An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychol

Child and Adolescent Depression: A Review of Theories, Evaluation Instruments, Prevention Programs, and Treatments
Elena bernaras.
1 Developmental and Educational Department, University of the Basque Country, Donostia/San Sebastián, Spain
Joana Jaureguizar
2 Developmental and Educational Psychology Department, University of the Basque Country, Lejona, Spain
Maite Garaigordobil
3 Personality, Evaluation and Psychological Treatments Department, University of the Basque Country, Donostia/San Sebastián, Spain
Depression is the principal cause of illness and disability in the world. Studies charting the prevalence of depression among children and adolescents report high percentages of youngsters in both groups with depressive symptoms. This review analyzes the construct and explanatory theories of depression and offers a succinct overview of the main evaluation instruments used to measure this disorder in children and adolescents, as well as the prevention programs developed for the school environment and the different types of clinical treatment provided. The analysis reveals that in mental classifications, the child depression construct is no different from the adult one, and that multiple explanatory theories must be taken into account in order to arrive at a full understanding of depression. Consequently, both treatment and prevention should also be multifactorial in nature. Although universal programs may be more appropriate due to their broad scope of application, the results are inconclusive and fail to demonstrate any solid long-term efficacy. In conclusion, we can state that: (1) There are biological factors (such as tryptophan—a building block for serotonin-depletion, for example) which strongly influence the appearance of depressive disorders; (2) Currently, negative interpersonal relations and relations with one's environment, coupled with social-cultural changes, may explain the increase observed in the prevalence of depression; (3) Many instruments can be used to evaluate depression, but it is necessary to continue to adapt tests for diagnosing the condition at an early age; (4) Prevention programs should be developed for and implemented at an early age; and (5) The majority of treatments are becoming increasingly rigorous and effective. Given that initial manifestations of depression may occur from a very early age, further and more in-depth research is required into the biological, psychological and social factors that, in an interrelated manner, may explain the appearance, development, and treatment of depression.
Introduction
Depression is the principal cause of illness and disability in the world. The World Health Organization (WHO) has been issuing warnings about this pathology for years, given that it affects over 300 million people all over the world and is characterized by a high risk of suicide (the second most common cause of death in those aged between 15 and 29) [World Health Organization (WHO), 2017 ]. Studies on the child population which use self-reports to evaluate severe symptoms of depression, specifically the Children's Depression Inventory (CDI, Kovacs, 1992 ) and the Children's Depression Scale (CDS, Lang and Tisher, 1978 ), have observed prevalence rates of, for example, 4% in Spain (Demir et al., 2011 ; Bernaras et al., 2013 ), 6% in Finland (Puura et al., 1997 ), 8% in Greece (Kleftaras and Didaskalou, 2006 ), 10% in Australia (McCabe et al., 2011 ), and 25% in Colombia (Vinaccia et al., 2006 ). The main classifications of mental disorders are the Diagnostic and Statistical Manual of Mental Disorders, DSM-5 (American Psychiatric Association, 2014 ), published by the American Psychiatric Association, which has become a key reference in clinical practice, and version 10 of the International Classification of Diseases (ICD-10, 1992), published by the WHO, which classifies and codifies all diseases, although initially its aim was to chart mortality rates. The new ICD-11 classification will be presented for approval to Member States at the World Health Assembly in May 2019, and is expected to come into effect on January 1, 2022 [World Health Organization (WHO), 2018 ]. The two classifications offer different categorizations of depressive disorders, although certain similarities do exist, and it should be borne in mind also that both have been criticized for hardly distinguishing at all between child and adult depression.
Throughout history, there have been many different explanatory theories of depression. Biological and psychological theories are the ones which have mainly tried to explain the origin of this mental disorder. Biological theories have, from a variety of different perspectives, postulated that depression may occur due to noradrenalin deficits (e.g., Schildkraut, 1965 ; Narbona, 2014 ), endocrine disorders (e.g. Birmaher et al., 1996 ), sleep-related disorders (e.g., Sivertsen et al., 2014 ; Pariante, 2017 ), alterations in brain structure (Whittle et al., 2014 ), or the influence of genetics (Scourfield et al., 2003 ). Psychological theories have attempted to explain depression on the basis of psychoanalysis and, more specifically, in terms of attachment theories (e.g., Bowlby, 1976 ; Ainsworth et al., 1978 ; Blatt, 2004 ; Bigelow et al., 2018 ), behavioral models (e.g., Skinner, 1953 ; Ferster, 1966 ; Lewinsohn, 1975 ), cognitive models (e.g., Seligman, 1975 ; Abramson et al., 1978 ; Beck, 1987 ), the self-control model (e.g., Rehm, 1977 ; Rehm et al., 1979 ), interpersonal theory (e.g., Markowitz and Weissman, 1995 ; Milrod et al., 2014 ), stressful life events (e.g., Reinherz et al., 1993 ; Frank et al., 1994 ), and sociocultural models (e.g., Lorenzo-Blanco et al., 2012 ; Chang et al., 2013 ; Reeves et al., 2014 ).
Evaluating depression accurately has been another concern upon which psychology has focused, with attention being centered specifically around diagnosing this pathology in childhood and adolescence. Although many diagnostic instruments have been developed and validated, mainly for the adolescent and adult stages of life, it is still difficult to find diagnostic tests for evaluating depression in children. Preventing depression is another aspect to which much importance is attached by the World Health Organization (WHO) ( 2017 ), which argues that school programs, interventions aimed at parents and specific exercises for the elderly population help reduce the prevalence of this pathology. Depression prevention programs do exist, but they are mainly targeted at adolescents and very few focus on children under the age of 10.
The treatment of depression is another aspect that should not be overlooked. In 2016, the WHO and the World Bank announced that investing in the treatment of depression and anxiety leads to four-fold returns, since these pathologies cost the global economy one trillion US dollars each year. Furthermore, they claimed that humanitarian emergencies and conflicts highlight a pressing need to broaden current therapeutic options. In this sense, the multiple different explanatory theories of depression have given rise to a plethora of different treatments (psychotherapeutic, behavioral, cognitive-behavioral, interpersonal, etc.) which are currently being analyzed with a high degree of precision and scientific rigor.
In light of the different aspects related to depression outlined above, the present study has the following aims: (1) To analyze the construct of depression offered by the two main mental disorder classifications (DSM-5 and ICD-10); (2) To provide an overview of the main explanatory theories of depression; (3) To outline the child and adolescent depression evaluation instruments most commonly used in scientific literature; (4) To provide a brief overview of child and adolescent depression prevention programs in the school environment; and (5) To describe the most scientifically rigorous and effective clinical treatments for this mental disorder.
The databases used for carrying out the searches were PubMed, PsycINFO, Web of Science, Scopus, Science Direct and Google Scholar, along with a range of different manuscripts. With the constant key word being depression, the search for information cross-referenced a series of other key words also, namely: childhood, adolescence, explanatory theories, etiology, evaluation instruments, prevention programs, and treatment. Searches were conducted for information published between 1970 and 2017.
Thus, first we describe the construct of depression and summarize the main explanatory theories. Next, we present the main evaluation instruments used to measure child and adolescent depression and report the results of a bibliographical review of prevention programs in school settings. Finally, we outline the main clinical treatments used nowadays to treat child and adolescent depression.
The Construct of Depression: DSM-5 and ICD-10
Depression features in both of the two most important global classifications: the DSM-5 and the ICD-10. As stated earlier in the introduction, the new ICD-11 classification will be presented for approval to Member States at the World Health Assembly in May 2019, and is expected to come into effect on January 1, 2022. The presentation of the new classification in 2019 will enable countries to plan for its implementation, prepare the necessary translations and train professionals accordingly [World Health Organization (WHO), 2018 ]. In texts published by WHO collaborators (Luciano, 2017 ), it has been suggested that the ICD-11 will include mood disorders within the mental and behavioral disorder category. However, until the final version is published, this information cannot be fully verified.
The two classifications (DSM-5 e IDC-10) offer different categorizations of depressive disorders, as shown in Table 1 . The WHO includes depressive disorders in the mood disorders category, although this review only focuses on Sections F32, F33, F34, and F38, which include the most frequent depressive disorders and which, in turn, contain subsections that will be further specified later on.
Depressive disorders according to the DSM-5 and the ICD-10.
| Depressive disorders | Mood (affective) disorders F32, F33, F34, and F38 |
| - Disruptive mood dysregulation disorder - Major depressive disorder - Persistent depressive disorder (dysthymia) - Premenstrual dysphoric disorder - Substance/medication-induced depressive disorder - Depressive disorder due to another medical condition - Other specified depressive disorder - Other unspecified depressive disorder | - Single episode (F32) - Recurrent depressive disorder (F33) - Persistent mood (affective) disorders (F34) - Other mood (affective) disorders (F38) |
According to the DSM-5, depressive disorders all have one common feature, namely the presence of sad, empty or irritable mood, accompanied by somatic and cognitive changes that significantly affect the individual's capacity to function (DSM-5). They may become a serious health problem if allowed to persist for long periods of time and occur with a moderate-to-severe degree of intensity. One important consequence of depression is the risk of suicide, which is, according the World Health Organization (WHO) ( 2017 ), the second most common cause of death among young people aged between 15 and 29.
The main novelty offered by the DSM-5 in its section on depressive disorders is the introduction to Disruptive mood dysregulation disorder (which should not be diagnosed before the age of 6 or after the age of 18). This disorder is characterized by severe recurrent temper outbursts manifested verbally (e.g., verbal rages) and/or behaviorally (e.g., physical aggression toward people or property). These outbursts often occur as the result of frustration and in order to be considered a diagnostic criterion must be inconsistent with the individual's developmental level, occur three or more times per week for at least a year in a number of different settings (at home, at school, etc.) and be severe in at least one of these. This disorder was added to the DSM-5 due to doubts arising in relation to how to classify and treat children presenting with chronic persistent irritability as opposed to other related disorders, specifically pediatric bipolar disorder. The prevalence of this disorder has been estimated at between 2 and 5%, with male children and teenage boys being more likely to suffer from it than their female counterparts.
Major Depressive Disorder
Major depressive disorder is characterized by a depressed mood most of the day, nearly every day, although in children and adolescents this mood may be irritable rather than depressed. The disorder causes a markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day, significant weight loss or gain, insomnia or hypersomnia, psychomotor agitation or retardation, fatigue or loss of energy, feelings of worthlessness, or excessive or inappropriate guilt, diminished ability to think or concentrate, recurrent thoughts of death, recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide. These symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. In the United States, the 12-month prevalence is ~7%, although it is three times higher among those aged between 18 and 29 than among those aged 60 or over. Moreover, the prevalence rates for women are ~1.5–3 times higher than for men.
Persistent Depressive Disorder (Dysthymia)
Persistent depressive disorder (dysthymia) is a consolidation of DSM-5-defined chronic major depressive disorder and dysthymic disorder, and is characterized by a depressed mood for most of the day, for more days than not, for at least 2 years. In children and adolescents, mood can be irritable and duration must be at least 1 year. The DSM-5 specifies that patients presenting symptoms that comply with the diagnostic criteria for major depressive disorder for 2 years should also be diagnosed with persistent depressive disorder. When the individual in question is experiencing a depressive mood episode, they must also present at least two of the following symptoms: poor appetite or overeating, insomnia or hypersomnia, low energy or fatigue, low self-esteem, poor concentration, or difficulty making decisions and feelings of hopelessness. The prevalence of this disorder in the United States is 0.5%.
Premenstrual Dysphoric Disorder
The diagnostic criterion for premenstrual dysphoric disorder states that, in the majority of menstrual cycles, at least five symptoms must be present during the last week before the start of menstruation, and individuals should start to feel better a few days later, with all symptoms disappearing completely or almost completely during the week after menstruation. The most important characteristics of this disorder are affective lability, intense irritability or anger, or increased interpersonal conflicts, markedly depressed mood and/or over-excitation, and symptoms of anxiety which may be accompanied by behavioral and somatic symptoms. Symptoms must be present during most menstrual cycles during the past year and must negatively affect occupational and social functioning. The most rigorous estimations of the prevalence of this disorder claim that 1.8% of women comply with the criterion but have no functional impairment, while 1.3% comply with the criterion and suffer functional impairment and other concomitant symptoms of another mental disorder.
Substance/Medication-Induced Depressive Disorder
Substance/medication-induced depressive disorder is characterized by the presence of the symptoms of a depressive disorder, such as major depressive disorder, induced by the consumption, inhalation or injection of a substance, with said symptoms persisting after the physiological effects or the effects of intoxication or withdrawal have disappeared. Some medication may generate depressive symptoms, which is why it is important to determine whether the symptoms were actually induced by the taking of the drug or whether the depressive disorder simply appeared during the period in which the medication was being taken. The prevalence of this disorder in the United States is 0.26%.
Depressive Disorder Due to Another Medical Condition
Depressive disorder due to another medical condition is characterized by the appearance of a depressed mood and a markedly diminished interest or pleasure in all activities within the context of another medical condition. The DSM-5 offers no information about the prevalence of this disorder.
The category Other specified depressive disorder is used when the symptoms characteristic of a depressive disorder appear and cause significant distress or impairment in social, occupational or other areas of functioning but do not comply with all the criteria of any depressive disorder, and the clinician opts to communicate the specific reason for this. In the Other unspecified depressive disorder category , on the other hand, the difference is that the clinician prefers not to specify the reason why the presentation fails to comply with all the criteria of a specific disorder and includes presentations about which there is insufficient information for giving a more specific diagnosis.
In the ICD-10, depressive disorders are included within the mood disorders category. The following disorders are analyzed below: single depressive episode, recurrent depressive disorder, and persistent mood (affective) disorders.
Single Depressive Episode
The classification Single depressive episode distinguishes between depressive episodes of varying severity: mild, moderate, and severe without psychotic symptoms. Characteristics common to all of them include lowering of mood, reduction of energy, and decrease in daily activity. There is a loss of interest in formerly pleasurable pursuits, a decrease in the capacity for concentration, and an increase in tiredness, even during activities requiring minimum effort. Changes occur in appetite, sleep is disturbed, self-esteem and self-confidence drop, ideas of guilt or worthlessness are present and the symptoms vary little from day to day. In its mildest form, two or three of the symptoms described above may be present, and the patient is able to continue with most of their daily activities. When the episode is moderate, four or more of the symptoms are usually present and the patient is likely to have difficulty continuing with ordinary activities. In its most severe form, several of the symptoms are marked and distressing, typically loss of self-esteem and ideas of worthlessness or guilt. Suicidal thoughts and acts are common and a number of somatic symptoms are usually present. If the depressive episode is with psychotic symptoms, it is characterized by the presence of hallucinations, delusions, psychomotor retardation, or stupor so severe that ordinary social activities are impossible; there may be danger to life from suicide, dehydration, or starvation.
Recurrent Depressive Disorder
Recurrent depressive disorder is characterized by repeated episodes of depression similar to those described above for single depressive episodes without mania. There may be brief episodes of mild mood elevation and over activity (hypomania) immediately after a depressive episode, sometimes precipitated by antidepressant treatment. The more severe forms of this disorder are very similar to manic-depressive depression, melancholia, vital depression, and endogenous depression. The first episode may occur at any age, from childhood to old age. The onset may be either acute or insidious and can last from a few weeks to many months. Recurrent depressive disorder can be mild or moderate, but in neither of these is there any history of mania. This section also includes recurrent depressive disorder currently in remission, in which the patient may have had two or more depressive episodes in the past, but has been free from depressive symptoms for several months.
Persistent Mood [Affective] Disorders
Persistent mood [affective] disorders are persistent and usually fluctuating disorders in which the majority of episodes are not sufficiently severe to warrant being diagnosed as hypomanic or mild depressive episodes. Since they last for many years and affect the patient's normal life, they involve considerable distress and disability. This section also includes cyclothymia and dysthymia. Cyclothymia is a persistent instability of mood involving numerous periods of depression and mild elation, none of which are sufficiently prolonged to justify a diagnosis of bipolar affective disorder or recurrent depressive disorder. This disorder is frequently found among the relatives of patients with bipolar affective disorder and some patients with cyclothymia eventually develop bipolar affective disorder. For its part, dysthymia is a chronic depression of mood, lasting at least several years, which is not sufficiently severe, or in which individual episodes are not sufficiently prolonged, to justify a diagnosis of mild, moderate, or severe recurrent depressive disorder.
Other Mood (Affective) Disorders
Finally, other mood (affective) disorders include any mood disorders that do not fall into the categories described above because they are not of sufficient severity or duration. They may be single, recurrent (brief), or specified episodes.
The manifestations and symptoms of depression vary in accordance with age and level of development. However, it is clear that the DSM-5 and the ICD-10 do not distinguish between adult and child depression, although by including disruptive mood dysregulation disorder, the DSM-5 does take into account the fact that children and young people aged between 7 and 18 may express their distress in other ways, through chronic, severe, and recurrent irritability manifested verbally and/or behaviorally. Similarly, major depressive disorder specifies that in children the mood may be irritable rather than depressed. However, no distinctions of this kind are found in the ICD-10, an absence which may lead to the faulty inference that the characteristics of child and adolescent depression are similar to those of adult depression.
Explanatory Theories of Depression
Depressive disorders cannot be explained by any single theory, since many different variables are involved in their onset and persistence. The principal biological and psychological theories were therefore taken as the main references for this section. Subsequently, the contributions made by each of these theories regarding depression were studied by conducting searches in PubMed, Web of Science, Science direct, and Google Scholar. With the constant key words being depression, child depression and adolescent depression, the search for information cross-referenced a series of other key words also in accordance with the specific theory in question. Due to the importance of some seminal works in relation to the development of psychological theories of depression, certain authors have remained key references for decades. A total of 64 bibliographical references were used. The following is a summary of the various explanations for the onset of depression, according to the different theoretical frameworks.
Biological Theories
If a mood disorder cannot be explained by family history or stressful life events, then it may be that the child or adolescent in question is suffering from a neurological disease. In such a case, depressive symptoms may manifest early in children and adolescents as epileptic syndromes, sleep disorders, chronic recurrent cephalalgias, several neurometabolic diseases, and intracranial tumors (Narbona, 2014 ).
Noradrenalin Deficit
Serotonin is a monoamine linked to adrenaline, norepinephrine, and dopamine which plays a key role, particularly in the brain, since it is involved in important life regulation functions (appetite, sleep, memory, learning, temperature regulation, and social behaviors, etc.), as well as many psychiatric pathologies (Nique et al., 2014 ). Serotonin modulates neuroplasticity, particularly during the early years of life, and dysfunctions in both systems contribute to the physiopathology of depression (Kraus et al., 2017 ). MRI tests in animals have revealed that a reduction in neuron density and size, as well as a reduction in hippocampal volume among depressive patients may be due to serotonergic neuroplasticity changes. Branchi ( 2011 ), however, argues that improving serotonin levels may increase the likelihood of both developing and recovering from the psychopathology, and underscores the role played by the social environment in this process. In this sense, Curley et al. ( 2011 ) point out that the quality of the social environment may influence the development and activity of neural systems, which in turn have an impact on behavioral, physiological, and emotional responses.
Endocrine Alterations
Age-related changes and the presence of biological risk factors, including endocrine, inflammatory or immune, cardiovascular and neuroanatomical factors, make people more vulnerable to depression (Clarke and Currie, 2009 ). Indeed, some studies suggest that depression may be linked to endocrine alterations: nocturnal cortisol secretions (Birmaher et al., 1996 ), nocturnal growth hormone secretion (Ryan et al., 1994 ), thyroid stimulating hormone secretion (Puig-Antich, 1987 ), melatonin and prolactin secretions (Waterman et al., 1994 ), high cortisol levels (Herane-Vives et al., 2018 ), or decreased growth hormone production (Dahl et al., 2000 ). Puberty and the accompanying hormonal and physical changes require special attention because it has been proposed that they could be associated with an increased incidence of depression (Reinecke and Simons, 2005 ).
Sleep Disorders
Sleep problems are often associated with situations of social deprivation, unemployment, or stressful life events (divorce, bad life habits, or poor working conditions) (Garbarino et al., 2016 ). It also seems, however, that sleep disorders are linked to the development of depression. This relationship occurs as a result of how insufficient sleep affects the hippocampus, heightening neural sensitivity to excitotoxic insult and vulnerability to neurotoxic challenges, resulting in a net decrease in gray matter in the hippocampus in the left orbitofrontal cortex (Novati et al., 2012 ).
For their part, Franzen and Buysse ( 2008 ) state that bidirectional associations between sleep disturbances (particularly insomnia) and depression make it more difficult to distinguish cause-effect relations between them. It is therefore unclear whether depression causes sleep disturbances or whether chronic sleep disturbances lead to the appearance of depression. What does seem clear, however, is that treating sleep disturbances (both insomnia and hypersomnia) may help reduce the severity of depression and accelerate recovery (Franzen and Buysse, 2008 ).
Longitudinal studies have identified insomnia as a risk factor for the onset or recurrence of depression in young people and adults (Sivertsen et al., 2014 ). In comparison with the non-clinical population, depressed children and adolescents report both trouble sleeping and longer sleep duration (Accardo et al., 2012 ).
For their part, Foley and Weinraub ( 2017 ) observed that, among preadolescent girls, early and later sleep problems directly or indirectly predicted a wide variety of social and emotional adjustment disorders (depressive symptoms, low school competence, poor emotion regulation, and risk-taking behaviors).
Altered Neurotransmission
Studies conducted over the past 20 years have shown that increased inflammation and hyperactivity of the hypothalamic–pituitary–adrenal (HPA) axis may explain major depression (Pariante, 2017 ). Some of the pathophysiological mechanisms of depression include altered neurotransmission, HPA axis abnormalities involved in chronic stress, inflammation, reduced neuroplasticity, and network dysfunction (Dean and Keshavan, 2017 ). Other studies report alterations in the brain structure: smaller hippocampus, amygdala, and frontal lobe (Whittle et al., 2014 ). Nevertheless, the underlying molecular and clinical mechanisms have yet to be discovered (Pariante, 2017 ). Major depressive disorder in children and adolescents has been associated with increased intracortical facilitation, a direct neurophysiological result of excessive glutamatergic neurotransmission. However, contrary to the findings in adults with depression, no deficits in cortical inhibition were found in children and adolescents with major depressive disorder (Croarkin et al., 2013 ).
Genetic Factors
Other studies have highlighted the importance of genetics in the onset of depression (40%) (Scourfield et al., 2003 ). It is important to recognize that a genetic predisposition to an excessive amygdala response to stress, or a hyperactive HPA axis (moderate hyperphenylalaninemia) due to stress during early childhood may trigger an excessive effect or alter an otherwise healthy psychological system (Dean and Keshavan, 2017 ). Kaufman et al. ( 2018 ) support a potential role for genes related to the homeobox 2 gene of Orthodenticle (OTX2) and to the OTX2-related gene in the physiopathology of stress-related depressive disorders in children. Furthermore, genetic anomalies in serotonergic transmission have been linked to depression. The serotonin-linked polymorphic region (5-HTTLPR) is a degenerate repeat in the gene which codes for the serotonin transporter (SLC6A4). The s/s genotype of this region is associated with a reduction serotonin expression, in turn linked to greater vulnerability to depression (Caspi et al., 2010 ).
For their part, Oken et al. ( 2015 ) claim that psychological disturbances may trigger changes in physiological parameters, such as DNA transcription, or may result in epigenetic modifications which alter the sensitivity of the neurotransmitter receptor.
Psychological Theories
This section outlines the different psychological theories which have attempted to explain the phenomenon of depression. Depression is a highly complex disorder influenced by multiple factors, and it is clear that no single theory can fully explain its etiology and persistence. It is likely that a more eclectic outlook must be adopted if we are to make any progress in determining the origin, development, and maintenance of this pathology.
Attachment-Informed Theories
Attachment theory was the term used by Bowlby ( 1976 ) to refer to a specific conceptualization of human beings' propensity to establish strong and long-lasting affective ties with other people. Bowlby ( 1969 , 1973 ) proposes that consistency, nurturance, protectiveness, and responsiveness in early interactions with caregivers contribute to the development of schemas or mental representations about the relationships of oneself with others, and that these schemas serve as models for later relationships. Bowlby's ethological model of attachment postulates that vulnerability to depression stems from early experiences which failed to satisfy the child's need for security, care and comfort, as well as from the current state of their intimate relations (Bowlby, 1969 , 1973 , 1988 ). Adverse early experiences can contribute to disturbances in early attachments, which may be associated with vulnerability for depression (Cummings and Cicchetti, 1990 ; Joiner and Coyne, 1999 ). Associations between insecure attachment among children and negative self-concept, sensitivity to loss, and an increased risk of depression in childhood and adolescence have been reported (Armsden et al., 1990 ; Koback et al., 1991 ; Kenny et al., 1993 ; Roelofs et al., 2006 ; Allen et al., 2007 ; Chorot et al., 2017 ). Relationships between secure attachment and depression seem also to be mediated by the development of maladaptive beliefs or schemas (Roberts et al., 1996 ; Reinecke and Rogers, 2001 ).
Thus, attachment theory has become a useful construct for conceptualizing many different disorders and provides valuable information for the treatment of depression (Reinecke and Simons, 2005 ).
Ainsworth described three attachment styles, in accordance with the child's response to the presence, absence, and return of the mother (or main caregiver): secure, anxious-avoidant, and anxious-resistant (Ainsworth et al., 1978 ). The least secure attachment styles may give rise to traumatic experiences during childhood, which in turn may result in the appearance of depressive symptoms.
Similarly, Hesse and Main ( 2000 ) argued that the central mechanism regulating infant emotional survival was proximity to attachment figures, i.e., those figures who help the child cope with frightening situations. Using Ainsworth's strange situation procedure, Main ( 1996 ) found that abused children engaged in more disorganized, disruptive, aggressive, and dissociative behaviors during both childhood and adolescence. Main ( 1996 ) also found that many people with clinical disorders have insecure attachment and that psychological-disoriented and disorganized children are more vulnerable.
For his part, Blatt ( 2004 ) explored the nature of depression and the life experiences which contribute to its appearance in more depth, identifying two types of depression which, despite a common set of symptoms, nevertheless have very different roots: (1) anaclitic depression, which arises from feelings of loneliness and abandonment; and (2) introjective depression, which stems from feelings of failure and worthlessness. This distinction is consistent with psychoanalytical formulations, since it considers defenselessness/dependency and desperation/negative feelings about oneself to be two key issues in depression.
Brazelton et al. ( 1975 ) found that at age 3 weeks, babies demonstrate a series of interactive behaviors during face-to-face mother-infant interactions. These behaviors were not found to be present in more disturbed interactions, which may trigger infant anxiety.
In a longitudinal study focusing on the relationship between risk of maternal depression and infant attachment behavior, Bigelow et al. ( 2018 ) analyzed babies at age 6 weeks, 4 and 12 months, finding that mothers at risk of depression soon after the birth of their child may have difficulty responding appropriately to their infant's attachment needs, giving rise to disorganized attachment, with all the psychological consequences that this may involve. Similarly, Beeghly et al. ( 2017 ) found that among infants aged between 2 and 18 months, greater maternal social support was linked to decreasing levels of maternal depressive symptoms over time, and that boys were more vulnerable than girls to early caregiving risks such as maternal depression, with negative consequences for mother-child attachment security during toddlerhood.
Authors such as Shedler and Westen ( 2004 ) have attempted to find solutions to the problems arising in relation to the DSM diagnostic categories, developing the Shedler Westen Assessment Procedure (SWAP-200) to capture the wealth and complexity of clinical personality descriptions and to identify possible diagnostic criteria which may better define personality disorders.
For their part, Ju and Lee ( 2018 ) argue that peer attachment reduces depression levels in at-risk children, and also highlight the curative aspect of attachment between adolescent peers.
Behavioral Models
The first explanations proposed by this model argued that depression occurs due to the lack of reinforcement of previously reinforced behaviors (Skinner, 1953 ; Ferster, 1966 ; Lewinsohn, 1975 ), an excess of avoidance behaviors and the lack of positive reinforcement (Ferster, 1966 ) or the loss of efficiency of positive reinforcements (Costello, 1972 ). A child with depression initially receives a lot of attention from his social environment (family, friends…), and behaviors such as crying, complaints or expressions of guilt are reinforced. When these depressive behaviors increase, the relationship with the child becomes aversive, and the people who used to accompany the child avoid being with him, which contributes to aggravating his depression (Lewinsohn, 1974 ). Low reinforcement rates can be explained by maternal rejection and lower parental support (Simons and Miller, 1987 ), by a lower rate of reinforcement offered to their children by mothers of depressed children (Cole and Rehm, 1986 ), or by low social competence (Shah and Morgan, 1996 ).
Depression is mainly a learned phenomenon, related to negative interactions between the individual and his or her environment (e.g., low rate of reinforcement or unsatisfactory social relations). These interactions are influenced by cognitions, behaviors and emotions (Antonuccio et al., 1989 ).
Cognitive Models
The attributional reformulation of the learned helplessness model (Abramson et al., 1978 ) and Beck's cognitive theory (Beck et al., 1979 ) are the two most widely-accepted cognitive theories among contemporary cognitive models of depression (Vázquez et al., 2000 ).
Learned helplessness is related to cognitive attributions, which can be specific/global, internal/external, and stable/unstable (Hiroto and Seligman, 1975 ; Abramson et al., 1978 ). Global attribution implies the conviction that the negative event is contextually consistent rather than specific to a particular circumstance. Internal attribution is related to the belief that the aversive situation occurs due to individual conditions rather than to external circumstances. Stable attribution is the belief that the aversive situation is unchanging over time (Miller and Seligman, 1975 ). People prone to depression attribute negative events to internal, stable and global factors and make external, unstable, and specific attributions for success (Abramson et al., 1978 ; Peterson et al., 1993 ), a cognitive style also present in children and adolescents with depression (Gladstone and Kaslow, 1995 ).
The Information Processing model (Beck, 1967 ; Beck et al., 1979 ) postulates that depression is caused by particular stresses that evoke the activation of a schema that screens and codes the depressed individual's experience in a negative fashion (Ingram, 1984 , p. 443). Beck suggests that this distortion of reality is expressed in three areas, which he calls the “cognitive triad”: negative views about oneself, the world and the future as a result of their learning history (Beck et al., 1983 ). These beliefs are triggered by life events which hold special meaning for the subject (Beck and Alford, 2009 ).
Self-Control Model
This theory assumes that depression is due to deficits in the self-control process, which consists of three phases: self-monitoring, self-evaluation, and self-administration of consequences (Rehm, 1977 ; Rehm et al., 1979 ). In the self-monitoring phase, individuals attend only to negative events and tend to recognize only immediate, short-term consequences. In the self-evaluation phase, depressed individuals establish unrealistic evaluation criteria and inaccurately attribute their successes and failures. If self-evaluation is negative, in the self-administration of consequences phase the individual tends to engage very little in self-reinforcement and very frequently in self-punishment.
Both Rehm's self-control model (Rehm, 1977 ) and Bandura's conception of child depression (Bandura, 1977 ) assume that children internalize external control guidelines. These guidelines are related to family interaction patterns and both may contribute to the etiology or persistence of depression in children.
In a study conducted with children aged between 8 and 12 years, Kaslow et al. ( 1988 ) found that depressed children had a more depressive attributional style and more self-control problems.
Interpersonal Theory
This model, which is closely linked to attachment theories, aims to identify and find solutions for an individual's problems with depression in their interpersonal functioning. It suggests that the difficulties experienced are linked to unresolved grief, interpersonal disputes, transition roles and interpersonal deficits (Markowitz and Weissman, 1995 ).
Milrod et al. ( 2014 ) argue that pathological attachment during early childhood has serious consequences for adults' ability to experience and internalize positive relationships.
Similarly, various different studies have highlighted the fact that one of the variables that best predicts depression in children is peer relations (Bernaras et al., 2013 ; Garaigordobil et al., 2017 ).
Stressful Life Events
Studies focusing on the adult population have reported that between 60 and 70% of depressed adults experienced one or more stressful events during the year prior to the onset of major depression (Frank et al., 1994 ). In children and adolescents, modest associations have been found between stressful life events and depression (Williamson et al., 1995 ). For their part, Shapero et al. ( 2013 ) found that people who had suffered severe emotional abuse during childhood experienced higher levels of depressive symptoms when faced with current stressors. Sokratous et al. ( 2013 ) argue that the onset of depression is not only triggered by major stressful events, but rather, minor life events (dropping out of school, your father losing his job, financial difficulties in the family, losing friends, or the illness of a family member) may also influence the appearance of depressive symptoms.
Events such as the loss of loved ones, divorce of parents, mourning or exposure to suicide (either individually or collectively) have all been associated with the onset of depression in childhood (Reinherz et al., 1993 ). Factors such as a history of additional interpersonal losses, added stress factors, a history of psychiatric problems in the family and prior psychopathology (including depression) increase the risk of depression in adolescents (Brent et al., 1993 ). Birmaher et al. ( 1996 ) found that prior research into stressful life events in relation to early-onset depression had been based on data obtained from self-reports, making it difficult to determine the causal relationship, since events may be both the cause and consequence of depression.
However, not everyone exposed to this kind of traumatic experience becomes depressed. Personality and the moment at which events occur are both involved in the relationship between depression and stressful life events, although biological factors such as serotonergic functioning (Caspi et al., 2010 ) also exert an influence.
Sociocultural Models
These models postulate that cultural variables are responsible for the appearance of depressive symptoms. These variables are mainly acculturation and enculturation. In acculturation, structural changes are observed (economic, political, and demographic), along with changes in people's psychological behavior (Casullo, 2001 ). Some studies link increased suicide rates with economic recession (Chang et al., 2013 ; Reeves et al., 2014 ). Enculturation occurs when the older generation invites, induces or forces the younger generation to adopt traditional mindsets and behaviors.
In an attempt to better understand the influence of culture and family on depressive symptoms, Lorenzo-Blanco et al. ( 2012 ) tested an acculturation, cultural values and family functioning model with Hispanic students born in the United States. The results revealed that both family conflict and family cohesion were related to depressive symptoms.
Another study carried out with girls aged 7–10 years (Evans et al., 2013 ) observed that internalizing an unrealistically thin ideal body predicted disordered eating attitudes through body dissatisfaction, dietary restraint and depression.
Finally, the importance of family interactions in the onset of depressive symptoms cannot be overlooked. Parenting style has been identified as a key factor in children's and adolescents' psychosocial adjustment (Lengua and Kovacs, 2005 ). Parental behavior has been studied from two different perspectives: warmth and control. Warmth is linked to aspects such as engagement and expression of affection, respect, and positive concern by parents and/or principal caregivers (Rohner and Khaleque, 2003 ). In this sense, prior studies have identified a significant association between parental warmth and positive adjustment among adolescents (Barber et al., 2005 ; Heider et al., 2006 ). Rohner and Khaleque ( 2003 ) argue that children's psychological adjustment is closely linked to their perception of being accepted or rejected by their principal caregivers, and other studies have found that weaker support from parents is associated with higher levels of depression and anxiety among adolescents (Yap et al., 2014 ).
Similarly, Jaureguizar et al. ( 2018 ) found that a low level of perceived parental warmth was linked to high levels of clinical and school maladjustment, and that the weaker the parental control, the greater the clinical maladjustment. These authors also found that young people with negligent mothers and authoritarian fathers had higher levels of clinical maladjustment.
In short, according to the different theories, depression may be due to (1) biological reasons; (2) insecure attachment; (3) lack of reinforcement of previously-reinforced behaviors; (4) negative interpersonal relations and relations with one's environment and the resulting negative consequences; (5) attributions made by individuals about themselves, the world and their future; and (6) sociocultural changes. It is likely that no single theory can fully explain the genesis and persistence of depression, although currently, negative interpersonal relations and relations with one's environment and sociocultural changes (economic, political, and demographic) may explain the observed increase in the prevalence of depression.
Evaluation Instruments
Many different evaluation instruments can be used to measure child and adolescent depression. Tables 2 , ,3 3 outline the ones most commonly used in scientific literature. Table 2 summarizes the main self-administered tests that specifically measure child and adolescent depression, while Table 3 presents tests that measure child and adolescent depression among other aspects (i.e., broader or more general tests). Finally, Table 4 summarizes the main hetero-administered psychometric tests for assessing this pathology.
Self-administered psychometric tests designed specifically for evaluating child and adolescent depression.
| Children's Depression Scale (CDS) | Lang and Tisher, | 66 | Depressive total: Affective Response, Social Problems, Self-esteem, Pre-occupation with own Sickness or Death, Guilt and Various Depressives. Positive Total: Mood-Joy and Various Positives. | 8–16 | K-R20 = 0.91; Alpha = 0.92–0.94; Guttman split-half coefficient = 0.90; Test-retest reliability = 0.74 (Bath and Middleton, ; Tisher et al., ) | Seisdedos, |
| Children's Depression Inventory (CDI) | Kovacs, | 27 | Scales: emotional problems, functional problems. Subscales: negative mood/physical symptoms, negative self-esteem, interpersonal problems, ineffectiveness | 7–17 | Alpha = 0.75–0.90; κ = 0.76; K-R20 = 0.80–0.94; Test-retest reliability = 0.62–0.82; Sensitivity = 0.81–0.95; Specificity = 0.64–0.96; PPV = 0.21–0.90; NPPV = 0.63–1.00 (view review by Stockings et al., ) | Del Barrio and Carrasco, |
| Center for Epidemiological Studies Depression Scale for Children (CES-DC) | Weissman et al., | 20 | Total depression | 12–18 | Alpha = 0.86–0.89; Sensitivity = 0.71–0.82; Specificity = 0.62–0.90; PPV = 015; NPV = 0.96 (view review by Stockings et al., ) | Soler et al., |
| Depression Self-Rating Scale for Children (DSRS) | Birleson, | 18 | Total depression | 8–14 | Alpha = 0.86 Test-retest reliability = 0.80; Sensitivity = 0.67; Specificity = 0.77; PPV = 0.15; NPV = 0.97 (Birleson et al., ) | No |
| Reynolds Adolescent Depression Scale (RADS) | Reynolds, | 30 | Total depression, dysphoric mood, Anhedonia/negative affect, Negative self-evaluation, somatic complaints | 13–17 | Alpha = 0.92 (view review by Stockings et al., ); Sensitivity = 0.86; Specificity = 0.49; PPV = 0.69; NPV = 0.72 (Krefetz et al., ) | Del Barrio et al., |
| Reynolds Child Depression Scale (RCDS) | Reynolds, | 30 | Total depression | 7–13 | Alpha = 0.85–0.91 Test-retest reliability = 0.82–0.85 (Reynolds, ); Sensitivity = 0.79; Specificity = 0.87 (Figueras et al., ) | Figueras et al., |
| Mood and Feelings Questionnaire (MFQ), and Short Mood and Feelings Questionnaire (SMFQ) | Angold et al., | 32 (MFQ) 13 (SMFQ) | Total depression | 8–18 | MFQ: Alpha = 0.90–0.93; AUC = 0.86 (95% CI: 0.81, 0.91), Sensitivity = 0.84; Specificity = 0.70. SMFQ: Alpha = 0.87–0.89; AUC = 0.86 (95% CI: 0.80, 0.91); Sensitivity = 0.84; Specificity = 0.68 (Thabrew et al., ) | No |
| Beck Depression Inventory (BDI-II) | (Beck et al., ) | 21 | Total depression | 13 and over | Alpha = 0.92–0.94; Sensitivity = 0.74–0.88; Specificity = 0.70–0.92; PPV = 0.76–0.85; NPV = 0.67–0.95 (view review by Stockings et al., ) | Sanz and Vázquez, |
| Revised Child Anxiety and Depression Scale—RCADS | Chorpita et al., | Two versions: with 47 and 30 items | Anxiety and separation disorders. Social phobia, Generalized anxiety, Panic, Obsessive compulsive disorder and Major depressive disorder. Total Anxiety and Depression Score | 8-18 | Alpha = 0.78; sensitivity = 0.74; specificity = 0.77 for the Major Depression scale (MDD). RCADS MDD scale correlated positively and significantly with the CDI | RCADS: (Sandín et al., ); RCADS-30: (Sandín et al., ) |
| Kutcher Adolescent Depression Scale (KADS) | Leblanc et al., | 16 (long), 11 (short), and 6 (brief) | Total depression | 6–18 | KADS-16 Alpha = 0.82; AUC = 0.85 KADS-11: Alpha = 0.84; AUC = 0.94, (95%CI: 0.91, 0.97); Sensitivity = 0.89; Specificity = 0.90 KADS-6: Alpha = 0.80 Sensitivity = 0.92 Specificity = 0.71; PPV = 0.10 for total sample and.26 for clinical sample; NPV = 1.0 for the total sample and.99 for the clinical sample (Leblanc et al., ; Brooks et al., ; Zhou et al., ) | There is a Spanish version, but no data are available regarding its validation. |
| Cuestionario Educativo Clínico de ansiedad y depresión ( ) (CECAD) | Lozano et al., | 50 | Depression, anxiety, worthlessness, irritability, problems with thinking and psycho-physiological symptoms | 7-adulthood | Alpha = > 0.83 Omega coefficient = 0.77–0.87. Correlations with CDI between 0.26 and 0.76. | – |
KR-20, Kuder-Richardson coefficient (formula 20); κ, Cohen's kappa reliability co-efficient; PPV, Positive predictive value; NPV, Negative predictive value; AUC, Area under the Receiver Operating Characteristic Curve (AUC) .
Self-administered general psychometric tests which, among other variables, also assess child and adolescent depression.
| Symptom Checklist-90. SCL-90 | Derogatis and Cleary, | 90 | Somatization, obsessive-compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism. Global severity index, Positive Symptom Distress Index, Positive Symptom Total. | 13 and over | Alpha = 0.98 | González De Rivera et al., |
| Pediatric Symptom Checklist (PSC) | Jellinek et al., | 35 | Attention, internalizing symptoms, and externalizing symptoms | 3-16 | Alpha = .91 | Version for adolescents: (Lemos et al., ) |
| Child Behavior Checklist (CBCL) | Achenbach and Edelbrock, | 133 | Scales: Withdrawal, somatic complaints, anxiety/depression, social problems, thought problems, attention problems, rule-breaking behavior and aggressive behavior | 4–18 | Alpha = between 0.72 and 0.97 | Rubio-Stipec et al., |
| Behavior Assessment System for Children (BASC-2) Sistema de Evaluación de la Conducta de Niños y Adolescentes | Reynolds and Kamphaus, | Total: 146. 15 items on depression | Negative attitude to school, negative attitude to teachers, atypicality, external locus of control, social stress, anxiety, depression, sense of inadequacy, interpersonal relations, relations with parents, self-esteem, self-reliance, clinical maladjustment, school maladjustment, personal adjustment, emotional symptoms index | 8–12 | Alpha = between 0.70 and 0.80 | González et al., |
| Self-administered Psychiatric Scales for Children and Adolescents (SAFA) | Cianchetti and Sannio Fascello, | 174 | Anxiety, depression, obsessive-compulsive symptoms, eating disorders, hypochondria, somatic symptoms and phobias | 8–18 | Alpha = 0.80 | No |
| Beck Youth Inventories (BYI-2) | Beck et al., | 100 | Depression, anxiety, anger, disruptive behavior and self-concept. | 7–18 | Alpha = between 0.90 and 0.95 | No (scheduled for the near future) |
Hetero-administered psychometric tests for assessing child and adolescent depression.
| Children's Depression Rating Scale-Revised (CDRS-R) | Poznanski et al., | 17 | Total depression | Clinical personnel (interviews with child and parents) | 6–12 | Alpha = .85 | No |
| Escala para la evaluación de la depresión para maestros ( ) (ESDM) | Domènech-Llaberia and Polaino-Lorente, | 16 | Performance, social interaction, inhibited depression, and anxious depression | Teachers | 8–12 | Alpha = 0.88 | – |
| Diagnostic Interview for Children and Adolescents–Revised (DICA-R) | Reich et al., | 1–2 h | Disruptive behavior disorders, mood disorders, anxiety disorders, eating disorders, and elimination disorders | Clinical personnel (interviews with child and parents) | 8–18 | High intra-rater reliability and moderate agreement between parents-children/adolescents (see Ezpeleta et al., ). | Ezpeleta et al., |
| Semistructured Clinical Interview for Children and Adolescents (SCICA) | McConaughy and Achenbach, | 224 | Anxiety, depression, motor/language problems, attention problems, self-control problems, aggression, somatic complaints | Clinical personnel | 6–18 | Mean test-retest reliability: 0.78 | No |
| The Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime (K-SADS-PL) | Kaufman et al., | 82+5 modules | Major depression, dysthymia, mania, hypomania, cyclothymia, bipolar disorder, schizoaffective disorder, schizophrenia, schizophreniform disorder, brief reactive psychosis, panic disorder, agoraphobia, separation anxiety disorder, avoidant disorder of childhood and adolescence, simple phobia, social phobia, generalized anxiety, obsessive compulsive disorder, attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, enuresis, encopresis, anorexia nervosa, bulimia, transient tic disorder, Tourette's disorder, chronic motor or vocal tic disorder, alcohol abuse, substance abuse, post-traumatic stress disorder, and adjustment disorders | Clinical personnel | 6–18 | High convergent validity and limited divergent validity (Lauth et al., ). | No |
| Diagnostic Interview Schedule for Children (DISC) | Shaffer et al., | 1–2 h | Anxiety disorders, mood disorders, disruptive disorders, substance abuse, others (anorexia, bulimia, enuresis/encopresis, selective mutism, schizophrenia, etc.) | Clinical personnel (interviews with child and parents) | 6–17 | No validity data available. Acceptable test-retest reliability (Shaffer et al., ) | Bravo et al., |
| Screening de problemas emocionales y de conducta infantil ( ) (SPECI) | Garaigordobil and Maganto, | 10 min | Withdrawal, somatization, anxiety, infantile-dependent, problems with thinking, attention-hyperactivity, disruptive behavior, academic performance, depression, and violent behavior | Teachers | 5–12 | Alpha = 0.82 | – |
As shown in the tables above, there are several self-administered instruments that can be used with children from age 6 to 7 onwards, although their duration should be taken into consideration in order to avoid overtiring subjects. While it is clear that an effort has been made to design shorter measures (compare, for example, the 66 items of the CDS with the 16 items of the longest version of the KADS), the duration of the test should not be the only aspect taken into account when selecting an evaluation instrument.
One of the most widely used instruments to measure child depression in the scientific literature is the Children's Depression Inventory-CDI (Kovacs, 1985 ), which is based on the Beck Depression Inventory-BDI (Beck and Beamesderfer, 1974 ). Thus, it is based on Beck's cognitive theory of depression. Following this same theoretical line, the Children's Depression Scale-CDS (Lang and Tisher, 1978 ) was designed, but in this case, this instrument was not created based on another instrument previously designed for adult population (as in the case of the CDI), but instead from its beginnings, it was conceived exclusively to assess child depression. Chorpita et al. ( 2005 ) explain that the CDI measures a broader construct of negative affectivity rather than depression as a separate construct, and that it may be useful for screening for trait dimensions or personality features, whereas other instruments, such as the Revised Child Anxiety and Depression Scale-RCADS (Chorpita et al., 2000 ), measure a specific clinical syndrome.
Table 2 describes many other instruments that are very useful as screening tests for depression and depressive disorder, such as the Center for Epidemiological Studies Depression Scale for Children-CES-DC (Weissman et al., 1980 ) (based on the Center for Epidemiological Studies Depression Scale for Adults, CES-D; Radloff, 1977 ), the Mood and Feelings Questionnaire-MFQ (Angold et al., 1995 ), or the Depression Self-Rating Scale for Children-DSRS (Birleson, 1981 ). This last one, for example, is useful to measure moderate to severe depression in childhood and is based on the operational definition of depressive disorder, that is, a specific affective-behavior pattern that implies an impairment of a child's or adolescent's ability to function effectively in his/her environment (Birleson, 1981 ).
The cognitive and affective component of depression is the one that is most present in the instruments described in Table 2 . In fact, for example, the Short Mood and Feelings Questionnaire (SMFQ) includes the cognitive and affective items from the original MFQ item pool, in addition to some items related to tiredness, restlessness, and poor concentration (Angold et al., 1995 ). In the SMFQ, more than half of the items from the MFQ were removed, and even so, high correlations between the MFQ and the SMFQ were found (Angold and Costello, 1995 ), which may be indicating that the really important items were the cognitive and affective items that were maintained. Reynolds et al. ( 1985 ) defended that children could accurately report their cognitive and affective characteristics, so “ if one wishes to know how a child feels, ask the child” (Reynolds et al., 1985 , p. 524).
Depending on the specific aim of the evaluation or research study, a broader diagnostic measure, such as those outlined in Table 3 , may also provide valuable information. Finally, it is worth noting that only two hetero-administered instruments were found for teachers, with all others being clearly oriented toward the clinical field. In this sense, special emphasis should be placed on the need to develop valid and reliable instruments for teachers, since they may be key agents for detecting symptoms among their students. While it is important to train teachers in this sense, it is also important to provide them with instruments to help them assess their students. The instruments that are currently available have produced very different results as regards their correlation with students' self-reported symptoms, although in general, teachers tend to underestimate their students' depressive symptoms (Jaureguizar et al., 2017 ).
Child and Adolescent Depression Prevention Programs in the School Environment
Extant scientific literature was reviewed in order to summarize the main depression prevention programs for children and adolescents in school settings. The databases used for conducting the searches were PubMed, PsycINFO, Web of Science, Scopus, Science Direct, and Google Scholar, along with a range of different manuscripts. With the constant key word being depression, the search for information cross-referenced a series of other key words also, namely: “child * OR adolescent * ,” “prevent * program,” and “school OR school-based.” Searches were conducted for information published between January 1, 1970 and December 31, 2017.
First, articles were screened (i.e., their titles and abstracts were read and a decision was made regarding their possible interest for the review study). The inclusion criteria were that the study analyzed all the research subjects of the review study (depression, childhood, or adolescence and prevention programs in school settings), that study participants were aged between 6 and 18, that the study was published in a peer-reviewed journal and that it was written in either English or Spanish. Review studies and their references were also analyzed. Studies focusing mainly on psychiatric disorders other than depression were excluded.
Finally, 39 studies were selected for the review, which explored 8 prevention programs that are outlined in Table 5 . In general terms, child depression prevention programs are divided into two main categories: universal programs for the general population, and targeted programs aimed at either the at-risk population or those with a clear diagnosis. Although scientific literature reports that targeted programs obtain better outcomes than universal ones, the latter type nevertheless offer certain advantages, since they reach a larger number of people without the social stigma attached to having been specially selected (Roberts et al., 2003 ; Huggins et al., 2008 ). Thus, the ideal context for instigating universal child depression prevention programs is the school environment.
School-based child and adolescent depression prevention programs.
| Penn Resiliency Program (PRP) | Gillham et al., | 8–15 | To raise awareness of the relationship between cognition, emotion and behavior, help youngsters develop social and decision-making skills and foster optimism | U | - Cognitive-behavioral perspective - 12 sessions, each lasting 90–120 min - Contents: cognitive restructuring, maladaptive coping strategies, attributional styles, assertiveness, negotiation, relaxation, decision-making, social skills | Significant reduction in depression levels assessed using the CDI (Gillham, ; Gillham et al., ; Quayle et al., ; Chaplin et al., ; Cardemil et al., ) as well as in anxiety levels and behavioral problems, and fostering of wellbeing and optimism. Other universal (Pattison and Lynd-Stevenson, ; Gillham et al., ) and targeted studies (Gillham and Reivich, ; Roberts et al., , ) failed to find any evidence that the program had any impact on the variables analyzed, in either the short or long term. The targeted study by Gillham et al. ( ) found that PRP did not significantly prevent depressive disorders but significantly prevented depression, anxiety, and adjustment disorders (when combined) among high-symptom participants |
| Coping with Stress Course (CWSC) | Clarke et al., | 13–17 | To challenge irrational thoughts, cope with negative moods, overcome passivity, and reach agreements with parents and peers; social skills training | T | - Target population: Adolescents with some known increased risk of depression: past episode of depression; persistent sub-diagnostic dysphoria and/or other depressive symptoms; depressed parents; pregnant, single teen mother; other known risk factors for depression - Based on Beck's (Beck et al., ) and Ellis' (Ellis and Harper, ) cognitive therapy - 15 sessions lasting 45 min and 8 sessions lasting 90 min - Contents: depression and its relationship with stress, training in cognitive restructuring skills and the modification of irrational thoughts | Significant reduction in depression levels and the risk of reappearance at posttest and during follow-up (8, 12, and 18 months) (Clarke et al., , ; Garber et al., ) (depressive symptoms assessed by the Center for Epidemiologic Studies-Depression Scale-CES-D). Participants who were currently on antidepressant medication were excluded from these studies |
| Aussie optimism program | Rooney et al., | 6–11 | To intervene in risk and protection factors for depression and anxiety (cognitive, emotional, and social characteristics). | U | - Cognitive-behavioral perspective - 10 sessions, each lasting 60 min - Contents: identifying negative beliefs about oneself and one's present and future circumstances, identifying and regulating emotions, engaging in pleasurable activities, working with hierarchies of situations which generate fear and learning to relax (Rooney et al., ) | - Rooney et al. ( ) applied the program to 72 children aged between 8 and 9 and found both a significant reduction in depression levels (assessed using the CDI) and more positive causal attributions at posttest and during short-term follow up, although these results were not found to persist in the long term. The effect sizes observed were low (η = 0.09 for the symptoms of depression and η = 0.16 for attributional style). - The program was also found to reduce depressive symptoms (assessed using the CDI) in a study with 47 female 7th grade students, with a 6-month follow up (Quayle et al., ) Resourceful Adolescent Program-Adolescents (RAP-A) |
| Resourceful Adolescent Program- Adolescents (RAP-A) | Shochet et al., | 12–15 | To identify and challenge irrational thoughts, provide training in social skills and problem solving and help prevent conflicts with parents and peers | U | - Cognitive-behavioral perspective - 11 sessions, each lasting 40–50 min - Contents: cognitive restructuring, problem-solving, social skills, and communication training | Significant results in preventing depression in random groups at posttest (measured using the BDI-II and RADS) but not during follow up, at least according to the BDI-II (the effect persisted according to the RADS) (Merry et al., ), although when non-random groups were used the results were also significant during follow up (Shochet et al., ) |
| FRIENDS | Barrett and Turner, | 7–16 | To reduce the incidence of anxiety and depression, emotional distress and social problems, teaching children how to cope with anxiety, both now and in the future | U | - Cognitive-behavioral perspective - 10 sessions, each lasting 120 min + 2 booster sessions - Contents: one's own and other people's emotions, relaxation, trying to do your best, planning steps, making time to have fun together, friendship and family skills, being happy, etc. | Reduced anxiety levels, although the results regarding reduced depression levels are more limited (Barrett and Turner, ; Lowry-Webster et al., ; Lock and Barrett, ). In Barrett and Turner's study with 489 children aged between 10 and 12, the effect size for depression (measured using the CDI) at posttest was 0.09. Curiously enough, self-reported depression decreased slightly in the psychologist-led condition, while slight increases were noted in the teacher-led condition, although these increases were statistically, but not clinically, significant (Barrett and Turner, ) |
| Problem Solving for Life (PSFL) | Spence et al., | 13–15 | Cognitive restructuring, problem solving | U | - Cognitive-behavioral perspective - 8 sessions, each lasting 45–50 min - Contents: challenging maladaptive thoughts, coping with problems | No significant results were found as regards preventing depressive symptoms (Spence et al., ; Sheffield et al., ), although an improvement was observed in all the variables studied in all study groups (those that did and those that did not participate in the program) (Sheffield et al., ) |
| Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST) | Young and Mufson, | 11–16 | Training in social skills, coping with life transitions, and overcoming interpersonal deficits | T | - Target population: adolescents with elevated symptoms of depression - Cognitive-behavioral perspective - 10 sessions, each lasting 90 min - Contents: social and communication skills | Immediate reduction in depressive symptoms, although the benefits did not persist longer than 6 months (Horowitz et al., ; Young et al., ) (depressive symptoms assessed using the Center for Epidemiologic Studies-Depression Scale-CSD-D and the Children's Depression Rating Scale (CDRS) |
| Adolescents Coping with Emotions (ACE) | Sheffield et al., | 14–15 | To prevent or reduce depression levels, improving coping skills, and fostering resilience | T | - Target population: adolescents with elevated symptoms of depression (those scoring in the top 20% on the combined scores, sum of standardized scores, the Children's Depression Inventory (CDI) and the Center for Epidemiologic Studies—Depression Scale (CES-D). - Cognitive-behavioral perspective - Applied by teachers - 8 sessions, each lasting 60 min - Contents: cognitive restructuring, training in social skills and assertiveness, negotiation and problem-solving skills, recognition of one's own achievements | Significant reduction in depressive symptoms and negative thoughts in girls after 6 months (Kowalenko et al., ), but not during the 12-month follow up (Sheffield et al., ). Depressive symptoms were assessed using the CDI and CES-D |
| FORTIUS | Méndez et al., | 8–13 | To psychologically strengthen participants at a cognitive, emotional and behavioral level | U | −12 sessions lasting 50–60 min +2 booster sessions one month later +1 final session 3 months later - Contents: understanding and controlling negative emotions, social skills, and the ability to organize everyday activities, detection and restructuring of negative thoughts, problem solving, decision making, and positive self-instruction | No significant differences were found in depression (measured using the CDI) at posttest, although a reduction was observed during follow up (12 months) in girls (Orenes, ) |
Type: T, targeted; U, universal .
Table 5 outlines the most important child depression prevention programs carried out in the school context. They are all cognitive-behavioral programs implemented either by psychologists or teachers with specialist training, consisting of between 8 and 15 sessions. Only a few universal programs designed to prevent the symptoms of depression focus on younger children, since most are targeted mainly at the adolescent population (Gillham et al., 1995 ; Barrett and Turner, 2001 ; Farrell and Barrett, 2007 ; Essau et al., 2012 ; Gallegos et al., 2013 ; Rooney et al., 2013 ). Indeed, in the present review, only four universal child depression prevention programs were found that were aimed at a younger age group (between 8 and 12): the Penn Resiliency Program, FRIENDS, the Aussie Optimism Program, and FORTIUS (see Table 5 ).
As shown in the table, the results of the various programs outlined are not particularly positive, since on many occasions the effects (if there are any) are not sustained over time or are limited in scope (being dependent on who applies the program or on the sex of the participant, etc.). Nor is the distinction between universal and targeted programs particularly clear as regards their effects, since although targeted programs may initially appear to be more effective, their impact is not found to be sustained in the long term.
Greenberg et al. ( 2001 ) argue that researchers should explain whether their prevention programs focus on one or various microsystems (basically family and school), mesosystems or exosystems, etc. (following the model described by Bronfenbrenner, 1979 ), or are centered exclusively on the individual and his or her environment, since this will influence the results reported. These same authors conclude that programs focused exclusively on children and adolescents themselves are less effective than those which aim to “educate” subjects and bring about positive changes in their family and school environments.
As Calear and Christensen ( 2010 ) point out in their review, some authors suggest that the fact that some targeted programs are aimed at people with high levels of depressive symptoms entails a broader range of possibilities for change; however, this does not help us understand why these changes are not sustained over time. Thus, further research is required in this field in order to identify what specific components of those programs observed to be effective actually have a positive impact on the level of depressive symptoms, how these programs are developed, who implements them and whether or not their effects are sustained in the short, medium, and long term.
Clinical Treatments for Depression
In order to draft this section, a search was conducted for the most commonly-used therapies with proven efficacy for treating depression. The databases used were PubMed, Web of Science, Science direct, and Google Scholar. The key words used in the search were treatment, depression, child depression, and adolescent depression. A total of 30 bibliographic references were used in the drafting of this summary, including the major contribution made by The American Psychological Association's Society of Clinical Psychology (American Psychological Association, Society of Clinical Psychology (APA), 2017 ) regarding the most effective psychological methods for treating depression.
Although the World Health Organization (WHO) ( 2017 ) claims that prevention programs reduce the risk of suffering from depression, it has yet to be ascertained what type of programs and what contents are the most effective. The WHO also states that there are effective treatments for moderate and severe depression, such as psychological treatments (behavioral activation, cognitive behavioral therapy, and interpersonal psychotherapy) and antidepressant drugs (although it also warns of adverse effects), as well as psychosocial treatments for cases of mild depression. Moreover, a study conducted with adolescents by Foster and Mohler-Kuo ( 2018 ) found that the combination of cognitive-behavioral therapy and fluoxetine (antidepressant drug) was more effective than drug therapy alone.
