods. It is also important that the aetiology identified in the PASS statement is one that the dietitian can influence because the aetiology forms the basis of the intervention. It may be difficult to identify the cause of the problem and in such circumstances the pragmatic approach may be to identify the contributing factors. Once identified, the aetiology may be linked to the problem using the phrase ‘related to’. Signs and symptoms Signs are the objective evidence that the problem exists; they may be from anthropometric measurements, biochemical or haematological results. Symptoms are subjective: they may be things that the patient/client has talked about such as tiredness, clothes being too tight or loose, difficulty swallowing and lack of understanding. Signs and symptoms gathered during the assessment process can be used to quantify the problem and indicate its severity. Signs and symptoms may be linked to the aetiology using the phrase ‘characterised by’. It is not necessary to have both signs and symptoms in the diagnostic statement; one or the other is adequate. Alternative diagnoses may be made when answering the questions in the case studies. It does not necessarily mean that your statement is incorrect; it may be a reasonable alternative or less of a priority. Check that your PASS statement describes a problem that can be altered by dietetic intervention and that the evidence collected during the assessment process suggests that it is important. The signs and symptoms should ideally be ones that can be measures to help advance the progress in alleviating the problem. 6 Dietetic and Nutrition Case Studies Nutrition intervention The nutrition intervention is the action taken by the dietitian to address the diagnosis. Ideally, the intervention should be aimed at the cause of the problem, the aetiology, but if this is not possible then the intervention should address the signs and symptoms of the problem. In some cases, the intervention may be to maintain a current situa- tion, for example, adult PKU. The intervention may involve the dietitian in delegating or co-ordinating the nutrition care done by others. The intervention has two stages: planning and implementation. For each PASS statement it is necessary to establish a goal based on the signs and symptoms (planning) and an appropriate interven- tion based on the aetiology (implementation). The intervention should of course be evidence based. Interventions may involve recommending, implementing, ordering, teaching or referring to other professionals. Planning Planning the intervention may involve collecting more information from the patient or from other sources. Planning should involve the patient/client/carer or group in agreeing and prioritising the necessary steps, to ensure that the care is patient centred. Implementation Implementing the intervention is the phase of the nutrition and dietetic care process, which involves taking action. The intervention may involve the dietitian in training someone else to take action, or in supporting the patient/client to make behavioural changes. The dietitian may facilitate change through others, for example a dietetic assistant, nurse, care assistant, carer or teacher. The implementation may be some- thing that is done to an unconscious patient such as the delivery of a prescribed total parenteral nutrition feeding regimen. Alternatively, the intervention may involve a community or group, for example a school meals project or lipid lowering group. Monitoring and review Monitoring focuses on changes in the signs and symptoms that were identified in the initial assessment to see if progress is being achieved and goals are met. The goals should be SMART: S – specific M – measurable A – achievable R – realistic T – timely SMART goals should make the monitoring process easier. Monitoring should be ongoing or carried out at planned intervals so that the results of the monitoring pro- cess can be used to review the intervention and modify it, if necessary. This may Model and process for nutrition and dietetic practice 7 involve a new assessment and a new nutrition and dietetic diagnosis, which will in turn lead to new goals and additional monitoring. Some of the case studies in this book involve more than one nutrition and dietetic diagnosis. Evaluation Evaluation takes place at the end of the process. It involves collecting data about the current situation and comparing it with data from the assessment, with a reference standard such as BMI indicators of obesity or HbA1c measures of diabetes, or with goals that were established early in the planning process. The effectiveness of the evaluation can be judged by changes in the signs and symptoms identified in the nutrition and dietetic diagnosis. The nutrition and dietetic care process may be an ongoing process where an indi- vidual patient is seen many times over a number of years for a chronic condition such as diabetes or it may be a short episode of care. References BDA (2012) Process and model for nutrition and dietetic practice. URL https://www.bda.uk.com/ professional/practice/process [accessed on 27 May 2015]. Gandy, J. (2014) Assessment of nutritional status. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. Lacey, K. & Pritchett, E. (2003) Nutrition care process and model: ADA adopts road map to quality care and outcomes management. J Am Diet Assoc, 103 (8), 1061–1072. Resource Qureshi, N. et al. (2014) Professional practice. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. CHAPTER 2 Nutrition care process terminology (NCPT) Pauline Douglas The challenges for the nutrition and dietetic practitioner are to prevent and reduce the burden of nutrition related health problems for individuals or groups of people. Dietitians and nutritionists must advance practice from experience based to evidence based and demonstrate quality practice and optimise nutritional outcomes. To do this they must have a common language that they can benchmark their practice with other dietitians. They must demonstrate practice through the acquisition and use of complex systems of communication. This allows them to convey meaningful infor- mation to others. In addition: • It provides supporting documentation for the reimbursement of dietetic services provided. • It engages dietitians from academia through to practice to provide a profession fit for purpose and competent to practice. With an increasing mobility of heath care professionals around the world the lan- guage needs to be standardised to convey meaningful information in a uniform way. This allows for the comparison of like messages in a logical process to facilitate the pro- duction of evidence-based practice. Also service users are travelling within countries and across borders for treatment and expect a consistent quality of care. Using standard terminology: • Promotes consistency and continuity of care; • Structures communication • Within and across professions; • Within and across nations; • Allows evaluation of the quality of care; • Facilitates research and building of a professional knowledge base (e.g. Practice-Based Evidence in Nutrition developed by Dietitians of Canada. There is now a PEN global dietetic partnership of associations of Australia, Canada, Ireland, New Zealand, South Africa and the UK, Evidence Analysis Library of Academy of Nutrition and Dietetics); • Facilitates professional development; and • Improves professional image, credibility, accountability of dietitians. Dietetic and Nutrition Case Studies, First Edition. Edited by Judy Lawrence, Pauline Douglas, and Joan Gandy. © 2016 John Wiley & Sons, Ltd. Published 2016 by John Wiley & Sons, Ltd. Companion Website: http://www.manualofdieteticpractice.com/ 8 Nutrition care process terminology (NCPT) 9 Why is standardised language important? It provides a common means of communication for healthcare professionals. Other healthcare professions, for example, nurses, physiotherapists, occupational therapists and so on have shown the benefits of having a standardised language. Making nurs- ing practice count (Beyea, 1999) ensures that when a nurse talks about a stage three pressure area, another nurse fully understands what the first nurse is describing. An example from dietetics is that there are differing definitions and understanding of what is meant by nutritional support. In some countries this relates to enteral and parenteral nutrition and in others this also includes food fortification and oral nutri- tional supplementation. A standardised language is complementary to a nutrition and dietetic process. It ensures that there is comparability in the terms used to describe diagnoses, interven- tions and outcomes of nutritional care. It is important to stress that this still ensures the dietitian provides individualised nutritional care for the patient or the population ensuring the patient/service user is at the centre of all care by taking into account their needs, values and culture. Dietitians do not work alone. They are integral members of the inter-professional health team. As such communication of their work needs to be accessible to other healthcare professionals, commissioners of service or those reimbursing them for their services. The World Health Organization uses the International Classification of Diseases (ICD) as the standard diagnostic tool for epidemiology, health manage- ment and clinical purposes. It is used to monitor the incidence and prevalence disease for general health and populations. Similarly the International Classification of Func- tioning, Disability and Health (ICF) is the WHO framework for measuring health and disability at both individual and population levels. In 2003 the Academy of Nutrition and Dietetics (AND) published the concepts of a nutrition care process and model. Other professional bodies have now modi- fied this to best meet the needs of their members and their healthcare provision, for example, BDA (2012). In 2008, AND defined the language to complement the pro- cess. This was called International Dietetic and Nutrition Terminology (IDNT) now known as the Nutrition Care Process Terminology (NCPT). In Europe, the Dutch Dietetic Association were also developing another dietetic language. This was mod- elled on the International Classification of Function (ICF) and is now recognised as the ICF – Dietetique. Now as the work of the National Dietetic Associations from across the world is being published, working groups are being established to facilitate international collaboration to further develop dietetic practice in this area. The International Health Terminology Standards Development Organization (IHTSDO) is a not for profit organisation based in Europe. This organisation owns and administers the rights to health terminologies and related standards includ- ing Systematised Nomenclature of Medicine – Clinical Terms (SNOMED – CT). SNOMED – CT is a comprehensive medical terminology incorporating several termi- nologies from various healthcare disciplines. While being of international scope it can be adapted to each countries requirements. This international dietetic working group has been working closely to incorporate NCPT as an integral element of SNOMED. 10 Dietetic and Nutrition Case Studies The WHO and IHTSDO have agreed to try to harmonise WHO classifications and SNOMED – CT terminologies to develop common terms used by both organisations. This has the potential to support further integration of different dietetic languages and thus enhance dietetic practice. In Europe a key priority is ‘to support Member States in developing common identification and authentication measures to facilitate transferability of data across border healthcare’ (Euro- pean Parliament and Council, 2011). As a result NCPT developments have facilitated eNCPT being available in several languages, for example, English, French, Italian, Spanish and Swedish again supporting international standards for dietetic practice and facilitating working across borders. Nutrition care process terminology The NCPT is used alongside the Nutrition and Dietetic Care Process. In the diagnosis the PASS statement (problem, aetiology, signs and symptoms) the problem is the change in nutrition state that is described by adjectives such as decreased/increased, excessive/inadequate, restricted and imbalanced. In addition nutrition and dietetic diagnosis terms fall into one of seven categories: • Energy balance; • Oral or nutritional support; • Nutrient intake; • Function, for example, swallowing; • Biochemical; • Weight; and • Behavioural/environmental. The descriptors used in the different countries can challenge the dietitian to define the problem in a way that their service users may find acceptable. The interested professional bodies are collaborating on this to gain appropriate, relevant country specific additions and alternatives. Dietetic professional bodies need to continue to work collaboratively to ensure deititians have a standardised language. It is important that the dietetic profession continue to engage with and use the NCPT. It should become an integral element of academic training, further developed within practice placement settings and then fully embraced by dietitians throughout their professional practice. Acknowledgements The Professional Practice Committee of the European Federation of Associations of Dietitians especially Constantina Papoutsakis, Ylva Orrevall, Lene Thorensen, Naomi Trostler, Remijnse Wineke and Claudia Bolleurs for their insight and knowledge. Nutrition care process terminology (NCPT) 11 References BDA (2012) Model and Process for Dietetic Practice. BDA, Birmingham. Beyea, S.C. (1999) Standardised language – making nursing practice count. AORN Journal, 70, 831–832, 834, 837–838. European Parliament and Council. (2011) Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011, on the application of patients’ rights in cross-border healthcare, Article 14, Official Journal of the European Union, L 88, 45. Resources AND Evidence Analysis Library. www.andeal.org. BDA Diagnosis Terms. www.bda.uk.com/professional/practice/terminology. Practice Based Evidence in Nutrition (PEN). www.pennutrition.com/index.aspx. CHAPTER 3 Record keeping Judy Lawrence In the UK the Health and Care Professions Council (HCPC) (2013) requires that dietitians ‘make reasoned decisions’ and ‘record the decisions and reasoning appropriately’ as part of their Standards of Proficiency. There is also a specific record keeping standard of proficiency; standard 10 which is ‘be able to maintain records appropriately’, this is expanded in points 10.1 and 10.2 which outline the need for records to be in line with relevant protocols, guidelines and legal requirements. This chapter discusses these guidelines and legal requirements. Dietitians from outside the UK should check with their own regulatory body and employer to ensure that their record keeping meets the required standard. Legislation In the UK there are a number of pieces of legislation that relate to records and record keeping. The Data Protection Act 1998 The Act relates to the protection of personal data (e.g. medical notes) about a liv- ing individual, such as data held by a public authority (e.g. NHS). This includes patient record cards kept by a dietitian, medical records to which a dietitian may contribute and electronic records. Data is said to be identifiable even if the informa- tion is recorded against a number that can then be matched to a person by accessing a different piece of information. The Act also regulates the processing of personal data. The term processing includes the storage, use, disclosure and the destruction of the data. The Act has six principles, they are that data should be processed fairly and lawfully, that data collected for a specific purpose or purposes should not be further processed for any purpose that is incompatible with the original purpose, that data collection should not be excessive in relation to the purpose, data should be accurate and where necessary up to date, data should not be kept for longer than is necessary and finally data should be processed in accordance with the rights of the individual. These principles may be subject to interpretation by an employer, and there will be Dietetic and Nutrition Case Studies, First Edition. Edited by Judy Lawrence, Pauline Douglas, and Joan Gandy. © 2016 John Wiley & Sons, Ltd. Published 2016 by John Wiley & Sons, Ltd. Companion Website: http://www.manualofdieteticpractice.com/ 12 Record keeping 13 local policies relating to them, for example a patient has the right to request access to information about