- When is Breech an Issue?
The later in pregnancy a baby is breech , the more difficult it is for the baby to flip head down. The baby’s size grows in relation to the uterus and there is a smaller percentage of amniotic fluid for the baby to move freely. The more complicated past births were due to fetal position, the earlier I suggest starting to get your muscles unwound and your pelvis aligned. If a previous baby remained either breech or posterior until birth, I suggest bodywork throughout the pregnancy.
In time, the breech baby’s head becomes heavy enough (between 5-7 months) for gravity to bring the head down in a symmetrical womb. The baby will move head down if there is room or if there is tone in the support to the uterus to direct the baby head down.

Common issues with breech:
- Health of the baby overall
- Safety of the birth
- Safety for the mother facing surgical birth
- Emotions of the birthing parent(s)
- Belly Mapping® Breech
- Flip a Breech
- When Baby Flips Head Down
- Breech & Bicornuate Uterus
- Breech for Providers
- What if My Breech Baby Doesn't Turn?
- Belly Mapping ®️ Method
After Baby Turns
- Head Down is Not Enough
- Sideways/Transverse
- Asynclitism
- Oblique Lie
- Left Occiput Transverse
- Right Occiput Anterior
- Right Occiput Posterior
- Right Occiput Transverse
- Face Presentation
- Left Occiput Anterior
- OP Truths & Myths
- Anterior Placenta
- Body Balancing
When should I be concerned about a breech position?
During the month before 30 weeks, about 15% of babies are breech. Since breech baby’s spine is vertical, the womb is “stretched” upwards. We expect babies to turn head down by 28-32 weeks.
Breech may not be an issue until 32-34 weeks. If you know your womb has an unusual limitation in shape or size, such as a bicornate uterus then begin body balancing before pregnancy and once 15 weeks in pregnancy. In this case, the baby needs to be head down much earlier so that the uterus still has the room for baby to turn. Every unique womb is unique so these dates are theoretical, not absolute.
The timeline for breech
This is a timeline of what to do and when to do it in order to help a breech baby move head down:
- Before 24-26 weeks, most babies lie diagonally or sideways in the Transverse Lie position .
- Between 24-29 weeks, most babies turn vertical and some will be breech.
- By 30-32 weeks, most babies flip head down and bottom-up.
- By 34 weeks pregnant, the provider expects the baby to be head down.
- Between 36-37 weeks, a provider may suggest an external cephalic version .
- Full term is from 37-42 weeks gestation, and about 3-4% of term babies are breech.
The medical model of care addresses the breech position between 36-37 weeks, when baby’s survival outside the womb won’t include special nursery care to breathe or suck. Physicians Oxorn and Foote, however, recommend helping babies turn head down at 34 weeks. Some home birth midwives suggest interacting with a baby at 30-34 weeks to encourage a head-down position (vertex).
Women who have had difficult previous births due to posterior, asynclitism , or a labor that didn’t progress, may want to begin bodywork and the Forward-leaning Inversion as soon as the second trimester of pregnancy (after morning sickness is gone and extra things like fetal positioning activities can be thought about).
Here is a general guideline for the average pregnancy:
10-24 weeks gestation
This is the time when fetal position is generally determined, even though the baby’s final position isn’t typically set before 34 weeks gestation. How can this be? The body has a habit, so to speak, of how the soft tissues, ligaments, muscles, and alignment of the pelvis and whole body is set. The baby simply follows this basic pattern. By adding body balancing now, the baby has an increased chance of ideal positioning for labor at 34 weeks and beyond.
24-30 weeks
Routine good posture with walking and exercise will help most babies be head down as the third trimester gets underway. A 30-second inversion is good practice for everyone. Unless you have a medical reason not to, please consider the Forward-leaning Inversion. If you have a history of car accidents, falls, uncomfortable pregnancies, hormonal imbalance, or a previous breech or posterior baby, then begin the inversion and body work before or during early pregnancy.
30-34 weeks
After 30 weeks, you can start following our 6-day program for Helping Your Breech Baby Turn . By 32-34 weeks, chiropractic adjustments are suggested. We recommend consulting with one of our Spinning Babies ® Aware Practitioners . The best time to flip a breech is now.
Oxorn and Foote recommend external version at 34 weeks, but most doctors want to wait for the baby’s lungs and suck reflex to be more developed in case the maneuver goes wrong and starts labor or pulls the placenta off the uterine wall. There is often enough amniotic fluid for an easy flip before 35 weeks.

Dad’s the hero in this “over the top” support to help his mate do a Breech Tilt in the comfort of a bed!
- Breech Tilt: Follow the FLI with the Breech Tilt for 10-20 minutes. This allows you to tuck your chin while upside down on a similar slanted surface. Use an ironing board against the couch, for instance.
- Open-knee Chest: Open-knee Chest has been studied and shown to help breeches flip. I like inversion positions that allow the mother to tuck her own chin. Myofascial workers tell me this relaxes her pelvis, whereas extending the chin tightens the pelvis.
- Professional bodywork: Acupuncture and Moxibustion both have good statistics for flipping breeches. Find out if there’s a Spinning Babies ® Aware Practitioner in your area.
- Therapeutic massage: There are muscle/fascia attachments at the base of the skull, respiratory diaphragm, inguinal ligament, and even the hip sockets! We are whole organisms, not machines with reproductive parts.
- Chiropractic or Osteopathic: Spinal adjustmentsof the neck do improve pelvic alignment, especially if accompanied by fascial release. Not all chiropractors are trained in soft tissue body work, however. And not all soft tissue work is equal. This is why we promote our Aware Practitioner Workshops for bodyworkers.
Should manual external cephalic version be done earlier?
A few midwives recommend version (manually turning the breech baby to head down) at 30 –31 weeks. Anne Frye, author of Holistic Midwifery, reported a very low incidence of breech at term when her midwifery group manually rotated babies during this gestational age.
Attempting to turn the baby now is over a month before the medical model of turning breeches. Utmost gentleness must be the protective factor. If forcing a baby to turn harms the baby or placenta, the baby is too young to be cared for outside of the Neonatal Intensive Care Unit.
Midwives who turn babies now believe there is less chance of hurting a baby and proceed very carefully, stopping at once if there is resistance. Typically, there is less resistance from the uterus because there is more fluid and the baby is still very small.
Body work is suggested before attempting this, especially for first-time moms or women who had a difficult time with their first birth. There are risks to a manual version, so the baby should be monitored closely in between each 10-30 degrees of rotation.
35-36 weeks
If your baby is breech during this time your doctor or midwife will begin to talk about how to help the baby flip head down, and possibly about scheduling a manual version for 36-37 weeks. Getting body work and having acupuncture or homeopathy may help soften the ligaments and a tense uterus to either help the baby flip spontaneously or to allow more success in an attempt at a version.
Moxibustion has its highest success rate this week.
36-37 weeks.
During this time, you can continue with the suggestions in the “Professional Help” page. Also, an obstetrician may suggest manually flipping the baby to a head down position at this time. A few midwives will also offer this, perhaps even earlier, at 30-34 weeks.
NOTE: Don’t let someone manually flip your baby without using careful monitoring of the baby’s heartbeat. Accidents can occur, even when there is good intention. The baby must be listened to and the version stopped immediately if the heart rate drops.
External cephalic version near the end of pregnancy
You may also agree to go through with a cephalic version at this time. The baby is in the womb with the cord and placenta and there is a small risk in turning the baby manually. This maneuver should be done with monitoring by experienced professionals, in a setting ready for a cesarean if needed.
There is about a 40-50% chance this will be successful. Sometimes the baby moves easily and sometimes the procedure is painful. I believe it’s important who performs it, and that ligament tightness would make this more uncomfortable. I suggest getting chiropractic, myofascial, acupuncture, homeopathy, or moxibustion (or all of these) before and after the version.
Doing the Three Sisters of Balance SM (or following the Turning Your Breech Baby guidelines) daily beforehand and just before the procedure would be relaxing and helpful. More birth professionals are using our approach in the hours or the week before the procedure and report that fewer procedures are necessary and those that are seem to be easier than average to do when the baby is able to be turned.
38-40 weeks
Sometimes a woman and her caregiver don’t know the baby is breech until this point or until labor. Rarely does a baby flip to breech this late in pregnancy but they can. Parents and providers may learn that baby is breech during a routine bio-physical ultrasound exam during this time or later in pregnancy.
An external cephalic version may yet be successful, depending on the fluid level and the flexibility of the uterus, the baby’s head position and location, a uterine septum, where the placenta is, etc.
It is still possible that the baby flips doing body balancing activities or even labor itself (contractions might be the very action that turns baby in about 1% of breeches). You may find turning easier if you keep doing the activities listed above.
40-41 weeks
Though many breeches are born about 37-39 weeks gestation, some will happily go to 41 or 42 weeks. For a head down baby, 41 weeks and 1 to 3 days is a common time for labor to begin on its own. SStarting labor at this gestation can certainly be normal for a healthy breechling, too.
If the pregnant person has a tendency to be somewhat overweight or lower energy, which can indicate low thyroid function, a longer pregnancy may be more likely. This tendency deserves looking after. Well-nourished and peppy women may also go a full pregnancy length, of course.
Going into labor and then having a planned cesarean is recommend by Dr. Michel Odent in his book, Cesarean. Going into labor spontaneously is safer for the breech vaginal birth, as well. Women who are trying to flip their baby often find it necessary to slow down the efforts and come to terms with a breech birth.
When facing a cesarean, it can be nurturing to you and your baby to plan a cesarean with skin-to-skin, delayed cord clamping, and breastfeeding on the operating room table or in the recovery room. Give yourself some time and compassion to feel your feelings and explore your options to adapt to the options you have available to you.
Postdates (after your due date) with a breech
With a breech, going all the way to 42 weeks may or may not be more of an issue. Some providers will have to end any plans for a vaginal birth by now. Midwifery statutes often limit midwifery care out of the hospital to 37-42 weeks (or 36-43, depending on where you live).
After 42 weeks, the baby’s skull bones are setting up more firmly and a vaginal birth is less favorable. I’ve been to a few breech births after 42 weeks gestation and everything went very well. But, I do sometimes wonder why labor isn’t starting and if metabolism is a reason, especially when there’s been regular bodywork for weeks.
For a person carrying a breech baby who does show signs of low thyroid function or otherwise a “sloshy” metabolism, I am inclined to transfer care to a kind hospital provider at 41.5 weeks. Intelligent and experienced monitoring may rule out issues that arise post dates that may complicate labor. With slow metabolism postdates issues with breech position may need extra attention before 42 weeks.
Continue body balancing and daily stretching but stop inversions for three days. Walk with a stride. See more at https://www.spinningbabies.com/pregnancy-birth/baby-position/breech/when-baby-flips-head-down/
If Baby Does Not Turn
Not every breech baby will turn on their own. Not every attempt at an External Cephalic Version works (It’s often 50-50). Adding body balancing has abundant anecdotal reporting to show success. But this balancing should be individualized if the pregnant person has followed general guidelines closely for 1-2 weeks without success.
Be compassionate to you and your baby. You are both doing the best you can with the resources you have.
Choose your path. Sometimes it may feel like you don’t have a choice. Consider why it feels that way. Perhaps your choice is safety over manner of birth? That’s totally valid. Just because a vaginal birth might be available to some doesn’t mean it is your first choice, too.
Sometimes babies choose, too. The labor goes too fast to do surgery for the birth. Or, the baby doesn’t come into the pelvis and surgical birth is necessary. (Remember reaching in and pulling out the baby is not reasonable if a cesarean is available in the region unless this is a second twin (subsequent triplet) or travel is impossible due to weather, war, or whatever reason. Life is real. Babies don’t follow a script. Be real with your own experience.
Inducing a breech
Inducing a breech is not recommended in out of hospital settings. Even in the hospital, the risk rises. In some areas where breech is common, Pitocin/Syntocin inductions are done with outcomes that are good enough to keep the options open. Induction by herbs is also considered out of scope for breech.
We need to respect the breech and not stress the baby, especially in settings where we don’t have the rescue setup to solve any potential problems. Try body balancing and see if labor begins on its own. That would be a non-invasive, non-manipulating approach.
The Breech Turned During Labor
It is a rare possibility that the baby flips to head down during labor. I once assisted a midwife who’s laboring mother’s water had released. Her labor was mild and not picking up, so after 24 hours we transferred and found that the baby had flipped. The doctor thought we’d misdiagnosed, but the mother’s abdomen was so thin we could feel the baby’s knuckles and elbow and found the baby in the opposite direction after entering the hospital!
Another mother had Dynamic Body Balancing in early labor with one of Dr. Carol Phillips students who was also a midwife. Her breech baby turned head down during transition phase of labor!
Laboring With a Breech Before The Cesarean
If the plan is to have a cesarean once labor begins, call the hospital and alert them of labor immediately. Go to the hospital right away. Breech births can go quite quickly and you want to be where people are ready to help you. If you plan to have a vaginal birth, don’t delay in getting to your birth location or getting your birth team to you.
While it can be totally normal to have a 24-hour or longer breech birth, many breech labors are quite short. Because the softer bottom is first, it may take you by surprise that you are progressing with such little pain (though some breech births are as painful as head down births). Just don’t base your decision to get to the hospital on your pain level!
A cesarean can be more complicated if the baby is wedged low in the pelvis. That is why there is a recommendation to have the cesarean in early labor. But cesareans are done everyday with head down babies low in the pelvis. Sometimes it’s how it is.
Starting labor in and of itself doesn’t make the surgery more dangerous. Rushing around and doing things in a hurry might. Alert your hospital before labor and again once you start labor. Be firm that you know what you are about and that they need to get the Operating Room ready while you are on your way.
Mostly, a leisurely transition into the hospital can be sustained with a sense of humor and practicality. There can be a sense of calm while you and the staff take the steps to welcome your baby. This is your birth. Be present with how your experience unfolds.
After the birth
While the concern about breech position is during the birthing, when the baby is breech for most of the third trimester, their skull bones become shaped by the inside of the upper womb (the fundus). This isn’t typically an issue but can be noticed.
Craniosacral therapy can gently (and without using force) reshape the baby’s head, ideally during the month or two after birth. Surgery on baby’s skull is seldom necessary after 3-6 sessions with a Craniosacral therapist. For most breech babies, this issue is not present. I list is here because I have heard some assumptions that can be dispelled.
A question about breech
Email from Wed, Feb 11, 2009:
…I’m 30 weeks and the baby is what I’d describe as oblique breech – his head is on my right side next to my belly button, his hips/butt are in my pelvis on the lower left side (my left) and his feet are in front of his face. I think he’s facing forward – towards my belly button. I’ve known this for weeks just because his big head is so hard I always bump that spot on accident. …. my first son was 9 lbs and born posterior, so I’m really hoping this baby is in the ideal position for delivery… so both of these things make me nervous that he won’t move. He has been in this position for a few weeks now. … Anyway, just wondering if I should worry and what, if anything, I can do to help him move now. My Midwife suggested a Chiropractor that can do some adjustments. I’d like to do the couch inversion too. Would it help for me to walk more? Also, should I sleep more on one side than the other? Thanks for your help! Great site!
Gail’s reply:
Hi…. now is a good time to take action, not so much that your baby is breech, but because your first baby was OP . You see, a pelvic misalignment and/or round ligament spasms (they often go together) can result in either a breech or a posterior fetal position . So, a breech will often flip to a posterior position and may stay that way unless you resolve the underlying issue. Maternal positioning is often not enough by itself to correct a posterior fetal position when there is a history of previous posterior or breech babies. While certainly most breech babies flip head down, it’s beneficial to help correct the symmetry of your uterine ligaments now, while the baby is still small enough to have plenty of room to flip head down once the reason for the previous posterior position is remedied. See some things a Chiropractor can do for breech and posterior by reading Professional Help .

Contact to Listing Owner
- Screening & Prevention
- Sexual Health & Relationships
- Birth Control
- Preparing for Surgery Checklist
- Healthy Teens
- Getting Pregnant
- During Pregnancy
- Labor and Delivery
- After Pregnancy
- Pregnancy Book
- Mental Health
- Prenatal Testing
- Menstrual Health
- Heart Health
- Special Procedures
- Diseases and Conditions
- Browse All Topics
- View All Frequently Asked Questions

Read common questions on the coronavirus and ACOG’s evidence-based answers.
If Your Baby Is Breech
URL has been copied to the clipboard
Frequently Asked Questions Expand All
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation . A breech presentation occurs when the fetus’s buttocks, feet, or both are in place to come out first during birth. This happens in 3–4% of full-term births.
It is not always known why a fetus is breech. Some factors that may contribute to a fetus being in a breech presentation include the following:
You have been pregnant before.
There is more than one fetus in the uterus (twins or more).
There is too much or too little amniotic fluid .
The uterus is not normal in shape or has abnormal growths such as fibroids .
The placenta covers all or part of the opening of the uterus ( placenta previa )
The fetus is preterm .
Occasionally fetuses with certain birth defects will not turn into the head-down position before birth. However, most fetuses in a breech presentation are otherwise normal.
Your health care professional may be able to tell which way your fetus is facing by placing his or her hands at certain points on your abdomen. By feeling where the fetus's head, back, and buttocks are, it may be possible to find out what part of the fetus is presenting first. An ultrasound exam or pelvic exam may be used to confirm it.
External cephalic version (ECV) is an attempt to turn the fetus so that he or she is head down. ECV can improve your chance of having a vaginal birth. If the fetus is breech and your pregnancy is greater than 36 weeks your health care professional may suggest ECV.
ECV will not be tried if:
You are carrying more than one fetus
There are concerns about the health of the fetus
You have certain abnormalities of the reproductive system
The placenta is in the wrong place
The placenta has come away from the wall of the uterus ( placental abruption )
ECV can be considered if you have had a previous cesarean delivery .
The health care professional performs ECV by placing his or her hands on your abdomen. Firm pressure is applied to the abdomen so that the fetus rolls into a head-down position. Two people may be needed to perform ECV. Ultrasound also may be used to help guide the turning.
The fetus's heart rate is checked with fetal monitoring before and after ECV. If any problems arise with you or the fetus, ECV will be stopped right away. ECV usually is done near a delivery room. If a problem occurs, a cesarean delivery can be performed quickly, if necessary.
Complications may include the following:
Prelabor rupture of membranes
Changes in the fetus's heart rate
Placental abruption
Preterm labor
More than one half of attempts at ECV succeed. However, some fetuses who are successfully turned with ECV move back into a breech presentation. If this happens, ECV may be tried again. ECV tends to be harder to do as the time for birth gets closer. As the fetus grows bigger, there is less room for him or her to move.
Most fetuses that are breech are born by planned cesarean delivery. A planned vaginal birth of a single breech fetus may be considered in some situations. Both vaginal birth and cesarean birth carry certain risks when a fetus is breech. However, the risk of complications is higher with a planned vaginal delivery than with a planned cesarean delivery.
In a breech presentation, the body comes out first, leaving the baby’s head to be delivered last. The baby’s body may not stretch the cervix enough to allow room for the baby’s head to come out easily. There is a risk that the baby’s head or shoulders may become wedged against the bones of the mother’s pelvis. Another problem that can happen during a vaginal breech birth is a prolapsed umbilical cord . It can slip into the vagina before the baby is delivered. If there is pressure put on the cord or it becomes pinched, it can decrease the flow of blood and oxygen through the cord to the baby.
Although a planned cesarean birth is the most common way that breech fetuses are born, there may be reasons to try to avoid a cesarean birth.
A cesarean delivery is major surgery. Complications may include infection, bleeding, or injury to internal organs.
The type of anesthesia used sometimes causes problems.
Having a cesarean delivery also can lead to serious problems in future pregnancies, such as rupture of the uterus and complications with the placenta.
With each cesarean delivery, these risks increase.
If you are thinking about having a vaginal birth and your fetus is breech, your health care professional will review the risks and benefits of vaginal birth and cesarean birth in detail. You usually need to meet certain guidelines specific to your hospital. The experience of your health care professional in delivering breech babies vaginally also is an important factor.
Amniotic Fluid : Fluid in the sac that holds the fetus.
Anesthesia : Relief of pain by loss of sensation.
Breech Presentation : A position in which the feet or buttocks of the fetus would appear first during birth.
Cervix : The lower, narrow end of the uterus at the top of the vagina.
Cesarean Delivery : Delivery of a fetus from the uterus through an incision made in the woman’s abdomen.
External Cephalic Version (ECV) : A technique, performed late in pregnancy, in which the doctor attempts to manually move a breech baby into the head-down position.
Fetus : The stage of human development beyond 8 completed weeks after fertilization.
Fibroids : Growths that form in the muscle of the uterus. Fibroids usually are noncancerous.
Oxygen : An element that we breathe in to sustain life.
Pelvic Exam : A physical examination of a woman’s pelvic organs.
Placenta : Tissue that provides nourishment to and takes waste away from the fetus.
Placenta Previa : A condition in which the placenta covers the opening of the uterus.
Placental Abruption : A condition in which the placenta has begun to separate from the uterus before the fetus is born.
Prelabor Rupture of Membranes : Rupture of the amniotic membranes that happens before labor begins. Also called premature rupture of membranes (PROM).
Preterm : Less than 37 weeks of pregnancy.
Ultrasound Exam : A test in which sound waves are used to examine inner parts of the body. During pregnancy, ultrasound can be used to check the fetus.
Umbilical Cord : A cord-like structure containing blood vessels. It connects the fetus to the placenta.
Uterus : A muscular organ in the female pelvis. During pregnancy, this organ holds and nourishes the fetus.
Vagina : A tube-like structure surrounded by muscles. The vagina leads from the uterus to the outside of the body.
Vertex Presentation : A presentation of the fetus where the head is positioned down.
Article continues below
Advertisement
If you have further questions, contact your ob-gyn.
Don't have an ob-gyn? Learn how to find a doctor near you .
Published: January 2019
Last reviewed: August 2022
Copyright 2024 by the American College of Obstetricians and Gynecologists. All rights reserved. Read copyright and permissions information . This information is designed as an educational aid for the public. It offers current information and opinions related to women's health. It is not intended as a statement of the standard of care. It does not explain all of the proper treatments or methods of care. It is not a substitute for the advice of a physician. Read ACOG’s complete disclaimer .
Clinicians: Subscribe to Digital Pamphlets
Explore ACOG's library of patient education pamphlets.
A Guide to Pregnancy from Ob-Gyns
For trusted, in-depth advice from ob-gyns, turn to Your Pregnancy and Childbirth: Month to Month.
ACOG Explains
A quick and easy way to learn more about your health.
What to Read Next
Cesarean Birth
Fetal Heart Rate Monitoring During Labor
What is back labor?
What is delayed cord clamping?
- Search Please fill out this field.
- Newsletters
- Sweepstakes
- Labor & Delivery
What Causes Breech Presentation?
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered.
What Is Breech Presentation?
Types of breech presentation, what causes a breech baby, can you turn a breech baby, how are breech babies delivered.
FatCamera/Getty Images
Toward the end of pregnancy, your baby will start to get into position for delivery, with their head pointed down toward the vagina. This is otherwise known as vertex presentation. However, some babies turn inside the womb so that their feet or buttocks are poised to be delivered first, which is commonly referred to as breech presentation, or a breech baby.
As you near the end of your pregnancy journey, an OB-GYN or health care provider will check your baby's positioning. You might find yourself wondering: What causes breech presentation? Are there risks involved? And how are breech babies delivered? We turned to experts and research to answer some of the most common questions surrounding breech presentation, along with what causes this positioning in the first place.
During your pregnancy, your baby constantly moves around the uterus. Indeed, most babies do somersaults up until the 36th week of pregnancy , when they pick their final position in the womb, says Laura Riley , MD, an OB-GYN in New York City. Approximately 3-4% of babies end up “upside-down” in breech presentation, with their feet or buttocks near the cervix.
Breech presentation is typically diagnosed during a visit to an OB-GYN, midwife, or health care provider. Your physician can feel the position of your baby's head through your abdominal wall—or they can conduct a vaginal exam if your cervix is open. A suspected breech presentation should ultimately be confirmed via an ultrasound, after which you and your provider would have a discussion about delivery options, potential issues, and risks.
There are three types of breech babies: frank, footling, and complete. Learn about the differences between these breech presentations.
Frank Breech
With frank breech presentation, your baby’s bottom faces the cervix and their legs are straight up. This is the most common type of breech presentation.
Footling Breech
Like its name suggests, a footling breech is when one (single footling) or both (double footling) of the baby's feet are in the birth canal, where they’re positioned to be delivered first .
Complete Breech
In a complete breech presentation, baby’s bottom faces the cervix. Their legs are bent at the knees, and their feet are near their bottom. A complete breech is the least common type of breech presentation.
Other Types of Mal Presentations
The baby can also be in a transverse position, meaning that they're sideways in the uterus. Another type is called oblique presentation, which means they're pointing toward one of the pregnant person’s hips.
Typically, your baby's positioning is determined by the fetus itself and the shape of your uterus. Because you can't can’t control either of these factors, breech presentation typically isn’t considered preventable. And while the cause often isn't known, there are certain risk factors that may increase your risk of a breech baby, including the following:
- The fetus may have abnormalities involving the muscular or central nervous system
- The uterus may have abnormal growths or fibroids
- There might be insufficient amniotic fluid in the uterus (too much or too little)
- This isn’t your first pregnancy
- You have a history of premature delivery
- You have placenta previa (the placenta partially or fully covers the cervix)
- You’re pregnant with multiples
- You’ve had a previous breech baby
In some cases, your health care provider may attempt to help turn a baby in breech presentation through a procedure known as external cephalic version (ECV). This is when a health care professional applies gentle pressure on your lower abdomen to try and coax your baby into a head-down position. During the entire procedure, the fetus's health will be monitored, and an ECV is often performed near a delivery room, in the event of any potential issues or complications.
However, it's important to note that ECVs aren't for everyone. If you're carrying multiples, there's health concerns about you or the baby, or you've experienced certain complications with your placenta or based on placental location, a health care provider will not attempt an ECV.
The majority of breech babies are born through C-sections . These are usually scheduled between 38 and 39 weeks of pregnancy, before labor can begin naturally. However, with a health care provider experienced in delivering breech babies vaginally, a natural delivery might be a safe option for some people. In fact, a 2017 study showed similar complication and success rates with vaginal and C-section deliveries of breech babies.
That said, there are certain known risks and complications that can arise with an attempt to deliver a breech baby vaginally, many of which relate to problems with the umbilical cord. If you and your medical team decide on a vaginal delivery, your baby will be monitored closely for any potential signs of distress.
Ultimately, it's important to know that most breech babies are born healthy. Your provider will consider your specific medical condition and the position of your baby to determine which type of delivery will be the safest option for a healthy and successful birth.
ACOG. If Your Baby Is Breech .
American Pregnancy Association. Breech Presentation .
Gray CJ, Shanahan MM. Breech Presentation . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Mount Sinai. Breech Babies .
Takeda J, Ishikawa G, Takeda S. Clinical Tips of Cesarean Section in Case of Breech, Transverse Presentation, and Incarcerated Uterus . Surg J (N Y). 2020 Mar 18;6(Suppl 2):S81-S91. doi: 10.1055/s-0040-1702985. PMID: 32760790; PMCID: PMC7396468.
Shanahan MM, Gray CJ. External Cephalic Version . [Updated 2022 Nov 6]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Fonseca A, Silva R, Rato I, Neves AR, Peixoto C, Ferraz Z, Ramalho I, Carocha A, Félix N, Valdoleiros S, Galvão A, Gonçalves D, Curado J, Palma MJ, Antunes IL, Clode N, Graça LM. Breech Presentation: Vaginal Versus Cesarean Delivery, Which Intervention Leads to the Best Outcomes? Acta Med Port. 2017 Jun 30;30(6):479-484. doi: 10.20344/amp.7920. Epub 2017 Jun 30. PMID: 28898615.
Related Articles

