- Search Menu
- Sign in through your institution
- Volume 2024, Issue 5, May 2024 (In Progress)
- Volume 2024, Issue 4, April 2024
- Case of the Year
- MSF Case Reports
- Audiovestibular medicine
- Cardiology and cardiovascular systems
- Critical care medicine
- Dermatology
- Emergency medicine
- Endocrinology and metabolism
- Gastroenterology and hepatology
- Geriatrics and gerontology
- Haematology
- Infectious diseases and tropical medicine
- Medical ophthalmology
- Medical disorders in pregnancy
- Paediatrics
- Palliative medicine
- Pharmacology and pharmacy
- Radiology, nuclear medicine, and medical imaging
- Respiratory disorders
- Rheumatology
- Sexual and reproductive health
- Sports medicine
- Substance abuse
- Author Guidelines
- Submission Site
- Open Access
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Answer to part 1, answer to part 2, answer to part 3, answer to part 4, answer to part 5.
- < Previous
Educational Case: A 57-year-old man with chest pain
Contributed equally.
- Article contents
- Figures & tables
- Supplementary Data
Nikhil Aggarwal, Subothini Selvendran, Vassilios Vassiliou, Educational Case: A 57-year-old man with chest pain, Oxford Medical Case Reports , Volume 2016, Issue 4, April 2016, Pages 62–65, https://doi.org/10.1093/omcr/omw008
- Permissions Icon Permissions
This is an educational case report including multiple choice questions and their answers. For the best educational experience we recommend the interactive web version of the exercise which is available via the following link: http://www.oxfordjournals.org/our_journals/omcr/ec01p1.html
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by paramedics in the community. He smoked 20 cigarettes daily (38 pack years) but was not aware of any other cardiovascular risk factors. On examination he appeared comfortable and was able to complete sentences fully. There were no heart murmurs present on cardiac auscultation. Blood pressure was 180/105 mmHg, heart rate was 83 bpm and regular, oxygen saturation was 97%.
What is the most likely diagnosis?
An ECG was requested and is shown in figure 1.
How would you manage the patient? (The patient has already received 300 mg aspirin).
30 minutes later the patient's chest pain returned with greater intensity whilst waiting in the emergency department. Now, he described the pain as though “an elephant is sitting on his chest”. The nurse has already done an ECG by the time you were called to see him. This is shown in figure 2.

ECG on admission.

ECG 30 minutes after admission.
What would be the optimal management for this patient?
He was taken to the catheterization lab where the left anterior descending coronary artery (LAD) was shown to be completely occluded. Following successful percutaneous intervention and one drug eluding stent implantation in the LAD normal flow is restored (Thrombosis in myocardial infarction, TIMI = 3). 72 hours later, he is ready to be discharged home. The patient is keen to return to work and asks when he could do so.
When would you advise him that he could return to work?
One week later, he receives a letter informing him that he is required to attend cardiac rehabilitation. The patient is confused as to what cardiac rehabilitation entails, although he does remember a nurse discussing this with him briefly before he was discharged. He phones the hospital in order to get some more information.
Which of the following can be addressed during cardiac rehabilitation?
A - Acute coronary syndrome
Although the presentation could be attributable to any of the above differential diagnoses, the most likely etiology given the clinical picture and risk factors is one of cardiac ischemia. Risk factors include gender, smoking status and age making the diagnosis of acute coronary syndrome the most likely one. The broad differential diagnosis in patients presenting with chest pain has been discussed extensively in the medical literature. An old but relevant review can be found freely available 1 as well as more recent reviews. 2 , 3
C - Atorvastatin 80 mg, Clopidogrel 300 mcg, GTN 500 mcg, Ramipril 2.5 mg,
In patients with ACS, medications can be tailored to the individual patient. Some medications have symptomatic benefit but some also have prognostic benefit. Aspirin 4 , Clopidogrel 5 , Atenolol 6 and Atorvastatin 7 have been found to improve prognosis significantly. ACE inhibitors have also been found to improve left ventricular modeling and function after an MI. 8 , 9 Furthermore, GTN 10 and morphine 11 have been found to be of only significant symptomatic benefit.
Oxygen should only to be used when saturations <95% and at the lowest concentration required to keep saturations >95%. 12
There is no evidence that diltiazem, a calcium channel blocker, is of benefit. 13
His ECG in figure 1 does not fulfil ST elevation myocardial infarction (STEMI) criteria and he should therefore be managed as a Non-STEMI. He would benefit prognostically from beta-blockade however his heart rate is only 42 bpm and therefore this is contraindicated. He should receive a loading dose of clopidogrel (300 mg) followed by daily maintenance dose (75 mg). 14 , 15 He might not require GTN if he is pain-free but out of the available answers 3 is the most correct.
D - Proceed to coronary angiography
The ECG shows ST elevation in leads V2-V6 and confirms an anterolateral STEMI, which suggests a completely occluded LAD. This ECG fulfils the criteria to initiate reperfusion therapy which traditionally require one of the three to be present: According to guidance, if the patient can undergo coronary angiography within 120 minutes from the onset of chest pain, then this represents the optimal management. If it is not possible to undergo coronary angiography and potentially percutaneous intervention within 2 hours, then thrombolysis is considered an acceptable alternative. 12 , 16
≥ 1 mm of ST change in at least two contiguous limb leads (II, III, AVF, I, AVL).
≥ 2 mm of ST change in at least two contiguous chest leads (V1-V6).
New left bundle branch block.
GTN and morphine administration can be considered in parallel but they do not have a prognostic benefit.
E - Not before an exercise test
This patient is a lorry driver and therefore has a professional heavy vehicle driving license. The regulation for driving initiation in a lorry driver following a NSTEMI/ STEMI may be different in various countries and therefore the local regulations should be followed.
In the UK, a lorry driver holds a category 2 driving license. He should therefore refrain from driving a lorry for at least 6 weeks and can only return to driving if he completes successfully an exercise evaluation. An exercise evaluation is performed on a bicycle or treadmill. Drivers should be able to complete 3 stages of the standard Bruce protocol 17 or equivalent (e.g. Myocardial perfusion scan) safely, having refrained from taking anti-anginal medication for 48 hours and should remain free from signs of cardiovascular dysfunction during the test, notably: angina pectoris, syncope, hypotension, sustained ventricular tachycardia, and/or electrocardiographic ST segment shift which is considered as being indicative of myocardial ischemia (usually >2 mm horizontal or down-sloping) during exercise or the recovery period. 18
For a standard car driving license (category 1), driving can resume one week after successful intervention providing that no other revascularization is planned within 4 weeks; left ventricular ejection fraction (LVEF) is at least 40% prior to hospital discharge and there is no other disqualifying condition.
Therefore if this patent was in the UK, he could restart driving a normal car one week later assuming an echocardiogram confirmed an EF > 40%. However, he could only continue lorry driving once he has passed the required tests. 18
E - All of the above
Cardiac rehabilitation bridges the gap between hospitals and patients' homes. The cardiac rehabilitation team consists of various healthcare professions and the programme is started during hospital admission or after diagnosis. Its aim is to educate patients about their cardiac condition in order to help them adopt a healthier lifestyle. This includes educating patients' about their diet, exercise, risk factors associated with their condition such as smoking and alcohol intake and finally, about the medication recommended. There is good evidence that adherence to cardiac rehabilitation programmes improves survival and leads to a reduction in future cardiovascular events. 19 , 20
Oille JA . Differential diagnosis of pain in the chest . Can Med Assoc J . 1937 ; 37 (3) : 209 – 216 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC536075/ .
Google Scholar
Lee TH , Goldman L . Evaluation of the patient with acute chest pain . N Engl J Med . 2000 ; 342 (16) : 1187 – 1195 . http://www.nejm.org/doi/full/10.1056/NEJM200004203421607 .
Douglas PS , Ginsburg GS . The evaluation of chest pain in women . N Engl J Med . 1996 ; 334 (20) : 1311 – 1315 . http://www.nejm.org/doi/full/10.1056/NEJM199605163342007 .
Baigent C , Collins R , Appleby P , Parish S , Sleight P , Peto R . ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. the ISIS-2 (second international study of infarct survival) collaborative group . BMJ . 1998 ; 316 (7141) : 1337 – 1343 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC28530/ .
Yusuf S , Zhao F , Mehta S , Chrolavicius S , Tognoni G , Fox K . Clopidogrel in unstable angina to prevent recurrent events trail investigators . effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation . N Engl J Med . 2001 ; 345 (7) : 494 – 502 . http://www.nejm.org/doi/full/10.1056/NEJMoa010746#t=articleTop .
Yusuf S , Peto R , Lewis J , Collins R , Sleight P . Beta blockade during and after myocardial infarction: An overview of the randomized trials . Prog Cardiovasc Dis . 1985 ; 27 (5) : 335 – 371 . http://www.sciencedirect.com/science/article/pii/S0033062085800037 .
Schwartz GG , Olsson AG , Ezekowitz MD et al. . Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: The MIRACL study: A randomized controlled trial . JAMA . 2001 ; 285 (13) : 1711 – 1718 . http://jama.jamanetwork.com/article.aspx?articleid=193709 .
Pfeffer MA , Lamas GA , Vaughan DE , Parisi AF , Braunwald E . Effect of captopril on progressive ventricular dilatation after anterior myocardial infarction . N Engl J Med . 1988 ; 319 (2) : 80 – 86 . http://content.onlinejacc.org/article.aspx?articleid=1118054 .
Sharpe N , Smith H , Murphy J , Hannan S . Treatment of patients with symptomless left ventricular dysfunction after myocardial infarction . The Lancet . 1988 ; 331 (8580) : 255 – 259 . http://www.sciencedirect.com/science/article/pii/S0140673688903479 .
Ferreira JC , Mochly-Rosen D . Nitroglycerin use in myocardial infarction patients . Circ J . 2012 ; 76 (1) : 15 – 21 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3527093/ .
Herlitz J , Hjalmarson A , Waagstein F . Treatment of pain in acute myocardial infarction . Br Heart J . 1989 ; 61 (1) : 9 – 13 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1216614/ .
Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC), Steg PG, James SK, et al . ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation . Eur Heart J . 2012 ; 33 (20) : 2569 – 2619 . http://eurheartj.oxfordjournals.org/content/33/20/2569 .
The effect of diltiazem on mortality and reinfarction after myocardial infarction . the multicenter diltiazem postinfarction trial research group . N Engl J Med . 1988 ; 319 (7) : 385 – 392 . http://www.nejm.org/doi/full/10.1056/NEJM198808183190701 .
Jneid H , Anderson JL , Wright RS et al. . 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non–ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update) A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2012 ; 60 (7) : 645 – 681 . http://circ.ahajournals.org/content/123/18/2022.full .
Hamm CW , Bassand JP , Agewall S et al. . ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: The task force for the management of acute coronary syndromes (ACS) in patients presenting without persistent ST-segment elevation of the european society of cardiology (ESC) . Eur Heart J . 2011 ; 32 (23) : 2999 – 3054 . http://eurheartj.oxfordjournals.org/content/32/23/2999.long .
O'Gara PT , Kushner FG , Ascheim DD et al. . 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: Executive summary: A report of the american college of cardiology foundation/american heart association task force on practice guidelines . J Am Coll Cardiol . 2013 ; 61 (4) : 485 – 510 . http://content.onlinejacc.org/article.aspx?articleid=1486115 .
BRUCE RA , LOVEJOY FW Jr . Normal respiratory and circulatory pathways of adaptation in exercise . J Clin Invest . 1949 ; 28 (6 Pt 2) : 1423 – 1430 . http://www.ncbi.nlm.nih.gov/pmc/articles/PMC439698/ .
DVLA . Https://Www.gov.uk/current-medical-guidelines-dvla-guidance-for-professionals-cardiovascular-chapter-appendix .
British Heart Foundation . Http://Www.bhf.org.uk/heart-health/living-with-heart-disease/cardiac-rehabilitation.aspx .
Kwan G , Balady GJ . Cardiac rehabilitation 2012: Advancing the field through emerging science . Circulation . 2012 ; 125 (7) : e369–73. http://circ.ahajournals.org/content/125/7/e369.full .
Author notes
- knowledge acquisition
Email alerts
Citing articles via, affiliations.
- Online ISSN 2053-8855
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

- General Dermatology
- Actinic Keratosis
- Precision Medicine and Biologics
- Rare Disease
- Psoriatic Arthritis
- Atopic Dermatitis
- Skin Cancer
- Hidradenitis Suppurativa
- Pigmentary Disorders
- Pediatric Dermatology
- Practice Management
Patient Case #2: 23-Year-Old Female With Plaque Psoriasis
- Terry Faleye, MPAS, PA-C
- Laura Bush, DMSc, PA-C, DFAAPA
- Lakshi Aldredge, MSN, ANP-BC
Jennifer Conner, MPAS, PA-C, and Terry Faleye, MPAS, PA-C, review a case of a young adult female with plaque psoriasis on the elbows, thighs, and scalp, and discuss switching systemic treatments to accommodate her lifestyle.

EP: 1 . The Role of Nurse Practitioners and Physician Assistants in Managing Plaque Psoriasis

EP: 2 . Evolution of Plaque Psoriasis

EP: 3 . Efficacy of Deucravacitinib in Plaque Psoriasis
Ep: 4 . approaches to treatment of plaque psoriasis, ep: 5 . importance of quick response to treatment for patients with plaque psoriasis, ep: 6 . metrics to determine disease clearance in plaque psoriasis.

EP: 7 . Addressing Unmet Needs in Psoriasis Treatment

EP: 8 . Patient Case #1: 50-Year-Old Female With Plaque Psoriasis
Ep: 9 . escalating treatment from topical to systemic in plaque psoriasis, ep: 10 . systemic treatment options in plaque psoriasis, ep: 11 . importance of long-term safety data in plaque psoriasis treatment, ep: 12 . patient case #2: 23-year-old female with plaque psoriasis, ep: 13 . use of systemic treatment in plaque psoriasis, ep: 14 . safety profile of tyk2 inhibitors in plaque psoriasis treatment, ep: 15 . role of advanced practice providers in plaque psoriasis treatment follow-up, ep: 16 . patient case #3: 40-year-old woman with a 10-year history of plaque psoriasis, ep: 17 . treating comorbidities with plaque psoriasis, ep: 18 . unmet needs in the treatment spectrum of plaque psoriasis, ep: 19 . take-home pearls on the management of plaque psoriasis.
Alexa Hetzel, MS, PA-C: Let’s move on to our next case. This is a 23-year-old female who presents with several thick, scaly, well-defined erythematous plaques that are silver in color. [It’s] very textbook for us to [make] this diagnosis. It’s very prominent, especially on her elbows, thighs, and her scalp, and it’s covering 15% of her body surface area. She mentions having rashes in the past but nothing severe. She was initially started on apremilast but is [experiencing] nausea and diarrhea.
Laura Bush, DMSc, PA-C: And she wants to wear shorts and put her hair in a ponytail.
Alexa Hetzel, MS, PA-C: I had this patient today…I was doing a full body check and she had her hair up. It looked really fancy, [so] I didn’t want to mess it up. I was combing through without being too crazy. I [asked her to take her] hair down, [and] her scalp was covered. I really wouldn’t have noticed; [she did a] good job of hiding and covering. But she said to me, “That’s why I wear my hair like this, because nobody can see the scales. And I keep my hair light because it blends in with the scales.” And that really hit me. I [said], “Why didn’t you tell me sooner? We can get this better.” But that was what her coping mechanism was. I think people come up with so many different things, and so many people really wouldn’t know. They’re so good at hiding it, but it really is affecting how she’s getting ready every day. That’s her style.
Laura Bush, DMSc, PA-C: Hair is important to young women.
Alexa Hetzel, MS, PA-C: Hair is important to everybody. Jennifer, what is your initial impression on this case?
Jennifer Conner, MPAS, PA-C: Apremilast is out. She’s already tried it [and] didn’t tolerate it well. I think she would be a great candidate for deucravacitinib if she wants to try another oral agent. She started with apremilast, so it sounds like she [may be] someone who likes an oral agent for an option. I would probably start there, then offer her biologics as well. We don’t know the rest of the story. Is she needle phobic? What does that look like? Deucravacitinib would be the next step for me with this patient, knowing the [adverse] effect profile is going to be much more tolerable for her.
Alexa Hetzel, MS, PA-C: Right. Terry, discuss with us the factors that influence your treatment options for her.
Terry Faleye, MPAS, PA-C: Just like Jennifer said, I would consider deucravacitinib for her. Just in itself, knowing the data—especially with scalp data deucravacitinib has and just seeing the level of improvement that patients see with it—I would consider it for her. She’s tried apremilast and didn’t have great success with that, and she didn’t want any of the [adverse] effects associated with it.
I would honestly even [ask about] how she [lives], too. Because even in the midst of it, I can sit back and say an oral agent would be awesome for her, but she may be someone [who doesn’t] want to take a pill every day. What if she [says she wants] wants it out of sight, out of mind? Maybe she is perfect for an injectable that she’s injecting once every 3 months or whatnot. I think it will truly be tailored to what fits her lifestyle, because I want her to be happy at the end of the day.
Alexa Hetzel, MS, PA-C: Yeah, somebody’s lifestyle [is a huge component]. If it’s going to be a daily pill, can they do that? I feel like a lot of people are on oral therapy for other things, like Lakshi mentioned, whether it’s high blood pressure or diabetes. We already assume most Americans are taking pills now, but are people good at being consistent? Is it easier to inject a biologic sometimes? I think that varies based on what you ask. That’s why it’s important to have a conversation.
Terry Faleye, MPAS, PA-C: And some patients don’t. Amazingly, even this time frame, there’s some people who [are] not on anything.
Alexa Hetzel, MS, PA-C: Or they can’t.
Terry Faleye, MPAS, PA-C: Yeah, and to go from the paradigm of never taking anything and all of a sudden—for the patient who doesn’t potentially have any high blood pressure or diabetes and this is the first time something major is going on with them, apart from having some type of infection—to now saying you have a chronic immune-mediated disease we need to get under control. To come to grips with the fact that we may have to pivot here could be a big shift to a daily usage. So for her, deucravacitinib, just like you said, would probably be a great option, especially transitioning already from an oral. But you never know, she may shock you.
Alexa Hetzel, MS, PA-C: Sometimes they do. Laura, is there any hesitation that you would have using an oral therapy as first line instead of just either [using] topical or biologic therapy?
Laura Bush, DMSc, PA-C: No, I wouldn’t hesitate to use deucravacitinib for her. I would hesitate to use methotrexate for her. I would not—that would be a definite no. Apremilast [already failed], so I would not hesitate at all, as long as she can swallow a pill—and she could swallow the apremilast, so she could swallow a pill. Believe it or not, there are people out there who can’t swallow a pill. So I would have no reservation. She’s young and able to do it, and I think [with her] lifestyle, a lot of us can manage 1 time a day. If it were twice a day, I would say probably not.
Alexa Hetzel, MS, PA-C: Right. Or, if she’s in graduate school and she’s living somewhere else and she can’t come into the office or can’t get a biologic shipped to her, sometimes that’s a little tricky. You want to keep those cold, so it’s much easier to sometimes give something that is room temperature stable.
Laura Bush, DMSc, PA-C: Yeah, good point. I also have a lot of patients [who] travel, so sometimes I’ll switch them to an oral agent because they’re traveling. A lot of young people are traveling these days…so it’s a good option to carry with you. You’re right.
Alexa Hetzel, MS, PA-C: Absolutely.
Transcript edited for clarity.
The Cutaneous Connection: An Inside Look of the Inclusive Atlas