themselves. A patient can ask to see what you have written during a consultation and comment on what has been written. If a patient or carer writes requesting to see the notes it is necessary to conform to local policy require- ments first, for example, an employer may require certain information as proof of identity from the patient or carer. All records are owned by the employing authority and requests for medical notes or electronic records should be dealt with by the clin- ical governance team. With regard to information being accurate, an opinion about a patient’s nutritional condition that you believe to be accurate but that the individ- ual disagrees with or believes to be inaccurate may be expressed. For example an anorexic patient may regard the statement that they are underweight as inaccurate. It is still legally possible to make this statement in their notes although a record that the patient disagrees with the assessment should be noted. The assessment should be backed by recording a weight and relevant BMI range. Freedom of Information Act 2000 The Freedom of Information Act covers information held by public bodies in England, Wales and Northern Ireland, information in Scotland is covered by Scotland’s 2002 Freedom of Information Act. The Freedom of Information Act is about removing unnecessary secrecy; it allows members of the public to request information from public authorities. The NHS and state schools are public authorities, but not all chari- ties that receive public money would necessarily be covered by the Act. The Act does not cover patient’s access to health records; this process is covered by the Data Protec- tion Act as discussed above. A dietitian employed by the NHS and working in private practice would only have to disclose information about their NHS work under the Act. The Act only covers information that is recorded, it is not necessary to write informa- tion down specifically to disclose it if it is not already recorded. Minutes of meetings and continuing professional development (CPD) portfolios are regarded as records. Private information on a work computer such as a private email does not have to be disclosed, but it would be necessary to disclose work related emails if requested. Organisations should have policies or guidelines in place to help employees comply with the Act. The Act does not interfere with copyright laws or intellectual property rights. Therefore someone can request copies of diet sheets that but they cannot use this information to produce copies if the work is subject to copyright. If a patient makes a request for information it is necessary to respond within 20 working days so it is important to contact the appropriate person in the organisation as soon as possible so that the request can be dealt with promptly. If a patient ver- bally asks for information they should be helped to put the request in writing and sent by post, email, a request on the organisation’s Facebook page or Twitter feed, to the appropriate person. Any information that can be shared easily such as clinic times or numbers of people working in a department should not be subject to formal procedures. The Data Protection Act may prohibit the release of data that has been requested; the clinical governance team or appropriate person, should be consulted for advice. Clinical records should only be released by a person specified to do so within the organisation. 14 Dietetic and Nutrition Case Studies Access to Health Records Act 1990 This Act gives people the right to request access to the health records of a deceased person. Guidelines There are a number of guidelines available. The NHS has an information gover- nance toolkit (https://www.igt.hscic.gov.uk/) that aims to help individuals and organisations to handle information properly. Each NHS organisation should have an individual appointed as a Caldicott Guardian, it is their responsibility to ensure that the organisation respects patient confidentiality and service user information. The BDA (2008) has guidance on record keeping although it is important to recognise that the nutrition and dietetic care process should guide the content of record keeping, for example, assessment, diagnosis, intervention and so on. The Royal College of Physicians (2013) has also produced record keeping standards covering electronic health records that have been endorsed by the BDA. The case studies in this book have questions about recording information and these guidelines may be helpful, but individual employer’s guidelines should be followed first. The introduction of electronic records should improve accuracy in health care records by improving legibility and access. The use of common language and SNOMED terms should also improve communication and understanding between the various health professionals using the health record. For more information about the nutrition and dietetic terms in SNOMED, see Chapter 2. Good record keeping should include the following points: • Records should be made at the time of the event or as near as possible to that time. • Records should be complete, accurate and fit for purpose. • A complete record should include details of an assessment, what care has been provided or is planned, and any action that has been taken or shared with other health professionals. • Handwriting on paper records should be legible and in black ink. • Records should be dated and signed with a name and designation. • Records should be clear, terms such as ‘ate well’ should be avoided. • Records should be relevant and opinions justified if possible. • Records should be in electronic format wherever possible. • Always log off an unattended computer. Social media Records can be in a variety of formats that includes social media, telephone messages and videos. The BDA (2013) and the Dietitians Association of Australia (2011) both have useful publications to help get the most out of social media whilst avoiding some of the pitfalls. In essence it is essential to think before posting and don’t make comments that would not be said a in person in a professional meeting. Don’t reveal Record keeping 15 information that could identify a patient or client either directly or indirectly and don’t repeat anything that is confidential. References BDA. (2008) Guidance for dietitians for records and record keeping. www.bda.uk.com/publications/ professional/record_keeping [accessed on 22 September 2015]. BDA. (2013) Professional guidance document. Making sense of social media. www.bda.uk.com/ professional/practice/professionalism/social_media [accessed on 22 September 2015]. Dietitians Association of Australia. (2011) Dialling into the digital age. Guidance on social media for DAA members. http://www.pennutrition.com/KnowledgePathway.aspx?kpid=3728& trid=22864&trcatid=33 [accessed on 8 October 2015]. Health and Care Professions Council (HCPC). (2013) Standards of proficiency. www.hpc- uk.org/assets/documents/1000050CStandards_of_Proficiency_Dietitians.pdf [accessed on 22 September 2015]. Royal College of Physicians. (2013) Standards for the clinical structure and content of patient records. https://www.rcplondon.ac.uk/resources/standards-clinical-structure-and-content-patient- records [accessed on 22 September 2015]. Resources Health and Social Care Information Centre Guide to confidentiality in health and social care. (2013) Treating confidential information with respect. http://www.hscic.gov.uk/media/12822/ Guide-to-confidentiality-in-health-and-social-care/pdf/HSCIC-guide-to-confidentiality.pdf [accessed on 22 September 2015]. Information Commission Office. The guide to data protection. https://ico.org.uk/for-organisations/ guide-to-data-protection/ [accessed on 22 September 2015]. Information Commission Office. The guide to freedom of information. https://ico.org.uk/media/ for-organisations/documents/1642/guide_to_freedom_of_information.pdf [accessed on 22 September 2015]. NHS England. (2014) Documents and record management policy. http://www.england.nhs.uk/wp- content/uploads/2014/02/rec-man-pol.pdf [accessed on 22 September 2015]. Qureshi, N. et al. (2014) Professional practice. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. CHAPTER 4 Assessment Joan Gandy Assessment is fundamental to dietetic and nutrition practice and an essential step in the nutrition and dietetic process (see Chapter 1). The BDA (2012) defined assess- ment as ‘ … a systematic process of collecting and interpreting information in order to make decisions about the nature and cause of nutrition related health issues that affect an individual, a group or a population’. It forms the basis of the nutrition and dietetic diagnosis and intervention and is key in establishing outcome measures in order to evaluate and monitor the intervention. The ABCDE format, as described by Gandy (2014) has been developed to structure and standardise dietetic and nutrition assessment. This format is used throughout this book and often summarised in a table. Table 4.1 gives details of the five domains used in this format. The information collected during assessment and the tools used to collect this information will vary depending on the setting, for example, individual, group, com- munity, and population. Domains Anthropometry, body composition and function Anthropometry is often used in nutrition and dietetic assessments with height and weight being used most frequently. Since the introduction of easily available equipment body composition and functional assessments, for example, bioelectri- cal impedance analysis (BIA) and dynamometry, are increasingly being used by dietitians and nutritionists in a variety of settings. Anthropometry Anthropometry is defined as the external measurement of the human body. It is affected by nutritional and health status and other factors including ethnicity, age and gender. Anthropometric measurements are often used in prediction equations, for example, body mass index (BMI), or compared with standards. It is essential that stan- dards that are appropriate to the age, ethnic or gender group be used. All equipment must be serviced regularly, for example, weighing scales, or replaced as appropriate Dietetic and Nutrition Case Studies, First Edition. Edited by Judy Lawrence, Pauline Douglas, and Joan Gandy. © 2016 John Wiley & Sons, Ltd. Published 2016 by John Wiley & Sons, Ltd. Companion Website: http://www.manualofdieteticpractice.com/ 16 Assessment 17 Table 4.1 Nutritional assessment domains. Domain Example procedure for individuals Anthropometry, body composition and Weight, height, body mass index, skinfold thickness, functional waist circumference Bioelectrical impedance analysis Biochemical and haematological Grip strength dynamometry Physical activity questionnaires Clinical Diet Vitamin status tests Environmental, behavioural and social Lipid status Iron status – haemoglobin, ferritin and so on Physical appearance, blood pressure, medication, indirect calorimetry 24 h recall, food frequency questionnaire (FFQ) Shopping habits, housing, cooking facilities, education Source: Gandy (2014), Table 2.2.1, p. 48. Reproduced with permission from Wiley Blackwell. for example tape measures will stretch over time. Anthropometry requires training and experience to produce reliable and reproducible results. It is essential to establish what, if any, standards are used within the local context, for example, NHS guidance. Body weight Weighing scales must be maintained and calibrated regularly and should be Class III or above. Body weight is affected by many factors including fluid retention (oedema, ascites), dehydration, accuracy of the scales, amputations, splints, casts and replace- ment joints. A weight adjustment table for amputations is shown in Appendix A5. If weight cannot be obtained self reported weight, estimated weight made by carers, relatives, dietitians or other health care professionals may be used. Specialist weigh- ing equipment, for example, weighing beds and chairs are available in some clinical settings, for example, spinal cord injury, obesity clinics. Height Height is usually measured using a stadiometer. When height cannot be measured, for example, bed bound patients, or is unreliable, for example, scoliosis it can be estimated using alternative methods such as ulna length, knee height or demispan (Appendix A5). Body mass index BMI is a weight for height indicator that may be used to classify overweight and obesity and is calculated as weight (kg)/height (m2). A ready reckoner and the WHO classifications of BMI for overweight and obesity are shown in Appendix A4. BMI does not give an indication of adipose distribution and therefore is being superseded as the preferred measure of non-communicable disease risk by waist circumference. It is affected by ethnicity, setting, age and body composition. If height is not available 18 Dietetic and Nutrition Case Studies in the elderly (over 64 years) demiquet or mindex can be used for men and women respectively (Appendix A4). Waist circumference Waist circumference assesses visceral adiposity and is therefore increasing used to assess obesity related morbidity risk. NICE (2006) recommend the use of both BMI and waist circumference to assess health risks. Appendix A5 shows the WHO waist circumference classifications for health risks (WHO, 2008). It is measured at the halfway point between the lowest rib and the iliac crest in the midaxillary line. Mid upper arm circumference When neither weight nor height can be measured, the BMI can be estimated using the mid upper arm circumference (MUAC), or mid arm circumference (MAC). Appendix A5 shows reference data derived from an American population; UK data is not available. Skinfold thickness Calipers are used to take skinfold measurements at specific sites to estimate per- centage body fat by substitution into prediction formulae, for example, Durnin & Womersley (1974). Triceps skinfold thickness (TSF) is used in bed bound patients to estimate endogenous fat stores (see Appendix A5). It can be combined with MUAC to evaluate body composition and is especially useful in patients with peripheral oedema or ascites Mid arm muscle circumference (MAMC) Mid arm muscle circumference (MAMC) is derived from TSF and MUAC as an indica- tor of muscle mass and therefore protein stores. The formulae used to derive MAMC and standards are shown in Appendix A5. Body composition Dietitians frequently use skinfold thicknesses to evaluate body composition however increasing other techniques such as BIA are being used. Functional assessment An example of this is hand grip strength (HGS) dynamometry (Appendix A5). Impaired HGS is associated with poor postoperative recovery (Griffiths & Clark, 1984) and related to loss of independence in the elderly. Increasingly dietitians assess physical activity levels; questionnaires are frequently used although other tools, for example, accelerometers are available. Biochemical and haematological markers Biochemical and haematological parameters are an important part of assessment and as outcome measures used in evaluation of the intervention. These markers are essen- tial when monitoring many clinical conditions, e.g. diabetes mellitus, renal disease and in assessing the status of some nutrients, for example, iron status in anaemia. Assessment 19 Appendix A7 gives examples of reference ranges for some parameters; it is essential to recognise that normal ranges and standards will vary between laboratories and that reference ranges from the local setting must be used. Clinical The clinical assessment will include physical appearance, medical history, test results and current medication; both prescribed and obtained without prescription. These details can usually be collated from the nursing or medical notes or family or carers. When collating information on medication it is important to consider drug nutrient interactions. The medical history and test results are vital elements of the assessment giving essential information for developing the intervention. Physical observations are vital indicators of nutritional status and should not be overlooked. For example loose clothing may indicate weight loss, breathlessness may indicate anaemia or other clinical conditions. Dietary assessment Establishing the extent to which nutritional needs are being met is core to the nutri- tion and dietetic assessment. It is usually important to assess current food and bever- age intake, changes (duration and severity) in appetite and factors that affect intake. In clinical situations may also be important to consider recent changes in meal pat- terns, food choice and consistency. The