Breech Presentation
- Author: Richard Fischer, MD; Chief Editor: Ronald M Ramus, MD more...
- Sections Breech Presentation
- Vaginal Breech Delivery
- Cesarean Delivery
- Comparative Studies
- External Cephalic Version
- Conclusions
- Media Gallery
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. The percentage of breech deliveries decreases with advancing gestational age from 22-25% of births prior to 28 weeks' gestation to 7-15% of births at 32 weeks' gestation to 3-4% of births at term. [ 1 ]
Predisposing factors for breech presentation include prematurity , uterine malformations or fibroids, polyhydramnios , placenta previa , fetal abnormalities (eg, CNS malformations, neck masses, aneuploidy), and multiple gestations . Fetal abnormalities are observed in 17% of preterm breech deliveries and in 9% of term breech deliveries.
Perinatal mortality is increased 2- to 4-fold with breech presentation, regardless of the mode of delivery. Deaths are most often associated with malformations, prematurity, and intrauterine fetal demise .
Types of breeches
See the list below:
Frank breech (50-70%) - Hips flexed, knees extended (pike position)
Complete breech (5-10%) - Hips flexed, knees flexed (cannonball position)
Footling or incomplete (10-30%) - One or both hips extended, foot presenting
Historical considerations
Vaginal breech deliveries were previously the norm until 1959 when it was proposed that all breech presentations should be delivered abdominally to reduce perinatal morbidity and mortality. [ 2 ]
Vaginal breech delivery
Three types of vaginal breech deliveries are described, as follows:
Spontaneous breech delivery: No traction or manipulation of the infant is used. This occurs predominantly in very preterm, often previable, deliveries.
Assisted breech delivery: This is the most common type of vaginal breech delivery. The infant is allowed to spontaneously deliver up to the umbilicus, and then maneuvers are initiated to assist in the delivery of the remainder of the body, arms, and head.
Total breech extraction: The fetal feet are grasped, and the entire fetus is extracted. Total breech extraction should be used only for a noncephalic second twin; it should not be used for a singleton fetus because the cervix may not be adequately dilated to allow passage of the fetal head. Total breech extraction for the singleton breech is associated with a birth injury rate of 25% and a mortality rate of approximately 10%. Total breech extractions are sometimes performed by less experienced accoucheurs when a foot unexpectedly prolapses through the vagina. As long as the fetal heart rate is stable in this situation, it is permissible to manage expectantly to allow the cervix to completely dilate around the breech (see the image below).

Technique and tips for assisted vaginal breech delivery
The fetal membranes should be left intact as long as possible to act as a dilating wedge and to prevent overt cord prolapse .
Oxytocin induction and augmentation are controversial. In many previous studies, oxytocin was used for induction and augmentation, especially for hypotonic uterine dysfunction. However, others are concerned that nonphysiologic forceful contractions could result in an incompletely dilated cervix and an entrapped head.
An anesthesiologist and a pediatrician should be immediately available for all vaginal breech deliveries. A pediatrician is needed because of the higher prevalence of neonatal depression and the increased risk for unrecognized fetal anomalies. An anesthesiologist may be needed if intrapartum complications develop and the patient requires general anesthesia .
Some clinicians perform an episiotomy when the breech delivery is imminent, even in multiparas, as it may help prevent soft tissue dystocia for the aftercoming head (see the images below).

The Pinard maneuver may be needed with a frank breech to facilitate delivery of the legs but only after the fetal umbilicus has been reached. Pressure is exerted in the popliteal space of the knee. Flexion of the knee follows, and the lower leg is swept medially and out of the vagina.
No traction should be exerted on the infant until the fetal umbilicus is past the perineum, after which time maternal expulsive efforts should be used along with gentle downward and outward traction of the infant until the scapula and axilla are visible (see the image below).

Use a dry towel to wrap around the hips (not the abdomen) to help with gentle traction of the infant (see the image below).

An assistant should exert transfundal pressure from above to keep the fetal head flexed.
Once the scapula is visible, rotate the infant 90° and gently sweep the anterior arm out of the vagina by pressing on the inner aspect of the arm or elbow (see the image below).

Rotate the infant 180° in the reverse direction, and sweep the other arm out of the vagina. Once the arms are delivered, rotate the infant back 90° so that the back is anterior (see the image below).

The fetal head should be maintained in a flexed position during delivery to allow passage of the smallest diameter of the head. The flexed position can be accomplished by using the Mauriceau Smellie Veit maneuver, in which the operator's index and middle fingers lift up on the fetal maxillary prominences, while the assistant applies suprapubic pressure (see the image below).

Alternatively, Piper forceps can be used to maintain the head in a flexed position (see the image below).

In many early studies, routine use of Piper forceps was recommended to protect the head and to minimize traction on the fetal neck. Piper forceps are specialized forceps that are placed from below the infant and, unlike conventional forceps, are not tailored to the position of the fetal head (ie, it is a pelvic, not cephalic, application). The forceps are applied while the assistant supports the fetal body in a horizontal plane.
During delivery of the head, avoid extreme elevation of the body, which may result in hyperextension of the cervical spine and potential neurologic injury (see the images below).