Efficacy of Risankizumab For Severe Psoriasis

The Cutaneous Connection: Episode 31- Molecular Targeting of Psoriasis Biologics

IL-17 Pathway Linked to HIF-1-alpha Activation in Psoriasis

Dose Escalation of Biologic PsO Treatment in Japan
2 Commerce Drive Cranbury, NJ 08512
609-716-7777
Health Case Studies
(29 reviews)
Glynda Rees, British Columbia Institute of Technology
Rob Kruger, British Columbia Institute of Technology
Janet Morrison, British Columbia Institute of Technology
Copyright Year: 2017
Publisher: BCcampus
Language: English
Formats Available
Conditions of use.
Learn more about reviews.
Reviewed by Jessica Sellars, Medical assistant office instructor, Blue Mountain Community College on 10/11/23
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and... read more
Comprehensiveness rating: 5 see less
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and plan. There is an appendix to refer to as well if you are needing to find something specific quickly. I have been looking for something like this to help my students have a base to do their project on. This is the most comprehensive version I have found on the subject.
Content Accuracy rating: 5
This is a book compiled of medical case studies. It is very accurate and can be used to learn from great care and mistakes.
Relevance/Longevity rating: 5
This material is very relevant in this context. It also has plenty of individual case studies to utilize in many ways in all sorts of medical courses. This is a very useful textbook and it will continue to be useful for a very long time as you can still learn from each study even if medicine changes through out the years.
Clarity rating: 5
The author put a lot of thought into the ease of accessibility and reading level of the target audience. There is even a "how to use this resource" section which could be extremely useful to students.
Consistency rating: 5
The text follows a very consistent format throughout the book.
Modularity rating: 5
Each case study is individual broken up and in a group of similar case studies. This makes it extremely easy to utilize.
Organization/Structure/Flow rating: 5
The book is very organized and the appendix is through. It flows seamlessly through each case study.
Interface rating: 5
I had no issues navigating this book, It was clearly labeled and very easy to move around in.
Grammatical Errors rating: 5
I did not catch any grammar errors as I was going through the book
Cultural Relevance rating: 5
This is a challenging question for any medical textbook. It is very culturally relevant to those in medical or medical office degrees.
I have been looking for something like this for years. I am so happy to have finally found it.
Reviewed by Cindy Sun, Assistant Professor, Marshall University on 1/7/23
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and... read more
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and students. For faculty, the introduction section titled ‘How to use this resource’ and individual notes to educators before each case study contain application tips. An appendix overview lists key elements as issues / concepts, scenario context, and healthcare roles for each case study. For students, learning objectives are presented at the beginning of each case study to provide a framework of expectations.
The content is presented accurately and realistic.
The case studies read similar to ‘A Day In the Life of…’ with detailed intraprofessional communications similar to what would be overheard in patient care areas. The authors present not only the view of the patient care nurse, but also weave interprofessional vantage points through each case study by including patient interaction with individual professionals such as radiology, physician, etc.
In addition to objective assessment findings, the authors integrate standard orders for each diagnosis including medications, treatments, and tests allowing the student to incorporate pathophysiology components to their assessments.
Each case study is arranged in the same framework for consistency and ease of use.
This compilation of eight healthcare case studies focusing on new onset and exacerbation of prevalent diagnoses, such as heart failure, deep vein thrombosis, cancer, and chronic obstructive pulmonary disease advancing to pneumonia.
Each case study has a photo of the ‘patient’. Simple as this may seem, it gives an immediate mental image for the student to focus.
Interface rating: 4
As noted by previous reviewers, most of the links do not connect active web pages. This may be due to the multiple options for accessing this resource (pdf download, pdf electronic, web view, etc.).
Grammatical Errors rating: 4
A minor weakness that faculty will probably need to address prior to use is regarding specific term usages differences between Commonwealth countries and United States, such as lung sound descriptors as ‘quiet’ in place of ‘diminished’ and ‘puffers’ in place of ‘inhalers’.
The authors have provided a multicultural, multigenerational approach in selection of patient characteristics representing a snapshot of today’s patient population. Additionally, one case study focusing on heart failure is about a middle-aged adult, contrasting to the average aged patient the students would normally see during clinical rotations. This option provides opportunities for students to expand their knowledge on risk factors extending beyond age.
This resource is applicable to nursing students learning to care for patients with the specific disease processes presented in each case study or for the leadership students focusing on intraprofessional communication. Educators can assign as a supplement to clinical experiences or as an in-class application of knowledge.
Reviewed by Stephanie Sideras, Assistant Professor, University of Portland on 8/15/22
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five... read more
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five overarching learning objectives pulled from the Institute of Medicine core competencies will clearly resonate with any faculty familiar with Quality and Safety Education for Nurses curriculum.
The presentation of symptoms, treatments and management of the health alterations was accurate. Dialogue between the the interprofessional team was realistic. At times the formatting of lab results was confusing as they reflected reference ranges specific to the Canadian healthcare system but these occurrences were minimal and could be easily adapted.
The focus for learning from these case studies was communication - patient centered communication and interprofessional team communication. Specific details, such as drug dosing, was minimized, which increases longevity and allows for easy individualization of the case data.
While some vocabulary was specific to the Canadian healthcare system, overall the narrative was extremely engaging and easy to follow. Subjective case data from patient or provider were formatted in italics and identified as 'thoughts'. Objective and behavioral case data were smoothly integrated into the narrative.
The consistency of formatting across the eight cases was remarkable. Specific learning objectives are identified for each case and these remain consistent across the range of cases, varying only in the focus for the goals for each different health alterations. Each case begins with presentation of essential patient background and the progress across the trajectory of illness as the patient moves from location to location encountering different healthcare professionals. Many of the characters (the triage nurse in the Emergency Department, the phlebotomist) are consistent across the case situations. These consistencies facilitate both application of a variety of teaching methods and student engagement with the situated learning approach.
Case data is presented by location and begins with the patient's first encounter with the healthcare system. This allows for an examination of how specific trajectories of illness are manifested and how care management needs to be prioritized at different stages. This approach supports discussions of care transitions and the complexity of the associated interprofessional communication.
The text is well organized. The case that has two levels of complexity is clearly identified
The internal links between the table of contents and case specific locations work consistently. In the EPUB and the Digital PDF the external hyperlinks are inconsistently valid.
The grammatical errors were minimal and did not detract from readability
Cultural diversity is present across the cases in factors including race, ethnicity, socioeconomic status, family dynamics and sexual orientation.
The level of detail included in these cases supports a teaching approach to address all three spectrums of learning - knowledge, skills and attitudes - necessary for the development of competent practice. I also appreciate the inclusion of specific assessment instruments that would facilitate a discussion of evidence based practice. I will enjoy using these case to promote clinical reasoning discussions of data that is noticed and interpreted with the resulting prioritizes that are set followed by reflections that result from learner choices.
Reviewed by Chris Roman, Associate Professor, Butler University on 5/19/22
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various... read more
Comprehensiveness rating: 4 see less
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various learning strategies to be employed to leverage the cases for deeper student learning and application.
The narrative form of the cases is less subject to issues of accuracy than a more content-based book would be. That said, the cases are realistic and reasonable, avoiding being too mundane or too extreme.
These cases are narrative and do not include many specific mentions of drugs, dosages, or other aspects of clinical care that may grow/evolve as guidelines change. For this reason, the cases should be “evergreen” and can be modified to suit different types of learners.
Clarity rating: 4
The text is written in very accessible language and avoids heavy use of technical language. Depending on the level of learner, this might even be too simplistic and omit some details that would be needed for physicians, pharmacists, and others to make nuanced care decisions.
The format is very consistent with clear labeling at transition points.
The authors point out in the introductory materials that this text is designed to be used in a modular fashion. Further, they have built in opportunities to customize each cases, such as giving dates of birth at “19xx” to allow for adjustments based on instructional objectives, etc.
The organization is very easy to follow.
I did not identify any issues in navigating the text.
The text contains no grammatical errors, though the language is a little stiff/unrealistic in some cases.
Cases involve patients and members of the care team that are of varying ages, genders, and racial/ethnic backgrounds
Reviewed by Trina Larery, Assistant Professor, Pittsburg State University on 4/5/22
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand... read more
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand and apply to the classroom. The E-reader format included hyperlinks that bring the students to subsequent clinical studies.
Content Accuracy rating: 4
The treatments were explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse. The case studies were accurate in explanation. The DVT case study incorrectly identifies the location of the clot in the popliteal artery instead of in the vein.
The content is relevant to a variety of different types of health care providers and due to the general nature of the cases, will remain relevant over time. Updates should be made annually to the hyperlinks and to assure current standard of practice is still being met.
Clear, simple and easy to read.
Consistent with healthcare terminology and framework throughout all eight case studies.
The text is modular. Cases can be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point providing great flexibility. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
The book is well organized, presenting in a logical clear fashion. The appendix allows the student to move about the case study without difficulty.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change based on current guidelines. A few hyperlinks had "page not found".
Few grammatical errors were noted in text.
The case studies include people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. There are roughly 25 broken online links or "pages not found", care needs to be taken to update at least annually and assure links are valid and utilizing the most up to date information.
Reviewed by Benjamin Silverberg, Associate Professor/Clinician, West Virginia University on 3/24/22
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what... read more
Comprehensiveness rating: 3 see less
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what is going on where, especially since each case is largely conversation-based. Since this presents 8 cases (really 7 with one being expanded upon), there are many medical topics (and venues) that are not included. It's impossible to include every kind of situation, but I'd love to see inclusion of sexual health, renal pathology, substance abuse, etc.
Though there are differences in how care can be delivered based on personal style, changing guidelines, available supplies, etc, the medical accuracy seems to be high. I did not detect bias or industry influence.
Relevance/Longevity rating: 4
Medications are generally listed as generics, with at least current dosing recommendations. The text gives a picture of what care looks like currently, but will be a little challenging to update based on new guidelines (ie, it can be hard to find the exact page in which a medication is dosed/prescribed). Even if the text were to be a little out of date, an instructor can use that to point out what has changed (and why).
Clear text, usually with definitions of medical slang or higher-tier vocabulary. Minimal jargon and there are instances where the "characters" are sorting out the meaning as well, making it accessible for new learners, too.
Overall, the style is consistent between cases - largely broken up into scenes and driven by conversation rather than descriptions of what is happening.
There are 8 (well, again, 7) cases which can be reviewed in any order. Case #2 builds upon #1, which is intentional and a good idea, though personally I would have preferred one case to have different possible outcomes or even a recurrence of illness. Each scene within a case is reasonably short.
Organization/Structure/Flow rating: 4
These cases are modular and don't really build on concepts throughout. As previously stated, case #2 builds upon #1, but beyond that, there is no progression. (To be sure, the authors suggest using case #1 for newer learners and #2 for more advanced ones.) The text would benefit from thematic grouping, a longer introduction and debriefing for each case (there are learning objectives but no real context in medical education nor questions to reflect on what was just read), and progressively-increasing difficulty in medical complexity, ethics, etc.
I used the PDF version and had no interface issues. There are minimal photographs and charts. Some words are marked in blue but those did not seem to be hyperlinked anywhere.
No noticeable errors in grammar, spelling, or formatting were noted.
I appreciate that some diversity of age and ethnicity were offered, but this could be improved. There were Canadian Indian and First Nations patients, for example, as well as other characters with implied diversity, but there didn't seem to be any mention of gender diverse or non-heterosexual people, or disabilities. The cases tried to paint family scenes (the first patient's dog was fairly prominently mentioned) to humanize them. Including more cases would allow for more opportunities to include sex/gender minorities, (hidden) disabilities, etc.
The text (originally from 2017) could use an update. It could be used in conjunction with other Open Texts, as a compliment to other coursework, or purely by itself. The focus is meant to be on improving communication, but there are only 3 short pages at the beginning of the text considering those issues (which are really just learning objectives). In addition to adding more cases and further diversity, I personally would love to see more discussion before and after the case to guide readers (and/or instructors). I also wonder if some of the ambiguity could be improved by suggesting possible health outcomes - this kind of counterfactual comparison isn't possible in real life and could be really interesting in a text. Addition of comprehension/discussion questions would also be worthwhile.
Reviewed by Danielle Peterson, Assistant Professor, University of Saint Francis on 12/31/21
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare... read more
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare workers in acute hospital settings. The cases are primarily set in the inpatient hospital setting, so the bulk of the clinical information is basic emergency care and inpatient protocol: vitals, breathing, medication management, etc. The text provides a table of contents at opening of the text and a handy appendix at the conclusion of the text that outlines each case’s issue(s), scenario, and healthcare roles. No index or glossary present.
Although easy to update, it should be noted that the cases are taking place in a Canadian healthcare system. Terms may be unfamiliar to some students including “province,” “operating theatre,” “physio/physiotherapy,” and “porter.” Units of measurement used include Celsius and meters. Also, the issue of managed care, health insurance coverage, and length of stay is missing for American students. These are primary issues that dictate much of the healthcare system in the US and a primary job function of social workers, nurse case managers, and medical professionals in general. However, instructors that wish to add this to the case studies could do so easily.
The focus of this text is on healthcare communication which makes it less likely to become obsolete. Much of the clinical information is stable healthcare practice that has been standard of care for quite some time. Nevertheless, given the nature of text, updates would be easy to make. Hyperlinks should be updated to the most relevant and trustworthy sources and checked frequently for effectiveness.
The spacing that was used to note change of speaker made for ease of reading. Although unembellished and plain, I expect students to find this format easy to digest and interesting, especially since the script is appropriately balanced with ‘human’ qualities like the current TV shows and songs, the use of humor, and nonverbal cues.
A welcome characteristic of this text is its consistency. Each case is presented in a similar fashion and the roles of the healthcare team are ‘played’ by the same character in each of the scenarios. This allows students to see how healthcare providers prioritize cases and juggle the needs of multiple patients at once. Across scenarios, there was inconsistency in when clinical terms were hyperlinked.
The text is easily divisible into smaller reading sections. However, since the nature of the text is script-narrative format, if significant reorganization occurs, one will need to make sure that the communication of the script still makes sense.
The text is straightforward and presented in a consistent fashion: learning objectives, case history, a script of what happened before the patient enters the healthcare setting, and a script of what happens once the patient arrives at the healthcare setting. The authors use the term, “ideal interactions,” and I would agree that these cases are in large part, ‘best case scenarios.’ Due to this, the case studies are well organized, clear, logical, and predictable. However, depending on the level of student, instructors may want to introduce complications that are typical in the hospital setting.
The interface is pleasing and straightforward. With exception to the case summary and learning objectives, the cases are in narrative, script format. Each case study supplies a photo of the ‘patient’ and one of the case studies includes a link to a 3-minute video that introduces the reader to the patient/case. One of the highlights of this text is the use of hyperlinks to various clinical practices (ABG, vital signs, transfer of patient). Unfortunately, a majority of the links are broken. However, since this is an open text, instructors can update the links to their preference.
Although not free from grammatical errors, those that were noticed were minimal and did not detract from reading.
Cultural Relevance rating: 4
Cultural diversity is visible throughout the patients used in the case studies and includes factors such as age, race, socioeconomic status, family dynamics, and sexual orientation. A moderate level of diversity is noted in the healthcare team with some stereotypes: social workers being female, doctors primarily male.
As a social work instructor, I was grateful to find a text that incorporates this important healthcare role. I would have liked to have seen more content related to advance directives, mediating decision making between the patient and care team, emotional and practical support related to initial diagnosis and discharge planning, and provision of support to colleagues, all typical roles of a medical social worker. I also found it interesting that even though social work was included in multiple scenarios, the role was only introduced on the learning objectives page for the oncology case.
Reviewed by Crystal Wynn, Associate Professor, Virginia State University on 7/21/21
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied... read more
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied health care team members are represented within the case study. Key terms appear throughout the case study textbook and readers are able to click on a hyperlink which directs them to the definition and an explanation of the key term.
Content is accurate, error-free and unbiased.
The content is up-to-date, but not in a way that will quickly make the text obsolete within a short period of time. The text is written and/or arranged in such a way that necessary updates will be relatively easy and straightforward to implement.
The text is written in lucid, accessible prose, and provides adequate context for any jargon/technical terminology used
The text is internally consistent in terms of terminology and framework.
The text is easily and readily divisible into smaller reading sections that can be assigned at different points within the course. Each case can be divided into a chronic disease state unit, which will allow the reader to focus on one section at a time.
Organization/Structure/Flow rating: 3
The topics in the text are presented in a logical manner. Each case provides an excessive amount of language that provides a description of the case. The cases in this text reads more like a novel versus a clinical textbook. The learning objectives listed within each case should be in the form of questions or activities that could be provided as resources for instructors and teachers.
Interface rating: 3
There are several hyperlinks embedded within the textbook that are not functional.
The text contains no grammatical errors.
Cultural Relevance rating: 3
The text is not culturally insensitive or offensive in any way. More examples of cultural inclusiveness is needed throughout the textbook. The cases should be indicative of individuals from a variety of races and ethnicities.
Reviewed by Rebecca Hillary, Biology Instructor, Portland Community College on 6/15/21
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health... read more
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health care program. I read the textbook in E-reader format and this includes hyperlinks that bring the students to subsequent clinical study if the book is being used in a clinical classroom. This book is significantly more comprehensive in its approach from other case studies I have read because it provides a bird’s eye view of the many clinicians, technicians, and hospital staff working with one patient. The book also provides real time measurements for patients that change as they travel throughout the hospital until time of discharge.
Each case gave an accurate sense of the chaos that would be present in an emergency situation and show how the conditions affect the practitioners as well as the patients. The reader gets an accurate big picture--a feel for each practitioner’s point of view as well as the point of view of the patient and the patient’s family as the clock ticks down and the patients are subjected to a number of procedures. The clinical information contained in this textbook is all in hyperlinks containing references to clinical skills open text sources or medical websites. I did find one broken link on an external medical resource.
The diseases presented are relevant and will remain so. Some of the links are directly related to the Canadian Medical system so they may not be applicable to those living in other regions. Clinical links may change over time but the text itself will remain relevant.
Each case study clearly presents clinical data as is it recorded in real time.
Each case study provides the point of view of several practitioners and the patient over several days. While each of the case studies covers different pathology they all follow this same format, several points of view and data points, over a number of days.
The case studies are divided by days and this was easy to navigate as a reader. It would be easy to assign one case study per body system in an Anatomy and Physiology course, or to divide them up into small segments for small in class teaching moments.
The topics are presented in an organized way showing clinical data over time and each case presents a large number of view points. For example, in the first case study, the patient is experiencing difficulty breathing. We follow her through several days from her entrance to the emergency room. We meet her X Ray Technicians, Doctor, Nurses, Medical Assistant, Porter, Physiotherapist, Respiratory therapist, and the Lab Technicians running her tests during her stay. Each practitioner paints the overall clinical picture to the reader.
I found the text easy to navigate. There were not any figures included in the text, only clinical data organized in charts. The figures were all accessible via hyperlink. Some figures within the textbook illustrating patient scans could have been helpful but I did not have trouble navigating the links to visualize the scans.
I did not see any grammatical errors in the text.
The patients in the text are a variety of ages and have a variety of family arrangements but there is not much diversity among the patients. Our seven patients in the eight case studies are mostly white and all cis gendered.
Some of the case studies, for example the heart failure study, show clinical data before and after drug treatments so the students can get a feel for mechanism in physiological action. I also liked that the case studies included diet and lifestyle advice for the patients rather than solely emphasizing these pharmacological interventions. Overall, I enjoyed reading through these case studies and I plan to utilize them in my Anatomy and Physiology courses.
Reviewed by Richard Tarpey, Assistant Professor, Middle Tennessee State University on 5/11/21
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate... read more
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate for entry-level health care students. The book includes important health problems, but I would like to see coverage of at least one more chronic/lifestyle issue such as diabetes. The book covers adult issues only.
Content is accurate without bias
The content of the book is relevant and up-to-date. It addresses conditions that are prevalent in today's population among adults. There are no pediatric cases, but this does not significantly detract from the usefulness of the text. The format of the book lends to easy updating of data or information.
The book is written with clarity and is easy to read. The writing style is accessible and technical terminology is explained with links to more information.
Consistency is present. Lack of consistency is typically a problem with case study texts, but this book is consistent with presentation, format, and terminology throughout each of the eight cases.
The book has high modularity. Each of the case studies can be used independently from the others providing flexibility. Additionally, each case study can be partitioned for specific learning objectives based on the learning objectives of the course or module.
The book is well organized, presenting students conceptually with differing patient flow patterns through a hospital. The patient information provided at the beginning of each case is a wonderful mechanism for providing personal context for the students as they consider the issues. Many case studies focus on the problem and the organization without students getting a patient's perspective. The patient perspective is well represented in these cases.
The navigation through the cases is good. There are some terminology and procedure hyperlinks within the cases that do not work when accessed. This is troubling if you intend to use the text for entry-level health care students since many of these links are critical for a full understanding of the case.
There are some non-US variants of spelling and a few grammatical errors, but these do not detract from the content of the messages of each case.
The book is inclusive of differing backgrounds and perspectives. No insensitive or offensive references were found.
I like this text for its application flexibility. The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology. The content is also helpful for the identification of healthcare administration managerial issues for students to consider. The book has many applications.
Reviewed by Paula Baldwin, Associate Professor/Communication Studies, Western Oregon University on 5/10/21
The different case studies fall on a range, from crisis care to chronic illness care. read more
The different case studies fall on a range, from crisis care to chronic illness care.
The contents seems to be written as they occurred to represent the most complete picture of each medical event's occurence.
These case studies are from the Canadian medical system, but that does not interfere with it's applicability.
It is written for a medical audience, so the terminology is mostly formal and technical.
Some cases are shorter than others and some go in more depth, but it is not problematic.
The eight separate case studies is the perfect size for a class in the quarter system. You could combine this with other texts, videos or learning modalities, or use it alone.
As this is a case studies book, there is not a need for a logical progression in presentation of topics.
No problems in terms of interface.
I have not seen any grammatical errors.
I did not see anything that was culturally insensitive.
I used this in a Health Communication class and it has been extraordinarily successful. My studies are analyzing the messaging for the good, the bad, and the questionable. The case studies are widely varied and it gives the class insights into hospital experiences, both front and back stage, that they would not normally be able to examine. I believe that because it is based real-life medical incidents, my students are finding the material highly engaging.
Reviewed by Marlena Isaac, Instructor, Aiken Technical College on 4/23/21
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with... read more
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with a situation in clinical they are not surprised and now how to move through it effectively.
The case studies provided accurate information that relates to the named disease.
It is relevant to health care studies and the development of critical thinking.
Cases are straightforward with great clinical information.
Clinical information is provided concisely.
Appropriate for clinical case study.
Presented to facilitate information gathering.
Takes a while to navigate in the browser.
Cultural Relevance rating: 1
Text lacks adequate representation of minorities.
Reviewed by Kim Garcia, Lecturer III, University of Texas Rio Grande Valley on 11/16/20
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at... read more
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at different levels of clinical knowledge. The human element of both patient and health care provider is well captured. The cases are presented with a focus on interprofessional interaction and collaboration, more so than teaching medical content.
Content is accurate and un-biased. No errors noted. Most diagnostic and treatment information is general so it will remain relevant over time. The content of these cases is more appropriate for teaching interprofessional collaboration and less so for teaching the medical care for each diagnosis.
The content is relevant to a variety of different types of health care providers (nurses, radiologic technicians, medical laboratory personnel, etc) and due to the general nature of the cases, will remain relevant over time.
Easy to read. Clear headings are provided for sections of each case study and these section headings clearly tell when time has passed or setting has changed. Enough description is provided to help set the scene for each part of the case. Much of the text is written in the form of dialogue involving patient, family and health care providers, making it easy to adapt for role play. Medical jargon is limited and links for medical terms are provided to other resources that expound on medical terms used.
The text is consistent in structure of each case. Learning objectives are provided. Cases generally start with the patient at home and move with the patient through admission, testing and treatment, using a variety of healthcare services and encountering a variety of personnel.
The text is modular. Cases could be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
Each case follows a patient in a logical, chronologic fashion. A clear table of contents and appendix are provided which allows the user to quickly locate desired content. It would be helpful if the items in the table of contents and appendix were linked to the corresponding section of the text.
The hyperlinks to content outside this book work, however using the back arrow on your browser returns you to the front page of the book instead of to the point at which you left the text. I would prefer it if the hyperlinks opened in a new window or tab so closing that window or tab would leave you back where you left the text.
No grammatical errors were noted.
The text is culturally inclusive and appropriate. Characters, both patients and care givers are of a variety of races, ethnicities, ages and backgrounds.
I enjoyed reading the cases and reviewing this text. I can think of several ways in which I will use this content.
Reviewed by Raihan Khan, Instructor/Assistant Professor, James Madison University on 11/3/20
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients. read more
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients.
The health information contained in the textbook is mostly accurate.
I think the book is written focusing on the current culture and health issues faced by the patients. To keep the book relevant in the future, the contexts especially the culture/lifestyle/health care modalities, etc. would need to be updated regularly.
The language is pretty simple, clear, and easy to read.
There is no complaint about consistency. One of the main issues of writing a book, consistency was well managed by the authors.
The book is easy to explore based on how easy the setup is. Students can browse to the specific section that they want to read without much hassle of finding the correct information.
The organization is simple but effective. The authors organized the book based on what can happen in a patient's life and what possible scenarios students should learn about the disease. From that perspective, the book does a good job.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change that is beyond the author's control. It's frustrating for the reader when the external link shows no information.
The book is free of any major language and grammatical errors.
The book might do a little better in cultural competency. e.g. Last name Singh is mainly for Sikh people. In the text Harj and Priya Singh are Muslim. the authors can consult colleagues who are more familiar with those cultures and revise some cultural aspects of the cases mentioned in the book.
The book is a nice addition to the open textbook world. Hope to see more health issues covered by the book.
Reviewed by Ryan Sheryl, Assistant Professor, California State University, Dominguez Hills on 7/16/20
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality... read more
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality improvement, and informatics. While the case studies do not cover all medical conditions or bodily systems, the book is thorough in conveying details of various patients and medical team members in a hospital environment. Rather than an index or glossary at the end of the text, it contains links to outside websites for more information on medical tests and terms referenced in the cases.
The content provided is reflective of best practices in patient care, interdisciplinary collaboration, and communication at the time of publication. It is specifically accurate for the context of hospitals in Canada. The links provided throughout the text have the potential to supplement with up-to-date descriptions and definitions, however, many of them are broken (see notes in Interface section).
The content of the case studies reflects the increasingly complex landscape of healthcare, including a variety of conditions, ages, and personal situations of the clients and care providers. The text will require frequent updating due to the rapidly changing landscape of society and best practices in client care. For example, a future version may include inclusive practices with transgender clients, or address ways medical racism implicitly impacts client care (see notes in Cultural Relevance section).
The text is written clearly and presents thorough, realistic details about working and being treated in an acute hospital context.
The text is very straightforward. It is consistent in its structure and flow. It uses consistent terminology and follows a structured framework throughout.
Being a series of 8 separate case studies, this text is easily and readily divisible into smaller sections. The text was designed to be taken apart and used piece by piece in order to serve various learning contexts. The parts of each case study can also be used independently of each other to facilitate problem solving.
The topics in the case studies are presented clearly. The structure of each of the case studies proceeds in a similar fashion. All of the cases are set within the same hospital so the hospital personnel and service providers reappear across the cases, giving a textured portrayal of the experiences of the various service providers. The cases can be used individually, or one service provider can be studied across the various studies.