choice of dietary assessment method will depend on many factors including setting, population, age, literacy, assessor training and experience, cost, nutrients to be assessed, etc (Welch, 2014). An understanding of the limitations and applications of each method is essential in clinical and other settings to ensure the most appropri- ate method. Assessment can be either respective or current. Table 4.2 describes the characteristics of the most frequently used dietary assessment methods. It is impor- tant to quantify foods and drinks consumed either by weighing or estimations. Pho- tographs, models and standard size serving vessels may be used to aid quantification. Dietary data can be used qualitatively, for example, to assess food preferences or meal patterns however in clinical practice it is most frequently used quantitatively. The energy and nutrient content of the diet are calculated using food composition data. A software programme is most frequently used to facilitate these calculations. However an understanding of the limitations of food composition data is essential (Landais & Holdsworth, 2014). The results of any dietary assessment need to be interpreted in the context of the individual or population’s requirements. This is usually done by comparison with dietary reference values such as those published by the Department of Health (1991) and SACN (2011) or dietary recommendations (SACN, 2008) or the Institute of Medicine. However it is important to consider the limitations of any dietary reference value (Gandy, 2014). Environmental, behavioural and social assessment These factors can have a significant impact on nutritional status. Relevant factors include psychological status, for example, depression, ability to buy, prepare and cook 20 Dietetic and Nutrition Case Studies Table 4.2 Characteristics of dietary assessment methods. Method Advantages Limitations Retrospective methods Not reliant on long-term Single 24 HR can be used for group 24 h recall (24 HR) (single or memory; interview length assessments but not for estimating multiple days) 20–45 min intake of individuals Diet history Respondent literacy not required Report of past intake is influenced by Food frequency questionnaire current diet; trained interviewers (FFQ) (if portion estimates Useful for large sample sizes; required included termed semi relatively straightforward to quantitative FFQ) complete Need to be developed for specific population group to ensure important Short frequency questionnaires Targeted to specific food types, food items are covered and requires administration simpler and updating to accommodate changes to easier than long questionnaires supply of foods; responses governed by cognitive, numeric, and literacy abilities of respondents also by length and complexity of the food list Not easy to develop for clinical practice since specific computer programs need to be developed Need to be developed for specific population group to ensure questions are relevant Current methods No requirement for memory Literate, cooperative respondents Weighed food record (weighed retrieval as it records current required as burden is high; possible inventory technique) intake; food intake weighed so that respondents change usual eating estimates of quantity patterns to simplify the record; high Food record with estimated consumed not required data entry costs weights No requirement for memory retrieval as it records current Literate, cooperative respondents Duplicate analysis intake required as burden is high; possible that respondents change usual eating Records using electronic Greater accuracy patterns to simplify the record equipment, for example, mobile phones, digital cameras Visual records of foods. Avoids Very labour intensive; requires need for paper records. Data laboratory to do food composition can be sent to investigators analysis electronically Currently involves labour intensive programmes to convert to usable data, that is, quantities and types of foods, although systems are in development to deal with this; limited use in older people who experience difficulties with using newer technology Source: Gandy (2014), Table 2.3.1, p. 62. Reproduced with permission from Wiley Blackwell. Assessment 21 food and social factors religious and cultural beliefs, income, education and addiction, for example, alcoholism. References BDA (2012). Process and model for nutrition and dietetic practice. www.bda.uk.com/professional/ practice/process [accessed on 27 May 2015]. Department of Health (DH) (1991) Dietary reference values for food energy and nutrients for the United Kingdom. Report of the Panel on dietary reference values of the Committee on Medical Aspects of Food Policy. Report on Health and Social Subjects 41. HMSO, London. Durnin, J.V.G.A. & Womersley, J. (1974) Body fat assessed from total body density and its esti- mation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. British Journal of Nutrition, 32, 77–97. Gandy, J. (2014) Assessment of nutritional status. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. Griffith, C.D.M. & Clark, R.G. (1984) A comparison of the ’Sheffield’ prognostic index with forearm muscle dynamometry in patients from Sheffield undergoing major abdominal and urological surgery. Clinical Nutrition, 3, 147–151. Landais, E. & Holdsworth, M. (2014) Food composition tables and databases. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. National Institute for Health and Clinical Excellence (NICE) (2006) Obesity Guidance on the Pre- vention, Identification, Assessment and Management of Overweight and Obesity in Adults and Children. Clinical Guideline 43. NICE, London. Scientific Advisory Committee on Nutrition (2008) Dietary Reference Values for Energy TSO London. www.sacn.gov.uk [accessed on 25 September 2015]. Scientific Advisory Committee on Nutrition (2011) The nutritional wellbeing of the British popula- tion TSO London. www.sacn.gov.uk [accessed on 25 September 2015]. Welch, A. (2014) Dietary assessment. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. World Health Organization (2008) Waist circumference and waist–hip ratio. Report of a WHO expert consultation. www.who.int [last accessed 16 February 2013]. Resources Gandy, J. (2014) Assessment of nutritional status. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. Gandy, J. (2014) Dietary reference values. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. Gibson, R.S. (2005) Principles of Nutritional Assessment, 2nd edn. Oxford University Press, Oxford. Landais, E. & Holdsworth, M. (2014) Food composition tables and databases. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. PEN: Practice Based Evidence in Nutrition-Nutrition assessment. http://www.pennutrition.com/ KnowledgePathway.aspx?kpid=16177&trid=16444&trcatid=42 [accessed on 25 September 2015]. UK Food Databanks. http://www.ifr.ac.uk/fooddatabanks/nutrients.htm [accessed on 25 September 2015]. Welch, A. (2014) Dietary assessment. In: Gandy, J. (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. PART II CASE STUDY 1 Veganism Sandra Hood Wendy is 32 years old, a single mother with a 6-year-old daughter. She has a law degree and works part time in a legal practice. Wendy has recently changed from a vegetarian diet, which she followed for the previous 10 years, to a vegan diet. Wendy is very active, walking her daughter to and from school daily, which is 3 miles away, making a total of 12 miles a day. She also attends ballet classes once a week. At her own request, she has been referred by her GP, following a recent diagnosis of rheuma- toid arthritis (RA). Assessment Weight 43 kg Domain Height 1.49 m Anthropometry, body None composition and functional Biochemical and No medical history of note documented haematological markers Breakfast Clinical Banana (100 g) or avocado (145 g) Diet Lunch Salad sandwich (140 g) followed by dried fruit Environmental, behavioural (60 g) and sunflower seeds (15 g) and social Dinner (main meal) Wholemeal rice (180 g) or other grain with salad (250 g) or stir fried vegetables (180 g) Snacks – fresh fruit Drinks – water Prior to changing to a vegan diet, was very reliant on cheese Very active Dietetic and Nutrition Case Studies, First Edition. Edited by Judy Lawrence, Pauline Douglas, and Joan Gandy. © 2016 John Wiley & Sons, Ltd. Published 2016 by John Wiley & Sons, Ltd. Companion Website: http://www.manualofdieteticpractice.com/ 25 26 Dietetic and Nutrition Case Studies She suffered from anorexia when she was 16 years old but is in remission and managing well although she remains anxious about her weight. Questions 1. What is the definition of a vegan diet? 2. What other information do you need? 3. What is the nutrition and dietetic diagnosis? Write it as a PASS statement. 4. Which nutrients in particular should be considered when assessing a vegan diet? 5. What is Wendy’s body mass index (BMI), and is this cause for concern? 6. Wendy has been self-referred via her GP. Do you need to inform the GP of your discussions with Wendy? Further questions 7. Fish oil supplements rich in n − 3 PUFAs have been found to ameliorate pain and symptoms of RA (Goldberg & Katz, 2007). Are there any plant-based alternatives? 8. Wendy is considering a further pregnancy. What would be your concerns? 9. What are the ethical implications of accepting a referral from Wendy when your clinical service is overstretched? References Appleby, P., Roddam, A., Allen, N. et al. (2007) Comparative fracture risk in vegetarians and non-vegetarians in EPIC Oxford. European Journal of Clinical Nutrition, 61 (12), 1400–1406. Carter, J.P., Furman, T. & Hutcheson, H.R. (1987) Preeclampsia and reproductive performance in a community of vegans. Southern Medical Journal, 80 (6), 692–697. Craig, W.J. & Mangels, A.R. (2009) Position of the American Dietetic Association: vegetarian diets. Journal of the American Dietetic Association, 109 (7), 1266–1282. Crowe, F.L., Steur, M., Allen, N.E. et al. (2011) Plasma concentrations of 25-hydroxy vitamin D in meat eaters, fish eaters, vegetarians and vegans: results from the EPIC Oxford study. Public Health and Nutrition, 14 (2), 340–346. Davis, B.C. & Kris-Etherton, P.M. (2003) Achieving optimal essential fatty acid status in veg- etarians: current knowledge and practical implications. American Journal of Clinical Nutrition, 78 (Suppl. 3), 640S–646S. De Bortoli, M.C. & Cozzolino, S.M. (2009) Zinc and selenium nutritional status in vegetarians. Biological Trace Element Research, 127 (3), 228–233. Erdeve, O., Arsan, S., Atasay, B. et al. (2009) A breast-fed newborn with megaloblastic anaemia- treated with vitamin B12 supplementation of the mother. Journal of Pediatric Hematology and Oncology, 31 (10), 763–765. Gibson, R.S. (1994) Content and bioavailability of trace elements in vegetarian diets. American Journal of Clinical Nutrition, 59 (Suppl. 5), 1223S–1232S. Goldberg, R.J. & Katz, J. (2007) A meta-analysis of the analgesic effects of omega-3 polyunsat- urated fatty acid supplementation for inflammatory joint pain. Pain, 129, 210–223. Institute of Medicine, Food and Nutrition Board (2001) Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc. National Academy Press, Washington, DC. Veganism 27 Kniskern, M.A. & Johnston, C.S. (2011) Protein dietary reference intakes may be inadequate for vegetarians if low amounts of animal protein are consumed. Nutrition, 27 (6), 727–730. Kornsteiner, M., Singer, I. & Elmadfa, I. (2008) Very low n − 3 long chain polyunsaturated fatty acid status in Austrian vegetarians and vegans. Annals of Nutrition and Metabolism, 52 (1), 37–47. Leung, A.M., Lamar, A., He, X. et al. (2011) Iodine status and thyroid function of Boston-area vegetarians and vegans. Journal of Clinical Endocrinology and Metabolism, 96 (8), E1303–E1307. Mangels, R., Messina, V. & Messina, M. (2010) The Dietitian’s Guide to Vegetarian Diets, 3rd edn. Jones and Bartlett, Sudbury, MA, pp. 530–535. Mariani, A., Chalies, S., Jeziorski, E. et al. (2009) Consequences of exclusive breast feeding in vegan mother newborn – case report. Archives of Pediatrics, 16 (11), 1461–1463. Mathey, C., Di Marco, N., Poujol, A. et al. (2007) Failure to thrive and psychomotor regression revealing vitamin B12 deficiency in 3 infants. Archives of Pediatrics, 14 (5), 467–471. Outilia, T.A., Karkkainen, M.U., Seppanen, R.H. et al. (2000) Dietary intake of vita- min D in premenopausal healthy vegans was insufficient to maintain concentrations of 25-hydroxyvitamin D and intact parathyroid hormone within normal ranges during the win- ter in Finland. Journal of the American Dietetic Association, 100 (4), 434–441. Roed, C., Skovby, F. & Lund, A.M. (2009) Severe vitamin B12 deficiency in infants breastfed by vegans. Ugeskr Laeger, 171 (43), 3099–3101. Rosell, M.S., Lloyd-Wright, Z., Appleby, P.N. et al. (2005) Long chain n − 3 polyunsaturated fatty acids in plasma in British meat-eating, vegetarian and vegan men. American Journal of Clinical Nutrition, 82 (2), 327–334. Sanders, T.A. (2009) DHA status of vegetarians. Prostaglandins, Leukotrienes and Essential Fatty Acids, 81 (2–3), 137–141. Simpoulous, A.P. (2009) Omega-6/omega-3 essential fatty acids: biological effects. In: A.P. Sim- poulous & N.G. Bazan (eds) Omega-3 fatty acids the brain and retina. World Review of Nutrition and Dietetics, 99, 1–16. Smolka, V., Bekarek, V., Hlidova, E. et al. (2001) Metabolic complications and neurologic mani- festations of vitamin B12 deficiency in children of vegetarian mothers. Journal of Czech Physi- cians, 140 (23), 732–735. Weiss, R., Fogelman, Y. & Bennett, M. (2004) Severe vitamin B12 deficiency in an infant asso- ciated with a maternal deficiency and a strict vegetarian diet. Journal of Pediatric Hematolgy and Oncology, 26 (4), 270–271. Welch, A.A., Shakya-Shrestha, S., Lentjes, M.A. et al. (2010) Dietary intake and status of n − 3 polyunsaturated fatty acids in a population of fish-eating and non-fish-eating meat-eaters, vegetarians and vegans and the product-precursor ratio [corrected] of alpha-linolenic acid to long-chain polyunsaturated fatty acids: results from the EPIC-Norfolk cohort. American Journal of Clinical Nutrition, 92 (5), 1040–1051. Resources Gardener, E. (2014) Vegetarianism and vegan diets. In: J. Gandy (ed), Manual of Dietetic Practice, 5th edn. Wiley Blackwell, Oxford. PEN: Practice Based Evidence in Nutrition. Do individuals with rheumatoid arthritis who follow a vegan diet have improvement in their arthritic symptoms compared to individuals with rheumatoid arthritis who follow a non-vegetarian diet?. http://www.pennutrition.com/KnowledgePathway .aspx?kpid=978&pqcatid=146&pqid=7876. CASE STUDY 2 Older person – ethical dilemma Nicola Howle∗ Rose is currently an inpatient at the mental health hospital; she is 93 years old. Her only family is her sister, who she lived with prior to admission. She often appears confused and has limited engagement in conversations. Rose is bedbound and hoisted for all transfers. She has been in hospital for 4 months; she was originally admitted to the acute hospital following a fall at home and was treated in the elderly assessment ward for a urinary tract infection. She was then discharged to a community hospital for assessment of her care needs and rehabilitation. During this time she refused to eat and drink, and underwent a period of naso-gastric (NG) feeding. She pulled the NG tube out twice and continued to refuse to eat and drink. The ward doctors felt she was depressed, so Rose was admitted to an older peoples assessment ward at the mental health hospital. At this time she was referred to the dietetic service for urgent provision of an NG feeding regimen to help build her up prior to commencing electroconvulsive therapy (ECT). On attending the ward, the doctor and nursing staff are very concerned about Rose. She has been assessed by a second opinion doctor who states that Rose is unlikely to survive ECT. The ward staff are unconvinced that she is depressed as Rose has lim- ited communication and they are unable to complete the assessments for depression. The ward staff and doctor feel that she is at the end of her life and should be kept comfortable. However, the consultant has asked for NG feeding for 2 weeks and to go ahead with ECT later that week. IV fluids have been prescribed as her oral intake is very poor. ∗On behalf of the BDA Older People Specialist Group. Dietetic and Nutrition Case Studies, First Edition. Edited by Judy Lawrence, Pauline Douglas, and Joan Gandy. © 2016 John Wiley & Sons, Ltd. Published 2016 by John Wiley & Sons, Ltd. Companion Website: http://www.manualofdieteticpractice.com/ 28

