- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- Writing a case report...
Writing a case report in 10 steps
- Related content
- Peer review
- Victoria Stokes , foundation year 2 doctor, trauma and orthopaedics, Basildon Hospital ,
- Caroline Fertleman , paediatrics consultant, The Whittington Hospital NHS Trust
- victoria.stokes1{at}nhs.net
Victoria Stokes and Caroline Fertleman explain how to turn an interesting case or unusual presentation into an educational report
It is common practice in medicine that when we come across an interesting case with an unusual presentation or a surprise twist, we must tell the rest of the medical world. This is how we continue our lifelong learning and aid faster diagnosis and treatment for patients.
It usually falls to the junior to write up the case, so here are a few simple tips to get you started.
First steps
Begin by sitting down with your medical team to discuss the interesting aspects of the case and the learning points to highlight. Ideally, a registrar or middle grade will mentor you and give you guidance. Another junior doctor or medical student may also be keen to be involved. Allocate jobs to split the workload, set a deadline and work timeframe, and discuss the order in which the authors will be listed. All listed authors should contribute substantially, with the person doing most of the work put first and the guarantor (usually the most senior team member) at the end.
Getting consent
Gain permission and written consent to write up the case from the patient or parents, if your patient is a child, and keep a copy because you will need it later for submission to journals.
Information gathering
Gather all the information from the medical notes and the hospital’s electronic systems, including copies of blood results and imaging, as medical notes often disappear when the patient is discharged and are notoriously difficult to find again. Remember to anonymise the data according to your local hospital policy.
Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
Coming up with a title
Discuss a title with your supervisor and other members of the team, as this provides the focus for your article. The title should be concise and interesting but should also enable people to find it in medical literature search engines. Also think about how you will present your case study—for example, a poster presentation or scientific paper—and consider potential journals or conferences, as you may need to write in a particular style or format.
Background research
Research the disease/pathology that is the focus of your article and write a background paragraph or two, highlighting the relevance of your case report in relation to this. If you are struggling, seek the opinion of a specialist who may know of relevant articles or texts. Another good resource is your hospital library, where staff are often more than happy to help with literature searches.
How your case is different
Move on to explore how the case presented differently to the admitting team. Alternatively, if your report is focused on management, explore the difficulties the team came across and alternative options for treatment.
Finish by explaining why your case report adds to the medical literature and highlight any learning points.
Writing an abstract
The abstract should be no longer than 100-200 words and should highlight all your key points concisely. This can be harder than writing the full article and needs special care as it will be used to judge whether your case is accepted for presentation or publication.
Discuss with your supervisor or team about options for presenting or publishing your case report. At the very least, you should present your article locally within a departmental or team meeting or at a hospital grand round. Well done!
Competing interests: We have read and understood BMJ’s policy on declaration of interests and declare that we have no competing interests.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 21, Issue 1
- What is a case study?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Roberta Heale 1 ,
- Alison Twycross 2
- 1 School of Nursing , Laurentian University , Sudbury , Ontario , Canada
- 2 School of Health and Social Care , London South Bank University , London , UK
- Correspondence to Dr Roberta Heale, School of Nursing, Laurentian University, Sudbury, ON P3E2C6, Canada; rheale{at}laurentian.ca
https://doi.org/10.1136/eb-2017-102845
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
What is it?
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research. 1 However, very simply… ‘a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units’. 1 A case study has also been described as an intensive, systematic investigation of a single individual, group, community or some other unit in which the researcher examines in-depth data relating to several variables. 2
Often there are several similar cases to consider such as educational or social service programmes that are delivered from a number of locations. Although similar, they are complex and have unique features. In these circumstances, the evaluation of several, similar cases will provide a better answer to a research question than if only one case is examined, hence the multiple-case study. Stake asserts that the cases are grouped and viewed as one entity, called the quintain . 6 ‘We study what is similar and different about the cases to understand the quintain better’. 6
The steps when using case study methodology are the same as for other types of research. 6 The first step is defining the single case or identifying a group of similar cases that can then be incorporated into a multiple-case study. A search to determine what is known about the case(s) is typically conducted. This may include a review of the literature, grey literature, media, reports and more, which serves to establish a basic understanding of the cases and informs the development of research questions. Data in case studies are often, but not exclusively, qualitative in nature. In multiple-case studies, analysis within cases and across cases is conducted. Themes arise from the analyses and assertions about the cases as a whole, or the quintain, emerge. 6
Benefits and limitations of case studies
If a researcher wants to study a specific phenomenon arising from a particular entity, then a single-case study is warranted and will allow for a in-depth understanding of the single phenomenon and, as discussed above, would involve collecting several different types of data. This is illustrated in example 1 below.
Using a multiple-case research study allows for a more in-depth understanding of the cases as a unit, through comparison of similarities and differences of the individual cases embedded within the quintain. Evidence arising from multiple-case studies is often stronger and more reliable than from single-case research. Multiple-case studies allow for more comprehensive exploration of research questions and theory development. 6
Despite the advantages of case studies, there are limitations. The sheer volume of data is difficult to organise and data analysis and integration strategies need to be carefully thought through. There is also sometimes a temptation to veer away from the research focus. 2 Reporting of findings from multiple-case research studies is also challenging at times, 1 particularly in relation to the word limits for some journal papers.
Examples of case studies
Example 1: nurses’ paediatric pain management practices.
One of the authors of this paper (AT) has used a case study approach to explore nurses’ paediatric pain management practices. This involved collecting several datasets:
Observational data to gain a picture about actual pain management practices.
Questionnaire data about nurses’ knowledge about paediatric pain management practices and how well they felt they managed pain in children.
Questionnaire data about how critical nurses perceived pain management tasks to be.
These datasets were analysed separately and then compared 7–9 and demonstrated that nurses’ level of theoretical did not impact on the quality of their pain management practices. 7 Nor did individual nurse’s perceptions of how critical a task was effect the likelihood of them carrying out this task in practice. 8 There was also a difference in self-reported and observed practices 9 ; actual (observed) practices did not confirm to best practice guidelines, whereas self-reported practices tended to.
Example 2: quality of care for complex patients at Nurse Practitioner-Led Clinics (NPLCs)
The other author of this paper (RH) has conducted a multiple-case study to determine the quality of care for patients with complex clinical presentations in NPLCs in Ontario, Canada. 10 Five NPLCs served as individual cases that, together, represented the quatrain. Three types of data were collected including:
Review of documentation related to the NPLC model (media, annual reports, research articles, grey literature and regulatory legislation).
Interviews with nurse practitioners (NPs) practising at the five NPLCs to determine their perceptions of the impact of the NPLC model on the quality of care provided to patients with multimorbidity.
Chart audits conducted at the five NPLCs to determine the extent to which evidence-based guidelines were followed for patients with diabetes and at least one other chronic condition.
The three sources of data collected from the five NPLCs were analysed and themes arose related to the quality of care for complex patients at NPLCs. The multiple-case study confirmed that nurse practitioners are the primary care providers at the NPLCs, and this positively impacts the quality of care for patients with multimorbidity. Healthcare policy, such as lack of an increase in salary for NPs for 10 years, has resulted in issues in recruitment and retention of NPs at NPLCs. This, along with insufficient resources in the communities where NPLCs are located and high patient vulnerability at NPLCs, have a negative impact on the quality of care. 10
These examples illustrate how collecting data about a single case or multiple cases helps us to better understand the phenomenon in question. Case study methodology serves to provide a framework for evaluation and analysis of complex issues. It shines a light on the holistic nature of nursing practice and offers a perspective that informs improved patient care.
- Gustafsson J
- Calanzaro M
- Sandelowski M
Competing interests None declared.
Provenance and peer review Commissioned; internally peer reviewed.
Read the full text or download the PDF:
Health Case Studies
(29 reviews)
Glynda Rees, British Columbia Institute of Technology
Rob Kruger, British Columbia Institute of Technology
Janet Morrison, British Columbia Institute of Technology
Copyright Year: 2017
Publisher: BCcampus
Language: English
Formats Available
Conditions of use.
Learn more about reviews.
Reviewed by Jessica Sellars, Medical assistant office instructor, Blue Mountain Community College on 10/11/23
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and... read more
Comprehensiveness rating: 5 see less
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and plan. There is an appendix to refer to as well if you are needing to find something specific quickly. I have been looking for something like this to help my students have a base to do their project on. This is the most comprehensive version I have found on the subject.
Content Accuracy rating: 5
This is a book compiled of medical case studies. It is very accurate and can be used to learn from great care and mistakes.
Relevance/Longevity rating: 5
This material is very relevant in this context. It also has plenty of individual case studies to utilize in many ways in all sorts of medical courses. This is a very useful textbook and it will continue to be useful for a very long time as you can still learn from each study even if medicine changes through out the years.
Clarity rating: 5
The author put a lot of thought into the ease of accessibility and reading level of the target audience. There is even a "how to use this resource" section which could be extremely useful to students.
Consistency rating: 5
The text follows a very consistent format throughout the book.
Modularity rating: 5
Each case study is individual broken up and in a group of similar case studies. This makes it extremely easy to utilize.
Organization/Structure/Flow rating: 5
The book is very organized and the appendix is through. It flows seamlessly through each case study.
Interface rating: 5
I had no issues navigating this book, It was clearly labeled and very easy to move around in.
Grammatical Errors rating: 5
I did not catch any grammar errors as I was going through the book
Cultural Relevance rating: 5
This is a challenging question for any medical textbook. It is very culturally relevant to those in medical or medical office degrees.
I have been looking for something like this for years. I am so happy to have finally found it.
Reviewed by Cindy Sun, Assistant Professor, Marshall University on 1/7/23
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and... read more
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and students. For faculty, the introduction section titled ‘How to use this resource’ and individual notes to educators before each case study contain application tips. An appendix overview lists key elements as issues / concepts, scenario context, and healthcare roles for each case study. For students, learning objectives are presented at the beginning of each case study to provide a framework of expectations.
The content is presented accurately and realistic.
The case studies read similar to ‘A Day In the Life of…’ with detailed intraprofessional communications similar to what would be overheard in patient care areas. The authors present not only the view of the patient care nurse, but also weave interprofessional vantage points through each case study by including patient interaction with individual professionals such as radiology, physician, etc.
In addition to objective assessment findings, the authors integrate standard orders for each diagnosis including medications, treatments, and tests allowing the student to incorporate pathophysiology components to their assessments.
Each case study is arranged in the same framework for consistency and ease of use.
This compilation of eight healthcare case studies focusing on new onset and exacerbation of prevalent diagnoses, such as heart failure, deep vein thrombosis, cancer, and chronic obstructive pulmonary disease advancing to pneumonia.
Each case study has a photo of the ‘patient’. Simple as this may seem, it gives an immediate mental image for the student to focus.
Interface rating: 4
As noted by previous reviewers, most of the links do not connect active web pages. This may be due to the multiple options for accessing this resource (pdf download, pdf electronic, web view, etc.).
Grammatical Errors rating: 4
A minor weakness that faculty will probably need to address prior to use is regarding specific term usages differences between Commonwealth countries and United States, such as lung sound descriptors as ‘quiet’ in place of ‘diminished’ and ‘puffers’ in place of ‘inhalers’.
The authors have provided a multicultural, multigenerational approach in selection of patient characteristics representing a snapshot of today’s patient population. Additionally, one case study focusing on heart failure is about a middle-aged adult, contrasting to the average aged patient the students would normally see during clinical rotations. This option provides opportunities for students to expand their knowledge on risk factors extending beyond age.
This resource is applicable to nursing students learning to care for patients with the specific disease processes presented in each case study or for the leadership students focusing on intraprofessional communication. Educators can assign as a supplement to clinical experiences or as an in-class application of knowledge.
Reviewed by Stephanie Sideras, Assistant Professor, University of Portland on 8/15/22
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five... read more
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five overarching learning objectives pulled from the Institute of Medicine core competencies will clearly resonate with any faculty familiar with Quality and Safety Education for Nurses curriculum.
The presentation of symptoms, treatments and management of the health alterations was accurate. Dialogue between the the interprofessional team was realistic. At times the formatting of lab results was confusing as they reflected reference ranges specific to the Canadian healthcare system but these occurrences were minimal and could be easily adapted.
The focus for learning from these case studies was communication - patient centered communication and interprofessional team communication. Specific details, such as drug dosing, was minimized, which increases longevity and allows for easy individualization of the case data.
While some vocabulary was specific to the Canadian healthcare system, overall the narrative was extremely engaging and easy to follow. Subjective case data from patient or provider were formatted in italics and identified as 'thoughts'. Objective and behavioral case data were smoothly integrated into the narrative.
The consistency of formatting across the eight cases was remarkable. Specific learning objectives are identified for each case and these remain consistent across the range of cases, varying only in the focus for the goals for each different health alterations. Each case begins with presentation of essential patient background and the progress across the trajectory of illness as the patient moves from location to location encountering different healthcare professionals. Many of the characters (the triage nurse in the Emergency Department, the phlebotomist) are consistent across the case situations. These consistencies facilitate both application of a variety of teaching methods and student engagement with the situated learning approach.
Case data is presented by location and begins with the patient's first encounter with the healthcare system. This allows for an examination of how specific trajectories of illness are manifested and how care management needs to be prioritized at different stages. This approach supports discussions of care transitions and the complexity of the associated interprofessional communication.
The text is well organized. The case that has two levels of complexity is clearly identified
The internal links between the table of contents and case specific locations work consistently. In the EPUB and the Digital PDF the external hyperlinks are inconsistently valid.
The grammatical errors were minimal and did not detract from readability
Cultural diversity is present across the cases in factors including race, ethnicity, socioeconomic status, family dynamics and sexual orientation.
The level of detail included in these cases supports a teaching approach to address all three spectrums of learning - knowledge, skills and attitudes - necessary for the development of competent practice. I also appreciate the inclusion of specific assessment instruments that would facilitate a discussion of evidence based practice. I will enjoy using these case to promote clinical reasoning discussions of data that is noticed and interpreted with the resulting prioritizes that are set followed by reflections that result from learner choices.
Reviewed by Chris Roman, Associate Professor, Butler University on 5/19/22
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various... read more
Comprehensiveness rating: 4 see less
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various learning strategies to be employed to leverage the cases for deeper student learning and application.
The narrative form of the cases is less subject to issues of accuracy than a more content-based book would be. That said, the cases are realistic and reasonable, avoiding being too mundane or too extreme.
These cases are narrative and do not include many specific mentions of drugs, dosages, or other aspects of clinical care that may grow/evolve as guidelines change. For this reason, the cases should be “evergreen” and can be modified to suit different types of learners.
Clarity rating: 4
The text is written in very accessible language and avoids heavy use of technical language. Depending on the level of learner, this might even be too simplistic and omit some details that would be needed for physicians, pharmacists, and others to make nuanced care decisions.
The format is very consistent with clear labeling at transition points.
The authors point out in the introductory materials that this text is designed to be used in a modular fashion. Further, they have built in opportunities to customize each cases, such as giving dates of birth at “19xx” to allow for adjustments based on instructional objectives, etc.
The organization is very easy to follow.
I did not identify any issues in navigating the text.
The text contains no grammatical errors, though the language is a little stiff/unrealistic in some cases.
Cases involve patients and members of the care team that are of varying ages, genders, and racial/ethnic backgrounds
Reviewed by Trina Larery, Assistant Professor, Pittsburg State University on 4/5/22
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand... read more
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand and apply to the classroom. The E-reader format included hyperlinks that bring the students to subsequent clinical studies.
Content Accuracy rating: 4
The treatments were explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse. The case studies were accurate in explanation. The DVT case study incorrectly identifies the location of the clot in the popliteal artery instead of in the vein.
The content is relevant to a variety of different types of health care providers and due to the general nature of the cases, will remain relevant over time. Updates should be made annually to the hyperlinks and to assure current standard of practice is still being met.
Clear, simple and easy to read.
Consistent with healthcare terminology and framework throughout all eight case studies.
The text is modular. Cases can be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point providing great flexibility. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
The book is well organized, presenting in a logical clear fashion. The appendix allows the student to move about the case study without difficulty.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change based on current guidelines. A few hyperlinks had "page not found".
Few grammatical errors were noted in text.
The case studies include people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. There are roughly 25 broken online links or "pages not found", care needs to be taken to update at least annually and assure links are valid and utilizing the most up to date information.
Reviewed by Benjamin Silverberg, Associate Professor/Clinician, West Virginia University on 3/24/22
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what... read more
Comprehensiveness rating: 3 see less
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what is going on where, especially since each case is largely conversation-based. Since this presents 8 cases (really 7 with one being expanded upon), there are many medical topics (and venues) that are not included. It's impossible to include every kind of situation, but I'd love to see inclusion of sexual health, renal pathology, substance abuse, etc.
Though there are differences in how care can be delivered based on personal style, changing guidelines, available supplies, etc, the medical accuracy seems to be high. I did not detect bias or industry influence.
Relevance/Longevity rating: 4
Medications are generally listed as generics, with at least current dosing recommendations. The text gives a picture of what care looks like currently, but will be a little challenging to update based on new guidelines (ie, it can be hard to find the exact page in which a medication is dosed/prescribed). Even if the text were to be a little out of date, an instructor can use that to point out what has changed (and why).
Clear text, usually with definitions of medical slang or higher-tier vocabulary. Minimal jargon and there are instances where the "characters" are sorting out the meaning as well, making it accessible for new learners, too.
Overall, the style is consistent between cases - largely broken up into scenes and driven by conversation rather than descriptions of what is happening.
There are 8 (well, again, 7) cases which can be reviewed in any order. Case #2 builds upon #1, which is intentional and a good idea, though personally I would have preferred one case to have different possible outcomes or even a recurrence of illness. Each scene within a case is reasonably short.
Organization/Structure/Flow rating: 4
These cases are modular and don't really build on concepts throughout. As previously stated, case #2 builds upon #1, but beyond that, there is no progression. (To be sure, the authors suggest using case #1 for newer learners and #2 for more advanced ones.) The text would benefit from thematic grouping, a longer introduction and debriefing for each case (there are learning objectives but no real context in medical education nor questions to reflect on what was just read), and progressively-increasing difficulty in medical complexity, ethics, etc.
I used the PDF version and had no interface issues. There are minimal photographs and charts. Some words are marked in blue but those did not seem to be hyperlinked anywhere.
No noticeable errors in grammar, spelling, or formatting were noted.
I appreciate that some diversity of age and ethnicity were offered, but this could be improved. There were Canadian Indian and First Nations patients, for example, as well as other characters with implied diversity, but there didn't seem to be any mention of gender diverse or non-heterosexual people, or disabilities. The cases tried to paint family scenes (the first patient's dog was fairly prominently mentioned) to humanize them. Including more cases would allow for more opportunities to include sex/gender minorities, (hidden) disabilities, etc.
The text (originally from 2017) could use an update. It could be used in conjunction with other Open Texts, as a compliment to other coursework, or purely by itself. The focus is meant to be on improving communication, but there are only 3 short pages at the beginning of the text considering those issues (which are really just learning objectives). In addition to adding more cases and further diversity, I personally would love to see more discussion before and after the case to guide readers (and/or instructors). I also wonder if some of the ambiguity could be improved by suggesting possible health outcomes - this kind of counterfactual comparison isn't possible in real life and could be really interesting in a text. Addition of comprehension/discussion questions would also be worthwhile.
Reviewed by Danielle Peterson, Assistant Professor, University of Saint Francis on 12/31/21
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare... read more
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare workers in acute hospital settings. The cases are primarily set in the inpatient hospital setting, so the bulk of the clinical information is basic emergency care and inpatient protocol: vitals, breathing, medication management, etc. The text provides a table of contents at opening of the text and a handy appendix at the conclusion of the text that outlines each case’s issue(s), scenario, and healthcare roles. No index or glossary present.
Although easy to update, it should be noted that the cases are taking place in a Canadian healthcare system. Terms may be unfamiliar to some students including “province,” “operating theatre,” “physio/physiotherapy,” and “porter.” Units of measurement used include Celsius and meters. Also, the issue of managed care, health insurance coverage, and length of stay is missing for American students. These are primary issues that dictate much of the healthcare system in the US and a primary job function of social workers, nurse case managers, and medical professionals in general. However, instructors that wish to add this to the case studies could do so easily.
The focus of this text is on healthcare communication which makes it less likely to become obsolete. Much of the clinical information is stable healthcare practice that has been standard of care for quite some time. Nevertheless, given the nature of text, updates would be easy to make. Hyperlinks should be updated to the most relevant and trustworthy sources and checked frequently for effectiveness.
The spacing that was used to note change of speaker made for ease of reading. Although unembellished and plain, I expect students to find this format easy to digest and interesting, especially since the script is appropriately balanced with ‘human’ qualities like the current TV shows and songs, the use of humor, and nonverbal cues.
A welcome characteristic of this text is its consistency. Each case is presented in a similar fashion and the roles of the healthcare team are ‘played’ by the same character in each of the scenarios. This allows students to see how healthcare providers prioritize cases and juggle the needs of multiple patients at once. Across scenarios, there was inconsistency in when clinical terms were hyperlinked.
The text is easily divisible into smaller reading sections. However, since the nature of the text is script-narrative format, if significant reorganization occurs, one will need to make sure that the communication of the script still makes sense.
The text is straightforward and presented in a consistent fashion: learning objectives, case history, a script of what happened before the patient enters the healthcare setting, and a script of what happens once the patient arrives at the healthcare setting. The authors use the term, “ideal interactions,” and I would agree that these cases are in large part, ‘best case scenarios.’ Due to this, the case studies are well organized, clear, logical, and predictable. However, depending on the level of student, instructors may want to introduce complications that are typical in the hospital setting.
The interface is pleasing and straightforward. With exception to the case summary and learning objectives, the cases are in narrative, script format. Each case study supplies a photo of the ‘patient’ and one of the case studies includes a link to a 3-minute video that introduces the reader to the patient/case. One of the highlights of this text is the use of hyperlinks to various clinical practices (ABG, vital signs, transfer of patient). Unfortunately, a majority of the links are broken. However, since this is an open text, instructors can update the links to their preference.
Although not free from grammatical errors, those that were noticed were minimal and did not detract from reading.
Cultural Relevance rating: 4
Cultural diversity is visible throughout the patients used in the case studies and includes factors such as age, race, socioeconomic status, family dynamics, and sexual orientation. A moderate level of diversity is noted in the healthcare team with some stereotypes: social workers being female, doctors primarily male.
As a social work instructor, I was grateful to find a text that incorporates this important healthcare role. I would have liked to have seen more content related to advance directives, mediating decision making between the patient and care team, emotional and practical support related to initial diagnosis and discharge planning, and provision of support to colleagues, all typical roles of a medical social worker. I also found it interesting that even though social work was included in multiple scenarios, the role was only introduced on the learning objectives page for the oncology case.
Reviewed by Crystal Wynn, Associate Professor, Virginia State University on 7/21/21
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied... read more
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied health care team members are represented within the case study. Key terms appear throughout the case study textbook and readers are able to click on a hyperlink which directs them to the definition and an explanation of the key term.
Content is accurate, error-free and unbiased.
The content is up-to-date, but not in a way that will quickly make the text obsolete within a short period of time. The text is written and/or arranged in such a way that necessary updates will be relatively easy and straightforward to implement.
The text is written in lucid, accessible prose, and provides adequate context for any jargon/technical terminology used
The text is internally consistent in terms of terminology and framework.
The text is easily and readily divisible into smaller reading sections that can be assigned at different points within the course. Each case can be divided into a chronic disease state unit, which will allow the reader to focus on one section at a time.
Organization/Structure/Flow rating: 3
The topics in the text are presented in a logical manner. Each case provides an excessive amount of language that provides a description of the case. The cases in this text reads more like a novel versus a clinical textbook. The learning objectives listed within each case should be in the form of questions or activities that could be provided as resources for instructors and teachers.
Interface rating: 3
There are several hyperlinks embedded within the textbook that are not functional.
The text contains no grammatical errors.
Cultural Relevance rating: 3
The text is not culturally insensitive or offensive in any way. More examples of cultural inclusiveness is needed throughout the textbook. The cases should be indicative of individuals from a variety of races and ethnicities.
Reviewed by Rebecca Hillary, Biology Instructor, Portland Community College on 6/15/21
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health... read more
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health care program. I read the textbook in E-reader format and this includes hyperlinks that bring the students to subsequent clinical study if the book is being used in a clinical classroom. This book is significantly more comprehensive in its approach from other case studies I have read because it provides a bird’s eye view of the many clinicians, technicians, and hospital staff working with one patient. The book also provides real time measurements for patients that change as they travel throughout the hospital until time of discharge.
Each case gave an accurate sense of the chaos that would be present in an emergency situation and show how the conditions affect the practitioners as well as the patients. The reader gets an accurate big picture--a feel for each practitioner’s point of view as well as the point of view of the patient and the patient’s family as the clock ticks down and the patients are subjected to a number of procedures. The clinical information contained in this textbook is all in hyperlinks containing references to clinical skills open text sources or medical websites. I did find one broken link on an external medical resource.
The diseases presented are relevant and will remain so. Some of the links are directly related to the Canadian Medical system so they may not be applicable to those living in other regions. Clinical links may change over time but the text itself will remain relevant.
Each case study clearly presents clinical data as is it recorded in real time.
Each case study provides the point of view of several practitioners and the patient over several days. While each of the case studies covers different pathology they all follow this same format, several points of view and data points, over a number of days.
The case studies are divided by days and this was easy to navigate as a reader. It would be easy to assign one case study per body system in an Anatomy and Physiology course, or to divide them up into small segments for small in class teaching moments.
The topics are presented in an organized way showing clinical data over time and each case presents a large number of view points. For example, in the first case study, the patient is experiencing difficulty breathing. We follow her through several days from her entrance to the emergency room. We meet her X Ray Technicians, Doctor, Nurses, Medical Assistant, Porter, Physiotherapist, Respiratory therapist, and the Lab Technicians running her tests during her stay. Each practitioner paints the overall clinical picture to the reader.
I found the text easy to navigate. There were not any figures included in the text, only clinical data organized in charts. The figures were all accessible via hyperlink. Some figures within the textbook illustrating patient scans could have been helpful but I did not have trouble navigating the links to visualize the scans.
I did not see any grammatical errors in the text.
The patients in the text are a variety of ages and have a variety of family arrangements but there is not much diversity among the patients. Our seven patients in the eight case studies are mostly white and all cis gendered.
Some of the case studies, for example the heart failure study, show clinical data before and after drug treatments so the students can get a feel for mechanism in physiological action. I also liked that the case studies included diet and lifestyle advice for the patients rather than solely emphasizing these pharmacological interventions. Overall, I enjoyed reading through these case studies and I plan to utilize them in my Anatomy and Physiology courses.
Reviewed by Richard Tarpey, Assistant Professor, Middle Tennessee State University on 5/11/21
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate... read more
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate for entry-level health care students. The book includes important health problems, but I would like to see coverage of at least one more chronic/lifestyle issue such as diabetes. The book covers adult issues only.
Content is accurate without bias
The content of the book is relevant and up-to-date. It addresses conditions that are prevalent in today's population among adults. There are no pediatric cases, but this does not significantly detract from the usefulness of the text. The format of the book lends to easy updating of data or information.
The book is written with clarity and is easy to read. The writing style is accessible and technical terminology is explained with links to more information.
Consistency is present. Lack of consistency is typically a problem with case study texts, but this book is consistent with presentation, format, and terminology throughout each of the eight cases.
The book has high modularity. Each of the case studies can be used independently from the others providing flexibility. Additionally, each case study can be partitioned for specific learning objectives based on the learning objectives of the course or module.
The book is well organized, presenting students conceptually with differing patient flow patterns through a hospital. The patient information provided at the beginning of each case is a wonderful mechanism for providing personal context for the students as they consider the issues. Many case studies focus on the problem and the organization without students getting a patient's perspective. The patient perspective is well represented in these cases.
The navigation through the cases is good. There are some terminology and procedure hyperlinks within the cases that do not work when accessed. This is troubling if you intend to use the text for entry-level health care students since many of these links are critical for a full understanding of the case.
There are some non-US variants of spelling and a few grammatical errors, but these do not detract from the content of the messages of each case.
The book is inclusive of differing backgrounds and perspectives. No insensitive or offensive references were found.
I like this text for its application flexibility. The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology. The content is also helpful for the identification of healthcare administration managerial issues for students to consider. The book has many applications.
Reviewed by Paula Baldwin, Associate Professor/Communication Studies, Western Oregon University on 5/10/21
The different case studies fall on a range, from crisis care to chronic illness care. read more
The different case studies fall on a range, from crisis care to chronic illness care.
The contents seems to be written as they occurred to represent the most complete picture of each medical event's occurence.
These case studies are from the Canadian medical system, but that does not interfere with it's applicability.
It is written for a medical audience, so the terminology is mostly formal and technical.
Some cases are shorter than others and some go in more depth, but it is not problematic.
The eight separate case studies is the perfect size for a class in the quarter system. You could combine this with other texts, videos or learning modalities, or use it alone.
As this is a case studies book, there is not a need for a logical progression in presentation of topics.
No problems in terms of interface.
I have not seen any grammatical errors.
I did not see anything that was culturally insensitive.
I used this in a Health Communication class and it has been extraordinarily successful. My studies are analyzing the messaging for the good, the bad, and the questionable. The case studies are widely varied and it gives the class insights into hospital experiences, both front and back stage, that they would not normally be able to examine. I believe that because it is based real-life medical incidents, my students are finding the material highly engaging.
Reviewed by Marlena Isaac, Instructor, Aiken Technical College on 4/23/21
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with... read more
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with a situation in clinical they are not surprised and now how to move through it effectively.
The case studies provided accurate information that relates to the named disease.
It is relevant to health care studies and the development of critical thinking.
Cases are straightforward with great clinical information.
Clinical information is provided concisely.
Appropriate for clinical case study.
Presented to facilitate information gathering.
Takes a while to navigate in the browser.
Cultural Relevance rating: 1
Text lacks adequate representation of minorities.
Reviewed by Kim Garcia, Lecturer III, University of Texas Rio Grande Valley on 11/16/20
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at... read more
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at different levels of clinical knowledge. The human element of both patient and health care provider is well captured. The cases are presented with a focus on interprofessional interaction and collaboration, more so than teaching medical content.
Content is accurate and un-biased. No errors noted. Most diagnostic and treatment information is general so it will remain relevant over time. The content of these cases is more appropriate for teaching interprofessional collaboration and less so for teaching the medical care for each diagnosis.
The content is relevant to a variety of different types of health care providers (nurses, radiologic technicians, medical laboratory personnel, etc) and due to the general nature of the cases, will remain relevant over time.
Easy to read. Clear headings are provided for sections of each case study and these section headings clearly tell when time has passed or setting has changed. Enough description is provided to help set the scene for each part of the case. Much of the text is written in the form of dialogue involving patient, family and health care providers, making it easy to adapt for role play. Medical jargon is limited and links for medical terms are provided to other resources that expound on medical terms used.
The text is consistent in structure of each case. Learning objectives are provided. Cases generally start with the patient at home and move with the patient through admission, testing and treatment, using a variety of healthcare services and encountering a variety of personnel.
The text is modular. Cases could be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
Each case follows a patient in a logical, chronologic fashion. A clear table of contents and appendix are provided which allows the user to quickly locate desired content. It would be helpful if the items in the table of contents and appendix were linked to the corresponding section of the text.
The hyperlinks to content outside this book work, however using the back arrow on your browser returns you to the front page of the book instead of to the point at which you left the text. I would prefer it if the hyperlinks opened in a new window or tab so closing that window or tab would leave you back where you left the text.
No grammatical errors were noted.
The text is culturally inclusive and appropriate. Characters, both patients and care givers are of a variety of races, ethnicities, ages and backgrounds.
I enjoyed reading the cases and reviewing this text. I can think of several ways in which I will use this content.
Reviewed by Raihan Khan, Instructor/Assistant Professor, James Madison University on 11/3/20
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients. read more
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients.
The health information contained in the textbook is mostly accurate.
I think the book is written focusing on the current culture and health issues faced by the patients. To keep the book relevant in the future, the contexts especially the culture/lifestyle/health care modalities, etc. would need to be updated regularly.
The language is pretty simple, clear, and easy to read.
There is no complaint about consistency. One of the main issues of writing a book, consistency was well managed by the authors.
The book is easy to explore based on how easy the setup is. Students can browse to the specific section that they want to read without much hassle of finding the correct information.
The organization is simple but effective. The authors organized the book based on what can happen in a patient's life and what possible scenarios students should learn about the disease. From that perspective, the book does a good job.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change that is beyond the author's control. It's frustrating for the reader when the external link shows no information.
The book is free of any major language and grammatical errors.
The book might do a little better in cultural competency. e.g. Last name Singh is mainly for Sikh people. In the text Harj and Priya Singh are Muslim. the authors can consult colleagues who are more familiar with those cultures and revise some cultural aspects of the cases mentioned in the book.
The book is a nice addition to the open textbook world. Hope to see more health issues covered by the book.
Reviewed by Ryan Sheryl, Assistant Professor, California State University, Dominguez Hills on 7/16/20
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality... read more
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality improvement, and informatics. While the case studies do not cover all medical conditions or bodily systems, the book is thorough in conveying details of various patients and medical team members in a hospital environment. Rather than an index or glossary at the end of the text, it contains links to outside websites for more information on medical tests and terms referenced in the cases.
The content provided is reflective of best practices in patient care, interdisciplinary collaboration, and communication at the time of publication. It is specifically accurate for the context of hospitals in Canada. The links provided throughout the text have the potential to supplement with up-to-date descriptions and definitions, however, many of them are broken (see notes in Interface section).
The content of the case studies reflects the increasingly complex landscape of healthcare, including a variety of conditions, ages, and personal situations of the clients and care providers. The text will require frequent updating due to the rapidly changing landscape of society and best practices in client care. For example, a future version may include inclusive practices with transgender clients, or address ways medical racism implicitly impacts client care (see notes in Cultural Relevance section).
The text is written clearly and presents thorough, realistic details about working and being treated in an acute hospital context.
The text is very straightforward. It is consistent in its structure and flow. It uses consistent terminology and follows a structured framework throughout.
Being a series of 8 separate case studies, this text is easily and readily divisible into smaller sections. The text was designed to be taken apart and used piece by piece in order to serve various learning contexts. The parts of each case study can also be used independently of each other to facilitate problem solving.
The topics in the case studies are presented clearly. The structure of each of the case studies proceeds in a similar fashion. All of the cases are set within the same hospital so the hospital personnel and service providers reappear across the cases, giving a textured portrayal of the experiences of the various service providers. The cases can be used individually, or one service provider can be studied across the various studies.
The text is very straightforward, without complex charts or images that could become distorted. Many of the embedded links are broken and require updating. The links that do work are a very useful way to define and expand upon medical terms used in the case studies.
Grammatical errors are minimal and do not distract from the flow of the text. In one instance the last name Singh is spelled Sing, and one patient named Fred in the text is referred to as Frank in the appendix.
The cases all show examples of health care personnel providing compassionate, client-centered care, and there is no overt discrimination portrayed. Two of the clients are in same-sex marriages and these are shown positively. It is notable, however, that the two cases presenting people of color contain more negative characteristics than the other six cases portraying Caucasian people. The people of color are the only two examples of clients who smoke regularly. In addition, the Indian client drinks and is overweight, while the First Nations client is the only one in the text to have a terminal diagnosis. The Indian client is identified as being Punjabi and attending a mosque, although there are only 2% Muslims in the Punjab province of India. Also, the last name Singh generally indicates a person who is a Hindu or Sikh, not Muslim.
Reviewed by Monica LeJeune, RN Instructor, LSUE on 4/24/20
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process. read more
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process.
Accurately presents health scenarios with real life assessment techniques and patient outcomes.
Relevant to nursing practice.
Clearly written and easily understood.
Consistent with healthcare terminology and framework
Has a good reading flow.
Topics presented in logical fashion
Easy to read.
No grammatical errors noted.
Text is not culturally insensitive or offensive.
Good book to have to teach nursing students.
Reviewed by april jarrell, associate professor, J. Sargeant Reynolds Community College on 1/7/20
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process. read more
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process.
The content is accurate and evidence based. There is no bias noted
The content in the text is relevant, up to date for nursing students. It will be easy to update content as needed because the framework allows for addition to the content.
The text is clear and easy to understand.
Framework and terminology is consistent throughout the text; the case study is a continual and takes the student on a journey with the patient. Great for learning!
The case studies can be easily divided into smaller sections to allow for discussions, and weekly studies.
The text and content progress in a logical, clear fashion allowing for progression of learning.
No interface issues noted with this text.
No grammatical errors noted in the text.
No racial or culture insensitivity were noted in the text.
I would recommend this text be used in nursing schools. The use of case studies are helpful for students to learn and practice the nursing process.
Reviewed by Lisa Underwood, Practical Nursing Instructor, NTCC on 12/3/19
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own... read more
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own set of learning objectives that can be tweaked to fit several allied health courses. Although the case studies are designed around the Canadian Healthcare System, they are quite easily adaptable to fit most any modern, developed healthcare system.
Content Accuracy rating: 3
Overall, the text is quite accurate. There is one significant error that needs to be addressed. It is located in the DVT case study. In the study, a popliteal artery clot is mislabeled as a DVT. DVTs are located in veins, not in arteries. That said, the case study on the whole is quite good. This case study could be used as a learning tool in the classroom for discussion purposes or as a way to test student understanding of DVTs, on example might be, "Can they spot the error?"
At this time, all of the case studies within the text are current. Healthcare is an ever evolving field that rests on the best evidence based practice. Keeping that in mind, educators can easily adapt the studies as the newest evidence emerges and changes practice in healthcare.
All of the case studies are well written and easy to understand. The text includes several hyperlinks and it also highlights certain medical terminology to prompt readers as a way to enhance their learning experience.
Across the text, the language, style, and format of the case studies are completely consistent.
The text is divided into eight separate case studies. Each case study may be used independently of the others. All case studies are further broken down as the focus patient passes through each aspect of their healthcare system. The text's modularity makes it possible to use a case study as individual work, group projects, class discussions, homework or in a simulation lab.
The case studies and the diagnoses that they cover are presented in such a way that educators and allied health students can easily follow and comprehend.
The book in itself is free of any image distortion and it prints nicely. The text is offered in a variety of digital formats. As noted in the above reviews, some of the hyperlinks have navigational issues. When the reader attempts to access them, a "page not found" message is received.
There were minimal grammatical errors. Some of which may be traced back to the differences in our spelling.
The text is culturally relevant in that it includes patients from many different backgrounds and ethnicities. This allows educators and students to explore cultural relevance and sensitivity needs across all areas in healthcare. I do not believe that the text was in any way insensitive or offensive to the reader.
By using the case studies, it may be possible to have an open dialogue about the differences noted in healthcare systems. Students will have the ability to compare and contrast the Canadian healthcare system with their own. I also firmly believe that by using these case studies, students can improve their critical thinking skills. These case studies help them to "put it all together".
Reviewed by Melanie McGrath, Associate Professor, TRAILS on 11/29/19
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case. read more
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case.
I saw no areas of inaccuracy
As in all healthcare texts, treatments and/or tests will change frequently. However, everything is currently up-to-date thus it should be a good reference for several years.
Each case is written so that any level of healthcare student would understand. Hyperlinks in the text is also very helpful.
All of the cases are written in a similar fashion.
Although not structured as a typical text, each case is easily assigned as a stand-alone.
Each case is organized clearly in an appropriate manner.
I did not see any issues.
I did not see any grammatical errors
The text seemed appropriately inclusive. There are no pediatric cases and no cases of intellectually-impaired patients, but those types of cases introduce more advanced problem-solving which perhaps exceed the scope of the text. May be a good addition to the text.
I found this text to be an excellent resource for healthcare students in a variety of fields. It would be best utilized in inter professional courses to help guide discussion.
Reviewed by Lynne Umbarger, Clinical Assistant Professor, Occupational Therapy, Emory and Henry College on 11/26/19
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational... read more
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational purposes. The material was easily understood by the students but challenging enough for classroom discussion. There are no mentions in the book about occupational therapy, but it is easy enough to add a couple words and make inclusion simple.
Very nice lab values are provided in the case study, making it more realistic for students.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
The material is easily understood by allied health students. The cases have links to additional learning materials for concepts that may be less familiar or should be explored further in a particular health field.
The language used in the book is consistent between cases. The framework is the same with each case which makes it easier to locate areas that would be of interest to a particular allied health profession.
The case studies are comprehensive but well-organized. They are short enough to be useful for class discussion or a full-blown assignment. The students seem to understand the material and have not expressed that any concepts or details were missing.
Each case is set up like the other cases. There are learning objectives at the beginning of each case to facilitate using the case, and it is easy enough to pull out material to develop useful activities and assignments.
There is a quick chart in the Appendix to allow the reader to determine the professions involved in each case as well as the pertinent settings and diagnoses for each case study. The contents are easy to access even while reading the book.
As a person who attends carefully to grammar, I found no errors in all of the material I read in this book.
There are a greater number of people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book. With each case, I could easily picture the person in the case. This book appears to be Canadian and more inclusive than most American books.
I was able to use this book the first time I accessed it to develop a classroom activity for first-year occupational therapy students and a more comprehensive activity for second-year students. I really appreciate the links to a multitude of terminology and medical lab values/issues for each case. I will keep using this book.
Reviewed by Cindy Krentz, Assistant Professor, Metropolitan State University of Denver on 6/15/19
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some... read more
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some understanding of the patient's background. I think it could benefit from having a glossary. I liked how the authors included the vital signs in an easily readable bar. I would have liked to see the labs also highlighted like this. I also felt that it would have been good written in a 'what would you do next?' type of case study.
The book is very accurate in language, what tests would be prudent to run and in the day in the life of the hospital in all cases. One inaccuracy is that the authors called a popliteal artery clot a DVT. The rest of the DVT case study was great, though, but the one mistake should be changed.
The book is up to date for now, but as tests become obsolete and new equipment is routinely used, the book ( like any other health textbook) will need to be updated. It would be easy to change, however. All that would have to happen is that the authors go in and change out the test to whatever newer, evidence-based test is being utilized.
The text is written clearly and easy to understand from a student's perspective. There is not too much technical jargon, and it is pretty universal when used- for example DVT for Deep Vein Thrombosis.
The book is consistent in language and how it is broken down into case studies. The same format is used for highlighting vital signs throughout the different case studies. It's great that the reader does not have to read the book in a linear fashion. Each case study can be read without needing to read the others.
The text is broken down into eight case studies, and within the case studies is broken down into days. It is consistent and shows how the patient can pass through the different hospital departments (from the ER to the unit, to surgery, to home) in a realistic manner. The instructor could use one or more of the case studies as (s)he sees fit.
The topics are eight different case studies- and are presented very clearly and organized well. Each one is broken down into how the patient goes through the system. The text is easy to follow and logical.
The interface has some problems with the highlighted blue links. Some of them did not work and I got a 'page not found' message. That can be frustrating for the reader. I'm wondering if a glossary could be utilized (instead of the links) to explain what some of these links are supposed to explain.
I found two or three typos, I don't think they were grammatical errors. In one case I think the Canadian spelling and the United States spelling of the word are just different.
This is a very culturally competent book. In today's world, however, one more type of background that would merit delving into is the trans-gender, GLBTQI person. I was glad that there were no stereotypes.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. Since we are becoming more interprofessional, I liked that we saw what the phlebotomist and other ancillary personnel (mostly different technicians) did. I think that it could become even more interdisciplinary so colleges and universities could have more interprofessional education- courses or simulations- with the addition of the nurse using social work, nutrition, or other professional health care majors.
Reviewed by Catherine J. Grott, Interim Director, Health Administration Program, TRAILS on 5/5/19
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this. read more
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this.
The book is accurate, however it has numerous broken online links.
Relevance/Longevity rating: 3
The content is very relevant, but some links are out-dated. For example, WHO Guidelines for Safe Surgery 2009 (p. 186) should be updated.
The book is written in clear and concise language. The side stories about the healthcare workers make the text interesting.
The book is consistent in terms of terminology and framework. Some terms that are emphasized in one case study are not emphasized (with online links) in the other case studies. All of the case studies should have the same words linked to online definitions.
Modularity rating: 3
The book can easily be parsed out if necessary. However, the way the case studies have been written, it's evident that different authors contributed singularly to each case study.
The organization and flow are good.
Interface rating: 1
There are numerous broken online links and "pages not found."
The grammar and punctuation are correct. There are two errors detected: p. 120 a space between the word "heart" and the comma; also a period is needed after Dr (p. 113).
I'm not quite sure that the social worker (p. 119) should comment that the patient and partner are "very normal people."
There are roughly 25 broken online links or "pages not found." The BC & Canadian Guidelines (p. 198) could also include a link to US guidelines to make the text more universal . The basilar crackles (p. 166) is very good. Text could be used compare US and Canadian healthcare. Text could be enhanced to teach "soft skills" and interdepartmental communication skills in healthcare.
Reviewed by Lindsey Henry, Practical Nursing Instructor, Fletcher on 5/1/19
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning... read more
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning objectives, which were effectively met in the readings.
As a seasoned nurse, I believe that the content regarding pathophysiology and treatments used in the case studies were accurate. I really appreciated how many of the treatments were also explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse.
The case studies are up to date and correlate with the current time period. They are easily understood.
I really loved how several important medical terms, including specific treatments were highlighted to alert the reader. Many interventions performed were also explained further, which is great to enhance learning for the nursing student or novice nurse. Also, with each scenario, a background and history of the patient is depicted, as well as the perspectives of the patient, patients family member, and the primary nurse. This really helps to give the reader a full picture of the day in the life of a nurse or a patient, and also better facilitates the learning process of the reader.
These case studies are consistent. They begin with report, the patient background or updates on subsequent days, and follow the patients all the way through discharge. Once again, I really appreciate how this book describes most if not all aspects of patient care on a day to day basis.
Each case study is separated into days. While they can be divided to be assigned at different points within the course, they also build on each other. They show trends in vital signs, what happens when a patient deteriorates, what happens when they get better and go home. Showing the entire process from ER admit to discharge is really helpful to enhance the students learning experience.
The topics are all presented very similarly and very clearly. The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough.
The book is very easy to navigate, prints well on paper, and is not distorted or confusing.
I did not see any grammatical errors.
Each case study involves a different type of patient. These differences include race, gender, sexual orientation and medical backgrounds. I do not feel the text was offensive to the reader.
I teach practical nursing students and after reading this book, I am looking forward to implementing it in my classroom. Great read for nursing students!
Reviewed by Leah Jolly, Instructor, Clinical Coordinator, Oregon Institute of Technology on 4/10/19
Good variety of cases and pathologies covered. read more
Good variety of cases and pathologies covered.
Content Accuracy rating: 2
Some examples and scenarios are not completely accurate. For example in the DVT case, the sonographer found thrombus in the "popliteal artery", which according to the book indicated presence of DVT. However in DVT, thrombus is located in the vein, not the artery. The patient would also have much different symptoms if located in the artery. Perhaps some of these inaccuracies are just typos, but in real-life situations this simple mistake can make a world of difference in the patient's course of treatment and outcomes.
Good examples of interprofessional collaboration. If only it worked this way on an every day basis!
Clear and easy to read for those with knowledge of medical terminology.
Good consistency overall.
Broken up well.
Topics are clear and logical.
Would be nice to simply click through to the next page, rather than going through the table of contents each time.
Minor typos/grammatical errors.
No offensive or insensitive materials observed.
Reviewed by Alex Sargsyan, Doctor of Nursing Practice/Assistant Professor , East Tennessee State University on 10/8/18
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study. read more
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study.
Overall the book is accurately depicting the clinical environment. There are numerous references to external sites. While most of them are correct, some of them are not working. For example Homan’s test link is not working "404 error"
Book is relevant in its current version and can be used in undergraduate and graduate classes. That said, the longevity of the book may be limited because of the character of the clinical education. Clinical guidelines change constantly and it may require a major update of the content.
Cases are written very clearly and have realistic description of an inpatient setting.
The book is easy to read and consistent in the language in all eight cases.
The cases are very well written. Each case is subdivided into logical segments. The segments reflect different setting where the patient is being seen. There is a flow and transition between the settings.
Book has eight distinct cases. This is a great format for a book that presents distinct clinical issues. This will allow the students to have immersive experiences and gain better understanding of the healthcare environment.
Book is offered in many different formats. Besides the issues with the links mentioned above, overall navigation of the book content is very smooth.
Book is very well written and has no grammatical errors.
Book is culturally relevant. Patients in the case studies come different cultures and represent diverse ethnicities.
Reviewed by Justin Berry, Physical Therapist Assistant Program Director, Northland Community and Technical College, East Grand Forks, MN on 8/2/18
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles,... read more
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles, interprofessional roles, when to initiate communication with other healthcare practitioners due to a change in patient status, and treatment ideas. Some additional patient information, such as lab values, would have been beneficial to include.
Case study information is accurate and unbiased.
Content is up to date. The case studies are written in a way so that they will not be obsolete soon, even with changes in healthcare.
The case studies are well written, and can be utilized for a variety of classroom assignments, discussions, and projects. Some additional lab value information for each patient would have been a nice addition.
The case studies are consistently organized to make it easy for the reader to determine the framework.
The text is broken up into eight different case studies for various patient diagnoses. This design makes it highly modular, and would be easy to assign at different points of a course.
The flow of the topics are presented consistently in a logical manner. Each case study follows a patient chronologically, making it easy to determine changes in patient status and treatment options.
The text is free of interface issues, with no distortion of images or charts.
The text is not culturally insensitive or offensive in any way. Patients are represented from a variety of races, ethnicities, and backgrounds
This book would be a good addition for many different health programs.
Reviewed by Ann Bell-Pfeifer, Instructor/Program Director, Minnesota State Community and Technical College on 5/21/18
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical... read more
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical laboratory technologists, medical radiology technologists, and respiratory therapists and their roles in caring for patients. Most of the overview is accurate. One suggestion is to provide an embedded radiologist interpretation of the exams which are performed which lead to the patients diagnosis.
Overall the book is accurate. Would like to see updates related to the addition of direct radiography technology which is commonly used in the hospital setting.
Many aspects of medicine will remain constant. The case studies seem fairly accurate and may be relevant for up to 3 years. Since technology changes so quickly in medicine, the CT and x-ray components may need minor updates within a few years.
The book clarity is excellent.
The case stories are consistent with each scenario. It is easy to follow the structure and learn from the content.
The book is quite modular. It is easy to break it up into cases and utilize them individually and sequentially.
The cases are listed by disease process and follow a logical flow through each condition. They are easy to follow as they have the same format from the beginning to the end of each case.
The interface seems seamless. Hyperlinks are inserted which provide descriptions and references to medical procedures and in depth definitions.
The book is free of most grammatical errors. There is a place where a few words do not fit the sentence structure and could be a typo.
The book included all types of relationships and ethnic backgrounds. One type which could be added is a transgender patient.
I think the book was quite useful for a variety of health care professionals. The authors did an excellent job of integrating patient cases which could be applied to the health care setting. The stories seemed real and relevant. This book could be used to teach health care professionals about integrated care within the emergency department.
Reviewed by Shelley Wolfe, Assistant Professor, Winona State University on 5/21/18
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should... read more
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should be noted that the authors include a statement that conveys that this text is not like traditional textbooks and is not meant to be read in a linear fashion. This allows the educator more flexibility to use the text as a supplement to enhance learning opportunities.
The content of the text appears accurate and unbiased. The “five overarching learning objectives” provide a clear aim of the text and the educator is able to glean how these objectives are captured into each of the case studies. While written for the Canadian healthcare system, this text is easily adaptable to the American healthcare system.
Overall, the content is up-to-date and the case studies provide a variety of uses that promote longevity of the text. However, not all of the blue font links (if using the digital PDF version) were still in working order. I encountered links that led to error pages or outdated “page not found” websites. While the links can be helpful, continued maintenance of these links could prove time-consuming.
I found the text easy to read and understand. I enjoyed that the viewpoints of all the different roles (patient, nurse, lab personnel, etc.) were articulated well and allowed the reader to connect and gain appreciation of the entire healthcare team. Medical jargon was noted to be appropriate for the intended audience of this text.
The terminology and organization of this text is consistent.
The text is divided into 8 case studies that follow a similar organizational structure. The case studies can further be divided to focus on individual learning objectives. For example, the case studies could be looked at as a whole for discussing communication or could be broken down into segments to focus on disease risk factors.
The case studies in this text follow a similar organizational structure and are consistent in their presentation. The flow of individual case studies is excellent and sets the reader on a clear path. As noted previously, this text is not meant to be read in a linear fashion.
This text is available in many different forms. I chose to review the text in the digital PDF version in order to use the embedded links. I did not encounter significant interface issues and did not find any images or features that would distract or confuse a reader.
No significant grammatical errors were noted.
The case studies in this text included patients and healthcare workers from a variety of backgrounds. Educators and students will benefit from expanding the case studies to include discussions and other learning opportunities to help develop culturally-sensitive healthcare providers.
I found the case studies to be very detailed, yet written in a way in which they could be used in various manners. The authors note a variety of ways in which the case studies could be employed with students; however, I feel the authors could also include that the case studies could be used as a basis for simulated clinical experiences. The case studies in this text would be an excellent tool for developing interprofessional communication and collaboration skills in a variety healthcare students.
Reviewed by Darline Foltz, Assistant Professor, University of Cincinnati - Clermont College on 3/27/18
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks... read more
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks Clinical Procedures for Safer Patient Care and Anatomy and Physiology: OpenStax" as noted by the authors.
The book appears to be accurate. Although one of the learning outcomes is as follows: "Demonstrate an understanding of the Canadian healthcare delivery system.", I did not find anything that is ONLY specific to the Canadian healthcare delivery system other than some of the terminology, i.e. "porter" instead of "transporter" and a few french words. I found this to make the book more interesting for students rather than deter from it. These are patient case studies that are relevant in any country.
The content is up-to-date. Changes in medical science may occur, i.e. a different test, to treat a diagnosis that is included in one or more of the case studies, however, it would be easy and straightforward to implement these changes.
This book is written in lucid, accessible prose. The technical/medical terminology that is used is appropriate for medical and allied health professionals. Something that would improve this text would to provide a glossary of terms for the terms in blue font.
This book is consistent with current medical terminology
This text is easily divided into each of the 6 case studies. The case studies can be used singly according to the body system being addressed or studied.
Because this text is a collection of case studies, flow doesn't pertain, however the organization and structure of the case studies are excellent as they are clear and easy to read.
There are no distractions in this text that would distract or confuse the reader.
I did not identify any grammatical errors.
This text is not culturally insensitive or offensive in any way and uses patients and healthcare workers that are of a variety of races, ethnicities and backgrounds.
I believe that this text would not only be useful to students enrolled in healthcare professions involved in direct patient care but would also be useful to students in supporting healthcare disciplines such as health information technology and management, medical billing and coding, etc.
Table of Contents
- Introduction
Case Study #1: Chronic Obstructive Pulmonary Disease (COPD)
- Learning Objectives
- Patient: Erin Johns
- Emergency Room
Case Study #2: Pneumonia
- Day 0: Emergency Room
- Day 1: Emergency Room
- Day 1: Medical Ward
- Day 2: Medical Ward
- Day 3: Medical Ward
- Day 4: Medical Ward
Case Study #3: Unstable Angina (UA)
- Patient: Harj Singh
Case Study #4: Heart Failure (HF)
- Patient: Meryl Smith
- In the Supermarket
- Day 0: Medical Ward
Case Study #5: Motor Vehicle Collision (MVC)
- Patient: Aaron Knoll
- Crash Scene
- Operating Room
- Post Anaesthesia Care Unit (PACU)
- Surgical Ward
Case Study #6: Sepsis
- Patient: George Thomas
- Sleepy Hollow Care Facility
Case Study #7: Colon Cancer
- Patient: Fred Johnson
- Two Months Ago
- Pre-Surgery Admission
Case Study #8: Deep Vein Thrombosis (DVT)
- Patient: Jamie Douglas
Appendix: Overview About the Authors
Ancillary Material
About the book.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
The case studies can be used online in a learning management system, in a classroom discussion, in a printed course pack or as part of a textbook created by the instructor. This flexibility is intentional and allows the educator to choose how best to convey the concepts presented in each case to the learner.
Because these case studies were primarily developed for an electronic healthcare system, they are based predominantly in an acute healthcare setting. Educators can augment each case study to include primary healthcare settings, outpatient clinics, assisted living environments, and other contexts as relevant.
About the Contributors
Glynda Rees teaches at the British Columbia Institute of Technology (BCIT) in Vancouver, British Columbia. She completed her MSN at the University of British Columbia with a focus on education and health informatics, and her BSN at the University of Cape Town in South Africa. Glynda has many years of national and international clinical experience in critical care units in South Africa, the UK, and the USA. Her teaching background has focused on clinical education, problem-based learning, clinical techniques, and pharmacology.
Glynda‘s interests include the integration of health informatics in undergraduate education, open accessible education, and the impact of educational technologies on nursing students’ clinical judgment and decision making at the point of care to improve patient safety and quality of care.
Faculty member in the critical care nursing program at the British Columbia Institute of Technology (BCIT) since 2003, Rob has been a critical care nurse for over 25 years with 17 years practicing in a quaternary care intensive care unit. Rob is an experienced educator and supports student learning in the classroom, online, and in clinical areas. Rob’s Master of Education from Simon Fraser University is in educational technology and learning design. He is passionate about using technology to support learning for both faculty and students.
Part of Rob’s faculty position is dedicated to providing high fidelity simulation support for BCIT’s nursing specialties program along with championing innovative teaching and best practices for educational technology. He has championed the use of digital publishing and was the tech lead for Critical Care Nursing’s iPad Project which resulted in over 40 multi-touch interactive textbooks being created using Apple and other technologies.
Rob has successfully completed a number of specialist certifications in computer and network technologies. In 2015, he was awarded Apple Distinguished Educator for his innovation and passionate use of technology to support learning. In the past five years, he has presented and published abstracts on virtual simulation, high fidelity simulation, creating engaging classroom environments, and what the future holds for healthcare and education.
Janet Morrison is the Program Head of Occupational Health Nursing at the British Columbia Institute of Technology (BCIT) in Burnaby, British Columbia. She completed a PhD at Simon Fraser University, Faculty of Communication, Art and Technology, with a focus on health information technology. Her dissertation examined the effects of telehealth implementation in an occupational health nursing service. She has an MA in Adult Education from St. Francis Xavier University and an MA in Library and Information Studies from the University of British Columbia.
Janet’s research interests concern the intended and unintended impacts of health information technologies on healthcare students, faculty, and the healthcare workforce.
She is currently working with BCIT colleagues to study how an educational clinical information system can foster healthcare students’ perceptions of interprofessional roles.
Contribute to this Page

