Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 03 October 2017

Grenfell Tower fire – a tragic case study in health inequalities
- R. G. Watt 1
British Dental Journal volume 223 , pages 478–480 ( 2017 ) Cite this article
19k Accesses
7 Citations
11 Altmetric
Metrics details
- Dental epidemiology
- Dental public health
Highlights that the recent Grenfell Tower fire has raised fundamental policy questions about safety regulation in the UK.
Suggests that, seen through a public health perspective, this tragic incident is ultimately about social inequality in the UK.
Suggests that as general and oral health inequalities are caused by the same underlying factors, the lessons learnt from this tragedy have relevance to oral health professionals committed to tackling social inequalities.
At least 80 people died in the recent Grenfell Tower fire in Kensington and Chelsea, West London. This incident has provoked much anger, debate and reflection on how such a tragedy could happen in London, one of the richest cities in the world. Seen through a public health lens, this disaster is ultimately about social inequality in modern Britain. Kensington and Chelsea is a deeply divided community, where many billionaires and very wealthy people live cheek by jowl with poor and disenfranchised people struggling to make ends meet. It is therefore not a surprise that such a terrible incident should happen in this socially unequal setting where very stark health inequalities already exist. This paper explores some of the broader underlying factors that may have contributed to this tragedy, the political determinants of health. As these factors are linked to both general and oral health inequalities, the lessons learnt from this incident have direct relevance and salience to oral health professionals concerned about tackling social inequalities in contemporary society.
Margaret Whitehead's classic definition of health inequalities as health differences that are 'avoidable, unjust, unfair and unacceptable', 1 perfectly describes the deaths caused by the recent Grenfell Tower fire in West London. On 12 June 2017 a fire started by a faulty fridge freezer in a fourth floor flat in Grenfell Tower, a 24-storey tower block in the Royal Borough of Kensington and Chelsea turned into an inferno in the space of minutes trapping many families, with at least 80 people believed to be dead – although the final death toll is expected to be much higher.
Following the tragic fire many commentators have been asking how such a terrible event could happen in twenty-first century London, one of the richest cities in the world. The UK used to be world renowned for its stringent health and safety record. What has gone so badly wrong for this event, the worst fire in the UK for over a century, to happen? The government has appointed Sir Martin Moore-Bick to lead a public inquiry into the fire and the police are conducting a criminal investigation, but these may take months or even years to report. There is a groundswell of pressure from the surviving victims, the local community and many others for answers to why this tragedy happened. Key questions that need answers include: What were the underlying causes behind this incident? How did public services respond to the unfolding events on 12th June? What are the longer-term policy implications to ensure that this terrible event is not repeated? It has been argued that this disaster is ultimately about social inequalities in modern Britain – a tragic tale of political ineptitude and neglect, disenfranchised and marginalised families ignored by those in positions of power and authority, and public services unable to cope with the immediate and longer-term consequences of the fire. 2 , 3
Although it is important to investigate the potential role of the recently placed cladding and other technical issues in the fire, it is essential that the broader underlying factors of this tragedy are investigated and uncovered. Several years ago the British Medical Journal banned the word 'accidents' in any of its scientific publications, preferring instead the use of the term injury. 4 This was principally because the word 'accident' strongly implied that the event leading to the injury happened by chance, at random. Major incidents like the Grenfell Tower fire do not happen by chance, they are caused by a web of inter-related factors that ultimately lead to the tragedy – the political determinants or as Rose (2008) described, 'the causes of the causes'. 5
The Royal Borough of Kensington and Chelsea is the richest borough in London with a staggeringly high mean income of £116,000 per year. 6 It is home to many billionaires (hence the extremely high mean income) and the average cost of a property is over £2 million. However, it is also characterised by stark economic and social inequality. Wards in the north of the borough, including Notting Barnes (the ward where Grenfell Tower is located), have higher rates of low income households, child poverty and registered homeless people compared to the London average. Although overall life expectancy is higher than the England average, shocking health inequalities exist in this area of West London. For example, life expectancy is 16 years lower for men living in the most deprived areas of Kensington and Chelsea compared to the least deprived. 7 Although the personal details of the victims are not, as yet fully available, it is very apparent that the families affected were mostly from disadvantaged and marginalised backgrounds, including many recent migrants and refugees. National data have shown that injury-related deaths are strongly associated with levels of deprivation, particularly deaths caused by fires. Children living in households where parents never worked or are long-term unemployed are 38 times more likely to die in a fire than children living in families with professional parents. 8 The death toll in Grenfell Tower provides yet more evidence on the grim statistics of deprivation, disadvantage and mortality.
Kensington and Chelsea local authority have been heavily criticised for many years as being out of touch, detached and elitist in nature, only concerned with the interests of their wealthy residents. Although £8.7 million was spent on refurbishing Grenfell Tower in 2016, almost immediately, residents voiced concerns about the fire risks in the newly refurbished building. The Grenfell Action Group, acting on behalf of the local residents complained to the council on ten separate occasions over concerns of the fire hazards in the tower block. All these warnings were totally ignored by those in positions of power. No one listened to the residents' fears. The local population were therefore powerless in their attempts to improve the safety of their homes. Although the council has amassed a budget reserve in excess of £274 million, during the building refurbishment a decision was made to use cheaper quality cladding material to save an estimated £290,000. This is the cladding material that is suspected of rapidly spreading the fire on the exterior of the building due to its combustible nature – a material that is not permitted for use in tall buildings in Germany and many other European countries. Major concerns have also been voiced about the council's immediate response to the unfolding events on 12 June. As the magnitude of the tragedy became apparent and hundreds of surviving victims and residents were in urgent need of help, both practical and emotional, the local politicians seemed incapable of providing the necessary assistance and support. It took days before an organised and effective response was mobilised. Eventually, amid a media frenzy the Conservative leader of the council, Nicholas Paget-Brown, took responsibility for the failings of the council and resigned with immediate effect.
It has also emerged that although fire crews from the London Fire Brigade managed to bravely save the lives of over 250 people from the inferno, the London fire service did not have a sufficiently tall ladder to deal with a fire in a 24-storey tower block and had to borrow a 42 m firefighting platform from Surrey fire service, causing a critical delay in their response and management of the fire. It seems bizarre in the extreme that London, with so many tall buildings and many others under construction, does not have access to the appropriate equipment to deal with fires in tower blocks.
How have national policies contributed to the events in Grenfell Tower? For decades governments of all political persuasions have failed to address the housing crisis in the UK. There is an acute shortage of affordable housing, particularly in the south of England where the costs of the private rental sector are beyond the reach of many. The right to buy policy introduced by Margaret Thatcher in the 1980s has greatly diminished the social housing stock across the country and very few new social housing developments have since been built. Increasingly, social housing has been perceived as the 'dumping ground' for the most marginalised and disadvantaged in society, and the residents vilified as 'scroungers' and social outcasts – see the portrayal of social housing residents in television programmes such as 'Benefits Street'. This combined with a backlash against a health and safety 'culture' has seen a steady relaxation of building regulations and controls. Deregulation, privatisation and the outsourcing of public services are all part of a political neo-liberal ideology that has influenced government policy in many countries across the globe over the last 30 years.
Government regulation is perceived as bad, interfering and stifling red tape. Freed up market forces are seen as the way forward in encouraging enterprise and innovation. In addition, since 2010, austerity measures introduced by the coalition government and continued by the Conservative administration have seen dramatic reductions in local authority budgets including housing inspection and maintenance services. Cuts to the legal aid budget have also had a significant effect in greatly limiting access of legal support for low-income people. With appropriate legal representation perhaps the safety concerns of the Grenfell Tower residents would have been taken seriously by those in positions of authority and the necessary improvements made to avoid the tragic events in June. All these policies have undoubtedly played a role in creating a deeply fractured and unequal society where the most vulnerable and disadvantaged live in unsafe conditions.
The dramatic events at Grenfell Tower may seem very remote and unconnected to oral health. However, the underlying causes and pathways for both general and oral health inequalities are shared. 9 What lessons, therefore, need to be learnt from this tragedy? Seen through a public health lens, the Grenfell fire has provided stark evidence on the social and political determinants of health inequalities – the direct impact of the conditions of living on health, and the need for appropriate upstream policies, including action by national and local government to deal with the housing crisis in this country. 10 , 11 Giving marginalised and disadvantaged people a voice so that their concerns and views are heard by those in positions of power is essential. Political processes and decision making also needs to be more open and accountable so that the needs of local populations, often very diverse backgrounds, are heard and responded to.
Speaking truth to power is a fundamental tenet of public health advocacy. In August 2016 the Joint Strategic Needs Assessment (JSNA) for Kensington and Chelsea focused on housing as a local public health priority, 12 but publication of this report clearly did not avert the subsequent disaster one year later. Public health professionals and other agencies need to be empowered and independent to challenge threats to the health of their local populations. Lastly, the underlying importance of effective regulation and legislation in improving the conditions of daily living needs to be recognised and strengthened. Housing, work places, schools, hospitals and other settings of modern life all need to comply with up-to-date and stringent regulations to ensure their safety and the promotion of health and the well-being of the people living, working and using these settings. This is important for the whole population but particularly for the most vulnerable in society.
The Grenfell Tower fire has been a wake-up call for British society in many different respects. Urgent changes are needed to ensure that the lessons learnt are acted upon to avoid such a tragedy ever happening again.
Whitehead M . The concepts and principles of equity and health. Int J Health Serv. 1992; 22 : 429–445.
Article PubMed Google Scholar
McKee M . Grenfell Tower fire: why we cannot ignore the political determinants of health. BMJ 2017; 357 : j2966. 10.1136/bmj.j2966.
Chakrabortty A . Over 170 years after Engels, Britain is still a country that murders its poor. The Guardian. 2017. Available at https://www.theguardian.com/commentisfree/2017/jun/20/engels-britain-murders-poor-grenfell-tower (accessed August 2017).
Davis R, Pless B . BMJ bans 'accidents'. BMJ 2001; 322 : 1320–1321.
Article PubMed PubMed Central Google Scholar
Rose G . Rose's strategy of preventive medicine . Oxford: Oxford University Press, 2008.
Book Google Scholar
London's Poverty Profile. New analysis of poverty in Kensington and Chelsea. [Internet]. Trust for London, New Policy Institute [cited 2017 Jul 19]. Available at http://www.londonspovertyprofile.org.uk/news/updated-profile-of-kensington/ (accessed August 2017).
Public Health England. Kensington and Chelsea Health Profile 2016. UK Government. Available at http://www.psnc.org.uk/kensington-chelsea-and-westminster-lpc/wp-content/uploads/sites/73/2017/05/2016.pdf (accessed 12 September 2017).
Edwards P, Green J, Roberts I, Lutchmun M . Deaths from injury in children and employment status in family: analysis of trends in class specific death rates. BMJ 2006; 333 : 119–121.
Marmot M, Bell R . Social determinants and dental health. Adv Dent Res 2011; 23 : 201–206.
Marmot M . Fair society, healthy lives: strategic review of health inequalities in England post – 2010. London: Department of Health, 2010.
Sheiham A . Improving oral health for all: focusing on determinants and conditions. Health Educ J 2000; 59 : 64–76.
Article Google Scholar
City of Westminster and Royal Borough of Kensington and Chelsea. Housing support and care: integrated solutions for integrated challenges. Joint Strategic Needs Assessment (JSNA), 2016.
Download references
Author information
Authors and affiliations.
Department of Epidemiology and Public Health, 1–19 Torrington Place, London, WC1E 6BT
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to R. G. Watt .
Additional information
Refereed Paper
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Watt, R. Grenfell Tower fire – a tragic case study in health inequalities. Br Dent J 223 , 478–480 (2017). https://doi.org/10.1038/sj.bdj.2017.785
Download citation
Accepted : 10 August 2017
Published : 03 October 2017
Issue Date : 13 October 2017
DOI : https://doi.org/10.1038/sj.bdj.2017.785
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Share full article
Advertisement
Supported by
Racial Inequities Persist in Health Care Despite Expanded Insurance
A series of studies in an influential medical journal takes a close look at longstanding gaps in medical care.