Perpustakaan PIM
Related publications.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.7(4); 2016 Jul
Creating the Future of Evidence-Based Nutrition Recommendations: Case Studies from Lipid Research 1, 2, 3
Johanna t dwyer.
4 Tufts Medical Center, Schools of Medicine and Nutrition Science and Policy, and Jean Mayer USDA Human Nutrition Research Center on Aging at Tufts University, Boston, MA;
Kristin H Rubin
5 Kraft Heinz Company, Glenview, IL;
Kevin L Fritsche
6 University of Missouri, Columbia, MO;
Tricia L Psota
7 USDA Center for Nutrition and Policy Promotion, Alexandria, VA;
DeAnn J Liska
8 Biofortis Research, Addison, IL;
William S Harris
9 OmegaQuant Analytics, LLC, Sioux Falls, SD;
10 University of South Dakota School of Medicine, Sioux Falls, SD;
Scott J Montain
11 United States Army Research Institute of Environmental Medicine, Natick, MA; and
Barbara J Lyle
12 School of Professional Studies, Northwestern University, Evanston, IL and North American Branch of the International Life Sciences Institute, Washington, DC
Strategic translational research is designed to address research gaps that answer specific guidance questions. It provides translational value with respect to nutrition guidance and regulatory and public policy. The relevance and the quality of evidence both matter in translational research. For example, design decisions regarding population, intervention, comparator, and outcome criteria affect whether or not high-quality studies are considered relevant to specific guidance questions and are therefore included as evidence within the context of systematic review frameworks used by authoritative food and health organizations. The process used in systematic reviews, developed by the USDA for its Nutrition Evidence Library, is described. An eating pattern and cardiovascular disease (CVD) evidence review is provided as an example, and factors that differentiated the studies considered relevant and included in that evidence base from those that were excluded are noted. Case studies on ω-3 (n–3) fatty acids (FAs) and industrial trans -FAs illustrate key factors vital to relevance and translational impact, including choice of a relevant population (e.g., healthy, at risk, or diseased subjects; general population or high-performance soldiers); dose and form of the intervention (e.g., food or supplement); use of relevant comparators (e.g., technically feasible and realistic); and measures for both exposure and outcomes (e.g., inflammatory markers or CVD endpoints). Specific recommendations are provided to help increase the impact of nutrition research on future dietary guidance, policy, and regulatory issues, particularly in the area of lipids.
Strategic Research Is Needed to Strengthen Future Nutrition Guidance
The intended targets of scientific research vary. Basic research focuses on fundamental knowledge and mechanisms of action or effects. In contrast, translational policy research focuses on guidance, recommendations, education, and improving program operations ( 1 ). Strategic research addresses the current situation in which “little is done to systematically link scholarship to policy” ( 2 ). Fortunately, many tools are available to help scientists link their scholarship to nutrition guidance, regulatory, and public policy.
Systematic evidence reviews play an instrumental role in the formation of nutrition guidance, recommendations, and policy decisions. Even high-quality research studies are excluded from systematic evidence reviews if they are not directly relevant to an important guidance or policy question; if they do not test a population, intervention, comparator, or outcome (PICO) 13 highly relevant to the specific question; or if essential information on them is lacking in the publication. This article provides insights with respect to these key factors by using, as an example, the evidence review on eating patterns and cardiovascular disease (CVD) from the USDA’s Nutrition Evidence Library (NEL) evidence review process for informing Dietary Guidelines Advisory Committees (DGACs). In addition, case studies focused on ω-3 FAs and industrial trans -FAs (iTFAs) highlight important issues related to research for addressing inconsistencies in conducting and reporting lipid studies, meeting evidence review criteria, and translating the research into guidance.
Key Steps in Strategic Research to Have an Impact
For research to have a substantial impact on guidance and policy, it must address a relevant question(s) and be designed, conducted, and reported with the necessary content to meet the screening criteria used in systematic evidence reviews. Although each authoritative body may follow unique systematic review criteria, they all share key elements related to relevance and quality.
Identify and test a question relevant to a specific policy or guidance gap
The first step is to identify a key research question that is relevant to a gap in dietary guidance or nutrition policy or guidance. In the Dietary Guidelines for Americans development process, each federal advisory committee not only summarizes evidence on diet and health, but also provides its recommendations on where future research should focus to inform future guideline committee decisions ( 3 ). For those who are performing research for supporting a claim about food or food components, the research should address questions specifically posed by the regulatory agency, such as the US FDA or the European Food Safety Administration (EFSA).
Consider systematic evidence-based review criteria throughout research design and conduct and in reporting results
Systematic reviews and the criteria they use are particularly important in developing food and nutrition policy and guidance. They are the basis for decision making by credible authoritative groups, including virtually all high-impact journals, as well as the FDA, EFSA, DGAC, the Academy of Medicine/Institute of Medicine, the American Heart Association, and others. For example, the USDA’s NEL includes over 130 systematic reviews, of which >100 were guided by the 2010 and 2015 DGACs. In the regulatory arena, the FDA has systematically reviewed evidence for ≥100 potential health claims, and the EFSA carried out ∼500 reviews, including both health and structure-function claims.
Attention to key criteria used by authoritative bodies when screening papers for policy and guidance decisions will maximize the likelihood of the scientist’s research being included in the review process. These include both PICO criteria and quality judgment criteria. Key elements of systematic review frameworks used by several authoritative bodies are listed in Table 1 .
Organization-specific systematic review frameworks
| Organization | Evidence review framework | Evidence informs | Web links |
| US Department of Health and Human Services, FDA Center for Food Safety and Applied Nutrition | Evidence-based review system for the scientific evaluation of health claims | Food label claims, e.g., health claims and qualified health claims | |
| Preconsultation dialogue available on request | |||
| USDA | Nutrition Evidence Library | Dietary Guidelines for Americans | |
| WHO | Multiple sources of evidence reviews (WHO, Cochrane, and high-quality studies published in peer-reviewed journals); totality of evidence assessed by use of Grading of Recommendations Assessment, Development and Evaluation | Global Nutrition Guidelines | |
| National Heart Lung and Blood Institute | Appointed expert panel | Clinical Practice Guidelines (e.g., Clinical Guidelines on Cholesterol Management in Adults) |
PICO criteria
The test population is an important and underappreciated variable in the PICO screening process that can affect whether results are considered relevant evidence with respect to specific guidance or policy decisions. Research conducted among high-risk or diseased subjects/populations would likely be of low or no relevance in an evidence review intended to inform decision making for the healthy population (e.g., health claims intended for food consumed by the general public). In the context of lipid research, conducting a study with hypercholesterolemic subjects will limit the study’s relevance for informing policy intended for generally healthy populations. Similarly, studies reporting findings on sedentary populations that spend most of their time indoors is probably insufficient for questions specific to subgroups, like military personnel who are very physically active and who often operate in extreme environmental situations. With respect to the intervention tested and comparator control, both must be relevant and have practical application to a specific policy or guidance. Intervention form (such as ω-3 FA in food compared with in supplement or drug), intake level (e.g., testing in the range of typical trans -FA intakes), and other factors related to the intervention and relevant comparison affect whether results translate to the specific question needed to develop policy and guidance.
Finally, to meet PICO criteria, the outcomes tested must include a validated health outcome or biomarker of health that is accepted by the specific organization or entity developing policy or guidance. Health outcomes, such as incidence of disease, are often considered the strongest evidence. Surrogate biomarkers (such as blood total or LDL cholesterol) are sometimes deemed to be acceptable, depending on the decision-making organization’s determination of their validity. The paucity of accepted validated biomarkers, such as inflammatory markers, is a shortcoming. More attention to the validation process and studies is needed if markers with substantial evidence for dietary influence are to become accepted surrogate outcomes by authoritative groups making policy and guidance decisions.
Quality criteria
Systematic review methods use quality criteria to determine whether evidence from a specific study is included and, if so, the strength of that study’s evidence. In evaluating the quality of each study, trained reviewers and decision makers give low quality grades or exclude studies with limitations in design and execution, inconsistency, indirectness (lack of applicability), poor description of PICO in the methods section, and imprecision (determined by number of events and confidence intervals). Although several approaches are currently in use to determine the quality of evidence in various systematic evidence review frameworks, the principles are similar ( Table 2 ). For example, randomized double-blinded clinical trials are usually considered stronger evidence than observational studies for establishing causal inference, because of less potential bias and confounding. For randomized clinical trials, a clear description of randomization procedures in the methods section of a publication is needed if it is to be scored as high quality.
Compilation of systematic review criteria and evidence grading standards 1
| Suggested factors | Low/limited evidence | Moderate evidence | Strong evidence |
| Factors for assessing individual studies | |||
| Design strength and validity | Extensive limitations of the design | Minor design limitations or uncertainties | Design/implementation of high quality: feasible intervention; appropriate control group; valid duration and measurement of outcome; appropriate statistical analysis used and adequately described |
| Risk of bias | Substantial risk of bias | Some presence or potential for risk of bias | Methods are described in detail to disclose that bias is minimized: comparable groups are randomly generated; design includes allocation concealment and blinding; measures of compliance are included; missing data are treated appropriately; outcomes are prespecified or justified |
| • Selection | |||
| • Performance detection | |||
| • Attrition | |||
| • Reporting | |||
| Impact | Most studied outcomes relate to the question indirectly; effect is small, uncertain, or lacks clinical significance; low confidence that the evidence reflects the true effect, likely to change with future research | Some indirectness of outcomes; doubt about the clinical significance of the effect; moderate confidence that the evidence reflects the true effect but may be changed by further research | Outcomes (validated surrogate endpoints/biomarkers) relate directly to the research question; size of effect is clinically relevant and statistically significant; high confidence that the evidence reflects the true effect; further research very unlikely to change the estimate of effect |
| Generalizability | Results are likely not generalizable; narrow study population | Some doubt about generalizability | Study subjects adequately represent the population of interest |
| Factors considering the totality of evidence across studies | |||
| Consistency | Unexplained inconsistency among results; not similar in direction or size of effect | Minor inconsistency among results in direction and size/significance of effect or degree of association that weaken confidence in relation | Consistent findings in direction and size/significance of effect and degree of association (very minor exceptions) |
| Quantity | Limited number of studies and subjects (inadequate sample size) | Moderate number of studies; some variety in investigators; doubts about adequacy of sample size to avoid type I and II errors | Large number of studies and subjects (sufficient for adequate statistical power); multiple investigators |