Lower Apgar scores, especially at 1 minute, are more common with vaginal breech deliveries. Many advocate obtaining an umbilical cord artery and venous pH for all vaginal breech deliveries to document that neonatal depression is not due to perinatal acidosis.
Fetal head entrapment may result from an incompletely dilated cervix and a head that lacks time to mold to the maternal pelvis. This occurs in 0-8.5% of vaginal breech deliveries. [ 3 ] This percentage is higher with preterm fetuses (< 32 wk), when the head is larger than the body. Dührssen incisions (ie, 1-3 cervical incisions made to facilitate delivery of the head) may be necessary to relieve cervical entrapment. However, extension of the incision can occur into the lower segment of the uterus, and the operator must be equipped to deal with this complication. The Zavanelli maneuver has been described, which involves replacement of the fetus into the abdominal cavity followed by cesarean delivery. While success has been reported with this maneuver, fetal injury and even fetal death have occurred.
Nuchal arms, in which one or both arms are wrapped around the back of the neck, are present in 0-5% of vaginal breech deliveries and in 9% of breech extractions. [ 3 ] Nuchal arms may result in neonatal trauma (including brachial plexus injuries) in 25% of cases. Risks may be reduced by avoiding rapid extraction of the infant during delivery of the body. To relieve nuchal arms when it is encountered, rotate the infant so that the fetal face turns toward the maternal symphysis pubis (in the direction of the impacted arm); this reduces the tension holding the arm around the back of the fetal head, allowing for delivery of the arm.
Cervical spine injury is predominantly observed when the fetus has a hyperextended head prior to delivery. Ballas and Toaff (1976) reported 20 cases of hyperextended necks, defined as an angle of extension greater than 90° ("star-gazing"), discovered on antepartum radiographs. [ 4 ] Of the 11 fetuses delivered vaginally, 8 (73%) sustained complete cervical spinal cord lesions, defined as either transection or nonfunction.
Cord prolapse may occur in 7.4% of all breech labors. This incidence varies with the type of breech: 0-2% with frank breech, 5-10% with complete breech, and 10-25% with footling breech. [ 3 ] Cord prolapse occurs twice as often in multiparas (6%) than in primigravidas (3%). Cord prolapse may not always result in severe fetal heart rate decelerations because of the lack of presenting parts to compress the umbilical cord (ie, that which predisposes also protects).
Prior to the 2001 recommendations by the American College of Obstetricians and Gynecologists (ACOG), approximately 50% of breech presentations were considered candidates for vaginal delivery. Of these candidates, 60-82% were successfully delivered vaginally.
Candidates can be classified based on gestational age. For pregnancies prior to 26 weeks' gestation, prematurity, not mode of delivery, is the greatest risk factor. Unfortunately, no randomized clinical trials to help guide clinical management have been reported. Vaginal delivery can be considered, but a detailed discussion of the risks from prematurity and the lack of data regarding the ideal mode of delivery should take place with the parent(s). For example, intraventricular hemorrhage, which can occur in an infant of extremely low birth weight, should not be misinterpreted as proof of a traumatic vaginal breech delivery.
For pregnancies between 26 and 32 weeks, retrospective studies suggest an improved outcome with cesarean delivery, although these reports are subject to selection bias. In contrast, between 32 and 36 weeks' gestation, vaginal breech delivery may be considered after a discussion of risks and benefits with the parent(s).
After 37 weeks' gestation, parents should be informed of the results of a recent multicenter randomized clinical trial that demonstrated significantly increased perinatal mortality and short-term neonatal morbidity associated with vaginal breech delivery (see Comparative Studies). For those attempting vaginal delivery, if estimated fetal weight (EFW) is more than 4000 g, some recommend cesarean delivery because of concern for entrapment of the unmolded head in the maternal pelvis, although data to support this practice are limited.
A frank breech presentation is preferred when vaginal delivery is attempted. Complete breeches and footling breeches are still candidates, as long as the presenting part is well applied to the cervix and both obstetrical and anesthesia services are readily available in the event of a cord prolapse.
The fetus should show no neck hyperextension on antepartum ultrasound imaging (see the image below). Flexed or military position is acceptable.
Regarding prior cesarean delivery, a retrospective study by Ophir et al of 71 women with one prior low transverse cesarean delivery who subsequently delivered a breech fetus found that 24 women had an elective repeat cesarean and 47 women had a trial of labor. [ 5 ] In the 47 women with a trial of labor, 37 (78.7%) resulted in a vaginal delivery. Two infants in the trial of labor group had nuchal arms (1 with a transient brachial plexus injury) and 1 woman required a hysterectomy for hemorrhage due to a uterine dehiscence discovered after vaginal delivery. Vaginal breech delivery after one prior cesarean delivery is not contraindicated, though larger studies are needed.
Primigravida versus multiparous
It had been commonly believed that primigravidas with a breech presentation should have a cesarean delivery, although no data (prospective or retrospective) support this view. The only documented risk related to parity is cord prolapse, which is 2-fold higher in parous women than in primigravid women.
Radiographic and CT pelvimetry
Historically, radiograph pelvimetry was believed to be useful to quantitatively assess the inlet and mid pelvis. Recommended pelvimetry criteria included a transverse inlet diameter larger than 11.5 cm, anteroposterior inlet diameter larger than 10.5 cm, transverse midpelvic diameter (between the ischial spines) larger than 10 cm, and anteroposterior midpelvic diameter larger than 11.5 cm. However, radiographic pelvimetry is rarely, if ever, used in the United States.
CT pelvimetry , which is associated with less fetal radiation exposure than conventional radiographic pelvimetry, was more recently advocated by some investigators. It, too, is rarely used today.
Ultimately, if the obstetrical operator is not experienced or comfortable with vaginal breech deliveries, cesarean delivery may be the best choice. Unfortunately, with the dwindling number of experienced obstetricians who still perform vaginal breech deliveries and who can teach future generations of obstetricians, this technique may soon be lost due to attrition.
In 1970, approximately 14% of breeches were delivered by cesarean delivery. By 1986, that rate had increased to 86%. In 2003, based on data from the National Center for Health Statistics, the rate of cesarean delivery for all breech presentations was 87.2%. Most of the remaining breeches delivered vaginally were likely second twins, fetal demises, and precipitous deliveries. However, the rise in cesarean deliveries for breeches has not necessarily equated with an improvement in perinatal outcome. Green et al compared the outcome for term breeches prior to 1975 (595 infants, 22% cesarean delivery rate for breeches) with those from 1978-1979 (164 infants, 94% cesarean delivery rate for breeches). [ 6 ] Despite the increase in rates of cesarean delivery, the differences in rates of asphyxia, birth injury, and perinatal deaths were not significant.
Maneuvers for cesarean delivery are similar to those for vaginal breech delivery, including the Pinard maneuver, wrapping the hips with a towel for traction, head flexion during traction, rotation and sweeping out of the fetal arms, and the Mauriceau Smellie Veit maneuver.
An entrapped head can still occur during cesarean delivery as the uterus contracts after delivery of the body, even with a lower uterine segment that misleadingly appears adequate prior to uterine incision. Entrapped heads occur more commonly with preterm breeches, especially with a low transverse uterine incision. As a result, some practitioners opt to perform low vertical uterine incisions for preterm breeches prior to 32 weeks' gestation to avoid head entrapment and the kind of difficult delivery that cesarean delivery was meant to avoid. Low vertical incisions usually require extension into the corpus, resulting in cesarean delivery for all future deliveries.
If a low transverse incision is performed, the physician should move quickly once the breech is extracted in order to deliver the head before the uterus begins to contract. If any difficulty is encountered with delivery of the fetal head, the transverse incision can be extended vertically upward (T incision). Alternatively, the transverse incision can be extended laterally and upward, taking great care to avoid trauma to the uterine arteries. A third option is the use of a short-acting uterine relaxant (eg, nitroglycerin) in an attempt to facilitate delivery.
Only 3 randomized studies have evaluated the mode of delivery of the term breech. All other studies were nonrandomized or retrospective, which may be subject to selection bias.
In 1980, Collea et al randomized 208 women in labor with term frank breech presentations to either elective cesarean delivery or attempted vaginal delivery after radiographic pelvimetry. [ 7 ] Oxytocin was allowed for dysfunctional labor. Of the 60 women with adequate pelves, 49 delivered vaginally. Two neonates had transient brachial plexus injuries. Women randomized to elective cesarean delivery had higher postpartum morbidity rates (49.3% vs 6.7%).
In 1983, Gimovsky et al randomized 105 women in labor with term nonfrank breech presentations to a trial of labor versus elective cesarean delivery. [ 8 ] In this group of women, 47 had complete breech presentations, 16 had incomplete breech presentations (hips flexed, 1 knee extended/1 knee flexed), 32 had double-footling presentations, and 10 had single-footling presentations. Oxytocin was allowed for dysfunctional labor. Of the labor group, 44% had successful vaginal delivery. Most cesarean deliveries were performed for inadequate pelvic dimensions on radiographic pelvimetry. The rate of neonatal morbidity did not differ between neonates delivered vaginally and those delivered by cesarean delivery, although a higher maternal morbidity rate was noted in the cesarean delivery group.
In 2000, Hannah and colleagues completed a large, multicenter, randomized clinical trial involving 2088 term singleton fetuses in frank or complete breech presentations at 121 institutions in 26 countries. [ 9 ] In this study, popularly known as the Term Breech Trial, subjects were randomized into a planned cesarean delivery group or a planned vaginal birth group. Exclusion criteria were estimated fetal weight (EFW) more than 4000 g, hyperextension of the fetal head, lethal fetal anomaly or anomaly that might result in difficulty with delivery, or contraindication to labor or vaginal delivery (eg, placenta previa ).
Subjects randomized to cesarean delivery were scheduled to deliver after 38 weeks' gestation unless conversion to cephalic presentation had occurred. Subjects randomized to vaginal delivery were treated expectantly until labor ensued. Electronic fetal monitoring was either continuous or intermittent. Inductions were allowed for standard obstetrical indications, such as postterm gestations. Augmentation with oxytocin was allowed in the absence of apparent fetopelvic disproportion, and epidural analgesia was permitted.
Adequate labor was defined as a cervical dilation rate of 0.5 cm/h in the active phase of labor and the descent of the breech fetus to the pelvic floor within 2 hours of achieving full dilation. Vaginal delivery was spontaneous or assisted and was attended by an experienced obstetrician. Cesarean deliveries were performed for inadequate progress of labor, nonreassuring fetal heart rate, or conversion to footling breech. Results were analyzed by intent-to-treat (ie, subjects were analyzed by randomization group, not by ultimate mode of delivery).
Of 1041 subjects in the planned cesarean delivery group, 941 (90.4%) had cesarean deliveries. Of 1042 subjects in the planned vaginal delivery group, 591 (56.7%) had vaginal deliveries. Indications for cesarean delivery included: fetopelvic disproportion or failure to progress in labor (226), nonreassuring fetal heart rate tracing (129), footling breech (69), request for cesarean delivery (61), obstetrical or medical indications (45), or cord prolapse (12).
The composite measurement of either perinatal mortality or serious neonatal morbidity by 6 weeks of life was significantly lower in the planned cesarean group than in the planned vaginal group (5% vs 1.6%, P < .0001). Six of 16 neonatal deaths were associated with difficult vaginal deliveries, and 4 deaths were associated with fetal heart rate abnormalities. The reduction in risk in the cesarean group was even greater in participating countries with overall low perinatal mortality rates as reported by the World Health Organization. The difference in perinatal outcome held after controlling for the experience level of the obstetrician. No significant difference was noted in maternal mortality or serious maternal morbidity between the 2 groups within the first 6 weeks of delivery (3.9% vs 3.2%, P = .35).
A separate analysis showed no difference in breastfeeding, sexual relations, or depression at 3 months postpartum, though the reported rate of urinary incontinence was higher in the planned vaginal group (7.3% vs 4.5%).
Based on the multicenter trial, the ACOG published a Committee Opinion in 2001 that stated "planned vaginal delivery of a singleton term breech may no longer be appropriate." This did not apply to those gravidas presenting in advanced labor with a term breech and imminent delivery or to a nonvertex second twin.
A follow-up study by Whyte et al was conducted in 2004 on 923 children who were part of the initial multicenter study. [ 10 ] The authors found no differences between the planned cesarean delivery and planned vaginal breech delivery groups with regards to infant death rates or neurodevelopmental delay by age 2 years. Similarly, among 917 participating mothers from the original trial, no substantive differences were apparent in maternal outcome between the 2 groups. [ 11 ] No longer-term maternal effects, such as the impact of a uterine scar on future pregnancies, have yet been reported.
A meta-analysis of the 3 above mentioned randomized trials was published in 2015. The findings included a reduction in perinatal/neonatal death, reduced composite short-term outcome of perinatal/neonatal death or serious neonatal morbidity with planned cesarean delivery versus planned vaginal delivery. [ 12 ] However, at 2 years of age, there was no significant difference in death or neurodevelopmental delay between the two groups. Maternal outcomes assessed at 2 years after delivery were not significantly different.
With regard to preterm breech deliveries, only one prospective randomized study has been performed, which included only 38 subjects (28-36 wk) with preterm labor and breech presentation. [ 13 ] Of these subjects, 20 were randomized to attempted vaginal delivery and 18 were randomized to immediate cesarean delivery. Of the attempted vaginal delivery group, 25% underwent cesarean delivery for nonreassuring fetal heart rate tracings. Five neonatal deaths occurred in the vaginal delivery group, and 1 neonatal death occurred in the cesarean delivery group. Two neonates died from fetal anomalies, 3 from respiratory distress, and 1 from sepsis.
Nonanomalous infants who died were not acidotic at delivery and did not have birth trauma. Differences in Apgar scores were not significant, although the vaginal delivery group had lower scores. The small number of enrolled subjects precluded any definitive conclusions regarding the safety of vaginal breech delivery for a preterm breech.
Retrospective analyses showed a higher mortality rate in vaginal breech neonates weighing 750-1500 g (26-32 wk), but less certain benefit was shown with cesarean delivery if the fetal weight was more than 1500 g (approximately 32 wk). Therefore, this subgroup of very preterm infants (26-32 wk) may benefit from cesarean delivery, although this recommendation is based on potentially biased retrospective data.
A large cohort study was published in 2015 from the Netherlands Perinatal Registry, which included 8356 women with a preterm (26-36 6/7 weeks) breech from 2000 to 2011, over three quarters of whom intended to deliver vaginally. In this overall cohort, there was no significant difference in perinatal mortality between the planned vaginal delivery and planned cesarean delivery groups (adjusted odds ratio 0.97, 95% confidence interval 0.60 – 1.57). However, the subgroup delivering at 28 to 32 weeks had a lower perinatal mortality with planned cesarean section (aOR 0.27, 95% CI 0.10 – 0.77). After adding a composite of perinatal morbidity, planned cesarean delivery was associated with a better outcome than a planned vaginal delivery (aOR 0.77, 95% CI 0.63 – 0.93. [ 14 ]
The Maternal-Fetal Medicine Units Network of the US National Institute of Child Health and Human Development considered a multicenter randomized clinical trial of attempted vaginal delivery versus elective cesarean delivery for 24- to 28-week breech fetuses. [ 15 ] However, it was not initiated because of anticipated difficulty with recruitment, inadequate numbers to show statistically significant differences, and medicolegal concerns. Therefore, this study is not likely to be performed.
External cephalic version (ECV) is the transabdominal manual rotation of the fetus into a cephalic presentation.
Initially popular in the 1960s and 1970s, ECV virtually disappeared after reports of fetal deaths following the procedure. Reintroduced to the United States in the 1980s, it became increasingly popular in the 1990s.
Improved outcome may be related to the use of nonstress tests both before and after ECV, improved selection of low-risk fetuses, and Rh immune globulin to prevent isoimmunization.
Prepare for the possibility of cesarean delivery. Obtain a type and screen as well as an anesthesia consult. The patient should have nothing by mouth for at least 8 hours prior to the procedure. Recent ultrasonography should have been performed for fetal position, to check growth and amniotic fluid volume, to rule out a placenta previa, and to rule out anomalies associated with breech. Another sonogram should be performed on the day of the procedure to confirm that the fetus is still breech.
A nonstress test (biophysical profile as backup) should be performed prior to ECV to confirm fetal well-being.
Perform ECV in or near a delivery suite in the unlikely event of fetal compromise during or following the procedure, which may require emergent delivery.
ECV can be performed with 1 or 2 operators. Some prefer to have an assistant to help turn the fetus, elevate the breech out of the pelvis, or to monitor the position of the baby with ultrasonography. Others prefer a single operator approach, as there may be better coordination between the forces that are raising the breech and moving the head.
ECV is accomplished by judicious manipulation of the fetal head toward the pelvis while the breech is brought up toward the fundus. Attempt a forward roll first and then a backward roll if the initial attempts are unsuccessful. No consensus has been reached regarding how many ECV attempts are appropriate at one time. Excessive force should not be used at any time, as this may increase the risk of fetal trauma.
Following an ECV attempt, whether successful or not, repeat the nonstress test (biophysical profile if needed) prior to discharge. Also, administer Rh immune globulin to women who are Rh negative. Some physicians traditionally induce labor following successful ECV. However, as virtually all of these recently converted fetuses are unengaged, many practitioners will discharge the patient and wait for spontaneous labor to ensue, thereby avoiding the risk of a failed induction of labor. Additionally, as most ECV’s are attempted prior to 39 weeks, as long as there are no obstetrical or medical indications for induction, discharging the patient to await spontaneous labor would seem most prudent.
In those with an unsuccessful ECV, the practitioner has the option of sending the patient home or proceeding with a cesarean delivery. Expectant management allows for the possibility of spontaneous version. Alternatively, cesarean delivery may be performed at the time of the failed ECV, especially if regional anesthesia is used and the patient is already in the delivery room (see Regional anesthesia). This would minimize the risk of a second regional analgesia.
In those with an unsuccessful ECV, the practitioner may send the patient home, if less than 39 weeks, with plans for either a vaginal breech delivery or scheduled cesarean after 39 weeks. Expectant management allows for the possibility of a spontaneous version. Alternatively, if ECV is attempted after 39 weeks, cesarean delivery may be performed at the time of the failed ECV, especially if regional anesthesia is used and the patient is already in the delivery room (see Regional anesthesia). This would minimize the risk of a second regional analgesia.
Success rate
Success rates vary widely but range from 35% to 86% (average success rate in the 2004 National Vital Statistics was 58%). Improved success rates occur with multiparity, earlier gestational age, frank (versus complete or footling) breech presentation, transverse lie, and in African American patients.
Opinions differ regarding the influence of maternal weight, placental position, and amniotic fluid volume. Some practitioners find that thinner patients, posterior placentas, and adequate fluid volumes facilitate successful ECV. However, both patients and physicians need to be prepared for an unsuccessful ECV; version failure is not necessarily a reflection of the skill of the practitioner.
Zhang et al reviewed 25 studies of ECV in the United States, Europe, Africa, and Israel. [ 16 ] The average success rate in the United States was 65%. Of successful ECVs, 2.5% reverted back to breech presentation (other estimates range from 3% to 5%), while 2% of unsuccessful ECVs had spontaneous version to cephalic presentation prior to labor (other estimates range from 12% to 26%). Spontaneous version rates depend on the gestational age when the breech is discovered, with earlier breeches more likely to undergo spontaneous version.
A prospective study conducted in Germany by Zielbauer et al demonstrated an overall success rate of 22.4% for ECV among 353 patients with a singleton fetus in breech presentation. ECV was performed at 38 weeks of gestation. Factors found to increase the likelihood of success were a later week of gestation, abundant amniotic fluid, fundal and anterior placental location, and an oblique lie. [ 17 ]
A systematic review in 2015 looked at the effectiveness of ECV with eight randomized trials of ECV at term. Compared to women with no attempt at ECV, ECV reduced non-cephalic presentation at birth by 60% and reduced cesarean sections by 40% in the same group. [ 18 ] Although the rate of cesarean section is lower when ECV is performed than if not, the overall rate of cesarean section remains nearly twice as high after successful ECV due to both dystocia and non-reassuring fetal heart rate patterns. [ 19 ] Nulliparity was the only factor shown in follow-up to increase the risk of instrumental delivery following successful ECV. [ 20 ]
While most studies of ECV have been performed in university hospitals, Cook showed that ECV has also been effective in the private practice setting. [ 21 ] Of 65 patients with term breeches, 60 were offered ECV. ECV was successful in 32 (53%) of the 60 patients, with vaginal delivery in 23 (72%) of the 32 patients. Of the remaining breech fetuses believed to be candidates for vaginal delivery, 8 (80%) had successful vaginal delivery. The overall vaginal delivery rate was 48% (31 of 65 patients), with no significant morbidity.
Cost analysis
In 1995, Gifford et al performed a cost analysis of 4 options for breech presentations at term: (1) ECV attempt on all breeches, with attempted vaginal breech delivery for selected persistent breeches; (2) ECV on all breeches, with cesarean delivery for persistent breeches; (3) trial of labor for selected breeches, with scheduled cesarean delivery for all others; and (4) scheduled cesarean delivery for all breeches prior to labor. [ 22 ]
ECV attempt on all breeches with attempted vaginal breech delivery on selected persistent breeches was associated with the lowest cesarean delivery rate and was the most cost-effective approach. The second most cost-effective approach was ECV attempt on all breeches, with cesarean delivery for persistent breeches.
Uncommon risks of ECV include fractured fetal bones, precipitation of labor or premature rupture of membranes , abruptio placentae , fetomaternal hemorrhage (0-5%), and cord entanglement (< 1.5%). A more common risk of ECV is transient slowing of the fetal heart rate (in as many as 40% of cases). This risk is believed to be a vagal response to head compression with ECV. It usually resolves within a few minutes after cessation of the ECV attempt and is not usually associated with adverse sequelae for the fetus.
Trials have not been large enough to determine whether the overall risk of perinatal mortality is increased with ECV. The Cochrane review from 2015 reported perinatal death in 2 of 644 in ECV and 6 of 661 in the group that did not attempt ECV. [ 18 ]
A 2016 Practice Bulletin by ACOG recommended that all women who are near term with breech presentations should be offered an ECV attempt if there are no contraindications (see Contraindications below). [ 23 ] ACOG guidelines issued in 2020 recommend that ECV should be performed starting at 37+0 weeks, in order to reduce the likelihood of reversion and to increase the rate of spontaneous version. [ 24 ]
ECV is usually not performed on preterm breeches because they are more likely to undergo spontaneous version to cephalic presentation and are more likely to revert to breech after successful ECV (approximately 50%). Earlier studies of preterm ECV did not show a difference in the rates of breech presentations at term or overall rates of cesarean delivery. Additionally, if complications of ECV were to arise that warranted emergent delivery, it would result in a preterm neonate with its inherent risks. The Early External Cephalic Version (ECV) 2 trial was an international, multicentered, randomized clinical trial that compared ECV performed at 34-35 weeks’ gestation compared with 37 weeks’ gestation or more. [ 25 ] Early ECV increased the chance of cephalic presentation at birth; however, no difference in cesarean delivery rates was noted, along with a nonstatistical increase in preterm births.
A systematic review from 2015 looked at 5 studies of ECV completed prior to 37 weeks and concluded that compared with no ECV attempt, ECV commenced before term reduces the non-cephalic presentation at birth, however early ECV may increase the risk of late preterm birth. [ 26 ]
Given the increasing awareness of the risks of late preterm birth and early term deliveries, the higher success of earlier ECV should be weighed against the risks of iatrogenic prematurity should a complication arise necessitating delivery.
Contraindications
Absolute contraindications for ECV include multiple gestations with a breech presenting fetus, contraindications to vaginal delivery (eg, herpes simplex virus infection, placenta previa), and nonreassuring fetal heart rate tracing.
Relative contraindications include polyhydramnios or oligohydramnios , fetal growth restriction , uterine malformation , and major fetal anomaly.
Controversial candidates
Women with prior uterine incisions may be candidates for ECV, but data are scant. In 1991, Flamm et al attempted ECV on 56 women with one or more prior low transverse cesarean deliveries. [ 27 ] The success rate of ECV was 82%, with successful vaginal births in 65% of patients with successful ECVs. No uterine ruptures occurred during attempted ECV or subsequent labor, and no significant fetal complications occurred.
In 2010 ACOG acknowledged that although there is limited data in both the above study and one more recently, [ 28 ] no serious adverse events occurred in these series. A larger prospective cohort study that was published in 2014 reported similar success rates of ECV among women with and without prior cesarean section, although lower vaginal birth rates. There were, however, no cases of uterine rupture or other adverse outcomes. [ 29 ]
Another controversial area is performing ECV on a woman in active labor. In 1985, Ferguson and Dyson reported on 15 women in labor with term breeches and intact membranes. [ 30 ] Four patients were dilated greater than 5 cm (2 women were dilated 8 cm). Tocolysis was administered, and intrapartum ECV was attempted. ECV was successful in 11 of 15 patients, with successful vaginal births in 10 patients. No adverse effects were noted. Further studies are needed to evaluate the safety and efficacy of intrapartum ECV.
Data regarding the benefit of intravenous or subcutaneous beta-mimetics in improving ECV rates are conflicting.
In 1996, Marquette et al performed a prospective, randomized, double-blinded study on 283 subjects with breech presentations between 36 and 41 weeks' gestation. [ 31 ] Subjects received either intravenous ritodrine or placebo. The success rate of ECV was 52% in the ritodrine group versus 42% in the placebo group ( P = .35). When only nulliparous subjects were analyzed, significant differences were observed in the success of ECV (43% vs 25%, P < .03). ECV success rates were significantly higher in parous versus nulliparous subjects (61% vs 34%, P < .0001), with no additional improvement with ritodrine.
A systematic review published in 2015 of six randomized controlled trials of ECV that compared the use of parenteral beta-mimetic tocolysis during ECV concluded that tocolysis was effective in increasing the rate of cephalic presentation in labor and reducing the cesarean delivery rate by almost 25% in both nulliparous and multiparous women. [ 32 ] Data on adverse effects and other tocolytics was insufficient. A review published in 2011 on Nifedipine did not show an improvement in ECV success. [ 33 ]
Regional anesthesia
Regional analgesia, either epidural or spinal, may be used to facilitate external cephalic version (ECV) success. When analgesia levels similar to that for cesarean delivery are given, it allows relaxation of the anterior abdominal wall, making palpation and manipulation of the fetal head easier. Epidural or spinal analgesia also eliminates maternal pain that may cause bearing down and tensing of the abdominal muscles. If ECV is successful, the epidural can be removed and the patient sent home to await spontaneous labor. If ECV is unsuccessful, a patient can proceed to cesarean delivery under her current anesthesia, if the gestational age is more than 39 weeks.
The main disadvantage is the inherent risk of regional analgesia, which is considered small. Additionally, lack of maternal pain could potentially result in excessive force being applied to the fetus without the knowledge of the operator.
In 1994, Carlan et al retrospectively analyzed 61 women who were at more than 36 weeks' gestation and had ECV with or without epidural. [ 34 ] The success rate of ECV was 59% in the epidural group and 24% in the nonepidural group ( P < .05). In 7 of 8 women with unsuccessful ECV without epidural, a repeat ECV attempt after epidural was successful. No adverse effects on maternal or perinatal morbidity or mortality occurred.
In 1997, Schorr et al randomized 69 subjects who were at least 37 weeks' gestation to either epidural or control groups prior to attempted ECV. [ 35 ] Those in whom ECV failed underwent cesarean delivery. The success rate of ECV was 69% in the epidural group and 32% in the control group (RR, 2.12; 95% CI, 1.24-3.62). The cesarean delivery rate was 79% in the control group and 34% in the epidural group ( P = .001). No complications of epidural anesthesia and no adverse fetal effects occurred.
In 1999, Dugoff et al randomized 102 subjects who were at more than 36 weeks' gestation with breech presentations to either spinal anesthesia or a control group. [ 36 ] All subjects received 0.25 mg terbutaline subcutaneously. The success rate of ECV was 44% in the spinal group and 42% in the nonspinal group, which was not statistically significant.
In contrast, a 2007 randomized clinical trial of spinal analgesia versus no analgesia in 74 women showed a significant improvement in ECV success (66.7% vs 32.4%, p = .004), with a significantly lower pain score by the patient. [ 37 ]
The 2015 systematic review asserted that regional analgesia in combination with a tocolytic was more effective than the tocolytic alone for increasing ECV success; however there was no difference in cephalic presentation in labor. Data from the same review was insufficient to assess regional analgesia without tocolysis [ 32 ]
Acoustic stimulation
Johnson and Elliott performed a randomized, blinded trial on 23 subjects to compare acoustic stimulation prior to ECV with a control group when the fetal spine was in the midline (directly back up or back down). [ 38 ] Of those who received acoustic stimulation, 12 of 12 fetuses shifted to a spine-lateral position after acoustic stimulation, and 11 (91%) underwent successful ECV. In the control group, 0 of 11 shifts and 1 (9%) successful ECV ( P < .0001) occurred. Additional studies are needed.
Amnioinfusion
Although an earlier study reported on the utility of amnioinfusion to successfully turn 6 fetuses who initially failed ECV, [ 39 ] a subsequent study was published of 7 women with failed ECV who underwent amniocentesis and amnioinfusion of up to 1 liter of crystalloid. [ 40 ] Repeat attempts of ECV were unsuccessful in all 7 cases. Amnioinfusion to facilitate ECV cannot be recommended at this time.
Vaginal delivery rates after successful version
The rate of cesarean delivery ranges from 0-31% after successful external cephalic version (ECV). Controversy has existed on whether there is a higher rate of cesarean delivery for labor dystocia following ECV. In 1994, a retrospective study by Egge et al of 76 successful ECVs matched with cephalic controls by delivery date, parity, and gestational age failed to note any significant difference in the cesarean delivery rate (8% in ECV group, 6% in control group). [ 41 ]
However, in 1997, Lau et al compared 154 successful ECVs to 308 spontaneously occurring cephalic controls (matched for age, parity, and type of labor onset) with regard to the cesarean delivery rate. [ 42 ] Cesarean delivery rates were higher after ECV (16.9% vs 7.5%, P < .005) because of higher rates of cephalopelvic disproportion and nonreassuring fetal heart rate tracings. This may be related to an increased frequency of compound presentations after ECV. Immediate induction of labor after successful ECV may also contribute to an increase in the cesarean delivery rate due to failed induction in women with unripe cervices and unengaged fetal heads.
Further, in another cohort study from 2015, factors were described which decreased the vaginal delivery rate after successful ECV including labor induction, less than two weeks between ECV and delivery, high body mass index and previous cesarean. [ 43 ] The overall caesarean delivery rate in this cohort was 15%.
Vaginal breech delivery requires an experienced obstetrician and careful counseling of the parents. Although studies on the delivery of the preterm breech are limited, the multicenter Term Breech Trial found an increased rate of perinatal mortality and serious immediate perinatal morbidity, though no differences were seen in infant outcome at 2 years of age.
Parents must be informed about potential risks and benefits to the mother and neonate for both vaginal breech delivery and cesarean delivery. Discussion of risks should not be limited only to the current pregnancy. The risks of a cesarean on subsequent pregnancies, including uterine rupture and placental attachment abnormalities ( placenta previa , abruption , accreta), as well as maternal and perinatal sequelae from these complications, should be reviewed as well.
It remains concerning that the dearth of experienced physicians to teach younger practitioners will lead to the abandonment of vaginal breeches altogether. For those wishing to learn the art of vaginal breech deliveries, simulation training with pelvic models has been advocated to familiarize trainees with the procedure in a nonthreatening environment. [ 44 ] Once comfortable with the appropriate maneuvers, vaginal delivery of the second, noncephalic twin, may be attempted under close supervision by an experienced physician. The cervix will already be fully dilated, and, assuming the second twin is not significantly larger, the successful vaginal delivery rate has been quoted to be as high as 96%.
External cephalic version (ECV) is a safe alternative to vaginal breech delivery or cesarean delivery, reducing the cesarean delivery rate for breech by 50%. ACOG (2016) recommends offering ECV to all women with a breech fetus near term. [ 23 ] Adjuncts such as tocolysis, regional anesthesia, and acoustic stimulation when appropriate may improve ECV success rates.
Hickok DE, Gordon DC, Milberg JA, Williams MA, Daling JR. The frequency of breech presentation by gestational age at birth: a large population-based study. Am J Obstet Gynecol . 1992 Mar. 166(3):851-2. [QxMD MEDLINE Link] .
Wright RC. Reduction of perinatal mortality and morbidity in breech delivery through routine use of cesarean section. Obstet Gynecol . 1959. 14:758-63.
Cheng M, Hannah M. Breech delivery at term: a critical review of the literature. Obstet Gynecol . 1993 Oct. 82(4 Pt 1):605-18. [QxMD MEDLINE Link] .
Ballas S, Toaff R. Hyperextension of the fetal head in breech presentation: radiological evaluation and significance. Br J Obstet Gynaecol . 1976 Mar. 83(3):201-4. [QxMD MEDLINE Link] .
Ophir E, Oettinger M, Yagoda A, Markovits Y, Rojansky N, Shapiro H. Breech presentation after cesarean section: always a section?. Am J Obstet Gynecol . 1989 Jul. 161(1):25-8. [QxMD MEDLINE Link] .
Green JE, McLean F, Smith LP, Usher R. Has an increased cesarean section rate for term breech delivery reduced in incidence of birth asphyxia, trauma, and death?. Am J Obstet Gynecol . 1982 Mar 15. 142(6 Pt 1):643-8. [QxMD MEDLINE Link] .
Collea JV, Chein C, Quilligan EJ. The randomized management of term frank breech presentation: a study of 208 cases. Am J Obstet Gynecol . 1980 May 15. 137(2):235-44. [QxMD MEDLINE Link] .
Gimovsky ML, Wallace RL, Schifrin BS, Paul RH. Randomized management of the nonfrank breech presentation at term: a preliminary report. Am J Obstet Gynecol . 1983 May 1. 146(1):34-40. [QxMD MEDLINE Link] .
Hannah ME, Hannah WJ, Hewson SA, Hodnett ED, Saigal S, Willan AR. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Term Breech Trial Collaborative Group. Lancet . 2000 Oct 21. 356(9239):1375-83. [QxMD MEDLINE Link] .
Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol . 2004 Sep. 191(3):864-71. [QxMD MEDLINE Link] .
Hannah ME, Whyte H, Hannah WJ, Hewson S, Amankwah K, Cheng M. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the international randomized Term Breech Trial. Am J Obstet Gynecol . 2004 Sep. 191(3):917-27. [QxMD MEDLINE Link] .
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev . 2015 Jul 21. 7:CD000166. [QxMD MEDLINE Link] .
Zlatnik FJ. The Iowa premature breech trial. Am J Perinatol . 1993 Jan. 10(1):60-3. [QxMD MEDLINE Link] .
Bergenhenegouwen L, Vlemmix F, Ensing S, Schaaf J, van der Post J, Abu-Hanna A, et al. Preterm Breech Presentation: A Comparison of Intended Vaginal and Intended Cesarean Delivery. Obstet Gynecol . 2015 Dec. 126 (6):1223-30. [QxMD MEDLINE Link] .
Eller DP, VanDorsten JP. Route of delivery for the breech presentation: a conundrum. Am J Obstet Gynecol . 1995 Aug. 173(2):393-6; discussion 396-8. [QxMD MEDLINE Link] .
Zhang J, Bowes WA Jr, Fortney JA. Efficacy of external cephalic version: a review. Obstet Gynecol . 1993 Aug. 82(2):306-12. [QxMD MEDLINE Link] .
Zielbauer AS, Louwen F, Jennewein L. External cephalic version at 38 weeks' gestation at a specialized German single center. PLoS One . 2021. 16 (8):e0252702. [QxMD MEDLINE Link] . [Full Text] .
Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev . 2015 Apr 1. 4:CD000083. [QxMD MEDLINE Link] .
de Hundt M, Velzel J, de Groot CJ, Mol BW, Kok M. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol . 2014 Jun. 123 (6):1327-34. [QxMD MEDLINE Link] .
de Hundt M, Vlemmix F, Bais JM, de Groot CJ, Mol BW, Kok M. Risk factors for cesarean section and instrumental vaginal delivery after successful external cephalic version. J Matern Fetal Neonatal Med . 2016 Jun. 29 (12):2005-7. [QxMD MEDLINE Link] .
Cook HA. Experience with external cephalic version and selective vaginal breech delivery in private practice. Am J Obstet Gynecol . 1993 Jun. 168(6 Pt 1):1886-9; discussion 1889-90. [QxMD MEDLINE Link] .
Gifford DS, Keeler E, Kahn KL. Reductions in cost and cesarean rate by routine use of external cephalic version: a decision analysis. Obstet Gynecol . 1995 Jun. 85(6):930-6. [QxMD MEDLINE Link] .
Practice Bulletin No. 161 Summary: External Cephalic Version. Obstet Gynecol . 2016 Feb. 127 (2):412-3. [QxMD MEDLINE Link] .
[Guideline] External Cephalic Version: ACOG Practice Bulletin, Number 221. Obstet Gynecol . 2020 May. 135 (5):e203-e212. [QxMD MEDLINE Link] .
Hutton E, Hannah M, Ross S, Delisle MF, Carson G, Windrim R, et al. The Early External Cephalic Version (ECV) 2 Trial: an international multicentre randomised controlled trial of timing of ECV for breech pregnancies. BJOG . 2011 Apr. 118(5):564-577. [QxMD MEDLINE Link] .
Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev . 2015 Jul 29. 7:CD000084. [QxMD MEDLINE Link] .
Flamm BL, Fried MW, Lonky NM, Giles WS. External cephalic version after previous cesarean section. Am J Obstet Gynecol . 1991 Aug. 165(2):370-2. [QxMD MEDLINE Link] .
de Meeus JB, Ellia F, Magnin G. External cephalic version after previous cesarean section: a series of 38 cases. Eur J Obstet Gynecol Reprod Biol . 1998 Oct. 81 (1):65-8. [QxMD MEDLINE Link] .
Burgos J, Cobos P, Rodríguez L, Osuna C, Centeno MM, Martínez-Astorquiza T, et al. Is external cephalic version at term contraindicated in previous caesarean section? A prospective comparative cohort study. BJOG . 2014 Jan. 121 (2):230-5; discussion 235. [QxMD MEDLINE Link] .
Ferguson JE 2nd, Dyson DC. Intrapartum external cephalic version. Am J Obstet Gynecol . 1985 Jun 1. 152(3):297-8. [QxMD MEDLINE Link] .
Marquette GP, Boucher M, Theriault D, Rinfret D. Does the use of a tocolytic agent affect the success rate of external cephalic version?. Am J Obstet Gynecol . 1996 Oct. 175(4 Pt 1):859-61. [QxMD MEDLINE Link] .
Cluver C, Gyte GM, Sinclair M, Dowswell T, Hofmeyr GJ. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev . 2015 Feb 9. 2:CD000184. [QxMD MEDLINE Link] .
Wilcox CB, Nassar N, Roberts CL. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG . 2011 Mar. 118 (4):423-8. [QxMD MEDLINE Link] .
Carlan SJ, Dent JM, Huckaby T, Whittington EC, Shaefer D. The effect of epidural anesthesia on safety and success of external cephalic version at term. Anesth Analg . 1994 Sep. 79(3):525-8. [QxMD MEDLINE Link] .
Schorr SJ, Speights SE, Ross EL, et al. A randomized trial of epidural anesthesia to improve external cephalic version success. Am J Obstet Gynecol . 1997 Nov. 177(5):1133-7. [QxMD MEDLINE Link] .
Dugoff L, Stamm CA, Jones OW 3rd, Mohling SI, Hawkins JL. The effect of spinal anesthesia on the success rate of external cephalic version: a randomized trial. Obstet Gynecol . 1999 Mar. 93(3):345-9. [QxMD MEDLINE Link] .
Weiniger CF, Ginosar Y, Elchalal U, Sharon E, Nokrian M, Ezra Y. External cephalic version for breech presentation with or without spinal analgesia in nulliparous women at term: a randomized controlled trial. Obstet Gynecol . 2007 Dec. 110(6):1343-50. [QxMD MEDLINE Link] .
Johnson RL, Elliott JP. Fetal acoustic stimulation, an adjunct to external cephalic version: a blinded, randomized crossover study. Am J Obstet Gynecol . 1995 Nov. 173(5):1369-72. [QxMD MEDLINE Link] .
Benifla JL, Goffinet F, Darai E, Madelenat P. Antepartum transabdominal amnioinfusion to facilitate external cephalic version after initial failure. Obstet Gynecol . 1994 Dec. 84(6):1041-2. [QxMD MEDLINE Link] .
Adama van Scheltema PN, Feitsma AH, Middeldorp JM, Vandenbussche FP, Oepkes D. Amnioinfusion to facilitate external cephalic version after initial failure. Obstet Gynecol . 2006 Sep. 108(3 Pt 1):591-2. [QxMD MEDLINE Link] .
Egge T, Schauberger C, Schaper A. Dysfunctional labor after external cephalic version. Obstet Gynecol . 1994 May. 83(5 Pt 1):771-3. [QxMD MEDLINE Link] .
Lau TK, Lo KW, Rogers M. Pregnancy outcome after successful external cephalic version for breech presentation at term. Am J Obstet Gynecol . 1997 Jan. 176(1 Pt 1):218-23. [QxMD MEDLINE Link] .
Burgos J, Iglesias M, Pijoan JI, Rodriguez L, Fernández-Llebrez L, Martínez-Astorquiza T. Probability of cesarean delivery after successful external cephalic version. Int J Gynaecol Obstet . 2015 Nov. 131 (2):192-5. [QxMD MEDLINE Link] .
Deering S, Brown J, Hodor J, Satin AJ. Simulation training and resident performance of singleton vaginal breech delivery. Obstet Gynecol . 2006 Jan. 107(1):86-9. [QxMD MEDLINE Link] .
- Footling breech presentation. Once the feet have delivered, one may be tempted to pull on the feet. However, a singleton gestation should not be pulled by the feet because this action may precipitate head entrapment in an incompletely dilated cervix or may precipitate nuchal arms. As long as the fetal heart rate is stable and no physical evidence of a prolapsed cord is evident, management may be expectant while awaiting full cervical dilation.
- Assisted vaginal breech delivery. Thick meconium passage is common as the breech is squeezed through the birth canal. This is usually not associated with meconium aspiration because the meconium passes out of the vagina and does not mix with the amniotic fluid.
- Assisted vaginal breech delivery. The Ritgen maneuver is applied to take pressure off the perineum during vaginal delivery. Episiotomies are often performed for assisted vaginal breech deliveries, even in multiparous women, to prevent soft tissue dystocia.
- Assisted vaginal breech delivery. No downward or outward traction is applied to the fetus until the umbilicus has been reached.
- Assisted vaginal breech delivery. With a towel wrapped around the fetal hips, gentle downward and outward traction is applied in conjunction with maternal expulsive efforts until the scapula is reached. An assistant should be applying gentle fundal pressure to keep the fetal head flexed.
- Assisted vaginal breech delivery. After the scapula is reached, the fetus should be rotated 90° in order to deliver the anterior arm.
- Assisted vaginal breech delivery. The anterior arm is followed to the elbow, and the arm is swept out of the vagina.
- Assisted vaginal breech delivery. The fetus is rotated 180°, and the contralateral arm is delivered in a similar manner as the first. The infant is then rotated 90° to the backup position in preparation for delivery of the head.
- Assisted vaginal breech delivery. The fetal head is maintained in a flexed position by using the Mauriceau maneuver, which is performed by placing the index and middle fingers over the maxillary prominence on either side of the nose. The fetal body is supported in a neutral position, with care to not overextend the neck.
- Piper forceps application. Piper forceps are specialized forceps used only for the after-coming head of a breech presentation. They are used to keep the fetal head flexed during extraction of the head. An assistant is needed to hold the infant while the operator gets on one knee to apply the forceps from below.
- Assisted vaginal breech delivery. Low 1-minute Apgar scores are not uncommon after a vaginal breech delivery. A pediatrician should be present for the delivery in the event that neonatal resuscitation is needed.
- Assisted vaginal breech delivery. The neonate after birth.
- Ultrasound demonstrating a fetus in breech presentation with a hyperextended head (ie, "star gazing").
Contributor Information and Disclosures
Richard Fischer, MD Professor, Division Head, Department of Obstetrics and Gynecology, Division of Maternal-Fetal Medicine, Cooper University Hospital Richard Fischer, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Association of Professors of Gynecology and Obstetrics , Society for Maternal-Fetal Medicine Disclosure: Stock ownership for: Pfizer Pharmaceuticals (< 5% of portfolio); Johnson & Johnson (< 5% of portfolio).
Alisa B Modena, MD, FACOG Assistant Professor, Cooper Medical School of Rowan University; Attending Physician, Division of Maternal-Fetal Medicine, Cooper University Hospital Alisa B Modena, MD, FACOG is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Philadelphia Perinatal Society, Society for Maternal-Fetal Medicine Disclosure: Nothing to disclose.
Francisco Talavera, PharmD, PhD Adjunct Assistant Professor, University of Nebraska Medical Center College of Pharmacy; Editor-in-Chief, Medscape Drug Reference Disclosure: Received salary from Medscape for employment. for: Medscape.
Richard S Legro, MD Professor, Department of Obstetrics and Gynecology, Division of Reproductive Endocrinology, Pennsylvania State University College of Medicine; Consulting Staff, Milton S Hershey Medical Center Richard S Legro, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , Society of Reproductive Surgeons , American Society for Reproductive Medicine , Endocrine Society , Phi Beta Kappa Disclosure: Received honoraria from Korea National Institute of Health and National Institute of Health (Bethesda, MD) for speaking and teaching; Received honoraria from Greater Toronto Area Reproductive Medicine Society (Toronto, ON, CA) for speaking and teaching; Received honoraria from American College of Obstetrics and Gynecologists (Washington, DC) for speaking and teaching; Received honoraria from National Institute of Child Health and Human Development Pediatric and Adolescent Gynecology Research Thi.
Ronald M Ramus, MD Professor of Obstetrics and Gynecology, Director, Division of Maternal-Fetal Medicine, Virginia Commonwealth University School of Medicine Ronald M Ramus, MD is a member of the following medical societies: American College of Obstetricians and Gynecologists , American Institute of Ultrasound in Medicine , Medical Society of Virginia , Society for Maternal-Fetal Medicine Disclosure: Nothing to disclose.
What would you like to print?
- Print this section
- Print the entire contents of
- Print the entire contents of article