The text is very straightforward, without complex charts or images that could become distorted. Many of the embedded links are broken and require updating. The links that do work are a very useful way to define and expand upon medical terms used in the case studies.
Grammatical errors are minimal and do not distract from the flow of the text. In one instance the last name Singh is spelled Sing, and one patient named Fred in the text is referred to as Frank in the appendix.
The cases all show examples of health care personnel providing compassionate, client-centered care, and there is no overt discrimination portrayed. Two of the clients are in same-sex marriages and these are shown positively. It is notable, however, that the two cases presenting people of color contain more negative characteristics than the other six cases portraying Caucasian people. The people of color are the only two examples of clients who smoke regularly. In addition, the Indian client drinks and is overweight, while the First Nations client is the only one in the text to have a terminal diagnosis. The Indian client is identified as being Punjabi and attending a mosque, although there are only 2% Muslims in the Punjab province of India. Also, the last name Singh generally indicates a person who is a Hindu or Sikh, not Muslim.
Reviewed by Monica LeJeune, RN Instructor, LSUE on 4/24/20
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process. read more
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process.
Accurately presents health scenarios with real life assessment techniques and patient outcomes.
Relevant to nursing practice.
Clearly written and easily understood.
Consistent with healthcare terminology and framework
Has a good reading flow.
Topics presented in logical fashion
Easy to read.
No grammatical errors noted.
Text is not culturally insensitive or offensive.
Good book to have to teach nursing students.
Reviewed by april jarrell, associate professor, J. Sargeant Reynolds Community College on 1/7/20
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process. read more
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process.
The content is accurate and evidence based. There is no bias noted
The content in the text is relevant, up to date for nursing students. It will be easy to update content as needed because the framework allows for addition to the content.
The text is clear and easy to understand.
Framework and terminology is consistent throughout the text; the case study is a continual and takes the student on a journey with the patient. Great for learning!
The case studies can be easily divided into smaller sections to allow for discussions, and weekly studies.
The text and content progress in a logical, clear fashion allowing for progression of learning.
No interface issues noted with this text.
No grammatical errors noted in the text.
No racial or culture insensitivity were noted in the text.
I would recommend this text be used in nursing schools. The use of case studies are helpful for students to learn and practice the nursing process.
Reviewed by Lisa Underwood, Practical Nursing Instructor, NTCC on 12/3/19
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own... read more
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own set of learning objectives that can be tweaked to fit several allied health courses. Although the case studies are designed around the Canadian Healthcare System, they are quite easily adaptable to fit most any modern, developed healthcare system.
Content Accuracy rating: 3
Overall, the text is quite accurate. There is one significant error that needs to be addressed. It is located in the DVT case study. In the study, a popliteal artery clot is mislabeled as a DVT. DVTs are located in veins, not in arteries. That said, the case study on the whole is quite good. This case study could be used as a learning tool in the classroom for discussion purposes or as a way to test student understanding of DVTs, on example might be, "Can they spot the error?"
At this time, all of the case studies within the text are current. Healthcare is an ever evolving field that rests on the best evidence based practice. Keeping that in mind, educators can easily adapt the studies as the newest evidence emerges and changes practice in healthcare.
All of the case studies are well written and easy to understand. The text includes several hyperlinks and it also highlights certain medical terminology to prompt readers as a way to enhance their learning experience.
Across the text, the language, style, and format of the case studies are completely consistent.
The text is divided into eight separate case studies. Each case study may be used independently of the others. All case studies are further broken down as the focus patient passes through each aspect of their healthcare system. The text's modularity makes it possible to use a case study as individual work, group projects, class discussions, homework or in a simulation lab.
The case studies and the diagnoses that they cover are presented in such a way that educators and allied health students can easily follow and comprehend.
The book in itself is free of any image distortion and it prints nicely. The text is offered in a variety of digital formats. As noted in the above reviews, some of the hyperlinks have navigational issues. When the reader attempts to access them, a "page not found" message is received.
There were minimal grammatical errors. Some of which may be traced back to the differences in our spelling.
The text is culturally relevant in that it includes patients from many different backgrounds and ethnicities. This allows educators and students to explore cultural relevance and sensitivity needs across all areas in healthcare. I do not believe that the text was in any way insensitive or offensive to the reader.
By using the case studies, it may be possible to have an open dialogue about the differences noted in healthcare systems. Students will have the ability to compare and contrast the Canadian healthcare system with their own. I also firmly believe that by using these case studies, students can improve their critical thinking skills. These case studies help them to "put it all together".
Reviewed by Melanie McGrath, Associate Professor, TRAILS on 11/29/19
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case. read more
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case.
I saw no areas of inaccuracy
As in all healthcare texts, treatments and/or tests will change frequently. However, everything is currently up-to-date thus it should be a good reference for several years.
Each case is written so that any level of healthcare student would understand. Hyperlinks in the text is also very helpful.
All of the cases are written in a similar fashion.
Although not structured as a typical text, each case is easily assigned as a stand-alone.
Each case is organized clearly in an appropriate manner.
I did not see any issues.
I did not see any grammatical errors
The text seemed appropriately inclusive. There are no pediatric cases and no cases of intellectually-impaired patients, but those types of cases introduce more advanced problem-solving which perhaps exceed the scope of the text. May be a good addition to the text.
I found this text to be an excellent resource for healthcare students in a variety of fields. It would be best utilized in inter professional courses to help guide discussion.
Reviewed by Lynne Umbarger, Clinical Assistant Professor, Occupational Therapy, Emory and Henry College on 11/26/19
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational... read more
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational purposes. The material was easily understood by the students but challenging enough for classroom discussion. There are no mentions in the book about occupational therapy, but it is easy enough to add a couple words and make inclusion simple.
Very nice lab values are provided in the case study, making it more realistic for students.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
The material is easily understood by allied health students. The cases have links to additional learning materials for concepts that may be less familiar or should be explored further in a particular health field.
The language used in the book is consistent between cases. The framework is the same with each case which makes it easier to locate areas that would be of interest to a particular allied health profession.
The case studies are comprehensive but well-organized. They are short enough to be useful for class discussion or a full-blown assignment. The students seem to understand the material and have not expressed that any concepts or details were missing.
Each case is set up like the other cases. There are learning objectives at the beginning of each case to facilitate using the case, and it is easy enough to pull out material to develop useful activities and assignments.
There is a quick chart in the Appendix to allow the reader to determine the professions involved in each case as well as the pertinent settings and diagnoses for each case study. The contents are easy to access even while reading the book.
As a person who attends carefully to grammar, I found no errors in all of the material I read in this book.
There are a greater number of people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book. With each case, I could easily picture the person in the case. This book appears to be Canadian and more inclusive than most American books.
I was able to use this book the first time I accessed it to develop a classroom activity for first-year occupational therapy students and a more comprehensive activity for second-year students. I really appreciate the links to a multitude of terminology and medical lab values/issues for each case. I will keep using this book.
Reviewed by Cindy Krentz, Assistant Professor, Metropolitan State University of Denver on 6/15/19
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some... read more
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some understanding of the patient's background. I think it could benefit from having a glossary. I liked how the authors included the vital signs in an easily readable bar. I would have liked to see the labs also highlighted like this. I also felt that it would have been good written in a 'what would you do next?' type of case study.
The book is very accurate in language, what tests would be prudent to run and in the day in the life of the hospital in all cases. One inaccuracy is that the authors called a popliteal artery clot a DVT. The rest of the DVT case study was great, though, but the one mistake should be changed.
The book is up to date for now, but as tests become obsolete and new equipment is routinely used, the book ( like any other health textbook) will need to be updated. It would be easy to change, however. All that would have to happen is that the authors go in and change out the test to whatever newer, evidence-based test is being utilized.
The text is written clearly and easy to understand from a student's perspective. There is not too much technical jargon, and it is pretty universal when used- for example DVT for Deep Vein Thrombosis.
The book is consistent in language and how it is broken down into case studies. The same format is used for highlighting vital signs throughout the different case studies. It's great that the reader does not have to read the book in a linear fashion. Each case study can be read without needing to read the others.
The text is broken down into eight case studies, and within the case studies is broken down into days. It is consistent and shows how the patient can pass through the different hospital departments (from the ER to the unit, to surgery, to home) in a realistic manner. The instructor could use one or more of the case studies as (s)he sees fit.
The topics are eight different case studies- and are presented very clearly and organized well. Each one is broken down into how the patient goes through the system. The text is easy to follow and logical.
The interface has some problems with the highlighted blue links. Some of them did not work and I got a 'page not found' message. That can be frustrating for the reader. I'm wondering if a glossary could be utilized (instead of the links) to explain what some of these links are supposed to explain.
I found two or three typos, I don't think they were grammatical errors. In one case I think the Canadian spelling and the United States spelling of the word are just different.
This is a very culturally competent book. In today's world, however, one more type of background that would merit delving into is the trans-gender, GLBTQI person. I was glad that there were no stereotypes.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. Since we are becoming more interprofessional, I liked that we saw what the phlebotomist and other ancillary personnel (mostly different technicians) did. I think that it could become even more interdisciplinary so colleges and universities could have more interprofessional education- courses or simulations- with the addition of the nurse using social work, nutrition, or other professional health care majors.
Reviewed by Catherine J. Grott, Interim Director, Health Administration Program, TRAILS on 5/5/19
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this. read more
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this.
The book is accurate, however it has numerous broken online links.
Relevance/Longevity rating: 3
The content is very relevant, but some links are out-dated. For example, WHO Guidelines for Safe Surgery 2009 (p. 186) should be updated.
The book is written in clear and concise language. The side stories about the healthcare workers make the text interesting.
The book is consistent in terms of terminology and framework. Some terms that are emphasized in one case study are not emphasized (with online links) in the other case studies. All of the case studies should have the same words linked to online definitions.
Modularity rating: 3
The book can easily be parsed out if necessary. However, the way the case studies have been written, it's evident that different authors contributed singularly to each case study.
The organization and flow are good.
Interface rating: 1
There are numerous broken online links and "pages not found."
The grammar and punctuation are correct. There are two errors detected: p. 120 a space between the word "heart" and the comma; also a period is needed after Dr (p. 113).
I'm not quite sure that the social worker (p. 119) should comment that the patient and partner are "very normal people."
There are roughly 25 broken online links or "pages not found." The BC & Canadian Guidelines (p. 198) could also include a link to US guidelines to make the text more universal . The basilar crackles (p. 166) is very good. Text could be used compare US and Canadian healthcare. Text could be enhanced to teach "soft skills" and interdepartmental communication skills in healthcare.
Reviewed by Lindsey Henry, Practical Nursing Instructor, Fletcher on 5/1/19
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning... read more
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning objectives, which were effectively met in the readings.
As a seasoned nurse, I believe that the content regarding pathophysiology and treatments used in the case studies were accurate. I really appreciated how many of the treatments were also explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse.
The case studies are up to date and correlate with the current time period. They are easily understood.
I really loved how several important medical terms, including specific treatments were highlighted to alert the reader. Many interventions performed were also explained further, which is great to enhance learning for the nursing student or novice nurse. Also, with each scenario, a background and history of the patient is depicted, as well as the perspectives of the patient, patients family member, and the primary nurse. This really helps to give the reader a full picture of the day in the life of a nurse or a patient, and also better facilitates the learning process of the reader.
These case studies are consistent. They begin with report, the patient background or updates on subsequent days, and follow the patients all the way through discharge. Once again, I really appreciate how this book describes most if not all aspects of patient care on a day to day basis.
Each case study is separated into days. While they can be divided to be assigned at different points within the course, they also build on each other. They show trends in vital signs, what happens when a patient deteriorates, what happens when they get better and go home. Showing the entire process from ER admit to discharge is really helpful to enhance the students learning experience.
The topics are all presented very similarly and very clearly. The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough.
The book is very easy to navigate, prints well on paper, and is not distorted or confusing.
I did not see any grammatical errors.
Each case study involves a different type of patient. These differences include race, gender, sexual orientation and medical backgrounds. I do not feel the text was offensive to the reader.
I teach practical nursing students and after reading this book, I am looking forward to implementing it in my classroom. Great read for nursing students!
Reviewed by Leah Jolly, Instructor, Clinical Coordinator, Oregon Institute of Technology on 4/10/19
Good variety of cases and pathologies covered. read more
Good variety of cases and pathologies covered.
Content Accuracy rating: 2
Some examples and scenarios are not completely accurate. For example in the DVT case, the sonographer found thrombus in the "popliteal artery", which according to the book indicated presence of DVT. However in DVT, thrombus is located in the vein, not the artery. The patient would also have much different symptoms if located in the artery. Perhaps some of these inaccuracies are just typos, but in real-life situations this simple mistake can make a world of difference in the patient's course of treatment and outcomes.
Good examples of interprofessional collaboration. If only it worked this way on an every day basis!
Clear and easy to read for those with knowledge of medical terminology.
Good consistency overall.
Broken up well.
Topics are clear and logical.
Would be nice to simply click through to the next page, rather than going through the table of contents each time.
Minor typos/grammatical errors.
No offensive or insensitive materials observed.
Reviewed by Alex Sargsyan, Doctor of Nursing Practice/Assistant Professor , East Tennessee State University on 10/8/18
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study. read more
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study.
Overall the book is accurately depicting the clinical environment. There are numerous references to external sites. While most of them are correct, some of them are not working. For example Homan’s test link is not working "404 error"
Book is relevant in its current version and can be used in undergraduate and graduate classes. That said, the longevity of the book may be limited because of the character of the clinical education. Clinical guidelines change constantly and it may require a major update of the content.
Cases are written very clearly and have realistic description of an inpatient setting.
The book is easy to read and consistent in the language in all eight cases.
The cases are very well written. Each case is subdivided into logical segments. The segments reflect different setting where the patient is being seen. There is a flow and transition between the settings.
Book has eight distinct cases. This is a great format for a book that presents distinct clinical issues. This will allow the students to have immersive experiences and gain better understanding of the healthcare environment.
Book is offered in many different formats. Besides the issues with the links mentioned above, overall navigation of the book content is very smooth.
Book is very well written and has no grammatical errors.
Book is culturally relevant. Patients in the case studies come different cultures and represent diverse ethnicities.
Reviewed by Justin Berry, Physical Therapist Assistant Program Director, Northland Community and Technical College, East Grand Forks, MN on 8/2/18
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles,... read more
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles, interprofessional roles, when to initiate communication with other healthcare practitioners due to a change in patient status, and treatment ideas. Some additional patient information, such as lab values, would have been beneficial to include.
Case study information is accurate and unbiased.
Content is up to date. The case studies are written in a way so that they will not be obsolete soon, even with changes in healthcare.
The case studies are well written, and can be utilized for a variety of classroom assignments, discussions, and projects. Some additional lab value information for each patient would have been a nice addition.
The case studies are consistently organized to make it easy for the reader to determine the framework.
The text is broken up into eight different case studies for various patient diagnoses. This design makes it highly modular, and would be easy to assign at different points of a course.
The flow of the topics are presented consistently in a logical manner. Each case study follows a patient chronologically, making it easy to determine changes in patient status and treatment options.
The text is free of interface issues, with no distortion of images or charts.
The text is not culturally insensitive or offensive in any way. Patients are represented from a variety of races, ethnicities, and backgrounds
This book would be a good addition for many different health programs.
Reviewed by Ann Bell-Pfeifer, Instructor/Program Director, Minnesota State Community and Technical College on 5/21/18
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical... read more
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical laboratory technologists, medical radiology technologists, and respiratory therapists and their roles in caring for patients. Most of the overview is accurate. One suggestion is to provide an embedded radiologist interpretation of the exams which are performed which lead to the patients diagnosis.
Overall the book is accurate. Would like to see updates related to the addition of direct radiography technology which is commonly used in the hospital setting.
Many aspects of medicine will remain constant. The case studies seem fairly accurate and may be relevant for up to 3 years. Since technology changes so quickly in medicine, the CT and x-ray components may need minor updates within a few years.
The book clarity is excellent.
The case stories are consistent with each scenario. It is easy to follow the structure and learn from the content.
The book is quite modular. It is easy to break it up into cases and utilize them individually and sequentially.
The cases are listed by disease process and follow a logical flow through each condition. They are easy to follow as they have the same format from the beginning to the end of each case.
The interface seems seamless. Hyperlinks are inserted which provide descriptions and references to medical procedures and in depth definitions.
The book is free of most grammatical errors. There is a place where a few words do not fit the sentence structure and could be a typo.
The book included all types of relationships and ethnic backgrounds. One type which could be added is a transgender patient.
I think the book was quite useful for a variety of health care professionals. The authors did an excellent job of integrating patient cases which could be applied to the health care setting. The stories seemed real and relevant. This book could be used to teach health care professionals about integrated care within the emergency department.
Reviewed by Shelley Wolfe, Assistant Professor, Winona State University on 5/21/18
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should... read more
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should be noted that the authors include a statement that conveys that this text is not like traditional textbooks and is not meant to be read in a linear fashion. This allows the educator more flexibility to use the text as a supplement to enhance learning opportunities.
The content of the text appears accurate and unbiased. The “five overarching learning objectives” provide a clear aim of the text and the educator is able to glean how these objectives are captured into each of the case studies. While written for the Canadian healthcare system, this text is easily adaptable to the American healthcare system.
Overall, the content is up-to-date and the case studies provide a variety of uses that promote longevity of the text. However, not all of the blue font links (if using the digital PDF version) were still in working order. I encountered links that led to error pages or outdated “page not found” websites. While the links can be helpful, continued maintenance of these links could prove time-consuming.
I found the text easy to read and understand. I enjoyed that the viewpoints of all the different roles (patient, nurse, lab personnel, etc.) were articulated well and allowed the reader to connect and gain appreciation of the entire healthcare team. Medical jargon was noted to be appropriate for the intended audience of this text.
The terminology and organization of this text is consistent.
The text is divided into 8 case studies that follow a similar organizational structure. The case studies can further be divided to focus on individual learning objectives. For example, the case studies could be looked at as a whole for discussing communication or could be broken down into segments to focus on disease risk factors.
The case studies in this text follow a similar organizational structure and are consistent in their presentation. The flow of individual case studies is excellent and sets the reader on a clear path. As noted previously, this text is not meant to be read in a linear fashion.
This text is available in many different forms. I chose to review the text in the digital PDF version in order to use the embedded links. I did not encounter significant interface issues and did not find any images or features that would distract or confuse a reader.
No significant grammatical errors were noted.
The case studies in this text included patients and healthcare workers from a variety of backgrounds. Educators and students will benefit from expanding the case studies to include discussions and other learning opportunities to help develop culturally-sensitive healthcare providers.
I found the case studies to be very detailed, yet written in a way in which they could be used in various manners. The authors note a variety of ways in which the case studies could be employed with students; however, I feel the authors could also include that the case studies could be used as a basis for simulated clinical experiences. The case studies in this text would be an excellent tool for developing interprofessional communication and collaboration skills in a variety healthcare students.
Reviewed by Darline Foltz, Assistant Professor, University of Cincinnati - Clermont College on 3/27/18
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks... read more
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks Clinical Procedures for Safer Patient Care and Anatomy and Physiology: OpenStax" as noted by the authors.
The book appears to be accurate. Although one of the learning outcomes is as follows: "Demonstrate an understanding of the Canadian healthcare delivery system.", I did not find anything that is ONLY specific to the Canadian healthcare delivery system other than some of the terminology, i.e. "porter" instead of "transporter" and a few french words. I found this to make the book more interesting for students rather than deter from it. These are patient case studies that are relevant in any country.
The content is up-to-date. Changes in medical science may occur, i.e. a different test, to treat a diagnosis that is included in one or more of the case studies, however, it would be easy and straightforward to implement these changes.
This book is written in lucid, accessible prose. The technical/medical terminology that is used is appropriate for medical and allied health professionals. Something that would improve this text would to provide a glossary of terms for the terms in blue font.
This book is consistent with current medical terminology
This text is easily divided into each of the 6 case studies. The case studies can be used singly according to the body system being addressed or studied.
Because this text is a collection of case studies, flow doesn't pertain, however the organization and structure of the case studies are excellent as they are clear and easy to read.
There are no distractions in this text that would distract or confuse the reader.
I did not identify any grammatical errors.
This text is not culturally insensitive or offensive in any way and uses patients and healthcare workers that are of a variety of races, ethnicities and backgrounds.
I believe that this text would not only be useful to students enrolled in healthcare professions involved in direct patient care but would also be useful to students in supporting healthcare disciplines such as health information technology and management, medical billing and coding, etc.
Table of Contents
- Introduction
Case Study #1: Chronic Obstructive Pulmonary Disease (COPD)
- Learning Objectives
- Patient: Erin Johns
- Emergency Room
Case Study #2: Pneumonia
- Day 0: Emergency Room
- Day 1: Emergency Room
- Day 1: Medical Ward
- Day 2: Medical Ward
- Day 3: Medical Ward
- Day 4: Medical Ward
Case Study #3: Unstable Angina (UA)
- Patient: Harj Singh
Case Study #4: Heart Failure (HF)
- Patient: Meryl Smith
- In the Supermarket
- Day 0: Medical Ward
Case Study #5: Motor Vehicle Collision (MVC)
- Patient: Aaron Knoll
- Crash Scene
- Operating Room
- Post Anaesthesia Care Unit (PACU)
- Surgical Ward
Case Study #6: Sepsis
- Patient: George Thomas
- Sleepy Hollow Care Facility
Case Study #7: Colon Cancer
- Patient: Fred Johnson
- Two Months Ago
- Pre-Surgery Admission
Case Study #8: Deep Vein Thrombosis (DVT)
- Patient: Jamie Douglas
Appendix: Overview About the Authors
Ancillary Material
About the book.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
The case studies can be used online in a learning management system, in a classroom discussion, in a printed course pack or as part of a textbook created by the instructor. This flexibility is intentional and allows the educator to choose how best to convey the concepts presented in each case to the learner.
Because these case studies were primarily developed for an electronic healthcare system, they are based predominantly in an acute healthcare setting. Educators can augment each case study to include primary healthcare settings, outpatient clinics, assisted living environments, and other contexts as relevant.
About the Contributors
Glynda Rees teaches at the British Columbia Institute of Technology (BCIT) in Vancouver, British Columbia. She completed her MSN at the University of British Columbia with a focus on education and health informatics, and her BSN at the University of Cape Town in South Africa. Glynda has many years of national and international clinical experience in critical care units in South Africa, the UK, and the USA. Her teaching background has focused on clinical education, problem-based learning, clinical techniques, and pharmacology.
Glynda‘s interests include the integration of health informatics in undergraduate education, open accessible education, and the impact of educational technologies on nursing students’ clinical judgment and decision making at the point of care to improve patient safety and quality of care.
Faculty member in the critical care nursing program at the British Columbia Institute of Technology (BCIT) since 2003, Rob has been a critical care nurse for over 25 years with 17 years practicing in a quaternary care intensive care unit. Rob is an experienced educator and supports student learning in the classroom, online, and in clinical areas. Rob’s Master of Education from Simon Fraser University is in educational technology and learning design. He is passionate about using technology to support learning for both faculty and students.
Part of Rob’s faculty position is dedicated to providing high fidelity simulation support for BCIT’s nursing specialties program along with championing innovative teaching and best practices for educational technology. He has championed the use of digital publishing and was the tech lead for Critical Care Nursing’s iPad Project which resulted in over 40 multi-touch interactive textbooks being created using Apple and other technologies.
Rob has successfully completed a number of specialist certifications in computer and network technologies. In 2015, he was awarded Apple Distinguished Educator for his innovation and passionate use of technology to support learning. In the past five years, he has presented and published abstracts on virtual simulation, high fidelity simulation, creating engaging classroom environments, and what the future holds for healthcare and education.
Janet Morrison is the Program Head of Occupational Health Nursing at the British Columbia Institute of Technology (BCIT) in Burnaby, British Columbia. She completed a PhD at Simon Fraser University, Faculty of Communication, Art and Technology, with a focus on health information technology. Her dissertation examined the effects of telehealth implementation in an occupational health nursing service. She has an MA in Adult Education from St. Francis Xavier University and an MA in Library and Information Studies from the University of British Columbia.
Janet’s research interests concern the intended and unintended impacts of health information technologies on healthcare students, faculty, and the healthcare workforce.
She is currently working with BCIT colleagues to study how an educational clinical information system can foster healthcare students’ perceptions of interprofessional roles.
Contribute to this Page
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Case Study: A Patient with Asthma, Covid-19 Pneumonia and Cytokine Release Syndrome Treated with Corticosteroids and Tocilizumab
Gunter k schleicher.
1 Department of Critical Care and Pulmonology, Wits Donald Gordon Medical Centre, Johannesburg, South Africa
Warren Lowman
2 Pathcare/Vermaak Laboratories, Department of Clinical Microbiology and Infectious Diseases, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
Guy A Richards
3 Department of Internal Medicine, School of Clinical Medicine, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa
INTRODUCTION
Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) is the novel coronavirus first detected in Wuhan, China, that causes coronavirus disease 2019 (Covid-19) and pneumonia. Covid-19 pneumonia is defined by a positive result for SARS-CoV-2 on a reverse-transcriptase–polymerase-chain-reaction (RT-PCR) assay of a specimen collected from the upper or lower respiratory tract together with radiological features of pneumonia and clinical features of hypoxaemia and dyspnoea. Although more than 80% of patients with Covid-19 infection have mild disease and make a full recovery, a significant proportion of patients progress to pneumonia, and about half of these cases will develop severe acute respiratory syndrome (ARDS). Initial reports from China suggested that age >65 years and medical comorbidities are risk factors for poor outcomes.( 1 ) The need for ICU admission and mechanical ventilation once ARDS develops is associated with a high mortality, ranging from 39% to 72%.( 2 , 3 ) Current guidelines recommend that corticosteroids or immunosuppressive therapy should not be used in patients with Covid-19 pneumonia unless there are other indications, such as shock, asthma or exacerbation of chronic obstructive pulmonary disease.( 4 ) However, the role of systemic corticosteroids is currently being re-evaluated in mechanically ventilated adults with ARDS, with some guidelines now suggesting their use.( 5 )
We describe a case of a patient with Covid-19 infection, progressive pneumonia, development of a hyperinflammatory state and cytokine release syndrome (CRS) who was successfully treated with steroids and tocilizumab.
CASE REPORT
In January 2020, a 53-year-old gentleman with a background of asthma on long-term low dose inhaled corticosteroid inhaler had an acute exacerbation of his asthma in February 2020 triggered by a viral upper respiratory tract infection and acute sinusitis and was managed with bronchodilator nebulization and a 7-day course of oral prednisone 30 mg daily. He made an uneventful recovery and proceeded to travel to Austria on 29 February 2020. During his stay in Austria, he had contact with a Covid-19 positive individual and started developing upper respiratory symptoms on 7 March. On his return to South Africa on 8 March he had a fever, sore throat, dry cough, severe wheezing and worsening dyspnoea. At that stage a commercial test for Covid-19 PCR was not yet available to the private pathology laboratories and blood tests showed a normal full blood count and a C-reactive protein (CRP) of 16 mg/L. He was advised to self-isolate at home and was managed telephonically with bronchodilator nebulization, oral prednisone 30 mg daily for 5 days and paracetamol. By 11 March he was not feeling any better and had ongoing fever and cough. The Covid-19 PCR test had become available at that stage and his initial test with a private pathology laboratory was negative.
Over the next 3 days his symptoms worsened, and on 16 March he was admitted to hospital to an isolation ward where blood tests showed a lymphopaenia and a rising CRP ( Table 1 ). A high-resolution CT scan of his chest showed bilateral asymmetrical peripheral ground glass infiltrates in a subsegmental distribution, particularly in the lower zones. A repeat Covid-19 PCR swab on this occasion was positive and he was diagnosed with Covid-19 pneumonia. His oxygen saturation was 86% on room air. He was haemodynamically stable and was kept in strict isolation, and treatment was commenced with supplemental oxygen via a nasal cannula, paracetamol, chloroquine, azithromycin and lopinavir/ritonavir. In keeping with national and international guidelines recommending against the use of systemic corticosteroids, prednisone was discontinued.
Laboratory and pathology results during hospital admission and post discharge
Arrows indicate treatment with tocilizumab 400 mg IV.
Over the next 5 days his clinical condition worsened despite antiviral therapy. His biomarkers, including lymphopaenia, CRP, pro-B-type natriuretic peptide (Pro-BNP), lactate dehydrogenase (LDH), D-dimers and ferritin all increased significantly ( Table 1 ). His hypoxaemia worsened and he had increased bilateral chest infiltrates on follow-up radiology ( Figure 1 ). His PaO2:FiO2 ratio decreased to 250. He was diagnosed as having Covid-19 hyperinflammatory syndrome, CRS and ARDS. After a discussion with the team he was treated with tocilizumab 800 mg IV, given as two doses of 400 mg 24 h apart on 23 and 24 March, as well as methylprednisolone 40 mg IV daily for 5 days. Chloroquine dose was reduced, and azithromycin and lopinavir/ritonavir were discontinued in view of QT prolongation (QTc > 500 ms).