Tools available to help researchers not only design, but also carefully report their studies with quality criteria in mind include the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) criteria for observational studies and CONSORT (Consolidated Standards of Reporting Trials) or Jadad scales for randomized clinical trials ( 4 – 6 ). PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) is intended to help authors improve the reporting of systematic reviews and may also be useful for critical appraisal of published systematic reviews ( 7 ). GRADE (Grading of Recommendations, Assessment, Development and Evaluation) considers factors necessary to have confidence in evidence review results, i.e., the quality and totality of evidence, as well as the magnitude of the effect ( 8 ).
How Evidence Reviews Were Conducted to Inform Dietary Guidelines for Americans
The NEL is comprised of systematic reviews developed within the USDA Center for Nutrition Policy and Promotion by use of a defined methodology to objectively review, evaluate, and synthesize research to answer important diet-related questions that inform federal nutrition policy and programs. The methodology to generate NEL reviews was designed to minimize bias, maximize transparency, and ensure the systematic reviews are relevant, timely, and high quality. USDA nutrition scientists use a scientifically rigorous and transparent 6-step process to review, assess, and synthesize available food and nutrition evidence to answer specific nutrition guidance gaps. Initially, a multidisciplinary research team develops a systematic review question using a PICO framework. They then search, screen, and select studies for consideration, after which they extract data and assess the risk of bias in the body of research evidence included in the analysis. Evidence is described and synthesized to develop evidence-based graded conclusion statements before making future research recommendations. To ensure objectivity, transparency, and reproducibility, each step of the process is documented in detail, and results are made available via www.NEL.gov .
Beginning in 2010 and again in 2015, the DGAC used NEL systematic reviews as a source of evidence to guide their recommendations to the USDA and the US Department of Health and Human Services on the state of science related to the Dietary Guidelines for Americans . An NEL systematic review of dietary patterns and CVD is used here to highlight critical components in each step of the NEL process and particularly the criteria used to select, evaluate, and grade the body of evidence ( 9 ). This particular evidence review is an example of how 55 research studies met the inclusion criteria such that a strong and consistent body of evidence informed dietary guidance. In using the PICO framework, the question for this review was stated as: “What is the relation between adherence to dietary guidelines/recommendations or specific dietary patterns, assessed by using an index or score, and the risk of cardiovascular disease?” The relevant population from which the evidence would be gathered was constrained to the general population aged ≥2 y in the United States or other countries with a high or very high human development index ( 10 ) who were considered healthy or at elevated chronic disease risk. Intervention exposures were defined by adherence to a dietary pattern determined by using an a priori numeric scoring system (e.g., Healthy Eating Index, Mediterranean Diet Score). The comparator was defined as low adherence to the dietary pattern or to a different dietary pattern. The evidence review considered both specific intermediary markers (i.e., triglycerides, LDL cholesterol, HDL cholesterol, hypertension, or blood pressure) and specific clinical endpoint outcomes (i.e., incidence of CVD, CVD-related deaths, myocardial infarction, or stroke). Inclusion/exclusion criteria were developed by use of these PICO criteria and standards of quality indicating study conduct and reporting. In addition, inclusions were restricted to studies published in peer-reviewed journals and, if they were controlled trials, with ≥30 participants/arm and 80% or more of the subjects completing the study.
Data from all studies meeting inclusion criteria were carefully extracted and rigorously assessed for bias and given a study-by-study quality score. Finally, the quality of the totality of evidence was graded by expert groups based on risk of bias, quantity of studies, and relevance of the subject population. The final result, as it is for all NEL reviews, was a clearly stated answer to the original question and a grade for the body of evidence. In this case, the evidence review concluded: “There is strong and consistent evidence that in healthy adults increased adherence to dietary patterns scoring high in fruits, vegetables, whole grains, nuts, legumes, unsaturated oils, low-fat dairy, poultry and fish; low in red and processed meat, high-fat dairy, and added sugars; and moderate in alcohol is associated with decreased risk of fatal and non-fatal cardiovascular diseases, including coronary heart disease and stroke (Grade I: Strong)” ( 9 ).
Understanding this review process is critical for nutrition researchers to design and report study findings that can be included in NEL systematic reviews and subsequently have a greater impact on nutrition guidance and policy. Experience to date indicates that 2 ways researchers can enhance the collective body of nutrition evidence used in dietary guidance decision-making are to minimize study bias by using valid and reliable measures consistently across all study groups and to describe study exposures in detail (e.g., dietary patterns, food components, foods, and/or nutrients) when reporting study findings. Researchers can use the gaps in the literature identified and research recommendations provided in NEL systematic reviews to inform future investigations with a high relevance to nutrition and dietary guidance.
Case Study: Use of Inflammatory Biomarkers in Developing Dietary Guidance for Fats in the Future
Current dietary advice for Americans on fats and FAs focuses on caloric intake (e.g., food sources supplying energy in excess of needs), the impact of specific fats and FAs on CVD risk (as assessed by CVD morbidity and mortality), and 3 biomarkers (i.e., total and LDL cholesterol and triglycerides). A growing body of evidence suggests that future dietary guidance for fats might be improved by broadening relevant health outcome measures to include biomarkers of inflammation ( 11 – 16 ). Several researchers and policy-making groups consider C-reactive protein (CRP), a widely used biomarker for tissue injury and inflammation, to be a useful biomarker for CVD risk ( 14 , 17 – 20 ). In addition, there is a growing body of research supporting the utility of CRP use in risk assessment for diabetes, metabolic syndrome, and morbidity and mortality of the elderly ( 21 ). The complexity of the inflammatory process, however, suggests that no single biomarker is likely to be valid under all circumstances ( 22 – 24 ). Nutrition-related human clinical trials should include measures of as many biomarkers of inflammation as possible. However, the suitability of some commonly measured biomarkers of inflammation (e.g., TNFα, IL-6) has not been adequately justified for nutrition studies with relatively healthy populations. The transient nature of their production, short half-life, and limitations in assay sensitivity collectively make gathering and interpreting data for normal healthy subjects problematic for some inflammatory biomarkers. In nutrition, and other health-related fields, there is also an urgent need to monitor the functional immune response and inflammation in a reliable and reproducible manner. In a 2014 report, Duffy et al. ( 25 ) described a newly developed whole-blood, syringe-based ex vivo immune stimulation assay system that measures dozens of inflammatory indicators in a clinically relevant context. Such an assay system could prove invaluable for monitoring the inflammatory status of human subjects; however, current high costs may limit widespread adoption.
Evidence from observational studies and clinical trials suggests that consuming diets high in trans -unsaturated FAs (TFAs) elevates low-grade inflammation ( 26 ). In contrast, the impact of other types of fats, including those rich in SFAs, MUFAs, or PUFAs on systemic inflammation, is uncertain ( 27 ). Diets rich in ω-6 PUFAs are believed to promote inflammation in part by increasing tissue arachidonic acid, a precursor to a variety of potent pro-inflammatory mediators. A 2012 systematic review of 15 randomized clinical trials, however, reported that diets rich in linoleic acid (an ω-6 PUFA) do not promote inflammation in healthy people ( 28 ). On the other hand, when ω-6 PUFAs were substituted for sugars, SFAs, or TFAs, they reduced inflammation. Results published recently from a relatively large, well-designed, prospective study showed that higher ω-6 PUFA intake in free-living adults was inversely related to CRP (4th quartile compared with 1st: β = −0.09, 95% confidence interval: −0.16, −0.01) with lower circulating CRP levels ( 29 ). Consuming a diet rich in ω-3 PUFAs has also been reported to have anti-inflammatory actions in humans, although the benefits tend to be modest, and the results tend to be inconsistent ( 30 , 31 ). A recent report from the Framingham Offspring study found that levels of 8 different biomarkers of inflammation were significantly and inversely associated with red blood cell EPA and DHA levels ( 32 ). The recent discovery of novel classes of lipid mediators derived from ω-3 and ω-6 PUFAs with inflammation-modulating activities has only just begun to be taken into account in nutrition clinical trials ( 33 ). Adopting more comprehensive FA metabolite analyses (i.e., lipidomics) is an important step in validating whether and how ω-6 and ω-3 PUFAs affect chronic inflammation in humans ( 34 , 35 ).
Finally, in addition to fats, it appears that many dietary constituents (e.g., sugars, vitamins, minerals, phytochemicals) and lifestyle factors (e.g., age, smoking, exercise) cause low-grade inflammation ( 11 , 15 , 36 ). Therefore, adopting inflammation biomarkers in future policy-making and dietary guidance recommendations will require that researchers use careful experimental design, coupled with rigorous statistical analyses ( 13 , 19 , 22 – 24 ). Importantly, such studies must be adequately powered so that covariants believed to affect the expression of inflammatory biomarkers (e.g., obesity, aging, smoking, anti-oxidant and pro-oxidant dietary constituents/nutrients) could be appropriately accounted for.
Case Study: Partially Hydrogenated Oils for Regulatory Decisions
The conduct and translation of research related to iTFAs and CVD illustrates the importance of testing relevant interventions (e.g., with respect to exposure level) against realistic comparators. A linear dose-response relation between iTFA intake and LDL cholesterol has been shown clinically for iTFA intakes >3% of total daily energy ( 37 – 41 ). Current US government recommendations call for limiting iTFA intakes, although the specific goals range from “<1% of total daily energy” to “as low as possible” ( 42 – 44 ). These recommendations are mainly based on data extrapolated from higher intake levels, with the assumption that a consistent linear relation exists throughout all iTFA exposure levels.
Dietary TFA is obtained from both ruminant sources and industrial oils (iTFAs), with a majority of iTFAs from partially hydrogenated oils (PHOs). Because of the relation with LDL cholesterol, the US FDA mandated labeling the amount of TFAs on processed food products in 2006. Subsequently, as food manufacturers reduced iTFAs to <0.5 g/serving in many foods (which rounds to 0 g on the label), mean iTFAs intake decreased from an estimated 4.6 g · person -1 · d -1 in 2003 to 1.0 g · person -1 · d -1 (∼0.5% of total daily energy) in 2012 ( 45 , 46 ). Although average dietary iTFA intakes are currently below recommended levels, FDA published a notice in June 2015 revoking the GRAS status of PHOs ( 46 ). The evidence base FDA used to determine safety assumes that any level of intake for iTFAs increases an individual’s risk of coronary heart disease in a linear fashion. Specifically, the FDA notice concluded: “there is no longer a consensus among qualified scientific experts that PHOs, the primary dietary source of industrially-produced trans -FAs, are safe under any condition of use in food.” This determination requires that manufacturers must submit food additive petitions in order to demonstrate safety and gain FDA approval for specific PHO levels and uses in food in the future.
With respect to testing relevant exposure levels, the question is whether iTFA consumption affects LDL cholesterol at the low-intake levels coinciding with current mean intakes. Linear regressions assess the “change” in LDL cholesterol associated with a change in iTFAs over a background intake level or to a comparator group intake. However, most often the comparator group’s baseline iTFA intakes are similar to current consumption levels, and therefore, these studies measure effects of levels above actual current intakes. Research is very limited on the effect of iTFAs on LDL cholesterol in the range of iTFA intakes representing current consumption patterns, presumably because conducting the large-scale trials needed to achieve statistical power at these low levels of intake is very costly.