By Roni Caryn Rabin
Two decades ago, only 9 percent of white Americans rated their health as fair or poor. But 14 percent of Hispanic Americans characterized their health in those terms, as did nearly 18 percent of Black Americans.
In recent years, access to care has improved in the wake of the Affordable Care Act, which reduced the number of uninsured Americans across all racial and ethnic groups. But the racial health gap has remained , according to a series of studies published on Tuesday in the journal JAMA.
A dismal picture of persistent health disparities in America was described in an issue devoted entirely to inequities in medicine. The wide-ranging issue included research on spending and patterns of care, comparative rates of gestational diabetes and the proportion of Black physicians at medical schools.
The journal’s editors committed to a sharper focus on racism in medicine after a controversy in June, in which a staff member seemed to suggest that racism was not a problem in health care. The ensuing criticism led to the resignation of the top editor and culminated with a pledge to increase staff diversity and publish a more inclusive array of papers.
“The topics of racial and ethnic disparities and inequities in medicine and health care are of critical importance,” Dr. Phil B. Fontanarosa, interim editor in chief of JAMA, said in a statement. He noted that more than 850 articles on racial and ethnic disparities and inequities have been published in JAMA and associated journals in the past five years.
The new issue offers studies on disparities in the utilization of health care services and in overall health spending. Together, the findings paint a portrait of a nation still plagued by medical haves and have-nots whose ability to benefit from scientific advances varies by race and ethnicity, despite the fact that the A.C.A. greatly expanded insurance.
The racial health gap did not significantly narrow from 1999 to 2018, according to one study whose author said it was tantamount to “a comprehensive national report card.”
“We’re failing,” added Dr. Harlan Krumholz, the study’s senior author.
“If our national goals are to improve the population’s health and promote more health equity, then we have to admit that whatever we’re doing now is not doing the trick,” he said. “This should wake us up, and spark us to think of new and better approaches.”
Other studies in the journal teased apart factors that may be contributing to the gap, including different patterns of care-seeking. White Americans, for example, are more likely than members of minority groups to visit primary care physicians and specialists in the community, rather than a hospital or emergency room.
The disparity was seen even when Americans from various racial and ethnic backgrounds shared the same insurance, like Medicare , the government health plan for seniors.
“Access to primary care physicians and specialists in the outpatient setting is really important, because they’re managing chronic conditions like diabetes, heart failure, asthma and chronic obstructive pulmonary disease,” said Kenton J. Johnston, an associate professor of health management at Saint Louis University and the lead author of the study.
“If you don’t get in to see the specialist or primary care doctor, you’re going to have complications and problems downstream.”
Dr. Johnston’s study found that minority patients on Medicare have more limited access than white individuals to outpatient health care services.
Despite innovations like Medicare Advantage, which increased access to health care overall, Medicare beneficiaries who are minorities — defined as Black, Hispanic, Native American or Asian-Pacific Islander — still have less access than white or multiracial individuals to a physician who is a regular source of care.
They are also less likely to have influenza and pneumonia vaccinations, and they have more limited access to specialists, the study found.
In Dr. Johnston’s hometown, St. Louis, as in other cities, fewer health care providers and specialists are found in low-income and minority neighborhoods, which is a function of structural racism and a legacy of residential segregation, Dr. Johnston said.
“It’s not a question of insurance — it has more to do with the supply side,” he added. “If you want to access a good specialist, your choice of cardiologists is going to be different if you live out in the counties that are more affluent versus if you live in the poor areas in northern St. Louis.”
Another study in the journal compared health care spending by race and ethnicity, finding that at $8,141 per year, spending for white individuals is higher than for Americans of other races and ethnicities, and the portion of it spent on outpatient care is higher than the average.
Health care spending for Black individuals is $7,361 per year, and a smaller proportion of the funds are spent on outpatient care. The amounts that go to pay for care of Black people in an emergency room and hospital are 12 percent and 19 percent higher, respectively, than the nationwide averages.
“This is about poverty, geography and where people live and where primary care clinics are located, and it is about health insurance,” said Joseph Dieleman, an associate professor at the Institute for Health Metrics and Evaluation at the University of Washington in Seattle and an author of the study.
But the difference also reflects patient behavior. “It is also about people’s past experiences with the health care system and the quality of care they or their loved ones have received, which leads to hesitation or resistance to accessing health care early,” Dr. Dieleman said.
The findings may explain some of the disparities in health outcomes, though social and economic factors also play a role, among them poverty, so-called food deserts and neighborhoods that expose residents to pollution and offer few opportunities for physical exercise and recreation.
Another study compared rates of gestational diabetes, finding that it became more prevalent in pregnant women of all ages and across all races and ethnic groups from 2011 to 2019, with the highest rates reported in Asian Indian women.
Overall, Black women face a much higher risk of dying from pregnancy complications than white women, with maternal mortality rates of 41.7 per 100,000 live births for Black women, compared with 13.4 per 100,000 live births for white women.
The disparity persists even when adjusted for factors like age and income, according to an editorial elsewhere in the journal. Black infant mortality rates are also higher, with death rates of 10.62 per 1,000 live births for Black newborns, compared with 4.68 per 1,000 live births for white babies.
Black patients opt for more preventive care when their physician is Black, according to the editorial, and mortality rates for newborns drop sharply when they are cared for by Black physicians.
The proportion of faculty physicians at American medical schools who identified as Black or African American has only slightly increased over the past 30 years, from 2.6 percent of faculty in 1990 to 3.8 percent of faculty in 2020, still far less than their proportion of the general population, the editorial said.
The pandemic has highlighted longstanding inequities, taking a greater toll on Black and Hispanic communities. An editorial in the journal noted that the health care system has a long history of racism. Hospitals only desegregated when they were threatened with the loss of federal funds from the Medicaid and Medicare programs, which were enacted in 1966.
While the A.C.A. and the expansion of Medicaid in many states has improved access to medical care, the inequities persist. The editorial, written by Alexander N. Ortega and Dylan H. Roby of Drexel University in Philadelphia, called for more investment in research, training, clinical practice and community engagement.
“Ending structural racism and inequities in the U.S. health care system has proved to be a challenge,” the authors wrote.
Because of an editing error, an earlier version of this article incorrectly described the journals that Dr. Phil B. Fontanarosa, interim editor in chief of JAMA, said had published more than 850 articles related to racial disparities. They were published in a variety of journals associated with JAMA, not just JAMA itself.
How we handle corrections
Pregnancy, Childbirth and Postpartum Experiences
Aspirin’s Benefits: Not enough pregnant women at risk of developing pre-eclampsia, life-threatening high blood pressure, know that low-dose aspirin can help lower that risk. Leading experts are hoping to change that.
‘A Chance to Live’: Cases of trisomy 18 may rise as many states restrict abortion. Some women have chosen to have these babies , love them tenderly and care for them devotedly.
Teen Pregnancies: A large study in Canada found that women who were pregnant as teenagers were more likely to die before turning 31 .
Weight-Loss Drugs: Doctors say they are seeing more women try weight-loss medications in the hopes of having a healthy pregnancy. But little is known about the impact of those drugs on a fetus.
Premature Births: After years of steady decline, premature births rose sharply in the United States between 2014 and 2022. Experts said the shift might be partly the result of a growing prevalence of health complications among mothers .
Depression and Suicide: Women who experience depression during pregnancy or in the year after giving birth have a greater risk of suicide and attempted suicide .
- Open access
- Published: 23 March 2023
Why and how has the United Kingdom become a high producer of health inequalities research over the past 50 years? A realist explanatory case study
- Lucinda Cash-Gibson ORCID: orcid.org/0000-0003-3292-5684 1 , 2 , 3 ,
- Eliana Martinez-Herrera 1 , 2 , 4 &
- Joan Benach 1 , 2 , 5
Health Research Policy and Systems volume 21 , Article number: 23 ( 2023 ) Cite this article
2362 Accesses
1 Citations
18 Altmetric
Metrics details
Evidence on health inequalities has been growing over the past few decades, yet the capacity to produce research on health inequalities varies between countries worldwide and needs to be strengthened. More in-depth understanding of the sociohistorical, political and institutional processes that enable this type of research and related research capacity to be generated in different contexts is needed. A recent bibliometric analysis of the health inequalities research field found inequalities in the global production of this type of research. It also found the United Kingdom to be the second-highest global contributor to this research field after the United States. This study aims to understand why and how the United Kingdom, as an example of a “high producer” of health inequalities research, has been able to generate so much health inequalities research over the past five decades, and which main mechanisms might have been involved in generating this specific research capacity over time.
We conducted a realist explanatory case study, which included 12 semi-structured interviews, to test six theoretical mechanisms that we proposed might have been involved in this process. Data from the interviews and grey and scientific literature were triangulated to inform our findings.
We found evidence to suggest that at least four of our proposed mechanisms have been activated by certain conditions and have contributed to the health inequalities research production process in the United Kingdom over the past 50 years. Limited evidence suggests that two new mechanisms might have potentially also been at play.
Conclusions
Valuable learning can be established from this case study, which explores the United Kingdom’s experience in developing a strong national health inequalities research tradition, and the potential mechanisms involved in this process. More research is needed to explore additional facilitating and inhibiting mechanisms and other factors involved in this process in this context, as well as in other settings where less health inequalities research has been produced. This type of in-depth knowledge could be used to guide the development of new health inequalities research capacity-strengthening strategies and support the development of novel approaches and solutions aiming to tackle health inequalities.
Growing evidence demonstrates that avoidable and unfair systematic differences in health outcomes (i.e. health inequalities [HI]) [ 1 ] exist within and between countries [ 2 , 3 , 4 ]. Research on HI is essential to be able to assess the characteristics and trends of HI and to establish their causes, and can be used to inform the design and implementation of policy interventions aiming to reduce HI in different settings. A strong capacity to produce HI research at the local, national and global levels is therefore crucial to be able to understand and work towards addressing HI, yet this capacity does not exist worldwide [ 5 , 6 ]. Despite notable advances and global efforts to invest in and strengthen such research capacities, further concerted efforts are still needed. In this paper, the term HI is used according to Whitehead and Dahlgren’s [ 1 ] conceptualization, and refers to all of the following terms: health disparities, HI, health inequities and social inequalities in health.
A recent bibliometric analysis of the global HI scientific production (1966–2015) identified significant inequalities within this research production worldwide [ 5 ]. The study also found the United Kingdom to be the second-highest global contributor to the HI research field after the United States [ 5 ]. Such findings raise important questions: why and how are some countries able to produce more research on this topic than others, and what types of mechanisms have been involved? Additionally, since scientific research output is generally considered as a proxy indication of research capacity, what do these diverse research outcomes suggest about HI research capacities in different settings? Furthermore, as an example of a “high HI researcher producer”, why and how has the United Kingdom been able to produce such a large volume of HI research during the last 50 years? Which key determinants and causal mechanisms might have been involved in generating this strong national HI research production and capacity over time?
In line with realist inquiries, our study therefore aims to generate valuable causal insights and knowledge about which mechanisms have worked in the United Kingdom, how, and under what conditions, for it to become a high HI research producer. Specifically, we aim to (i) understand why and how the United Kingdom has produced a high volume of HI research over the past five decades; (ii) test six theoretical mechanisms that we propose might have been involved in this national HI research production process over time and (iii) identify evidence to support, refute or refine these hypotheses.
We conducted a realist explanatory case study, which included 12 semi-structured interviews with key informants. Data from the interviews were then triangulated with grey and scientific literature in order to strengthen our overall findings. Explanatory case studies attempt to explain causal relationships, and answer “how” and “why” questions. Realism is a strand of philosophy of science, and realist models of explanation attempt to consider the role of structure and human agency in social change. They aim to reveal the nature of hidden underlying causal forces (i.e. mechanisms) that are sensitive to different contextual conditions, and which can create series of changes that generate certain outcomes of interest [ 7 , 8 , 9 ].
We selected our “unique case of interest” (i.e. an example of a high producer of HI scientific research) based on previous findings of a recent bibliometric analysis [ 5 ]. Combining Pawson and Tilley’s [ 7 ] and Shankardass et al.’s [ 8 ] methodologies for realist evaluations and realist explanatory case studies, we developed our own realist explanatory case study protocol that explains how to design and implement realist explanatory case studies [ 9 ]. The study design included developing (i) a guiding abstract conceptual model based on existing literature on HI research production processes [ 10 ], (ii) a guiding context + mechanism = outcome (CMO) configuration and (iii) the rationale for proposing our theoretical mechanisms that we aim to test and refine through the case study [ 9 ]. The purpose of the guiding CMO configuration is to simplify the main process of interest (i.e. HI research production process) down to its key attributes [ 8 ]. This serves to “artificially isolate” the key combinations of factors that are embedded in specific historical, political and institutional contexts within the United Kingdom (C) and likely interacted over time to activate certain mechanisms (M), which collectively led to our outcome of interest (O) (i.e. high HI research production) [ 7 ].
Through our realist explanatory case study, we aimed to test six theoretical causal mechanisms (M1–M6) that we proposed based on a review of multidisciplinary literature. We hypothesized that these mechanisms might have been involved in this process, with the intention of refining them based on our study findings [ 7 , 9 ]. Table 1 shows the CMO configuration that was created to guide our realist explanatory case study in the United Kingdom. (See the study protocol [ 9 ] for further details on how to design and implement realist explanatory case studies, and the rationale for proposing these six theoretical mechanisms.)
Through the semi-structured interviews, we aimed to understand how and why the United Kingdom’s HI research field was initiated and how it has evolved over the past few decades. Study participants were initially identified from the published HI literature [ 5 ] and invited via email for interview if they met the following inclusion criteria: (i) senior researcher working or having worked in United Kingdom during the last five decades, of any gender; and (ii) has produced (and published) research on HI while working in United Kingdom during the last five decades. Out of the 13 people invited to interview, one potential participant declined to be interviewed.
Interview questions were developed using a political economy perspective and in line with our guiding abstract conceptual model, CMO configuration and supporting literature on HI research production and research capacities (refer to [ 9 , 11 ] for details about the conceptual models). These research questions were tested in a pilot interview conducted by two of the authors and then adjusted accordingly to establish the core set of key questions for the rest of interviews. Participants were asked the following:
Their professional background and initial motivation for working in the field of HI (to establish positionality)
Why and how has the United Kingdom produced such a high volume of HI research over the past five decades, and why and how have certain institutions in the United Kingdom produced more HI research than others?
What key historical, political, research and institutional events might have been important for the initiation and development of the HI research field in the United Kingdom over the past five decades, and why?
Which factors have been important for developing national capacity (human and technical research infrastructure) to conduct HI research in the United Kingdom and why?
Have individual or institutional ideologies and values been important for the process of generating our outcome of interest? If so, why?
What role have research networks played in the HI research field over time?
Twelve interviews were conducted until saturation was attained [ 12 ]. In terms of the profiles of the study participants, the majority of the participants were male ( n = 7) and professors ( n = 11) who worked in different institutions and cities throughout the United Kingdom and had been trained in a range of disciplines, such as political and social sciences, medicine, public health and epidemiology, statistics and geography. Given the sample size, and the well-known profiles of many HI researchers from the United Kingdom, we do not provide further details to preserve study participant anonymity.
Participants signed an informed consent form prior to their interview, in line with ethics approval. Interviews were conducted in English by either one or two of the authors. Five interviews were conducted in person, and seven by teleconference. All interviews were audio-recorded, and one author was responsible for transcribing and translating the audio recordings, which were double-checked. All data were anonymized by the removal of any personal information that might reveal their personal identity. Participants were coded as P1–P12 in the results. The original and anonymized data (audio and transcripts) were stored separately in secure encrypted external hard drives that only the research team had access to. These data were iteratively triangulated with grey and scientific literature, which was identified through snowballing techniques and reviewed with the research questions and interview data in mind. One author initially coded the data using Microsoft Word 10 and analysed all the texts to identify recurrent themes, which were reviewed and agreed on by a second author [ 9 ]. Evidence from the various data sources was then synthesized, examined, interpreted and discussed between the authors until consensus was reached.
Through our case study, we found evidence to support our hypothesis that at least four of our proposed mechanisms (M) have been present and activated by a combination of contextual conditions (C) at different moments over the past five decades, which has likely led to the identified high production of HI research (O) in the United Kingdom [ 5 ]. In particular, we found strong evidence to support our hypotheses that M1 ( recognition with concern ) and M2 ( sense of moral responsibility ) have been present and activated during this process and time period and have contributed to the outcome of interest (O). In addition, based on our study findings, we refined several of our proposed mechanisms (M3, M4, M5 and M6) and identified two new potential mechanisms (M7 and M8) that might have been at play as well (Table 2 ).
M1: recognition with concern
Strong evidence gathered from the different data sources suggests that M1 has been present in the United Kingdom during different moments over the past few decades, and has actively contributed to the initiation and development of the national production of HI research (O). Evidence also suggests that during different historical periods, “recognition” alone has acted as a contextual factor (C); however, once it is combined with “concern” it becomes activated, and together they act as a mechanism of change (M).
The United Kingdom’s production of HI research was established in the 1980s [ 3 , 13 , 14 , 15 ], yet important questions are raised such as why and how was it established. Evidence suggests that “dramatic events” and/or perceptions of socioeconomic crisis [ 16 , 17 , 18 ] lead to public debate, recognition of and widespread concern about socially relevant issues (such as HI), which stimulates active investigation [ 14 , 19 , 20 ]. The following quotes illustrate this:
I think it’s a kind of long running line of debate and concern, political concern…it was really about a kind of moral panic… there are these sort of moments I think, partly political, partly science based, and partly a kind of public outcry about social conditions. (P11: Professor) You get a sudden collection of interests in social inequality, which may be because of either a change of government or a mini-revolution… and people may ask the question, why is there a lot of inequality in these country … So that’s the spark. (P6: Professor)
Prior to the mid-1970s, there had been an economic crisis in the United Kingdom and an increase in social and HI [ 16 , 17 , 21 , 22 ], which triggered “ public outcry [with a] growing public perception of a divided society ” [ 23 ] (p. 484). Also, after the establishment of the United Kingdom’s welfare state and National Health Service (NHS) in the early post-Second World War period, there had been a general assumption that population health would improve and HI would eventually decline, which they initially did [ 14 , 15 ]. Yet, by the 1970s, they had increased once again, which raised concern over the effectiveness of the NHS and related public expenditure [ 15 , 16 , 21 , 24 , 25 ] (C).
Whitehead’s [ 10 ] Action spectrum on inequalities in health model includes recognition of HI as one of the initial activities (C). Whitehead explains that there is already a strong tradition of research and recognition of HI in the United Kingdom, dating back to the nineteenth century, when there were “ pioneering collectors of statistics, also offering social commentary on the data they gathered ” [ 10 ] (p. 480) (C). This, in combination with the new recognition of noticeable “ deteriorating socio-economic conditions [and] worsening health trends ” [ 10 ] (p. 472–3) during the 1960s and 1970s (C), and strategies of “ promoting awareness ” of the problems (C), raised “ voices of concern…about the extent of [HI]” (C, and M1). Whitehead also mentions the role of “ professional advocates ” [ 23 ] (p. 487) and the “ intense professional pressures from health-related bodies and medical journals ” [ 23 ] (p. 483) (C), which in combination with various reports and other actions [ 26 ] helped to raise further awareness and interest in HI (C and/or M1). In addition, the author states that “ concern reached such a level by 1977 that the Labour government was persuaded to set up the [HI] Research Working Group, under the chairmanship of Sir Douglas Black ” [ 10 ] (p. 482) (M1).
The Black Committee was set up to assess national and international evidence on HI and draw up policy implications. The work of this committee led to the famous 1980 Black Report [ 13 , 27 ]. The Black Report was said to have represented a significant shift in political thinking about HI [ 16 ]: it accumulated evidence that confirmed the existence of HI and showed the clear link between health and social position [ 15 ]. Evidence suggests that these findings sparked a key interest in HI and a growth in this research field, both in the United Kingdom (O) and abroad [ 3 , 13 , 27 , 28 ].
We suspect that M1 might have also been activated in 1997, when HI were once again “recognized” as an important issue to be addressed (C) and were placed on the national political agenda by the New Labour (moderate social democratic party) government at the time [ 3 , 15 , 20 , 29 , 30 ] (C). This may have activated M1 at the political level, as the new government then commissioned an independent inquiry into HI, the so-called Acheson Report [ 31 ]. This report provided a comprehensive up-to-date synthesis of the HI scientific evidence and recommendations, mainly consistent with those of the Black Report [ 3 , 15 ]. During this time, there was a strong political commitment to tackling HI [ 30 ], which in turn created favourable HI research conditions (C), such as an increase in dedicated HI research funding (C and/or M4) [ 15 ], resulting in more HI research being produced (O). This process may have occurred again in 2010, when the New Labour government commissioned the English review of the social determinants of health (SDH) (also known as the Marmot Review ) to compile the latest evidence on HI [ 22 , 32 ].
Inhibition of M1: recognition with concern, or a potential new mechanism M7—misrecognition and denial
Interestingly, there is evidence to suggest that the lack of political recognition and concern (M1)—or even misrecognition and denial acting as a potential new mechanism (M7)—regarding HI during the 1980s and 1990s [ 10 ] was important to stimulate the generation of HI research (O). For the sake of chronological continuity in terms of the historical timelines of the HI research production process in the United Kingdom, we include this section on M7 here, since its contents will be important to understand the following sections.
By the time the Black Report was published in 1980 (despite having been commissioned by the former Labour government), the Conservative Thatcher government was in power, and evidence states that they were not keen to acknowledge the evidence and recommendations presented in the report [ 3 , 20 , 33 ]. However, the way in which the Conservative government released the Black Report , dismissed its findings and refuted the evidence on HI triggered an outcry by the public health community and top medical journals, as well as intrigue from the media [ 3 , 18 , 27 , 33 , 34 ] (potentially C and/or M1). As the following quote discusses:
The publication of the Black Report in 1980 was absolutely pivotal… Its fame was fuelled by the fact that the government tried to bury it, and when it couldn’t, it tried to discredit it…that was like a red rag to a bull as far as the medical professional was concerned… and The Lancet and the BMJ… there was a feeling that it was being somehow pushed under the carpet, so as soon as journalists got wind of it, they thought “oh, there’s a story here, you know the government is trying to hide it”, so that helped circulate it. (P8: Professor)
Findings suggest that the Conservative government’s negative reaction (C and/or M7) also “incentivized” certain individuals to act [ 3 , 22 ]. Throughout the 1980s and 1990s, while the Conservative government was in power, there was a sociopolitical and scientific struggle for recognition of HI, both in and outside of academia, determined to prove that HI existed [ 9 , 35 ] (M1 and M2), as the following quotes illustrate:
Back in the ’80s, there was a real attack on any idea that health inequality was real, and a lot of us spent a lot of time on this… we had a big struggle to prove health inequalities exist. (P4: Professor) As a result of Thatcher’s suppression of the health inequalities discourse… it sort of went underground, but equally true, it flourished outside the [central] government public sector…there were lots of Labour local authorities that produced what we used to call “local Black Reports”… and the third sector… [all] working together to keep the flag flying, and the concept alive. (P1: Lecturer)
Furthermore, evidence suggests that the media and certain academic journals have been important for circulating the HI discourse over the years (C) [ 18 , 28 ], due to their “ recognition of the importance of the issue ” [ 18 ] (p. 28) and willingness to publish material on the topic [ 3 , 18 , 26 ]. This likely helped to circulate or “diffuse” HI ideas (C), which were then picked up by others [ 10 , 18 , 36 ]. This process seems to have helped to circulate wider recognition and concern for HI (M1). The follow quote touches on this:
When I first started doing research on health inequalities… [people] didn’t know whether they were higher at the top or bottom … then all the little bits of research on poverty and health, unemployment and health and so on… 10–15 years later you could talk to people … they’d ask what are you doing… you’d [explain] and they would say “what’s the point, isn’t it obvious?” and that was such a huge change. I think that was done though little bits and pieces, over time, by little bits of research coming out in the media ... [creating] a common sense that hadn’t existed earlier. (P5: Professor)
Evidence on M2: sense of moral responsibility to act
Strong evidence, particularly from the interviews, suggests that M2 has been present and has acted during different moments over the past few decades, which has contributed to the development of the national production of HI research (O). All participants reported that individual and institutional values, views and ideology have played an important role (C and/or via M2) in the HI research production process in the United Kingdom over time (O). The following quote explains this:
Certainly, all of my research has been driven by my values…and my commitment—personally and politically—to social justice. So I don’t think my research is biased by that, but it’s driven by that…I think that it’s probably the case for anyone in this field. I just think that some people are more explicit about it than others… for me, health inequalities are profoundly political…You can depoliticize health inequalities in a research frame…but you can’t depoliticize the issue really. (P2: Professor)
During the 1980s and 1990s, it was apparently difficult to obtain funding for HI research, and scholars have since reported that it was “ a lonely time ” for any HI researcher who decided to “ stick it out ” [ 37 ], and that their work was heavily scrutinized [ 28 ]. The presence of strong personal (egalitarian) values and a sense of moral responsibility to address social injustice seem to partly explain why some researchers remained so committed to working in this research field, despite the unfavourable working conditions (M2). In addition, several interviewees also stated that they thought that individual values and views, combined with different disciplinary perspectives and other factors (C), have been important to produce not only HI research (O), but also different types of HI research (i.e. focusing on more upstream or downstream determinants of health and HI). For example:
There are researchers who would focus more on the psychosocial explanations, and there are researchers who would focus more on the social-material conditions, and would maybe have different values around that ... you get these very deep and personally felt controversies… I’m sure there is a whole mix… the psychological and the political, and the two are probably entwined. (P11: Professor) Most people studying health inequalities…identify themselves as left-of-centre, but then there is a really big difference between how left-of-centre, and who they see as their allies…those kinds of personal relationships have an impact on how the field is shaped…there’s political and ideological, and kind of value-based things that everyone is bringing to the field, but they are also bringing their disciplinary training, and their personal likes…and all of those things interact. (P3: Professor)
Evidence on M3 potential refined: Stewardship and/or leadership for HI research
Findings suggest that stewardship and leadership existed at the individual and institutional levels during certain historical periods, which have helped to create an enabling HI research environment (C), and in turn lead to the production of HI research (O). It is unclear whether M3 should remain as “stewardship” or be refined to “leadership”, or whether these are potentially two different mechanisms. Some interview participants discussed the important role of individual HI scientific leadership; for example:
Oh, it will be a story of individuals…a couple of plucky individuals who would have plugged away. (P10: Professor) There have been some really key figureheads, who have set up institutions and they’ve attracted a lot of funding, got a strong reputation, and there’ve been people who have been training through them. (P4: Professor)
Several participants also emphasized the importance of certain academic institutions as HI research stewards and leaders, due to their history and strong tradition within certain cities. These institutions have then attracted certain individuals to work in them (M3 at the individual level). As the following interviews illustrate:
Some of it is the more disadvantaged cities…Liverpool [for example] … it’s very proud of the fact that the city council appointed the first medical officer of health in the country, and then the rest of the country followed, and he was very active in advocating for public health, so [it] has always felt that it’s had a tradition to uphold, and I think that Glasgow is the same . (P8: Professor). I think that institutions or centres within institutions that have either unique or special access to key data are well positioned... For example, UCL [University College London] holds the ’46 and ’58, and ’70s, and also the millennium cohort study, so those are extraordinary resources...So I think there is a kind of science bit, but I also think that the politics of the city is really important…I guess it’s a combination of the history of the city, and the access to datasets…I’m sure lots of other people would say it’s the individuals. I think that maybe the individuals are drawn to cities that have a strong social history or politics. I am not a great believer that science is created by individuals, I think it emerges in particular contexts that are rich for certain sorts of research to develop. (P11: Professor)
Evidence suggests that the United Kingdom’s national research funding institutions, such as the Medical Research Council (MRC), the Economic and Social Research Council (ESRC) [ 3 , 15 , 28 , 37 , 38 ] and the National Institute for Health Research (NIHR) in England [ 39 , 40 , 41 , 42 ], have played important roles in stewarding HI research (M3) at certain points over the past few decades, as well as in investing in and allocating resources to HI research infrastructure (see more examples under M4 on this point). However, evidence suggests that these national research funding institutions have mainly acted as HI research stewards (M3) within supportive political climates [ 18 , 20 , 21 , 36 , 37 , 43 ]. The following quotes highlight this:
A large chunk of the government funding comes through NIHR, through government sources, and that research agenda…so there is a kind of clear link between the political climate of the day and the type of research that gets funded. (P2: Professor) Universities also respond en masse to where the funders are putting the money. So if they legitimize the studies, by doing calls and funding different groups, then the universities will recognize those groups and support them. (P8: Professor)
M4 refined: allocation of dedicated resources for HI research infrastructure—human resources
Findings suggest that the allocation of dedicated resources for HI research infrastructure, specifically related to human resources (M4 refined), has been activated by a number of contextual conditions during different periods, which has helped to produce HI research (O). Over the past five decades, there have been a range of MRC- and ESRC-funded initiatives (M3?) that have provided new resources for strengthening the HI research infrastructure in the United Kingdom, focusing on human resources (M4). These resources have potentially helped to produce HI research (O) via the activation of M3 amongst other things [ 3 , 15 , 38 ]. The following quotes explain the role of the ESRC in building national HI research capacities:
ESRC…decide [d] to fund a big programme and they decided to do that shortly before we had a [New] Labour government…that made clear commitments to reducing health inequalities…and there were a lot of people who were trained during that programme ... [also] there have been specific initiatives from the ESRC to train people in more kind of “more sophisticated quantitative” approaches at various points, and health inequalities researchers have kind of connected to that… [which] have been developed in quite a strategic, conscious way. (P3: Professor) The ESRC got the health variations programme going…in terms of capacity-building it was very enormously successful… [also] the MRC set up a “health of the public” initiative which was pretty much the same…and then obviously the millennium birth cohort study was founded, and once you’ve got something like that, then you get a kind of gravitational pull of early career researchers who want to work on it for their PhDs… So I think it’s a combination of investment in research infrastructure, and then these grants which really provide stepping stones for early career researchers. (P11: Professor)
In addition, the creation of new Master’s programmes, Doctoral fellowships and dedicated research groups within universities (M4 refined) have also been important to develop this particular HI-related human resource capacity, which has led to HI research (O). The following quote illustrates how this has might have occurred:
There are a few senior figures, at various points they will have done some teaching, some PhD supervision…probably been involved in setting up courses, so then you get institutions settings up courses and programmes, specially focused on health inequalities… [also] people who are recognized for having expertise in an issue attract PhD funding and PhD students who want to study an issue. (P3: Professor)
In addition, participants mentioned the 5-year Faculty of Public Health training programme in place that forms part of the NHS and has a strong focus on HI (M4 refined) [ 44 ]. As the following quote explains:
The Public Health training programme in the UK [is] a large investment in a 5-year programme…it's traditionally been a kind of medical programme…but also because it’s been open to non-medics, it means that it is actually a much broader set of expertise…It’s very much framed around health inequalities…it generally takes that as its starting point, the historical work that has been done around health inequalities... [and therefore] there are basically advocates for that approach in every area across the whole country. (P9: Professor)
M4 refined: allocation of dedicated resources for HI research infrastructure—information resources
Evidence suggests that since the nineteenth century, there has been a strong recognition (and concern) of HI (C and M1) and of the need to have a strong research infrastructure in order to develop public health evidence and be able to inform policy and practice [ 15 , 45 , 46 ] (C). For example, in the nineteenth century, the Registrar General decennial censuses were developed in England and Wales, and the work of William Farr introduced the classification of causes of death [ 45 , 46 ]. In the early twentieth century, THC Stevenson incorporated social class (e.g. occupation) into the official death statistics, which led to the Registrar General’s Social Class (RGSC) schema, and published a long series of reports on the distribution of HI by social class, which lasted into the early twenty-first century [ 22 , 46 , 47 , 48 ] (C and/or M4 and potentially M1, M2 and M3). These resources laid important foundations from which a strong body of quantitative evidence on HI has been produced in the United Kingdom (O) [ 15 ]. The following quote explains why these have been important resources:
Some of it is to do with the foresight of some of the people who set up some of the national data collection…the first census was [in] 1838, and almost at the last moment they decided to add age and occupation to the death certificates, and that actually allowed you to do all sorts of things…so we were one of the few countries that actually had some measure of social class attached to the official births and marriages and deaths, so that was very fortuitous and farsighted of them to do that, but they were extraordinary social reforms as well...every 10 years the Registrar General does a social class analysis of all the data—the decennial supplements, and from the very beginning, they are powerfully written documents. (P8: Professor)
Following that, the United Kingdom Office of National Statistics developed the Longitudinal Study that linked census longitudinal data to mortality [ 49 ], the British Regional Heart Study [ 18 ] and the Whitehall Studies, which were set up by various grants [ 15 , 50 ] (M4). In addition, a range of MRC- and ESRC-funded initiatives have helped to strengthen technical resources for health and sociodemographic (e.g. HI-related) research through the country [ 3 , 15 , 38 ] (M4 and M3) . Furthermore, the famous British birth cohorts were created, apparently due to bottom-up foresight and pressure, and top-down investment [ 51 ] (M4). These cohorts have enabled more explanatory models of HI to be proposed (e.g. the psycho-social stress at work, social isolation and life-course perspectives/approaches) (O) [ 15 , 27 ]. The following quotes illustrate the importance of these resources:
I think there has been an enormous farsighted investment in datasets. Like some of the different birth cohorts that have been set up in the UK, fantastic longitudinal studies; that sort of infrastructures and resources and data that goes back a long way, and that requires investment over many decades to maintain it… and support for all sorts of people to use them… actually they are officially called the national treasures, so some people house the national treasures. So nurturing those is really important . (P8: Professor) The birth cohort studies I think is the kind of unique bit of the UK infrastructure. It was all very accidental, and it was people working really hard to try and keep, get the money for the next wave…they got the ’46 money and then they said “right, we need to raise some money to go back”, so it’s been a wave by wave process... these things came together by good will and tenacity, so I don’t think the government had this overarching strategy, I think its scientists pushing very hard and Research Councils responding, and realizing that…I think it’s been very much a bottom up pressure... [this] creation of incredibly rich data . (P11: Professor)
M6 refined: sense of cognitive social capital
Evidence from different state sources suggests that the formation of informal and formal research networks has been extremely important to support HI researchers in a number of ways. These networks have acted as both platforms for and sources of new ideas through the sharing and exchange of knowledge and resources, and have contributed to the creation and activation of a strong sense of cognitive social capital (e.g. social values, norms related to social trust, solidarity/collective efficacy, sharing, and social participation and integration) (M6) [ 9 ]. This has likely interacted with other mechanisms (such as M1 and M2), leading to the coproduction of new HI research (O) [ 11 , 34 ]. The following quotes illustrate this:
It was probably 1976…I always remember thinking that we had a kind of telephone community, and because we all had shared an interest in social justice, we could ring each other up with questions and so on, and always know you would get some help…we were always of course reviewing each other’s research proposals and papers and so on. (P5: Professor) Informal networks, I think that that’s really important…both within countries and between countries, it gives people the academic support, the intellectual support and the personal support…to continue to do the research over four decades, when over that period you get these massive shifts in the political climate. (P2: Professor) The informal stuff is really important…I do think the formal networks kind of catalyse informal connections, connections of trust and respect, and it’s those that then become the kind of stepping stones to closer collaborations. (P11: Professor)
In addition, the United Kingdom has a strong tradition of integrating different disciplinary perspectives and approaches to studying HI, which has been important for developing different types of HI research (O) and a better understanding of HI and their causes [ 11 , 15 , 36 , 38 , 52 , 53 , 54 ], as the following quotes explain:
I think having a health inequalities research tradition that is open at its boundaries to social science has been incredibly important. So in the UK context, the overlap between social inequalities research and health inequalities research…and in the interest in class, and how inequalities and class are reproduced over generations. I think this has been probably an under-acknowledged resource for health inequalities research. (P11: Professor) I guess a lot of the strength of UK research has come through people working… across disciplines and sharing expertise, and synthesizing their approaches… maybe that kind of public health tradition has helped to have a more interdisciplinary approach. (P9: Professor)
These interactions seem to have been important for strengthening the national capacity to produce different types of research HI over time (O).
Potential M8: identification of professional benefits (i.e. potential new intellectual territory) and/or scientific interests
Interestingly, we found some evidence to suggest that M1 and M2 may not have been the only mechanisms present and activated to stimulate or motivate certain academics to work in this research field over the past 50 years. Limited evidence suggests that the identification of other professional benefits (i.e. potential new intellectual territory) and/or scientific interests [ 18 ] (M8?) may have also been activated during certain historical periods, leading to HI research (O). The following quotes illustrate how the identification of scientific interests may have played a role in driving the production of HI research (O):
I’ve always been left wing, and worried about social justice, but being more honest, the real reason I did so much work on [it] was just that the data was good. (P10: Professor) My concern started with scientific interest, “gosh look at this, this is interesting, I wonder how we explain that”… it didn’t start with a strong political commitment... it’s not like my politics led me to do research on health inequalities…my political commitment grew stronger the longer I looked at the evidence, the more I did the research...when I was younger, I was just more interested in doing the research. (P7: Professor)
The following quotes illustrate how the identification of other professional benefits (i.e. potential new intellectual territory) may have played a role in driving the production of HI research (O):
Researchers who don’t have that feeling and passion, will just go where the money is… I mean now [HI research] is more fashionable than it was, better funded than it was, in this country anyway. (P8: Professor) I think that there was a period in which health inequalities looked like a way of creating territory, [an area] that you could then get a job in. (P4: Professor)
For example, with the presence and activation of M8, some researchers may have entered the HI research field at certain points, particularly when the topic became a political and research funding priority (C), and therefore “fashionable” to work on, and with more resources available to foster more HI research to be produced (O). This is in line with previous sociology of science research, which suggests that scientists view themselves as competing with one another for access to resources, credibility and intellectual territory (M8?) [ 18 , 52 , 53 , 55 , 56 ].
Our study provides important insights into why and how the United Kingdom has developed a strong capacity to produce a high volume of HI research over the past five decades. Using a realist explanatory case study approach, we were able to test our six theoretical causal mechanisms (M1–M6). Through the development of the case study, we found strong evidence to suggest that two of these mechanisms (M1 and M2), and potentially three others when refined (M3, M4 and M6 refined), have been present and activated, and have contributed to the United Kingdom’s HI research production process over the past five decades. This evidence suggests that the proposed M5 is potentially the same as M4, just with different types of HI research-related resources involved. We also identified limited evidence to suggest that two other potential mechanisms (M7 and M8) may have also been at play during different historical moments. Our findings also strongly suggest that there has been a combination of key historical socio–political–institutional contextual factors and conditions (C) that activated these mechanisms (M), leading to the increased production of HI research in the United Kingdom (O). Given the exploratory nature of this study, these mechanisms, factors and research processes warrant further investigation, both in the United Kingdom and in other global settings, particularly where lower volumes of HI research have been produced.
How and why the United Kingdom’s HI research field was initiated and has developed
During the 1970s, there was some research produced on HI in the United Kingdom; however, evidence suggests that the national HI research field was not really established until after the publication of the Black Report in 1980 [ 3 , 13 , 14 , 15 ]. The Black Report provided strong evidence on HI (O) and proposed different explanatory models for HI, which evidence states helped to guide further exploration of these ideas and generate more HI research (O) [ 13 , 15 , 22 , 27 ]. In terms of the type of HI research produced, each disciplinary perspective frames the problem of HI differently and provides different accounts of their causes, which makes it challenging to reach consensus on which research findings to follow, and which political approach to take to try to address these inequalities [ 3 , 11 , 15 , 16 , 33 , 52 , 57 ]. However, over time, the United Kingdom has developed a tradition of integrating diverse disciplinary perspectives for the study of HI, which has created novel research and strengthened overall understanding about HI.
Whitehead [ 23 ] characterizes the diffusion of HI ideas during the United Kingdom’s Conservative political period of the 1980s and 1990s as “ confrontational ” [ 23 ], where “ political confrontation [was] met with denial” [ 23 ] (p. 481) (M7?). It was mentioned during the witness seminar of the Black Report that “ the Government at the time was very sensitive to any criticism…they saw the inequalities issue as a direct attack on their policies, so they were very keen to counter any of those arguments” [ 34 ] (p. 164). Scholars also mention how “ egalitarian ideas disappeared from public debate and those with a strong sense of justice became—in effect—closet egalitarians ” [ 19 ] (p. 298) (M7?). Availability of research funding to study HI was also extremely limited during that period [ 37 ], and there have been claims that the Conservative government attempted to suppress reports that presented evidence on HI, such as the Black Report in 1980 [ 34 ] and the Health Divide in 1987 [ 3 , 34 ] , as well as official population data used to conduct research on HI [ 13 , 18 , 27 , 58 , 59 ].
Despite the hostile sociopolitical and research environment in the 1980s and 1990s (C), some HI research was still produced (O). Our case study findings suggest that the controversy around the Black Report ´s publication, the lack of political recognition or concern about—or their denial of—HI (M7?) and the government’s hostility towards evidence of HI in fact fuelled some people to act (via M1 and M2) and produce evidence of HI [ 5 , 10 , 15 , 25 , 60 ]. Again, during the witness seminar of the Black Report , John Fox, a prominent HI research producer in the United Kingdom at the time, stated, “ The government’s disapproval motivated a lot of people…There was a lot of discussion about alternative explanations. And I think that promoted a lot of different research to help to address those issues ” [ 34 ] (p. 168). During this period, there appears to have been a persistent underlying “struggle for recognition” of HI [ 15 , 25 , 34 , 35 , 60 ], mixed with heightened concern (M1). In particular, a number of motivated individuals with strong egalitarian values and a strong sense of moral responsibility to act to address social injustices (M2) persevered in their research efforts (M3?) to prove that HI existed (O). Other research has also identified that many individuals working in HI research and policy in the United Kingdom “ frame health inequalities as a moral issue around which urgent action is required ” [ 61 ] (p. 82). In addition, Garthwaite et al. [ 52 ] identify different types of HI researchers within the United Kingdom who use distinct perspectives and approaches, which “seem to relate to deeply held epistemological and ideological positions” [ 52 ] (p. 475).
Interestingly, some limited findings also alluded to the potential presence and activation of M8?, whereby the identification of professional benefits such as access to resources, credibility and intellectual territory [ 18 , 52 , 53 , 55 , 56 ] and/or scientific interests, besides the activation of M2, may have motivated some individuals to enter this research field at certain points and therefore contributed to the HI research field (O). This mechanism may have been activated in particular when the topic became “fashionable” and a political and research funding priority (C)—for example, after 1997, when New Labour was in power and there was a strong shift in political focus towards addressing HI, although mainly towards the so-called downstream, individual-level determinants of health and HI [ 30 ] as well as a mandate for “policy-relevant” evidence to be produced (C) [ 30 ]. The National Research Council and other research funders subsequently placed HI as a priority research area (M3), which translated into the provision of more resources for strengthening HI research capacities (M4), fuelling the production of HI (O) [ 11 , 41 , 42 , 62 ]. Whitehead (1998) has in fact characterized the “diffusion of HI ideas ” during this time period as “ pragmatism ” [ 23 ] (p. 480). The availability of these new research funding pots and professional opportunities (C and/or M8?) might have incentivized other academics, with or without strong individual and egalitarian values (M2), to enter this research field and start to produce research on HI (O). Furthermore, it may have influenced the type of HI research produced.
Connected to this last point, substantial evidence emphasizes the key roles of politics (C) and research funding (C) in not only influencing the volume of HI research that is produced but also shaping (and framing) the type of HI research produced, and subsequently the type of HI research used to inform policy and practice [ 11 , 15 , 18 , 36 , 38 , 52 , 53 , 54 ]. For example, after 1997, when New Labour was in power, there was a strong political preference towards promoting research focused on downstream determinants of HI [ 15 , 30 , 38 ]. This caused some scholars to raise concern over the predominant policy and research focus on “lifestyle drift” [ 52 , 54 , 63 ] and the “ limit[ed] opportunities to study the impacts of macro-level policy changes ” [ 52 ] (p. 473), which some study participants also touched upon. These findings therefore highlight the importance of evaluating the sociopolitical context in which HI research and research priorities are planned and implemented in different settings when evaluating HI research capacities [ 11 ].
Evidence shows how the United Kingdom has had a unique and strong tradition of recognition and foresight (C) for producing systematic, available and reliable health and sociodemographic data (M4 refined) that are used to produce evidence on HI [ 3 , 15 , 22 ]. The existence of such data has helped to greatly enhance overall understanding of HI [ 3 , 15 , 51 ]. Findings also identified a number of “stewards” and/or “leaders” of HI research, that is, committed individuals and groups and/or supportive institutions (M3?), which have helped to strengthen the national HI research infrastructure over time (M4 refined).
In addition, the formation of research networks (C?) has been important [ 18 , 34 ], particularly informal networks at the beginning, which appear to have formed due to aligned perspectives (M1) and individual (egalitarian) values (M2) amongst other things. Such networks have helped to build trust, solidarity and a strong sense of cognitive social capital within the field of HI (M6). For example, during the Black Report witness seminar, it was mentioned that during the 1980s and 1990s, “lots of people [were] supporting each other, strong networks [were] building up, which didn’t exist before that time” [ 34 ] (p. 168). Interestingly, new public health funding initiatives, such as the MRC United Kingdom Prevention, Research, Partnership programme [ 64 ] (M3), recognize the importance of strengthening transdisciplinary research networks (C) in order to build and establish new perspectives to address complex issues (M6?), with a strong focus placed on the upstream determinants. The programme supports existing research networks, but also actively fosters the formation of new ones (C and/or M?). Hopefully, such initiatives will contribute to addressing concerns about past efforts being excessively focused downstream [ 52 , 54 , 63 ] and will lead to novel ideas and approaches on how to effectively tackle HI.
Key learnings and recommendations
Important learnings can be derived from studying the United Kingdom’s experience of generating a high volume of HI research and in developing a strong HI research capacity in the process. We summarize these learnings in the form of recommendations:
Widespread recognition and concern for HI amongst different agents (i.e. researchers, practitioners, policy-makers and civil servants, as well as civil society and the public) should be fostered. This includes recognition of the benefits of having solid, locally relevant evidence on HI, consistently produced over time, and used to inform future research, policy and practice. This should be accompanied by strengthening public awareness and literacy on HI and its potential causes, in line with the different disciplinary perspectives used to study HI.
The formation of HI research networks should be prioritized and invested in, and should be formed across disciplines, sectors and institutions, to foster a sense of cognitive social capital and coproduce critical research and innovative solutions for tackling HI. In addition, HI-related communication and dissemination channels between different agents (i.e. researchers, practitioners, policy-makers and civil servants, as well as civil society and the public) should be fostered.
Dedicated research funding for HI should be provided, which promotes the use of diverse, integrated, disciplinary perspectives and methods in HI research.
Institutional and individual leaders and stewards for HI research should be fostered and invested in. In addition, investment in and allocation of HI-related human resources should be prioritized in order to foster scientific leadership in HI and develop a critical mass of HI-trained professionals at the local, regional, national and global levels.
The investment and allocation of HI-related information resources should be prioritized to ensure that comprehensive, reliable sociodemographic and health data are consistently produced, collected, monitored and reported over time. This can then be used to inform future research, policy and practice.
More HI research capacity assessments should be developed and conducted at the local, regional, national and global levels to identify HI research capacity strengths, weaknesses and potential information gaps. This valuable information can guide the development of more effective strategies to strengthen HI research capacities.
Study strengths and limitations
As discussed in the study protocol [ 9 ], the realist, mechanism-focused approach can help to reveal previously hidden aspects of a process and an outcome of interest. This approach is highly relevant for answering our research questions and generating understanding on why and how a large production of HI research and strong HI research capacities have been created in the United Kingdom over time. To enhance the study’s rigour, and the validity and credibility of our findings, we provided prior justification for our case selection and proposed mechanisms, which were aligned with existing literature [ 5 , 9 ]. We also triangulated different sources of data in order to test and refine these mechanisms [ 9 , 65 ]. However, there are of course limitations to this approach. For example, since it attempts to simplify the process that leads to the outcome of interest (O), it reduces the predominant study focus to certain mechanisms (M). Therefore, the presence and interaction of a factor (C and/or M) is considered “relevant” only if it appears to cause a significant change to the outcome of interest (O); otherwise it is considered irrelevant and is “abstracted” away through the research process. As a result, other potentially important factors that might contribute to certain outcomes of interest may be missed.
Given the novelty of our work, we encourage more research that explores these mechanisms and processes further, both in the United Kingdom and in other global settings, as well as the perspectives and roles of other stakeholders. A similar historical in-depth realist explanatory case study was recently conducted in the city of Barcelona, which shares a number of similar findings [ 66 ]. A comprehensive comparison of these case study findings would be insightful; however, this is beyond the scope of this study. It will be particularly interesting to conduct similar case studies in contexts where a lower production of HI research has been found, to better understand why and how this outcome has occurred, and what some of the facilitating and inhibiting contextual conditions and mechanisms might be. Lastly, it should be noted that the focus of this study was the production of HI research, rather than the HI research usage process, which is considered to be a separate process [ 11 ] and has been studied in the United Kingdom context [ 36 ].
Important learnings can be derived from the United Kingdom’s experience of generating a high volume of HI research over the past five decades and in developing a seemingly strong HI research capacity in the process. The case study takes a novel approach to exploring the HI research production process in the United Kingdom over the past five decades, and tries to identify the mechanisms and contextual conditions that are potentially involved in generating this high research output. We encourage more realist explanatory case studies to be conducted to explore the HI research production process in different global settings, particularly where less HI research has been produced. This type of in-depth knowledge can help to identify facilitating and inhibiting conditions and mechanisms, and could be used to guide future strategies for strengthening HI research capacities. Strengthening HI research capacities in different countries is essential for the ability to develop new locally relevant research ideas and evidence, which are needed to inform innovative action that aims to tackle HI and improve health for all.
Availability of data and materials
Anonymized data can be made available to the journal editors, if requested.
Abbreviations
Contextual conditions
Economic and Social Research Council
- Health inequalities
Medical Research Council
National Health Service
Outcome of interest
Social determinants of health
- United Kingdom
Whitehead M, Dahlgren G. Concepts and principles for tackling social inequities in health: Levelling up Part 1. 2006. Available: www.euro.who.int .
Mackenbach JP, Bakker M. Reducing inequalities in health: a European perspective. In: Mackenback J, Bakker M, editors. Routledge; 2002.
Berridge V, Blume S. Poor health: social inequality before and after the Black report. In: Blume S, Berridge V, editors. Frank Cass; 2003.
Ashton J, Seymour H. The New Public Health. First. Open University Press; 1988.
Cash-Gibson L, Rojas-Gualdrón DF, Pericàs JM, Benach J. Inequalities in global health inequalities research: a 50-year bibliometric analysis (1966–2015). PLoS ONE. 2018;13:e0191901. https://doi.org/10.1371/journal.pone.0191901 .
Article CAS PubMed PubMed Central Google Scholar
CSDH. Closing the gap in a generation: Health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva; 2008.
Pawson R, Tilley N. Realistic evaluation. USA: SAGE Publications; 1997.
Google Scholar
Shankardass K, Renahy E, Muntaner C, O’campo P. Strengthening the implementation of Health in All Policies: a methodology for realist explanatory case studies. Health Policy Plan. 2015;30:462–73. https://doi.org/10.1093/heapol/czu021 .
Article PubMed Google Scholar
Cash-Gibson L, Martinez-Herrera E, Benach J. What key conditions and mechanisms generate health inequalities research in different contexts? Study protocol for two realist explanatory case studies and critical considerations. Eval Program Plann.
Whitehead M. Diffusion of ideas on social inequalities in health: a European perspective. Milbank Q. 1998;76:469–92. https://doi.org/10.1111/1468-0009.00099 .
Cash-Gibson L, Harris M, Guerra G, Benach J. A novel conceptual model and heuristic tool to strengthen understanding and capacities for health inequalities research. Heal Res Policy Syst. 2020;18:42. https://doi.org/10.1186/s12961-020-00559-z .
Article Google Scholar
Small ML. `How many cases do I need?’. Ethnography. 2009;10:5–38. https://doi.org/10.1177/1466138108099586 .
Townsend P, Whitehead M, Davidson N. Inequalities in Health: The Black Report & the Health Divide. third. Townsend P, Davidson N, editors. Penguin Books Ltd; 1992. Available: http://research-information.bristol.ac.uk/en/publications/inequalities-in-health-the-black-report--the-health-divide-new-third-edition(d343fa63-8cbf-4d4d-ac9f-697c67ab8406)/export.html .
Walker A, Gordon D, Levitas R, Phillimore P, Phillipson C, Salomon M, et al., editors. The Peter Townsend reader. Policy Press; 2010. Available: https://policy.bristoluniversitypress.co.uk/the-peter-townsend-reader .
Bartley M. Health inequality: an introduction to concepts, theories and methods. 2nd ed. USA: Wiley; 2016.
Webster C. Investigating Inequalities in Health before Black. In: Berridge V, Blume S, editors. Poor Health: Social Inequalities before and after the Black Report. Frank Cass; 2003. pp. 81–106.
Dorling D. Injustice: why social inequality still persists. 2nd ed. England: Policy Press; 2015.
Bartley M. Authorities and partisans: the debate on unemployment and health. Edinburgh: Edinburgh University Press; 1992.
Wilkinson R, Pickett K. The Spirit Level: why more equal societies almost always do better. UK: Penguin Books; 2010.
Exworthy M. The “Second Black Report”? The Acheson Report as Another Opportunity to Tackle Health Inequalities. In: Berridge V, Blume S, editors. Poor Health: Social Inequalities before and after the Black Report. Cass; 2003. pp. 175–197.
Szreter S. Health, Class, Place and Politics: Social Capital and Collective Provision in Britain. In: Berridge V, Blume S, editors. Poor Health: Social Inequalities before and after the Black Report. Cass; 2003. pp. 27–57.
Bartley M, Blane D. Reflections on the legacy of British health inequalities research. In: Smith K, Hill S, Bambra C, editors. Health Inequalities Critical Perspectives. Oxford: Oxford University Press; 2016. p. 22–32. https://doi.org/10.1093/acprof:oso/9780198703358.001.0001 .
Chapter Google Scholar
Whitehead M. Diffusion of ideas on social inequalities in health: a European perspective. Milbank Q. 1998;76: 469–92, 306. Available: http://www.ncbi.nlm.nih.gov/pubmed/9738171 .
Tudor HJ. the inverse care law. Lancet. 1971;297:405–12. https://doi.org/10.1016/S0140-6736(71)92410-X .
Berridge V, Blume S. Poor health: social inequality before and after the Black report. UK: Frank Cass; 2003.
Berridge V. The origins of the Black Report: a conversation with Richard Wilkinson. In: Berridge V, Blume S, editors. Poor Health: social inequalities before and after the Black Report. Cass: UK; 2002. p. 120–2.
DHSS. Inequalities in health: report of a working group. (The Black Report). London; 1980.
Macintyre S. Before and after the Black Report: four fallacies. In: Berridge V, Blume S, editors. Poor Health: social inequalities before and after the Black Report. Cass: UK; 2003. p. 198–220.
Scott-Samuel A. Health inequalities recognised in UK. Lancet. 1997;350:753. https://doi.org/10.1016/S0140-6736(05)62561-5 .
Article CAS PubMed Google Scholar
Schrecker T, Bambra C. How politics makes us sick: neoliberal epidemics. UK: Palgrave Macmillan; 2015. https://doi.org/10.1057/9781137463074 .
Book Google Scholar
Acheson D. Independent Inquiry into Inequalities in Health Report. London; 1988.
Fair Society, Healthy Lives: The Marmot Review. Strategic Review of Health Inequalities in England post-2010. 2010.
Blume S. The Black Report Committee on Health Inequalities (1977–80): a personal view of its work. In: Berridge V, Blume S, editors. Poor Health: Social Inequalities before and after the Black Report. Frank Cass: UK; 2003. p. 107–19.
Berridge V. Witness Seminar: the Black Report and The Health Divide. In: Berridge V, Blume S, editors. Poor Health: social inequalities before and after the Black Report. Frank Cass: UK; 2003. p. 131–74.
Recognition (Stanford Encyclopedia of Philosophy). [cited 9 May 2020]. Available: https://plato.stanford.edu/entries/recognition/ .
Smith K. Evidence-informed policy in public health: beyond evidence-based policy in public health. Palgrave Macmillan UK; 2013. https://doi.org/10.1057/9781137026583_2 .
Bartley M, Blane D, Davey SG. Introduction: beyond the black report. Sociol Health Illn. 1998;20:563–77. https://doi.org/10.1111/1467-9566.00119 .
Popay J, Williams G, Thomas C, Gatrell T. Theorising Inequalities in Health: the place of lay knowledge. Sociol Health Illn. 1998;20:619–44. https://doi.org/10.1111/1467-9566.00122 .
Hanney SR, González Block MA. Building health research systems to achieve better health. Heal Res Policy Syst. 2006;4:10. https://doi.org/10.1186/1478-4505-4-10 .
Shergold M, Grant J. Freedom and need: the evolution of public strategy for biomedical and health research in England. Health Res Policy Syst. 2008;6:2. https://doi.org/10.1186/1478-4505-6-2 .
Article PubMed PubMed Central Google Scholar
Hanney SR, Kanya L, Pokhrel S, Jones TH, Boaz A. How to strengthen a health research system: WHO’s review, whose literature and who is providing leadership? Health Res Policy Syst. 2020;18:72. https://doi.org/10.1186/s12961-020-00581-1 .
Hanney S, Kuruvilla S, Soper B, Mays N. Who needs what from a national health research system: lessons from reforms to the English Department of Health’s R&D system. Health Res Policy Syst. 2010;8:11. https://doi.org/10.1186/1478-4505-8-11 .
Muntaner C, Chung H, Murphy K, Ng E. Barriers to knowledge production, knowledge translation, and urban health policy change: Ideological, economic, and political considerations. J Urban Heal. 2012;89:915–24. https://doi.org/10.1007/s11524-012-9699-1 .
UK Faculty of Public Health- Training Curriculum. [cited 7 Jul 2020]. Available: https://www.fph.org.uk/training-careers/specialty-training/curriculum/ .
Farr W. Vital statistics: memorial volume of selections and writings of William Farr. In: Humphreys NA, editor. London: The Sanitary Institute of Great Britain.
Davey-Smith G, Dorling D, Shaw M, editors. Poverty, inequality and health in Britain 1800–2000: a Reader. Bristol: The Policy Press; 2001.
Marmot M, Goldblatt P. Importance of monitoring health inequalities. BMJ. 2013;347:f6576. https://doi.org/10.1136/bmj.f6576 .
Stevenson T. The social distribution of mortality from different causes in England and Wales, 1910–1912. 1923.
Fox AJ, Goldblatt PO. Longitudinal study—socio-demographic mortality differentials 1971–1975. London: HMSO; 1982.
Marmot M, Brunner E. Cohort Profile: the Whitehall II study. Int Epidemiol Assoc Int J Epidemiol. 2005;34:251–6. https://doi.org/10.1093/ije/dyh372 .
Pearson H. The life project: How the study of six generations showed us who we are. UK: Penguin; 2016.
Garthwaite K, Smith KE, Bambra C, Pearce J. Desperately seeking reductions in health inequalities: perspectives of UK researchers on past, present and future directions in health inequalities research. Sociol Heal Illn. 2016;38:459–78. https://doi.org/10.1111/1467-9566.12374 .
Collier T, Smith K. An Atlas of health inequalities and health disparities research: “How is this all getting done in silos, and why?” Soc Sci Med. 2020. https://doi.org/10.1016/j.socscimed.2020.113330 .
Douglas M. Beyond health: why dont we tackle the causes of health inequalities? In: Smith KE, Bambra C, Hill SE, editors. Health inequalities critical perspectives. Oxford: Oxford University Press; 2015.
Gieryn TF. Boundary-Work and the Demarcation of Science from non-science: strains and interests in professional ideologies of scientists. Am Sociol Rev. 1983;48:781. https://doi.org/10.2307/2095325 .
Latour B. Science in action: how to follow scientists and engineers through society. Milton Keynes: Open University Press; 1987.
Blume SS. Explanation and Social Policy: ‘The’ problem of social inequalities in health. J Soc Policy. 1982;11:7–31. https://doi.org/10.1017/s0047279400011296 .
Lawrence J. How ministers fiddle figures. New Society. 1986.
Lies, damned lies, and suppressed statistics. Br Med J. 1986;293: 349–350. https://doi.org/10.1136/bmj.293.6543.349 .
Townsend P, Davidson N, Whitehead M. Inequalities in health: the black report and the health divide. UK: Penguin; 1988.
Smith K, Garthwaite K. Contrasting views on ways forward for health inequalities research. In: Smith K, Hill S, Bambra C, editors. Health inequalities critical perspectives. Oxford: Oxford University Press; 2016. p. 81–94. https://doi.org/10.1093/acprof:oso/9780198703358.001 .
Atkinson P, Sheard S, Walley T. “All the stars were aligned”? the origins of England’s National Institute for Health Research. Health Res Policy Syst. 2019;17:95. https://doi.org/10.1186/s12961-019-0491-5 .
Popay J, Whitehead M, Hunter D. Injustice is killing people on a large scale—but what is to be done about it? J Public Health. 2010;32:148–9.
Council MR. UKPRP—Research—Medical Research Council. [cited 5 Jul 2020]. Available: https://mrc.ukri.org/research/initiatives/prevention-research/ukprp/ .
Yin R. Case study research and applications: design and methods. 4th ed. USA: SAGE Publications; 1999.
Cash-Gibson L, Martinez-Herrera E, Escrig-Pinol E, Benach J. Why and how Barcelona has become a health inequalities research hub? A realist explanatory case study. J Crit Realism. 2022. https://doi.org/10.1080/14767430.2022.2095121 .
Macintyre S. The black report and beyond what are the issues? Soc Sci Med. 1997;44:723–45. https://doi.org/10.1016/S0277-9536(96)00183-9 .
Small ML. Causal thinking and ethnographic research. Am J Sociol. 2013;119:597–601. https://doi.org/10.1086/675893 .
Mitchell JC. Case and situation analysis. Sociol Rev. 1983;31:187–211. https://doi.org/10.1111/j.1467-954X.1983.tb00387.x .
Download references
Acknowledgements
This study formed part of the PhD thesis of the first author. JB gratefully acknowledges the financial support from the Catalan Institution for Research and Advanced Studies (ICREA) under the ICREA Academia programme. However, ICREA did not provide direct financial support for this study. The authors would like to thank Aeve Ribbons and the peer reviewers for their valuable review and comments on a previous version of this paper.
This study received no funding.
Author information
Authors and affiliations.
Department of Political and Social Sciences, Research Group on Health Inequalities, Environment, Employment Conditions Knowledge Network (GREDS-EMCONET), Universitat Pompeu Fabra, Mercè Rodoreda 24 Building, Campus Ciutadella UPF, Ramon Trias Fargas, 25-27, 08003, Barcelona, Catalonia, Spain
Lucinda Cash-Gibson, Eliana Martinez-Herrera & Joan Benach
Johns Hopkins University-Pompeu Fabra University Public Policy Center (UPF-BSM), Barcelona, Catalonia, Spain
UPF Barcelona School of Management (UPF-BSM), Barcelona, Spain
Lucinda Cash-Gibson
Research Group of Epidemiology, National School of Public Health “Héctor Abad Gómez”, University of Antioquia, Calle 62 No. 52–59 Bloque 33 Segundo Piso, Medellín, Colombia
Eliana Martinez-Herrera
Ecological Humanities Research Group (GHECO), Universidad Autónoma, Madrid, Spain
Joan Benach
You can also search for this author in PubMed Google Scholar
Contributions
LCG and JB conceived the idea for the study and conducted the interviews; LCG drafted the manuscript and conducted the first analysis; JB and EMH made substantial contributions to the analysis and manuscript writing. LCG reviewed the consistency of the manuscript and the veracity of data, ensured the approval of all authors and submitted the paper on behalf of the authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Lucinda Cash-Gibson .
Ethics declarations
Ethics approval and consent to participate.
This work has received approval by the Institutional Committee for Ethical Review of Projects (CIREP) at Universitat Pompeu Fabra, Approval Number 138; 31.01.2020.
Consent for publication
Consent for publication of autonomous data was obtained from all study participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Cash-Gibson, L., Martinez-Herrera, E. & Benach, J. Why and how has the United Kingdom become a high producer of health inequalities research over the past 50 years? A realist explanatory case study. Health Res Policy Sys 21 , 23 (2023). https://doi.org/10.1186/s12961-023-00968-w
Download citation
Received : 02 February 2023
Accepted : 17 February 2023
Published : 23 March 2023
DOI : https://doi.org/10.1186/s12961-023-00968-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Research capacities
- Critical realism
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 05 September 2023
A holistic model of health inequalities for health policy and state administration: a case study in the regions of the Czech Republic
- Dana Hübelová 1 ,
- Jan Caha 2 ,
- Lenka Janošíková 2 &
- Alice Kozumplíková 1
International Journal for Equity in Health volume 22 , Article number: 183 ( 2023 ) Cite this article
1371 Accesses
1 Citations
8 Altmetric
Metrics details
Health inequities exist within and between societies at different hierarchical levels. Despite overall improvements in health status in European Union countries, disparities persist among socially, economically, and societally disadvantaged individuals. This study aims to develop a holistic model of health determinants, examining the complex relationship between various determinants of health inequalities and their association with health condition.
Health inequalities and conditions were assessed at the territorial level of Local Administrative Units (LAU1) in the Czech Republic. A dataset of 57 indicators was created, categorized into seven determinants of health and one health condition category. The necessary data were obtained from publicly available databases. Comparisons were made between 2001–2003 and 2016–2019. Various methods were employed, including composite indicator creation, correlation analysis, the Wilcoxon test, aggregate index calculation, cluster analysis, and data visualization using the LISA method.
The correlation matrix revealed strong relationships between health inequality categories in both periods. The most significant associations were observed between Economic status and social protection and Education in the first period. However, dependencies weakened in the later period, approaching values of approximately 0.50. The Wilcoxon test confirmed variations in determinant values over time, except for three specific determinants. Data visualization identified persistently adverse or worsening health inequalities in specific LAU1, focusing on categories such as Economic status and social protection, Education, Demographic situation, Environmental status, Individual living status, and Road safety and crime. The health condition indices showed no significant change over time, while the aggregate index of health inequalities improved with widened differences.
Spatial inequalities in health persist in the Czech Republic, influenced by economic, social, demographic, and environmental factors, as well as local healthcare accessibility. Both inner and outer peripheries exhibit poor health outcomes, challenging the assumption that urban areas fare better. The combination of poverty and vulnerabilities exacerbates these inequalities. Despite the low rates of social exclusion and poverty, regional health inequalities persist in the long term. Effectively addressing health inequalities requires interdisciplinary collaboration and evidence-based policy interventions. Efforts should focus on creating supportive social and physical environments, strengthening the healthcare system, and fostering cooperation with non-medical disciplines.
Health inequalities are viewed as unfair differences resulting from a large number of determinants often of a very different nature [ 1 ]. Ideally, every individual should have an equal opportunity to reach their full health potential, and no one should be disadvantaged in achieving it if such disadvantage can be avoided [ 2 ]. Health inequalities that could be prevented by appropriate means are perceived as the result of inequities in society [ 3 ]. These inequalities begin at birth [ 4 ] and are largely shaped by socioeconomic determinants over the course of one’s life. These are the conditions in which people are born, grow up, live, work and age [ 5 ]. In general, real conditions are shaped by the distribution of finance, energy and global resources at the national and local levels. Health inequalities are caused by government policies affecting the quantity, quality and distribution of determinants and are also influenced by policy decisions [ 6 ].
A body of research demonstrates that preventable systematic inequalities in health exist both between and within societies, and at all hierarchical levels [ 7 , 8 , 9 , 10 , 11 ]. Health inequalities are also spatial between regions, urban and rural areas, and within urban areas [ 12 , 13 ]. While the overall level of health in European Union countries has been improving in recent decades, significant disparities remain for people living in socially, economically or societally disadvantaged conditions [ 14 ].
Given the multitude of factors that influence the emergence of health inequalities, it is desirable that the assessment of the determinants is as comprehensive as possible. This leads us to the idea of forming a holistic concept of health inequalities, even though the holistic approach is more commonly associated with health as such. The holistic approach is closely associated with the concept as emphasized in the study [ 1 ], particularly concerning the approach to the patient and the need to develop tools for systematic healthcare application. By applying this approach, our goal is to contribute to the evaluation of health inequalities through a complex and detailed assessment at the local level. We draw on earlier comprehensive health studies, where the Canadian Health Report “ A new perspective on the health of Canadians” [ 15 ] can be considered the first comprehensive conception of health. The study [ 1 ] proposed a conceptual framework for the social determinants of health, including four highly interrelated categories. The categorization of determinants of health has also been used in other studies [ 16 , 17 ]. The study, which presents a comprehensive perspective on the factors influencing human health [ 18 ], merged the categories from other studies [ 17 , 19 ] to create a broad framework for defining a holistic conceptualization of the determinants of health. However, these determinants are not the same in relation to individual health potential. The study proposed a three-level system with behavioral, social and environmental categories. Determinants in each category (layer) may interact with each other and may interact independently but also collectively with determinants of other categories. Some determinants may be influenced by personal decisions, others by the economic situation or political reform [ 18 ].
Context of health inequalities and research objectives
Several classifications of the determinants of health inequalities and their impact on population health are well-known (refer to, for example, the Conceptual Framework for Action on the Social Determinants of Health [ 20 ]). The influence of various factors on population health has been identified as follows: the genetic basis accounts for 10–15%, health and healthcare contribute 10–15%, the environment contributes 20%, and lifestyle factors contribute 50% [ 21 ]. Additionally, the County Health Ranking Model [ 22 ] uses the following proportions: health and healthcare contribute 20%, the environment contributes 10%, social and economic factors contribute 40%, and lifestyle factors contribute 30%. The Euro-Healthy project [ 14 ] produces a population health index (PHI) for EU countries at the NUTS2 level (regional level unit for the application of regional policies) and to 10 selected metropolitan areas. The results show that systematic spatial inequalities persist in Europe at the NUTS2 level. In a spatial context, the study carried out in France [ 13 ], which presents the Geographical Classification for Health Studies (GeoClasH) is inspiring and thought-provoking due to its focus on the municipal scale while assessing variables from the physical environment, social characteristics of population, and spatial accessibility to healthcare.
Our baseline study on health inequalities [ 2 ] was based on a comprehensive systems analysis in which we formed a methodological and analytical framework to integrate social, economic, demographic, health, environmental, and individual determinants of health inequalities. We created an extensive dataset and visualizations that are available online [ 23 ]. This framework respects a holistic health determinants model for public health [ 1 , 18 ]. The intention of our outputs was to support policy decisions and target-selective health intervention and prevention in the Czech Republic [ 2 ]. The framework is modular and scalable. We also applied different methodological approaches to spatiotemporal analysis and comparison of results [ 24 ].
The intent of the present paper is to extend the original methodological and analytical framework of health inequalities to include the spatiotemporal dimension and the context of geographical classification. The aim of the presented study is to use the example of regions LAU1 (Local Administrative Units, level 1) of the Czech Republic to: 1) evaluate the determinants of health inequalities in space and time, 2) determine the relationship between the categories of determinants of health inequalities and their association with health condition, and 3) develop a holistic health determinants model for public health and test its objectivity in assessing health conditions.
The starting point for the concept of health inequalities
In this paper, we build upon the results of the health inequalities assessment [ 2 , 24 ]. To comprehensively record, analyze, and interpret health inequalities, it is necessary to have the broadest possible set of determinants for these inequalities. Therefore, in determining health inequalities, we start from the original concept of a holistic understanding of health, considering not only genetic and environmental factors but also extending it with additional categories. We divided contextual risk determinants into seven categories (see Appendix 1 with the List of determinants of health and health condition for more details):
A.1 Economic status and social protection (theme Employment rate and Economic conditions and social benefits)
A.2 Education (theme Educational structure)
A.3 Demographic situation (theme Migration, Aging and Urbanization)
A.4 Environmental status (theme Air quality and Countryside)
A.5 Individual living status (theme Living condition and Technical infrastructure)
A.6 Road safety and crime (theme Traffic accidents and Crime)
A.7 Sources of health and social care (theme Health and social care capacities)
Category A.1 Economic status and social protection: Socioeconomic conditions are considered to be an objective cause of spatial variation in health outcomes (e.g., [ 25 , 26 , 27 , 28 , 29 ]), although their importance is debated and the evidence is not entirely consistent [ 30 , 31 ]. Nevertheless, socioeconomic characteristics are a useful differentiator of differences in health status (or mortality; [ 32 ]). Economic status can be indirectly measured by (un)employment rates. Long-term unemployment ranks as a highly stressful life event that affects not only psychological but also physical health [ 33 ]. The social category has been studied, for example, by using indices of deprivation, which are mainly used in social epidemiology [ 34 , 35 , 36 ].
Category A.2 Education: Education has a significant impact on spatial and hierarchical differentials in health inequalities, as well as morbidity and mortality. One disadvantage of formal education indicators is that they fail to capture the socioeconomic positions of adults [ 20 ]. Nevertheless, education remains an input factor for the future structure of occupation and income [ 37 ]. Individuals with lower educational attainment are known to die earlier than those who are more educated [ 26 , 38 ]. Moreover, knowledge and skills acquired through education also influence cognitive ability, health literacy, and health-promoting lifestyle choices [ 39 ].
Category A.3 Demographic situation: The age structure of the population shapes the current health status of the population and will also influence the future situation, including the types of population health interventions [ 40 ]. In the context of demographic aging, there will be an increase in polymorbidity and the prevalence of chronic diseases, especially cardiovascular diseases and degenerative diseases of the nervous system. These conditions are associated with overall health status and the need for outpatient and inpatient care [ 41 , 42 ].
Category A.4 Environmental status: This category includes studies on the external environment that focus on exposure to various environmental components, such as air pollution [ 43 ], noise [ 44 ], water contamination [ 45 ], ultraviolet radiation [ 46 ] or green spaces [ 47 , 48 , 49 , 50 , 51 ]. For the assessment of Environmental status, we chose a combination of air quality indicators and the coefficient of ecological stability. The coefficient represents the proportion of ecologically stable areas, typically including green and blue areas, to unstable areas.
Category A.5 Individual living status: This category includes factors such as housing quality and technical infrastructure, which are considered important contributors to (social) inequalities in health [ 3 , 19 ]. The relationship between the size of living space and subjective well-being is generally considered to be positive. The quality of housing indicator has been used as one of the quality-of-life indicators, for example in [ 52 , 53 ].
Category A.6 Road safety and crime: This category serves as an indicator of inequality, as road accidents are not solely caused by driver error but are influenced by multiple factors, including road users, vehicles, transport infrastructure, and the surrounding environment [ 54 , 55 ]. Crime, on the other hand, is a socially determined phenomenon influenced by various factors, such as the level of social control, sense of community [ 56 ] or income inequality [ 57 ].
Category A.7 Sources of health and social care: The availability and accessibility of health care services are generally improving, although studies indicate lower health care utilization in regions with lower density and availability of medical care [ 58 , 59 , 60 ]. There is an increasing interest in utilizing social care data, including sources of social care, as the demand for both quantity and quality of care rises due to population aging. This necessitates enhancing decision-making processes and transforming public services [ 61 ]. Furthermore, it is crucial to gain a better understanding of social service delivery at the local level [ 62 ].
We examined the impact of categories A.1 to A.7 on the health condition identified as category B.1. The health condition indicators we included were life expectancy by age and sex, which serves as a comprehensive indicator of mortality intensity. In a broader context, life expectancy is considered an indicator of quality of life as it reflects social and economic conditions [ 63 , 64 , 65 ], educational attainment [ 66 ], and the quality and availability of public health and healthcare infrastructure [ 67 ]. Health status indicators, represented by the mortality structure based on the most common causes of death, reproductive health indicators (abortion rate and maturity of a child at birth) and incidence of diabetes are influenced by socioeconomic and demographic determinants [ 68 ].
Material and methods
Spatial differentiation of determinants of health inequalities and health condition was assessed at the territorial level of LAU 1 (Local Administrative Units) in the Czech Republic, which consists of 76 units and the capital city of Prague. The Czech Republic is characterized by a significant fragmentation of the settlement structure and an inconsistent urban network. Differences in the settlement structure, as well as the level of urbanization, are evident in the distribution of the population into size categories of municipalities and the average size of municipalities, which varies significantly across regions. While four LAU1 (NUTS 4) units are directly formed by large cities, highly urbanized LAU1 units are predominantly found in regions with structural challenges. Conversely, the suburban hinterland of large cities lacks representation of any major cities. Figure 1 shows the spatial distribution of urban and rural areas in the Czech Republic, including Prague, the capital city, and Brno, the second-largest city, along with their suburban hinterland. The grey areas represent rural peripheries, typically characterized by inferior locational factors (such as transport accessibility and access to services) and socio-economic indicators (e.g., higher unemployment rates, limited job opportunities, negative population growth, an aging population, etc.). These rural peripheries encompass both internal peripheries within the country and external peripheries located along the borders with neighboring countries (Germany, Poland, Slovakia, and Austria). The hatched areas represent regions with historical structural disadvantages, previously focused on industrial activity.
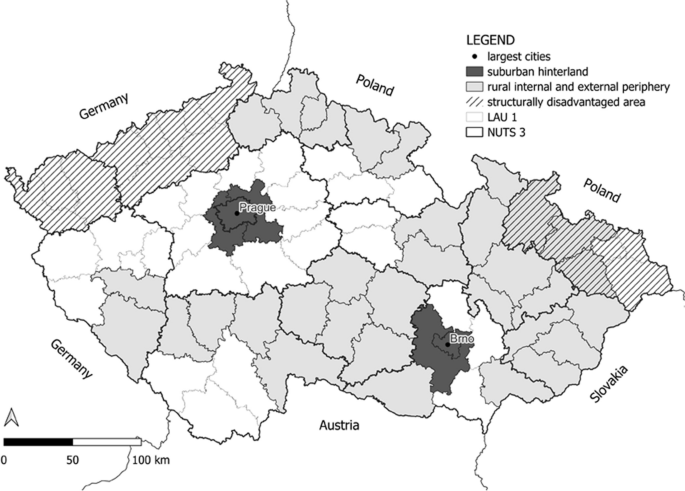
Czech Republic urban and periphery map based on the RDS CZ 2021 +
A dataset was created for each region, comprising 57 indicators. These indicators were divided into seven categories (A.1 to A.7) with a total of 33 health determinants, and one category for health condition (B.1) with 24 health indicators (see Appendix 1 ). The choice of the LAU 1 territorial level was practical, as it allowed us to gather all the necessary data, even though it lacks legislative support in the Czech Republic. Higher territorial units (NUTS2 and NUTS3) have a legal basis but are geographically and economically fragmented in the Czech Republic, making them less significant for our detailed assessment. We obtained data from various publicly available databases (CZSO: Czech Statistical Office, IHIS: Institute of Health Information and Statistics of the Czech Republic, MoLSA: Ministry of Labour and Social Affairs, and CHMI: Czech Hydrometeorological Institute). Our analysis covers two distinct periods: 2001–2003 and 2016–2019, chosen based on data availability. The first period (2001–2003) was selected because it provided data for all the chosen indicators in connection with the implementation of the Census in the Czech Republic. The second period (2016–2019) was chosen to utilize the most up-to-date data available at the time of the research.
The data analyzed corresponds to these specified periods, which were selected due to the unavailability of data for a single matching calendar year (the specific year for which the data was available is stated for each indicator in Appendix 1 ). Two exceptions exist: 1) for variables related to Education, data from the 2011 Census had to be used within the second period; and 2) for variables related to air pollution, data from five-year averages (2007–2011) had to be utilized within the first period.
To facilitate interpretation of the results, a composite indicator (index) was created for each category (A.1 to A.7 and B.1). This index combines multiple variables mathematically and ranges from 0 to 1, with higher values indicating better outcomes. We employed the WSA (Weighted Sum Approach) method, a weighted sum method based on utility maximization principles, to calculate these composite indicators. This method assumes linearity and maximization of all partial utility functions, obtained by normalizing the original input data. The WSA method is based on 3 phases. In the first phase, the evaluation of LAU1 was obtained according to each categories A.1 to A.7 and B.1 (as health condition index) separately and with the equal weights of criteria. In the second phase the same method was used for the complete categories A.1 to A.7 together and with equal weights. This result could be taken as the aggregate index of determinants of health inequalities of each district (see [ 24 ] for more details on the methods). In the WSA method criteria can be minimized or maximized. Two formulas could be applied for the data normalization – formula ( 1 ) for maximization type and (2) for minimization criteria type:
The final ranking is based on the utility – the higher is the better: \(u\left({a}_{i}\right)=\sum_{j=1}^{k}{v}_{j}{r}_{ij}, \forall i=1, \cdots , p.\)
We used Pearson's correlation coefficient for correlation analysis to identify relationships between the categories of health inequalities. The correlation coefficient varies between + 1 through 0 to -1, the closer the value of the correlation coefficient is to one or minus one, the stronger the relationship. Values around zero indicate that the variables have no relationship. Positive values indicate that as one variable increases, the other variable also increases. Negative values indicate that as one variable increases, the other variable decreases. This analysis explored the correlation among categories A.1 to A.7, as well as the correlation between these categories and the health condition category B.1, examining their changes over time. The Wilcoxon test, which assesses the goodness of fit of the mean for data that may not have a normal distribution, was used to test the change in values of individual determinants in all categories. A result below 0.05 indicates a significant change in values over time.
Subsequently, the sub-indexes of categories A.1 to A.7 were utilized to calculate an aggregate index, which provides a single numerical value assessing all determinants of health inequalities. This aggregate index is also employed in the cluster method. Cluster analysis is a multivariate statistical method, working with a large number of variables. An agglomerative clustering was used, the main task of which was to divide the file into several sub-files containing elements with similar variable values. The aim is to maximize inter-cluster variability while minimizing intra-cluster variability. Clustering was carried out as hierarchical, when clusters are created gradually, in individual steps. Distance measurements using a square of Euclidean distance were used to assess the similarities between clusters: \(\sqrt{{(x}_{1}- {x}_{2}{)}^{2}+{(y}_{1}- {y}_{2}{)}^{2}}\) .
Clusters were created using the Ward method, which uses variance. For each formed cluster, we calculated the z-scores of the determinant categories A.1 to A.7 by linearly transforming the original measured values. The z-score helps express the position of individual indices relative to the entire set. A positive sign indicates an observed value above the mean, while a negative sign signifies a value below the mean.
To visualize the data, we employed cartograms generated using the LISA (Local Indicator of Spatial Association) method, which identifies clusters with similar or different values, as well as spatial outliers. The cartograms (Figs. 3 , 4 , and 7 ) use a bivariate legend displaying low values for both indicators in the lower left corner and high values for both indicators in the upper right corner. The hatching in the legend illustrates intervals that are not present in the cartogram. For presenting results that are not primarily spatial in nature, we utilized tables and graphs.
The correlation matrix illustrates the final Pearson correlation coefficient among each category of health inequalities during the periods of 2001–2003 and 2016–2019 (see Fig. 2 ). In the initial period 2001–2003, the strongest relationship is observed between the categories A.1 Economic status and social protection and A.2 Education, with a correlation coefficient of 0.61. Additionally, a significant correlation is found between A.2 Education and A.3 Demographic situation, with a coefficient of -0.56. In the later period of 2016–2019, all dependencies weaken, and the most intense ones approach a coefficient of 0.50, with both positive and negative dependency values. Specifically, the correlation between A.1 Economic status and social protection and A.2 Education is 0.46, while the correlation between A.1 Economic status and social protection and A.3 Demographic situation is -0.47 (see Fig. 2 ).