- HIV in Pregnancy
- Pulmonary Disease and Pregnancy
- Kidney Disease and Pregnancy
- Vaccinations/Immunizations During Pregnancy
- Anemia and Thrombocytopenia in Pregnancy
- Shock and Pregnancy
- Multifetal Pregnancy
- Is immunotherapy for cancer safe in pregnancy?
- Are Nicotine Patches and E-Cigarettes Safe in Pregnancy?
- Prenatal Exercise Cuts Common Pregnancy Complications

- Drug Interaction Checker
- Pill Identifier
- Calculators

- 2020/viewarticle/immunotherapy-cancer-safe-pregnancy-2024a100083dnews news Is immunotherapy for cancer safe in pregnancy?

- 2002261369-overviewDiseases & Conditions Diseases & Conditions Postterm Pregnancy


- Pregnancy Classes

Breech Births
In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby’s buttocks, feet, or both are positioned to come out first during birth. This happens in 3–4% of full-term births.
What are the different types of breech birth presentations?
- Complete breech: Here, the buttocks are pointing downward with the legs folded at the knees and feet near the buttocks.
- Frank breech: In this position, the baby’s buttocks are aimed at the birth canal with its legs sticking straight up in front of his or her body and the feet near the head.
- Footling breech: In this position, one or both of the baby’s feet point downward and will deliver before the rest of the body.
What causes a breech presentation?
The causes of breech presentations are not fully understood. However, the data show that breech birth is more common when:
- You have been pregnant before
- In pregnancies of multiples
- When there is a history of premature delivery
- When the uterus has too much or too little amniotic fluid
- When there is an abnormally shaped uterus or a uterus with abnormal growths, such as fibroids
- The placenta covers all or part of the opening of the uterus placenta previa
How is a breech presentation diagnosed?
A few weeks prior to the due date, the health care provider will place her hands on the mother’s lower abdomen to locate the baby’s head, back, and buttocks. If it appears that the baby might be in a breech position, they can use ultrasound or pelvic exam to confirm the position. Special x-rays can also be used to determine the baby’s position and the size of the pelvis to determine if a vaginal delivery of a breech baby can be safely attempted.
Can a breech presentation mean something is wrong?
Even though most breech babies are born healthy, there is a slightly elevated risk for certain problems. Birth defects are slightly more common in breech babies and the defect might be the reason that the baby failed to move into the right position prior to delivery.
Can a breech presentation be changed?
It is preferable to try to turn a breech baby between the 32nd and 37th weeks of pregnancy . The methods of turning a baby will vary and the success rate for each method can also vary. It is best to discuss the options with the health care provider to see which method she recommends.
Medical Techniques
External Cephalic Version (EVC) is a non-surgical technique to move the baby in the uterus. In this procedure, a medication is given to help relax the uterus. There might also be the use of an ultrasound to determine the position of the baby, the location of the placenta and the amount of amniotic fluid in the uterus.
Gentle pushing on the lower abdomen can turn the baby into the head-down position. Throughout the external version the baby’s heartbeat will be closely monitored so that if a problem develops, the health care provider will immediately stop the procedure. ECV usually is done near a delivery room so if a problem occurs, a cesarean delivery can be performed quickly. The external version has a high success rate and can be considered if you have had a previous cesarean delivery.
ECV will not be tried if:
- You are carrying more than one fetus
- There are concerns about the health of the fetus
- You have certain abnormalities of the reproductive system
- The placenta is in the wrong place
- The placenta has come away from the wall of the uterus ( placental abruption )
Complications of EVC include:
- Prelabor rupture of membranes
- Changes in the fetus’s heart rate
- Placental abruption
- Preterm labor
Vaginal delivery versus cesarean for breech birth?
Most health care providers do not believe in attempting a vaginal delivery for a breech position. However, some will delay making a final decision until the woman is in labor. The following conditions are considered necessary in order to attempt a vaginal birth:
- The baby is full-term and in the frank breech presentation
- The baby does not show signs of distress while its heart rate is closely monitored.
- The process of labor is smooth and steady with the cervix widening as the baby descends.
- The health care provider estimates that the baby is not too big or the mother’s pelvis too narrow for the baby to pass safely through the birth canal.
- Anesthesia is available and a cesarean delivery possible on short notice
What are the risks and complications of a vaginal delivery?
In a breech birth, the baby’s head is the last part of its body to emerge making it more difficult to ease it through the birth canal. Sometimes forceps are used to guide the baby’s head out of the birth canal. Another potential problem is cord prolapse . In this situation the umbilical cord is squeezed as the baby moves toward the birth canal, thus slowing the baby’s supply of oxygen and blood. In a vaginal breech delivery, electronic fetal monitoring will be used to monitor the baby’s heartbeat throughout the course of labor. Cesarean delivery may be an option if signs develop that the baby may be in distress.
When is a cesarean delivery used with a breech presentation?
Most health care providers recommend a cesarean delivery for all babies in a breech position, especially babies that are premature. Since premature babies are small and more fragile, and because the head of a premature baby is relatively larger in proportion to its body, the baby is unlikely to stretch the cervix as much as a full-term baby. This means that there might be less room for the head to emerge.
Want to Know More?
- Creating Your Birth Plan
- Labor & Birth Terms to Know
- Cesarean Birth After Care
Compiled using information from the following sources:
- ACOG: If Your Baby is Breech
- William’s Obstetrics Twenty-Second Ed. Cunningham, F. Gary, et al, Ch. 24.
- Danforth’s Obstetrics and Gynecology Ninth Ed. Scott, James R., et al, Ch. 21.
BLOG CATEGORIES
- Pregnancy Symptoms 5
- Can I get pregnant if… ? 3
- Paternity Tests 2
- The Bumpy Truth Blog 7
- Multiple Births 10
- Pregnancy Complications 68
- Pregnancy Concerns 62
- Cord Blood 4
- Pregnancy Supplements & Medications 14
- Pregnancy Products & Tests 8
- Changes In Your Body 5
- Health & Nutrition 2
- Labor and Birth 65
- Planning and Preparing 24
- Breastfeeding 29
- Week by Week Newsletter 40
- Is it Safe While Pregnant 55
- The First Year 41
- Genetic Disorders & Birth Defects 17
- Pregnancy Health and Wellness 149
- Your Developing Baby 16
- Options for Unplanned Pregnancy 18
- Child Adoption 19
- Fertility 54
- Pregnancy Loss 11
- Uncategorized 4
- Women's Health 34
- Prenatal Testing 16
- Abstinence 3
- Birth Control Pills, Patches & Devices 21
- Thank You for Your Donation
- Unplanned Pregnancy
- Getting Pregnant
- Healthy Pregnancy
- Privacy Policy
- Pregnancy Questions Center
Share this post:
Similar post.

Episiotomy: Advantages & Complications

Retained Placenta

What is Dilation in Pregnancy?
Track your baby’s development, subscribe to our week-by-week pregnancy newsletter.
- The Bumpy Truth Blog
- Fertility Products Resource Guide
Pregnancy Tools
- Ovulation Calendar
- Baby Names Directory
- Pregnancy Due Date Calculator
- Pregnancy Quiz
Pregnancy Journeys
- Partner With Us
- Corporate Sponsors
What does it mean when a baby is breech?
Signs of a breech baby, why are some babies breech, how to turn a breech baby: is it possible, will i need a c-section if my baby is breech, how to turn a breech baby naturally.
Breech is a term used to describe your baby's position in the womb. Breech position means your baby is bottom-down instead of head-down.
Babies are often active in early pregnancy, moving into different positions. But by around 8 months, there's not much room in the uterus. Most babies maximize their cramped quarters by settling in head down, in what's known as a cephalic or vertex presentation. But if you have a breech baby, it means they're poised to come out buttocks and/or feet first. At 28 weeks or less, about a quarter of babies are breech, and at 32 weeks, 7 percent are breech. By the end of pregnancy, only 3 to 4 percent of babies are in breech position. At term, a baby in breech position is unlikely to turn on their own.
There are several types of breech presentations:
- Frank breech (bottom first with feet up near the head)
- Complete breech (bottom first with legs crossed)
- Incomplete or footling breech (one or both feet are poised to come out first)
(In rare cases, a baby will be sideways in the uterus with their shoulder, back, or arm presenting first – this is called a transverse lie.)
See what these breech presentations look like .
If your baby is in breech position, you may feel them kicking in your lower belly. Or you may feel pressure under your ribcage, from their head.
By the beginning of your third trimester , your practitioner may be able to tell what position your baby is in by feeling your abdomen and locating the baby's head, back, and bottom.
If your baby's position isn't clear during an abdominal exam at 36 weeks, your caregiver may do an internal exam to try to feel what part of the baby is in your pelvis. In some cases, they may use ultrasound to confirm the baby's position.
We don't usually know why some babies are breech – in most cases it seems to be chance. While sometimes a baby with certain birth defects may not turn to a head-down position, most babies in breech position are perfectly fine. Here are some things that might increase the risk of a breech presentation:
- You're carrying multiples
- You've been pregnant before
- You've had a breech presentation before
- There's too much amniotic fluid or not enough amniotic fluid
- You have placenta previa (the placenta is covering all of part of the opening of the uterus)
- Your baby is preterm
- Your uterus is shaped abnormally or has growths, such as fibroids
- The umbilical cord is short
- You were a breech delivery, or your sibling or parent was a breech delivery
- Advanced maternal age (especially age 45 and older)
- Your baby is a low weight at delivery
- You're having a girl
There is a procedure for turning a breech baby. It's called an external cephalic version (ECV). An ob/gyn turns your baby by applying pressure to your abdomen and manually manipulating the baby into a head-down position. Some women find it very uncomfortable or even painful.
An EVC has about a 58 percent success rate, and it's more likely to work if this isn't your first baby. It's not for everyone – you can't have the procedure if you're carrying multiples or if you have too little amniotic fluid or placental abruption , for example. Your provider also won't attempt to turn your breech baby if your baby has any health problems.
The procedure is done after 36 weeks and in the hospital, where your baby can be monitored and where you'll be near a delivery room should any complications arise.
It depends, and it's something you'll want to talk with your caregiver about ahead of time. Discuss your preferences, the advantages and risks of each option ( vaginal and cesarean delivery of a breech presentation), and their experience. The biggest risk of a breech delivery is when the body delivers but the head stays entrapped within the cervix.
In the United States, most breech babies are delivered via cesarean. You may wind up having a vaginal breech delivery if your labor is so rapid that you arrive at the hospital just about to deliver. Another scenario is if you have a twin pregnancy where the first baby is in the head-first position and the second baby is not. A baby who delivers head-first will make room for the breech baby.
However, the vast majority of babies who remain breech arrive by c-section. If a c-section is planned, it will usually be scheduled at 39 weeks. To make sure your baby hasn't changed position in the meantime, you'll have an ultrasound at the hospital to confirm their position just before the surgery.
If you go into labor or your water will break s before your planned c-section, be sure to call your provider right away and head for the hospital.
In rare circumstances, if you're at low risk of complications and your caregiver is experienced delivering breech babies vaginally, you may choose to have what is called a "trial of vaginal birth." This means that you can attempt to deliver vaginally but should be prepared to have a cesarean delivery if labor isn't progressing well. You and your baby will be closely monitored during labor.
In addition to ECV, there are some alternative, natural ways to try to turn your baby. There's no proof that any of them work – or that all of them are safe. Consult your practitioner before trying them.
There's no conclusive proof that the mother's position has any effect on the baby's position, but the idea is to employ gravity to help your baby somersault into a head-down position. A few tips:
- Get into one of the following positions twice a day, starting at around 32 weeks.
- Be sure to do these moves on an empty stomach, lest your lunch comes back up.
- Make sure there's someone around to help you get up if you start feeling lightheaded.
- If you find these positions uncomfortable, stop doing them.
Position 1: Lie flat on your back and raise your pelvis so that it's 9 to 12 inches off the floor. Support your hips with a pillow and stay in this position for five to 15 minutes. Position 2: Kneel down, with your forearms on the floor in front of you, so that your bottom sticks up in the air. Stay in this position for five to 15 minutes. Sleeping position
Many women wonder if there are sleeping positions to turn a breech baby. But the positions you use to try to coax your baby head down for a short time shouldn't be used while you're sleeping. (It's not safe to sleep flat on your back in late pregnancy, for example, because the weight of your baby may compress the blood vessels that provide oxygen and nutrients to them.)
The best position for sleeping during pregnancy is on your side. Placing a pillow between your legs in this position may help open your pelvis, giving your baby room to move more easily. Support your back with plenty of pillows, too. Again, there's no proof that this works, but since it's the best sleeping position for you and your baby, you may as well give it a try.
Moxibustion
This ancient Chinese technique burns herbs to stimulate key acupressure points. To help turn a breech baby, an acupuncturist or other practitioner burns mugwort near the acupressure point of your pinky toes. According to Chinese medicine, this should stimulate your baby's activity enough that they may change position on their own. Some studies show that moxibustion in combination with acupuncture and/or positioning methods may be of some benefit. Others show moxibustion to provide no help in coaxing a baby into cephalic position. If you've discussed it with your caregiver and want to give it a try, contact your state acupuncture or Chinese medicine association and ask for the names of licensed practitioners.
One small study found that women who are regularly hypnotized into a state of deep relaxation at 37 to 40 weeks are more likely to have their baby turn than other women. If you're willing to try this technique, look for a licensed hypnotherapist with experience working with pregnant women.
Chiropractic care
There's a technique – called The Webster Breech Technique – that aims to reduce stress on the pelvis by relaxing the uterus and surrounding ligaments. The idea is that a breech baby can turn more naturally in a relaxed uterus, but research is limited as to the risks and benefits of this technique. If you're interested, talk with your provider about working with a chiropractor who's experienced with the technique.
This is a safe – and again, unproven – method based on the fact that your baby can hear sounds outside the womb. Simply play music close to the lower part of your abdomen (some women use headphones) to encourage your baby to move in the direction of the sound.
Learn more:
- C-section recovery
- Third trimester pregnancy guide and checklist
- Hospital bag checklist
Was this article helpful?
Breech, posterior, transverse lie: What position is my baby in?

9 of the most jaw-dropping breech birth photos

C-section recovery: Timeline, aftercare tips, and expectations

Measuring fundal height during pregnancy

BabyCenter's editorial team is committed to providing the most helpful and trustworthy pregnancy and parenting information in the world. When creating and updating content, we rely on credible sources: respected health organizations, professional groups of doctors and other experts, and published studies in peer-reviewed journals. We believe you should always know the source of the information you're seeing. Learn more about our editorial and medical review policies .
ACOG. 2019. If your baby is breech. FAQ. The American College of Obstetricians and Gynecologists. https://www.acog.org/womens-health/faqs/if-your-baby-is-breech Opens a new window [Accessed November 2021]
ACOG. 2018. Mode of term singleton breech delivery. Committee opinion number 745. The American College of Obstetricians and Gynecologists. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/08/mode-of-term-singleton-breech-delivery Opens a new window [Accessed November 2021]
Brici P et al. 2019. Turning foetal breech presentation at 32-35 weeks of gestational age by acupuncture and moxibustion. Evidence-based Complementary and Alternative Medicine https://www.hindawi.com/journals/ecam/2019/8950924/ Opens a new window [Accessed November 2021]
Ekeus C et al. 2019. Vaginal breech delivery at term and neonatal morbidity and mortality — a population-based cohort study in Sweden. Journal of Maternal Fetal Neonatal Medicine 32(2):265. https://pubmed.ncbi.nlm.nih.gov/28889774/ Opens a new window [Accessed November 2021]
Fruscalzo A et al 2014. New and old predictive factors for breech presentation: our experience in 14433 singleton pregnancies and a literature review. Journal of Maternal Fetal Neonatal Medicine 27(2): 167-72. https://pubmed.ncbi.nlm.nih.gov/23688372/ Opens a new window [Accessed November 2021]
Garcia MM et al. 2019 Effectiveness and safety of acupuncture and moxibustion in pregnant women with noncephalic presentation: An overview of systematic reviews. Evidence Based Complementary Alternative Medicine 7036914. https://pubmed.ncbi.nlm.nih.gov/31885661/ Opens a new window [Accessed November 2021]
Gray C. 2021. Breech presentation. StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK448063/ Opens a new window [Accessed November 2021]
Meaghan M et al. 2021. External cephalic version. NCBI StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK482475/ Opens a new window [Accessed November 2021]
MedlinePlus. 2020. Breech - series - Types of breech presentation. https://medlineplus.gov/ency/presentations/100193_3.htm Opens a new window [Accessed November 2020]
Noli SA et al. 2019. Preterm birth, low gestational age, low birth weight, parity, and other determinants of breech presentation: Results from a large retrospective population-based study. Biomed Research International https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6766171/ Opens a new window [Accessed November 2021]
Pistolese RA. 2002. The Webster Technique: A chiropractic technique with obstetric implications. Journal of Manipulative and Physiological Therapeutics 25(6): E1-9. https://pubmed.ncbi.nlm.nih.gov/12183701/ Opens a new window [Accessed November 2021]

Where to go next

Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
- Management of breech presentation
Evidence review M
NICE Guideline, No. 201
National Guideline Alliance (UK) .
- Copyright and Permissions
Review question
What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy?
Introduction
Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman’s and the baby’s health. The aim of this review is to determine the most effective way of managing a breech presentation in late pregnancy.
Summary of the protocol
Please see Table 1 for a summary of the Population, Intervention, Comparison and Outcome (PICO) characteristics of this review.
Summary of the protocol (PICO table).
For further details see the review protocol in appendix A .
Methods and process
This evidence review was developed using the methods and process described in Developing NICE guidelines: the manual 2014 . Methods specific to this review question are described in the review protocol in appendix A .
Declarations of interest were recorded according to NICE’s conflicts of interest policy .
Clinical evidence
Included studies.
Thirty-six randomised controlled trials (RCTs) were identified for this review.
The included studies are summarised in Table 2 .
Three studies reported on external cephalic version (ECV) versus no intervention ( Dafallah 2004 , Hofmeyr 1983 , Rita 2011 ). One study reported on a 4-arm trial comparing acupuncture, sweeping of fetal membranes, acupuncture plus sweeping, and no intervention ( Andersen 2013 ). Two studies reported on postural management versus no intervention ( Chenia 1987 , Smith 1999 ).
Seven studies reported on ECV plus anaesthesia ( Chalifoux 2017 , Dugoff 1999 , Khaw 2015 , Mancuso 2000 , Schorr 1997 , Sullivan 2009 , Weiniger 2010 ). Of these studies, 1 study compared ECV plus anaesthesia to ECV plus other dosages of the same anaesthetic ( Chalifoux 2017 ); 4 studies compared ECV plus anaesthesia to ECV only ( Dugoff 1999 , Mancuso 2000 , Schorr 1997 , Weiniger 2010 ); and 2 studies compared ECV plus anaesthesia to ECV plus a different anaesthetic ( Khaw 2015 , Sullivan 2009 ).
Ten studies reported ECV plus a β2 receptor agonist ( Brocks 1984 , Fernandez 1997 , Hindawi 2005 , Impey 2005 , Mahomed 1991 , Marquette 1996 , Nor Azlin 2005 , Robertson 1987 , Van Dorsten 1981 , Vani 2009 ). Of these studies, 5 studies compared ECV plus a β2 receptor agonist to ECV plus placebo ( Fernandez 1997 , Impey 2005 , Marquette 1996 , Nor Azlin 2005 , Vani 2009 ); 1 study compared ECV plus a β2 receptor agonist to ECV alone ( Robertson 1987 ); and 4 studies compared ECV plus a β2 receptor agonist to no intervention ( Brocks 1984 , Hindawi 2005 , Mahomed 1991 , Van Dorsten 1981 ).
One study reported on ECV plus Ca 2+ channel blocker versus ECV plus placebo ( Kok 2008 ). Two studies reported on ECV plus β2 receptor agonist versus ECV plus Ca 2+ channel blocker ( Collaris 2009 , Mohamed Ismail 2008 ). Four studies reported on ECV plus a µ-receptor agonist ( Burgos 2016 , Liu 2016 , Munoz 2014 , Wang 2017 ), of which 3 compared against ECV plus placebo ( Liu 2016 , Munoz 2014 , Wang 2017 ) and 1 compared to ECV plus nitrous oxide ( Burgos 2016 ).
Four studies reported on ECV plus nitroglycerin ( Bujold 2003a , Bujold 2003b , El-Sayed 2004 , Hilton 2009 ), of which 2 compared it to ECV plus β2 receptor agonist ( Bujold 2003b , El-Sayed 2004 ) and compared it to ECV plus placebo ( Bujold 2003a , Hilton 2009 ). One study compared ECV plus amnioinfusion versus ECV alone ( Diguisto 2018 ) and 1 study compared ECV plus talcum powder to ECV plus gel ( Vallikkannu 2014 ).
One study was conducted in Australia ( Smith 1999 ); 4 studies in Canada ( Bujold 2003a , Bujold 2003b , Hilton 2009 , Marquette 1996 ); 2 studies in China ( Liu 2016 , Wang 2017 ); 2 studies in Denmark ( Andersen 2013 , Brocks 1984 ); 1 study in France ( Diguisto 2018 ); 1 study in Hong Kong ( Khaw 2015 ); 1 study in India ( Rita 2011 ); 1 study in Israel ( Weiniger 2010 ); 1 study in Jordan ( Hindawi 2005 ); 5 studies in Malaysia ( Collaris 2009 , Mohamed Ismail 2008 , Nor Azlin 2005 , Vallikkannu 2014 , Vani 2009 ); 1 study in South Africa ( Hofmeyr 1983 ); 2 studies in Spain ( Burgos 2016 , Munoz 2014 ); 1 study in Sudan ( Dafallah 2004 ); 1 study in The Netherlands ( Kok 2008 ); 2 studies in the UK ( Impey 2005 , Chenia 1987 ); 9 studies in US ( Chalifoux 2017 , Dugoff 1999 , El-Sayed 2004 , Fernandez 1997 , Mancuso 2000 , Robertson 1987 , Schorr 1997 , Sullivan 2009 , Van Dorsten 1981 ); and 1 study in Zimbabwe ( Mahomed 1991 ).
The majority of studies were 2-arm trials, but there was one 3-arm trial ( Khaw 2015 ) and two 4-arm trials ( Andersen 2013 , Chalifoux 2017 ). All studies were conducted in a hospital or an outpatient ward connected to a hospital.
See the literature search strategy in appendix B and study selection flow chart in appendix C .
Excluded studies
Studies not included in this review with reasons for their exclusions are provided in appendix K .
Summary of clinical studies included in the evidence review
Summaries of the studies that were included in this review are presented in Table 2 .
Summary of included studies.
See the full evidence tables in appendix D and the forest plots in appendix E .
Quality assessment of clinical outcomes included in the evidence review
See the evidence profiles in appendix F .
Economic evidence
A systematic review of the economic literature was conducted but no economic studies were identified which were applicable to this review question.
A single economic search was undertaken for all topics included in the scope of this guideline. See supplementary material 2 for details.
Economic studies not included in this review are listed, and reasons for their exclusion are provided in appendix K .
Summary of studies included in the economic evidence review
No economic studies were identified which were applicable to this review question.
Economic model
No economic modelling was undertaken for this review because the committee agreed that other topics were higher priorities for economic evaluation.
Evidence statements
Clinical evidence statements, comparison 1. complementary therapy versus control (no intervention), critical outcomes, cephalic presentation in labour.
No evidence was identified to inform this outcome.
Method of birth
Caesarean section.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.74 (95% CI 0.38 to 1.43).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 1.29 (95% CI 0.73 to 2.29).