The relation between LDL cholesterol and iTFAs at low intakes is unclear, and a clinically meaningful change may not occur until a threshold is reached. Clinical data below 3% of total daily energy intakes are limited, and the heterogeneity in study designs confounds interpretation of the data. In order to strengthen the evidence base and provide results that translate to dietary recommendations, standards for reporting intake units of iTFAs should be established. In addition, studies should define whether an iTFA-rich oil intervention is produced from a partial hydrogenation process. The FDA GRAS restriction is related to PHOs use in foods and not on TFAs in general. However, the majority of published data does not report processing details needed to distinguish the sources and types of trans -fats (iTFAs and ruminant trans -FAs), despite presumed differing biologic responses. Therefore, more details on test oil preparation, and specifically the inclusion of a partial hydrogenation process, is necessary for research to be translatable with respect to FDA status determination.
Realistic composition of comparators also requires particular attention. Studies characteristically replace iTFAs with a caloric component (primarily cis -MUFAs) that has been shown to attenuate LDL cholesterol. This substitution is unrealistic from a food functionality perspective and therefore not relevant for translating into recommendations. The choice of suitable lipid substitutions (in consultation with experts aware of current food industry practices) for iTFAs is a critical factor in translating results to real-life scenarios. For guidance and policy, studies need to test iTFAs relative to suitable alternatives for replacing PHO in the food supply and at exposure levels that reflect realistic intakes representative of current consumption patterns by the US population.
Case Study: Research Informing Dietary Guidance on ω-3 Fatty Acids
The relation between ω-3 FAs and CVD risk was graded in an NEL evidence review as “limited” to “moderate” (depending on source for ω-3 FAs) for consideration by the 2010 DGAC ( 47 ). A considerable volume of data has accumulated since 2010 on this question, yet the situation in 2015 is even less clear than previously. An updated systematic review of the evidence is currently underway by the Agency for Healthcare Research and Quality. Studies designed to test EPA and DHA as drugs, rather than nutrients, contribute to this problem because they are short-duration interventions started late in life rather than long duration food consumption studies over a lifetime ( 48 ). In addition, there is uncertainty regarding unmeasured confounding in observational studies. Efficacy depends on many PICO factors, including dose, duration of treatment, EPA/DHA balance, timing of supplement consumption, subject/patient type, use of composite endpoints, background drugs, and the dietary intake of not only EPA and DHA but also other ω-3 (and possibly ω-6) FAs as well.
Between 2009 and 2012, 9 meta-analyses reported varying conclusions ( 49 ), with the diverse findings likely being attributable to multiple issues such as the following: relatively low doses of EPA and DHA (840 mg/d or less) ( 50 – 53 ) that do not achieve cardioprotective blood levels of EPA and DHA [which requires >1500 mg/d ( 54 )], treatments lasting only 1–5 y, use of ethyl ester forms that are poorly absorbed when taken without food ( 55 ), and including subjects with established disease who are also taking multiple background drugs and who are often consuming dietary ω-3 FAs near protective levels in both treatment and control groups. Moreover, composite endpoints (e.g., combining fatal and nonfatal myocardial infarction or stroke, hospitalization for angina, etc.) can hide the effects of EPA and DHA that affect one but not other outcomes ( 56 ). Several of these factors conspire to reduce overall event rates, leaving studies underpowered to detect an effect of the intervention ( 57 ). The future of dietary guidance on ω-3 FAs depends on research that consistently overcomes limitations related to population, intervention, comparator, and outcome limitations.
None of the major ω-3 FA randomized clinical trials used a biomarker of low EPA and DHA status in subject selection criteria. Hence, even subjects with high baseline EPA and DHA levels (derived from diet and/or metabolism) could have been included in both intervention and placebo control groups. New studies should include only subjects below a predetermined blood level of ω-3 FAs (or at least adjust for baseline levels) and should track changes from baseline to control for differences in compliance. The latter can involve drop-outs (those assigned to the active agent who do not take them) and drop-ins (those assigned to placebo who start taking EPA and DHA over the counter). The “ω-3 index,” a measure of the amount of EPA and DHA in red blood cell membranes expressed as a percentage of total FAs, appears to be a sensitive biomarker of ω-3 FA status ( 58 ). The ω-3 index is thought by some to be to EPA and DHA status what a hemoglobin A1c is to glucose status: a stable measure of relatively long-term tissue levels. The resources to conduct the “optimal” EPA and DHA study enrolling tens of thousands of middle-aged, healthy subjects given >1 g EPA and DHA or placebo (and prohibited from taking other fish-oil supplements) for several decades are unavailable. Therefore it is likely that less expensive, well-conducted (albeit never-conclusive) studies will continue to serve as the basis for understanding the role of these FAs on health. Some experts believe current evidence indicates EPA and DHA are likely to benefit individuals who have low baseline ω-3 status, who consume ≥1 g EPA and DHA/d for decades (from supplements or food), and who are not on optimal drug therapy or optimally compliant with drug treatment. Future studies should be designed to overcome the limitations described here, particularly improving on inclusion criteria, forms and doses, study length, and specific health outcomes. Informed dietary guidance and policy depends on designing studies and conducting systematic reviews with respect to these PICO considerations.
Case Study: Evidence Approach to Nutrition Guidance in the US Military
The US military relies on nutrition guidance from authoritative bodies such as the National Academy of Medicine (formerly the Institute of Medicine) when establishing food policies and nutritional feeding practices. Unique occupational related physical requirements and environmental stress exposures illustrate the specificity that needs to be considered when defining these policies and how PICO decisions in designing studies ensure that research results are relevant to the intended guidance.
The occupational lifestyle of a soldier presents several unique challenges for food and food policy. The energy requirements of military personnel are often quite high because of long hours of physical work, but in combat, space for food is limited, creating the need for energy-dense meals. Under-eating is common, because eating is often restricted to brief intermittent episodes as time or situation permit. As a result, it is critically important to provide sufficient food and high-quality nutrition between combat missions to offset any energy deficit and to provide necessary nutrients to refuel and recover. All of these considerations affect the PICO factors that will be considered relevant in translating research findings into dietary guidance for this subpopulation.
Food and nutrition policy developers must also take into consideration that individual field rations, such as the ration used for troops forward-deployed Meal, Ready to Eat, require a 3-y shelf life. Although this increases the versatility of the ration, it has historically limited the types of foods and ingredients used in formulating ration menus. Dietary supplements are not a viable option either, because the bias is to use subsistence money to buy food, and historic evidence indicates that service members will more likely eat fortified foods than supplements provided in pill form. Lastly, the food costs of rations are constrained by military budgets, forcing difficult choices when new items are considered. Research designed for use by the military will be most useful if these challenges are considered in the experimental design.
The FA composition of the military diet and military rations is similar to that of the typical American diet, i.e., sufficient in ω-6 FA but providing limited quantities of ω-3 FA. Based on some evidence that dietary fat might be aggravating the inflammatory response or hindering its resolution, food-based approaches that improve the FA composition of operational rations, as well as dining hall foods, are underway.
To generate the evidence base that is needed to make military policy decisions in regards to the recommended intake of ω-3 FAs and guidance for achieving diets with the desired ω-3 FA composition, data are needed to demonstrate both efficacy and effectiveness under real-life conditions (i.e., realistic foods among relevant environmental conditions). In recently conducted studies, ω-3 FA levels and the ω-3 index were dramatically improved when traditional foods were substituted with like items but with lowered ω-6 FA and elevated EPA and DHA. Studies are now underway, within the relevant PICO context, to determine whether soldiers will consume these foods frequently enough and in enough quantity to produce meaningful improvements in ω-3 PUFA status when the foods are provided in an ad libitum multiple-choice dining hall environment.
High-quality strategic research and systematic reviews are essential for generating evidence-based nutrition guidance, policies, and regulations. Recommendations for conducting strategic research are summarized in Table 3 . Research studies designed to answer questions relevant to specific guidance, as well as systematic review PICO criteria and quality factors, are likely to substantially impact diet and nutrition guidance, regulations, and policy. Strategically considering PICO decisions with the intended target in mind (e.g., dietary guidance gap) when designing, conducting, and reporting research is likely to lead to such studies having a greater impact in strengthening future nutrition guidance.
Specific recommendations for research with greater impact on dietary guidance 1
| • Address specific research gaps stated in the Dietary Guidelines Advisory Committee report or other influential guidance documents from authoritative bodies |
| • Consider PICO in designing and reporting results with respect to specific nutrition or dietary guidance |
| • Assume your study will be evaluated for both relevance (with PICO) and for quality of design, conduct, and reporting |
| • Use valid and reliable methods for dietary intake measures collected at multiple points in time |
| • Describe exposures and intervention in detail in observational studies and clinical trials, respectively |
| • Determine whether dose is relevant to current intakes and addresses a research gap |
| • Use qualified surrogate markers of chronic disease risk in randomized clinical trials |
| • Use relevant and realistic comparators |
| • Capture as much baseline data for a cohort as possible and know what to adjust for (and what not to adjust for) |
| • Recognize that adherence effects occur in randomized controlled trials and are associated with better health outcomes for both intervention and placebo subjects |
| • Consider practicality of food solutions for intended population |
| • Consider meaningfulness of the experimental outcomes in interpreting the data |
| • Use appropriate statistical analysis to evaluate differences between the control and intervention |
| • Design study to appropriately test the food or a specific, well-defined, and relevant food component |
| • Submit scientific evidence in response to policy and agency organization proposals |
Acknowledgments
We are grateful to Courtney McComber at ILSI North America for her administrative leadership, Ray DeVirgiliis at ILSI North America for helping to develop this as a symposium presented at the 2015 American Society for Nutrition annual scientific sessions, Dr. Dave Baer at USDA for his insights during session development and planning, and the ILSI North America Lipids Committee members for their thoughtful suggestions. All authors read and approved the final manuscript.
13 Abbreviations used: CRP, C-reactive protein; CVD, cardiovascular disease; DGAC, Dietary Guidelines Advisory Committee; EFSA, European Food Safety Authority; iTFA, industrial trans -FA; NEL, Nutrition Evidence Library; PHO, partially hydrogenated oils; PICO, population, intervention, comparator, outcome; TFA, trans -FA.
Americans are just about failing when it comes to nutrition, says a food-as-medicine researcher. A few simple diet tweaks could help.
- Americans' diets have remained largely unchanged since 1999, according to a new study.
- Meals remain high in processed foods that can increase a person's risk of disease.
- Ditching sugary drinks and eating two fewer processed meals a week could help.