Correlation matrix of each category of health inequalities in period 2001–2003 and 2016–2019
The Wilcoxon test tested whether there is a change in the values of each determinant over time (2001–2003 and 2016–2019). The results of the test indicated that all values were found to be less than 0.05, suggesting that they do indeed vary over time. However, there were three exceptions where the values were greater than 0.05. These exceptions included the proportion of job seekers with primary education, the population per 1 physician, and standardized mortality due to liver disease.
In our research, the spatiotemporal framework plays a crucial role, particularly in identifying the LAU1s that exhibit the most significant inequalities in health within the studied categories (Fig. 3 ). In the following commentary, we specifically focus on the LAU1s where the assessed categories of health inequalities consistently show adverse or worsening trends over time. For these particular LAU1s, we provide detailed information about their geographical context (Table 1 ).
Category A.1 Economic status and social protection, as well as A.2 Education, consistently remain below average in LAU1s located in both the outer (border) and inner periphery (within NUTS3 administrative boundaries). The values in these regions either remain stable or worsen over time.
In category A.3 The demographic situation, we observe values that are below average or worsening in the regions of the outer and inner periphery. Additionally, the capital city of Prague (LAU1) exhibits similar patterns.
Category A.4 Environmental status shows a deterioration in fifteen LAU1s located in lowland areas. Furthermore, regions focused on extractive and downstream industries consistently exhibit below-average environmental status.
A.5 Individual living status remains below average in LAU1s characterized by a predominantly rural settlement pattern and those located in the northeastern border. Moreover, these values do not significantly change over time.
A.6 Road safety and crime indicate below average values in a small proportion of urbanized LAU1s. Additionally, only five regions have experienced a deterioration in road safety and crime over time.
Category A.7 Sources of health and social care typically demonstrate below-average values in LAU1s that are closely adjacent to core regions. This is due to the hierarchical organization of the health and social care system in the Czech Republic. In some LAU1s located in the inner periphery (at NUTS3 administrative boundaries) or the border periphery, this system has deteriorated.
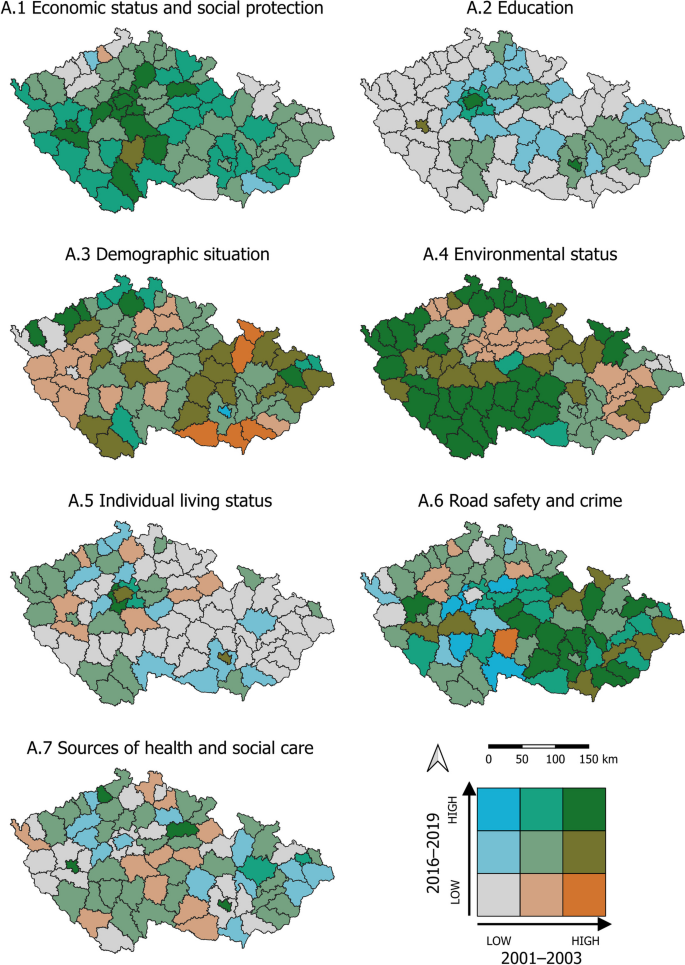
Spatiotemporal change of health determinants of categories A.1 to A.7
The composite indicator B.1 Health condition index was calculated for each LAU1 region and for each period. The values of the B.1 Health condition index did not exhibit significant changes between the periods of 2001–2003 and 2016–2019 across the entire set of LAU1 regions (see Table 2 ). Furthermore, the spatial differentials in the health condition index remained unchanged. In both compared periods, LAU1s with below-average health condition were identified, including structurally affected regions such as West Bohemia and the regions of the northeastern border periphery. Conversely, LAU1s with above-average health condition were found in the capital city of Prague and its suburban hinterland, the north–south central belt, and LAU1s in the southeastern border region.
In the case of the Health condition index, the change over time and space is not particularly positive. Although the value of this index for many LAU1 regions was already relatively high in the first observed period, it did not improve compared to the second period. Out of the total number of LAU1s, 56 (73%) experienced a decline in health condition over time, while only 21 (27%) showed improvement. It should be emphasized that the negative changes observed over time are very slight, with a difference of 0.032 for the mean and 0.033 for the median between 2016–2019 and 2001–2003, but they are supported by the fact that most LAU1s are situated in the negative portion of the "box" section of the chart, indicating a predominance of negative trends in health condition (Fig. 4 ; Change in B.1).
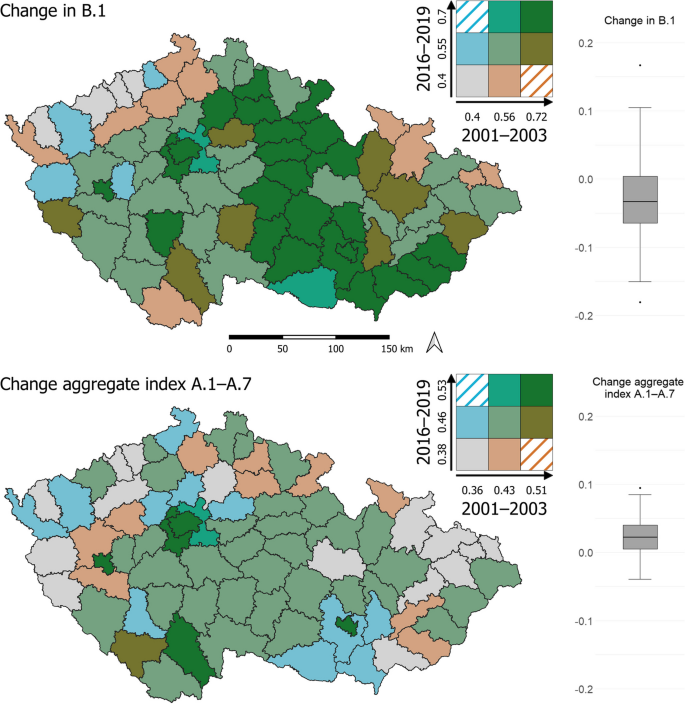
Change in health condition and aggregate index categories of determinants of health inequalities
Moving on to the aggregate index of the categories of determinants of health inequalities, the values improved very slightly between 2001–2003 and 2016–2019 (Table 2 ), but the differences between the values widened in LAU1 regions. In the case of the aggregate health inequality index, the spatial change over time is rather positive. Out of the total number of LAU1s, 14 (18%) experienced a decrease in the aggregate index over time, while 63 (82%) showed improvement. However, the changes over time are relatively weak, with a difference of 0.023 for the mean and 0.022 for the median between 2016–2019 and 2001–2003. Most LAU1s are situated in the positive portion of the "box" section of the diagram (Fig. 4 ; Change aggregate index A.1–A.7).
These observations indicate that while the health condition index remained relatively stable, the aggregate index of health inequalities improved, albeit with wider differences between the values. The majority of LAU1s exhibited positive trends in the aggregate index, reflecting some improvements in health inequalities, although these changes were relatively weak.
In this study, we also aimed to assess the influence of our categories of determinants of health inequalities on health indicators, specifically the health condition. We attempted to assess the relationship between health determinants and health indicators (health condition) based on the results of Pearson's correlation coefficient. The results of the correlation analysis using the Pearson correlation coefficient between categories A.1 to A.7 and category B.1 Health condition are as follows (Table 3 ).
These results are in line with previously published classifications of health determinants and their impact on population health [ 1 , 19 ]. Building upon the original concept of a classification that focuses on health determinants [ 10 , 13 , 19 ], we used our findings to develop a schematic model illustrating the holistic concept of inequalities in health determinants (see Fig. 5 ).
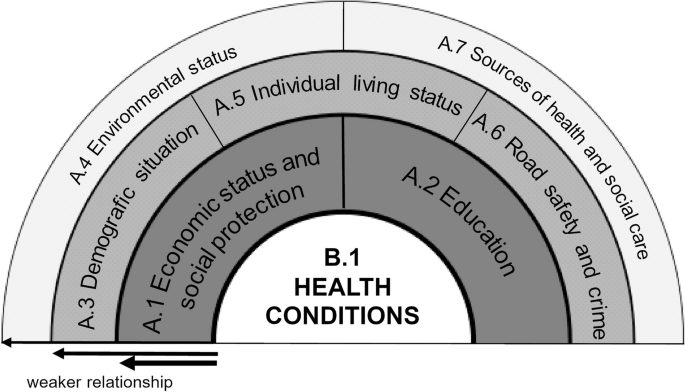
A model of the holistic concept of inequalities of determinants in health (inspired and adapted from [ 19 ])
When comparing the values of individual indices over time in aggregates of all LAU1 between 2001–2003 and 2016–2019, different trends emerge. The majority of categories have shown improvement over time, as indicated by positive values in the middle "box" section of the chart. However, there are noteworthy outliers in the case of A.3 Demographic situation and A.6 Road safety and crime (Fig. 6 ).
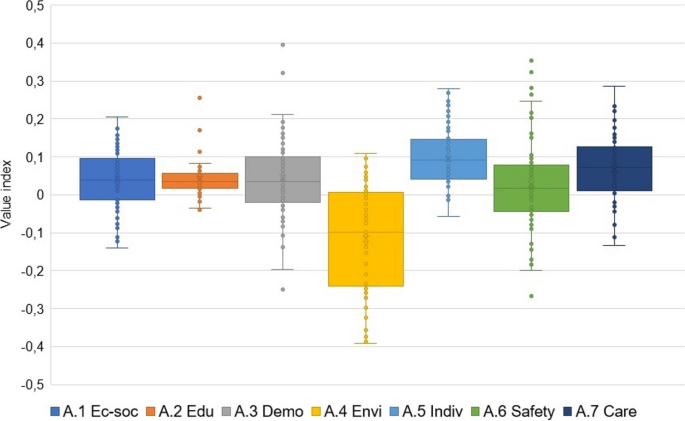
Change in indices of categories of determinants of health inequalities in comparison 2001–2003 and 2016–2019
We once again utilize visualizations to assess spatiotemporal changes. Our assessment focuses on two aspects: i) Examining how the values of the indices for individual categories of health inequalities (A.1 to A.7) in combination with Health condition (B.1) change over time, comparing the two periods (Fig. 7 ). ii) Analyzing how the proportion (%) of LAU1 regions out of the total of 77 changes over time in relation to the values of the indices for categories of health inequalities (A.1 to A.7) with Health condition (B.1) (Table 4 ). It was confirmed that A.1 Economic status and social protection and A.2 Education have the most significant effect on the change of spatial differentiations in the B.1 Health condition index over time. In the group of high values for the category A.1 Economic status and social protection, along with Health condition, the proportion of LAU1 regions increases from 9.1% (of all regions, n = 77) in the period 2001–2003 to 22.1% in 2016–2019. In the low-value group for the category A.1 Economic status and social protection, along with Health condition, there is a negative increase from 3.9% to 10.4% of all LAU1 regions. Similarly, for the category A.2 Education, in the high-value group, the proportion increases from 3.9% to 5.2% of LAU1 regions, while in the low-value group, the negative change is more significant, increasing from 10.4% to 16.9%. Regarding the categories A.3 Demographic situation and A.4 Environmental status, the main observation is the decrease in the proportion of positively assessed regions (from 10.4% to 1.3%; and from 22.1% to 9.1%, respectively). Additionally, for category A.4, the proportion of regions with both low value in this category and low Health condition increases (from 0.0% to 6.5%). In the other categories, there was only one positive change, for A.6 Road safety and crime (from 16.9% to 20.1%). The results show that the values of the categories of determinants of health inequalities improve over time (see Fig. 7 , Table 4 ).
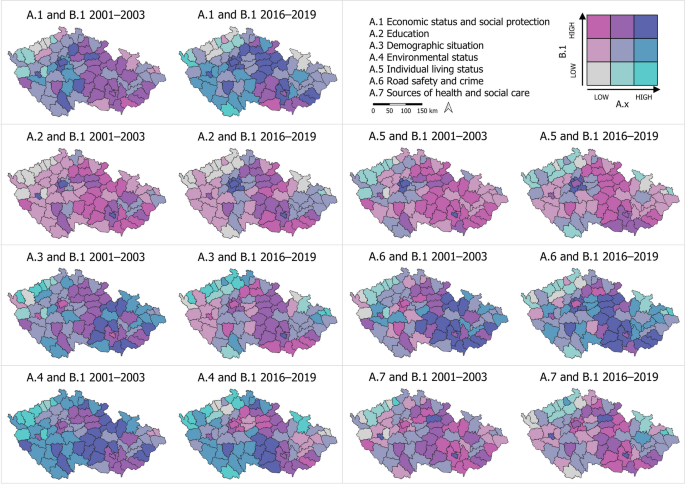
Combination of health inequality category with health condition
For each of the individual categories A.1 to A.7, we selected the percentages (%) of LAU1 regions with high and low values of the indices for both periods. The same procedure was applied for the Health condition index B.1. The selection of "high" and "low" values was based on data visualization, where these values were determined using natural interval calculation (using QGIS). Specifically, the selected regions always correspond to the LAU1 regions in Fig. 7 , represented in the legend by gray (low) or dark blue (high) color. Among the defined categories, A.2 Education, where a low value indicates a low health condition, and A.1 Economic status and social protection, where both high and low values are associated with high and low health condition, play crucial roles. However, the impact of A.4 Environmental status on health condition has diminished over time, particularly for high category values. In the case of A.3 Demographic situation and A.5 Individual living status, the effect on health condition is not significant, as some regions may experience an improvement in health condition despite a decrease in their category values. The influence of A.6 Road safety and crime and A.7 Sources of health and social care on health condition remains relatively unchanged in the area (Table 4 ).
An intriguing finding arises when comparing changes in the "opposite" relationships between determinant categories and health condition. While the proportion of LAU1 regions with a high category value and low health condition is minimal to zero, and the change over time is insignificant, there are more significant changes observed in the combination of a low category value with a high health condition. In these relationships, the proportion of such LAU1s increased for categories A.3, A.4, and A.5, and decreased notably for category A.2, with a lesser extent for A.6 and A.7 (in Table 4 , columns on the right).
The clusters formed based on the aggregate index of health inequality determinants (from categories A.1 to A.7) delineate geographical regions (Fig. 8 ).
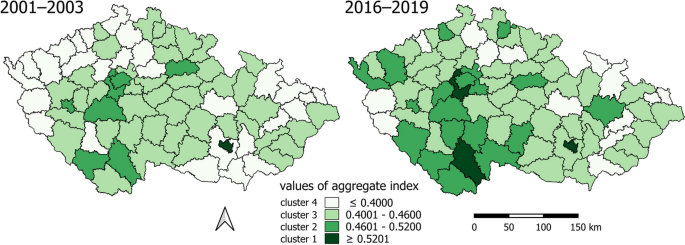
Clusters by aggregate index of determinants of health inequalities
The comparison of spatiotemporal distribution of clusters reveals a favorable change: the proportion of areas with a lower, rather negative value of the aggregate index (light color, clusters 3 and 4) has decreased, while the proportion with a higher, rather positive value (darker color, clusters 1 and 2) has increased:
Cluster 4 exhibits the most pronounced health inequalities. In the period 2001–2003, LAU1 consisted of an urbanized outer periphery and rural inner and outer peripheries. The outer urbanized periphery, particularly in the northwest and northeast, experienced economic development during the industrialization era but now suffers from structural unemployment. The border periphery, settled after World War II, faces below-average social capital, economic challenges, and selective migration, which contribute to social exclusion. A positive finding is a significant decrease in urbanized LAU1s in the outer periphery in 2016–2019.
In contrast, causes of inequality in the rural periphery, whether external or internal, primarily stem from demographic and institutional factors and an inadequate labor market [ 69 ]. The number of these LAU1s also declined in 2016–2019.
Cluster 3 is characterized by significant health inequalities. In the period 2001–2003, it mainly comprises the rural inner periphery, primarily in the central part of the country, and the outer periphery. In 2016–2019, LAU1s from the urbanized outer periphery were added, transitioning from Cluster 1 with the highest health inequalities.
Cluster 2 exhibits more moderate health inequalities. In the period 2001–2003, it consists of a relatively small number of LAU1s, representing developing regions with various-sized cores (cities as NUTS3 and LAU1 centers) and their surrounding areas. Regions in the hinterland of cities are characterized by the diversification of the Czech countryside, experiencing intensive suburbanization, often serving as migratory-income regions with natural population growth, low unemployment rates, and above-average educational attainment. A positive spatiotemporal change is the increase of these regions in Cluster 3 in 2016–2019.
Cluster 1 is characterized by the smallest health inequalities but also includes the fewest LAU1s. It comprises highly urbanized LAU1s, with one additional LAU1 in 2016–2019 as a suburban rural area.
The clusters formed reveal various types of health inequalities and degrees of disadvantage that evolve over time (Fig. 9 ). A negative value in the z-score of a category signifies a disadvantage or inequality that is challenging to mitigate through other means, given the multidimensional nature of health inequalities and the interplay of determinants [ 70 ].
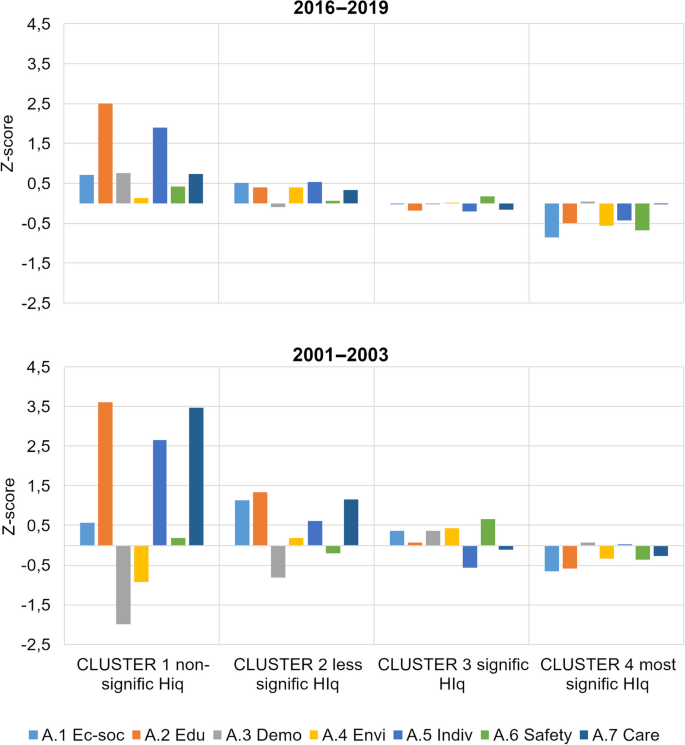
Mean z-score for each of the variables within the clusters
Across all clusters, there has been a moderation of differences in the values of categories related to determinants of health inequalities over time. In clusters 1 and 2, which represent areas with milder inequalities, almost all categories have values in the positive range, indicating an above-average condition. The main improvement in these clusters has occurred in category A.3 Demographic situation. In cluster 3, characterized by more pronounced inequalities, all categories fall around the average values in both periods. Cluster 4, which exhibits the largest health inequalities, shows a stable condition over time, with negative or below-average values.
Leaving aside the genetic basis, environmental, and healthcare factors, socioeconomic factors have a significantly greater influence on health [ 21 , 22 ]. Our results are consistent with previously published classifications of health determinants and their impact on population health [ 1 , 19 ]. The strongest relationships between the categories of determinants of health inequalities and Health condition were observed in A.1 Economic status and social protection [ 27 , 37 , 68 , 70 , 71 ], and A.2 Education [ 32 , 38 , 39 , 66 ]. Based on our findings, we developed a schematic model illustrating the holistic concept of health inequalities determinants. This concept builds upon the original classification that focuses on health determinants [ 10 , 13 , 19 ].
In comparison to epidemiological studies, quantifying the influence of the geographic environment on health inequalities proves challenging due to the identification of numerous determinants with spatial characteristics [ 13 ]. The clusters in cluster analysis align with the concept of peripheries and cores in the Czech Republic. However, characterizing the typical geographic features of clusters in the Czech environment presents difficulties, given the country's specificities in periphery classification. The Czech periphery encompasses both urban and rural regions, requiring a distinction between inner and outer peripheries. Nevertheless, we can assert that the geographic features correspond to fundamental theories of periphery delineation, albeit with consideration of Czech peculiarities. Economic, social, and societal inequalities observed between peripheries and core areas exhibiting high economic performance in the Czech Republic align with the theory of geographical polarization. In the periphery, additional causes of inequality arise alongside economic challenges, as postulated by the theory of cumulative causes [ 72 ]. The rural periphery's current state is shaped by societal and local processes, as well as the transition to post-industrialization, which resonates with the theory of rural restructuring [ 73 ].
The spatial inequalities in health and their consistent trends over time indicate that these inequalities do not occur randomly [ 3 ]. They reflect the uneven distribution of health risks within the context of geographical characteristics. The combined influence of economic, social [ 26 , 27 , 29 ], and environmental factors [ 44 , 50 , 51 ], along with the availability of local health [ 60 , 67 ] and social care [ 7 , 61 ], contribute to regional health disparities. At the spatial scale, both the inner and outer peripheries of LAU1 in the Czech Republic exhibit poorer performance, although it is necessary to differentiate between urban and rural peripheries. The assumption that urban areas perform better than rural areas does not hold true here [ 13 ], although improvements have been observed over time in the urbanized periphery. It is positive that when comparing data from the periods 2001–2003 and 2019–2019, regional health inequalities are decreasing. The share of LAU1 areas with a lower (negative) value of the overall health inequality index is declining, while the share with a higher (positive) value is increasing. The largest health inequalities are observed in LAU1 areas located in urbanized outer peripheries and in rural inner and outer peripheries. Urbanized peripheries suffer primarily from structural unemployment and all its consequences. In rural peripheries, the main issues are related to demographic and institutional factors, as well as insufficient labor market opportunities [ 74 ]. Additionally, unsatisfactory transportation accessibility, civic amenities, and infrastructure [ 75 ], along with selective loss migration, which may exacerbate population aging and unfavorable educational structures, and weak social and cultural capital, are contributing factors [ 76 , 77 ]. The economic, social, and demographic situation in "peripheral rural areas" is based on processes related to labor market development, land use, construction intensity, and property prices [ 78 ].
The combination of poverty and other vulnerability indicators such as age (children, elderly), health disabilities, or minority backgrounds can further amplify these inequalities [ 71 ]. Despite the Czech Republic's relative demographic, social, economic, and ethnic homogeneity, and its low proportion of socially excluded individuals or those living below the poverty line compared to other EU countries, it appears that (micro)regional health inequalities persist in the long term [ 2 ]. Our results, however, demonstrate that there has been an improvement in the status of most determinants of health inequalities. Despite this improvement, the Czech Republic is not as successful in reducing mortality rates and lowering the intensity of mortality, which are factors influencing the resulting Health Condition Index [ 68 , 70 ].
Inequalities in health encompass multiple dimensions, including the number of determinants (categories) and their spatiotemporal aspects [ 13 , 25 , 79 ]. In our comprehensive study, we highlight the necessity of interdisciplinary collaboration across various fields such as medicine, sociology, economics, environmental science, and more to address health inequalities effectively. Only through multi-sectoral collaboration can we devise optimal measures that lead to improvements and strengthen policies based on objective and relevant evidence [ 1 ]. This collaborative approach is arguably a perspective capable of comprehensively analyzing and tackling 21st-century health challenges [ 80 ]. Eliminating or at least mitigating the consequences of health inequalities is not solely an individual concern but, more importantly, a policy issue [ 3 ] hat extends beyond the realm of public health [ 81 ].
Limitations of the study
Geographical contexts can be measured and spatial indices constructed differently across various studies, leading to variations in methodological approaches and geographical frameworks. As a result, the comparability of results becomes limited [ 82 ]. To address this, we deliberately utilized reliable and publicly available data that present fewer methodological challenges and offer detailed geographical and demographic information. The selection of determinants was guided by the need for applicability and adaptability of methods at international, national, and local levels. However, we acknowledge certain data limitations, particularly in terms of comparability over longer time series. For instance, air quality monitoring in the Czech Republic has undergone significant improvements and refinements since 2001. The original nine monitoring stations that measured benzo[a]pyrene have now been expanded to 46 stationary stations, complemented by mobile stations. Consequently, there has been a perceived deterioration in the benzo[a]pyrene indicator over time. This change can be attributed to the enhanced monitoring coverage of local heating sites and long-range transmission, resulting in more accurate data for interpolation purposes.
The outcomes of our study can serve as valuable tools for health policy-making and government decision-making. They support targeted actions to eliminate health inequalities and enhance the health of all population groups, aligning with the adopted Strategic Framework for Healthcare Development in the Czech Republic until 2030. The enhancement of the health of the Czech population should be particularly achieved by providing strategic and conceptual support for lifelong prevention.
The regional dimension of the study also holds significant advantages. Within this context, the results are beneficial as a basis for developing regional health policy concepts or formulating documents at the level of the Czech Republic's regions (NUTS3). By acknowledging regional disparities and the multifaceted causes of health inequalities, the translation of results into tools for precise, specialized prevention in public health becomes possible. Additionally, these results bolster and motivate individual prevention efforts.
The implemented measures should aim to nurture a social and physical environment that fosters health, improves the quality of life, and promotes health-promoting behaviors throughout all stages of life. The prioritized measures include supporting the network of regional health centers and exerting a positive influence on key socio-economic determinants. These determinants encompass reducing poverty, especially among seniors, decreasing unemployment in structurally disadvantaged regions and peripheral areas, fostering regional social cohesion, and enhancing healthcare accessibility. Our results support measures defined by the Strategic Framework that focus not only on supporting education in disease prevention but on introducing health education in both primary and secondary schools, and enhancing health literacy across the Czech population.
The implementation of these objectives and measures necessitates optimizing and integrating the core functions of the healthcare system while fostering collaboration with other non-medical disciplines. By doing so, we can aspire to longer lives free from health limitations and major preventable illnesses.
Availability of data and materials
All data presented in this study are available from official data sources, namely the Czech Statistical Office, the Institute of Health Information and Statistics of the Czech Republic, the Ministry of Labour and Social Affairs, and the Czech Hydrometeorological Institute. The descriptions of all determinants within each category are included in the Appendix 1 . The dataset supporting the conclusions of this article is available in the Zenodo repository, https://doi.org/10.5281/zenodo.8033298 .
Abbreviations
Local Administrative level
Nomenclature of territorial units for statistics
Regional Development Strategy of the Czech Republic 2021 +
Ministry of Labour and Social Affairs
Czech Statistical Office
Czech Hydrometeorological Institute
Institute of Health Information and Statistics of the Czech Republic
Weighted Sum Approach
Local Indicator of Spatial Association
Schoon PM, Krumwiede K. A holistic health determinants model for public health nursing education and practice. Public Health Nurs. 2022;39:1070–7. https://doi.org/10.1111/phn.13063 .
Article PubMed Google Scholar
Hubelova D, Chromkova-Manea BE, Kozumplikova A, editors. Territorial Differentiation of Health Inequalities in the Czech Republic. Prague: Grada press; 2021.
Google Scholar
Marmot M. Fair Society: Health Lives. The Marmot Review. London: Strategic review of health inequalities in England post-2010; 2010.
Chiavarini M, Minelli L, Pieroni L, Salmasi L. Decomposition of health inequalities at birth: A Shapley Value approach. Eur. J. Public Health. 2014;24:cku162–065. https://doi.org/10.1093/eurpub/cku162.065 .
Office of Disease Prevention and Health Promotion. Social Determinants of Health. Healthy People 2030. U.S. Department of Health and Human Services. 2020. https://health.gov/healthypeople/objectives-and-data/social-determinants-health . Accessed on 14 Feb 2021.
WHO. Review of social determinants and the health divide in the WHO European Region: final report. Coppenhagen: WHO Regional Office for Europe; 2014. https://apps.who.int/iris/bitstream/handle/10665/108636/9789289000307-eng.pdf?sequence=1&isAllowed=y .
Graham H. Social determinants and their unequal distribution: clarifying policy understandings. Milbank Q. 2004;82(1):101–24. https://doi.org/10.1111/j.0887-378X.2004.00303.x .
Article PubMed PubMed Central Google Scholar
WHO. Closing the gap in a generation: health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health. Geneva: WHO Press; 2008. https://www.who.int/publications/i/item/WHO-IER-CSDH-08.1 .
Ottersen OP, Dasgupta J, Blouin C, Buss P, Chongsuvivatwong V, Frenk J, et al. The political origins of health inequity: prospects for change. Lancet. 2014;383:630–67. https://doi.org/10.1016/S0140-6736(13)62407-1 .
Cabrera-Barona P, Murphy T, Kienberger S, Blaschke T. A multi-criteria spatial deprivation index to support health inequality analyses. Int J Health Geogr. 2015;14:11. https://doi.org/10.1186/s12942-015-0004-x .
Agenor M. Future Directions for Incorporating Intersectionality Into Quantitative Population Health Research. Am J Public Health. 2020;110(6):803–6. https://doi.org/10.2105/AJPH.2020.305610 .
Lakes T, Brückner M, Krämer A. Development of an environmental justice index to determine socio-economic disparities of noise pollution and green space in residential areas in Berlin. J Environ Plan Manag. 2014;57(4):538–56. https://doi.org/10.1080/09640568.2012.755461 .
Article Google Scholar
Fayet Y, Praud D, Fervers B, Ray-Coquard I, Blay JI, Ducimetiere F, Fagherazzi G, Faure E. Beyond the map: evidencing the spatial dimension of health inequalities. Int J Health Geogr. 2020;19:46. https://doi.org/10.1186/s12942-020-00242-0 .
EURO-HEALTHY consortium. EURO-HEALTHY Population Health Index. The healthyregionseurope webgis. University of Coimbra; 2017. https://healthyregionseurope.uc.pt . Accessed on 14 Jan 2020.
Lalonde M. A new perspective on the health of Canadians. Ottawa: ON Minister of Supply and Services Canada; 1974.
Barton H. A Health Map for Urban Planners: Towards a Conceptual Model for Healthy, Sustainable Settlements. Built Environ (1978-). 2005;31(4):339–55.
Barton H, Grant M, Guise R. Shaping Neighbourhoods: For Local health and Global Sustainability. Bristol: Univerzity of the West England; 2010.
Shi Y, Zhong S. From Genomes to Societies: A Holistic View of Determinants of Human Health. Curr Opin Biotechnol. 2014;28:134–42. https://doi.org/10.1016/j.copbio.2014.03.001 .
Article CAS PubMed Google Scholar
Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health. Background document to WHO - Strategy paper for Europe. Stockholm: Institute for Futures Studies; 1991.
Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). Geneva: WHO; 2010. https://apps.who.int/iris/bitstream/handle/10665/44489/9789241500852_eng.pdf?sequence=1&isAllowed=y . Accessed on 14 Jan 2020.
Marmot M, Wilkinson RG. Social Determinants of Health. 2nd edn. Oxford: Oxford University Press; 2005. https://doi.org/10.1093/acprof:oso/9780198565895.001.0001 . Accessed on 14 Jan 2020.
University of Wisconsin Population Health Institute. Ten-Year Reflections on the County Health Rankings & Roadmaps; 2020. https://www.countyhealthrankings.org/sites/default/files/media/document/CHRR10_year_reflections_report.pdf . Accessed on 14 Jan 2020.
FRRMS MENDELU. Health Index; health-insights.eu [online]; 2020. https://health-insights.eu/en/about-project/ . Accessed on 14 Jan 2020.
Hubelova D, Kuncova M, Vojackova H, Coufalova J, Kozumplikova A, Lategan FS, Chromkova Manea B-E. Inequalities in Health: Methodological Approaches to Spatial Differentiation. Int J Environ Res Public Health. 2021;18(23):12275. https://doi.org/10.3390/ijerph182312275 .
Santana P, Costa C, Freitas A, Stefanik I, Quintal C, Bana e Costa C, et al. Atlas of Population Health in European Union Regions. Coimbra: Imprensa da Universidade de Coimbra; 2017. p. 2017.
Book Google Scholar
Mackenbach JP, Valverde JR, Artnik B, Bopp M, Brønnum-Hansen H, Deboosere P, Kalediene R, Kovacs K, Leinsalu M, Martikainen P, Menvielle G, Regidor E, Rychtarikova J, Rodriguez-Sanz M, Vineis P, White C, Wojtyniak B, Hu Y, Nusselder WJ. Trends in health inequalities in 27 European countries. Proc Natl Acad Sci U S A. 2018;115(25):6440–5. https://doi.org/10.1073/pnas.1800028115 .
Article CAS PubMed PubMed Central Google Scholar
Bosakova L, Rosicova K, Filakovska Bobakova D, Rosic M, Dzurova D, Pikhart H, Lustigova M, Santana P. Mortality in the Visegrad countries from the perspective of socioeconomic inequalities. Int J Public Health. 2019;64(3):365–76. https://doi.org/10.1007/s00038-018-1183-6 .
Costa C, Santana P, Dimitroulopoulou S, Burstrom B, Borrell C, Schweikart J, Dzurova D, Zangarini N, Katsouyanni K, Deboseree P, Freitas Â, Mitsakou C, Samoli E, Vardoulakis S, Marí Dell’Olmo M, Gotsens M, Lustigova M, Corman D, Costa G. Population Health Inequalities Across and Within European Metropolitan Areas through the Lens of the EURO-HEALTHY Population Health Index. Int J Environ Res Public Health. 2019;16(5):836. https://doi.org/10.3390/ijerph16050836 .
Costa C, Freitas Â, Stefanik I, Krafft T, Pilot E, Morrison J, Santana P. Evaluation of data availability on population health indicators at the regional level across the European Union. Popul Health Metr. 2019;17(1):11. https://doi.org/10.1186/s12963-019-0188-6 .
Elstad JI. Health-related mobility, health inequalities and gradient constraint. Discussion and results from a Norwegian study. Eur J Public Health. 2001;11(2):135–40. https://doi.org/10.1093/eurpub/11.2.135 .
Manor O, Matthews S, Power C. Health selection: the role of inter- and intra-generational mobility on social inequalities in health. Soc Sci Med. 2003;57(11):2217–27. https://doi.org/10.1016/s0277-9536(03)00097-2 .
Davey Smith G, Hart C, Hole D, MacKinnon P, Gillis C, Watt G, Blane D, Hawthorne V. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998;52(3):153–60. https://doi.org/10.1136/jech.52.3.153 .
Norström F, Waenerlund AK, Lindholm L, Nygren R, Sahlén KG, Brydsten A. Does unemployment contribute to poorer health-related quality of life among Swedish adults? BMC Public Health. 2019;19(1):457. https://doi.org/10.1186/s12889-019-6825-y .
Carstairs V, Morris R. Deprivation: explaining differences in mortality between Scotland and England and Wales. BMJ. 1989;299(6704):886–9. https://doi.org/10.1136/bmj.299.6704.886 .
Rey G, Jougla E, Fouillet A, Hémon D. Ecological association between a deprivation index and mortality in France over the period 1997–2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health. 2009;9:33. https://doi.org/10.1186/1471-2458-9-33 .
Pornet C, Delpierre C, Dejardin O, Grosclaude P, Launay L, Guittet L, Lang T, Launoy G. Construction of an adaptable European transnational ecological deprivation index: the French version. J Epidemiol Community Health. 2012;66(11):982–9. https://doi.org/10.1136/jech-2011-200311 .
Lahelma E, Martikainen P, Laaksonen M, Aittomäki A. Pathways between socioeconomic determinants of health. J Epidemiol Community Health. 2004;58(4):327–32. https://doi.org/10.1136/jech.2003.011148 .
Petrelli A, Di Napoli A, Sebastiani G, Rossi A, Giorgi Rossi P, Demuru E, Costa G, Zengarini N, Alicandro G, Marchetti S, Marmot M, Frova L. Italian Atlas of mortality inequalities by education level. Epidemiol Prev. 2019;43(1S1):1–120. https://doi.org/10.19191/EP19.1.S1.002 .
Kickbusch IS. Health literacy: addressing the health and education divide. Health Promot Int. 2001;16(3):289–97. https://doi.org/10.1093/heapro/16.3.289 .
Srivarathan A, Jensen AN, Kristiansen M. Community-based interventions to enhance healthy aging in disadvantaged areas: perceptions of older adults and health care professionals. BMC Health Serv Res. 2019;19(1):7. https://doi.org/10.1186/s12913-018-3855-6 .
Ramos LR, Tavares NU, Bertoldi AD, Farias MR, Oliveira MA, Luiza VL, Pizzol TD, Arrais PS, Mengue SS. Polypharmacy and Polymorbidity in Older Adults in Brazil: a public health challenge. Rev Saude Publica. 2016;50(suppl 2):9s. https://doi.org/10.1590/S1518-8787.2016050006145 .
O’Connell MDL, Marron MM, Boudreau RM, Canney M, Sanders JL, Kenny RA, Kritchevsky SB, Harris TB, Newman AB. Mortality in Relation to Changes in a Healthy Aging Index: The Health, Aging, and Body Composition Study. J Gerontol A Biol Sci Med Sci. 2019;74(5):726–32. https://doi.org/10.1093/gerona/gly114 .
WHO. 2018. Ambient (outdoor) air quality and health. www.who.int [online]; 2018. https://www.who.int/news-room/factsheets/detail/ambient-(outdoor)-air-quality-and-health . Accessed 12 Sept 2019.
WHO. Environmental noise guidelines for the European Region. Coppenhagen: WHO Regional Office for Europe; 2019.
Roh T, Lynch CF, Weyer P, Wang K, Kelly KM, Ludewig G. Low-level arsenic exposure from drinking water is associated with prostate cancer in Iowa. Environ Res. 2017;159:338–43. https://doi.org/10.1016/j.envres.2017.08.026 .
Savoye I, Olsen CM, Whiteman DC, Bijon A, Wald L, Dartois L, Clavel-Chapelon F, Boutron-Ruault MC, Kvaskoff M. Patterns of Ultraviolet Radiation Exposure and Skin Cancer Risk: the E3N-SunExp Study. J Epidemiol. 2018;28(1):27–33. https://doi.org/10.2188/jea.JE20160166 .
James P, Hart JE, Banay RF, Laden F. Exposure to Greenness and Mortality in a Nationwide Prospective Cohort Study of Women. Environ Health Perspect. 2016;124(9):1344–52. https://doi.org/10.1289/ehp.1510363 .
Crouse DL, Pinault L, Balram A, Hystad P, Peters PA, Chen H, van Donkelaar A, Martin RV, Ménard R, Robichaud A, Villeneuve PJ. Urban greenness and mortality in Canada’s largest cities: a national cohort study. Lancet Planet Health. 2017;1(7):e289–97. https://doi.org/10.1016/S2542-5196(17)30118-3 .
Crouse DL, Pinault L, Balram A, Brauer M, Burnett RT, Martin RV, van Donkelaar A, Villeneuve PJ, Weichenthal S. Complex relationships between greenness, air pollution, and mortality in a population-based Canadian cohort. Environ Int. 2019;128:292–300. https://doi.org/10.1016/j.envint.2019.04.047 .
Rojas-Rueda D, Nieuwenhuijsen MJ, Gascon M, Perez-Leon D, Mudu P. Green spaces and mortality: a systematic review and meta-analysis of cohort studies. Lancet Planet Health. 2019;3(11):e469–77. https://doi.org/10.1016/S2542-5196(19)30215-3 .
Sun S, Sarkar C, Kumari S, James P, Cao W, Lee RS, Tian L, Webster C. Air pollution associated respiratory mortality risk alleviated by residential greenness in the Chinese Elderly Health Service Cohort. Environ Res. 2020;183:109139. https://doi.org/10.1016/j.envres.2020.109139 .
OECD. How's Life? 2020: Measuring Well-being, Paris: OECD Publishing; 2020. https://doi.org/10.1787/9870c393-en . Accessed 12 Sept 2021.
Eurofound. European Quality of Life Survey. www.eurofound.europa.eu/ [online]; 2021. https://www.eurofound.europa.eu/data/european-quality-of-life-survey . Accessed 12 Dec 2021.
Christie N. Why we need to view road safety through a public health lens? Transp Rev. 2018;38(2):139–41. https://doi.org/10.1080/01441647.2018.1411226 .
Touahmia M. 2018. Identification of Risk Factors Influencing Road Traffic Accidents. Eng. Technol. Appl. Sci. Res., 2018;8(1):2417–2421. https://doi.org/10.48084/etasr.1615 .
Nolan JJ. Establishing the statistical relationship between population size and UCR crime rate: Its impact and implications. J Crim Just. 2004;32(6):547–55. https://doi.org/10.1016/j.jcrimjus.2004.08.002 .
UNODC. Global study on homicide 2019. Vienna: Division for Policy Analysis and Public Affairs, United Nations Office on Drugs and Crime; 2019. https://reliefweb.int/attachments/32341c33-60a1-3c34-809a-fa17d766aed1/Booklet1.pdf
Guagliardo MF. Spatial accessibility of primary care: concepts, methods and challenges. Int J Health Geogr. 2004;3(1):3. https://doi.org/10.1186/1476-072X-3-3 .
Tanke MA, Ikkersheim DE. A new approach to the tradeoff between quality and accessibility of health care. Health Policy. 2012;105(2–3):282–7. https://doi.org/10.1016/j.healthpol.2012.02.016 .
Šídlo L, Maláková K. Spatial Healthcare Accessibility: A District-Level Analysis of Travel for Outpatient Diabetology in Czechia. Healthcare (Basel). 2022;10(2):395. https://doi.org/10.3390/healthcare10020395 .
Foster M, Harris J, Jackson K, Glendinning C. Practitioners’ Documentation of Assessment and Care Planning in Social Care: The Opportunities for Organizational Learning. Br J Soc Work. 2008;38(3):546–60. https://doi.org/10.1093/bjsw/bcl366 .
Chotvijit S, Thiarai M, Jarvis S. Big data analytics in social care provision: spatial and temporal evidence from Birmingham. In Proceedings of the 19th Annual International Conference on Digital Government Research: Governance in the Data Age (dg.o '18). Association for Computing Machinery, New York. 2018;5:1–8. https://doi.org/10.1145/3209281.3209300 .
Elo IT. Social Class Differentials in Health and Mortality: Patterns and Explanations in Comparative Perspective. Annu Rev Sociol. 2009;35(1):553–72. https://doi.org/10.1146/annurev-soc-070308-115929 .
Kaikkonen R, Rahkonen O, Lallukka T, Lahelma E. Physical and psychosocial working conditions as explanations for occupational class inequalities in self-rated health. Eur J Public Health. 2009;19(5):458–63. https://doi.org/10.1093/eurpub/ckp095 .
Aittomäki A, Martikainen P, Laaksonen M, Lahelma E, Rahkonen O. The associations of household wealth and income with self-rated health–a study on economic advantage in middle-aged Finnish men and women. Soc Sci Med. 2010;71(5):1018–26. https://doi.org/10.1016/j.socscimed.2010.05.040 .
Leinsalu M, Vågerö D, Kunst AE. Estonia 1989–2000: enormous increase in mortality differences by education. Int J Epidemiol. 2003;32(6):1081–7. https://doi.org/10.1093/ije/dyg192 .
Ho JY, Hendi AS. Recent trends in life expectancy across high income countries: retrospective observational study. BMJ. 2018;362:k2562. https://doi.org/10.1136/bmj.k2562 .
Hübelová D, Kozumplíková A, Walicová V. The Mortality Structure of Populations the Demographic and Socio-Economic Situation in European Union Countries: Development and Differentiation in the Period 2011–2014. Eur. Spat. Res. Policy. 2020a;27(1):173–193. https://doi.org/10.18778/1231-1952.27.1.08 .
Friedmann J. A General Theory of Polarized Development. In: Hansen NM, editor. Growth Centers in Regional Economic Development. New York: The Free Press; 1972. p. 82–107.
Hübelová D, Kozumplíková A, Kosová P, Walicová V. Relationship between Socio-demographic and Economic Determinants of Cause-Specific Mortality in the EU Countries in the Period 2011–2014. Geographia Cassoviensis. 2020b;14(2). https://doi.org/10.33542/GC2020-2-01 .
Chen E, Martin AD, Matthews KA. Socioeconomic status and health: do gradients differ within childhood and adolescence? Soc Sci Med. 2006;62(9):2161–70. https://doi.org/10.1016/j.socscimed.2005.08.054 .
Myrdal G. Economic Theory and Under-Developed Regions by Gunnar Myrdal. London: G. Duckworth; 1957.
Marsden T, Lowe P, Whatmore S. Rural Restructuring: Global Processes and Their Responses. London: David Fulton Publishers Ltd.; 1990.
Bernard J. Kompletní jmenná databáze kandidátů do zastupitelstev měst a obcí jako nástroj pro výzkum populace kandidátů a zastupitelů. Acta politologica. 2013;5(1):82–93 (in Czech).
Gløersen E, Michelet J, Corbineau C, Perez-Soba M, van Eupen M, Roupioz, LFS, Schuiling C. European Perspective on Specific Types of Territories: Final Report. Geneva: ESPON, University of Geneva; 2012.
Chromý P, Skála J. Kulturněgeografické aspekty rozvoje příhraničních periferií: analýza vybraných složek územní identity obyvatelstva Sušicka. Geografie. 2010;115: 223–246. https://doi.org/10.37040/geografie2010115020223 . (in Czech).
Pileček J, Chromý P, Jančák V. Social Capital and Local Socio-economic Development: The Case of Czech Peripheries. Tijdschr Econ Soc Geogr. 2013;104(5):604–20. https://doi.org/10.1111/tesg.12053 .
Marsden T, Murdoch J, Lowe P, Munton R, Flynn A. Constructuring The Countryside: An Approach To Rural Development. 1st ed. London: Routledge; 1993.
Arcaya MC, Tucker-Seeley RD, Kim R, Schnake-Mahl A, So M, Subramanian SV. Research on neighborhood effects on health in the United States: A systematic review of study characteristics. Soc Sci Med. 2016;168:16–29. https://doi.org/10.1016/j.socscimed.2016.08.047 .
Pourbohloul B, Kieny MP. Complex systems analysis: towards holistic approaches to health systems planning and policy. Bull World Health Organ. 2011;89(4):242. https://doi.org/10.2471/BLT.11.087544 .
Thomson K, Hillier-Brown F, Todd A, McNamara C, Huijts T, Bambra C. The effects of public health policies on health inequalities in high-income countries: an umbrella review. BMC Public Health. 2018;18(1):869. https://doi.org/10.1186/s12889-018-5677-1 .
Abel GA, Barclay ME, Payne RA. Adjusted indices of multiple deprivation to enable comparisons within and between constituent countries of the UK including an illustration using mortality rates. BMJ Open. 2016;6(11):e012750. https://doi.org/10.1136/bmjopen-2016-012750 .
Download references
This research was supported by the Internal Grant Agency FRRMS MENDELU (Grant number: GA-FRRMS-22–015).
Author information
Authors and affiliations.
Department of Social Studies, Mendel University in Brno, Zemedelska 1, Brno, 613 00, Czech Republic
Dana Hübelová & Alice Kozumplíková
Department of Regional Development, Mendel University in Brno, Zemedelska 1, Brno, 613 00, Czech Republic
Jan Caha & Lenka Janošíková
You can also search for this author in PubMed Google Scholar
Contributions
DH and AK wrote the initial versions of the manuscript. DH prepared tables and Figs. 1 , 5 , and 8 , while LJ and JC prepared Figs. 2 , 3 , and 6 . AK prepared Figs. 4 and 7 . DH extracted data from the Czech Statistical Office, the Institute of Health Information and Statistics of the Czech Republic, and the Ministry of Labour and Social Affairs. AK extracted data from the Czech Hydrometeorological Institute. DH and JC processed and interpreted all statistical analyses. All authors contributed to the interpretation of results through their analyses and graphical outputs. LJ and JC were responsible for the final graphical outputs. Finally, all authors reviewed the manuscript.
Corresponding author
Correspondence to Alice Kozumplíková .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: appendix 1. .
List of determinants of health.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hübelová, D., Caha, J., Janošíková, L. et al. A holistic model of health inequalities for health policy and state administration: a case study in the regions of the Czech Republic. Int J Equity Health 22 , 183 (2023). https://doi.org/10.1186/s12939-023-01996-2
Download citation
Received : 13 June 2023
Accepted : 23 August 2023
Published : 05 September 2023
DOI : https://doi.org/10.1186/s12939-023-01996-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Determinants of health
- Regional disparities in health
- Spatial differentiation of health
- Health promotion and prevention
- Healthcare system optimization
International Journal for Equity in Health
ISSN: 1475-9276
- General enquiries: [email protected]
- Careers" data-insights-filter="categories:Careers" id="related_field_careers" /> Careers
- Careers › Gyrfaoedd" data-insights-filter="categories:Careers › Gyrfaoedd" id="related_field_gyrfaoedd" /> Careers › Gyrfaoedd
- Current projects" data-insights-filter="categories:Current projects" id="related_field_projects" /> Current projects
- Events" data-insights-filter="categories:Events" id="related_field_events" /> Events
- Events › CEN events" data-insights-filter="categories:Events › CEN events" id="related_field_cen-events" /> Events › CEN events
- Events › Hub events" data-insights-filter="categories:Events › Hub events" id="related_field_hub-events" /> Events › Hub events
- Learning and development" data-insights-filter="categories:Learning and development" id="related_field_learning-and-development" /> Learning and development
- Learning and development › Practice-based learning" data-insights-filter="categories:Learning and development › Practice-based learning" id="related_field_practice-based-learning" /> Learning and development › Practice-based learning
- Professional guidance" data-insights-filter="categories:Professional guidance" id="related_field_professional-guidance" /> Professional guidance
- RCSLT updates" data-insights-filter="categories:RCSLT updates" id="related_field_rcslt-updates" /> RCSLT updates
- Research" data-insights-filter="categories:Research" id="related_field_research-categories" /> Research
- Students" data-insights-filter="categories:Students" id="related_field_students" /> Students
- Topic area" data-insights-filter="categories:Topic area" id="related_field_topic-area" /> Topic area
- AAC" data-insights-filter="categories:AAC" id="related_field_augmentative-and-alternative-communication" /> AAC
- Acquired motor speech disorders" data-insights-filter="categories:Acquired motor speech disorders" id="related_field_acquired-motor-speech-disorders" /> Acquired motor speech disorders
- Anti-racism" data-insights-filter="categories:Anti-racism" id="related_field_anti-racism" /> Anti-racism
- Aphasia" data-insights-filter="categories:Aphasia" id="related_field_aphasia" /> Aphasia
- Autism" data-insights-filter="categories:Autism" id="related_field_autism" /> Autism
- Awake craniotomy" data-insights-filter="categories:Awake craniotomy" id="related_field_awake-craniotomy" /> Awake craniotomy
- Bilingualism" data-insights-filter="categories:Bilingualism" id="related_field_bilingualism" /> Bilingualism
- Brain injury" data-insights-filter="categories:Brain injury" id="related_field_brain-injury" /> Brain injury
- Children's services" data-insights-filter="categories:Children's services" id="related_field_childrens-services" /> Children's services
- Cleft lip and palate" data-insights-filter="categories:Cleft lip and palate" id="related_field_cleft-lip-and-palate" /> Cleft lip and palate
- COVID-19" data-insights-filter="categories:COVID-19" id="related_field_covid-19" /> COVID-19
- CPD" data-insights-filter="categories:CPD" id="related_field_cpd" /> CPD
- Craniofacial conditions" data-insights-filter="categories:Craniofacial conditions" id="related_field_craniofacial-conditions" /> Craniofacial conditions
- Critical care" data-insights-filter="categories:Critical care" id="related_field_critical-care" /> Critical care
- Deafblindness" data-insights-filter="categories:Deafblindness" id="related_field_deafblindness" /> Deafblindness
- Deafness" data-insights-filter="categories:Deafness" id="related_field_deafness" /> Deafness
- Dementia" data-insights-filter="categories:Dementia" id="related_field_dementia" /> Dementia
- Developmental language disorder" data-insights-filter="categories:Developmental language disorder" id="related_field_developmental-language-disorder" /> Developmental language disorder
- Digital health" data-insights-filter="categories:Digital health" id="related_field_digital-health" /> Digital health
- Dysfluency" data-insights-filter="categories:Dysfluency" id="related_field_dysfluency" /> Dysfluency
- Dysphagia" data-insights-filter="categories:Dysphagia" id="related_field_dysphagia" /> Dysphagia
- Education" data-insights-filter="categories:Education" id="related_field_education" /> Education
- End of life care" data-insights-filter="categories:End of life care" id="related_field_end-of-life-care" /> End of life care
- Head and neck cancer" data-insights-filter="categories:Head and neck cancer" id="related_field_head-and-neck-cancer" /> Head and neck cancer
- Justice" data-insights-filter="categories:Justice" id="related_field_justice" /> Justice
- Learning disabilities" data-insights-filter="categories:Learning disabilities" id="related_field_learning-disabilities" /> Learning disabilities
- LGBTQIA+" data-insights-filter="categories:LGBTQIA+" id="related_field_lgbtqia" /> LGBTQIA+
- Long covid" data-insights-filter="categories:Long covid" id="related_field_long-covid" /> Long covid
- Looked after children" data-insights-filter="categories:Looked after children" id="related_field_looked-after-children" /> Looked after children
- Mental health (adults)" data-insights-filter="categories:Mental health (adults)" id="related_field_mental-health-adults" /> Mental health (adults)
- Motor disorders" data-insights-filter="categories:Motor disorders" id="related_field_motor-disorders" /> Motor disorders
- Neonatal care" data-insights-filter="categories:Neonatal care" id="related_field_neonatal-care" /> Neonatal care
- Outcome measurement" data-insights-filter="categories:Outcome measurement" id="related_field_outcome-measurement" /> Outcome measurement
- Progressive neurological disorders" data-insights-filter="categories:Progressive neurological disorders" id="related_field_progressive-neurological-disorders" /> Progressive neurological disorders
- Public health" data-insights-filter="categories:Public health" id="related_field_public-health" /> Public health
- Risk feeding" data-insights-filter="categories:Risk feeding" id="related_field_risk-feeding" /> Risk feeding
- Selective mutism" data-insights-filter="categories:Selective mutism" id="related_field_selective-mutism" /> Selective mutism
- Social communication disorder" data-insights-filter="categories:Social communication disorder" id="related_field_social-communication-disorder" /> Social communication disorder
- Social, emotional and mental health (children)" data-insights-filter="categories:Social, emotional and mental health (children)" id="related_field_social-emotional-and-mental-health-children" /> Social, emotional and mental health (children)
- Speech sound disorders" data-insights-filter="categories:Speech sound disorders" id="related_field_speech-sound-disorders" /> Speech sound disorders
- Stroke" data-insights-filter="categories:Stroke" id="related_field_stroke" /> Stroke
- Stutter" data-insights-filter="categories:Stutter" id="related_field_stutter" /> Stutter
- Telehealth" data-insights-filter="categories:Telehealth" id="related_field_telehealth" /> Telehealth
- Trans voice" data-insights-filter="categories:Trans voice" id="related_field_trans-voice" /> Trans voice
- Upper airway disorders" data-insights-filter="categories:Upper airway disorders" id="related_field_respiratory-care-adults" /> Upper airway disorders
- Visual impairment" data-insights-filter="categories:Visual impairment" id="related_field_visual-impairment" /> Visual impairment
- Voice" data-insights-filter="categories:Voice" id="related_field_voice" /> Voice
- Wellbeing" data-insights-filter="categories:Wellbeing" id="related_field_wellbeing" /> Wellbeing
- Bulletin" data-insights-filter="content-type:Bulletin" id="related_field_bulletin" /> Bulletin
- Campaigns" data-insights-filter="content-type:Campaigns" id="related_field_campaigns" /> Campaigns
- Case study" data-insights-filter="content-type:Case study" id="related_field_case-study" /> Case study
- Document" data-insights-filter="content-type:Document" id="related_field_document" /> Document
- Guidance" data-insights-filter="content-type:Guidance" id="related_field_guidance" /> Guidance
- Hubs" data-insights-filter="content-type:Hubs" id="related_field_hubs" /> Hubs
- Policy" data-insights-filter="content-type:Policy" id="related_field_policy" /> Policy
- Press release" data-insights-filter="content-type:Press release" id="related_field_press-release" /> Press release
- Research" data-insights-filter="content-type:Research" id="related_field_research" /> Research
- Video" data-insights-filter="content-type:Video" id="related_field_video" /> Video
- Webinar" data-insights-filter="content-type:Webinar" id="related_field_webinar" /> Webinar
- England" data-insights-filter="locations:England" id="related_field_england" /> England
- International" data-insights-filter="locations:International" id="related_field_international" /> International
- Northern Ireland" data-insights-filter="locations:Northern Ireland" id="related_field_northern-ireland" /> Northern Ireland
- Scotland" data-insights-filter="locations:Scotland" id="related_field_scotland" /> Scotland
- UK" data-insights-filter="locations:UK" id="related_field_uk" /> UK
- Wales" data-insights-filter="locations:Wales" id="related_field_wales" /> Wales
No search results found
- Diversity, inclusion and anti-racism information
- Health inequalities
- Addressing health inequalities
Health inequalities case studies
Read case study examples of good practice to deliver quality service and meet the needs of under-served groups
Back to Health inequalities index page for guidance and resources.
Page content
- What the case studies cover
- Case study 1: Mental health diagnoses
- Case study 2: Public health messages
- Case study 3: developing a modified diet
- Case study 4: Linguistic and cultural translators
- Case study 5: Eating and drinking at risk
- Case study 6: Health screening in a youth offending service
- Case study 7: Meeting diverse needs in criminal justice
These case studies showcase good practice in meeting the needs of under-served groups and delivering quality care to service users who may be particularly vulnerable to health inequalities.
The case studies illustrate successful examples of speech and language therapy practice, but it should be noted that each service user is an individual and it should not be considered that the care exemplified in a case study is suitable for all people who meet the descriptions given.
Interested in sharing your own case study? Download the c ase study template and send your completed case study to [email protected]
Case study one: Understanding mental health diagnoses with consideration of cultural beliefs
This case study examines how support is provided to a non-English speaking family, with consideration of their cultural beliefs around mental health.
What was the clinical challenge?
In an adult mental health context, we worked with a young South Asian male patient diagnosed with schizophrenia and, subsequently, autism. His parents spoke Hindi and lacked awareness about mental health illnesses, as well as how to navigate through the NHS system.
How did you gather the information that you required?
In order to help meet the needs of the local population, the service has employed a Band 4 speech and language therapy assistant, who can speak several South Asian languages. Both the assistant and the therapist working with the family are Indian and were able to use their own experiences, alongside knowledge of appropriate vocabulary and possible perceptions of mental health in this community.
How was the information you collated used to improve the care for the individual/community/group?
- The home language of the family, Hindi, was used with awareness that vocabulary choices when translating into other languages can be challenging. For example, the translation of ‘mental health’ can be closer to ‘crazy’. The solution, rather than use Hindi to label, was to describe in detail the symptoms of autism and schizophrenia and continue with those labels.
- Being aware that there is often a stigma that surrounds mental health in this community, we were prepared that parents could be upset and have some difficulty around acceptance. Additional time was allowed for a face-to-face appointment with parents. This provided an opportunity for discussing topics relevant to the family such as stigma within the community, what to say to extended family, beliefs of the ‘evil eye’, and worry that parents may have caused the mental health needs.
- The SLT and assistant’s experiences and understanding were shared with the ward staff so that care could be tailored to the patient and family. The consultant on this particular ward allowed the SLT and assistant to take the lead.
What was the outcome?
The family were given the information in the language and context that they could understand and were also given the time and opportunity to discuss their specific concerns around stigma and their community. Staff worked together to ensure individuals with relevant experience and cultural sensitivity were able to use and share their knowledge. This way of working continues to be embedded in the care of all individuals in this setting.
Alpana Marwaha
Case study two: Promoting public health messages that matter to adults with learning disabilities
People with a learning disability are more likely to experience health inequalities (NIHR 2020), so supporting this group of people to be able to access and implement public health information is particularly important. Up to 90% of adults with a learning disability experience some form of communication difficulty (RCSLT 2013) and literacy levels among this group are known to be low (All party parliamentary group for education 2011).
The learning disability speech and language therapy team worked with a group of experts by experience (the Southampton community learning disability team service user group) to identify public health issues that matter to them. These issues included: physical activity, healthy eating, oral hygiene and mental wellbeing. The experts by experience worked jointly with the speech and language therapist (SLT) and SLT assistant on this piece of work. They spent three sessions on physical activity, and three sessions on healthy eating. These sessions involved:
- Understanding key messages relating to these topics (eg aiming for five portions of fruit and vegetables a day, alongside being active every day).
- Reviewing three apps relating to physical health and three apps relating to healthy eating on an iPad.
- Using talking mats to review the accessibility and usefulness of each app (rating each app on usefulness of information, amount of information, images, text, ease of use and how engaging/interesting it was).
After reviewing each app, arranging a road show event, visiting a local college/day service, sharing the key public health messages and demonstrating the apps, they rated favourably to other people with a learning disability. The roadshows were popular with attendees and a lot of people were interested in the apps. There were between four and fifteen people attending each roadshow event.
The group reviewed digital apps relating to areas that might be useful in supporting people with a learning disability keep physically active and eat healthily. They focused on each topic for three sessions (one session per month). The group reviewed the usefulness and accessibility of six different apps while learning more about the public health messages associated with them. The group then shared their learning with their peers at day services/colleges.
At the start of this study, none of the members of the Southampton Service User Group had ever used an app to help to support their health, although some members of the group were familiar with the term ‘apps’. Members reported that they would not use the internet as a source of health information. Awareness of public health related messages was generally low. For example, one member of the group thought we should aim to complete thirty minutes of exercise a week. This knowledge was raised, by the end of the work, he said twenty minutes a day.
The group rated 33% of the apps reviewed as useful and accessible. The apps they could relate to and incorporate into their daily routine were rated favourably. Barriers to accessibility included: issues with images, text size and overall ease of use.
Following this piece of work all members of the Service User Group reported that they were more likely to use the apps to support their health in the future. There was also an increase in the groups understanding of public health messages relating to physical activity and healthy eating. The group reported really enjoying the roadshow events particularly sharing their learning with other people with a learning disability and demonstrating the different apps.
Were there any challenges you had to overcome?
Not all apps available to support with public health are viewed as accessible by people with learning disabilities. However, there are apps which are rated as being accessible and clinicians working with adults with learning disabilities should signpost people to them and support them to access these to enable them to have the opportunity to manage their own health.
Rachael Middle, Anna Raby, Sophie Woodford, Matthew Horton
Case study three: developing a modified diet suiting the religious and cultural preferences of the patient
I received a referral for Mr A who was dysphagic and, following inpatient videofluoroscopy, had opted for an International Dysphagia Diet Standardisation Initiative (IDDSI) Level 4 pureed diet, which reduced the degree of aspiration. The referral requested I support setting Mr A up with these recommendations when home.
The referral stated that Mr A spoke Tamil and that he had possible mild memory and cognitive impairments. It also stated that he lived alone and had one daughter who spoke English, but phone calls with an interpreter revealed he was now living with his other daughter “P” who spoke Tamil, not English. P prepared Mr A’s meals.
Since coming home, Mr A had been having a subset of his meals which would blend into puree but it made him “feel sick” and reduced his diet intake, leading to weight loss. He said the doctors in hospital told him to start having pureed food so he had carried on. He wasn’t sure, or couldn’t remember, why he was having pureed food.
Mr A and his daughters then asked me about a range of foods that he wanted to eat and which IDDSI level they would be. I knew almost no Sri Lankan foods, aside from one or two items I happened to have had from a local Sri Lankan takeaway.
I wrote down the food names and we used Google image screen sharing, with family members holding items to the camera and describing items with the interpreter, to help me to understand exactly what presentation of the foods he was asking about. We agreed I would research options and come back to them with ideas of which foods fell into which IDDSI level.
I couldn’t find any IDDSI Level information sheets with examples of Sri Lankan foods online. To get this information myself, I tried some of the foods from my local Sri Lankan takeaway, spoke to the takeaway owners about the other foods, and continued to research different ways of preparing the foods online.
I presented the options again with the foods categorised into IDDSI levels with pictures and explanations of which features made them this texture. I made it clear which features made the foods correspond to each level, in order to help to try and generalise the concepts for other foods Mr A and his family eat.
Mr A expressed that he felt he would eat enough and enjoy meals made to the IDDSI Level 6 soft and bite-sized texture. Across the next few weeks, I phoned Mr A and P with an interpreter. We discussed how to: aid P in preparing meals, answer questions about further foods, monitor Mr A’s diet intake and chest status, and check he found the texture remained within his wishes across time.
This clinical case made me aware of the gap in resources for non-White British/American patients and led me to create a website for Swallow’s Kitchen for SLTs to make these info sheets with service users/multidisciplinary team (MDT) staff/interpreters etc. and share with other SLTs. I am making my first leaflet with a nursing home that has a large cohort of patients who eat traditionally Indian foods, and have an offer from the Sri Lankan takeaway to continue to make the leaflet for Sri Lankan foods.
Do you have any anonymised clinical data that you could share, to illustrate your case (eg language samples, observations, swallow test results and so on)?
You can see some examples of Sri Lankan foods I classified (PDF) .
Not being familiar with the foods the patient was asking me about and lack of resources for me to find this information was a real challenge. It felt embarrassing and almost discriminatory not to be able to answer these questions, given I knew if a patient/family member of a similar cultural background to myself had asked I could answer then and there myself and easily email them various IDDSI leaflets with multiple examples from within their usual diet. I also knew to be mindful of how one Sri Lankan family prepares food may differ from another.
There is a big gap in SLT resources for non- White British/American patients and it’s possible individual SLTs may be doing this work in isolation from each other, which is why I have started the website.
Do you have any tips for other members in similar situations?
Do the research! We owe it to our patients of other cultures to treat them equally to our patients who eat the traditionally British foods we know well. If you can, please get involved with Swallow’s Kitchen so we can try and narrow the resource gap. There has been lots of interest for Swallow’s Kitchen on Twitter and in CENs, however few other SLTs/student SLT have volunteered to make a leaflet at this point. It would be great if others were aware of this and in a position to make more leaflets!
I think this is important to facilitate more equal access to information, prevent delay to care for patients of other backgrounds and to reduce the chance of misunderstanding, which would otherwise lead to patients of other cultures being given foods that have not been agreed as in their best interests. I hope leaflet-making can be used as student placement projects and can also be used as opportunities to help patients, families, carers and others who collaborate on leaflet-making understand (their) dysphagia better.
Kerry Corley Brent inpatient and community neurorehabilitation team, London North West University Healthcare Trust.
Case study four: Developing a service to recruit bilingual co-workers acting as linguistic and cultural translators
We had lengthy waiting lists in the speech and language therapy service, and we had a vacant full-time SLT post. At the same time, many parents of children, particularly the mothers, and older adult patients did not speak English and I felt it was impossible for us to deliver services without interpreters, alongside the necessary information regarding cultural differences. We had worked with the interpreter unit but we needed more interpreter time than they could offer, and we needed to train the co-workers specifically to work with our client groups.
I found out more about the local populations (Oldham) – it had (and still has) one of the highest South Asian populations of any town – 18.1 % (England total 14.3%). For our caseload, I needed both Urdu and Bangla speakers in particular, who could also translate our information leaflets. I sought advice from an existing NHS interpreter / translator unit, whose services I had used before too.
I converted a vacant full-time SLT post to two bi-lingual co-worker posts.
This transformed our services. Bilingual co-workers are needed if we are to provide an effective service to ethnic minorities. Following the success of this, I later obtained funding for another co-worker and brought in some minority ethnic interpreters for other groups such as the Pashto-speaking Afghan population.
Case study five: Supporting informed decision-making for eating and drinking at risk
In a community adult SLT setting, I received a referral from the acute hospital team for “Mr A” who was deemed to be “feeding with acknowledged risk of aspiration” across consistencies. The referral told me in hospital that Mr A had opted for the diet texture which reduced the degree of aspiration on inpatient videofluoroscopy – the International Dysphagia Diet Standardisation Initiative (IDDSI) Level 4 pureed diet. The referral requested I support setting Mr A up with these recommendations when home.
Since coming home, Mr A had been having a subset of his meals which would blend into puree but it made him “feel sick” and reduced his diet intake leading to weight loss. He said the doctors in hospital told him to start having pureed food so he had carried on. He wasn’t sure, or couldn’t remember, why he was having pureed food.
The initial aim was to ensure Mr A and his family understood his needs and could make informed decisions about his diet. During discussions, different cultural opinions on the roles of professionals also emerged.
Based on the referral, I knew that I needed to contact Mr A with a Tamil interpreter and that he would likely benefit from short and repeated information. It was also important to personalise the information to Mr A to aid him to relate the options to concrete options in his life. In previous telehealth appointments I gathered examples of which Sri Lankan foods Mr A enjoyed eating and ensured I understood how these would usually be prepared for him, such that I could categorise them in IDDSI levels and present the options visually to Mr A in a powerpoint to support decision making ( see case study example 3).
We arranged a video call with Mr A, his daughters, and a Tamil interpreter. I shared videofluoroscopy findings through a presentation including short written sentences the interpreter could translate, and pictures supporting what I was saying, eg of a videofluoroscopy, of hospital, of usual IDDSI meal examples.
After the information was given, questions asked if he had understood and retained the information and had capacity to make the decision, alongside the options offered; Mr A asked me what he should do. I explained it was his choice, but this led to the family and interpreter laughing and saying, “you’re the doctor here, you tell him what to do”. I explained the roles within mental capacity assessment and said we could make the decision “together” balancing the costs and benefits of the options.
I was clear about what the roles were and took a “meet in the middle” approach saying we’d decide “together” what to do. I continued asking questions for Mr A to express his opinion such that we were able to have a constructive discussion about appropriate diet and meal preparation (for further information, read case study three ).
Use an interpreter and don’t rely on family members. Check the language and dialect before requesting an interpreter. It can be helpful to have written sentences for the interpreter to interpret for some contacts, for example, here, key information I’d prepared in a simplified form.
Consider how to balance different cultural norms of your roles. I did this by trying to be transparent of what role we each had in the legal framework of mental capacity assessments.
Is there anything you would do differently in future?
It would be useful to have more guidance on how to best manage cultural differences in mental capacity assessments. I don’t know if there was a better course of action for managing this. I could have done as asked and expressed what I would do in his position. However, I didn’t feel comfortable doing this given this is not part of the role I learnt that an SLT has in these mental capacity assessments.
Kerry Corley , Brent inpatient and community neurorehabilitation team, London North West University Healthcare Trust.
Case study 6: health screening in a youth offending service
Our youth offending service (YOS) deliver services to children aged 10 – 18. The children receive routine screenings from specialists based within the YOS, which contribute to the essential AssetPlus assessment overseen by the Case Manager (CM). Many of the individuals within the YOS population are at increased risk of experiencing health inequalities, eg due to poverty; poor social support; poor health literacy; being from some under-served ethnic/cultural groups that are over-represented in the youth justice system.
During the COVID-19 pandemic, the speech and language therapist (SLT) and restorative justice officer (RJO) identified a gap in team communication that had been created by the pandemic. Furthermore, face-to-face appointments with children were no longer possible.
There was no standard process in the team for coordinating the specialist screenings that take place at the onset of the child’s involvement with YOS and as such, their experience varied depending on which CM they were allocated to. Subsequently, differences in each CM’s operational approach and the impact on engagement became more apparent.
Children and their families were reporting being overwhelmed from poorly coordinated separate phone contacts from specialists, eg several hours of screenings attempted on the same day; or when families had not yet spoken to the CM and/or had not been informed of the screenings, specialists had attempted screenings without providing reasonable adaptations due to a lack of information, eg interpreters, avoiding potentially triggering/retraumatising topics or arranging COVID-19 compliant face-to-face meetings for those experiencing digital poverty. This led to inequitable health outcomes for the clients.
Incidents involving children becoming distressed at repeating traumatising history were common.
The SLT and RJO raised the issue with other health specialists in team. The team agreed that in order to be trauma-informed, it was necessary to clarify the intake pathway, specify that information must be shared prior to specialists contacting the family and outline the coordinating role of the CM.
The SLT approached the head of YOS who agreed and the change was introduced to CMs. The SLT checked with the NHS line manager and information governance team that information sharing from health system for the purposes of safeguarding was appropriate at this early stage of client input.
The head of YOS formalised and distributed new intake pathway process requiring virtual ‘Case Coordination’ meetings as mode of information sharing.
Head of YOS introduced performance management aspects to enforcing Initial Case Coordination Meetings in September 2020 after inconsistent implementation across CMs
There were 60 initial case coordination meetings carried out between August 2020 and end of March 2021.
Information regarding SLCN; physical and mental health; family factors including contact with social care; education and SEN; substance misuse; current and prior offences as well as contact with local child criminal exploitation agencies able to be shared across team at beginning of contact with service.
Feedback from families and specialist team has been positive, who feel screenings are better prepared for and engagement with children and families is improved.
There are numerous examples where screenings have been individualised to suit the needs of the client and address health inequalities:
- Adapting to the needs of the family improved overall engagement, addressing where attitudes towards health providers and the youth justice system (YJS) were acting as barriers to effective information gathering by professionals and equitable access to positive health outcomes for the client.
- Interpreters booked for parents who require support accessing the complexities of the YJS and may otherwise have difficulties accessing partner health services based on ethnic and cultural differences.
- Identification of families experiencing systemic pressures due to parental mental or physical ill-health and identifying most convenient way for team to contact them to remove barriers to positive experiences of YOS health and specialist services.
Initially the specialist team attempted to initiate the service change by introducing the idea for discussion at a whole team meeting. The emphasis was initially to allow for better time management in regards to scheduling and meeting screening deadlines for the specialists within the YOS team. This did not create buy-in from the case managers who would ultimately be responsible for coordinating the meetings and the feedback from some was that it would be another task to manage on top of having to adjust to the pandemic.
However once this was fed back to management, they were responsive and were able to provide direction; clear protocols; wider strategic rationale in line with the Hounslow YOS objective to become a trauma-informed service; and structures for performance managing CMs to ensure they were implementing the change.
Is there anything you would do differently in future or ongoing learning that you want to share?
Future plans involve developing more structured outcome measures to capture the positive impact of the meetings. This might involve approaching parents and children for their feedback about the screening process as well as comparing DNA/unsuccessful screening contact information before/after the meetings commenced during the pandemic
Next time a change in protocol is suggested, baseline information about how the change will create more resources for the children and young people (eg SLT intervention time) for the children should be presented/emphasised to promote initial buy-in from the CMs.
Up to this point, implementation oversight has focused on whether the meetings are carried out consistently across the team. Future oversight may seek to capture the quality of the meetings, ie whether the CM has had an initial discussion with the family prior to holding the meeting so that current circumstances may be shared with specialists; whether information about co-defendants has been readied for sharing with the RJO.
Management are also considering how to incorporate a similar model for exit planning at the end of a child’s journey with the YOS.
Jill Brennan , Highly specialist speech and language therapist – YOS specialist, Hounslow Youth Offending Service
Ruth Hall Restorative justice officer, Hounslow Youth Offending Service
Case study 7: Meeting diverse needs in criminal justice What was the clinical challenge?
People within criminal justice settings have a higher incidence of SLCN than the general population. At the time of writing there is no formal guidance in place stipulating need (or amount) for SLT to be involved in services for this population or how to deliver this.
Our Criminal Justice liaison and Diversion Service (CJLD) obtained funding for a two-year, 2 day a week (0.4wte) secondment for speech and language therapy for their service.
SLT have a unique role in identifying the SLCN of this population and as part of the secondment we needed to develop a SLT service embedded within the CJLD and prove need .
To begin the process of determining how best to offer a SLT service (identification, assessment, and advice) we first realised we needed to increase awareness of the SLCN of this population within our local area. This involved offering training to our CJLD service and the police, and networking with a variety of other agencies and criminal justice settings.
Using a quality improvement approach of PDSA cycles (plan-do-study-act) we developed a series of pilots which involved collating data about the SLCNs of the population that we encountered. We engage with several stakeholders and agencies in order to attune and develop a pathway which works for everyone involved.
The data so far, has been shared with members of our local police force and NHS trust, highlighting the SLCN needs of this population. We have also provided training regarding the huge demands the criminal justice processes make on SLCN regardless of any identified SLCN vulnerability.
Police (and other agencies) are actively seeking our advice and support with accessible information and interactions.
We continue to regularly review our data and gain / give feedback. We hope to develop a screening process which best identifies the often-hidden SLCN of this population. With our data we will submit a business case to obtain funding, so that we can provide at the very least a full time SLT to support the needs of this population.
There has been established focus on children (0-18) in the justice system with SLCNs, and youth offending teams often have SLT regularly embedded within their services. However, with our presence, screening, and assessment we have cultivated an all-age focus within our local justice settings, with an increased understanding of “vulnerability” which includes SLCN and neurodiversity. We have provided advice about accessible information, and how services could routinely consider SLCNs despite age or more obvious confirmed diagnoses. Staff are asking about vulnerabilities in more specific detail and are better able to make reasonable adjustments.
Our reports highlight service users’ needs and advocate for reasonable adjustments so that individuals are supported to participate in justice processes effectively, resulting in fairer trials and improved justice outcomes. Our reports may highlight the need for therapies and programmes to be adapted, in order for the person to be able to engage and participate, thus reducing reoffending.
Were there any challenges you had to overcome?
Several! Many highlighted above but also learning a new system (and skills) and how to navigate this, as well as ensuring our service is as effective as it can be on such reduced provision.
Link in with other SLTs in similar settings. Be creative, find CENS, set up MS Teams meetings and What’s App groups. It is a great way to share ideas, resources, learn and supervise one another. It can also provide motivation and support for when challenges may sometimes feel overwhelming .
Is there anything you would do differently in future or ongoing learning that you want to share?
Initially why SLT had been commissioned and what we could provide to the CJLD team and population served was not clear to the team, which made asking for their support with screening difficult. To get more buy in we continue to share case studies to support the positive outcomes and benefits SLT can support. We also feedback directly to the police regarding our assessment findings and how to support reasonable adjustments. We regularly attend CJLD team meetings and offer bespoke training at request and share positive stories. This supports our profile, continues to raise awareness, and supports rapport and service design. We also reach out to other services and try to “connect the dots” – this is important due to complexity of NHS and other public sector systems but also raises the profile of SLT and all that we can do.
Steph Hammond and Jenni Kingman, Speech and Language Therapists in Criminal Justice Liaison and Diversion Service
Is something wrong with this page? Submit feedback
A case study of new approaches to address health inequalities: Due North five years on
Affiliation.
- 1 Public Health England, UK. Also Visiting Professor, Leeds Beckett University.
- PMID: 31886485
- DOI: 10.1093/bmb/ldz037
Introduction: When local councils took on responsibility for public health in England in 2013, leaders from across the north of England met to consider the scale of the challenge. As a result, Public Health England commissioned the Due North Report which outlined new approaches in tackling health inequalities. This second paper outlines what has been learnt in five years as a case study. This includes influencing devolution deals and new elected city mayors, planning for economic growth in deprived areas and developing community asset-based approaches. The paper outlines a new framework for place-based planning to reduce health inequalities.
Sources of data: Data was gathered from annual reports from north of England directors of public health, Office for National Statistics, Public Health England's fingertips database and regional and national publications and strategies such as the Northern Powerhouse.
Areas of agreement: Devolution to English cities and councils as 'places' is a new opportunity to address local needs and inequalities. Due North has supported a new public health narrative which locates health action in the most fundamental determinants-how local economies are planned, jobs created and power is to be transferred to communities and connects reducing years of premature ill health to increased economic productivity. Community asset approaches to empower local leaders and entrepreneurs can be effective ways to achieve change.
Areas of controversy: The north-south divide in health is not closing and may be worsening. Different ways of working between local government, health and business sectors can inhibit in working together and with communities.
Growing points: Place-based working with devolved powers can help move away from top down and silo working, empower local government and support communities. Linking policies on health inequalities to economic planning can address upstream determinants such as poverty, homelessness and unsafe environments.
Areas timely for developing research: More research is needed on; (i) addressing inequalities at scale for interventions to influence community-led change and prosperity in deprived areas, and (ii) the impact of devolution policy on population health particularly for deprived areas and marginalised group.
Discussion and conclusions: Commissioning high profile reports like Due North is influential in supporting new approaches in reducing inequality of health through local government, elected mayors; and working with deprived communities. This second paper describes progress and lessons.
Keywords: community assets; devolution; health inequalities; new approaches.
© The Author(s) 2019. Published by Oxford University Press. All rights reserved. For Permissions, please email: [email protected].
Publication types
- Delivery of Health Care / organization & administration
- Health Status Disparities*
- Life Expectancy
- Local Government
- Poverty Areas
- Public Health
- Public Health Administration / methods*
- Social Determinants of Health
- Socioeconomic Factors
- State Medicine / organization & administration
Advertisement
Health Inequalities: To What Extent are Decision-Makers and Economic Evaluations on the Same Page? An English Case Study
- Current Opinion
- Open access
- Published: 29 June 2022
- Volume 20 , pages 793–802, ( 2022 )
Cite this article
You have full access to this open access article