The efficacy of treatment with antidepressants has been called into question for some years now. Iruela et al. ( 2009 ) claim that tricyclic antidepressants (imipramine, clomipramine, amitriptyline) are not recommended in childhood and adolescence since no benefits other than the placebo effect have been proven and furthermore, they generate major side effects due to their cardiotoxicity. They are therefore particularly dangerous in cases of attempted suicide. These same authors also advise against the use of monoamine oxidase inhibitors (MAOIs) due to dietary restrictions, interactions with other medication and the lack of clinical trials with sufficiently large groups which guarantee their efficacy. SSRIs or serotonergic antidepressants are the ones that have been most extensively studied in this population. The most effective is fluoxetine, the use of which is recommended in association with cognitive psychotherapy for cases of moderate and severe child depression.
On another hand, Wagner and Ambrosini ( 2001 ) analyzed the efficacy of pharmacological treatment in children and adolescents and stated that, at best, antidepressant therapy for depressed youth was moderately effective. Peiró et al. ( 2005 ) indicate that there is a great debate about the safety of selective serotonin reuptake inhibitors (SSRIs) in childhood. SSRIs, except for fluoxetine in the United States, have never been authorized by any agency for use in children or adolescents, mainly because of the risk of suicide to which they are associated. In 1991, the Food and Drugs Administration (FDA) claimed that there was insufficient evidence to confirm a causal association between SSRIs and suicide. Vitiello and Ordoñez ( 2016 ) conducted a systematic review of the topic and found more than 30 controlled clinical trials in adolescents and a few studies with children. Most studies found no differences between studies that administered drugs and those that used placebo, but they did find fluoxetine to be effective. They noted that antidepressants increased the risk of suicide (suicidal ideation and behaviors) compared to studies that had used placebos. The authors recommend using antidepressants with caution in young people and limiting them to patients with moderate to severe depression, especially when psychosocial interventions are not effective or are not feasible.
As regards the effectiveness of psychodynamic treatments, Luyten and Blatt ( 2012 ) advocate the inclusion of psychoanalytic therapy in the treatment of child, adolescent and adult depression. After conducting a review of both the theoretical assumptions of psychodynamic treatments of depression and the evidence supporting the efficacy of these interventions, these authors concluded that brief psychoanalytic therapy (BPT) is as effective in treating depression as other active psychotherapeutic treatments or pharmacotherapy, and its effects tend to be maintained in the longer term. They also observed that the combination of BPT and medication obtained better results than medication alone. Longer-term psychoanalytic treatment (LTPT) was found to be effective for patients suffering from chronic depression and co-morbid personality problems. Together, the authors argue, these findings justify the inclusion of psychoanalytic therapy as a first-line treatment in adult, child, and adolescent depression.
In a qualitative study carried out by Brown ( 2018 ) on parents' expectations regarding the recovery of their depressed children, a direct relationship was observed between said expectations and type of attachment. Parents who remained more passive and expected expert helpers to fix their child experienced reduced hope months after finishing the program. However, when parents changed their interactions with their child and adopted more positive expectations regarding their cure, they felt a more sustained sense of hope. Moreover, when parents themselves participated in therapy sessions, as part of their child's treatment, they felt greater hope and effectiveness in contributing to their child's recovery.
The American Psychological Association's Society of Clinical Psychology [American Psychological Association, Society of Clinical Psychology (APA), 2017 ] has published a list of psychological treatments that have been tested with the most scientific rigor and which, moreover, have been found to be most effective in treating depression. These treatments are as follows:
- – Self-Management/Self-Control Therapy (Kanfer, 1970 ). Depression is due to selective attention to negative events and immediate consequences of events, inaccurate attributions of responsibility for events, insufficient self-reinforcement, and excessive self-punishment. During therapy, the patient is provided with information about depression and taught skills they can use in their everyday life. This 10-session program can be delivered either in group or individual formats, at any age.
- – Cognitive Therapy (Beck, 1987 ). Individuals suffering from depression are taught cognitive and behavioral skills to help them develop more positive beliefs about themselves, others, and the world. Méndez ( 1998 ) argues that therapists working with depressed children should pursue three changes: (1) Learn to value their own feelings; (2) Replace behaviors which generate negative feelings with more appropriate behaviors; and (3) Modify distorted thoughts and inaccurate reasoning. The number of sessions varies between 8 and 16 in patients with mild symptoms. Those with more severe symptoms show improvement after 16 sessions.
- – Interpersonal Therapy (Klerman et al., 1984 ). García and Palazón ( 2010 ) identified four typical focal points for tension in depression, related to loss (complicated mourning), conflicts (interpersonal disputes), change (life transitions), and deficits in relations with others (interpersonal deficits), which generate and maintain a depressive state. It uses certain behavioral strategies such as problem solving and social skills training and lasts between 12 and 16 sessions in the most severe cases, and between 3 and 8 sessions in milder cases.
- – Cognitive Behavioral Analysis System of Psychotherapy (McCullough, 2000 ). This therapy combines components of cognitive, behavioral, interpersonal, and psychodynamic therapies. According to McCullough ( 2003 ), it is the only therapy developed specifically to treat chronic depression. Patients undergoing this therapy generate more empathic behaviors and identify, change and heal interpersonal patterns related to depression. Patients are recommended to combine the therapy with a regime of antidepressant medication.
- – Behavior Therapy/Behavioral Activation (BA) (Martell et al., 2013 ). Depression prompts sufferers to disengage from their routines and become increasingly isolated. Over time, this isolation exacerbates their depressive symptoms. Depressed individuals lose opportunities to be positively reinforced through pleasant experiences or social activities. The therapy aims to increase patients' chances of being positively reinforced by increasing their activity levels and improving their social relations. The therapy usually lasts between 20 and 24 sessions, with the brief version consisting of between 8 and 15 sessions.
- – Problem-Solving Therapy (Nezu et al., 2013 ). The aim is to enhance patients' personal adjustment to their problems and stress using affective, cognitive, and behavioral strategies. The therapy usually comprises around 12 sessions, although substantial changes are generally observed from the fourth session onwards. This therapy is widely used in primary care. It is an adaptation that is easy to apply in general medicine by personnel working in those contexts, and can be completed in around 6 weeks (Areán, 2000 ).
The treatments that, according to the American Psychological Association, Society of Clinical Psychology (APA) ( 2017 ), have modest research support and could be used with children are as follows:
- – Rational Emotive Behavioral Therapy (Ellis, 1994 ). This short-term, present-focused therapy works on changing the thinking which contributes to emotional and behavioral problems using an active-directive, philosophical and empirical intervention model. Using the A-B-C model (A: events observed by the individual; B: Individual's interpretation of the observed event; C: Emotional consequences of the interpretations made), the aim is to bring about the cognitive restructuring of erroneous thoughts, so as to replace them with more rational ones. The most commonly used techniques are cognitive, behavioral, and emotional.
- – Self-System Therapy (Higgins, 1997 ). Depression occurs as the result of the individual's chronic failure to achieve their established goals. During therapy, patients review their situation, analyze their beliefs and, on the basis of the results, alter their regulation style and move toward a new vision of themselves. Therapy generally consists of between 20 and 25 sessions.
- – Short-Term Psychodynamic Therapy (Hilsenroth et al., 2003 ). The aim of this therapy is to help patients understand that past experiences influence current functioning, and to analyze affect and the expression of emotion. The therapy focuses on the therapeutic relationship, the facilitation of insight, the avoidance of uncomfortable topics and the identification of core conflictual relationship themes. It is usually combined with pharmacological treatment to alleviate depressive episodes.
- – Emotion-Focused Therapy (emotion regulation therapy or Greenberg's experiential therapy) (Greenberg, 2004 ). According to Greenberg et al. ( 2015 ), this therapy combines elements of client-based practices (Rogers, 1961 ), Gestalt therapy (Perls et al., 1951 ), the theory of emotions and a dialectic-constructivist meta-theory. The aim is to create a safe environment in which the individual's anxiety is reduced, thereby enabling them to confront difficult emotions, raising their awareness of said emotions, exploring their emotional experiences in more depth and identifying maladaptive emotional responses. The therapy is delivered in 8–20 sessions.
- – Acceptance and Commitment Therapy (Hayes, 2005 ). This theory has become increasingly popular over recent years and is the contextual or third-generation therapy that is supported by the largest body of empirical evidence. It is based on a realization of the importance of human language in experience and behavior and aims to change the relationship individuals have with depression and their own thoughts, feelings, memories, and physical sensations that are feared or avoided. Strategies are used to teach patients to decrease avoidance and negative cognitions, and to increase focus on the present. The aim is not to modify the content of the patient's thoughts, but rather to teach them how to change the way they analyze them, since any attempt to correct thoughts may, paradoxically, only serve to intensify them (Hayes, 2005 ).
Ferdon and Kaslow ( 2008 ), for their part, in a theoretical review of the treatment of depression in children and adolescents, concluded that the cognitive-behavioral-therapy-based specific programs of the Penn Prevention program meet the criteria to conduct effective interventions in children with depression. In adolescent depression, the cognitive-behavioral therapy and the Interpersonal Therapy–Adolescent seem to have a well-established efficacy. Weersing et al. ( 2017 ), in this same line, state that, although the efficacy of treatments in children is rather weak, cognitive-behavioral therapy is probably the most effective therapy. They also confirm that, in depressed adolescents, cognitive behavioral therapy, and interpersonal psychotherapy are appropriate interventions.
There are other studies also which focus on treatments for depression in childhood. For example, Crowe and McKay ( 2017 ) carried out a meta-analysis of the effects of Cognitive Behavioral Therapy (CBT) on children suffering from anxiety and depression, concluding that CBT can be considered an effective treatment for child depression. According to these authors, the majority of protocols for children have been adapted from protocols for adults, and the most common techniques are psychoeducation, self-monitoring, identification of emotions, problem solving, coping skills, and reward plans. Similarly, cognitive strategies include the identification of cognitive errors, also known as cognitive restructuring. In another meta-analysis conducted to analyze the efficacy and acceptability of CBT in cases of child depression, Yang et al. ( 2017 ) observed that, in comparison with the control groups that did not receive treatment, the experimental groups showed significant improvement, although they also pointed out that the relevance of this finding was limited due to the small size of the trial groups.
Another study carried out in Saudi Arabia concluded that student counseling in schools may help combat and directly reduce anxiety and depression levels among Saudi children and adolescents (Alotaibi, 2015 ).
Family-based treatment may also be effective in treating the interpersonal problems and symptoms observed among depressed children. The data indicate that the characteristics of the family environment predict recovery from persistent depression among depressed children (Tompson et al., 2016 ). In this sense, Tompson et al. ( 2017 ) compared the effects of a family-focused treatment for child depression (TCF-DI) with those of individual supportive psychotherapy among children aged 7–14 with depressive disorders. The results revealed that incorporating the family into the therapy resulted in a significant improvement in depressive symptoms, global response, functioning, and social adjustment.
To conclude this section, it can be stated that treatment for depression should be multifactorial and should bear in mind the personal characteristics of the patient, their coping strategy for problems, the type of relationship they have with themselves and the type of relationship they establish with their environment (friends, school, family, etc.). Thus, in order for the individual to attain the highest possible level of psychological wellbeing, attention should focus on both these and other related aspects.
Conclusions
The present review aims to shed some light on the complex and broad-ranging field of child and adolescent depression, starting with a review of the construct itself and its explanatory theories, before continuing on to analyze existing evaluation instruments, the main prevention programs currently being implemented and the various treatments currently being applied. All these aspects are intrinsically linked: how the concept is defined depends on the explanatory variables upon which said definition is based, and this in turn influences how we measure it and the variables we define as being key elements for its prevention and treatment.
It is interesting to note the low level of specificity of both the construct itself and the explanatory theories offered by child and adolescent psychology, which suggest that child depression can be understood on the basis of the adult version of the pathology. This may well be a basic error in our approach to depression among younger age groups. The fact that universal prevention programs specifically designed for children are obtaining only modest results may indicate that we have perhaps failed to correctly identify the key variables involved in the genesis and maintenance of child and adolescent depression.
The review of current child and adolescent depression prevention programs revealed that the vast majority coincide in adopting a cognitive-behavioral approach, with contents including social skills and problem solving training, emotional education, cognitive restructuring, and strategies for coping with anxiety. These contents are probably included because they are important elements in the treatment of depression, as shown in this review. But if their inclusion is important and effective in the treatment of depression, why do they not seem to be so effective in preventing this pathology? There are probably many factors linked to prevention programs which, in one way or another, influence their efficacy: who implements the program and what prior training they receive; the characteristics of the target group; group dynamics; how sessions are run; how the program is evaluated; and if the proposed goals are really attained (e.g., training in social skills may be key, but perhaps we are not training students correctly). Moreover, in universal prevention programs carried out in schools, the intervention focuses on students themselves rather than adopting a more holistic approach, as recommended by certain authors such as Greenberg et al. ( 2001 ). But, if we accept that depression is multifactorial and that risk and protection factors may be found not only in the school environment but also in the family and social contexts, should prevention not also be multifactorial?
There is therefore still much work to be done in order to fully understand child and adolescent depression and its causes, and so design more effective evaluation instruments and prevention and treatment programs. Given the important social and health implications of this disorder, we need to make a concerted effort to further our research in this field.
Author Contributions
MG designed the study and wrote the protocol. EB and JJ conducted literature review and provided summaries of previous research studies, and wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Funding. The Research Project was sponsored by the Alicia Koplowitz Foundation, with grant number FP15/62.
- Abramson L. Y., Seligman M. E. P., Teasdale J. D. (1978). Learned helplessness in humans: critique and reformulation . J. Abnorm. Psychol. 87 , 49–74. 10.1037/0021-843X.87.1.49 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Accardo J., Marcus C. L., Leonard M. B., Shults J., Meltzer L. J., Elia J. (2012). Associations between psychiatric comorbidities and sleep disturbances in children with attention-deficit/hyperactivity disorder . J. Dev. Behav. Pediatr. 33 , 97–105. 10.1097/DBP.0b013e31823f6853 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Achenbach T. M., Edelbrock C. S. (1985). Manual for the Child Behavior Checklist and Revised Child Behavior Profile . Burlington, VT: University Associates in Psychiatry. [ Google Scholar ]
- Ainsworth M., Blehar M., Waters E., Wall S. (1978). Patterns of Attachment . Hillsdale, NJ: Erlbaum. [ Google Scholar ]
- Allen J. P., Porter M., McFarland C., McElhaney K. B., Marsh P. (2007). The relation of attachment security to adolescents' paternal and peer relationships, depression, and externalizing behavior . Child Dev. 78 , 1222–1239. 10.1111/j.1467-8624.2007.01062.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Alotaibi T. (2015). Combating anxiety and depression among school children and adolescents through student counselling in Saudi Arabia . Proc. Soc. Behav. Sci. 205 , 18–29. 10.1016/j.sbspro.2015.09.006 [ CrossRef ] [ Google Scholar ]
- American Psychiatric Association (2014). Manual Diagnóstico y Estad í stico de los Trastornos Mentales (DSM-5) [Diagnostic and Statistical Manual of Mental Disorders (DSM − 5)] Madrid: Médica Panamericana. [ Google Scholar ]
- American Psychological Association Society of Clinical Psychology (APA). (2017). Depression . Available online at: http://www.div12.org/psychological-treatments/disorders/depression/
- Angold A., Costello E. J. (1995). A test-retest reliability study of child-reported psychiatric symptoms and diagnoses using the Child and Adolescent Psychiatric Assessment (CAPA-C) . Psychol. Med. 25 , 755–762. [ PubMed ] [ Google Scholar ]
- Angold A., Costello E. J., Messer S. C., Pickles A., Winder F., Silver D. (1995). The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents . Int. J. Methods Psychiatr. Res. 5 , 237–249. [ Google Scholar ]
- Antonuccio D. O., Ward C. H., Tearnan B. H. (1989). The behavioral treatment of unipolar depression in adult outpatients , in Progress in Behavior Modification , eds Hersen M., Eisler R. M., Miller P. M. (Newbury Park, CA: Sage; ), 152–191. [ PubMed ] [ Google Scholar ]
- Areán P. A. (2000). Terapia de solución de problemas para la depresión: teoría, investigación y aplicaciones [Therapy for the solution of depression problems: theory, research and implementations] . Psicol. Conduct. 8 , 547–559. [ Google Scholar ]
- Armsden G., McCauley E., Greenberg M., Burke E., Mitchell J. (1990). Parent and peer attachment in early adolescent depression . J. Abnorm. Child Psychol. 18 , 683–698. 10.1007/BF01342754 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bandura A. (1977). Social learning theory of aggression . J. Commun. 8 , 12–29. [ PubMed ] [ Google Scholar ]
- Barber B. K., Stolz H. E., Olsen J. A. (2005). Parental support, psychological control, and behavioral control: assessing relevance across time, culture, and method . Monogr. Soc. Res. Child Dev. 70 , 1–137. 10.1111/j.1540-5834.2005.00365.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barrett P., Turner C. (2001). Prevention of anxiety symptoms in primary school children: preliminary results from a universal school-based trial . Br. J. Clin. Psychol. 40 , 399–410. 10.1348/014466501163887 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bath H. J., Middleton M. R. (1985). The Children's Depression Scale: psychometric properties and factor structure . Aust. J. Psychol. 37 , 81–88. [ Google Scholar ]
- Beck A. T. (1967). Depression: Clinical, Experimental and Theoretical Aspects . New York, NY: Hoeber. [ Google Scholar ]
- Beck A. T. (1987). Cognitive models of depression . J. Cogn. Psychother. 1 , 5–37. [ Google Scholar ]
- Beck A. T., Alford B. A. (2009). Depression: Causes and Treatment, 2nd Edn . Philadelphia, PA: University of Pennsylbania Press. [ Google Scholar ]
- Beck A. T., Beamesderfer A. (1974). Assessment of depression: the depression inventory , in Psychological Measurements in Psychopharmacology , eds Pichot P., Olivier-Martin R. (Oxford: Karger Publishers; ). 10.1159/000395074 [ CrossRef ] [ Google Scholar ]
- Beck A. T., Epstein N., Harrison R. (1983). Cognitions, attitudes and personality dimensions in depression . Br. J. Cogn. Psychother. 1 , 1–16. [ Google Scholar ]
- Beck A. T., Rush A. J., Shaw B. F., Emery G. (1979). Cognitive therapy of depression . Aust. N.Z. J. Psychiatry 36 , 272–275. [ Google Scholar ]
- Beck A. T., Steer R. A., Brown G. K. (1996). Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation. [ Google Scholar ]
- Beck J. S., Beck A. T., Jolly J. B., Steer R. A. (2005). The Beck Youth Inventories, 2nd Edn. San Antonio, TX: Psychological Corporation. [ Google Scholar ]
- Beeghly M., Partridge T., Tronick E., Muzik M., Mashhadi M. R., Boeve J., et al.. (2017). Associations between early maternal depressive symptom trajectories and toddlers' felt security at 18 months: are boys and girls at differential risk? Infant Ment. Health J. 38 , 53–67. 10.1002/imhj.21617 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bernaras E., Jaureguizar J., Soroa M., Ibabe I., de las Cuevas M. C. (2013). Evaluación de la sintomatología depresiva en el contexto escolar y variables asociadas [Evaluation of depressive symptomatology and the related variables in the school context] . Anal. Psicol. 29 , 131–140. 10.6018/analesps.29.1.137831 [ CrossRef ] [ Google Scholar ]
- Bigelow A. E., Beebe B., Power M., Stafford A. L., Ewing J., Egleson A., et al.. (2018). Longitudinal relations among maternal depressive symptoms, maternal mind-mindedness, and infant attachment behavior . Infant Behav. Dev. 51 , 33–44. 10.1016/j.infbeh.2018.02.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birleson P. (1981). The validity of depressive disorder in childhood and the development of a self-rating scale: a research report . J. Child Psychol. Psychiatry 22 , 73–88. 10.1111/j.1469-7610.1981.tb00533.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birleson P., Hudson I., Grey-Buchanan D., Wolff S. (1987). Clinical evaluation of a self-rating scale for depressive disorder in childhood (Depression Self-Rating Scale) . J. Child Psychol. Psychiatry 28 , 43–60. 10.1111/j.1469-7610.1987.tb00651.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Birmaher B., Ryan N. D., Williamson D. E., Brent D. A., Kaufman J., Dahl R. E., et al. (1996). Childhood and adolescent depression: a review of the past 10 years. Part I . J. Am. Acad. Child Adolesc. Psychiatry 5 , 1427–1439. 10.1097/00004583-199611000-00011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Blatt S. J. (2004). Experiences of Depression: Theoretical, Clinical, and Research Perspectives . Washington, DC: American Psychological Association; 10.1037/10749-000 [ CrossRef ] [ Google Scholar ]
- Bowlby J. (1969). Attachment and Loss: Attachment . New York, NY: Basic Books. [ Google Scholar ]
- Bowlby J. (1973). Attachment and Loss: Separation, Anxiety, and Anger . New York, NY: Basic Books. [ Google Scholar ]
- Bowlby J. (1976). Attachment and Loss (II). La Separación Afectiva . Buenos Aires: Paidós. [ Google Scholar ]
- Bowlby J. (1988). Developmental psychiatry comes of age . Am. J. Psychiatry 145 , 1–10. 10.1176/ajp.145.1.1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Branchi I. (2011). The double edged sword of neural plasticity: increasing serotonin levels leads to both greater vulnerability to depression and improved capacity to recover . Psychoneuroendocrinology 36 , 339–351. 10.1016/j.psyneuen.2010.08.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bravo M., Ribera J., Rubio-Stipec M., Canino G., Shrout P., Ramírez R., et al.. (2001). Test retest reliability of the Spanish version of the Diagnostic Interview Schedule for Children (DISC IV) . J. Abnorm. Child Psychol. 29 , 433–444. 10.1023/A:1010499520090 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brazelton T. B., Tronick E., Adamson L., Als H., Wise S. (1975). Early mother-infant reciprocity . Ciba Found. Symp. 33 , 137–154. 10.1002/9780470720158.ch9 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brent D. A., Perper J. A., Moritz G., Allman C., Schweers J., Roth C., et al.. (1993). Psychiatric sequelae to the loss of an adolescent peer to suicide . J. Am. Acad. Child Adolesc. Psychiatry 32 , 509–517. 10.1097/00004583-199305000-00004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bronfenbrenner U. (1979). The Ecology of Human Development: Experiments by Nature and Design. Cambridge, MA: Harvard University Press. [ Google Scholar ]
- Brooks S. J., Krulewicz S. P., Kutcher S. (2003). The Kutcher Adolescent Depression Scale: assessment of its evaluative properties over the course of an 8-week pediatric pharmacotherapy trial . J. Child Adolesc. Psychopharmacol. 13 , 337–349. 10.1089/104454603322572679 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brown J. (2018). Parents' experiences of their adolescent's mental health treatment: helplessness or agency-based hope . Clin. Child Psychol. Psychiatry 23 , 644–662. 10.1177/1359104518778330 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Calear A. L., Christensen H. (2010). Systematic review of school-based prevention and early intervention programs for depression . J. Adolesc. 33 , 429–438. 10.1016/j.adolescence.2009.07.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cardemil E. V., Reivich K. J., Beevers C. G., Seligman M. E. P., James J. (2007). The prevention of depressive symptoms in low-income, minority children: two year follow-up . Behav. Res. Ther. 45 , 313–327. 10.1016/j.brat.2006.03.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Caspi A., Hariri A. R., Holmes A., Uher R., Moffitt T. E. (2010). Genetic sensitivity to the environment: the case of the serotonin transporter gene and its implications for studying complex diseases and traits . Am. J. Psychiatry 167 , 509–527. 10.1176/appi.ajp.2010.09101452 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Casullo M. M. (2001). Depresión y suicidio en la adolescencia [Depression and suicide in adolescence] , in Detección y Prevención en el Aula de Los Problemas del Adolescente [Detection and Prevention of Adolescent's Problems in the Classroom] , ed C. Saldaña (Madrid: Pirámide; ), 83–99. [ Google Scholar ]
- Chang S. S., Stuckler D., Yip P., Gunnel D. (2013). Impact of 2008 global economic crisis on suicide: time trend study in 54 countries . BMJ 347 , 1–16. 10.1136/bmj.f5239 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chaplin T. M., Gillham J. E., Reivich K., Elkon A. G. L., Samuels B., Freres D. R., et al.. (2006). Depression prevention for early adolescent girls: a pilot study of all girls versus co-ed groups . J. Early Adolesc. 26 , 110–126. 10.1177/0272431605282655 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chorot P., Valiente R. M., Magaz A. M., Santed M. A., Sadin B. (2017). Perceived parental child rearing and attachment as predictors of anxiety and depressive disorder symptoms in children: the mediational role of attachment . Psychiatry Res. 253 , 287–295. 10.1016/j.psychres.2017.04.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chorpita B. F., Moffitt C. E., Gray J. (2005). Psychometric properties of the Revised Child Anxiety and Depression Scale in a clinical sample . Behav. Res. Ther. 43 , 309–322. 10.1016/j.brat.2004.02.004 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Chorpita B. F., Yim L. M., Moffitt C. E., Umemoto L. A., Francis S. E. (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: a Revised Child Anxiety and Depression Scale . Behav. Res. Ther. 38 , 835–855. 10.1016/S0005-7967(99)00130-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cianchetti C., Sannio Fascello G. (2001). Scale Psichiatriche di Autosomministrazione per Fanciulli e Adolescenti (SAFA) [Psychiatric Scales of Self-Administration for Children and Adolescents] . Firenze: Organizzazioni Speciali. [ Google Scholar ]
- Clarke D. M., Currie K. C. (2009). Depression, anxiety and their relationship with chronic diseases: a review of the epidemiology, risk and treatment evidence . Med. J. Aust. 190 , 54–60. [ PubMed ] [ Google Scholar ]
- Clarke G. N., Hawkins W., Murphy M., Sheeber L. B., Lewinsohn P. M., Seeley J. R. (1995). Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: a randomized trial of a group cognitive intervention . J. Am. Acad. Child Adolesc. Psychiatry 34 , 312–321. 10.1097/00004583-199503000-00016 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Clarke G. N., Hornbrook M., Lynch F., Polen M., Gale J., Beardslee W., et al.. (2001). A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents . Arch. Gen. Psychiatry 58 , 1127–1134. 10.1001/archpsyc.58.12.1127 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cole D., Rehm L. P. (1986). Family interaction patterns and childhood depression . J. Abnorm. Child Psychol. 14 , 297–314. 10.1007/BF00915448 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Costello C. G. (1972). Depression: loss of reinforcers or loss of reinforcer effectiveness? Behav. Ther. 3 , 240–247. 10.1016/S0005-7894(72)80084-4 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Croarkin P. E., Nakonezny P. A., Husain M. M., Melton T., Buyukdura J. S., Kennard B. D., et al.. (2013). Evidence for increased glutamatergic cortical facilitation in children and adolescents with major depressive disorder . JAMA Psychiatry 70 , 291–299. 10.1001/2013.jamapsychiatry.24 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Crowe K., McKay D. (2017). Efficacy of cognitive-behavioral therapy for childhood anxiety and depression . J. Anxiety Disord. 49 , 76–87. 10.1016/j.janxdis.2017.04.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cummings E. M., Cicchetti D. (1990). Toward a transactional model of relations between attachment and depression , in The John D. and Catherine T. MacArthur Foundation Series on Mental Health and Development. Attachment in the Preschool Years: Theory, Research, and Intervention , eds Greenberg M. T., Cicchetti D., Cummings E. M. (Chicago, IL: University of Chicago Press; ), 339–372. [ Google Scholar ]
- Curley J. P., Jensen C. L., Mashoodh R., Campagne F. A. (2011). Social influences on neurobiology and behavior: epigenetic effects during development . Psychoneuroendocrinology 36 , 352–371. 10.1016/j.psyneuen.2010.06.005 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dahl R. E., Birmaher B., Williamson D. E., Dorn L., Perel J., Kaufman J., et al.. (2000). Low growth hormone response to growth hormone–releasing hormone in child depression . Biol. Psychiatry 48 , 981–988. 10.1016/S0006-3223(00)00932-X [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dean J., Keshavan M. (2017). The neurobiology of depression: an integrative view . Asian J. Psychiatr. 27 , 101–111. 10.1016/j.ajp.2017.01.025 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Del Barrio V., Carrasco M. A. (2004). Adaptación del CDI, Inventario de Depresión Infantil de Maria Kovacs . Madrid: TEA. [ Google Scholar ]
- Del Barrio V., Colondrón M. F., de Pablo C., Roa M. L. (1996). Primera adaptación española de las escalas de depresión de Reynolds RCDS y RADS a población española [First Spanish adaptation of the Reynolds depression scales RCDS and RADS to the Spanish population] . RIDEP 2 ,75–100. [ Google Scholar ]
- Demir T., Karacetin G., Demir D. E., Uysal O. (2011). Epidemiology of depression in an urban population of Turkish children and adolescents . J. Affect. Disord. 134 , 168–176. 10.1016/j.jad.2011.05.041 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Derogatis L. R., Cleary P. A. (1977). Confirmation of the dimensional structure of the SCL-90: a study in construct validation . J. Clin. Psychol. 33 , 981–989. 10.1002/1097-4679(197710)33:4<981::AID-JCLP2270330412>3.0.CO;2-0 [ CrossRef ] [ Google Scholar ]
- Domènech-Llaberia E., Polaino-Lorente A. (1990). La escala ESDM como instrumento adicional en el diagnóstico de la depresión infantil [ESDM scale as an additional instrument in the diagnosis of child-depression] . Rev. Psiquiatr. Fac. Med. Barc. 17 , 105–113. [ Google Scholar ]
- Ellis A. (1994). Reason and Emotion in Psychotherapy, Rev. Edn. Secaucus, NJ: Birch Lane. [ Google Scholar ]
- Ellis A., Harper R. A. (1961). A Guide to Rational Living. Oxford: Prentice-Hall. [ Google Scholar ]
- Essau C. A., Conradt J., Sasagawa S., Ollendick T. H. (2012). Prevention of anxiety symptoms in children: results from a universal school-based trial . Behav. Ther. 43 , 450–464. 10.1016/j.beth.2011.08.003 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Evans E., Tovee M. J., Boothroyd L. G., Drewett R. F. (2013). Body dissatisfaction and disordered eating attitudes in 7- to 11-year-old girls: testing a sociocultural model . Body Image 10 , 8–15. 10.1016/j.bodyim.2012.10.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ezpeleta L., de la Osa M., Doménech J. M., Navarro J. B., Losilla J. M. (1995). Diagnostic Interview for Children and Adolescent-DICA-R: acuerdo diagnóstico entre niños/adolescentes y sus padres [Diagnostic Interview for Children and Adolescent-DICA-R: diagnostic agreement between children/adolescents and their parents] . Rev. Psiquiatr. Fac. Med. Barc. 22 , 153–163. [ Google Scholar ]
- Farrell L. J., Barrett P. M. (2007). Prevention of childhood emotional disorders: reducing the burden of suffering associated with anxiety and depression . Child Adolesc. Ment. Health 12 , 58–65. 10.1111/j.1475-3588.2006.00430.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferdon C. D., Kaslow N. J. (2008). Evidence-based psychosocial treatments for child and adolescent depression . J. Clin. Child Adolesc. Psychol. 37 , 62–104, 10.1080/15374410701817865 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ferster C. B. (1966). Animal behavior and mental illness . Psychol. Rec. 16 , 345–356. 10.1007/BF03393678 [ CrossRef ] [ Google Scholar ]
- Figueras A., Amador J. A., Guàrdia J. (2008). Psychometric properties of the Reynolds Child Depression Scale in community and clinical samples . Span. J. Psychol. 11 , 641–649. [ PubMed ] [ Google Scholar ]
- Foley J. E., Weinraub M. (2017). Sleep, affect, and social competence from preschool to preadolescence: distinct pathways to emotional and social adjustment for boys and for girls . Front. Psychol. 8 :711. 10.3389/fpsyg.2017.00711 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Foster S., Mohler-Kuo M. (2018). Treating a broader range of depressed adolescents with combined therapy . J. Affect. Disord. 241 , 417–424. 10.1016/j.jad.2018.08.027 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frank E., Anderson B., Reynold C. F., Ritenour A., Kupfer D. J. (1994). Life events and the research diagnostic criteria endogenous subtype. A confirmation of the distinction using the Bellford College methods . Arch. Gen. Psychiatry 51 , 519–524. 10.1001/archpsyc.1994.03950070011005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Franzen P. L., Buysse D. J. (2008). Sleep disturbances and depression: risk relationships for subsequent depression and therapeutic implications . Dialogues Clin. Neurosci. 10 , 473–481. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gallegos J., Linan-Thompson S., Stark K., Ruvalcaba N. (2013). Preventing childhood anxiety and depression: testing the effectiveness of a school-based program in Mexico . Psicol. Educ. 19 , 37–44. 10.5093/ed2013a6 [ CrossRef ] [ Google Scholar ]
- Garaigordobil M., Bernaras E., Jaureguizar J., Matxinbarrena J. M. (2017). Childhood depression: relation to adaptative, clinical and predictor variables . Front. Psychol. 8 :821 10.3389/fpsyg.2017.00821 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garaigordobil M., Maganto C. (2012). SPECI: Screening de Problemas Emocionales y de Conducta Infantiles [Screening of Emotional and Behavioral Problems During Childhood]. Madrid: TEA. [ Google Scholar ]
- Garbarino S., Lanteri P., Durando P., Magnavita N., Sannita W. G. (2016). Co-morbidity, mortality, quality of life and the healthcare/welfare/social costs of disordered sleep: a rapid review . Int. J. Environ. Res. Public Health 13 :831. 10.3390/ijerph13080831 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Garber J., Clarke G. N., Robin Weersing V., Beardslee W. R., Brent D. A., Gladstone T. R. G., et al.. (2009). Prevention of depression in at-risk adolescents: a randomized controlled trial . JAMA J. Am. Med. Assoc. 301 , 2215–2224. 10.1001/jama.2009.788 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- García J., Palazón P. (2010). Afronta tu Depresión con Terapia Interpersonal [Face Your Depression with Interpersonal Therapy] . Bilbao: Desclée de Brouwer. [ Google Scholar ]
- Gillham J. E. (1994). Preventing Depressive Symptoms in School Children . Doctoral dissertation, University of Pennsylvania. [ Google Scholar ]
- Gillham J. E., Hamilton J., Freres D. R., Patton K., Gallop R. (2006). Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the Penn Resiliency Program . J. Abnorm. Child Psychol. 34 , 203–219. 10.1007/s10802-005-9014-7 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillham J. E., Jaycox L. H., Reivich K. J., Seligman M. E. P., Silver T. (1990). The Penn Resiliency Program. Unpublished manuscript, University of Pennsylvania. [ Google Scholar ]
- Gillham J. E., Reivich K. J. (1999). Prevention of depressive symptoms in school children: a research update . Psychol. Sci. 10 , 461–462. 10.1111/1467-9280.00188 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillham J. E., Reivich K. J., Freres D. R., Chaplin T. M., Shatt,é A. J., Samuels B., et al.. (2007). School-based prevention of depressive symptoms: a randomized controlled study of the effectiveness and specificity of the Penn Resiliency Program . J. Consult. Clin. Psychol. 75 , 9–19. 10.1037/0022-006X.75.1.9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gillham J. E., Reivich K. J., Jaycox L. H., Seligman M. E. P. (1995). Prevention of depressive symptoms in schoolchildren: two-year follow-up . Psychol. Sci. 6 , 343–351. 10.1111/j.1467-9280.1995.tb00524.x“ [ CrossRef ] [ Google Scholar ]
- Gladstone T. R. G., Kaslow N. J. (1995). Depression and attributions in children and adolescents: a meta-analytic review . J. Abnorm. Child Psychol. 23 , 597–606. 10.1007/BF01447664 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- González De Rivera J. L., De Las Cuevas C., Rodríguez-Abuín M. J., Rodríguez-Pulido F. (2002). El Cuestionario de 90 S í ntomas (Adaptación Española del SCL-90R de L. R. Derogatis) [THE 90 Symptoms Checklist (Spanish Adaptation of the SCL-90R of L. R. Derogatis] Madrid: TEA [ Google Scholar ]
- González J., Fernández S., Pérez E., Santamaría P. (2004). Adaptación Española del Sistema de Evaluación de la Conducta en Niños y Adolescentes: BASC [Spanish Adaptation of the Behavior Assessment System for Children]. Madrid: TEA. [ Google Scholar ]
- Greenberg L., Elliot R., Pos A. (2015). La teoría focalizada en las emociones: una visión de conjunto [The theory focused on emotions: the joint vission] . Mental. Rev. Psicoanál. Psicoter. 5 , 1–19. [ Google Scholar ]
- Greenberg L. S. (2004). Emotion-focused therapy . Clin. Psychol. Psychother. 11 , 3–16. 10.1002/cpp.388 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Greenberg M. T., Domitrovich C., Bumbarger B. (2001). The prevention of mental disorders in school-aged children: current state of the field . Prevent. Treat. 4 , 1–59. 10.1037/1522-3736.4.1.41a [ CrossRef ] [ Google Scholar ]
- Hayes S. C. (2005). Get Out of Your Mind and Into Your Life: The New Acceptance and Commitment Therapy . New York, NY: New Harbinger Publications. [ Google Scholar ]
- Heider D., Matschinger H., Bernet S., Alonso J., Angermeyer M. (2006). Relationship between parental bonding and mood disorder in six European countries . Psychiatry Res. 143 , 89–98. 10.1016/j.psychres.2005.08.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Herane-Vives A., Fischer S., de Angel V., Wise T., Cheung E., Chua K. C., et al.. (2018). Elevated fingernail cortisol levels in major depressive episodes . Psychoneuroendocrinology 88 , 17–23. 10.1016/j.psyneuen.2017.10.026 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hesse E., Main M. (2000). Disorganized infant, child, and adult attachment: collapse in behavioral and attentional strategies . J. Am. Psychoanal. Assoc. 48 , 1097–1127. 10.1177/00030651000480041101 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Higgins E. (1997). Beyond pleasure and pain . Am. Psychol. 52 , 1280–1300. 10.1037/0003-066X.52.12.1280 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hilsenroth M. J., Ackerman S. J., Blagys M. D., Baity M. R., Mooney M. A. (2003). Short-term psychodynamic psychotherapy for depression: an examination of statistical, clinically significant, and technique-specific change . J. Nerv. Mental Dis. 191 , 349–357. 10.1097/01.NMD.0000071582.11781.67 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hiroto D. S., Seligman M. E. P. (1975). Generality of learned helplessness in man . J. Pers. Soc. Psychol. 31 , 311–327. 10.1037/h0076270 [ CrossRef ] [ Google Scholar ]
- Horowitz J. L., Garber J., Ciesla J. A., Young J. F., Mufson L. (2007). Prevention of depressive symptoms in adolescents: a randomized trial of cognitive-behavioral and interpersonal prevention programs . J. Consult. Clin. Psychol. 75 :693. 10.1037/0022-006X.75.5.693 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huggins L., Davis M. C., Rooney R. M., Kane R. T. (2008). Socially prescribed and self-orientated perfectionism as predictors of depressive diagnosis in preadolescents . Aust. J. Guid. Couns. 18 , 182–194. 10.1375/ajgc.18.2.182 [ CrossRef ] [ Google Scholar ]
- Ingram R. E. (1984). Toward and information-processing analysis of depression . Cogn. Ther. Res. 8 , 443–478. 10.1007/BF01173284 [ CrossRef ] [ Google Scholar ]
- Iruela L. M., Picazo J., Peláez C. (2009). Tratamiento farmacológico de la depresión en niños y adolescentes [Pharmacological treatment of depression in children and adolescents] . Inf. Técnico Sist. Nac. Salud 33 , 35–38. [ Google Scholar ]
- Jaureguizar J., Bernaras E., Bully P., Garaigordobil M. (2018). Perceived parenting and adolescents' adjustment . Psicol. Reflex. Crítica 31 :8 10.1186/s41155-018-0088-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jaureguizar J., Bernaras E., Garaigordobil M. (2017). Child depression: prevalence and comparison between self-reports and teacher reports . Span. J. Psychol. 20 , 1–10. 10.1017/sjp.2017.14 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Jellinek M., Evans N., Knight R. B. (1979). Use of a behavior checklist on a pediatric inpatient unit . J. Pediatr. 94 , 156–158. 10.1016/S0022-3476(79)80386-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Joiner T., Coyne J. C. (1999). The Interactional Nature of Depression. Washington, DC: American Psychological Association. [ Google Scholar ]
- Ju S., Lee Y. (2018). Developmental trajectories and longitudinal mediation effects of self-esteem, peer attachment, child maltreatment and depression on early adolescents . Child Abuse Negl. 76 , 353–363. 10.1016/j.chiabu.2017.11.015 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kanfer F. H. (1970). Self-regulation: research, issues and speculations , in Behavior Modification in Clinical Psychology , eds Neuringer C., Michael J. L. (New York, NY: Appleton-Century-Crofts; ), 178–220. [ Google Scholar ]
- Kaslow N., Rehm L. P., Pollack S. L., Siegel A. W. (1988). Attributional style and self-control behavior in depressed and nondepressed children and their parents . J. Abnorm. Child Psychol. 16 , 163–175. 10.1007/BF00913592 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kaufman J., Birmaher B., Brent D., Rao U., Ryan N. (1996). The Schedule for Affective Disorders and Schizophrenia for School-Age Children. Pittsburgh, PA: University of Pittsburgh Medical Center. [ PubMed ] [ Google Scholar ]
- Kaufman J., Wymbs N. F., Montalvo-Ortiz J. L., Orr C., Albaugh M. D., Althoff R., et al.. (2018). Methylation in OTX2 and related genes, maltreatment, and depression in children . Neuropsychopharmacology 43 , 2204–2211. 10.1038/s41386-018-0157-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kenny M., Moilanen D., Lomax R., Brabeck M. (1993). Contributions of parental attachments to view of self and depressive symptoms among early adolescents . J. Early Adolesc. 13 , 408–430. 10.1177/0272431693013004004 [ CrossRef ] [ Google Scholar ]
- Kleftaras G., Didaskalou E. (2006). Incidence and teachers' perceived causation of depression in primary school children in Greece . Sch. Psychol. Int. 27 , 296–314. 10.1177/0143034306067284 [ CrossRef ] [ Google Scholar ]
- Klerman G. L., Weissman M. M., Rounsaville B. J., Chevron E. S. (1984). Interpersonal Psychotherapy of Depression . New York, NY: Basic Books. [ Google Scholar ]
- Koback R., Sudler N., Gamble W. (1991). Attachment and depressive symptoms during adolescence: a developmental pathways analysis . Dev. Psychopathol. 3 , 461–474. 10.1017/S095457940000763X [ CrossRef ] [ Google Scholar ]
- Kovacs M. (1985). The children's depression inventory (CDI) . Psychopharmacol. Bull. 21 , 995–998. [ PubMed ] [ Google Scholar ]
- Kovacs M. (1992). The Children's Depression Inventory Manual . New York, NY: Multi-Health Systems, Inc. [ Google Scholar ]
- Kowalenko N., Rapee R. M., Simmons J., Wignall A., Hoge R., Whitefield K., et al. (2005). Short-term effectiveness of a school-based early intervention program for adolescent depression . Clin. Child Psychol. Psychiatry 10 , 493–507. 10.1177/1359104505056311 [ CrossRef ] [ Google Scholar ]
- Kraus C., Castrén E., Kasper S., Lanzenberger R. (2017). Serotonin and neuroplasticity – links between molecular, functional and structural pathophysiology in depression . Neurosci. Biobehav. Rev. 77 , 317–326. 10.1016/j.neubiorev.2017.03.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Krefetz D. G., Steer R. A., Gulab N. A., Beck A. T. (2002). Convergent validity of the beck depression inventory-II with the Reynolds Adolescent Depression Scale in psychiatric inpatients . J. Pers. Assess. 78 , 451–460. 10.1207/S15327752JPA7803_05 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lang M., Tisher M. (1978). Children's Depression Scale. Camberbell, VIC: Australian Council for Educational Research. [ Google Scholar ]
- Lauth B., Arnkelsson G. B., Magnússon P., Skarphedinsson G. A., Ferrari P., Pétursson H. (2010). Validity of K-SADS-PL (Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime version) depression diagnoses in an adolescent clinical population . Nord. J. Psychiatry 64 , 409–420. 10.3109/08039481003777484 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Leblanc J. C., Almudevar A., Brooks S. J. (2002). Screening for adolescent depression: comparison of the Kutcher Adolescent Scale with the beck depression inventory . J. Child Adolesc. Psychopharmacol. 12 , 113–126. 10.1089/104454602760219153 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lemos S., Fidalgo A. M., Calvo P., Menéndez P. (1992). Estructura factorial de la prueba YSR y su utilidad en psicopatología infanto-juvenil [Factorial structure of YSR scale and its utility in child-youth psychopathology] . Anál. Modif. Conduct. 3 , 183–194. [ Google Scholar ]
- Lengua L. J., Kovacs E. A. (2005). Bidirectional associations between temperament and parenting and the prediction of adjustment problems in middle childhood . Appl. Dev. Psychol. 26 , 21–38. 10.1016/j.appdev.2004.10.001 [ CrossRef ] [ Google Scholar ]
- Lewinsohn P. M. (1974). Clinical and theoretical aspects of depression , in Innovative Treatment Methods in Psychopathology , eds Calhoun K. S., Adams H. E., Mitchel K. M. (New York, NY: Wiley; ), 63–120. [ Google Scholar ]
- Lewinsohn P. M. (1975). Clinical and theoretical aspects of depression , in Innovative Treatment Methods of Psychopathology , eds Calhoun K. S., Adams H. E., Mitchell K. M. (New York, NY: Wiley; ), 63–120. [ Google Scholar ]
- Lock S., Barrett P. M. (2003). A longitudinal study of developmental differences in universal preventive intervention for child anxiety . Behav. Change 20 , 183–199. 10.1375/bech.20.4.183.29383 [ CrossRef ] [ Google Scholar ]
- Lorenzo-Blanco E. I., Unger J. B., Baezconde-Garbatani L.A, Soto D. (2012). Acculturation, enculturation, and symptoms of depression in hispanic youth: the roles of gender, hispanic cultural values, and family functioning . J. Youth Adolesc. 41, 1350–1365. 10.1007/s10964-012-9774-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lowry-Webster H., Barrett P. M., Dadds M. R. (2001). A universal prevention trial of anxiety and depressive symptomatology in childhood: preliminary data from an Australian study . Behav. Change 18 , 36–50. 10.1375/bech.18.1.36 [ CrossRef ] [ Google Scholar ]
- Lozano L., García-Cueto E., Lozano L. M. (2007). Cuestionario Educativo Cl í nico de Ansiedad y Depresión [Educative and Clinical Questionnaire of Anxiety and Depression] Madrid: TEA Ediciones. [ Google Scholar ]
- Luciano M. (2017). Versiones provisionales del capítulo de la CIE-11 sobre trastornos mentales . Actas Españolas Psiquiatr. 45 , 79–88. [ Google Scholar ]
- Luyten P., Blatt S. J. (2012). Psychodynamic treatment of depression . Psychiatr. Clin. North Am. 35 , 111 10.1016/j.psc.2012.01.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Main M. (1996). Introduction to the special section on attachment and psychopathology. 2. Overview of the field of attachment . J. Consult. Clin. Psychol. 64 , 237–243. 10.1037/0022-006X.64.2.237 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Markowitz J. C., Weissman M. M. (1995). Interpersonal psychotherapy , in Handbook of Depression , eds Beckham E., Leber W. R. (New York, NY: Guilford; ), 376–390. [ Google Scholar ]
- Martell C. R., Dimidjian S., Herman-Dunn (2013). Behavioral Activation for Depression. A Clinician's Guide . New York, NY: Guilford. [ Google Scholar ]
- McCabe M., Ricciardelli L., Banfield S. (2011). Depressive symptoms and psychosocial functioning in preadolescent children . Depress. Res. Treat. 2011 , 1–7. 10.1155/2011/548034 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McConaughy S. H., Achenbach T. M. (1994). Manual for the Semistructured Clinical Interview for Children and Adolescents . Burlington, NJ: Department of Psychiatry; University of Vermont. [ Google Scholar ]
- McCullough J. P. (2000). Treatment for Chronic Depression: Cognitive Behavioral Analysis System of Psychotherapy (CBASP) . New York, NY: Guilford. [ Google Scholar ]
- McCullough J. P. (2003). Treatment for chronic depression using Cognitive Behavioral Analysis System of Psychotherapy (CBASP) . J. Clin. Psychol. 59 , 833–846. 10.1002/jclp.10176 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Méndez F. X. (1998). El niño que no sonr í e. Estrategias Para Superar la Tristeza y la Depresión Infantil [The Child that Does not Smile. Strategies to Face the Sadness and Child Depression] . Madrid: Pirámide. [ Google Scholar ]
- Méndez F. X., Llavona L. M., Espada J. P., Orgilés M. (2013). Programa Fortius. Fortaleza Psicológica y Prevención de las Dificultades Emocionales [Fortius Program. Psychological Strength and Prevention of Emotional Difficulties]. Madrid: Pirámide. [ Google Scholar ]
- Merry S., McDowell H., Wild C. J., Bir J., Cunliffe R. (2004). A randomized placebo-controlled trial of a school-based depression prevention program . J. Am. Acad. Child Adolesc. Psychiatry 43 , 538–547. 10.1097/00004583-200405000-00007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Miller W. R., Seligman M. E. (1975). Depression and learned helplessness in man . J. Abnorm. Psychol. 84 , 228–238. 10.1037/h0076720 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Milrod B., Markowitz J. C., Gerber A. J., Cyranowski J., Altemus M., Shapiro T., et al.. (2014). Childhood separation anxiety and the pathogenesis and treatment of adult anxiety . Am J Psychiatry 171 , 34–43. 10.1176/appi.ajp.2013.13060781. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Narbona J. (2014). Depressive phenomenology at the outset of neuropaediatric diseases . Rev. Neurol. 58 ( Suppl. 1 ), S71–S75. [ PubMed ] [ Google Scholar ]
- Nezu A. M., Nezu C. M., D'Zurilla T. J. (2013). Problem-Solving Therapy. A Treatment Manual . New York, NY: Springer Publishing Company. [ Google Scholar ]
- Nique S., Fournis G., El_Hage W., Nabhan-Abou N., Garr,é J.-B., Gohier B. (2014). Transporteur de la sérotonine, troubles ansieux et dépression: revue de la littérature . Eur. Psychiatry 29 , 544–545. 10.1016/j.eurpsy.2014.09.328 [ CrossRef ] [ Google Scholar ]
- Novati A., Hulshof H. J., Granic I., Meerlo P. (2012). Chronic partial sleep deprivation reduces brain sensitivity to glutamate N -methyl-d-aspartate receptor-mediated neurotoxicity . J. Sleep Res. 21 , 3–9. 10.1111/j.1365-2869.2011.00932.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oken B., Chamine I., Wakelan W. (2015). A systems approach to stress, stressors and resilience in humans . Behav. Brain Res. 282 , 144–154. 10.1016/j.bbr.2014.12.047 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Orenes A. M. (2015). Evaluación de la Ansiedad por Separación y Prevención Escolar de las Dificultades Emocionales [Evaluation of Separation Anxiety and School Prevention of Emotional Difficulties] . Doctoral dissertation, University of Murcia, Murcia. [ Google Scholar ]
- Pariante C. M. (2017). Why are depressed patients inflamed? A reflection on 20 years of research on depression, glucocorticoid resistance and inflammation . Eur. Neuropscychopharmacol. 27 , 554–559. 10.1016/j.euroneuro.2017.04.001 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pattison C., Lynd-Stevenson R. M. (2001). The prevention of depressive symptoms in children: The immediate and long-term outcomes of a school based program . Behav. Change 18 , 92–102. 10.1375/bech.18.2.92 [ CrossRef ] [ Google Scholar ]
- Peiró S., Cervera P., Bernal-Delgado E. (2005). Los inhibidores selectivos de la recaptación de serotonina en la depresión infantil: un “culebrón” que refleja importantes problemas de seguridad de los medicamentos [Selective inhibitors of serotonine reuptake in child depression: a “soap opera” that reflects important safety problems of medication]. Gac. Sanit . 19 . Available online at: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0213–91112005000500010 [ PubMed ]
- Perls F., Hefferline R. F., Goodman P. (1951). Gestalt Therapy . New York, NY: Dell. [ Google Scholar ]
- Peterson C., Maier S. F., Seligman M. E. (1993). Learned Helplessness. A Theory for the Age of Personal Control . New York, NY: Oxford University Press. [ Google Scholar ]
- Poznanski E. O., Cook S. C., Carroll B. J. (1979). A depression rating scale for children . Pediatrics 64 , 442–450. [ PubMed ] [ Google Scholar ]
- Puig-Antich J. (1987). Affective disorder in children and adolescents: diagnosis, validity and psychobiology , in Psychopharmacology: The Third Generation of Progress , ed Meltzer H. Y. (New York, NY: Raven Press; ), 843–860. [ Google Scholar ]
- Puura K., Tamminen T., Almqvist F., Kresanov K., Kumpulainen K., Moilanen I., et al. (1997). Should depression in young-children be diagnosed with different criteria? Eur. Child Adolesc. Psychiatry 6 , 12–19. 10.1007/BF00573635 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Quayle D., Dzuirawiec S., Roberts C., Kane R., Ebsworthy G. (2001). The effect of an optimism and lifeskills program on depressive symptoms in preadolescence . Behav. Change 18 , 194–203. 10.1375/bech.18.4.194 [ CrossRef ] [ Google Scholar ]
- Radloff L. S. (1977). A CES-D scale: a self-report depression scale for research in the general population . Appl. Psychol. Meas. 1 , 385–401. 10.1177/014662167700100306 [ CrossRef ] [ Google Scholar ]
- Reeves A., McKee M., Stuckler D. (2014). Economic suicides in the great recession in Europe and North America . Br. J. Psychiatry J. Mental Sci. 205 , 246–247. 10.1192/bjp.bp.114.144766 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rehm L. P. (1977). A self-control model of depression . Behav. Ther. 8 , 787–804. 10.1016/S0005-7894(77)80150-0 [ CrossRef ] [ Google Scholar ]
- Rehm L. P., Fuchs C. Z., Roth D. M., Kornblith S. J., Romano J. (1979). A comparison of self-control and social skills treatments of depression . Behav. Ther. 10 :4442 10.1016/S0005-7894(79)80048-9 [ CrossRef ] [ Google Scholar ]
- Reich W., Shayka J. J., Taibleson C. H. (1991). Diagnostic Interview Schedule for Children and Adolescen-DICA-R. Unpublished manuscript, Washington University, Division of Child Psychiatry. [ Google Scholar ]
- Reinecke M. A., Rogers G. M. (2001). Dysfunctional attitudes and attachment style among clinically depressed adults . Behav. Cogn. Psychother. 29 , 129–141. 10.1017/S1352465801002016 [ CrossRef ] [ Google Scholar ]
- Reinecke M. A., Simons A. (2005). Vulnerability to depression among adolescents: Implications for cognitive-behavioral treatment . Cogn. Behav. Pract. 12 , 166–176. 10.1016/S1077-7229(05)80022-7 [ CrossRef ] [ Google Scholar ]
- Reinherz H. Z., Giaconia R. M., Palus B., Silverman A. B., Frost A. K., Lefkowitz E. S. (1993). Psychosocial risks for major depression in late adolescence: a longitudinal community study . J. Am. Acad. Child Adolesc. Psychiatry 32 , 1155–1163. 10.1097/00004583-199311000-00007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reynolds C. R., Kamphaus R. W. (1992). Behavior Assessment System for Children (BASC). Circle Pines, MN: American Guidance Services. [ Google Scholar ]
- Reynolds W. M. (1987). Reynolds Adolescent Depression Scale. Professional manual. Odessa, FL: Psychological Assessment Resources. [ Google Scholar ]
- Reynolds W. M. (1989). Reynolds Child Depression Scale. Professional manual. Odessa, FL: Psychological Assessment Resources. [ Google Scholar ]
- Reynolds W. M., Anderson G., Bartell N. (1985). Measuring depression in children: a multimethod assessment investigation . J. Abnorm. Child Psychol. 13 , 513–526. 10.1007/BF00923138 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts C., Kane R., Bishop B., Matthews H., Thomson H. (2004). The prevention of depressive symptoms in rural school children: a follow-up study . Int. J. Mental Health Promot. 6 , 4–16. 10.1080/14623730.2004.9721934 [ CrossRef ] [ Google Scholar ]
- Roberts C., Kane R., Thomson H., Bishop B., Hart B. (2003a). The prevention of depressive symptoms in rural school children: a randomized controlled trial . J. Consult. Clin. Psychol. 71 , 622–628. 10.1037/0022-006X.71.3.622 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roberts C. M., Mazzucchelli T., Taylor K., Reid R. (2003). Early intervention for children with challenging behavior and developmental disabilities . Int. J. Disabil. Dev. Educ. 50 , 275–292. 10.1080/1034912032000120453 [ CrossRef ] [ Google Scholar ]
- Roberts J., Gotlib I., Kassel J. (1996). Adult attachment security and symptoms of depression: the mediating roles of dysfunctional attitudes and low self-esteem . J. Pers. Soc. Psychol. 70 , 310–320. 10.1037/0022-3514.70.2.310 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Roelofs J., Meesters C., ter Huurne M., Bamelis L., Muris P. (2006). On the links between attachment style, parental rearing behaviors, and internalizing and externalizing problems in non-clinical children . J. Child Fam. Stud. 15 , 319–332. 10.1007/s10826-006-9025-1 [ CrossRef ] [ Google Scholar ]
- Rogers C. R. (1961). On Becoming a Person: A Psychotherapists View of Psychotherapy . Boston, MA: Houghton Mifflin. [ Google Scholar ]
- Rohner R. P., Khaleque A. (2003). Reliability and validity of the parental control scale: a meta-analysis of cross-cultural and intracultural studies . J. Cross Cult. Psychol. 34 , 643–649. 10.1177/0022022103255650 [ CrossRef ] [ Google Scholar ]
- Rooney R., Hassan S., Kane R., Roberts C. M., Nesa M. (2013). Reducing depression in 9-10 year old children in low SES schools: a longitudinal universal randomized controlled trial . Behav. Res. Ther. 51 , 845–854. 10.1016/j.brat.2013.09.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rooney R., Pike L., Roberts C. (2000). The Positive Thinking Program: Prevention Manual. Unpublished manuscript, Curtin University of Technology. [ Google Scholar ]
- Rooney R., Roberts C., Kane R., Pike L., Winsor A., White J., et al. (2006). The prevention of depression in 8- to 9-year-old children: a pilot study . Aust. J. Guid. Couns. 16 , 76–90. 10.1375/ajgc.16.1.76 [ CrossRef ] [ Google Scholar ]
- Rubio-Stipec M., Bird H., Canino G., Gould M. (1990). The internal consistency and concurrent validity of a Spanish translation of the child behavior checklist . J. Abnorm. Child Psychol. 18 , 393–406. 10.1007/BF00917642 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ryan N. D., Dahl R. E., Birmaher B., Williamson D. E., Iyendar S., Nelson B., et al. (1994). Stimulatory test of growth hormone secretion in prepuberal major depression: depressed versus normal children . J. Am. Acad. Child Adolesc. Psychiatry 33 , 824–833. 10.1097/00004583-199407000-00008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandín B., Chorot P., Valiente R. M., Chorpita B. F. (2010). Development of a 30-item version of the Revised Child Anxiety and Depression Scale . Rev. Psicopatol. Psicol. Clín. 15 , 165–178. 10.5944/rppc.vol.15.num.3.2010.4095 [ CrossRef ] [ Google Scholar ]
- Sandín B., Valiente R. M., Chorot P. (2009). RCADS: evaluación de los síntomas de trastornos de ansiedad y depresión en niños y adolescentes [RCADS: evaluation of symptoms of anxiety and depression disorders in children and adolescents] . Rev. Psicopatol. Psicol. Clín. 14 , 193–206. 10.5944/rppc.vol.14.num.3.2009.4078 [ CrossRef ] [ Google Scholar ]
- Sanz J., Vázquez C. (1998). Fiabilidad, validez y datos normativos del Inventario para la Depresión de Beck [Reliability, validity and normative data of the Beck Depression Inventory] . Psicothema 10 , 303–318. [ Google Scholar ]
- Schildkraut J. J. (1965). The catecholamine hypothesis of affective disorders: a review of supporting evidence . Am. J. Psychiatr. 122 , 509–522. 10.1176/ajp.122.5.509 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Scourfield J., Rice F., Thapar A., Harold G., Martin N., McGuffin P. (2003). Depressive symptoms in children and adolescents: changing aetiological influences with development . J. Child Psychol. Psychiatry 44 , 968–976. 10.1111/1469-7610.00181 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seisdedos N. (2003). Cuestionario de Depresión para Niños [Child Depression Scale], 7th Edn. Manual. Madrid: TEA. [ Google Scholar ]
- Seligman M. E. P. (1975). Helplessness. On Depression, Development, and Death. San Francisco, CA: Freeman. [ Google Scholar ]
- Shaffer D., Fisher P., Lucas C., Dulcan M. K., Schwab-Stone M. (2000). NIMH Diagnostic Interview Schedule for Children, Version IV (NIMH DISC-IV): description, differences from previous versions and reliability of some common diagnoses . J. Am. Acad. Child Adolesc. Psychiatry 39 , 28–38. 10.1097/00004583-200001000-00014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shah F., Morgan S. B. (1996). Teachers' ratings of social competence of children with high versus low levels of depressive symptoms . J. Sch. Psychol. 34 , 337–349. [ Google Scholar ]
- Shapero B. G., Black S. K., Liu R. T., Klugman J., Bender R. E., Abramson L. Y., et al.. (2013). Stressful life events and depression symptoms: the effect of childhood emotional abuse on stress reactivity . J. Clin. Psychol. 70 , 209–223. 10.1002/jclp.22011 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shedler J., Westen D. (2004). Dimensions of personality pathology: an alternative to the five-factor model . Am. J. Psychiatry 161 , 1743–1754. 10.1176/ajp.161.10.1743 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sheffield J. K., Spence S. H., Rapee R. M., Kowalenko N., Wignall A., Davis A., et al.. (2006). Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents . J. Consult. Clin. Psychol. 74 :66. 10.1037/0022-006X.74.1.66 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Shochet I. M., Dadds M. R., Holland D., Whitefield K., Harnett P. H., Osgarby S. M. (2001). The efficacy of a universal school-based program to prevent adolescent depression . J. Clin. Child Psychol. 30 , 303–315. 10.1207/S15374424JCCP3003_3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Simons R. L., Miller M. G. (1987). Adolescent depression: assessing the impact of negative cognitions and socioenvironmental problems . Soc. Work 32 , 326–330. 10.1093/sw/32.4.326 [ CrossRef ] [ Google Scholar ]
- Sivertsen B., Harvey A., Lundrevold A. J., Hysing M. (2014). Sleep problems and depression in adolescence: results from a large population-based study of Norwegian adolescents aged 16-18 years . Eur. Child Adolesc. Psychiatry 23 , 681–689. 10.1007/s00787-013-0502-y [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Skinner B. F. (1953). Science and Human Behavior . New York, NY: Macmillan Company. [ Google Scholar ]
- Sokratous S., Merkouris A., Middeleton N., Karanikola M. (2013). The association between stressful life events and depressive symptoms among Cypriot university students: a cross-sectional descriptive correlational study . Bio. Med. Central Public Health 13 :1121. 10.1186/1471-2458-13-1121 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Soler J., Pérez-Sola V., Puigdemont D., Pérez-Blanco J., Figueres M., Álvarez E. (1997). Estudio de validación del Center for Epidemiologic Studies-Depression (CES-D) en una población española de pacientes con trastornos afectivos [A validity study of the Center for Epidemiologic Studies-Depression (CES-D) in a Spanish population of patients with affective disorders] . Actas Luso Esp. Neurol. Psiquiatr. Cien Afines 25 , 243–294. [ PubMed ] [ Google Scholar ]
- Spence S. H., Sheffield J. K., Donovan C. L. (2003). Preventing adolescent depression: an evaluation of the problem solving for life program . J. Consult. Clin. Psychol. 71 , 3–13. 10.1037/0022-006X.71.1.3 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Spence S. H., Sheffield J. K., Donovan C. L. (2005). Long-term outcome of a school-based, universal approach to prevention of depression in adolescents . J. Consult. Clin. Psychol. 73 , 160–167. 10.1037/0022-006X.73.1.160 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stockings E., Degenhardt L., Lee Y. Y., Mihalopoulos C., Liu A., Hobbs M., et al.. (2015). Symptom screening scales for detecting major depressive disorder in children and adolescents: a systematic review and meta-analysis of reliability, validity and diagnostic utility . J. Affect. Disord. 174 , 447–463. 10.1016/j.jad.2014.11.061 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thabrew H., Stasiak K., Bavin L. M., Frampton C., Merry S. (2017). Validation of the Mood and Feelings Questionnaire (MFQ) and Short Mood and Feelings Questionnaire (SMFQ) in New Zealand help-seeking adolescents . Int. J. Methods Psychiatr. Res. 27 :e1610. 10.1002/mpr.1610 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tisher M., Lang-Takac E., Lang M. (1992). The Children's Depression Scale: review of Australian and overseas experience . Aust. J. Psychol. 44,27–35. [ Google Scholar ]
- Tompson M. C., Langer D. A., Hughes J. L., Asarnow J. R. (2016). Family-focused treatment for childhood depression: model and case illustrations . Cogn. Behav. Pract. 24 , 269–287. 10.1016/j.cbpra.2016.06.003 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tompson M. C., Sugar C. A., Langer D., Asarnow J. R. (2017). A randomized clinical trial comparing family-focused treatment and individual supportive therapy for depression in childhood and early adolescence . J. Am. Acad. Child Adolesc. Psychiatry 56 , 515–523. 10.1016/j.jaac.2017.03.018 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vázquez F. L., Muñoz R. F., Becoña E. (2000). Depresión: diagnóstico, modelos teóricos y tratamiento a finales del siglo XX [Depression: diagnosis, theoretical models and treatments on the verge of 20th century] . Psicol. Conduct. 8 , 417–449. [ Google Scholar ]
- Vinaccia S., Gaviria A. M., Atehortúa L. F., Martínez P. H., Trujillo C., Quiceno J. M. (2006). Prevalencia de la depresión en niños escolarizados entre 8 y 12 años del oriente antioqueño a partir del “Child depression inventory”-CDI- [Prevalence of depression in 8-12 years-old children in east Antioquia using the “Child depression inventory”-CDI-] . Rev. Divers. Perspect. Psicol. 2 , 217–227. 10.15332/s1794-9998.2006.0002.03 [ CrossRef ] [ Google Scholar ]
- Vitiello B., Ordoñez A. E. (2016). Pharmacological treatment of children and adolescents with depression . Expert Opin. Pharmacother. 17 , 2273–2279. 10.1080/14656566.2016.1244530 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wagner K. D., Ambrosini P. J. (2001). Childhood depression: pharmacological therapy/treatment (pharmacotherapy of childhood depression) . J. Clin. Child Adolesc. Psychol. 30 , 88–97. 10.1207/S15374424JCCP3001_10 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Waterman G. S., Dahl R. E., Birmaher B., Ambrosini P., Rabinovich H., Williamson D. E., et al.. (1994). The 24-hour pattern of prolactin secretion in depressed and normal adolescents . Biol. Psychiatry 35 , 440–445. 10.1016/0006-3223(94)90041-8 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weersing V. R., Jeffreys M., Do M.-C. T., Schwartz K. T. G., Bolano C. (2017). Evidence base update of psychosocial treatments for child and adolescent depression . J. Clin. Child Adolesc. Psychol. 46 , 11–43, 10.1080/15374416.2016.1220310 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Weissman M. M., Orvaschel H., Padian N. (1980). Children's symptom and social functioning self-report scales: comparison of mothers' and children's reports . J. Nerv. Mental Disord. 168 , 736–740. [ PubMed ] [ Google Scholar ]
- Whittle S., Lichter R., Dennison M., Vijayakumar N., Schwartz O., Byrne M. L., et al.. (2014). Structural brain development and depression onset during adolescence: a prospective longitudinal study . Am. J. Psychiatry 171 , 564–571. 10.1176/appi.ajp.2013.13070920 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Williamson D. E., Birmaher B., Anderson B. P., Al-Shabbout M., Ryan N. D. (1995). Stressful life events in depressed adolescents: the role of dependent events during the depressive episode . Am. Acad. Child Adolesc. Psychiatry 33 , 591–598. 10.1097/00004583-199505000-00011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization (WHO) (2017). Depression. Fact sheet . Available online at: http://www.who.int/mediacentre/factsheets/fs369/en/
- World Health Organization (WHO) (2018). WHO Releases New International Classification of Diseases (ICD 11) . Available online at: http://www.who.int/news-room/detail/18-06-2018-who-releases-new-international-classification-of-diseases-(icd-11)
- Yang L., Zhou X., Zhou CH., Zhang Y., Pu. J, Liu L., Gong X., et al.. (2017). Efficacy and acceptability of cognitive behavioral therapy for depression in children: a systematic review and meta-analysis . Acad. Pediatr. 17 , 9–16. 10.1016/j.acap.2016.08.002 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yap M. B., Pilkington P. D., Ryan S. M., Jorm A. F. (2014). Parental factors associated with depression and anxiety in young people: a systematic review and meta-analysis . J. Affect. Disord. 156 , 8–23. 10.1016/j.jad.2013.11.007 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Young J. F., Mufson L. (2003). Manual for Interpersonal Psychotherapy-Adolescent Skills Training (IPT-AST) . New York, NY: Columbia University. [ Google Scholar ]
- Young J. F., Mufson L., Gallop R. (2010). Preventing depression: a randomized trial of interpersonal psychotherapy adolescent skills training . Depress. Anxiety 27 , 426–433. 10.1002/da.20664 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhou H., Hao N., Liu Y., Sui Y., Wang Y., Ciu Y., et al. (2016). Reliability and validity of the eleven item Kutcher Adolescent Depression Scale, Chinese Version (KADS-11CV) . J. Child Adolesc. Behav. 4 :4 10.4172/2375-4494.1000308 [ CrossRef ] [ Google Scholar ]