Admission to SCBU/NICU
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.19 (95% CI 0.02 to 1.62).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.40 (0.08 to 2.01).
Fetal death after 36 +0 weeks gestation
Infant death up to 4 weeks chronological age, important outcomes, apgar score <7 at 5 minutes.
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.32 (95% CI 0.01 to 7.78).
- Very low quality evidence from 1 RCT (N=200) showed that there is no clinically important difference between acupuncture plus membrane sweeping and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.33 (0.01 to 8.09).
Birth before 39 +0 weeks of gestation
Comparison 2. complementary therapy versus other treatment.
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.64 (95% CI 0.34 to 1.22).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 0.57 (95% CI 0.30 to 1.07).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on the number of caesarean sections in pregnant women with breech presentation: RR 1.13 (95% CI 0.66 to 1.94).
- Very low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.33 (95% CI 0.03 to 3.12).
- Very low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.48 (95% CI 0.04 to 5.22).
- Very low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.69 (95% CI 0.12 to 4.02).
- Low quality evidence from 1 RCT (N=207) showed that there is no clinically important difference between acupuncture and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=204) showed that there is no clinically important difference between acupuncture and acupuncture plus membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
- Low quality evidence from 1 RCT (N=203) showed that there is no clinically important difference between acupuncture plus membrane sweeping and membrane sweeping on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 3. ECV versus no ECV
- Moderate quality evidence from 2 RCTs (N=680) showed that there is clinically important difference favouring ECV over no ECV on cephalic presentation in labour in pregnant women with breech presentation: RR 1.83 (95% CI 1.53 to 2.18).
Cephalic vaginal birth
- Very low quality evidence from 3 RCTs (N=740) showed that there is a clinically important difference favouring ECV over no ECV on cephalic vaginal birth in pregnant women with breech presentation: RR 1.67 (95% CI 1.20 to 2.31).
Breech vaginal birth
- Very low quality evidence from 2 RCTs (N=680) showed that there is no clinically important difference between ECV and no ECV on breech vaginal birth in pregnant women with breech presentation: RR 0.29 (95% CI 0.03 to 2.84).
- Very low quality evidence from 3 RCTs (N=740) showed that there is no clinically important difference between ECV and no ECV on the number of caesarean sections in pregnant women with breech presentation: RR 0.52 (95% CI 0.23 to 1.20).
- Very low quality evidence from 1 RCT (N=60) showed that there is no clinically important difference between ECV and no ECV on admission to SCBU//NICU in pregnant women with breech presentation: RR 0.50 (95% CI 0.14 to 1.82).
- Very low evidence from 3 RCTs (N=740) showed that there is no statistically significant difference between ECV and no ECV on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: Peto OR 0.29 (95% CI 0.05 to 1.73) p=0.18.
- Very low quality evidence from 2 RCTs (N=120) showed that there is no clinically important difference between ECV and no ECV on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.28 (95% CI 0.04 to 1.70).
Comparison 4. ECV + Amnioinfusion versus ECV only
- Very low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.74 (95% CI 0.74 to 4.12).
- Low quality evidence from 1 RCT (N=109) showed that there is no clinically important difference between ECV plus amnioinfusion and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.95 (95% CI 0.75 to 1.19).
Comparison 5. ECV + Anaesthesia versus ECV only
- Very low quality evidence from 2 RCTs (N=210) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic presentation in labour in pregnant women with breech presentation: RR 1.16 (95% CI 0.56 to 2.41).
- Very low quality evidence from 5 RCTs (N=435) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.16 (95% CI 0.77 to 1.74).
- Very low quality evidence from 1 RCT (N=108) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on breech vaginal birth in pregnant women with breech presentation: RR 0.33 (95% CI 0.04 to 3.10).
- Very low quality evidence from 3 RCTs (N=263) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 0.76 (95% CI 0.42 to 1.38).
- Moderate quality evidence from 1 RCT (N=69) showed that there is a clinically important difference favouring ECV plus anaesthesia over ECV alone on admission to SCBU/NICU in pregnant women with breech presentation: MD −1.80 (95% CI −2.53 to −1.07).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus anaesthesia and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 6. ECV + Anaesthesia versus ECV + Anaesthesia
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.13 (95% CI 0.73 to 1.74).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 0.05mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.69 (95% CI 0.37 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.81 (95% CI 0.53 to 1.23).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 0.96 (95% CI 0.61 to 1.50).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on cephalic vaginal birth in pregnant women with breech presentation: RR 1.19 (95% CI 0.79 to 1.79).
- Low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.92 (95% CI 0.68 to 1.24).
- Very low evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.08 (95% CI 0.78 to 1.50).
- Very low evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 2.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.70 to 1.28).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.17 (95% CI 0.86 to 1.61).
- Very low quality evidence from 1 RCT (N=120) showed that there is no clinically important difference between ECV plus 5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 1.03 (95% CI 0.77 to 1.37).
- Low quality evidence from 1 RCT (N=119) showed that there is no clinically important difference between ECV plus 7.5mg Bupivacaine plus 0.015mg Fentanyl and ECV plus 10mg Bupivacaine plus 0.015mg Fentanyl on the number of caesarean sections in pregnant women with breech presentation: RR 0.88 (95% CI 0.64 to 1.20).
Comparison 7. ECV + β2 agonist versus Control (no intervention)
- Moderate quality evidence from 2 RCTs (N=256) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on cephalic presentation in labour in pregnant women with breech presentation: RR 4.83 (95% CI 3.27 to 7.11).
- Very low quality evidence from 3 RCTs (N=265) showed that there no clinically important difference between ECV plus β2 agonist and control (no intervention) on cephalic vaginal birth in pregnant women with breech presentation: RR 2.03 (95% CI 0.22 to 19.01).
- Very low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on breech vaginal birth in pregnant women with breech presentation: RR 0.38 (95% CI 0.20 to 0.69).
- Low quality evidence from 4 RCTs (N=513) showed that there is a clinically important difference favouring ECV plus β2 agonist over control (no intervention) on the number of caesarean sections in pregnant women with breech presentation: RR 0.53 (95% CI 0.41 to 0.67).
- Very low quality evidence from 1 RCT (N=48) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on admission to SCBU/NICU in pregnant women with breech presentation: RD 0.00 (95% CI −0.08 to 0.08).
- Very low quality evidence from 3 RCTs (N=208) showed that there is no statistically significant difference between ECV plus β2 agonist and control (no intervention) on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD −0.01 (95% CI −0.03 to 0.01) p=0.66.
- Very low quality evidence from 2 RCTs (N=208) showed that there is no clinically important difference between ECV plus β2 agonist and control (no intervention) on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.80 (95% CI 0.31 to 2.10).
Comparison 8. ECV + β2 agonist versus ECV only
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on cephalic vaginal birth in pregnant women with breech presentation: RR 1.32 (95% CI 0.67 to 2.62).
- Very low quality evidence from 1 RCT (N=58) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on breech vaginal birth in pregnant women with breech presentation: RR 0.75 (95% CI 0.22 to 2.50).
- Very low quality evidence from 2 RCTs (N=172) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 0.79 (95% CI 0.27 to 2.28).
- Very low quality evidence from 1 RCT (N=114) showed that there is no clinically important difference between ECV plus β2 agonist and ECV only on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.00 (95% CI 0.21 to 4.75).
Comparison 9. ECV + β2 agonist versus ECV + Placebo
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.54 (95% CI 0.24 to 9.76).
- Very low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 1.27 (95% CI 0.41 to 3.89).
- Very low quality evidence from 2 RCTs (N=227) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on breech vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.33 to 2.97).
- Low quality evidence from 4 RCTs (N=532) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.81 (95% CI 0.72 to 0.92)
- Very low quality evidence from 2 RCTs (N=146) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: RR 0.78 (95% CI 0.17 to 3.63).
- Very low quality evidence from 1 RCT (N=124) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 10. ECV + Ca 2+ channel blocker versus ECV + Placebo
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.87 to 1.48).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.90 (95% CI 0.73 to 1.12).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 1.11 (95% CI 0.88 to 1.40).
- High quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on admission to SCBU/NICU in pregnant women with breech presentation: MD −0.20 (95% CI −0.70 to 0.30).
- Moderate quality evidence from 1 RCT (N=310) showed that there is no statistically significant difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.01 to 0.01) p=1.00.
- Low quality evidence from 1 RCT (N=310) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus placebo on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.52 (95% 0.05 to 5.02).
Comparison 11. ECV + Ca2+ channel blocker versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=90) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on cephalic presentation in labour in pregnant women with breech presentation: RR 0.62 (95% CI 0.39 to 0.98).
- Very low quality evidence from 2 RCTs (N=126) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 1.26 (95% CI 0.55 to 2.89).
- Very low quality evidence from 2 RCTs (N=132) showed that there is a clinically important difference favouring ECV plus β2 agonist over ECV plus Ca 2+ channel blocker on the number of caesarean sections in pregnant women with breech presentation: RR 1.42 (95% CI 1.06 to 1.91).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on admission to SCBU/NICU in pregnant women with breech presentation: Peto OR 0.53 (95% CI 0.05 to 5.22).
- Very low quality evidence from 2 RCTs (N=176) showed that there is no clinically important difference between ECV plus Ca 2+ channel blocker and ECV plus β2 agonist on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 12. ECV + µ-receptor agonist versus ECV only
- High quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on cephalic vaginal birth in pregnant women with breech presentation: RR 1.00 (95% CI 0.80 to 1.24).
- Low quality evidence from 1 RCT (N=80) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on the number of caesarean sections in pregnant women with breech presentation: RR 1.00 (95% CI 0.42 to 2.40).
- Low quality evidence from 1 RCT (N=126) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV alone on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03).
Comparison 13. ECV + µ-receptor agonist versus ECV + Placebo
Cephalic vaginal birth after successful ecv.
- High quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on cephalic vaginal birth after successful ECV in pregnant women with breech presentation: RR 1.00 (95% CI 0.86 to 1.17).
Caesarean section after successful ECV
- Low quality evidence from 2 RCTs (N=98) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after successful ECV in pregnant women with breech presentation: RR 0.97 (95% CI 0.33 to 2.84).
Breech vaginal birth after unsuccessful ECV
- High quality evidence from 3 RCTs (N=186) showed that there is a clinically important difference favouring ECV plus µ-receptor agonist over ECV plus placebo on breech vaginal birth after unsuccessful ECV in pregnant women with breech presentation: RR 0.10 (95% CI 0.02 to 0.53).
Caesarean section after unsuccessful ECV
- Moderate quality evidence from 3 RCTs (N=186) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus placebo on caesarean section after unsuccessful ECV in pregnant women with breech presentation: RR 1.19 (95% CI 1.09 to 1.31).
- Low quality evidence from 1 RCT (N=137) showed that there is no statistically significant difference between ECV plus µ-receptor agonist and ECV plus placebo on fetal death after 36 +0 weeks gestation in pregnant women with breech presentation: RD 0.00 (95% CI −0.03 to 0.03) p=1.00.
Comparison 14. ECV + µ-receptor agonist versus ECV + Anaesthesia
- Moderate quality evidence from 1 RCT (N=92) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on cephalic vaginal birth in pregnant women with breech presentation: RR 1.04 (95% CI 0.84 to 1.29).
- Very low quality evidence from 2 RCTs (N=212) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on the number of caesarean sections in pregnant women with breech presentation: RR 0.90 (95% CI 0.61 to 1.34).
- Very low quality evidence from 1 RCT (N=129) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on admission to SCBU/NICU in pregnant women with breech presentation: RR 2.30 (95% CI 0.21 to 24.74).
- Low quality evidence from 2 RCTs (N=255) showed that there is no clinically important difference between ECV plus µ-receptor agonist and ECV plus anaesthesia on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RD 0.00 (95% CI −0.02 to 0.02).
Comparison 15. ECV + Nitric oxide donor versus ECV + Placebo
- Very low quality evidence from 3 RCTs (N=224) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic presentation in labour in pregnant women with breech presentation: RR 1.13 (95% CI 0.59 to 2.16).
- Low quality evidence from 1 RCT (N=99) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on cephalic vaginal birth in pregnant women with breech presentation: RR 0.78 (95% CI 0.49 to 1.22).
- Low quality evidence from 2 RCTs (N=125) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus placebo on the number of caesarean sections in pregnant women with breech presentation: RR 0.83 (95% CI 0.68 to 1.01).
Comparison 16. ECV + Nitric oxide donor versus ECV + β2 agonist
- Low quality evidence from 1 RCT (N=74) showed that there is no clinically important difference between ECV plus β2 agonist and ECV plus nitric oxide donor on cephalic presentation in labour in pregnant women with breech presentation: RR 0.56 (95% CI 0.29 to 1.09).
- Very low quality evidence from 2 RCTs (N=97) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on cephalic vaginal birth in pregnant women with breech presentation: RR 0.98 (95% CI 0.47 to 2.05).
- Very low quality evidence from 1 RCT (N=59) showed that there is no clinically important difference between ECV plus nitric oxide donor and ECV plus β2 agonist on the number of caesarean sections in pregnant women with breech presentation: RR 1.07 (95% CI 0.73 to 1.57).
Comparison 17. ECV + Talcum powder versus ECV + Gel
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic presentation in labour in pregnant women with breech presentation: RR 1.02 (95% CI 0.68 to 1.53).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on cephalic vaginal birth in pregnant women with breech presentation: RR 1.08 (95% CI 0.67 to 1.74).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on the number of caesarean sections in pregnant women with breech presentation: RR 0.94 (95% CI 0.67 to 1.33).
- Low quality evidence from 1 RCT (N=95) showed that there is no clinically important difference between ECV plus talcum powder and ECV plus gel on admission to SCBU/NICU in pregnant women with breech presentation: RR 1.96 (95% CI 0.38 to 10.19).
Comparison 18. Postural management versus No postural management
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic presentation in labour in pregnant women with breech presentation: RR 1.26 (95% CI 0.70 to 2.30).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on cephalic vaginal birth in pregnant women with breech presentation: RR 1.11 (95% CI 0.59 to 2.07).
Breech vaginal delivery
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on breech vaginal delivery in pregnant women with breech presentation: RR 1.15 (95% CI 0.67 to 1.99).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on the number of caesarean sections in pregnant women with breech presentation: RR 0.69 (95% CI 0.31 to 1.52).
- Low quality evidence from 1 RCT (N=76) showed that there is no clinically important difference between postural management and no postural management on Apgar score <7 at 5 minutes in pregnant women with breech presentation: RR 0.24 (95% CI 0.03 to 2.03).
Comparison 19. Postural management + ECV versus ECV only
- Moderate quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on the number of caesarean sections in pregnant women with breech presentation: RR 1.05 (95% CI 0.80 to 1.38).
- Low quality evidence from 1 RCT (N=100) showed that there is no clinically important difference between postural management plus ECV and ECV only on Apgar score <7 at 5 minutes in pregnant women with breech presentation: Peto OR 0.13 (95% CI 0.00 to 6.55).
Economic evidence statements
No economic evidence was identified which was applicable to this review question.
The committee’s discussion of the evidence
Interpreting the evidence, the outcomes that matter most.
Provision of antenatal care is important for the health and wellbeing of both mother and baby with the aim of avoiding adverse pregnancy outcomes and enhancing maternal satisfaction and wellbeing. Breech presentation in labour may be associated with adverse outcomes for the fetus, which has contributed to an increased likelihood of caesarean birth. The committee therefore agreed that cephalic presentation in labour and method of birth were critical outcomes for the woman, and admission to SCBU/NICU, fetal death after 36 +0 weeks gestation, and infant death up to 4 weeks chronological age were critical outcomes for the baby. Apgar score <7 at 5 minutes and birth before 39 +0 weeks of gestation were important outcomes for the baby.
The quality of the evidence
The quality of the evidence for interventions for managing a longitudinal lie fetal malpresentation (that is breech presentation) in late pregnancy ranged from very low to high, with most of the evidence being of a very low or low quality.
This was predominately due to serious overall risk of bias in some outcomes; imprecision around the effect estimate in some outcomes; indirect population in some outcomes; and the presence of serious heterogeneity in some outcomes, which was unresolved by subgroup analysis. The majority of included studies had a small sample size, which contributed to imprecision around the effect estimate.
No evidence was identified to inform the outcomes of infant death up to 4 weeks chronological age and birth before 39 +0 weeks of gestation.
There was no publication bias identified in the evidence. However, the committee noted the influence pharmacological developers may have in these trials as funders, and took this into account in their decision making.
Benefits and harms
The committee discussed that in the case of breech presentation, a discussion with the woman about the different options and their potential benefits, harms and implications is needed to ensure an informed decision. The committee discussed that some women may prefer a breech vaginal birth or choose an elective caesarean birth, and that her preferences should be supported, in line with shared decision making.
The committee discussed that external cephalic version is standard practice for managing breech presentation in uncomplicated singleton pregnancies at or after 36+0 weeks. The committee discussed that there could be variation in the success rates of ECV based on the experience of the healthcare professional providing the ECV. There was some evidence supporting the use of ECV for managing a breech presentation in late pregnancy. The evidence showed ECV had a clinically important benefit in terms of cephalic presentations in labour and cephalic vaginal deliveries, when compared to no intervention. The committee noted that the evidence suggested that ECV was not harmful to the baby, although the effect estimate was imprecise relating to the relative rarity of the fetal death as an outcome.
Cephalic (head-down) vaginal birth is preferred by many women and the evidence suggests that external cephalic version is an effective way to achieve this. The evidence suggested ECV increased the chance for a cephalic vaginal birth and the committee agreed that it was important to explain this to the woman during her consultation.
The committee discussed the optimum timing for ECV. Timing of ECV must take into account the likelihood of the baby turning naturally before a woman commences labour and the possibility of the baby turning back to a breech presentation after ECV if it is done too early. The committee noted that in their experience, current practice was to perform ECV at 37 gestational weeks. The majority of the evidence demonstrating a benefit of ECV in this review involved ECV performed around 37 gestational weeks, although the review did not look for studies directly comparing different timings of ECV and their relative success rates.
The evidence in this review excluded women with previous complicated pregnancies, such as those with previous caesarean section or uterine surgery. The committee discussed that a previous caesarean section indicates a complicated pregnancy and that this population of women are not the focus of this guideline, which concentrates on women with uncomplicated pregnancies.
The committee’s recommendations align with other NICE guidance and cross references to the NICE guideline on caesarean birth and the section on breech presenting in labour in the NICE guideline on intrapartum care for women with existing medical conditions or obstetric complications and their babies were made.
ECV combined with pharmacological agents
There were some small studies comparing a variety of pharmacological agents (including β2 agonists, Ca 2+ channel blockers, µ-receptor agonists and nitric oxide donors) given alongside ECV. Overall the evidence typically showed no clinically important benefit of adding any pharmacological agent to ECV except in comparisons with a control arm with no ECV where it was not possible to isolate the effect of the ECV versus the pharmacological agent. The evidence tended toward benefit most for β2 agonists and µ-receptor agonists however there was no consistent or high quality evidence of benefit even for these agents. The committee agreed that although these pharmacological agents are used in practice, there was insufficient evidence to make a recommendation supporting or refuting their use or on which pharmacological agent should be used.
The committee discussed that the evidence suggesting µ-receptor agonist, remifentanil, had a clinically important benefit in terms reducing breech vaginal births after unsuccessful ECV was biologically implausible. The committee noted that this pharmacological agent has strong sedative effects, depending on the dosage, and therefore studies comparing it to a placebo had possible design flaws as it would be obvious to all parties whether placebo or active drug had been received. The committee discussed that the risks associated with using remifentanil such as respiratory depression, likely outweigh any potential added benefit it may have on managing breech presentation.
There was some evidence comparing different anaesthetics together with ECV. Although there was little consistent evidence of benefit overall, one small study of low quality showed a combination of 2% lidocaine and epinephrine via epidural catheter (anaesthesia) with ECV showed a clinically important benefit in terms of cephalic presentations in labour and the method of birth. The committee discussed the evidence and agreed the use of anaesthesia via epidural catheter during ECV was uncommon practice in the UK and could be expensive, overall they agreed the strength of the evidence available was insufficient to support a change in practice.
Postural management
There was limited evidence on postural management as an intervention for managing breech presentation in late pregnancy, which showed no difference in effectiveness. Postural management was defined as ‘knee-chest position for 15 minutes, 3 times a day’. The committee agreed that in their experience women valued trying interventions at home first which might make postural management an attractive option for some women, however, there was no evidence that postural management was beneficial. The committee also noted that in their experience postural management can cause notable discomfort so it is not an intervention without disadvantages.
Cost effectiveness and resource use
A systematic review of the economic literature was conducted but no relevant studies were identified which were applicable to this review question.
The committee’s recommendations to offer external cephalic version reinforces current practice. The committee noted that, compared to no intervention, external cephalic version results in clinically important benefits and that there would also be overall downstream cost savings from lower adverse events. It was therefore the committee’s view that offering external cephalic version is cost effective and would not entail any resource impact.
Andersen 2013
Brocks 1984
Bujold 2003
Burgos 2016
Chalifoux 2017
Chenia 1987
Collaris 2009
Dafallah 2004
Diguisto 2018
Dugoff 1999
El-Sayed 2004
Fernandez 1997
Hindawi 2005
Hilton 2009
Hofmeyr 1983
Mahomed 1991
Mancuso 2000
Marquette 1996
Mohamed Ismail 2008
NorAzlin 2005
Robertson 1987
Schorr 1997
Sullivan 2009
VanDorsten 1981
Vallikkannu 2014
Weiniger 2010
Appendix A. Review protocols
Review protocol for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 260K)
Appendix B. Literature search strategies
Literature search strategies for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 281K)
Appendix C. Clinical evidence study selection
Clinical study selection for: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 113K)
Appendix D. Clinical evidence tables
Clinical evidence tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.2M)
Appendix E. Forest plots
Forest plots for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 678K)
Appendix F. GRADE tables
GRADE tables for review question: What is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy? (PDF, 1.0M)
Appendix G. Economic evidence study selection
Economic evidence study selection for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix h. economic evidence tables, economic evidence tables for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix i. economic evidence profiles, economic evidence profiles for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, appendix j. economic analysis, economic evidence analysis for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No economic analysis was conducted for this review question.
Appendix K. Excluded studies
Excluded clinical and economic studies for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy, clinical studies, table 24 excluded studies.
View in own window
| Study | Reason for exclusion |
|---|---|
| Ahmed, R. J., Gafni, A., Hutton, E. K., Early, E. C. V.Trial Collaborative Group, The Cost Implications in Ontario, Alberta, and British Columbia of Early Versus Delayed External Cephalic Version in the Early External Cephalic Version 2 (EECV2) Trial, Journal of Obstetrics & Gynaecology Canada: JOGCJ Obstet Gynaecol Can, 38, 235–245.e3, 2016 [ ] | HE analysis. |
| Akhtar,N., Early versus late external cephalic version, Journal of Postgraduate Medical Institute, 27, 164–169, 2013 | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36 0 weeks. |
| Albaladejo, M. I., Esquius, N. P., Trabado, C. R., Sabate, G. S., Marmol, R. U., Ventura, C. V., Brito, M. Z., Torres, M. D., Evaluation of the effectiveness of the moxibustion in non-cephalic presentations in pregnant women assisted in Primary Care, Matronas profesion, 18, 27–33, 2017 | This study is not available in English. |
| American College of, Obstetricians, Gynecologists’ Committee on Practice, Bulletins-Obstetrics, Practice Bulletin No. 161 Summary: External Cephalic Version, Obstetrics & GynecologyObstet Gynecol, 127, 412–3, 2016 [ ] | Duplicate. |
| Annapoorna,V., Arulkumaran,S., Anandakumar,C., Chua,S., Montan,S., Ratnam,S.S., External cephalic version at term with tocolysis and vibroacoustic stimulation, International Journal of Gynaecology and Obstetrics, 59, 13–18, 1997 [ ] | Study design is a non-randomised trial. |
| Bolaji, I., Alabi-Isama, L., Central neuraxial blockade-assisted external cephalic version in reducing caesarean section rate: systematic review and meta-analysis, Obstetrics & Gynecology International, 2009, 718981, 2009 [ ] [ ] | Systematic review for ECV anaesthesia. Relevant references examined and included if appropriate. |
| Bue, L., Lauszus, F. F., Moxibustion did not have an effect in a randomised clinical trial for version of breech position, Danish Medical JournalDan Med J, 63, 2016 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| CardiniF, Weixin, H, Moxibustion for correction of breech presentation: a randomized controlled trial, JAMA, 280, 1580–4, 1998 [ ] | Duplicate. |
| Cardini, F., Lombardo, P., Regalia, A. L., Regaldo, G., Zanini, A., Negri, M. G., Panepuccia, L., Todros, T., A randomised controlled trial of moxibustion for breech presentation, BJOG, 112, 743–747, 2005 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Cardini, F., Weixin, H., Moxibustion for correction of breech presentation: a randomized controlled trial, JamaJama, 280, 1580–4, 1998 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Carvalho, B., Tan, J. M., MacArio, A., El-Sayed, Y. Y., Sultan, P., A cost analysis of neuraxial anesthesia to facilitate external cephalic version for breech fetal presentation, Anesthesia and Analgesia, 117, 155–159, 2013 [ ] | HE analysis. |
| Chi, Ctr Trc, External cephalic version for breech presentation: a randomised controlled trial of anaesthetic interventions, .who.int/trialsearch/trial2 .aspx?Trialid =chictr-trc-12002644, 2012 | No full text available. |
| Chung, T., Neale, E., Lau, T. K., Rogers, M., A randomized, double blind, controlled trial of tocolysis to assist external cephalic version in late pregnancy, Acta Obstet Gynecol ScandActa obstetricia et gynecologica Scandinavica, 75, 720–4, 1996 [ ] | The study does not report any outcomes that match our protocol. |
| Couceiro Naveira, E., Lopez Ramon, Y.CajalC., Atosiban versus ritodrine as tocolytics in external cephalic version, Journal of Maternal-Fetal & Neonatal MedicineJ Matern Fetal Neonatal Med, 1–6, 2020 [ ] | Study design is a non-randomised trial. |
| Coulon, C., Poleszczuk, M., Paty-Montaigne, M. H., Gascard, C., Gay, C., Houfflin-Debarge, V., Subtil, D., Version of breech fetuses by moxibustion with acupuncture: A randomized controlled trial, Obstetrics and Gynecology, 124, 32–39, 2014 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Coyle,M.E., Smith,C.A., Peat,B., Cephalic version by moxibustion for breech presentation, Cochrane database of systematic reviews (Online), 5, CD003928-, 2012 [ ] | Systematic review for moxibustion. Relevant references examined and included if appropriate. |
| Delisle, Marie-France, Kamani, Allaudin, Douglas, Joanne, Bebbington, Michael, 124 Antepartum external cephalic version under spinal anesthesia: A randomized controlled trial, American Journal of Obstetrics & Gynecology, 185, S115, 2001 | No full text article available. |
| Do, C. K., Smith, C. A., Dahlen, H., Bisits, A., Schmied, V., Moxibustion for cephalic version: A feasibility randomised controlled trial, BMC Complementary and Alternative Medicine, 11, 81, 2011 [ ] [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Do, C., Smith, C., Dahlen, H., Bissets, A., Schmeid, V., Moxibustion for cephalic version: A feasibility study, Journal of Paediatrics and Child Health, 47, 37, 2011 | Duplicate. |
| Dochez, V., Esbelin, J., Volteau, C., Winer, N., Efficiency of nitrous oxide in external cephalic version on success rate: A randomised controlled trial, BJOG: An International Journal of Obstetrics and Gynaecology, 124 (Supplement 1), 111, 2017 | No full text available. |
| Founds, S. A., Clinical implications from an exploratory study of postural management of breech presentation, Journal of midwifery & women’s health, 51, 292–296, 2006 [ ] [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Garcia-Mochon, L., Martin, J. J., Aranda-Regules, J. M., Rivas-Ruiz, F., Vas, J., Cost effectiveness of using moxibustion to correct non-vertex presentation, Acupuncture in Medicine, 33, 136–41, 2015 [ ] | HE analysis. |
| Guittier,M.J., Klein,T.J., Dong,H., Andreoli,N., Irion,O., Boulvain,M., Side-effects of moxibustion for cephalic version of breech presentation, Journal of Alternative and Complementary Medicine, 14, 1231–1233, 2008 [ ] | This article reports on an unfinished trial. |
| Guittier,M.J., Pichon,M., Dong,H., Irion,O., Boulvain,M., Moxibustion for breech version: a randomized controlled trial, Obstetrics and Gynecology, 114, 1034–1040, 2009 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Hofmeyr, G. J., Kulier, R., Cephalic version by postural management for breech presentation, Cochrane Database of Systematic Reviews, 10, CD000051, 2012 [ ] [ ] | Cochrane review on postural management. Relevant references examined and included if appropriate. |
| Hofmeyr, G. J., Kulier, R., West, H. M., External cephalic version for breech presentation at term, Cochrane Database of Systematic Reviews, 2016, CD000083, 2015 [ ] [ ] | Cochrane review on ECV. Relevant references examined and included if appropriate. |
| Hofmeyr, GJ, External cephalic version facilitation for breech presentation at term, Cochrane Database of Systematic Reviews, 2, 2001 [ ] | Relevant references extracted and added to review. |
| Hofmeyr, GJ, External cephalic version for breech presentation before term, Cochrane Database of Systematic Reviews, 2, 2001 [ ] | Relevant references extracted and included in review. |
| Hofmeyr, GJ, Interventions to help external cephalic version for breech presentation at term, Cochrane Database of Systematic Reviews, 4, 2002 [ ] | Relevant references extracted and included in review. |
| Hofmeyr, GJ, Kulier, R, Cephalic version by postural management for breech presentation, Cochrane Database of Systematic Reviews, 1, 2003 [ ] | Relevant references extracted and included in review. |
| Hunter, S., Hofmeyr, G. J., Kulier, R., Hands and knees posture in late pregnancy or labour for fetal malposition (lateral or posterior), Cochrane Database of Systematic Reviews, CD001063, 2007 [ ] [ ] | Cochrane review for postural management. Relevant references examined and included if appropriate. |
| Hutton, E. K., Hannah, M. E., Ross, S. J., Delisle, M. F., Carson, G. D., Windrim, R., Ohlsson, A., Willan, A. R., Gafni, A., Sylvestre, G., Natale, R., Barrett, Y., Pollard, J. K., Dunn, M. S., Turtle, P., Early, E. C. V.Trial Collaborative Group, The Early External Cephalic Version (ECV) 2 Trial: an international multicentre randomised controlled trial of timing of ECV for breech pregnancies, BJOG: An International Journal of Obstetrics & GynaecologyBjog, 118, 564–77, 2011 [ ] [ ] | Duplicate. |
| Hutton, E. K., Hannah, M. E., Ross, S. J., Delisle, M. F., Carson, G. D., Windrim, R., Ohlsson, A., Willan, A. R., Gafni, A., Sylvestre, G., Natale, R., Barrett, Y., Pollard, J. K., Dunn, M. S., Turtle, P., The early external cephalic version 2 trial: An international multicenter randomized controlled trial of timing of external cephalic version for breech pregnancies, Obstetrical and Gynecological Survey, 66, 469–470, 2011 | No full text available. |
| Hutton, E. K., Hofmeyr, G. J., Dowswell, T., External cephalic version for breech presentation before term, Cochrane Database of Systematic Reviews, 2015 [ ] [ ] | Cochrane review on ECV. Relevant references examined and included if appropriate. |
| Johnson,R.L., Elliott,J.P., Fetal acoustic stimulation, an adjunct to external cephalic version: a blinded, randomized crossover study, American Journal of Obstetrics and Gynecology, 173, 1369–1372, 1995 [ ] | This study does not focus on breech presentation and instead focuses on fetal mid-line spine position. |
| Jorge, V., Manuel, A. R. J., Manuela, M., Mercedes, B., Nicolas, B. P., Francisco, R. R., Moxibustion applied at home for non-vertex presentation: A multicentre randomised controlled clinical trial, European Journal of Integrative Medicine, 4, 47, 2012 | No full text available. |
| Jprn, Umin, Utility of acupuncture and moxibustion for repositioning breech presentation. -Randomized Controlled Trial, .who.int/trialsearch/trial2 .aspx?Trialid =jprn-umin000011757, 2013 | No full text available. |
| Kim, S. Y., Chae, Y., Lee, S. M., Lee, H., Park, H. J., The effectiveness of moxibustion: an overview during 10 years, Evidence-Based Complementary & Alternative Medicine: eCAMEvid Based Complement Alternat Med, 2011, 306515, 2011 [ ] [ ] | Systematic review on moxibustion. Relevant references examined and included if appropriate. |
| Langer, B. P., Roth, G. E., Aissi, G., Meyer, N., Bigler, A., Bouschbacher, J. M., Hemlinger, C., Viville, B., Guilpain, M., Gaudineau, A., Akladios, C., Nisand, I., Vayssiere, C., Favre, R., Sananes, N., Acupuncture version of breech presentation: A randomized placebo-controlled single-blinded trial, American Journal of Obstetrics and Gynecology, 214, S65, 2016 | No full text available. |
| Lee, M. S., Are acupuncture-type interventions beneficial for correcting breech presentation?, Complementary Therapies in Medicine, 16, 238–9, 2008 [ ] | The study does not use RCT study design. |
| Lee, M. S., Kang, J. W., Ernst, E., Does moxibustion work? An overview of systematic reviews, BMC Research NotesBMC Res Notes, 3, 284, 2010 [ ] [ ] | Systematic review on moxibustion. Relevant references examined and included if appropriate. |
| Li, Q, Clinical observation on correcting malposition of fetus by electro-acupuncture, Journal of Traditional Chinese Medicine, 16, 260–2, 1996 [ ] | Duplicate. |
| Li, Q., Wang, L., Clinical observation on correcting malposition of fetus by electro-acupuncture, J Tradit Chin MedJournal of traditional Chinese medicine = Chung i tsa chih ying wen pan, 16, 260–2, 1996 [ ] | Included in CG62 but is not a RCT-observational study of women with malpresentation at 28 gestational weeks and more. |
| Li, X., Hu, J., Wang, X., Zhang, H., Liu, J., Moxibustion and other acupuncture point stimulation methods to treat breech presentation: A systematic review of clinical trials, Chinese Medicine, 4 (no pagination), 2009 [ ] [ ] | Systematic review on moxibustion. Relevant references examined and included if appropriate. |
| Liu, M. L., Lan, L., Tang, Y., Liang, F. R., Acupuncture and moxibustion for breech presentation: a systematic review, Chinese journal of evidence-based medicine, 9, 840–843, 2009 | This study is not available in English. |
| Magro-Malosso, E. R., Saccone, G., Di Tommaso, M., Mele, M., Berghella, V., Neuraxial analgesia to increase the success rate of external cephalic version: a systematic review and meta-analysis of randomized controlled trials, American Journal of Obstetrics & Gynecology, 215, 276–86, 2016 [ ] | Systematic review for ECV anaesthesia. Relevant references examined and included if appropriate. |
| Massalha, M., Garmi, G., Zafran, N., Carmeli, J., Gimburg, G., Salim, R., Clinical outcomes after external cephalic version with spinal anesthesia after failure of a first attempt without anesthesia, International Journal of Gynecology and Obstetrics, 139, 324–328, 2017 [ ] | The study does not use RCT study design. |
| Millereau, M., Branger, B., Darcel, F., Fetal version by acupuncture (moxibustion) versus control group, Journal de Gynecologie, Obstetrique et Biologie de la Reproduction, 38, 481–487, 2009 [ ] | Study is not written in English. |
| Morris, S., Geraghty, S., Sundin, D., Moxibustion: An alternative option for breech presentation, British Journal of Midwifery, 26, 440–445, 2018 | The study does not use RCT study design. |
| Muslim, I., Tan, I., Rodriguez, P., Tan, T. L., Cost effectiveness of external cephalic version, BJOG: An International Journal of Obstetrics and Gynaecology, 119, 121, 2012 | HE analysis. |
| Neri, I., De Pace, V., Venturini, P., Facchinetti, F., Effects of three different stimulations (acupuncture, moxibustion, acupuncture plus moxibustion) of BL.67 acupoint at small toe on fetal behavior of breech presentation, American Journal of Chinese Medicine, 35, 27–33, 2007 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Nor AzlinMI, MaryasalwatiI, NorzilalwatiMN, ZalehaAM, MohammadAJ, ZainulRMR, Nifedipine versusterbutaline for tocolysis in external cephalic version, International Journal of Gynecology & Obstetrics, 102, 263–266, 2008 [ ] | Duplicate. |
| Nor Azlin,, M. I., Ibrahim, M., Mohd Naim, N., Mahdy, Z. A., Jamil, M. A., Mohd Razi, Z. R., Nifedipine versus terbutaline for tocolysis in external cephalic version, Int J Gynaecol ObstetInternational journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics, 102, 263–6, 2008 [ ] | Duplicate. |
| O’Brien, J. A., Adashi, E. Y., Coming out ahead: the cost effectiveness of external cephalic version using spinal anesthesia, Israel Journal of Health Policy ResearchIsr J Health Policy Res, 3, 6, 2014 [ ] [ ] | HE analysis. |
| Paraiso Torras, B., Rodriguez Martin, N., Lazaro Carrasco Delgado, C., Jimenez Fournier, M. C., Canete Palomo, M. L., Economic impact of the introduction of the cephalic external version in a tertiary Hospital, Journal of Perinatal Medicine, 43, 2015 | HE analysis. |
| Predanic,M., External cephalic version for breech presentation with or without spinal analgesia in nulliparous women at term: a randomized controlled trial, Obstetrics and Gynecology, 111, 776–777, 2008 [ ] | The study does not use RCT study design. |
| Preston, R., Jee, R., Anesthesia-facilitated external cephalic version: pennywise or pound-foolish?, Canadian Journal of AnaesthesiaCan J Anaesth, 60, 6–13, 2013 [ ] | Systematic review for ECV anaesthesia. Relevant references examined and included if appropriate. |
| Reinhard, J., Peiffer, S., Reichenbach, L., Tottel, E., Reitter, A., Sinanovic, B., Yuan, J., Louwen, F., The effects of clinical hypnosis versus Neuro-Linguistic Programming (NLP) before External Cephalic Version (ECV)-A prospective off-centre randomised double blind controlled trial, Archives of Gynecology and Obstetrics, 1), S213–S214, 2012 [ ] [ ] | No full text available. |
| Reinhard, J., Peiffer, S., Sanger, N., Herrmann, E., Yuan, J., Louwen, F., The Effects of Clinical Hypnosis versus Neurolinguistic Programming (NLP) before External Cephalic Version (ECV): A Prospective Off-Centre Randomised, Double-Blind, Controlled Trial, Evidence-Based Complementary & Alternative Medicine: eCAMEvid Based Complement Alternat Med, 2012, 626740, 2012 [ ] [ ] | Duplicate. |
| Rosim, R. P., Carmo, E. V., Cost-effectiveness of breech version by moxibustion associated with acupuncture for women at 33 weeks gestation: A modeling approach by the brazilian public health care system perspective, Value in Health, 20, A924, 2017 | HE analysis. |
| Rosman, Ageeth, Vlemmix, Floortje, Fleuren, Margot, Rijnders, Marlies, Beuckens, Antje, Opmeer, Brent, Hardeman, Rob, Kok, Olga, Mol, Ben Willem, Kok, Marjolein, Implementation of external cephalic version: A multicentre cluster randomised controlled trial, Women & Birth, 26, S16–S16, 2013 | No full text available. |
| Sananes, N., Roth, G. E., Aissi, G. A., Meyer, N., Bigler, A., Bouschbacher, J. M., Helmlinger, C., Viville, B., Guilpain, M., Gaudineau, A., Akladios, C. Y., Nisand, I., Langer, B., Vayssiere, C., Favre, R., Acupuncture version of breech presentation: a randomized sham-controlled single-blinded trial, European Journal of Obstetrics, Gynecology, & Reproductive BiologyEur J Obstet Gynecol Reprod Biol, 204, 24–30, 2016 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Sloos, J. H., [The value of external version in at-term breech presentation], Ned Tijdschr GeneeskdNederlands tijdschrift voor geneeskunde, 135, 241–2, 1991 [ ] | Not available in English. |
| Smith, C. A., Cochrane, S., Does acupuncture have a place as an adjunct treatment during pregnancy? A review of randomized controlled trials and systematic reviews, Birth, 36, 246–253, 2009 [ ] | Systematic review on acupuncture. Relevant references examined and included if appropriate. |
| Sonia, B., Alessandro, B., Sylvie, B., Enrica, B., Filippa, T., Antonella, T., Federica, S., Catia, V., Valeria, M. M., Breech presentation of the foetus and traditional Chinese medicine, European Journal of Integrative Medicine, 4, 56, 2012 | No full text available. |
| Stock, A., Chung, T., Rogers, M., Ming, W. W., Randomized, double blind, placebo controlled comparison of ritodrine and hexoprenaline for tocolysis prior to external cephalic version at term, Aust N Z J Obstet GynaecolThe Australian & New Zealand journal of obstetrics & gynaecology, 33, 265–8, 1993 [ ] | The study does not report any outcomes that match our protocol. |
| Sullivan, J. T., Scavone, B. M., Patel, R., Robles, C., McCarthy, R. J., Wong, C. A., A randomized controlled trial of the impact of combined spinal-epidural analgesia on the success of external cephalic version for breech presentation, Anesthesiology, 104, 10, 2006 [ ] | Duplicate. |
| Sultan, P., Carvalho, B., Neuraxial blockade for external cephalic version: a systematic review, International Journal of Obstetric Anesthesia, 20, 299–306, 2011 [ ] | Systematic review for ECV anaesthesia. Relevant references examined and included if appropriate. |
| Tan,J.M., Macario,A., Carvalho,B., Druzin,M.L., El-Sayed,Y.Y., Cost-effectiveness of external cephalic version for term breech presentation, BMC Pregnancy and Childbirth, 10, 3-, 2010 [ ] [ ] | HE analysis. |
| van den Berg, I., Bosch, J. L., Jacobs, B., Bouman, I., Duvekot, J. J., Hunink, M. G., Effectiveness of acupuncture-type interventions versus expectant management to correct breech presentation: a systematic review, Complementary Therapies in Medicine, 16, 92–100, 2008 [ ] | Systematic review on acupuncture. Relevant references examined and included if appropriate. |
| van den Berg, I., Kaandorp, G. C., Bosch, J. L., Duvekot, J. J., Arends, L. R., Hunink, M. G., Cost-effectiveness of breech version by acupuncture-type interventions on BL 67, including moxibustion, for women with a breech foetus at 33 weeks gestation: a modelling approach, Complementary Therapies in Medicine, 18, 67–77, 2010 [ ] | HE analysis. |
| van den Berg, I., Kaandorp, G., Bosch, J. L., Duvekot, J. J., Hunink, M. G. M., The effectiveness and cost-effectiveness of Breech Version Acumoxa compared to standard care to correct breech presentation…13th Annual Symposium on Complementary Health Care, 12th-14th December, 2006, University of Exeter, UK, Focus on Alternative & Complementary Therapies, 11, 5–5, 2006 | HE analysis. |
| van Loon, AJ, Mantingh, A, Serlier, EK, Kroon, G, Mooyaart, EL, Huisjes, HJ, Randomised controlled trial of magnetic-resonance pelvimetry in breech presentation at term, Lancet, 350, 1799–804, 1997 [ ] | This study does not focus on interventions for breech management but rather on breech identification. |
| Vas, J., Aranda-Regules, J. M., Modesto, M., Ramos-Monserrat, M., Baron, M., Aguilar, I., Benitez-Parejo, N., Ramirez-Carmona, C., Rivas-Ruiz, F., Using moxibustion in primary healthcare to correct non-vertex presentation: a multicentre randomised controlled trial, Acupuncture in Medicine, 31, 31–8, 2013 [ ] | Population did not include women with a longitudinal lie fetal malpresentation (breech presentation) confirmed by ultrasound scan at ≥36+0 weeks. |
| Vas, J., Aranda-Regules, J. M., Modesto, M., Ramos-Monserrat, M., Baron, M., Aguilar, I., Benitez-Parejo, N., Ramirez-Carmona, C., Rivas-Ruiz, F., Using moxibustion in primary healthcare to correct non-vertex presentation: a multicentre randomised controlled trial, Revista Internacional de Acupuntura, 8, 41–49, 2014 | Duplicate. |
| Vas, J., Aranda-Regules, J. M., Modesto, M., Ramos-Monserrat, M., Barón, M., Aguilar, I., Benítez-Parejo, N., Ramírez-Carmona, C., Rivas-Ruiz, F., Using moxibustion in primary healthcare to correct non-vertex presentation: a multicentre randomised controlled trial, Acupuncture in Medicine, 31, 31–38, 2013 [ ] | Duplicate. |
| Vas,J., Aranda,J.M., Nishishinya,B., Mendez,C., Martin,M.A., Pons,J., Liu,J.P., Wang,C.Y., Perea-Milla,E., Correction of nonvertex presentation with moxibustion: a systematic review and metaanalysis, American Journal of Obstetrics and Gynecology, #201, 241–259, 2009 [ ] | Systematic review on moxibustion. Relevant references examined and included if appropriate. |
| Velzel, J., Vlemmix, F., Opmeer, B. C., Mol, B. W., Kok, M., Atosiban versus fenoterol as a uterine relaxant for external cephalic version: A randomized controlled trial, Journal of Paediatrics and Child Health, 51, 53, 2015 [ ] [ ] | No full text available. |
| Velzel, J., Vlemmix, F., Opmeer, B. C., Molkenboer, J. F., Verhoeven, C. J., van Pampus, M. G., Papatsonis, D. N., Bais, J. M., Vollebregt, K. C., van der Esch, L., Van der Post, J. A., Mol, B. W., Kok, M., Atosiban versus fenoterol as a uterine relaxant for external cephalic version: randomised controlled trial, BMJ, 356, i6773, 2017 [ ] [ ] | Duplicate. |
| Vlemmix, F., Rosman, A., Fleuren, M., Rijnders, M., Beuckens, A., Opmeer, B., Hardeman, R., Dirken, J., De Vaan, M., Kok, O., Bazairi, M., Cikot, R., Renes, C., Mol, B., Kok, M., Implementation of external cephalic version; A multicentre cluster randomised controlled trial, American Journal of Obstetrics and Gynecology, 208, S320, 2013 | No full text available. |
| Weiniger, C. F., Ginosaur, Y., Elchalal, U., Einav, S., Nucrietin, M., Guage, P., Ezra, Y., Prospective randomised study of external cephalic version for breech presentation at term in nulliparous women: spinal analgesia versus no analgesia, International Journal of Obstetric Anesthesia, 16, S21, 2007 | Duplicate. |
| Weiniger,C.F., Ginosar,Y., Elchalal,U., Sharon,E., Nokrian,M., Ezra,Y., External cephalic version for breech presentation with or without spinal analgesia in nulliparous women at term: a randomized controlled trial, Obstetrics and Gynecology, 110, 1343–1350, 2007 [ ] | The study does not report any outcomes that match our protocol. |
| Weomoger, C. F., Ginosar, Y., Elchalal, U., Sharon, E., Nokrian, M., Ezra, Y., External cephalix version for breech presentation with or without spinal analgesia in nulliparous women at term: a randomized controlled trial, Obstetrics & GynecologyObstet Gynecol, 110, 1343–1350, 2007 [ ] | Duplicate. |
| Wilcox, C. B., Nassar, N., Roberts, C. L., Effectiveness of nifedipine tocolysis to facilitate external cephalic version: A systematic review, BJOG: An International Journal of Obstetrics and Gynaecology, 118, 423–428, 2011 [ ] | Systematic review on ECV pharmaceutical component. Relevant references examined and included if appropriate. |
| Y. K.Yang, M.Mao, Y. P.Huet al, Effect of moxibustion at zhiyin (BL67) to correct the fetus malposition: multi-center randomized controlled clinical study, Journal of Traditional Chinese Medicine, 48, 1097–1110, 2007 | Not available in English. |
| Yamasato, K., Kaneshiro, B., Salcedo, J., Neuraxial blockade for external cephalic version: Cost analysis, Journal of Obstetrics & Gynaecology Research, 41, 1023–31, 2015 [ ] [ ] | HE analysis. |
| YangYK, MaoM, HuYP, et al., Effect of moxibustion at zhiyin (BL67) to correct the fetus malposition: multi-center randomized controlled clinical study, Journal of traditional Chinese medicine, 48, 1097–1110, 2007 | Duplicate. |
| Yang, F., Comparison of knee-chest plus moxibustion on Zhiyin with knee-chest position for breech position, Journal of sichuan traditional chinese medicine, 24, 106–107, 2006 | Not written in English. |
| Zhang,Q.H., Yue,J.H., Liu,M., Sun,Z.R., Sun,Q., Han,C., Wang,D., Moxibustion for the correction of nonvertex presentation: A systematic review and meta-analysis of randomized controlled trials, Evidence-based Complementary and Alternative Medicine, 2013, 2013. Article Number, -, 2013 [ ] [ ] | Systematic review on moxibustion. Relevant references examined and included if appropriate. |
Economic studies
No economic evidence was identified for this review.
Appendix L. Research recommendations
Research recommendations for review question: what is the most effective way of managing a longitudinal lie fetal malpresentation (breech presentation) in late pregnancy.
No research recommendations were made for this review question.
Evidence reviews underpinning recommendation 1.2.38
These evidence reviews were developed by the National Guideline Alliance, which is a part of the Royal College of Obstetricians and Gynaecologists
Disclaimer : The recommendations in this guideline represent the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, professionals are expected to take this guideline fully into account, alongside the individual needs, preferences and values of their patients or service users. The recommendations in this guideline are not mandatory and the guideline does not override the responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or their carer or guardian.
Local commissioners and/or providers have a responsibility to enable the guideline to be applied when individual health professionals and their patients or service users wish to use it. They should do so in the context of local and national priorities for funding and developing services, and in light of their duties to have due regard to the need to eliminate unlawful discrimination, to advance equality of opportunity and to reduce health inequalities. Nothing in this guideline should be interpreted in a way that would be inconsistent with compliance with those duties.
NICE guidelines cover health and care in England. Decisions on how they apply in other UK countries are made by ministers in the Welsh Government , Scottish Government , and Northern Ireland Executive . All NICE guidance is subject to regular review and may be updated or withdrawn.
- Cite this Page National Guideline Alliance (UK). Management of breech presentation: Antenatal care: Evidence review M. London: National Institute for Health and Care Excellence (NICE); 2021 Aug. (NICE Guideline, No. 201.)
- PDF version of this title (2.2M)
In this Page
Other titles in this collection.
- NICE Evidence Reviews Collection
Related NICE guidance and evidence
- NICE Guideline 201: Antenatal care
Supplemental NICE documents
- Supplement 1: Methods (PDF)
- Supplement 2: Health economics (PDF)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Identification of breech presentation: Antenatal care: Evidence review L [ 2021] Review Identification of breech presentation: Antenatal care: Evidence review L National Guideline Alliance (UK). 2021 Aug
- Vaginal delivery of breech presentation. [J Obstet Gynaecol Can. 2009] Vaginal delivery of breech presentation. Kotaska A, Menticoglou S, Gagnon R, MATERNAL FETAL MEDICINE COMMITTEE. J Obstet Gynaecol Can. 2009 Jun; 31(6):557-566.
- Review Cephalic version by moxibustion for breech presentation. [Cochrane Database Syst Rev. 2005] Review Cephalic version by moxibustion for breech presentation. Coyle ME, Smith CA, Peat B. Cochrane Database Syst Rev. 2005 Apr 18; (2):CD003928. Epub 2005 Apr 18.
- [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. [Gynecol Obstet Fertil Senol. 2...] [Fetal expulsion: Which interventions for perineal prevention? CNGOF Perineal Prevention and Protection in Obstetrics Guidelines]. Riethmuller D, Ramanah R, Mottet N. Gynecol Obstet Fertil Senol. 2018 Dec; 46(12):937-947. Epub 2018 Oct 28.
- Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. [J Obstet Gynaecol Br Emp. 1961] Foetal weight, presentaion and the progress of labour. II. Breech and occipito-posterior presentation related to the baby's weight and the length of the first stage of labour. BAINBRIDGE MN, NIXON WC, SMYTH CN. J Obstet Gynaecol Br Emp. 1961 Oct; 68:748-54.
Recent Activity
- Management of breech presentation Management of breech presentation
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Breech Position: What It Means if Your Baby Is Breech
Medically reviewed for accuracy.
What does it mean if a baby is breech?
What are the different types of breech positions, what causes a baby to be breech, recommended reading, how can you tell if your baby is in a breech position, what does it mean to turn a breech baby, how can you turn a breech baby, how does labor usually start with a breech baby.
If your cervix dilates too slowly, if your baby doesn’t move down the birth canal steadily or if other problems arise, you’ll likely have a C-section. Talk your options over with your practitioner now to be prepared. Remember that though you may feel disappointed things didn’t turn out exactly as you envisioned, these feelings will melt away once your bundle of joy safely enters the world.
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: 3rd trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be part of the cutting-edge research and care that's changing medicine.