- Sebastian Hinde ORCID: orcid.org/0000-0002-7117-4142 1 ,
- Dan Howdon 2 ,
- James Lomas 3 &
- Matthew Franklin 4
3928 Accesses
3 Citations
11 Altmetric
Explore all metrics
Economic evaluations have increasingly sought to understand how funding decisions within care sectors impact health inequalities. However, there is a disconnect between the methods used by researchers (e.g., within universities) and analysts (e.g., within publicly funded commissioning agencies), compared to evidence needs of decision makers in regard to how health inequalities are accounted for and presented. Our objective is to explore how health inequality is defined and quantified in different contexts. We focus on how specific approaches have developed, what similarities and differences have emerged, and consider how disconnects can be bridged. We explore existing methodological research regarding the incorporation of inequality considerations into economic evaluation in order to understand current best practice. In parallel, we explore how localised decision makers incorporate inequality considerations into their commissioning processes. We use the English care setting as a case study, from which we make inference as how local commissioning has evolved internationally. We summarise the recent development of distributional cost-effectiveness analysis in the economic evaluation literature: a method that makes explicit the trade-off between efficiency and equity. In the parallel decision-making setting, while the alleviation of health inequality is regularly the focus of remits, few details have been formalised regarding its definition or quantification. While data development has facilitated the reporting and comparison of metrics of inequality to inform commissioning decisions, these tend to focus on measures of care utilisation and behaviour rather than measures of health. While both researchers and publicly funded commissioning agencies are increasingly putting the identification of health inequalities at the core of their actions, little consideration has been given to ensuring that they are approaching the problem in a consistent way. The extent to which researchers and commissioning agencies can collaborate on best practice has important implications for how successful policy is in addressing health inequalities.
Similar content being viewed by others
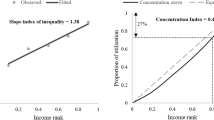
Methods to promote equity in health resource allocation in low- and middle-income countries: an overview