Depression in Children and Teens
- • Persistent feelings of sadness that interfere with the ability to function in daily life
- • Some symptoms include acting out, irritability, anger, trouble at school, fatigue, feeling worthless
- • Cognitive behavioral therapy (CBT) and antidepressant medication may be recommended
- • Involves Psychiatry, Pediatrics, Child Study Center
What is childhood depression?
How common is suicide ideation in children, what are the symptoms of childhood depression, how is depression in children treated, what makes yale medicine’s approach to treating depression and suicide ideation in children unique.
Learning to balance life’s positive experiences and emotions with the unhappy ones is an important part of growing up, but some children find this to be a struggle. An estimated 3.2 percent of American children and adolescents have diagnosed depression. And while depression was long seen as an adult problem, researchers now know that even a 2-year-old can experience depression.
As children get older, some of those who suffer from depression have thoughts of killing themselves, a condition otherwise known as suicide ideation. Such thoughts can be fleeting ideas that suicide may be a solution to a situation (such as a painful breakup), or they may be more carefully thought out plans on how to make it happen.
At Yale Medicine Child Study Center , our highly trained clinicians have extensive experience delving into the environmental contexts of child depression, including family influence. We work with families to properly diagnose an array of mental health concerns among children and treat them.
Depression may be diagnosed when a child or teen has persistent feelings of sadness that interfere with the ability to function. Loss, stress, co-occurring mental health conditions (such as ADHD or anxiety), and a family history of depression raise the odds that a child may experience depression.
In survey of students at U.S. high schools, 10 percent of boys and 22 percent of girls reported suicide ideation in the previous year, says Yann Poncin, MD , a child psychiatrist and assistant professor at the Child Study Center. He calls it “common in the context of depression.” Though many kids have these thoughts, most don’t act on them, says Dr. Poncin, but even so, the symptom should be taken seriously, he says.
Depression can look very different from one child to the next. When a provider makes a diagnosis, it’s important to focus on what’s normal for a particular child. Symptoms that may suggest depression include:
- “Acting out” behaviors, ranging from oppositional defiance to disruptiveness
- Anger or irritability
- Difficulty at school, including changes in grades or refusing to attend
- Fatigue and sleep difficulties, including trouble falling asleep, staying asleep or wanting to sleep much more than is usual
- Feelings of worthlessness, restlessness, or low self-esteem
- Loss of pleasure from friends, family, or activities the child once enjoyed
- Mood disruptions, such as mood swings or pervasive sadness that is out of proportion to a situation or that persists and overwhelms a child
- Physical complaints, such as headache; digestive complaints, including loss of appetite, and other aches and pains
Adolescents may experience the same symptoms along with others, such as:
- Preoccupation with song lyrics, books, poetry, or art that suggest that life is meaningless
- Significant change in weight, loss or gain
- Thoughts of death or suicide
Less frequently, some children and teens may show more extreme symptoms, such as:
- Paranoid delusions
- Auditory hallucinations
- Self-harming behaviors, such as cutting
Because depression treatment is always individualized, strategies are very different for a 4-year-old than they are for a 14-year-old. Typically, the best approach is psychotherapy, most often in the form of cognitive behavioral therapy (CBT), which teaches the use of new, more effective strategies to regulate their emotions, thoughts, and behaviors. Often, parents participate in the psychotherapy.
For children whose depression doesn’t respond to psychotherapy, medication can be an option. According to Laine Taylor, DO, associate medical director of the Yale New Haven Hospital Child Psychiatry Service and an expert in medication management for children, the goal with children (especially in the preschool and grade-school years) is “to use the fewest medications at the lowest effective dose.” A form of antidepressant medication called selective serotonin re-uptake inhibitors (SSRIs) is FDA-approved for use by adolescents and teens and often brings improvement.
Widely known for extensive research and expertise in mental health disorders that affect children, the Yale Medicine Child Study Center treats children with severe mental illness, including those who have experienced trauma. The knowledge and experience gained from these challenging cases contribute to broad expertise and a deep commitment to helping children move past depression and into happier, more productive lives.
Poncin says that treating “the illest of ill children” leads to deep insight into complex and sensitive issues surrounding pediatric mental health care. The Child Study Center uses highly detailed clinical guidelines, sorting out which therapeutic approach is most likely to help a particular type of depression, and understanding how to safely treat children already on other medications for co-occurring conditions.
Additionally, the Child Study Center has wide experience in developing, refining and applying a variety of evidence-based therapies. For example, if cognitive behavioral therapy proves ineffective for a child, other types of psychotherapy may be more beneficial.
The Child Study Center offers a unique combination of advanced, leading-edge science and deep insight into the environmental context of child depression, including the influence of family. “Understanding the generational components to treatment, we offer family-centered therapy combined with an understanding of how a child’s individual biology and symptomatology contribute to depression,” Dr. Poncin says.
Children and Depression
Reviewed by Psychology Today Staff
One of the sad facts of life is that mental health disorders such as depression are afflicting people at an ever-younger age. Children, even preschoolers, are not immune to depression. Evidence currently indicates that depression affects 1 to 3 percent of children before puberty. Early-onset depression is a treatable condition, and treatment is urgent for several reasons. If ignored, the early-onset depression can recur through life, and it is associated with such later problems as criminality, substance abuse, and suicidality. Depression in children warrants special attention because the disorder can interfere with the normal course of learning and development, impeding education, the establishment of relationships, and disrupting family life.
On This Page
- What does depression look like in children?
- Do children get depressed if a parent is depressed?
- Why do children get depressed?
- How is depression best treated in children?
- Are antidepressant drugs safe for children?
- Do children ever outgrow depression?
- What's the best way to help a child with depression?