Americans are eating healthier than in previous years, but they still have a long way to go, according to a researcher who studies food as medicine.
Dr. Dariush Mozaffarian, director of the Food is Medicine Institute at Tufts University in Boston, co-authored a study on the quality of nearly 52,000 American adults' diets between 1999 and 2020. The results were published online Tuesday in the Annals of Internal Medicine.
Mozaffarian and his co-author, Junxiu Liu, examined data from the National Health and Nutrition Examination Survey and found that the American diet has remained nearly the same over the past two decades.
Between 1999 and 2020, 10.5% of study participants transitioned from "poor" diets to healthier diets with more fruits, vegetables, and whole grains and less sodium, processed meat, and saturated fat.
But only 1% of study participants ate an "ideal" diet — 4 to 5 cups of fruits and vegetables daily, plus beans, whole grains, and nuts — during that same time period.
"People often ask me, 'Well, if the diet's slowly improving, why is obesity and diabetes still going up?' It's still going up because only 1.58% of Americans have an ideal diet. We still have a long way to go," Mozaffarian told CNN .
Related stories
"We have stalled as a nation — and that does not bode well for our health. If I was grading America on its diet, I'd give it a D—just up from an F," Mozaffarian said.
Why are Americans failing in the diet department?
Typically, the American diet consists of ultra-processed foods and foods high in salt and sugar. These foods can increase a person's risk of cancer , heart disease, stroke, and early death Accordingng to Heidi Silver, a registered dietitian and director of the Vanderbilt Diet, Body Composition, and Human Metabolism Core at Vanderbilt University Medical Center in Nashvil, factors like food insecurity and poverty have contributed to the overall lack of improvement in peoples' diets over the last two decadesle.
"Food insecurity affects diet quality via lower consumption of healthier foods, especially those that are more expensive, don't have a long shelf life and don't provide enough volume to fill a hungry child," Silver told Yahoo .
These systemic limitations can make it difficult for food-insecure populations like Black people, older people, and low-income people to make lasting diet changes.
Simple diet tweaks could help reduce health risks
For those seeking simple and inexpensive ways to improve their diets, removing sugary drinks is a good first step, according to Dr. Gregory Katz, a cardiologist at NYU Langone.
" Drinking calories and drinking alcohol are the biggest modifiable risk factors. The number of people I see drinking 500 calories a day blows my mind," Katz told Business Insider's Gabby Landsverk. "Just because it's simple doesn't make it easy."
Katz suggested doing away with soda, juice, sugar-laden coffee drinks, and cocktails and replacing them with unsweetened tea or water flavored with a splash of juice or flavored with citrus.
Aiming to swap out two servings of processed foods each week is another strategy that doesn't involve overhauling your entire diet, according to Dr. W. Taylor Kimberly. Kimberly, a professor of neurology at Harvard Medical School and the senior author of a recent study linking ultra-processed foods to health risks like dementia and stroke.
You could, for example, swap French fries for a baked sweet potato or nosh on nuts and carrots instead of cookies and crackers.
Kimberly said that a good rule of thumb is to prepare meals at home as much as possible.
"If you look at it and think, that could be made in my kitchen, that's a good indicator," he said.
More from Julia Naftulin
Most popular
Watch: how to spot ultra-processed foods we mistake for healthy.
- Main content
- How we do it
- Imperatives
- Vision 2050
- Be the voice of leading business
- Become more circular
- Cultivate sustainable agriculture
- Finance the transition
- Improve buildings and transport
- Improve performance & accountability
- Learn and educate
- Manage materials and deal with pollution
- Put people in focus
- Reduce emissions
- Regenerate nature
The Nature Restoration Law is a historic milestone for Europe
The European Council's recent adoption of the Nature Restoration Regulation…
Detangling the EU Deforestation Regulation
Practical examples for companies to understand EUDR regulations & how…
SWCA Environmental Consultants Joins World Business Council for Sustainable Development
Geneva, Switzerland: The World Business Council for Sustainable Development (WBCSD)…
- Global network
- Our history
- Asia Pacific
- North America
- Publication
- Past events
- Insights from the CEO
- Member spotlight
- WBCSD insights
- Become a member
- How to cultivate sustainable agriculture
Introduction
Food fuels our bodies and plays a powerful role in human health, culture, productivity and potential. it is central to livelihoods and creates connection to family, community and natural ecosystems on land and in water..
The food system, however, is also contributing to pressing global challenges. It contributes to approximately 25% of greenhouse gas (GHG) emissions, three-quarters of biodiversity loss and is a leading cause of non-communicable disease.
We must transition towards a future in which business, farmers, policymakers and civil society collaborate to deliver regenerative and equitable agricultural systems producing quality raw material and nutritious food for all by 2050.
To contribute to achieving our vision, leading businesses from across the agriculture and food value chain work within WBCSD’s Agriculture and Food Pathway to raise ambition, accelerate action and strengthen accountability, building vibrant economies and societies, protecting climate and restoring nature while supporting food and nutrition security for the world’s growing population.
Our Highlights