Cost transferability problems in economic evaluation as a framework for an European health care and social costs database

Costs in Comparative Effectiveness Research
Avoid common mistakes on your manuscript.
1 Introduction
The burden of inequalities in health are as internationally ubiquitous as they are nebulous in scope and definition. From a global perspective, inequality in health and access to care underpin the majority of the World Health Organization’s (WHO) Sustainable Development Goals [ 1 ]. While the 17 targets set out in the WHO’s goal to ‘ensure healthy lives and promote well-being for all at all ages’ would be considered a minimum standard of care in most high-income countries, they grapple with health inequality nonetheless, with the achievement of this minimum standard not a guarantee of health equity within a nation. While every nation has a unique history of how their healthcare provision has emerged over time, and the scale and type of health inequality within that country varying, pertinent health inequality challenges exist in all settings.
Central to the attempts by decision makers around the world to reduce health inequalities has been the question of where the level of action should lie between national and local agencies, how associated agencies should function, and how to maximise total health while minimising inequality [ 2 ]. The underlying trade-off being characterised as one where centralised agencies may be able to achieve greater efficiency by reducing replication of roles, but a decentralised one may be able to be more attuned and responsive to local needs [ 3 ].
In parallel to its public policy relevance, there has been a recent expansion in health and care research attempts to incorporate the impact of commissioning decisions on health inequality alongside the traditional focus of total population health [ 4 ]. This development has been motivated by two complementary factors: firstly, the recognition that existing, internationally applied, methods of cost-effectiveness analysis fail to facilitate the consistent consideration of health maximisation relative to inequality minimisation [ 5 ]. Second, the observation that assessment approaches taken by national health technology assessment agencies, such as the National Institute for Health and Care Excellence (NICE) in England, resulted in recommendations which implied overall population health improvement, but at the detriment of worsening health inequality [ 6 ].
Our aim is to understand the methodological research that has been conducted for incorporating health inequality considerations into economic evaluations (i.e., the ‘researcher-led approach’), and to explore how this compares to existing approaches that have evolved within publicly funded commissioning agencies (i.e., the ‘commissioner-led approach’, where ‘commissioner’ is used in a broad sense to encompass the associated analysts and decision makers).
First, we explore the current state of play on how researcher-led approaches have sought to account for inequality alongside the traditional aim to maximise population health [ 7 ]. Second, we consider the commissioner-led approach: specifically, how local commissioners have interpreted and acted on inequalities. To facilitate a clear understanding of how these approaches compare we conducted a detailed exploration of the English setting, later reflecting on the generalisability to other national settings. Finally, we deliberate on how well the two approaches integrate, data available or required to facilitate the approaches, and potential steps to minimise any disconnect when it comes to quantifying and tackling health inequalities. This research was stimulated and informed by workshop discussions between researchers and commissioners as part of a project exploring the potential for “Unlocking data to inform public health policy and practice” [ 8 ].
2 Defining Inequality and the Context of Inequality in Health
For descriptive purposes, we define ‘health inequality’ as any difference in individual or group health profiles that can be quantified in a meaningful way, e.g., variation in care service use or access, healthcare needs, or their lived health experience. We consider inequality to have relevance both in terms of geographic variations (e.g., regional commissioning jurisdictions) and population sub-groups (e.g., ethnicities). For the purposes of this paper, we additionally consider health inequality to be relevant to both differences in the stock of health (outcomes such as life expectancy) and access to health care resulting from variations in supply (e.g., the number of GPs in an area), as discussed below this is consistent with the approach often taken in commissioning settings. While an interest in health inequalities is motivated by judgements that are inherently normative, we do not explore the issues regarding the normative or objective nature of inequality, which are explored elsewhere [ 9 , 10 , 11 ].
3 Setting the Scene: The English Context
In England, equal access to tax-funded healthcare was one of the founding principles of the National Health Service (NHS) during the 1940s [ 12 , 13 ]. However, whilst this principle has been largely preserved for over 70 years [ 14 ], eliminating differences in population subgroups’ health remains elusive. For example, there is a 7.6-year life expectancy gap between women, and 9.4 years for men, in the least and most deprived areas of England [ 15 ]. As is true to a varying extent internationally, health inequality in England persists despite a long-running objective of successive governments being its reduction, with a succession of national reports and strategies—the 1980 Black Report [ 16 ], the 1998 Acheson Report [ 17 ], New Labour’s Health Inequalities Strategy [ 18 ], the 2010 Marmot Review [ 19 ] and its 10-year reassessment [ 20 ]—on the topic.
In England, a plethora of commissioning and administrative structures have been created and re-created with inequality reduction routinely at the heart of their policy mandates in response to these national reports and other stimuli [ 21 ]. Related to the NHS, the current shift is towards Integrated Care Systems (ICS), with ICSs having ‘improving outcomes and addressing inequalities’ as a key tenet of their formation [ 22 ]. In comparison, Local Authorities (LAs) are responsible for commissioning publicly-funded social care and, since 2013, some public health services. We focus on local commissioners given that the majority of current and planned commissioning responsibility related to health in England can be attributed to LAs (e.g., City Councils), Clinical Commissioning Groups (CCGs), and (from 2022) ICSs. We provide brief details of the role of each in the English healthcare system in Sect. 5 , but additional details are available elsewhere [ 23 , 24 ].
4 The Researcher-Led Approach to Health Inequalities
One innovation developed and refined by health economists in recent decades has been the creation and application of a methodological framework with which to assess care interventions covering a diverse range of health-related factors (e.g., illness, acute and chronic conditions, adverse health events) using an incremental cost-effectiveness analysis (CEA) approach. In brief, this approach assesses competing interventions by their incremental impact on some measure of health-related outcome, most commonly quality-adjusted life-years (QALYs, a metric capturing both quality and quantity of life), relative to the incremental costs (usually only those borne by the care system), with the ratio of incremental costs and incremental QALYs being termed the incremental cost-effectiveness ratio (ICER). In a budget-constrained care system, this ICER is conventionally compared to some threshold value—representing the maximum ICER at which decision-makers will fund a new intervention—in order to assess cost-effectiveness. Where the aim is to ensure each individual decision increases population health, this threshold should represent the cost-effectiveness of existing interventions that are candidates for defunding in the case of acceptance of this new intervention [ 25 ]. However, in practice the threshold value often reflects a wider set of considerations than the cost-effectiveness of what may be defunded [ 26 ].
Fundamental to traditional CEA application is the notion that ‘a QALY is a QALY is a QALY’ [ 27 ]. This represents the idea that a QALY is equivalent, comparable, and transferable in the determination of cost-effectiveness irrespective of who gains or loses, with the primary aim being population health maximisation as measured by the QALY. However, this approach has been argued to ignore the trade-offs that are made between overall population health and health equality [ 28 ]. By overlooking such occurrences, including the opportunity cost of disinvestment falling inequitably and differential uptake of common healthcare interventions [ 29 ], CEA recommendations risk running contrary to the dual-aim of many healthcare decision makers [ 30 ]. This lack of explicit consideration of interventions’ inequality impact occurs in many health technology assessment (HTA) processes internationally [ 31 ].
In the case of NICE in England, their current reference guide for conducting economic evaluations states: “An additional QALY has the same weight regardless of the other characteristics of the people receiving the health benefit” [ 32 ]. Footnote 1 This is perhaps in conflict with their stated aim “to reduce health inequalities” [ 34 ], alongside an acknowledgement of the body’s legal responsibilities in this regard, and a note that the institute “[takes] into account inequalities arising from socioeconomic factors and the circumstances of certain groups” [ 35 ]. While the extent to which any trade-off between equity and population health is currently considered in deliberations is at most limited, research has shown that HTA recommendations made by NICE have had quantifiable impacts on the distribution of health [ 36 ], with further research identifying that more deprived groups also bear more of the health loss burden when funding is redistributed [ 29 ]. However, in recent years there has been an increasing trend in research to explicitly reflect the trade-off between total health and inequality [ 4 , 37 ].
In this section we briefly review some of the methods by which inequality has been considered in the researcher-led economic evaluation literature and explore some of the emerging methods in detail to determine their level of consistency with the commissioner-led approach.
4.1 Methods to Reflect Inequality Alongside Cost-Effectiveness
Analytical methods to account for inequality concerns alongside CEA can generally be grouped into equity impact or equity weighting approaches [ 4 ]. Avanceña and Prosser’s systematic review of CEAs incorporating equality considerations identified 54 studies, with most published since 2015. The majority were found to take an equity impact approach ( n = 46), with five conducting both, and three equity weighting alone [ 4 ].
Equity impact analysis produces summaries of cost-effectiveness stratified by the sub-groups of interest, then reports the respective costs and health outcomes for each stratified group alongside the headline summaries of intervention cost-effectiveness for the full population. Although useful when demonstrating the potential subgroup’s inequitable gains and losses, the approach does not incorporate inference of the acceptability of any health and inequality trade-off as no socially acceptable weighting is applied to the potentially competing outcomes.
In contrast, equity weighting methods explicitly incorporate differential QALY weighting, allowing for informative analysis as to any trade-off between total population health and inequality. Details of CEA methods incorporating equity weighting, often called distributional CEA (DCEA), and associated tutorials are published [ 38 ]. In brief, as with equity impact analysis, the approach involves CEA stratified by relevant subgroups, but with the additional step of allocating a set of weightings to the QALY impact by subgroup. This facilitates the estimation of incremental cost-effectiveness dependent on the weighting set applied to inequality impact versus total population gain. Inevitably the choice of weightings is a key challenge for DCEA as there is currently no routinely accepted set of weightings [ 28 ]. In practice, DCEA results are presented using a distribution of weights, so that society’s aversion to inequality is directly compared against the total population QALY gains they would be willing to forgo to minimise inequality. In addition to the challenge of identifying an appropriate estimate of society’s inequality aversion, there is currently no standard weighting approach; Avanceña and Prosser’s review noted that eight identified equity weighting studies each took a different weighting approach [ 4 ].
Across both approaches, an additional challenge of incorporating equality concerns into CEA is determining how to categorise the groups of interest. Avanceña and Prosser found “at least 11 different equity criteria have been used” (p. 136), commonly stratified by socioeconomic status ( n = 28) or race/ethnicity ( n = 16) [ 4 ]. Distributional CEA tutorials recommend categorising by index of multiple deprivation (IMD) equity groups, although any grouping for which society’s view of inequality aversion has been quantifiably weighted can be used. While this variation in group categorisation represents a challenge for cross-comparability, the flexibility to the decision maker’s needs is an important benefit when incorporating equity. Distributional CEA does not seek to provide “an algorithmic approach to replace context-specific deliberation with a universal equity formula. Rather, it can be used as an input into context-specific deliberation by decision makers and stakeholders” (p. 119) [ 39 ].
In addition to the methods with which to implement the inclusion of inequality considerations, checklists to guide economic evaluations seeking to incorporate inequality considerations have been developed, e.g., the Equity Checklist for Health Technology Assessment [ 31 ].
5 The Meaning and Role of Inequality to Local Commissioners
Here we explore the definition and application of health inequality terminology using the setting of English local commissioning as a case study, exploring LAs’, CCGs’, and ICSs’ mandated duty or obligation to consider or act upon inequalities in their commissioning decisions, their potential resources for quantifying their jurisdiction’s inequality levels, each described alongside some examples for discussion purposes. Although we focus on English commissioners, the use of local commissioners to tackle regional health challenges, such as care access and inequality in health considerations, is common internationally, although these organisations may be named differently, with varying degrees of responsibility and geographic scope [ 2 ].
5.1 Legal Considerations: The 2010 Equalities Act
Underpinning all UK provision of public services is the 2010 Equalities Act [ 40 ], which protects against direct and indirect discrimination across nine characteristics: age, disability, gender, marriage and civil partnership, pregnancy and maternity, race, religion or belief, sex, and sexual orientation. Additionally, the Act’s Sect. 1 contains a “socio-economic duty” to consider broader inequalities within a commissioner’s jurisdiction: they must “have due regard to the desirability of exercising (their functions) in a way that is designed to reduce the inequalities of outcome which result from socio-economic disadvantage” [ 40 ].
However, while the 2010 Equalities Act was enshrined in law, Sect. 1 was not a legal requirement until 2018 in Scotland and 2021 in Wales; but currently (as of April 2022) it is still not a legal requirement in England. As a result, public agencies in England may choose if and how to consider inequality in their decisions. While some have acted on Sect. 1 [ 41 ], they are not legally required to beyond the nine protected characteristics: this permits significant variation in the actions taken depending on whether or not the authorities have chosen to take the socio-economic duty upon themselves [ 41 ].
5.2 Local Authorities (LAs)
Since the Health and Social Care Act 2012 [ 42 ], LAs have had a remit to deliver public health services in addition to their traditional remit, which covers social determinants of health (e.g., housing, education, social care, and transportation); thus, a LA’s inequality remit goes beyond the provision of care services [ 43 , 44 ]. Here we focus on LAs’ public health responsibilities associated with the Health and Social Care Act 2012 and elements of the Public Health Profiles commissioning indicators provided by the Office for Health Improvement and Disparities (OHID) [ 45 ].
Despite LAs’ public health remit, there is little legal requirement or good practice guidance to facilitate their attempts to alleviate health inequality. Publications such as the Local Government Organisation 2018 report ‘A matter of justice: Local government’s role in tackling health inequalities’ [ 44 ] speaks to this, with a large emphasis of the burden of inequalities and potential solutions that fall within LA remit, but nothing on the associated legal requirements. Relatedly, and beyond Sect. 1 (whether legally enshrined or not), LAs may be seen as having a moral obligation to address inequality in their respective geographical areas and associated funding structures: council tax, business rates, and government grants. While LAs in poorer areas inevitably have lower revenues through council tax and business rates, these are supported to some extent by government grants, resulting in higher levels of total revenue than richer LAs [ 46 ]. However, since 2008 poorer LAs have lost a higher proportion of funding, associated with a corresponding reduction in relative life expectancy [ 47 ].
Local authorities’ variation in actioned responsibility to reduce inequalities in their populations was demonstrated in Just Fair’s 2018 report detailing quantitative interviews and analyses with seven LAs [ 41 ]. At the time of interview, they found that only one of the seven had embedded the requirements of Sect. 1 into their decision making, doing so voluntarily, with the remaining six pursuing a range of policies seeking to alleviate socio-economic disadvantage but not to the same extent.
Vital to all discussions about reducing inequality is the ability to assess the impact of any action or inaction with robust evidence, with Just Fair identifying aspects associated with data as two of their five essential features: ‘meaningful data assessment’ and ‘using data effectively’ [ 41 ]. While it is not possible to be conclusive as to how each LA uses data (e.g., social or health care data) to inform the assessment of inequality at an inter- or intra-authority level, Public Health England's Public Health Profiles, provide valuable insight [ 45 ]. This platform gives absolute and relative estimates for a wide range of health indicators and determinants of health. While these are valuable for informing inter- and intra-authority comparisons, as the majority of estimates provide a single estimate for each authority—e.g., prevalence of obesity—they are of little value when seeking to address intra-authority inequality. The exception to this within the Public Health Profiles system is the Health Inequalities Dashboard [ 48 ], which provides estimates of relative and absolute gaps within an authority for a number of inequality indicators—both health and its determinants. However, to our knowledge, informed by a review of the relevant literature on the use of data by local governments [ 49 ], it is not currently recorded how, or if, LAs use the data in their commissioning decisions.
5.3 Clinical Commissioning Groups (CCGs)
The reduction of inequalities in the access to and outcomes from healthcare interventions has been part of CCGs’ remit since their formation under the Health and Social Care Act 2012. Each CCG must: “(a) reduce inequalities between patients with respect to their ability to access health services, and (b) reduce inequalities between patients with respect to the outcomes achieved for them by the provision of health services” [ 42 ].
This is reflected in CCG funding allocations from NHS England. While the allocation formula has changed over time, specifically in w met and unmet needs are reflected, inequality has always played a part in these allocations [ 50 ]. Since 2019/20, funding allocations include adjustments that reflect the relative standardised mortality ratio of those aged ≤ 75 years in the CCG’s region, with the associated proportion of funding allocated on this basis being: primary care, 15%; CCG commissioned services, 10%; speciality services, 5% [ 51 ].
In addition to its role in their funding, inequality is also considered in the Oversight and Assessment process, under which NHS England conducts a statutory annual assessment of each CCG. The Oversight Framework that informs the process combines aspects of ‘preventing ill health and reducing inequalities’ [ 52 ], recording data on:
Maternal smoking at delivery
Percentage of children aged 10–11 classified as overweight or obese
Injuries from falls in people aged 65+ years
Antimicrobial resistance: appropriate prescribing of antibiotics in primary care
Proportion of people on GP severe mental illness register receiving physical health checks
Inequality in unplanned hospitalisation for chronic ambulatory and urgent care sensitive conditions
Where inequality is considered in the Oversight Framework, it is typically presented in terms of absolute inequality gradient calculated for each CCG. Importantly, these estimates are not used as a blunt measure to assess the CCG’s performance but to provide ‘a focal point for joint work, support and dialogue’ between the various stakeholders [ 53 ].
5.4 Integrated Care Systems (ICSs)
Integrated Care Systems will become statutory bodies in 2022, taking over the commissioning function currently held by CCGs and with their modus operandi ‘improving outcomes and addressing inequalities’ [ 22 ]. Underpinning this aim is the hypothesis that improved integration of services both within healthcare and between sectors represents a better approach than the more competitive process of service commissioning that underpinned CCG functioning. Local authorities and ICSs will have a duty to collaborate, replacing current collaboration processes, which may have previously existed between LAs and CCGs. Additionally, ICSs will shift to ‘place-based working’, focussing on individual geographic localities, the needs of their populations, and existing partnerships. As such, integration is likely to be interpreted and operationalised differently across ICSs that will inevitably vary in these elements.
At the time of writing, the details as how the modus operandi will be operationalised by the ICSs and monitored by NHS England are limited to the high-level aims outlined in the White Paper [ 22 ], with the expectation that each ICS will have significant flexibility in deciding their path forward. However, the increased focus on local needs and solutions suggests ICS decision-making is likely to shift further towards approaches that are tailored to local systems, e.g., inequality measures selected to address known local issues such as smoking cessation. Secondly, the pragmatic approach to monitoring inequality levels by NHS England for CCGs may well continue for ICSs, with the limited reporting of inequality measures (see Sect. 5.3 ) continuing to inform dialogue between NHS England and ICSs.
Overall, this suggests that a two-level approach to inequality might continue to emerge: one level focussing on inter-ICS comparisons to inform the funding allocation, and one level within each ICS that is specific to the needs and challenges faced locally. This risks producing potentially inconsistent pressures within each ICS as they attempt to grapple with the health and inequality considerations that are specific to their jurisdictions as well as broader inequality measures for comparisons with other ICSs [ 54 ].
6 Generalisability of the English Local Commissioning Landscape Internationally
With the diverse nature of care commissioning responsibilities internationally it is not feasible to determine whether the experience in England is directly comparable to other nations. However, it is self-evident that, due to commissioners’ proximity to service provision data, such as patient care records, the most readily available approach to conceptualising and monitor health inequality will always be informed by such data. Furthermore, frameworks the UK’s 2010 Equalities Act are mirrored internationally. Therefore, the experience in England, described in Sect. 5 , is expected to be internationally transferable in the pertinent details.
7 Comparing the Two Approaches and Recommendations
To discuss where and how the researcher and commissioner-led approaches can begin to come together and the potential benefits of doing so, it is important to consider their relative practical and methodological strengths and limitations when the goal is to inform localised commissioning. Our suggested considerations are in Table 1 .
Building on these strengths and limitations, and the English case-study, we have a number of recommendations to begin to address the disconnect:
The time and financial costs involved with the creation of DCEA models implies that it is not feasible for each commissioner to have locally tailored models. Instead, models should be commissioned nationally, or collaboratively across LAs and ICSs, with flexibility to local context, accessibility, and co-development seen as fundamental parts of model development. Such an approach would facilitate research impact from an academic perspective, and better use the skills, knowledge, and data availability of all parties.
A common set of agreed vocabulary around the definitions of health inequality, and agreement on how aspects of health inequality are to best quantified, e.g., through minimum data specifications and reporting standards.
To address the overall divide in the two disciplines, closer collaboration must be prioritised with a focus on the ease with which the two settings can identify potential research partners and disseminate the latest research.
Better reflection and documentation of where existing quantitative frameworks for determining cost-effectiveness may differ from the commissioning reality faced by the commissioners, e.g., finance and policy cycles, ring-fenced budgets, risk aversion to overspend, and diverse outcome measures.
Development and maintenance of local and national metadata to provide a clear understanding of who holds what data relevant to healthcare inequality, and how it can be accessed. The supplementary appendix to this paper provides further details of the challenges of identifying and accessing key data regarding pertinent inequality data in the English case study.
Make the analysis and reporting of the distributional impact of interventions subjected to CEA as minimum standard, with the conducting of DCEA an expectation where once course of action does not strictly dominate all others.
8 Discussion
We have explored researcher- and commissioner-led approaches to define, quantify, and analyse health inequalities. Based on the English care setting example, the different perspectives and their starting points have resulted in approaches that in many ways share little beyond the use of the term ‘health inequality’; this is likely to be the case internationally. The researcher-led approach, specifically DCEA, puts overall patient health at its centre, in addition to assumptions regarding the ability to categorise patients into their demographic groups, and requires access to an underlying CEA model. In contrast, the commissioner-led approach focusses on available data, relying on the comparative summaries of measures of healthcare utilisation and diagnoses, typically stratified into geographic groupings often based on a commissioner’s jurisdiction. Although, in the English setting the recent White Paper on ‘Levelling Up the United Kingdom’ has underlined aims to better use the Healthy Life Expectancy measure to record inequalities [ 55 ]. Availability of data and ability to quantify inequalities will be a challenge internationally, often dependent on the extent to which countries/regions are willing and able to collect the relevant and necessary data.
It would be misleading to suggest there have been no interactions to date between researchers and commissioners to inform these approaches, For example, a report commissioned by the Department of Health and Social Care has called for ‘better, broader, and safer’ use of health data for research and analysis [ 56 ]. However, there are a number of existing barriers to overcome in order to enable consistency across approaches. Most significantly, these include finding a common set of vocabulary around definitions of health inequality, and agreement on how aspects of health inequality are to be quantified. Research has found that while many decision makers desire a greater level of integration of economic evaluation into the decision-making process, in practice this does not occur because of issues of accessibility [ 57 ] and the perceived limited relevance of current frameworks to the reality faced by commissioners [ 58 ]. From the commissioner perspective, economic evaluations of care interventions have conventionally focussed on the national decision-making context, assuming local commissioners are able to take on a level of decision uncertainty and fund interventions based on cost-effectiveness rather than affordability [ 59 ]. Furthermore, some challenges to the alignment of the approaches are likely to be perpetual, such as commissioners’ requirement to place their legal duty at the heart of any commissioning decision, and the cost of producing economic evaluations such as DCEAs to inform all budget allocation decisions.
9 Conclusion
Developments in economic evaluation methodology, specifically DCEA, have given analysts a means of presenting the cost-effectiveness of care technologies for the whole eligible population alongside the associated impact on health inequality. However, limited consideration has been given to how this approach can be applied at the point where health inequalities are most relevant and arguably best addressed, often at a local commissioner level. Additionally, lessons need to be learnt in the researcher-led world for such approaches to have greater relevance and impact, and consideration needs to be given to the data used to quantify and evaluate aspects of health inequality within different contexts. Ultimately, it is important that researchers and commissioners are consistent in their approach to defining, quantifying, and analysing health inequalities if the repeated aim of reducing health inequalities is to be achieved.
Despite this statement, additional weight was previously given to QALYs gained subject to meeting ‘end-of-life’ criteria [ 33 ]. The recent methods review has seen a shift away from this approach to instead focusing on the level of severity of health burden of beneficiaries, which could, in principle, be consistent with the aim to reduce health inequalities—particularly if consideration is taken of the distribution of opportunity costs. In practice, this can be achieved by using a method that we discuss in the next section: distributional cost-effectiveness analysis (DCEA).
World Health Organization. The sustainable development goals report. Geneva: WHO; 2021.
Google Scholar
World Health Organization. The role of local government in health: comparative experiences and major issues. Geneva: WHO; 1997.
Peckham SEM, Powell M, Greener I. Decentralisation, centralisation and devolution in publicly funded health services: decentralisation as an organisational model for health-care in England. In: Technical Report. London: LSHTM; 2005.
Avanceña AL, Prosser LA. Examining equity effects of health interventions in cost-effectiveness analysis: a systematic review. Value Health. 2021;24(1):136–43.
Article PubMed Google Scholar
Cookson R, et al. Using cost-effectiveness analysis to address health equity concerns. Value Health. 2017;20(2):206–12.
Article PubMed PubMed Central Google Scholar
Griffin S, et al. Evaluation of intervention impact on health inequality for resource allocation. Med Decis Mak. 2019;39(3):171–82.
Article Google Scholar
Drummond MF, et al. Methods for the economic evaluation of health care programmes. Oxford: Oxford University Press; 2015.
Franklin M. Unlocking real-world data to promote and protect health and prevent ill-health in the Yorkshire and Humber region. https://doi.org/10.15131/shef.data.14723685.v1 . 2021.
Arcaya MC, Arcaya AL, Subramanian SV. Inequalities in health: definitions, concepts, and theories. Glob Health Action. 2015;8:27106–27106.
Global Health Europe. Inequity and inequality in Health. 2009. [accessed 10/12/2021]. Available from: https://globalhealtheurope.org/values/inequity-and-inequality-in-health/ .
Whitehead M. The concepts and principles of equity and health. Int J Health Serv. 1992;22(3):429–45.
Article CAS PubMed Google Scholar
National Health Service Bill, in 9&10 Geo. 6, CH81. 1946.
Delamothe T. NHS at 60: founding principles. BMJ (Clin Res Ed). 2008;336(7655):1216–8.
Department of Health & Social Care. The NHS constitution for England. London: DHSC; 2021.
Office for National Statistics. Health state life expectancies by national deprivation deciles, England: 2017 to 2019. Newport: ONS; 2021.
Department of Health Social Security. Working Group on Inequalities in Health, Inequalities in health: report of a research working group. HM Stationery Office; 1980.
Acheson D. Independent inquiry into inequalities in health report. In: Department of Health and Social Care. London: DHSC; 2001.
House of Commons Health Committee. Health inequalities: third report of session 2008–09. London: The Stationery Office; 2009.
Marmot M, Bell R. Fair society, healthy lives. Public Health. 2012;126:S4–10.
Marmot M. Health equity in England: the Marmot review 10 years on. BMJ. 2020;368:m693.
Turner D, et al. Prospects for progress on health inequalities in England in the post-primary care trust era: professional views on challenges, risks and opportunities. BMC Public Health. 2013;13(1):274.
Department of Health & Social Care. Working together to improve health and social care for all. London: DHSC; 2021.
Charles, A. Integrated care systems explained: making sense of systems, places and neighbourhoods. 2021. [cited accessed: 13/04/2022]. Available from: https://www.kingsfund.org.uk/publications/integrated-care-systems-explained .
Humphries R. The NHS, local authorities and the long-term plan: in it together? 2019. [cited accessed: 13/04/2022]. Available from: https://www.kingsfund.org.uk/blog/2019/03/nhs-local-authorities-long-term-plan .
Culyer AJ. Cost-effectiveness thresholds in health care: a bookshelf guide to their meaning and use. Health Econ Policy Law. 2016;11(4):415–32.
Dillon A. Carrying NICE over the threshold. 2015. https://www.nice.org.uk/news/blog/carrying-nice-over-the-threshold . Accessed 21 June 2022.
Weinstein MC. A QALY is a QALY is a QALY—or is it? J Health Econ. 1988;7(3):289–90.
Cookson R, et al. Distributional cost-effectiveness analysis: quantifying health equity impacts and trade-offs. Oxford: Oxford University Press; 2020.
Book Google Scholar
Love-Koh J, et al. Estimating social variation in the health effects of changes in health care expenditure. Med Decis Mak. 2020;40(2):170–82.
Avanceña ALV, Prosser LA. Innovations in cost-effectiveness analysis that advance equity can expand its use in health policy. BMJ Glob Health. 2022;7(2): e008140.
Benkhalti M, et al. Development of a checklist to guide equity considerations in health technology assessment. Int J Technol Assess Health Care. 2021;37:e17.
National Institute for Health and Clinical Excellence. The guidelines manual. London: NICE; 2012.
Collins M, Latimer N. NICE’s end of life decision making scheme: impact on population health. BMJ Br Med J. 2013;346: f1363.
NICE. Our principles: the principles that guide the development of NICE guidance and standards. [cited 2022 21st Janaury]. Available from: https://www.nice.org.uk/about/who-we-are/our-principles .
Charlton V. Justice, transparency and the guiding principles of the UK’s National Institute for Health and Care Excellence. Health Care Anal. 2021;30:115–45.
Love-Koh J, et al. Aggregate distributional cost-effectiveness analysis of health technologies. Value Health. 2019;22(5):518–26.
Ward T, et al. Incorporating equity concerns in cost-effectiveness analyses: a systematic literature review. Pharmacoeconomics. 2022;40(1):45–64.
Asaria M, Griffin S, Cookson R. Distributional cost-effectiveness analysis: a tutorial. Med Decis Mak. 2016;36(1):8–19.
Cookson R, et al. Distributional cost-effectiveness analysis comes of age. Value Health. 2021;24(1):118.
Government Equalities Office. Equality Act 2010: guidance. London: GEO; 2013.
Fair J. Tackling socio-economic inequality locally. London: Just Fair; 2018.
Department of Health & Social Care. Health and social care act 2012. London: DHSC; 2012.
Department of Health & Social Care. The new public health role of local authorities. London: DHSC; 2012.
Local Government Association. A matter of justice: local government’s role in tackling health inequalities. London: LGA; 2018.
Public Health England. Public health profiles. 2021. [Accessed 15/9/2021]. Available from: https://fingertips.phe.org.uk .
Institute for Fiscal Studies. English local government funding: trends and challenges in 2019 and beyond. London: IFS; 2019.
Alexiou A, et al. Local government funding and life expectancy in England: a longitudinal ecological study. Lancet Public Health. 2021;6(9):e641–7.
Public Health England. Health inequalities dashboard. 2021. Acessed 10/12/2021.
Clowes M, Sutton A. “It’s A Grey Area”: searching the grey literature on how local governments use real-world data. Sheffield: The University of Sheffield; 2021.
Buck D, Dixon A. Improving the allocation of health resources in England. London: Kings Fund; 2013.
England NHS. Note on Clinical Commissioning Group (CCG) allocations 2019/20–2023/24. London: NHS England; 2019.
England NHS, Improvement NHS. NHS oversight framework 2019/20: CCG metrics technical annex. London: NHS England; 2019.
England NHS. NHS oversight framework for 2019/20. London: NHS England; 2019.
Charles A, Ewbank L, Naylor C, Walsh N, Murray R. Developing place-based partnerships: the foundation of effective integrated care systems. London: Kings Fund; 2021.
HM Government. Levelling up the United Kingdom: white paper. London: HM Government; 2022.
Department of Health and Social Care. Better, broader, safer: using health data for research and analysis. London: DHSC; 2022.
Frew E, Breheny K. Health economics methods for public health resource allocation: a qualitative interview study of decision makers from an English local authority. Health Econ Policy Law. 2020;15(1):128–40.
Hinde S, et al. The relevant perspective of economic evaluations informing local decision makers: an exploration in weight loss services. Appl Health Econ Health Policy. 2020;18(3):351–6.
Lomas J, et al. Resolving the “Cost-Effective but Unaffordable” paradox: estimating the health opportunity costs of nonmarginal budget impacts. Value Health. 2018;21(3):266–75.
Download references
Acknowledgements
The authors would like to thank: William Whittaker, Steven Senior, Katherine Brown, Gerry Richardson, Thomas Clarke, Tony Stone, and Suzanne Mason for their valuable contributions to the many different stages of this research.
Author information
Authors and affiliations.
Centre for Health Economics, University of York, Heslington, YO10 5DD, UK
Sebastian Hinde
Academic Unit of Health Economics, Leeds Institute of Health Sciences, University of Leeds, Leeds, UK
Department of Economics and Related Studies, University of York, Heslington, UK
James Lomas
School of Health and Related Research, University of Sheffield, Sheffield, UK
Matthew Franklin
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Sebastian Hinde .
Ethics declarations
This study is funded by the National Institute for Health Research (NIHR) Public Health Research (PHR) programme (NIHR award identifier: 133634) with in kind support provided by the NIHR Applied Research Collaboration Yorkshire and Humber (ARC-YH; NIHR award identifier: 200166). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Conflict of interest
No authors have any conflicts of completing interests to declare.
Ethics approval
Not applicable.
Consent to participate
Consent for publication, availability of data and material, code availability, author contributions.
SH, MF, and DH were responsible for the conceptualisation of the research, SH wrote the original draft with review, editing, and additional input from DH, MF, and JL.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (DOCX 21 KB)
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/ .
Reprints and permissions
About this article
Hinde, S., Howdon, D., Lomas, J. et al. Health Inequalities: To What Extent are Decision-Makers and Economic Evaluations on the Same Page? An English Case Study. Appl Health Econ Health Policy 20 , 793–802 (2022). https://doi.org/10.1007/s40258-022-00739-8
Download citation
Accepted : 10 May 2022
Published : 29 June 2022
Issue Date : November 2022
DOI : https://doi.org/10.1007/s40258-022-00739-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
The independent source for health policy research, polling, and news.


Race, Inequality, and Health
Published: May 28, 2024
KFF Authors:

Nambi Ndugga

Latoya Hill

Drishti Pillai

Samantha Artiga
Nambi Ndugga , Latoya Hill , Drishti Pillai and Samantha Artiga
Table of Contents
Introduction.
Despite being documented for decades, racial and ethnic disparities in health and health care persist with some widening in recent years. The COVID-19 pandemic and the nationwide racial justice movement in 2020 increased attention and calls to address racial and ethnic disparities in health and recognition of their root causes, including the ongoing impacts of racism and discrimination . Addressing health disparities is not only important from an equity standpoint but also for improving the nation’s overall health and economic prosperity. This chapter provides an overview of racial and ethnic disparities in health and health care and the factors that drive them, examines the actions to address them, and outlines future considerations.
What are Health and Health Care Disparities?
Health and health care disparities refer to differences in health and health care between groups that stem from broader social and economic inequities . There are multiple definitions of health disparities. Healthy People 2030 defines a health disparity as “a particular type of health difference that is linked with social, economic, and/or environmental disadvantage” and that adversely affects groups of people who have systematically experienced greater obstacles to health. The Centers for Disease Control and Prevention (CDC) defines health disparities as “preventable differences in the burden, disease, injury, violence, or in opportunities to achieve optimal health experienced by socially disadvantaged racial, ethnic, and other population groups and communities.” A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms “health inequality” and “inequity” are also sometimes used to describe unjust differences. Racism, which the CDC defines as the structures, policies, practices, and norms that assign value and determine opportunities based on the way people look or the color of their skin, results in conditions that unfairly advantage some and disadvantage others, resulting in negative mental and physical health outcomes for marginalized groups.
Reflecting the intersectional nature of people’s identities, some individuals experience disparities across multiple dimensions such as race and ethnicity, gender, or sexual orientation. Beyond race and ethnicity, disparities occur across other factors, including socioeconomic status, age, geography, language, gender, disability status, citizenship status , and sexual identity and orientation . Federal efforts to reduce disparities focus on designated priority populations , including “members of underserved communities: Black, Latino, and Indigenous and Native American persons, Asian Americans and Pacific Islanders and other persons of color; members of religious minorities; lesbian, gay, bisexual, transgender, and queer (LGBTQ+) persons; persons with disabilities; persons who live in rural areas; and persons otherwise adversely affected by persistent poverty or inequality.” These groups are not mutually exclusive and often intersect in meaningful ways. Disparities also occur within subgroups of broader racial and ethnic groups, such as ethnic identity, immigration status , and English proficiency .
Health equity generally refers to individuals achieving their highest level of health through the elimination of disparities in health and health care. Healthy People 2030 defines health equity as the attainment of the highest level of health for all people and notes that it requires valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and health and health care disparities. The CDC describes health equity as when everyone has the opportunity to be as healthy as possible.
What Factors Drive Racial and Ethnic Health Disparities?
The U.S. has a long history of policies and events that have resulted in stark differences in access to resources, opportunities, and power that contribute to racial and ethnic disparities in health today. Dating back to slavery and colonization of the Americas, people of color have been subject to abuse and mistreatment, including medical exploitation and experimentation, family separation, and efforts to eliminate cultural practices and languages. Historic discriminatory policies, such as redlining , have lasting effects today , leading to residential segregation of Black and Hispanic people into urban neighborhoods with more limited resources and increased health risks, including climate-related risks . Anti-immigrant policies have excluded and discriminated against certain groups, contributing to “othering” and “perpetual foreigner” stereotypes, particularly among Asian immigrants , with a resurgence in anti-Asian rhetoric amid the COVID-19 pandemic. Within medicine, disproven beliefs about biologic differences by race have led to race permeating clinical decision making and treatment in multiple ways, including through providers’ attitudes and implicit biases, disease stereotyping and clinical nomenclature, and its use in clinical algorithms, tools, and treatment guidelines.
Underlying inequities in social and economic factors that reflect historic and contemporary policies drive racial and ethnic disparities in health (Figure 1). Though health care is essential to health, studies suggest that social and economic factors, often referred to as social determinants of health , are the primary drivers of health outcomes. These include factors such as access to housing and food and economic and educational opportunities. Hispanic, Black, American Indian and Alaska Native, (AIAN) and Native Hawaiian and Pacific Islander (NHPI) people fare worse compared to White people across many social and economic factors compared to White people. Experiences for Asian people are mixed, although some subgroups of Asian people fare worse compared to White people, and Asian immigrants face certain additional challenges.