Portable chest radiographs on 17 and 20 March 2020 showing progressive bilateral pulmonary infiltrates
Within 24 h following the tocilizumab infusion, there was an improvement in his fever, biomarkers ( Table 1 ) and hypoxaemia. Mechanical ventilation was avoided and he was monitored for another 6 day in the isolation unit. His saturations on room air improved to 90%. He was discharged home on 27 March, where he continued to make an uneventful recovery. Follow-up blood tests as an outpatient showed normalization of his lymphocyte count and CRP ( Table 1 ). His saturations on room air improved to 92%. A repeat nasopharyngeal and throat swab test for Covid-19 on 31 March was negative.
It has been postulated that there are three distinct but overlapping phases and pathological subsets of Covid-19 infection and subsequent Covid-19 disease in humans, the first two triggered by the virus itself and the third, by the host response.( 6 ) Treatment recommendations differ depending on the stage of the Covid-19 disease: the viral response phase (about 1–6 days after start of symptoms), the pneumonic phase (about days 6–10) which may progress to acute lung injury and ARDS, and the hyperinflammatory phase which typically occurs after day 8 in a minority of patients. This last phase is associated with worsening ARDS, multi-organ dysfunction syndrome (MODS), coagulation abnormalities, myocarditis and death. Patients progressing to this last severe phase of Covid-19 have clinical and laboratory evidence of an exaggerated inflammatory response, similar to the CRS, with persistent fever, worsening ARDS, elevated inflammatory markers and proinflammatory cytokines and MODS.
The Covid-19 virus binds to alveolar epithelial cells, activating the innate and adaptive immune systems resulting in the release of pro-inflammatory cytokines. This can lead to the CRS which is characterised by a hyperinflammatory state with raised inflammatory cytokines and biomarkers such as interleukin (IL)-2, IL-6, IL-7, granulocyte-colony stimulating factor, macrophage inflammatory protein 1-α, tumour necrosis factor-α, CRP, ferritin, Pro-BNP and D-dimer.( 7 ) The clinical picture is one of progressive ARDS and fulminant MODS.
Although corticosteroids are not routinely recommended for the treatment of Covid-19-associated lung injury, CRS immunosuppression with corticosteroids and other therapies is likely to be beneficial. Although there are currently no controlled clinical trials on the use of corticosteroids in Covid-19 patients, several published reports of corticosteroid therapy in severe Covid-19 have shown a shorter duration of supplemental oxygen use, improved radiographic findings and lower mortality in patients with ARDS.( 8 , 9 )
Tocilizumab, an IL-6 receptor blocker registered for CRS treatment, is being investigated for the treatment of patients with severe Covid-19, CRS and elevated IL-6 levels. IL-6 plays an important role in CRS and tocilizumab binds specifically to both soluble and membrane-bound IL-6 receptors (sIL-6R and mIL-6R), inhibiting sIL-6R and mIL-6R-mediated signalling. Small observational studies support the concept that tocilizumab may be an effective drug for patients with severe Covid-19 and respiratory failure requiring mechanical ventilation.( 10 , 11 ) In a study of 21 patients with Covid-19-related ARDS who received tocilizumab, the ICU mortality was less than 5%, all surviving patients became apyrexial within 72 h, pulmonary infiltrates on follow-up CT scan improved in 90%, hypoxaemia resolved in the majority and 90.5% of patients were discharged from the ICU after a median of 13.5 days.( 12 ) A large randomised, double-blind, placebo-controlled phase 3 clinical trial to evaluate the safety and efficacy of tocilizumab plus standard of care in hospitalised adult patients with severe Covid-19 pneumonia and ARDS has been being initiated.( 13 )
Currently, tocilizumab is available in South Africa for patients with severe Covid-19 and ARDS under the Monitored Emergency use of Unregistered and Investigational Interventions framework.( 14 ) This requires the treating physician to consult with an expert panel prior to enrolment, detailed patient data collection and ensuring that the patient meets the strict inclusion and exclusion criteria. Other immune modulating agents under investigation include siltuximab (IL-6 inhibitor), bevacizumab (vascular endothelial growth factor inhibitor), convalescent plasma from patients who have recovered from SARS-CoV-2 infection and intravenous immune globulin (Polygam).( 15 , 16 )
This case study also highlights some of the many controversies and complications in managing patients with severe Covid-19:
- • The use of inhaled or oral corticosteroids as a risk factor for severe Covid-19 is not certain. Individuals taking long-term corticosteroids for chronic conditions such as asthma, allergies and arthritis may be unable to mount an appropriate immune response and are generally considered high risk for severe disease if infected with Covid-19.( 17 ) Corticosteroids can also result in increased viral replication and prolonged viral shedding. Even a short course of oral corticosteroids in the preceding month for an asthma exacerbation, such as in this case study, is a risk factor for ARDS and mechanical ventilation.( 18 ) Conversely, in vitro studies with ciclesonide showed antiviral activity against Covid-19, and there have been reports of clinical effectiveness of inhaled ciclesonide in the treatment of Covid-19.( 19 ) Studies are currently underway to investigate whether inhaled ciclesonide alone, or in combination with hydroxychloroquine, could eradicate SARS-CoV-2 from respiratory tract earlier in patients with mild Covid-19.( 20 )
- • Diagnosis of SARS-CoV-2 pneumonia is not always straightforward. Currently, the gold standard in clinical practice is the detection of Covid-19 RNA by RT-PCR in respiratory tract specimens. Nasopharyngeal and throat swabs are recommended over expectorated or induced sputum. Lower respiratory tract specimens, such as tracheal aspirates or bronchoalveolar lavage in intubated patients may have higher viral loads and be more likely to yield positive tests (up to 95% sensitive) but come with a higher risk of transmission of infection to health-care workers.( 21 ) False-negative tests from upper respiratory specimens have been documented, as with this case study. If initial testing is negative in a patient with risk factors for infection and clinical or radiological features are highly suggestive of Covid-19 or determining the presence of infection is important for further management and infection control, repeat testing is recommended.
- • Chloroquine, azithromycin and lopinavir/ritonavir can all cause QT prolongation and ventricular arrhythmia, in particular drug-induced torsades de pointes and sudden cardiac death.( 22 ) Patients treated with any combination of these drugs should have 12–24 hourly ECG with QTc monitoring. If QTc >500 ms (as in the case study), or QTc increases >60 ms from baseline after initiating drug therapy, discontinue azithromycin and lopinavir/ritonavir, and consider reducing dose of chloroquine. Frequent monitoring of QTc is mandatory and chloroquine should also be discontinued if QTc remains >500 ms. The risk of serious ventricular arrhythmia may be reduced by performing a screening ECG prior to initiation of therapy, inquiring about a personal or family history of QT interval prolongation or sudden unexplained cardiac death, avoiding exposure to other medications known to affect QT interval, and aggressively treating hypocalcaemia, hypokalaemia and hypomagnesaemia. Hypokalaemia is especially common in patients with Covid-19 and is associated with a poorer prognosis.( 23 ) The correction of hypokalaemia can be challenging due to continuous renal loss of potassium resulting from the degradation of angiotensin converting enzyme 2 by binding of SAR-CoV-2.
This case study of severe Covid-19 pneumonia and CRS illustrates some of the diagnostic and therapeutic challenges and controversies regarding the management of this novel and complex infection. Meticulous monitoring for and early treatment of the hyperinflammatory phase of the disease may be crucial in preventing progression to severe ARDS, MODS and death.
ACKNOWLEDGEMENTS
We thank Dr L. Brannigan for his assistance with the management of this patient, and Dr E. Boschoff for the radiographs.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present patient...
How to present patient cases
- Related content
- Peer review
- Mary Ni Lochlainn , foundation year 2 doctor 1 ,
- Ibrahim Balogun , healthcare of older people/stroke medicine consultant 1
- 1 East Kent Foundation Trust, UK
A guide on how to structure a case presentation
This article contains...
-History of presenting problem
-Medical and surgical history
-Drugs, including allergies to drugs
-Family history
-Social history
-Review of systems
-Findings on examination, including vital signs and observations
-Differential diagnosis/impression
-Investigations
-Management
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1
The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the patient’s condition and further management can be planned accordingly. 2 To give a high quality presentation you need to take a thorough history. Consultants make decisions about patient care based on information presented to them by junior members of the team, so the importance of accurately presenting your patient cannot be overemphasised.
As a medical student, you are likely to be asked to present in numerous settings. A formal case presentation may take place at a teaching session or even at a conference or scientific meeting. These presentations are usually thorough and have an accompanying PowerPoint presentation or poster. More often, case presentations take place on the wards or over the phone and tend to be brief, using only memory or short, handwritten notes as an aid.
Everyone has their own presenting style, and the context of the presentation will determine how much detail you need to put in. You should anticipate what information your senior colleagues will need to know about the patient’s history and the care he or she has received since admission, to enable them to make further management decisions. In this article, I use a fictitious case to show how you can structure case presentations, which can be adapted to different clinical and teaching settings (box 1).
Box 1: Structure for presenting patient cases
Presenting problem, history of presenting problem, medical and surgical history.
Drugs, including allergies to drugs
Family history
Social history, review of systems.
Findings on examination, including vital signs and observations
Differential diagnosis/impression
Investigations
Case: tom murphy.
You should start with a sentence that includes the patient’s name, sex (Mr/Ms), age, and presenting symptoms. In your presentation, you may want to include the patient’s main diagnosis if known—for example, “admitted with shortness of breath on a background of COPD [chronic obstructive pulmonary disease].” You should include any additional information that might give the presentation of symptoms further context, such as the patient’s profession, ethnic origin, recent travel, or chronic conditions.
“ Mr Tom Murphy is a 56 year old ex-smoker admitted with sudden onset central crushing chest pain that radiated down his left arm.”
In this section you should expand on the presenting problem. Use the SOCRATES mnemonic to help describe the pain (see box 2). If the patient has multiple problems, describe each in turn, covering one system at a time.
Box 2: SOCRATES—mnemonic for pain
Associations
Time course
Exacerbating/relieving factors
“ The pain started suddenly at 1 pm, when Mr Murphy was at his desk. The pain was dull in nature, and radiated down his left arm. He experienced shortness of breath and felt sweaty and clammy. His colleague phoned an ambulance. He rated the pain 9/10 in severity. In the ambulance he was given GTN [glyceryl trinitrate] spray under the tongue, which relieved the pain to 5/10. The pain lasted 30 minutes in total. No exacerbating factors were noted. Of note: Mr Murphy is an ex-smoker with a 20 pack year history”
Some patients have multiple comorbidities, and the most life threatening conditions should be mentioned first. They can also be categorised by organ system—for example, “has a long history of cardiovascular disease, having had a stroke, two TIAs [transient ischaemic attacks], and previous ACS [acute coronary syndrome].” For some conditions it can be worth stating whether a general practitioner or a specialist manages it, as this gives an indication of its severity.
In a surgical case, colleagues will be interested in exercise tolerance and any comorbidity that could affect the patient’s fitness for surgery and anaesthesia. If the patient has had any previous surgical procedures, mention whether there were any complications or reactions to anaesthesia.
“Mr Murphy has a history of type 2 diabetes, well controlled on metformin. He also has hypertension, managed with ramipril, and gout. Of note: he has no history of ischaemic heart disease (relevant negative) (see box 3).”
Box 3: Relevant negatives
Mention any relevant negatives that will help narrow down the differential diagnosis or could be important in the management of the patient, 3 such as any risk factors you know for the condition and any associations that you are aware of. For example, if the differential diagnosis includes a condition that you know can be hereditary, a relevant negative could be the lack of a family history. If the differential diagnosis includes cardiovascular disease, mention the cardiovascular risk factors such as body mass index, smoking, and high cholesterol.
Highlight any recent changes to the patient’s drugs because these could be a factor in the presenting problem. Mention any allergies to drugs or the patient’s non-compliance to a previously prescribed drug regimen.
To link the medical history and the drugs you might comment on them together, either here or in the medical history. “Mrs Walsh’s drugs include regular azathioprine for her rheumatoid arthritis.”Or, “His regular drugs are ramipril 5 mg once a day, metformin 1g three times a day, and allopurinol 200 mg once a day. He has no known drug allergies.”
If the family history is unrelated to the presenting problem, it is sufficient to say “no relevant family history noted.” For hereditary conditions more detail is needed.
“ Mr Murphy’s father experienced a fatal myocardial infarction aged 50.”
Social history should include the patient’s occupation; their smoking, alcohol, and illicit drug status; who they live with; their relationship status; and their sexual history, baseline mobility, and travel history. In an older patient, more detail is usually required, including whether or not they have carers, how often the carers help, and if they need to use walking aids.
“He works as an accountant and is an ex-smoker since five years ago with a 20 pack year history. He drinks about 14 units of alcohol a week. He denies any illicit drug use. He lives with his wife in a two storey house and is independent in all activities of daily living.”
Do not dwell on this section. If something comes up that is relevant to the presenting problem, it should be mentioned in the history of the presenting problem rather than here.
“Systems review showed long standing occasional lower back pain, responsive to paracetamol.”
Findings on examination
Initially, it can be useful to practise presenting the full examination to make sure you don’t leave anything out, but it is rare that you would need to present all the normal findings. Instead, focus on the most important main findings and any abnormalities.
“On examination the patient was comfortable at rest, heart sounds one and two were heard with no additional murmurs, heaves, or thrills. Jugular venous pressure was not raised. No peripheral oedema was noted and calves were soft and non-tender. Chest was clear on auscultation. Abdomen was soft and non-tender and normal bowel sounds were heard. GCS [Glasgow coma scale] was 15, pupils were equal and reactive to light [PEARL], cranial nerves 1-12 were intact, and he was moving all four limbs. Observations showed an early warning score of 1 for a tachycardia of 105 beats/ min. Blood pressure was 150/90 mm Hg, respiratory rate 18 breaths/min, saturations were 98% on room air, and he was apyrexial with a temperature of 36.8 ºC.”
Differential diagnoses
Mentioning one or two of the most likely diagnoses is sufficient. A useful phrase you can use is, “I would like to rule out,” especially when you suspect a more serious cause is in the differential diagnosis. “History and examination were in keeping with diverticular disease; however, I would like to rule out colorectal cancer in this patient.”
Remember common things are common, so try not to mention rare conditions first. Sometimes it is acceptable to report investigations you would do first, and then base your differential diagnosis on what the history and investigation findings tell you.
“My impression is acute coronary syndrome. The differential diagnosis includes other cardiovascular causes such as acute pericarditis, myocarditis, aortic stenosis, aortic dissection, and pulmonary embolism. Possible respiratory causes include pneumonia or pneumothorax. Gastrointestinal causes include oesophageal spasm, oesophagitis, gastro-oesophageal reflux disease, gastritis, cholecystitis, and acute pancreatitis. I would also consider a musculoskeletal cause for the pain.”
This section can include a summary of the investigations already performed and further investigations that you would like to request. “On the basis of these differentials, I would like to carry out the following investigations: 12 lead electrocardiography and blood tests, including full blood count, urea and electrolytes, clotting screen, troponin levels, lipid profile, and glycated haemoglobin levels. I would also book a chest radiograph and check the patient’s point of care blood glucose level.”
You should consider recommending investigations in a structured way, prioritising them by how long they take to perform and how easy it is to get them done and how long it takes for the results to come back. Put the quickest and easiest first: so bedside tests, electrocardiography, followed by blood tests, plain radiology, then special tests. You should always be able to explain why you would like to request a test. Mention the patient’s baseline test values if they are available, especially if the patient has a chronic condition—for example, give the patient’s creatinine levels if he or she has chronic kidney disease This shows the change over time and indicates the severity of the patient’s current condition.
“To further investigate these differentials, 12 lead electrocardiography was carried out, which showed ST segment depression in the anterior leads. Results of laboratory tests showed an initial troponin level of 85 µg/L, which increased to 1250 µg/L when repeated at six hours. Blood test results showed raised total cholesterol at 7.6 mmol /L and nil else. A chest radiograph showed clear lung fields. Blood glucose level was 6.3 mmol/L; a glycated haemoglobin test result is pending.”
Dependent on the case, you may need to describe the management plan so far or what further management you would recommend.“My management plan for this patient includes ACS [acute coronary syndrome] protocol, echocardiography, cardiology review, and treatment with high dose statins. If you are unsure what the management should be, you should say that you would discuss further with senior colleagues and the patient. At this point, check to see if there is a treatment escalation plan or a “do not attempt to resuscitate” order in place.
“Mr Murphy was given ACS protocol in the emergency department. An echocardiogram has been requested and he has been discussed with cardiology, who are going to come and see him. He has also been started on atorvastatin 80 mg nightly. Mr Murphy and his family are happy with this plan.”
The summary can be a concise recap of what you have presented beforehand or it can sometimes form a standalone presentation. Pick out salient points, such as positive findings—but also draw conclusions from what you highlight. Finish with a brief synopsis of the current situation (“currently pain free”) and next step (“awaiting cardiology review”). Do not trail off at the end, and state the diagnosis if you are confident you know what it is. If you are not sure what the diagnosis is then communicate this uncertainty and do not pretend to be more confident than you are. When possible, you should include the patient’s thoughts about the diagnosis, how they are feeling generally, and if they are happy with the management plan.
“In summary, Mr Murphy is a 56 year old man admitted with central crushing chest pain, radiating down his left arm, of 30 minutes’ duration. His cardiac risk factors include 20 pack year smoking history, positive family history, type 2 diabetes, and hypertension. Examination was normal other than tachycardia. However, 12 lead electrocardiography showed ST segment depression in the anterior leads and troponin rise from 85 to 250 µg/L. Acute coronary syndrome protocol was initiated and a diagnosis of NSTEMI [non-ST elevation myocardial infarction] was made. Mr Murphy is currently pain free and awaiting cardiology review.”
Originally published as: Student BMJ 2017;25:i4406
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 - 3 . doi:10.1007/s11606-008-0900-x pmid:19139965 . OpenUrl CrossRef PubMed Web of Science
- ↵ Olaitan A, Okunade O, Corne J. How to present clinical cases. Student BMJ 2010;18:c1539.
- ↵ Gaillard F. The secret art of relevant negatives, Radiopedia 2016; http://radiopaedia.org/blog/the-secret-art-of-relevant-negatives .
Multimodality treatment planning using the Markov decision process: a comprehensive study of applications and challenges
- Published: 28 May 2024
Cite this article

- Pushpendra Singh ORCID: orcid.org/0000-0001-8608-5188 1 ,
- Seema Singh nAff2 ,
- Alka Mishra nAff1 &
- Santosh Kumar Mishra nAff1
Explore all metrics
According to the oncologist, a single medication is insufficient to completely cure the disease; as a result, most patients undergo treatment from two or more types of therapy, sometimes in succession, in order to control the progression of their cancer.
This comprehensive review explores the applications and challenges associated with multimodality treatment planning utilizing the Markov decision process (MDP) framework. The benefits of employing MDP in treatment planning include its ability to incorporate multiple treatment modalities, optimize treatment sequences, and account for uncertainties in patient response. However, several limitations exist, such as the complexity of modeling interactions between different treatment modalities, the need for accurate input data, and the computational burden associated with solving large-scale MDP problems.
This review highlights the importance of considering both the benefits and limitations of using MDP in multimodality treatment planning to enhance patient outcomes and optimize resource allocation in healthcare settings. Finally, by taking a case analysis into consideration, we analyze how altering the ultimate cost function affects the efficacy of MDP optimal plans.
We summarize the findings of several studies that have employed MDP in treatment planning and discuss the benefits, limitations, and potential future directions of this approach. It also provides a comprehensive review of the benefits of MDP-based multimodality treatment planning, including improved treatment outcomes, reduced toxicities, personalized treatment decisions, and optimized sequencing and timing of treatment modalities.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
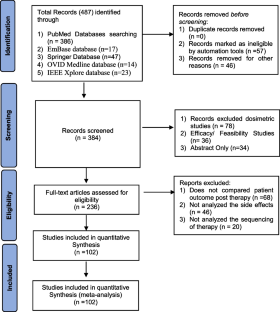
Similar content being viewed by others

SEOM-GEICAM-SOLTI clinical guidelines for early-stage breast cancer (2022)
Informing Structural Assumptions for Three State Oncology Cost-Effectiveness Models through Model Efficiency and Fit