Breech Presentation
- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE , Medicine , Surgery , Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Table of Contents
Suggest an improvement
- Hidden Post Title
- Hidden Post URL
- Hidden Post ID
- Type of issue * N/A Fix spelling/grammar issue Add or fix a link Add or fix an image Add more detail Improve the quality of the writing Fix a factual error
- Please provide as much detail as possible * You don't need to tell us which article this feedback relates to, as we automatically capture that information for you.
- Your Email (optional) This allows us to get in touch for more details if required.
- Which organ is responsible for pumping blood around the body? * Enter a five letter word in lowercase
- Phone This field is for validation purposes and should be left unchanged.
Introduction
Breech presentation is a type of malpresentation and occurs when the fetal head lies over the uterine fundus and fetal buttocks or feet present over the maternal pelvis (instead of cephalic/head presentation).
The incidence in the United Kingdom of breech presentation is 3-4% of all fetuses. 1
Breech presentation is most commonly idiopathic .
Types of breech presentation
The three types of breech presentation are:
- Complete (flexed) breech : one or both knees are flexed (Figure 1)
- Footling (incomplete) breech : one or both feet present below the fetal buttocks, with hips and knees extended (Figure 2)
- Frank (extended) breech : both hips flexed and both knees extended. Babies born in frank breech are more likely to have developmental dysplasia of the hip (Figure 3)