- Previous Article
- Next Article
Case Presentation
Case study: a patient with uncontrolled type 2 diabetes and complex comorbidities whose diabetes care is managed by an advanced practice nurse.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Geralyn Spollett; Case Study: A Patient With Uncontrolled Type 2 Diabetes and Complex Comorbidities Whose Diabetes Care Is Managed by an Advanced Practice Nurse. Diabetes Spectr 1 January 2003; 16 (1): 32–36. https://doi.org/10.2337/diaspect.16.1.32
Download citation file:
- Ris (Zotero)
- Reference Manager
The specialized role of nursing in the care and education of people with diabetes has been in existence for more than 30 years. Diabetes education carried out by nurses has moved beyond the hospital bedside into a variety of health care settings. Among the disciplines involved in diabetes education, nursing has played a pivotal role in the diabetes team management concept. This was well illustrated in the Diabetes Control and Complications Trial (DCCT) by the effectiveness of nurse managers in coordinating and delivering diabetes self-management education. These nurse managers not only performed administrative tasks crucial to the outcomes of the DCCT, but also participated directly in patient care. 1
The emergence and subsequent growth of advanced practice in nursing during the past 20 years has expanded the direct care component, incorporating aspects of both nursing and medical care while maintaining the teaching and counseling roles. Both the clinical nurse specialist (CNS) and nurse practitioner (NP) models, when applied to chronic disease management, create enhanced patient-provider relationships in which self-care education and counseling is provided within the context of disease state management. Clement 2 commented in a review of diabetes self-management education issues that unless ongoing management is part of an education program, knowledge may increase but most clinical outcomes only minimally improve. Advanced practice nurses by the very nature of their scope of practice effectively combine both education and management into their delivery of care.
Operating beyond the role of educator, advanced practice nurses holistically assess patients’ needs with the understanding of patients’ primary role in the improvement and maintenance of their own health and wellness. In conducting assessments, advanced practice nurses carefully explore patients’ medical history and perform focused physical exams. At the completion of assessments, advanced practice nurses, in conjunction with patients, identify management goals and determine appropriate plans of care. A review of patients’ self-care management skills and application/adaptation to lifestyle is incorporated in initial histories, physical exams, and plans of care.
Many advanced practice nurses (NPs, CNSs, nurse midwives, and nurse anesthetists) may prescribe and adjust medication through prescriptive authority granted to them by their state nursing regulatory body. Currently, all 50 states have some form of prescriptive authority for advanced practice nurses. 3 The ability to prescribe and adjust medication is a valuable asset in caring for individuals with diabetes. It is a crucial component in the care of people with type 1 diabetes, and it becomes increasingly important in the care of patients with type 2 diabetes who have a constellation of comorbidities, all of which must be managed for successful disease outcomes.
Many studies have documented the effectiveness of advanced practice nurses in managing common primary care issues. 4 NP care has been associated with a high level of satisfaction among health services consumers. In diabetes, the role of advanced practice nurses has significantly contributed to improved outcomes in the management of type 2 diabetes, 5 in specialized diabetes foot care programs, 6 in the management of diabetes in pregnancy, 7 and in the care of pediatric type 1 diabetic patients and their parents. 8 , 9 Furthermore, NPs have also been effective providers of diabetes care among disadvantaged urban African-American patients. 10 Primary management of these patients by NPs led to improved metabolic control regardless of whether weight loss was achieved.
The following case study illustrates the clinical role of advanced practice nurses in the management of a patient with type 2 diabetes.
A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes. Although he was diagnosed in 1997, he had symptoms indicating hyperglycemia for 2 years before diagnosis. He had fasting blood glucose records indicating values of 118–127 mg/dl, which were described to him as indicative of “borderline diabetes.” He also remembered past episodes of nocturia associated with large pasta meals and Italian pastries. At the time of initial diagnosis, he was advised to lose weight (“at least 10 lb.”), but no further action was taken.
Referred by his family physician to the diabetes specialty clinic, A.B. presents with recent weight gain, suboptimal diabetes control, and foot pain. He has been trying to lose weight and increase his exercise for the past 6 months without success. He had been started on glyburide (Diabeta), 2.5 mg every morning, but had stopped taking it because of dizziness, often accompanied by sweating and a feeling of mild agitation, in the late afternoon.
A.B. also takes atorvastatin (Lipitor), 10 mg daily, for hypercholesterolemia (elevated LDL cholesterol, low HDL cholesterol, and elevated triglycerides). He has tolerated this medication and adheres to the daily schedule. During the past 6 months, he has also taken chromium picolinate, gymnema sylvestre, and a “pancreas elixir” in an attempt to improve his diabetes control. He stopped these supplements when he did not see any positive results.
He does not test his blood glucose levels at home and expresses doubt that this procedure would help him improve his diabetes control. “What would knowing the numbers do for me?,” he asks. “The doctor already knows the sugars are high.”
A.B. states that he has “never been sick a day in my life.” He recently sold his business and has become very active in a variety of volunteer organizations. He lives with his wife of 48 years and has two married children. Although both his mother and father had type 2 diabetes, A.B. has limited knowledge regarding diabetes self-care management and states that he does not understand why he has diabetes since he never eats sugar. In the past, his wife has encouraged him to treat his diabetes with herbal remedies and weight-loss supplements, and she frequently scans the Internet for the latest diabetes remedies.
During the past year, A.B. has gained 22 lb. Since retiring, he has been more physically active, playing golf once a week and gardening, but he has been unable to lose more than 2–3 lb. He has never seen a dietitian and has not been instructed in self-monitoring of blood glucose (SMBG).
A.B.’s diet history reveals excessive carbohydrate intake in the form of bread and pasta. His normal dinners consist of 2 cups of cooked pasta with homemade sauce and three to four slices of Italian bread. During the day, he often has “a slice or two” of bread with butter or olive oil. He also eats eight to ten pieces of fresh fruit per day at meals and as snacks. He prefers chicken and fish, but it is usually served with a tomato or cream sauce accompanied by pasta. His wife has offered to make him plain grilled meats, but he finds them “tasteless.” He drinks 8 oz. of red wine with dinner each evening. He stopped smoking more than 10 years ago, he reports, “when the cost of cigarettes topped a buck-fifty.”
The medical documents that A.B. brings to this appointment indicate that his hemoglobin A 1c (A1C) has never been <8%. His blood pressure has been measured at 150/70, 148/92, and 166/88 mmHg on separate occasions during the past year at the local senior center screening clinic. Although he was told that his blood pressure was “up a little,” he was not aware of the need to keep his blood pressure ≤130/80 mmHg for both cardiovascular and renal health. 11
A.B. has never had a foot exam as part of his primary care exams, nor has he been instructed in preventive foot care. However, his medical records also indicate that he has had no surgeries or hospitalizations, his immunizations are up to date, and, in general, he has been remarkably healthy for many years.
Physical Exam
A physical examination reveals the following:
Weight: 178 lb; height: 5′2″; body mass index (BMI): 32.6 kg/m 2
Fasting capillary glucose: 166 mg/dl
Blood pressure: lying, right arm 154/96 mmHg; sitting, right arm 140/90 mmHg
Pulse: 88 bpm; respirations 20 per minute
Eyes: corrective lenses, pupils equal and reactive to light and accommodation, Fundi-clear, no arteriolovenous nicking, no retinopathy
Thyroid: nonpalpable
Lungs: clear to auscultation
Heart: Rate and rhythm regular, no murmurs or gallops
Vascular assessment: no carotid bruits; femoral, popliteal, and dorsalis pedis pulses 2+ bilaterally
Neurological assessment: diminished vibratory sense to the forefoot, absent ankle reflexes, monofilament (5.07 Semmes-Weinstein) felt only above the ankle
Lab Results
Results of laboratory tests (drawn 5 days before the office visit) are as follows:
Glucose (fasting): 178 mg/dl (normal range: 65–109 mg/dl)
Creatinine: 1.0 mg/dl (normal range: 0.5–1.4 mg/dl)
Blood urea nitrogen: 18 mg/dl (normal range: 7–30 mg/dl)
Sodium: 141 mg/dl (normal range: 135–146 mg/dl)
Potassium: 4.3 mg/dl (normal range: 3.5–5.3 mg/dl)
Lipid panel
• Total cholesterol: 162 mg/dl (normal: <200 mg/dl)
• HDL cholesterol: 43 mg/dl (normal: ≥40 mg/dl)
• LDL cholesterol (calculated): 84 mg/dl (normal: <100 mg/dl)
• Triglycerides: 177 mg/dl (normal: <150 mg/dl)
• Cholesterol-to-HDL ratio: 3.8 (normal: <5.0)
AST: 14 IU/l (normal: 0–40 IU/l)
ALT: 19 IU/l (normal: 5–40 IU/l)
Alkaline phosphotase: 56 IU/l (normal: 35–125 IU/l)
A1C: 8.1% (normal: 4–6%)
Urine microalbumin: 45 mg (normal: <30 mg)
Based on A.B.’s medical history, records, physical exam, and lab results, he is assessed as follows:
Uncontrolled type 2 diabetes (A1C >7%)
Obesity (BMI 32.4 kg/m 2 )
Hyperlipidemia (controlled with atorvastatin)
Peripheral neuropathy (distal and symmetrical by exam)
Hypertension (by previous chart data and exam)
Elevated urine microalbumin level
Self-care management/lifestyle deficits
• Limited exercise
• High carbohydrate intake
• No SMBG program
Poor understanding of diabetes
A.B. presented with uncontrolled type 2 diabetes and a complex set of comorbidities, all of which needed treatment. The first task of the NP who provided his care was to select the most pressing health care issues and prioritize his medical care to address them. Although A.B. stated that his need to lose weight was his chief reason for seeking diabetes specialty care, his elevated glucose levels and his hypertension also needed to be addressed at the initial visit.
The patient and his wife agreed that a referral to a dietitian was their first priority. A.B. acknowledged that he had little dietary information to help him achieve weight loss and that his current weight was unhealthy and “embarrassing.” He recognized that his glucose control was affected by large portions of bread and pasta and agreed to start improving dietary control by reducing his portion size by one-third during the week before his dietary consultation. Weight loss would also be an important first step in reducing his blood pressure.
The NP contacted the registered dietitian (RD) by telephone and referred the patient for a medical nutrition therapy assessment with a focus on weight loss and improved diabetes control. A.B.’s appointment was scheduled for the following week. The RD requested that during the intervening week, the patient keep a food journal recording his food intake at meals and snacks. She asked that the patient also try to estimate portion sizes.
Although his physical activity had increased since his retirement, it was fairly sporadic and weather-dependent. After further discussion, he realized that a week or more would often pass without any significant form of exercise and that most of his exercise was seasonal. Whatever weight he had lost during the summer was regained in the winter, when he was again quite sedentary.
A.B.’s wife suggested that the two of them could walk each morning after breakfast. She also felt that a treadmill at home would be the best solution for getting sufficient exercise in inclement weather. After a short discussion about the positive effect exercise can have on glucose control, the patient and his wife agreed to walk 15–20 minutes each day between 9:00 and 10:00 a.m.
A first-line medication for this patient had to be targeted to improving glucose control without contributing to weight gain. Thiazolidinediones (i.e., rosiglitizone [Avandia] or pioglitizone [Actos]) effectively address insulin resistance but have been associated with weight gain. 12 A sulfonylurea or meglitinide (i.e., repaglinide [Prandin]) can reduce postprandial elevations caused by increased carbohydrate intake, but they are also associated with some weight gain. 12 When glyburide was previously prescribed, the patient exhibited signs and symptoms of hypoglycemia (unconfirmed by SMBG). α-Glucosidase inhibitors (i.e., acarbose [Precose]) can help with postprandial hyperglycemia rise by blunting the effect of the entry of carbohydrate-related glucose into the system. However, acarbose requires slow titration, has multiple gastrointestinal (GI) side effects, and reduces A1C by only 0.5–0.9%. 13 Acarbose may be considered as a second-line therapy for A.B. but would not fully address his elevated A1C results. Metformin (Glucophage), which reduces hepatic glucose production and improves insulin resistance, is not associated with hypoglycemia and can lower A1C results by 1%. Although GI side effects can occur, they are usually self-limiting and can be further reduced by slow titration to dose efficacy. 14
After reviewing these options and discussing the need for improved glycemic control, the NP prescribed metformin, 500 mg twice a day. Possible GI side effects and the need to avoid alcohol were of concern to A.B., but he agreed that medication was necessary and that metformin was his best option. The NP advised him to take the medication with food to reduce GI side effects.
The NP also discussed with the patient a titration schedule that increased the dosage to 1,000 mg twice a day over a 4-week period. She wrote out this plan, including a date and time for telephone contact and medication evaluation, and gave it to the patient.
During the visit, A.B. and his wife learned to use a glucose meter that features a simple two-step procedure. The patient agreed to use the meter twice a day, at breakfast and dinner, while the metformin dose was being titrated. He understood the need for glucose readings to guide the choice of medication and to evaluate the effects of his dietary changes, but he felt that it would not be “a forever thing.”
The NP reviewed glycemic goals with the patient and his wife and assisted them in deciding on initial short-term goals for weight loss, exercise, and medication. Glucose monitoring would serve as a guide and assist the patient in modifying his lifestyle.
A.B. drew the line at starting an antihypertensive medication—the angiotensin-converting enzyme (ACE) inhibitor enalapril (Vasotec), 5 mg daily. He stated that one new medication at a time was enough and that “too many medications would make a sick man out of me.” His perception of the state of his health as being represented by the number of medications prescribed for him gave the advanced practice nurse an important insight into the patient’s health belief system. The patient’s wife also believed that a “natural solution” was better than medication for treating blood pressure.
Although the use of an ACE inhibitor was indicated both by the level of hypertension and by the presence of microalbuminuria, the decision to wait until the next office visit to further evaluate the need for antihypertensive medication afforded the patient and his wife time to consider the importance of adding this pharmacotherapy. They were quite willing to read any materials that addressed the prevention of diabetes complications. However, both the patient and his wife voiced a strong desire to focus their energies on changes in food and physical activity. The NP expressed support for their decision. Because A.B. was obese, weight loss would be beneficial for many of his health issues.
Because he has a sedentary lifestyle, is >35 years old, has hypertension and peripheral neuropathy, and is being treated for hypercholestrolemia, the NP performed an electrocardiogram in the office and referred the patient for an exercise tolerance test. 11 In doing this, the NP acknowledged and respected the mutually set goals, but also provided appropriate pre-exercise screening for the patient’s protection and safety.
In her role as diabetes educator, the NP taught A.B. and his wife the importance of foot care, demonstrating to the patient his inability to feel the light touch of the monofilament. She explained that the loss of protective sensation from peripheral neuropathy means that he will need to be more vigilant in checking his feet for any skin lesions caused by poorly fitting footwear worn during exercise.
At the conclusion of the visit, the NP assured A.B. that she would share the plan of care they had developed with his primary care physician, collaborating with him and discussing the findings of any diagnostic tests and procedures. She would also work in partnership with the RD to reinforce medical nutrition therapies and improve his glucose control. In this way, the NP would facilitate the continuity of care and keep vital pathways of communication open.
Advanced practice nurses are ideally suited to play an integral role in the education and medical management of people with diabetes. 15 The combination of clinical skills and expertise in teaching and counseling enhances the delivery of care in a manner that is both cost-reducing and effective. Inherent in the role of advanced practice nurses is the understanding of shared responsibility for health care outcomes. This partnering of nurse with patient not only improves care but strengthens the patient’s role as self-manager.
Geralyn Spollett, MSN, C-ANP, CDE, is associate director and an adult nurse practitioner at the Yale Diabetes Center, Department of Endocrinology and Metabolism, at Yale University in New Haven, Conn. She is an associate editor of Diabetes Spectrum.
Note of disclosure: Ms. Spollett has received honoraria for speaking engagements from Novo Nordisk Pharmaceuticals, Inc., and Aventis and has been a paid consultant for Aventis. Both companies produce products and devices for the treatment of diabetes.
Email alerts
- Advanced Practice Care: Advanced Practice Care in Diabetes: Epilogue
- Advanced Practice Care: Advanced Practice Care in Diabetes: Preface
- Online ISSN 1944-7353
- Print ISSN 1040-9165
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
- PRO Courses Guides New Tech Help Pro Expert Videos About wikiHow Pro Upgrade Sign In
- EDIT Edit this Article
- EXPLORE Tech Help Pro About Us Random Article Quizzes Request a New Article Community Dashboard This Or That Game Popular Categories Arts and Entertainment Artwork Books Movies Computers and Electronics Computers Phone Skills Technology Hacks Health Men's Health Mental Health Women's Health Relationships Dating Love Relationship Issues Hobbies and Crafts Crafts Drawing Games Education & Communication Communication Skills Personal Development Studying Personal Care and Style Fashion Hair Care Personal Hygiene Youth Personal Care School Stuff Dating All Categories Arts and Entertainment Finance and Business Home and Garden Relationship Quizzes Cars & Other Vehicles Food and Entertaining Personal Care and Style Sports and Fitness Computers and Electronics Health Pets and Animals Travel Education & Communication Hobbies and Crafts Philosophy and Religion Work World Family Life Holidays and Traditions Relationships Youth
- Browse Articles
- Learn Something New
- Quizzes Hot
- This Or That Game
- Train Your Brain
- Explore More
- Support wikiHow
- About wikiHow
- Log in / Sign up
- Education and Communications
- Medical Studies
How to Write a Medical Case Study Report
Last Updated: April 18, 2024 Fact Checked
This article was medically reviewed by Mark Ziats, MD, PhD and by wikiHow staff writer, Jennifer Mueller, JD . Dr. Mark Ziats is an Internal Medicine Physician, Scientist, Entrepreneur, and the Medical Director of xBiotech. With over five years of experience, he specializes in biotechnology, genomics, and medical devices. He earned a Doctor of Medicine degree from Baylor College of Medicine, a Ph.D. in Genetics from the University of Cambridge, and a BS in Biochemistry and Chemistry from Clemson University. He also completed the INNoVATE Program in Biotechnology Entrepreneurship at The Johns Hopkins University - Carey Business School. Dr. Ziats is board certified by the American Board of Internal Medicine. There are 15 references cited in this article, which can be found at the bottom of the page. This article has been fact-checked, ensuring the accuracy of any cited facts and confirming the authority of its sources. This article has been viewed 187,446 times.
You've encountered an interesting and unusual case on your rounds, and a colleague or supervising physician says, "Why don't you write up a case study report?" If you've never written one before, that might sound intimidating, but it's a great way to get started in medical writing. Case studies always follow a standard structure and format, so the writing is very formulaic once you get the hang of it. Read on for a step-by-step guide to writing your first case study report.
What is a case study report?