Case Studies: Food & Agriculture

Food and Agriculture Roadmap
Related actions.

Equitable Livelihoods

Healthy & Sustainable Diets

Positive Agriculture

One Planet Business for Biodiversity (OP2B)

Soft Commodities Forum (SCF)
News & insights.

Nature-positive in agri-food value chains: the why and the how
7 June, 2024

The living income agenda in agri-food value chains: no time to waste
8 April, 2024

Plant-forward is the future: How food businesses can make the most of the opportunity
25 April, 2024
Related Resources
Living Income: what, why and how

The Business Case for Scope 3 GHG Action in Agriculture & Food Value Chains
26 March, 2024

COP28 Business Statement of Action
10 December, 2023
Let's transform together
Emeline fellus.
Senior Director, Agriculture and Food
Stefania Avanzini
Director, One Planet Business for Biodiversity (OP2B)
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Comprehensive land consolidation as a development strategy for rural revitalization: the political ecology mechanisms and benefits of the pastoral complex.

Share and Cite
Chen, B.; Huang, Z.; He, W.; Wang, M. Comprehensive Land Consolidation as a Development Strategy for Rural Revitalization: The Political Ecology Mechanisms and Benefits of the Pastoral Complex. Land 2024 , 13 , 897. https://doi.org/10.3390/land13060897
Chen B, Huang Z, He W, Wang M. Comprehensive Land Consolidation as a Development Strategy for Rural Revitalization: The Political Ecology Mechanisms and Benefits of the Pastoral Complex. Land . 2024; 13(6):897. https://doi.org/10.3390/land13060897
Chen, Borui, Zirou Huang, Wei He, and Min Wang. 2024. "Comprehensive Land Consolidation as a Development Strategy for Rural Revitalization: The Political Ecology Mechanisms and Benefits of the Pastoral Complex" Land 13, no. 6: 897. https://doi.org/10.3390/land13060897
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Skip to main content
Update your browser for the best possible experience
As of January 1st, 2020, Internet Explorer (versions 11 and below) is no longer supported by Evolve. To get the best possible experience using Evolve, we recommend that you use another web browser. For HESI iNet users click here .

IMAGES
VIDEO
COMMENTS
A global epidemic of diet related chronic disease has prompted experimentation using food as a formal part of patient care and treatment. One of every five deaths across the globe is attributable to suboptimal diet, more than any other risk factor including tobacco. 1 Individual interactions with the healthcare system are an important opportunity to offer evidence based food and nutrition ...
1 Model and process for nutrition and dietetic practice, 3 2 Nutrition care process terminology (NCPT), 8 3 Record keeping, 12 4 Assessment, 16 PART II Case studies 1 Veganism, 25 2 Older person - ethical dilemma, 28 3 Older person, 31 4 Learning disabilities: Prader-Willi syndrome, 34 5 Freelance practice, 39 6 Public health - weight ...
CS_82. Food insecurity has clear health implications. Adults who are food-insecure may be at an increased risk of health problems, including obesity, heart disease, diabetes, depression, and increased susceptibility to COVID-19. CS_83, CS_84, CS_85 Food insecurity also puts children at a higher risk of asthma, anemia, and obesity, as well as ...
Building food and nutrition resilience in Quezon City: A case study on integrated food systems About Quezon City is at a paradox where some communities suffer from hunger while others are eating too much of the wrong foods. Increasing evidence of the triple burden of malnutrition—undernutrition, micronutrient deficiencies and overweight ...
Food is Prevention: The Case for Integrating Food and Nutrition Interventions into Healthcare is written by Sarah Downer, Robert Greenwald, Emily Broad Leib, Kellen Wittkop, Kristen Hayashi, Marissa Leonce, and Morgan Menchaca. ... CASE STUDY: Food as Tertiary Prevention - Medically-Tailored Meals for People Living with HIV/AIDS and Other ...
In September 2022, the Biden-Harris Administration convened the White House Conference on Hunger, Nutrition, and Health and revealed a national strategy to end hunger and increase healthy eating and physical activity in the United States. Pillar 2 of the National Strategy on Hunger, Nutrition, and Health aims to integrate nutrition and health by prioritizing the role of nutrition and food ...
The diversity of initiatives featured in this case study showcase the potential for utilising various entry points to transform the urban food system in a way that results in co-benefits across the SDG agenda. Four recurring themes stand out among Quezon City's efforts to improve its food system: 1. Leadership—at all levels. In this case study,
2. Nutrition for Healthy Ageing. The science of nutrition or the "nutritional science" is a highly advanced field of study, and numerous excellent books, journals and other resources are available for fundamental information about all nutritional components [].Briefly, the three essential macronutrients which provide the basic materials for building biological structures and for producing ...
In the current "nutrition transition," the consumption of high-calorie, nutrient-poor foods high in fats and sweeteners is increasing throughout the developing world. The nutrition transition, implicated in the rapid rise of obesity and diet-related chronic diseases worldwide, is rooted in the processes of globalization. Globalization affects the nature of the food supply chain, thereby ...
Nutrition and Health is an online international peer-reviewed journal that focusses on the relationship between nutrition and health. The journal welcomes original investigations, short communications, reviews, systematic reviews and meta-analyses, protocols, commentaries, hypotheses and case studies on current topics relating to the full spectrum of the effects of diet and nutrition on health ...
The case study takes the focus off analyzing a personal record. If needed, you can adjust the questions to focus more on the quality of the diet versus analyzing numbers like calories or grams of protein etc. You could also add more open-ended questions that include students looking for recipes that are suitable for that case study scenario.
Case studies on ω-3 ... Food and nutrition policy developers must also take into consideration that individual field rations, such as the ration used for troops forward-deployed Meal, Ready to Eat, require a 3-y shelf life. Although this increases the versatility of the ration, it has historically limited the types of foods and ingredients ...
National Food Security Act, 2013. "An Act to provide for food and nutritional security in human life cycle approach, by ensuring access to adequate quantity of quality food at affordable prices to people to live a life with dignity and for matters connected therewith or incidental thereto.". Every person belonging to priority households ...
A new research case series published in Frontiers in Nutrition presents food as medicine as a potential treatment for autoimmune diseases, describing three patients with chronic autoimmune disease ...
Judy Lawrence is a Research Officer, BDA & Visiting Researcher at King's College London, England. Joan Gandy is a Freelance Dietitian & Visiting Researcher, Nutrition & Dietetics, University of Hertfordshire, Englan.. Pauline Douglas is Senior Lecturer & Clinical Dietetic Facilitator, Northern Ireland Centre for Food and Health (NICHE), Ulster University, Northern Ireland.
Market and consumer evaluation of the marketplace for nutritious foods program: Tarakwo case study - Eldoret, Uasin Gishu County, Kenya. June 18, 2019. The Global Alliance for Improved Nutrition's Marketplace for Nutritious Foods program sparks private sector production and marketing of nutritious.
The clinical nutrition case study is a neglected area of activity and publication. This may be in part because it is not regarded as a serious contributor to evidence-based nutrition (EBN). ... 1 Fuli Institute of Food Science and Nutrition, Room D437 Agricultural, Biological and Environmental Building, Zijingang Campus, Zhejiang University ...
McGRAW HILL 1 CASE STUDY SERIES Digital Product in Use: Connect® Nutrition LMS Integration: D2L Brightspace Course Name: Nutrition and Food Sciences 207: General Nutrition Course Type: Online Credit Hours: 3 Credit Hours Program in Use: Wardlaw's Perspectives in Nutrition: A Functional Approach by Carol Byrd-Bredbenner, second edition
INTEGRATED NUTRITION AND FOOD SECURITY STRATEGIES FOR CHILDREN AND VULNERABLE GROUPS IN VIET NAM Case Study SDGs addressed More info: www.sdgfund.org This case study is based on lessons from the joint programme, "Integratednutrition and food security strategies for children and vulnerable Groups in Viet Nam."Read more CHAPTERS: HANOI
The first step in writing a nutrition case study is selecting the patient. Typically, the patient has sought out nutritional counseling or treatment for a specific reason. These reasons include weight management, a chronic disease, or a food allergy. The patient should be willing to participate in the case study and provide detailed information ...
Case Study A: This table demonstrates how the weight loss program addresses JO's nutrition diagnosis, and how that nutrition diagnosis might change over time. Content is organized to present food and nutrition-related history first, since this is the critical data set contributed by dietitians. 4th Edition: 2013
The study, published Monday in the Annals of Internal Medicine, analyzed dietary information on nearly 52,000 US adults who participated in the National Health and Nutrition Examination Survey, or ...
Check Pages 1-50 of Dietetic and Nutrition Case Studies in the flip PDF version. Dietetic and Nutrition Case Studies was published by Perpustakaan PIM on 2020-09-15. ... Pain, 129, 210-223. Institute of Medicine, Food and Nutrition Board (2001) Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron ...
Case Study: Evidence Approach to Nutrition Guidance in the US Military. ... Food and nutrition policy developers must also take into consideration that individual field rations, such as the ration used for troops forward-deployed Meal, Ready to Eat, require a 3-y shelf life. Although this increases the versatility of the ration, it has ...
A landmark study suggested we eat about 500 extra calories per day on ultra-processed diets. Scientists are working to disentangle why this happens. They're developing new recipes for ultra ...
Dr. Dariush Mozaffarian, director of the Food is Medicine Institute at Tufts University in Boston, co-authored a study on the quality of nearly 52,000 American adults' diets between 1999 and 2020.
Introduction Food fuels our bodies and plays a powerful role in human health, culture, productivity and potential. It is central to livelihoods and creates connection to family, community and natural ecosystems on land and in water. The food system, however, is also contributing to pressing global challenges. It contributes to approximately 25% of greenhouse gas
The case studies of the pastoral complex present the practice of national-capital-land-social relationships and changes in land benefits, showcasing a Chinese approach to rural development and social justice. ... This study illustrates that in Guangzhou, comprehensive land consolidation is indispensable for ensuring food security and ...
This case study is about the regular diet intended for our diabetic client. This regular diabetic diet is designed to promote the optimum health of diabetic individuals through good nutrition. This has several chapters that will cover significant topics regarding the client's illness, his diet restrictions, computations, and the meal plan ...
Skip to main content