SEOM-GEMCAD-TTD clinical guidelines for the systemic treatment of metastatic colorectal cancer (2022)
Abdellatif AA, Mhaisen N, Mohamed A, Erbad A, Guizani M. Reinforcement learning for intelligent healthcare systems: a review of challenges, applications, and open research issues. IEEE Internet of Things Journal (IEEE). 2023;10(24):21982–2007. https://doi.org/10.1109/JIOT.2023.3288050 .
Article Google Scholar
Adeyiola AO, Rabia SI, Elsaid A, Fadel S, Zakaria A. A Markov decision process framework for optimal cancer chemotherapy dose selection. In J Phys: Conf Ser. 2022;2287(1):012002.
Google Scholar
Alagoz O, Maillart LM, Schaefer AJ, Roberts MS. The optimal timing of living-donor liver transplantation. Manage Sci. 2004;50(10):1420–30.
Alagoz O, Hsu H, Schaefer AJ, Roberts MS. Markov decision processes: a tool for sequential decision making under uncertainty. Med Decis Making. 2010;30(4):474–83. https://doi.org/10.1177/0272989X09353194 .
Bäuerle N, Rieder U. Markov decision processes with applications to finance. Germany: Springer Science & Business Media; 2011. https://doi.org/10.1007/978-3-642-18324-9 .
Book Google Scholar
Bazrafshan N, Lotfi MM. A finite-horizon Markov decision process model for cancer chemotherapy treatment planning: an application to sequential treatment decision making in clinical trials. Ann Oper Res. 2020;295:483–502.
Article MathSciNet Google Scholar
Bennett CC, Hauser K. Artificial intelligence framework for simulating clinical decision-making: a Markov decision process approach. Artif Intell Med. 2013a;57(1):9–19.
Bennett CC, Hauser K. Artificial intelligence framework for simulating clinical decision-making: a Markov decision process approach. Artif Intell Med. 2013b;57(1):9–19. https://doi.org/10.1016/j.artmed.2012.12.003 .
Bertuzzi A, Conte F, Papa F, Sinisgalli C. Applications of nonlinear programming to the optimization of fractionated protocols in cancer radiotherapy. Information. 2020;11(6):313.
Bird TG, Ngan SY, Chu J, Kroon R, Lynch AC, Heriot AG. Outcomes and prognostic factors of multimodality treatment for locally recurrent rectal cancer with curative intent. Int J Colorectal Dis. 2018;33:393–401.
Borera EC, Moore BL, Pyeatt LD. Partially observable markov decision process for closed-loop anesthesia control. IOS Press; 2012.
Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc: JMLA. 2016;104(3):240.
Briggs A, Sculpher M. An introduction to Markov modelling for economic evaluation. Pharmacoeconomics. 1998;13:397–409.
Calderone D, Shankar Sastry S. Markov decision process routing games. In: 2017 ACM/IEEE 8th international conference on cyber-physical systems (ICCPS). Pittsburgh: Association for Computing Machinery; 2017. pp. 273–9. https://doi.org/10.1145/3055004.3055026 .
Chapter Google Scholar
Chanchaichujit J, Tan A, Meng F, Eaimkhong S, Chanchaichujit J, Tan A, Meng F, Eaimkhong S. Optimization, simulation and predictive analytics in healthcare. In: Healthcare 4.0: next generation processes with the latest technologies. Singapore: Palgrave Pivot; 2019. pp. 95–121. https://doi.org/10.1007/978-981-13-8114-0_5 .
Choi SE, Brandeau ML, Basu S. Dynamic treatment selection and modification for personalised blood pressure therapy using a Markov decision process model: a cost-effectiveness analysis. BMJ Open. 2017;7(11):e018374.
Choi J, Tocco B, Smith A, Ahmad S, Josephides E, Bille A. Multimodality treatment and salvage surgery for the treatment of lung cancer. Cancers. 2023;15(14):3586.
Debela DT, Muzazu SGY, Heraro KD, Ndalama MT, Mesele BW, Haile DC, Kitui SK, Manyazewal T. New approaches and procedures for cancer treatment: current perspectives. SAGE Open Medicine. 2021;9:20503121211034370.
Deli T, Orosz M, Jakab A. Hormone replacement therapy in cancer survivors–review of the literature. Pathol Oncol Res. 2020;26:63–78.
Deng J, Wang C, Xiang M, Liu F, Liu Y, Zhao K. Meta-analysis of postoperative efficacy in patients receiving chemoradiotherapy followed by surgery for resectable esophageal carcinoma. Diagn Pathol. 2014;9(1):1–8. https://doi.org/10.1186/1746-1596-9-151 .
Dhas N, Kudarha R, Pandey A, Nikam AN, Sharma S, Singh A, Garkal A, Hariharan K, Singh A, Bangar P, Yadhav D. Stimuli responsive and receptor targeted iron oxide based nanoplatforms for multimodal therapy and imaging of cancer: conjugation chemistry and alternative therapeutic strategies. J Control Release. 2021;333:188–245.
Du F, Plaisant C, Spring N, Crowley K, Shneiderman B. Eventaction: a visual analytics approach to explainable recommendation for event sequences. ACM Trans Interact Intell Syst (TiiS). 2019;9(4):1–31.
Fiorica F, Di Bona D, Filippo Schepis A, Licata L, Shahied A, Venturi AM, Falchi A, Craxì CC. Preoperative chemoradiotherapy for oesophageal cancer: a systematic review and meta-analysis. Gut. 2004;53(7):925–30. https://doi.org/10.1136/gut.2003.025080 .
Forastiere AA, Zhang Q, Weber RS, Maor MH, Goepfert H, Pajak TF, Morrison W. Long-term results of RTOG 91–11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer. J Clin Oncol. 2013;31(7):845. https://doi.org/10.1200/JCO.2012.43.6097 .
Franklin M, Hunter RM. A modelling-based economic evaluation of primary-care-based fall-risk screening followed by fall-prevention intervention: a cohort-based Markov model stratified by older age groups. Age Ageing. 2020;49(1):57–66. https://doi.org/10.1093/ageing/afz125 .
Garcia G-GP, Steimle LN, Marrero WJ, Sussman JB. Interpretable policies and the price of interpretability in hypertension treatment planning. Manuf Serv Oper Manag. 2024;26(1):80–94. https://doi.org/10.1287/msom.2021.0373 .
Gazdar AF, Girard L, Lockwood WW, Lam WL, Minna JD. Lung cancer cell lines as tools for biomedical discovery and research. J Natl Cancer Inst. 2010;102(17):1310–21. https://doi.org/10.1093/jnci/djq279 .
Ge L, Mourits MCM, Kristensen AR, Huirne RBM. A modelling approach to support dynamic decision-making in the control of FMD epidemics. Prev Vet Med. 2010;95(3–4):167–74. https://doi.org/10.1016/j.prevetmed.2010.04.003 .
Gebski V, Burmeister B, Smithers BM, Foo K, Zalcberg J, Simes J, Australasian Gastro-Intestinal Trials Group. Survival benefits from neoadjuvant chemoradiotherapy or chemotherapy in oesophageal carcinoma: a meta-analysis. Lancet Oncol. 2007;8(3):226–34. https://doi.org/10.1016/S1470-2045(07)70039-6 .
Gondi S, Wright AA, Landrum MB, Zubizarreta J, Chernew ME, Keating NL. Multimodality cancer care and implications for episode-based payments in cancer. Am J Manag Care. 2019;25(11):537–8.
Greer SE, Goodney PP, Sutton JE, Birkmeyer JD. Neoadjuvant chemoradiotherapy for esophageal carcinoma: a meta-analysis. Surgery. 2005;137(2):172–7. https://doi.org/10.1016/j.surg.2004.06.033 .
Harrold JM, Parker RS. Clinically relevant cancer chemotherapy dose scheduling via mixed integer optimization. Comput Chem Eng. 2009;33(12):2042–54.
Hauskrecht M, Fraser H. Planning treatment of ischemic heart disease with partially observable Markov decision processes. Artif Intell Med. 2000;18(3):221–44.
Imani F, Qiu Z, Yang H. Markov decision process modeling for multi-stage optimization of intervention and treatment strategies in breast Cancer. In: 2020 42nd annual international conference of the IEEE engineering in Medicine & Biology Society (EMBC). Montreal: IEEE; 2020. pp. 5394–7. https://doi.org/10.1109/EMBC44109.2020.9175905 .
Ishizawa S. Medical decision making on cancer treatment with Markov decision process. PhD Thesis, Applied Mathematics and Statistics, Stony Brook University. Stony Brook: State University of New York; 2023. https://www.proquest.com/openview/7f7ab3420ffec0cfc7038ad47c5d9edc/1?pqorigsite=gscholar&cbl=18750&diss=y .
Kaplan B. Evaluating informatics applications—clinical decision support systems literature review. Int J Med Informatics. 2001;64(1):15–37.
Katakami N, Tada H, Mitsudomi T, Kudoh S, Senba H, Matsui K, Saka H, Kurata T, Nishimura Y, Fukuoka M. A phase 3 study of induction treatment with concurrent chemoradiotherapy versus chemotherapy before surgery in patients with pathologically confirmed N2 stage IIIA nonsmall cell lung cancer. Cancer. 2012;118(24):6126–35. https://doi.org/10.1002/cncr.26689 .
Kinjo K, Uchibe E, Doya K. Evaluation of linearly solvable Markov decision process with dynamic model learning in a mobile robot navigation task. Front Neurorobot. 2013;7:7.
Kürzinger M-L, Douarin L, Uzun I, El-Haddad C, Hurst W, Juhaeri J, Tcherny-Lessenot S. Structured benefit–risk evaluation for medicinal products: review of quantitative benefit–risk assessment findings in the literature. Ther Adv Drug Saf. 2020;11:2042098620976951.
Larizadeh MH, Mohammadi F, Shabani M, Damghani MA. Induction chemotherapy followed by either chemoradiotherapy or bioradiotherapy in laryngeal cancer. Asian Pac J Cancer Prev. 2021;22(5):1633–7. https://doi.org/10.31557/APJCP.2021.22.5.1633 .
Lazzerini M, Gray D. Oral zinc for treating diarrhoea in children. Commentary. Int J Epidemiol. 2008;37(5):938–40.
Lefebvre JL, Rolland F, Tesselaar M, Bardet E, Leemans CR, Geoffrois L, Hupperets P. Phase 3 randomized trial on larynx preservation comparing sequential vs alternating chemotherapy and radiotherapy. J Natl Cancer Inst. 2009;101(3):142–52. https://doi.org/10.1093/jnci/djn460 .
Lefebvre J-L, Andry G, Dominique Chevalier B, Luboinski LC, Traissac L, De Raucourt D, Langendijk JA. Laryngeal preservation with induction chemotherapy for hypopharyngeal squamous cell carcinoma: 10-year results of EORTC trial 24891. Ann Oncol. 2012;23(10):2708–14. https://doi.org/10.1093/annonc/mds065 .
Lefebvre JL, Pointreau Y, Rolland F, Alfonsi M, Baudoux A, Sire C, de Raucourt D. Induction chemotherapy followed by either chemoradiotherapy or bioradiotherapy for larynx preservation: the TREMPLIN randomized phase II study. J Clin Oncol. 2013;31(7):853–9. https://doi.org/10.1200/JCO.2012.42.3988 .
Li F, Jörg F, Li X, Feenstra T. A promising approach to optimizing sequential treatment decisions for depression: Markov decision process. Pharmacoeconomics. 2022;40(11):1015–32.
Maass K, Kim M. A Markov decision process approach to optimizing cancer therapy using multiple modalities. Math Med Biol: A J IMA. 2020;37(1):22–39.
Magni P, Quaglini S, Marchetti M, Barosi G. Deciding when to intervene: a Markov decision process approach. Int J Med Informatics. 2000a;60(3):237–53.
Magni P, Quaglini S, Marchetti M, Barosi G. Deciding when to intervene: a Markov decision process approach. Int J Med Informatics. 2000b;60(3):237–53. https://doi.org/10.1016/S1386-5056(00)00099-X .
Maitre P, Krishnatry R, Chopra S, Gondhowiardjo S, Likonda BM, Hussain QM, Zubizarreta EH, Agarwal JP. Modern radiotherapy technology: obstacles and opportunities to access in low-and middle-income countries. JCO Global Oncol. 2022;8:e2100376.
Mathur P, Sathishkumar K, Chaturvedi M, Das P, Sudarshan KL, Santhappan S, Nallasamy V, et al. Cancer statistics, 2020: report from national cancer registry programme, India. JCO Global Oncol. 2020;6:1063–75.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
Murray J, Tree AC. Prostate cancer–advantages and disadvantages of MR-guided RT. Clin Transl Radiat Oncol. 2019;18:68–73.
Ni Y, Wang Ke, Zhao L. A Markov decision process model of allocating emergency medical resource among multi-priority injuries. Int J Math Oper Res. 2017;10(1):1–17.
Oh S-H, Lee SJ, Noh J, Mo J. Optimal treatment recommendations for diabetes patients using the Markov decision process along with the South Korean electronic health records. Sci Rep. 2021;11(1):6920.
Ortega-Calvo AS, Morcillo-Jimenez R, Fernandez-Basso C, Gutiérrez-Batista K, Vila M-A, Martin-Bautista MJ. AIMDP: an artificial intelligence modern data platform. Use case for Spanish national health service data silo. Futur Gener Comput Syst. 2023;143:248–64.
Osheroff JA, Teich JM, Middleton B, Steen EB, Wright A, Detmer DE. A roadmap for national action on clinical decision support. J Am Med Inform Assoc. 2007;14(2):141–5.
Pointreau Y, Garaud P, Chapet S, Sire C, Tuchais C, Tortochaux J, Faivre S, Guerrif S, Alfonsi M, Calais G. Randomized trial of induction chemotherapy with cisplatin and 5-fluorouracil with or without docetaxel for larynx preservation. J Natl Cancer Inst. 2009;101(7):498–506. https://doi.org/10.1093/jnci/djp007 .
Pushpendra S, Tripathi S, Gupta S. A unified approach for optimal dose delivery and trajectory optimization for the treatment of prostate cancer. Biomed Signal Process Control. 2021;69:102884.
Pushpendra S, Mishra A, Mishra SK. A comprehensive analysis of the challenges and potential side effects of radiation therapy for palliative cancer treatment. Méd Palliat. 2024. https://doi.org/10.1016/j.medpal.2023.12.002 .
Puterman ML. Markov decision processes: discrete stochastic dynamic programming. John Wiley Sons. 1994. https://doi.org/10.1002/9780470316887 .
Saketkoo LA, Russell AM, Jensen K, Mandizha J, Tavee J, Newton J, Rivera F, Howie M, Reese R, Goodman M, Hart P. Health-related quality of life (HRQoL) in sarcoidosis: diagnosis, management, and health outcomes. Diagnostics. 2021;11(6):1089.
Saure A, Patrick J, Tyldesley S, Puterman ML. Dynamic multi-appointment patient scheduling for radiation therapy. Eur J Oper Res. 2012;223(2):573–84. https://doi.org/10.1016/j.ejor.2012.06.046 .
Schaefer AJ, Bailey MD, Shechter SM, Roberts MS. Modeling medical treatment using Markov decision processes. In: Operations research and health care. Boston, MA: Springer; 2004. pp. 593–612. https://doi.org/10.1007/1-4020-8066-2_23 .
Schell GJ, Marrero WJ, Lavieri MS, Sussman JB, Hayward RA. Data-driven Markov decision process approximations for personalized hypertension treatment planning. MDM Policy Pract. 2016;1(1):2381468316674214.
Sher DJ, Fidler MJ, Liptay MJ, Koshy M. Comparative effectiveness of neoadjuvant chemoradiotherapy versus chemotherapy alone followed by surgery for patients with stage IIIA non-small cell lung cancer. Lung Cancer. 2015;88(3):267–74. https://doi.org/10.1016/j.lungcan.2015.03.015 .
Shi J, Alagoz O, Erenay FS, Qiang Su. A survey of optimization models on cancer chemotherapy treatment planning. Ann Oper Res. 2014;221:331–56.
Shields GE, Elvidge J. Challenges in synthesising cost-effectiveness estimates. Syst Rev. 2020;9(1):1–7.
Singh P, Tripathi S, Tamrakar RK. Dose-volume constraints based inverse treatment planning for optimizing the delivery of radiation therapy. Gedrag Organisatie Rev. 2020a;33(3):1049–58.
Singh P, Tripathi S, Tamrakar RK. Fluence map optimisation for prostate cancer intensity modulated radiotherapy planning using iterative solution method. Polish J Med Phys Eng. 2020b;26(4):201–9.
Sjoquist KM, Burmeister BH, Mark Smithers B, Zalcberg JR, John Simes R, Barbour A, Gebski V. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12(7):681–92. https://doi.org/10.1016/S1470-2045(11)70142-5 .
Tan AC, Ashley DM, López GY, Malinzak M, Friedman HS, Khasraw M. Management of glioblastoma: state of the art and future directions. CA: A Cancer J Clin. 2020;70(4):299–312.
Tcheng JE, Bakken S, Bates DW. Optimizing strategies for clinical decision support: summary of a meeting series. In: National Academy of medicine; the learning health system series. Washington (DC): National Academies Press (US); 2017. https://doi.org/10.17226/27122 .
Thomas M, Rübe C, Hoffknecht P, Macha HN, Freitag L, Linder A, Willich N. Effect of preoperative chemoradiation in addition to preoperative chemotherapy: a randomised trial in stage III non-small-cell lung cancer. Lancet Oncol. 2008;9(7):636–48. https://doi.org/10.1016/S1470-2045(08)70156-6 .
Tsoukalas A, Albertson T, Tagkopoulos I. From data to optimal decision making: a data-driven, probabilistic machine learning approach to decision support for patients with sepsis. JMIR Med Inform. 2015;3(1):e3445.
Tunc S, Alagoz O, Burnside E. Opportunities for operations research in medical decision making. IEEE Intell Syst. 2014;29(3):59.
Urschel JD, Vasan H. A meta-analysis of randomized controlled trials that compared neoadjuvant chemoradiation and surgery to surgery alone for resectable esophageal cancer. Am J Surg. 2003;185(6):538–43. https://doi.org/10.1016/S0002-9610(03)00066-7 .
Valenca LB, Sweeney CJ, Pomerantz MM. Sequencing current therapies in the treatment of metastatic prostate cancer. Cancer Treat Rev. 2015;41(4):332–40. https://doi.org/10.1016/j.ctrv.2015.02.010 .
Van A, Kyle J, Chow EKH, James NT, Orandi BJ, Ellison TA, Smith JM, Colombani PM, Segev DL. Choosing the order of deceased donor and living donor kidney transplantation in pediatric recipients: a Markov decision process model. Transplantation. 2015;99(2):360. https://doi.org/10.1097/TP.0000000000000588 .
Varni JW, Limbers CA, Burwinkle TM. How young can children reliably and validly self-report their health-related quality of life?: an analysis of 8,591 children across age subgroups with the PedsQL™ 4.0 Generic Core Scales. Health Qual Life Outcomes. 2007;5(1):1–13.
Vozikis A, Goulionis JE, Benos VK. The partially observable Markov decision processes in healthcare: an application to patients with ischemic heart disease (IHD). Oper Res Int Journal. 2012;12(1):3–14. https://doi.org/10.1007/s12351-010-0095-x .
Wang Z, Li H, Guan Y. Machine learning for cancer drug combination. Clin Pharmacol Ther. 2020;107(4):749.
Weaver DT. Novel approaches for optimal therapy design in drug-resistant populations. PhD thesis, Department of Nutrition Systems Biology and Bioinformatics. Cleveland, OH: Case Western Reserve University; 2023.
Wu C, Jarrett AM, Zhou Z, Elshafeey N, Adrada BE, Candelaria RP, Mohamed RM, Boge M, Huo L, White JB, Tripathy D. MRI-based digital models forecast patient-specific treatment responses to neoadjuvant chemotherapy in triple-negative breast cancer. Can Res. 2022;82(18):3394–404.
Yan L, Shen J, Wang J, Yang X, Dong S, Saijun Lu. Nanoparticle-based drug delivery system: a patient-friendly chemotherapy for oncology. Dose-Response. 2020;18(3):1559325820936161.
Youn S, Neil Geismar H, Pinedo M. Planning and scheduling in healthcare for better care coordination: current understanding, trending topics, and future opportunities. Prod Oper Manag. 2022;31(12):4407–23.
Yu C, Liu J, Nemati S, Yin G. Reinforcement learning in healthcare: a survey. ACM Comput Surv (CSUR). 2021;55(1):1–36.
Zhang S, Suen S-C, Gong CL, Pham J, Trebicka J, Duvoux C, Klein AS, Tiffany Wu, Jalan R, Sundaram V. Early transplantation maximizes survival in severe acute-on-chronic liver failure: results of a Markov decision process model. JHEP Rep (HEP Reports). 2021;3(6):100367. https://doi.org/10.1016/j.jhepr.2021.100367 .
Zhao L, Li J, Bai C, Nie Y, Lin G. Multi-modality treatment for patients with metastatic gastric cancer: a real-world study in China. Front Oncol. 2019a;9:1155.
Zhao Z, Zheng L, Chen W, Weng W, Song J, Ji J. Delivery strategies of cancer immunotherapy: recent advances and future perspectives. J Hematol Oncol. 2019b;12(1):126.
Download references
Author information
Alka Mishra & Santosh Kumar Mishra
Present address: Bhilai Institute of Technology, Durg, Chhattisgarh, India
Seema Singh
Present address: Shri Shankaracharya Group of Institutions: Shri Shankaracharya Technical Campus Bhilai, Chhattisgarh, India
Authors and Affiliations
Bhilai Institute of Technology, Durg, Chhattisgarh, India
Pushpendra Singh
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Seema Singh .
Ethics declarations
Conflict of interest.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Singh, P., Singh, S., Mishra, A. et al. Multimodality treatment planning using the Markov decision process: a comprehensive study of applications and challenges. Res. Biomed. Eng. (2024). https://doi.org/10.1007/s42600-024-00349-4
Download citation
Received : 19 July 2023
Accepted : 02 April 2024
Published : 28 May 2024
DOI : https://doi.org/10.1007/s42600-024-00349-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Multimodality treatment planning
- Markov decision process
- Cancer therapy
- Find a journal
- Publish with us
- Track your research
- Case Report
- Open access
- Published: 27 May 2024
A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient
- Wei Fu 1 , 2 na1 ,
- Zi Wei Deng 3 na1 ,
- Pei Wang 1 ,
- Zhen Wang Zhu 1 ,
- Zhi Bing Xie 1 ,
- Yong Zhong Li 1 &
- Hong Ying Yu 1
BMC Infectious Diseases volume 24 , Article number: 533 ( 2024 ) Cite this article
245 Accesses
1 Altmetric
Metrics details
Hepatitis B virus (HBV) infection can cause liver failure, while individuals with Acquired Immunodeficiency Virus Disease (AIDS) are highly susceptible to various opportunistic infections, which can occur concurrently. The treatment process is further complicated by the potential occurrence of immune reconstitution inflammatory syndrome (IRIS), which presents significant challenges and contributes to elevated mortality rates.
Case presentation
The 50-year-old male with a history of chronic hepatitis B and untreated human immunodeficiency virus (HIV) infection presented to the hospital with a mild cough and expectoration, revealing multi-drug resistant pulmonary tuberculosis (MDR-PTB), which was confirmed by XpertMTB/RIF PCR testing and tuberculosis culture of bronchoalveolar lavage fluid (BALF). The patient was treated with a regimen consisting of linezolid, moxifloxacin, cycloserine, pyrazinamide, and ethambutol for tuberculosis, as well as a combination of bictegravir/tenofovir alafenamide/emtricitabine (BIC/TAF/FTC) for HBV and HIV viral suppression. After three months of treatment, the patient discontinued all medications, leading to hepatitis B virus reactivation and subsequent liver failure. During the subsequent treatment for AIDS, HBV, and drug-resistant tuberculosis, the patient developed disseminated cryptococcal disease. The patient’s condition worsened during treatment with liposomal amphotericin B and fluconazole, which was ultimately attributed to IRIS. Fortunately, the patient achieved successful recovery after appropriate management.
Enhancing medical compliance is crucial for AIDS patients, particularly those co-infected with HBV, to prevent HBV reactivation and subsequent liver failure. Furthermore, conducting a comprehensive assessment of potential infections in patients before resuming antiviral therapy is essential to prevent the occurrence of IRIS. Early intervention plays a pivotal role in improving survival rates.
Peer Review reports
HIV infection remains a significant global public health concern, with a cumulative death toll of 40 million individuals [ 1 ]. In 2021 alone, there were 650,000 deaths worldwide attributed to AIDS-related causes. As of the end of 2021, approximately 38 million individuals were living with HIV, and there were 1.5 million new HIV infections reported annually on a global scale [ 2 ]. Co-infection with HBV and HIV is prevalent due to their similar transmission routes, affecting around 8% of HIV-infected individuals worldwide who also have chronic HBV infection [ 3 ]. Compared to those with HBV infection alone, individuals co-infected with HIV/HBV exhibit higher HBV DNA levels and a greater risk of reactivation [ 4 ]. Opportunistic infections, such as Pneumocystis jirovecii pneumonia, Toxoplasma encephalitis, cytomegalovirus retinitis, cryptococcal meningitis (CM), tuberculosis, disseminated Mycobacterium avium complex disease, pneumococcal pneumonia, Kaposi’s sarcoma, and central nervous system lymphoma, are commonly observed due to HIV-induced immunodeficiency [ 5 ]. Tuberculosis not only contributes to the overall mortality rate in HIV-infected individuals but also leads to a rise in the number of drug-resistant tuberculosis cases and transmission of drug-resistant strains. Disseminated cryptococcal infection is a severe opportunistic infection in AIDS patients [ 6 ], and compared to other opportunistic infections, there is a higher incidence of IRIS in patients with cryptococcal infection following antiviral and antifungal therapy [ 7 ]. This article presents a rare case of an HIV/HBV co-infected patient who presented with MDR-PTB and discontinued all medications during the initial treatment for HIV, HBV, and tuberculosis. During the subsequent re-anti-HBV/HIV treatment, the patient experienced two episodes of IRIS associated with cryptococcal infection. One episode was classified as “unmasking” IRIS, where previously subclinical cryptococcal infection became apparent with immune improvement. The other episode was categorized as “paradoxical” IRIS, characterized by the worsening of pre-existing cryptococcal infection despite immune restoration [ 8 ]. Fortunately, both episodes were effectively treated.
A 50-year-old male patient, who is self-employed, presented to our hospital in January 2022 with a chief complaint of a persistent cough for the past 2 months, without significant shortness of breath, palpitations, or fever. His medical history revealed a previous hepatitis B infection, which resulted in hepatic failure 10 years ago. Additionally, he was diagnosed with HIV infection. However, he ceased taking antiviral treatment with the medications provided free of charge by the Chinese government for a period of three years. During this hospital visit, his CD4 + T-cell count was found to be 26/μL (normal range: 500–1612/μL), HIV-1 RNA was 1.1 × 10 5 copies/ml, and HBV-DNA was negative. Chest computed tomography (CT) scan revealed nodular and patchy lung lesions (Fig. 1 ). The BALF shows positive acid-fast staining. Further assessment of the BALF using XpertMTB/RIF PCR revealed resistance to rifampicin, and the tuberculosis drug susceptibility test of the BALF (liquid culture, medium MGIT 960) indicated resistance to rifampicin, isoniazid, and streptomycin. Considering the World Health Organization (WHO) guidelines for drug-resistant tuberculosis, the patient’s drug susceptibility results, and the co-infection of HIV and HBV, an individualized treatment plan was tailored for him. The treatment plan included BIC/TAF/FTC (50 mg/25 mg/200 mg per day) for HBV and HIV antiviral therapy, as well as linezolid (0.6 g/day), cycloserine (0.5 g/day), moxifloxacin (0.4 g/day), pyrazinamide (1.5 g/day), and ethambutol (0.75 g/day) for anti-tuberculosis treatment, along with supportive care.
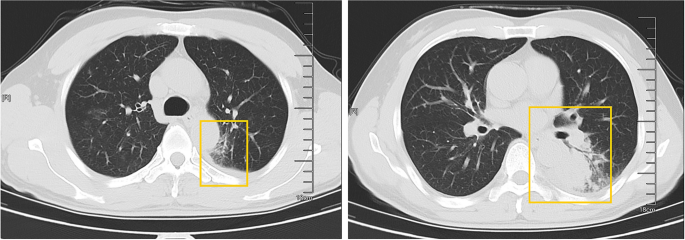
The patient’s pulmonary CT scan shows patchy and nodular lesions accompanied by a small amount of pleural effusion, later confirmed to be MDR-PTB
Unfortunately, after 3 months of follow-up, the patient discontinued all medications due to inaccessibility of the drugs. He returned to our hospital (Nov 12, 2022, day 0) after discontinuing medication for six months, with a complaint of poor appetite for the past 10 days. Elevated liver enzymes were observed, with an alanine aminotransferase level of 295 IU/L (normal range: 0–40 IU/L) and a total bilirubin(TBIL) level of 1.8 mg/dL (normal range: 0–1 mg/dL). His HBV viral load increased to 5.5 × 10 9 copies/ml. Considering the liver impairment, elevated HBV-DNA and the incomplete anti-tuberculosis treatment regimen (Fig. 2 A), we discontinued pyrazinamide and initiated treatment with linezolid, cycloserine, levofloxacin, and ethambutol for anti-tuberculosis therapy, along with BIC/TAF/FTC for HIV and HBV antiviral treatment. Additionally, enhanced liver protection and supportive management were provided, involving hepatoprotective effects of medications such as glutathione, magnesium isoglycyrrhizinate, and bicyclol. However, the patient’s TBIL levels continued to rise progressively, reaching 4.4 mg/dL on day 10 (Fig. 3 B). Suspecting drug-related factors, we discontinued all anti-tuberculosis medications while maintaining BIC/TAF/FTC for antiviral therapy, the patient’s TBIL levels continued to rise persistently. We ruled out other viral hepatitis and found no significant evidence of obstructive lesions on magnetic resonance cholangiopancreatography. Starting from the day 19, due to the patient’s elevated TBIL levels of 12.5 mg/dL, a decrease in prothrombin activity (PTA) to 52% (Fig. 3 D), and the emergence of evident symptoms such as abdominal distension and poor appetite, we initiated aggressive treatment methods. Unfortunately, on day 38, his hemoglobin level dropped to 65 g/L (normal range: 120–170 g/L, Fig. 3 A), and his platelet count decreased to 23 × 10 9 /L (normal range: 125–300 × 10 9 /L, Fig. 3 C). Based on a score of 7 on the Naranjo Scale, it was highly suspected that “Linezolid” was the cause of these hematological abnormalities. Therefore, we had to discontinue Linezolid for the anti-tuberculosis treatment. Subsequently, on day 50, the patient developed recurrent fever, a follow-up chest CT scan revealed enlarged nodules in the lungs (Fig. 2 B). The patient also reported mild dizziness and a worsening cough. On day 61, the previous blood culture results reported the growth of Cryptococcus. A lumbar puncture was performed on the same day, and the cerebrospinal fluid (CSF) opening pressure was measured at 130 mmH 2 O. India ink staining of the CSF showed typical encapsulated yeast cells suggestive of Cryptococcus. Other CSF results indicated mild leukocytosis and mildly elevated protein levels, while chloride and glucose levels were within normal limits. Subsequently, the patient received a fungal treatment regimen consisting of liposomal amphotericin B (3 mg/kg·d −1 ) in combination with fluconazole(600 mg/d). After 5 days of antifungal therapy, the patient’s fever symptoms were well controlled. Despite experiencing bone marrow suppression, including thrombocytopenia and worsening anemia, during this period, proactive symptom management, such as the use of erythropoietin, granulocyte colony-stimulating factor, and thrombopoietin, along with high-calorie dietary management, even reducing the dosage of liposomal amphotericin B to 2 mg/kg/day for 10 days at the peak of severity, successfully controlled the bone marrow suppression. However, within the following week, the patient experienced fever again, accompanied by a worsened cough, increased sputum production, and dyspnea. Nevertheless, the bilirubin levels did not show a significant increase. On day 78 the patient’s lung CT revealed patchy infiltrates and an increased amount of pleural effusion (Fig. 2 C). The CD4 + T-cell count was 89/μL (normal range: 500–700/μL), indicating a significant improvement in immune function compared to the previous stage, and C-reactive protein was significantly elevated, reflecting the inflammatory state, other inflammatory markers such as IL-6 and γ-IFN were also significantly elevated. On day 84, Considering the possibility of IRIS, the patient began taking methylprednisolone 30 mg once a day as part of an effort to control his excessive inflammation. Following the administration of methylprednisolone, the man experienced an immediate improvement in his fever. Additionally, symptoms such as cough, sputum production, dyspnea, and poor appetite gradually subsided over time. A follow-up lung CT showed significant improvement, indicating a positive response to the treatment. After 28 days of treatment with liposomal amphotericin B in combination with fluconazole, liposomal amphotericin B was discontinued, and the patient continued with fluconazole to consolidate the antifungal therapy for Cryptococcus. Considering the patient’s ongoing immunodeficiency, the dosage of methylprednisolone was gradually reduced by 4 mg every week. After improvement in liver function, the patient’s anti-tuberculosis treatment regimen was adjusted to include bedaquiline, contezolid, cycloserine, moxifloxacin, and ethambutol. The patient’s condition was well controlled, and a follow-up lung CT on day 117 indicated a significant improvement in lung lesions (Fig. 2 D).
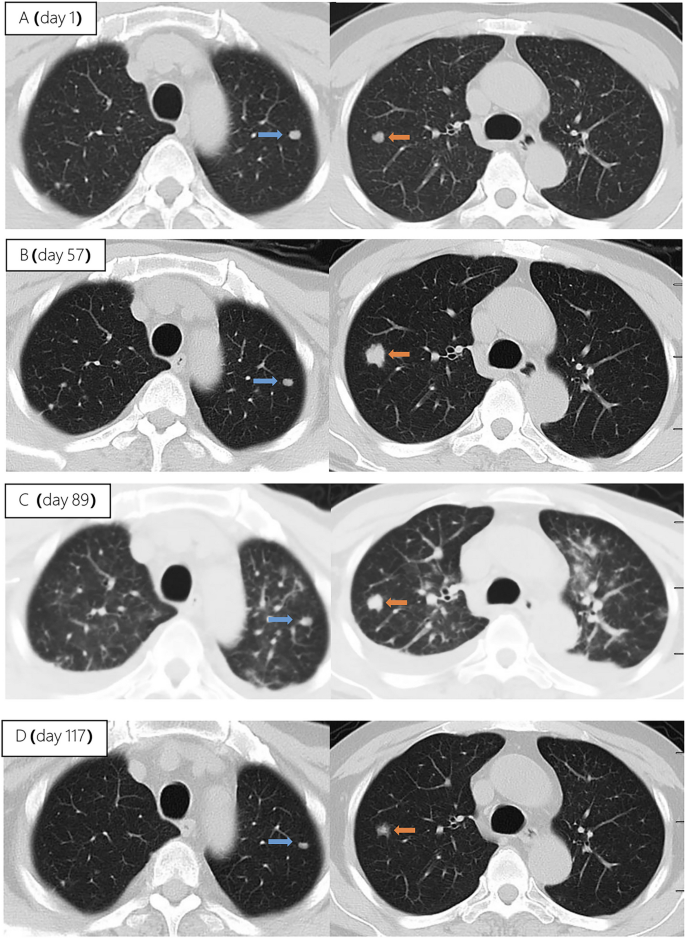
Upon second hospitalization admission ( A ), nodular lesions were already present in the lungs, and their size gradually increased after the initiation of ART ( B , C ). Notably, the lung lesions became more pronounced following the commencement of anti-cryptococcal therapy, coinciding with the occurrence of pleural effusion ( C ). However, with the continuation of antifungal treatment and the addition of glucocorticoids, there was a significant absorption and reduction of both the pleural effusion and pulmonary nodules ( D )
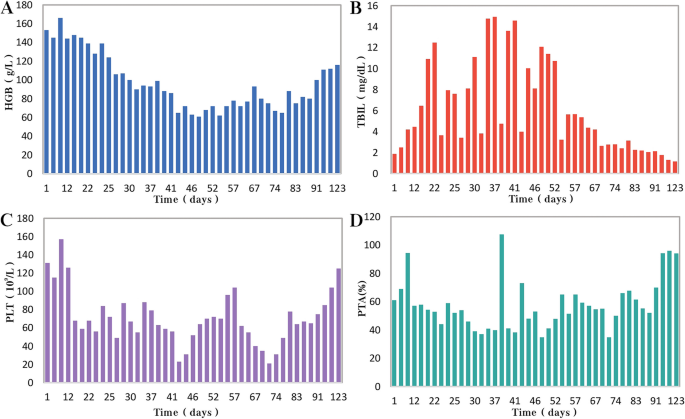
During the patient's second hospitalization, as the anti-tuberculosis treatment progressed and liver failure developed, the patient’s HGB levels gradually decreased ( A ), while TBIL levels increased ( B ). Additionally, there was a gradual decrease in PLT count ( C ) and a reduction in prothrombin activity (PTA) ( D ), indicating impaired clotting function. Moreover, myelosuppression was observed during the anti-cryptococcal treatment ( C )
People living with HIV/AIDS are susceptible to various opportunistic infections, which pose the greatest threat to their survival [ 5 ]. Pulmonary tuberculosis and disseminated cryptococcosis remain opportunistic infections with high mortality rates among AIDS patients [ 9 , 10 ]. These infections occurring on the basis of liver failure not only increase diagnostic difficulty but also present challenges in treatment. Furthermore, as the patient’s immune function and liver function recover, the occurrence of IRIS seems inevitable.
HIV and HBV co-infected patients are at a higher risk of HBV reactivation following the discontinuation of antiviral drugs
In this case, the patient presented with both HIV and HBV infections. Although the HBV DNA test was negative upon admission. However, due to the patient’s self-discontinuation of antiretroviral therapy (ART), HBV virologic and immunologic reactivation occurred six months later, leading to a rapid increase in viral load and subsequent hepatic failure. Charles Hannoun et al. also reported similar cases in 2001, where two HIV-infected patients with positive HBsAg experienced HBV reactivation and a rapid increase in HBV DNA levels after discontinuing antiretroviral and antiviral therapy, ultimately resulting in severe liver failure [ 11 ]. The European AIDS Clinical Society (EACS) also emphasize that abrupt discontinuation of antiviral therapy in patients co-infected with HBV and HIV can trigger HBV reactivation, which, although rare, can potentially result in liver failure [ 12 ].
Diagnosing disseminated Cryptococcus becomes more challenging in AIDS patients with liver failure, and the selection of antifungal medications is significantly restricted
In HIV-infected individuals, cryptococcal disease typically manifests as subacute meningitis or meningoencephalitis, often accompanied by fever, headache, and neck stiffness. The onset of symptoms usually occurs approximately two weeks after infection, with typical signs and symptoms including meningeal signs such as neck stiffness and photophobia. Some patients may also experience encephalopathy symptoms like somnolence, mental changes, personality changes, and memory loss, which are often associated with increased intracranial pressure (ICP) [ 13 ]. The presentation of cryptococcal disease in this patient was atypical, as there were no prominent symptoms such as high fever or rigors, nor were there any signs of increased ICP such as somnolence, headache, or vomiting. The presence of pre-existing pulmonary tuberculosis further complicated the early diagnosis, potentially leading to the clinical oversight of recognizing the presence of cryptococcus. In addition to the diagnostic challenges, treating a patient with underlying liver disease, multidrug-resistant tuberculosis, and concurrent cryptococcal infection poses significant challenges. It requires considering both the hepatotoxicity of antifungal agents and potential drug interactions. EACS and global guideline for the diagnosis and management of cryptococcosis suggest that liposomal amphotericin B (3 mg/kg·d −1 ) in combination with flucytosine (100 mg/kg·d −1 ) or fluconazole (800 mg/d) is the preferred induction therapy for CM for 14 days [ 12 , 14 ]. Flucytosine has hepatotoxicity and myelosuppressive effects, and it is contraindicated in patients with severe liver dysfunction. The antiviral drug bictegravir is a substrate for hepatic metabolism by CYP3A and UGT1A1 enzymes [ 15 ], while fluconazole inhibits hepatic enzymes CYP3A4 and CYP2C9 [ 16 ]. Due to the patient's liver failure and bone marrow suppression, we reduced the dosage of liposomal amphotericin B and fluconazole during the induction period. Considering the hepatotoxicity of fluconazole and its interaction with bictegravir, we decreased the dosage of fluconazole to 600 mg/d, while extending the duration of induction therapy to 28 days.
During re-antiviral treatment, maintaining vigilance for the development of IRIS remains crucial
IRIS refers to a series of inflammatory diseases that occur in HIV-infected individuals after initiating ART. It is associated with the paradoxical worsening of pre-existing infections, which may have been previously diagnosed and treated or may have been subclinical but become apparent due to the host regaining the ability to mount an inflammatory response. Currently, there is no universally accepted definition of IRIS. However, the following conditions are generally considered necessary for diagnosing IRIS: worsening of a diagnosed or previously unrecognized pre-existing infection with immune improvement (referred to as “paradoxical” IRIS) or the unmasking of a previously subclinical infection (referred to as “unmasking” IRIS) [ 8 ]. It is estimated that 10% to 30% of HIV-infected individuals with CM will develop IRIS after initiating or restarting effective ART [ 7 , 17 ]. In the guidelines of the WHO and EACS, it is recommended to delay the initiation of antiviral treatment for patients with CM for a minimum of 4 weeks to reduce the incidence of IRIS. Since we accurately identified the presence of multidrug-resistant pulmonary tuberculosis in the patient during the early stage, we promptly initiated antiretroviral and anti-hepatitis B virus treatment during the second hospitalization. However, subsequent treatment revealed that the patient experienced at least two episodes of IRIS. The first episode was classified as “unmasking” IRIS, as supported by the enlargement of pulmonary nodules observed on the chest CT scan following the initiation of ART (Fig. 2 A). Considering the morphological changes of the nodules on the chest CT before antifungal therapy, the subsequent emergence of disseminated cryptococcal infection, and the subsequent reduction in the size of the lung nodules after antifungal treatment, although there is no definitive microbiological evidence, we believe that the initial enlargement of the lung nodules was caused by cryptococcal pneumonia. As ART treatment progressed, the patient experienced disseminated cryptococcosis involving the blood and central nervous system, representing the first episode. Following the initiation of antifungal therapy for cryptococcosis, the patient encountered a second episode characterized by fever and worsening pulmonary lesions. Given the upward trend in CD4 + T-cell count, we attributed this to the second episode of IRIS, the “paradoxical” type. The patient exhibited a prompt response to low-dose corticosteroids, further supporting our hypothesis. Additionally, the occurrence of cryptococcal IRIS in the lungs, rather than the central nervous system, is relatively uncommon among HIV patients [ 17 ].
Conclusions
From the initial case of AIDS combined with chronic hepatitis B, through the diagnosis and treatment of multidrug-resistant tuberculosis, the development of liver failure and disseminated cryptococcosis, and ultimately the concurrent occurrence of IRIS, the entire process was tortuous but ultimately resulted in a good outcome (Fig. 4 ). Treatment challenges arose due to drug interactions, myelosuppression, and the need to manage both infectious and inflammatory conditions. Despite these hurdles, a tailored treatment regimen involving antifungal and antiretroviral therapies, along with corticosteroids, led to significant clinical improvement. While CM is relatively common among immunocompromised individuals, especially those with acquired immunodeficiency syndrome (AIDS) [ 13 ], reports of disseminated cryptococcal infection on the background of AIDS complicated with liver failure are extremely rare, with a very high mortality rate.
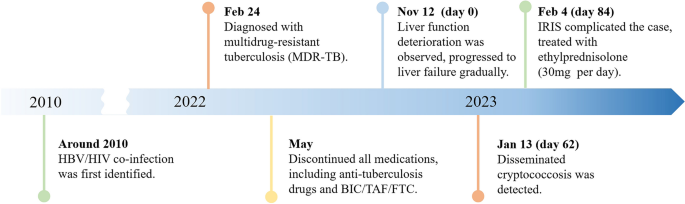
A brief timeline of the patient's medical condition progression and evolution
Through managing this patient, we have also gained valuable insights. (1) Swift and accurate diagnosis, along with timely and effective treatment, can improve prognosis, reduce mortality, and lower disability rates. Whether it's the discovery and early intervention of liver failure, the identification and treatment of disseminated cryptococcosis, or the detection and management of IRIS, all these interventions are crucially timely. They are essential for the successful treatment of such complex and critically ill patients.
(2) Patients who exhibit significant drug reactions, reducing the dosage of relevant medications and prolonging the treatment duration can improve treatment success rates with fewer side effects. In this case, the dosages of liposomal amphotericin B and fluconazole are lower than the recommended dosages by the World Health Organization and EACS guidelines. Fortunately, after 28 days of induction therapy, repeat CSF cultures showed negative results for Cryptococcus, and the improvement of related symptoms also indicates that the patient has achieved satisfactory treatment outcomes. (3) When cryptococcal infection in the bloodstream or lungs is detected, prompt lumbar puncture should be performed to screen for central nervous system cryptococcal infection. Despite the absence of neurological symptoms, the presence of Cryptococcus neoformans in the cerebrospinal fluid detected through lumbar puncture suggests the possibility of subclinical or latent CM, especially in late-stage HIV-infected patients.
We also encountered several challenges and identified certain issues that deserve attention. Limitations: (1) The withdrawal of antiviral drugs is a critical factor in the occurrence and progression of subsequent diseases in patients. Improved medical education is needed to raise awareness and prevent catastrophic consequences. (2) Prior to re-initiating antiviral therapy, a thorough evaluation of possible infections in the patient is necessary. Caution should be exercised, particularly in the case of diseases prone to IRIS, such as cryptococcal infection. (3) There is limited evidence on the use of reduced fluconazole dosage (600 mg daily) during antifungal therapy, and the potential interactions between daily fluconazole (600 mg) and the antiviral drug bictegravir and other tuberculosis medications have not been extensively studied. (4) Further observation is needed to assess the impact of early-stage limitations in the selection of anti-tuberculosis drugs on the treatment outcome of tuberculosis in this patient, considering the presence of liver failure.
In conclusion, managing opportunistic infections in HIV patients remains a complex and challenging task, particularly when multiple opportunistic infections are compounded by underlying liver failure. Further research efforts are needed in this area.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
Hepatitis B virus
Acquired immunodeficiency virus disease
Immune reconstitution inflammatory syndrome
Human immunodeficiency virus
Multi-drug resistant pulmonary tuberculosis
Bronchoalveolar lavage fluid
Bictegravir/tenofovir alafenamide/emtricitabine
Cryptococcal meningitis
World Health Organization
Computed tomography
Total bilirubin
Cerebrospinal fluid
European AIDS Clinical Society
Intracranial pressure
Antiretroviral therapy
Prothrombin activity
Bekker L-G, Beyrer C, Mgodi N, Lewin SR, Delany-Moretlwe S, Taiwo B, et al. HIV infection. Nat Rev Dis Primer. 2023;9:1–21.
Google Scholar
Data on the size of the HIV epidemic. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/data-on-the-size-of-the-hiv-aids-epidemic?lang=en . Accessed 3 May 2023.
Leumi S, Bigna JJ, Amougou MA, Ngouo A, Nyaga UF, Noubiap JJ. Global burden of hepatitis B infection in people living with human immunodeficiency virus: a systematic review and meta-analysis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71:2799–806.
Article Google Scholar
McGovern BH. The epidemiology, natural history and prevention of hepatitis B: implications of HIV coinfection. Antivir Ther. 2007;12(Suppl 3):H3-13.
Article CAS PubMed Google Scholar
Kaplan JE, Masur H, Holmes KK, Wilfert CM, Sperling R, Baker SA, et al. USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus: an overview. USPHS/IDSA Prevention of Opportunistic Infections Working Group. Clin Infect Dis Off Publ Infect Dis Soc Am. 1995;21 Suppl 1:S12-31.
Article CAS Google Scholar
Bamba S, Lortholary O, Sawadogo A, Millogo A, Guiguemdé RT, Bretagne S. Decreasing incidence of cryptococcal meningitis in West Africa in the era of highly active antiretroviral therapy. AIDS Lond Engl. 2012;26:1039–41.
Müller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M, et al. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:251–61.
Article PubMed PubMed Central Google Scholar
Haddow LJ, Easterbrook PJ, Mosam A, Khanyile NG, Parboosing R, Moodley P, et al. Defining immune reconstitution inflammatory syndrome: evaluation of expert opinion versus 2 case definitions in a South African cohort. Clin Infect Dis Off Publ Infect Dis Soc Am. 2009;49:1424–32.
Obeagu E, Onuoha E. Tuberculosis among HIV patients: a review of Prevalence and Associated Factors. Int J Adv Res Biol Sci. 2023;10:128–34.
Rajasingham R, Govender NP, Jordan A, Loyse A, Shroufi A, Denning DW, et al. The global burden of HIV-associated cryptococcal infection in adults in 2020: a modelling analysis. Lancet Infect Dis. 2022;22:1748–55.
Manegold C, Hannoun C, Wywiol A, Dietrich M, Polywka S, Chiwakata CB, et al. Reactivation of hepatitis B virus replication accompanied by acute hepatitis in patients receiving highly active antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2001;32:144–8.
EACS Guidelines | EACSociety. https://www.eacsociety.org/guidelines/eacs-guidelines/ . Accessed 7 May 2023.
Cryptococcosis | NIH. 2021. https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/cryptococcosis . Accessed 6 May 2023.
Chang CC, Harrison TS, Bicanic TA, Chayakulkeeree M, Sorrell TC, Warris A, et al. Global guideline for the diagnosis and management of cryptococcosis: an initiative of the ECMM and ISHAM in cooperation with the ASM. Lancet Infect Dis. 2024;10:S1473-3099(23)00731-4.
Deeks ED. Bictegravir/emtricitabine/tenofovir alafenamide: a review in HIV-1 infection. Drugs. 2018;78:1817–28.
Article CAS PubMed PubMed Central Google Scholar
Bellmann R, Smuszkiewicz P. Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection. 2017;45:737–79.
Shelburne SA, Darcourt J, White AC, Greenberg SB, Hamill RJ, Atmar RL, et al. The role of immune reconstitution inflammatory syndrome in AIDS-related Cryptococcus neoformans disease in the era of highly active antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2005;40:1049–52.
Download references
Acknowledgements
We express our sincere gratitude for the unwavering trust bestowed upon our medical team by the patient throughout the entire treatment process.
This work was supported by the Scientific Research Project of Hunan Public Health Alliance with the approval No. ky2022-002.
Author information
Wei Fu and Zi Wei Deng contributed equally to this work.
Authors and Affiliations
Center for Infectious Diseases, Hunan University of Medicine General Hospital, Huaihua, Hunan, China
Wei Fu, Pei Wang, Zhen Wang Zhu, Ye Pu, Zhi Bing Xie, Yong Zhong Li & Hong Ying Yu
Department of Tuberculosis, The First Affiliated Hospital of Xinxiang Medical University, XinXiang, Henan, China
Department of Clinical Pharmacy, Hunan University of Medicine General Hospital, Huaihua, Hunan, China
Zi Wei Deng
You can also search for this author in PubMed Google Scholar
Contributions
WF and ZWD integrated the data and wrote the manuscript, YHY contributed the revision of the manuscript, PW and YP provided necessary assistance and provided key suggestions, ZWZ, YZL and ZBX contributed data acquisition and interpretation for etiological diagnosis. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Hong Ying Yu .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethics Committee of the Hunan University of Medicine General Hospital (HYZY-EC-202306-C1), and with the informed consent of the patient.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fu, W., Deng, Z.W., Wang, P. et al. A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient. BMC Infect Dis 24 , 533 (2024). https://doi.org/10.1186/s12879-024-09431-9
Download citation
Received : 30 June 2023
Accepted : 24 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12879-024-09431-9