- Medical students or residents typically do the bulk of the writing of the report. If you're just starting your medical career, a case study report is a great way to get a publication under your belt. [2] X Research source

- If the patient is a minor or is incapable of giving informed consent, get consent from their parents or closest relative. [4] X Trustworthy Source PubMed Central Journal archive from the U.S. National Institutes of Health Go to source
- Your hospital likely has specific consent forms to use. Ask your supervising physician if you're not sure where to get one.
- Some journals also have their own consent form. Check your target journal's author or submission information to make sure. [5] X Research source
How is a case study report structured?

- Even though the introduction is the first part of a case study report, doctors typically write it last. You'll have a better idea of how to introduce your case study to readers after you've written it.
- Your abstract comes at the top, before the introduction, and provides a brief summary of the entire report. Unless your case study is published in an open-access journal, the abstract is the only part of the article many readers will see.

- Many journals offer templates and checklists you can use to make sure your case study includes everything necessary and is formatted properly—take advantage of these! Some journals, such as BMJ Case Reports , require all case studies submitted to use their templates.
Drafting Your Medical Case Study Report

- Patient description
- Chronological case history
- Physical exam results
- Results of any pathological tests, imaging, or other investigations
- Treatment plan
- Expected outcome of treatment
- Actual outcome of treatment

- Why the patient sought medical help (you can even use their own words)
- Important information that helped you settle on your diagnosis
- The results of your clinical examination, including diagnostic tests and their results, along with any helpful images
- A description of the treatment plan
- The outcome, including how and why treatment ended and how long the patient was under your care [11] X Trustworthy Source PubMed Central Journal archive from the U.S. National Institutes of Health Go to source

- You will need references to back up symptoms of the condition, common treatment, and the expected outcome of that common treatment.
- Use your research to paint a picture of the usual case of a patient with a similar condition—it'll help you show how unusual and different your patient's case is.
- Generally, aim for around 20 references—no fewer than 15, but no more than 25. [13] X Trustworthy Source PubMed Central Journal archive from the U.S. National Institutes of Health Go to source

- Close your discussion section with a summary of the lessons learned from the case and why it's significant to consider when treating similar cases in the future.
- Outline any open questions that remain. You might also provide suggestions for future research.

- In your conclusion, you might also give suggestions or recommendations to readers based on what you learned as a result of the case.
- Some journals don't want a separate conclusion section. If that's the case for one of your target journals, just move this paragraph to the end of your discussion section.
Polishing Your Report for Submission to Publishers

- Most titles are fewer than 10 words long and include the name of the disease or condition treated.
- You might also include the treatment used and whether the outcome was successful. When deciding what to include, think about the reason you wrote the case study in the first place and why you think it's important for other clinicians to read.

- Made a significant intellectual contribution to the case study report
- Was involved in the medical care of the patient reported
- Can explain and defend the data presented in the report
- Has approved the final manuscript before submission for publication

- Keep in mind that the abstract is not just going to be the first thing people read—it will often be the only thing people read. Make sure that if someone is going to walk away having only read the abstract, they'll still get the same message they would have if they read the whole thing.
- There are 2 basic types of abstract: narrative and structured. A narrative abstract is a single paragraph written in narrative prose. A structured abstract includes headings that correspond with the sections of the paper, then a brief summary of each section. Use the format preferred by your target journal.

- Look for keywords that are relevant to your field or sub-field and directly related to the content of your article, such as the name of the condition or specific treatments you used.
- Most journals allow 4-8 keywords but check the submission guidelines of your target journal to make sure.

- Blur out the patient's face as well as any tattoos, birthmarks, or unrelated scars that are visible in diagnostic images.

- It's common to thank the patient, but that's up to you. Even if you don't, include a statement indicating that you have the patient's written, informed consent to publish the information.
- Read the journal's submission guidelines for a definition of what that journal considers a conflict of interest. They're generally the same, but some might be stricter than others. [22] X Research source

- If you're not familiar with the citation style used by your target journal, check online for a guide. There might also be one available at your hospital or medical school library.
- Medical librarians can also help with citation style and references if you run into something tricky—don't just wing it! Correct citation style insures that readers can access the materials you cite.

- It's also a good idea to get a beta reader who isn't a medical professional. Their comments can help you figure out where you need to clarify your points.
- Read a lot of case studies published in your target journals—it will help you internalize the tone and style that journal is looking for.
Submitting Your Report to Publishers

- Look into the background and reputation of journals before you decide to submit to them. Only seek publication from reputable journals in which articles go through a peer-review process.
- Find out what publishing fees the journals charge. Keep in mind that open-access journals tend to charge higher publishing fees. [26] X Research source
- Read each journal's submission and editorial guidelines carefully. They'll tell you exactly how to format your case study, how long each section should be, and what citation style to use. [27] X Research source
- For electronic journals that only publish case reports, try BMJ Case Reports , Journal of Medical Case Reports , or Radiology Case Reports .

- If your manuscript isn't suitable for the journal you submitted to, the journal might offer to forward it to an associated journal where it would be a better fit.
- When your manuscript is provisionally accepted, the journal will send it to other doctors for evaluation under the peer-review process.
- Most medical journals don't accept simultaneous submissions, meaning you'll have to submit to your first choice, wait for their decision, then move to the next journal on the list if they don't bite.

- Along with your revised manuscript, include a letter with your response to each of the reviewer's comments. Where you made revisions, add page numbers to indicate where the revisions are that address that reviewer's comments.
- Sometimes, doctors involved in the peer review process will indicate that the journal should reject the manuscript. If that's the case, you'll get a letter explaining why your case study report won't be published and you're free to submit it elsewhere.

- Some journals require you to have your article professionally copy-edited at your own cost while others do this in-house. The editors will let you know what you're responsible for.

- With your acceptance letter, you'll get instructions on how to make payment and how much you owe. Take note of the deadline and make sure you pay it as soon as possible to avoid publication delays.
- Some journals will publish for free, with an "open-access option" that allows you to pay a fee only if you want open access to your article. [32] X Research source

- Through the publishing agreement, you assign your copyright in the article to the journal. This allows the journal to legally publish your work. That assignment can be exclusive or non-exclusive and may only last for a specific term. Read these details carefully!
- If you published an open-access article, you don't assign the copyright to the publisher. The publishing agreement merely gives the journal the right to publish the "Version of Record." [33] X Research source
How do I find a suitable case for a report?

- A rare disease, or unusual presentation of any disease
- An unusual combination of diseases or conditions
- A difficult or inconclusive diagnosis
- Unexpected developments or responses to treatment
- Personal impact
- Observations that shed new light on the patient's disease or condition

- There might be other members of your medical team that want to help with writing. If so, use one of these brainstorming sessions to divvy up writing responsibilities in a way that makes the most sense given your relative skills and experience.
- Senior doctors might also be able to name some journals that would potentially publish your case study. [36] X Research source
Expert Q&A
You Might Also Like

- ↑ https://www.elsevier.com/connect/authors-update/the-dos-and-donts-of-writing-and-publishing-case-reports
- ↑ https://www.bmj.com/content/350/bmj.h2693
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5686928/
- ↑ https://health.usf.edu/medicine/internalmedicine/im-impact/~/media/B3A3421F4C144FA090AE965C21791A3C.ashx
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2597880/
- ↑ https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6476221/
- ↑ https://www.springer.com/gp/authors-editors/authorandreviewertutorials/writing-a-journal-manuscript/title-abstract-and-keywords/10285522
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2597880/
- ↑ https://thelancet.com/pb/assets/raw/Lancet/authors/tl-info-for-authors.pdf
- ↑ https://jmedicalcasereports.biomedcentral.com/articles/10.1186/s13256-017-1351-y
- ↑ https://guides.himmelfarb.gwu.edu/casereports
- ↑ https://casereports.bmj.com/pages/authors/
- ↑ https://jmedicalcasereports.biomedcentral.com/articles/10.1186/1752-1947-7-239
- ↑ https://research.chm.msu.edu/students-residents/writing-a-case-report
- ↑ https://authorservices.taylorandfrancis.com/publishing-your-research/moving-through-production/copyright-for-journal-authors/#
About This Article

Medical Disclaimer
The content of this article is not intended to be a substitute for professional medical advice, examination, diagnosis, or treatment. You should always contact your doctor or other qualified healthcare professional before starting, changing, or stopping any kind of health treatment.
Read More...
To start a medical case study report, first choose a title that clearly reflects the contents of the report. You’ll also need to list any participating authors and develop a list of keywords, as well as an abstract summarizing the report. Your report will need to include an introduction summarizing the context of the report, as well as a detailed presentation of the case. Don’t forget to include a thorough citation list and acknowledgements of anyone else who participated in the study. For more tips from our Medical co-author, including how to get your case study report published, keep reading! Did this summary help you? Yes No
- Send fan mail to authors
Reader Success Stories
Sep 5, 2020
Did this article help you?
Asfia Banu Pasha
Apr 10, 2017
Jun 20, 2021
Mar 1, 2017

Featured Articles

Trending Articles

Watch Articles

- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
Get all the best how-tos!
Sign up for wikiHow's weekly email newsletter

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

Evaluating the Efficacy of Lumateperone for MDD and Bipolar Depression With Mixed Features

Blue Light, Depression, and Bipolar Disorder

Efficacy of Modafinil for Treatment of Neurocognitive Impairment in Bipolar Disorder

Four Myths About Lamotrigine

Securing the Future of Lithium Research

An Update on Early Intervention in Psychotic Disorders
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 16 October 2014
A woman with asthma: a whole systems approach to supporting self-management
- Hilary Pinnock 1 ,
- Elisabeth Ehrlich 1 ,
- Gaylor Hoskins 2 &
- Ron Tomlins 3
npj Primary Care Respiratory Medicine volume 24 , Article number: 14063 ( 2014 ) Cite this article
16k Accesses
2 Citations
6 Altmetric
Metrics details
- Health care
A 35-year-old lady attends for review of her asthma following an acute exacerbation. There is an extensive evidence base for supported self-management for people living with asthma, and international and national guidelines emphasise the importance of providing a written asthma action plan. Effective implementation of this recommendation for the lady in this case study is considered from the perspective of a patient, healthcare professional, and the organisation. The patient emphasises the importance of developing a partnership based on honesty and trust, the need for adherence to monitoring and regular treatment, and involvement of family support. The professional considers the provision of asthma self-management in the context of a structured review, with a focus on a self-management discussion which elicits the patient’s goals and preferences. The organisation has a crucial role in promoting, enabling and providing resources to support professionals to provide self-management. The patient’s asthma control was assessed and management optimised in two structured reviews. Her goal was to avoid disruption to her work and her personalised action plan focused on achieving that goal.
Similar content being viewed by others

Barriers to implementing asthma self-management in Malaysian primary care: qualitative study exploring the perspectives of healthcare professionals

The self-management abilities test (SMAT): a tool to identify the self-management abilities of adults with bronchiectasis