One of the most common symptoms of depression in children is irritability. But children may also show symptoms more like those adults exhibit: sadness, lethargy, lack of interest in and withdrawal from activities once enjoyed, disturbed sleep patterns, feelings of worthlessness or guilt, and engaging in self-destructive behavior. That’s especially the case with teenagers. Other children may appear angry and act out frequently. Parents don’t often know when their child is depressed , and children do not always let on to parents that they are emotionally distressed; children may in fact withhold such information in an effort to protect their parents from feeling bad about having a child with a mental illness.
A family history of depression (especially in a parent) can put a child at risk for depression in several ways; there may be genetic transmission of vulnerability, but just as likely depression keeps parents from engaging with children in ways needed for neural development, a sense of security, and a sense of self. Further, depressed parents can unwittingly transmit their negative world view or negative styles of interpreting experience to their children.
Because children are dependent on their parent for most of their needs, a significant source of depression in children is persistent turbulence in the family home or severe familial adversity, such as poverty Abuse or neglect are notable adverse childhood experiences (ACEs) that can reset children’s stress response so that even minor upsets can trigger depression. The loss of a parent or beloved caregiver is another source of depression in children, just as is the loss of a significant relationship among adolescents. Bullying is a form of abuse that can give rise to depression in victims. Developmental and learning problems can severely affect children’s sense of self and pave the way for depression. The decline of free play in childhood is another contributor to depression, and it deprives children of an important source of joy. Among teenagers, there is mounting evidence that social media can have profoundly negative effects on mental health, especially among girls. Teens increasingly report they feel lonely; they spend more time communicating electronically, less time face-to-face interacting with friends.
Early detection and treatment of depression is important, because the longer depression goes untreated, the harder it is to treat. Medication is often prescribed for children with depression, but its effectiveness is very much a matter of debate, and many studies show that it is little more effective than a placebo. Moreover, the long-term effects of medication on the developing brain are unknown. On the other hand, psychotherapy of children, especially in conjunction with parents, is consistently shown to have a large and lasting effect on depressive symptoms in children. Evidence suggests that the most effective treatment for childhood depression involves some form of psychotherapy , with or without medication. The younger children are, the more important it is for them to be treated in conjunction with a parent—dyadic therapy. There is evidence that therapy specifically focused on parent-child interaction patterns can alleviate depression in children aged 3 to7—and in the parents as well. For older children, both cognitive behavioral therapy (CBT), which aims to correct the negative thinking patterns that underlie depression, and interpersonal therapy (IPT), which looks at children in the context of their relationships, have lasting therapeutic value.
Few mental health topics have inspired as much controversy as the use of antidepressant drugs in children and, arguably to a lesser extent, in teens. Antidepressant medications carry a so-called black-box warning that the drugs may increase the risk of suicidal thinking and behavior in those under age 25. What’s more, no antidepressants are approved for use in children under 8. Nevertheless, there are times when the benefits of antidepressants outweigh the risks. Antidepressants work best when their use is regularly monitored by a psychiatrist and the treated child is carefully observed by parents.
Ignoring depression or expecting it to go away on its own is never a wise policy, particularly in children. If untreated, an episode of depression lasts an average of four to eight months . That can have major effects on a child’s learning and on relationships in the family and with peers. Further, untreated or incompletely treated depression sets children up for repeated bouts of depression later in life. Among teens, whose depression may be related more to their expanding social sensitivities than among younger children, 50 percent of those who experience one episode of depression will never experience another.
Aim for fast and effective action. Both the quality of parent-child communication and the tone of the family environment are important. If there are tensions in the household, seek to address and reduce them, even if it means marital therapy for the parents, Support is crucial. Let a child know you are aware of their struggles , that they are not alone, and demonstrate willingness to listen when they want to talk. Parents can help children understand their feelings by putting names to them and distinguishing one from the other, such as sadness and loneliness; knowing what someone is feeling is a requirement for knowing what remedial steps are necessary. Parents can also help spot and bring awareness of a child to the negative self-talk that can trigger a downward emotional spiral. Going for walks or bike rides with a child has special value: It not only counters lethargy and presents opportunities for nurturing the parent-child bond , but outdoor activity is itself beneficial and involves exposure to sunlight, a natural antidepressant.

Examining the interplay between the gut microbiome, the brain, and the immune system throughout life and the role of nutrition in optimizing treatment strategies.

A Personal Perspective: Recovering from the loss of a loved one.

Symptoms, risk factors, and gender-based treatment strategies for paternal postpartum depression.

Any kind of exercise, from low to moderate to high intensity, will work wonders for your mental health and well-being.

A Personal Perspective: Let go of preconceived ideas about wellness tools and allow yourself the freedom to find what works for you, no matter how uncommon it seems.
How to overcome your past, embrace hope, and find lasting happiness.

Accurate clinical information is needed for good decision-making about suicide.

MDMA (ecstasy) and Vagus Nerve Stimulation hit road blocks on the treatment development pathway.

Veterans are more at risk of suicide than the general public due to chronic stress as well as increased incidence of TBI. Resilience models and access to services are essential.

Do you have ten minutes a day to improve your mental and emotional well-being? Various forms of meditation may suit your individual needs.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

- High contrast
- Developmental milestones
- Mini parenting master classes
Search UNICEF
What is depression, recognize signs of low mood and depression in children and learn ways to help them feel better..

- Available in:
All children feel low or down at times, it’s a natural part of growing up. But these emotions can be worrisome when felt intensely over long periods of time, particularly if they affect your child’s social, family and school life.
Although it's hard for anyone to feel optimistic when they're depressed, depression can be treated and there are things you can do to help your child feel better.
Jump to:
What is depression? What causes depression? Depression in children and adolescents Signs and symptoms of depression in kids Ways to help your child cope When to seek professional help
Depression is one of the most common types of mental health conditions and often develops alongside anxiety .
Depression can be mild and short-lived or severe and long-lasting. Some people are affected by depression only once, while others may experience it multiple times.
Depression can lead to suicide, but this is preventable when appropriate support is provided. It’s important to know that much can be done to help young people who are thinking about suicide.
What causes depression?
Depression can happen as a reaction to something like abuse, violence in school, the death of someone close or family problems like domestic violence or family breakdown. Someone might get depressed after being stressed for a long time. It can also run in the family. Sometimes we may not know why it happens.
>> Learn more about stress and effective ways to deal with it
Depression in children and adolescents
Depression can show up in children and adolescents as prolonged periods of unhappiness or irritability. It is quite common among older children and teenagers, but often goes unrecognized.
Some children might say they feel “unhappy” or “sad”. Others might say they want to hurt or even kill themselves. Children and adolescents who experience depression are at greater risk of self-harm, so such responses should always be taken seriously.
Just because a child seems sad, it doesn't necessarily mean they have depression. But if the sadness becomes persistent or interferes with normal social activities, interests, schoolwork or family life, it may mean they need support from a mental health professional.
Remember, only a doctor or a mental health professional can diagnose depression, so don’t hesitate to ask your health-care provider for advice if you are worried about your child.
> Discover: Tips and resources to support your family's mental health
Signs and symptoms of depression in kids
Depression can feel different for different children. Here are some of the common signs and symptoms of depression:
- Tiredness or low energy, even when rested
- Restlessness or difficulty concentrating
- Difficulty in carrying out daily activities
- Changes in appetite or sleep patterns
- Aches or pains that have no obvious cause
Emotional and mental:
- Persistent sadness, anxiousness or irritability
- Loss of interest in friends and activities that they normally enjoy
- Withdrawal from others and loneliness
- Feelings of worthlessness, hopelessness or guilt
- Taking risks they wouldn’t normally take
- Self-harming or suicidal thoughts
Experiencing one or more of these symptoms doesn’t mean a child is affected by depression, but there are a number of ways you can help your child cope. If you are worried about your child, do not hesitate to ask your health-care provider for advice.
Ways to help your child cope
Here are some things you can do to support your child if you think they may be depressed:
- Find out what’s happening: Ask them how they’re feeling and listen openly without judgment or advice. Ask people you trust who know your child, like a favourite teacher or close friend, to find out if they’ve noticed anything that might be worrying them or changes in their reactions to things. Pay particular attention to their well-being during important life changes like starting a new school or puberty.
- Spend time with them: Try to build an environment of warmth, reassurance and support by talking or doing age-appropriate activities together that they will enjoy. Take an interest in their life, like how their day was at school or what they love most about their friends.
- Encourage positive habits: Encourage your child to do the things they usually enjoy, stick to regular eating and sleeping habits and stay active. Physical activity is an important way to boost their mood. Music can have a strong influence on our moods, so try listening to songs together that make them feel positive about life.
- Let them express themselves: Let them talk to you. Listen carefully to what they say about how they feel. Never press your child to share, instead you can encourage other forms of creative expression like painting, crafts or journaling their thoughts and experiences. Mood-journaling can help some children let their feelings out by observing the things that make them upset or low. They can also be a great reminder of the positive aspects of their life and the things they are proud of.
- Protect them from stressful surroundings: Try to keep your child away from situations where they may experience excessive stress, maltreatment or violence. And remember to model healthy behaviour and reactions to the stresses in your own life, including setting boundaries and maintaining positive self-care habits.
When to seek professional help
As depression can only be diagnosed by a qualified expert, it's important to seek help from your health care provider who may refer your child to a mental health expert or psychiatrist. If the mental health expert thinks your child would benefit from treatment, the options might include some form of talk therapy – where they learn how to manage their thoughts and feelings, or a combination of therapy and medication.
If your child has thoughts of self-harm, or has already self-harmed, seek help from emergency services or a health-care professional. Don’t delay getting in touch if you’re worried.
Depression can be treated and the sooner you speak to an expert, the sooner your child can feel better.
Mental health and well-being
Tips and resources to help you support your child and yourself
What is anxiety?
Feelings of anxiety among children are preventable and treatable
What are panic attacks?
Understanding the triggers is the first step to helping your child overcome the condition
What is stress?
A common feeling that affects children as much as adults, just differently
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
A half century of research on childhood and adolescent depression: science mapping the literature, 1970 to 2019.