Experiences with unfair treatment and discrimination negatively impact health and well-being. Despite growing calls to address racism, many adults continue to experience unfair treatment and discrimination in their daily lives and in health care settings. A 2023 KFF survey shows that at least half of AIAN (58%), Black (54%), and Hispanic adults (50%) and about 4 in 10 Asian adults (42%) say they experienced at least one type of discrimination in daily life in the past year. These experiences include receiving poorer service than others at restaurants or stores; people acting as if they are afraid of them or as if they aren’t smart; being threatened or harassed; or being criticized for speaking a language other than English. Consistent with other research, which shows that racism has negative effects on mental health and results in certain negative physical health outcomes , the KFF survey finds that adults who report experiences with discrimination in daily life are more likely than others to report adverse effects from worry or stress as well as regular feelings of loneliness, anxiety and depression. Among those with discrimination experiences, 4 in 10 (40%) say they “always” or “often” felt anxious in the past year, compared to 14% of adults who rarely or never experience such discrimination (Figure 2). Similarly, those with discrimination experiences in their daily life are more than three times as likely as others to say they always or often felt lonely (26% vs. 7%) or depressed (25% vs. 7%) in the past year.
Racism and discrimination also negatively affect people’s health care experiences. Black, Hispanic, AIAN, and Asian adults report higher levels of unfair treatment when seeking health care than their White counterparts and are more likely to report having certain negative experiences with a health care provider because of their race and ethnicity (Figure 3). Reflecting these experiences, half or more of Hispanic, Black, and AIAN adults say they prepare for possible insults from providers or staff and/or feel they must be very careful about their appearance to be treated fairly during health care visits at least some of the time. About a quarter of adults who experienced unfair treatment, a negative experience with a provider, or a language access challenge say it led to worse health, being less likely to seek care, and/or switching providers.
Why Is It Important to Address Disparities?
Addressing disparities in health and health care is important not only from an equity standpoint but also for improving the nation's overall health and economic prosperity . Racial and ethnic health and health care disparities result in higher rates of illness and death across a wide range of health conditions, limiting the overall health of the nation. Research further finds that health disparities are costly, resulting in excess medical care costs and lost productivity, as well as additional economic losses due to premature deaths each year.
It is increasingly important to address health disparities as the population becomes more diverse and stark income inequalities persist. The U.S. Census projects that people of color will account for over half (52%) of the population in 2050, with the largest growth occurring among people who identify as Asian or Hispanic (Figure 2). Over time, the population has become increasingly racially diverse, reflecting shifting immigration patterns, a growing multiracial population, as well as adjustments to how the Census Bureau measures race and ethnicity. Over time, income inequality within the U.S. has also widened. As of 2022 , the top 10% of households in the U.S. had incomes above $216,000 compared with incomes at or below $17,100 among the lowest 10% of households.
What Is the Status of Racial and Ethnic Disparities in Health Today?
Major recognition of health disparities began nearly four decades ago. In 1985, the Report of the Secretary’s Task Force on Black and Minority Health (commonly known as the Heckler Report) documented persistent health disparities that accounted for 60,000 excess deaths each year and synthesized ways to advance health equity. The Heckler Report led to the creation of the U.S. Department of Health and Human Services Office of Minority Health and influenced federal recognition of and investment in many aspects of health equity. Federal recognition of disparities continued in 2003 with the Institute of Medicine’s, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care report, which identified systemic racism as a major cause of health disparities in the United States.
Despite the recognition and documentation of disparities for decades and overall improvements in population health over time, many disparities persist , and, in some cases, have widened over time. Analysis across a broad range of measures of health finds that Black and AIAN people fare worse than their White counterparts across half or more of these measures. Data for Hispanic people are more mixed relative to White people, with them faring better on some measures but worse than others. In the aggregate, Asian people fare the same or better than White people on many measures of health, although this finding masks disparities among subgroups of the population. Data gaps limit the ability to examine disparities among NHPI people; where data are available, they point to disparities, particularly for certain subgroups of this population. Some examples of disparities in health outcomes include:
- Black infants were more than two times as likely to die as White infants, and NHPI and AIAN infants were nearly twice as likely to die as White infants as of 2021 (Figure 5). Black and AIAN women also had the highest rates of pregnancy-related mortality across groups between 2017 and 2019.
- In 2021, the age-adjusted mortality rates for diabetes for AIAN, NHPI, and Black people were about twice as high as the rate for White people; Hispanic people also had a higher diabetes death rate compared to White people.
- Although Black people did not have higher cancer incidence rates than White people overall and across most types of cancer, they were more likely to die from cancer in 2020.
- In 2021, the HIV diagnosis rate for Black people was roughly eight times higher than the rate for White people, and the rate for Hispanic people was about four times higher than the rate for White people. AIAN and NHPI people also had higher HIV diagnosis rates compared to White people.
There also are ongoing racial and ethnic disparities in health coverage and access to care. Overall, Black, Hispanic, and AIAN people fare worse compared to White people across many measures of health coverage and access to and use of care. Despite large gains in coverage across groups since the Affordable Care Act, as of 2022, nonelderly AIAN, Hispanic, Black, and NHPI people were more likely to be uninsured compared to their White counterparts (Figure 6), with even higher uninsured rates among noncitizen Hispanic adults . In addition, Hispanic, Black, Asian, AIAN, and NHPI adults are more likely than White adults to report not having a personal health care provider, and Hispanic, Black, AIAN, and NHPI adults are more likely than White adults to report not seeing a doctor in the past 12 months because of cost.
The COVID-19 pandemic widened some racial and ethnic health disparities, including in life expectancy and mortality. During the height of the COVID-19 pandemic , AIAN, Hispanic, and Black people experienced higher rates of death. Beyond these direct health impacts, the pandemic disproportionately negatively impacted the well-being and social and economic factors that drive health for these and other underserved groups. Largely reflecting the impacts of the pandemic, between 2019 and 2021, there was a sharp drop-off in life expectancy , with particularly large declines among some racial and ethnic groups. AIAN people experienced the largest decline in life expectancy of 6.2 years, followed by Hispanic and Black people (4.1 and 3.6 years, respectively) (Figure 7). Following these declines, provisional data for 2022 show a recent uptick in life expectancy, however disparities persist across racial and ethnic groups. In 2022, life expectancy was lowest for AIAN people at 67.9 years, followed by Black people, whose expectancy was 72.8 years, both lower compared with the life expectancy of 77.5 years for White people.
What Are Recent Actions to Address Disparities?
Early in his presidency, President Biden issued a series of executive orders focused on advancing health equity. These included orders that outlined equity as a priority for the federal government broadly and as part of the pandemic response and recovery efforts . Federal agencies were directed to develop Equity Action Plans . In its Equity Action Plan, the Department of Health and Human Services (HHS) outlined a series of strategies, including addressing increased pregnancy and postpartum morbidity and mortality among Black and AIAN women; addressing barriers that individuals with limited English proficiency face in obtaining information, services, and benefits from HHS programs; leveraging grants to incorporate equity consideration into funding opportunities; implementing equity assessments; investing in resources to advance civil rights; and expanding contracting opportunities for small, disadvantaged businesses. The plan builds on earlier efforts that included increasing stakeholder engagement, establishing the Office of Climate Change and Health Equity , and establishing the National Institutes of Health UNITE Initiative to address structural racism and racial inequities in biomedical research. Since the release of its Equity Action Plan, HHS has taken actions to extend postpartum coverage through Medicaid and CHIP; issued rules to strengthen patient protections, including nondiscrimination protections; and issued guidance to ensure that telehealth services are accessible to people with disabilities and those with limited English proficiency.
The Centers for Medicare and Medicaid Services (CMS) released an updated framework to advance health equity for people covered by Medicare, Medicaid, CHIP, and the Health Insurance Marketplaces. The framework outlines five priorities, including expanding the collection, reporting, and analysis of standardized data on demographics and social determinants of health; assessing the causes of disparities within CMS programs and addressing inequities in policies and operations; building capacity of health care organizations and the workforce to reduce disparities; advancing language access, health literacy, and the provision of culturally tailored services; and increasing all forms of accessibility to health services and coverage. State Medicaid programs also are focused on addressing racial disparities in health outcomes. States have increasingly requested and/or received approval for waivers that aim to advance equity . Further, a growing number of states have approved or pending waivers with provisions related to addressing health-related social needs , such as food and housing, often focused on specific populations with high needs or risks.
The Administration and Congress took a range of actions to stabilize and increase access to health coverage amid the pandemic, with some extending beyond the Public Health Emergency but others ending. Early in the pandemic, Congress passed the Families First Coronavirus Response Act (FFCRA), which included a temporary requirement that Medicaid programs keep people continuously enrolled during the COVID-19 Public Health Emergency in exchange for enhanced federal funds. Primarily due to this provision, Medicaid enrollment grew substantially and the uninsured rate dropped, with AIAN and Hispanic people experiencing the largest decline. The American Rescue Plan Act (ARPA) of 2021 included an option, made permanent in the Consolidated Appropriations Act 2023, to allow states to extend Medicaid postpartum coverage from 60 days to 12 months, and the majority of states have taken steps to extend postpartum coverage. The Consolidated Appropriations Act also included a requirement for all states to implement 12 months of continuous coverage for children in Medicaid, supporting their coverage stability. However, the broader Medicaid continuous enrollment provision adopted during the Public Health Emergency ended on March 31, 2023, and millions of Medicaid enrollees have been disenrolled since then.
There has been a growing focus on addressing disparities in maternal health. The Biden Administration launched several initiatives focused on addressing inequities in maternal health, including releasing a Blueprint for Addressing the Maternal Health Crisis . Federal agencies also have announced plans and actions to support the Blueprint, including CMS, which released a maternity care action plan ; the Health Resources and Services Administration , which committed $90 million to various efforts aimed at improving maternal health, and the Office of the Assistant Secretary for Health , which invested $8.5 million in initiatives designed to reduce pregnancy-related deaths and complications that disproportionately impact people of color and those living in rural areas. Other recent actions have focused on enhancing data on maternal and infant health outcomes and disparities, increasing health care workforce diversity, and expanding access to doula and other services. States, providers, and health systems; foundations; and communities also are engaged in a broad range of efforts to advance maternal and child health and reduce disparities. Moreover, organizations are advocating for more interventions and supports to address maternal mental health and substance use issues , major causes of pregnancy-related mortality and morbidity.
There are efforts underway to increase data available to identify and address disparities. The exclusion of disaggregated data for smaller population groups, including AIAN and NHPI people from many datasets and analyses, limits the visibility and understanding of the health and health care disparities they face and inhibits efforts to address them. There are efforts underway to expand and improve availability of disaggregated data, including a charge from the Biden Administration to address the systemic lack of disaggregated data. In 2023, the Office of Management and Budget (OMB) released proposals to update the minimum standards for collecting and presenting data on race and ethnicity for all federal reporting by adding a new racial category for people who identify as Middle Eastern and North African, moving to collect race and ethnicity through a combined single question instead of asking about Hispanic or Latino ethnicity in a separate question from race, and requiring the collection of detailed racial and ethnic categories. Efforts to disaggregate data may help identify health disparities among smaller racial and ethnic groups and subgroups of larger racial and ethnic groups. They also may inform more culturally attuned and community-informed responses to addressing disparities.
What Are Emerging Issues Related to Racial and Ethnic Health Disparities?
Growing mental health and substance use concerns may contribute to racial and ethnic health disparities. Drug overdose and suicide deaths have increased since the onset of the COVID-19 pandemic, with some groups particularly affected. These trends may lead to new and widening racial and ethnic disparities. For example, AIAN, Black, and Hispanic people experienced larger increases in drug overdose death rates than White people between 2019 and 2021, resulting in the death rate for Black people newly surpassing that of White people by 2020. As of 2022, AIAN people had the highest suicide death rate, about one and a half times higher than the rate for White people (Figure 8). Despite growing mental health concerns, people of color continue to face disproportionate barriers to accessing mental health care, including lack of health insurance coverage and financial and logistical barriers to accessing care, lack of a diverse mental health care workforce, the absence of culturally informed treatment options, and stereotypes and discrimination associated with poor mental health. As such, it will be important for efforts to expand access to behavioral health to ensure that services address the cultural and linguistic needs of diverse populations.
The Dobbs decision may exacerbate the already large racial disparities in maternal and infant health. The decision to overturn the longstanding Constitutional right to abortion and elimination of federal standards on abortion access has resulted in growing variation across states in laws protecting or restricting abortion. These changes may disproportionately impact women of color, as they are more likely to obtain abortions, have more limited access to health care, and face underlying inequities that would make it more difficult to travel out of state for an abortion compared to their White counterparts. Restricted access to abortions may widen the already stark racial disparities in maternal and infant health. It may also have economic consequences associated with the direct costs of raising children and impacts on educational and employment opportunities. Further, women from underserved communities may be at increased risk for criminalization, as prior to the ruling, there were already cases of women being criminalized for their miscarriages, stillbirths, or infant death, many of whom were low-income or women of color.
Coverage losses following the end of the Medicaid continuous enrollment provision may lead to widening disparities in coverage. The Medicaid continuous enrollment provision, which had halted Medicaid disenrollments since March 2020 as a mechanism to stabilize coverage during the COVID-19 pandemic, ended on March 31, 2023.Following the end of the Medicaid continuous enrollment provision, states resumed Medicaid redeterminations and KFF tracking shows that millions of enrollees have been disenrolled from Medicaid. Although some may transition to other sources of coverage including Marketplace coverage or eventually reenroll in Medicaid, others may become uninsured. While the limited data available on disenrollments by race and ethnicity do not show large differences in disenrollment rates by race or ethnicity, people of color are more likely to be affected since they are disproportionately likely to be covered by Medicaid. Moreover, some groups, such as individuals with limited English proficiency and people with disabilities may face increased challenges in completing the Medicaid renewal process, increasing their risk of coverage loss even if they remain eligible for coverage.
Evolving immigration policies may impact the health and well-being of immigrant families. KFF survey data show that although most immigrants say their finances and employment are better as a result of moving to the U.S., many report facing serious challenges, which extend into health care . Although most immigrants are healthy and employed, they have high uninsured rates, face challenges affording care, and encounter linguistic and cultural barriers to care (Figure 9). Many immigrants lack sufficient information to understand how U.S. immigration laws affect them and their families, and immigration-related fears lead some to avoid certain activities, including participating in assistance programs for food, housing, or health care for which they or their children may be eligible. These fears persist despite the Biden Administration reversing Trump Administration public charge regulations with the aim of reducing fears about participating in programs, including Medicaid and CHIP. Some immigrants also face uncertainty about their immigration status, including people with Temporary Protected Status and Deferred Action for Childhood Arrivals (DACA) recipients. DACA implementation is currently limited subject to court orders , and if the DACA program is found to be unlawful, individuals would lose their DACA status and, subsequently, their work authorizations. Immigration-related fears may increase amid a growing focus on immigration enforcement following the lifting of the Title 42 restrictions that had suspended the entry of individuals at the U.S. border to protect public health during the COVID-19 pandemic and increasing anti-immigrant rhetoric leading into the next presidential election.
Expansions in access to health coverage for immigrants could mitigate some of the challenges they face accessing health care. States vary in the coverage they provide for their low-income population overall and immigrants specifically. Those that have adopted the ACA Medicaid expansion have broader eligibility for low-income adults, but noncitizen immigrants still face eligibility restrictions for this coverage. Some states have expanded coverage for immigrants by taking up options available in Medicaid and CHIP to cover recent lawfully present immigrant children and pregnant women , and some states have extended coverage to some groups regardless of immigration status through fully state-funded programs . Immigrants in states that have taken up more of these coverage options are less likely to be uninsured. It remains to be seen if additional states will take action to adopt these options or provide state-funded coverage. In April 2023, the Biden Administration proposed a rule to expand eligibility for health coverage to DACA recipients, who are prohibited from enrolling in federally-funded coverage under existing rules, but the proposed rule is yet to be finalized as of March 2024 and the future of the DACA program remains uncertain.
As climate-related events become more common, the impacts on health and health care will increase in both frequency and intensity, with disproportionate impacts on historically marginalized and under-resourced groups. Climate and weather can negatively impact individual and population-level health through multiple pathways, and climate-related health risks are expected to increase going forward. While climate change poses health threats for everyone, people of color, low-income people, and other marginalized or high-need groups face disproportionate risks due to underlying inequities and structural racism and discrimination. For example, historical policies such as redlining have led to residential segregation of Black people into urban neighborhoods that increase their exposure to extreme heat and poor air quality.
Disparities in access to novel drug therapies and technologies may contribute to and potentially widen racial and ethnic health disparities. People of color have higher rates of chronic diseases, including Alzheimer’s, diabetes, obesity, and other diseases which may benefit from new medical advancements. However, at the same time, they may face increased barriers to accessing new or novel drugs or therapies, which may exacerbate disparities in health going forward.These include affordability challenges due to the high out-of-pocket costs for many new drugs and therapies, which often are not covered by insurance; lack of racial diversity in clinical trials used to test the effectiveness and safety of new drugs and therapies, and underlying biases in clinical decision-making processes, which may increasingly rely on artificial intelligence or algorithms.
Future Outlook
Looking to the future, racial and ethnic disparities in health and health care remain a persistent problem despite their longstanding recognition and growing calls to address them. These disparities reflect ongoing impacts of racism that lead to structural inequities in resources and opportunities as well as bias and discrimination in health care and daily life. Some key challenges ahead for eliminating racial and ethnic health and health care disparities include:
- How to address underlying social and economic inequities that drive disparities in health?
- How to close racial and ethnic gaps in health coverage and prevent further widening of disparities in health coverage?
- How to increase diversity of the health care workforce and expand access to culturally and linguistically competent care?
- How to ensure all communities are visible in data to identify and address disparities?
- How to protect communities from the uneven impacts of climate change and mitigate widening disparities due to climate-related health risks?
- How to mitigate the perpetuation of disparities amid the growing use of AI and clinical algorithms to guide clinical decision-making?
Addressing racial and ethnic health and health care disparities is of increasing significance as the diversity of the country grows. It is important not only from an equity standpoint but also for improving the overall health and economic prosperity of our nation.
- Survey on Racism, Discrimination and Health: Experiences and Impacts Across Racial and Ethnic Groups
- Health and Health Care Experiences of Immigrants: The 2023 KFF/LA Times Survey of Immigrants
- Disparities in Health and Health Care: 5 Key Questions and Answers
- Key Data on Health and Health Care by Race and Ethnicity
- Health Coverage by Race and Ethnicity, 2010-2021
- What is Driving Widening Racial Disparities in Life Expectancy?
- Racial Disparities in Maternal and Infant Health: Current Status and Efforts to Address Them
- Key Facts on Health Coverage of Immigrants
- Climate Change and Health Equity: Key Questions and Answers
- Medicaid and Racial Health Equity
- How History Has Shaped Racial and Ethnic Health Disparities: A Timeline of Policies and Events
Ndugga, Nambi, Hill, Latoya, Pillai, Drishti, & Artiga, Samantha, Race, Inequality, and Health. In Altman, Drew (Editor), Health Policy 101, (KFF, May 28, 2024) https://www.kff.org/health-policy-101-race-inequality-and-health/ (date accessed).
- Search Menu
- Sign in through your institution
- Accident and Trauma
- Anaesthesia
- Cardiothoracic Surgery
- Cardiovascular Disease
- Child and Adolescent Psychiatry
- Critical Care/Intensive Care/Emergency Medicine
- Dermatology
- Endocrinology
- Environment and Disease
- Gastroenterology
- General Practice
- Geriatric Medicine
- Haematology
- Health Policy
- Health Economics
- Infectious Diseases
- Liver Disease
- Neonate Medicine
- Neurophysiology
- Neurosurgery
- Obstetrics and Gynaecology
- Occupational Medicine
- Ophthalmology
- Otolaryngology
- Paediatric Medicine & Surgery
- Palliative Medicine
- Perioperative Medicine
- Public Health Medicine
- Renal Medicine
- Respiratory Medicine
- Rheumatology
- Sports Medicine
- Transplantation
- Tropical Medicines
- Advance articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About British Medical Bulletin
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, trends in health inequalities, share power over resources and increase the influence that the public has on resources to improve determinants of health, promote healthy development in early childhood, strengthen the role of the health sector, place working and a new framework for addressing inequalities, acknowledgements.
- < Previous
A case study of new approaches to address health inequalities: Due North five years on
- Article contents
- Figures & tables
- Supplementary Data
Paul W Johnstone, A case study of new approaches to address health inequalities: Due North five years on, British Medical Bulletin , Volume 132, Issue 1, December 2019, Pages 17–31, https://doi.org/10.1093/bmb/ldz037
- Permissions Icon Permissions
When local councils took on responsibility for public health in England in 2013, leaders from across the north of England met to consider the scale of the challenge. As a result, Public Health England commissioned the Due North Report which outlined new approaches in tackling health inequalities. This second paper outlines what has been learnt in five years as a case study. This includes influencing devolution deals and new elected city mayors, planning for economic growth in deprived areas and developing community asset-based approaches. The paper outlines a new framework for place-based planning to reduce health inequalities.
Data was gathered from annual reports from north of England directors of public health, Office for National Statistics, Public Health England’s fingertips database and regional and national publications and strategies such as the Northern Powerhouse.
Devolution to English cities and councils as ‘places’ is a new opportunity to address local needs and inequalities. Due North has supported a new public health narrative which locates health action in the most fundamental determinants—how local economies are planned, jobs created and power is to be transferred to communities and connects reducing years of premature ill health to increased economic productivity. Community asset approaches to empower local leaders and entrepreneurs can be effective ways to achieve change.
The north–south divide in health is not closing and may be worsening. Different ways of working between local government, health and business sectors can inhibit in working together and with communities.
Place-based working with devolved powers can help move away from top down and silo working, empower local government and support communities. Linking policies on health inequalities to economic planning can address upstream determinants such as poverty, homelessness and unsafe environments.
More research is needed on; (i) addressing inequalities at scale for interventions to influence community-led change and prosperity in deprived areas, and (ii) the impact of devolution policy on population health particularly for deprived areas and marginalised group.
Commissioning high profile reports like Due North is influential in supporting new approaches in reducing inequality of health through local government, elected mayors; and working with deprived communities. This second paper describes progress and lessons.
The North of England, with a population 15 million, has a long history of poor health and inequalities. This has led to calls to address the ‘north–south health divide’. 1 Poor health at this scale is caused by a complex mix of economic, environmental and social factors, and the causes outlined by Marmot and others are well known. 2 Most determinants of health lie outside the influence of the health sector. When responsibility for public health returned to local government from the National Health Service (NHS) in England in 2013, 3 leaders and directors of public health from 50 local councils met to consider how best to use these new powers in the north to develop fresh approaches to tackling wider determinants of health. As a result, Public Health England commissioned a panel of leading academics in the north to assess the evidence and actions needed. The panel’s response, published in the Due North Report in 2014, has four overarching recommendations and has been a landmark in fostering change through new collaborations, actions and policies locally and nationally. 4
Due North Report recommendations (4).

Due North has supported a new public health narrative which locates health action in the most fundamental determinants—how local economies are planned, jobs created and power transferred to areas and communities. New asset-based approaches with local communities have developed with a focus on health inequalities. These bring together policies of councils, devolution, local community ‘asset’ development and health services and focus on communities living in a geographic ‘place’.
The Due North Report and initial work were described as a case study in this journal in 2015. 5 In response to the national and international interest, this second paper describes what has happened since, with learning and growing points and further action needed.
As context, a short summary on health trends is first outlined. Health inequalities are usually measured as the difference in life expectancy between the most affluent and most deprived deciles. In England, this has widened between 2010/12 and 2015/17, with decreasing life expectancy at birth for women in the poorest decile (see Fig. 1 ).
Life expectancy at birth by deprivation decile for women showing widening inequality of life expectancy. England. 2010–12 to 2015–17. Source: PHE, Public Health Outcomes Framework.

In more detail, the average life expectancy at birth in each of the 152 upper tier local authorities in England gives a clear picture of the north–south divide when compared against the England average. ( Fig 2 ).
Female life expectancy at birth by local authorities 2015–17, comparing areas with the England average. Source: PHE analysis of data from Office for National Statistics.

A better measure of the impact of poor health is by ‘healthy life expectancy’-the number of years living in good health. This measure helps show the burden of disease to groups, towns and cities and the levels of inability to work and contribute to society and the local economy. Figure 3 shows the gap for years spent in good health by deprivation deciles. There is a 19 year difference between the most deprived and most affluent deciles of the population for men and for women. Men in the most deprived decile will live in good health to only 52 years. At ward level, there is an even greater difference. For example, in Blackpool, healthy life expectancy for men in one ward is just 47.1 years. 6
The gap in healthy life expectancy for men and for women by neighbourhood areas (lower super outputs areas) in deprivation deciles, 2014–16.

Trend in life expectancy at birth by English Regions (and change in years) from 2010–12 to 2015–17 (women). Source: PHE analysis of data from Office for National Statistics.

Has the north–south divide changed?
Figure 4 shows the life expectancy from birth trend for females by English regions. This shows little change in position for inequalities for the three regions of the north of England.
For male healthy life expectancy, there is a widening inequality by English regions shown in Figure 5 . 1 In the South East region, the average man can expect to live for 66.1 years without a long-term condition whereas in the North East this is 59.5 years. Again, there appears to be no closure of the gap in healthy life expectancy across the three northern regions.
Trend in healthy life expectancy at birth (males) by English Regions (and change in years). Source: PHE analysis of data from Office for National Statistics.

Despite these headline indicators, there have been important developments to reframe action on the wider determinants of health and inequalities with the location of the public health role into local government, something Due North has supported. Practitioners and academics meet annually in what has become a movement to advocate for change and exchange learning. As a result, we have developed an impressive body of evidence via a network of academics and practitioners across the north. 7
These are now described using the recommendations of the Due North Report.
Tackle poverty and economic inequality within the North
Due North identified weak labour markets, worklessness and poverty as major contributors to intergenerational poor health and inequalities in the north. It recommended linking economic plans to reduce poverty. Other national recommendations included introducing a living wage and promoting a ‘Health in All Policies' approach. 8
The coalition government in 2010 recognised the need to invest in the north and initiatives such as the Northern Powerhouse 9 and Transport for the North 10 are still in place. However, the government’s devolution policies provided a bigger potential impact using Due North’s evidence. After the coalition government abolished Regional Development Agencies in 2010, business-led partnerships involving councils were formed to promote sub-regional economic development called local enterprise partnerships (LEPs) funded through Local Growth Funds and European Structural Funds. 11 LEPs became the principal organisations for providing business support, innovation and business grant funding. The government also asked groups of councils to work together on common issues including infrastructures and urban areas to strengthen the voice of ‘city regions’. Known as ‘combined authorities’, they were subsequently encouraged to apply for more powers through so-called ‘devolution deals’. 12 This meant some places could take on new powers to elect ‘metro-mayors’ drawing on experience from London, Scotland and Wales and LEPs effectively became their advisory economic arm. Subsequently, all LEPs and Mayoral Combined Authorities have been asked to lead the development of Local Industrial Strategies drawing on the government’s Industrial Strategy published in 2017. 13
Local industrial strategies bring together planning for physical infrastructure, human capital and economic investment. The National Industrial Strategy tasks areas with a ‘Grand Challenge’ to increase healthy life expectancy by at least 5 years over a 17-year period, while reducing the gap between the richest and poorest. A key part of these new strategies is to draw on an approach called ‘inclusive growth’, using evidence published by the Inclusive Growth Commission which set out how economic growth should systematically include deprived areas. 14 This has opened up a number of innovated approaches, for example combining anti-poverty and homelessness strategies with economic development (in Leeds City Council). 15 The different approaches to devolution and industrial strategies across the north (for example between the electoral mayoral models in Greater Manchester and Liverpool) provide an opportunity to assess different impacts on economies and other outcomes such as social value—the way local people value their experience of living in a local place.
For public health, these developments led to a new narrative linking healthy life expectancy to economic productivity which has resonated strongly across the North of England. This recognises that poor areas with high levels of chronic disease are an economic burden to a place. The health service has a role in addressing this together with improved economies leading to a stronger job market and improved health; so health and wealth are ‘two sides of the same coin’. This changes the purpose of tackling inequalities from a social, moral and justice argument to one that embraces the economy and productivity—a narrative that appeals to politicians and mayors across the political spectrum. Many councils across the north use this narrative. This also reflects in other northern strategies such as Transport for the North—the latest version of which mentions health 128 times. 10 Furthermore, Directors of Public Health in the north reflect this new narrative with local recommendations in annual reports as a way of tackling this most fundamental of health determinants. 16 , 17 Reports such as this linked health and creating jobs for the first time in this context.
The Due North Report cited powerlessness as a fundamental determinant. People and communities who feel that they have little control over their lives are less likely to be employed, leave school early and live in unsafe environments that reduce the chance of better health. This sense of hopelessness is reflected in weak democratic engagement. The one exception to this was the Brexit referendum in 2016, where higher rates of people from deprived areas voted for the first time. Commentators were quick to point out the connection: ‘Brexit is a cry of outrage against the imbalance of wealth and power’ said the head of the Institute for Public Policy Research (North). 18 Indeed, Theresa May on becoming Prime Minister said she wanted to ‘fight against the burning injustice that, if you’re born poor, you will die on average 9 years earlier than others.’ 19 Greg Clark, Secretary of State for Local Government in 2016 with responsibility for devolution in England, commented on Brexit that ‘among the answers so the challenge that the referendum result poses is to have a much bigger role for the local in our national life’. 20
Elected ‘metro’ mayors
As a result of the government’s devolution policy described earlier, six new ‘metro-mayors’ were elected in May 2017 covering leading city regions and had increased responsibilities for local services. At the time of writing, five out of nine devolution plans are in the North of England. Figure 6 shows the elected mayors and devolution agreements covering 37% of English population including Greater London Authority by January 2019. 21
Metro Mayoral Map of England 2018.

Public Health England with local directors worked alongside new elected mayors in a variety of ways, joining joint health and social care partnership boards (Greater Manchester) 22 , mayoral teams (Liverpool) and new ‘prevention’ boards. The North of Tyne devolution deal, which elected a mayor in 2019, was specifically supported by a health and social care commission led by Public Health England. 23 Six out of seven mayoral manifestos and subsequent work programmes have health as a key theme linking to inclusive growth electoral promises. 21 , 24
Communities
The Due North Report argued that those with less influence and power are less enabled to control their lives, environment and use of public resources in improving their health and well being. Devolution of power should be strengthened still further from local authorities to communities and neighbourhoods. This means giving local community leaders, the voluntary and community sector and social enterprises more power over decisions about their lives and places, particularly in the poorest and most marginalised communities. For many in public services, this means a change in ‘mindset’ from the traditional way of identifying needs and deficits and then providing services, to one that supports the development and spread of existing ‘assets’ in the community. This requires change by public services to supporting ideas, motivation and leadership from the communities themselves rather than from outside the area. 25
Infographic of the Wortley community programme showing return on investment.

Well North challenges traditional approaches to regeneration.

Findings from NHSA’s Health for Wealth Report. 41

The last five years has seen a real growth of interest in community asset approaches with a rich, diverse mix in public health practice across the North—reflected the need for local development with local communities rather than top-down standardised interventions. Sharing this learning has been an essential part of the approach with PHE’s support and NICE guidance (2016) supporting development of a local approach to engaging and empowering communities. 26 The annual Due North conference is the cornerstone of this sharing, and the 2018 event held at Anfield (the home of Liverpool Football Club) was a good example. 27 The role of community ‘anchor organisations’ was a key theme. ‘Anchors’ is a term to describe organisations from the public, private and voluntary sectors who have developed their roles as assets working with and for their local communities to improve health and well-being. Mersey Care Trust for example has a ‘staff wellbeing scheme’ based on a 360-degree mentoring programme for all its employees from the immediate area of Sefton, one of Liverpool’s most deprived areas. As the area’s main employer, they report a measurable impact on well-being. Another example is Liverpool City Museums, who teamed up with the NHS to support people with dementia. The ‘House of Memories’ programme uses museum memorabilia and digital technology and has measured its impact in economic terms as ‘return on investment’. 28 Other community projects now have wider support for their health improving agendas such as Royds in Bradford 29 and Wortley Community Association in Leeds. 30 The Wortley programme evaluates its work using health economic methods to show social value and return on investment for donors demonstrating the connection between community projects, anchors and linking to local economies (See Figure 7 ).
Some places such as Wigan Council in Greater Manchester are beginning to mainstream community asset approaches and redefine their relationship with local communities—‘a new contract between ‘the citizen and state’. 31
Another leading North of England project is Well North. Started in 2015, Well North is made of 10 pilots in the most challenged and deprived communities. The Well North team develop a relationship with a local community in partnership with them, their local council and businesses. The essence is an organic approach which moves beyond the traditional siloed approaches and traditional barriers between sectors, government departments and communities. The approach supports local ideas and entrepreneurs through discussion and ‘moments of critical change’. 32 It recognises large amounts of tax payers’ money have been spent on top-down initiatives which fail and generate dependency cultures. This undermines people’s health, energy and passion. The evaluation, led by the University of Manchester, challenges traditional evaluation methods and provides real-time web-based evaluation for communities and local organisations. This is available at the Well North website (See Figures 8 and 9 ).
Learning from Well North and other asset approaches is published with a suite of evidence to support asset approaches by PHE 33 , 34 and a national movement called Locality. 35
The Due North Inquiry recommended a ‘rights based’ approach to promoting child health, extending children’s centres and services, flexibly working for parents and tackling child poverty. Progress has been mixed and locally councils, and the NHS has struggled to prioritise children’s services against budget reductions due to austerity. Recent publications suggest the impact of austerity has been highest in the north and for children’s services, and this is reflected in a worsening trend in infant mortality—a headline indicator of child health. 36 , 37 PHE’s recent analysis confirms a persistent inequality nationally between 2010–12 and 2015–17, with infant mortality rate in most deprived decile being 2.3 times higher than for the least deprived. 38
Yet despite this, there have been some developments in the context of Due North thinking. Greater Manchester, for example, has combined NHS and local government approaches in a single ‘Early Years Framework’ which pools children’s services resource to fund agreed priorities. The measurement and support for disadvantage children in ‘school readiness’—the physical, mental and social preparedness so a child can maximise their education development, is one such priority, and Greater Manchester has reported improvements in this important health outcome. 39
The Due North Inquiry called on public services, the NHS and PHE to influence health inequalities, integrate services with employment, debt and welfare advice and for NHS providers to enhance their role as local employers and procurers. In the last 5 years the impact of these recommendations has been mixed where competition and opening up to markets has been the prevailing NHS policy following the 2013 reforms. This is set to change with the introduction of a new NHS ‘Long Term Plan’. This is discussed shortly.
Firstly though, as a result of the Due North report, progress has been made in the recognition of NHS hospitals as economic powerhouses for their local areas. A major new report published in 2018 was led by a consortium of Due North academics and NHS provider leaders—the Northern Health Service Alliance (NHSA). 40 The research shows productivity between the North and the South of England is £4 per person per hour lower. Given both health and productivity are lower in the North, the NHSA confirms ‘public health and the NHS are vital for productivity in the North and links evidence of health to wealth creation’. Improving health in the North to reduce this gap in productivity by 30% will generate an additional £13.2 billion in UK GVA. It recommends that ‘improving public health in the North is a route to increase productivity and national prosperity’ (See Fig. 10 ).
The new NHS Long Term Plan to reduce health inequalities.

The ‘Manchester Economic Assessment’ commissioned by Greater Manchester is a similar report and recommends reorientating the NHS to link health and prosperity. 42 These publications have supported wider discussions that have informed the new national NHS Long Term Plan which recognises this economic generator role (See Box 2 ). 43 It also requires the NHS to develop population health management approaches (PHM) to reduce healthcare inequalities and for healthcare to have a focus on prevention and strengthen primary care through the development of networks. PHM is defined as a healthcare discipline which studies and facilitates care delivery across a general population or group of individuals and was initially developed in the USA. 44 The Long Term Plan recommends developing PHM for the NHS context and is widely supported. 45 Analytics to support PHM are provided by a national data resource called RightCare. 46 Applying PHM approaches to a population identifies care needs and deficits at scale for certain disease groups or high-intensity service users such as blood pressure monitoring and identification of patients with atrial fibrillation at risk of developing stroke.
At the time of publication, the first drafts of local Long Term Plans are being agreed. These include the development of primary care networks; groups of general practices cover populations of 30–50 000 and plans to integrate care across health and social care. Many local areas are using this opportunity to link primary care to community development using the learning from Due North, for the first time bringing together health service plans for prevention via primary care with devolution and asset community approaches. Key to this will be aligning with place-based working, and this is now explored.
Place-based working has evolved since the 1990s following government strategies for neighbourhood renewal, 47 health action zones, 48 local area agreements 49 and more recently devolution deals as described above. Due North recommended integrating budgets and focusing on prevention, and many local authorities in the north have pioneered this approach. PHE defines place-based working as ‘blurring (sic) institutional boundaries across a location to provide integrated care for individuals, families and communities. Energy, money and power shifts from institutions to citizens and communities. Devolution becomes an enabler for a reform programme that starts to deliver on the long held promise of joining up health and social care for a population in a place, with the ultimate aim to improve the public’s health and reduce health inequalities’. 50
Thus, with the introduction of PHM, integrated care and primary care networks for the NHS, three complementary approaches are being developed which offer a model of working to reduce health inequalities. Three categories of interventions are identified: civic decision-making (such as industrial strategies); community asset approaches and the NHS addressing inequalities through population health management. The separate contributory effects are potentially additive so that together a more substantial change will be possible. PHE is developing this model called a Population Intervention Triangle (PIT) 51 (See Fig. 11 ).
This model shows how interventions can be coordinated at a place-based level to maximise reduction of health inequalities. In this way, with less emphasis on spending and more on mobilisation, a place-based approach is not only cost-effective but is also more effective than single interventions.
The Population Intervention Triangle developed by PHE.

More research
The learning from Due North and subsequent new approaches to tackling health inequalities requires more research, particularly on complex interventions such as devolution and asset approaches for marginalised populations. This will need new methods for measuring inequality outcomes, as existing measures rely on reducing deaths across socioeconomic groups and infant mortality and are not helpful for local communities and leaders. Indeed, the latest report from the Chief Medical Officer (England) made a recommendation to revise health inequalities measures. 52 Alternative approaches to measuring health and inequalities are currently being explored by the Medical Research Council and the National Institute of Health Research. Key to this will be development of new collaborations across academic centres, public services and the communities. Due North specifically led to the development of two networks: Equal North—a collaboration of over 200 practitioners and academics across the north; and more recently, the creation of the North Universities Public Health Alliance launched in 2019. 53 , 54 These two networks have an important role to develop new community orientated outcomes research.
This case study demonstrates the role of collective leadership across councils and health, business and voluntary sectors in influencing change for local government's public health role. Evidence from the Due North Report has led to influencing economic planning, manifestos of elected majors and devolution deals. Due North pitched its recommendation in the North of England but has been influential nationally. It has supported the evolution of local thinking on ‘place’, and planning for inclusive growth and health and how to engage with and empower local communities. Public health practitioners have used Due North as a guide and continue to meet annually to share learning. For the northern regions, it has played a role in supporting the Northern Powerhouse and Transport Strategy and universities through practitioner and academic networks.
Due North as a movement continues to share learning. It supports a new narrative linking public health and inequality to economic productivity which offers wider appeal. Further devolution of power in England to cities and councils is likely to be beneficial, empowering to address local needs. At a neighbourhood level new approaches to community asset working offer huge potential for change, particularly with local entrepreneurs and ‘anchor’ organisations such as schools, hospitals, museums and religious centres. Learning from the WHO healthy cities movement will help in developing both these approaches. 55 Finally, the NHS Long Term Plan now means the NHS is prioritising prevention and inequalities of healthcare through population health management and an increased role for primary care. These developments offer a potential framework for inequalities bringing together at a place-level, local authority civic plans such as industrial growth with community-led action and the NHS, in one aligned local strategy.
Yet health inequalities are widening. The most marginalised and deprived communities continue to feel a sense of hopelessness. This was a significant message from the Brexit referendum. ‘Place working’ remains an aspiration in many areas due to cultural and accountability differences within and between the public sector and business and local communities. Therefore, to further address the north–south divide, the following are recommended for the next stage of this journey.
Firstly, the role of central government is not addressed in the case study. A stronger national economic and fiscal policy is needed to support the Northern Powerhouse, re-balance the economy and invest in infrastructure. Without this fundamental determinant, local action to improve health will be limited. The Industrial strategy with its Grand Challenge offers an opportunity to develop a consensus on health inequality at a national level, learning from previous national inequalities strategies. 56 The health of children and young people must be prioritised. Secondly, devolution policy should be extended with meaningful devolution of resources and power. Mayors could assume greater responsibility, for example in raising taxes on tobacco, alcohol and sugar, or reducing taxes to promote healthy lifestyles tailored to the needs and priorities of local areas. There is a risk that devolution stops at city level and does not continue to local communities. Asset approaches are often small projects, not at scale, with the role of local leaders, especially local entrepreneurs, being underdeveloped. Elected mayors could move to develop holistic approaches to health with engaged communities. Thirdly, the NHS, which is so used to being managed from national government, needs to use different types of ‘place’ leadership helping to break down cultural barriers and engage their communities as ‘anchors’ and integrate action on access to services.
Finally,there are no quick fixes. Meaningful reductions in health inequalities and a reduced north-south divide will take time. We must use evidence from movements like Due North, as a social movement for change which creates networks with communities, supports agencies and places and shares best practice and learning.
I would like to thank Dr Andrew Furber and David Herne in PHE Yorkshire and Humber and North West, and Allan Baker and Simon Lewry in PHE’s Knowledge and Intelligence Directorate for helpful comments on the text and analyses. I wish to thank Ben Lucas from Metro-dynamics for his expertise in supporting Public Health England in working with new elected mayors which is reflected in this paper. Finally, I thank Prof. Jane South from Leeds Beckett University, as a PHE adviser on communities and for helpful comments.
This indicator is based on self-assessment of general health, so people may have a long-term condition and still consider themselves to be in good general health.
The Big Debate : North-South Divide . Yorkshire Post . 18 Nov 2013 . https://www.yorkshirepost.co.uk/news/analysis/the-big-debate-north-south-divide-1-6250935 .
Google Scholar
Google Preview
Marmot M et al. ( 2010 ) Fair Society Healthy Lives ( The Marmot Review ) http://www.instituteofhealthequity.org/projects/fair-society-healthy-lives-the-marmot- review .
UK Government . Health and Social Care Act 2012 . London : HMSO . https://www.gov.uk/government/publications/health-and-social-care-act-2012-fact-sheets .
The Due North Report https://cles.org.uk/our-work/publications/due-north-report-of-the-inquiry-on-health- equity-for-the-north/ .
Johnstone PW . Health, equity and the north of England: a case study on a new approach . Br Med Bull 2015 ; 116 : 29 – 41 . doi: 10.1093/bmb/ldv048 Advance Access Publication Date: 17 November 2015 .
Health state life expectancy by 2011 Census wards in England and Wales . Office for National Statistics . https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandlifeexpectancies/datasets/healthstatelifeexpectancyby2011censuswardsinenglandandwales .
Equal North research network . http://www.fuse.ac.uk/research/healthinequalities/equalnorthresearchandpracticenetwork/ .
Health in All Policies . A framework for country action . World Health Organisation 2013 . https://www.who.int/healthpromotion/frameworkforcountryaction/en/ .
‘ We Need a Northern Powerhouse ’: Rt Hon George Osborne. Chancellor of Exchequer . HM Treasury . June 2014 . https://www.gov.uk/government/speeches/chancellorwe-need-a-northern-powerhouse .
Transport for the North . https://www.who.int/healthpromotion/frameworkforcountryaction/en/ .
Local Enterprise Partnerships . 2010 to 2015 government policy: Local Enterprise Partnerships (LEPs) and enterprise zones . Updated May 2015 . https://www.gov.uk/government/publications/2010 -to-2015-government-policy-local-enterprise-partnerships-leps-and-enterprise-zones/2010-to-2015-government-policy-local-enterprise-partnerships-leps-and- enterprise-zones .
Devolution and mayors: what does it mean? . UK Government . 2017 . https://www.gov.uk/government/publications/devolution-and-mayors-what-does-it-mean .
The UK industrial strategy . Department of Business, Innovation and Skills . 2017 . https://www.gov.uk/government/topical-events/the-uks-industrial-strategy .
Inclusive Growth Commission . Royal Society of Arts . https://www.thersa.org/action-and-research/rsa-projects/public-services-and-communities-folder/inclusive-growth-commission .
Leeds Inclusive Growth Strategy . 2018–2023. Leeds City Council . http://www.leedsgrowthstrategy.co.uk/wp-content/uploads/2018/06/Leeds-Inclusive-Growth-Strategy-FINAL.pdf .
Director of Public Health Report . Sheffield City Council. Greg Fell . 2018 . Sheffield City Council . https://www.sheffield.gov.uk/content/dam/sheffield/docs/public-health/health-wellbeing/Health%20and%20Wealth%20report%202018%20updated.pdf .
Annual Report of the Director of Public Health . 2016–17. Salford City Council . David Herne . https://www.partnersinsalford.org/media/1044/public_health_annual_report_1617.pdf .
IPPR North . Ed Cox https://www.ippr.org/impact-story/the-state-of-the-north-2016 (and quoted in Yorkshire Post 2016).
Theresa May , Prime Minister. 13 July 2016 .
Greg Clark MP . Secretary of State for Local Government , 2016 .
Metro-dynamics . Ben Lucas . http://www.metrodynamics.co.uk/our-team/ .
Greater Manchester Health and Social Care Partnership board . http://www.gmhsc.org.uk/ .
North East Health and Social Care Commission . NE Councils Association . 2016 . https://northeastca.gov.uk/wp-content/uploads/2018/04/Health-and-Wealth-Closing-the-Gap-in-the-North-East-Full-Report.pdf .
Doyle Y , Johnstone P . Health benefits of devolution in England: international lessons . Postgrad Med J 2016 ; 0 : 1 – 4 .
Kretzmann J , McKnight J . Building Communities From the Inside Out: A Path Toward Finding and Mobilizing a Community’s Assets , 3rd edn. Chicago, IL : ACTA Publications , 1993 , 14. ISBN 978-0-87946-108-9. OCLC 36708153 .
Community engagement : Improving health and wellbeing and reducing health inequalities . NICE guideline [NG44] Published date: March 2016 https://www.nice.org.uk/guidance/ng44 .
Twitter . #DueNorth5
Liverpool City Museum Dementia programme . House of Memories . http://houseofmemories.co.uk/ .
Royds Community Association . Enterprise Park. Bradford . http://www.royds.org.uk/ .
Wortley community Centre . Leeds . https://newwortleycc.org/ .
Wigan Council . The Deal . https://www.wigan.gov.uk/Council/The-Deal/The-Deal.aspx .
Well North . http://www.wellnorth.co.uk/ .
A guide to community-centred approaches for health and wellbeing (Full report) . Public Health England . 2015 . https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/417515/A_guide_to_community-centred_approaches_for_health_and_wellbeing__full_report_.pdf .
The Knowledge Hub . https://khub.net/web/guest/welcome?p_p_state=normal&p_p_mode=view&refererPlid=105027891&saveLastPath=false&_com_liferay_login_web_portlet_LoginPortlet_mvcRenderCommandName=%2Flogin%2Flogin&p_p_id=com_liferay_login_web_portlet_LoginPortlet&p_p_lifecycle=0&_com_liferay_login_web_portlet_LoginPortlet_redirect=%2Fgroup%2Fphe-community-centred-asset-based-approaches .
Locality. Keep it Local . The campaign calling for councils to commission locally . Accessed May 2019 . https://locality.org.uk/policy-campaigns/keep-it-local/ .
Robinson T , Barr B , Brown H , et al. OP18 evaluating the impact of the English health inequalities strategy on socioeconomic inequalities in the regional infant mortality rate . J Epidemiol Community Health 2018 ; 72 : A9 .
Taylor-Robinson D , Lai E , Whitehead M , Barr B . Child health unravelling in UK . BMJ 2019 ; 364 : l963 doi: 10.1136/bmj.l963 (Published 5 March 2019).
Health Inequalities Dashboard . Public Health England . May 2019 . http://80.82.119.182/health_inequalities_dashboard/ .
Great Manchester . Early Years Delivery Model . https://www.eif.org.uk/resource/greater-manchester-early-years-new-delivery-model/ .
Northern Health Service Alliance . NHSA . http://www.thenhsa.co.uk/ .
Health and Wealth . NHSA http://www.thenhsa.co.uk/2018/11/major-new-report-connects-norths-poor-health-with-poor-productivity/ .
Manchester Economic Assessment (2) . Greater Manchester 2018 . https://issuu.com/greatermcr/docs/gmipr_reviewersreport_web_20190208?e=35861904/67626379 .
The NHS Long Term Plan . 2018 . https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan.pdf .
A definition of Population Health Management . https://searchhealthit.techtarget.com/definition/Population-health-management-PHM .
https://gregfellpublichealth.wordpress.com/2017/12/14/capabilities-for-population-health-management/ .
Right Care . https://www.england.nhs.uk/rightcare/ .
National Neighbourhood Renewal Strategy . UK Government . 2003 . https://www.communities-ni.gov.uk/articles/introduction-neighbourhood-renewal .
Health action zones . 1998 . https://api.parliament.uk/historic-hansard/commons/1998/mar/31/health-action-zones .
Local area agreements- background . https://en.wikipedia.org/wiki/Local_area_agreement .
PHE ( 2016 ) ‘ The journey to place based health ’ https://publichealthmatters.blog.gov.uk/2016/03/17/the-journey-to-place-based-health .
Reducing health inequalities: system, scale and sustainability . Public Health England . 2017 https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/641625/Reducing_health_inequalities_system_scale_and_sustainability.pdf .
CMO report 2018 . DHSC . https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/767549/Annual_report_of_the_Chief_Medical_Officer_2018_-_health_2040_-_better_health_within_reach.pdf .
Maddison M , Kaner E , Johnstone P , Hillier-Brown F , Moffat S , Russell S , Bar B , Holland P , Salway S , Whitehead M , Bambra C. Equal north: how can we reduce health inequalities in the north of England? A prioritization exercise with researchers, policymakers and practitioners . J Public Health , fdy170 , doi: 10.1093/pubmed/fdy170 .
Northern Universities Public Health Alliance (NUPHA) 2018 . https://www.nupha.ac.uk/ .
WHO Healthy Cities http://www.euro.who.int/en/health-topics/environment-and-health/urban-health/who-european-healthy-cities-network .
Investigating the impact of the English health inequalities strategy : Time trend analysis Barr B . BMJ 2017 ; 358 doi: 10.1136/bmj.j3310 (Published 26 July 2017).
- local government
- public health medicine
- health disparity
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1471-8391
- Print ISSN 0007-1420
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Health inequalities case studies
21 February 2023
- Twitter logo
- Facebook logo
- LinkedIn logo