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Liver failure
- Disseminated cryptococcal disease
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Outbreak of Human Trichinellosis — Arizona, Minnesota, and South Dakota, 2022
Weekly / May 23, 2024 / 73(20);456–459
Shama Cash-Goldwasser, MD 1 ; Dustin Ortbahn, MPH 2 ; Muthu Narayan, DO 3 ; Conor Fitzgerald, MPH 4 ; Keila Maldonado 5 ; James Currie, MD 6 ; Anne Straily, DVM 7 ; Sarah Sapp, PhD 7 ; Henry S. Bishop 7 ; Billy Watson, PhD 7 ; Margaret Neja 7 ; Yvonne Qvarnstrom, PhD 7 ; David M. Berman, DO 8 ; Sarah Y. Park, MD 8 ; Kirk Smith, DVM, PhD 9 ; Stacy Holzbauer, DVM 9 ,10 ( View author affiliations )
What is already known about this topic?
Human trichinellosis cases in the United States are rare and are usually acquired through consumption of wild game.
What is added by this report?
Among eight persons who shared a meal that included the meat of a black bear harvested in Canada and frozen for 45 days, six trichinellosis cases were identified. The meat was grilled with vegetables and served rare; two cases occurred in persons who ate only the vegetables. Motile freeze-resistant Trichinella nativa larvae were identified in remaining meat frozen for >15 weeks.
What are the implications for public health practice?
Cooking meat to an internal temperature of ≥165°F (≥74°C) is necessary to kill Trichinella spp. parasites. Trichinella -infected meat can cross-contaminate other foods, and raw meat should be kept and prepared separate from other foods to prevent cross-contamination.
- Article PDF
- Full Issue PDF
Trichinellosis is a parasitic zoonotic disease transmitted through the consumption of meat from animals infected with Trichinella spp. nematodes. In North America, human trichinellosis is rare and is most commonly acquired through consumption of wild game meat. In July 2022, a hospitalized patient with suspected trichinellosis was reported to the Minnesota Department of Health. One week before symptom onset, the patient and eight other persons shared a meal that included bear meat that had been frozen for 45 days before being grilled and served rare with vegetables that had been cooked with the meat. Investigation identified six trichinellosis cases, including two in persons who consumed only the vegetables. Motile Trichinella larvae were found in remaining bear meat that had been frozen for >15 weeks. Molecular testing identified larvae from the bear meat as Trichinella nativa , a freeze-resistant species. Persons who consume meat from wild game animals should be aware that that adequate cooking is the only reliable way to kill Trichinella parasites and that infected meat can cross-contaminate other foods.
Investigation and Results
Index patient notification.
In July 2022, the Minnesota Department of Health was notified of a man aged 29 years who was hospitalized with fever, severe myalgias, periorbital edema, eosinophilia, and other laboratory abnormalities ( Table ); health care providers suspected trichinellosis. The patient had sought care for his symptoms, which commenced in early July, four times and had been hospitalized twice over a 17-day period. During his second hospitalization, providers obtained a history of bear meat consumption, and empiric albendazole treatment for probable trichinellosis was initiated. An investigation was launched to confirm the diagnosis, identify additional cases, and ascertain the source of infection to prevent future cases. The index patient’s diagnosis was confirmed by a positive Trichinella immunoglobulin (Ig) G antibody test result.
Potential Exposure Source Identification
Six days before symptom onset in the index patient, he and eight extended family members from three states (Arizona, Minnesota, and South Dakota) had gathered for several days in South Dakota and shared a meal that included kabobs made from the meat of a black bear ( Ursus americanus ), which had been harvested by one of the family members in northern Saskatchewan, Canada in May 2022. The hunting outfitter had recommended freezing the meat to kill parasites. The meat was frozen in a household freezer* for 45 days until being thawed and grilled with vegetables. The meat was initially inadvertently served rare, reportedly because the meat was dark in color, and it was difficult for the family members to visually ascertain the level of doneness. After some of the family members began eating the meat and noticed that it was undercooked, the meat was recooked before being served again. The family reunion concluded before onset of illness in the index patient.
Laboratory Investigation and Case Definition
Public health authorities in Arizona, Minnesota, and South Dakota interviewed eight of the nine persons who had attended the implicated meal. The ninth attendee was a person aged <18 years whose exposure status could not be confirmed; however, that person reportedly remained healthy. Testing of paired acute and convalescent sera for Trichinella IgG antibodies was recommended for the eight exposed persons and was completed for six. Pathogen-agnostic microbial cell-free metagenomic DNA sequencing ( 1 ) was performed on plasma samples from the index patient and one other person who had sought care twice before being hospitalized with fever, myalgias, abdominal pain, periorbital edema, and laboratory abnormalities. Trichinellosis cases were classified according to the 2014 case definition from the Council for State and Territorial Epidemiologists (CSTE), † (i.e., the presence of clinically compatible symptoms in a person who had consumed an epidemiologically implicated meal or meat in which the parasite was demonstrated [probable] or had a positive serologic test result for Trichinella antibodies [confirmed]). Samples of frozen bear meat were obtained from the household freezer and sent to CDC for artificial tissue digestion and microscopic examination for larvae and molecular testing for Trichinella spp.
Additional Case Detection and Exposure Source Confirmation
Among the eight interviewed persons, five consumed the bear meat, and eight consumed the vegetables that had been cooked with it. Six of the eight persons who attended the meal, including four who consumed the bear meat and the vegetables, and two who consumed only the vegetables (but no meat), had symptoms consistent with trichinellosis, and met case criteria (two confirmed and four probable). Patients with trichinellosis ranged in age from 12 to 62 years and lived in three states: Arizona (one), Minnesota (four), and South Dakota (one). All cases were diagnosed in the patients’ state of residence. Three of the six symptomatic persons, two of whom sought care at least twice before being offered treatment, were hospitalized. The three hospitalized persons received trichinellosis-directed treatment with albendazole. § All six symptomatic persons recovered; the nonhospitalized patients did not receive trichinellosis-directed treatment because their symptoms had resolved with supportive care only, and the benefit of treatment after larval invasion of muscle is unclear ( 2 ). Six persons submitted a serum sample, each collected within 4 weeks of symptom onset; two specimens tested positive for Trichinella IgG antibodies by enzyme-linked immunosorbent assay. Two persons submitted a plasma sample for microbial cell-free DNA sequencing during hospitalization for trichinellosis-compatible symptoms, and both plasma samples tested positive for Trichinella spp. DNA. Microscopy identified motile Trichinella larvae (>800 larvae/g) in samples of bear meat that had been frozen for 110 days in a household freezer ( Figure ). Real-time multiplex polymerase chain reaction testing ( 3 ) of the bear meat was positive for T. nativa and whole genome sequencing identified mitochondrial sequences 100% identical to T. nativa.
Public Health Response
The family member who harvested the bear and provided meat samples for testing was advised to discard any remaining meat. All identified trichinellosis cases were reported to appropriate state health departments and to CDC. CDC notified the Public Health Agency of Canada of the outbreak and the confirmed source of infection. This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy. ¶
Trichinellosis is rarely reported in the United States. As a result of changes in pork production practices from historical norms that fostered transmission, most cases reported in recent years are attributed to consumption of meat from wild game ( 4 ). During January 2016–December 2022, seven U.S. trichinellosis outbreaks, including 35 probable and confirmed cases, were reported to CDC; bear meat was the suspected or confirmed source of infection in the majority of those outbreaks (CDC, unpublished data, 2022). Estimates of Trichinella infection prevalence among wild animal host species vary widely. A Trichinella infection prevalence range of at least 1% to 24% among black bears in Canada and Alaska has been reported, and even higher prevalences of Trichinella infection are reported among species of predators that are strict carnivores (e.g., polar bear, wolverine, and cougar) ( 5 ). The frequency with which black bear meat is the implicated source of human infection might be driven by hunting practices, ecological factors, and the relatively high parasite density observed in the muscle of infected black bears compared with that of other species ( 6 , 7 ).
Because symptoms of trichinellosis are typically nonspecific, diagnosis of infection requires a high index of suspicion; however, periorbital edema and certain laboratory abnormalities (e.g., eosinophilia and elevated creatine kinase levels) can provide etiologic clues. In this outbreak, two of the hospitalized patients sought care multiple times before receiving a diagnosis. Four of the six patients met clinical and epidemiologic criteria and thus were considered probable cases. Laboratory confirmation can be challenging because of the limited sensitivity of antibody testing early in illness ( 8 ); in this investigation, acute Trichinella IgG test results were positive in only two of six tested patient specimens. The clinical utility of trichinellosis test results obtained after acute illness is limited, and historically, public health investigators have had difficulty obtaining convalescent serum samples from persons who have recovered. Laboratory criteria in the current CSTE trichinellosis case definition do not include nucleic acid testing of human specimens. The sensitivity of such assays to detect Trichinella DNA in blood is uncharacterized; however, plasma samples from both patients tested by metagenomic sequencing ( 1 ) yielded positive results for Trichinella DNA. As demonstrated in this outbreak, pathogen-agnostic molecular assays can be useful for detection of rare diseases when standard workup is unrevealing and if other diagnostic tests lack sensitivity.
Implications for Public Health Practice
Although freezing kills Trichinella species commonly implicated in pork-associated outbreaks, freeze-resistant Trichinella species, including T. nativa and the T6 genotype ( 9 ), predominate in Arctic and sub-Arctic regions ( 6 ). Larval motility was observed in bear meat that had been frozen for nearly 4 months (110 days). Persons who consume game meat, especially that harvested in northern latitudes, should be informed that adequate cooking is the only reliable way to kill Trichinella parasites. Cooking wild game meat to an internal temperature of ≥165°F (≥74°C) is recommended by public health authorities**; temperatures should be verified with a meat thermometer. As demonstrated in this outbreak, the color of meat is not a good indicator of cooking adequacy. Safe handling of raw meat (i.e., separating raw or undercooked meat and its juices from other foods) is recommended to prevent trichinellosis; this investigation and previous investigations suggest that Trichinella -infected meat can cross-contaminate other foods ( 10 ). Government and private entities that oversee and organize hunting should educate hunters about these risks and effective preventative measures.
Acknowledgments
The persons affected by this outbreak; Lauren Ahart, Sue Montgomery, Parasitic Diseases Branch, CDC.
Corresponding author: Shama Cash-Goldwasser, [email protected] .
1 Epidemic Intelligence Service, CDC; 2 South Dakota Department of Health; 3 University of Minnesota, Minneapolis, Minnesota; 4 Arizona Department of Health Services; 5 Maricopa County Department of Public Health, Phoenix, Arizona; 6 Lakeview Clinic, Waconia, Minnesota; 7 Division of Parasitic Diseases and Malaria, Center for Global Health, CDC; 8 Medical Affairs, Karius, Inc., Redwood City, California; 9 Minnesota Department of Health; 10 Division of State and Local Readiness, Center for Preparedness and Response, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. David M. Berman reports that he is a paid laboratory medical consultant for Precision Health Solutions and reports ownership of company shares in Karius, Inc. No other potential conflicts of interest were disclosed.
* The temperature of the freezer is not known.
† https://ndc.services.cdc.gov/case-definitions/trichinellosis-2014/
§ https://www.cdc.gov/trichinellosis/hcp/clinical-care/index.html
¶ 45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq.
** https://www.cdc.gov/trichinellosis/prevention/index.html
- Blauwkamp TA, Thair S, Rosen MJ, et al. Analytical and clinical validation of a microbial cell-free DNA sequencing test for infectious disease. Nat Microbiol 2019;4:663–74. https://doi.org/10.1038/s41564-018-0349-6 PMID:30742071
- Pozio E, Sacchini D, Sacchi L, Tamburrini A, Alberici F. Failure of mebendazole in the treatment of humans with Trichinella spiralis infection at the stage of encapsulating larvae. Clin Infect Dis 2001;32:638–42. https://doi.org/10.1086/318707 PMID:11181129
- Almeida M, Bishop H, Nascimento FS, Mathison B, Bradbury RS, Silva AD. Multiplex TaqMan qPCR assay for specific identification of encapsulated Trichinella species prevalent in North America. Mem Inst Oswaldo Cruz 2018;113:e180305. https://doi.org/10.1590/0074-02760180305 PMID:30379199
- Wilson NO, Hall RL, Montgomery SP, Jones JL. Trichinellosis surveillance—United States, 2008-2012. MMWR Surveill Summ 2015;64(No. SS-1):1–8. PMID:25590865
- Oksanen A, Kärssin A, Berg RPKD, et al. Epidemiology of Trichinella in the Arctic and subarctic: a review. Food Waterborne Parasitol 2022;28:e00167. https://doi.org/10.1016/j.fawpar.2022.e00167 PMID:35812081
- Gajadhar AA, Forbes LB. A 10-year wildlife survey of 15 species of Canadian carnivores identifies new hosts or geographic locations for Trichinella genotypes T2, T4, T5, and T6. Vet Parasitol 2010;168:78–83. https://doi.org/10.1016/j.vetpar.2009.10.012 PMID:19926223
- Harms NJ, Larivee M, Scandrett B, Russell D. High prevalence and intensity of Trichinella infection in Yukon American Black ( Ursus americanus ) and Grizzly ( Ursus arctos ) bears. J Wildl Dis 2021;57:429–33. https://doi.org/10.7589/JWD-D-20-00135 PMID:33822166
- Yang Y, Cai YN, Tong MW, et al. Serological tools for detection of Trichinella infection in animals and humans. One Health 2016;2:25–30. https://doi.org/10.1016/j.onehlt.2015.11.005 PMID:28616474
- Pozio E. Adaptation of Trichinella spp. for survival in cold climates. Food Waterborne Parasitol 2016;4:4–12. https://doi.org/10.1016/j.fawpar.2016.07.001
- Hall RL, Lindsay A, Hammond C, et al. Outbreak of human trichinellosis in Northern California caused by Trichinella murrelli . Am J Trop Med Hyg 2012;87:297–302. https://doi.org/10.4269/ajtmh.2012.12-0075 PMID:22855761
Abbreviations: eos = eosinophils; F = female; M = male; NA = not applicable; ND = not done; WBC = white blood cell. * Initial results are from hospitalization during which trichinellosis was suspected. Reference ranges varied among different laboratories that conducted testing. † Reference range = 4–88. § Reference range = 39–208. ¶ Consumed vegetables that were cooked and served with the bear meat. ** Reference range = 39–308.
FIGURE . Microscopic examination of encapsulated larvae in a direct black bear meat muscle squash prep (A), larvae liberated from artificially digested bear meat (B), and motile larvae viewed with differential interference contrast microscopy (C and D)* from black bear meat suspected as the source of an outbreak of human Trichinella nativa infections — Arizona, Minnesota, and South Dakota, 2022
Photos/Division of Parasitic Diseases and Malaria, Center for Global Health, CDC
* Scale bars = 100 µ m.
Suggested citation for this article: Cash-Goldwasser S, Ortbahn D, Narayan M, et al. Outbreak of Human Trichinellosis — Arizona, Minnesota, and South Dakota, 2022. MMWR Morb Mortal Wkly Rep 2024;73:456–459. DOI: http://dx.doi.org/10.15585/mmwr.mm7320a2 .
MMWR and Morbidity and Mortality Weekly Report are service marks of the U.S. Department of Health and Human Services. Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services. References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of pages found at these sites. URL addresses listed in MMWR were current as of the date of publication.
All HTML versions of MMWR articles are generated from final proofs through an automated process. This conversion might result in character translation or format errors in the HTML version. Users are referred to the electronic PDF version ( https://www.cdc.gov/mmwr ) and/or the original MMWR paper copy for printable versions of official text, figures, and tables.
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
- Open access
- Published: 29 May 2024
Using 2% PVPI topical solution for serial intravitreous injections and ocular surface findings: a case control study
- José Henrique Casemiro 1 ,
- Ana Paula Miyagusko Taba Oguido 2 &
- Antonio Marcelo Barbante Casella 3
International Journal of Retina and Vitreous volume 10 , Article number: 41 ( 2024 ) Cite this article
27 Accesses
Metrics details
The use of povidone-iodine for ocular surface asepsis is widespread for intravitreal injections. They became frequent procedures, leading to serial exposure of patients’ eyes to iodinated solutions. In this study, we investigate the changes in the ocular surface in patients submitted to repeated use of povidine for intravitreal injection of anti-VEGF asepsis, analyzing Ocular Surface Disease Index, non-invasive break up time, blinking quality, lipid layer, meniscus height and osmolarity.
This case-control study included 34 individuals (68 eyes), 14 males, 20 females aged 48 to 94. Inclusion criteria were individuals who received application of 2% povidone-iodine eyedrops for intravitreal injections treatment with the non-treated contralateral eye used as control. Ocular surface examinations were performed at a single occasion. A pre-intravitreal injection asepsis protocol with povidone-iodine was applied. All statistical analysis was performed using the STATA® 18.0 Software and a p-value = 0.05 was considered as the statistical significance value in all tests.
The median number of IVIs in treated eyes was 12 (range 6–20). The results in treated eyes compared with untreated eyes were respectively : median OSDI 16 (IQR 6–39) and 12.5 (IQR 8–39) ( p = 0.380); mean NIBUT 10.30 (SD ± 2.62) and 10.78 (SD ± 2.92) ( s, p = 0.476); median blinking quality 100 (IQR 100) and 100 (IQR 100 ) (%, p = 0.188); median lipid layer 87 (IQR 77–90) and 86 (IQR 74–100) (nm, p = 0.451); median meniscus height 0.22 (IQR 0.19-0,31) and 0.24 (IQR 0.20–0.27) (mm, p = 0.862), median Meibomian gland atrophy 33 (IQR 24–45) and 31.5 (IQR 25–39) (%, p = 0.524); and mean osmolarity 306.6 (SD ± 21.13) and 313.8 (SD ± 29) (mOsm, p = 0.297). There was no statistically significant relationship between the repetitive use of 2% iodinated solution and signs or symptoms compatible with dry eye syndrome in this group of patients.
Conclusions
The findings suggest that 2% povidone iodine is a safe and efficacious agent for ocular surface antisepsis during intravitreal injections, not leading to substantial ocular surface modifications. This conclusion supports the continued use of povidone iodine in routine ophthalmic procedures without increased risk of inducing dry eye syndrome.
The use of povidone iodine (PVPI) for ocular surface asepsis is widespread, both for surgical procedures and intravitreal injections [ 1 , 2 , 3 , 4 , 5 ]. Surgeries for cataracts, glaucoma, and intravitreal injections have become common and frequent procedures in ophthalmology, leading to the serial exposure of patients’ eyes to iodine solutions [ 5 , 6 , 7 , 8 , 9 , 10 ]. These changes are directly associated with dry eye syndrome [ 11 , 12 ].
In particular, studies have demonstrated that intravitreal injections used to treat diabetic macular edema or age-related macular degeneration result in significant changes in the ocular surface, leading to dry eye syndrome and damage to homeostasis of the ocular surface [ 5 , 11 , 13 , 14 ].
Dry eye syndrome is a multifactorial disease of the ocular surface characterized by the loss of tear film homeostasis, hyperosmolarity, inflammation, damage and neurosensory abnormalities [ 11 , 15 , 16 , 17 , 18 ]. Its etiology is variable, ranging from nonspecific inflammation of the ocular surface to direct chemical or physical aggression, infections, and autoimmune diseases [ 11 , 12 , 15 , 19 ].
In addition to the most common symptoms, burning sensation, itching, speck, eye redness, excess tearing reflex, brightness sensitivity, and quality of vision loss are also frequent findings that affect efficiency at work and the quality of life of patients [ 11 , 12 , 15 , 19 , 20 ].
This study aimed to observe changes in the ocular surface and tear film due the serial use of 2% PVPI, the gold standard drug for asepsis of the ocular surface. As it is well known that pre-injection antisepsis of the ocular surface with PVPI has a toxic effect on the corneal epithelium, the aim is to identify changes in the tear film and ocular surface and avoid serious problem like dry eye syndrome [ 11 , 12 , 21 , 22 ].
A case-control study was conducted at the Ophthalmology and Psicology Clinic (APMTO MD) in Londrina, Paraná. The patients were recruited from the Retina and Vitreous Institute (AMBC MD) in Londrina, Paraná. The study included 34 individuals (68 eyes). 14 males, 20 females, aged 48 to 94 years. All participants signed the informed consent form, which allowed their participation in the study. Inclusion criteria were individuals who received application of 2% PVPI eyedrops for anti-VEGF IVIs treatment with the contralateral eye used as control, that had not been treated with any topical medication during the same period of applications and good comprehension of the Ocular Questionnaire Surface Disease Index (OSDI). Exclusion criteria were patients who could not understand the OSDI questionnaire; patients using antidepressant medicine, diuretics, sympathomimetics, eye drops for glaucoma, or eye lubricants; people with allergies to iodine; unfavorable clinical conditions to undergo the examination procedures for the study; inappropriate test quantity and quality; unsatisfactory images or unsatisfactory and inadequate data.
The study was approved by the Ethics and Research Committee Involving Human Beings of the State University of Londrina by N. 5.300.176.
The individuals underwent directed clinical and ophthalmological analysis, received explanations about the study, used their data, and signed consent forms. All clinical measures were performed using the IDRA equipment (SBSSISTEMI, Orbasano, Torino, Italy), at which time the OSDI questionnaire was also applied and tear osmolarity was collected using the I-PEN ® (I-MED PHARMA INC. Dollard-des-Ormeaux, QC, Canada). All examinations and administration of the questionnaire were performed by the same professional. No drops or medications that could cause changes in any subsequent measurements were used.
The variables analyzed were age, sex, date of the last PVPI application, number of PVPI applications, OSDI questionnaire, tear osmolarity, NBUT, tear film interferometry, tear meniscus height, percentage of meibomian gland loss, and blink quality. The sequence of procedures obeyed the following order: Explanation to the subject regarding the exams and questionnaire to which he would be submitted, guidance to the patient not to identify in any way the eye being treated and the eye not treated during data collection, nor during the questionnaire OSDI; patient positioning in the IDRA® equipment; capture of blinking quality video images; capture of tear film interferometry; capture of images to measure the height of the tear meniscus and immediate measurement; capture of tear film (NBUT); image capture for the percentage of meibomian gland loss by everting the lower eyelid with a cotton swab; positioning the patient outside the IDRA equipment; application of the I-PEN® electrode to capture tear osmolarity in the lower conjunctiva, first in the right eye, and subsequently in the left eye; application of the OSDI questionnaire.
All statistical analyses were performed using STATA® 18.0 Software and p-values ≤ 0.05 indicated statistical significance.
The Shapiro-Wilk test was used to verify data normality. Data that did not follow a normal distribution were analyzed using the Wilcoxon rank-sum test and were described as means and as medians and interquartile ranges. Data that showed normality were analyzed using the Student’s T test and presented as means and standard deviations. Descriptive, quantitative, and multivariate analyses compared treated (case) and untreated (control) eyes.
The average number of IVIs in treated eyes was 12 (range 6–20). The results in treated eyes compared with untreated eyes were respectively: median OSDI 16 (IQR 6–39) and 12.5 (IQR 8–39) ( p = 0.380); mean NIBUT 10.30 (SD ± 2,62) and 10.78 (SD ± 2.92) ( s, p = 0.476); median blinking quality 100 (IQR 100) and 100 (IQR 100 ) (%, p = 0.188); median lipid layer 87 (IQR 77–90) and 86 (IQR 74–100) (nm, p = 0.451); median meniscus height 0,22 (IQR 0.19–0.31) and 0.24 (IQR 0.20–0.27) (mm, p = 0.862), median Meibomian gland athrophy 33 (IQR 24–45) and 31.5 (IQR 25–39) (%, p = 0.524); and mean osmolarity 306.6 (SD ± 21.13) and 313.8 (SD ± 29) (mOsm, p = 0.297).). The results revealed that the use of 2% PVPI did not affect the analyzed variables in a statistically significant way. All data is summarized on Table 1 .
These results are disposable on fig 1 , 2 , 3 , 4 , 5 , 6 , 7 , 8 and 9 as annexed.
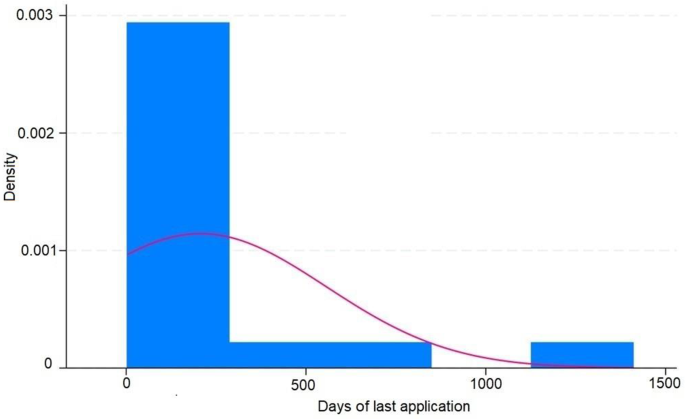
Histogram showing the days of last application of IVIS ( intravitreal injections ) in treated eyes and the density showing the proportion of eyes in each period of time
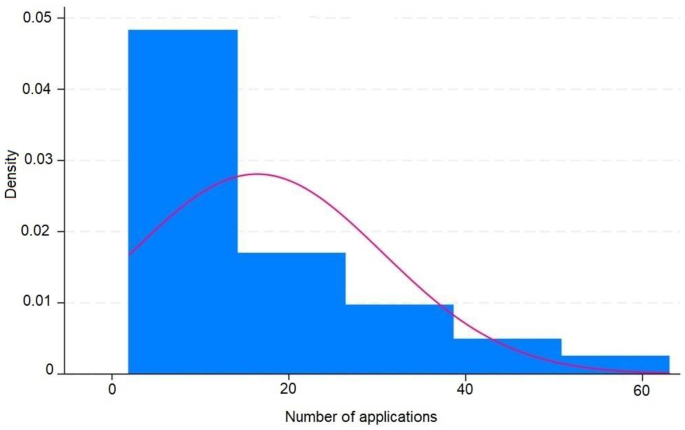
Histogram showing the number of application ov IVIS ( intravitreal injections ) in treated eyes and the density showing the proportion of eyes in each amount of number of applications
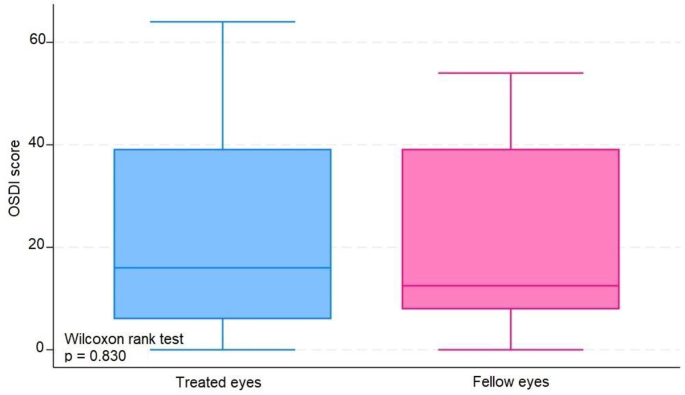
Blue box plot showing score OSDI ( Ocular Surface Disease Index ) in treated eyes comparing with pink box plot showing score OSDI in fellow eyes
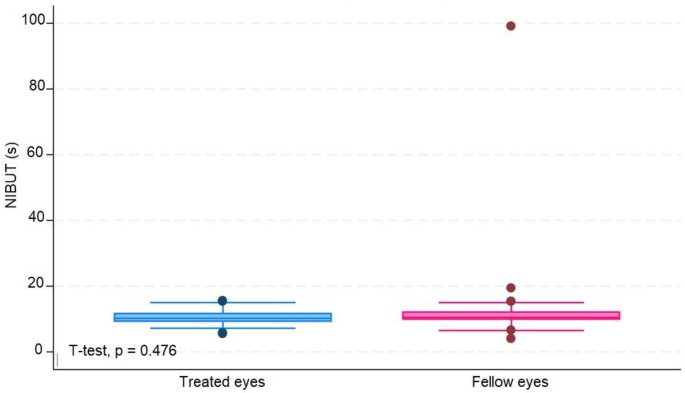
Blue box plot showing NIBUT ( non invasive break up time ) in seconds in treated eyes comparing with pink box plot showing NIBUT in seconds in fellow eyes
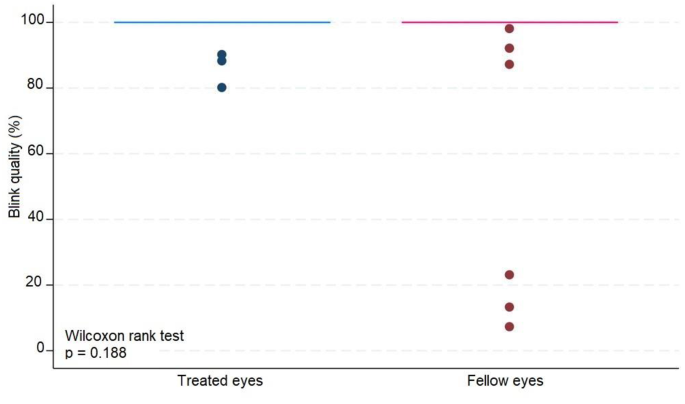
Blue box plot showing blink quality in treated eyes comparing with pink box plot showing blink quality in fellow eyes
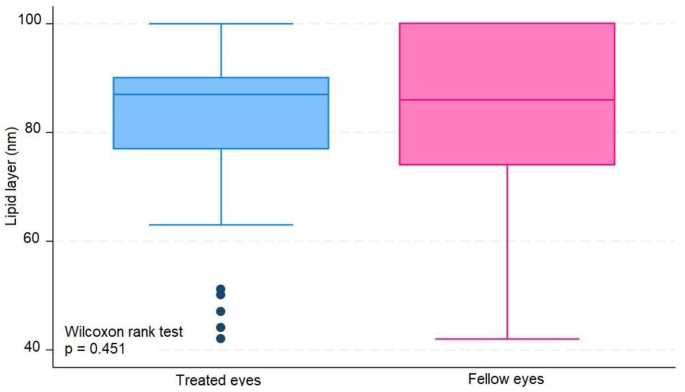
Blue box plot showing lipid layer in treated eyes comparing with pink box plot showing lipid layer in fellow eyes
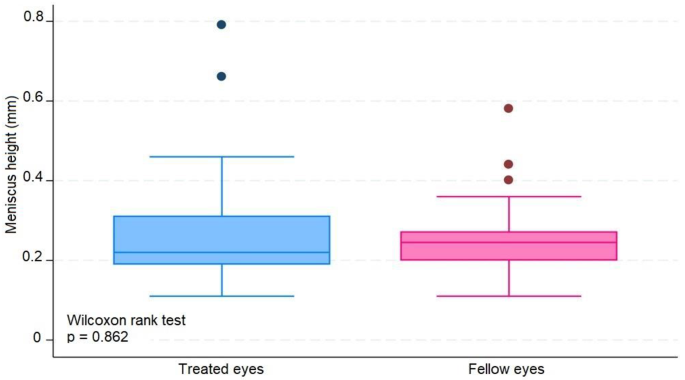
Blue box plot showing meniscus height in milimeters in treated eyes comparing with pink box plot showing meniscus height in milimeters in fellow eyes
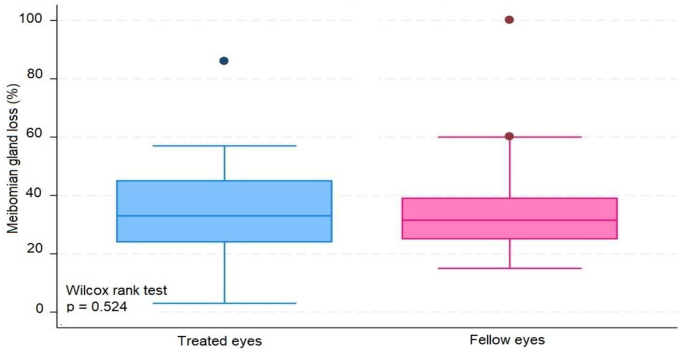
Blue box plot showing Meibomian gland loss in treated eyes comparing with pink box plot showing Meibomian gland loss in fellow eyes
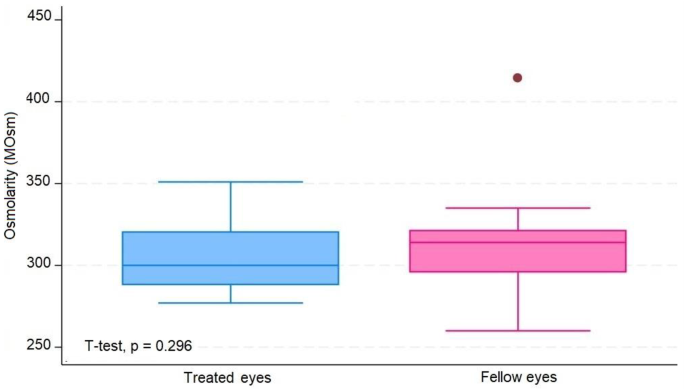
Blue box plot showing tear osmolarity in miliosmoles in treated eyes comparing with pink box plot showing osmolarity in miliosmoles in fellow eyes
Through multivariate analysis, we obtained some interesting outcomes as follows:
When controlling for NIBUT, meibomian gland atrophy, number of applications, and days of the last application according to treatment, sex was an important variable in explaining the variability in the OSDI score (coef = 15.63 | p-value = 0.003). On average, controlling for the abovementioned variables, being female contributed to an increase in the OSDI to 15.63 points.
After controlling for meniscus height and age according to treatment, tear osmolarity contributed significantly to variability in the lipid layer (coef = -0.266, p = 0.004). In this sense, the addition of one unit in tear osmolarity led to a -0.266 drop in the lipid layer.
After controlling for meniscus height, OSDI, days since the last application, age, and sex according to the treatment, these factors contributed significantly to the variability in the lipid layer [(coef = 0.562 | p-value = 0.004) (coef = − 5.622 | p-value = 0.048)]. In this sense, the addition of one year of age led to a decrease of -0.562 on average. For the same treatment group, female sex led to a decrease of -5,622.
Age, lipid layer, meniscus height, sex according to treatment, age according to treatment, and sex were important factors for explaining the variability in tear osmolarity.
We noticed that a greater age correlated with lower tear osmolarity. However, being in the treated group reduced the decrease in tear osmolarity with advancing age.
Being female implied higher tear osmolarity. However, the increase in tear osmolarity was smaller in the treated group.
A greater height of the lipid layer and meniscus correlated with lower tear osmolarity.
The present study showed that the use of topical PVPI at 2% did not cause significant damage to the ocular surface when the findings of the ocular surface and tear film analyses were used.
Our results contradict some existing data indicating the toxicity of long-term iodine use on the ocular surface; we found two statistically relevant results that the application of iodine may improve the stability of the tear film in the elderly and women, since the eyes in older individuals and female patients that received iodine showed a smaller increase in tear osmolarity [ 4 , 14 , 23 , 24 ].
Moreover, the results of this study corroborated some hypotheses that the use of PVPI could be positive in some dry eye disease diagnostic features, such as the improvement of the tear film meniscus height and the decrease of the tear film osmolarity [ 25 , 26 ].
A localized anti-inflammatory surface effect of the anti-VEGF agent used in intravitreous injections should be considered and assessed in further studies [ 22 , 25 ].
The literature review also shows that there was an improvement in the tear function of some patients who used iodine in ocular asepsis [ 25 , 26 , 27 ], perhaps due to an antimicrobial action preventing the proliferation of bacterial flora that could produce harmful enzymes or cause meibomitis and blepharitis [ 25 , 26 , 28 ].
The cell regeneration mechanism might have satisfactorily recomposed the ocular surface or the tear homeostasis might have compensates for the damage caused by iodine in the cells in question; furthermore, these are just hypotheses.
We also determined that the risk factors for dry eye disease, age and female sex [ 10 , 16 , 29 , 30 ], were associated with the observed clinical data: greater ages lower the height of the tear meniscus, the greater the tear osmolarity, and the smaller the lipid layer of the tear film. The female sex was also associated with higher OSDI scores and fewer tear film lipid layers.
Regardless of the cause or consequence, the osmolarity and lipid layer of the tear film were inversely proportional.
Through multivariate analysis, we determined that the risk factors for dry eye syndrome, age, and female sex correlated with worse results in the tear meniscus measurement tests, OSDI questionnaire, and tear film interferometry, corroborating the literature implicating them as risk factors for dry eye disease [ 20 , 30 , 31 ].
Moreover, due to the sample size, false negatives, or simply because in practice, iodine in the amount and frequency used does not lead to histological damage that may reflect functional changes. The results did not discourage the use of iodine for ocular asepsis but also did not indicate its use for protocols with higher concentrations or more applications than those used in current protocols.
The strengths of the study are as follows: the same patient was the control and treated group, avoiding any environmental or medical bias. The number of injections administered was higher than that reported in other studies. No drops were used during the examination to avoid artificial changes to the tear film.
The limitations of this study were as follows: the study had a small sample size of 34 patients, resulting in 68 eyes being analyzed, which may have caused an analysis bias when using these data in the general population. We must remember that the analyzed population was from southern Brazil and had mostly descended from Italian, German, Spanish, and Portuguese immigrants; therefore, these data may only reflect the specific epidemiology of this population. The meibomian glands analyzed were located in the inferior tarsus.
The use of iodine on the ocular surface was not significantly associated with any of the evaluated parameters. There were no statistically significant correlations between the tests applied to the case eyes. The current study indicates that the application of 2% topical povidone-iodine (PVPI) does not inflict significant damage to the ocular surface, as evidenced by the analyses of the ocular surface and tear film. Notable strengths of this study include the use of the same patient as both the control and the treated subject, which minimizes potential biases from environmental or medical factors. Additionally, the absence of any artificial agents during the examination ensures that the tear film remains unaltered.
Contrary to previous concerns regarding the long-term toxicity of iodine on the ocular surface, our findings suggest potential benefits of iodine application in stabilizing the tear film, particularly in older individuals and female patients. This is supported by a smaller increase in tear osmolarity in these groups following iodine application. Furthermore, the study corroborates hypotheses that PVPI may positively affect certain Dry Eye Disease diagnostic features, such as improved tear film meniscus height and reduced tear film osmolarity.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Povidine or polyvinylpyrrolidone-iodine
- Intravitreal injections
Vascular endothelial growth factor
Ocular Surface Disease Index
Non invasive break up time
Blink quality
Lipid layer
Standard deviation
Interquartile range
Oakley C, Allen P, Hooshmand J, Vote BJT. PAIN AND ANTISEPSIS AFTER OCULAR ADMINISTRATION OF POVIDONE-IODINE VERSUS CHLORHEXIDINE. Retina. 2018;38:2064–6.
Article CAS PubMed Google Scholar
Fukuda M, Shibata S, Shibata N, Fujita N, Miyashita H, Tanimura N, et al. Polyvinyl alcohol-iodine induced corneal epithelial injury in vivo and its protection by topical rebamipide treatment. PLoS ONE. 2018;13:e0208198.
Article PubMed PubMed Central Google Scholar
Grzybowski A, Brona P. Povidone-iodine is still a premium antiseptic measure in ocular surgery. Acta Ophthalmol. 2017;95.
Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C-K, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276–83.
Article PubMed Google Scholar
Craig JP, Nelson JD, Azar DT, Belmonte C, Bron AJ, Chauhan SK, et al. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017;15:802–12.
Moss SE. Prevalence of and risk factors for Dry Eye Syndrome. Arch Ophthalmol. 2000;118:1264.
Jiang X, Wang Y, Lv H, Liu Y, Zhang M, Li X. Efficacy of intra-meibomian gland injection of the anti-VEGF agent bevacizumab for the treatment of meibomian gland dysfunction with lid-margin vascularity. Drug Des Devel Ther. 2018;12:1269–79.
Article CAS PubMed PubMed Central Google Scholar
Kim S, Ahn Y, Lee Y, Kim H. Toxicity of povidone-iodine to the ocular surface of rabbits. BMC Ophthalmol. 2020;20:359.
Malmin A, Thomseth VM, Førland PT, Khan AZ, Hetland HB, Chen X, et al. Associations between serial Intravitreal injections and Dry Eye. Ophthalmology. 2023;130:509–15.
Audelan T, Legrand M, M’Garrech M, Best A-L, Barreau E, Labetoulle M, et al. Vieillissement de la surface oculaire : physiopathologie et conséquences pratiques pour la prise en charge. J Fr Ophtalmol. 2018;41:262–70.
Kanclerz P, Myers WG. Potential substitutes for povidone-iodine in ocular surgery. Eye. 2021;35:2657–9.
Reibaldi M, Avitabile T, Bandello F, Longo A, Bonfiglio V, Russo A, et al. The effectiveness of 0.6% povidone Iodine Eye drops in reducing the Conjunctival bacterial load and needle contamination in patients undergoing Anti-VEGF intravitreal injection: a prospective, randomized study. J Clin Med. 2019;8:1031.
Han SB. Prevalence of Dry Eye Disease in an Elderly Korean Population. Arch Ophthalmol. 2011;129:633.
Silas MR, Schroeder RM, Thomson RB, Myers WG. Optimizing the antisepsis protocol: effectiveness of 3 povidone–iodine 1.0% applications versus a single application of povidone–iodine 5.0%. J Cataract Refract Surg. 2017;43:400–4.
Zhang X, Wang L, Zheng Y, Deng L, Huang X. Prevalence of dry eye disease in the elderly. Medicine. 2020;99:e22234.
Donnenfeld ED, Holland EJ, Solomon KD, Fiore J, Gobbo A, Prince J, et al. A Multicenter Randomized Controlled Fellow Eye Trial of pulse-dosed Difluprednate 0.05% Versus Prednisolone acetate 1% in cataract surgery. Am J Ophthalmol. 2011;152:609–e6171.