Improving primary care management of asthma: do we know what really works?
A 35-year-old sales representative attends the practice for an asthma review. Her medical record notes that she has had asthma since childhood, and although for many months of the year her asthma is well controlled (when she often reduces or stops her inhaled steroids), she experiences one or two exacerbations a year requiring oral steroids. These are usually triggered by a viral upper respiratory infection, though last summer when the pollen count was particularly high she became tight chested and wheezy for a couple of weeks.
Her regular prescription is for fluticasone 100 mcg twice a day, and salbutamol as required. She has a young family and a busy lifestyle so does not often manage to find time to attend the asthma clinic. A few weeks previously, an asthma attack had interfered with some important work-related travel, and she has attended the clinic on this occasion to ask about how this can be managed better in the future. There is no record of her having been given an asthma action plan.
What do we know about asthma self-management? The academic perspective
Supported self-management reduces asthma morbidity.
The lady in this case study is struggling to maintain control of her asthma within the context of her busy professional and domestic life. The recent unfortunate experience which triggered this consultation offers a rare opportunity to engage with her and discuss how she can manage her asthma better. It behoves the clinician whom she is seeing (regardless of whether this is in a dedicated asthma clinic or an appointment in a routine general practice surgery) to grasp the opportunity and discuss self-management and provide her with a (written) personalised asthma action plan (PAAP).
The healthcare professional advising the lady is likely to be aware that international and national guidelines emphasise the importance of supporting self-management. 1 – 4 There is an extensive evidence base for asthma self-management: a recent synthesis identified 22 systematic reviews summarising data from 260 randomised controlled trials encompassing a broad range of demographic, clinical and healthcare contexts, which concluded that asthma self-management reduces emergency use of healthcare resources, including emergency department visits, hospital admissions and unscheduled consultations and improves markers of asthma control, including reduced symptoms and days off work, and improves quality of life. 1 , 2 , 5 – 12 Health economic analysis suggests that it is not only clinically effective, but also a cost-effective intervention. 13
Personalised asthma action plans
Key features of effective self-management approaches are:
Self-management education should be reinforced by provision of a (written) PAAP which reminds patients of their regular treatment, how to monitor and recognise that control is deteriorating and the action they should take. 14 – 16 As an adult, our patient can choose whether she wishes to monitor her control with symptoms or by recording peak flows (or a combination of both). 6 , 8 , 9 , 14 Symptom-based monitoring is generally better in children. 15 , 16
Plans should have between two and three action points including emergency doses of reliever medication; increasing low dose (or recommencing) inhaled steroids; or starting a course of oral steroids according to severity of the exacerbation. 14
Personalisation of the action plan is crucial. Focussing specifically on what actions she could take to prevent a repetition of the recent attack is likely to engage her interest. Not all patients will wish to start oral steroids without advice from a healthcare professional, though with her busy lifestyle and travel our patient is likely to be keen to have an emergency supply of prednisolone. Mobile technology has the potential to support self-management, 17 , 18 though a recent systematic review concluded that none of the currently available smart phone ‘apps’ were fit for purpose. 19
Identification and avoidance of her triggers is important. As pollen seems to be a trigger, management of allergic rhinitis needs to be discussed (and included in her action plan): she may benefit from regular use of a nasal steroid spray during the season. 20
Self-management as recommended by guidelines, 1 , 2 focuses narrowly on adherence to medication/monitoring and the early recognition/remediation of exacerbations, summarised in (written) PAAPs. Patients, however, may want to discuss how to reduce the impact of asthma on their life more generally, 21 including non-pharmacological approaches.
Supported self-management
The impact is greater if self-management education is delivered within a comprehensive programme of accessible, proactive asthma care, 22 and needs to be supported by ongoing regular review. 6 With her busy lifestyle, our patient may be reluctant to attend follow-up appointments, and once her asthma is controlled it may be possible to make convenient arrangements for professional review perhaps by telephone, 23 , 24 or e-mail. Flexible access to professional advice (e.g., utilising diverse modes of consultation) is an important component of supporting self-management. 25
The challenge of implementation
Implementation of self-management, however, remains poor in routine clinical practice. A recent Asthma UK web-survey estimated that only 24% of people with asthma in the UK currently have a PAAP, 26 with similar figures from Sweden 27 and Australia. 28 The general practitioner may feel that they do not have time to discuss self-management in a routine surgery appointment, or may not have a supply of paper-based PAAPs readily available. 29 However, as our patient rarely finds time to attend the practice, inviting her to make an appointment for a future clinic is likely to be unsuccessful and the opportunity to provide the help she needs will be missed.
The solution will need a whole systems approach
A systematic meta-review of implementing supported self-management in long-term conditions (including asthma) concluded that effective implementation was multifaceted and multidisciplinary; engaging patients, training and motivating professionals within the context of an organisation which actively supported self-management. 5 This whole systems approach considers that although patient education, professional training and organisational support are all essential components of successful support, they are rarely effective in isolation. 30 A systematic review of interventions that promote provision/use of PAAPs highlighted the importance of organisational systems (e.g., sending blank PAAPs with recall reminders). 31 A patient offers her perspective ( Box 1 ), a healthcare professional considers the clinical challenge, and the challenges are discussed from an organisational perspective.
Box 1: What self-management help should this lady expect from her general practitioner or asthma nurse? The patient’s perspective
The first priority is that the patient is reassured that her condition can be managed successfully both in the short and the long term. A good working relationship with the health professional is essential to achieve this outcome. Developing trust between patient and healthcare professional is more likely to lead to the patient following the PAAP on a long-term basis.
A review of all medication and possible alternative treatments should be discussed. The patient needs to understand why any changes are being made and when she can expect to see improvements in her condition. Be honest, as sometimes it will be necessary to adjust dosages before benefits are experienced. Be positive. ‘There are a number of things we can do to try to reduce the impact of asthma on your daily life’. ‘Preventer treatment can protect against the effect of pollen in the hay fever season’. If possible, the same healthcare professional should see the patient at all follow-up appointments as this builds trust and a feeling of working together to achieve the aim of better self-management.
Is the healthcare professional sure that the patient knows how to take her medication and that it is taken at the same time each day? The patient needs to understand the benefit of such a routine. Medication taken regularly at the same time each day is part of any self-management regime. If the patient is unused to taking medication at the same time each day then keeping a record on paper or with an electronic device could help. Possibly the patient could be encouraged to set up a system of reminders by text or smartphone.
Some people find having a peak flow meter useful. Knowing one's usual reading means that any fall can act as an early warning to put the PAAP into action. Patients need to be proactive here and take responsibility.
Ongoing support is essential for this patient to ensure that she takes her medication appropriately. Someone needs to be available to answer questions and provide encouragement. This could be a doctor or a nurse or a pharmacist. Again, this is an example of the partnership needed to achieve good asthma control.
It would also be useful at a future appointment to discuss the patient’s lifestyle and work with her to reduce her stress. Feeling better would allow her to take simple steps such as taking exercise. It would also be helpful if all members of her family understood how to help her. Even young children can do this.
From personal experience some people know how beneficial it is to feel they are in a partnership with their local practice and pharmacy. Being proactive produces dividends in asthma control.
What are the clinical challenges for the healthcare professional in providing self-management support?
Due to the variable nature of asthma, a long-standing history may mean that the frequency and severity of symptoms, as well as what triggers them, may have changed over time. 32 Exacerbations requiring oral steroids, interrupting periods of ‘stability’, indicate the need for re-assessment of the patient’s clinical as well as educational needs. The patient’s perception of stability may be at odds with the clinical definition 1 , 33 —a check on the number of short-acting bronchodilator inhalers the patient has used over a specific period of time is a good indication of control. 34 Assessment of asthma control should be carried out using objective tools such as the Asthma Control Test or the Royal College of Physicians three questions. 35 , 36 However, it is important to remember that these assessment tools are not an end in themselves but should be a springboard for further discussion on the nature and pattern of symptoms. Balancing work with family can often make it difficult to find the time to attend a review of asthma particularly when the patient feels well. The practice should consider utilising other means of communication to maintain contact with patients, encouraging them to come in when a problem is highlighted. 37 , 38 Asthma guidelines advocate a structured approach to ensure the patient is reviewed regularly and recommend a detailed assessment to enable development of an appropriate patient-centred (self)management strategy. 1 – 4
Although self-management plans have been shown to be successful for reducing the impact of asthma, 21 , 39 the complexity of managing such a fluctuating disease on a day-to-day basis is challenging. During an asthma review, there is an opportunity to work with the patient to try to identify what triggers their symptoms and any actions that may help improve or maintain control. 38 An integral part of personalised self-management education is the written PAAP, which gives the patient the knowledge to respond to the changes in symptoms and ensures they maintain control of their asthma within predetermined parameters. 9 , 40 The PAAP should include details on how to monitor asthma, recognise symptoms, how to alter medication and what to do if the symptoms do not improve. The plan should include details on the treatment to be taken when asthma is well controlled, and how to adjust it when the symptoms are mild, moderate or severe. These action plans need to be developed between the doctor, nurse or asthma educator and the patient during the review and should be frequently reviewed and updated in partnership (see Box 1). Patient preference as well as clinical features such as whether she under- or over-perceives her symptoms should be taken into account when deciding whether the action plan is peak flow or symptom-driven. Our patient has a lot to gain from having an action plan. She has poorly controlled asthma and her lifestyle means that she will probably see different doctors (depending who is available) when she needs help. Being empowered to self-manage could make a big difference to her asthma control and the impact it has on her life.
The practice should have protocols in place, underpinned by specific training to support asthma self-management. As well as ensuring that healthcare professionals have appropriate skills, this should include training for reception staff so that they know what action to take if a patient telephones to say they are having an asthma attack.
However, focusing solely on symptom management strategies (actions) to follow in the presence of deteriorating symptoms fails to incorporate the patients’ wider views of asthma, its management within the context of her/his life, and their personal asthma management strategies. 41 This may result in a failure to use plans to maximise their health potential. 21 , 42 A self-management strategy leading to improved outcomes requires a high level of patient self-efficacy, 43 a meaningful partnership between the patient and the supporting health professional, 42 , 44 and a focused self-management discussion. 14
Central to both the effectiveness and personalisation of action plans, 43 , 45 in particular the likelihood that the plan will lead to changes in patients’ day-to-day self-management behaviours, 45 is the identification of goals. Goals are more likely to be achieved when they are specific, important to patients, collaboratively set and there is a belief that these can be achieved. Success depends on motivation 44 , 46 to engage in a specific behaviour to achieve a valued outcome (goal) and the ability to translate the behavioural intention into action. 47 Action and coping planning increases the likelihood that patient behaviour will actually change. 44 , 46 , 47 Our patient has a goal: she wants to avoid having her work disrupted by her asthma. Her personalised action plan needs to explicitly focus on achieving that goal.
As providers of self-management support, health professionals must work with patients to identify goals (valued outcomes) that are important to patients, that may be achievable and with which they can engage. The identification of specific, personalised goals and associated feasible behaviours is a prerequisite for the creation of asthma self-management plans. Divergent perceptions of asthma and how to manage it, and a mismatch between what patients want/need from these plans and what is provided by professionals are barriers to success. 41 , 42
What are the challenges for the healthcare organisation in providing self-management support?
A number of studies have demonstrated the challenges for primary care physicians in providing ongoing support for people with asthma. 31 , 48 , 49 In some countries, nurses and other allied health professionals have been trained as asthma educators and monitor people with stable asthma. These resources are not always available. In addition, some primary care services are delivered in constrained systems where only a few minutes are available to the practitioner in a consultation, or where only a limited range of asthma medicines are available or affordable. 50
There is recognition that the delivery of quality care depends on the competence of the doctor (and supporting health professionals), the relationship between the care providers and care recipients, and the quality of the environment in which care is delivered. 51 This includes societal expectations, health literacy and financial drivers.
In 2001, the Australian Government adopted a programme developed by the General Practitioner Asthma Group of the National Asthma Council Australia that provided a structured approach to the implementation of asthma management guidelines in a primary care setting. 52 Patients with moderate-to-severe asthma were eligible to participate. The 3+ visit plan required confirmation of asthma diagnosis, spirometry if appropriate, assessment of trigger factors, consideration of medication and patient self-management education including provision of a written PAAP. These elements, including regular medical review, were delivered over three visits. Evaluation demonstrated that the programme was beneficial but that it was difficult to complete the third visit in the programme. 53 – 55 Accordingly, the programme, renamed the Asthma Cycle of Care, was modified to incorporate two visits. 56 Financial incentives are provided to practices for each patient who receives this service each year.
Concurrently, other programmes were implemented which support practice-based care. Since 2002, the National Asthma Council has provided best-practice asthma and respiratory management education to health professionals, 57 and this programme will be continuing to 2017. The general practitioner and allied health professional trainers travel the country to provide asthma and COPD updates to groups of doctors, nurses and community pharmacists. A number of online modules are also provided. The PACE (Physician Asthma Care Education) programme developed by Noreen Clark has also been adapted to the Australian healthcare system. 58 In addition, a pharmacy-based intervention has been trialled and implemented. 59
To support these programmes, the National Asthma Council ( www.nationalasthma.org.au ) has developed resources for use in practices. A strong emphasis has been on the availability of a range of PAAPs (including plans for using adjustable maintenance dosing with ICS/LABA combination inhalers), plans for indigenous Australians, paediatric plans and plans translated into nine languages. PAAPs embedded in practice computer systems are readily available in consultations, and there are easily accessible online paediatric PAAPs ( http://digitalmedia.sahealth.sa.gov.au/public/asthma/ ). A software package, developed in the UK, can be downloaded and used to generate a pictorial PAAP within the consultation. 60
One of the strongest drivers towards the provision of written asthma action plans in Australia has been the Asthma Friendly Schools programme. 61 , 62 Established with Australian Government funding and the co-operation of Education Departments of each state, the Asthma Friendly Schools programme engages schools to address and satisfy a set of criteria that establishes an asthma-friendly environment. As part of accreditation, the school requires that each child with asthma should have a written PAAP prepared by their doctor to assist (trained) staff in managing a child with asthma at school.
The case study continues...
The initial presentation some weeks ago was during an exacerbation of asthma, which may not be the best time to educate a patient. It is, however, a splendid time to build on their motivation to feel better. She agreed to return after her asthma had settled to look more closely at her asthma control, and an appointment was made for a routine review.
At this follow-up consultation, the patient’s diagnosis was reviewed and confirmed and her trigger factors discussed. For this lady, respiratory tract infections are the usual trigger but allergic factors during times of high pollen count may also be relevant. Assessment of her nasal airway suggested that she would benefit from better control of allergic rhinitis. Other factors were discussed, as many patients are unaware that changes in air temperature, exercise and pets can also trigger asthma exacerbations. In addition, use of the Asthma Control Test was useful as an objective assessment of control as well as helping her realise what her life could be like! Many people with long-term asthma live their life within the constraints of their illness, accepting that is all that they can do.
After assessing the level of asthma control, a discussion about management options—trigger avoidance, exercise and medicines—led to the development of a written PAAP. Asthma can affect the whole family, and ways were explored that could help her family understand why it is important that she finds time in the busy domestic schedules to take her regular medication. Family and friends can also help by understanding what triggers her asthma so that they can avoid exposing her to perfumes, pollens or pets that risk triggering her symptoms. Information from the national patient organisation was provided to reinforce the messages.
The patient agreed to return in a couple of weeks, and a recall reminder was set up. At the second consultation, the level of control since the last visit will be explored including repeat spirometry, if appropriate. Further education about the pathophysiology of asthma and how to recognise early warning signs of loss of control can be given. Device use will be reassessed and the PAAP reviewed. Our patient’s goal is to avoid disruption to her work and her PAAP will focus on achieving that goal. Finally, agreement will be reached with the patient about future routine reviews, which, now that she has a written PAAP, could be scheduled by telephone if all is well, or face-to-face if a change in her clinical condition necessitates a more comprehensive review.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2012. Available from: http://www.ginasthma.org (accessed July 2013).
British Thoracic Society/Scottish Intercollegiate Guideline Network British Guideline on the Management of Asthma. Thorax 2008; 63 (Suppl 4 iv1–121, updated version available from: http://www.sign.ac.uk (accessed January 2014).
Article Google Scholar
National Asthma Council Australia. Australian Asthma Handbook. Available from: http://www.nationalasthma.org.au/handbook (accessed May 2014).
National Asthma Education and Prevention Program (NAEPP) Coordinating Committee. Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. Available from: https://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm (accessed May 2014).
Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke H . A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. (PRISMS Practical Systematic Review of Self-Management Support for long-term conditions). Health Serv Deliv Res (in press).
Gibson PG, Powell H, Wilson A, Abramson MJ, Haywood P, Bauman A et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No. CD001117.
Tapp S, Lasserson TJ, Rowe BH . Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007: (Issue 3) Art No. CD003000.
Powell H, Gibson PG . Options for self-management education for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No: CD004107.
Toelle B, Ram FSF . Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev 2004: (Issue 1) Art No. CD002171.
Lefevre F, Piper M, Weiss K, Mark D, Clark N, Aronson N . Do written action plans improve patient outcomes in asthma? An evidence-based analysis. J Fam Pract 2002; 51 : 842–848.
PubMed Google Scholar
Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M . Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009: (Issue 2) Art No.CD001290.
Bravata DM, Gienger AL, Holty JE, Sundaram V, Khazeni N, Wise PH et al. Quality improvement strategies for children with asthma: a systematic review. Arch Pediatr Adolesc Med 2009; 163 : 572–581.
Bower P, Murray E, Kennedy A, Newman S, Richardson G, Rogers A . Self-management support interventions to reduce health care utilisation without compromising outcomes: a rapid synthesis of the evidence. Available from: http://www.nets.nihr.ac.uk/projects/hsdr/11101406 (accessed April 2014).
Gibson PG, Powell H . Written action plans for asthma: an evidence-based review of the key components. Thorax 2004; 59 : 94–99.
Article CAS Google Scholar
Bhogal SK, Zemek RL, Ducharme F . Written action plans for asthma in children. Cochrane Database Syst Rev 2006: (Issue 3) Art No. CD005306.
Zemek RL, Bhogal SK, Ducharme FM . Systematic review of randomized controlled trials examining written action plans in children: what is the plan?. Arch Pediatr Adolesc Med 2008; 162 : 157–163.
Pinnock H, Slack R, Pagliari C, Price D, Sheikh A . Understanding the potential role of mobile phone based monitoring on asthma self-management: qualitative study. Clin Exp Allergy 2007; 37 : 794–802.
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R . Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012: (Issue 12) Art No. CD007459.
Huckvale K, Car M, Morrison C, Car J . Apps for asthma self-management: a systematic assessment of content and tools. BMC Med 2012; 10 : 144.
Allergic Rhinitis and its Impact on Asthma. Management of Allergic Rhinitis and its Impact on Asthma: Pocket Guide. ARIA 2008. Available from: http://www.whiar.org (accessed May 2014).
Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011; 85 : e131–e143.
Moullec G, Gour-Provencal G, Bacon SL, Campbell TS, Lavoie KL . Efficacy of interventions to improve adherence to inhaled corticosteroids in adult asthmatics: Impact of using components of the chronic care model. Respir Med 2012; 106 : 1211–1225.
Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D et al. Accessibility, acceptability and effectiveness of telephone reviews for asthma in primary care: randomised controlled trial. BMJ 2003; 326 : 477–479.
Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A . Accessibility, clinical effectiveness and practice costs of providing a telephone option for routine asthma reviews: phase IV controlled implementation study. Br J Gen Pract 2007; 57 : 714–722.
PubMed PubMed Central Google Scholar
Kielmann T, Huby G, Powell A, Sheikh A, Price D, Williams S et al. From support to boundary: a qualitative study of the border between self care and professional care. Patient Educ Couns 2010; 79 : 55–61.
Asthma UK . Compare your care report. Asthma UK, 2013. Available from: http://www.asthma.org.uk (accessed January 2014).
Stallberg B, Lisspers K, Hasselgren M, Janson C, Johansson G, Svardsudd K . Asthma control in primary care in Sweden: a comparison between 2001 and 2005. Prim Care Respir J 2009; 18 : 279–286.
Reddel H, Peters M, Everett P, Flood P, Sawyer S . Ownership of written asthma action plans in a large Australian survey. Eur Respir J 2013; 42 . Abstract 2011.
Wiener-Ogilvie S, Pinnock H, Huby G, Sheikh A, Partridge MR, Gillies J . Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J 2007; 16 : 369–377.
Kennedy A, Rogers A, Bower P . Support for self care for patients with chronic disease. BMJ 2007; 335 : 968–970.
Ring N, Malcolm C, Wyke S, Macgillivray S, Dixon D, Hoskins G et al. Promoting the Use of Personal Asthma Action Plans: A Systematic Review. Prim Care Respir J 2007; 16 : 271–283.
Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB et al. A new perspective on concepts of asthma severity and control. Eur Respir J 2008; 32 : 545–554.
Horne R . Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130 (suppl): 65S–72S.
Reddel HK, Taylor DR, Bateman ED, Boulet L-P, Boushey HA, Busse WW et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009; 180 : 59–99.
Thomas M, Kay S, Pike J, Rosenzweig JR, Hillyer EV, Price D . The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Prim Care Respir J 2009; 18 : 41–49.
Hoskins G, Williams B, Jackson C, Norman P, Donnan P . Assessing asthma control in UK primary care: use of routinely collected prospective observational consultation data to determine appropriateness of a variety of control assessment models. BMC Fam Pract 2011; 12 : 105.
Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshon J, Price D et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010; 19 : 75–83.
McKinstry B, Hammersley V, Burton C, Pinnock H, Elton RA, Dowell J et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010; 19 : 298–303.
Gordon C, Galloway T . Review of Findings on Chronic Disease Self-Management Program (CDSMP) Outcomes: Physical, Emotional & Health-Related Quality of Life, Healthcare Utilization and Costs . Centers for Disease Control and Prevention and National Council on Aging: Atlanta, GA, USA, 2008.
Beasley R, Crane J . Reducing asthma mortality with the self-management plan system of care. Am J Respir Crit Care Med 2001; 163 : 3–4.
Ring N, Jepson R, Pinnock H, Wilson C, Hoskins G, Sheikh A et al. Encouraging the promotion and use of asthma action plans: a cross study synthesis of qualitative and quantitative evidence. Trials 2012; 13 : 21.
Jones A, Pill R, Adams S . Qualitative study of views of health professionals and patients on guided self-management plans for asthma. BMJ 2000; 321 : 1507–1510.
Bandura A . Self-efficacy: toward a unifying theory of behavioural change. Psychol Rev 1977; 84 : 191–215.
Gollwitzer PM, Sheeran P . Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol 2006; 38 : 69–119.
Google Scholar
Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham NJ, Kinmonth AL . Application of the theory of planned behaviour change interventions: a systematic review. Psychol Health 2002; 17 : 123–158.
Schwarzer R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008; 57 : 1–29.
Sniehotta F . Towards a theory of intentional behaviour change: plans, planning, and self-regulation. Br J Health Psychol 2009; 14 : 261–273.
Okelo SO, Butz AM, Sharma R, Diette GB, Pitts SI, King TM et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics 2013; 132 : 517–534.
Grol R, Grimshaw RJ . From best evidence to best practice: effective implementation of change in patients care. Lancet 2003; 362 : 1225–1230.
Jusef L, Hsieh C-T, Abad L, Chaiyote W, Chin WS, Choi Y-J et al. Primary care challenges in treating paediatric asthma in the Asia-Pacific region. Prim Care Respir J 2013; 22 : 360–362.
Donabedian A . Evaluating the quality of medical care. Milbank Q 2005; 83 : 691–729.
Fardy HJ . Moving towards organized care of chronic disease. The 3+ visit plan. Aust Fam Physician 2001; 30 : 121–125.
CAS PubMed Google Scholar
Glasgow NJ, Ponsonby AL, Yates R, Beilby J, Dugdale P . Proactive asthma care in childhood: general practice based randomised controlled trial. BMJ 2003; 327 : 659.
Douglass JA, Goemann DP, Abramson MJ . Asthma 3+ visit plan: a qualitative evaluation. Intern Med J 2005; 35 : 457–462.
Beilby J, Holton C . Chronic disease management in Australia; evidence and policy mismatch, with asthma as an example. Chronic Illn 2005; 1 : 73–80.
The Department of Health. Asthma Cycle of Care. Accessed on 14 May 2014 at http://www.health.gov.au/internet/main/publishing.nsf/Content/asthma-cycle .
National Asthma Council Australia. Asthma and Respiratory Education Program. Accessed on 14 May 2014 at http://www.nationalasthma.org.au/health-professionals/education-training/asthma-respiratory-education-program .
Patel MR, Shah S, Cabana MD, Sawyer SM, Toelle B, Mellis C et al. Translation of an evidence-based asthma intervention: Physician Asthma Care Education (PACE) in the United States and Australia. Prim Care Respir J 2013; 22 : 29–34.
Armour C, Bosnic-Anticevich S, Brilliant M, Burton D, Emmerton L, Krass I et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax 2007; 62 : 496–502.
Roberts NJ, Mohamed Z, Wong PS, Johnson M, Loh LC, Partridge MR . The development and comprehensibility of a pictorial asthma action plan. Patient Educ Couns 2009; 74 : 12–18.
Henry RL, Gibson PG, Vimpani GV, Francis JL, Hazell J . Randomised controlled trial of a teacher-led asthma education program. Pediatr Pulmonol 2004; 38 : 434–442.
National Asthma Council Australia. Asthma Friendly Schools program. Accessed on 14 May 2014 at http://www.asthmaaustralia.org.au/Asthma-Friendly-Schools.aspx .
Download references
Author information
Authors and affiliations.
Asthma UK Centre for Applied Research, Centre for Population Health Sciences, The University of Edinburgh, Edinburgh, UK,
Hilary Pinnock & Elisabeth Ehrlich
NMAHP-RU, University of Stirling, Stirling, UK,
Gaylor Hoskins
Discipline of General Practice, University of Sydney, Sydney, NSW, Australia
Ron Tomlins
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hilary Pinnock .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
Reprints and permissions
About this article
Cite this article.
Pinnock, H., Ehrlich, E., Hoskins, G. et al. A woman with asthma: a whole systems approach to supporting self-management. npj Prim Care Resp Med 24 , 14063 (2014). https://doi.org/10.1038/npjpcrm.2014.63
Download citation
Received : 23 June 2014
Revised : 15 July 2014
Accepted : 15 July 2014
Published : 16 October 2014
DOI : https://doi.org/10.1038/npjpcrm.2014.63
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
he Prescription Medicines Code of Practice Authority (PMCPA) in the UK has stated that patient case studies are likely to be viewed as promotional , and this obviously significantly limits how and when they can be employed. This article focuses on how compliance with the Association of the British Pharmaceutical Industry (ABPI) Code can still be achieved when case studies differ in their content and use. The ABPI code sets standards for pharmaceutical companies with respect to the promotion of medicines as well as the provision of information to patients. Some facts about patient case studies:
- Patient case studies can be theoretical or actual examples of a patient’s story, or in clinical terms, a particular medical case.
- These stories can range from discussing symptoms and diagnoses as well as charting the impact of treatment(s) and eventual outcome(s).
- They are used to make the intended audience aware of and more educated about patients and/or treatments.
- They are used in a variety of different educational or supporting materials like educational tools for healthcare professionals or supporting materials for patients that are prescribed a specific medicine and by different pharma functions.
But there are also questions that cause confusion or inconsistency in how and when they can be used in an effective and compliant way. The questions below frame some of the confusion. How Are Patient Case Studies Captured?
- Passively: Insights gathered from discussions, presentations, papers, or even advisory boards and market research can be used by pharmaceutical companies to create case studies.
- Actively: Patients or healthcare professionals (HCPs) can be engaged under an agreement and with compensation to specifically provide case studies. Patients can be approached directly, but often this is done through HCPs, patient organizations, or other third-party vendors.
When Are Theoretical Versus Actual Versus Anonymized Case Studies Best?
- Actual: To use the “testimony,” name, and photograph of a patient requires their prior explicit consent because a pharmaceutical company is storing and processing their sensitive personal data. But from an impact perspective, it can be credible for the company and valuable for the audience to hear the patient’s own words.
- Anonymized: These medical cases include minimal but relevant information (e.g., “Caucasian female, age 52 years”) that does not identify the patient. They are often used to avoid getting consent, particularly in scenarios where logistics can be problematic; e.g., an HCP engaged to speak at a meeting on behalf of a company about their experience may choose to describe several patients and convey their clinical experiences rather than relay their thoughts.
- Theoretical: Some clinical data about the use of a medicine may be best illustrated or “brought to life” in story terms. These case studies can still be based on actual stories.
Can Treatments Be Mentioned?
If a case study mentions a specific company, medicine, or the class it belongs to, then the company must consider carefully how this case study can be used.
- Acceptable: in promotional materials (campaign documentation, speaker slides, mailings) with a clear promotional intent.
- NOT acceptable: in proactive medical education.
- Might be acceptable: certain non-promotional settings, such as advisory boards or market research, but with very strict criteria in place. Furthermore, if the case study mentions the use of the medicine outside the approved label, then it has very limited uses (possibly in response to a very specific request for information).
If a case study mentions disease only (such as signs, symptoms, markers, diagnosis) and not medicine, then it could be used in a variety of promotional and non-promotional settings.
What Are Typical Versus Atypical Case Studies?
- Typical case studies reflect the summary of product characteristics (SPC) and the data that support the license approval. They should give a picture of what should generally be expected from treatment.
- Atypical case studies portray unexpected outcomes and can be associated with unlicensed uses or dosages.
While care should be taken that atypical case studies are never used in a manner similar to typical case studies, disclaimers are not enough in mitigating poor perception. For example, an HCP speaker should not present an atypical patient case study at a promotional meeting, because it is a European requirement that promotion of a medicine must not be inconsistent with its license particulars. So, a disclaimer cannot simply say “These are my views and not that of X company,” as the company is still liable under the code in ensuring that code requirements are always met.
Who can Case Studies be Used With?
- Members of the public: The case study is used as part of an effective disease awareness campaign, describing the disease but not the medicine/drug class.
- Patients on a company’s medicine: The case study describes a patient’s treatment experience as part of the medicine’s accompanying patient support material or programs.
- Journalists: To include case studies in a press release (e.g., backgrounders), it is imperative that the press release is newsworthy and relevant to a media outlet and its audience.
- Other audiences include regulators , e.g., Medicines and Healthcare Products Regulatory Agency (MHRA); national public bodies , e.g., National Institute for Health and Care Excellence (NICE); payers , parliamentarians , charities , and patient organizations .
Medical Versus Nonmedical Uses
Often, the demarcation between medical and nonmedical functions forces case studies to be used for one or the other. But if a case study mentions the respective disease only, then it can be used in both promotional and non-promotional contexts by all functions, for example:
- Promotional sales representatives can use the case study to help the HCP identify which of their patients present with the same symptoms and carry the conversation on to treatments.
- Non-promotional medical scientific liaison staff can use the case study to proactively educate HCPs on possible diagnoses.
- Head offices can use the case study in disease awareness campaigns, mailings to patient organizations, and internal education.