1. Introduction
2. methodology, 3.1. volume, growth trajectory, and geographic distribution of the literature, 3.2. influential journals, authors, and documents, 3.2.1. journal analysis, 3.2.2. author and co-authorship analysis, 3.2.3. citation and co-citation analysis of documents.
| Rank | Document | Topic | Citations |
|---|---|---|---|
| 1 | Kovacs, M. (1985) [ ]. The Children’s Depression Inventory (CDI) | Depression Inventory | 2432 |
| 2 | Kovacs, M. (1981) [ ]. Rating-scales to assess depression in school-aged children | Depression Inventory | 1604 |
| 3 | Lewinsohn, P.M., Hops, H., Roberts, R.E., Seeley, J.R., Andrews, J.A. (1993) [ ]. Adolescent Psychopathology. 1. Prevalence and Incidence of Depression and Other DSM-III-R Disorders in High-School-Students | Depression Prevalence | 1243 |
| 4 | Radloff, L.S. (1991) [ ]. The Use of The Center for Epidemiologic Studies Depression Scale in Adolescents and Young-Adults | Depression Inventory | 1236 |
| 5 | Chapman, D.P., Whitfield, C.L., Felitti, V.J., Dube, S.R., Edwards, V.J., Anda, R.F. (2004) [ ]. Adverse childhood experiences and the risk of depressive disorders in adulthood | Childhood Abuse and Depressive Disorders | 1153 |
| 6 | Pine, D.S., Cohen, P., Gurley, D., Brook, J. (1998) [ ]. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders | Depression Risk | 1148 |
| 7 | Angold, A., Costello, E.J., Messer, S.C., Pickles, A. (1995a) [ ]. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents | Depression Inventory | 1127 |
| 8 | Thapar, A., Collishaw, S., Pine, D.S., Thapar, A.K. (2012) [ ]. Depression in adolescence | Depression Prevalence, Risk and Prevention | 889 |
| 9 | Chorpita, B.F., Yim, L., Moffitt, C., Umemoto, L.A., Francis, S.E. (2000) [ ]. Assessment of symptoms of DSM-IV anxiety and depression in children | Depression Inventory | 876 |
| 10 | Saylor, C.F., Finch, A.J., Spirito, A., Bennett, B. (1984) [ ]. The Children’s Depression Inventory-A systematic evaluation of psychometric properties | Depression Inventory | 817 |
| 11 | Cyranowski, J.M., Frank, E., Young, E., Shear, M.K. (2000) [ ]. Adolescent onset of the gender difference in lifetime rates of major depression | Depression Prevalence | 726 |
| 12 | Emslie, G.J., Rush, A.J., Weinberg, W.A., Kowatch, R.A., Hughes, C.W., Carmody, T., Rintelmann, J. (1997) [ ]. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression | Depression Treatment | 708 |
| 13 | Whittington, C.J., Kendall, T., Fonagy, P., Cottrell, D., Cotgrove, A., Boddington, E. (2004) [ ]. Selective serotonin reuptake inhibitors in childhood depression: systematic review of published versus unpublished data | Depression Treatment | 696 |
| 14 | Nanni, V., Uher, R., Danese, A. (2012) [ ]. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression | Childhood maltreatment and Depression | 678 |
| 15 | Danese, A., Moffitt, T.E., Harrington, H., Milne, B.J., Polanczyk, G., Pariante, C.M., Poulton, R., Caspi, A. (2009) [ ]. Adverse childhood experiences and adult risk factors for age-related disease depression, inflammation, and clustering of metabolic risk markers | Adverse Childhood Experiences and Depression | 653 |
| 16 | Widom, C.S., DuMont, K., Czaja, S.J. (2007) [ ]. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up | Childhood Abuse and Depressive Disorders | 648 |
| 17 | Twenge, J.M., Nolen-Hoeksema, S. (2002) [ ]. Age, gender, race, socioeconomic status, and birth cohort differences on the Children’s Depression Inventory | Depression Inventory | 644 |
| 18 | Smucker, M.R., Craighead, W.E., Craighead, L.W., Green, B.J. (1986) [ ]. Normative and reliability data for the Children’s Depression Inventory | Depression Inventory | 621 |
| 19 | Kovacs, M., Feinberg, T.L., Crousenovak, M.A., Paulauskas, S.L., Finkelstein, R. (1984) [ ]. Depressive-disorders in childhood | Psychiatric Status and Characteristics | 585 |
| 20 | Costello, E.J., Erkanli, A., Angold, A. (2006) [ ]. Is there an epidemic of child or adolescent depression? | Depression Prevalence | 575 |
| Rank | Cited Reference | Year | Source | Paper Type | Co-Citations |
|---|---|---|---|---|---|
| 1 | Radloff, L. S. The CES-D Scale [ ]. | 1977 | Applied Psychological Measurement | Con | 1234 |
| 2 | American Psychiatric Association (APA). Diagnostic and statistical manual of mental disorders. | 1994 | Washington DC: American Psychiatric Association | --- | 715 |
| 3 | Kovacs, M., Goldston, D., Obrosky, D.S. Prevalence and predictors of pervasive noncompliance with medical-treatment among youths with insulin-dependent diabetes-mellitus [ ]. | 1992 | Journal of The American Academy of Child and Adolescent Psychiatry | Emp | 493 |
| 4 | Kaufman, J., et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children Present and Lifetime version (K-SADS-PL) [ ]. | 1997 | Journal of The American Academy of Child and Adolescent Psychiatry | Emp | 460 |
| 5 | Beck, A.T., et al. An Inventory for Measuring Depression [ ]. | 1961 | Archives of General Psychiatry | Con | 452 |
| 6 | Hankin, B.L., et al. Development of depression from preadolescence to young adulthood [ ]. | 1998 | Journal of Abnormal Psychology | Emp | 445 |
| 7 | Baron, R.M., Kenny, D.A. The moderator-mediator variable distinction in social psychological research [ ]. | 1986 | Journal of Personality and Social Psychology | Con | 443 |
| 8 | Kovacs, M. The Childrens Depression, Inventory [ ]. | 1985 | Psychopharmacology Bulletin | Con | 417 |
| 9 | Birmaher, B., et al. Childhood and adolescent depression [ ]. | 1996 | Journal of The American Academy of Child and Adolescent Psychiatry | Rev | 352 |
| 10 | Kovacs, M. Rating-scales to assess depression in school-aged children [ ]. | 1981 | Acta Paedopsychiatrica | Con | 350 |
| 11 | Hu, L.T., Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis [ ]. | 1999 | Structural Equation Modeling | Con | 346 |
| 12 | Goodman, S.H., Gotlib, I.H. Risk for psychopathology in the children of depressed mothers [ ]. | 1999 | Psychological Review | Con | 345 |
| 13 | Nolenhoeksema, S., Girgus, J.S. The Emergence of Gender Differences in Depression During Adolescence [ ]. | 1994 | Psychological Bulletin | Rev | 299 |
| 14 | Lovejoy, M.C., Graczyk, P.A., O’Hare, E., Neuman, G. Maternal depression and parenting behavior [ ]. | 2000 | Clinical Psychology Review | Rev | 290 |
| 15 | Lewinsohn, P.M., Rohde, P., Seeley, J.R., Fischer, S.A. Age-Cohort Changes in The Lifetime Occurrence of Depression and Other Mental-Disorders [ ]. | 1993 | Journal of Abnormal Psychology | Emp | 289 |
| 16 | Downey, G. and Coyne, J.C. Children of depressed parents [ ]. | 1990 | Psychological Bulletin | Rev | 287 |
| 17 | Muthen, L. K., Muthen, B. Mplus User Guide [ ]. | 1998 | --- | --- | 279 |
| 18 | West, S.G., Hepworth, J.T. Statistical Issues in The Study of Temporal Data [ ]. | 1991 | Journal of Personality | Con | 267 |
| 19 | Cox, J.L., Holden, J.M., Sagovsky, R. Detection of postnatal depression [ ]. | 1987 | British Journal of Psychiatry | Con | 263 |
| 20 | Saylor, C.F., et al. The Childrens Depression Inventory [ ]. | 1984 | Journal of Consulting and Clinical Psychology | Rev | 254 |
3.3. Research Topics
4. discussion and conclusions, author contributions, institutional review board statement, informed consent statement, data availability statement, conflicts of interest.
- Thapar, A.; Collishaw, S.; Pine, D.S.; Thapar, A.K. Depression in adolescence. Lancet 2012 , 379 , 1056–1067. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Thapar, A.; Collishaw, S.; Potter, R.; Thapar, A.K. Managing and preventing depression in adolescents. BMJ 2010 , 340 , c209. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lewinsohn, P.M.; Pettit, J.W.; Joiner, T.E.; Seeley, J.R. The symptomatic expression of major depressive disorder in adolescents and young adults. J. Abnorm. Psychol. 2003 , 112 , 244–252. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Schumacher, H.C. The depression and its effect on the mental health of the child. Am. J. Public Health Nations Health 1934 , 24 , 367–371. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Friedman, R.J.; Doyal, G.T. Depression in children—Some observations for school psychologist. Psychol. Sch. 1974 , 11 , 19–23. [ Google Scholar ]
- Connell, H.M. Depression in Childhood. Child Psychiatry Hum. Dev. 1973 , 4 , 71–85. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Poznanski, E.O.; Krahenbuhl, V.; Zrull, J.P. Childhood depression—Longitudinal perspective. J. Am. Acad. Child Adolesc. Psychiatry 1976 , 15 , 491–501. [ Google Scholar ] [ CrossRef ]
- Poznanski, E.O.; Zrull, J.P. Childhood depression-clinical characteristics of overtly depressed children. Arch. Gen. Psychiatry 1970 , 23 , 8–15. [ Google Scholar ] [ CrossRef ]
- Cytryn, L.; Mcknew, D.H. Proposed classification of childhood depression. Am. J. Psychiatry 1972 , 129 , 149–155. [ Google Scholar ] [ CrossRef ]
- Mcconville, B.J.; Boag, L.C.; Purohit, A.P. 3 types of childhood depression. Can. Psychiatr. Assoc. J. 1973 , 18 , 133–138. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Pearce, J.B. Recognition of depressive disorder in children. J. R. Soc. Med. 1978 , 71 , 494–500. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Petti, T.A. Depression in hospitalized child-psychiatry patients-approaches to measuring depression. J. Am. Acad. Child. Adolesc. Psychiatry 1978 , 17 , 5–49. [ Google Scholar ] [ CrossRef ]
- Poznanski, E.O.; Cook, S.C.; Carroll, B.J. Depression rating-scale for children. Pediatrics 1979 , 64 , 442–450. [ Google Scholar ] [ CrossRef ]
- Cantwell, D.P.; Carlson, G. Problems and prospects in the study of childhood depression. J. Nerv. Ment. Dis. 1979 , 16 , 522–529. [ Google Scholar ] [ CrossRef ]
- Goodman, S.H.; Rouse, M.H.; Connell, A.M.; Broth, M.R.; Hall, C.M.; Heyward, D. Maternal depression and child psychopathology: A meta-analytic review. Clin. Child. Fam. Psychol. Rev. 2011 , 14 , 1–27. [ Google Scholar ] [ CrossRef ]
- Nolenhoeksema, S.; Girgus, J.S. The Emergence of Gender Differences in Depression during Adolescence. Psychol. Bull. 1994 , 115 , 424–443. [ Google Scholar ] [ CrossRef ]
- Birmaher, B.; Ryan, N.D.; Williamson, D.E.; Brent, D.A.; Kaufman, J.; Dahl, R.E.; Perel, J.; Nelson, B. Childhood and adolescent depression: A review of the past 10 years. J. Am. Acad. Child. Adolesc. Psychiatry 1996 , 35 , 1427–1439. [ Google Scholar ] [ CrossRef ]
- Weisz, J.R.; McCarty, C.A.; Valeri, S.M. Effects of psychotherapy for depression in children and adolescents: A meta-analysis. Psychol. Bull. 2006 , 132 , 132–149. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Wang, Z.H.; Zhao, Y.D.; Wang, B. A bibliometric analysis of climate change adaptation based on massive research literature data. J. Clean Prod. 2018 , 199 , 1072–1082. [ Google Scholar ] [ CrossRef ]
- Hallinger, P.; Kovacevic, J. A Bibliometric Review of Research on Educational Administration: Science Mapping the Literature, 1960 to 2018. Rev. Educ. Res. 2019 , 89 , 335–369. [ Google Scholar ] [ CrossRef ]
- Shiffrin, R.M.; Börner, K. Mapping knowledge domains. Proc. Natl. Acad. Sci. USA 2004 , 101 , 5183–5185. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Chen, Y.; Liu, Z.Y.; Chen, J.; Hou, J.H. History and theory of mapping knowledge domains. Stud. Sci. Sci. 2008 , 26 , 449–460. (In Chinese) [ Google Scholar ]
- Zupic, I.; Čater, T. Bibliometric methods in management and organization. Organ. Res. Methods 2015 , 18 , 429–472. [ Google Scholar ] [ CrossRef ]
- Small, H. Co-citation in the scientific literature: A new measure of the relationship between two documents. J. Am. Soc. Inf. Sci. 1973 , 24 , 265–269. [ Google Scholar ] [ CrossRef ]
- Merton, R.K. The Sociology of Science: Theoretical and Empirical Investigations ; University of Chicago Press: Chicago, IL, USA, 1973. [ Google Scholar ]
- Gilbert, G.N. Referencing as persuasion. Soc. Stud. Sci. 1977 , 7 , 113–122. [ Google Scholar ] [ CrossRef ]
- Goncalves, M.C.P.; Kieckbusch, T.G.; Perna, R.F.; Fujimoto, J.T.; Morales, S.A.V.; Romanelli, J.P. Trends on enzyme immobilization researches based on bibliometric analysis. Process. Biochem. 2019 , 76 , 95–110. [ Google Scholar ] [ CrossRef ]
- Strotmann, A.; Zhao, D.Z. Author name disambiguation: What difference does it make in author-based citation analysis? J. Am. Soc. Inf. Sci. Technol. 2012 , 63 , 1820–1833. [ Google Scholar ] [ CrossRef ]
- Kovacs, M. Rating-scales to assess depression in school-aged children. Acta Paedopsychiatr. 1981 , 46 , 305–315. [ Google Scholar ] [ PubMed ]
- Kovacs, M. The Children’s Depression, Inventory (CDI). Psychol. Bull. 1985 , 21 , 995–998. [ Google Scholar ]
- Radloff, L.S. The Use of The Center for Epidemiologic Studies Depression Scale in Adolescents and Young-Adults. J. Youth Adolesc. 1991 , 20 , 149–166. [ Google Scholar ] [ CrossRef ]
- Saylor, C.F.; Finch, A.J.; Spirito, A.; Bennett, B. The Children’s depression inventory—A systematic evaluation of psychometric properties. J. Consult. Clin. Psychol. 1984 , 52 , 955–967. [ Google Scholar ] [ CrossRef ]
- Smucker, M.R.; Craighead, W.E.; Craighead, L.W.; Green, B.J. Normative and reliability data for the children’s depression inventory. J. Abnorm. Child. Psychol. 1986 , 14 , 25–39. [ Google Scholar ] [ CrossRef ]
- Angold, A.; Costello, E.J.; Messer, S.C.; Pickles, A.; Winder, F.; Silver, D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int. J. Methods. Psychiatr. Res. 1995 , 5 , 237–249. [ Google Scholar ]
- Chorpita, B.F.; Yim, L.; Moffitt, C.E.; Umemoto, L.A.; Francis, S.E. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behav. Res. Ther. 2000 , 38 , 835–855. [ Google Scholar ] [ CrossRef ]
- Twenge, J.M.; Nolen-Hoeksema, S. Age, gender, race, socioeconomic status, and birth cohort differences on the Children’s Depression Inventory: A meta-analysis. J. Abnorm. Psychol. 2002 , 111 , 578–588. [ Google Scholar ] [ CrossRef ]
- Chapman, D.P.; Whitfield, C.L.; Felitti, V.J.; Dube, S.R.; Edwards, V.J.; Anda, R.F. Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect. Disord. 2004 , 82 , 217–225. [ Google Scholar ] [ CrossRef ]
- Widom, C.S.; DuMont, K.; Czaja, S.J. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch. Gen. Psychiatry. 2007 , 64 , 49–56. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Danese, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Polanczyk, G.; Pariante, C.M.; Poulton, R.; Caspi, A. Adverse childhood experiences and adult risk factors for age-related disease depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatr. Adolesc. Med. 2009 , 163 , 1135–1143. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Nanni, V.; Uher, R.; Danese, A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: A meta-analysis. Am. J. Psychiatry. 2012 , 169 , 141–151. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Lewinsohn, P.M.; Hops, H.; Roberts, R.E.; Seeley, J.R.; Andrews, J.A. Adolescent Psychopathology. 1. Prevalence and Incidence of Depression and Other DSM-III-R Disorders in High-School-Students. J. Abnorm. Psychol. 1993 , 102 , 133–144. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Pine, D.S.; Cohen, P.; Gurley, D.; Brook, J. The risk for early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Arch. Gen. Psychiatry 1998 , 55 , 56–64. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Cyranowski, J.M.; Frank, E.; Young, E.; Shear, M.K. Adolescent onset of the gender difference in lifetime rates of major depression—A theoretical model. Arch. Gen. Psychiatry 2000 , 57 , 21–27. [ Google Scholar ] [ CrossRef ]
- Emslie, G.J.; Rush, A.J.; Weinberg, W.A.; Kowatch, R.A.; Hughes, C.W.; Carmody, T.; Rintelmann, J. A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Arch. Gen. Psychiatry 1997 , 54 , 1031–1037. [ Google Scholar ] [ CrossRef ]
- Whittington, C.J.; Kendall, T.; Fonagy, P.; Cottrell, D.; Cotgrove, A.; Boddington, E. Selective serotonin reuptake inhibitors in childhood depression: Systematic review of published versus unpublished data. Lancet 2004 , 363 , 1341–1345. [ Google Scholar ] [ CrossRef ]
- Kovacs, M.; Feinberg, T.L.; Crousenovak, M.A.; Paulauskas, S.L.; Finkelstein, R. Depressive-disorders in childhood.1. a longitudinal prospective-study of characteristics and recovery. Arch. Gen. Psychiatry 1984 , 41 , 229–237. [ Google Scholar ] [ CrossRef ]
- Costello, E.J.; Erkanli, A.; Angold, A. Is there an epidemic of child or adolescent depression? J. Child. Psychol. Psychiatry 2006 , 47 , 1263–1271. [ Google Scholar ] [ CrossRef ]
- Beck, A.T.; Erbaugh, J.; Ward, C.H.; Mock, J.; Mendelsohn, M. An inventory for measuring depression. Arch. Gen. Psychiatry 1961 , 4 , 561–571. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Radloff, L.S. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977 , 1 , 385–401. [ Google Scholar ] [ CrossRef ]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 1986 , 51 , 1173–1182. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Modeling 1999 , 6 , 1–55. [ Google Scholar ] [ CrossRef ]
- West, S.G.; Hepworth, J.T. Statistical Issues in The Study of Temporal Data. J. Pers. 1991 , 59 , 609–662. [ Google Scholar ] [ CrossRef ]
- Kovacs, M.; Goldston, D.; Obrosky, D.S. Prevalence and predictors of pervasive noncompliance with medical-treatment among youths with insulin-dependent diabetes-mellitus. J. Am. Acad. Child. Adolesc. Psychiatry 1992 , 31 , 1112–1119. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.M.A.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for affective disorders and schizophrenia for school-age children present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child. Adolesc. Psychiatry 1997 , 36 , 980–988. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hankin, B.L.; Abramson, L.Y.; Moffitt, T.E.; Silva, P.A.; McGee, R.; Angell, K.E. Development of depression from preadolescence to young adulthood: Emerging gender differences in a 10-year longitudinal study. J. Abnorm. Psychol. 1998 , 107 , 128–140. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Goodman, S.H.; Gotlib, I.H. Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychol. Rev. 1999 , 106 , 458–490. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lovejoy, M.C.; Graczyk, P.A.; O’Hare, E.; Neuman, G. Maternal depression and parenting behavior: A meta-analytic review. Clin. Psychol. Rev. 2000 , 20 , 561–592. [ Google Scholar ] [ CrossRef ]
- Lewinsohn, P.M.; Rohde, P.; Seeley, J.R.; Fischer, S.A. Age-Cohort Changes in The Lifetime Occurrence of Depression and Other Mental-Disorders. J. Abnorm. Psychol. 1993 , 102 , 110–120. [ Google Scholar ] [ CrossRef ]
- Downey, G.; Coyne, J.C. Children of depressed parents: An integrative review. Psychol. Bull. 1990 , 108 , 50–76. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987 , 150 , 782–786. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders , 4th ed.; Revised; American Psychiatric Association: Washington, DC, USA, 2000. [ Google Scholar ]
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders , 3rd ed.; Revised; American Psychiatric Association: Washington, DC, USA, 1987. [ Google Scholar ]
- Mohammadi, M.R.; Alavi, S.S.; Ahmadi, N.; Khaleghi, A.; Kamali, K. The prevalence, comorbidity and socio-demographic factors of depressive disorder among Iranian children and adolescents: To identify the main predictors of depression. J. Affect. Disord. 2019 , 247 , 1–10. [ Google Scholar ] [ CrossRef ]
- Sarkar, S.; Sinha, V.K.; Praharaj, S.K. Depressive disorders in school children of suburban India: An epidemiological study. Soc. Psychiatry Psychiatr. Epidemiol. 2012 , 47 , 783–788. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Demir, T.; Karacetin, G.; Demir, D.E.; Uysal, O. Epidemiology of depression in an urban population of Turkish children and adolescents. J. Affect. Disord. 2011 , 134 , 168–176. [ Google Scholar ] [ CrossRef ]
- Giannakopoulos, G.; Kazantzi, M.; Dimitrakaki, C.; Tsiantis, J.; Kolaitis, G.; Tountas, Y. Screening for children’s depression symptoms in Greece: The use of the Children’s Depression Inventory in a nation-wide school-based sample. Eur. Child. Adolesc. Psychiatry 2009 , 18 , 485–492. [ Google Scholar ] [ CrossRef ]
- Bitsko, R.H.; Holbrook, J.R.; Ghandour, R.M.; Blumberg, S.J.; Visser, S.N. Epidemiology and impact of health care provider-diagnosed anxiety and depression among US children. J. Dev. Behav. Pediatr. 2018 , 39 , 395–403. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Frigerio, A.; Pesenti, S.; Molteni, M.; Snider, J.; Battaglia, M. Depressive symptoms as measured by the CDI in a population of northern Italian children. Eur. Psychiatry 2001 , 16 , 33–37. [ Google Scholar ] [ CrossRef ]
- Wang, L.; Feng, Z.; Yang, G.; Yang, Y.; Wang, K.; Dai, Q.; Zhao, M.; Hu, C.; Zhang, R.; Liu, K.; et al. Depressive symptoms among children and adolescents in western china: An epidemiological survey of prevalence and correlates. Psychiat. Res. 2016 , 246 , 267–274. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhou, M.; Zhang, G.; Rozelle, S.; Kenny, K.; Xue, H. Depressive symptoms of Chinese children: Prevalence and correlated factors among subgroups. Int. J. Envl. Res. Pub. He. 2018 , 15 , 283. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Akimana, B.; Abbo, C.; Balagadde-Kambugu, J.; Nakimuli-Mpungu, E. Prevalence and factors associated with major depressive disorder in children and adolescents at the Uganda Cancer Institute. BMC Cancer 2019 , 19 , 466. [ Google Scholar ] [ CrossRef ]
- Sorensen, M.J.; Nissen, J.B.; Mors, O.; Thomsen, P.H. Age and gender differences in depressive symptomatology and comorbidity: An incident sample of psychiatrically admitted children. J. Affect. Disord. 2005 , 84 , 85–91. [ Google Scholar ] [ CrossRef ]
- Jaureguizar, J.; Bernaras, E.; Garaigordobil, M. Child Depression: Prevalence and comparison between self-reports and teacher reports. Span. J. Psychol. 2017 , 20 , e17. [ Google Scholar ] [ CrossRef ]
- Shooshtari, S.; Brownell, M.; Dik, N.; Chateau, D.; Yu, C.T. A population-based longitudinal study of depression in children with developmental disabilities in Manitoba. J. Ment. Health Res. Intellect. Disabil. 2014 , 7 , 191–207. [ Google Scholar ] [ CrossRef ]
- Pereira, T.S.; Silva, A.A.; Alves, M.T.; Simões, V.M.; Batista, R.F.; Rodriguez, J.D.; Figueiredo, F.P.; Lamy-Filho, F.; Barbieri, M.A.; Bettiol, H. Perinatal and early life factors associated with symptoms of depression in Brazilian children. BMC Public Health 2012 , 12 , 605. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Edelsohn, G.; Ialongo, N.; Werthamer-Larsson, L.; Crockett, L.; Kellam, S. Self-reported depressive symptoms in first-grade children: Developmentally transient phenomena? J. Am. Acad. Child. Adolesc. Psychiatry 1992 , 31 , 282–290. [ Google Scholar ] [ CrossRef ]
- Ialongo, N.; Edelsohn, G.; Werthamerlarsson, L.; Crockett, L.; Kellam, S. Are self-reported depressive symptoms in 1st-grade children developmentally transient phenomena-a further look. Dev. Psychopathol. 1993 , 5 , 433–457. [ Google Scholar ] [ CrossRef ]
- Dubois, D.L.; Felner, R.D.; Bartels, C.L.; Silverman, M.M. Stability of self-reported depressive symptoms in a community sample of children and adolescents. J. Clin. Child. Psychol. 1995 , 24 , 386–396. [ Google Scholar ] [ CrossRef ]
- Ozono, S.; Nagamitsu, S.; Matsuishi, T.; Yamashita, Y.; Ogata, A.; Suzuki, S.; Mashida, N.; Koseki, S.; Sato, H.; Ishikawa, S.; et al. Reliability and validity of the children’s depression inventory-Japanese version. Pediatr. Int. 2019 , 61 , 1159–1167. [ Google Scholar ] [ CrossRef ]
- Stahlschmidt, L.; Chorpita, B.F.; Wager, J. Validating the German version of the revised children’s anxiety and depression scale in a sample of pediatric chronic pain patients. J. Psychosom. Res. 2019 , 124 , 109786. [ Google Scholar ] [ CrossRef ]
- Balluerka, N.; Gorostiaga, A.; Haranburu, M. Validation of children’s depression scale in the basque-speaking population. Span. J. Psychol. 2012 , 15 , 1400–1410. [ Google Scholar ] [ CrossRef ]
- Speilberger, C.D. Manual for the State-Trait Anxiety Inventory for Children ; Consulting Psychologists Press: Palo Alto, CA, USA, 1973. [ Google Scholar ]
- Lang, M.; Tisher, M. Children’s Depression Scale ; Australian Council for Educational Research: Camberwell, Australia, 1978. [ Google Scholar ]
- Poznanski, E.O.; Grossman, J.A.; Buchsbaum, Y.; Banegas, M.; Freeman, L.; Gibbons, R. Preliminary studies of the reliability and validity of the children’s depression rating-scale. J. Am. Acad. Child Adolesc. Psychiatry 1984 , 23 , 191–197. [ Google Scholar ]
- Poznanski, E.O.; Freeman, L.N.; Mokros, H.B. Children’s depression rating scale-revised. Psychopharmacol. Bull. 1985 , 21 , 979–989. [ Google Scholar ]
- Lefkowitz, M.M.; Tesiny, E.P. Assessment of childhood depression. J. Consult. Clin. Psychol. 1980 , 48 , 43–50. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Weissman, M.M.; Orvaschel, H.; Padian, N. Children’s symptom and social functioning self- report scales: Comparison of mothers’ and children’s reports. J. Nerv. Ment. Dis. 1980 , 168 , 736–740. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Birleson, P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. J. Child. Psychol. Psychiatry 1981 , 22 , 73–88. [ Google Scholar ] [ CrossRef ]
- Achenbach, T.M.; Edelbrock, C.S. Behavioral-problems and competencies reported by parents of normal and disturbed-children aged 4 through 16. Monogr. Soc. Res. Child. Dev. 1981 , 46 , 1–82. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Achenbach, T.M.; Edelbrock, C.S. Manual for the Teachers Report form and the Teacher Version of the Child Behavior Profile ; University of Vermont, Department of Psychiatry: Burlington, VT, USA, 1986. [ Google Scholar ]
- Kovacs, M. Children’s Depression Inventory Manual ; Western Psychological Services: Los Angeles, CA, USA, 1992. [ Google Scholar ]
- Reynolds, C.R.; Richmond, B.O. Revised Children’s Manifest Anxiety Scale ; Western Psychological Services: Los Angeles, CA, USA, 1985. [ Google Scholar ]
- Reynolds, W.M. Reynolds Adolescent Depression Scale ; Psychological Assessment Resources: Odessa, FL, USA, 1986. [ Google Scholar ]
- Reynolds, W.M. Reynolds Child. Depression Scale. Professional Manual ; Psychological Assessment Resources: Odessa, FL, USA, 1989. [ Google Scholar ]
- Angold, A.; Prendergast, M.; Cox, A.; Harrington, R.; Simonoff, E.; Rutter, M. The Child and adolescent psychiatric-assessment (CAPA). Psychol. Med. 1995 , 25 , 739–753. [ Google Scholar ] [ CrossRef ]
- Angold, A.; Costello, E.J. The child and adolescent psychiatric assessment (CAPA). J. Am. Acad. Child. Adolesc. Psychiatry 2000 , 39 , 39–48. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Spence, S.H. Structure of anxiety symptoms among children: A confirmatory factor-analytic study. J. Abnorm. Psychol. 1997 , 106 , 280–297. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Crook, K.; Beaver, B.R.; Bell, M. Anxiety and depression in children: A preliminary examination of the utility of the PANAS-C. J. Psychopathol. Behav. Assess. 1998 , 20 , 333–350. [ Google Scholar ] [ CrossRef ]
- Reich, W. Diagnostic Interview for Children and Adolescents (DICA). J. Am. Acad. Child. Adolesc. Psychiatry 2000 , 39 , 59–66. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Shaffer, D.; Fisher, P.; Lucas, C.P.; Dulcan, M.K.; Schwab-Stone, M.E. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J. Am. Acad. Child. Adolesc. Psychiatry 2000 , 39 , 28–38. [ Google Scholar ] [ CrossRef ]
- Brooks, S.J.; Kutcher, S. Diagnosis and measurement of adolescent depression: A review of commonly utilized instruments. J. Child. Adolesc. Psychopharmacol. 2001 , 11 , 341–376. [ Google Scholar ] [ CrossRef ]
- Marien, W.E.; Bell, D.J. Anxiety- and depression-related thoughts in children: Development and evaluation of a cognition measure. J. Clin. Child. Adolesc. Psychol. 2004 , 33 , 717–730. [ Google Scholar ] [ CrossRef ]
- D’Alessandro, D.U.; Burton, K.D. Development and validation of the dysfunctional attitudes scale for children: Tests of beck’s cognitive diathesis-stress theory of depression, of its causal mediation component, and of developmental effects. Cognit. Ther. Res. 2006 , 30 , 335–353. [ Google Scholar ] [ CrossRef ]
- Singh, A.L.; D’onofrio, B.M.; Slutske, W.S.; Turkheimer, E.; Emery, R.E.; Harden, K.P.; Heath, A.C.; Madden, P.A.F.; Statham, D.J.; Martin, N.G. Parental depression and offspring psychopathology: A children of twins study. Psychol. Med. 2011 , 41 , 1385–1395. [ Google Scholar ] [ CrossRef ]
- Abela, J.R.Z.; Skitch, S.A.; Auerbach, R.P.; Adams, P. The impact of parental borderline personality disorder on vulnerability to depression in children of affectively ill parents. J. Pers. Disord. 2005 , 19 , 68–83. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Swartz, H.A.; Shear, M.K.; Wren, F.J.; Greeno, C.G.; Sales, E.; Sullivan, B.K.; Ludewig, D.P. Depression and anxiety among mothers who bring their children to a pediatric mental health clinic. Psychiatr. Serv. 2005 , 56 , 1077–1083. [ Google Scholar ] [ CrossRef ]
- Tully, E.C.; Iacono, W.G.; McGue, M. An adoption study of parental depression as an environmental liability for adolescent depression and childhood disruptive disorders. Am. J. Psychiatry 2008 , 165 , 1148–1154. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Kane, P.; Garber, J. Parental depression and child externalizing and internalizing symptoms: Unique effects of fathers’ symptoms and perceived conflict as a mediator. J. Child. Fam. Stud. 2009 , 18 , 465–472. [ Google Scholar ] [ CrossRef ]
- Weitzman, M.; Rosenthal, D.G.; Liu, Y.H. Paternal depressive symptoms and child behavioral or emotional problems in the united states. Pediatrics 2011 , 128 , 1126–1134. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Mezulis, A.H.; Hyde, J.S.; Clark, R. Father involvement moderates the effect of maternal depression during a child’s infancy on child behavior problems in kindergarten. J. Fam. Psychol. 2004 , 18 , 575–588. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Beck, C.T. Maternal depression and child behaviour problems: A meta-analysis. J. Adv. Nurs. 1999 , 29 , 623–629. [ Google Scholar ] [ CrossRef ]
- Gross, D.; Conrad, B.; Fogg, L.; Willis, L.; Garvey, C. A longitudinal-study of maternal depression and preschool children’s mental-health. Nurs. Res. 1995 , 44 , 96–101. [ Google Scholar ] [ CrossRef ]
- Turney, K. Pathways of disadvantage: Explaining the relationship between maternal depression and children’s problem behaviors. Soc. Sci. Res. 2012 , 41 , 1546–1564. [ Google Scholar ] [ CrossRef ]
- Silberg, J.L.; Maes, H.; Eaves, L.J. Genetic and environmental influences on the transmission of parental depression to children’s depression and conduct disturbance: An extended Children of Twins study. J. Child. Psychol. Psychiatry 2010 , 51 , 734–744. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Murray, L.; Cooper, P.J. The impact of postpartum depression on child development. Int. Rev. Psychiatry 1996 , 8 , 55–63. [ Google Scholar ] [ CrossRef ]
- Stein, A.; Netsi, E.; Lawrence, P.J.; Granger, C.; Kempton, C.; Craske, M.G.; Nickless, A.; Mollison, J.; Stewart, D.A.; Rapa, E.; et al. Mitigating the effect of persistent postnatal depression on child outcomes through an intervention to treat depression and improve parenting: A randomised controlled trial. Lancet Psychiat. 2018 , 5 , 134–144. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ramchandani, P.G.; Stein, A.; O’Connor, T.G.; Heron, J.; Murray, L.; Evans, J. Depression in men in the postnatal period and later child psychopathology: A population cohort study. J. Am. Acad. Child. Adolesc. Psychiatry 2008 , 47 , 390–398. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Quarini, C.; Pearson, R.M.; Stein, A.; Ramchandani, P.G.; Lewis, G.; Evans, J. Are female children more vulnerable to the long-term effects of maternal depression during pregnancy? J. Affect. Disord. 2016 , 189 , 329–335. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Agorastos, A.; Pittman, J.O.E.; Angkaw, A.C.; Nievergelt, C.M.; Hansen, C.J. The cumulative effect of different childhood trauma types on self-reported symptoms of adult male depression and PTSD, substance abuse and health-related quality of life in a large active-duty military cohort. J. Psychiatr. Res. 2014 , 58 , 46–54. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bailer, J.; Witthoft, M.; Wagner, H.; Mier, D.; Diener, C.; Rist, F. Childhood maltreatment is associated with depression but not with hypochondriasis in later life. J. Psychosom. Res. 2014 , 77 , 104–108. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Harkness, K.L.; Lumley, M.N.; Truss, A.E. Stress generation in adolescent depression: The moderating role of child abuse and neglect. J. Abnorm. Child. Psychol. 2008 , 36 , 421–432. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Hovens, J.G.F.M.; Giltay, E.J.; Spinhoven, P.; van Hemert, A.M.; Penninx, B.W.J.H. Impact of childhood life events and childhood trauma on the onset and recurrence of depressive and anxiety disorders. J. Clin. Psychiat. 2015 , 76 , 931–938. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Schoedl, A.F.; Costa, M.C.P.; Mari, J.J.; Mello, M.F.; Tyrka, A.R.; Carpenter, L.L.; Price, L.H. The clinical correlates of reported childhood sexual abuse: An association between age at trauma onset and severity of depression and PTSD in adults. J. Child. Sex. Abus. 2010 , 19 , 156–170. [ Google Scholar ] [ CrossRef ]
- Fletcher, J.M. Childhood mistreatment and adolescent and young adult depression. Soc. Sci. Med. 2009 , 68 , 799–806. [ Google Scholar ] [ CrossRef ]
- Arnow, B.A.; Blasey, C.M.; Hunkeler, E.M.; Lee, J.; Hayward, C. Does gender moderate the relationship between childhood maltreatment and adult depression? Child. Maltreat. 2011 , 16 , 175–183. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Huh, H.J.; Kim, K.H.; Lee, H.K.; Chae, J.H. The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: The mediating role of cognitive emotion regulation strategies. J. Affect. Disord. 2017 , 213 , 44–50. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Carvalho Fernando, S.; Beblo, T.; Schlosser, N.; Terfehr, K.; Otte, C.; Löwe, B.; Wolf, O.T.; Spitzer, C.; Driessen, M.; Wingenfeld, K. The impact of self-reported childhood trauma on emotion regulation in borderline personality disorder and major depression. J. Trauma Dissociation 2014 , 15 , 384–401. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ding, H.S.; Han, J.; Zhang, M.; Wang, K.G.; Gong, J.L.; Yang, S.B. Moderating and mediating effects of resilience between childhood trauma and depressive symptoms in Chinese children. J. Affect. Disord. 2017 , 211 , 130–135. [ Google Scholar ] [ CrossRef ]
- Poole, J.C.; Dobson, K.S.; Pusch, D. Childhood adversity and adult depression: The protective role of psychological resilience. Child. Abuse Negl. 2017 , 64 , 89–100. [ Google Scholar ] [ CrossRef ]
- Hovens, J.G.F.M.; Giltay, E.J.; van Hemert, A.M.; Penninx, B.W.J.H. Childhood maltreatment and the course of depressive and anxiety disorders: The contribution of personality characteristics. Depress. Anxiety 2016 , 33 , 27–34. [ Google Scholar ] [ CrossRef ]
- Spinhoven, P.; Elzinga, B.M.; Van Hemert, A.M.; de Rooij, M.; Penninx, B.W. Childhood maltreatment, maladaptive personality types and level and course of psychological distress: A six-year longitudinal study. J. Affect. Disord. 2016 , 191 , 100–108. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Miu, A.C.; Bilc, M.I.; Bunea, L.; Szentagotai-Tatar, A. Childhood trauma and sensitivity to reward and punishment: Implications for depressive and anxiety symptoms. Pers. Individ. Dif. 2017 , 119 , 134–140. [ Google Scholar ] [ CrossRef ]
- Kounou, K.B.; Bui, E.; Dassa, K.S.; Hinton, D.; Fischer, L.; Djassoa, G.; Birmes, P.; Schmitt, L. Childhood trauma, personality disorders symptoms and current major depressive disorder in Togo. Soc. Psychiatry Psychiatr. Epidemiol. 2013 , 48 , 1095–1103. [ Google Scholar ] [ CrossRef ]
- Alto, M.; Handley, E.; Rogosch, F.; Cicchetti, D.; Toth, S. Maternal relationship quality and peer social acceptance as mediators between child maltreatment and adolescent depressive symptoms: Gender differences. J. Adolesc. 2018 , 63 , 19–28. [ Google Scholar ] [ CrossRef ]
- Harper, F.W.K.; Arias, I. The role of shame in predicting adult anger and depressive symptoms among victims of child psychological maltreatment. J. Fam. Violence 2004 , 19 , 367–375. [ Google Scholar ] [ CrossRef ]
- Powers, A.; Ressler, K.J.; Bradley, R.G. The protective role of friendship on the effects of childhood abuse and depression. Depress. Anxiety 2009 , 26 , 46–53. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Kim, J.S.; Jin, M.J.; Jung, W.; Hahn, S.W.; Lee, S.H. Rumination as a mediator between childhood trauma and adulthood depression/anxiety in non-clinical participants. Front. Psychol. 2017 , 8 , 597. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Wu, Q.L.; Chi, P.L.; Lin, X.Y.; Du, H.F. Child maltreatment and adult depressive symptoms: Roles of self-compassion and gratitude. Child. Abuse Negl. 2018 , 80 , 62–69. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Korkeila, J.; Vahtera, J.; Nabi, H.; Kivimaki, M.; Korkeila, K. Childhood adversities, adulthood life events and depression. J. Affect. Disord. 2010 , 127 , 130–138. [ Google Scholar ] [ CrossRef ]
- Uhl, K.; Halpern, L.F.; Tam, C.; Fox, J.K.; Ryan, J.L. Relations of emotion regulation, negative and positive affect to anxiety and depression in middle childhood. J. Child. Fam. Stud. 2019 , 28 , 2988–2999. [ Google Scholar ] [ CrossRef ]
- Hopfinger, L.; Berking, M.; Bockting, C.L.H.; Ebert, D.D. Emotion regulation mediates the effect of childhood trauma on depression. J. Affect. Disord. 2016 , 198 , 189–197. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- John, S.G.; Cisler, J.M.; Sigel, B.A. Emotion regulation mediates the relationship between a history of child abuse and current PTSD/depression severity in adolescent females. J. Fam. Violence 2017 , 32 , 565–575. [ Google Scholar ] [ CrossRef ]
- Rodman, A.M.; Jenness, J.L.; Weissman, D.G.; Pine, D.S.; McLaughlin, K.A. Neurobiological markers of resilience to depression following childhood maltreatment: The role of neural circuits supporting the cognitive control of emotion. Bio. Psychiatry 2019 , 86 , 464–473. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- World Health Organization (WHO). Depression. Fact Sheet. Available online: http://www.who.int/mediacentre/factsheets/fs369/en/ (accessed on 11 October 2020).
- Chan, E.Y.Y.; Lam, H.C.Y.; So, S.H.W.; Goggins, W.B.; Ho, J.Y.; Liu, S.D.; Chung, P.P.W. Association between Ambient Temperatures and Mental Disorder Hospitalizations in a Subtropical City: A Time-Series Study of Hong Kong Special Administrative Region. Int. J. Env. Res. Pub. He. 2019 , 15 , 754. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Noelke, C.; McGovern, M.; Corsi, D.J.; Jimenez, M.P.; Stern, A.; Wing, I.S.; Berkman, L. Increasing ambient temperature reduces emotional well-being. Environ. Res. 2016 , 151 , 124–129. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Chen, N.T.; Lin, P.H.; Guo, Y.L.L. Long-term exposure to high temperature associated with the incidence of major depressive disorder. Sci. Total Environ. 2019 , 659 , 1016–1020. [ Google Scholar ] [ CrossRef ]
| Journal Title | Number of Publications | IF | H-Index | Subject Category of the Journal (2020) |
|---|---|---|---|---|
| Journal of Affective Disorders | 352 | 5.515 | 59 | Clinical Neurology (Q2) Psychiatry (Q1) |
| Journal of The American Academy of Child and Adolescent Psychiatry | 299 | 10.606 | 95 | Pediatrics (Q1) Psychiatry (Q1) Psychology, Developmental (Q1) |
| Journal of Abnormal Child Psychology | 240 | 4.836 | 67 | Psychology, Clinical (Q2) Psychology, Developmental (Q1) |
| Journal of Youth and Adolescence | 163 | 5.613 | 45 | Psychology, Developmental (Q1) |
| Journal of Clinical Child and Adolescent Psychology | 146 | 5.644 | 45 | Psychology, Clinical (Q1) Psychology, Developmental (Q1) |
| Journal of Adolescence | 120 | 4.181 | 39 | Psychology, Developmental (Q2) |
| Journal of Child Psychology and Psychiatry | 118 | 9.917 | 55 | Psychiatry (Q1) Psychology (Q1) Psychology, Developmental (Q1) |
| Development and Psychopathology | 111 | 5.643 | 40 | Psychology, Developmental (Q1) |
| Journal of Child and Family Studies | 110 | 2.91 | 18 | Family Studies (Q2) Psychiatry (Q3) Psychology, Developmental (Q3) |
| Journal of Abnormal Psychology | 100 | 8.756 | 60 | Psychiatry (Q1) Psychology Clinical (Q1) |
| Author | Country/Institute | Active | Citations | Numbers | Average Citations Per Publication | H-Index |
|---|---|---|---|---|---|---|
| Seeley, JR | USA/Oregon Research Institute | 1991–2014 | 8258 | 50 | 165.2 | 40 |
| Kovacs, M | USA/University of Pittsburgh | 1981–2019 | 8064 | 47 | 171.77 | 33 |
| Lewinsohn, PM | USA/Oregon Research Institute | 1990–2014 | 7864 | 51 | 172.06 | 40 |
| Birmaher, B | USA/University of Pittsburgh | 1992–2018 | 6434 | 70 | 91.94 | 44 |
| Ryan, ND | USA/University of Pittsburgh | 1986–2019 | 4945 | 56 | 88.32 | 38 |
| Pine, DS | USA/National Institute of Mental Health (NIMH) | 1998–2019 | 3939 | 20 | 196.95 | 18 |
| Emslie, GJ | USA/University of Texas Southwestern Medical Center Dallas | 1987–2018 | 3862 | 54 | 71.56 | 31 |
| Hammen, C | USA/University of California Los Angeles | 1984–2016 | 3623 | 36 | 100.72 | 31 |
| Brent, DA | USA/University of Pittsburgh | 1987–2018 | 3619 | 42 | 86.31 | 32 |
| Garber, J | USA/Vanderbilt University | 1980–2019 | 3603 | 44 | 82.02 | 28 |
| Cole, DA | USA/Vanderbilt University | 1986–2019 | 3527 | 49 | 71.98 | 33 |
| Klein, DN | USA/State University of New York Stony Brook | 1994–2019 | 3327 | 48 | 69.33 | 27 |
| Dahl, RE | USA/University of California Berkeley | 1990–2019 | 3109 | 41 | 75.83 | 28 |
| Weissman, MM | USA/Columbia University | 1980–2019 | 3005 | 26 | 115.58 | 21 |
| Wagner, KD | USA/University of Texas Medical Branch Galveston | 1993–2014 | 2902 | 35 | 86.46 | 23 |
| Hankin, BL | USA/University of Illinois Urbana-Champaign | 2001–2019 | 2775 | 37 | 72.92 | 24 |
| Asarnow, JR | USA/University of California Los Angeles | 1985–2019 | 2757 | 43 | 64.98 | 26 |
| McCauley, E | USA/University of Washington | 1988–2017 | 2625 | 42 | 62.50 | 27 |
| Thapar, A | England/Cardiff University | 1994–2019 | 2257 | 38 | 60.68 | 20 |
| Compas, BE | USA/Vanderbilt University | 1993–2019 | 2229 | 32 | 67.88 | 19 |
| Name | Simple Description | References |
|---|---|---|
| State-Trait Anxiety Inventory for Children (STAIC) | A widely used instrument of 20-item instrument to measure anxiety symptoms. | Speilberger, 1973 [ ] |
| Children’s Depression Scale (CDS) | A commonly used instrument of 66-item instrument to measure child depression in psycho-educational and clinical spheres. | Lang and Tisher, 1978 [ ] |
| Children’s Depression Rating Scale-Revised (CDRS-R) | A 17-item instrument designed to measure severity of depression in children aged 6 to 12 years. Total score ranges from 17 to 113. 40 or more presents a major depressive disorder. | Poznanski et al., 1979, 1984, 1985 [ , , ] |
| Peer Nomination Inventory of Depression (PNID) | A well-developed peer-report instrument with 19 items rating depression, happiness, and popularity | Lefkowitz & Tesiny, 1980 [ ] |
| Center for Epidemiological Studies Depression Scale for Children (CES-DC) | A 20-item rating scale ranging from 0 to 3, a general measure of current childhood psychopathology | Weissman et al., 1980 [ ] |
| Depression Self-Rating Scale for Children (DSRSC) | An 18-item self-report questionnaire used to measure the depression status of the children. | Birleson, 1981 [ ] |
| Child Behavior Checklist (CBCL) | A caregiver-completed and widely utilized questionnaire consists of 20 social competence items and 118 behavior problems items. | Achenbach & Edelbrock, 1981 [ ] |
| Child Behavior Checklist-Teacher Report Form (CBCL-T) | A 120-item standardized teacher rating scale assessing social competence and behavior problems in children and adolescents | Achenbach & Edelbrock, 1986 [ ] |
| Children’s Depression Inventory (CDI) | A widely used self-report measure of 27-item measure designed for school-age children and adolescents. Total score ranges from 0 to 54. | Kovacs, 1985, 1992 [ , ] |
| Revised Children’s Manifest Anxiety Scale (RCMAS) | A 37-item self-report measure that provides an estimate of a child’s level and degree of experienced anxiety. | Reynolds & Richmond, 1985 [ ] |
| Reynolds Adolescent Depression Scale (RADS) | A 30-item scale used to assess the severity of depressive symptomatology in adolescent populations. | Reynolds, 1986 [ ] |
| Reynolds Child Depression Scale (RCDS) | A 30-item scale designed to assess depressive symptomatology in children between the ages of 8 and 12 years. | Reynolds, 1989 [ ] |
| Short Mood and Feelings Questionnaire (SMFQ) | A brief, easy-to-administer, self-report measure of childhood and adolescent depression | Angold et al., 1995a [ ] |
| Child and Adolescent Psychiatric Assessment (CAPA) | A semistructured interview designed for use by clinicians or highly trained lay persons to assess 9-to 17-year-olds. | Angold et al., 1995b [ ]; Angold et al., 2000 [ ] |
| Spence Children’s Anxiety Scale (SCAS) | A 45-item scale with 38 items designed to assess children’s report of anxiety symptoms and 7 items designed to assess social desirability. | Spence, 1997 [ ] |
| Schedule for Affective Disorders and Schizophrenia for School-age Children-Present and Lifetime version (K-SADS-PL) | An interviewer-based schedule designed for assessing and diagnosing episodes of psychopathology in youngsters. | Kaufman et al., 1997 [ ] |
| Positive and Negative Affect Schedule for Children (PANAS-C) | A 20-item self-report measure consisting of two scales: Positive Affect (PA) and Negative Affect (NA). | Crook et al., 1998 [ ] |
| Diagnostic Interview for Children and Adolescents (DICA) | A respondent-based interview schedule for youngsters aged 6 to 17 years that can be administered either by clinicians or by lay interviewers. | Reich, 2000 [ ] |
| Diagnostic Interview Schedule for Children (DISC-IV) | An instrument designed to address more than 30 psychiatric diagnoses that occur in children and adolescents | Shaffer et al., 2000 [ ] |
| Revised Child Anxiety and Depression Scales (RCADS) | A 47-item self-report questionnaire designed to assess for clinical syndromes in youth. | Chorpita et al., 2000 [ ] |
| Kutcher Adolescent Depression Scale (KADS) | An 11-item, self-report instrument designed to aid in diagnosis and monitoring the change in the severity of symptoms during the course of treatment. | Brooks & Kutcher, 2001 [ ] |
| Children’s Thought Questionnaire (CTQ) | A 60-item scale designed to assess children’s self-reported anxious, depressive, and positive thoughts. | Marien and Bell, 2004 [ ] |
| Dysfunctional Attitudes Scale for Children (DAS-C) | A 22-item self-report measure with sound psychometric properties. | D’Alessandro and Burton, 2006 [ ] |
| MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
Share and Cite
Zhou, M.; Bian, B.; Zhu, W.; Huang, L. A Half Century of Research on Childhood and Adolescent Depression: Science Mapping the Literature, 1970 to 2019. Int. J. Environ. Res. Public Health 2021 , 18 , 9524. https://doi.org/10.3390/ijerph18189524
Zhou M, Bian B, Zhu W, Huang L. A Half Century of Research on Childhood and Adolescent Depression: Science Mapping the Literature, 1970 to 2019. International Journal of Environmental Research and Public Health . 2021; 18(18):9524. https://doi.org/10.3390/ijerph18189524
Zhou, Mi, Biyu Bian, Weiming Zhu, and Li Huang. 2021. "A Half Century of Research on Childhood and Adolescent Depression: Science Mapping the Literature, 1970 to 2019" International Journal of Environmental Research and Public Health 18, no. 18: 9524. https://doi.org/10.3390/ijerph18189524
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
- Share full article
Advertisement
Supported by
We Have Ruined Childhood
For youngsters these days, an hour of free play is like a drop of water in the desert. Of course they’re miserable.