Risk factors
Risk factors for breech presentation can be divided into maternal , fetal and placental risk factors:
- Maternal : multiparity, fibroids, previous breech presentation, Mullerian duct abnormalities
- Fetal : preterm, macrosomia, fetal abnormalities (anencephaly, hydrocephalus, cystic hygroma), multiple pregnancy
- Placental : placenta praevia , polyhydramnios, oligohydramnios , amniotic bands
Clinical features
Before 36 weeks , breech presentation is not significant, as the fetus is likely to revert to a cephalic presentation. The mother will often be asymptomatic with the diagnosis being incidental.
The incidence of breech presentation is approximately 20% at 28 weeks gestation, 16% at 32 weeks gestation and 3-4% at term . Therefore, breech presentation is more common in preterm labour . Most fetuses with breech presentation in the early third trimester will turn spontaneously and be cephalic at term.
However, spontaneous version rates for nulliparous women with breech presentation at 36 weeks of gestation are less than 10% .
Clinical examination
Typical clinical findings of a breech presentation include:
- Longitudinal lie
- Head palpated at the fundus
- Irregular mass over pelvis (feet, legs and buttocks)
- Fetal heart auscultated higher on the maternal abdomen
- Palpation of feet or sacrum at the cervical os during vaginal examination
For more information, see the Geeky Medics guide to obstetric abdominal examination .
Positions in breech presentation
There are multiple fetal positions in breech presentation which are described according to the relation of the fetal sacrum to the maternal pelvis .
These are: direct sacroanterior, left sacroanterior, right sacroanterior, direct sacroposterior, right sacroposterior, left sacroposterior, left sacrotransverse and right sacrotranverse. 5
Investigations
An ultrasound scan is diagnostic for breech presentation. Growth, amniotic fluid volume and anatomy should be assessed to check for abnormalities.
There are three management options for breech presentation at term, with consideration of maternal choice: external cephalic version , vaginal delivery and Caesarean section .
External cephalic version
External cephalic version (ECV) involves manual rotation of the fetus into a cephalic presentation by applying pressure to the maternal abdomen under ultrasound guidance. Entonox and subcutaneous terbutaline are used to relax the uterus.
ECV has a 40% success rate in primiparous women and 60% in multiparous women . It should be offered to nulliparous women at 36 weeks and multiparous women at 37 weeks gestation.
If ECV is unsuccessful, then delivery options include elective caesarean section or vaginal delivery.
Contraindications for undertaking external cephalic version include:
- Antepartum haemorrhage
- Ruptured membranes
- Previous caesarean section
- Major uterine abnormality
- Multiple pregnancy
- Abnormal cardiotocography (CTG)
Vaginal delivery
Vaginal delivery is an option but carries risks including head entrapment, birth asphyxia, intracranial haemorrhage, perinatal mortality, cord prolapse and fetal and/or maternal trauma.
The preference is to deliver the baby without traction and with an anterior sacrum during delivery to decrease the risk of fetal head entrapment .
The mother may be offered an epidural , as vaginal breech delivery can be very painful. 6
Contraindications for vaginal delivery in a breech presentation include:
- Footling breech: the baby’s head and trunk are more likely to be trapped if the feet pass through the dilated cervix too soon
- Macrosomia: usually defined as larger than 3800g
- Growth restricted baby: usually defined as smaller than 2000g
- Other complications of vaginal birth: for example, placenta praevia and fetal compromise
- Lack of clinical staff trained in vaginal breech delivery
Caesarean section
A caesarian section booked as an elective procedure at term is the most common management for breech presentation.
Caesarean section is preferred for preterm babies (due to an increased head to abdominal circumference ratio in preterm babies) and is used if the external cephalic version is unsuccessful or as a maternal preference. This option has fewer risks than a vaginal delivery.
Complications
Fetal complications of breech presentation include:
- Developmental dysplasia of the hip (DDH)
- Cord prolapse
- Fetal head entrapment
- Birth asphyxia
- Intracranial haemorrhage
- Perinatal mortality
Complications of external cephalic version include:
- Transient fetal heart abnormalities (common)
- Fetomaternal haemorrhage
- Placental abruption (rare)
- There are three types of breech presentation: complete, incomplete and frank breech
- The most common clinical findings include: longitudinal lie, smooth fetal head-shape at the fundus, irregular masses over the pelvis and abnormal placement being required for fetal hear auscultation
- The diagnostic investigation is an ultrasound scan
- Breech presentation can be managed in three ways: external cephalic version , vaginal delivery or elective caesarean section
- Complications are more common in vaginal delivery , such as cord prolapse, fetal head entrapment, intracranial haemorrhage and birth asphyxia
Miss Saba Al Juboori
Consultant in Obstetrics and Gynaecology
Miss Neeraja Kuruba
Dr chris jefferies.
- Oxford Handbook of Obstetrics and Gynaecology. Breech Presentation: Overview. Published in 2011.
- Jemimah Thomas. Image: Complete breech.
- Bonnie Urquhart Gruenberg. Footling breech. Licence: [ CC BY-SA ]
- Bonnie Urquhart Gruenberg. Frank breech . Licence: [ CC BY-SA ]
- A Comprehensive Textbook of Obstetrics and Gynaecology. Chapter 50: Malpresentation and Malposition: Breech Presentation. Published in 2011.
- Diana Hamilton Fairley. Lecture Notes: Obstetrics and Gynaecology, Malpresentation, Breech Presentation. Published in 2009.

Other pages
- Product Bundles 🎉
- Join the Team 🙌
- Institutional Licence 📚
- OSCE Station Creator Tool 🩺
- Create and Share Flashcards 🗂️
- OSCE Group Chat 💬
- Newsletter 📰
- Advertise With Us
Join the community
Breech presentation
Highlights & basics.
- Diagnostic Approach
- Risk Factors
History & Exam
- Differential Diagnosis
- Tx Approach
- Emerging Tx
- Complications
PATIENT RESOURCES
- Patient Instructions
Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head.
Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal mortality.
Incidence decreases as pregnancy progresses and by term occurs in 3% to 4% of singleton term pregnancies.
Treatment options include external cephalic version to increase the likelihood of vaginal birth or a planned cesarean section, the optimal gestation being 37 and 39 weeks, respectively.
Planned cesarean section is considered the safest form of delivery for infants with a persisting breech presentation at term.
Quick Reference
Key Factors
Other Factors
Diagnostics Tests
Treatment Options
Epidemiology
Pathophysiology.