Case Study: Patient with Rare Breast Cancer Has Surprising Response to NAC
"Medical Journeys" is a set of clinical resources reviewed by doctors, meant for physicians and other healthcare professionals as well as the patients they serve. Each episode of this journey through a disease state contains both a physician guide and a downloadable/printable patient resource. "Medical Journeys" chart a path each step of the way for physicians and patients and provide continual resources and support, as the caregiver team navigates the course of a disease.
This installment: A noteworthy case study.
What are the recommended next steps for this 68-year-old woman who discovered a lump in her left breast when she was referred by her family physician for imaging? That's what Kumaraman Srivastava of Anne Burnett Marion School of Medicine at Texas Christian University in Fort Worth, and colleagues set out to determine.
As they explained in the Journal of Surgical Case Reports , the patient had no noteworthy medical history nor had she received routine breast screenings or breast biopsies. When she presented for assessment, she explained that for the last 9 months, she had become increasingly concerned when a new bluish/purple discoloration developed over the lump.
The imaging showed numerous abnormalities in the left breast and armpit, including a 4.6-cm irregular mass at 11 o'clock; a suspicious, enlarged axillary lymph node; and an area of 2.5 cm of heterogeneous calcifications in the 3 o'clock position.
The patient was given a mammography assessment, categorized as Breast Imaging-Reporting and Data System 5. Investigations included ultrasound-guided core needle biopsies of the two lesions located at 11:00 and in the axillary lymph node. Clinicians also performed a stereotactic core needle biopsy of the 3:00 calcifications.
The 4.6-cm lesion was found to be a grade 3 infiltrating ductal carcinoma with a minor squamous component. It was estrogen receptor (ER)+ (100%), progesterone receptor (PR)+ (100%), HER2/neu negative on fluorescence in situ hybridization (FISH). The Ki-67 score was 95%, and p53 was 100%.
Analysis of the sample from the lymph node identified metastatic breast carcinoma. Although this was primarily keratinizing squamous cell type, some of the tissue sample was similar to that of the breast tumor. "The node was ER 5%, PR-, and HER2/neu negative on FISH. Ki-67 was 80%, and p53 was 95. Biopsy of the calcifications revealed a small ductal carcinoma in situ.
Clinicians did not make any predictions about outcome at that time.
The team proposed a modified radical mastectomy of the left breast, with or without chemotherapy. Because her cancer was fairly extensive, the patient opted to receive neoadjuvant chemotherapy (NAC). Prior to that, she underwent staging scans, which showed no evidence of distant metastasis.
One month after her diagnosis, the patient started a regimen of doxorubicin and cyclophosphamide, which she received every 14 days for four cycles, followed by weekly treatment with paclitaxel for 12 cycles. She received her last round of chemotherapy 5 months after beginning treatment.
Clinicians monitored the patient's response to treatment with regular physical examinations. When the first cycle of chemotherapy had been completed, the primary tumor and lymph node had both decreased in size.
After the chemotherapy was completed, the patient had a final physical exam and diagnostic imaging of the breast and axilla. The results were positive, with indications that she had a complete pathologic response.
This meant, they said, that she was a candidate for a left localized partial mastectomy at the 12:00 and 3:00 positions with targeted axillary lymph node dissection. On the day before surgery, the team placed wireless localization reflectors at both breast sites and the clipped node. Surgery was performed successfully, and there were no complications.
During the surgery, the team performed a frozen section examination of four sentinel lymph nodes, including the prior biopsied node. Microscopic analysis showed no evidence of metastatic disease. Specimen x-rays taken during the surgery showed two partial mastectomy specimens with biopsy clips centered and reflectors in place.
Final testing of the sentinel lymph nodes showed a residual 8 mm invasive ductal carcinoma with negative margins at the 11:00 position. Tests of the four lymph nodes were negative, and the second sentinel lymph node showed the biopsy clip and evidence of scarring.
Pathologic analysis of the nodes at the 3 o'clock position found no evidence of residual carcinoma. Lobular carcinoma in situ was noted with all negative margins, and the patient's final pathologic stage was ypT1bypN0/stage IA breast carcinoma. The patient finished adjunct radiation treatment and continues to take antiestrogen therapy, the team reported.
Metaplastic breast carcinoma ( MpBC ) is a heterogeneous group of malignancies characterized by a non-glandular differentiation of breast tissue, including osseous, sarcomatous, and squamous histology, the case authors explained.
Under the World Health Organization classification of breast tumors, MpBC may be divided variously as epithelial, sarcomatoid, or mixed metaplastic. It typically presents as a triple-negative cancer, and tends to be larger and higher grade. Thus, compared with other triple-negative breast cancers, MpBC tends to have a worse prognosis -- likely related to its biology and generally poor response to chemotherapy.
MpBC is one of a rare group of malignancies, accounting for just 0.2-5% of breast cancers. Hence, data on MpBC are scarce, and currently limited to case reports, case series, and retrospective analyses. In the absence of consensus-based guidance on treatment, "physicians rely on case reports to help guide their understanding to help formulate optimal treatment options for patients," the authors stated.
Despite reports of some degree of response among some patients with MpBC, NAC remains largely ineffective in many patients, and their disease progresses.
"Due to the low reported response to NAC, and possible disease progression, treatment recommendations include early surgical resection and adjuvant therapy -- except in tumors <0.5 cm in size with no nodal or metastatic disease," Srivastava and co-authors noted.
Since these tumors are typically diagnosed at a later stage, when they tend to be large and high-grade, mastectomy is often necessary; surgery may be accompanied by adjuvant radiation, which has demonstrated survival benefits in these patients.
While chemotherapy also improves survival, its optimal role in treatment of patients who can undergo surgery is a subject of debate. And there is a lack of research data comparing adjuvant chemotherapy with NAC.
Complete pathological response to NAC is relatively rare in this cancer, the case authors noted. The positive outcome reported in their patient's case reflects the limited experience in this setting, which suggests similar overall survival rates with neoadjuvant and adjuvant chemotherapy in patients with node-positive disease.
Although MpBC is less likely than other breast cancers to respond to neoadjuvant treatment, patients who do receive to NAC have a higher likelihood of response or disease stability versus progression, Srivastava and co-authors noted.
Presurgical NAC has the potential to shrink the tumor, thus potentially reducing the extent of surgery required. Furthermore, data show similar outcomes with a conservative surgical approach compared with mastectomy, the team explained. "Additionally, NAC allows for in-vivo chemo-responsiveness to aid in adjuvant therapy planning and potential nodal regression, thus avoiding complete axillary node dissection."
That NAC was associated with a close to complete response in this patient's node-positive MpBC highlights the potential benefit of starting such patients on this treatment, the team concluded. Compared with initiating surgical treatment early, as recommended, starting NAC "could allow for decreased morbidity without increased mortality."
Read previous installments in this series:
Part 1: Breast Cancer -- The Basics of Diagnosis, Staging, and Treatment
Part 2: Breast Cancer: Making the Diagnosis With Breast Biopsy
Part 3: What to Know About Management of Early-Stage Breast Cancer
Part 4: New Treatment Options for Locally Advanced and Metastatic Breast Cancer
Part 5: Genetic Testing in Breast Cancer: Mutations, Multigene Panels, and More
Part 6: Case Study: Older Male With Rash, Chest Swelling, and Mysterious Skin Issues
Part 7: Breast Cancer Palliative Care and Metastatic Disease: Looking Beyond End of Life
Part 8: Breast Cancer and Post-Surgical Screening: Advising Patients on Appropriate Imaging
Part 9: The Key Role of Primary Care Providers in Managing Breast Cancer Tx-Related AEs
Srivastava and co-authors reported no conflicts of interest.

Association between MFN2 gene polymorphisms and the risk and prognosis of acute liver failure: a case-control study in a Chinese population
Affiliation.
- 1 Department of Infectious Diseases, Linyi People's Hospital, Linyi, China.
- PMID: 28513770
- PMCID: PMC5479382
- DOI: 10.1590/1414-431X20175758
This study aimed to determine the role of mitofusin 2 (MFN2) gene polymorphisms in the risk and prognosis of acute liver failure (ALF). A total of 298 blood samples were collected from 138 ALF patients (case group) and 160 healthy participants (control group). Coagulation function, glutamic pyruvic transaminase (GPT), glutamic oxaloacetic transaminase (GOT), total bilirubin (TB), blood ammonia and lactic acid (LA) were measured. The predictive evaluation of MFN2 gene polymorphisms in the risk and prognosis of ALF patients was estimated using Kaplan-Meier survival analysis, haplotype analysis, binary logistic regression analysis and Cox regression analysis. Higher levels of GPT, GOT, TB, blood ammonia and LA were observed in ALF patients with the GG genotype of rs873457 or the TT genotype of rs4846085 than in those with the CC genotype of these two SNPs. The GTACAGC and GTGTGGC haplotypes were a protective factor and a risk factor for ALF, respectively. Blood ammonia and LA levels were independent risk factors and the CC genotype of rs873457 and the CC genotype of rs4846085 were protective factors for ALF. ALF patients with the GG genotype of rs873457 or the TT genotype of rs4846085 had a lower survival rate than those with other genotypes of these two SNPs. The rs4846085 and rs873457 polymorphisms were both independent factors affecting the prognosis of ALF patients. MFN2 gene polymorphisms (rs873457, rs2336384, rs1474868, rs4846085 and rs2236055) may be associated with ALF and the rs873457 and rs4846085 polymorphisms are correlated with the risk and prognosis of ALF.
- Ammonia / blood
- Asian People / genetics
- Case-Control Studies
- GTP Phosphohydrolases / genetics*
- Gene Frequency / genetics
- Genetic Predisposition to Disease / genetics
- Hepatitis A / genetics
- Kaplan-Meier Estimate
- Lactic Acid / blood
- Liver Failure, Acute / blood
- Liver Failure, Acute / genetics*
- Middle Aged
- Mitochondrial Proteins / genetics*
- Polymorphism, Single Nucleotide*
- Risk Factors
- Survival Analysis
- Young Adult
- Mitochondrial Proteins
- Lactic Acid
- GTP Phosphohydrolases
- MFN2 protein, human
- Open access
- Published: 05 June 2024
Current status and ongoing needs for the teaching and assessment of clinical reasoning – an international mixed-methods study from the students` and teachers` perspective
- F. L Wagner 1 ,
- M. Sudacka 2 ,
- A. A Kononowicz 3 ,
- M. Elvén 4 , 5 ,
- S. J Durning 6 ,
- I. Hege 7 &
- S. Huwendiek 1
BMC Medical Education volume 24 , Article number: 622 ( 2024 ) Cite this article
Metrics details
Clinical reasoning (CR) is a crucial ability that can prevent errors in patient care. Despite its important role, CR is often not taught explicitly and, even when it is taught, typically not all aspects of this ability are addressed in health professions education. Recent research has shown the need for explicit teaching of CR for both students and teachers. To further develop the teaching and learning of CR we need to improve the understanding of students' and teachers' needs regarding content as well as teaching and assessment methods for a student and trainer CR curriculum.
Parallel mixed-methods design that used web-surveys and semi-structured interviews to gather data from both students (n survey = 100; n interviews = 13) and teachers (n survey = 112; n interviews = 28). The interviews and surveys contained similar questions to allow for triangulation of the results. This study was conducted as part of the EU-funded project DID-ACT ( https://did-act.eu ).
Both the surveys and interview data emphasized the need for content in a clinical reasoning (CR) curriculum such as “gathering, interpreting and synthesizing patient information”, “generating differential diagnoses”, “developing a diagnostic and a treatment plan” and “collaborative and interprofessional aspects of CR”. There was high agreement that case-based learning and simulations are most useful for teaching CR. Clinical and oral examinations were favored for the assessment of CR. The preferred format for a train-the-trainer (TTT)-course was blended learning. There was also some agreement between the survey and interview participants regarding contents of a TTT-course (e.g. teaching and assessment methods for CR). The interviewees placed special importance on interprofessional aspects also for the TTT-course.
Conclusions
We found some consensus on needed content, teaching and assessment methods for a student and TTT-course in CR. Future research could investigate the effects of CR curricula on desired outcomes, such as patient care.
Peer Review reports
Introduction
Clinical reasoning (CR) is a universal ability that mobilizes integration of necessary fundamental knowledge while delivering high-quality patient care in a variety of contexts in a timely and effective way [ 1 , 2 ]. Daniel et al. [ 3 ] define it as a “skill, process or outcome wherein clinicians observe, collect, and interpret data to diagnose and treat patients”. CR encompasses health professionals thinking and acting in patient assessment, diagnostic, and management processes in clinical situations, taking into account the patient ‘s specific circumstances and preferences [ 4 ]. How CR is defined can vary between health professions, but there are also similarities [ 5 ]. Poor CR is associated with low-quality patient care and increases the risk of medical errors [ 6 ]. Berner and Graber [ 7 ] suggested that the rate of diagnostic error is around 15%, underlining the threat that insufficient CR ability poses to patient safety as well as increasing healthcare costs [ 8 ]. Despite the importance of CR, it appears to be rarely taught or assessed explicitly, often only parts of the CR process are covered in existing curricula, and there seems to be a lack of progression throughout curricula (e.g. [ 9 , 10 , 11 , 12 , 13 , 14 ].). Moreover, teachers are often not trained to explicitly teach CR, including explaining their own reasoning to others [ 10 , 11 , 12 ] although this appears to be an important factor in the implementation of a CR curriculum [ 15 ]. Some teachers even question whether CR can be explicitly taught [ 16 ]. Considering these findings, efforts should be made to incorporate explicit teaching of CR into health care professions curricula and training for teachers should be established based on best evidence. However, to date, little is known about what a longitudinal CR curriculum should incorporate to meet the needs of teachers and students.
Insights regarding teaching CR were provided from a global survey by Kononowicz et al. [ 10 ], who reported a need for a longitudinal CR curriculum. However, the participants in their study were mainly health professions educators, leaving the needs of students for a CR curriculum largely unknown. As students are future participants of a CR curriculum, their needs should also be investigated. Kononowicz et al. [ 10 ] also identified a lack of qualified faculty to teach CR. A train-the-trainer course for CR could help reduce this barrier to teaching CR. To the best of our knowledge, in addition to the work by Kononowicz et al. [ 10 ], no research exists yet that addresses the needs of teachers for such a course, and Kononowicz et al. [ 10 ] did not investigate their needs beyond course content. Recently, Gupta et al. [ 12 ] and Gold et al. [ 13 ] conducted needs analyses regarding clinical reasoning instruction from the perspective of course directors at United States medical schools, yet a European perspective is missing. Thus, our research questions were the following:
What aspects of clinical reasoning are currently taught and how important are they in a clinical reasoning curriculum according to teachers and students?
What methods are currently used to teach and assess clinical reasoning and which methods would be ideal according to teachers and students?
In what study year does the teaching of clinical reasoning currently begin and when should it ideally begin according to teachers and students?
How should a train-the-trainer course for teachers of clinical reasoning be constructed regarding content and format?
In this study, we used a convergent parallel mixed-methods design [ 17 ] within a pragmatic constructivist case study approach [ 18 ]. We simultaneously collected data from students and educators using online questionnaires and semi-structured interviews to gain deeper insight into their needs on one particular situation [ 19 ]– the development of a clinical reasoning curriculum—to address our research questions. To help ensure that the results of the survey and the interviews could be compared and integrated, we constructed the questions for the survey and the interviews similarly with the exception that in the interviews, the questions were first asked openly. The design was parallel both in that we collected data simultaneously and also constructed the survey and interviews to cover similar topics. We chose this approach to obtain comprehensive answers to the research questions and to facilitate later triangulation [ 17 ] of the results.
Context of this study
We conducted this study within the EU-funded (Erasmus + program) project DID-ACT (“Developing, implementing, and disseminating an adaptive clinical reasoning curriculum for healthcare students and educators”; https://did-act.eu ). Institutions from six European countries (Augsburg University, Germany; Jagiellonian University in Kraków, Poland; Maribor University, Slovenia; Örebro University, Sweden; University of Bern, Switzerland; EDU, a higher medical education institution based in Malta, Instruct GmbH, Munich, Germany) with the support of associate partners (e.g., Prof. Steven Durning, Uniformed Services University of the Health Sciences, USA; Mälardalen University, Sweden.) were part of this project. For further information, see https://did-act.eu/team-overview/team/ . In this project, we developed an interprofessional longitudinal clinical reasoning curriculum for students in healthcare education and a train-the-trainer course for health profession educators. The current curriculum (for a description of the curriculum, see Hege et al. [ 20 ]) was also informed by this study. This study was part of the Erasmus + Knowledge Alliance DID-ACT (612,454-EPP-1–2019-1-DE-EPPKA2-KA).
Target groups
We identified two relevant target groups for this study, teachers and students, which are potential future users and participants of a train—the—trainer (TTT-) course and a clinical reasoning curriculum, respectively. The teacher group also included individuals who were considered knowledgeable regarding the current status of clinical reasoning teaching and assessment at their institutions (e.g. curriculum managers). These specific participants were individually selected by the DID-ACT project team to help ensure that they had the desired level of expertise. The target groups included different health professions from a large number of countries (see Table 1 ), as we wanted to gather insights that are not restricted to one profession.
Development of data collection instruments
Development of questions.
The questions in this study addressed the current status and needs regarding content, teaching, and assessment of clinical reasoning (CR). They were based on the questions used by Kononowicz et al. [ 10 ] and were expanded to obtain more detailed information. Specifically, regarding CR content, we added additional aspects (see Table 8 in the Appendix for details). The contents covered in this part of the study also align with the five domains of CR education (clinical reasoning concepts, history and physical examination, choosing and interpreting diagnostic tests, problem identification and management and shared decision-making) that were reported by Cooper et al. [ 14 ]. It has been shown that there are similarities between professions regarding the definition of CR (e.g. history taking or an emphasis on clinical skills), while nurses placed greater importance on a patient-centered approach [ 5 ]. We aimed to cover as many aspects of CR in the contents as possible to represent these findings. We expanded the questions on CR teaching formats to cover a broader range of formats. Furthermore, two additional assessment methods were added to the respective questions. Finally, one aspect was added to the content questions for a train-the-trainer course (see Table 8 in the Appendix ). As a lack of qualified faculty to teach CR was identified in the study by Kononowicz et al. [ 10 ], we added additional questions on the specific needs for the design of a CR train-the-trainer course beyond content. Table 8 in the Appendix shows the adaptations that we made in detail.
We discussed the questions within the interprofessional DID-ACT project team and adapted them in several iterative cycles until the final versions of the survey questionnaire and the interview guide were obtained and agreed upon. We tested the pre-final versions with think-alouds [ 21 ] to ensure that the questions were understandable and interpreted as intended, which led to a few changes. The survey questionnaires and interview-guides can be found at https://did-act.eu/results/ and accessed via links in table sections D1.1a (survey questions) and D1.1b (interview guides), respectively. Of these questions, we included only those relevant to the research questions addressed in this study. The questions included in this study can be found in the Appendix in Table8.
Teachers were asked questions about all content areas, but only the expert subgroup was asked to answer questions on the current situation regarding the teaching and assessment of clinical reasoning at their institutions, as they were considered the best informed group on the matter. Furthermore, students were not asked questions on the train-the-trainer course. Using the abovementioned procedures, we also hoped to improve the response rate as longer surveys were found to be associated with lower response rates [ 22 ].
We created two different versions of the interview guide, one for teachers and one for students. The student interview guide did not contain questions on the current status of clinical reasoning teaching and assessment or questions about the train-the-trainer course. The interview guides were prepared with detailed instructions to ensure that the interviews were conducted in a comparable manner at all locations. By using interviews, we intended to obtain a broad picture of existing needs. Individual interviews further allowed participants to speak their own languages and thus to express themselves naturally and as precisely as possible.