By Kim Brooks
Ms. Brooks is a writer.
According to the psychologist Peter Gray, children today are more depressed than they were during the Great Depression and more anxious than they were at the height of the Cold War. A 2019 study published in the Journal of Abnormal Psychology found that between 2009 and 2017, rates of depression rose by more than 60 percent among those ages 14 to 17, and 47 percent among those ages 12 to 13. This isn’t just a matter of increased diagnoses. The number of children and teenagers who were seen in emergency rooms with suicidal thoughts or having attempted suicide doubled between 2007 and 2015 .
To put it simply, our kids are not O.K.
For a long time, as a mother and as a writer, I searched for a single culprit. Was it the screens? The food? The lack of fresh air and free time, the rise of the overscheduled, overprotected child, the overarching culture of anxiety and fear?
Those things might all contribute. But I’ve come to believe that the problems with children’s mental and emotional health are caused not by any single change in kids’ environment but by a fundamental shift in the way we view children and child-rearing, and the way this shift has transformed our schools, our neighborhoods and our relationships to one another and our communities.
The work of raising children, once seen as socially necessary labor benefiting the common good, is an isolated endeavor for all but the most well-off parents. Parents are entirely on their own when it comes to their offspring’s well-being. Many have had to prioritize physical safety and adult supervision over healthy emotional and social development.
[Read the most thought-provoking, funny, delightful and raw stories from The New York Times Opinion section. Sign up for our Sunday Best newsletter.]
No longer able to rely on communal structures for child care or allow children time alone, parents who need to work are forced to warehouse their youngsters for long stretches of time. School days are longer and more regimented. Kindergarten, which used to be focused on play, is now an academic training ground for the first grade. Young children are assigned homework even though numerous studies have found it harmful. STEM, standardized testing and active-shooter drills have largely replaced recess, leisurely lunches, art and music.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .
Concept of Childhood Depression Research Paper
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment
Introduction
Observable indicators of childhood depression, facts about childhood depression, treatment of childhood depression, psychosocial therapy, medical option of treatment, prevention of childhood depression, reference list.
The mental challenge of depression is crosscutting in affecting persons of all age levels, races, nationality, ethnicity, cultures and regions of the world. In as much as it affects adults even so it does afflict adolescents and young children alike. Childhood depression is mostly triggered by the prevailing psychosocial environment within the child’s vicinity. As such, the resultant pressure issuing from the immediate psychosocial environment may either obstruct or trigger the child’s mental wellbeing.
It follows therefore that childhood depression can not only be considered to be the state of exhibiting prolonged, persistent and unpredictable cycles of an irritable and sad mood but also the state of minimal appetite on all pleasant undertakings. The afore mentioned afflictions are coupled with a broad range of negative outcomes which encompass reduced desire for food, sporadic sleep patterns, reduction of mental concentration, minimal level of performance in childhood development activities, and a lowered self – esteem.
Therefore, childhood depression is that mental illness which inhibits and disrupts a proper functioning of reasoning, sensing, and acting faculties of a child (John, 2010, p. 1).
The affliction of children by depression involves much more than the general attitude that most of us assume in considering childhood depression as a result of the child’s disappointment experiencing a challenging encounter within the course of the day. It is distinctly unique from the usual sorrow and grief which normally befalls those families which have been bereaved, neither is it associated with character shortfalls in the child’s personality.
As sure as any other disease or illness has to be medically or therapeutically attended to, even so must childhood depression be dealt with, for a depressed child can never overcome such childhood affliction. Nonetheless, the better side of the story is that childhood depression can be curbed either through medical treatment or by psychosocial therapies (John, 2010, p. 1).
It is estimated that almost 5% of depression cases in the general populace are childhood oriented. In an interactive situation, for instance a classroom situation, a stressed child is openly indentified by anxiety, lack of concentration, minimal cooperation, reduced memory and an overall truant attendance to school.
The event of overlooking childhood depression as an illness which warrants immediate medical care is associated with widespread negative ramifications which are normally marked by school failure and dropout, substance and drug abuse and at the very worst, suicide (Thompson, 2010, p. 1).
It is therefore important that parents should be observant in noting the onset of any of the following indicators of childhood depression to raise a timely alarm to medical practitioners and aid in timely intervention, referral and treatment measures. A depressed child is thus characterized by;
- Complacency and passiveness.
- Social reservation; does not interact with other children.
- Withdrawal from childhood activities and isolation.
- Inferiority complex; low self worth.
- Truancy from school coupled with dismal performance.
- Distracted concentration and reduced memory.
- Maintains a rejection consciousness.
- Reduced appetite and uncomfortable sleeping dispositions.
- Hostile and generally irritable.
- Emotional breakdown; crying and sadness.
- Hopelessness coupled with despair.
- Inclinations toward self destructive tendencies.
- Contemplates suicide evident in verbal utterances.
- General body weakness; unpredictable illnesses.
Truly observable indicators of potential self-destructive depression are evident, and as such the socio-environmental influence cannot be overlooked when identifying self-destructive depression dispositions, for instance, when young ones form juvenile gang cocoons, the associated self destructive practices such as substance abuse, robbery, ingestion of toxic substances are inevitable (Favazza, 1996, p. 1).
Even at the family level, homegrown childhood depression is characterized by eating disorders, self neglect, and sexual abuse, persistent emotional strain such as mental stress, crying, hopelessness, despair and self destructive practices (Favazza, 1996, p. 1). In most cases, children who exhibit sings inclined towards depression tend to isolate themselves from the rest of societal entities and are normally afraid and suspicious of other people.
Their conduct is marked with excessive regression, withdrawal, self acclaim and self justification. They hardly acknowledge their mistakes, but rather rationalize their conducts through varied projection devices. These mental patients hold unrealistic expectations and are emotionally disoriented.
The other key feature of those children suffering from depression is corruption of the mental strength evident in lowered self-esteem or the idealistic self-perfectionism.
As an expression of withdrawal, passiveness and inferiority complex, a depressed child does not derive any joy in the activities and games he/she was once a fun of. At the very worst, childhood depression may ultimately lead to self-destructive practices which takes the form of self-injury as evident in extensive body piercing tattoos, self-poisoning and for extreme cases – suicidal attempts.
- In the classroom scenario, academically challenged children bear an overall inclination towards childhood depression (Thompson, 2010, p. 1).
- Depressed children have associated disorders which coexist as a result of depression (Thompson, 2010, p. 1).
- Childhood depression is the main contributor to the heightened cases of runaway children (Thompson, 2010, p. 1).
- Medical intervention for childhood victims is as successful as that of their adult counterparts (Thompson, 2010, p. 1).
- One’s childhood depressions are a reflection of terminal adult depressions in the individual’s life.
Although depression is cross-cutting in affecting persons of all age groups, its manifestation in depressed children is to some extend different from that of a depressed adult.
As such, psychiatrists and medical practitioners take a very keen interest in early diagnosis of childhood depression, through establishing whether the afore-mentioned indicators of childhood depression may have been observed by the child’s immediate acquaintances. Such establishments form the foundation of the remedial action along the medical or psychosocial lines of therapy.
Now that many of the childhood depressive dispositions result from mental-injury, it is necessary that people should uphold each other’s mental health by ensuring a favorable psychosocial environment thrives; where a child’s autonomy is honored and respected rather than being considered an object of scorn.
Psychosocial therapy is therefore vested on the child’s mental welfare and it considers the family as the basic unit upon which the child’s recovery from childhood depression has to be effected. In addressing the child’s mental wellbeing, a psychiatrist employs the cognitive behavioral therapy, which is the most dominant, reliable and effective method of treating childhood depression (Graham, 2008, p. 1).
The cognitive therapy is based on the lemma that a child’s wrong self-perceptions concerning him/herself and his/her immediate environment distort the child’s cognitive normality resulting to childhood depression, as such, the therapy involves the identification of mental distortions, after which strategies are developed to restore the child’s cognitive normality.
Some of the strategies employed in this remedial endeavor include; a change of attitude to that positive attitude which fosters the child’s cognitive functions, programmed learning which enhances quick behavioral adjustments and the physiological domain is upheld by encouraging the child to exploit his/her leisure time wisely, for instance, by either relaxing or meditating (Irina, 2003, p.1).
This holistic integration of the personality of a child in the treatment process has ranked psychosocial therapy as the most effective means of curbing childhood depression way above the medical treatment option.
Medical practitioners in the field of childhood depression use antidepressants to minimize depression levels in children. The other class of effective anti-depression drug administered by doctors is mood stabilizers which include antipsychotic and anticonvulsant drugs. Medical research and experimentations in the treatment of childhood depression has confirmed that fluoxetine is usually superior to placebo in containing acute childhood depression cases (Graham, 2008, p. 1).
Antidepressants can only reduce childhood depression, instead of eliminating it. It is this fact which spells the importance of instituting a multidisciplinary treatment outlook in curbing childhood depression, lest it recurs in adulthood. It is therefore advisable that both the psychosocial therapy and the medical option of treating childhood depression be administered concurrently, for only then would there be a mutually enhanced intervention which ultimately guarantees the success of the treatment operation (Graham, 2008, p. 1).
Therefore, is arguable that the success of treating a depressed child lies not only in incorporating psychosocial therapy which encompasses the trio domains of the child’s personality; cognitive, behavioral and physiological – to the medical option, but also in instituting family educative forums as a follow-up program.
For each of these bipolar strategies of treating childhood depression, early diagnosis of the illness is of central importance in containing the depression afflicting the child before it gains root to attain its terminal stature, thus, the need to strengthen the family and schooling units with educative forums on the necessary detective devices which would aid in intervention and referral measures (Favazza, 1996, p. 1).
The strategies employed in psychosocial and medical front of treating or lowering childhood depression can similarly be harnessed in inoculating the young ones against childhood depression. Preventive measures to childhood depression are anchored on the pillar of early diagnosis at the onset of childhood depression and carrying out immediate referral and prescriptive measures.
Minor childhood depressions arising from strained family frictions form one such class of preventive depressions, whereby, timely psychosocial therapy accommodates and acknowledges the welfare of children in such situations and therefore heals the child’s inherent psychological wound before it worsens (Irina, 2003, p.1).
Medical and psychosocial follow up initiatives are also an integral part of preventing childhood depression and the recurrence of unpleasant psycho-environmental settings which trigger childhood depression (Irina, 2003, p.1).
The introduction of psycho educational strategy to therapy, as opposed to direct lecture to parents only, has created an open forum which has in turn realized heightened child involvement in psychosocial therapies and it has been marked with unprecedented success. This success has been evident along the lines of client satisfaction, openness in the dialogue, and the attainment of the twin objectives of attitude and behavioral change.
Favazza, S. (1996). What do we know about self-injury? Web.
Irina, V. (2003). Depression in Children: What Causes It and How We Can Help . Web.
Graham, E. (2008). The Depressed Child . Web.
Thompson, T. (2010). Major Depression Treatment Options: Why Psychological Treatment Methods for Depression Can Work Better Than Antidepressants. Web.
John M. (2010). Childhood Depression. Web.
- Psychosocial theory by Erik Erikson
- Pre-Referral Team Comparison
- Psychological Development of the Teens
- Definition of the Hostile and Instrumental Aggression in Society
- Concept of the Theory of Behaviorism in Psychology
- Anxiety and Its Types
- Re-entry collateral consequences on education and housing
- Concept of the Assessing the Competency in Trial
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2018, October 10). Concept of Childhood Depression. https://ivypanda.com/essays/childhood-depression/
"Concept of Childhood Depression." IvyPanda , 10 Oct. 2018, ivypanda.com/essays/childhood-depression/.
IvyPanda . (2018) 'Concept of Childhood Depression'. 10 October.
IvyPanda . 2018. "Concept of Childhood Depression." October 10, 2018. https://ivypanda.com/essays/childhood-depression/.
1. IvyPanda . "Concept of Childhood Depression." October 10, 2018. https://ivypanda.com/essays/childhood-depression/.
Bibliography
IvyPanda . "Concept of Childhood Depression." October 10, 2018. https://ivypanda.com/essays/childhood-depression/.

ParentSmart Healthline TM
Caring pediatric nurses are available 24/7 to help answer your questions.
Send Postal Mail To:
Children’s Hospital Colorado Anschutz Medical Campus 13123 East 16th Avenue Aurora, CO 80045
Looking for a different location?
Emergency and urgent care locations
In life-threatening emergencies, find the emergency room location nearest you. For non-life-threatening medical needs when your pediatrician is unavailable, visit one of our urgent care locations.
Emergency locations (24/7)
Urgent care locations (hours vary).
Not sure if you need urgent or emergency care? Help me decide
All locations
See a listing of all our Children’s Hospital Colorado locations including inpatient, outpatient, therapy, surgery facilities and more.
Locations near you
- Healthcare Professionals
- Urgent Care
- Schedule an Appointment
- Departments
Find a Doctor
Find a department.
- Conditions and Symptoms
- Symptom Checker
- Parent Resources
- The Connection Journey
- Calm A Crying Baby
- Sports Articles
- Dosage Tables
Find a Condition or Symptom
- Prepare for Your Visit
- Your Overnight Stay
- Send a Cheer Card
- Family and Patient Resources
- Patient Cost Estimate
- Insurance and Financial Resources
- Online Bill Pay
- Medical Records
- Policies and Procedures
- We Ask Because We Care
Find locations by region

Denver metro

Southern Colorado

Virtual visit
- Addressing the Youth Mental Health Crisis
- Calendar of Events
- Child Health Advocacy
- Community Health
- Community Partners
- Corporate Relations
- Global Health
- Patient Advocacy
- Patient Stories
- Pediatric Affiliations
- Support Children’s Colorado
- Specialty Outreach Clinics
Your Support Matters
All children should have a chance for a healthy future.
Upcoming Events
Child life 101.
Join us to learn about the work of a child life specialist, including...
See All Events
- Pediatric Clinical Trials
- Q: Pediatric Health Advances
- Discoveries and Milestones
- Training and Internships
- Academic Affiliation
- Investigator Resources
- Funding Opportunities
- Center For Innovation
- Support Our Research
- Research Areas

It starts with a Q:
For the latest cutting-edge research, innovative collaborations and remarkable discoveries in child health, read stories from across all our areas of study in Q: Advances and Answers in Pediatric Health .
Discover more in Q:
We use cookies to provide you with the best online experience. If you continue browsing, it means that you accept and agree to our Terms of Use & Privacy Policy
Accept and agree
Pediatric Depression
Parents and caregivers know their kids best. That’s why we put families at the center of every care team.

Would you like to learn more about us?
Do you have questions about your child’s condition, ways to contact us, 720-777-6200, what is depression.
It’s normal for kids to be sad or feel intense feelings sometimes, even for small periods of time. But pediatric depression is different from everyday sadness, and it can be caused by multiple factors including medical problems.
Childhood depression is a mental health disorder defined by a sad or irritable mood that is lengthy and severe and is accompanied by changes in motivation, thinking and functioning. It’s important to know that more than 18% of children will experience depression before they turn 15.
If the sadness or irritability persists for two weeks or more and is affecting day-to-day life, it may be clinical depression. Depression is a serious illness that kids can’t “snap out of” and should be taken seriously, but it is also treatable. Depression is also a risk factor for developing other mental health symptoms and disorders.
What causes depression?
Although the exact cause of mood disorders such as depression is unknown, similarly to adults, depression in children is often caused by a combination of factors. Depression could be caused by:
- Poor physical health or chronic illness
- Life events including major transitions or changes
- Family history
- Environment
- Genetics or biochemical changes such as puberty
- Abuse or trauma
- Excessive stress
Who gets depression?
It’s hard to know how many kids have depression at any given time, but it is common for kids to experience some symptoms of depression during childhood. In children, depression is much more common in boys under age 10 and by age 14, girls are more likely to have depression.
What are the signs and symptoms of depression in children?
Symptoms of depression can differ from child to child. Depression is often mistaken for typical emotional and psychological changes in childhood and because of this, many children go undiagnosed and untreated. It’s common for younger children with a depressed mood to be irritable and act out or frequently display angry behavior. Many children may also display sadness or low mood like depressed adults.
Children may also have physical symptoms such as frequent headaches, stomachaches, body pains or digestive issues. If your child is experiencing physical symptoms, visit your pediatrician to rule out physical problems or conditions and request to have your child screened for depression.
Other symptoms of depression in children can include:
- Unusual grouchiness or anger
- Withdrawing from friends and family
- Becoming more isolated
- Having a negative view of themselves, life or the future
- Changes in sleep
- Changes in appetite
- Crying more
- Difficulty with focus and concentration
- Fatigue and low energy
- Thoughts of suicide or death
What tests are used to diagnose depression in teens and kids?
At Children's Hospital Colorado, we diagnose depression through a clinical interview with a specially trained mental health professional.
A children’s mental health specialist at our Pediatric Mental Health Institute performs a multi-part intake process to ensure a fast and accurate diagnosis. This helps families begin targeted treatment to meet their specific needs. This intake process includes:
- A clinical interview with parents and children
- A standardized Behavior Assessment for Children (BASC-3)
- Questionnaires
When diagnosing this condition, we focus on the symptoms of depression and how they impact your child's daily life. While there are no lab tests or imaging procedures to diagnose depression, our caregivers use tools such as intake questionnaires combined with personal information from the clinical interview, which are very helpful in diagnosing depression in children. Within those intake assessment sessions, therapists may also identify other conditions that contribute to depression such as attention-deficit/hyperactivity disorder (ADHD), anxiety or other mental health conditions.
What can I expect from the intake process at Children’s Colorado?
When you contact us regarding therapy services or to describe your child’s symptoms, we’ll ask you some initial screening questions. A diagnosis requires time to get to know your child and their symptoms, and to build an individualized treatment plan.
We’ll ask you to complete an online intake packet and then schedule an intake interview with you and your child. We can do this interview in person or via telehealth online. We’ll then schedule a follow-up visit for one week after the initial intake interview. At this follow-up visit, we provide families with assessment results, diagnoses and treatment recommendations.
How do we treat depression in teens and children?
Treatment type and length varies based on many factors including the causes of a child’s depression.
Evidence-based treatment for children with depression starts with therapy. For some children, adding medication to therapy can help. Cognitive behavioral therapy (CBT) is the treatment of choice for depression and is the foundational approach to treatment at Children’s Colorado. For many children experiencing depression, once a week outpatient therapy can help a child recover from depression within three to six months. More severe cases may require a brief hospitalization.
We also utilize dialectical behavior therapy (DBT), which is an evidence-based treatment that has been shown to be very effective for children and teens experiencing problems with impulsivity, coping with strong emotions, dealing with stress and interpersonal conflict. This therapy is also very helpful for youth who experience suicidal thoughts or who have engaged in self-injury. Also, acceptance and commitment therapy (ACT) has been shown to be particularly effective for treating both anxiety and depression. Both treatments are based in mindful awareness, which has been shown to reduce anxiety, depression and pain symptoms.
In addition to therapy, families can create routines to support their child’s recovery from depression. These include:
- Getting physical activity every day
- Eating nutritious meals regularly
- Staying engaged in school and family life
- Maintaining a regular sleep schedule
- Keeping up with friends and doing fun activities
Why choose Children’s Colorado for treatment of depression in kids?
Experts in our Pediatric Mental Health Institute are trained and experienced in treating childhood depression. When you receive care here, you can be certain that you and your child are receiving evidence-based treatment that ensures the best possible outcomes.
We provide high quality evaluations that are grounded in the most up-to-date research. Research into depression treatment continues to validate CBT as the most effective treatment with the highest recovery rates. Our providers have years of experience providing children with CBT and have seen its benefits.
In addition to traditional CBT, our providers are the foremost experts in the region in DBT and ACT, which have proven to help children with depression.
Moreover, all our staff are experienced with and sensitive to the needs of children who may be nervous or scared. We include resources like experts from our Ponzio Art Therapy Program and child life specialists to help kids and teens process difficult experiences and feelings. We have toys, art materials, snacks and other soothing items to help put kids at ease.
Anxiety and Depression Association of America
Anxiety and Depression in Children (Centers for Disease Control and Prevention)
"Put Your Feelings Here: A Creative DBT Journal for Teens with Intense Emotions" by Lisa M Schab
Patient ratings and reviews are not available
Children's Hospital Colorado partners with NRC Health to gather star ratings and reviews from patients, residents and family survey data. This provider either practices in a department or specialty that we currently do not survey, or does not have at least 10 ratings in the last 12 months. Learn more about patient ratings and reviews .
Provider affiliation
Children's hospital colorado providers.
Children’s Hospital Colorado providers are faculty members of the University of Colorado School of Medicine. Our specialists are nationally ranked and globally recognized for delivering the best possible care in pediatrics.
Community providers
Some healthcare professionals listed on our website have medical privileges to practice at Children’s Hospital Colorado, but they are community providers. They schedule and bill separately for their services, and are not employees of the Hospital.
- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Adversity in childhood...
Adversity in childhood is linked to mental and physical health throughout life
Read our collection on toxic stress and ptsd in children.
- Related content
- Peer review
- Charles A Nelson , Richard David Scott chair in pediatric developmental medicine 1 ,
- Zulfiqar A Bhutta , co-director, director of research 2 3 ,
- Nadine Burke Harris , surgeon general 4 ,
- Andrea Danese , professor of child and adolescent psychiatry 5 ,
- Muthanna Samara , professor of psychology 6
- 1 Department of Pediatrics, Boston Children’s Hospital and Harvard Medical School, Harvard Graduate School of Education, Boston, MA, USA
- 2 Centre for Global Child Health, Hospital for Sick Children, Toronto, Canada
- 3 Institute for Global Health and Development, Aga Khan University, South Central Asia, East Africa and UK
- 4 State of California, CA, USA
- 5 Institute of Psychiatry, Psychology and Neuroscience, King’s College London and the National and Specialist CAMHS Clinic for Trauma, Anxiety, and Depression, South London and Maudsley NHS Foundation Trust, London, UK
- 6 Department of Psychology, Kingston University London, London, UK
- Correspondence to: C Nelson charles_nelson{at}harvard.edu
The prevalence of “toxic stress” and huge downstream consequences in disease, suffering, and financial costs make prevention and early intervention crucial, say Charles A Nelson and colleagues
Today’s children face enormous challenges, some unforeseen in previous generations, and the biological and psychological toll is yet to be fully quantified. Climate change, terrorism, and war are associated with displacement and trauma. Economic disparities cleave a chasm between the haves and have nots, and, in the US at least, gun violence has reached epidemic proportions. Children may grow up with a parent with untreated mental illness. Not least, a family member could contract covid-19 or experience financial or psychological hardship associated with the pandemic.
The short and long term consequences of exposure to adversity in childhood are of great public health importance. Children are at heightened risk for stress related health disorders, which in turn may affect adult physical and psychological health and ultimately exert a great financial toll on our healthcare systems.
Growing evidence indicates that in the first three years of life, a host of biological (eg, malnutrition, infectious disease) and psychosocial (eg, maltreatment, witnessing violence, extreme poverty) hazards can affect a child’s developmental trajectory and lead to increased risk of adverse physical and psychological health conditions. Such impacts can be observed across multiple systems, affecting cardiovascular, immune, metabolic, and brain health, and may extend far beyond childhood, affecting life course health. 1 2 3 These effects may be mediated in various direct and indirect ways, presenting opportunities for mitigation and intervention strategies.
Defining toxic stress
It is important to distinguish between adverse events that happen to a child, “stressors,” and the child’s response to these events, the “toxic stress response.” 4 A consensus report published by the US National Academy of Sciences, Engineering, and Medicine (2019) defined the toxic stress response as:
Prolonged activation of the stress response systems that can disrupt the development of brain architecture and other organ systems and increase the risk for stress related disease and cognitive impairment, well into the adult years. The toxic stress response can occur when a child experiences strong, frequent, and/or prolonged adversity—such as physical or emotional abuse, chronic neglect, caregiver substance abuse or mental illness, exposure to violence, and/or the accumulated burdens of family economic hardship—without adequate adult support. Toxic stress is the maladaptive and chronically dysregulated stress response that occurs in relation to prolonged or severe early life adversity. For children, the result is disruption of the development of brain architecture and other organ systems and an increase in lifelong risk for physical and mental disorders.
What is childhood adversity?
A large number of adverse experiences (ie, toxic stressors) in childhood can trigger a toxic stress response. 4 5 6 These range from the commonplace (eg, parental divorce) to the horrific (eg, the 6 year old “soldier” ordered to shoot and kill his mother 7 ).
Adversity can affect development in myriad ways, at different points in time, although early exposures that persist over time likely lead to more lasting impacts. Moreover, adversity can become biologically embedded, increasing the likelihood of long term change. Contextual factors are important.
Type of adversity— Not all adversities exert the same impact or trigger the same response; for example, being physically or sexually abused may have more serious consequences for child development than does parental divorce. 8 9
Duration of adversity— How long the adversity lasts can have an impact on development. However, it is often difficult to disentangle duration of adversity from the type of adversity (eg, children are often born into poverty, whereas maltreatment might begin later in a child’s life).
Developmental status and critical period timing— The child’s developmental status at the time he or she is exposed to adversity will influence the child’s response, as will the timing of when these adversities occur. 10
Number of adversities and the interaction among them—— The Adverse Childhood Experiences (ACE) study 11 12 and subsequent body of ACE research provide compelling evidence that the risk of adverse health consequences increases as a function of the number of categories of adversities adults were exposed to in childhood. Although this seems intuitive, it belies the fact that, when it comes to severe adversity (eg, maltreatment), few children are exposed to only a single form of adversity at a single point in time. In addition, the effects of exposure to multiple adversities is likely more than additive. Thus, multiple forms of adversity may act in complex and synergistic ways over time to affect development.
Exacerbating factors— Children with recurrent morbidities, concurrent malnutrition, key micronutrient deficiencies, or exposure to environmental toxicants may be more sensitive to the adverse effects of other forms of toxic exposures. 13
Supportive family environments— Children develop in an environment of relationships, 14 15 16 and supportive relationships can buffer the response to toxic stress. Safe, stable, and nurturing relationships and environments are associated with reduced neuroendocrine, immunologic, metabolic, and genetic regulatory markers of toxic stress, as well as improved clinical outcomes of physical and mental health. 17 18
Pre-existing characteristics —Many of the adversities being considered are not distributed at random in the population. They may occur more commonly in children and families with pre-existing vulnerabilities linked to genetic or fetal influences that lead to cognitive deficits. 19 20 21 Infants who are more vulnerable to adverse life events (eg, stigma) include those born very early (eg, at 25 weeks’ gestation) or very small (eg, <1500 g), those born with substantial perinatal complications (eg, hypoxic-ischaemic injury), infants exposed prenatally to high levels of alcohol, or those born with greater genetic liability to develop an intellectual or developmental disability (eg, fragile X syndrome) or impairments in social communication (eg, autism).
Individual variation— Finally, children may have different physiological reactions to the same stressor. For example, Boyce, 22 has proposed that by virtue of temperament, some children (such as those who are particularly shy and behaviourally inhibited) are highly sensitive to their environments and unless the environment accommodates such children, the risk of developing serious lifelong psychopathology is greatly increased; conversely, some children thrive under almost any conditions.
Figures 1 and 2 illustrate how duration and type of adversity interact with family environments and pre-existing characteristics to affect development ( fig 1 ), and how early adversity may become biologically embedded ( fig 2 ).