Grzybowski A, Kanclerz P, Myers WG. The use of povidone–iodine in ophthalmology. Curr Opin Ophthalmol. 2018;29:19–32.
Bramantyo T, Roeslani RD, Andriansjah A, Sitorus RS. The efficacy of 1% Chloramphenicol Eye Ointment Versus 2.5% povidone-iodine Ophthalmic Solution in reducing bacterial colony in Newborn Conjunctivae. Asia-Pacific J Ophthalmol. 2015;4:180–3.
Article CAS Google Scholar
Bourcier T, Acosta MC, Borderie V, Borra´s F, Gallar J, Bury T, et al. Decreased corneal sensitivity in patients with Dry Eye. Invest Opthalmology Visual Sci. 2005;46:2341.
Article Google Scholar
Niederkorn JY, Kaplan HJ. Rationale for Immune Response and the Eye. Immune Response and the Eye. Basel: KARGER; 2007. pp. 1–3.
Google Scholar
Saedon H, Nosek J, Phillips J, Narendran N, Yang YC. Ocular surface effects of repeated application of povidone iodine in patients receiving frequent intravitreal injections. Cutan Ocul Toxicol. 2017;36:343–6.
Beni´tez-del-Castillo JM, Acosta MC, Wassfi MA, Di´az-Valle D, Gegu´ndez JA, Fernandez C et al. Relation between Corneal Innervation with Confocal Microscopy and Corneal Sensitivity with Noncontact Esthesiometry in Patients with Dry Eye. Investigative Opthalmology & Visual Science. 2007;48:173.
Yu K, Asbell PA, Shtein RM, Ying G-S. Dry Eye subtypes in the Dry Eye Assessment and Management (DREAM) study: a latent Profile Analysis. Transl Vis Sci Technol. 2022;11:13.
Dohlman TH, Lertsuwanroj B, D’Amico DJ, Ciralsky JB, Kiss S. Evaluation of signs and symptoms of ocular surface disease after intravitreal injection. Acta Ophthalmol. 2019;97.
Zoukhri D. Effect of inflammation on lacrimal gland function. Exp Eye Res. 2006;82:885–98.
Shelanski HASM. PVP-iodine: history, toxicity, and therapeutic uses. J Int Coll Surg. 1956;25:727–34.
CAS PubMed Google Scholar
Kemeny-Beke A, Szodoray P. Ocular manifestations of rheumatic diseases. Int Ophthalmol. 2020;40:503–10.
Zamora JL. Chemical and microbiologic characteristics and toxicity of povidone-iodine solutions. Am J Surg. 1986;151:400–6.
Mantelli F, Lambiase A, Sacchetti M, Orlandi V, Rosa A, Casella P, et al. Cocaine snorting may induce ocular surface damage through corneal sensitivity impairment. Graefe’s Archive Clin Experimental Ophthalmol. 2015;253:765–72.
Bever GJ, Brodie FL, Hwang DG. Corneal Injury from Presurgical Chlorhexidine Skin Preparation. World Neurosurg. 2016;96:610.e1-610.e4.
Wolffsohn JS, Arita R, Chalmers R, Djalilian A, Dogru M, Dumbleton K, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15:539–74.
Download references
Acknowledgements
APMO provided IDRA analysis, and was a contributor to design the study, revised, written and approved the manuscript. AMBC Applied intravitreal injections and provided patients for the study and was a contributor to design the study, revised, written and approved the manuscript.
No grant Money was received for this resesearch.
Author information
Authors and affiliations.
Postgraduate Program in Health Sciences, State University of Londrina, UEL, Londrina, Brazil
José Henrique Casemiro
Department of Health Sciences, Surgical Clinic, State University of Londrina, UEL, Londrina, Brazil
Ana Paula Miyagusko Taba Oguido
Londrina State University, Avenida Robert Koch, 60, Londrina, Paraná, 86038-440, Brazil
Antonio Marcelo Barbante Casella
You can also search for this author in PubMed Google Scholar
Contributions
JHC analyzed and interpreted patient data, reviewed the literature and was a major contributor to the acquisition of data, interviewed the patients, sponsored supplies, designed the study and written the manuscript. APMO provided IDRA analysis, and was a contributor to design the study, revised, written and approved the manuscript. AMBC Applied intravitreal injections and provided patients for the study and was a contributor to design the study, revised, written and approved the manuscript.
Corresponding author
Correspondence to Antonio Marcelo Barbante Casella .
Ethics declarations
Ethics approval and consent to participate and consent for publication.
Approval for the anonymous analisys of Imaging data and medical records was obtained from the Institutional Review Board.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Casemiro, J.H., Oguido, A.P.M.T. & Casella, A.M.B. Using 2% PVPI topical solution for serial intravitreous injections and ocular surface findings: a case control study. Int J Retin Vitr 10 , 41 (2024). https://doi.org/10.1186/s40942-024-00557-1
Download citation
Received : 11 March 2024
Accepted : 07 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s40942-024-00557-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dry eye disease
- Povidone iodine
- Ocular surface disease
International Journal of Retina and Vitreous
ISSN: 2056-9920
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 28 May 2024
Triggers of intensive care patients with palliative care needs from nurses’ perspective: a mixed methods study
- Manuela Schallenburger 1 ,
- Jacqueline Schwartz 1 , 5 ,
- Andrea Icks 2 , 5 ,
- Jürgen in der Schmitten 3 ,
- Yann-Nicolas Batzler 1 ,
- Stefan Meier 4 ,
- Miguel Mendez-Delgado 4 ,
- Theresa Tenge 4 &
- Martin Neukirchen 1 , 4 , 5
Critical Care volume 28 , Article number: 181 ( 2024 ) Cite this article
195 Accesses
Metrics details
Triggers have been developed internationally to identify intensive care patients with palliative care needs. Due to their work, nurses are close to the patient and their perspective should therefore be included. In this study, potential triggers were first identified and then a questionnaire was developed to analyse their acceptance among German intensive care nurses.
For the qualitative part of this mixed methods study, focus groups were conducted with intensive care nurses from different disciplines (surgery, neurosurgery, internal medicine), which were selected by convenience. Data were analysed using the “content-structuring content analysis” according to Kuckartz. For the quantitative study part, the thus identified triggers formed the basis for questionnaire items. The questionnaire was tested for comprehensibility in cognitive pretests and for feasibility in a pilot survey.
In the qualitative part six focus groups were conducted at four university hospitals. From the data four main categories (prognosis, interprofessional cooperation, relatives, patients) with three to 15 subcategories each could be identified. The nurses described situations requiring palliative care consults that related to the severity of the disease, the therapeutic course, communication within the team and between team and patient/relatives, and typical characteristics of patients and relatives. In addition, a professional conflict between nurses and physicians emerged. The questionnaire, which was developed after six cognitive interviews, consists of 32 items plus one open question. The pilot had a response rate of 76.7% (23/30), whereby 30 triggers were accepted with an agreement of ≥ 50%.
Intensive care nurses see various triggers, with interprofessional collaboration and the patient's prognosis playing a major role. The questionnaire can be used for further surveys, e.g. interprofessional triggers could be developed.
Intensive care units (ICU) are places of surviving in which patients in crisis situations are stabilised to such extent that discharge can be aimed for and the possibility of recovery exists [ 1 , 2 , 3 ]. It is often claimed that a reduction in quality of life is accepted in return. However, attempts are made to include aspects of quality of life in therapy goals and treatment planning. Patients’ values are also enquired about and should be taken into account [ 4 ].
Despite the efforts of intensive care teams, critically ill people who can no longer be cured lie in intensive care units. In addition 20% of patients die in an ICU or shortly after admission to an ICU [ 1 , 2 ]. ICU patients and their relatives can therefore suffer from distressing symptoms [ 1 , 2 ]. Therefore palliative care needs may arise [ 2 ]. Appropriate pain and symptom management, as well as consistent communication and decision-making, can be a challenge in patients with life-threatening illness [ 5 ]. Recommendations support the early integration of palliative care structures within the ICU setting [ 6 , 7 , 8 ]. Integration of such structures is possible at various levels. Primary palliative care can be provided by the ICU teams themselves without specialised palliative care (sPC) teams by addressing all palliative needs of patients and relatives. Another option would be the consultative model, in which the specialised palliative care team addresses all palliative care needs. However, the mixed model is the most recommended. Here, ICU and sPC teams work together to fulfil the palliative needs of patients and relatives [ 9 ].
Palliative care teams focus on symptom relief, effective communication about treatment goals, alignment of treatment with patients’ preferences, family support and care planning [ 5 ]. Co-treatment by multiprofessional sPC teams therefore is an appropriate option for ICU patients and can also be offered in conjunction with life-prolonging treatments and especially in collaboration with ICU teams [ 10 , 11 , 12 ]. Timely integration of palliative care can complement counselling, treatment and support for relatives and patients, which can lead to improved quality of life and satisfaction for both [ 13 ]. The length of stay in ICU may be reduced and inappropriate therapies avoided [ 2 , 5 ]. Communication between physicians and nurses can improve and lead to higher patient and care-taker satisfaction [ 13 ].
Despite the advantages of collaboration between intensive and palliative care, difficulties of identifying patients who benefit from such shared care persist. Various studies have investigated different incentives that should lead to involvement of palliative care, including treatment preferences and options, length of stay and conflicts [ 5 , 14 , 15 , 16 , 17 ]. Such so-called triggers were either determined in expert panels or retrospectively collected using patient data.
In Germany, these triggers were supplemented in an expert panel and checked for acceptance among ICU physicians [ 18 ]. Table 1 describes examples of possible clinical situations to which potential triggers may apply and how patients can benefit from collaboration between ICU and sPC teams.
As nurses play a major role in the care of ICU patients, they should be involved in decision-making [ 10 ] as well as in the development of triggers [ 15 ].
The aim of this study was to identify triggers that, from the perspective of German ICU nurses, should prompt the involvement of sPC for an ICU patient, and to evaluate the acceptance of these triggers.
In order to achieve the study objective, focus groups were conducted to identify triggers. These were then formulated into items for a questionnaire. The questionnaire was tested and an initial analysis of the acceptance of the triggers was carried out. Figure 1 illustrates the detailed study design and objectives.
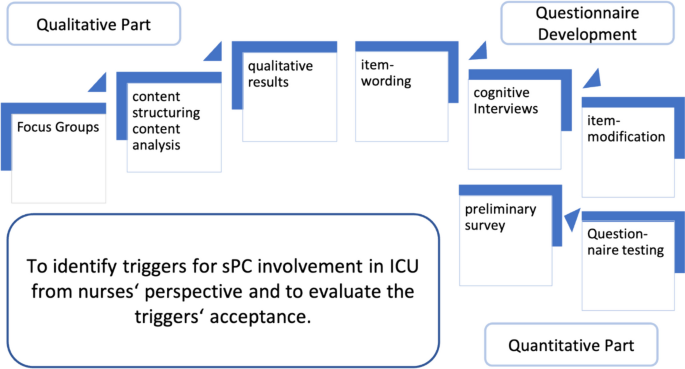
Conceptional model and study aims. sPC specialised palliative care, ICU intensive care unit
Focus groups
Semi-structured focus groups were conducted with ICU nurses to obtain their perspectives. Potential participants were informed about the study by gatekeepers, in this case management staff, and asked to participate. Volunteers participated in the sense of a convenience sample. Nurses with at least 1 year of professional experience and current work in ICU who had contact with sPC were included. The interview guide was developed by the author team based on the research question about possible triggers for sPC involvement, including sub-questions and targeted follow-up questions. The focus groups were moderated by MS, a nurse and research assistant (Dr. PH) with experience in qualitative research and palliative and neonatal intensive care. This experience and her interest in the study—to deeper understand and strengthen the nurses' perspective—was disclosed to the participants in advance. Focus groups were recorded as audio files and transcribed according to “simple rules” [ 19 ]. No field notes were made.
Data were analysed in seven steps (initiating textwork–main categories–coding–compile passages–subcodes–coding–analysis) using the “content-structuring content analysis” according to Kuckartz [ 20 ]. Data coding was primarily done by MS using MAXQDA (Version 12, Verbi GmbH). The authors MN and JidS participated in the analysis and coding. This took place in close consultation.
Questionnaire development
The qualitative analysis took place independently of the following step of item formulation. Nevertheless, it was the basis for developing a questionnaire to assess the acceptance of the identified triggers. These were worded into items considering the ten principles of question framing [ 21 ]. An intention was to correspond to as closely as possible to the data material. Not only the main categories and subcategories were relevant, but also the data material in the sense of the transcripts of the focus groups in order to include the content mentioned. The formulated items were repeatedly discussed in a multi-stage process within the research group with regard to appropriateness and understanding. Participants were asked for agreement on a five-point Likert scale.
In order to optimise comprehensibility, cognitive interviews were conducted to learn more about the cognitive processes that take place when answering the questions. Of interests here is how the interviewees interpret and understand terms or questions, how they recall information and events from mind, how they make decisions about how to answer and how they allocate their answers to the formal answer categories. In the present study, the techniques of inquiring for understanding, paraphrasing and thinking aloud were used [ 22 ]. When inquiring about understanding, participants are asked to describe their understanding of certain terms or the entire item. Paraphrasing asks participants to repeat an item in their own words without remembering the literal text. Thinking aloud is intended to capture the mental processes that take place when answering the items. To do this, the item is read out loud and the participants are asked to speak out their thoughts on answering. The interviews were recorded as audio files and then also transcribed according to “simple rules” [ 19 ]. When MS conducted the interviews, care was taken not to use any non-verbal amplifiers.
In this way, almost all items were assessed for understanding. Only items that seemed evident were left out, such as the question whether the patients’ age could be a trigger for involving sPC. Test persons were nurses with intensive and palliative care experience.
Questionnaire testing with preliminary survey
Following the cognitive interview screening, a pilot was conducted in which the questionnaire was given to a small sample (n = 30) of the envisaged target group. For recruitment, head staff from three intensive care units were approached, who distributed the questionnaires to potential participants. The sample was asked to complete the questionnaire, and invited to critically comment on each item as well as at the end of the questionnaire. In addition, the time needed to complete the questionnaire was measured.
The analysis of the pilot also indicated a first tendency of the acceptance of triggers. For this purpose, as in a former study on the acceptance of triggers for sPC involvement among ICU physicians, all triggers that received at least 50% agreement were defined as accepted [ 18 ].
The study was approved by the Ethic Committee of the Medical Faculty of the Heinrich-Heine-University Duesseldorf, Germany (Study ID: 6114R) and conform to the Declaration of Helsinki. Written informed consent was obtained from all participants, who were all at least 18 years old.
Between February 2018 and July 2019, six focus groups were conducted at four German university hospitals, involving a total of 28 ICU nurses. They represented the fields of surgery, neurosurgery and internal medicine. Three participants cancelled their participation due to illness. The duration of the focus groups, which took place in separate rooms in the work environment, was 45–90 min.
After four focus groups, there seemed to be a saturation, which became more apparent after the fifth. To strengthen this assumption, a sixth focus group took place which yielded no relevant additional information.
Since all the triggers mentioned were to be included in the evaluation and thus in the development of the questionnaire, no member check, in which the analysis is returned to the participants for review, took place.
All participants were able to report experiences of cooperation with sPC. They expressed seeing the patients’ benefit from the support, but they would like the teams to be involved earlier and more regularly. The most important element is that sPC do something good for the patients and that nurses themselves can benefit from the expertise.
Just do something good for the person for an hour (FG 1) Simply use the expertise they bring with them (FG 6)
Overall, four main categories “prognosis, interprofessional cooperation, relatives, patients” could be formed out of the data with three to 15 subcategories each. Table 2 shows the main categories of the focus groups with examples of the related quotes and examples of the answers to the open question on piloting the questionnaire.
In this category, factors are named that have an influence on or are associated with a certain course and thus the prognosis. Consequently, it is about the ethical assessment of the patient's situation and the treatments undertaken, in which the ICU nurses ask for support from sPC.
SPC can support in raising comprehensive awareness of the patient's situation and enable a natural passing in the highly technical field by looking at the overall situation.
Severe pre-existing conditions such as certain oncological diseases, complications, the need for resuscitation or ventilation and length of stay in the ICU can have an influence on the prognosis and were therefore seen as triggers for the involvement of sPC.
Interprofessional cooperation
The participants described a potential for conflicts between ICU nurses and physicians at various points of care when nurses would like to have support from sPC.
ICU nurses prefer to be more involved in decisions, especially in order not to maintain life-sustaining treatment unnecessarily. In addition, they see different levels of knowledge and understanding about the work and tasks of sPC which can intensify a conflict.
Conflicts can also arise in terms of communication. The participants see that ICU physicians do not always communicate openly with relatives as well as with themselves, the nurses. This can make decision-making more difficult and increase burdens.
Factors that can trigger sPC consultation can also be found in relatives. For example, they may be so burdened by the situation that they need additional support. This is particularly relevant in decision-making, where relatives may feel a sense of responsibility. SPC can also provide support in involving relatives in care processes.
Relatives` wish for palliative care counts also as a trigger for the participants. Conversely, a relative`s forceful request for ongoing life-sustaining treatment in a clear palliative situation also represents a trigger.
Personal characteristics of the patients can also be reasons for involving sPC.
Concerning age, sPC is more likely to be involved in the case of young patients.
The triggers developed from the qualitative results led to 32 questionnaire items. These related to the individual patients` situation, the disease or the overall situation between the patient and the treatment team. The items were supplemented by an open free-text field in which further, unnamed triggers could be specified, as well as nine questions on demographics.
Cognitive interviews
In the cognitive interviews, 6 items were not tested because they were clearly understandable, such as the question about the age of the patient or the length of stay in the ICU.
In order to test the 26 other items, five cognitive interviews were conducted with one participant each, all of whom had experience in both intensive and palliative care. None of them had been part of the previous focus groups. They were asked about five or six items each in 60–90 min interviews.
The evaluation showed that four items should be modified. For example, the term “natural death” had to be defined more precisely. The remaining 22 items were understood as they were meant. The items’ interpretation by the participants was consistent to what the focus groups had described.
Questionnaire pilot with preliminary survey
The questionnaire used for the pilot consisted of 32 triggers to be tested, one open question for triggers not mentioned, nine questions on demographics and three additional questions at the end that can give statements on the piloting of the questionnaire, i.e., a total of 45 questions.
Possible participation was openly addressed in the participating ICU teams, as was the voluntariness of participation. Due to the SARS-CoV-2 pandemic and the associated burdens as well as a general shortage of staff in nursing teams, the response rate was 76.7% of the 30 questionnaires distributed. The study team consulted with each other and decided that the number of questionnaires was sufficient for an initial survey and thus for the tendency of the results. Data on the participants are listed in Table 3 .
On average, completion of the questionnaire took 27 min. Twelve participants used the free text fields under the items (Table 2 ). The free comments related mainly to a reason for accepting or rejecting the particular trigger.
Some free text statements were similar to the statements in the focus groups, describing own experiences with the sPC teams.
One item which refers to the likelihood to achieve treatment goals was adjusted on the basis of the free text comments because the term “treatment goal” was perceived as ambiguous.
The answers “fully agree” and “rather agree” were evaluated as acceptance of the respective trigger, and “rather disagree” and “strongly disagree” as rejection. “No statement” was also collected and indicated, but was not included in acceptance or rejection. With at least 50% agreement, 30 of the 32 triggers were accepted and two were rejected. Figure 2 illustrates the results of the individual items.
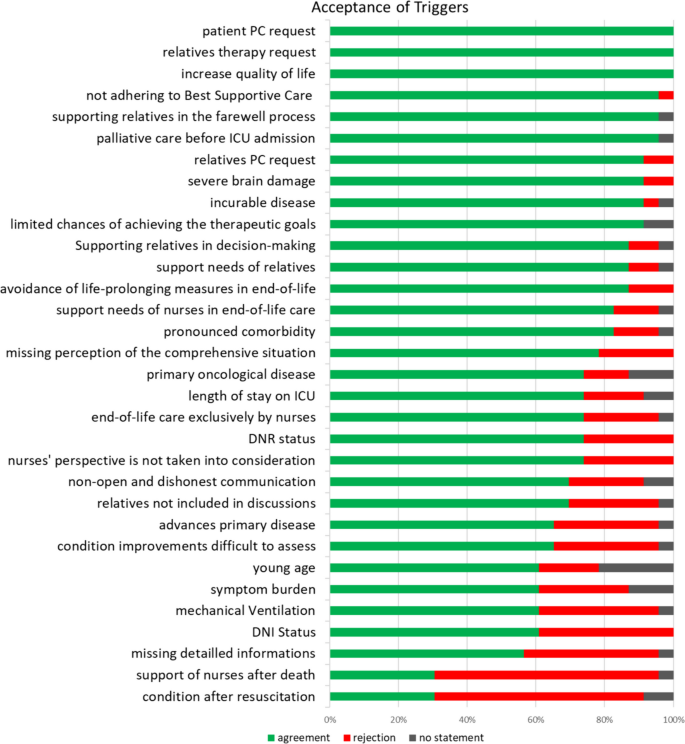
Acceptance of the triggers in the pilot. ICU intensive care unit, PC palliative care, DNR do not resuscitate, DNI no ICU transfer
For further differentiation, the participants were able to provide detailed information on time and age for the questions on age, duration of ventilation and length of stay in the ICU. The median duration of ventilation was 21 days, the median duration of stay in the ICU was 14 days and the median age was < 50 years.
A further more detailed description was possible for the item symptom burden in order to name symptoms for which the participants expect a benefit from involving a sPC team. Anxiety, pain and depression were named most frequently.
The present study aimed to identify possible triggers for the involvement of sPC for ICU patients and their relatives from the perspective of ICU nurses. The identification of patients who benefit most from sPC involvement is important both to address the patients individual needs and to use sPC as a limited resource efficiently [ 9 , 23 ]. The triggers identified in the present study relate to the individual patient situation and the support needs of patients, relatives and the intensive care nurses.
The focus groups show a conflict between physicians and nurses. Intensive care nurses feel not sufficiently involved in treatment decisions, decisions about further procedures and discussions with the patient, as mentioned in the focus groups, which leads to frustration [ 3 ]. They feel that they would involve sPC more often if they were more involved in decisions or had the opportunity to involve sPC themselves. However, physicians still want to initiate sPC involvement themselves [ 16 ].
ICU nurses ask for support from sPC in recognising and adhering to treatment limitations and in including their perceptions in decision-making processes. Especially when the prognosis is unclear, the challenge often is to recognize timely when maximum therapeutic measures represent a burdensome overtreatment that is out of proportion to the possible outcome [ 4 ]. A good ethical climate in the ICU and nursing involvement at the end of life can reduce excessive care [ 24 ]. The rejection of the trigger “support of nurses after death” is difficult to interpret. In the literature, relatives describe the situation very differently, sometimes they continue to receive support, sometimes they have the feeling that care ends quickly after death [ 25 ]. Perhaps more education is needed here about the fact that palliative care does not have to end with the death of the patient, but that it can initially accompany the relatives. ICU and sPC nurses can then provide this support together. Perhaps ICU nurses do not see any need for themselves here because they have sufficient expertise in this area and do not have any need for further support. Further consideration is required here.
Pre-existing diseases, whether related to the acute crisis or not, can have an influence on prognosis. These can include oncological diseases or brain damage like mentioned in the focus groups. Other advanced conditions such as chronic obstructive pulmonary disease or heart failure may also worsen prognosis [ 26 , 27 ]. Such underlying diseases may facilitate the involvement of sPC. Here the tasks of palliative care lie in recovery and maintenance of quality of life [ 5 , 28 ].
The importance of relatives in the decision to involve the sPC team is made clear in the study by the fact that they were often mentioned in the focus groups and also agreed with the items concerning them in the questionnaire. They should therefore be given prominence and taken into account not only in decision-making processes, but also in the provision of care.
They experience an exceptional situation, which can lead to increased stress and thus to an increased need for support [ 3 ]. SPC can offer additional support here, also because they can offer psycho(onco)logical support due to the multiprofessional structure. This can increase the quality of care [ 15 ].
ICU patients are often unable to communicate and thus express their wishes. As a result, relatives oftentimes communicate the patient's wishes on the basis of advance directives or presumed patient will and, if they are legal representatives, make decisions on their behalf. Therefore, they have to be adequately informed about the current condition, therapeutic options, their consequences and short- and long-term prognosis [ 29 ].
It may be helpful for them to be able to identify triggers for sPC involvement through discussion or involvement in decision-making and care. These may even be co-developed or asked for their perspective during the development. There is a need for further research.
The length of stay in an intensive care unit is mentioned as a trigger both in this study and in the literature. A stay of more than 7 days [ 15 ] or 1 month [ 14 ] is cited as a reason for sPC involvement. SPC can provide support in clarifying the prognosis, but can also be a constant reference person for relatives with frequently changing intensive care staff [ 30 ].
In the case of age, the literature tends to see old age as a trigger [ 5 , 17 ]. The reason why young age is mentioned more in the focus groups may be due to the additional emotional burden felt by the caregivers.
In this study, triggers were analysed from the perspective of nurses. As nurses and physicians work together in the ICU, acceptance of the triggers by both professional groups is important.
The triggers in this study can only be partially compared with those from the literature due to the different identification. However, eight triggers— patients’ request, relatives' request, incurable disease , (severe) brain damage, length of stay in ICU, primary oncological disease, (high) symptom burden , mechanical ventilation—were tested for acceptance among German ICU physicians [ 18 ] and were also named by nursing staff in the present study. The four in italics are accepted by both professional groups and can therefore form the basis for interprofessional decisions or further studies on multiprofessional triggers.
Limitations
It cannot be excluded that for the focus groups mainly nurses volunteered who felt that the involvement of the sPC was particularly important, and therefore had a greater interest in participating. This may mean that other perspectives are underrepresented in our sample.
Much of what is said in the focus groups can also be part of an ethics consultation [ 31 ]. Here it would be necessary to differentiate whether sPC is necessary or whether an ethic consultation can support.
The pilot was planned with 30 questionnaires in order to test the questionnaire, but also to conduct a first evaluation. Due to the tense situation, also caused by the SARS-CoV-2 pandemic, which led to enormous stress for the carers, this number was not reached. The response rate of 23 questionnaires allows no more than an explorative analysis of pure agreement versus rejection.
The participants in this study were ICU nurses. The results show that relatives are highly relevant. They and their perspective should therefore be the target group of future studies on this topic.
The nurses interviewed in the focus groups see a clear benefit for those affected in the shared care provided by sPC. In the perspective of ICU nurses, the relevant functions of sPC can be both advisory and (co-)treating.
With the formulated triggers, they can now bring this into decision-making processes. A shared exchange based on the triggers can also support the conflict described.
The piloted questionnaire can now be used to test the triggers for acceptance in a larger cohort. The initial evaluation confirms the triggers brought forward in the focus groups. A cross-professional survey is also possible to develop multi-professional triggers.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due the extend but are available from the corresponding author on reasonable request.
Abbreviations
Intensive care unit
Specialised palliative care
Doctoral degree in public health
Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32:638–43. https://doi.org/10.1097/01.CCM.0000114816.62331.08 .
Article PubMed Google Scholar
Aslakson R, Cheng J, Vollenweider D, Galusca D, Smith TJ, Pronovost PJ. Evidence-based palliative care in the intensive care unit: a systematic review of interventions. J Palliat Med. 2014;17:219–35. https://doi.org/10.1089/jpm.2013.0409 .
Article PubMed PubMed Central Google Scholar
Clemens KE, Klaschik E. Integration palliativmedizinischer Prinzipien in die Behandlung von Intensivpatienten: Vom “shared decision making” und der Begleitung von Angehörigen. Anästhesiol Intensivmed Notfallmed Schmerzther. 2009;44:88–94.
Michalsen A, Neitzke G, Dutzmann J, Rogge A, Seidlein A-H, Jöbges S, et al. Überversorgung in der Intensivmedizin: erkennen, benennen, vermeiden: Positionspapier der Sektion Ethik der DIVI und der Sektion Ethik der DGIIN. [Overtreatment in intensive care medicine-recognition, designation, and avoidance: Position paper of the Ethics Section of the DIVI and the Ethics section of the DGIIN]. Med Klin Intensivmed Notfmed. 2021. https://doi.org/10.1007/s00063-021-00794-4 .
Norton SA, Hogan LA, Holloway RG, Temkin-Greener H, Buckley MJ, Quill TE. Proactive palliative care in the medical intensive care unit: effects on length of stay for selected high-risk patients. Crit Care Med. 2007;35:1530–5. https://doi.org/10.1097/01.CCM.0000266533.06543.0C .
Michels G, John S, Janssens U, Raake P, Schütt KA, Bauersachs J, et al. Palliativmedizinische Aspekte in der klinischen Akut- und Notfallmedizin sowie Intensivmedizin: Konsensuspapier der DGIIN, DGK, DGP, DGHO, DGfN, DGNI, DGG, DGAI, DGINA und DG Palliativmedizin. [Palliative aspects in clinical acute and emergency medicine as well as intensive care medicine: Consensus paper of the DGIIN, DGK, DGP, DGHO, DGfN, DGNI, DGG, DGAI, DGINA and DG Palliativmedizin]. Med Klin Intensivmed Notfmed. 2023;118:1–25. https://doi.org/10.1007/s00063-023-01016-9 .
Article Google Scholar
Michels G, Schallenburger M, Neukirchen M. Recommendations on palliative care aspects in intensive care medicine. Crit Care. 2023;27:355. https://doi.org/10.1186/s13054-023-04622-3 .
Neukirchen M, Metaxa V, Schaefer MS. Palliative care in intensive care. Intensive Care Med. 2023;49:1538–40. https://doi.org/10.1007/s00134-023-07260-z .
Curtis JR, Higginson IJ, White DB. Integrating palliative care into the ICU: a lasting and developing legacy. Intensive Care Med. 2022;48:939–42. https://doi.org/10.1007/s00134-022-06729-7 .
Edwards JD, Voigt LP, Nelson JE. Ten key points about ICU palliative care. Intensive Care Med. 2017;43:83–5. https://doi.org/10.1007/s00134-016-4481-6 .
Frontera JA, Curtis JR, Nelson JE, Campbell M, Gabriel M, Mosenthal AC, et al. Integrating palliative care into the care of neurocritically ill patients. Crit Care Med. 2015;43:1964–77. https://doi.org/10.1097/CCM.0000000000001131 .
Mentzelopoulos SD, Chen S, Nates JL, Kruser JM, Hartog C, Michalsen A, et al. Derivation and performance of an end-of-life practice score aimed at interpreting worldwide treatment-limiting decisions in the critically ill. Crit Care. 2022;26:106. https://doi.org/10.1186/s13054-022-03971-9 .
Gade G, Venohr I, Conner D, McGrady K, Beane J, Richardson RH, et al. Impact of an inpatient palliative care team: a randomized control trial. J Palliat Med. 2008;11:180–90. https://doi.org/10.1089/jpm.2007.0055 .
Bradley CT, Brasel KJ. Developing guidelines that identify patients who would benefit from palliative care services in the surgical intensive care unit. Crit Care Med. 2009;37:946–50. https://doi.org/10.1097/CCM.0b013e3181968f68 .
Nelson JE, Curtis JR, Mulkerin C, Campbell M, Lustbader DR, Mosenthal AC, et al. Choosing and using screening criteria for palliative care consultation in the ICU: a report from the improving palliative care in the ICU (IPAL-ICU) Advisory Board. Crit Care Med. 2013;41:2318–27. https://doi.org/10.1097/CCM.0b013e31828cf12c .
Wysham NG, Hua M, Hough CL, Gundel S, Docherty SL, Jones DM, et al. Improving ICU-based palliative care delivery: a multicenter, multidisciplinary survey of critical care clinician attitudes and beliefs. Crit Care Med. 2017;45:e372–8. https://doi.org/10.1097/CCM.0000000000002099 .
Hua MS, Li G, Blinderman CD, Wunsch H. Estimates of the need for palliative care consultation across united states intensive care units using a trigger-based model. Am J Respir Crit Care Med. 2014;189:428–36. https://doi.org/10.1164/rccm.201307-1229OC .
Adler K, Schlieper D, Kindgen-Milles D, Meier S, Schallenburger M, Sellmann T, et al. Will your patient benefit from palliative care? A multicenter exploratory survey about the acceptance of trigger factors for palliative care consultations among ICU physicians. Intensive Care Med. 2019;45:125–7. https://doi.org/10.1007/s00134-018-5461-9 .
Dresing T, Pehl T. Praxisbuch transkription: regelsysteme, software und praktische anleitungen für qualitative forscherinnen. 2nd ed. Marburg: Eigenverlag; 2011.
Google Scholar
Kuckartz U. Qualitative inhaltsanalyse. Methoden, praxis, computerunterstützung. 4th ed. Weinheim: Beltz Juventa; 2018.
Porst R. Praxis der umfrageforschung. Wiesbaden: VS Verlag für Sozialwissenschaften; 2000.
Book Google Scholar
Prüfer P, Rexroth M. Kognitive interviews. Mannheim: Zentrum für Umfragen; 2005.
Downar J, Hua M, Wunsch H. Palliative care in the intensive care unit: past, present, and future. Crit Care Clin. 2023;39:529–39. https://doi.org/10.1016/j.ccc.2023.01.007 .
Benoit DD, Jensen HI, Malmgren J, Metaxa V, Reyners AK, Darmon M, et al. Outcome in patients perceived as receiving excessive care across different ethical climates: a prospective study in 68 intensive care units in Europe and the USA. Intensive Care Med. 2018;44:1039–49. https://doi.org/10.1007/s00134-018-5231-8 .
Article CAS PubMed PubMed Central Google Scholar
Nelson JE, Cortez TB, Curtis JR, Lustbader DR, Mosenthal AC, Mulkerin C, et al. Integrating palliative care in the ICU. J Hosp Palliat Nurs. 2011;13:89–94. https://doi.org/10.1097/NJH.0b013e318203d9ff .
Cao Y, Xing Z, Long H, Huang Y, Zeng P, Janssens J-P, Guo Y. Predictors of mortality in COPD exacerbation cases presenting to the respiratory intensive care unit. Respir Res. 2021;22:77. https://doi.org/10.1186/s12931-021-01657-4 .
Dai Y, Qin S, Pan H, Chen T, Bian D. Impacts of comorbid chronic obstructive pulmonary disease and congestive heart failure on prognosis of critically ill patients. Int J Chron Obstruct Pulmon Dis. 2020;15:2707–14. https://doi.org/10.2147/COPD.S275573 .
Berendt J, Ostgathe C, Simon ST, Tewes M, Schlieper D, Schallenburger M, et al. Zusammenarbeit von Intensivmedizin und Palliativmedizin: Eine Bestandsaufnahme an den deutschen onkologischen Spitzenzentren. [Cooperation between intensive care and palliative care: The status quo in German Comprehensive Cancer Centers]. Med Klin Intensivmed Notfmed. 2020. https://doi.org/10.1007/s00063-020-00712-0 .
Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–94. https://doi.org/10.1097/CCM.0b013e3181ab86ed . ( quiz 2904 ).
Murali KP, Fonseca LD, Blinderman CD, White DB, Hua M. Clinicians’ views on the use of triggers for specialist palliative care in the ICU: a qualitative secondary analysis. J Crit Care. 2022;71: 154054. https://doi.org/10.1016/j.jcrc.2022.154054 .