Reflexivity statement
Seven researchers representing different perspectives and professions form the study team. MS has been a PhD candidate representing the junior researcher perspective, while also experienced researchers with a broad background in clinical reasoning and qualitative as well as quantitative research are part of the team (SD, SH, AK, IH, ME, FW). ME represents the physiotherapist perspective, SD, SH, and MS represent the medical perspective. We discussed all steps of the study in the team and made joint decisions.
Data collection and analysis
The survey was created using LimeSurvey software (LimeSurvey GmbH). The survey links were distributed via e-mail (individual invitations, posts to institutional mailing lists, newsletters) by the DID-ACT project team and associate partners (the target groups received specific links to the online-survey). The e-mail contained information on the project and its goals. By individually contacting persons in the local language, we hoped to increase the likelihood of participation. The survey was anonymous. The data were collected from March to July 2020.
Potential interview participants were contacted personally by the DID-ACT project team members in their respective countries. We used a convenience sampling approach by personally contacting potential interview partners in the local language to motivate as many participants as possible. With this approach we also hoped to increase the likelihood of participation. The interviews were conducted in the local languages also to avoid language barriers and were audio-recorded to help with the analysis and for documentation purposes. Most interviews were conducted using online meeting services (e.g. Skype or Zoom) because of restrictions due to the ongoing coronavirus pandemic that occurred with the start of data collection at the beginning of the DID-ACT project. The data were collected from March to July 2020. All interview partners provided informed consent.
Ethics approval and consent to participate
We asked the Bern Ethics Committee to approve this multi-institutional study. This type of study was regarded as exempt from formal ethical approval according to the regulations of the Bern Ethics Committee (‘Kantonale Ethikkommission Bern’, decision Req-2020–00074). All participants voluntarily participated and provided informed consent before taking part in this study.
Data analysis
Descriptive analyses were performed using SPSS statistics software (version 28, 2021). Independent samples t-tests were computed for comparisons between teachers and students. When the variances of the two groups were unequal, Welch’s test was used. Bonferroni correction of significance levels was used to counteract alpha error accumulation in repeated tests. The answers to the free text questions were screened for recurring themes. There were very few free-text comments, typically repeating aspects from the closed questions, hence, no meaningful analysis was possible. For this reason, the survey comments are mentioned only where they made a unique contribution to the results.
The interviews were translated into English by the partners. An overarching summarizing qualitative content analysis [ 23 ] of the data was conducted. A summarizing content analysis is particularly useful when the content level of the material is of interest. Its goal is to reduce the material to manageable short texts in a way that retains the essential meaning [ 23 ]. The analysis was conducted first by two of the authors of the study (FW, SH) and then discussed by the entire author team. The analysis was carried out as an iterative process until a complete consensus was reached within the author team.
The results from the surveys and interviews were compared and are presented together in the results section. The qualitative data are reported in accordance with the standards for reporting qualitative research (SRQR, O’Brien et al. [ 24 ]).
Table 1 shows the professional background and country of the interviewees and survey samples. The survey was opened by 857 persons, 212 (25%) of whom answered the questions included in this study. The expert sub-group of teachers who answered the questions on the current status of clinical reasoning teaching and assessment encompassed 45 individuals.
Content of a clinical reasoning curriculum for students
The survey results show that “Gathering, interpreting, and synthesizing patient information”, is currently most extensively taught, while “Theories of clinical reasoning” are rarely taught (see Table 2 ). In accordance with these findings, “Gathering, interpreting, and synthesizing patient information” received the highest mean importance rating for a clinical reasoning curriculum while “Theories of clinical reasoning” received the lowest importance rating. Full results can be found in Table 9 in the Appendix .
Teachers and students differed significantly in their importance ratings of two content areas, “Gathering, interpreting, and synthesizing patient information” ( t (148.32) = 4.294, p < 0.001, d = 0.609) and “Developing a problem formulation/hypothesis” ( t (202) = 4.006, p < 0.001, d = 0.561), with teachers assigning greater importance to both of these content areas.
The results from the interviews are in line with those from the survey. Details can be found in Table 12 in the Appendix .
Clinical reasoning teaching methods
The survey participants reported that, most often, case-based learning is currently applied in the teaching of clinical reasoning (CR). This format was also rated as most important for teaching CR (see Table 3 ). Full results can be found in Table 10 in the Appendix .
Teachers and students differed significantly in their importance ratings of Team-based learning ( t (202) = 3.079, p = 0.002, d = 0.431), with teachers assigning greater importance to this teaching format.
Overall, the interviewees provided very similar judgements to the survey participants. Next to the teaching formats shown in Table 3 , some of them would employ blended learning, and clinical teaching formats such as bedside teaching and internships were also mentioned. Details can be found in the Appendix in Table 13. In addition to the importance of each individual teaching format, it was also argued that all of the formats can be useful because they all are meant to reach different objectives and that there is not one single best format for teaching CR.
Start of clinical reasoning teaching in curricula
Most teachers (52.5%) reported that currently, the teaching of clinical reasoning (CR) starts in the first year of study. Most often (46.4%) the participants also chose the first study year as the optimal year for starting the teaching CR. In accordance with the survey results, the interviewees also advocated for an early start of the teaching of CR. Some interview participants who advocated for a later start of CR teaching suggested that the students first need a solid knowledge base and that once the clinical/practical education starts, explicit teaching of CR should begin.
Assessment of clinical reasoning
The survey results suggest that currently written tests or clinical examinations are most often used, while Virtual Patients are used least often (see Table 4 ). Despite written tests being the most common current assessment format, they received the lowest importance rating for a future longitudinal CR curriculum. Full results can be found in Table 11 in the Appendix .
Teachers and students differed significantly in their importance ratings of clinical examinations ( t (161.81) = 2.854, p = 0.005, d = 0.413) and workplace-based assessments ( t (185) = 2.640, p = 0.009, d = 0.386) with teachers assigning greater importance to both of these assessment formats.
The interviewees also placed importance on all assessment methods but found it difficult to assess CR with written assessment methods. The students seemed to associate clinical examinations more with practical skills than with CR. Details can be found in the Appendix in Table 14. Two of the interview participants mentioned that CR is currently not assessed at their institutions, and one person mentioned that students are asked to self-reflect on their interactions with patients and on potential improvements.
Train-the-trainer course
The following sections highlight the results from the needs analysis regarding a train-the-trainer (TTT-) course. The questions presented here were posed only to the teachers.
Most survey participants reported that there is currently no TTT- course on clinical reasoning at their institution but that they think such a course is necessary (see Table 5 ). The same was also true for the interviewees (no TTT- course on clinical reasoning existing but need for one).
In the interviews, 22 participants (78.6%) answered that a TTT-course is necessary for healthcare educators, two participants answered that no such course was necessary, and two other participants were undecided about its necessity. At none of the institutions represented by the interviewees, a TTT-course for teaching clinical reasoning exists.
When asked what the best format for a clinical reasoning TTT- course would be (single answer question), the majority of the survey participants favored a blended learning / flipped classroom approach, a combination of e-learning and face-to-face meetings. (see Table 6 ).
In the survey comments it was noted that blended-learning encompasses the benefits of both self-directed learning and discussion/learning from others. It would further allow teachers to gather knowledge about CR first in an online learning phase where they can take the time they need before coming to a face-to-face meeting.
The interviewees also found a blended-learning approach particularly suitable for a TTT-course. An e-learning course only was seen as more critical because teachers may lack motivation to participate in an online-only setting, while a one-time face-to-face meeting would not provide enough time. In some interviews, it was emphasized that teachers should experience themselves what they are supposed to teach to the students and also that the trainers for the teachers need to have solid education and knowledge on clinical reasoning.
Table 7 shows the importance ratings of potential content of a TTT-course generated from the survey. To elaborate on this content, comments by the interviewees were added. On average, all content was seen as (somewhat) important with teaching methods on the ward and/or clinic receiving the highest ratings. Some interviewees also mentioned the importance of interprofessional aspects and interdisciplinary understanding of CR. In the survey comments, some participants further expressed their interest in such a course.
Finally, the interviewees were asked about the ideal length of a clinical reasoning TTT-course. The answers varied greatly from 2–3 hours to a two-year educational program, with a tendency toward 1–2 days. Several interviewees commented that the time teachers are able to spend on a TTT-course is limited. This should be considered in the planning of such a course to make participation feasible for teachers.
In this study, we investigated the current status of and suggestions for teaching and assessment of clinical reasoning (CR) in a longitudinal curriculum as well as suggestions for a train-the-trainer (TTT-) course for CR. Teachers and students were invited to participate in online-surveys as well as semi-structured interviews to derive answers to our research questions. Regarding the contents of a CR curriculum for students, the results of the surveys and interviews were comparable and favoured content such as gathering, interpreting, and synthesizing patient information, generating differential diagnoses, and developing a diagnostic and a treatment plan. In the interviews, high importance was additionally placed on collaborative and interprofessional aspects of CR. Case-based learning and simulations were seen as the most useful methods for teaching CR, and clinical and oral examinations were favoured for the assessment of CR. The preferred format for a TTT-course was blended learning. In terms of course content, teaching and assessment methods for CR were emphasized. In addition to research from the North American region [ 11 ], this study provides results from predominantly European countries that support the existing findings.
Content of a clinical reasoning curriculum
Our results revealed that there are still aspects of clinical reasoning (CR), such as “Errors in the clinical reasoning process and strategies to avoid them” or “Interprofessional aspects of CR” that are rarely taught despite their high importance, corroborating the findings of Kononowicz et al. [ 10 ]. According to the interviewees, students should have basic knowledge of CR before they are taught about errors in the CR process and strategies to avoid them. The lack of teaching of errors in CR may also stem from a lack of institutional culture regarding how to manage failures in a constructive way (e.g. [ 16 , 25 ]), making it difficult to explicitly address errors and strategies to avoid them. Although highly relevant in the everyday practice of healthcare professions and underpinned by CR theoretical frameworks (e.g., distributed cognition [ 26 ]), interprofessional and collaborative aspects of CR are currently rarely considered in the teaching of CR. The interviews suggested that hierarchical distance and cultural barriers may contribute to this finding. Sudacka et al. [ 16 ] also reported cultural barriers as one reason for a lack of CR teaching. Generally, the interviewees seemed to place greater importance on interprofessional and collaborative aspects than did the survey-participants This may have been due to differences in the professions represented in the two modalities (e.g., a greater percentage of nurses among the interview participants, who tend to define CR more broadly than physicians [ 5 ]).
“Self-reflection on clinical reasoning performance and strategies for future improvement”, “Developing a problem formulation/hypothesis” and “Aspects of patient-participation in CR” were rated as important but are currently rarely taught, a finding not previously reported. The aspect “Self-reflection on clinical reasoning performance and strategies for future improvement”, received high importance ratings, but only 25% of the survey-participants answered that it is currently taught to a great extent. The interviewees agreed that self-reflection is important and added that ideally, it should be guided by specific questions. Ogdie et al. [ 27 ] found that reflective writing exercises helped students identify errors in their reasoning and biases that contributed to these errors.
“Gathering, interpreting, and synthesizing patient information” and “Developing a problem formulation/hypothesis” were rated significantly more important by teachers than by students. It appears that students may be less aware yet of the importance of gathering, interpreting, and synthesizing patient information in the clinical reasoning process. There was some indication in the interviews that the students may not have had enough experience yet with “Developing a problem formulation/hypothesis” or associate this aspect with research, possibly contributing to the observed difference.
Overall, our results on the contents of a CR curriculum suggest that all content is important and should be included in a CR curriculum, starting with basic theoretical knowledge and data gathering to more advanced aspects such as errors in CR and collaboration. Two other recent surveys conducted in the United States among pre-clerkship clinical skills course directors [ 12 ] and members of clerkship organizations [ 13 ] came to similar conclusions regarding the inclusion of clinical reasoning content at various stages of medical curricula. How to fit the content into already dense study programs, however, can still be a challenge [ 16 ].
In addition to case-based learning and clinical teaching, human simulated patients and Team-based learning also received high importance ratings for teaching clinical reasoning (CR), a finding not previously reported. Lectures, on the other hand, are seen as the least important to teach CR (see also Kononowicz et al. [ 10 ]), as they mainly deliver factual knowledge according to the interviewees. High-fidelity simulations (mannequins) and Virtual Patients (VPs) are rarely used to teach CR at the moment and are rated less important compared to other teaching formats. Some interviewees see high-fidelity simulations as more useful for teaching practical skills. The lower importance rating of VPs was surprising given that this format is case-based, provides a safe environment for learning, and is described in the literature as a well-suited tool for teaching CR [ 28 , 29 ]. Considering that VPs seemed to be used less often at the institutions involved in this study, the lack of experience with this format may have led to this result.
Teachers rated Team-based learning as significantly more important for teaching clinical reasoning than students. In the interviews, many students seemed not to be familiar with Team-based learning, possibly explaining the lower ratings the students gave this format in the survey.
Taken together, our results suggest that there is not one best format for teaching all aspects of clinical reasoning but rather that the use of all teaching formats is justified depending on the specific content to be taught and goals to be achieved. However, there was agreement that a safe learning environment where no patients can be harmed is preferred for teaching clinical reasoning, and that discussions should be possible.
There was wide agreement that clinical reasoning (CR) teaching should start in the first year of study in the curriculum. However, a few participants of this study argued that students first need to develop some general knowledge before CR is taught. Rencic et al. [ 11 ] reported that according to internal medicine clerkship directors, CR should be taught throughout all years of medical school, with a particular focus during the clinical teaching years. A similar remark was made by participants in a survey among pre-clerkship clinical skills course directors by Gupta et al. [ 12 ] where the current structure of some curricula (e.g. late introduction of the pathophysiology) was regarded as a barrier to introducing CR from the first year of study on [ 12 ].
Our results show that the most important format for assessing clinical reasoning (CR) that is also currently used to the greatest extent are clinical examinations (e.g. OSCE), consistent with Kononowicz et al. [ 10 ]. The interviewees emphasized that CR should ideally be assessed in a conversation or discussion where the learners can explain their reasoning. Given this argument, all assessment formats enabling a conversation are suitable for assessing CR. This is reflected in our survey results, where assessment formats that allow for a discussion with the learner received the most favourable importance ratings, including oral examinations. In agreement with Kononowicz et al. [ 10 ], we also found that written tests are currently used most often to assess CR but are rated as least important and suitable only for the assessment of some aspects of CR. Daniel et al. [ 3 ] argued that written exams such as MCQs, where correct answers have to be selected from a list of choices, are not the best representation of real practical CR ability. Thus, there still seems to be potential for improvement in the way CR is assessed.
Teachers rated clinical examinations and workplace-based assessments significantly higher than students. Based on the interviews, the students seemed to associate clinical examinations such as OSCEs more with a focus on practical skills than CR, potentially explaining their lower ratings of this format.
What a clinical reasoning train-the-trainer course should look like
Our results show a clear need for a clinical reasoning (CR) train-the-trainer course (see also Singh et al. [ 15 ]), which currently does not exist at most institutions represented in this study, corroborating findings by Kononowicz et al. [ 10 ]. A lack of adequately trained teachers is a common barrier to the introduction of CR content into curricula [ 12 , 16 ]. According to our results such a course should follow a blended learning/flipped classroom approach or consist of a series of face-to-face meetings. A blended-learning course would combine the benefits of both self-directed learning and the possibility for trainers to discuss with and learn from their peers, which could also increase their motivation to participate in such a course. An e-learning only course or a one-time face-to-face meeting were considered insufficient. The contents “Clinical reasoning strategies” and “Common errors in the clinical reasoning process” were given greater importance for the trainer-curriculum than for the students-curriculum, possibly reflecting higher expectations of trainers as “CR experts” compared with students. There was some agreement in the interviews that ideally, the course should not be too time-consuming, with participants tending towards an overall duration of 1–2 days, considering that most teachers usually have many duties and may not be able or willing to attend the course if it were too long. Lack of time was also identified as a barrier to attending teacher training [ 12 , 13 , 16 ].
Strengths and limitations
The strengths of this study include its international and interprofessional participants. Furthermore, we explicitly included teachers and students as target groups in the same study, which enables a comparison of different perspectives. Members of the target groups not only participated in a survey but were also interviewed to gain in-depth knowledge. A distinct strength of this study is its mixed-methods design. The two data collection methods employed in parallel provided convergent results, with responses from the web survey indicating global needs and semi-structured interviews contributing to a deeper understanding of the stakeholder groups’ nuanced expectations and perspectives on CR education.
This study is limited in that most answers came from physicians, making the results potentially less generalizable to other professions. Furthermore, there were participants from a great variety of countries, with some countries overrepresented. Because of the way the survey-invitations were distributed, the exact number of recipients is unknown, making it impossible to compute an exact response rate. Also, the response rate of the survey was rather low for individuals who opened the survey. Because the survey was anonymous, it cannot completely be ruled out that some individuals participated in both interviews and survey. Finally, there could have been some language issues in the interview analysis, as the data were translated to English at the local partner institutions before they were submitted for further analysis.
Our study provides evidence of an existing need for explicit clinical reasoning (CR) longitudinal teaching and dedicated CR teacher training. More specifically, there are aspects of CR that are rarely taught that our participants believe should be given priority, such as self-reflection on clinical reasoning performance and strategies for future improvement and aspects of patient participation in CR that have not been previously reported. Case-based learning and clinical teaching methods were again identified as the most important formats for teaching CR, while lectures were considered relevant only for certain aspects of CR. To assess CR, students should have to explain their reasoning, and assessment formats should be chosen accordingly. There was also still a clear need for a CR train-the-trainer course. In addition to existing research, our results show that such a course should ideally have a blended-learning format and should not be too time-consuming. The most important contents of the train-the-trainer course were confirmed to be teaching methods, CR strategies, and strategies to avoid errors in the CR process. Examples exist for what a longitudinal CR curriculum for students and a corresponding train-the-trainer course could look like and how these components could be integrated into existing curricula (e.g. DID-ACT curriculum [ 20 ], https://did-act.eu/integration-guide/ or the described curriculum of Singh et al. [ 15 ]). Further research should focus on whether and to what extent the intended outcomes of such a curriculum are actually reached, including the potential impact on patient care.
Availability of data and materials
All materials described in this manuscript generated during the current study are available from the corresponding author on reasonable request without breaching participant confidentiality.
Connor DM, Durning SJ, Rencic JJ. Clinical reasoning as a core competency. Acad Med. 2020;95:1166–71.
Article Google Scholar
Young M, Szulewski A, Anderson R, Gomez-Garibello C, Thoma B, Monteiro S. Clinical reasoning in CanMEDS 2025. Can Med Educ J. 2023;14:58–62.
Google Scholar
Daniel M, Rencic J, Durning SJ, Holmboe E, Santen SA, Lang V, Gruppen LD. Clinical reasoning assessment methods: a scoping review and practical guidance. Acad Med. 2019;94:902–12.
Scott IA. Errors in clinical reasoning: causes and remedial strategies. BMJ. 2009. https://doi.org/10.1136/bmj.b1860 .
Huesmann L, Sudacka M, Durning SJ, Georg C, Huwendiek S, Kononowicz AA, Schlegel C, Hege I. Clinical reasoning: what do nurses, physicians, and students reason about. J Interprof Care. 2023;37:990–8.
Norman GR, Eva KW. Diagnostic error and clinical reasoning. Med Educ. 2010;44:94–100.
Berner E, Graber M. Overconfidence as a cause of diagnostic error in medicine. Am J Med. 2008;121:2–23.
Cooper N, Da Silva AL, Powell S. Teaching clinical reasoning. In: Cooper N, Frain J, editors. ABC of clinical reasoning. 1st ed. Hoboken, NJ: John Wiley & Sons Ltd; 2016. p. 44–50.
Elvén M, Welin E, Wiegleb Edström D, Petreski T, Szopa M, Durning SJ, Edelbring S. Clinical reasoning curricula in health professions education: a scoping review. J Med Educ Curric Dev. 2023. https://doi.org/10.1177/23821205231209093 .
Kononowicz AA, Hege I, Edelbring S, Sobocan M, Huwendiek S, Durning SJ. The need for longitudinal clinical reasoning teaching and assessment: results of an international survey. Med Teach. 2020;42:457–62.
Rencic J, Trowbridge RL, Fagan M, Szauter K, Durning SJ. Clinical reasoning education at US medical schools: results from a national survey of internal medicine clerkship directors. J Gen Intern Med. 2017;32:1242–6.
Gupta S, Jackson JM, Appel JL, Ovitsh RK, Oza SK, Pinto-Powell R, Chow CJ, Roussel D. Perspectives on the current state of pre-clerkship clinical reasoning instruction in United States medical schools: a survey of clinical skills course directors. Diagnosis. 2021;9:59–68.
Gold JG, Knight CL, Christner JG, Mooney CE, Manthey DE, Lang VJ. Clinical reasoning education in the clerkship years: a cross-disciplinary national needs assessment. PLoS One. 2022;17:e0273250.
Cooper N, Bartlett M, Gay S, Hammond A, Lillicrap M, Matthan J, Singh M. UK Clinical Reasoning in Medical Education (CReME) consensus statement group. Consensus statement on the content of clinical reasoning curricula in undergraduate medical education. Med Teach. 2021;43:152–9.
Singh M, Collins L, Farrington R, Jones M, Thampy H, Watson P, Grundy J. From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. Diagnosis. 2021;9:184–94.
Sudacka M, Adler M, Durning SJ, Edelbring S, Frankowska A, Hartmann D, Hege I, Huwendiek S, Sobočan M, Thiessen N, Wagner FL, Kononowicz AA. Why is it so difficult to implement a longitudinal clinical reasoning curriculum? A multicenter interview study on the barriers perceived by European health professions educators. BMC Med Educ. 2021. https://doi.org/10.1186/s12909-021-02960-w .
Hingley A, Kavaliova A, Montgomery J, O’Barr G. Mixed methods designs. In: Creswell JW, editor. Educational research: planning, conducting, and evaluating quantitative and qualitative research. 4th ed. Boston: Pearson; 2012. p. 534–75.
Merriam SB. Qualitative research and case study applications in education. In: from" case study research in education.". Sansome St. Revised and Expanded. San Francisco, CA: Jossey-Bass Publishers; 1998.
Cleland J, MacLeod A, Ellaway RH. The curious case of case study research. Med Educ. 2021;55:1131–41.
Hege I, Adler M, Donath D, Durning SJ, Edelbring S, Elvén M, Wiegleb Edström D. Developing a European longitudinal and interprofessional curriculum for clinical reasoning. Diagnosis. 2023;10:218–24.
Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res. 2003;12:229–38.
Liu M, Wronski L. Examining completion rates in web surveys via over 25,000 real-world surveys. Soc Sci Comput Rev. 2018;36:116–24.
Mayring P, Fenzl T. Qualitative inhaltsanalyse. In: Baur N, Blasius J, editors. Handbuch methoden der empirischen Sozialforschung. Wiesbaden: Springer VS; 2019. p. 633–48.
Chapter Google Scholar
O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89:1245–51.
Edmondson AC. Learning from failure in health care: frequent opportunities, pervasive barriers. BMJ Qual Saf. 2004;13 Suppl 2:ii3-ii9.
Merkebu J, Battistone M, McMains K, McOwen K, Witkop C, Konopasky A, Durning SJ. Situativity: a family of social cognitive theories for understanding clinical reasoning and diagnostic error. Diagnosis. 2020;7:169–76.
Ogdie AR, Reilly JB, Pang WG, Keddem S, Barg FK, Von Feldt JM, Myers JS. Seen through their eyes: residents’ reflections on the cognitive and contextual components of diagnostic errors in medicine. Acad Med. 2012;87:1361–7.
Berman NB, Durning SJ, Fischer MR, Huwendiek S, Triola MM. The role for virtual patients in the future of medical education. Acad Med. 2016;91:1217–22.
Plackett R, Kassianos AP, Mylan S, Kambouri M, Raine R, Sheringham J. The effectiveness of using virtual patient educational tools to improve medical students’ clinical reasoning skills: a systematic review. BMC Med Educ. 2022. https://doi.org/10.1186/s12909-022-03410-x .
Download references
Acknowledgements
We want to thank all participants of the interviews and survey who took their time to contribute to this study despite the ongoing pandemic in 2020. Furthermore, we thank the members of the DID-ACT project team who supported collection and analysis of survey and interview data.
The views expressed herein are those of the authors and not necessarily those of the Department of Defense, the Uniformed Services University or other Federal Agencies.
This study was partially supported by the Erasmus + Knowledge Alliance DID-ACT (612454-EPP-1–2019-1-DE-EPPKA2-KA).
Author information
Authors and affiliations.
Institute for Medical Education, Department for Assessment and Evaluation, University of Bern, Bern, Switzerland
F. L Wagner & S. Huwendiek
Center of Innovative Medical Education, Department of Medical Education, Jagiellonian University, Kraków, Poland
Faculty of Medicine, Department of Bioinformatics and Telemedicine, Jagiellonian University, Kraków, Poland
A. A Kononowicz
School of Health, Care and Social Welfare, Mälardalen University, Västerås, Sweden
Faculty of Medicine and Health, School of Health Sciences, Örebro University, Örebro, Sweden
Uniformed Services University of the Health Sciences, Bethesda, MD, USA
S. J Durning
Institute of Medical Education, University Hospital, LMU Munich, Munich, Germany
You can also search for this author in PubMed Google Scholar
Contributions
FW and SH wrote the first draft of the manuscript. All authors critically revised the manu-script in several rounds and approved the final manuscript.
Corresponding author
Correspondence to F. L Wagner .
Ethics declarations
This type of study was regarded as exempt from formal ethical approval according to the regulations of the Bern Ethics Committee (‘Kantonale Ethikkommission Bern’, decision Req-2020–00074). All participants voluntarily participated and provided informed consent before taking part in this study.
Consent for publication
All authors consent to publication of this manuscript.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wagner, F., Sudacka, M., Kononowicz, A. et al. Current status and ongoing needs for the teaching and assessment of clinical reasoning – an international mixed-methods study from the students` and teachers` perspective. BMC Med Educ 24 , 622 (2024). https://doi.org/10.1186/s12909-024-05518-8
Download citation
Received : 16 January 2024
Accepted : 06 May 2024
Published : 05 June 2024
DOI : https://doi.org/10.1186/s12909-024-05518-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical reasoning
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Inpatient case characteristics of SGLT2 inhibitor-associated diabetic ketoacidosis: a retrospective study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0009-0008-4991-7190 Zhongpei Yang 1 ,
- Weixia Zhang 2 ,
- Hefeng Chen 2 ,
- Qianwen Peng 2
- 1 Department of Pharmacy , The People's Hospital of QianNan , Duyun , China
- 2 Department of Pharmacy , Shanghai Jiao Tong University Medical School Affiliated Ruijin Hospital , Shanghai , China
- Correspondence to Dr Weixia Zhang, Department of Pharmacy, Shanghai Jiao Tong University Medical School Affiliated Ruijin Hospital, Shanghai, China; wxzhang2001{at}163.com
Objectives Diabetic ketoacidosis (DKA) is a serious complication in patients treated with sodium-glucose co-transporter 2 inhibitors (SGLT2i). The aim of this study was to investigate the relationship between SGLT2i and the risk of DKA, and to identify high-risk groups and characteristics that should be emphasised.
Methods A retrospective case series study was conducted to collect medical records of inpatients diagnosed with DKA and using SGLT2i before the onset of the disease from September 2022 to September 2023 in a tertiary hospital in Shanghai. Cases that met the inclusion criteria were retrieved through the electronic medical record system. Information was collected to compare the risk of DKA in patients with different characteristics.
Results A total of 21 patients (12 men and 9 women) met the criteria for SGLT2i-associated DKA. The mean diabetes duration was 10.4 years, with 47.6% (10/21) of patients diagnosed with euglycaemic DKA. The drug treatment regimen most commonly used was the combination of SGLT2i and metformin, representing 52.4% (11/21) of cases. The most common clinical symptoms were nausea, vomiting, abdominal pain and malaise. Common predisposing factors were acute infections, acute pancreatitis (predominantly hyperlipidaemic type), dietary inappropriateness, acute cardiovascular and cerebrovascular events and surgery. 71.4% of patients (15/21) had multiple risk factors.
Conclusion The use of SGLT2i in diabetic patients is associated with an increased risk of DKA, particularly in the presence of predisposing factors such as infection. Furthermore, long diabetes duration, decreased pancreatic β-cell function and the combined use of metformin may also contribute to the risk of DKA in patients treated with SGLT2i. The findings of this study provide valuable insights for better identification and management of DKA risks associated with SGLT2i in clinical practice.
- Diabetes Mellitus
- DRUG-RELATED SIDE EFFECTS AND ADVERSE REACTIONS
- HEALTH SERVICES ADMINISTRATION
- Pharmacovigilance
- Substance-Related Disorders
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
https://doi.org/10.1136/ejhpharm-2024-004124
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Diabetic ketoacidosis (DKA) is a rare adverse drug reaction of sodium-glucose co-transporter 2 inhibitors (SGLT2i), which mostly occurs in people with DKA inducement factors or those who are at high risk for DKA.
With the widespread clinical application of SGLT2i, its potential risks cannot be ignored and it becomes crucial to identify the risk factors for this serious complication.
WHAT THIS STUDY ADDS
Unlike previous studies, our findings help to identify individuals at high risk for SGLT2i-associated DKA and underscore the significance of specific factors.
We observed a significantly increased risk of DKA during acute stressful situations, emphasising the need for doctors to carefully consider a patient’s stress level when prescribing SGLT2i.
Longstanding diabetes, decreased pancreatic β-cell function and the concurrent use of metformin may also heighten the risk of DKA in SGLT2i users.
HOW THIS STUDY MIGHT AFFECT RESEARCH PRACTICE OR POLICY
Our study serves as a warning signal for the potential risk of SGLT2i-associated DKA and warrants further validation through large-scale randomised controlled trials.
Introduction
Diabetic ketoacidosis (DKA) is a serious complication of diabetes mellitus that has been linked to the use of sodium-glucose co-transporter 2 inhibitors (SGLT2i). 1 The latest research shows that the estimated incidence of DKA due to SGLT2i ranges from 0.1% to 0.6%. 2 3 Although this incidence is relatively low, with the increasing popularity of SGLT2 inhibitors its potential risk cannot be overlooked.
Evidence from clinical studies has shown that SGLT2i has cardiorenal protective effects independent of glucose-lowering effects, 4 making it an important treatment option for diabetes. Consequently, SGLT2i is used in the treatment of type 2 diabetes and has also been approved for use in adults with heart failure and chronic kidney disease. However, as this class of drugs is increasingly used the incidence of DKA may have increased, so identifying risk factors for this serious complication becomes critical.
SGLT2i-associated DKA may occur with normoglycaemia or mild hyperglycaemia (<13.9 mmol/L), known as euglycemic diabetic ketoacidosis (euDKA). 5 This particular type of DKA may be more prevalent in clinical practice, but research on its mechanisms and risk factors is still limited. To better understand the clinical and biochemical parameters characteristic of patients with SGLT2i-associated DKA, our aim is to further identify potential risk factors or danger signals that lead to the development of DKA in SGLT2i-treated patients. This will provide an important reference for safe and rational medication administration and monitoring, and will help to reduce the risk of DKA and ensure the safety of patients’ medication.
Study design and patient sources
The medical records of hospitalised patients with DKA at a tertiary hospital in Shanghai between September 2022 and September 2023 were retrieved through the electronic medical record system. During the screening process we focused on patients who used SGLT2i prior to the onset of DKA and selected them as study subjects.
Inclusion criteria
All patients diagnosed with DKA and prior use of SGLT2i were eligible for inclusion. The diagnosis of DKA was based on the following criteria: 1 (1) elevated blood ketone bodies (≥3 mmol/L) or positive urine glucose and ketone bodies (++ or more); (2) reduced blood pH (pH <7.3) and/or carbon dioxide binding capacity (HCO3 − <18 mmol/L). Given that patients with SGLT2i-induced ketoacidosis may have normal or mildly elevated blood glucose, we further categorised the patients into those with glucose <13.9 mmol/L (euglycaemic DKA, euDKA) or ≥13.9 mmol/L (hyperglycaemic DKA, hDKA).
Exclusion criteria
Patients treated for DKA but not using SGLT2i and those with a non-initial diagnosis of DKA and incomplete test data related to the diagnosis of DKA were not considered eligible for inclusion in the trial.
The research process and overview are summarised in figure 1 .
- Download figure
- Open in new tab
- Download powerpoint
Research process and overview of the trial. DKA, diabetic ketoacidosis; SGLT2i, sodium-glucose co-transporter 2 inhibitors.
Data extraction
We collected various characteristics of the identified cases including age, gender, body mass index (BMI), type of diabetes, history of diabetes and history of DKA. Additionally, we recorded details regarding the purpose for the medication, type of medication, comorbidities, first symptoms of DKA and known predisposing factors. We also obtained data from laboratory tests such as blood glucose, C-peptide level, glycated haemoglobin, blood pH, bicarbonate value, β-hydroxybutyric acid, urinary ketones, urinary glucose, urea nitrogen, blood creatinine and glomerular filtration rate.
Statistical analysis
IBM SPSS 23.0 software was used to compile and analyse the collected data. Measurement information was expressed as mean±SD and the independent samples t-test was used to compare the two groups of normally distributed measurement data. For non-normally distributed measurements, the rank sum test was used for comparison. For categorical information, we presented absolute values and percentages (%) and used the χ 2 test to compare the two groups of categorical data. All statistical analyses were conducted using α=0.05 as the statistical significance level. We used descriptive and summary statistics to provide a comprehensive overview of the clinical and biochemical parameters of the study cohort.
Demographic and clinical characteristics
A total of 21 patients were included in the study. Of these, 20 patients were diagnosed with type 2 diabetes mellitus and one patient with occult adult autoimmune diabetes mellitus at the time of admission. Among them, one patient was discharged with a revised diagnosis of type 1 diabetes and one patient had type 2 diabetes mellitus complicated by cardiac insufficiency. The purpose of the medication was to lower the blood glucose levels and also to improve the prognosis of heart failure. Of the 21 patients, 47.6% (10/21) had euDKA and 52.4% (11/21) had hDKA. There were no significant differences between the two groups in terms of baseline data such as age, sex, BMI and medication history ( table 1 ).
- View inline
Characteristics of the study sample
SGLT2i medication use
Eighteen of the 21 patients had dapagliflozin as their antidiabetic agent, two had empagliflozin and one patient used canagliflozin. Of these, three patients used SGLT2i as monotherapy for glucose lowering while 18 patients had multi-drug combination therapy. Among the patients who received multi-drug combination therapy, the proportion of dual and multi-drug combination therapy based on SGLT2i combined with insulin or metformin was 76.2% (16/21); the proportion of SGLT2i combined with metformin-based regimens was the highest, accounting for 52.4% (11/21). The specific distribution of patient medication schemes is shown in table 2 .
Distribution of patients’ hypoglycaemic treatment regimens
Laboratory indicators
The average blood glucose concentration of the 21 patients at the time of consultation was 17.0 mmol/L. Notably, the average blood glucose concentration in the euDKA group was 10.3 mmol/L while that of the hDKA group was 23.2 mmol/L. The average HbA1c of the euDKA group was significantly lower than that of the hDKA group; however, due to the relatively small sample size, this difference did not reach statistical significance.
Except for the statistical difference in the blood glucose level at the time of treatment, no statistical difference was found in other biochemical indicators between the two groups (see table 3 for further details). Among the 21 patients, eight patients underwent testing for C-peptide levels. Four patients had significantly decreased C-peptide levels with a decrease rate of 50.0% (4/8). In the euDKA group, 66.7% of patients (2/3) had decreased C-peptide levels whereas, in the hDKA group, 40.0% of patients (2/5) had decreased C-peptide levels.
Comparison of biochemical indicators between the euDKA and hDKA groups
Clinical presentation
The initial symptoms observed in the 21 patients primarily involved the digestive symptoms, accounting for 71.2% (42/59) of all reported symptoms. These symptoms predominantly induced nausea, vomiting and abdominal pain. This was followed by the emergence of systemic reactions, most notable of which was malaise. The frequency distribution of these symptoms is shown in table 4 .
Frequency distribution of initial symptoms in patients with diabetic ketoacidosis
Predisposing factor distribution
Among the known predisposing factors, 1 in three of the 21 patients these were induced by SGLT2i use only. The remaining 18 patients presented with various concurrent predisposing factors, mainly including acute infection in 54.5% (12/22), acute pancreatitis in 18.2% (4/22) and inappropriate diet in 9.1% (2/22). Of these, inadequate dietary intake and excessive dietary intake each accounted for one case. Other predisposing factors included acute cardiac infarction (one case), acute cerebral infarction (one case), sudden interruption of insulin therapy (one case) and surgery (one case). Notably, all four cases of acute pancreatitis were associated with hyperlipidaemia. By counting the number of predisposing factors, we found that 71.4% (15/21) of the patients had two concurrent predisposing factors. The distribution of the number of combined predisposing factors among the 21 patients is shown in table 5 .
Distribution of risk factor numbers in patients with DKA
DKA is a severe metabolic disorder that is primarily caused by inadequate insulin levels and inappropriately elevated glucagon levels. 1 SGLT2i, a novel hypoglycaemic agent, facilitates glycaemic control by inhibiting renal glucose reabsorption. However, it can also increase the risk of developing DKA through various mechanisms. 6
In our study all 21 patients had a comorbidity of diabetes mellitus, with no patients found to have no history of diabetes mellitus. Of these patients, 20 were diagnosed with type 2 diabetes mellitus and one patient with occult adult autoimmune diabetes mellitus at the time of admission, Among them, one was later diagnosed with type 1 diabetes mellitus following further investigations. Eight patients underwent C-peptide level testing to assess their pancreatic islet function. The results showed that C-peptide levels were significantly reduced in four patients, accounting for 19.1% (4/21) of the total. This suggests that the development of DKA is associated with patients with significantly reduced pancreatic islet function. The US Food and Drug Administration estimated that one additional case of ketoacidosis will occur for every 26 patients with type 1 diabetes receiving SGLT2i treatment (~4000 cases per year for every 100 000 patients under treatment). 7 The risk is greater in patients with type 1 diabetes than in those with type 2 diabetes. 7 To date, no SGLT2i has been approved for the treatment of type 1 diabetes in China. Real-world off-label use of SGLT2i in patients with type 1 diabetes also showed that the risk for DKA was notable. 8 It is worth noting that 13 patients in our study did not undergo antibody and C-peptide level testing to assess pancreatic β-cell function. These patients may have ketosis-prone diabetes such as undiagnosed type 1 diabetes or latent autoimmune diabetes in adults. This suggests that accurate classification of diabetes mellitus and assessment of islet function before medication may be beneficial for the prevention of SGLT2i-related DKA. Furthermore, it has also been found that, as the duration of type 2 diabetes increases, the insulin secretion reserve function may be impaired, leading to an increased risk of DKA. 9 The study also showed that type 2 diabetes with a disease duration of ≥7.625 years is a risk factor for DKA associated with the use of dagliflozin. 10 In our study, the mean duration of diabetes in the patients was 10.4 years, which is consistent with related studies. This suggests that a long duration of diabetes may be a risk factor for the development of DKA.
Moreover, the concurrent use of metformin may increase the risk of DKA induced by SGLT2i. A study conducted by Donnan et al showed that the combination of metformin and SGLT2i may increase the risk of metabolic acidosis. 11 A meta-analysis of patients with SGLT2i-associated DKA showed that euDKA is common in middle-aged women with type 2 diabetes who are taking SGLT2 inhibitors and metformin. 12 Additionally recent studies have shown that the concurrent use of acarbose and metformin is an independent risk factor for DK/DKA by dagliflozin. 13 Therefore, clinicians should carefully evaluate the patient’s medication risk when prescribing metformin in combination with SGLT2i to patients with type 2 diabetes.
The distribution of the number of risk factors for DKA shows that the use of SGLT2i in diabetic patients entails a risk of DKA, particularly in the presence of one common risk factor such as acute infection, pancreatitis, poor diet, insulin dosage reduction, cardiovascular or cerebrovascular events or surgery. Surgery is a major precipitating factor for SGLT2i-associated DKA. 1 To lessen the risk of developing ketoacidosis after surgery, the US Food and Drugs Administration has approved changes to the prescribing information for SGLT2i medicines. Healthcare professionals should consider stopping canagliflozin, dapagliflozin and empagliflozin at least 3 days before scheduled surgery and ertugliflozin at least 4 days before scheduled surgery. 14 According to the latest expert consensus in the Asia-Pacific region states, 15 SGLT2i should be immediately discontinued in emergency surgical procedures or stressful situations (eg, inadequate caloric intake, severe infection, volume depletion, critical illness). Preoperative SGLT2i exposure was associated with increased risks of postoperative DKA (incidence 6.40/1000 person-years; incidence rate ratio (IRR) 6.33, 95% CI 5.57 to 7.18; p<0.001). 16 Risk factors of SGLT2i-associated postoperative DKA included emergency operation (IRR 24.56, 95% CI 7.42 to 81.24; p<0.001). 16 In our study, one patient did not discontinue SGLT2i before emergency surgery and developed ketoacidosis after surgery. This case suggests that the risk of DKA should be fully considered when using SGLT2i in diabetic patients, especially in surgical or stressful situations, in order to reduce the risk of serious complications.
The main limitation of this study is the relatively small sample size, which restricts the generalisability of the finddings. Additionally, the absence of a control group or comparisons with other glucose-lowering medications prevented us from assessing the relative risk of SGLT2i compared with other medications. It is important to note that DKA can be caused by various factors, with SGLT2i being only one of them. Therefore, our study serves as a warning signal for the potential risk of SGLT2i-associated DKA and warrants further validation through large-scale randomised controlled trials. Nevertheless, our research offers valuable insights. Unlike previous studies, our data help to identify individuals at high risk for SGLT2i-associated DKA and underscore the significance of specific factors. For instance, we observed a significantly increased risk of DKA during acute stressful situations, emphasising the need for doctors to carefully consider a patient’s stress level when prescribing SGLT2i. Moreover, longstanding diabetes, decreased pancreatic β-cell function and the concurrent use of metformin may also heighten the risk of DKA in SGLT2i users. Consequently, accurate diabetes typing and pancreatic islet function assessments are essential in identifying individuals prone to ketosis before prescribing SGLT2i. Consideration should be given to discontinuing SGLT2i if patients have additional risk factors. Furthermore, nausea, vomiting, abdominal pain and malaise are common symptoms of DKA but lack specificity. Therefore, when these symptoms occur in SGLT2i users, they should be promptly reported to healthcare providers to rule out the possibility of DKA. To minimise medication-related risks, physicians and pharmacists should enhance medication education and monitoring for patients using SGLT2i.
Despite the limitations of this study, our findings offer valuable insights into the identification and management of DKA risk associated with SGLT2i in clinical practice. Future research should aim to validate our findings by increasing the sample size, establishing a control group and comparing with other glucose-lowering medications. This will provide stronger evidence to support clinical decision-making and ultimately improve patient outcomes.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by The The Ethics Committee of Ruijin Hospital affiliated with Shanghai Jiao Tong University School of Medicine approved this study (approval number: 022313). The need for informed consent was waived by the Ethics Committee.
- Chinese Medical Association Diabetes Branch
- Dawwas GK ,
- Hennessy S , et al
- Heerspink HJL ,
- Stefánsson BV ,
- Correa-Rotter R , et al
- Koyfman A , et al
- Taylor SI ,
- Rother KI , et al
- Horgan C , et al
- Fadini GP ,
- Bonora BM ,
- Zhang Y , et al
- Singh S , et al
- Wu Q , et al
- US Food and Drug Administration
- Matawaran BJ , et al
- Au ICH , et al
EAHP Statement 5: Patient Safety and Quality Assurance.
Contributors ZY conceived the idea and wrote the original draft of the manuscript. ZY, WZ, HC and QP were responsible for data acquisition and analysis. All authors discussed the data and commented on the manuscript. ZY and WZ revised and edited the manuscript. WZ is guarantor.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:
- Open access
- Published: 29 May 2024
Using 2% PVPI topical solution for serial intravitreous injections and ocular surface findings: a case control study
- José Henrique Casemiro 1 ,
- Ana Paula Miyagusko Taba Oguido 2 &
- Antonio Marcelo Barbante Casella 3
International Journal of Retina and Vitreous volume 10 , Article number: 41 ( 2024 ) Cite this article
92 Accesses
Metrics details
The use of povidone-iodine for ocular surface asepsis is widespread for intravitreal injections. They became frequent procedures, leading to serial exposure of patients’ eyes to iodinated solutions. In this study, we investigate the changes in the ocular surface in patients submitted to repeated use of povidine for intravitreal injection of anti-VEGF asepsis, analyzing Ocular Surface Disease Index, non-invasive break up time, blinking quality, lipid layer, meniscus height and osmolarity.
This case-control study included 34 individuals (68 eyes), 14 males, 20 females aged 48 to 94. Inclusion criteria were individuals who received application of 2% povidone-iodine eyedrops for intravitreal injections treatment with the non-treated contralateral eye used as control. Ocular surface examinations were performed at a single occasion. A pre-intravitreal injection asepsis protocol with povidone-iodine was applied. All statistical analysis was performed using the STATA® 18.0 Software and a p-value = 0.05 was considered as the statistical significance value in all tests.
The median number of IVIs in treated eyes was 12 (range 6–20). The results in treated eyes compared with untreated eyes were respectively : median OSDI 16 (IQR 6–39) and 12.5 (IQR 8–39) ( p = 0.380); mean NIBUT 10.30 (SD ± 2.62) and 10.78 (SD ± 2.92) ( s, p = 0.476); median blinking quality 100 (IQR 100) and 100 (IQR 100 ) (%, p = 0.188); median lipid layer 87 (IQR 77–90) and 86 (IQR 74–100) (nm, p = 0.451); median meniscus height 0.22 (IQR 0.19-0,31) and 0.24 (IQR 0.20–0.27) (mm, p = 0.862), median Meibomian gland atrophy 33 (IQR 24–45) and 31.5 (IQR 25–39) (%, p = 0.524); and mean osmolarity 306.6 (SD ± 21.13) and 313.8 (SD ± 29) (mOsm, p = 0.297). There was no statistically significant relationship between the repetitive use of 2% iodinated solution and signs or symptoms compatible with dry eye syndrome in this group of patients.
Conclusions
The findings suggest that 2% povidone iodine is a safe and efficacious agent for ocular surface antisepsis during intravitreal injections, not leading to substantial ocular surface modifications. This conclusion supports the continued use of povidone iodine in routine ophthalmic procedures without increased risk of inducing dry eye syndrome.
The use of povidone iodine (PVPI) for ocular surface asepsis is widespread, both for surgical procedures and intravitreal injections [ 1 , 2 , 3 , 4 , 5 ]. Surgeries for cataracts, glaucoma, and intravitreal injections have become common and frequent procedures in ophthalmology, leading to the serial exposure of patients’ eyes to iodine solutions [ 5 , 6 , 7 , 8 , 9 , 10 ]. These changes are directly associated with dry eye syndrome [ 11 , 12 ].
In particular, studies have demonstrated that intravitreal injections used to treat diabetic macular edema or age-related macular degeneration result in significant changes in the ocular surface, leading to dry eye syndrome and damage to homeostasis of the ocular surface [ 5 , 11 , 13 , 14 ].
Dry eye syndrome is a multifactorial disease of the ocular surface characterized by the loss of tear film homeostasis, hyperosmolarity, inflammation, damage and neurosensory abnormalities [ 11 , 15 , 16 , 17 , 18 ]. Its etiology is variable, ranging from nonspecific inflammation of the ocular surface to direct chemical or physical aggression, infections, and autoimmune diseases [ 11 , 12 , 15 , 19 ].
In addition to the most common symptoms, burning sensation, itching, speck, eye redness, excess tearing reflex, brightness sensitivity, and quality of vision loss are also frequent findings that affect efficiency at work and the quality of life of patients [ 11 , 12 , 15 , 19 , 20 ].
This study aimed to observe changes in the ocular surface and tear film due the serial use of 2% PVPI, the gold standard drug for asepsis of the ocular surface. As it is well known that pre-injection antisepsis of the ocular surface with PVPI has a toxic effect on the corneal epithelium, the aim is to identify changes in the tear film and ocular surface and avoid serious problem like dry eye syndrome [ 11 , 12 , 21 , 22 ].
A case-control study was conducted at the Ophthalmology and Psicology Clinic (APMTO MD) in Londrina, Paraná. The patients were recruited from the Retina and Vitreous Institute (AMBC MD) in Londrina, Paraná. The study included 34 individuals (68 eyes). 14 males, 20 females, aged 48 to 94 years. All participants signed the informed consent form, which allowed their participation in the study. Inclusion criteria were individuals who received application of 2% PVPI eyedrops for anti-VEGF IVIs treatment with the contralateral eye used as control, that had not been treated with any topical medication during the same period of applications and good comprehension of the Ocular Questionnaire Surface Disease Index (OSDI). Exclusion criteria were patients who could not understand the OSDI questionnaire; patients using antidepressant medicine, diuretics, sympathomimetics, eye drops for glaucoma, or eye lubricants; people with allergies to iodine; unfavorable clinical conditions to undergo the examination procedures for the study; inappropriate test quantity and quality; unsatisfactory images or unsatisfactory and inadequate data.
The study was approved by the Ethics and Research Committee Involving Human Beings of the State University of Londrina by N. 5.300.176.
The individuals underwent directed clinical and ophthalmological analysis, received explanations about the study, used their data, and signed consent forms. All clinical measures were performed using the IDRA equipment (SBSSISTEMI, Orbasano, Torino, Italy), at which time the OSDI questionnaire was also applied and tear osmolarity was collected using the I-PEN ® (I-MED PHARMA INC. Dollard-des-Ormeaux, QC, Canada). All examinations and administration of the questionnaire were performed by the same professional. No drops or medications that could cause changes in any subsequent measurements were used.
The variables analyzed were age, sex, date of the last PVPI application, number of PVPI applications, OSDI questionnaire, tear osmolarity, NBUT, tear film interferometry, tear meniscus height, percentage of meibomian gland loss, and blink quality. The sequence of procedures obeyed the following order: Explanation to the subject regarding the exams and questionnaire to which he would be submitted, guidance to the patient not to identify in any way the eye being treated and the eye not treated during data collection, nor during the questionnaire OSDI; patient positioning in the IDRA® equipment; capture of blinking quality video images; capture of tear film interferometry; capture of images to measure the height of the tear meniscus and immediate measurement; capture of tear film (NBUT); image capture for the percentage of meibomian gland loss by everting the lower eyelid with a cotton swab; positioning the patient outside the IDRA equipment; application of the I-PEN® electrode to capture tear osmolarity in the lower conjunctiva, first in the right eye, and subsequently in the left eye; application of the OSDI questionnaire.
All statistical analyses were performed using STATA® 18.0 Software and p-values ≤ 0.05 indicated statistical significance.
The Shapiro-Wilk test was used to verify data normality. Data that did not follow a normal distribution were analyzed using the Wilcoxon rank-sum test and were described as means and as medians and interquartile ranges. Data that showed normality were analyzed using the Student’s T test and presented as means and standard deviations. Descriptive, quantitative, and multivariate analyses compared treated (case) and untreated (control) eyes.
The average number of IVIs in treated eyes was 12 (range 6–20). The results in treated eyes compared with untreated eyes were respectively: median OSDI 16 (IQR 6–39) and 12.5 (IQR 8–39) ( p = 0.380); mean NIBUT 10.30 (SD ± 2,62) and 10.78 (SD ± 2.92) ( s, p = 0.476); median blinking quality 100 (IQR 100) and 100 (IQR 100 ) (%, p = 0.188); median lipid layer 87 (IQR 77–90) and 86 (IQR 74–100) (nm, p = 0.451); median meniscus height 0,22 (IQR 0.19–0.31) and 0.24 (IQR 0.20–0.27) (mm, p = 0.862), median Meibomian gland athrophy 33 (IQR 24–45) and 31.5 (IQR 25–39) (%, p = 0.524); and mean osmolarity 306.6 (SD ± 21.13) and 313.8 (SD ± 29) (mOsm, p = 0.297).). The results revealed that the use of 2% PVPI did not affect the analyzed variables in a statistically significant way. All data is summarized on Table 1 .
These results are disposable on fig 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 and 9 as annexed.
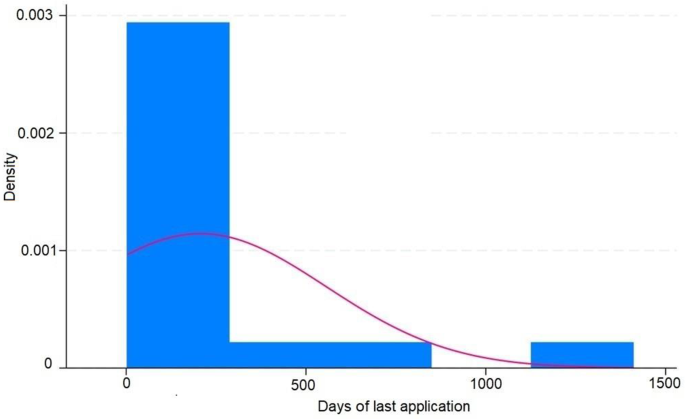
Histogram showing the days of last application of IVIS ( intravitreal injections ) in treated eyes and the density showing the proportion of eyes in each period of time
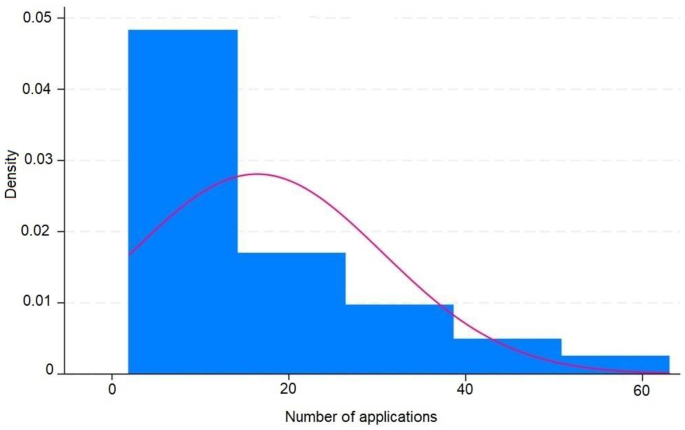
Histogram showing the number of application ov IVIS ( intravitreal injections ) in treated eyes and the density showing the proportion of eyes in each amount of number of applications
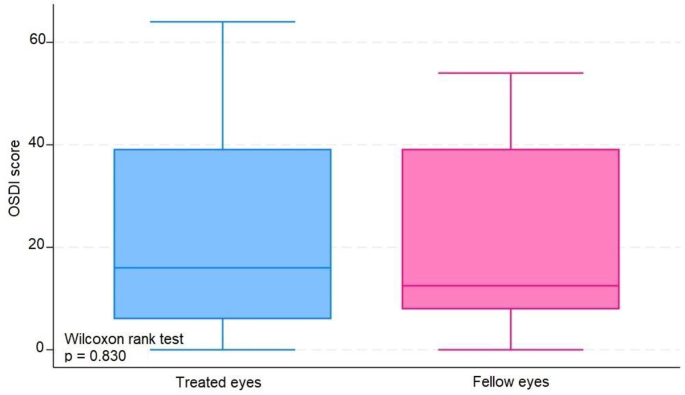
Blue box plot showing score OSDI ( Ocular Surface Disease Index ) in treated eyes comparing with pink box plot showing score OSDI in fellow eyes
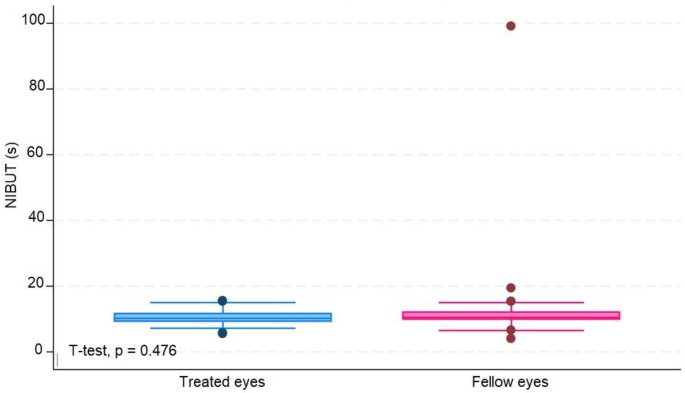
Blue box plot showing NIBUT ( non invasive break up time ) in seconds in treated eyes comparing with pink box plot showing NIBUT in seconds in fellow eyes
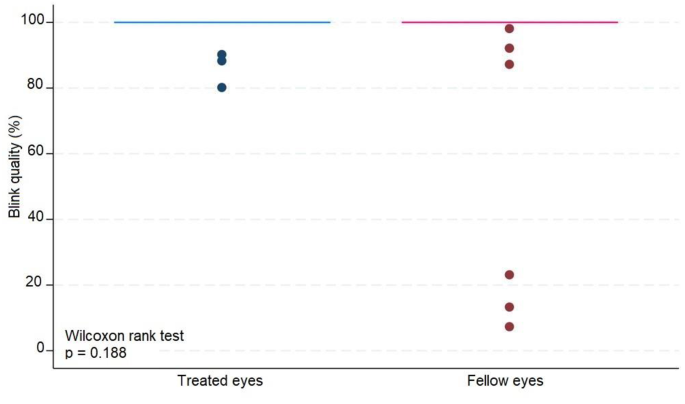
Blue box plot showing blink quality in treated eyes comparing with pink box plot showing blink quality in fellow eyes
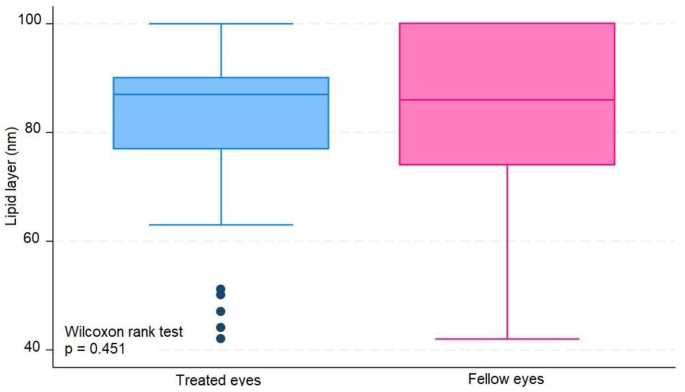
Blue box plot showing lipid layer in treated eyes comparing with pink box plot showing lipid layer in fellow eyes
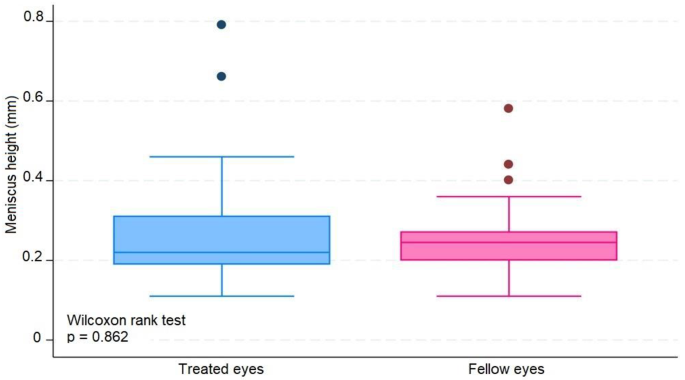
Blue box plot showing meniscus height in milimeters in treated eyes comparing with pink box plot showing meniscus height in milimeters in fellow eyes
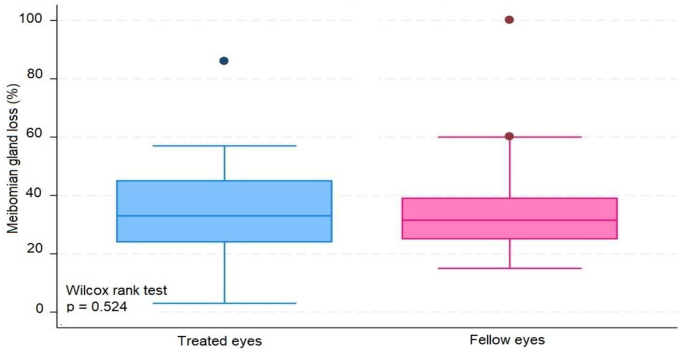
Blue box plot showing Meibomian gland loss in treated eyes comparing with pink box plot showing Meibomian gland loss in fellow eyes
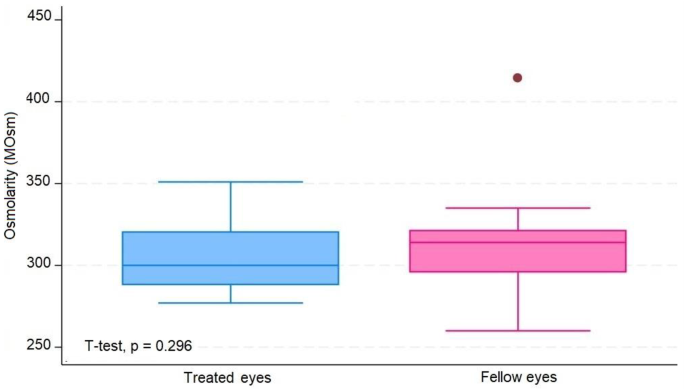
Blue box plot showing tear osmolarity in miliosmoles in treated eyes comparing with pink box plot showing osmolarity in miliosmoles in fellow eyes
Through multivariate analysis, we obtained some interesting outcomes as follows:
When controlling for NIBUT, meibomian gland atrophy, number of applications, and days of the last application according to treatment, sex was an important variable in explaining the variability in the OSDI score (coef = 15.63 | p-value = 0.003). On average, controlling for the abovementioned variables, being female contributed to an increase in the OSDI to 15.63 points.
After controlling for meniscus height and age according to treatment, tear osmolarity contributed significantly to variability in the lipid layer (coef = -0.266, p = 0.004). In this sense, the addition of one unit in tear osmolarity led to a -0.266 drop in the lipid layer.
After controlling for meniscus height, OSDI, days since the last application, age, and sex according to the treatment, these factors contributed significantly to the variability in the lipid layer [(coef = 0.562 | p-value = 0.004) (coef = − 5.622 | p-value = 0.048)]. In this sense, the addition of one year of age led to a decrease of -0.562 on average. For the same treatment group, female sex led to a decrease of -5,622.
Age, lipid layer, meniscus height, sex according to treatment, age according to treatment, and sex were important factors for explaining the variability in tear osmolarity.
We noticed that a greater age correlated with lower tear osmolarity. However, being in the treated group reduced the decrease in tear osmolarity with advancing age.
Being female implied higher tear osmolarity. However, the increase in tear osmolarity was smaller in the treated group.
A greater height of the lipid layer and meniscus correlated with lower tear osmolarity.
The present study showed that the use of topical PVPI at 2% did not cause significant damage to the ocular surface when the findings of the ocular surface and tear film analyses were used.
Our results contradict some existing data indicating the toxicity of long-term iodine use on the ocular surface; we found two statistically relevant results that the application of iodine may improve the stability of the tear film in the elderly and women, since the eyes in older individuals and female patients that received iodine showed a smaller increase in tear osmolarity [ 4 , 14 , 23 , 24 ].
Moreover, the results of this study corroborated some hypotheses that the use of PVPI could be positive in some dry eye disease diagnostic features, such as the improvement of the tear film meniscus height and the decrease of the tear film osmolarity [ 25 , 26 ].
A localized anti-inflammatory surface effect of the anti-VEGF agent used in intravitreous injections should be considered and assessed in further studies [ 22 , 25 ].
The literature review also shows that there was an improvement in the tear function of some patients who used iodine in ocular asepsis [ 25 , 26 , 27 ], perhaps due to an antimicrobial action preventing the proliferation of bacterial flora that could produce harmful enzymes or cause meibomitis and blepharitis [ 25 , 26 , 28 ].
The cell regeneration mechanism might have satisfactorily recomposed the ocular surface or the tear homeostasis might have compensates for the damage caused by iodine in the cells in question; furthermore, these are just hypotheses.
We also determined that the risk factors for dry eye disease, age and female sex [ 10 , 16 , 29 , 30 ], were associated with the observed clinical data: greater ages lower the height of the tear meniscus, the greater the tear osmolarity, and the smaller the lipid layer of the tear film. The female sex was also associated with higher OSDI scores and fewer tear film lipid layers.
Regardless of the cause or consequence, the osmolarity and lipid layer of the tear film were inversely proportional.
Through multivariate analysis, we determined that the risk factors for dry eye syndrome, age, and female sex correlated with worse results in the tear meniscus measurement tests, OSDI questionnaire, and tear film interferometry, corroborating the literature implicating them as risk factors for dry eye disease [ 20 , 30 , 31 ].
Moreover, due to the sample size, false negatives, or simply because in practice, iodine in the amount and frequency used does not lead to histological damage that may reflect functional changes. The results did not discourage the use of iodine for ocular asepsis but also did not indicate its use for protocols with higher concentrations or more applications than those used in current protocols.
The strengths of the study are as follows: the same patient was the control and treated group, avoiding any environmental or medical bias. The number of injections administered was higher than that reported in other studies. No drops were used during the examination to avoid artificial changes to the tear film.
The limitations of this study were as follows: the study had a small sample size of 34 patients, resulting in 68 eyes being analyzed, which may have caused an analysis bias when using these data in the general population. We must remember that the analyzed population was from southern Brazil and had mostly descended from Italian, German, Spanish, and Portuguese immigrants; therefore, these data may only reflect the specific epidemiology of this population. The meibomian glands analyzed were located in the inferior tarsus.
The use of iodine on the ocular surface was not significantly associated with any of the evaluated parameters. There were no statistically significant correlations between the tests applied to the case eyes. The current study indicates that the application of 2% topical povidone-iodine (PVPI) does not inflict significant damage to the ocular surface, as evidenced by the analyses of the ocular surface and tear film. Notable strengths of this study include the use of the same patient as both the control and the treated subject, which minimizes potential biases from environmental or medical factors. Additionally, the absence of any artificial agents during the examination ensures that the tear film remains unaltered.
Contrary to previous concerns regarding the long-term toxicity of iodine on the ocular surface, our findings suggest potential benefits of iodine application in stabilizing the tear film, particularly in older individuals and female patients. This is supported by a smaller increase in tear osmolarity in these groups following iodine application. Furthermore, the study corroborates hypotheses that PVPI may positively affect certain Dry Eye Disease diagnostic features, such as improved tear film meniscus height and reduced tear film osmolarity.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Povidine or polyvinylpyrrolidone-iodine
- Intravitreal injections
Vascular endothelial growth factor
Ocular Surface Disease Index
Non invasive break up time
Blink quality
Lipid layer
Standard deviation
Interquartile range
Oakley C, Allen P, Hooshmand J, Vote BJT. PAIN AND ANTISEPSIS AFTER OCULAR ADMINISTRATION OF POVIDONE-IODINE VERSUS CHLORHEXIDINE. Retina. 2018;38:2064–6.
Article CAS PubMed Google Scholar
Fukuda M, Shibata S, Shibata N, Fujita N, Miyashita H, Tanimura N, et al. Polyvinyl alcohol-iodine induced corneal epithelial injury in vivo and its protection by topical rebamipide treatment. PLoS ONE. 2018;13:e0208198.
Article PubMed PubMed Central Google Scholar
Grzybowski A, Brona P. Povidone-iodine is still a premium antiseptic measure in ocular surgery. Acta Ophthalmol. 2017;95.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C-K, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Article PubMed Google Scholar
Craig JP, Nelson JD, Azar DT, Belmonte C, Bron AJ, Chauhan SK, et al. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017;15:802–12.
Moss SE. Prevalence of and risk factors for Dry Eye Syndrome. Arch Ophthalmol. 2000;118:1264.
Jiang X, Wang Y, Lv H, Liu Y, Zhang M, Li X. Efficacy of intra-meibomian gland injection of the anti-VEGF agent bevacizumab for the treatment of meibomian gland dysfunction with lid-margin vascularity. Drug Des Devel Ther. 2018;12:1269–79.
Article CAS PubMed PubMed Central Google Scholar
Kim S, Ahn Y, Lee Y, Kim H. Toxicity of povidone-iodine to the ocular surface of rabbits. BMC Ophthalmol. 2020;20:359.
Malmin A, Thomseth VM, Førland PT, Khan AZ, Hetland HB, Chen X, et al. Associations between serial Intravitreal injections and Dry Eye. Ophthalmology. 2023;130:509–15.
Audelan T, Legrand M, M’Garrech M, Best A-L, Barreau E, Labetoulle M, et al. Vieillissement de la surface oculaire : physiopathologie et conséquences pratiques pour la prise en charge. J Fr Ophtalmol. 2018;41:262–70.
Kanclerz P, Myers WG. Potential substitutes for povidone-iodine in ocular surgery. Eye. 2021;35:2657–9.
Reibaldi M, Avitabile T, Bandello F, Longo A, Bonfiglio V, Russo A, et al. The effectiveness of 0.6% povidone Iodine Eye drops in reducing the Conjunctival bacterial load and needle contamination in patients undergoing Anti-VEGF intravitreal injection: a prospective, randomized study. J Clin Med. 2019;8:1031.
Han SB. Prevalence of Dry Eye Disease in an Elderly Korean Population. Arch Ophthalmol. 2011;129:633.
Silas MR, Schroeder RM, Thomson RB, Myers WG. Optimizing the antisepsis protocol: effectiveness of 3 povidone–iodine 1.0% applications versus a single application of povidone–iodine 5.0%. J Cataract Refract Surg. 2017;43:400–4.
Zhang X, Wang L, Zheng Y, Deng L, Huang X. Prevalence of dry eye disease in the elderly. Medicine. 2020;99:e22234.
Donnenfeld ED, Holland EJ, Solomon KD, Fiore J, Gobbo A, Prince J, et al. A Multicenter Randomized Controlled Fellow Eye Trial of pulse-dosed Difluprednate 0.05% Versus Prednisolone acetate 1% in cataract surgery. Am J Ophthalmol. 2011;152:609–e6171.
Grzybowski A, Kanclerz P, Myers WG. The use of povidone–iodine in ophthalmology. Curr Opin Ophthalmol. 2018;29:19–32.
Bramantyo T, Roeslani RD, Andriansjah A, Sitorus RS. The efficacy of 1% Chloramphenicol Eye Ointment Versus 2.5% povidone-iodine Ophthalmic Solution in reducing bacterial colony in Newborn Conjunctivae. Asia-Pacific J Ophthalmol. 2015;4:180–3.
Article CAS Google Scholar
Bourcier T, Acosta MC, Borderie V, Borra´s F, Gallar J, Bury T, et al. Decreased corneal sensitivity in patients with Dry Eye. Invest Opthalmology Visual Sci. 2005;46:2341.
Article Google Scholar
Niederkorn JY, Kaplan HJ. Rationale for Immune Response and the Eye. Immune Response and the Eye. Basel: KARGER; 2007. pp. 1–3.
Google Scholar
Saedon H, Nosek J, Phillips J, Narendran N, Yang YC. Ocular surface effects of repeated application of povidone iodine in patients receiving frequent intravitreal injections. Cutan Ocul Toxicol. 2017;36:343–6.
Beni´tez-del-Castillo JM, Acosta MC, Wassfi MA, Di´az-Valle D, Gegu´ndez JA, Fernandez C et al. Relation between Corneal Innervation with Confocal Microscopy and Corneal Sensitivity with Noncontact Esthesiometry in Patients with Dry Eye. Investigative Opthalmology & Visual Science. 2007;48:173.
Yu K, Asbell PA, Shtein RM, Ying G-S. Dry Eye subtypes in the Dry Eye Assessment and Management (DREAM) study: a latent Profile Analysis. Transl Vis Sci Technol. 2022;11:13.
Dohlman TH, Lertsuwanroj B, D’Amico DJ, Ciralsky JB, Kiss S. Evaluation of signs and symptoms of ocular surface disease after intravitreal injection. Acta Ophthalmol. 2019;97.
Zoukhri D. Effect of inflammation on lacrimal gland function. Exp Eye Res. 2006;82:885–98.
Shelanski HASM. PVP-iodine: history, toxicity, and therapeutic uses. J Int Coll Surg. 1956;25:727–34.
CAS PubMed Google Scholar
Kemeny-Beke A, Szodoray P. Ocular manifestations of rheumatic diseases. Int Ophthalmol. 2020;40:503–10.
Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg. 1986;151:400–6.
Mantelli F, Lambiase A, Sacchetti M, Orlandi V, Rosa A, Casella P, et al. Cocaine snorting may induce ocular surface damage through corneal sensitivity impairment. Graefe’s Archive Clin Experimental Ophthalmol. 2015;253:765–72.
Bever GJ, Brodie FL, Hwang DG. Corneal Injury from Presurgical Chlorhexidine Skin Preparation. World Neurosurg. 2016;96:610.e1-610.e4.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15:539–74.
Download references
Acknowledgements
APMO provided IDRA analysis, and was a contributor to design the study, revised, written and approved the manuscript. AMBC Applied intravitreal injections and provided patients for the study and was a contributor to design the study, revised, written and approved the manuscript.
No grant Money was received for this resesearch.
Author information
Authors and affiliations.
Postgraduate Program in Health Sciences, State University of Londrina, UEL, Londrina, Brazil
José Henrique Casemiro
Department of Health Sciences, Surgical Clinic, State University of Londrina, UEL, Londrina, Brazil
Ana Paula Miyagusko Taba Oguido
Londrina State University, Avenida Robert Koch, 60, Londrina, Paraná, 86038-440, Brazil
Antonio Marcelo Barbante Casella
You can also search for this author in PubMed Google Scholar
Contributions
JHC analyzed and interpreted patient data, reviewed the literature and was a major contributor to the acquisition of data, interviewed the patients, sponsored supplies, designed the study and written the manuscript. APMO provided IDRA analysis, and was a contributor to design the study, revised, written and approved the manuscript. AMBC Applied intravitreal injections and provided patients for the study and was a contributor to design the study, revised, written and approved the manuscript.
Corresponding author
Correspondence to Antonio Marcelo Barbante Casella .
Ethics declarations
Ethics approval and consent to participate and consent for publication.
Approval for the anonymous analisys of Imaging data and medical records was obtained from the Institutional Review Board.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Casemiro, J.H., Oguido, A.P.M.T. & Casella, A.M.B. Using 2% PVPI topical solution for serial intravitreous injections and ocular surface findings: a case control study. Int J Retin Vitr 10 , 41 (2024). https://doi.org/10.1186/s40942-024-00557-1
Download citation
Received : 11 March 2024
Accepted : 07 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s40942-024-00557-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dry eye disease
- Povidone iodine
- Ocular surface disease
International Journal of Retina and Vitreous
ISSN: 2056-9920
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Equity
- v.3(1); 2019