To realise a step change in health and wellbeing, systems will need to adopt new approaches to health inequalities as well as wider inequalities in society.
Our library of case studies shares work being delivered by organisations who have adopted innovative ways of tackling health inequalities, providing models for others to follow.
- Identifying and optimising the care of respiratory patients in Oxfordshire
- Knowsley community respiratory support service
- Integration with purpose: supporting Oliver and Dylan to live well
- Pre-transfer clinical discussion and assessment (PTCDA)
- Supporting the refugee community in Kirklees
- Resetting human and financial resource in general practice
- Taking a system-wide collaborative approach to people and workforce
- Hidden Talents: refugee and asylum seeker community recruitment
- Addressing health inequalities in Surrey through a BAME health alliance
- Supporting the refugee community in Kirklees
- Hidden Talents: refugee and asylum seeker community recruitment
- Tackling long waiting lists and health inequalities in Coventry and Warwickshire
- Pre-transfer clinical discussion and assessment (PTCDA)
- Mental health support for young people and working-age adults
- Improving timely access to mental health support in a PCN
- Adapting Time to Talk
- Improving access and quality of treatment for people who identify as LGBTQI+
Related content
Save the date: welsh nhs confederation annual conference and exhibition 2024.
Register your interest for Wales' health and care event of the year.
6 November 2024 08:30 - 16:00 GMT

NHS ConfedExpo 2024
Join us at Manchester Central as we and NHS England unite health and care leaders and their teams at one of the biggest health and care conferences.
12 June 2024 08:30 - 13 June 2024 16:45 GMT
NICON24 is the premiere event for HSC Leaders and partners, bringing them together to discuss how to secure the best health and care outcomes for NI.
16 October 2024 08:00 - 17 October 2024 13:30 GMT

InFocus with Matthew Taylor, CEO of the NHS Confederation
Hear Matthew’s reflections on partnerships, as well as how the Confed aims to enhance its work with external organisations to support our NHS members.
25 June 2024 14:00 - 14:45 GMT

- RCPCH Learning
- Child Protection Portal
- Archives of Disease in Childhood
- BMJ Paediatrics Open
- RCPCH Committees
- Start by increasing personal awareness of the problem and being aware of unconscious personal bias.
- Prove and measure health inequality by audit so that there is a bench mark from which to improve, then re-audit.
- Raise awareness by publishing and sharing findings locally and nationally.
- Look at what initiatives other trusts have started and what research has already been done- including national audits.
- Listen to people from the disadvantaged groups, including voice of the child.
- Involve multidisciplinary team, as health inequality is a complex multifaceted problem
- If resources (time or infrastructure) are limited, start small, with something easy to measure or an easy win, to encourage the team and generate momentum.
- Work with a friend or colleague for accountability and encouragement.
Find out more about this project (please note amendment needed to socioeconomic data in this linked article).
To find out more, contact [email protected] .
RESPOND is a community-based integrated health service for asylum-seekers. Many asylum-seeking children and families arrive with complex profiles of health and well-being needs for which traditional NHS healthcare systems struggle to offer appropriate, joined-up and trauma-informed care. The RESPOND service aims to unite practitioners from across multiple agencies to support holistic health screening and care planning for recently arrived asylum-seeking children, adults and families.
Find out more about the RESPOND Project:
Refugee migration to the UK shows little sign of diminishing. Many asylum-seeking children and families arrive with complex profiles of health and well-being needs for which traditional NHS healthcare systems struggle to offer appropriate, joined-up and trauma-informed care. Significant barriers to accessing health services exist for asylum-seekers, including language difficulties, stigma, economic and digital poverty and repeated residential relocation. The RESPOND service was developed at UCLH to help overcome barriers to accessing health care for asylum-seekers, and to ensure they get the right care, at the right time, delivered by the right people.
The RESPOND service aims to unite practitioners from across multiple agencies (including but not limited to primary care, NHS and third sector mental health services, social care and safeguarding, general and community paediatric and infection specialists) to support holistic health screening and care planning for recently arrived asylum-seeking children, adults and families. Specialist nurse-led screening takes place in the community at or near temporary accommodation sites, using a trauma-informed approach and language interpretation. Each health assessment explores physical and mental health needs and includes infection screening as well enquiry about safeguarding, social and developmental needs. Signposting and referrals to relevant NHS services are made and close partnerships with local authority ‘Early Help’ teams, education services and the voluntary sector provide support with housing, schooling, and welfare.
An individualised, integrated health care plan is created, with input from a tertiary-level multidisciplinary refugee health MDT for the most complex cases. Each child and family receives a written health plan, outlining key health issues identified and specific actions needed to address these. This health plan travels with the family on relocation, avoiding a ‘back to square one’ situation with each short notice move between temporary accommodation sites.
They have screened more than 900 patients, more than a third of which are families with young children. Issues identified are wide-ranging and include undiagnosed or unmanaged conditions such as epilepsy, diabetes and genetic syndromes as well as significant safeguarding concerns related to domestic violence, human trafficking and separated children. They have seen patients with shrapnel wounds, evidence of torture, and provided a space for the first disclosures of sexual violence. Out of every 10 families seen, nine require onward referral for further assessment and support of mental health needs. Infections have been found and treated in a third of those screened, including latent TB, strongyloidiasis and schistosomiasis.
Collaboration. Effective strategy. Seek funding. Understand your target group. Be flexible and adapt!

Tool 1 - Improve your understanding of child poverty

Tool 2 - Develop skills for talking to families

Tool 3 - Prepare your own QI project

Tool 4 - Advocate for change

Tool 5 - Take national political action

Tool 6 - Influence local children's services
- Health inequalities
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Reducing healthcare inequalities using population health management

Over 10,000 people at high risk of health deterioration have been identified for extra help and support to stay well and independent thanks to the National Population Health Management Programme.
Running for over three years, the Population Health Management Development Programme has supported thousands of health and care professionals including commissioning and service improvement teams, to adopt a population health management approach to address health inequalities in their area.
Equipping participants with the leadership, knowledge and skills to use data and analysis to inform decision-making, the programme has helped 40 Integrated Care Systems across the country to design proactive models of care which meet the needs of their local population and address the wider determinants of health.
Using joined up information from across health and care partners to understand which factors are driving health inequalities within different population groups, population health management provides an opportunity for the NHS to work together with public services including councils, the public, schools, fire service, voluntary sector, housing associations, social services and police, to tackle the underlying causes of ill health.
Many examples of good practice have emerged from the programme including:
- Over 100 people at risk of heart failure living in deprivation in inner city Bristol being offered medication reviews People living in the more deprived areas of the Bristol, North Somerset and South Gloucestershire Integrated Care System are more likely to die earlier and on average have 10 fewer years of good health. By using new techniques such as segmentation and risk stratification the ICS found 100 people aged 40 to 69 living in high levels of deprivation in Bristol inner city, who also had a combination of obesity, high blood pressure, depression and anxiety. These patients were offered a medication review, a healthy hearts group consultation and an appointment with a social prescriber to help with exercise, mental health and lifestyle issues.
- South Asian communities in East Milton Keynes supported to better manage their diabetes Analysis pinpointed poorer diabetes management and higher risk of cardiovascular disease in South Asian communities in East Milton Keynes. Rates were also higher among those working in unskilled jobs and those without employment. The primary care network offered advice from the Wellbeing team, including information on diet, nutrition and exercise as well as culturally informed cooking sessions, free gym membership and use of community facilities including local allotments. People were encouraged to monitor their weight and diet by directly inputting to their medical records using a health app.
- Addressing wider determinants of health for those with multi-morbidities including depression in the North East and Cumbria People with depression, at high risk of becoming unwell due to a chronic physical health problem were contacted to explore if there were wider issues impacting their health. Thirty-four individuals were identified and given early support by a social prescribing link worker to help them address issues with finance, housing and social isolation. Help was also available to support people stop smoking and access physical activities and weight management services to improve their wellbeing including their cardio-vascular health.
You can read more about these, and other projects supported by the programme by signing up to the Population Health Management Academy on FutureNHS.
Anne Wray, an advanced nurse practitioner who co-led a population health management project for Bristol Inner City Primary Care Network, said: “Locally we have a number of health inequalities and this project really helped us get to the most vulnerable. People were very pleased to have someone reach out and try to help – it’s so motivating as a nurse to know that we can use data to actively try and help people before their health has already declined. To know we are adding many years of health to people’s lives really motivates a team.”
Speaking about the Programme, Bev Evans, Head of Population Health Management for NHS England , said: “Addressing health inequalities is everybody’s business. The COVID-19 pandemic highlighted the widening gaps in our communities but population health management is actively helping to prevent this from worsening.
“Using this approach, we can identify communities and individuals impacted by health inequalities including people struggling to access services, those living in areas of high deprivation or belonging to inclusion health groups and individuals at high-risk of developing life-threatening conditions.
“By supporting these individuals sooner and more effectively we can reduce the possibility of them becoming unwell and improve their health and well-being in the long run. Essentially, we want to help those most vulnerable people in our society to live longer and have more years in good health.
“Population health management is one of 10 priorities systems are being asked to focus on over the next year and we are committed to working with local councils and voluntary community and social enterprises through systems to develop our approach, prevent ill-health and address health inequalities.
“One of the ways we plan to do this is through the Place Development Programme which will follow on from the Population Health Management Development Programme which ends later this year. Funded and led by NHS England, in partnership with the Local Government Association, the Place Development Programme is available to all 42 Integrated Care Systems (ICS) in England and aims to accelerate and embed population health management within local operating models.
“Rooted in action learning, the programme will equip participating Places with practical tools, techniques and approaches that embed and deliver effective population health management. It has been designed to complement the ongoing NHS England Population Health Management Development Programme and presents an opportunity for creating real change on the ground through understanding and addressing the causes of ill health.”
Find out more about the Place Development Programme: Place Development Programme – Population Health Management Academy – Integrated Care (future.nhs.uk)
- Open access
- Published: 30 May 2024
Social-emotional and behavioural problems in young children of healthcare worker mothers during the COVID-19 outbreak: a case-control study
- Mahmut Caner Us ORCID: orcid.org/0000-0003-1120-3498 1 ,
- Perran Boran ORCID: orcid.org/0000-0002-9885-7656 2 ,
- Sıddika Songül Yalçın ORCID: orcid.org/0000-0001-9061-4281 3 ,
- Refia Gözdenur Savcı ORCID: orcid.org/0000-0001-6239-3442 4 ,
- Bahar Kural ORCID: orcid.org/0000-0001-9528-1009 5 &
- Dilşad Foto Özdemir ORCID: orcid.org/0000-0002-9077-8419 6
BMC Psychiatry volume 24 , Article number: 407 ( 2024 ) Cite this article
91 Accesses
Metrics details
The pandemic has had a significant impact on the daily lives of children and their families, particularly the children of health care workers, due to changes in family routines as a result of their parents’ work schedules. We aimed to explore the socioemotional and behavioural (SEB) problems of children of healthcare worker mothers (HCWM) during the COVID-19 pandemic and compare them with age-matched children and their mothers from other occupations.
A case-control study design was applied, and a snowball approach was used to enrol volunteered participants aged between 6 and 36 months of age, through a Google survey. We used the Brief Infant-Toddler Social and Emotional Assessment (BITSEA) questionnaire to assess children’s SEB problems and a Brief Symptom Inventory (BSI) to evaluate the psychological distress of mothers. Differences in BITSEA, BSI and MSPSS scores were examined using chi-square and Mann-Whitney U tests, as appropriate. A logistic regression model was used to identify independent predictors of children’s behavioural and emotional problems.
In total, 600 questionnaires were analysed. It was observed that children in the HCWM group were separated from their mothers more often and for longer periods of time than their counterparts ( p < 0.010, p = 0.002). Changes in the child’s structured outdoor activities during the pandemic period were more likely to be observed in the HCWM group ( p < 0.05). The percentage of children with the BITSEA problem subscale above the subclinical cut-off, externalizing and dysregulation scores were significantly higher in the HCWM group ( p = 0.044, p = 0.031, and p = 0.016). Moreover, each point increase in BSI global index scores ( p < 0.001, RR:3.34, 95%CI:1.91–5.82) was found as a risk factor for clinically significant SEB problems.
Overall, the current study suggests HCWM’s have experienced occupational inequality, and young children of HCWM’s were at increased risk for externalizing and dysregulation problems during the pandemic. Maternal psychological stress had a significant impact on their children’s socio-emotional well-being.
Peer Review reports
Introduction
The COVID-19 epidemic began in China, spread quickly to other countries, and has been declared a public health emergency of international concern on January 30th 2020 by the World Health Organization (WHO) [ 1 ]. Figures from around the world show that approximately 7 to 11% of healthcare workers (HCWs) have been diagnosed with COVID-19 [ 2 ]. Political measures adopted to control the disease such as closure of childcare services, and disrupted socialization exacerbated existing inequities and posed additional challenges for HCW mothers (HCWM) with young children [ 3 ]. They had to balance work responsibilities such as providing patient care against their responsibilities to protect their own well-being from the effects of chronic stress and their children’s mental health [ 4 ]. HCWMs with young children raised their concerns about access to childcare, parenting, and household duties [ 5 ]. Inability to find caregivers and elderly parents for childcare support was a significant contributor to this inequity. While there is limited research on this specific topic, these challenges may have contributed to increased child behaviour problems particularly at a young age. In addition, as noted in the United Nations report on Turkey’s gender equality performance from 2000 to 2019, Türkiye still maintains a strong traditional division of labour. Although it is improving day by day, women still spend four times more time than men on unpaid domestic work (the double burden of housework and childcare), which is not sufficiently shared by family members, especially men, increasing women’s workload [ 6 ].
Children of HCWMs were disadvantaged relative to their peers due to deprivation of maternal care for an extended duration, the risk of their parents contracting the virus, the fear of losing their parents, and changes in family routines due to their parents’ work schedules [ 7 ]. Trauma faced at a young age may have long-term adverse developmental consequences across their lifespan [ 8 ].
Studies have shown that HCWs have experienced higher levels of stress, anxiety, and depression compared to the general population during the pandemic [ 9 , 10 , 11 ]. Notably, parental distress can be a significant contributor to child behavioural problems. Distressed parents tend to demonstrate emotional unavailability thus leading to the occurrence of child behaviour problems [ 9 , 12 ]. On the other hand, parental distress has been shown to be associated with lack of social support. It has been shown that social support provided by family and friends can help reduce parental distress and have a positive effect on parenting behaviours. Due to social distancing measures these protective close relationships of families were cut off [ 10 ]. Social support plays an important role in a person’s mental health, and even more in disasters acts as a buffer against the negative effects of trauma-related events, minimizing the potential of developing negative consequences [ 11 , 13 ]. Therefore, measuring the social support of HCWs would be of critical importance in planning interventions for this vulnerable population [ 7 ].
Overall, the pandemic has had a significant impact on the daily lives of children such as changes in daily routines, increased stress and anxiety, reduced physical activity, reduced peer interactions, increased screen time and changes in sleep environment which can contribute to sleep disturbances in young children [ 12 , 14 ]. On the other hand, other studies have found that improved parent-child interactions due to home confinement could allow for better sleep [ 12 , 14 , 15 , 16 ].
The study was planned based on the hypothesis that children of HCWMs experienced more socioemotional and behavioural (SEB) problems than children of mothers from other occupations during the COVID-19 pandemic. We aimed to explore SEB problems and sleep patterns in children of HCWMs; assess the psychological distress of mothers and their perceived social support during the COVID-19 pandemic, and compare them with age-matched peers and their mothers from other occupations.
Materials and methods
A case-control study was applied and a snowball approach was used to enrol volunteered participants. All women having children aged between 6 and 36 months of age were invited to participate via websites, social media and e-mail between August 18th 2020 - October 17th 2020. All surveys were conducted in Türkiye. Personal identifying information was not collected or recorded.
An online survey was developed on the Google platform securing data collection by a confidential login system which can be filled out through smartphones, tablets or computers. The questionnaire took approximately 15 min to complete. It was pilot tested on 15 mothers and found acceptable. Due to pandemic restrictions, the study has been promoted via social media (such as Whatsapp, Telegram doctor and parent groups, Instagram, websites) and they are being asked to send links to volunteers in their area. Volunteers were sent an invitation email or message with a link to an anonymous online questionnaire, depending on their contact preferences. To access the questionnaire, respondents were asked to read the informed consent form and tick the mandatory box. Questionnaire responses were converted to excel spreadsheets.
Children aged 6–36 months and working mothers aged 20–45 years with at least some college/university education were eligible to participate in the study. Children whose parents didn’t approve the consent form or who had a known chronic health problem were excluded from the study. Children of HCWMs were grouped as Group 1 (HCWM group), and children of mothers from other occupations were grouped as Group 2 (non-HCWM group). Doctors, nurses, and paramedics are considered as HCWMs. For two groups, the difference between the groups was predicted to be statistically significant at the medium effect size (according to the percentage of SEB and sleep problems in that age group), and the total sample size was calculated as 600 for 95% power and 0.05 alpha significance level, taking into account dropouts and other possible problems (Fig. 1 ).
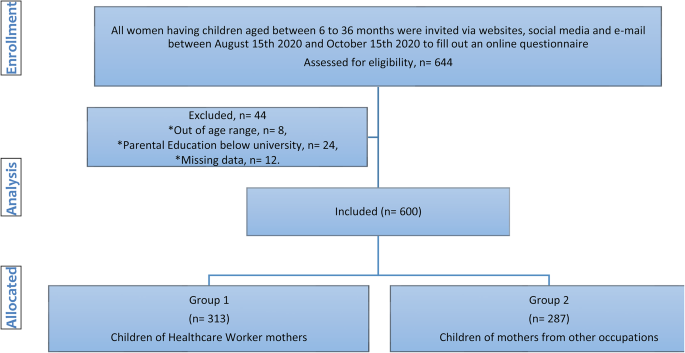
Flow chart of the study
Brief Infant Sleep Questionnaire (BISQ) [ 17 , 18 , 19 , 20 ] and Brief Infant-Toddler Social and Emotional Assessment (BITSEA) questionnaires [ 21 , 22 , 23 ] were used to assess children’s sleep, and social-emotional development, respectively. Multidimensional Scale of Perceived Social Support (MSPSS) [ 24 , 25 ], and Brief Symptom Inventory (BSI) [ 26 , 27 ] questionnaires were used to evaluate maternal social support and psychological distress.
Questionnaires
The BISQ functions as a tool designed to assess the early childhood sleep environment, covering aspects such as parental practices, daytime and night-time routines, and sleep issues, relying on responses from parents [ 17 ]. Through validation, BISQ demonstrated significant correlations with sleep measures obtained from actigraphy and sleep diaries. The Turkish translation of BISQ has been deemed acceptable, comprehensible, and reliable for evaluating sleep-related factors in infants [ 18 ]. In this study, maternal perception of sleep problems was categorized based on the expanded BISQ version. A parent-reported sleep problem was defined as moderate or severe while no problem was designated for those with no problem or a very small problem, as indicated in previous studies [ 17 , 19 ]. Parents were asked a single question to assess the pandemic’s impact on their children’s sleep. The question of whether there was a change in their children’s sleep during the pandemic period and if the answer is “yes”, what has changed was added to the beginning of the BISQ survey. If the child woke up > 3 times/night and woke up after sleep onset (WASO) for > 1 h or spent < 1 SD of the study population’s sleep duration (10 h), the child was considered a poor sleeper [ 17 , 20 ].
The BITSEA is a tool for screening social, emotional and behavioural development in early childhood which consists of 42 items [ 21 ]. The BITSEA encompasses two scales: the Problem scale (BITSEAp) with 31 items and the Competence scale (BITSEAc) with 11 items. Each item utilizes a response format with three choices: “not true/rarely” (0), “sometimes true/sometimes” (1), and “very true/often (2).” Problematic behavior is addressed in the externalizing (6 items, e.g., impulsivity, defiance, peer aggression), internalizing (8 items, e.g., fearfulness, worry, anxiety, sadness), and dysregulation (8 items, e.g., sleep and eating problems, negative emotionality, sensory sensitivities) domains [ 22 ]. Higher total scores on BITSEAp indicate a greater level of behavioral and emotional problems, while lower total scores on BITSEAc indicate a lower level of competence. The Turkish version of BITSEA has demonstrated reliability, validity, and simplicity, making it an effective instrument for screening social, emotional, and behavioral problems in toddlers [ 23 ]. Identified cut-offs of BITSEAp in gender groups for subclinical scores were ≥ 18 for males, and ≥ 21 for females. It was ≥ 24 for clinical scores in both genders [ 21 , 23 ].
The MSPSS is a concise self-administered tool comprising 12 items, divided into three subscales [ 24 ]. Respondents rate each item on a seven-point Likert scale, ranging from 1 (very strongly disagree) to 7 (very strongly agree). A higher score on the Likert scale indicates a greater perception of social support. The total score, ranging from 12 to 84, can be calculated by adding the items within each subscale and then dividing by 4. The instrument assesses the level of social support and identifies its sources from family, friends, or significant others. Elevated scores are indicative of higher levels of perceived social support. The Turkish adaptation of MSPSS has demonstrated reliability, validity, and ease of application, establishing it as an effective tool for screening perceived social support [ 25 ].
The BSI comprises a self-report symptom inventory with 53 items, encompassing nine symptom dimensions: Somatization, Obsession-Compulsion, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism; along with three global distress indices: Global Severity Index, Positive Symptom Distress Index, and Positive Symptom Total [ 26 ]. This instrument facilitates the evaluation of psychological distress and psychiatric disorders. Respondents rate items on a five-point Likert scale, ranging from 0 (not at all) to 4 (extremely), indicating the degree of distress experienced in the past week. Scores are generated for nine primary symptom dimensions and three global distress indices. The Turkish adaptation of BSI has demonstrated reliability, validity, and simplicity, making it a valuable tool for assessing maternal psychological distress, including depression, anxiety, hostility, negative self-perception, somatization, and global distress indices [ 27 ].
Statistical analyses
IBM SPSS Statistics software (version 28.0, IBM Inc., United States) was employed for all analyses. Descriptive statistics, including mean and standard deviations (SD) for normally distributed continuous variables, and median and quartiles for non-normally distributed data, were presented. Normal distribution conformity was assessed using Kolmogorov-Smirnov and Shapiro-Wilk tests. Categorical variables were summarized using frequencies and percentages. Differences in family characteristics, sleep parameters, BITSEA, BSI, and MSPSS scores were examined using the chi-square and Mann-Whitney U test, as appropriate. Given the non-normal distribution of all parameters, Spearman’s Rho Correlation analysis test was utilized to calculate correlation coefficients and assess significance.
Adjusted odds ratios (ORs) and 95% confidence intervals (CIs) were reported. To compare study group data with nationally representative data, a one-sample T-test and chi-square test were applied for sleep parameters, and the chi-square test was used for SEB problem frequency. In multivariate analysis, factors identified in univariate analysis, without collinearity, were entered into logistic regression to determine independent predictors of children’s behavioral and emotional problems. The Hosmer–Lemeshow test assessed the goodness-of-fit of the model. A 5% type-I error level was set for determining statistical significance.
In total, 600 questionnaires were analysed, 313 children were included in the HCWM group and 287 were included in the non-HCWM group (Fig. 1 ). There were no statistically significant differences in maternal and paternal occupation between the groups. Although the mothers who had a college/university education and above were included in the study, there was a statistically significant difference between the groups according to the level of parental education. Although the median age of children was significantly higher in the HCWM group ( p = 0.005), age groups (< 24 months vs. 24–36 months) and gender distribution was similar in both groups ( p = 0.133, p = 0.416).The sociodemographic and parental data of groups are summarized in Table 1 .
Changes in the daily routines and family members’ COVID-19 exposure status were presented in Table 2 . A significantly higher proportion of mothers in the HCWM group were separated from their children during the pandemic (HCWM vs. non-HCWM: 27.8% vs. 10.8%). Moreover, the duration of separation was significantly longer (20 vs. 3 days, p = 0.002) in the HCWM group. Childcare support by nannies and grandparents and changes in the child’s structured outdoor activities during the pandemic period were more likely observed in the HCWM group ( p < 0.05).
Total and subscale scores of the BITSEA, BSI and MSPSS are presented in Fig. 2 ; Table 1 . Although there were no significant differences in children’s BITSEAp median scores between groups, the externalizing and dysregulation scores were significantly higher in the HCWM group ( p = 0.031, p = 0.016). There were no significant differences in the BITSEAp and BITSEAc scores between boys and girls (boys vs. girls median BITSEAp 15 vs. 14, p = 0.461; median BITSEAc 17 vs. 17, p = 0.093). The median BITSEAc and total score were significantly higher in the HCWM group ( p = 0.030, p = 0.031). Although children above BITSEAp subclinical cut-off were found significantly higher in the HCWM group (30.7% vs. 23.3%, p = 0.044), there was no significant difference between clinical cut-off points. There were no significant differences in mothers’ BSI and MSPSS total and subscale median scores between the groups (Fig. 3 ; Table 1 ).

BITSEA, BSI and MSPSS scores for each subscale [* p < 0.05 (Mann-Whitney u test); For each scale first column indicates Group 1 and second column indicates Group 2; BITSEA: brief infant–toddler social and emotional assessment, BITSEAp: The brief infant–toddler social and emotional assessment problem scale, BITSEAc: brief infant–toddler social and emotional assessment competence scale, BSI: Brief Symptom Inventory, MSPSS: Multidimensional Scale of Perceived Social Support]

Distribution of BITSEAp scores above the cut-off [* p < 0.05 at Chi-square test, BITSEAp: The brief infant–toddler social and emotional assessment problem scale, identified cut-offs of BITSEA/P in gender groups for subclinical scores were ≥ 18 for males and ≥ 21 for females. It was ≥ 24 for clinical scores in both genders]
While other BSI subscales and BITSEAp had a mild positive correlation, BSI global index and BITSEAp had a positive moderate correlation ( r = 0.412, p < 0.001). All BSI subscales (anxiety, depression, hostility, somatization, negative-self and global index) and BITSEAp subscales (externalizing, internalizing and dysregulation) had a mild positive correlation ( p < 0.001). Additionally, the MSPSS total and BSI global index had a negative moderate correlation ( r =-0.430, p < 0.001). It was shown that almost all MSPSS and BSI subscales had negative mild to moderate correlations. Bivariate correlation of BITSEA, BSI, MSPSS subscales, sleep parameters and associated sociodemographic variables are summarized in Supplemental File Table 1 .
Although there were no significant differences between study groups, it was shown that the percentage of SEB problems in HCWM’s children was significantly higher than national representative data (13.5% vs. 11.9%, with a chi-square test p < 0.001) [ 28 ].
In the logistic analysis, male gender ( p < 0.001, RR: 3.68, 95% CI: 1.99–6.80), each point increases in BSI global index scores ( p < 0.001, RR: 2.56, 95% CI: 1.61–4.09), and having HCWM ( p = 0.018, RR: 2.27, 95% CI: 1.15–4.48) were found as the risk factors for BITSEAp scores above the subclinical cut-off. Besides, each point increases in BSI global index scores ( p < 0.001, RR: 3.34, 95% CI: 1.91–5.82) was found as a risk factor for clinically significant SEB problems (Table 3 ).
Table 4 provides a summary of maternal perceptions regarding sleep problems and sleep variables based on BISQ. It reveals that both total and night-time sleep durations were significantly shorter in the HCWM group. Furthermore, the HCWM group demonstrated a significantly higher prevalence of perceiving their child’s sleep as a moderate to severe problem.
Changes in sleep patterns and sleep disturbances in children pre- versus post-pandemic were analysed. Changes in sleep pattern were 1.38 times and night wakening’s were 1.8 times higher as compared to the pre-pandemic period in the HCWM group (HCWM vs. non-HCWM group: 41.5% vs. 30% p = 0.004, OR: 1.38; 23.3% vs. 12.9% p = 0.001, OR: 1.80). HCWMs were more likely to perceive their children’s sleep as a moderate to severe problem compared to the non-HCWM group (25.9% vs. 17.1%, p = 0.01, OR: 1.51). Wake-up time was significantly earlier, and night-time and total sleep duration were significantly shorter in the HCWM group ( p = 0.004, p = 0.003, p = 0.003). Overall, 22.8% of the study population were classified as poor sleepers and there was no significant difference between the groups ( p = 0.097).
Compared with the recent study that represents Türkiye’s nationwide sleep characteristics of the same age group, whole study groups differed significantly from the normative distribution in almost all sleep parameters (Night waking’s increased by 2.63 vs. 2.3, p < 0.001; decreased night-time sleep duration 9.3 vs. 9.6 h, p < 0.001; shorter total sleep duration 11.2 vs. 11.5 h, p = 0.002; increased WASO 59.1 vs. 48.1 min, p = 0.01; decreasing nap number 1.4 vs. 1.6, p < 0.001) [ 29 ].
There is limited research available on whether children of HCWMs exhibit more SEB problems compared to their peers during the pandemic. Overall, the current study suggests HCWMs have experienced occupational inequality, and young children of HCWMs were at increased risk for externalizing and dysregulation problems during the pandemic. Our findings showed a significantly higher proportion of HCWMs were separated from their children for longer periods. Disrupted childcare support and changes in daily routines have disproportionally impacted HCWMs. Children of HCWMs had higher scores on the externalizing and dysregulation domains of SEB problems than children of non-HCWMs. On the other hand, psychological distress and perceived social support were not different in HCWMs compared to non-HCWMs. Moreover, competence scores were significantly higher in children of HCWMs, suggesting young children of HCWMs may have experienced positive outcomes as well. Maternal psychological distress was found as a potentially modifiable factor affecting the child’s SEB problems. Our findings also showed that these children of HCWMs had higher parent-reported sleep problems, shorter total and night-time sleep, and earlier wake time compared to their peers of non-HCW parents. Moreover, they had an increase in their night wakening and changes in sleep patterns compared to the pre-pandemic period.
Parent-reported SEB problems in infancy and throughout toddlerhood have been reported between 5 and 24% in different studies before the pandemic period [ 30 , 31 ]. Children of HCWs faced unique stressors, including the risk of their parents contracting the virus, changes in family routines due to their parents’ work schedules, and separation from their parents due to long working hours or quarantine measures. While there is limited research suggesting that children of HCWs may be at increased risk of experiencing SEB problems during the pandemic, the available evidence shows that these stressors can contribute to SEB problems in young children. It is known that externalizing problems are mainly encountered in early childhood because they have limited abilities to communicate about their emotions and use externalizing behaviours to express their emotions [ 32 ]. The findings of our study showed young children of HCWMs faced additional stressors such as separation from their parents and disruption of their daily routines due to their parent’s occupations. We also found that children of HCWMs had higher externalizing and dysregulation behaviours compared to their peers. Overall, clinically significant SEB problem was found in 13.5% of the children. The study from Türkiye has shown that parent-reported clinically significant SEB problem was observed in 11.9% of Turkish children aged between 2 and 3 years [ 28 ]. In the validation and reliability study of the BITSEA Turkish version, clinically significant SEB problem was found at 13.1% for males and 17.6% for females [ 23 ]. In this current study, although there were no significant differences between groups, it was shown that the percentage of SEB problems in HCWM’s children was significantly higher than the nationally representative data [ 28 ]. Further, the number of children above BITSEAp subclinical cut-off was found significantly higher in the HCWM group suggesting subclinical difficulties at younger ages may also increase the risk for later psychopathology [ 32 , 33 ].
Research findings have been mixed and some studies have suggested that children of HCWs may experience positive outcomes as well [ 34 ]. Similarly, the current study found that competence scores were significantly higher in children of HCWMs, suggesting young children of HCWMs may have experienced positive outcomes as well. It is important to note that the impact may vary depending on the type of healthcare work their parents are engaged in, the family’s overall social and economic circumstances, and the child’s level of resilience and coping strategies. The current study has not shown a significant difference in perceived social support between HCWMs and non-HCWMs. Social support can take many forms including emotional support, and practical support. It can be particularly important for parents who are experiencing additional challenges. Further research is needed to fully understand the issue.
SEB problems have been linked with high maternal depression and parenting stress [ 33 ]. Stress and anxiety levels of parents are associated with children’s SEB [ 35 ] and psychological development [ 36 ]. During stressful events, children’s emotional adjustment develops and changes mostly depending on the emotional state of their parents [ 37 ]. It has been suggested that mothers with depressive symptoms have difficulty responding appropriately in interactions with their children, show less sensitivity to cues from their children, participates less in positive interactions with their children, and cannot use the right strategies to manage their children’s behaviour [ 38 ]. Higher total BSI scores of the primary caregiver and being separated from the mother for more than a month were considered clinically significant risk factors for SEB problems in children [ 39 ]. Similarly, the study findings showed that higher maternal psychological distress levels were significantly associated with clinically significant SEB problems.
The COVID-19 pandemic has had a significant impact on the daily lives of young children which can contribute to sleep disturbances. In a recent study, it was shown that altered daily routines due to COVID-19 confinement, caused worsened sleep quality in children aged 0–36 months and the caregiver’s stress level was identified as a significant risk factor for this impairment [ 40 ]. Similarly, when the parents were asked about the reason for the altered sleep habits, they reported their children slept later than usual, sleep routines were disrupted, did not nap during the day, and had changes in feeding routines [ 41 ]. Our study showed that young children of HCWMs faced increased night wakening, earlier wake-up times and shorter night-time and total sleep times than peers. Compared with the recent study that represents Türkiye’s nationwide sleep characteristics of the same age group, almost all the sleep parameters were significantly worse than the normative distribution [ 29 ]. Additionally, HCWMs reported that their children’s sleep patterns changed compared to the pre-pandemic period. Sleep problems were found to be associated with SEB problems in the first 3 years of life [ 42 ]. Changes in daily routines, and sleep patterns might have contributed to SEB problems in young children who are particularly at a critical stage of social and emotional development. Parents need to establish consistent routines and support healthy sleep habits for young children to address these challenges.
It is important to note that this study only included young children living in Türkiye, and may not be representative of all children of HCWMs. The case-control design of our study did not let us provide information about the causality of SEB and sleep problems. Due to the snowball sampling approach, the generalizability of these findings is limited. To avoid this limitation, we calculated and reached the minimum sampling size to represent our population. The measures used for this study were self-reported. Reliable and valid questionnaires for our country had been used to overcome this limitation. Because the number of children above the clinical cut-off is limited, the significant difference shown in the subclinical cut-off may have not been demonstrated at the clinical cut-off. More research is needed to fully understand the impact of the pandemic on the SEB problems and the well-being of children of HCWMs. The differences between the groups in terms of parental education and family type were notable, although having at least a university/college education was an inclusion criterion. Our aim was to assess mothers’ perceptions but the lack of data on fathers is also a limitation of this study.
The findings of this study suggest that young children of HCWMs were disproportionally affected due to their mothers’ occupations during the COVID-19 pandemic. Addressing psychological distress in HCWMs, improving social support and implementing structured daily routines may serve as potential protective factors for behavioural functioning in these children and thus reduce occupation-related inequalities during the crisis. There is a need for further research into occupational inequality and its potential impact on social and emotional factors particularly for children and parents.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
WHO. COVID-19 weekly epidemiological update, edition 101, 20 July 2022. 2022. World Health Organization. https://iris.who.int/handle/10665/360561 .
Gomez-Ochoa SA, Franco OH, Rojas LZ, Raguindin PF, Roa-Diaz ZM, Wyssmann BM, et al. COVID-19 in Health-Care workers: a living systematic review and Meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2021;190(1):161–75.
Article PubMed Google Scholar
Matulevicius SA, Kho KA, Reisch J, Yin H. Academic Medicine Faculty perceptions of work-life balance before and since the COVID-19 pandemic. JAMA Netw Open. 2021;4(6):e2113539.
Article PubMed PubMed Central Google Scholar
Diver S, Buccheri N, Ohri C. The value of healthcare worker support strategies to enhance wellbeing and optimise patient care. Future Healthc J. 2021;8(1):e60–6.
Halley MC, Mathews KS, Diamond LC, Linos E, Sarkar U, Mangurian C, et al. The intersection of Work and Home challenges Faced by Physician Mothers during the Coronavirus Disease 2019 pandemic: a mixed-methods analysis. J Womens Health (Larchmt). 2021;30(4):514–24.
Kızılırmak B, Memiş E, Toksöz G. Turkey’s gender equality performance from 2000 to 2019: A rights-based analysis via undp human development and gender development indices. CEİD Association for Gender Equality & UNDP Turkey. 2022:1–92. https://dspace.ceid.org.tr/xmlui/handle/1/2035 .
Skokauskas N, Leventhal B, Cardeli EL, Belfer M, Kaasboll J, Cohen J. Supporting children of healthcare workers during the COVID-19 pandemic. Eur Child Adolesc Psychiatry. 2022;31(1):203–4.
Walker SP, Wachs TD, Grantham-McGregor S, Black MM, Nelson CA, Huffman SL, et al. Inequality in early childhood: risk and protective factors for early child development. Lancet. 2011;378(9799):1325–38.
Moran G, Forbes L, Evans E, Tarabulsy GM, Madigan S. Both maternal sensitivity and atypical maternal behavior independently predict attachment security and disorganization in adolescent mother-infant relationships. Infant Behav Dev. 2008;31(2):321–5.
Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. 2020;75(5):631–43.
Zhang J, Deng X, Liu H, Xu X, Fang R. Evaluation of the mental health status of community healthcare workers during the COVID-19 outbreak. Med (Baltim). 2021;100(6):e24739.
Article CAS Google Scholar
Çiçek S, Yalçin SS. Emotional status and problem behavior of pre-school children according to the pandemic period and occupational status of the mother. Int J Environ Health Res. 2023;33(12):1406–1417. https://doi.org/10.1080/09603123.2022.2096208 .
Altinel Açoğlu E, Aydin B, Isiyel E, Çelik M, Yalçın SS. Mother’s psychopathological conditions and parenting characteristics according to smoke exposure. Int J Environ Health Res. 2024;34(3):1701–1712. https://doi.org/10.1080/09603123.2023.2234844 .
Yildiz D, Yalcin SS. Change in screen time of preschool children according to parental attitudes during the COVID-19 pandemic with an online survey. Int J Environ Health Res. 2024;34(2):864–873. https://doi.org/10.1080/09603123.2023.2179027 .
Boran P. Bebeklik dönemi uyku sorunları ve çözümleri. Yalçın SS, editör. İlk İki Yaşta Sık Karşılaşılan Sorunlar. 1. Baskı. Ankara: Türkiye Klinikleri Pediatrik Bilimler-Özel Konular. 2018;14(4):403–10.
Google Scholar
Boran P. Çocuklarda normal uyku fizyolojisi ve farklı gelişim dönemlerinde uyku sorunları. İlk Beş Yaşta Çocuk Sağlığı İzlemi. 2017:331 – 43.
Sadeh A. A brief screening questionnaire for infant sleep problems: validation and findings for an internet sample. Pediatrics. 2004;113(6):e570–7.
Boran P, Ay P, Akbarzade A, Küçük S, Ersu R. Translation into Turkish of the expanded version of the Brief Infant Sleep Questionnaire and its application to infants. Marmara Medical Journal 2014;27:178–183.
Teng A, Bartle A, Sadeh A, Mindell J. Infant and toddler sleep in Australia and New Zealand. J Paediatr Child Health. 2012;48(3):268–73.
Henderson JM, France KG, Blampied NM. The consolidation of infants’ nocturnal sleep across the first year of life. Sleep Med Rev Aug. 2011;15(4):211–20.
Article Google Scholar
Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The brief infant-toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol. 2004;29(2):143–55.
Alakortes J, Fyrsten J, Carter AS, Moilanen IK, Ebeling HE. Finnish mothers’ and fathers’ reports of their boys and girls by using the brief infant-toddler Social and Emotional Assessment (BITSEA). Infant Behav Dev. 2015;39:136–47.
Karabekiroglu K, Rodopman-Arman A, Ay P, Ozkesen M, Akbas S, Tasdemir GN, et al. The reliability and validity of the Turkish version of the brief infant-toddler social emotional assessment (BITSEA). Infant Behav Dev. 2009;32(3):291–7.
Zimet GD, Dahlem NW, Zimet SG, Farley GK. The multidimensional scale of perceived social support. J Pers Assess. 1988;52(1):30–41.
Eker D, Arkar H, Yaldız H. Çok Boyutlu Algılanan Sosyal Destek Ölçeği’nin gözden geçirilmiş formunun faktör yapısı, geçerlik ve güvenirliği. Türk Psikiyatri Dergisi. 2001;12(1):17–25.
Derogatis L. Brief Symptom Inventory (Baltimore, Clinical Psychometric Research). Psychopathology. 1975;27(1–2):14–8.
Sahin NH, Durak A. Kisa Semptom Envanteri (brief Symptom Invetory-BSI): Turk Gencleri Icin Uyarlanmasi. Türk Psikoloji Dergisi; 1994.
Erol N, Simsek Z, Oner O, Munir K. Behavioral and emotional problems among Turkish children at ages 2 to 3 years. J Am Acad Child Adolesc Psychiatry. 2005;44(1):80–7.
Boran P, Ergin A, Us MC, Dinleyici M, Velipasaoglu S, Yalcin SS, et al. Young children’s sleep patterns and problems in paediatric primary healthcare settings: a multicentre cross-sectional study from a nationally representative sample. J Sleep Res. 2022;31(6):e13684.
Baillargeon RH, Sward GD, Keenan K, Cao G. Opposition-defiance in the Second Year of Life: a Population-based Cohort Study. Infancy. 2011;16(4):418–34.
Moricke E, Lappenschaar GA, Swinkels SH, Rommelse NN, Buitelaar JK. Latent class analysis reveals five homogeneous behavioural and developmental profiles in a large Dutch population sample of infants aged 14–15 months. Eur Child Adolesc Psychiatry. 2013;22(2):103–15.
Gardner F, Shaw DS. Behavioral problems of infancy and preschool children (0–5). In Rutter M, Bishop D, Pine D, Scott S, Stevenson J, Taylor E, Thapar A (Eds.), Rutter’s child and adolescent psychiatry. 5th ed. Wiley Blackwell. 2008;882–893. https://doi.org/10.1002/9781444300895.ch53 .
Briggs-Gowan MJ, Carter AS, Bosson-Heenan J, Guyer AE, Horwitz SM. Are infant-toddler social-emotional and behavioral problems transient? J Am Acad Child Adolesc Psychiatry. 2006;45(7):849–58.
Karaaslan BT, Akoğlu G, Özyurt G, Oral E. Changes in emotion regulation skills of school age children from the eyes of healthcare workers during the COVID-19 pandemic in Turkey: a cross-sectional study. Health Sci Rep. 2023;6(1):e964.
Madigan S, Oatley H, Racine N, Fearon RMP, Schumacher L, Akbari E, et al. A Meta-analysis of maternal prenatal depression and anxiety on child Socioemotional Development. J Am Acad Child Adolesc Psychiatry. 2018;57(9):645–57. e8.
Verkuijl NE, Richter L, Norris SA, Stein A, Avan B, Ramchandani PG. Postnatal depressive symptoms and child psychological development at 10 years: a prospective study of longitudinal data from the South African birth to twenty cohort. Lancet Psychiatry. 2014;1(6):454–60.
Shorer M, Leibovich L. Young children’s emotional stress reactions during the COVID-19 outbreak and their associations with parental emotion regulation and parental playfulness. Early Child Dev Care. 2022;192(6):861–71.
Chung FF, Wan GH, Kuo SC, Lin KC, Liu HE. Mother-infant interaction quality and sense of parenting competence at six months postpartum for first-time mothers in Taiwan: a multiple time series design. BMC Pregnancy Childbirth. 2018;18(1):365.
Karabekiroglu K, Uslu R, Kapci-Seyitoglu EG, Ozbaran B, Oztop DB, Ozel-Ozcan O, et al. A nationwide study of social-emotional problems in young children in Turkey. Infant Behav Dev. 2013;36(1):162–70.
Markovic A, Muhlematter C, Beaugrand M, Camos V, Kurth S. Severe effects of the COVID-19 confinement on young children’s sleep: a longitudinal study identifying risk and protective factors. J Sleep Res. 2021;30(5):e13314.
Wearick-Silva LE, Richter SA, Viola TW, Nunes ML, Group C-SR. Sleep quality among parents and their children during COVID-19 pandemic. J Pediatr (Rio J). 2022;98(3):248–55.
Makela TE, Kylliainen A, Saarenpaa-Heikkila O, Paavonen EJ, Paunio T, Leppanen JM et al. Signaled night awakening and its association with social information processing and socio-emotional development across the first two years. Sleep. 2021;44(12).
Download references
Acknowledgements
We would like to thank the children and their families who participated in this study.
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and affiliations.
Institute of Health Sciences, Social Pediatrics PhD Program, Marmara University, Istanbul, Turkey
Mahmut Caner Us
School of Medicine, Department of Social Paediatrics, Marmara University, Istanbul, Turkey
Perran Boran
Faculty of Medicine, Department of Pediatrics, Hacettepe University, Samanpazari, Ankara, 06100, Turkey
Sıddika Songül Yalçın
Department of Pediatrics, Alaçam State Hospital, Samsun, Turkey
Refia Gözdenur Savcı
School of Medicine, Department of Pediatrics, Istanbul Haliç University, Istanbul, Turkey
Bahar Kural
School of Medicine, Department of Child Psychiatry, Hacettepe University, Ankara, Turkey
Dilşad Foto Özdemir
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Mahmut Caner Us, Perran Boran, Sıddika Songül Yalçın. Mahmut Caner Us, Perran Boran, Sıddika Songül Yalçın, Refia Gözdenur Savcı, Bahar Kural collected data. The first draft of the manuscript was written by Mahmut Caner Us, Perran Boran, Songül Yalçın, Bahar Kural, Dilşad Foto Özdemir and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sıddika Songül Yalçın .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Conflict of interest disclosure
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Marmara University Faculty of Medicine Clinical Research Ethics Committee; date of approval: 17/08/2020 and protocol number: 09.2020.942.
Consent to participate
The study participants were only mothers who have a child aged 6 to 36 months. Informed consent via online checking was obtained from all the participating mothers. Subsequently, these mothers can access the Google Survey Form.
Consent to publish
Not applicable.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was presented as oral presentation at the Social Pediatric Society of Turkey’s in the selected abstracts of the 2nd International Eurasian Social Pediatric congress organized in Istanbul (Turkey) between October 26th-29th 2022. “SS-66”.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
: Bivariate correlation of variables
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Us, M.C., Boran, P., Yalçın, S.S. et al. Social-emotional and behavioural problems in young children of healthcare worker mothers during the COVID-19 outbreak: a case-control study. BMC Psychiatry 24 , 407 (2024). https://doi.org/10.1186/s12888-024-05801-4
Download citation
Received : 18 November 2023
Accepted : 29 April 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12888-024-05801-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Healthcare workers
- Socio-emotional development
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Maternal inequality: scoping the threats and reflecting on our opportunities to affect positive change
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-3262-9607 Elizabeth Bailey 1 ,
- http://orcid.org/0000-0002-3493-8967 Lizzie Ette 2 , 3
- 1 Elizabeth Bryan Multiple Birth Centre, College of Nursing and Midwifery , Birmingham City University , Birmingham , UK
- 2 School of Nursing and Midwifery, Faculty of Health Sciences , University of Hull , Hull , UK
- 3 Research Student , Edinburgh Napier University , Edinburgh , UK
- Correspondence to Dr Elizabeth Bailey, EBMBC/CSCHaRR, Birmingham City University, Birmingham, UK; elizabeth.bailey{at}bcu.ac.uk
https://doi.org/10.1136/ebnurs-2024-104098
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
- Maternal-Child Nursing
- Public Health
- Nurse Midwives
This editorial seeks to shine a spotlight on maternal inequalities, which will feature in our blog posts from the end of May for a few weeks. Undoubtedly, this is a broad and complex topic and, so our spotlight will take a view on how we might work towards positive change. Partly inspired by the plan–do–study–act cycle approach, 1 which is often used to provide a structure for working towards improved quality of systems, we will consider four aspects of how we are (1) identifying and quantifying the problem maternal inequalities and how (2) discovery of data has supported our understanding of the intersectionality of inequality; this discovery then offers (3) the opportunity to seek effective solutions while reflecting on personal action and how we might all (4) advocate for/drive the necessary change ( figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Maternal inequality change cycle, scoping the threats and reflecting on opportunities to affect positive change.
Identifying and quantifying the problems of maternal inequality
In recent years, there has been a growing focus on the inequalities that are driving global disparities in perinatal outcomes within a range of populations and across multiple settings. Where reductions in maternal mortality over time are observed, they are associated with access to good quality reproductive health and maternity care, whereas conditions that create barriers to sexual and reproductive health services are where inequalities flourish.
Discovery of data and understanding of the intersectionality of inequality
To draw attention to the consequences of inequality, greater awareness of perinatal outcomes is required and in recent years improved data surveillance has led to observations of the size and nature of inequalities in differing settings. A report from the USA in 2023, which looked into circumstances contributing to pregnancy-related death, determined that discrimination contributed to 30% of deaths, 3 and reports from UK maternal mortality surveillance have highlighted disparities by maternal ethnicity for over 10 years 4 with the most recent noting that Asian women were two times as likely to die, and black women were four times as likely to die when compared with deaths in white women in the perinatal period. These sobering statistics have served as a call to action and illustrate that high-income countries are not immune to the issue of maternal inequality. In recent years, charities and activist groups have been advocating for improvements to maternity care for black women and other minority groups have been raising awareness through representation of experiences. Black women were over-represented in those admitted to hospital with confirmed SARS-CoV-2 in pregnancy in the UK, 5 6 and the global surveillance that came with the SARS-CoV-2 pandemic further highlighted inequalities, again shining a spotlight and raising questions about why some groups were suffering the worst outcomes unequally. The pandemic raised awareness of many aspects of societal inequality and the murder of George Floyd in the USA in May 2020 initiated a global antiracist movement, which saw protests in the USA and many countries across Europe bringing with it a new discourse about structural and individual level bias and discrimination. 7 In August 2020, the American College of Obstetrics and Gynecology led a joint statement for collective action addressing racism with many US-based reproductive health organisations and in September 2020, the International Confederation of Midwives also released an antiracism statement. 8 There seemed to be a positive shift towards top–down drivers for change.
However, racial inequality is not the only disparity that requires our attention. Other broader determinants of health 9 remain as powerful as ever in influencing all health outcomes, including maternal and foetal health outcomes. Household wealth, for example, affects access to maternal health services. 10 Cultural, language, geography, disability and underlying prepregnancy chronic health conditions (which are more prevalent in some groups of women) all impact on maternal health outcomes and women who experience any combination of these factors are even further disadvantaged. Intersectionality (combined or multiple disadvantages, primarily in relation to protected characteristics) 11 can create or compound inequality. Furthermore, a complex relationship exists between intergenerational socioeconomic advantage and health literacy. 12
Disappointingly, despite long-standing efforts to highlight the multiple well-established contributors to inequality, the evidence suggests that it continues to grow. 13
Seeking effective solutions while reflecting on personal action
As nurses, midwives and health professionals, what can we do to reduce these inequalities and what might be effective? A recent systematic review of interventions to reduce inequalities in maternal and child health in low-income and middle-income settings found that studies were limited, but where there was evidence for impact was with outreach and community level improvements in healthcare together with increased human resource. 14 The opportunity to receive perinatal care from a known caregiver via a model that promotes continuity of carer has also been suggested as a way to build trust, break down barriers and support those otherwise affected by inequalities. 15
Organisations are encouraged to take an intersectional approach to maternity care practice and provision and to identify and understand structural inequality and thereby minimise its effect. 11
Advocate for and drive the necessary change
The Surgeon General’s Call to Action to Improve Maternal Health 16 offers detailed suggestions as to how women, their families, their communities and the organisations serving them can contribute at microlevel, mesolevel and macrolevel to shift practice towards greater accessibility, increased inclusivity and reduced inequality. Specifically, the Call to Action suggests healthcare professionals should support women to access maternity care and address racial and other disparities by offering services that are culturally and linguistically appropriate, underpinned by self and situational awareness.
Throughout our upcoming blog spotlight, we will hear from those working in practice to address inequality and in considering the maternity workforce, as well as hearing from those driving the discovery of new data and insights. Through further understanding, each of us can reflect on our own position and potential to reduce inequity, through identifying the gaps, building knowledge, working towards effective solutions and driving the change.
Ethics approval
Not applicable.
- Taylor MJ ,
- McNicholas C ,
- Nicolay C , et al
- ↵ United Nations population Fund, state of world population . 2024 . Available : https://www.unfpa.org/sites/default/files/pub-pdf/swp2024-english-240327-web.pdf [Accessed 3 May 2024 ].
- Busacker A ,
- Wright M , et al
- Patel R , et al
- Alcindor ML ,
- Alcindor F ,
- Alcindor MA
- Vousden N , et al
- Kocyba P , et al
- ↵ International Confederation of midwives anti-racism statement released . Available : https://internationalmidwives.org/resources/anti-racism-statement/ [Accessed 3 May 2024 ].
- ↵ Patient safety learning Hub [Internet] the Dahlgren-Whitehead Rainbow . 1991 . Available : https://www.pslhub.org/learn/improving-patient-safety/health-inequalities/the-dahlgren-whitehead-rainbow-1991-r5870/ [Accessed 3 May 2024 ].
- Methun MIH ,
- Ahinkorah BO ,
- Roy S , et al
- ↵ Scottish government, using Intersectionality to understand structural inequality in Scotland: evidence synthesis . 2022 . Available : https://www.gov.scot/publications/using-intersectionality-understand-structural-inequality-scotland-evidence-synthesis/pages/3/ [Accessed 3 May 2024 ].
- Castedo A ,
- Alexander M , et al
- Målqvist M ,
- Trygg N , et al
- Rayment-Jones H ,
- Dalrymple K ,
- Harris J , et al
- Office of the Surgeon General (OSG)
X @Liz8ailey, @busygirlizzie
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Provenance and peer review Not commissioned; internally peer reviewed.
Read the full text or download the PDF:

New study raises concerns as health threat targeting older people expected to double in coming decades: 'This is a question of intergenerational inequality'
T he number of older people worldwide exposed to dangerous heat conditions is projected to double by 2050, according to a new study .
Dangerous heat conditions are those with a heat index — which is a measure of what it feels like when relative humidity is factored into air temperature — between 103 and 124 degrees Fahrenheit.
What's happening?
Earth's population is aging rapidly. By 2050, scientists predict that one of every five people will be over 60 years old and subject to extreme heat conditions. By then, 25% of Europe's population, for example, is projected to be 70 or older, as The Guardian reported . Heat-related deaths across Europe have also increased by 30% over the last 20 years, per Earth.org.
"Two-thirds of [older adults] will live in low- and middle-income countries where extreme climate events are especially likely," the paper's authors predicted .
Why is this trend concerning?
As we age, our body's ability to regulate temperature diminishes. Older people are also more likely to have chronic illnesses, including heart and lung problems, that worsen in dangerous heat conditions.
Hotspots with high concentrations of older adults and extreme heat , such as Europe and Asia, will become more common, increasing vulnerability.
Watch now: Lime executive reveals true impact sustainable choices have had on business
The intensity and duration of last year's heat waves across Europe concerned public health officials, who recommended that health care organizations be more prepared for heat-related illnesses in the future.
Younger generations in many countries will have to bear a heavy social burden because of declining fertility rates and a shrinking working-age population.
The Guardian noted "the impact on health systems and global inequality will be huge" and that "a large part of the social burden will fall on taxpayers."
"This is a question of intergenerational inequality," said Giacomo Falchetta, one of the study's authors.
What's being done about it?
A U.K. startup has developed innovative clothing that allows the people wearing it to be significantly cooler when temperatures rise.
Texas and California found success running their electrical grids on battery power during summer 2023, when Texas had its second-hottest summer on record.
At an individual level, you can go in several directions to make an impact. Ensure your home is weatherized correctly to keep your air conditioning running efficiently and avoid breakdowns.
If you want to run your AC less, consider investing in solar shades , which offer an eco-friendly way to keep your home cool.
Join our free newsletter for cool news and actionable info that makes it easy to help yourself while helping the planet.
New study raises concerns as health threat targeting older people expected to double in coming decades: 'This is a question of intergenerational inequality' first appeared on The Cool Down .

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.12(9); 2022

Original research
Systematic review of the effectiveness of the health inequalities strategy in england between 1999 and 2010, ian holdroyd.
1 Department of Public Health and Primary Care, University of Cambridge, Cambridge, UK
Alice Vodden
2 University College London Hospitals NHS Foundation Trust, London, UK
Akash Srinivasan
3 Imperial College London Faculty of Medicine, South Kensington Campus, London, UK
4 Medical Library, School of Clinical Medicine, University of Cambridge, Cambridge, UK
Clare Bambra
5 Newcastle University Population Health Sciences Institute, Newcastle upon Tyne, UK
John Alexander Ford
Associated data.
bmjopen-2022-063137supp001.pdf
Data sharing not applicable as no datasets generated and/or analysed for this study.
The purpose of this systematic review is to explore the effectiveness of the National Health Inequality Strategy, which was conducted in England between 1999 and 2010.
Three databases (Ovid Medline, Embase and PsycINFO) and grey literature were searched for articles published that reported on changes in inequalities in health outcomes in England over the implementation period. Articles published between January 1999 and November 2021 were included. Title and abstracts were screened according to an eligibility criteria. Data were extracted from eligible studies, and risk of bias was assessed using the Risk of Bias in Non-randomized Studies of Interventions tool.
The search strategy identified 10 311 unique studies, which were screened. 42 were reviewed in full text and 11 were included in the final review. Six studies contained data on inequalities of life expectancy or mortality, four on disease-specific mortality, three on infant mortality and three on morbidities. Early government reports suggested that inequalities in life expectancy and infant mortality had increased. However, later publications using more accurate data and more appropriate measures found that absolute and relative inequalities had decreased throughout the strategy period for both measures. Three of four studies found a narrowing of inequalities in all-cause mortality. Absolute inequalities in mortality due to cancer and cardiovascular disease decreased, but relative inequalities increased. There was a lack of change, or widening of inequalities in mental health, self-reported health, health-related quality of life and long-term conditions.
Conclusions
With respect to its aims, the strategy was broadly successful. Policymakers should take courage that progress on health inequalities is achievable with long-term, multiagency, cross-government action.
Trial registration number
This study was registered in PROSPERO (CRD42021285770).
Strengths and limitations of this study
- This is the first study to synthesise all published studies and grey literature on the health inequalities strategy conducted in England from 1999 to 2010.
- This study used a broad search strategy of peer-reviewed and grey literature.
- The retrospective nature of studies and lack of counterfactual means that causal claims as to the effect of the strategy cannot easily be made. This resulted in an increased risk of bias of studies.
Introduction
The pandemic has exacerbated societal health inequalities, with higher numbers of COVID-19 related cases and deaths in areas of higher socioeconomic disadvantage and among minority ethnic groups. 1 2 In England, the COVID-19 mortality rate for those under 65 was 3.7× greater in the most deprived 10% of local areas compared with the least deprived. Age-standardised COVID-19 mortality rates were more than twice as high in the most deprived 10% of areas compared with the least. 2
Knowledge of the existence of health inequalities is not new. The first major UK publication describing health inequalities was the Black report in 1980, although health inequalities had been described and debated in the academic literature for decades before that. It was not until 1997, with a newly elected government, that health inequalities became a policy priority. The government commissioned a health inequalities review, subsequently published in 1998 as the Acheson report, and committed itself to implement the evidence-based policy recommendations. 3 Subsequently, a wide-ranging national health inequalities strategy was implemented, with various strategies and aims updated over time. This was the first and most extensive international attempt to address health inequalities through a widespread programme of cross-government action.
Two national documents set out the health inequalities strategy. First, ‘Reducing health inequalities: an action report’ was published in 1999 in response to the Acheson report. It described a wide variety of policies designed to reduce health inequalities: both more ‘downstream’ initiatives, such as increased National Health Service (NHS) funding or the establishment of a National Institute for Clinical Excellence, and more ‘upstream’ policies, such as a national minimum wage, the new deal for employment and increased funding for schools, housing and transport. 4 Second, ‘Tackling health inequalities: a Program for Action’ was published in 2003. 5 It set out 82 cross-departmental commitments, along with 12 headline indicators of the key areas to be monitored. Again, these commitments included a range of ‘upstream’ and ‘downstream’ policies. Other studies have previously summarised the strategy. 6–8 The strategy involved a wide range of policy actions across different sectors. These included large increases in levels of public spending on a range of social programmes (such as the introduction of the Child Tax Credit; SureStart Children’s Centres), the introduction of the national minimum wage, area-based interventions such as the Health Action Zones and Neighbourhood Renewal funds and a substantial increase in expenditure on the NHS. The latter was targeted at more deprived neighbourhoods when, after 2001, a ‘health inequalities weighting’ was added to the way in which NHS funds were geographically distributed, so that areas of higher deprivation received more funds per head to reflect higher health need. 9
The programme for action included two national targets: (1) by 2010, to reduce by at least 10% the gap in infant mortality between routine and manual groups and the population as a whole and (2) by 2010, to reduce by at least 10% the gap between the fifth of areas with the lowest life expectancy at birth and the population as a whole. The ‘areas with the lowest life expectancy at birth and the population as a whole’ were defined by later documents as the ‘Spearhead areas’. 10–12 These 70 local authority areas were identified as being the worst performing local authorities associated with three or more of: male and female life expectancy at birth, cancer and cardiovascular disease mortality rates for the under 75s and Index of Multiple Deprivation (IMD) 2004 scores. These targets were based on relative, rather than absolute, inequalities. 12 13 This is important as debate exists as to which of these is the most appropriate measure of inequality. 3 14 15 Absolute inequalities measure the numerical gap between groups, while relative inequalities measure the percentage difference between groups.
One major criticism of health inequalities research and policy is that there has been too much effort put into describing the problem, rather than finding solutions. The National Health Inequalities Strategy in England 1999–2010 provides a key international example of the latter. It is a high-profile international case study of long term multifaceted government action. Discussions to date of the effects of the strategy have been polarised, with some prominent commentators arguing that it failed, 8 while others have asserted that it was effective. 16 17 This is partly because early evaluations of this health inequalities strategy suggested that it had failed to reach its targets and that inequalities may have increased during this period. 8 10 16 18 However, subsequent research found that this period was associated with a reduction in health inequalities. 6 9 19–21 As governments around the world consider how to respond to inequalities compounded by the pandemic, here we present a systematic review of the studies assessing the effectiveness of this health inequalities strategy.
This systematic review was conducted in accordance with established methodology 22 and reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. 23 This systematic review was registered with PROSPERO (CRD42021285770).
Search strategy and selection criteria
Three electronic databases (Ovid Medline, Ovid Embase and Ebsco PsycINFO) were systematically searched from January 1999 to November 2021. The search terms were based in part on previous literature, which identified key search terms to identify studies investigating inequality and inequity 24 and the UK. 25 Online supplemental table 1 presents the search terms. After removing duplicate records, abstracts and titles were screened according to the eligibility criteria by two researchers (IH and AS) using the software Rayyan by December 2021. Discrepancies were resolved by a third researcher (JAF). Each researcher cross screened 20% of the abstracts and titles of the other to ensure accuracy. Three conflicts arose, which were resolved after discussion. A detailed grey literature search of the UK Government Web Archives, specific websites (such as the King’s Fund) and a broad search using an internet search engine (Google) was used. Relevant citations of included studies were also screened.
Supplementary data
Inclusion criteria were:
- Studies assessing the impact of the health inequalities strategy in England between 1999 and 2010 on inequality in health outcomes in England.
- Any form of quantitative study.
- Studies reporting primary research.
- Studies in any language.
Exclusion criteria were:
- Studies whose methodology make it impossible to draw conclusions about the impact of the strategy.
- Studies that reported non-health inequalities.
- Earlier editions of included reports.
The full text of all articles screened as meeting the eligibility criteria or possibly meeting the criteria were reviewed. The following information was independently extracted from each study by two authors (IH and AV): first author, year of publication, aim, design, data sources, time period of analysis, population, health inequalities measured, main findings and risk of bias. The main outcomes of interest were absolute or relative changes in socioeconomic inequalities in life expectancy and infant mortality in the population of England between 1999 and 2010 to reflect the aims of the strategy. All results compatible with each outcome domain were sought from each study. Secondary outcomes included changes to socioeconomic inequalities in mortality, comorbidities or self-reported health.
Quality assessment
Risk of bias was assessed at a study level using the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool, which assesses the risk of bias across seven domains. One author (IH) undertook the risk of bias assessment, and this was double checked by a second author (AS or AV) with disagreements resolved by a third (JAF).
Patient and public involvement
Patients were not involved in the design or execution of this study. Nor were members of the public.
Due to the small number of studies with a large amount of data heterogeneity, it was deemed inappropriate to perform a meta-analysis. Instead, studies were synthesised narratively.
After removal of duplicates, the search identified 10 311 unique records. Forty-two were reviewed in full text, and 11 were included in the final review. A flow diagram of the screening and selection process can be found in figure 1 . Six studies contained data on inequalities of life expectancy or mortality, 6 7 9 10 12 19 three on disease-specific mortality, 10 12 26 three on infant mortality 10 13 21 and three on morbidities. 7 20 27 Six studies investigated geographical health inequalities, four investigated health inequalities at an individual level and one had statistics from both measures. Measures of socioeconomic status included income, living in a spearhead area, deprivation, occupation, social class and education. Data were collected between 1983 and 2017 ( table 1 ). Results from these papers are summarised in table 2 . Table 3 shows the risk of bias of each study across seven domains.
Study characteristics
ONS, Office for National Statistics.
Study findings
Risk of bias – ROBINS-I tool
NI, No Information; ROBINS-I, Risk of Bias in Non-randomized Studies of Interventions.

Study selection process.
Life expectancy, all-cause mortality and disease-specific mortality
Six studies reported data on life expectancy or mortality. Two earlier studies reported a widening of inequalities in life expectancy with one showing narrowing of mortality inequalities. The four more recent studies showed a narrowing of inequalities.
Two early government reports showed widening of life expectancy inequalities and mixed results for mortality inequalities. ‘Tackling Health Inequalities: 2007 Status Report on the Programme for Action’ used Office for National Statistics (ONS) data based on life estimates made using the 2006 census. It compared life expectancy in spearhead areas and the rest of the country. While life expectancy had increased for both spearhead and non-spearhead areas, absolute and relative inequalities between them had increased between 1995–1997 and 2004–2006. 10 The second reported ONS data up to and including 2010. 12 Compared with the 1995–1997 baseline, the absolute and relative gap in life expectancy between spearhead areas and England as a whole increased by 2008–2010.
Four later published studies found that inequalities had narrowed. The first study by Barr and colleagues 9 compared individuals living in the fifth most deprived areas to those living in the fifth least deprived areas. The authors found that inequalities of healthcare amenable mortality, defined as mortality from causes that would be prevented provided appropriate access to high-quality healthcare, narrowed between 2001 and 2011. Absolute inequalities for men and women fell with 85% of the change explained by redistributive resource allocation changes between areas. The relative gap narrowed for males and females. However, the authors found that absolute or relative inequalities of mortality not amenable to healthcare failed to change noticeably between 2001 and 2011. 9
The second study by Barr and colleagues 6 investigated geographical inequalities between 1983 and 2015 using ONS data based on the 2011 census, rather than 2006, which informed earlier government publications. They analysed trends in the absolute difference of life expectancy and mortality in the 20% most deprived local authorities compared with the rest of England. Supplementary analysis compared life expectancy in spearhead and non-spearhead areas. The authors identified breakpoints to account for the lag between implementation and outcomes. Both socioeconomic inequalities and inequalities between spearhead and non-spearhead areas in life expectancy for men and women statistically significantly increased year-on-year before the strategy and decreased during the time of the strategy, with no evidence that this decrease continued after the strategy. Relative socioeconomic inequalities in mortality fell year-on-year throughout the strategy for both men and women and increased before and after the strategy for men. Further analysis showed that the gap in life expectancy between spearhead areas and the rest of the country did not decrease until after 2005. Relative socioeconomic inequalities in life expectancy widened before and after the strategy period and narrowed during it. The authors found that using population estimates using the 2006 census caused an artificial increase in life expectancy inequalities compared with 2011 estimates.
Hu and colleagues 7 compared data from the health survey for England to similar surveys done in other European countries. They investigated trends in inequalities of all-cause mortality between those with high (tertiary) education and the rest of the country. The gap narrowed more significantly in 2000–2010 compared with 1990–2000 in England.
While aforementioned studies, analysing differences between the most and least deprived areas, are important concerning the strategies aims, they fail to describe the change in the social gradient across the whole of the population. Buck and Maguire 19 examined the relationship between area-based income deprivation and life expectancy, comparing data from 1999 to 2003 to 2006–2010. The authors found improved life expectancy for all levels of deprivation but a greater improvement in more deprived areas. It was noted that both unemployment and older people’s deprivation played a particularly important role in determining differences in life expectancy between areas.
Three studies reported changes in inequalities in disease-specific mortality. Two government documents examined inequalities in mortality due to cancer between spearhead areas and England as a whole from 1995 to 1997 to 2006–2008 and 2008–2010 using ONS data. By 2006–2008, absolute inequalities fell, without a change in relative inequalities. 10 By 2010, the absolute gap had fallen further, with an increase in the relative gap. 12 Absolute inequalities in mortality due to circulatory disease decreased by 2006–2008, but relative inequalities widened. By 2008–2010, there was a further decrease in absolute but an increase in relative inequalities. Exarchakou and colleagues 26 reported inequalities of 1-year survival rate following a diagnosis of one of the 24 most common cancers between 1996 and 2013. They investigated the absolute difference between individuals living in the fifth most and fifth least deprived areas. The gap narrowed in only 6 of 20 cancers in men and 2 of 21 cancers in women and widened for three cancers (two in women and one in men). One final study examined inequalities in road accident causality in the fifth most deprived local authority districts areas compared with England as a whole. 10 The absolute gap decreased between 1998 and 2006.
Infant mortality
Three studies reported changes in the infant mortality rate. Initial reporting using ONS data from 2004 to 2006 found that inequalities had widened between routine plus manual groups and the population as a whole compared with the 1997–1999 baseline. 10 A later report found that by 2008–2010, inequalities had narrowed compared with the baseline. 13 Robinson and colleagues 21 calculated the infant mortality rate in 323 lower tier local authorities between 1983 and 2017 to investigate changes in inequalities between the 20% most deprived areas and the rest of the country. Absolute inequality increased year on year before the strategy and decreased during it. A non-significant increase was seen after the strategy ended. Relative inequalities marginally decreased during the time of the strategy, in contrast to an increase that was seen before and after the strategy period.
Morbidities
Three studies reported on morbidities using Health Survey of England data. Specifically, these studies investigated self-assessed health, health-related quality of life, mental health and long-term health. The Health Survey of England contains data collected from a nationally representative sample of those residing at private residential addresses and has been carried out since 1991. 28 Around 8000 adults and 2000 children take part in the survey each year.
Mixed results were found concerning self-reported health. Between 1996 and 2009, the probability of reporting bad or very bad health remained relatively constant for those in the highest social class but increased for those in lower social classes. 27 When comparing those with high and low education, there was no significant difference in inequality trends between 2000 and 2010 compared with 1990–2000. Additionally, there was no significant difference in the change of these trends between these periods compared with three European countries. 7 Costa Font and colleagues 20 measured inequalities in self-reported health using concentration indices, whereby a high result indicates more inequality. Equalised household income was used to measure inequality across the whole population. In contrast to the two aforementioned studies, they reported a fall in the concentration index between 1997 and 2007, indicating a reduction in inequality.
Health-related quality of life did not change between social classes from 1996 to 2008. 27 When assessed by a concentration index comparing different household incomes, inequalities of long-term health problems increased between 1997 and 2007. 20 There was no significant change in the trend of inequalities of long-term health problems by education in 2000–2010 compared with 1990–2000. Nor was there a significant difference in the change in trend in England compared with three European countries. 7 While mental health improved in all social classes between 1997 and 2009, it did so more for individuals in higher social classes. 27
Principle findings
There is evidence that the strategy met the infant mortality target, while the life expectancy target was reached for men but not women. Absolute health inequalities in life expectancy, mortality, infant mortality and multiple major causes of death reduced. Less evidence is available concerning relative inequalities. More recent data suggest that relative socioeconomic inequalities in life expectancy and infant mortality narrowed. Relative inequalities of mortality narrowed between the fifth most deprived areas and the country as a whole, but not between the fifth most and fifth least deprived areas. The only data available on disease-specific conditions suggest an increase in relative inequalities. This may be due to a lack of newly published studies, using more recent census data and sampling from the later years of the strategy being available as it is for life expectancy and infant mortality. The difference may also be due to the statistical relationship whereby relative inequalities may increase as a result of a fall in absolute inequalities. 29 30 There was a lack of change or worsening of change for inequalities in mental health, health-related quality of life and long-term conditions. This lack of change or increased inequality for self-reported health measures may be due to multiple reasons. As all studies used the same survey, with data collected shortly after the 2008 financial crash, perceptions of economic security may have altered results. It may be that self-reported measures are more resilient to change. Alternatively, small changes in categorically assessed self-assessed measures may be less easily observed compared with life expectancy and infant mortality that are continuous measures. Health inequalities were found to have narrowed more consistently when measured between geographical areas rather than between individuals. This may be due to longer follow-up periods in many of the studies that were measured at a geographical level, extending beyond the immediate aftermath of the banking crises. Alternatively, it could have been caused by the redistributive resource allocation changes that occurred between areas. 9
Strengths and limitations
This is the first study to collate and synthesise all evidence of the first international attempt at a cross-government strategy to address health inequalities. We used an extensive search strategy with robust screening, data extraction and quality assessment processes. We included peer-reviewed articles and grey literature, including documents published at the time and identified through the UK government archives.
The main limitation is that the studies included are retrospective using either time-trend or before and after methods. All of the studies have a high risk of bias due to deviations from intended interventions. This was predominantly because of the lack of a robust counterfactual that makes it difficult to unpick the impact of the strategy against the impact of other factors, such as broad economic growth before the financial crash in 2008. These limitations are common to any attempt to assess the impact of national policy; however, considering the breadth and ambition of the strategy it is disappointing that more comprehensive evaluations or data are not available. The strategy’s wide-ranging nature does however allow many of these factors to be considered a part of it rather than as a confounding factor. For example, the large decrease in poverty rates, especially in children 31 and pensioners, 32 may both have contributed. Additionally, not every abstract was double screened. However, 40% of abstracts were cross checked to ensure consistency, and only three discrepancies arose, none of which were included in the review.
The included articles use different measures that make direct comparisons impossible, for example, comparing the most deprived areas to either the least deprived areas or the rest of the population and using individual-level measures of socio-economic status (eg, occupation) or area-based measures (eg, IMD). Morbidity data are based on self-reported measures within a nationally representative survey, rather than chronic disease registers.
As indicated by guidance, absolute and relative inequalities were included. 14 33 This aligns with existing guidance and debate both from those who argue that absolute inequalities are the more important measure for policymakers 3 and others who support the idea that relative inequalities are also of significant importance. 34
What this research means
A lack of progress on health inequalities, despite policy priority, can lead to a sense of fatalism and powerlessness to effect change. These findings are therefore important because they show that with sustained cross-government action, progress on health inequalities is possible. It is particularly encouraging that improvements were made in both of the areas that the strategy predominantly set out to improve: inequalities in life expectancy and infant mortality.
These results are even more encouraging when considering that they came from a strategy that was far from perfect. Critics have noted various points about the strategy, for example, that it was insufficiently based on reliable evidence, 8 18 35 36 flawed in delivery, 8 16 18 insufficiently focused on the wider determinants of health 16 34 37 and that efforts may not have been large enough. 8 34 38
Earlier findings consistently showed no improvement in life expectancy inequalities, yet later results were more positive. This may be due to a lag period between the implementation of the strategy of interventions and changes in health outcomes. Certain initiatives would take considerably longer to impact inequalities in life expectancy, such as reducing childhood poverty, compared with more downstream factors, such as blood pressure control. Alternatively, it may be due to more accurate and up-to-date data, such as the 2011 census. Importantly, this shows that sufficient time is needed between implementation and measuring outcomes.
Implications for policy and research
Governments around the world are taking steps to address health inequalities, particularly in light of the growing evidence of an unequal pandemic. 39 For example, the UK government has committed to a programme of ‘levelling up’ regional inequalities and setting out new legislation to address health inequalities. This review suggests that it is possible to reduce health inequalities through long-term cross-government action, which was wide reaching both in terms of government departments and across the life course. Most encouragingly with respect to current government aims, geographical health inequalities especially narrowed. The strategy was supported by significant increases in both funding and reform of public services, of which only one has continued. Since the end of the strategy period, public services internationally, but particularly in the UK, have experienced reduced funding as a result of austerity policies from 2010 onwards. In the UK, this has particularly impacted on local authorities, social security, children’s services and, until the pandemic, to the NHS. Indeed, there is evidence that from 2010 onwards (and before the unequal impact of the pandemic) the improvements in health inequalities under the English strategy have reversed with, for example, increasing inequalities in infant mortality rates 40 and falling life expectancy in the most deprived areas. 41 Considerable investments in these services would be necessary to recreate a proactive attempt to tackle the social determinants of health inequalities.
The strategy used relative measures of inequality. Absolute measures are easier to change, making them appealing to policymakers as progress can be more easily proven. The goals were based on long-term changes in life expectancy and infant mortality rather than shorter term changes in measures such as blood pressure and heart rate. These were appropriate for the strategy given the wide-ranging, cross-departmental approach that aimed to target determinants of ill health. The fact that long-term, ambitious health inequalities targets require a cross-departmental approach can be of benefit to policy makers. They can provide rationale and strengthen the argument for a wide range of potentially transformative policies that may otherwise fail to be enacted due to a lack of political support. Goals were based on changes between the most and least deprived areas, rather than changes in the societal gradient in health. This again would be an easier target for policymakers to achieve. The government’s current targets, through the ‘levelling up’ programme are less ambitious than the strategy’s. 42 Only an absolute narrowing in life expectancy and well-being is aimed for, rather than the 10% change targeted by the strategy. Additionally, the absolute gap in life expectancy by area is measured between the top and bottom 10% rather than 20%.
Arguably more policy priority should have been given to reducing the gap in morbidities as the data fail to show a convincing narrowing of inequalities of self-reported health, mental health, health-related quality of life and long-term conditions.
More research is needed to unpick the active ingredients and exact initiatives that were most effective during the strategy. This should start with a more detailed understanding of which diseases drove the reduction in life expectancy and a broader understanding of how the wider determinants of health such as housing, income and education may have impacted changes in infant mortality, mortality and life expectancy.
In summary, this review found some evidence that the 1999–2010 cross-government health inequalities strategy led to a reduction in the absolute inequalities in life expectancy, mortality, infant mortality and major causes of death. While the impact on relative inequalities is less clear, there seemed to be a narrowing of relative inequalities in at least life expectancy and infant mortality. The national targets relating to life expectancy were met for men, but not women, and were achieved for infant mortality. Policymakers should take courage that progress on health inequalities is achievable with long-term, multiagency, cross-government action. These findings are especially pertinent at present times whereby many governments are aiming to use postpandemic recovery as an opportunity to build back better.
Supplementary Material
Twitter: @ilk21
Contributors: JAF conceptualised the study. JAF and IH drafted the protocol, and IK and AV provided comments. IK developed the searches with the support of IH and JAF. IH and AS screened the titles and abstract and were supported by JAF. IH and JF screened the full text articles. IH, AS and AV extracted and checked the extraction. IH wrote the first draft of the manuscript. JAF, IK, CB, AS and AV redrafted. All authors approved the final version. JAF is the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Ethics statements, patient consent for publication.
Not applicable.

IMAGES
VIDEO
COMMENTS
Eliminating racial health inequities requires a movement away from disparities as the focus of research and toward a research agenda centered on achieving equity by dismantling structural racism.
Dental public health. At least 80 people died in the recent Grenfell Tower fire in Kensington and Chelsea, West London. This incident has provoked much anger, debate and reflection on how such a ...
In response to the pandemic, the need for studies focused on racial inequity in health in the US and UK has been highlighted (Bhala et al., 2020), suggesting that COVID-19 may represent a force capable of more closely uniting 'health inequalities' and 'health disparities' scholarship. However, while this study supplies an atlas for ...
In order to help accomplish this task successfully, the objective of this study is to perform a systematic review of the most common topics and indicators used for measuring and monitoring health inequalities in the reports, projects, and databases of international, national, and regional governmental organizations.
In this essay, we focus on the potential and promise that intersectionality holds as a lens for studying the social determinants of health, reducing health disparities, and promoting health equity and social justice. Research that engages intersectionality as a guiding conceptual, methodological, and praxis-oriented framework is focused on power dynamics, specifically the relationships between ...
We will likely look back on 2020 as a turning point. The pandemic put a spotlight on existing societal issues, accelerated the pace of change in others, and created some new ones too. For example, concerns about inequalities in health by income and race are not new, but they became more apparent to a larger number of people during 2020. The speed and starkness of broadening societal ...
But the racial health gap has remained, according to a series of studies published on Tuesday in the journal JAMA. A dismal picture of persistent health disparities in America was described in an ...
Evidence on health inequalities has been growing over the past few decades, yet the capacity to produce research on health inequalities varies between countries worldwide and needs to be strengthened. ... We conducted a realist explanatory case study, which included 12 semi-structured interviews, to test six theoretical mechanisms that we ...
Health inequities exist within and between societies at different hierarchical levels. Despite overall improvements in health status in European Union countries, disparities persist among socially, economically, and societally disadvantaged individuals. This study aims to develop a holistic model of health determinants, examining the complex relationship between various determinants of health ...
These case studies showcase good practice in meeting the needs of under-served groups and delivering quality care to service users who may be particularly vulnerable to health inequalities. The case studies illustrate successful examples of speech and language therapy practice, but it should be noted that each service user is an individual and ...
As a result, Public Health England commissioned the Due North Report which outlined new approaches in tackling health inequalities. This second paper outlines what has been learnt in five years as a case study. This includes influencing devolution deals and new elected city mayors, planning for economic growth in deprived areas and developing ...
Here we explore the definition and application of health inequality terminology using the setting of English local commissioning as a case study, exploring LAs', CCGs', and ICSs' mandated duty or obligation to consider or act upon inequalities in their commissioning decisions, their potential resources for quantifying their jurisdiction ...
A health care disparity typically refers to differences between groups in health insurance coverage, affordability, access to and use of care, and quality of care. The terms "health inequality ...
The Due North Report and initial work were described as a case study in this journal in 2015. 5 In response to the national and international interest, this second paper describes what has happened since, with learning and growing points and further action needed. Trends in health inequalities
Health inequalities case studies. Access our library of case studies sharing innovative work underway across the sector to tackle health inequalities. 21 February 2023. To realise a step change in health and wellbeing, systems will need to adopt new approaches to health inequalities as well as wider inequalities in society.
Framing inequalities to ensure a systematic and logical approach in health systems. Framing is a way of structuring or presenting a problem and can be helpful, potentially vitally so, to ensuring action. 36 How we discuss and present inequalities must be developed with and for any audience it is hoped might contribute to effective changes; for example, NHS staff are more likely to engage if ...
24 per cent of Bangladeshi households living in crowded accommodation compared to two per cent of White British. These case studies demonstrate how local government is at the heart of addressing the health inequalities that are having a detrimental impact on ethnic minorities. They form part of the health inequalities hub, which is funded by UK ...
Health inequalities case studies. Social and economic inequalities have a significant impact on children's health outcomes. We are showcasing projects that are working to address health inequalities. These provide you as paediatricians with best practice examples of initiatives you might be able to replicate or implement in your local area.
The Equality and Health Inequalities Hub; Case studies; How Lambeth is closing the health inequality gap for Black and minority ethnic patients with high blood pressure. How entrepreneurship in the NHS is helping to narrow healthcare inequalities.
Reducing health inequalities means giving everyone the same opportunities to lead a healthy life, no matter where they live or who they are. Wider action on prevention will help people stay healthy and also moderate demand on the health and care service. Integrated care systems provide stronger foundations for working with local government and ...
The Equality and Health Inequalities Hub; Case studies; Reducing healthcare inequalities using population health management; Reducing healthcare inequalities using population health management. Over 10,000 people at high risk of health deterioration have been identified for extra help and support to stay well and independent thanks to the ...
NEW YORK, GENEVA, 28 May 2024 - Around the world, menstrual health and hygiene needs are being overlooked due to limited access to information, education, products and services, as well as inadequate facilities and inequalities. A new report, Progress on drinking water, sanitation, and hygiene in schools 2015-2023: special focus on menstrual health, launched by UNICEF and WHO on Menstrual ...
A case-control study design was applied, and a snowball approach was used to enrol volunteered participants aged between 6 and 36 months of age, through a Google survey. We used the Brief Infant-Toddler Social and Emotional Assessment (BITSEA) questionnaire to assess children's SEB problems and a Brief Symptom Inventory (BSI) to evaluate the ...
Motivation for studying health inequalities. Despite considerable attention to the problem of health inequalities since the 1980s (), striking differences in health still exist among and within countries today ().In 2010, for example, Haitian men had a healthy life expectancy of 27.8 years, while men in Japan could expect 70.6 years, over twice as long, in full health ().
This editorial seeks to shine a spotlight on maternal inequalities, which will feature in our blog posts from the end of May for a few weeks. Undoubtedly, this is a broad and complex topic and, so our spotlight will take a view on how we might work towards positive change. Partly inspired by the plan-do-study-act cycle approach,1 which is often used to provide a structure for working ...
The events marked the release of, Adolescents in a changing world - The case for urgent investment, a landmark report which finds that failure by stakeholders to increase investments in programmes targeted at improving adolescent well-being would result in staggering social and economic costs.The report, commissioned by PMNCH, working with Victoria Institute of Strategic Economic Studies ...
"The impact on health systems and global inequality will be huge." New study raises concerns as health threat targeting older people expected to double in coming decades: 'This is a question of ...
It is a high-profile international case study of long term multifaceted government action. ... Health inequalities were found to have narrowed more consistently when measured between geographical areas rather than between individuals. This may be due to longer follow-up periods in many of the studies that were measured at a geographical level ...
Health Science Reports is a broad scope journal covering all medical and health sciences disciplines, including clinical care, ... This case-control study enrolled 41 children and adolescents (aged 8-18 years) with asthma and their age and gender-matched controls in 2019-2020. Serum Calcium, phosphate, vitamin D, and bone mineral density ...