The interplay of adversities, context, and human development
- Download figure
- Open in new tab
- Download powerpoint

Some of the pathways that mediate exposure to early adversity and adult outcomes. Exposure to adversity early in life interacts with a child’s genetic endowment (eg variations in genetic polymorphisms), which in turn leads to a host of biological changes across multiple levels. These changes, in turn, influence adult outcomes (adapted from Berens et al 23 ). HPA axis (SHRP)=hypothalamic pituitary adrenal axis (stress hyporesponsive period)
Consequences of exposure to adversity
Behavioral consequences —Childhood exposure to adversity may result in a variety of behavioral and emotional problems 7 —for example, increased risk taking, aggressive behaviour, involvement in violence (home, school, and neighbourhood), and difficulties in relationships with others. 24 25 Of great concern is the development of post-traumatic stress disorder (PTSD). 9 26
Children experiencing trauma (eg, witnessing the murder of a family member; sexual assault) are also at elevated risk of several other psychiatric disorders, including depression, PTSD, conduct problems, substance abuse, self-harm, and suicidal thoughts and attempts. 8 25 Some forms of physical and psychological abuse in early childhood can be associated with eating disorders and mental health issues affecting typical development and education.
Neurobiological consequences —Many studies have identified structural and functional differences in brain development associated with environmental stressors, such as low socioeconomic status, 27 28 29 30 31 physical abuse, 32 and care giving neglect. 33 34 For example, exposure to maternal stress in infancy has been associated with reduced brain activity, as inferred from electroencephalogram testing 35 , and profound psychosocial deprivation has been associated with differences in overall brain volume along with reductions in white and grey matter volume in several brain areas 36 37 and reduced brain electrical activity. 38 39 Differences in brain development have also been associated with decreases in several cognitive functions, 40 and particularly executive functions, 41 and distally, in educational achievement. 42
Physical consequences —Early exposure to adversities, especially poverty, is associated with linear growth failure and wasting, and has recently been shown to be associated with reduced brain volume 43 and altered functional connectivity. 44 Children exposed to higher psychological stress have been shown to have higher cortisol levels and greater risk of common diseases of childhood, including otitis media, viral infections, asthma, dermatitis, urticaria, intestinal infectious diseases, and urinary tract infections. 45
Childhood adversities have also been associated with greater risk of adult chronic conditions, including cardiovascular disease, stroke, cancer (excluding skin cancer), asthma, chronic obstructive pulmonary disease, kidney disease, diabetes, overweight or obesity, and depression, as well as increased health risk behaviours. 46 47
Tables 1 and 2 show many of the physical and psychological harms observed among children and adults exposed to adversity early in life.
Health conditions in children associated with adverse childhood experiences (ACE)
- View inline
ACE-associated health conditions in adults associated with adverse childhood experiences (ACE)
What mediates the effects of adversity?
The link between exposure to adversity early in life and physical and psychological development are thought to be mediated through several direct and indirect pathways. We first talk about the effects on physical development, then turn our attention to psychological development.
Effects mediated directly may include altering the regulation of stress-signalling pathways and immune system function 48 ; changing brain structure and function 49 ; and changing the expression of DNA and by accelerating cellular ageing. 50 51 For example, abuse or neglect might directly lead to physical injury or undernutrition or malnutrition. Similarly, stress can directly lead to dysregulation of the hypothalamic-pituitary-adrenal axis and associated neuro-endocrine-immune 19 as well as epigenetic effects. 52
Effects mediated indirectly might include changing the quality of the care giving environment (eg, less responsive care 3 ) or the surrounding distal environment (eg, neighbourhood violence, which in turn will affect child development across several levels 53 ); or building dysfunctional cognitions about the self and the world. 25 54 55 The effects of food insecurity (leading to undernutrition or malnutrition) and unsafe or substandard housing (resulting in exposure to asthmagens or environmental toxicants such as lead) can lead to social disparities in health. 4 Distal effects of adversity include the early adoption of health damaging behaviors (eg, smoking, poor food choices) that later in life lead to diabetes, heart disease, and metabolic syndrome. 47
On the psychological side, early adversity can lead to the development of psychopathology early in life (eg, disruptive behavior) that later in life manifests in more severe forms (eg, antisocial personality). Furthermore, it can lead to the development of dysfunctional cognition about self and others. 54 The interplay of these different mediation mechanisms remains largely unclear.
Modelling the effects of adversity must take into consideration the type of adversity, the duration and timing of the adversity, the synergistic effects of multiple forms of adversity with the child’s genetic endowment ( fig 2 ), and the social supports and interventions on which the child can depend (such as caregivers to whom the child is attached).
What can we do now?
If we wish for today’s youth to inherit a world that is safe and conducive to healthy development, we must do all we can to create such a world, by preventing disorders from developing and intervening once they are apparent.
Even for children living in adverse circumstances, much can be done now to make a difference by preventing such disorders from developing and intervening once they have surfaced. For example, we can screen children experiencing adverse life events, and once screened refer such children to early intervention services, as California is doing (see elsewhere in this collection).
Intervention strategies have been developed to help children manage their toxic stress response 7 56 and to help families cope with adversity. Many children are resilient, and physician-community partnerships can help foster resilience. 26
Recommendations for research
Much of the evidence has depended on the use of self- or parent-report measures, which are relatively easy to score, can be scaled at population level, and can be used (with modification) across cultures. However, such measures are inherently subjective and prone to biases (eg, recall bias). Other measures, such as official court or child protection records, provide a more objective assessment but often underestimate the prevalence of adversity.
Objective and subjective measures of childhood adversity identify largely non-overlapping groups of individuals 57 and, thus, may be associated with health outcomes through different pathways. Subjective experience is particularly important for psychopathology, over and above objective experience. 54
A challenge in examining the effects of adversity on development is how to compare children growing up in different cultures. For example, one study 58 reported that a questionnaire on bullying used in different cultures and countries did not generalize well (eg, how one culture interpreted bullying differed from another). Adversity and trauma should be considered in context, and investigators in different cultures may need to develop different assessments.
To move away from subjective evaluations of toxic stress (eg, self- or other-report), and to gain insight into the neural and biological mechanisms that mediate the toxic stress response, several investigators have started to develop more objective biomarker panels for screening for toxic stress that use markers of neurological, immunological, metabolic, and genetic regulatory derangements. 59 60 61 As this work continues, issues to consider include how much better (eg, as predictors) such measures are than behavior, how early in life they can be used, and whether they are scalable.
The study of toxic stress and the toxic stress response needs to move away from correlational and cross-sectional studies and deploy designs that are amenable to drawing causal inference. This would include longitudinal studies and ideally studies that involve interventions. An advantage of the latter includes the ability to shed light on mechanism.
More attention also needs to be paid to individual differences. Different people respond differently to the same stressors. For example, only a minority of children who experience trauma or maltreatment go on to develop enduring psychiatric disorders; and some children develop physical health disorders such as asthma whereas others will not. 62 In addition, individual differences exist in biological sensitivity to stressors: for example, children identified as shy or inhibited early in life may be more vulnerable to stressors than children with more robust temperaments and who are less fearful of novelty 63 64 65 and are more predisposed to anxiety as adults. 66
Recommendations for policy
Policy is only as good as the underpinning evidence, and these recommendations have sufficient evidence to support them.
Careful consideration should be given to implementing evidence-informed policies for optimizing health, nutrition, and early child development, 67 which in turn can be expanded to include older children and adolescents. Although the first three years of life are generally emphasized, older children exhibit remarkable plasticity in molding their personalities and behaviors. 27 68 Effective interventions exist to treat and possibly prevent psychopathology emerging after childhood trauma, but implementation needs to be scaled up. 7
Linking and optimizing preventive child health and education initiatives early in life are key to successful intervention 69 and need to be done at the appropriate level in the health and education systems. The development of the nurturing care framework 70 has been a welcome step in this direction, engaging platforms such as community health workers and pre-schools . 71
Community, school, and after-school based interventions can reduce the effects of traumatic events among children and adolescents living in adverse circumstances. 25 72
Public health strategies for primary, secondary, and tertiary prevention of childhood maltreatment and adversity include both universal and targeted interventions, ranging from home visiting programs to parent training programs, routine screening for adversity, and cognitive behavioral therapy. 73 74
Key recommendations
Researchers should consider both objective and subjective measures of childhood adversity
Researchers should broaden assessment of interventions beyond mental health measures to more regularly include health outcomes such as asthma, infection, inflammation, and insulin resistance
Adversity and trauma should be considered in context, and investigators in different cultures may need to develop different assessments
Researchers should consider how much better (eg, as predictors) objective biomarker panels are than behavior, how early in life they can be used, and whether they are scalable
Researchers should move towards longitudinal studies and ideally studies that involve interventions
Researchers should pay more attention to individual differences
Governments should implement evidence-informed policies for optimizing health, nutrition, and early child development
Health and education systems should link and optimize preventive child health and education initiatives early in life at the appropriate level
Use community, school, and after-school based interventions
Consider public health strategies for primary, secondary, and tertiary prevention of childhood maltreatment and adversity

Acknowledgments
We thank Lee Anglin and Lily Breen for proofing the manuscript.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no relevant interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a series commissioned by The BMJ for the World Innovation Summit for Health (WISH) 2020. The BMJ peer reviewed, edited, and made the decisions to publish. The series, including open access fees, is funded by WISH.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- Bellis MA ,
- Ramos Rodriguez G ,
- Nurius PS ,
- Logan-Greene P ,
- ↵ Shonkoff JP, Levitt P, Bunge S, et al. Supportive relationships and active skill-building strengthen the foundations of resilience: working paper 13. 2015. www.developingchild.net
- Shonkoff JP ,
- Garner AS ,
- Siegel BS ,
- Committee on Psychosocial Aspects of Child and Family Health ,
- Committee on Early Childhood, Adoption, and Dependent Care ,
- Section on Developmental and Behavioral Pediatrics
- Burke Harris N
- McLaughlin K ,
- Fleisher W ,
- Arseneault L ,
- Nelson CA 3rd . ,
- Gabard-Durnam LJ
- Felitti VJ ,
- Nordenberg D ,
- Hillis SD ,
- Marchbanks PA
- McDonald CM ,
- Flaxman S ,
- Nutrition Impact Model Study
- Estrada P ,
- Arsenio WF ,
- Holloway SD
- Gunnar MR ,
- Brodersen L ,
- Nachmias M ,
- Boynton-Jarrett R
- van Harmelen A-L
- Moffitt TE ,
- ↵ Boyce, WT. The orchid and the dandelion: why some children struggle and how all can thrive. Knofp Doubleday 2019.
- Berens AE ,
- Jensen SKG ,
- Nelson CA 3rd .
- Taillieu T ,
- El-Khodary B ,
- Hammuda S ,
- Vostanis P ,
- Jenkins LM ,
- Chiang JJ ,
- Johnson SB ,
- Houston SM ,
- Teicher MH ,
- Samson JA ,
- Anderson CM ,
- McLaughlin KA ,
- Sheridan MA ,
- McLaughlin KA
- Pierce LJ ,
- Thompson BL ,
- Zeanah CH ,
- Marshall PJ ,
- Bucharest Early Intervention Project Core Group
- Vanderwert RE ,
- Burneo-Garcés C ,
- Cruz-Quintana F ,
- Pérez-García M ,
- Fernández-Alcántara M ,
- Fasfous A ,
- Pérez-Marfil MN
- Ursache A ,
- Pediatric Imaging, Neurocognition and Genetics Study
- Hanson JL ,
- Turesky TK ,
- Ludvigsson J ,
- Hedmark M ,
- Faresjö Å ,
- Theodorsson E ,
- Merrick MT ,
- Suglia SF ,
- Koenen KC ,
- Boynton-Jarrett R ,
- American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Functional Genomics and Translational Biology; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research
- Elwenspoek MMC ,
- Muller CP ,
- Stamoulis C ,
- Blackburn EH ,
- Theall KP ,
- Shirtcliff EA ,
- Dismukes AR ,
- Wallace M ,
- Jichlinski A
- Baldwin JR ,
- Newbury JB ,
- Altawil M ,
- Scheithauer H
- Aschbacher K
- Deighton S ,
- Neville A ,
- Shonkoff JP
- Gjelsvik A ,
- Crawford H ,
- Morales S ,
- Degnan KA ,
- Vaivada T ,
- Gaffey MF ,
- Dow-Edwards D ,
- MacMaster FP ,
- Peterson BS ,
- Niesink R ,
- Andersen S ,
- Britto PR ,
- Early Childhood Development Interventions Review Group, for the Lancet Early Childhood Development Series Steering Committee
- ↵ World Health Organization, United Nations Children’s Fund, World Bank Group. Nurturing care for early childhood development. 2018. https://apps.who.int/iris/bitstream/handle/10665/272603/9789241514064-eng.pdf
- Richter LM ,
- Daelmans B ,
- Lombardi J ,
- Paper 3 Working Group and the Lancet Early Childhood Development Series Steering Committee
- El Asam A ,
- Khadaroo A ,
- Macmillan HL ,
- Wathen CN ,
- Fergusson DM ,
- Leventhal JM ,
- National Academies of Sciences Engineering and Medicine

SHELLEY S. SELPH, MD, MPH, AND MARIAN S. MCDONAGH, PharmD
Am Fam Physician. 2019;100(10):609-617
Patient information: See related handout on depression in children and adolescents , written by the authors of this article.
Author disclosure: No relevant financial affiliations.
The prevalence of major unipolar depression in children and adolescents is increasing in the United States. In 2016, approximately 5% of 12-year-olds and 17% of 17-year-olds reported experiencing a major depressive episode in the previous 12 months. Screening for depression in adolescents 12 years and older should be conducted annually using a validated instrument, such as the Patient Health Questionnaire-9: Modified for Teens. If the diagnosis is confirmed, treatment should be initiated for persistent, moderate, and severe depression. Active support and monitoring may be sufficient for mild, self-limited depression. For more severe depression, evidence indicates greater response to treatment when psychotherapy (e.g., cognitive behavior therapy) and an antidepressant are used concurrently, compared with either treatment alone. Fluoxetine and escitalopram are the only antidepressants approved by the U.S. Food and Drug Administration for treatment of depression in children and adolescents. Fluoxetine may be used in patients older than eight years, and escitalopram may be used in patients 12 years and older. Monitoring for suicidality is necessary in children and adolescents receiving pharmacotherapy, with frequency of monitoring based on each patient's individual risk. The decision to modify treatment (add, increase, change the medication or add psychotherapy) should be made after about four to eight weeks. Consultation with or referral to a mental health subspecialist is warranted if symptoms worsen or do not improve despite treatment and for those who become a risk to themselves or others.
The prevalence of depression is increasing among youth in the United States. The 2005 to 2014 National Surveys on Drug Use and Health, which included 172,495 adolescents 12 to 17 years of age, found that the percentage of adolescents who experienced one or more major depressive episodes in the previous 12 months increased from 9% in 2005 to 11% in 2014. 1 In 2016, this percentage was approximately 13% (5% in 12-year-olds, 13% in 14-year-olds, and 17% in 17-year-olds), and although 70% of youths experienced severe impairment from depression, only about 40% received treatment. 1 Treatment rates have changed little since 2005, raising concern that adolescents are not receiving needed care for depression. 1
| , | Recommendation from evidence-based guidelines | |
| – | Evidence from response in placebo arms of trials and recommendation from consensus guidelines | |
| , – | Consistent evidence from several randomized trials | |
| , – | Evidence from several randomized trials and systematic reviews |
Risk Factors
Increased risk of depression in children and adolescents may be due to biologic, psychological, or environmental factors ( Table 1 ) . 2 – 34 In children 12 years and younger, depression is slightly more common in boys than in girls (1.3% vs. 0.8%). 35 However, after puberty, adolescent girls are more likely to experience depression. 35
| Being overweight Chronic illness (e.g., lupus, diabetes mellitus, asthma) – Early puberty (girls) Family history of depression Female sex , High-functioning autism , LGBTQ identified Polymorphisms in the serotonin, dopamine, or monoamine oxidase genes | Body dissatisfaction and early dieting , , ; sweetened beverage consumption Dysfunctional emotional regulation Internet gaming disorder or video game addiction , Less attachment to parents and peers, or problems with peers – , Low self-esteem and lack of self-kindness , Negative thinking and recall styles , Other mental health and behavior problems, including previous depression and cannabis or tobacco use – , , Problematic use of social media (e.g., Facebook) Worried about school grades or standardized testing | Academic difficulties Being victimized or bullied or witnessing violence , , , ; physical, sexual, or emotional abuse or neglect , Exposure to natural disasters , Few opportunities for physical activity and sports ; low physical activity ; greater than two hours per day of leisure-time screen use Foreign born or perceived discrimination , Loss of a loved one Low socioeconomic status , , , Parental rejection or low parental involvement , , Poor family functioning or caretaker depression , , |
Screening for Depression
The U.S. Preventive Services Task Force (USPSTF) recommends screening children and adolescents 12 to 18 years of age for major depressive disorder with adequate systems in place to ensure accurate diagnosis, effective treatment, and appropriate follow-up. 36 The American Academy of Family Physicians supports the USPSTF recommendation. 37 In 2018, the American Academy of Pediatrics endorsed the Guidelines for Adolescent Depression in Primary Care (GLAD-PC), which recommends screening adolescents 12 years and older annually for depressive disorders using a self-report screening tool. 38 , 39
There are various instruments to screen adolescents for depression. One popular instrument for use in primary care is the Patient Health Questionnaire-9: Modified for Teens (also called PHQ-A) for patients 11 to 17 years of age. The PHQ-A is shown in Figure 1 and Table 2 , along with four questions not used in scoring that address suicidality, dysthymia, and severity of depression. 40 , 41
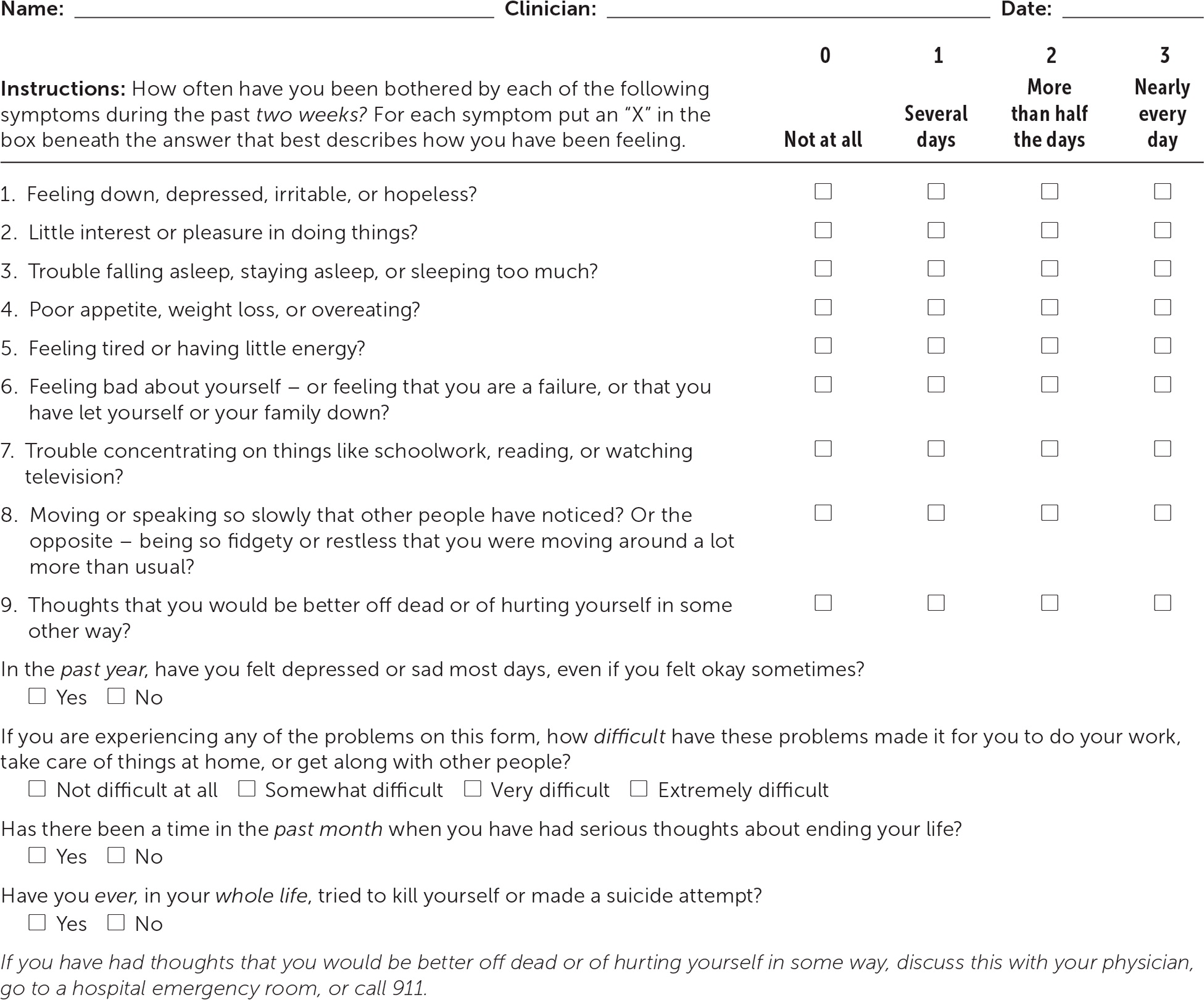
| Scoring is easy but involves thinking about several different aspects of depression. | |
| To use the PHQ-9 as a diagnostic aid for major depressive disorder: answers are needed. | |
| To use the PHQ-9 to screen for all types of depression or other mental illness: answers should be followed by a clinical interview. | |
| To use the PHQ-9 to aid in the diagnosis of dysthymia: | |
| To use the PHQ-9 to screen for suicide risk: | |
| To use the PHQ-9 to obtain a total score and assess depressive severity: | |
| 0 to 4 | No or minimal depression |
| 5 to 9 | Mild depression |
| 10 to 14 | Moderate depression |
| 15 to 19 | Moderately severe depression |
| 20 to 27 | Severe depression |
Clinical Presentation
The presenting sign of major depressive disorder may be insomnia or hypersomnia; weight loss or gain; difficulty concentrating; loss of interest in school, sports, or other previously enjoyable activities; increased irritability; or feeling sad or worthless. 42 To distinguish between normal grief, such as after the loss of a loved one, and a major depressive episode, it may be helpful to determine whether the predominant symptom is a sense of loss or emptiness (more typical of grief) vs. a persistent depressed mood with the inability to anticipate future enjoyable events (more typical of depression). 42
When a child or adolescent screens positive using a formal screening tool, such as the PHQ-A, or when he or she presents with symptoms indicating a possible depressive disorder, the primary care physician should assess whether the symptoms are a result of a major depressive episode or another condition that could present with similar symptoms. To diagnose major depressive disorder, criteria from the Diagnostic and Statistical Manual of Mental Disorders , 5th ed. (DSM-5), must be met and not explained by substance abuse, medication use, or other medical or psychological condition. 42 The full DSM-5 criteria are available at https://www.aafp.org/afp/2018/1015/p508.html#afp20181015p508-t6 . Some children may develop a cranky mood or irritability rather than sadness.
Medical conditions that may present similarly to depression include hypothyroidism, anemia, autoimmune disease, and vitamin deficiency. Laboratory tests that may be helpful in ruling out common medical conditions that could be mistaken for depression include complete blood count; comprehensive metabolic profile panel; an inflammatory biomarker, such as C-reactive protein or erythrocyte sedimentation rate; thyroid-stimulating hormone; vitamin B 12 ; and folate.
Other psychological conditions that may present similarly to major depressive disorder include persistent depressive disorder (also called dysthymia) and disruptive mood dysregulation disorder. If a child or adolescent has a depressed mood for more days than not for at least one year, the diagnosis may be persistent depressive disorder, which is often treated the same as a major depressive episode (e.g., antidepressants, psychotherapy). 42 If a child or adolescent is predominantly angry with temper outbursts, the diagnosis may be disruptive mood dysregulation disorder or posttraumatic stress disorder. 42
Symptoms of bipolar disorder, eating disorders, and conduct disorders may also overlap with major depressive disorder. Children and adolescents may have more than one psychiatric diagnosis concurrently, such as comorbid depression and anxiety. According to the Centers for Disease Control and Prevention, 74% of children three to 17 years of age who have depression also have anxiety, and 47% of children with depression also have a behavior problem. Therefore, a thorough assessment is needed, with possible mental health consultation or referral.
Risk Assessment for Suicide
Suicide is the second leading cause of death for people 10 to 24 years of age after unintentional injury. 43 Depression is a risk factor for suicide, but at-risk youth can be easily missed without specific suicide screening. In one study, nurses in a pediatric emergency department used the Ask Suicide-Screening Questions (ASQ) tool to assess suicide risk in 970 adolescents who presented with psychiatric problems. 44 Of those who screened positive, 53% did not present with suicide-related problems. The sensitivity and specificity for a return visit to the emergency department because of suicidality within six months were 93% and 43%, respectively, for a positive predictive value of 10% and a negative predictive value of 99%. 44 The ASQ screening test is shown in Figure 2 . 45 The complete ASQ toolkit is available at https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials/index.shtml#outpatient .
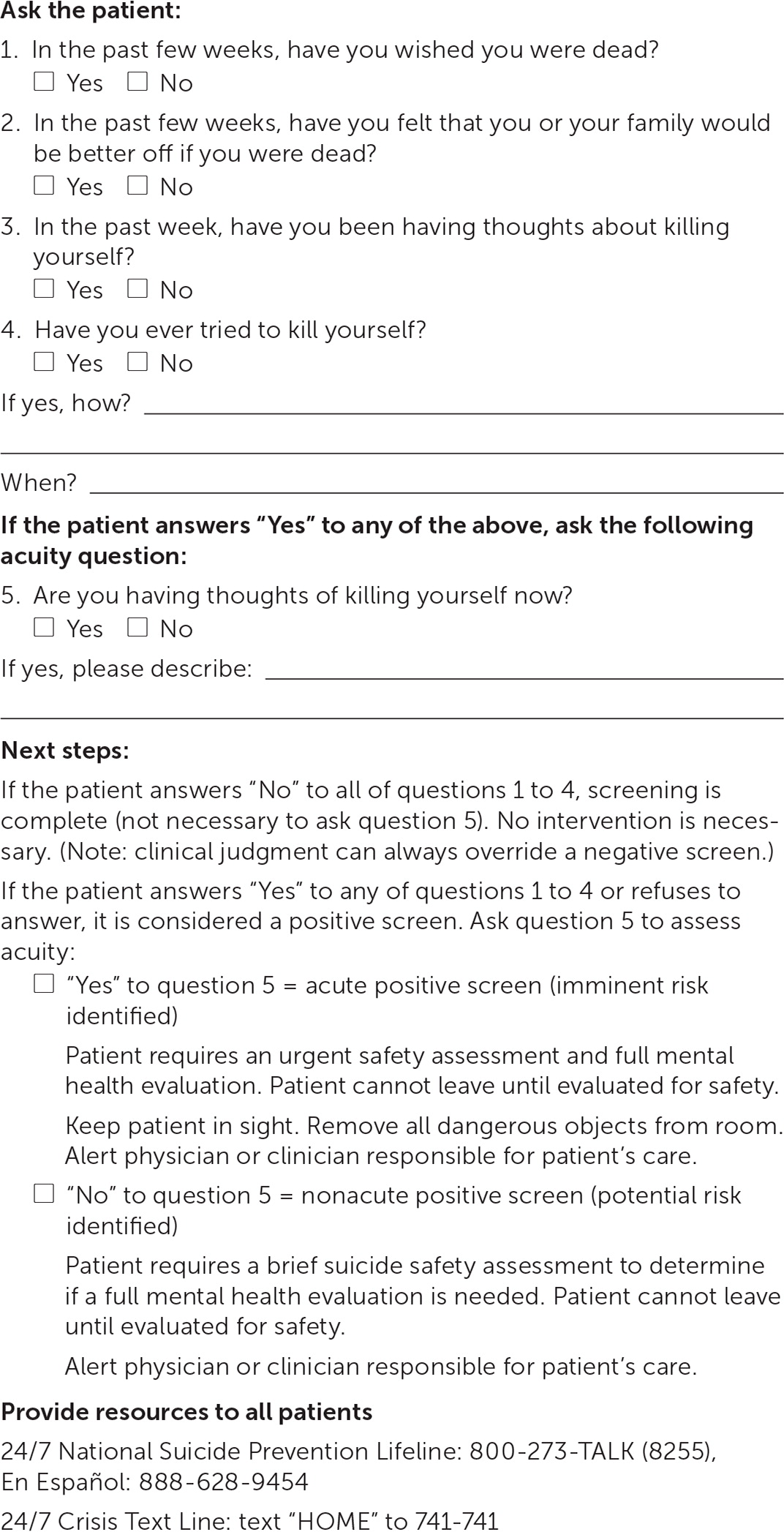
INITIAL MANAGEMENT
The GLAD-PC guidelines recommend that primary care physicians counsel families and patients about depression and develop a treatment plan that includes setting specific goals involving functioning at home, at school, and with peers. 38 For example, a treatment plan might include treating others with respect, attending family meals, keeping up with schoolwork, and spending time in activities with supportive peers. Additionally, a safety plan should be established that limits access to lethal means, such as removing firearms from the home or locking them up. It should also provide a way for the patient to communicate during an acute crisis (e.g., providing phone numbers for people to contact if suicidal thoughts occur, creating a list of coping skills, educating the parents on how to recognize if the patient is a risk to self or others). 38 If the danger of suicide becomes imminent, psychiatric evaluation in a hospital emergency department or psychiatry crisis clinic is needed.
For mild depression, which may be short-lived, primary care physicians should consider active support such as counseling about depression and treatment options, facilitating caregiver/patient depression self-management, and monitoring the patient every week or two for six to eight weeks before initiating pharmacotherapy and/or psychotherapy. 46 – 50 According to the DSM-5, although the symptoms of mild depression are distressing, they are manageable and result in only minor impairment in functioning, whereas severe depression causes more seriously distressing, unmanageable symptoms that greatly impact functioning. See Figure 3 for a suggested approach to the management of depression in children and adolescents. 43 , 50
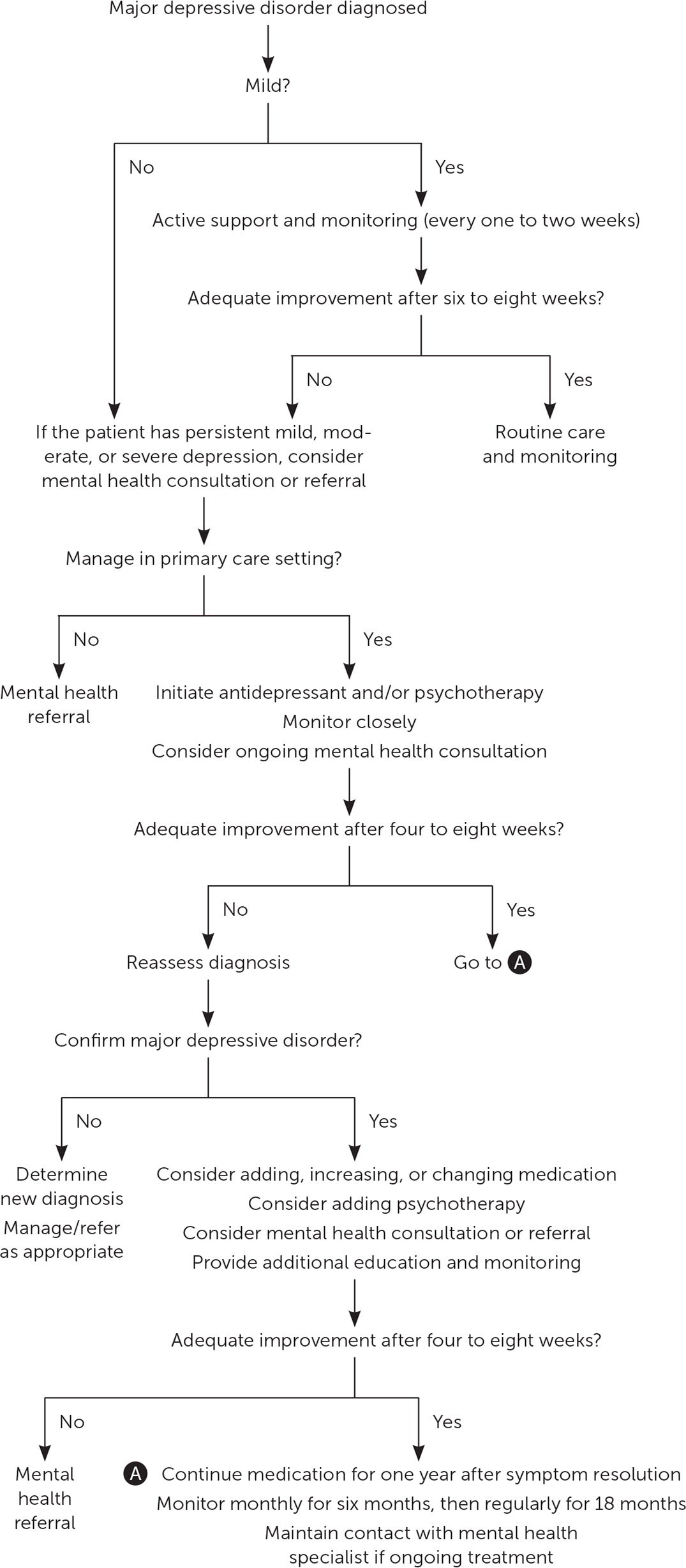
ONGOING MANAGEMENT
Treatment options for children and adolescents with depression include psychotherapy and anti-depressants. Cognitive behavior therapy (CBT) is a form of talk therapy that focuses on changing behaviors by correcting faulty or potentially harmful thought patterns and generally includes five to 20 sessions. Whereas CBT focuses on cognition and behaviors, interpersonal psychotherapy concentrates on improving interpersonal relationships and typically includes around 12 to 16 sessions.
Fluoxetine (Prozac) and escitalopram (Lexapro) are the only two medications approved by the U.S. Food and Drug Administration to treat major depressive disorder in children and adolescents. Fluoxetine is approved for patients eight years and older, and escitalopram is approved for patients 12 years and older. There are concerns of increased suicidality with the use of fluoxetine and escitalopram in this population. 51 Although there were no suicides in trials of children and adolescents taking antidepressants, suicidal thoughts and behaviors were increased compared with placebo (4% vs. 2%). 51 Children and adolescents who are taking these medications should be monitored for suicidality. The frequency of monitoring should be based on the individual patient's risk (e.g., weekly monitoring at treatment onset, monthly monitoring in a child showing steady improvement on antidepressants).
PHARMACOTHERAPY ALONE
Three systematic reviews of randomized controlled trials including children and adolescents with major depressive disorder support the use of fluoxetine as the first-line antidepressant medication. 52 – 54 Two reviews also support the use of escitalopram as initial therapy. 52 , 54 However, the effects of fluoxetine and escitalopram as monotherapy were often similar to placebo, depending on the outcome measured. Tricyclic antidepressants, other selective serotonin reuptake inhibitors, and serotonin-norepinephrine reupta ke inhibitors have not been shown to be effective in treating depression in children and adolescents. 46 , 52 – 54 If neither fluoxetine nor escitalopram is effective and antidepressant therapy is desired, referral to a child or adolescent psychiatrist is recommended.
PSYCHOTHERAPY ALONE
Evidence is mixed for the use of CBT as monotherapy in children and adolescents with depression. A systematic review for the USPSTF found no benefit of CBT on remission or recovery and inconsistent effects on symptoms, response, and functioning. 54 One trial of youth with major depression who declined antidepressants found that compared with self-selected treatment as usual, 12 weeks of CBT was associated with shorter time to treatment response and remission and improved depression scores through week 52 but not in weeks 53 to 104. 55 In children and adolescents with subclinical depression, one systematic review (19 trials) found moderate-quality evidence that CBT is associated with a small effect on depressive symptoms vs. waitlist or no treatment. 56
COMBINED THERAPY
Evidence from a good-quality randomized trial suggests that adolescents are most likely to achieve remission with 12 weeks of combined therapy with fluoxetine and CBT (37%; number needed to treat = 4) compared with either therapy alone (23% with fluoxetine; number needed to treat = 11; 16% with CBT) or placebo (17%). 47 , 57 Suicidality declined with duration of treatment for all therapies, but the decline was less steep for fluoxetine alone (26.2% at baseline to 13.7% at week 36) vs. combination therapy (39.6% to 2.5%) and CBT alone (25.2% to 3.9%). 47 , 57
In another trial of adolescents who achieved at least a 50% decrease in depression scores following six weeks of fluoxetine treatment, those who were randomized to receive the addition of CBT to fluoxetine therapy for six months were less likely to relapse at 78 weeks compared with continued fluoxetine monotherapy (36% vs. 62%). 58
Children and adolescents with moderate or severe depression or persistent mild depression should be treated with fluoxetine or escitalopram in conjunction with CBT or other talk therapy. 47 , 57 – 59 If combination therapy is not used, monotherapy with an antidepressant or psychotherapy is recommended, although the likelihood of benefit is lower. 46 , 52 – 56
Reassessing Treatment and Treatment Duration
One trial found that early reassessment of depression is valuable. 43 In this study, all youth received interpersonal psychotherapy and were randomized to a four- or eight-week follow-up assessment for treatment modification. If additional treatment was needed because of inadequate response, patients were further randomized to add-on fluoxetine or more intense (twice weekly) psychotherapy. Those who were reassessed at four weeks improved the most at 16 weeks (a difference of 5.7 points on the Hamilton Rating Scale for Depression; scores on this scale can range from 0 to 58 points, with a score of 0 to 7 considered normal and a score of 20 associated with moderate depression; P < .05). Additionally, those who began add-on fluoxetine at four weeks had better posttreatment depression scores than those who began intense interpersonal psychotherapy at eight weeks, although there was no difference in global assessment scores between the two groups.
Treatment duration for talk therapy in adolescents with unipolar depression is typically six months or less, but longer treatment may be necessary. Although good evidence regarding the duration of medication treatment in adolescents with depression is lacking, the GLAD-PC guidelines recommend continuing medication for one year beyond the resolution of symptoms. 50
Referral to a Mental Health Subspecialist
If a child or adolescent does not improve after initial treatment for depression, the primary care physician may add, change, or increase a medication and may consider referral for psychotherapy. Referral to a licensed mental health professional is appropriate at any point in the treatment process. However, if the depression does not improve or the child deteriorates even with treatment, consultation with or referral to a child or adolescent psychiatrist is necessary.
This article updates previous articles on this topic by Clark, et al. 60 ; Bhatia and Bhatia 61 ; and Son and Kirchner . 62
Data Sources: We conducted general and targeted searches using Essential Evidence Plus, Ovid Medline, PubMed, the Cochrane Database of Systematic Reviews, the U.S. Preventive Services Task Force, the Agency for Healthcare Research and Quality, and UpToDate, including the key words children or adolescents with depression. Search dates: November 2018 to January 2019, and September 27, 2019.
The authors thank Alycia Brown, MD, for her review of the manuscript and Ngoc Wasson, MPH, and Chandler Weeks, BS, for help with formatting the manuscript.
National Institute of Mental Health. Major depression. Accessed December 13, 2018. https://www.nimh.nih.gov/health/statistics/major-depression.shtml#part_155031
Xie B, Unger JB, Gallaher P, et al. Overweight, body image, and depression in Asian and Hispanic adolescents. Am J Health Behav. 2010;34(4):476-488.
Shankar M, Fagnano M, Blaakman SW, et al. Depressive symptoms among urban adolescents with asthma: a focus for providers. Acad Pediatr. 2019;19(6):608-614.
Buchberger B, Huppertz H, Krabbe L, et al. Symptoms of depression and anxiety in youth with type 1 diabetes: a systematic review and meta-analysis. Psychoneuroendocrinology. 2016;70:70-84.
Sibbitt WL, Brandt JR, Johnson CR, et al. The incidence and prevalence of neuropsychiatric syndromes in pediatric onset systemic lupus erythematosus. J Rheumatol. 2002;29(7):1536-1542.
Benoit A, Lacourse E, Claes M. Pubertal timing and depressive symptoms in late adolescence: the moderating role of individual, peer, and parental factors. Dev Psychopathol. 2013;25(2):455-471.
Kounali D, Zammit S, Wiles N, et al. Common versus psychopathologyspecific risk factors for psychotic experiences and depression during adolescence. Psychol Med. 2014;44(12):2557-2566.
Song SJ, Ziegler R, Arsenault L, et al. Asian student depression in American high schools: differences in risk factors. J Sch Nurs. 2011;27(6):455-462.
Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6):12. Accessed September 29, 2019. https://pediatrics.aappublications.org/content/138/6/e20161878.long
Whitehouse AJ, Durkin K, Jaquet EK, et al. Friendship, loneliness and depression in adolescents with Asperger's syndrome. J Adolesc. 2009;32(2):309-322.
De-la-Iglesia M, Olivar JS. Risk factors for depression in children and adolescents with high functioning autism spectrum disorders. Scientific World Journal. 2015;2015:127853.
McDonald K. Social support and mental health in LGBTQ adolescents: a review of the literature. Issues Ment Health Nurs. 2018;39(1):16-29.
Lavigne JV, Herzing LB, Cook EH, et al. Gene × environment effects of serotonin transporter, dopamine receptor D4, and monoamine oxidase A genes with contextual and parenting risk factors on symptoms of oppositional defiant disorder, anxiety, and depression in a community sample of 4-year-old children. Dev Psychopathol. 2013;25(2):555-575.
Ferreiro F, Seoane G, Senra C. A prospective study of risk factors for the development of depression and disordered eating in adolescents. J Clin Child Adolesc Psychol. 2011;40(3):500-505.
Bisaga K, Whitaker A, Davies M, et al. Eating disorder and depressive symptoms in urban high school girls from different ethnic backgrounds. J Dev Behav Pediatr. 2005;26(4):257-266.
Pabayo R, Dias J, Hemenway D, et al. Sweetened beverage consumption is a risk factor for depressive symptoms among adolescents living in Boston, Massachusetts, USA. Public Health Nutr. 2016;19(17):3062-3069.
Kullik A, Petermann F. Attachment to parents and peers as a risk factor for adolescent depressive disorders: the mediating role of emotion regulation. Child Psychiatry Hum Dev. 2013;44(4):537-548.
Torres-Rodríguez A, Griffiths MD, Carbonell X, et al. Internet gaming disorder in adolescence: psychological characteristics of a clinical sample. J Behav Addict. 2018;7(3):707-718.
Brunborg GS, Mentzoni RA, Frøyland LR. Is video gaming, or video game addiction, associated with depression, academic achievement, heavy episodic drinking, or conduct problems?. J Behav Addict. 2014;3(1):27-32.
Orth U, Robins RW, Widaman KF, et al. Is low self-esteem a risk factor for depression? Findings from a longitudinal study of Mexican-origin youth. Dev Psychol. 2014;50(2):622-633.
Muris P, van den Broek M, Otgaar H, et al. Good and bad sides of self-compassion: a face validity check of the self-compassion scale and an investigation of its relations to coping and emotional symptoms in non-clinical adolescents. J Child Fam Stud. 2018;27(8):2411-2421.
Orchard F, Reynolds S. The combined influence of cognitions in adolescent depression: biases of interpretation, self-evaluation, and memory. Br J Clin Psychol. 2018;57(4):420-435.
Rawal A, Rice F. Examining overgeneral autobiographical memory as a risk factor for adolescent depression. J Am Acad Child Adolesc Psychiatry. 2012;51(5):518-527.
Marino C, Gini G, Vieno A, et al. The associations between problematic Facebook use, psychological distress and well-being among adolescents and young adults: a systematic review and meta-analysis. J Affect Disord. 2018;226:274-281.
Kodish T, Herres J, Shearer A, et al. Bullying, depression, and suicide risk in a pediatric primary care sample [published correction appears in Crisis . 2016;37(3):247]. Crisis. 2016;37(3):241-246.
Hamm MP, Newton AS, Chisholm A, et al. Prevalence and effect of cyberbullying on children and young people: a scoping review of social media studies. JAMA Pediatr. 2015;169(8):770-777.
Adams J, Mrug S, Knight DC. Characteristics of child physical and sexual abuse as predictors of psychopathology. Child Abuse Negl. 2018;86:167-177.
Cohen JR, McNeil SL, Shorey RC, et al. Maltreatment subtypes, depressed mood, and anhedonia: a longitudinal study with adolescents [published online December 27, 2018]. Psychol Trauma . Accessed September 29, 2019. https://psycnet.apa.org/doiLanding?doi=10.1037%2Ftra0000418
Lai BS, La Greca AM, Auslander BA, et al. Children's symptoms of post-traumatic stress and depression after a natural disaster: comorbidity and risk factors. J Affect Disord. 2013;146(1):71-78.
Tang B, Liu X, Liu Y, et al. A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health. 2014;14:623.
Kremer P, Elshaug C, Leslie E, et al. Physical activity, leisure-time screen use and depression among children and young adolescents. J Sci Med Sport. 2014;17(2):183-187.
Korczak DJ, Madigan S, Colasanto M. Children's physical activity and depression: a meta-analysis. Pediatrics. 2017;139(4):e20162266.
Uddin M, Jansen S, Telzer EH. Adolescent depression linked to socioeconomic status? Molecular approaches for revealing premorbid risk factors. Bioessays. 2017;39(3):03. Accessed September 29, 2019. https://onlinelibrary.wiley.com/doi/abs/10.1002/bies.201600194
Shanahan L, Copeland WE, Costello EJ, et al. Child-, adolescent- and young adult-onset depressions: differential risk factors in development?. Psychol Med. 2011;41(11):2265-2274.
Douglas J, Scott J. A systematic review of gender-specific rates of uni-polar and bipolar disorders in community studies of pre-pubertal children. Bipolar Disord. 2014;16(1):5-15.
U.S. Preventive Services Task Force. Depression in children and adolescents: screening. February 2016. Accessed August 12,2019. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/depression-in-children-and-adolescents-screening1
American Academy of Family Physicians. Adolescent health clinical recommendations and guidelines. Depression – clinical preventive service recommendation. Accessed August 12, 2019. https://www.aafp.org/patient-care/browse/topics.tag-adolescent-health.html
Zuckerbrot RA, Cheung A, Jensen PS, et al.; GLAD-PC Steering Group. Guidelines for adolescent depression in primary care (GLAD-PC): part I. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018;141(3):e20174081.
The Reach Institute. Adolescent Depression in Primary Care (GLAD-PC) Toolkit. Accessed August 12, 2019. http://www.glad-pc.org
Patient Health Questionnaire (PHQ) screeners. Accessed August 12, 2019. http://www.phqscreeners.com
American Academy of Child & Adolescent Psychiatry. PHQ-9: Modified for Teens. Accessed August 12, 2019. http://www.aacap.org/App_Themes/AACAP/docs/member_resources/toolbox_for_clinical_practice_and_outcomes/symptoms/GLAD-PC_PHQ-9.pdf
Diagnostic and Statistical Manual of Mental Disorders . 5th ed. American Psychiatric Association; 2014.
Gunlicks-Stoessel M, Mufson L, Bernstein G, et al. Critical decision points for augmenting interpersonal psychotherapy for depressed adolescents: a pilot sequential multiple assignment randomized trial. J Am Acad Child Adolesc Psychiatry. 2019;58(1):80-91.
Ballard ED, Cwik M, Van Eck K, et al. Identification of at-risk youth by suicide screening in a pediatric emergency department. Prev Sci. 2017;18(2):174-182.
National Institute of Mental Health. Suicide risk screening tool. Accessed August 12, 2019. https://www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials/index.shtml#outpatient
Weihs KL, Murphy W, Abbas R, et al. Desvenlafaxine versus placebo in a fluoxetine-referenced study of children and adolescents with major depressive disorder. J Child Adolesc Psychopharmacol. 2018;28(1):36-46.
Kennard B, Silva S, Vitiello B, et al.; TADS Team. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45(12):1404-1411.
Clarke GN, Rohde P, Lewinsohn PM, et al. Cognitive-behavioral treatment of adolescent depression: efficacy of acute group treatment and booster sessions. J Am Acad Child Adolesc Psychiatry. 1999;38(3):272-279.
Wagner KD, Jonas J, Findling RL, et al. A double-blind, randomized, placebo-controlled trial of escitalopram in the treatment of pediatric depression. J Am Acad Child Adolesc Psychiatry. 2006;45(3):280-288.
Cheung AH, Zuckerbrot RA, Jensen PS, et al. Guidelines for adolescent depression in primary care (GLAD-PC): part II. treatment and ongoing management. Pediatrics. 2018;141(3):e20174082.
U.S. Food and Drug Administration. Suicidality in children and adolescents being treated with antidepressant medications. Accessed August 12, 2019. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/suicidality-children-and-adolescents-being-treated-antidepressant-medications
Ignaszewski MJ, Waslick B. Update on randomized placebo-controlled trials in the past decade for treatment of major depressive disorder in child and adolescent patients: a systematic review [published online July 31, 2018]. J Child Adolesc Psychopharmacol . Accessed September 29, 2019. https://www.liebertpub.com/doi/abs/10.1089/cap.2017.0174?journalCode=cap
Cipriani A, Zhou X, Del Giovane C, et al. Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents. Lancet. 2016;388(10047):881-890.
Forman-Hoffman VL, McClure E, McKeeman J, et al. Screening for major depressive disorder among children and adolescents: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2016;164(5):342-349.
Clarke G, DeBar LL, Pearson JA, et al. Cognitive behavioral therapy in primary care for youth declining antidepressants: a randomized trial. Pediatrics. 2016;137(5):e20151851.
Oud M, de Winter L, Vermeulen-Smit E, et al. Effectiveness of CBT for children and adolescents with depression: a systematic review and meta-regression analysis. Eur Psychiatry. 2019;57:33-45.
March JS, Silva S, Petrycki S, et al. The Treatment for Adolescents With Depression Study (TADS): long-term effectiveness and safety outcomes [published correction appears in Arch Gen Psychiatry . 2008;65(1):101]. Arch Gen Psychiatry. 2007;64(10):1132-1143.
Emslie GJ, Kennard BD, Mayes TL, et al. Continued effectiveness of relapse prevention cognitive-behavioral therapy following fluoxetine treatment in youth with major depressive disorder. J Am Acad Child Adolesc Psychiatry. 2015;54(12):991-998.
Foster S, Mohler-Kuo M. Treating a broader range of depressed adolescents with combined therapy. J Affect Disord. 2018;241:417-424.
Clark MS, Jansen KL, Cloy JA. Treatment of childhood and adolescent depression. Am Fam Physician. 2012;86(5):442-448. Accessed August 12, 2019. https://www.aafp.org/afp/2012/0901/p442.html
Bhatia SK, Bhatia SC. Childhood and adolescent depression. Am Fam Physician. 2007;75(1):73-80. Accessed August 12, 2019. https://www.aafp.org/afp/2007/0101/p73.html
Son SE, Kirchner JT. Depression in children and adolescents. Am Fam Physician. 2000;62(10):2297-2308. Accessed August 12, 2019. https://www.aafp.org/afp/2000/1115/p2297.html
Continue Reading