Key Articles
Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. Mar 2017 [internet publication]. [Full Text]
Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
Referenced Articles
1. Cunningham F, Gant N, Leveno K, et al. Williams obstetrics. 21st ed. New York: McGraw-Hill; 1997.
2. Kish K, Collea JV. Malpresentation and cord prolapse. In: DeCherney AH, Nathan L, eds. Current obstetric and gynecologic diagnosis and treatment. New York: McGraw-Hill Professional; 2002.
3. Scheer K, Nubar J. Variation of fetal presentation with gestational age. Am J Obstet Gynecol. 1976 May 15;125(2):269-70. [Abstract]
4. Nassar N, Roberts CL, Cameron CA, et al. Diagnostic accuracy of clinical examination for detection of non-cephalic presentation in late pregnancy: cross sectional analytic study. BMJ. 2006 Sep 16;333(7568):578-80. [Abstract] [Full Text]
5. Roberts CL, Peat B, Algert CS, et al. Term breech birth in New South Wales, 1990-1997. Aust N Z J Obstet Gynaecol. 2000 Feb;40(1):23-9. [Abstract]
6. Roberts CL, Algert CS, Peat B, et al. Small fetal size: a risk factor for breech birth at term. Int J Gynaecol Obstet. 1999 Oct;67(1):1-8. [Abstract]
7. Brar HS, Platt LD, DeVore GR, et al. Fetal umbilical velocimetry for the surveillance of pregnancies complicated by placenta previa. J Reprod Med. 1988 Sep;33(9):741-4. [Abstract]
8. Kian L. The role of the placental site in the aetiology of breech presentation. J Obstet Gynaecol Br Commonw. 1963 Oct;70:795-7. [Abstract]
9. Rayl J, Gibson PJ, Hickok DE. A population-based case-control study of risk factors for breech presentation. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):28-32. [Abstract]
10. Westgren M, Edvall H, Nordstrom L, et al. Spontaneous cephalic version of breech presentation in the last trimester. Br J Obstet Gynaecol. 1985 Jan;92(1):19-22. [Abstract]
11. Brenner WE, Bruce RD, Hendricks CH. The characteristics and perils of breech presentation. Am J Obstet Gynecol. 1974 Mar 1;118(5):700-12. [Abstract]
12. Hall JE, Kohl S. Breech presentation. Am J Obstet Gynecol. 1956 Nov;72(5):977-90. [Abstract]
13. Morgan HS, Kane SH. An analysis of 16,327 breech births. JAMA. 1964 Jan 25;187:262-4. [Abstract]
14. Luterkort M, Persson P, Weldner B. Maternal and fetal factors in breech presentation. Obstet Gynecol. 1984 Jul;64(1):55-9. [Abstract]
15. Braun FH, Jones KL, Smith DW. Breech presentation as an indicator of fetal abnormality. J Pediatr. 1975 Mar;86(3):419-21. [Abstract]
16. Albrechtsen S, Rasmussen S, Dalaker K, et al. Reproductive career after breech presentation: subsequent pregnancy rates, interpregnancy interval, and recurrence. Obstet Gynecol. 1998 Sep;92(3):345-50. [Abstract]
17. Zlopasa G, Skrablin S, Kalafatić D, et al. Uterine anomalies and pregnancy outcome following resectoscope metroplasty. Int J Gynaecol Obstet. 2007 Aug;98(2):129-33. [Abstract]
18. Acién P. Breech presentation in Spain, 1992: a collaborative study. Eur J Obstet Gynecol Reprod Biol. 1995 Sep;62(1):19-24. [Abstract]
19. Michalas SP. Outcome of pregnancy in women with uterine malformation: evaluation of 62 cases. Int J Gynaecol Obstet. 1991 Jul;35(3):215-9. [Abstract]
20. Fianu S, Vaclavinkova V. The site of placental attachment as a factor in the aetiology of breech presentation. Acta Obstet Gynecol Scand. 1978;57(4):371-2. [Abstract]
21. Haruyama Y. Placental implantation as the cause of breech presentation [in Japanese]. Nihon Sanka Fujinka Gakkai Zasshi. 1987 Jan;39(1):92-8. [Abstract]
22. Filipov E, Borisov I, Kolarov G. Placental location and its influence on the position of the fetus in the uterus [in Bulgarian]. Akush Ginekol (Sofiia). 2000;40(4):11-2. [Abstract]
23. Waterstone M, Bewley S, Wolfe C. Incidence and predictors of severe obstetric morbidity: case-control study. BMJ. 2001 May 5;322(7294):1089-93. [Abstract] [Full Text]
24. Beischer NA, Mackay EV, Colditz P, eds. Obstetrics and the newborn: an illustrated textbook. 3rd ed. London: W.B. Saunders; 1997.
25. Impey LWM, Murphy DJ, Griffiths M, et al; Royal College of Obstetricians and Gynaecologists. Management of breech presentation: green-top guideline no. 20b. BJOG. 2017 Jun;124(7):e151-77. [Full Text]
26. Royal College of Obstetricians and Gynaecologists. Antepartum haemorrhage: green-top guideline no. 63. November 2011 [internet publication]. [Full Text]
27. American College of Obstetricians and Gynecologists. Practice bulletin no. 175: ultrasound in pregnancy. Obstet Gynecol. 2016 Dec;128(6):e241-56. [Abstract]
28. Enkin M, Keirse MJNC, Neilson J, et al. Guide to effective care in pregnancy and childbirth. 3rd ed. Oxford: Oxford University Press; 2000.
29. Hofmeyr GJ, Kulier R, West HM. External cephalic version for breech presentation at term. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000083. [Abstract] [Full Text]
30. Hofmeyr GJ, Hannah M, Lawrie TA. Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. 2015 Jul 21;(7):CD000166. [Abstract] [Full Text]
31. Royal College of Obstetricians and Gynaecologists. External cephalic version and reducing the incidence of term breech presentation. Mar 2017 [internet publication]. [Full Text]
32. Rosman AN, Guijt A, Vlemmix F, et al. Contraindications for external cephalic version in breech position at term: a systematic review. Acta Obstet Gynecol Scand. 2013 Feb;92(2):137-42. [Abstract]
33. American College of Obstetricians and Gynecologists. Practice bulletin no. 221: external cephalic version. May 2020 [internet publication]. [Full Text]
34. Bogner G, Xu F, Simbrunner C, et al. Single-institute experience, management, success rate, and outcome after external cephalic version at term. Int J Gynaecol Obstet. 2012 Feb;116(2):134-7. [Abstract]
35. Hofmeyr GJ. Effect of external cephalic version in late pregnancy on breech presentation and caesarean section rate: a controlled trial. Br J Obstet Gynaecol. 1983 May;90(5):392-9. [Abstract]
36. Beuckens A, Rijnders M, Verburgt-Doeleman GH, et al. An observational study of the success and complications of 2546 external cephalic versions in low-risk pregnant women performed by trained midwives. BJOG. 2016 Feb;123(3):415-23. [Abstract]
37. Nassar N, Roberts CL, Barratt A, et al. Systematic review of adverse outcomes of external cephalic version and persisting breech presentation at term. Paediatr Perinat Epidemiol. 2006 Mar;20(2):163-71. [Abstract]
38. Sela HY, Fiegenberg T, Ben-Meir A, et al. Safety and efficacy of external cephalic version for women with a previous cesarean delivery. Eur J Obstet Gynecol Reprod Biol. 2009 Feb;142(2):111-4. [Abstract]
39. Pichon M, Guittier MJ, Irion O, et al. External cephalic version in case of persisting breech presentation at term: motivations and women's experience of the intervention [in French]. Gynecol Obstet Fertil. 2013 Jul-Aug;41(7-8):427-32. [Abstract]
40. Nassar N, Roberts CL, Raynes-Greenow CH, et al. Evaluation of a decision aid for women with breech presentation at term: a randomised controlled trial [ISRCTN14570598]. BJOG. 2007 Mar;114(3):325-33. [Abstract] [Full Text]
41. Cluver C, Gyte GM, Sinclair M, et al. Interventions for helping to turn term breech babies to head first presentation when using external cephalic version. Cochrane Database Syst Rev. 2015 Feb 9;(2):CD000184. [Abstract] [Full Text]
42. US Food & Drug Administration. FDA Drug Safety Communication: new warnings against use of terbutaline to treat preterm labor. Feb 2011 [internet publication]. [Full Text]
43. European Medicines Agency. Restrictions on use of short-acting beta-agonists in obstetric indications - CMDh endorses PRAC recommendations. October 2013 [internet publication]. [Full Text]
44. Magro-Malosso ER, Saccone G, Di Tommaso M, et al. Neuraxial analgesia to increase the success rate of external cephalic version: a systematic review and meta-analysis of randomized controlled trials. Am J Obstet Gynecol. 2016 Sep;215(3):276-86. [Abstract]
45. de Hundt M, Velzel J, de Groot CJ, et al. Mode of delivery after successful external cephalic version: a systematic review and meta-analysis. Obstet Gynecol. 2014 Jun;123(6):1327-34. [Abstract]
46. American College of Obstetricians and Gynecologists. Committee opinion no. 745: mode of term singleton breech delivery. Aug 2018 (reaffirmed 2023) [internet publication]. [Full Text]
47. Berhan Y, Haileamlak A. The risks of planned vaginal breech delivery versus planned caesarean section for term breech birth: a meta-analysis including observational studies. BJOG. 2016 Jan;123(1):49-57. [Abstract] [Full Text]
48. Lydon-Rochelle M, Holt VL, Martin DP, et al. Association between method of delivery and maternal rehospitalisation. JAMA. 2000 May 10;283(18):2411-6. [Abstract]
49. Yokoe DS, Christiansen CL, Johnson R, et al. Epidemiology of and surveillance for postpartum infections. Emerg Infect Dis. 2001 Sep-Oct;7(5):837-41. [Abstract]
50. van Ham MA, van Dongen PW, Mulder J. Maternal consequences of caesarean section. A retrospective study of intra-operative and postoperative maternal complications of caesarean section during a 10-year period. Eur J Obstet Gynecol Reprod Biol. 1997 Jul;74(1):1-6. [Abstract]
51. Murphy DJ, Liebling RE, Verity L, et al. Early maternal and neonatal morbidity associated with operative delivery in second stage of labour: a cohort study. Lancet. 2001 Oct 13;358(9289):1203-7. [Abstract]
52. Lydon-Rochelle MT, Holt VL, Martin DP. Delivery method and self-reported postpartum general health status among primiparous women. Paediatr Perinat Epidemiol. 2001 Jul;15(3):232-40. [Abstract]
53. Wilson PD, Herbison RM, Herbison GP. Obstetric practice and the prevalence of urinary incontinence three months after delivery. Br J Obstet Gynaecol. 1996 Feb;103(2):154-61. [Abstract]
54. Persson J, Wolner-Hanssen P, Rydhstroem H. Obstetric risk factors for stress urinary incontinence: a population-based study. Obstet Gynecol. 2000 Sep;96(3):440-5. [Abstract]
55. MacLennan AH, Taylor AW, Wilson DH, et al. The prevalence of pelvic disorders and their relationship to gender, age, parity and mode of delivery. BJOG. 2000 Dec;107(12):1460-70. [Abstract]
56. Thompson JF, Roberts CL, Currie M, et al. Prevalence and persistence of health problems after childbirth: associations with parity and method of birth. Birth. 2002 Jun;29(2):83-94. [Abstract]
57. Australian Institute of Health and Welfare. Australia's mothers and babies 2015 - in brief. October 2017 [internet publication]. [Full Text]
58. Mutryn CS. Psychosocial impact of cesarean section on the family: a literature review. Soc Sci Med. 1993 Nov;37(10):1271-81. [Abstract]
59. DiMatteo MR, Morton SC, Lepper HS, et al. Cesarean childbirth and psychosocial outcomes: a meta-analysis. Health Psychol. 1996 Jul;15(4):303-14. [Abstract]
60. Greene R, Gardeit F, Turner MJ. Long-term implications of cesarean section. Am J Obstet Gynecol. 1997 Jan;176(1 Pt 1):254-5. [Abstract]
61. Coughlan C, Kearney R, Turner MJ. What are the implications for the next delivery in primigravidae who have an elective caesarean section for breech presentation? BJOG. 2002 Jun;109(6):624-6. [Abstract]
62. Hemminki E, Merilainen J. Long-term effects of cesarean sections: ectopic pregnancies and placental problems. Am J Obstet Gynecol. 1996 May;174(5):1569-74. [Abstract]
63. Gilliam M, Rosenberg D, Davis F. The likelihood of placenta previa with greater number of cesarean deliveries and higher parity. Obstet Gynecol. 2002 Jun;99(6):976-80. [Abstract]
64. Morrison JJ, Rennie JM, Milton PJ. Neonatal respiratory morbidity and mode of delivery at term: influence of timing of elective caesarean section. Br J Obstet Gynaecol. 1995 Feb;102(2):101-6. [Abstract]
65. Annibale DJ, Hulsey TC, Wagner CL, et al. Comparative neonatal morbidity of abdominal and vaginal deliveries after uncomplicated pregnancies. Arch Pediatr Adolesc Med. 1995 Aug;149(8):862-7. [Abstract]
66. Hook B, Kiwi R, Amini SB, et al. Neonatal morbidity after elective repeat cesarean section and trial of labor. Pediatrics. 1997 Sep;100(3 Pt 1):348-53. [Abstract]
67. Stock SJ, Thomson AJ, Papworth S, et al. Antenatal corticosteroids to reduce neonatal morbidity and mortality: Green-top Guideline No. 74. BJOG. 2022 Jul;129(8):e35-60. [Abstract] [Full Text]
68. American College of Obstetricians and Gynaecologists. Committee opinion no. 713: antenatal corticosteroid therapy for fetal maturation. Aug 2017 (reaffirmed 2024) [internet publication]. [Full Text]
69. Nassar N, Roberts CL, Cameron CA, et al. Outcomes of external cephalic version and breech presentation at term: an audit of deliveries at a Sydney tertiary obstetric hospital, 1997-2004. Acta Obstet Gynecol Scand. 2006;85(10):1231-8. [Abstract]
70. Nwosu EC, Walkinshaw S, Chia P, et al. Undiagnosed breech. Br J Obstet Gynaecol. 1993 Jun;100(6):531-5. [Abstract]
71. Flamm BL, Ruffini RM. Undetected breech presentation: impact on external version and cesarean rates. Am J Perinatol. 1998 May;15(5):287-9. [Abstract]
72. Cockburn J, Foong C, Cockburn P. Undiagnosed breech. Br J Obstet Gynaecol. 1994 Jul;101(7):648-9. [Abstract]
73. Leung WC, Pun TC, Wong WM. Undiagnosed breech revisited. Br J Obstet Gynaecol. 1999 Jul;106(7):638-41. [Abstract]
74. Wilcox C, Nassar N, Roberts C. Effectiveness of nifedipine tocolysis to facilitate external cephalic version: a systematic review. BJOG. 2011 Mar;118(4):423-8. [Abstract]
75. Qureshi H, Massey E, Kirwan D, et al. BCSH guideline for the use of anti-D immunoglobulin for the prevention of haemolytic disease of the fetus and newborn. Transfus Med. 2014 Feb;24(1):8-20. [Abstract] [Full Text]
76. Hutton EK, Hofmeyr GJ, Dowswell T. External cephalic version for breech presentation before term. Cochrane Database Syst Rev. 2015 Jul 29;(7):CD000084. [Abstract] [Full Text]
77. Coyle ME, Smith CA, Peat B. Cephalic version by moxibustion for breech presentation. Cochrane Database Syst Rev. 2012 May 16;(5):CD003928. [Abstract] [Full Text]
78. Hofmeyr GJ, Kulier R. Cephalic version by postural management for breech presentation. Cochrane Database Syst Rev. 2012 Oct 17;(10):CD000051. [Abstract] [Full Text]
79. National Institute for Health and Care Excellence. Caesarean birth. Jan 2024 [internet publication]. [Full Text]
80. Hannah ME, Whyte H, Hannah WJ, et al. Maternal outcomes at 2 years after planned cesarean section versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):917-27. [Abstract]
81. Eide MG, Oyen N, Skjaerven R, et al. Breech delivery and Intelligence: a population-based study of 8,738 breech infants. Obstet Gynecol. 2005 Jan;105(1):4-11. [Abstract]
82. Whyte H, Hannah ME, Saigal S, et al. Outcomes of children at 2 years after planned cesarean birth versus planned vaginal birth for breech presentation at term: the International Randomized Term Breech Trial. Am J Obstet Gynecol. 2004 Sep;191(3):864-71. [Abstract]
83. Brown S, Lumley J. Maternal health after childbirth: results of an Australian population based survey. Br J Obstet Gynaecol. 1998 Feb;105(2):156-61. [Abstract]
Sign in to access our clinical decision support tools
What happens if your baby is breech?
Babies often twist and turn during pregnancy, but most will have moved into the head-down (also known as head-first) position by the time labour begins. However, that does not always happen, and a baby may be:
- bottom first or feet first (breech position)
- lying sideways (transverse position)
Bottom first or feet first (breech baby)
If your baby is lying bottom or feet first, they are in the breech position. If they're still breech at around 36 weeks' gestation, the obstetrician and midwife will discuss your options for a safe delivery.
Turning a breech baby
If your baby is in a breech position at 36 weeks, you'll usually be offered an external cephalic version (ECV). This is when a healthcare professional, such as an obstetrician, tries to turn the baby into a head-down position by applying pressure on your abdomen. It's a safe procedure, although it can be a bit uncomfortable.
Giving birth to a breech baby
If an ECV does not work, you'll need to discuss your options for a vaginal birth or caesarean section with your midwife and obstetrician.
If you plan a caesarean and then go into labour before the operation, your obstetrician will assess whether it's safe to proceed with the caesarean delivery. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
The Royal College of Obstetricians and Gynaecologists (RCOG) website has more information on what to expect if your baby is still breech at the end of pregnancy .
The RCOG advises against a vaginal breech delivery if:
- your baby's feet are below its bottom – known as a "footling breech"
- your baby is larger or smaller than average – your healthcare team will discuss this with you
- your baby is in a certain position – for example, their neck is very tilted back, which can make delivery of the head more difficult
- you have a low-lying placenta (placenta praevia)
- you have pre-eclampsia
Lying sideways (transverse baby)
If your baby is lying sideways across the womb, they are in the transverse position. Although many babies lie sideways early on in pregnancy, most turn themselves into the head-down position by the final trimester.
Giving birth to a transverse baby
Depending on how many weeks pregnant you are when your baby is in a transverse position, you may be admitted to hospital. This is because of the very small risk of the umbilical cord coming out of your womb before your baby is born (cord prolapse). If this happens, it's a medical emergency and the baby must be delivered very quickly.
Sometimes, it's possible to manually turn the baby to a head-down position, and you may be offered this.
But, if your baby is still in the transverse position when you approach your due date or by the time labour begins, you'll most likely be advised to have a caesarean section.
Video: My baby is breech. What help will I get?
In this video, a midwife describes what a breech position is and what can be done if your baby is breech.
Page last reviewed: 1 November 2023 Next review due: 1 November 2026
Breech baby at the end of pregnancy
Published: July 2017
Please note that this information will be reviewed every 3 years after publication.
This patient information page provides advice if your baby is breech towards the end of pregnancy and the options available to you.
It may also be helpful if you are a partner, relative or friend of someone who is in this situation.
The information here aims to help you better understand your health and your options for treatment and care. Your healthcare team is there to support you in making decisions that are right for you. They can help by discussing your situation with you and answering your questions.
This information is for you if your baby remains in the breech position after 36 weeks of pregnancy. Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies.
This information includes:
- What breech is and why your baby may be breech
- The different types of breech
- The options if your baby is breech towards the end of your pregnancy
- What turning a breech baby in the uterus involves (external cephalic version or ECV)
- How safe ECV is for you and your baby
- Options for birth if your baby remains breech
- Other information and support available
Within this information, we may use the terms ‘woman’ and ‘women’. However, it is not only people who identify as women who may want to access this information. Your care should be personalised, inclusive and sensitive to your needs, whatever your gender identity.
A glossary of medical terms is available at A-Z of medical terms .
- Breech is very common in early pregnancy, and by 36–37 weeks of pregnancy most babies will turn into the head-first position. If your baby remains breech, it does not usually mean that you or your baby have any problems.
- Turning your baby into the head-first position so that you can have a vaginal delivery is a safe option.
- The alternative to turning your baby into the head-first position is to have a planned caesarean section or a planned vaginal breech birth.
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position.
Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech position.
A breech baby may be lying in one of the following positions:
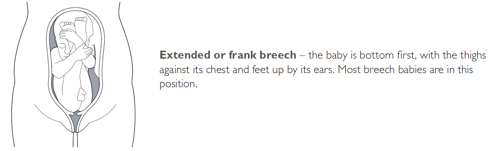
It may just be a matter of chance that your baby has not turned into the head-first position. However, there are certain factors that make it more difficult for your baby to turn during pregnancy and therefore more likely to stay in the breech position. These include:
- if this is your first pregnancy
- if your placenta is in a low-lying position (also known as placenta praevia); see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- if you have too much or too little fluid ( amniotic fluid ) around your baby
- if you are having more than one baby.
Very rarely, breech may be a sign of a problem with the baby. If this is the case, such problems may be picked up during the scan you are offered at around 20 weeks of pregnancy.
If your baby is breech at 36 weeks of pregnancy, your healthcare professional will discuss the following options with you:
- trying to turn your baby in the uterus into the head-first position by external cephalic version (ECV)
- planned caesarean section
- planned vaginal breech birth.
What does ECV involve?
ECV involves applying gentle but firm pressure on your abdomen to help your baby turn in the uterus to lie head-first.
Relaxing the muscle of your uterus with medication has been shown to improve the chances of turning your baby. This medication is given by injection before the ECV and is safe for both you and your baby. It may make you feel flushed and you may become aware of your heart beating faster than usual but this will only be for a short time.
Before the ECV you will have an ultrasound scan to confirm your baby is breech, and your pulse and blood pressure will be checked. After the ECV, the ultrasound scan will be repeated to see whether your baby has turned. Your baby’s heart rate will also be monitored before and after the procedure. You will be advised to contact the hospital if you have any bleeding, abdominal pain, contractions or reduced fetal movements after ECV.
ECV is usually performed after 36 or 37 weeks of pregnancy. However, it can be performed right up until the early stages of labour. You do not need to make any preparations for your ECV.
ECV can be uncomfortable and occasionally painful but your healthcare professional will stop if you are experiencing pain and the procedure will only last for a few minutes. If your healthcare professional is unsuccessful at their first attempt in turning your baby then, with your consent, they may try again on another day.
If your blood type is rhesus D negative, you will be advised to have an anti-D injection after the ECV and to have a blood test. See the NICE patient information Routine antenatal anti-D prophylaxis for women who are rhesus D negative , which is available at: www.nice.org.uk/guidance/ta156/informationforpublic .
Why turn my baby head-first?
If your ECV is successful and your baby is turned into the head-first position you are more likely to have a vaginal birth. Successful ECV lowers your chances of requiring a caesarean section and its associated risks.
Is ECV safe for me and my baby?
ECV is generally safe with a very low complication rate. Overall, there does not appear to be an increased risk to your baby from having ECV. After ECV has been performed, you will normally be able to go home on the same day.
When you do go into labour, your chances of needing an emergency caesarean section, forceps or vacuum (suction cup) birth is slightly higher than if your baby had always been in a head-down position.
Immediately after ECV, there is a 1 in 200 chance of you needing an emergency caesarean section because of bleeding from the placenta and/or changes in your baby’s heartbeat.
ECV should be carried out by a doctor or a midwife trained in ECV. It should be carried out in a hospital where you can have an emergency caesarean section if needed.
ECV can be carried out on most women, even if they have had one caesarean section before.
ECV should not be carried out if:
- you need a caesarean section for other reasons, such as placenta praevia; see the RCOG patient information Placenta praevia, placenta accreta and vasa praevia
- you have had recent vaginal bleeding
- your baby’s heart rate tracing (also known as CTG) is abnormal
- your waters have broken
- you are pregnant with more than one baby; see the RCOG patient information Multiple pregnancy: having more than one baby .
Is ECV always successful?
ECV is successful for about 50% of women. It is more likely to work if you have had a vaginal birth before. Your healthcare team should give you information about the chances of your baby turning based on their assessment of your pregnancy.
If your baby does not turn then your healthcare professional will discuss your options for birth (see below). It is possible to have another attempt at ECV on a different day.
If ECV is successful, there is still a small chance that your baby will turn back to the breech position. However, this happens to less than 5 in 100 (5%) women who have had a successful ECV.
There is no scientific evidence that lying down or sitting in a particular position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called mugwort) at 33–35 weeks of pregnancy may help your baby to turn into the head-first position, possibly by encouraging your baby’s movements. This should be performed under the direction of a registered healthcare practitioner.
Depending on your situation, your choices are:
There are benefits and risks associated with both caesarean section and vaginal breech birth, and these should be discussed with you so that you can choose what is best for you and your baby.
Caesarean section
If your baby remains breech towards the end of pregnancy, you should be given the option of a caesarean section. Research has shown that planned caesarean section is safer for your baby than a vaginal breech birth. Caesarean section carries slightly more risk for you than a vaginal birth.
Caesarean section can increase your chances of problems in future pregnancies. These may include placental problems, difficulty with repeat caesarean section surgery and a small increase in stillbirth in subsequent pregnancies. See the RCOG patient information Choosing to have a caesarean section .
If you choose to have a caesarean section but then go into labour before your planned operation, your healthcare professional will examine you to assess whether it is safe to go ahead. If the baby is close to being born, it may be safer for you to have a vaginal breech birth.
Vaginal breech birth
After discussion with your healthcare professional about you and your baby’s suitability for a breech delivery, you may choose to have a vaginal breech birth. If you choose this option, you will need to be cared for by a team trained in helping women to have breech babies vaginally. You should plan a hospital birth where you can have an emergency caesarean section if needed, as 4 in 10 (40%) women planning a vaginal breech birth do need a caesarean section. Induction of labour is not usually recommended.
While a successful vaginal birth carries the least risks for you, it carries a small increased risk of your baby dying around the time of delivery. A vaginal breech birth may also cause serious short-term complications for your baby. However, these complications do not seem to have any long-term effects on your baby. Your individual risks should be discussed with you by your healthcare team.
Before choosing a vaginal breech birth, it is advised that you and your baby are assessed by your healthcare professional. They may advise against a vaginal birth if:
- your baby is a footling breech (one or both of the baby’s feet are below its bottom)
- your baby is larger or smaller than average (your healthcare team will discuss this with you)
- your baby is in a certain position, for example, if its neck is very tilted back (hyper extended)
- you have a low-lying placenta (placenta praevia); see the RCOG patient information Placenta Praevia, placenta accreta and vasa praevia
- you have pre-eclampsia or any other pregnancy problems; see the RCOG patient information Pre-eclampsia .
With a breech baby you have the same choices for pain relief as with a baby who is in the head-first position. If you choose to have an epidural, there is an increased chance of a caesarean section. However, whatever you choose, a calm atmosphere with continuous support should be provided.
If you have a vaginal breech birth, your baby’s heart rate will usually be monitored continuously as this has been shown to improve your baby’s chance of a good outcome.
In some circumstances, for example, if there are concerns about your baby’s heart rate or if your labour is not progressing, you may need an emergency caesarean section during labour. A paediatrician (a doctor who specialises in the care of babies, children and teenagers) will attend the birth to check your baby is doing well.
If you go into labour before 37 weeks of pregnancy, the balance of the benefits and risks of having a caesarean section or vaginal birth changes and will be discussed with you.
If you are having twins and the first baby is breech, your healthcare professional will usually recommend a planned caesarean section.
If, however, the first baby is head-first, the position of the second baby is less important. This is because, after the birth of the first baby, the second baby has lots more room to move. It may turn naturally into a head-first position or a doctor may be able to help the baby to turn. See the RCOG patient information Multiple pregnancy: having more than one baby .
If you would like further information on breech babies and breech birth, you should speak with your healthcare professional.
Further information
- NHS information on breech babies
- NCT information on breech babies
If you are asked to make a choice, you may have lots of questions that you want to ask. You may also want to talk over your options with your family or friends. It can help to write a list of the questions you want answered and take it to your appointment.
Ask 3 Questions
To begin with, try to make sure you get the answers to 3 key questions , if you are asked to make a choice about your healthcare:
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to help me make a decision that is right for me?
*Ask 3 Questions is based on Shepherd et al. Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counselling, 2011;84:379-85
- https://aqua.nhs.uk/resources/shared-decision-making-case-studies/
Sources and acknowledgements
This information has been developed by the RCOG Patient Information Committee. It is based on the RCOG Green-top Clinical Guidelines No. 20a External Cephalic Version and Reducing Incidence of Term Breech Presentation and No. 20b Management of Breech Presentation . The guidelines contain a full list of the sources of evidence we have used.
This information was reviewed before publication by women attending clinics in Nottingham, Essex, Inverness, Manchester, London, Sussex, Bristol, Basildon and Oxford, by the RCOG Women’s Network and by the RCOG Women’s Voices Involvement Panel.
Please give us feedback by completing our feedback survey:
- Members of the public – patient information feedback
- Healthcare professionals – patient information feedback
External Cephalic Version and Reducing the Incidence of Term Breech Presentation Green-top Guideline
Management of Breech Presentation Green-top Guideline

COMMENTS
Breech presentation refers to the fetus in the longitudinal lie with the buttocks or lower extremity entering the pelvis first. The three types of breech presentation include frank breech, complete breech, and incomplete breech. ... Before 26 weeks, there is a lack of quality clinical evidence to guide mode of delivery. One large retrospective ...
Since breech baby's spine is vertical, the womb is "stretched" upwards. We expect babies to turn head down by 28-32 weeks. Breech may not be an issue until 32-34 weeks. If you know your womb has an unusual limitation in shape or size, such as a bicornate uterus then begin body balancing before pregnancy and once 15 weeks in pregnancy.
In the last weeks of pregnancy, a fetus usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation.A breech presentation occurs when the fetus's buttocks, feet, or both are in place to come out first during birth. This happens in 3-4% of full-term births.
The main types of breech presentation are: Frank breech - Both hips are flexed and both knees are extended so that the feet are adjacent to the head ( figure 1 ); accounts for 50 to 70 percent of breech fetuses at term. Complete breech - Both hips and both knees are flexed ( figure 2 ); accounts for 5 to 10 percent of breech fetuses at term.
Summary. Breech presentation refers to the baby presenting for delivery with the buttocks or feet first rather than head. Associated with increased morbidity and mortality for the mother in terms of emergency cesarean section and placenta previa; and for the baby in terms of preterm birth, small fetal size, congenital anomalies, and perinatal ...
Learn more about the types, causes, and risks of breech presentation, along with how breech babies are typically delivered. ... These are usually scheduled between 38 and 39 weeks of pregnancy ...
Breech presentation is defined as a fetus in a longitudinal lie with the buttocks or feet closest to the cervix. This occurs in 3-4% of all deliveries. ... (26-36 6/7 weeks) breech from 2000 to 2011, over three quarters of whom intended to deliver vaginally. In this overall cohort, there was no significant difference in perinatal mortality ...
Breech Births. In the last weeks of pregnancy, a baby usually moves so his or her head is positioned to come out of the vagina first during birth. This is called a vertex presentation. A breech presentation occurs when the baby's buttocks, feet, or both are positioned to come out first during birth. This happens in 3-4% of full-term births.
At full term, around 3%-4% of births are breech. The different types of breech presentations include: Complete: The fetus's knees are bent, and the buttocks are presenting first. Frank: The fetus's legs are stretched upward toward the head, and the buttocks are presenting first. Footling: The fetus's foot is showing first.
At 28 weeks or less, about a quarter of babies are breech, and at 32 weeks, 7 percent are breech. By the end of pregnancy, only 3 to 4 percent of babies are in breech position. ... New and old predictive factors for breech presentation: our experience in 14433 singleton pregnancies and a literature review. ... 26. weeks pregnant. 27. weeks ...
Labour with a preterm breech should be managed as with a term breech. C. Where there is head entrapment, incisions in the cervix (vaginal birth) or vertical uterine D incision extension (caesarean section) may be used, with or without tocolysis. Evidence concerning the management of preterm labour with a breech presentation is lacking.
Introduction. Breech presentation of the fetus in late pregnancy may result in prolonged or obstructed labour with resulting risks to both woman and fetus. Interventions to correct breech presentation (to cephalic) before labour and birth are important for the woman's and the baby's health. The aim of this review is to determine the most ...
If you've had a previous breech baby, you run a somewhat higher chance of subsequent babies turning out breech as well. Premature birth. The earlier your baby is born, the higher the chance she'll be breech: About 25 percent of babies are breech at 28 weeks, but only 3 percent or so are breech at term. You or your partner were breech.
Frank breech. When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head.
The incidence of breech presentation is approximately 20% at 28 weeks gestation, 16% at 32 weeks gestation and 3-4% at term. Therefore, breech presentation is more common in preterm labour. Most fetuses with breech presentation in the early third trimester will turn spontaneously and be cephalic at term.
This is called breech presentation. While most breech babies are born healthy, complications can occur if not treated. As you prepare for the arrival of your baby and your 36-week appointment, read on to know more about breech births and your options for safely delivering your baby. Why would my baby be breech?
Complete. Baby's buttocks are pointing down and legs are crossed beneath it. Frank. Baby's bottom is positioned down and legs are pointed up toward the head. Footling. Baby has one leg pointed toward the cervix, poised to deliver before the rest of their body. "There's also a double footling breech, where the baby's feet and legs are ...
A woman in labor with a breech presentation <37 weeks gestation is an area of clinical controversy. Optimal mode of delivery for preterm breech has not been fully evaluated in clinical trials, and the relative risks for the preterm infant and mother remain unclear. ... 26. Royal College of Obstetricians and Gynaecologists. Antepartum ...
Turning a breech baby. If your baby is in a breech position at 36 weeks, you'll usually be offered an external cephalic version (ECV). This is when a healthcare professional, such as an obstetrician, tries to turn the baby into a head-down position by applying pressure on your abdomen. It's a safe procedure, although it can be a bit uncomfortable.
Babies lying bottom first or feet first in the uterus (womb) instead of in the usual head-first position are called breech babies. Breech is very common in early pregnancy, and by 36-37 weeks of pregnancy, most babies turn naturally into the head-first position. Towards the end of pregnancy, only 3-4 in every 100 (3-4%) babies are in the breech ...
A breech presentation is defined when a baby is in a longitudinal lie with the buttocks or feet presenting at the pelvic brim and the head occupying the upper pole of uterus. • The incidence of a breech presentation at term is 3-4% (where term is defined as 3742 weeks)