A Cancer Patient Journey: Complete Review During Acute Treatment Phase
Saima siddiqui.
Department of Family and Community Medicine, University of Texas Health Science Center at San Antonio, San Antonio, Texas.
Purpose: Cancer is a chronic illness with acute episodes lasting for years. Most cancer patients have coexisting comorbidities, which affect cancer treatment outcomes and make a shared care model for chronic diseases essential. There is a considerable gap between the achievable and delivered quality of care for cancer patients.
Methods: We used a case study approach to examine the complexity of cancer management, from the perspective of one person's case as interpreted by the care team. It allowed the complexity of cancer management to retain its holistic and meaningful characteristics. We interviewed the patient, caregiver, primary care physician (PCP), and oncologist. Interviews were audio recorded and analyzed with ATLASti, qualitative statistical software. Participants also completed a basic demographic survey. Common themes were identified, analyzed, and discussed.
Results: Main themes were lack of longitudinal relationship with PCP, communication barriers, and ambiguous health care provider roles. Communication barriers can be associated with the other two main themes.
Conclusion: Our results showed that shared care for cancer management is lacking during the acute cancer treatment phase. Communication barriers between the PCP and oncologist along with lack of continuity of care and unclear role of the PCP are major contributors for fragmented cancer care in U.S. health care system.
Introduction
Cancer is a leading cause of morbidity and mortality worldwide. In 2013, there were ∼1,660,290 new cancer cases and 580,350 cancer deaths in the United States. 1 A diagnosis of cancer is still very stressful and frightening for the majority of patients and families 2–4 although the number of patients living with cancer has increased threefold since 1971. 5 According to the Center for Disease Control and Prevention (CDC), cancer is classified as a chronic disease and described as of long duration and generally slow progression.
Studies have shown that cancer patients receive fragmented care especially during the acute treatment phase 6–9 stemming from system problems such as lack of health insurance, communication problems between health care team members, 7 , 10 and lack of role clarity among team members 11–14 The National Cancer Policy Board has concluded that for many Americans with cancer, there is a wide gulf between what could be construed as the “ideal and the reality of their experience with cancer care.” 15 There is not just a “gap, but a chasm.” 16
The purpose of this study was to gather a qualitative description of collaborative care from viewpoints of cancer patient (Pt), caregiver, primary care physician (PCP), and oncologist to better understand cancer patient's journey in the health care system.
A case study approach was used because it allowed us to examine the complexity of cancer management from the perspective of one person's case as interpreted by multiple people, retaining its holistic and meaningful characteristics while being studied 17 answering how and why questions. 18 Interviews from four participants presented multiple perspectives of the same interested topic, therefore achieving data triangulation.
The study is guided by the chronic care model (CCM), a proactive approach to keep patient healthy through productive collaboration between community and health systems; therefore, the study generalizes to the theoretical propositions of the CCM and not the population. 19 CCM identifies six structural elements: the community, the health system, self-management support, delivery system design, decision support, and clinical information systems. The interview guide was developed based on these areas. Development of the interview guide was an iterative process in which the researchers developed and discussed questions, which contextualized the CCM within cancer management. Once questions were approved, they became part of the official interview guide (12 total questions), which was re-evaluated for consistency and changed if researchers felt that questions were being misinterpreted. Main questions included were as follows: Tell me the story of how you learned you had cancer? Who did you talk to about your cancer diagnosis? How do your PCP and oncologist work together to manage your cancer and general medical care? The researcher conducting the interviews was knowledgeable in social science research of chronic conditions. Her inexperience served as a strength because she was not able to create leading questions or force participants into expected outcomes.
The study utilized a purposeful sampling method. 20 , 21 PCP identified and referred the cancer patient to the study. The patient then identified her caregiver and oncologist.
Data collection consisted of about 1 h long semistructured interview. The approach of starting with the patient and then interviewing the caregiver and the clinicians helped to understand how the same events were viewed from different perspectives. Each interview was recorded and transcribed for analysis. All research activities were reviewed and approved by the University of Texas Health Science Center San Antonio Office of Institutional Review Board.
Our sample included interviews with one cancer patient, her caregiver, PCP, and oncologist. Specifics of sample demographics are in Tables 1 and and2 2 ).
Demographics of Patient and Caregiver in Case Study
Demographics of Providers in Case Study
M, male; PCP, primary care physician.
The results identified a major breakdown in the delivery system design highlighted in the CCM. The three main themes, which are organized around the patients' experience through the health care system—from cancer diagnosis to treatment, are as follows:
- (a) Lack of longitudinal relationship with PCP
- (b) Communication barriers
- (c) Ambiguous health care provider role.
(a) Lack of longitudinal relationship with PCP: This theme supports a known system problem in which people who are the sickest and need health insurance the most do not have it. This particular patient lost insurance, secondary to unemployment because of uncontrolled hypertension.
The patient ended up in the emergency room (ER) for severe chest pain and was diagnosed as having leukemia.
Pt: “At that time, I did not [have a PCP] … I was one of those persons that go from payday to payday and I could not afford health insurance…Here I am very sick, quitting because I am very sick…So when I went into ER, I did not have a doctor…”
The first PCP visit was 4 months after her leukemia diagnosis and after receiving three cycles of chemotherapy.
Pt: “After my fourth visit to the [cancer treatment center] they told me that I need to call the [healthcare system] and I needed to get a PCP…”
The patient was assigned a new PCP in a teaching facility with residents and faculty members divided into teams and different providers saw the patient every time. The lack of a longitudinal relationship with a PCP appeared normal to the patient; therefore, she began to rely heavily on the oncology team and ER for things that a PCP could manage.
Pt: “Usually I see a different [provider], it is like a set of doctors that all work together. So, I can't say it is one doctor…”
(b) Communication barriers: The communication barriers surrounding cancer treatment began between the patient, caregiver, and health care providers almost immediately. As the patient was diagnosed with cancer in the ER, she felt she was not able to get the answers for her questions,
Pt: “The whole time all I was thinking, I have cancer! What is Leukemia… am I going to die… I heard them talking between themselves that it might be Leukemia…[And] they didn't want to give me the exact diagnosis yet.”
Similarly, the caregiver was not included in any stage of cancer management. After a few months, the oncologist provided a video to share with family members.
Caregiver: “..a lot of questions I had, I just used my own resources… [the providers asked] if you have questions…and then they gave us some packets and pamphlets. I relied mostly on my mom for communication… My mom has a high school education, GED, and she doesn't understand lots of words.”
The teaching practice setting also prevented her from communicating with the health care team. The caregiver's impression was that due to patient's privacy, physicians were not supposed to communicate with her, and residents' learning will be interrupted by her questions.
Caregiver: “I always assume, it's a privacy thing… I just wish there was a means for me to communicate directly with them or staff or nurse. I feel like there's residents that come in as a group with the doctors and learn, so I feel like I didn't want to interrupt their learning with questions.”
Caregiver also identified lack of communication between the PCP and oncologist.
Caregiver: “I feel like there's a lack of communication between them. That's a prescription given to her by her cancer doctor. Then the PCP will say that's not working out for you, let's take them off so that makes me uncomfortable, just in the sense that I feel like you should ask [the oncologist] first… My mom's been bounced back and forth between vitamins and medications that she'll get prescribed by one doctor, and then another doctor will change their mind..”
There was no specific arrangement for cancer patients to contact PCP for early or urgent appointments. When the caregiver called to report a concern, appointment clerk asked her to go to the ER. At times, the ability to provide advice was contingent on the flow of clinic traffic, sometimes the patient and caregiver were able to contact the oncologist but got same advice.
Both the PCP and oncologist identified lack of communication as a barrier for patient management. The health care providers were not able to effectively communicate because of the distance between facilities, a physical difficulty, and relational issue.
Oncologist : “The physical issue of being based in a downtown [building] and having oncology services out at medical center [approximately 12 miles away]. You can't pop over at lunch for a meeting ever, I suppose..”
Time constraint was another factor. PCPs do not have time to serve on cancer boards and oncologists do not communicate with PCP by phone or with follow-up letters.
Oncologist: “No one's going to serve on a board if they're all in clinic full time, of course… Everyone's busy so the communication is lacking…because we in oncology have been very short staffed.”
Use of different electronic health record (EHR) systems break communication further.
PCP: “It is not possible for providers to look into each other notes and management plan. You've got the problem of the two computer systems that don't talk to each other, so they don't see what they are doing in [EHR] and we don't see what they are doing in their EHR, so that makes it very difficult just all around.”
No point of contact within the PCP and oncology clinic was assigned for communication about patients. The PCP was expected to communicate through the oncology on-call resident or the front desk person for any question or concern. It resulted in duplicate laboratory tests and confusion about patient's treatment and patient served as the main communicator between the PCP and oncologist. It also resulted in care delay.
PCP: “These are all unnecessary barriers in communication between the two offices and one of them is the fact that you can't just book the patient before the patient leaves… sometimes you think you are conveying information, sometimes they don't receive it.”
(c) Ambiguous health care provider role: The patient, caregiver, and health care providers agree that the PCP should be an essential part of the management team; however, all ambiguously understands the role. The PCP was viewed as important for the emotional support of the patient and family.
Pt: “She [the PCP] asked me if I ever got depressed. I told her no… She said, it is okay to say it if you are…I told her when I get in the shower I just breakdown crying sometimes for no reason. She says good, let it out. She says it is okay to feel that way. I would feel that way too.”
However, the PCP was not comfortable in managing specific chemotherapy-related side effects. The PCP felt that their strengths were in management of chronic diseases. The oncologist felt that they should be able to rely on the PCP for support of common disease management.
Oncologist: “..honestly my knowledge of ideal hypertension management has declined… even though I am an internist at heart… I quickly need primary care support to manage hypertension, as well as routine health maintenance of immunizations and recommended cancer screenings. We [the oncologist] make the diabetes worse, so we constantly want to work with primary care teams.”
The oncologist identified that the PCP should be seen as (Oncologist): “an educator or tie-breaker in terms of treatment decision making.”
This study reflects a typical journey of an underprivileged uninsured cancer patient through the American health care system. It is unique in that data were collected and interpreted from the patients' perspective but captures several perspectives on the experience. No other studies, focusing on the patient perspective from a case study methodology, were found in the current literature. The patient lost her health insurance due to uncontrolled hypertension resulting in the loss of employment. This resulted in a delay of cancer diagnosis as the patient kept on postponing and neglecting the symptoms as long as she could tolerate. Main barriers identified in our study were the same as identified in earlier studies. Similarities included a lack of longitudinal relationships with the PCP, communication issues between patient, caregiver, PCP, and oncologist, and a lack of role clarification for providers and patient. 14 , 22–25 New finding was the patient and caregiver's inability to communicate with PCP due to the teaching practice setting.
This study identifies the serious gaps and areas of improvement for cancer. Our findings confirm that the PCP is not an active member of patients' management team during chemotherapy. 25–27 The first PCP visit took place after the fourth chemotherapy visit, ∼3½ months into chemotherapy. Studies have shown that one in five Americans reported not getting or delaying medical care, and the percentage of uninsured patients 45–64 years of age increased from 13.1% to 15.6%. 28 , 29 In addition, the patient did not have access to a PCP after obtaining health care insurance due to the PCP's busy schedule and the absence of special arrangements for cancer patients, which resulted in patients using the ER. Previous studies have shown that there is an increased use of health care services by cancer patients when they are undergoing acute cancer treatment by chemotherapy and radiation as well as after treatment. 30 , 31 Ideally, there needs to be special provisions or the identification of a key contact person for cancer patients in PCP offices.
Lack of communication was the most prominent problem identified by the patient, caregiver, and physicians. The main communication failure was between the PCP and the oncology team, confirming similar findings identified in other studies. 32–36 The federal government has offered incentives for meaningful use of information technology as a key tool for improving care coordination, which resulted in an increased use of EHR by physicians and hospitals. 37 , 38 In our study, the use of different EHRs by the oncologist and the PCP office was problematic. The PCP could not access patient information from the oncology visit and there was no formal follow-up letter from oncology. Therefore, the PCP did not have any idea about chemotherapy regime or patient prognosis. Ideally, EHR should account for human factors both tolerating human limitations and augmenting human strengths, 39 and bridging the gap between different segments of patient care rather than collecting numbers and producing reports to fulfill government requirements.
Similarly, the patient and caregiver expressed frustration about the lack of communication because it placed a larger burden on the patient as main communicator between oncologist and PCP, which is not an acceptable practice.
Not knowing the point of contact in the PCP and oncology office was an additional reason for communication breakdown. Good care coordination for safe and appropriate management of chronic conditions such as cancer are essential, but the care coordination remains inadequate and a major cause of health care expenditure and mistakes. 40 , 41 Possible solutions include uniform access to EHRs, clear identification of the patient's PCP and oncologist, a point of contact in each office, and a structured follow-up letter from oncologist to PCP. 42 Further studies are needed to evaluate the efficacy of these measures.
Time constraint was an additional reason identified by the PCP and oncologist for the communication breakdown. There is no formal reimbursement for physician or staff time used for communication and coordination between providers or by insurance companies. 43 In addition, the shortage of PCPs and oncologists, and increased number of cancer patients makes care coordination more difficult. 44 A system-wide change is needed to address these issues and acknowledge that time reimbursement will produce real improvement in patient care and reduce health care cost. The patient and caregiver identified the teaching hospital setting as an inhibitory factor because they felt that asking questions and communicating with health care providers would interfere with learning, which is a new finding by this study. It requires that teaching physicians take extra steps to include the patient and care giver in their discussions and make them feel like part of the team by formally including the patient in discussions.
Lack of PCP role clarification was another barrier identified for effective collaboration. 45–47 The current norm accepts that PCPs will not be a part of the cancer patient health care team. The patient and caregiver expectations were that the PCP would serve as emotional support, manage chronic disease, and perform routine health maintenance such as cancer screening and immunizations. Studies have shown that PCPs can play an important role in the management of cancer patients' coexisting chronic conditions and common side effects of chemotherapy, treating acute conditions such as viral illnesses and helping patient to make informed decisions about management, and end-of-life issues. 48 The oncologist agreed that the PCP was an important part of the health care team, and the PCP was comfortable in fulfilling all these roles. Clear role assignment of health care team members will decrease the role confusion and potentially impact patients' unnecessary ER visits, reducing patient discomfort and health care cost.
Our study revealed many barriers for collaboration during the initial cancer treatment phase between the PCP and oncologist. Even though there is an abundance of resources and expertise available, the lack of collaboration and fragmented effort resulted in a wide gap between possible and actual care delivery for cancer patients.
Limitations
The major weaknesses of this study are that it was conducted in a teaching hospital setting and describes the experience of only one patient. However, the purpose of a case study was to examine the complexity of a phenomenon (cancer management) while it retains its holistic and meaningful characteristics. Major strength of this study is that it describes the complete experience, as it has been understood by an underserved and uninsured patient, caregiver, and patient health care team.
Implications
The barriers identified in this study should be used to devise interventions to be tested in large-scale prospective studies to fill gaps in present system of cancer patient care.
Acknowledgments
This study was funded by American Cancer Society. We thank Robert L. Ferrer, MD, and Sarah Gill, PhD, for helping at every stage of article development and supervising all aspects of this project.
Abbreviations Used
Author disclosure statement.
No competing financial interests exist.
Cite this article as: Siddiqui S, Cruz I (2019) A cancer patient journey: complete review during acute treatment phase, Health Equity 3:1, 403–408, DOI: 10.1089/heq.2019.0046.
An Observational Study to Assess the Outcome of Canal Wall Window Tympanomastoidectomy in Chronic Suppurative Otitis Media
- Original Article
- Published: 06 June 2024
Cite this article