More in AFP
More in pubmed.
Copyright © 2019 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
Anxiety and depression in children: Get the facts

Many children have fears and worries, and may feel sad and hopeless from time to time. Strong fears may appear at different times during development. For example, toddlers are often very distressed about being away from their parents, even if they are safe and cared for. Although some fears and worries are typical in children, persistent or extreme forms of fear and sadness could be due to anxiety or depression. Learn about anxiety and depression in children.
- 9.4% of children aged 3-17 years (approximately 5.8 million) had diagnosed anxiety in 2016-2019.
- 4.4% of children aged 3-17 years (approximately 2.7 million) have diagnosed depression in 2016-2019.
- “Ever having been diagnosed with either anxiety or depression” among children aged 6-17 years increased from 5.4% in 2003 to 8% in 2007 and to 8.4% in 2011–2012.
- “Ever having been diagnosed with anxiety” among children aged 6-17 years increased from 5.5% in 2007 to 6.4% in 2011–2012.
- “Ever having been diagnosed with depression” among children aged 6-17 years did not change between 2007 (4.7%) and 2011–2012 (4.9%).
Learn more facts about children’s mental health
When children do not outgrow the fears and worries that are typical in young children, or when there are so many fears and worries that they interfere with school, home, or play activities, the child may be diagnosed with an anxiety disorder. Examples of different types of anxiety disorders include
- Being very afraid when away from parents (separation anxiety)
- Having extreme fear about a specific thing or situation, such as dogs, insects, or going to the doctor (phobias)
- Being very afraid of school and other places where there are people (social anxiety)
- Being very worried about the future and about bad things happening (general anxiety)
- Having repeated episodes of sudden, unexpected, intense fear that come with symptoms like heart pounding, having trouble breathing, or feeling dizzy, shaky, or sweaty (panic disorder)
Anxiety may present as fear or worry, but can also make children irritable and angry. Anxiety symptoms can also include trouble sleeping, as well as physical symptoms like fatigue, headaches, or stomachaches. Some anxious children keep their worries to themselves and, thus, the symptoms can be missed.
Occasionally being sad or feeling hopeless is a part of every child’s life. However, some children feel sad or uninterested in things that they used to enjoy, or feel helpless or hopeless in situations they are able to change. When children feel persistent sadness and hopelessness, they may be diagnosed with depression.
Examples of behaviors often seen in children with depression include
- Feeling sad, hopeless, or irritable a lot of the time
- Not wanting to do, or enjoy doing, fun things
- Showing changes in eating patterns – eating a lot more or a lot less than usual
- Showing changes in sleep patterns – sleeping a lot more or a lot less than normal
- Showing changes in energy – being tired and sluggish or tense and restless a lot of the time
- Having a hard time paying attention
- Feeling worthless, useless, or guilty
- Showing self-injury and self-destructive behavior
Extreme depression can lead a child to think about suicide or plan for suicide. For youth ages 10-24 years, suicide is among the leading causes of death 1 . Read about youth suicide prevention
Some children may not talk about their helpless and hopeless thoughts, and may not appear sad. Depression might also cause a child to make trouble or act unmotivated, causing others not to notice that the child is depressed, or to incorrectly label the child as a trouble-maker or lazy.
Treatment for Anxiety and Depression
The first step to treatment is to talk with a healthcare provider, such as your child’s primary care provider or a mental health specialist, about getting an evaluation. Some of the signs and symptoms of anxiety or depression in children could be caused by other conditions, such as trauma . A mental health professional can develop a therapy plan that works best for the child and family. Behavior therapy includes child therapy, family therapy, or a combination of both. For very young children, involving parents in treatment is key; the school can also be included in the treatment plan. Consultation with a healthcare provider can help determine if medication should be part of the treatment.
If you need help finding treatment, visit MentalHealth.gov .
Managing Symptoms: Staying Healthy
Being healthy is important for all children, and can be especially important for children with depression or anxiety. In addition to getting the right treatment, leading a healthy lifestyle can play a role in managing symptoms of depression or anxiety. Here are some healthy behaviors that may help:
- Having a healthy eating plan centered on fruits, vegetables, whole grains, legumes (beans, peas, and lentils), lean protein sources, and nuts and seeds
- Participating in physical activity each day based on age
- Getting the recommended amount of sleep each night based on age
- Practicing mindfulness or relaxation techniques
CDC: Children’s Mental Health
CDC: Suicide Prevention
CDC: Bullying Research
CDC: Positive Parenting Tips
CDC: Adolescent and School Mental Health
Stopbullying.gov
- Bitsko RH, Claussen AH, Lichtstein J, Black LJ, Everett Jones S, Danielson MD, Hoenig JM, Davis Jack SP, Brody DJ, Gyawali S, Maenner MM, Warner M, Holland KM, Perou R, Crosby AE, Blumberg SJ, Avenevoli S, Kaminski JW, Ghandour RM. Surveillance of Children’s Mental Health – United States, 2013 – 2019 MMWR, 2022 / 71(Suppl-2);1–42. [Read article]
- Bitsko RH, Holbrook JR, Ghandour RM, Blumberg SJ, Visser SN, Perou R, Walkup J. Epidemiology and impact of healthcare provider-diagnosed anxiety and depression among U.S. children. Journal of Developmental and Behavioral Pediatrics . 2018;39:395-403. [ Read article ]
To receive email updates about this topic, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Early Childhood Depression
How it works
- 1 The Sources
- 2 Annotative Bibliographies
- 3 Take Home Points
- 4 Works Cited
The Sources
The first article is from the ADAA website, which is the Anxiety and Depression Association of America. This association was founded in 1979. It focuses on helping people with these disorders of all ages. They also educate others on how these disorders can affect them or their loved ones. “ADAA strives to improve patient care by promoting implementation of evidence-based treatments and best practices across disciplines through continuing education and trainings and accelerating dissemination of research into practice” (Bhatia). There goal is to eventually be able to prevent and cure disorders like anxiety and depression.
What’s great is that their “passion” is to help people understand these disorders instead of being uncomfortable around them and not talking about them. ADAA is helping to get the conversation started and steering it in the right direction. They started as The Phobia Society of America then expanded to “anxiety disorders, mood disorders, depression, OCD and PTSD” (Bhatia). They have worked very hard over the years to expand the scientific understanding of these disorders in order to better treat them and help educate others about them.
The second article is from NCBI (National Center for Biotechnology Information) website and under the PMC (PubMed Central). NCBI is an organization whose mission is “uncovering new knowledge” (Luby). It was founded in 1988 for the purpose of providing biomedical information so more people can understand the “fundamental molecular and genetic processes that control health and disease” (Luby). This happens to include anxiety and depression because these disorders are often linked to an imbalance of hormones or other environmental causes. They try to gather as much information as possible “nationally and internationally” to help build a bigger understanding in the medical community (Luby). They conduct their own research, collaborate with other institutions, sponsor workshops and lectures, support training in the research field, provide a large variety of sources for people, and promote standards for databases (Luby).
Annotative Bibliographies
The first article from the ADAA is about childhood depression. Many people do not catch childhood depression because they assume that it is just the kids being kids, but the rate of childhood depression has gone up in recent years. Depression is real, and it is definitely real in kids. It has “biological, psychological, and social underpinnings” meaning that these are mostly what causes depression in humans of any age (Bhatia). Children and teenagers are more likely to have depression if a family member has it, but this is only based on probability. Most children with depression go unnoticed. If more parents know the signals to look for they could save their child’s life. Children are more likely to have physical symptoms when depressed but there are other symptoms such as; “loss of interest in fun activities, withdrawal from social or usual pleasurable activities, difficulties with concentration, running away from home, talk about death or dying, sleep increase or decrease, appetite or weight changes, new onset agitation or aggression, and comments indication hopelessness or low self-worth” (Bhatia). They may not have all the symptoms, but they only need to occur on most days for at least 2 weeks for it to be considered depression. Before arriving to the conclusion of it being depression, though, the best thing to do is to rule out any other medical conditions that can cause depression. For example, hypothyroidism, anemia, or a Vitamin D deficiency (Bhatia). It could also be another psychiatric disorder that can also result in depressive symptoms like ADHD. Treatment is important because, if left untreated, it could lead to loss of life for the child. Most treatment involves an assessment, then a referral to a psychiatrist or a psychotherapist, and there could also be some medication involved. Treatment varies on the child, their age, and the degree of their depression. SSRI’s or other antidepressants can be helpful but there is a risk when treating younger children with these. They can increase thoughts of suicide, but my monitoring them and changing the dose as needed as decreased this risk (Bhatia). Treatment will vary if the depression is a symptom of another condition like anxiety or ADHD. Other than their symptoms going unnoticed, many children and teens with depression are simply ignored because of the stigma against mental illnesses. “Research shows that stigma and embarrassment were the top reasons why people with mental illnesses did not engage in medication adherence, such as self-care, therapy, and medication compliance” (Bhatia). If these young children do not get the help they need soon, their illnesses could follow them into their teenage years into high school and on. ADAA is partnered with Bring Change to Mind to encourage people to talk more about mental health and raising awareness about it.
The second article from NCBI is also about early childhood depression. The study of depression in children younger than 6 is fairly new, but research over the past few years has proven against the thought that children of this age are “too immature” to have depressive symptoms (Luby). Researchers have also realized that children of these ages are more mature and intellectual than they thought. They are able to experience the depressive symptoms like guilt and shame. Studies have also shown that they show “alterations in the hypothalamic-pituitary-adrenal axis” just like in adult depression (Luby). Whether depression from this age continues on or reoccurs is still in question. There was a study done on a 4-year-old girl who showed depressive symptoms. She showed “extreme irritability, periods of social withdrawal, negativity, and periods of decreased appetite” (Luby). Her parents noticed these symptoms and their increasing over a period of time and decided to bring her to a mental health clinic. She was uninterested in play or like negative play themes. She was in the right stage of development for her motor and language skills, but she did not enjoy play like someone at her age should (Luby). Diagnosing depression in children of such a young age can be difficult because their depressive symptoms could be associated with another disorder. There is still work to be done to educate parents and others about the signs and symptoms of depression that way one can distinguish if there is really another problem going on. Since this is still so new in the medical community, there are no specific set treatments for depression in preschool children. Psychotherapy has been known to be effective as well as CBT (Cognitive Behavioral Therapy). Tests are being done and they seem promising for future researchers and others to be more informed. PCIT-ED (Parent Child Interaction Therapy-Emotional Development) has also been known to be effective. It is designed to target the child’s emotional development through the use of emotional education. The parent is trained to respond whenever the child has an episode and to coach them through it (Luby). This particular therapy, however; is still in its testing phases. Early intervention is also something that can be tried when treating children of this age. The goal is to teach them how to use their emotions properly and how to recognize them. Early intervention has been known to help in many cases that are not just mental illnesses but also disorders. Children are more likely to suffer from depression if a parent or other relatives has suffered or is suffering from it. Treatment that targets the child is necessary in this situation because emotion development is unavailable (Luby). The use of antidepressants on preschool children is not recommended because of the effects. This would require family members to fully comply with the treatment plan.
Take Home Points
I did not realize that children so young could actually have depression. I, like many others I’m sure, did not think that they had the mental capacity for these emotions yet. But the studies and the information provided by these two articles has proven me wrong. I learned that children of this age need to be monitored more closely when it comes to their emotions because if they go unnoticed, it could be fatal in the future. I also learned that the study of early childhood depression is very rare and that even though the rates of childhood depression are growing, the means to prevent it or treat it are not. Many people are not educated enough on this topic and should realize that it is a real thing that it physically wrong with the person it is affecting. Many children are just brushed off when it comes to their feelings because “kids will be kids”. But this can no longer be used as an excuse to ignore the symptoms of depression in a child. I think that there should be more studies done and more research going on about this topic so that more parents of the world can be educated and learn to recognize the signs so that they can prevent it or treat it. Treatments for teens and adults with depression are so common these days, but no one seems to be thinking that a 5-year-old child can be depressed, too. This is something that the psychological community should be teaching us, not only so we can be more informed about the situation, but so that the stigma against mental illnesses can be removed all together.
Works Cited
Bhatia, Richa, n.d., Childhood Depression, Retrieved from https://adaa.org/learn-from-us/from-the-experts/blog-posts/consumer/childhood-depression
Luby, Joan L., n.d., Early Childhood Depression, Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3184299/
Cite this page
Early Childhood Depression. (2020, Jan 16). Retrieved from https://papersowl.com/examples/early-childhood-depression/
"Early Childhood Depression." PapersOwl.com , 16 Jan 2020, https://papersowl.com/examples/early-childhood-depression/
PapersOwl.com. (2020). Early Childhood Depression . [Online]. Available at: https://papersowl.com/examples/early-childhood-depression/ [Accessed: 10 Jun. 2024]
"Early Childhood Depression." PapersOwl.com, Jan 16, 2020. Accessed June 10, 2024. https://papersowl.com/examples/early-childhood-depression/
"Early Childhood Depression," PapersOwl.com , 16-Jan-2020. [Online]. Available: https://papersowl.com/examples/early-childhood-depression/. [Accessed: 10-Jun-2024]
PapersOwl.com. (2020). Early Childhood Depression . [Online]. Available at: https://papersowl.com/examples/early-childhood-depression/ [Accessed: 10-Jun-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
The effects of parental respect for children's decision-making and respect for human rights on depression in early adolescents: The mediating effect of self-esteem
- Lee, Sangmi
This study investigated the structural relationships among parental respect for children's decision-making, respect for human rights, and self-esteem, and their impact on depression in early adolescents. The study utilized data from 2,747 middle school students who participated in the 2020 Survey on the Current Status of Korean Children's and Youth's Rights conducted by the National Youth Policy Institute. The data were analyzed using a structural equation model based on partial least squares with SmartPLS 3.0. The analysis revealed that both parental respect for children's decision-making and respect for human rights perceived by middle school students had a significant positive impact on self-esteem and a significant negative impact on depression. Furthermore, self-esteem was found to have a significant negative effect on depression. Importantly, self-esteem also played a significant mediating role in the relationship between parental respect for children's decision-making and depression, as well as the relationship between respect for human rights and depression. Therefore, in order to manage depression, it is necessary to develop strategies that encourage parental respect for children's decision-making, promote respect for human rights, and foster self-esteem in early adolescents.

IMAGES
VIDEO
COMMENTS
Introduction. Depression is the principal cause of illness and disability in the world. The World Health Organization (WHO) has been issuing warnings about this pathology for years, given that it affects over 300 million people all over the world and is characterized by a high risk of suicide (the second most common cause of death in those aged between 15 and 29) [World Health Organization ...
Symptoms that may suggest depression include: "Acting out" behaviors, ranging from oppositional defiance to disruptiveness. Anger or irritability. Anxiety. Difficulty at school, including changes in grades or refusing to attend. Fatigue and sleep difficulties, including trouble falling asleep, staying asleep or wanting to sleep much more ...
Signs and symptoms of depression in a child include: Mood changes. Your child might seem sadder or more irritable than usual, and they feel this way most of the time. Lack of interest in fun activities. Low energy levels or general tiredness. Negative self-talk or low self-esteem.
The Characteristics of the Disorder. Childhood depression is an emotional illness that is accompanied by conduct impairment and mood changes. In infants, depression can start to develop from 3 to 4 months of age (Barch et al., 2019). A kid suffering from this illness loses all interest in life and experiences constant apathy.
Evidence currently indicates that depression affects 1 to 3 percent of children before puberty. Early-onset depression is a treatable condition, and treatment is urgent for several reasons. If ...
Depression can show up in children and adolescents as prolonged periods of unhappiness or irritability. It is quite common among older children and teenagers, but often goes unrecognized. Some children might say they feel "unhappy" or "sad". Others might say they want to hurt or even kill themselves. Children and adolescents who ...
In order to gain an in-depth understanding of research about childhood and adolescent depression, this article analyzes the scale, development, and geographic distribution of the literature in the field based on 8491 articles extracted from the Web of Science Core database. Using citation analysis, this article identifies influential journals, scholars, and documents in this field. The study ...
We Have Ruined Childhood. For youngsters these days, an hour of free play is like a drop of water in the desert. Of course they're miserable. Ms. Brooks is a writer. According to the ...
Childhood depression is the main contributor to the heightened cases of runaway children (Thompson, 2010, p. 1). Medical intervention for childhood victims is as successful as that of their adult counterparts (Thompson, 2010, p. 1). One's childhood depressions are a reflection of terminal adult depressions in the individual's life.
Childhood depression is a mental health disorder defined by a sad or irritable mood that is lengthy and severe and is accompanied by changes in motivation, thinking and functioning. It's important to know that more than 18% of children will experience depression before they turn 15. If the sadness or irritability persists for two weeks or ...
Information on childhood depression should be passed on to community members, children, and families with children (Dubuque 1998). Training programs can be implemented for school staff about childhood depression (Dubuque, 1998). ... From simple essay plans, through to full dissertations, you can guarantee we have a service perfectly matched to ...
Children experiencing trauma (eg, witnessing the murder of a family member; sexual assault) are also at elevated risk of several other psychiatric disorders, including depression, PTSD, conduct problems, substance abuse, self-harm, and suicidal thoughts and attempts.8 25 Some forms of physical and psychological abuse in early childhood can be ...
638 Words. 3 Pages. Open Document. for that reason. Children tend to express their sadness by behavioral changes, poor Recognizing the symptoms and early signs of childhood depression, seeking diagnosis and treatment and learning to live with and accept the disorder and still live for yourself are all important steps for knowledgeable parents.
Increased risk of depression in children and adolescents may be due to biologic, psychological, or environmental factors ( Table 1). 2 - 34 In children 12 years and younger, depression is ...
Anxiety and depression affect many children1. 9.4% of children aged 3-17 years (approximately 5.8 million) had diagnosed anxiety in 2016-2019. 4.4% of children aged 3-17 years (approximately 2.7 million) have diagnosed depression in 2016-2019. Anxiety and depression have increased over time2. "Ever having been diagnosed with either anxiety or ...
View Full Essay. Childhood Depression Major depressive disorder, or MDD, may affect up to twenty percent of the adult population. The recognition of depression as a serious and common mental disorder has been vital in the identification and treatment of depression in adults. Leaps and bounds have been made in the field of depression research.
Essay Example: The Sources The first article is from the ADAA website, which is the Anxiety and Depression Association of America. This association was founded in 1979. It focuses on helping people with these disorders of all ages. They also educate others on how these disorders can affect them
This study investigated the structural relationships among parental respect for children's decision-making, respect for human rights, and self-esteem, and their impact on depression in early adolescents. The study utilized data from 2,747 middle school students who participated in the 2020 Survey on the Current Status of Korean Children's and Youth's Rights conducted by the National Youth ...