Bell JAH, Salis M, Tong E, Nekolaichuk E, Barned C, Bianchi A, et al. Clinical ethics consultations: a scoping review of reported outcomes. BMC Med Ethics. 2022;23:99. https://doi.org/10.1186/s12910-022-00832-6 .
Download references
Acknowledgements
We would like to thank all the participants who openly reported on their daily work and without whom the study would not have been possible.
Open Access funding enabled and organized by Projekt DEAL. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Interdisciplinary Centre for Palliative Medicine, Medical Faculty, University Hospital Düsseldorf, Heinrich-Heine-University Düsseldorf, Düsseldorf, Germany
Manuela Schallenburger, Jacqueline Schwartz, Yann-Nicolas Batzler & Martin Neukirchen
Institute of Health Services Research and Health Economics, Centre for Health and Society, Medical Faculty, Heinrich Heine University Düsseldorf, Düsseldorf, Germany
Andrea Icks
Institute of Family Medicine/General Practice, Medical Faculty, University of Duisburg-Essen, Essen, Germany
Jürgen in der Schmitten
Department of Anaesthesiology, Medical Faculty, Heinrich Heine University Düsseldorf, Düsseldorf, Germany
Stefan Meier, Miguel Mendez-Delgado, Theresa Tenge & Martin Neukirchen
Center of Integrated Oncology Aachen, Bonn, Cologne (CIO ABCD), Heinrich-Heine-University, Düsseldorf, Germany
Jacqueline Schwartz, Andrea Icks & Martin Neukirchen
You can also search for this author in PubMed Google Scholar
Contributions
MS, MN, JS, AI, JidS developed the study. MS, MN, JidS, AI conducted and primarily evaluated the study. AI, JS, YNB, MMD, TT, SM provided support and advice. All authors contributed to the manuscript and agreed with the submission.
Corresponding author
Correspondence to Jacqueline Schwartz .
Ethics declarations
Ethics approval and consent to participate.
This study was conducted in accordance with the Declaration of Helsinki and received a positive ethics approval from the Ethics Committee of the Medical Faculty of the Heinrich Heine University Düsseldorf, Germany (Study-ID: 6114R). Written informed consent was obtained from all participants, which were all older than 18 years old.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Schallenburger, M., Schwartz, J., Icks, A. et al. Triggers of intensive care patients with palliative care needs from nurses’ perspective: a mixed methods study. Crit Care 28 , 181 (2024). https://doi.org/10.1186/s13054-024-04969-1
Download citation
Received : 10 April 2024
Accepted : 24 May 2024
Published : 28 May 2024
DOI : https://doi.org/10.1186/s13054-024-04969-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Trigger factors
- Palliative care
- Intensive care
- Intensive care nurses
- Interprofessional care
- Interdisciplinary care
Critical Care
ISSN: 1364-8535
- Submission enquiries: [email protected]
- Open access
- Published: 29 May 2024
Neoadjuvant chemotherapy followed by surgery versus concurrent chemoradiotherapy in patients with stage IIB cervical squamous cell carcinoma: a retrospective cohort study
- Xin-Bin Pan 1 ,
- You-Sheng Wei 2 &
- De-Sheng Yao 2
BMC Cancer volume 24 , Article number: 655 ( 2024 ) Cite this article
69 Accesses
Metrics details
This study aims to compare treatment outcomes between neoadjuvant chemotherapy (NACT) followed by surgery and concurrent chemoradiotherapy (CCRT) in patients with stage IIB cervical squamous cell carcinoma (CSCC).
Materials and methods
We conducted a retrospective cohort study involving patients with stage IIB CSCC treated at Guangxi Medical University Cancer Hospital between June 2012 and June 2019. We compared overall survival (OS), locoregional-free survival (LRFS), and distant metastasis-free survival (DMFS) between the NACT + surgery and CCRT groups.
A total of 257 patients were enrolled: 165 underwent NACT + surgery and 92 received CCRT. Before propensity score matching, the NACT + surgery group exhibited lower 5-year OS (68.2% vs. 85.6%; hazard ratio [HR] = 2.50, 95% confidence interval [CI]: 1.26–4.96; P = 0.009), LRFS (85.2% vs. 96.9%; HR = 5.88, 95% CI: 1.33–25.94; P = 0.019), and DMFS (81.9% vs. 97.4%; HR = 6.65, 95% CI: 1.51–29.23; P = 0.012) compared to the CCRT group. After propensity score matching, OS, LRFS, and DMFS remained worse in the NACT + surgery group compared to the CCRT group.
NACT followed by surgery is associated with decreased OS, LRFS, and DMFS compared to CCRT among patients with stage IIB CSCC.
Peer Review reports
Introduction
Cervical squamous cell carcinoma (CSCC) presents a significant health challenge globally, especially affecting women in developing countries [ 1 ]. In these regions, patients frequently present with advanced stages of the disease [ 2 ]. While concurrent chemoradiotherapy (CCRT) has been established as the standard treatment modality for these locally advanced CSCC [ 3 , 4 ], surgical intervention is also proposed as a viable alternative [ 5 , 6 ]. However, the efficacy of surgery in comparison to CCRT is currently a subject of debate. Divergent studies have reported variable outcomes. Some studies indicate that surgery may yield overall survival (OS) rates comparable to those achieved with CCRT [ 7 , 8 , 9 , 10 ]. In contrast, others indicate worse survival outcomes with surgical approaches [ 11 , 12 ]. Our study is designed to compare the survival outcomes between neoadjuvant chemotherapy (NACT) followed by surgery and CCRT in patients with stage IIB CSCC.
This retrospective cohort study analyzed CSCC patients treated at Guangxi Medical University Cancer Hospital from June 2012 to June 2019. Inclusion criteria were as follows: [ 1 ] pathologically confirmed cervical cancer, [ 2 ] squamous cell carcinoma, [ 3 ] stage IIB according to the International Federation of Gynaecology and Obstetrics (FIGO) staging system [ 13 ], [ 4 ] patients received CCRT or NACT + surgery. Exclusion criteria were as follows: [ 1 ] patients did not receive any treatments, [ 2 ] patients had incomplete data, [ 3 ] patients did not complete treatments, [ 4 ] patients underwent surgery alone, [ 5 ] patients received CCRT combined with neoadjuvant or adjuvant therapies.
Clinical variables collected included Eastern Cooperative Oncology Group (ECOG) status, age, tumor grade, human papillomavirus (HPV) infection status, hemoglobin levels, and tumor diameter. Tumor status, lymph node status, and systemic status were recorded according to clinical, imaging, pathological findings [ 13 ].
Surgical procedures comprised laparoscopic or open hysterectomy, as detailed in our previous studies [ 14 , 15 , 16 ]. Procedures included Piver-Rutledge class III abdominal hysterectomy, bilateral pelvic lymphadenectomy, and lower para-aortic lymph node sampling, all performed by expert gynecologic oncologists. Before surgery, 1 mL of carbon nanoparticles was injected into the cervix surrounding the tumor. The injection process lasted at least 3 min. The first lymph nodes to exhibit black staining after the injection initiation were identified as the sentinel lymph nodes. The number and location of these sentinel lymph nodes were recorded. Subsequently, the sentinel lymph nodes were excised and sent for pathological examination.
Prior to surgery, patients underwent 1 to 3 cycles of platinum-based NACT every three weeks. The surgery was scheduled 3–4 weeks after the final NACT cycle, based on the clinical response. Post-surgery, patients identified with risk prognostic factors were administered tailored adjuvant therapies. These therapies included options like chemotherapy, radiotherapy, or concurrent chemoradiotherapy [ 17 , 18 ]. The prognostic risk factors guiding these decisions included more than one third stromal invasion, capillary lymphatic space involvement, a tumor diameter exceeding 4 cm, positive pelvic lymph nodes, positive surgical margins, and microscopic involvement of the parametrium.
- Concurrent chemoradiotherapy
Radiotherapy combined pelvic external beam radiotherapy (48–50 Gy over 24–25 fractions using intensity-modulated radiotherapy) with high-dose-rate intracavitary brachytherapy (28–35 Gy over 4–5 fractions targeting the high-risk clinical target volume). Cone beam computed tomography was used for daily verification during the first week of treatment, followed by weekly verification thereafter.
The radiation doses were carefully adjusted to minimize impact on surrounding structures like the tumor, rectum, and bladder. To standardize bladder filling and reduce interaction motion, we employed a systematic drinking protocol. Patients were instructed to drink 500 mL of water 45 min before each radiotherapy session. This protocol was consistently followed to ensure reproducible bladder volumes, which is critical for maintaining the precision of radiation delivery and minimizing dose variations to surrounding organs at risk.
Concurrent chemotherapy involved weekly intravenous cisplatin (30–40 mg/m2/d1) or nedaplatin (50 mg/m2/d1) administered during the external beam radiotherapy period.
The primary endpoint of our study was OS, defined as the duration from diagnosis to death from any cause. Secondary endpoints were locoregional-free survival (LRFS) and distant metastasis-free survival (DMFS), which measured the time from diagnosis to either locoregional recurrence or distant metastasis, respectively.
Statistical analysis
Patients were divided into two groups: those receiving NACT + surgery, and those undergoing CCRT. We categorized continuous variables like age and hemoglobin levels at their median values. Tumor diameter, a continuous variable, was grouped at 4 cm [ 19 ]. Categorical variables, including ECOG status, age, tumor grade, HPV infection status, hemoglobin levels, and tumor diameter, were analyzed using the χ 2 test or Fisher’s exact test.
For survival analysis, we employed the Kaplan-Meier method, using log-rank tests to compare OS, LRFS, and DMFS between NACT + surgery and CCRT groups. Multivariable proportional hazards models, adjusted for ECOG status, age, tumor grade, HPV infection status, hemoglobin levels, tumor diameter, and treatment modalities, were used to identify independent prognostic factors. The results were presented as hazard ratios (HRs) with 95% confidence intervals (CIs).
To minimize selection bias between the NACT + surgery and CCRT groups, we used a matched case-control approach through propensity score matching (PSM). The scores were calculated using a logistic regression model with CCRT as the dependent variable. We matched cases one-to-one without replacement, based on nearest-neighbor matching on the logit of the propensity score, considering confounding factors and a caliper of 0.01.
All statistical analyses were performed using SPSS Statistics Version 26.0 (IBM Co., Armonk, NY, USA) and R software (version 4.2.2). A two-tailed P value below 0.05 was considered statistically significant.
Ethical approval for this study was obtained from the Guangxi Medical University Cancer Hospital Ethics Committee. The study was conducted in compliance with the principles outlined in the Declaration of Helsinki. However, informed consent was not obtained due to the retrospective nature of the study.
Patient characteristics
The selection process is illustrated in Fig. 1 . Our study included 257 patients: 165 (64.2%) underwent NACT + surgery and 92 (35.8%) received CCRT. Patient characteristics, both before and after PSM, are detailed in Table 1 . Prior to PSM, baseline characteristics like age, ECOG status, and HPV infection status showed imbalances between the NACT + surgery and CCRT groups. After PSM, 69 patients who received NACT + surgery and 69 patients who received CCRT were matched. Patient characteristics showing no significant differences across all covariates ( P > 0.05).
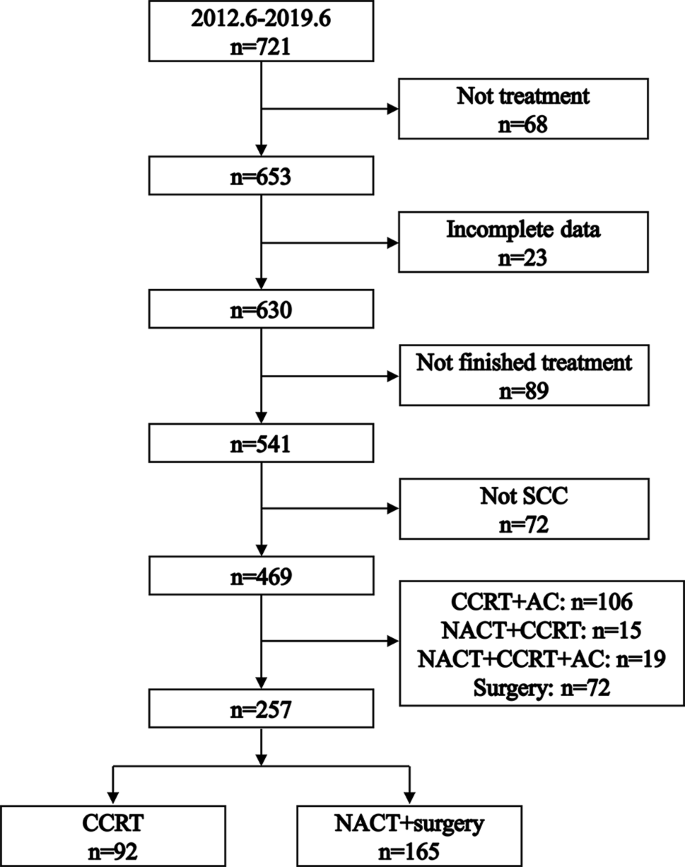
Flowchart illustrating the process of patient selection. SCC: squamous cell carcinoma. NACT: neoadjuvant chemotherapy. CCRT: concurrent chemoradiotherapy. AC: adjuvant chemotherapy
Within the CCRT group, the median number of concurrent chemotherapy cycles was 4 (interquartile range: 3–5 cycles). In the NACT + surgery group, 76 (46.1%) patients receive NACT + surgery alone, 51 (30.9%) patents receive radiotherapy after NACT + surgery, 5 (3.0%) patients received chemotherapy after NACT + surgery, and 33 (20.0%) patients received CCRT after NACT + surgery. Post-surgery, 68 (41.2%) patients in the NACT + surgery group were diagnosed with lymph node metastases.
Logistic regression for factors associated with NACT + surgery
Figure 2 presents the logistic regression analysis results, exploring factors influencing the choice of NACT + surgery. The analysis revealed a significant association between the selection of NACT + surgery and both age and ECOG status. Specifically, patients older than 54 years were less likely to undergo NACT + surgery (odds ratio = 0.37, 95% CI: 0.20–0.66; P < 0.001). Similarly, a lower likelihood of opting for NACT + surgery was observed in patients with an ECOG score of 1 (odds ratio = 0.51, 95% CI: 0.26–0.99; P = 0.048).
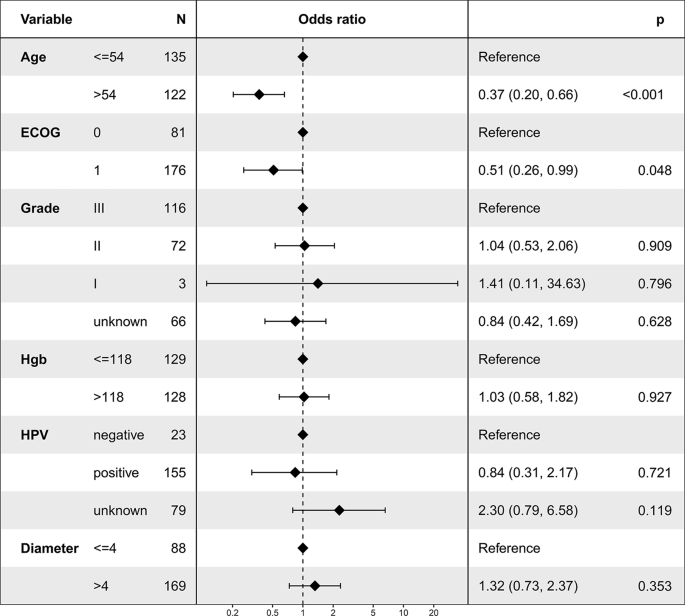
Logistic regression analysis depicting factors associated with the utilization of neoadjuvant chemotherapy followed by surgery
Overall survival
Before PSM, the 5-year OS rates were 68.2% in the NACT + surgery group and 85.6% in the CCRT group ( P = 0.004, Fig. 3 A). Multivariable proportional hazards models revealed that NACT + surgery was an independent risk prognostic factor for OS (HR = 2.50, 95% CI: 1.26–4.96; P = 0.009, Table 2 ).
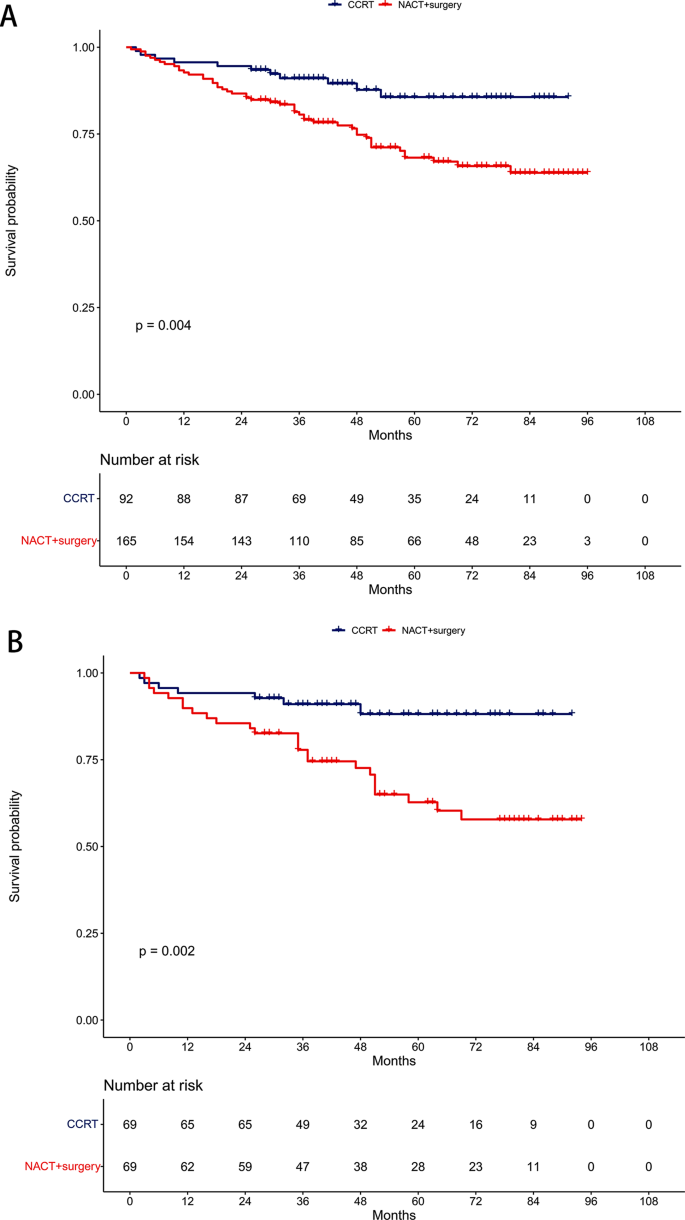
Comparison of overall survival between the neoadjuvant chemotherapy followed by surgery and concurrent chemoradiotherapy groups. ( A ) Unmatched cohort. ( B ) Propensity-matched cohort
After PSM, the 5-year OS rates were 62.7% in the NACT + surgery group and 88.2% in the CCRT group ( P = 0.002, Fig. 3 B). Similarly, NACT + surgery remained an independent risk prognostic factor for OS in multivariable proportional hazards models (HR = 3.67, 95% CI: 1.58–8.52; P = 0.003, Table 3 ).
Locoregional-free survival
Pre-PSM, the 5-year LRFS rates were 85.2% in the NACT + surgery group and 96.9% in the CCRT group ( P = 0.009, Fig. 4 A). Multivariable proportional hazards models demonstrated that NACT + surgery was an independent risk prognostic factor for LRFS (HR = 5.88, 95% CI: 1.33–25.94; P = 0.019, Table 2 ).
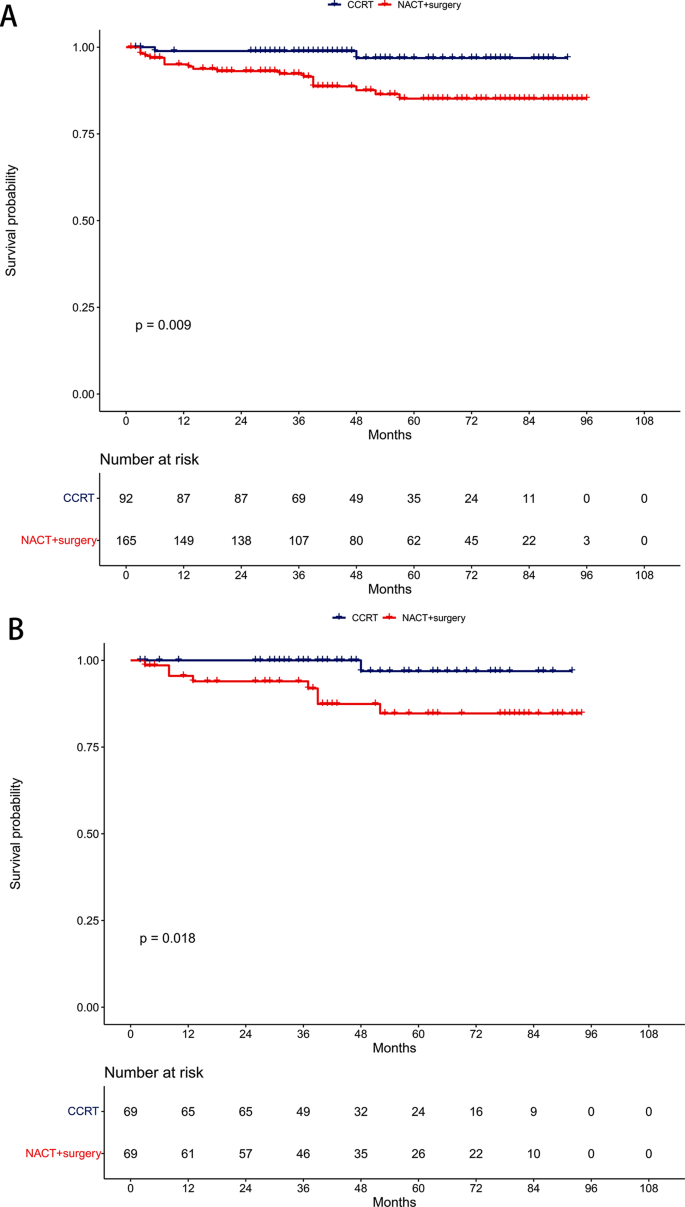
Comparison of locoregional-free survival between the neoadjuvant chemotherapy followed by surgery and concurrent chemoradiotherapy groups. ( A ) Unmatched cohort. ( B ) Propensity-matched cohort
Post-PSM, the 5-year LRFS rates were 84.7% in the NACT + surgery group and 96.9% in the CCRT group ( P = 0.018, Fig. 4 B). NACT + surgery retained its significance as an independent risk prognostic factor for LRFS in multivariable proportional hazards models (HR = 8.31, 95% CI: 1.03–67.32; P = 0.047, Table 3 ).
Distant metastasis-free survival
Before PSM, the 5-year DMFS rates were 81.9% in the NACT + surgery group and 97.4% in the CCRT group ( P = 0.002, Fig. 5 A). Multivariable proportional hazards models revealed NACT + surgery as an independent risk prognostic factor for DMFS (HR = 6.65, 95% CI: 1.51–29.23; P = 0.012, Table 2 ).
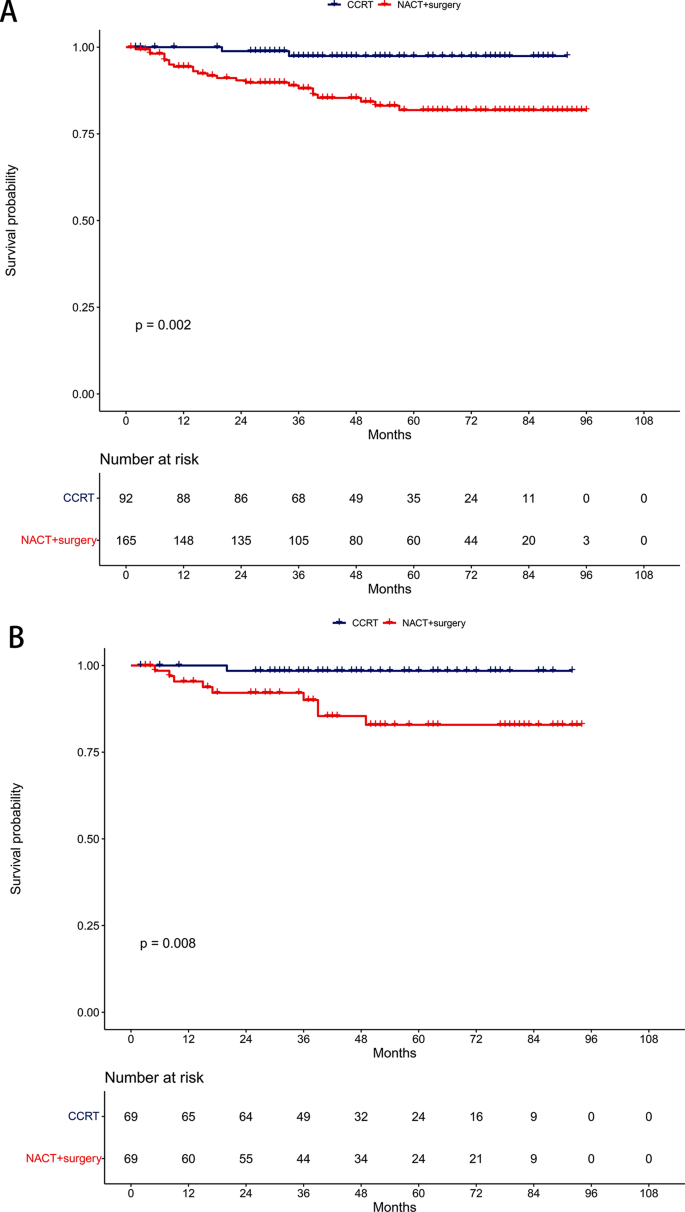
Comparison of distant metastasis-free survival between the neoadjuvant chemotherapy followed by surgery and concurrent chemoradiotherapy groups. ( A ) Unmatched cohort. ( B ) Propensity-matched cohort
After PSM, the 5-year DMFS rates were 82.9% in the NACT + surgery group and 98.5% in the CCRT group ( P = 0.008, Fig. 5 B). NACT + surgery continued to be an independent risk prognostic factor for DMFS in multivariable proportional hazards models (HR = 10.94, 95% CI: 1.34–89.21; P = 0.026, Table 3 ).
Our study offered a pivotal understanding that NACT before surgery did not improve survival outcomes in stage IIB CSCC patients. This aligns with the existing perspective that stage IIB CSCC is an unresectable disease [ 20 ]. Consequently, CCRT remains the fundamental treatment strategy. These results strongly suggested that surgery as an initial radical approach should not be considered for this patient subgroup [ 21 ].
Our results may suggest that the delay in surgery due to NACT might compromise survival rates. The initial decrease in 5-year LRFS and DMFS associated with NACT + surgery could adversely affect OS, indicating that NACT-induced tumor size reduction may not be adequate for effective radical surgery in this specific patient group [ 22 ].
Despite being the preferred treatment, CCRT for stage IIB CSCC may lead to significant long-term radiation-induced complications, including ovarian failure, vaginal fibrosis, enteritis, fistulas, bowel obstruction, and lymphedema [ 23 ]. These adverse effects significantly impact the quality of life for patients during long-term survival [ 24 ]. This reality might incline clinicians toward considering surgical interventions for these patients. However, recent studies indicate that achieving an optimal dose distribution, compliant with the treatment planning objectives of the EMBRACE II protocol, is more feasible when the external beam radiotherapy dose is limited to 45 Gy [ 25 ]. Moreover, the systematic use of an interstitial brachytherapy component can increase the dose delivered to 98% of the volume from 83 ± 14 Gy to 92 ± 13 Gy without increasing the dose to organs at risk. Adhering to these updated international guidelines could substantially reduce the complications associated with CCRT and increase the locoregional control rates [ 13 ].
However, the approach to treating stage IIB CSCC is not always consistent in clinical practice, primarily due to the subjective nature of staging, which relies on physical examination. This variability often leads to different surgical decisions among clinicians [ 26 , 27 ]. In certain cases, experts might recommend surgery, basing their decision on specific factors such as tumor size, histopathological grade, and lymph node status [ 28 ].
Moreover, recent advancements in chemotherapy regimens, particularly those involving platinum and cisplatin, have shown notable effectiveness in CSCC [ 29 ]. Platinum-based NACT has been found to reduce the primary tumor burden, which could lead to a higher rate of complete resection. Additionally, Platinum-based NACT is believed to have the capability to prevent cancer cell implantation and to eradicate circulating cancer cells, thereby potentially diminishing subclinical metastasis. This could lead to improved DMFS, a hypothesis that is gaining support from various studies [ 30 , 31 , 32 ].
The primary aim of using NACT is to enhance treatment outcomes compared to CCRT. However, findings from a single-center, phase III, randomized controlled trial presented a different picture [ 12 ]. This study reported a 5-year disease-free survival of 69.3% in the NACT + surgery group, compared to 76.7% in the CCRT group (HR = 1.38, 95% CI: 1.02–1.87; P = 0.038). Interestingly, the corresponding 5-year OS rates were quite similar: 75.4% for NACT + surgery and 74.7% for CCRT (HR = 1.025, 95% CI: 0.752–1.398; P = 0.87). This suggested that NACT + surgery did not significantly improve survival rates over CCRT.
A notable observation from this trial was that the reduced disease-free survival in the NACT + surgery group did not lead to a worse OS. This could be attributed to the effectiveness of salvage treatments following recurrence. It is important to note that a majority of first recurrences (102 out of 162 recurrences, constituting 62.96%) were localized, emphasizing the critical role of local control. After recurrence, 30.0% of patients in the NACT + surgery group received local radiotherapy, compared to just 11.0% in the CCRT group. This finding underscored the importance of local control in managing recurrent CSCC and illustrated the complexity inherent in treatment decisions and their long-term implications.
A major strength of our study was the consistent quality of treatment delivery by a multidisciplinary team of experts. However, its retrospective nature introduced potential limitations, including possible confounders between the NACT + surgery and CCRT groups. Although we employed PSM and multivariable proportional hazards models to address these biases, our findings need to be validated by larger-scale studies conducted at diverse centers.
In conclusion, our research highlights that NACT + surgery decreased OS, LRFS, and DMFS compared to CCRT in treating stage IIB CSCC, emphasizing the need for cautious consideration in treatment planning.
Data availability
The data are available from the corresponding author upon request.
Abbreviations
- Cervical squamous cell carcinoma
- Neoadjuvant chemotherapy
The International Federation of Gynaecology and Obstetrics
Eastern Cooperative Oncology Group
Human papilloma virus
Propensity score matching
Hazard ratio
Confidence interval
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Article PubMed Google Scholar
Zhang M, Zhong Y, Zhao Z, Huang Z, Zhang X, Li C, et al. Cervical Cancer Screening Rates among Chinese Women - China, 2015. China CDC Wkly. 2020;2(26):481–6.
Article CAS PubMed PubMed Central Google Scholar
Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340(15):1144–53.
Article CAS PubMed Google Scholar
National Health Commission Of The People’s Republic Of C. Chinese guidelines for diagnosis and treatment of cervical cancer 2018 (English version). Chin J Cancer Res. 2019;31(2):295–305.
Article Google Scholar
Marth C, Landoni F, Mahner S, McCormack M, Gonzalez-Martin A, Colombo N, et al. Cervical cancer: ESMO Clinical Practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl4):iv72–83.
Ebina Y, Mikami M, Nagase S, Tabata T, Kaneuchi M, Tashiro H, et al. Japan Society of Gynecologic Oncology guidelines 2017 for the treatment of uterine cervical cancer. Int J Clin Oncol. 2019;24(1):1–19.
Kokka F, Bryant A, Olaitan A, Brockbank E, Powell M, Oram D. Hysterectomy with radiotherapy or chemotherapy or both for women with locally advanced cervical cancer. Cochrane Database Syst Rev. 2022;8(8):CD010260.
PubMed Google Scholar
Ye Q, Yang Y, Tang X, Li J, Li X, Zhang Y. Neoadjuvant Chemotherapy followed by radical surgery versus Radiotherapy (with or without chemotherapy) in patients with stage IB2, IIA, or IIB cervical Cancer: a systematic review and Meta-analysis. Dis Markers. 2020;2020:7415056.
Article PubMed PubMed Central Google Scholar
Hu Y, Han Y, Shen Y, Chen J, Chen Y, Chen Y, et al. Neoadjuvant chemotherapy for patients with international federation of gynecology and obstetrics stages IB3 and IIA2 cervical cancer: a multicenter prospective trial. BMC Cancer. 2022;22(1):1270.
Zou W, Han Y, Zhang Y, Hu C, Feng Y, Zhang H, et al. Neoadjuvant chemotherapy plus surgery versus concurrent chemoradiotherapy in stage IB2-IIB cervical cancer: a systematic review and meta-analysis. PLoS ONE. 2019;14(11):e0225264.
Miriyala R, Mahantshetty U, Maheshwari A, Gupta S. Neoadjuvant chemotherapy followed by surgery in cervical cancer: past, present and future. Int J Gynecol cancer: Official J Int Gynecol Cancer Soc. 2022;32(3):260–5.
Gupta S, Maheshwari A, Parab P, Mahantshetty U, Hawaldar R, Sastri Chopra S, et al. Neoadjuvant Chemotherapy followed by radical surgery Versus Concomitant Chemotherapy and Radiotherapy in patients with Stage IB2, IIA, or IIB squamous cervical Cancer: a Randomized Controlled Trial. J Clin Oncol. 2018;36(16):1548–55.
Cibula D, Raspollini MR, Planchamp F, Centeno C, Chargari C, Felix A, et al. ESGO/ESTRO/ESP guidelines for the management of patients with cervical cancer - update 2023. Int J Gynecol Cancer. 2023;33(5):649–66.
Lu Y, Wei JY, Yao DS, Pan ZM, Yao Y. Application of carbon nanoparticles in laparoscopic sentinel lymph node detection in patients with early-stage cervical cancer. PLoS ONE. 2017;12(9):e0183834.
Wei YS, Yao DS, Long Y. Evaluation of the association between perineural invasion and clinical and histopathological features of cervical cancer. Mol Clin Oncol. 2016;5(3):307–11.
Long Y, Yao DS, Wei YS, Wei CH, Chen XY. Prognostic significance of perineural invasion in vulvar squamous cell carcinoma. Cancer Manag Res. 2019;11:4461–9.
Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncology: Official J Am Soc Clin Oncol. 2000;18(8):1606–13.
Article CAS Google Scholar
Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006;65(1):169–76.
Carlson JA, Rusthoven C, DeWitt PE, Davidson SA, Schefter TE, Fisher CM. Are we appropriately selecting therapy for patients with cervical cancer? Longitudinal patterns-of-care analysis for stage IB-IIB cervical cancer. Int J Radiat Oncol Biol Phys. 2014;90(4):786–93.
Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri. Int J Gynaecol Obstet. 2018;143(Suppl 2):22–36.
Borghi C, Biagioli E, Mauro J, Roberto A, Borghese M, Buda A. Neoadjuvant chemotherapy prior to radical hysterectomy in locally advanced cervical cancer: a systematic review and meta-analysis. Int J Gynecol Cancer. 2023.
Chidambaram S, Owen R, Sgromo B, Chmura M, Kisiel A, Evans R et al. Delayed Surgical Intervention After Chemoradiotherapy in Esophageal Cancer: (DICE) Study. Annals of surgery. 2023.
Hoekman EJ, Knoester D, Peters AAW, Jansen FW, de Kroon CD, Hilders C. Ovarian survival after pelvic radiation: transposition until the age of 35 years. Arch Gynecol Obstet. 2018;298(5):1001–7.
Bergmark K, Avall-Lundqvist E, Dickman PW, Henningsohn L, Steineck G. Vaginal changes and sexuality in women with a history of cervical cancer. N Engl J Med. 1999;340(18):1383–9.
Chargari C, Tanderup K, Planchamp F, Chiva L, Humphrey P, Sturdza A, et al. ESGO/ESTRO quality indicators for radiation therapy of cervical cancer. Int J Gynecol Cancer. 2023;33(6):862–75.
Fujii S, Takakura K, Matsumura N, Higuchi T, Yura S, Mandai M, et al. Precise anatomy of the vesico-uterine ligament for radical hysterectomy. Gynecol Oncol. 2007;104(1):186–91.
Swailes AL, Gockley A, Phaeton R, Kesterson JP. The Wertheim hysterectomy: development, modifications, and impact in the present day. Gynecol Oncol. 2017;145(1):3–8.
Mallmann P, Mallmann C. Neoadjuvant and Adjuvant Chemotherapy of Cervical Cancer. Oncol Res Treat. 2016;39(9):522–4.
Moore DH, Blessing JA, McQuellon RP, Thaler HT, Cella D, Benda J, et al. Phase III study of cisplatin with or without paclitaxel in stage IVB, recurrent, or persistent squamous cell carcinoma of the cervix: a gynecologic oncology group study. J Clin Oncology: Official J Am Soc Clin Oncol. 2004;22(15):3113–9.
Rydzewska L, Tierney J, Vale CL, Symonds PR. Neoadjuvant chemotherapy plus surgery versus surgery for cervical cancer. Cochrane Database Syst Rev. 2012;12(12):CD007406.
Chen H, Liang C, Zhang L, Huang S, Wu X. Clinical efficacy of modified preoperative neoadjuvant chemotherapy in the treatment of locally advanced (stage IB2 to IIB) cervical cancer: randomized study. Gynecol Oncol. 2008;110(3):308–15.
Huang X, Lan C, Huang H, Zhang Y, Huang H, Cao X, et al. Neoadjuvant docetaxel combined with cisplatin and followed by radical surgery for the treatment of locally advanced (stage IB2 - IIB) cervical cancer: preliminary results of a single-institution experience. Expert Opin Pharmacother. 2011;12(2):165–73.
Download references
Acknowledgements
Not Applicable.
Author information
Authors and affiliations.
Department of Radiation Oncology, Guangxi Medical University Cancer Hospital, Nanning, Guangxi, 530021, P.R. China
Xin-Bin Pan
Department of Gynecologic Oncology, Guangxi Medical University Cancer Hospital, No. 71 Hedi Road, Qingxiu District, Nanning, Guangxi, 530021, P.R. China
Yan Lu, You-Sheng Wei & De-Sheng Yao
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: X-B.P., Methodology: Y.L., Formal Analysis: Y-S.W., Investigation: X-B.P., Resources: Y.L., Validation: Y.L. and Y-S.W., Writing-Original Draft Preparation: X-B.P., Writing-Review & Editing: D-S.Y.
Corresponding author
Correspondence to De-Sheng Yao .
Ethics declarations
Ethics approval and consent to participate.
The requirement for ethics approval was approved by the ethics committee/Institutional Review Board of Guangxi Medical University Cancer Hospital. The requirement for informed consent was waived by the ethics committee/Institutional Review Board of Guangxi Medical University Cancer Hospital. All methods were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pan, XB., Lu, Y., Wei, YS. et al. Neoadjuvant chemotherapy followed by surgery versus concurrent chemoradiotherapy in patients with stage IIB cervical squamous cell carcinoma: a retrospective cohort study. BMC Cancer 24 , 655 (2024). https://doi.org/10.1186/s12885-024-12411-6
Download citation
Received : 18 January 2024
Accepted : 22 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s12885-024-12411-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The patient subsequently underwent evaluation at her primary care clinic. Her score on the Epworth Sleepiness Scale was 20, with scores ranging from 0 (low-normal daytime sleepiness) to 24 ...
23.9: 16.2 Monocytes: 4-11 ... Several published case reports suggest that her ... on the basis of historical and contemporary data from nonrandomized studies of its use in patients with proven ...
Imaging studies show bilateral peripheral opacities. ... as was the case in this patient. ... than dose-adjusted intravenous unfractionated heparin. 23 The use of up-front direct oral ...
A 57 year-old male lorry driver, presented to his local emergency department with a 20-minute episode of diaphoresis and chest pain. The chest pain was central, radiating to the left arm and crushing in nature. The pain settled promptly following 300 mg aspirin orally and 800 mcg glyceryl trinitrate (GTN) spray sublingually administered by ...
Patient Case #2: 23-Year-Old Female With Plaque Psoriasis. Jennifer Conner, MPAS, PA-C, and Terry Faleye, MPAS, PA-C, review a case of a young adult female with plaque psoriasis on the elbows, thighs, and scalp, and discuss switching systemic treatments to accommodate her lifestyle.
Case presentation. We report a case of a 23-year-old Croatian man with a parapharyngeal abscess on the left side of the neck with spreading of infection in the mediastinum and left side of the thorax and consequent major atelectasis of the left lung. The patient was mechanically ventilated.
CHARACTERIZING HYPERGLYCEMIA. This patient's hyperglycemia reached a threshold that was diagnostic of diabetes 1 on two occasions: when she was 25 years of age, she had a randomly obtained blood glucose level of 217 mg per deciliter with polyuria (with diabetes defined as a level of ≥200 mg per deciliter [≥11.1 mmol per liter] with symptoms), and when she was 30 years of age, she had on ...
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. ... Blue Mountain Community College on 10/11/23 This is a book of compiled and very well organized patient case studies. The author has ...
the doctor's note for Patient 23 for week 3. When Patient 23 felt healthy during week 1, the C. jejuni bacteria was not present in his gut microbiome. In week 3, when he felt sick, C. jejuni was present. Therefore, C. jejuni is probably the cause of his sickness. Argument Two: Patient 23 felt sick during week 3 because he was infected with ...
Patient Case A 23-year-old biology PhD candidate presents for further evaluation of her gastrointestinal (GI) symptoms (Table 1). These symptoms have been present for the past 3 years and were not triggered by any specific precipitants. She reports recurrent achy abdominal pain radiating through-out her lower abdomen. This pain usually develops ...
CASE REPORT. In January 2020, a 53-year-old gentleman with a background of asthma on long-term low dose inhaled corticosteroid inhaler had an acute exacerbation of his asthma in February 2020 triggered by a viral upper respiratory tract infection and acute sinusitis and was managed with bronchodilator nebulization and a 7-day course of oral prednisone 30 mg daily.
Abdomen: Good bowel sounds, soft. No pain or masses or tenderness. No hepatosplenomegaly. Impression: Painful Urination. Plan: I am sending the patient to the hospital for a chest x-ray and a complete blood work-up. Study with Quizlet and memorize flashcards containing terms like R51.9, R06.02, R18.8 and more.
Zyah Burnett Case Study 23 - Community Acquired Pneumonia (CAP) Scenario: C.'s sister has brought her 71 yo brother to the primary care clinic; he came down with a fever 2 days ago. ... The patient is having issues getting enough oxygen within the normal breaths per minute which is a concern. d. Temp 103 F - We would want to monitor and ...
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence.1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Purpose According to the oncologist, a single medication is insufficient to completely cure the disease; as a result, most patients undergo treatment from two or more types of therapy, sometimes in succession, in order to control the progression of their cancer. Methods This comprehensive review explores the applications and challenges associated with multimodality treatment planning utilizing ...
Expert-Verified Answer. Analyzing Patient 23's case study data from weeks 7 to 9 would involve observing changes over the given period, determining the causes of these changes, and predicting the effects of continued trends. This process should be guided by scientific knowledge, critical reasoning, and additional data in the case study.
The patient had a history of diabetes, hypertension, hyperlipidemia, coronary artery disease, obesity, and obstructive sleep apnea. A drug-eluting stent had been placed in the left anterior ...
Initial Management of a Patient with Burns Patient Profile M. is a 23-year-old white woman transferred via ambulance to the hospital after a fire in her apartment. She was asleep when the fire started and managed to make her way out of the apartment through the smoke. ... Shock MODS case study w answers; Unit 6 renal study guide; Related ...
Case Study, Chapter 23, Management of Patients With Chest and Lower Respiratory Tract Disorders. Harry Smith, 70 years of age, is a male patient who is admitted to the medical-surgical unit with acute community-acquired pneumonia. He was diagnosed with paraseptal emphysema 3 years ago.
A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient ... Fig. 3A), and his platelet count decreased to 23 × 10 9 /L (normal range: 125-300 × 10 9 /L, Fig. ... In this case, the patient presented with both HIV and HBV infections ...
Background Patient satisfaction is an important indicator of the quality of healthcare. Pain is one of the most common symptoms among cancer patients that needs optimal treatment; rather, it compromises the quality of life of patients. Objective To assess the levels and associated factors of satisfaction with cancer pain treatment among adult patients at cancer centers found in Northern ...
Weekly / May 23, 2024 / 73(20);456-459 ... The family reunion concluded before onset of illness in the index patient. Laboratory Investigation and Case Definition. Public health authorities in Arizona, Minnesota, and South Dakota interviewed eight of the nine persons who had attended the implicated meal. The ninth attendee was a person aged ...
The use of povidone-iodine for ocular surface asepsis is widespread for intravitreal injections. They became frequent procedures, leading to serial exposure of patients' eyes to iodinated solutions. In this study, we investigate the changes in the ocular surface in patients submitted to repeated use of povidine for intravitreal injection of anti-VEGF asepsis, analyzing Ocular Surface Disease ...
The identification of patients who benefit most from sPC involvement is important both to address the patients individual needs and to use sPC as a limited resource efficiently [9, 23]. The triggers identified in the present study relate to the individual patient situation and the support needs of patients, relatives and the intensive care nurses.
e14700 Background: Checkpoint inhibitor pneumonitis (CIP) is the most common high-grade immune-related adverse event among patients with lung cancer. Risk factors for CIP include interstitial lung disease, fibrosis on pre-treatment CT imaging, and likely COPD. This study aims to compare COPD variables and CIP outcomes between cases of high and low-grade CIP, and controls without CIP. We ...
On examination, the patient appeared to be in respiratory distress. The temperature was 35.9°C, the pulse 98 beats per minute, the blood pressure 129/58 mm Hg, the respiratory rate 24 breaths per ...
This study aims to compare treatment outcomes between neoadjuvant chemotherapy (NACT) followed by surgery and concurrent chemoradiotherapy (CCRT) in patients with stage IIB cervical squamous cell carcinoma (CSCC). We conducted a retrospective cohort study involving patients with stage IIB CSCC treated at Guangxi Medical University Cancer Hospital between June 2012 and June 2019.
Case Study, Chapter 23, Management of Patients With Chest and Lower Respiratory Tract Disorders. Harry Smith, 70 years of age, is a male patient who is admitted to the medical-surgical unit with acute community-acquired pneumonia. He was diagnosed with paraseptal emphysema 3 years ago.
Evidence card E: From Patient 23's Case study data Week 7 The Patient in week seven doctor's notes- Patient reports stomach pains, diarrhea, and bloating. The patient is missing most of their gut biome.
Patients who underwent McKeown-type esophagectomy between January 2021 and March 2022 were included in this study. Postoperative outcomes of patients who underwent ultra-proximal jejunostomy are also presented. ... This retrospective case series was approved by the Ethics Committee of Quanzhou First Hospital (2020-202), and all participants ...