- Sameeksha Mishra ORCID: orcid.org/0000-0002-5376-5483 1 &
- Sudhakar Vaidya 1
This study was undertaken to assess the outcome of canal wall window tympanomastoidectomy in chronic suppurative otitis media in a tertiary care centre of central India. A total of 50 patients were taken for this study in which the youngest patient was 13-year-old male and oldest 55-year female. Maximum patients were in between age group 10 to 20 years, 20 (40%) patients and minimum 03 (6%) between age group 51 to 60 year. The study mainly emphasized on: To study the clinical profile of the cases of chronic suppurative otitis media, to study the hearing outcome after 3 months of Canal wall window tympanomastoidectomy technique, to study the post-operative condition of ear after 3 months whether dry or wet and to study the post-operative follow up of cases to assess the graft uptake. Average PTA & ABG improvement of different tympanoplasty was also calculated in our study in which Type I tympanoplasty had 12.20dB gain, Type II of 10.50 and Type III of 10.31dB.An overall average improvement in all patients with tympanoplasty was 11.00dB.At the end of the study 100% dry ears were achieved. The technique of canal wall window tympanomastoidectomy involves formation of a window in the outer attic wall to look at the disease extent which was then closed by a snuggly fitting cartilage.It is a novel technique & without compromising the structural integrity in case of a limited disease which is only extending till attic and aditus good anatomical and hearing results could be gained.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Nadol JB (1993) Chronic otitis media. In: Nadol JB, Schuknecht HF (eds) Surgery of the ear and temporal bone. Raven, New York, pp 155–170
Google Scholar
Sheehy JL, Smyth GDL, Toner JG (1994) In: Brackman DE, Shelton C, Arriga M (eds) Otologic surgery. WB Saunders, Pheladelphia: WB Saunders, 1994; 211–224 and 225–239.
Roland D, Eavey MD, Jose F (2000) Lubianca Neto, Md: Canal Wall window tympan- omastoidectomy. Laryngoscope 110:1410–1414
Article Google Scholar
Sheely Jl (1996) Cholesteatoma surgery, Canal wall down procedure, annals of Otology. Rhinology Laryngology 1(97):30–35
Ricado A, Godinho, Syed H, Kamil,JoseN. Lubianca IJ, Keogh,Roland D, Eavey (2005) Pediatric Cholesteatoma: Canal Wall Window Alternative to Canal Wall Down Mastoidectomy. Otology Neurotology 26:446–471
63.Reddy Tn, Dutt SN, Shetty A, Maini S (2001) Transcanal attico-aditotomy and trans cortical mastoidectomy for choles- teatoma: the Farrior- Olaizola technique revisited. Ann Otol Rhinol Laryngol 110:739–745
Dornhoffer JL (2000) Retrograde mastoi- dectomy with canal wall reconstruction: a single-stage technique for choles- teatoma removal. Ann Otol Rhinol Laryngol 109:1033–1039
Article CAS PubMed Google Scholar
Hartwein J, Hormann K (1990) A technique for the reconstruction of the posterior canal wall and mastoid obliteration in radical cavity surgery. Am J Otol 11:169–173
CAS PubMed Google Scholar
Eviatar A (1978) Tragal perichondrium and cartilage in reconstructive ear surgery. Laryngoscope 88(suppl 11):1–23
Rosenfeld RM, Moura RL, Bluestone CD (1992) Predectors of residual-recurrent cholesteatoma in children. Arch Otolaryngol Head Neck surg 118:384–391
Sanna M, Xini C, Gamoletti R, Delogu P, Russo A (1987) The surgical management of childhood cholesteatoma. J Laryngol Otol 101:1221–1226
Mutlu C, Khashaba A, Saleh F (1995) Surgical management of cholesteatoma in children. Otolaryngol Head Neck Surg 113:56–60
Dodson EE, Hashisaki GT, Hobgood TC (1998) Intact canal wall mastoidectomy with tympanoplasty for cholesteatoma in children. Laryngoscope 108:977–983
Ina mitsu M, Komune S, Toh S (1999) Treatment of cholesteatoma in children. Eur Arch Otorhinolaryngol 256(Suppl 1):S8–10
Iino Y, Imamura Y, Kojima C (1998) TakegoshiS. Risk factors for recurrent and residual cholesteatoma in children determined by second stage operation. Int J Pediatr Otorhinolaryngol 46:57–65
Arriaga M (1994) Cholesteatoma in children. Otolaryngol Clin North Am 27:573–591
Download references
Author information
Authors and affiliations.
Department of ENT, R.D Gardi Medical College, Ujjain, MP, India
Sameeksha Mishra & Sudhakar Vaidya
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sameeksha Mishra .
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Mishra, S., Vaidya, S. An Observational Study to Assess the Outcome of Canal Wall Window Tympanomastoidectomy in Chronic Suppurative Otitis Media. Indian J Otolaryngol Head Neck Surg (2024). https://doi.org/10.1007/s12070-024-04771-z
Download citation
Received : 07 February 2024
Accepted : 19 May 2024
Published : 06 June 2024
DOI : https://doi.org/10.1007/s12070-024-04771-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Canal wall window
- Hypertrophied mucosa
- Cholesteatoma
- Antral wash
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
A 44-year-old woman presented with cough, dyspnea, and chest pain. On examination, she had tachycardia and hypotension. Evaluation revealed SARS-CoV-2 RNA in a nasopharyngeal swab, as well as eleva...
Imaging studies show bilateral peripheral opacities. ... A massive or submassive pulmonary embolism is preferentially managed with mechanical intervention. 20 In this case, the patient's ...
Summarize the major points of the case. Provide a limited number (e.g. 3) of takeaway points for the audience. Tailor summary and takeaway points to your audience. Critical Thinking Skills. Successful patient case presentations: Integrate disease and drug knowledge, clinical evidence, and patient factors.
The patient subsequently underwent evaluation at her primary care clinic. Her score on the Epworth Sleepiness Scale was 20, with scores ranging from 0 (low-normal daytime sleepiness) to 24 ...
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Notes on patient consent. Informed consent in an ethical requirement for most studies involving humans, so before you start writing your case report, take a written consent from the patient as all journals require that you provide it at the time of manuscript submission. In case the patient is a minor, parental consent is required.
Writing up. Write up the case emphasising the interesting points of the presentation, investigations leading to diagnosis, and management of the disease/pathology. Get input on the case from all members of the team, highlighting their involvement. Also include the prognosis of the patient, if known, as the reader will want to know the outcome.
Case study is a research methodology, typically seen in social and life sciences. There is no one definition of case study research.1 However, very simply… 'a case study can be defined as an intensive study about a person, a group of people or a unit, which is aimed to generalize over several units'.1 A case study has also been described as an intensive, systematic investigation of a ...
The patient reported that episodes of hypoglycemia occurred. Polyhydramnios developed. The child was born at 38 weeks 6 days of gestation and weighed 3.5 kg. The patient sought care at the diabetes clinic of this hospital for clarification of her diagnosis. The patient reported following a low-carbohydrate diet and exercising 5 days per week.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
Case studies are an invaluable record of the clinical practices of a profession. While case studies cannot provide specific guidance for the management of successive patients, they are a record of clinical interactions which help us to frame questions for more rigorously designed clinical studies. Case studies also provide valuable teaching ...
Even a short course of oral corticosteroids in the preceding month for an asthma exacerbation, such as in this case study, is a risk factor for ARDS and mechanical ventilation. Conversely, in vitro studies with ciclesonide showed antiviral activity against Covid-19, and there have been reports of clinical effectiveness of inhaled ciclesonide in ...
The following case study illustrates the clinical role of advanced practice nurses in the management of a patient with type 2 diabetes. Case Presentation A.B. is a retired 69-year-old man with a 5-year history of type 2 diabetes.
On examination, the patient appeared to be in respiratory distress. The temperature was 35.9°C, the pulse 98 beats per minute, the blood pressure 129/58 mm Hg, the respiratory rate 24 breaths per ...
5. Complete your introduction and conclusion after you've written the body. Since these sections summarize key points of your case study, it's best to write them last. The introduction gives a brief overview of the basic condition of your patient and the problem you'll address in your case study.
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Effective implementation of this recommendation for the lady in this case study is considered from the perspective of a patient, healthcare professional, and the organisation. ... The patient ...
Patient case studies can be theoretical or actual examples of a patient's story, or in clinical terms, a particular medical case. These stories can range from discussing symptoms and diagnoses as well as charting the impact of treatment (s) and eventual outcome (s). They are used to make the intended audience aware of and more educated about ...
Case Study: Patient with Rare Breast Cancer Has Surprising Response to NAC. Story by Kate Kneisel • 18h "Medical Journeys" is a set of clinical resources reviewed by doctors, meant for ...
Health-science document from Curtin University, 13 pages, Applied Bioscience for Health Complexity 2 (GMED3009) Acute Kidney Injury Case Study Case study- Learning outcomes Discuss the aetiology and pathophysiology of acute kidney injury (AKI) Describe Explain the clinical assessment of a patient with AKI the r
This study aimed to determine the role of mitofusin 2 (MFN2) gene polymorphisms in the risk and prognosis of acute liver failure (ALF). A total of 298 blood samples were collected from 138 ALF patients (case group) and 160 healthy participants (control group). Coagulation function, glutamic pyruvic …
In one study, 69.8% of the patients had a partial or complete response after receiving an ... Mehta V, Goel S, Kabarriti R, et al. Case fatality rate of cancer patients with COVID-19 in a New York ...
Design. In this study, we used a convergent parallel mixed-methods design [] within a pragmatic constructivist case study approach [].We simultaneously collected data from students and educators using online questionnaires and semi-structured interviews to gain deeper insight into their needs on one particular situation []- the development of a clinical reasoning curriculum—to address our ...
Objectives Diabetic ketoacidosis (DKA) is a serious complication in patients treated with sodium-glucose co-transporter 2 inhibitors (SGLT2i). The aim of this study was to investigate the relationship between SGLT2i and the risk of DKA, and to identify high-risk groups and characteristics that should be emphasised. Methods A retrospective case series study was conducted to collect medical ...
Randomized, non-randomized, descriptive, controlled, cohort, case-studies, cross-sectional, mixed method, and qualitative publications ... is imperative to providing patient care. In fact, a study by Stockbridge et al 17 on strengthening tuberculosis protection for Muslim refugees showed the impact of culturally humility in healthcare. Prior to ...
A case-control study was conducted at the Ophthalmology and Psicology Clinic (APMTO MD) in Londrina, Paraná. The patients were recruited from the Retina and Vitreous Institute (AMBC MD) in Londrina, Paraná. The study included 34 individuals (68 eyes). 14 males, 20 females, aged 48 to 94 years.
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
Methods. A case study approach was used because it allowed us to examine the complexity of cancer management from the perspective of one person's case as interpreted by multiple people, retaining its holistic and meaningful characteristics while being studied 17 answering how and why questions. 18 Interviews from four participants presented multiple perspectives of the same interested topic ...
This study was undertaken to assess the outcome of canal wall window tympanomastoidectomy in chronic suppurative otitis media in a tertiary care centre of central India. A total of 50 patients were taken for this study in which the youngest patient was 13-year-old male and oldest 55-year female. Maximum patients were in between age group 10 to 20 years, 20 (40%) patients and minimum 03 (6% ...
Unfortunately, many patients with severe acute kidney injury are not eligible for these studies or are required to discontinue participation (as in this case) because remdesivir is eliminated ...